Abstract
Background
Despite consistent reporting of high fertility levels in Nigeria, contraceptive prevalence rates remain low. Information on the type of contraceptive uptake among women who visit family planning (FP) clinics is still sketchy in Ibadan. Therefore, we assessed the trend and pattern of contraceptive use among women attending a FP clinic at a tertiary health facility in Ibadan.
Methods
A mixed-method design was adopted for the study. Records of women (n = 1,619) who accessed FP services at the University College Hospital [UCH] from 2018 to 2022 were reviewed. The qualitative data included a key informant interview (KII) involving a senior officer of the FP Clinic and a focus group discussion (FGD) among high-fertility (≥ 4 living children) women. Data were analysed using a logistic regression model (α0.05), and thematic analysis was used for the qualitative part of the study.
Results
The mean age of women was 33.8 ± 6.34 years, 87.7% were in monogamous marriages, 82.3% were Yoruba, and 47.2% did not intend to bear more children. The uptake of long-term and short-term contraceptive methods showed a declining (slope = -3.5) and increasing (slope = + 4.4) trend, respectively. The likelihood of non-use of a long-term contraceptive method was lower among women with ≥ 3 surviving children who had tertiary education (uOR = 0.539, 95% C.I = 0.338–0.859, p = 0.009) and were Christians (uOR = 0.410, 95% C.I = 0.258–0.652, p < 0.001) compared to their counterparts with at most secondary education and were Muslims, respectively. High fertility women who are not using Long-acting reversible contraceptive methods (LACMs) identified fear, partner’s influence, misconceptions, cost, parity, privacy, and inconvenience as reasons for the non-use of the methods.
Conclusions
Conceptive uptake at the UCH followed an increasing trend from 2018 to 2022. Sensitisation on the adoption of LACMs among high-fertility women might improve the use of such methods in the study area.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-23284-0.
Keywords: Contraceptive use, Long-acting contraceptive methods, Short-acting methods, University College Hospital
Background
Fertility is one of the key drivers of population change and its level is among the metrics often used as health indicators in any nation. Nigeria’s Total Fertility Rate (TFR = 5.4) is one of the highest, worldwide [44]. If the expected reduction in the world fertility rate is achieved by 2050, Nigeria’s fertility dynamics will be important to that change. The 1994 International Conference on Population and Development (ICPD), the 2015 Sustainable Development Goals (SDGs), the 2063 African Agenda, and the 8-point reform agenda of the Federal Republic of Nigeria underscore the need for population control and improving the individual’s well-being through the reduction of the accelerated population growth rate. One of the requirements for that change will be to increase the contraceptive prevalence rate among women aged 15–49 years in Nigeria. Regrettably, different family planning interventions and policies instituted in Nigeria are yet to translate to a high contraceptive prevalence rate (CPR) as observed in some sub-Saharan African countries like Malawi (66%), Kenya (65%), Rwanda (64%), Cabo Verde (56%), and South Africa (55%), but in Nigeria the CPR remains 17% [44]. The demand-side deficits for contraceptive use in Nigeria undermine the government’s interventions to control the fertility rate and population growth [17, 39].
The desire for pregnancy and side effects such as breast tenderness, headache, amenorrhoea, weight gain, infrequent or prolonged bleeding, spotting, and menorrhagia were identified to be the major barriers to the use of the long-acting contraceptives in Ethiopia, Uganda, and Nigeria [13, 13, 39]. However, Thanel et al. [26] argued that long-acting contraceptive methods (LACMs) offered more effectiveness in pregnancy prevention, with higher continuation rates and rapid return to fertility compared to short-acting contraceptive methods [SACMs]. Sambah et al. [22] suggested that adolescent girls and young women with at least one birth were more likely to use LACMs than women without children in sub-Saharan Africa [SSA]. Studies admit that LACMs use may increase with an increase in the number of births in which parity significantly impacted women’s fertility behaviours in Kenya, Uganda, and 26 other SSA countries [18, 18, 25, 37].
Studies are limited on factors influencing the non-use of LACMs amongst highly fertile women (women with at least 4 children) in Nigeria. LACMs uptake in Nigeria is low but there is limited evidence of how women’s preferences influence their choices [3]. Previous studies in Nigeria were either community-based or focused on the general population of women of reproductive age [3, 36]. Arguably, an increase in the number of fecund women with more than 4 living births may contribute to Nigeria’s high TFR, found that contraceptive-type use was a factor in the inability to achieve the Nigeria Population Policy 1988 standard of 4 living births per woman/family.
Behavioural theories explain women’s motivation for contraceptive use and the choice of type. Williams et al. [27] theorised that women make decisions regarding contraceptives choices that reflect their needs and preferences. Ajzen [42] planned behaviour theory suggests that individuals’ decision to adopt specific behaviours are based on their perceived benefit. Accordingly, the behavioural construct is expected to be influenced by individuals' attitudes, subjective norms, and perceived behavioural control [42]. This theory has been expanded by other researchers and concisely applied to contraceptive choices and use. Montano and Kasprzyk [29] opined that women’s contraceptive use intention and utilisation are often motivated by the premise that the outcome would be beneficial to their health, people’s expectation about the outcome of use, and the perceived behavioural control concerning its drivers and barriers. DeMaria et al., [9] observed that women using other modern contraceptive types adopt the use of long-acting methods by leveraging on the experience of their relatives or friends who have previously used the specific product. This implies that greater attitudes to long-acting methods will likely lead to greater information-seeking. Thus, this approach explains the impact of contraceptive use intention in overcoming the subjective norms or perceived threats to adopting the long-acting method [35]. However, behavioural influence on the use of the long-acting methods could change when women are exposed to divergent subjective norms and sensitisation on the benefits of using the methods, particularly among fecund high-fertility women.
The foundation of this mixed-method study was that high-fertility women are expected to use long-acting rather than short-acting methods. Previous studies have established that long-acting methods are more protective against unwanted pregnancy than short-acting methods which have higher failure rates [31, 46]. Therefore, this study was designed to assess the type of modern contraceptives used among women attending a family planning clinic at the University College Hospital, Ibadan from 2018 to 2022. The specific objectives were to,examine the trends in contraceptive use among women; identify the factors influencing the use of long-acting methods among high-fertility women; and explore the reasons for the non-use of long-term methods among high-fertility women accessing FP services at the University College Hospital. Therefore, findings from this study are expected to assist in policy formulation and inform factor-specific interventions on how to encourage high-fertility women to use long-acting contraceptive methods. Drawing inferences from the characteristics and experience of women using FP services at UCH, Ibadan being one of the leading tertiary health facilities in Nigeria might help in the development of relevant strategies that can facilitate the use of long-acting contraceptives, most especially among high fertility women in Nigeria.
Methods
The study setting
The University College Hospital (UCH), strategically located in Ibadan, was established in 1952 to train medical personnel and other healthcare professionals in Nigeria and the West African sub-Region. The hospital and the University of Ibadan function in excellent symbiosis in the areas of health workforce training, research, and clinical service. The UCH provides services for undergraduate and postgraduate residency training programmes in all specialties. Although the hospital is a tertiary institution with a focus on clinical and research services, it provides primary and secondary care services to patients. The Hospital enjoys wide patronage from both national and international clients. The UCH Fertility Research Centre is the pioneer of reproductive health research in Nigeria offering contraceptive services such as counselling, insertion of intra-uterine contraceptive devices (IUCDs) and implants, Bilateral Tubal Ligation (BTL), and vasectomy.
Study design and population
A mixed-method (quantitative and qualitative) approach was adopted for the study. The study population was women of reproductive age (15–49 years) who accessed family planning services in UCH over five years (2018–2022). The data extraction was limited to the year 2022, because complete data for the study was available till the end of 2022 at the time of implementing the study in July 2023. The quantitative arm of the study relied on the data extracted from the records of women who accessed FP services at the facility within the coverage period (2018–2022). The qualitative arm focused on 1 senior staff of the UCH Fertility Research Centre and the head of the FP unit with at least 5 years experience handling clients’ cases to explore his/her in-depth perspectives on FP services at the facility and also a Focused Group Discussion (FGD) was conducted among high fertility women currently accessing care at the unit.
Variable definition
The dependent variable was the use of LACMs. The independent variables available in the records were Demographic Characteristics (Age, age at marriage, marital status, number of marriages, number of siblings, and ethnicity), Socio-Economic Characteristics (level of education of women, level of education of husbands, occupation (for women and their husbands), monthly income (for women and their husbands), and religion), and Fertility-Related Characteristics (desire for more children, number of additional children desired, number of previous pregnancies, number of miscarriages, number of children alive, and number of children ever born.
Data collection
From the case file, 1,619 patients’ records were reviewed. For the FGD, a single group of 8 participants was selected from the strata of women with at least 4 living children using short-term methods. Hence, the recruitment of participants for the FGD was based on their knowledge, experience, and characteristics as applicable to this study. Also, 1 senior staff of the UCH Fertility Research Centre was involved in a key informant interview. The authors interviewed the assistant chief Nursing Officer of the facility. This Key Information Interview [KII] helped to leverage the experience and expertise of the senior staff in understanding the trends and issues around contraceptive choices by women accessing the FP clinic in the UCH, Ibadan. The FGD and KII questions were specifically designed for this study and have not been published elsewhere.
The FGD and KII were audio recorded and transcribed into text using Google Translate and manually reviewed to ensure consistency of translation. The KII took approximately 37.00 min while FGD took approximately 1 h 42 min. Data saturation was achieved across the interviews when no new information, themes, or ideas could be introduced thus avoiding repetition or data overload [38].
The inclusion criteria for KII included; (i) Being a senior FP provider at the facility (ii) Having a minimum of 5 years of experience (iii) Consent to being part of this study. The inclusion criteria for FGD included; (i) Being a woman of reproductive age using FP service at the facility (ii) Having 4 or more living births at the time of data collection (iii) Using a short-term method at the time of data collection (iv) Using the FP service at the facility for a minimum of 1 calendar year and (v) Consenting to be part of the study. The knowledge, experience and characteristics of participants helped to purposively identify and recruit them for this study [23]. The authors conducted KII while FGDs were conducted with the support of a senior FP service provider at the facility. The interview was conducted from 5 to 15th of April 2024 at the Family Planning Research Clinic, University College Hospital (UCH), Ibadan, Nigeria.
Data management
Excel worksheet was used to extract the quantitative data from the case files and the harvested data were exported to SPSS version 23.0 for further analysis. Chi-square model was used to examine the association between contraceptive use type and socioeconomic variables. The logistic regression analysis was used to identify factors influencing the use of long-term contraceptive methods, among high-fertility women accessing FP services at the UCH, Ibadan (α0.05). The NVivo software (version 11.0) was used for theme generation from the conducted FGD and IDI. The themes generated include factors for the use or non-use of modern contraceptive methods, Reasons for high fertility women using SARCs instead of LARCs, and others.
Ethical considerations
The approval to conduct this study was granted by the ethical committee, Institute for Advanced Medical Research and Training [IAMRAT], College of Medicine, University of Ibadan with approval number NHREC/05/012008a. Within the hospital system, the study received approval for data collection and patient access from the Department of Obstetrics and Gynaecology, Faculty of Clinical Sciences, College of Medicine, University of Ibadan. This approval was needed to access the Family Planning Research Unit where patients’ case files were accessed and a service provider and patients were accessed for a qualitative explorative study. For the qualitative part of the study, informed consent to participate was obtained from each participant before the commencement of the study. The respondents were informed that they would not be subjected to any form of harm and their involvement would not induce mental health risk on them. We ensured that the secondary data from the women’s case files were not commercialised or made accessible to unauthorised individuals who may use the information to the detriment of the women.
Results
The mean age of the women was 33.78 ± 6.34 years, 31.9% were in the age group 30–34 years, while 24.3%, 20.0%, and 11.6% were in the age group 35–39 years, 25–29 years, and 40–44 years respectively (Fig. 1).
Fig. 1.
Percentage distribution of women (%(n)) according to age group
Table 1 presents the percentage distribution of the women by the background characteristics. The majority of the women (94.7%) married at ages above 18 years, only 1.9% married at ages below 18 years, and 2.0% had been married at least twice. The women were predominantly Yoruba (82.3%), while 8.0% were Igbo and 9.7% belonged to other ethnic groups. According to the level of education of the women and their partners, a majority had tertiary education, 83.3% and 83.9%, respectively. The women were mostly Christians (79.4%), 19.0% Muslims, and 1.5% belonged to other religions. The data showed that most of the women (91.4%) and their husbands (86.7%) engaged in an occupation or the other. Among the 306 women where the information concerning their monthly income was available in their case file, 29.1%, 28.1% and 25.2% earned at least USD66.63, USD33.32—USD65.97 and less than USD19.99, respectively.
Table 1.
Percentage distribution of respondents by sociodemographic characteristics
| Variable | Frequency | Percentage |
|---|---|---|
| Age at Marriage | ||
| < 18 | 31 | 1.9 |
| 18 + | 1520 | 94.7 |
| Not Married | 55 | 3.4 |
| Marital Status | ||
| Single | 55 | 3.4 |
| Married | 1543 | 95.3 |
| Divorced/Separated | 15 | 0.9 |
| Widowed | 6 | 0.4 |
| Number of Marriages | ||
| None | 55 | 3.4 |
| One | 1532 | 94.6 |
| 2 + | 32 | 2.0 |
| Number of Siblings | ||
| 0 | 133 | 8.2 |
| 1 | 69 | 4.3 |
| 2–3 | 517 | 31.9 |
| 4 + | 900 | 55.6 |
| Ethnicity | ||
| Yoruba | 1333 | 823 |
| Igbo | 129 | 8.0 |
| Others | 157 | 9.7 |
| Education | ||
| At Most Secondary | 270 | 16.7 |
| Tertiary Education | 1349 | 83.3 |
| Partner’s Education | ||
| At Most Secondary | 261 | 16.1 |
| Tertiary Education | 1358 | 83.9 |
| Occupation | ||
| Not Working | 140 | 8.6 |
| Business/Self-Employed | 617 | 38.1 |
| Civil Servants | 166 | 10.3 |
| Private Organisations/Professionals | 490 | 30.3 |
| Health Workers | 206 | 12.7 |
| Partner’s Occupation | ||
| Student/Not Working | 216 | 13.3 |
| Business/Self-Employed | 467 | 28.8 |
| Civil Servants | 165 | 10.2 |
| Private Organisations/Professionals | 630 | 38.9 |
| Health Workers | 141 | 8.7 |
| Monthly Income | ||
| Less than $19.99 | 77 | 25.2 |
| $19.99—$32.65 | 54 | 17.6 |
| $33.32—$65.97 | 86 | 28.1 |
| ≥ $66.63 | 89 | 29.1 |
| Total | 306 | |
| Partner’s Monthly Income | ||
| Less than $19.99 | 20 | 9.2 |
| $19.99—$32.65 | 23 | 10.6 |
| $33.32—$65.97 | 59 | 27.2 |
| ≥ $66.63 and above | 115 | 53.0 |
| Total | 217 | |
| Religion | ||
| Christianity | 1286 | 79.4 |
| Islam | 309 | 19.1 |
| Others | 24 | 1.5 |
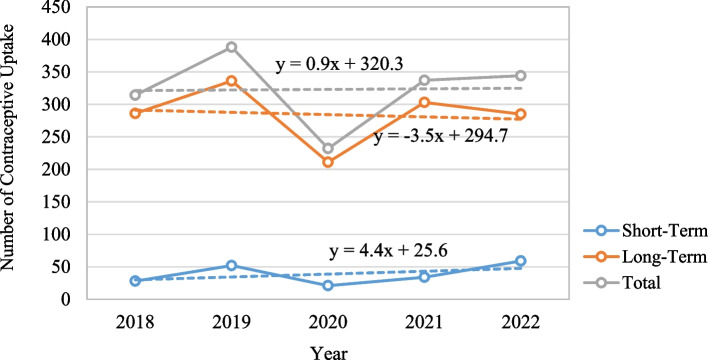
The data show the number of clients that accessed FP services at the health facility under investigation followed an increasing trend (β = + 0.9). The number increased from 314 in 2018 to 344 in 2022. However, the year 2019 (388 cases) recorded the highest number of clients across the 5 years, this dropped to 232 in the year 2020 during the COVID-19 era. Consistently, across the survey years, more women strikingly accessed the FP clinic for the uptake of a long-term method rather than a short-term method. At the clinic, the use of a long-term contraceptive method (β =—3.5) showed a declining trend, while an increasing trend was observed for the short-term (β = + 4.4) contraceptive methods (Fig. 2).
Fig. 2.
Trend in the uptake of contraceptives at the FP clinic UCH, Ibadan (2018–2022)
Figure 3 presents the distribution of women according to fertility-related characteristics. The data show that 51.0% of the women had no desire to give birth to more children, while 21.8% desired one more child, and 27.2% desired to bear at least two more children. The proportion of women who had not been pregnant was 4.5%. 47.9%, 41.4%, and 6.1% had been pregnant for 1–2, 3–4, and at least five times, respectively. The majority of the women (66.2%) had no miscarriages, 29.3% had experienced miscarriages 1–2 times, and 4.5% had miscarriages at least 5 times. The distribution of women by the number of children ever born revealed that 42.5% of the women had given birth to 3–4 children, while 17.0% and 37.0% had given birth to at least 5 children and 1–2 children respectively. About 5.2% of the women had no living children, while 49.8%, 40.2%, and 4.8% of the women had 1–2, 3–4, or at least 5 of their children alive respectively, at the time of reporting at the health facility.
Fig. 3.
Percentage distribution of women according to fertility-related characteristics
Across the period of review (2018–2022), 88.0% of women used long-term contraceptive methods. The use of long-term methods reduced from 91.1% in 2018 to 82.8% in 2022. However, the uptake of short-term contraceptive methods increased from 8.9% of the total contraceptive use in 2018 to 17.2% in 2022 (Fig. 4a). The use of long-term and short-term contraceptive methods was across different age groups (Fig. 4b). The highest proportion of women who used the long-acting method was found among women aged 25–29 years (90.7%) while the least was reported by women in the age group 15–24 years (81.3%).
Fig. 4.
a Percentage distribution of the type of method used by year. b Percentage distribution of the type of method used by age group
The distribution of women according to contraceptive type is presented in Table 2. The data showed that 87.8% of the women opted for a long-acting contraceptive method. The proportion of women who sought long-term contraceptive methods was higher among those who were Yoruba (87.7%) compared to those from other ethnic groups. The use of long-acting contraceptive methods was higher among women who had tertiary education (88.4%) compared with those who had at most secondary education (84.8%). The uptake of long-term contraceptive methods was highest among healthcare workers (93.2%) and women whose partners were healthcare workers (95.0%). The data is evident that the uptake of long-term contraceptive methods was higher among the Christians (89.3%) than the Muslims (81.2%). Of the women who used long-term contraceptive methods, 89.2% had no desire for more children, 83.6% desired one more children, and 88.4% desired 2 children or more.
Table 2.
Percentage Distribution of Women according to Contraceptive Method Type by Background Characteristics
| Background Characteristics | Contraceptive Method | Total | χ2-Statistic | P-value | |
|---|---|---|---|---|---|
| Short-Acting | Long-Acting | ||||
| Total | 12.2(198) | 87.8(1421) | |||
| Age at Marriage | 3.612 | 0.164 | |||
| < 18 | 22.6(7) | 77.4(24) | 31 | ||
| 18 + | 12.1(186) | 87.9(1347) | 1533 | ||
| Not Married | 9.1(5) | 90.9(50) | 55 | ||
| Marital Status | 8.579 | 0.073 | |||
| Single | 9.1(5) | 90.9(50) | 55 | ||
| Married | 12.2(188) | 87.8(1355) | 1543 | ||
| Divorced/Separated | 13.3(2) | 86.7(13) | 15 | ||
| Widowed | 50.0(3) | 50.0(3) | 6 | ||
| Number of Marriages | |||||
| None | 9.1(5) | 90.9(50) | 55 | 0.851 | 0.653 |
| One | 12.3(188) | 87.7(1344) | 1532 | ||
| 2 + | 15.6(5) | 84.4(27) | 32 | ||
| Number of Siblings | 3.870 | 0.276 | |||
| 0 | 14.3(19) | 85.7(114) | 133 | ||
| 1 | 5.8(4) | 94.2(65) | 69 | ||
| 2–3 | 11.4(59) | 88.6(458) | 517 | ||
| 4 + | 12.9(116) | 87.1(784) | 900 | ||
| Ethnicity | 0.053 | 0.974 | |||
| Yoruba | 12.3(164) | 87.7(1169) | 1333 | ||
| Igbo | 11.6(15) | 88.4(114) | 129 | ||
| Others | 12.1(19) | 87.9(138) | 157 | ||
| Education | 2.637 | 0.104 | |||
| At Most Secondary Education | 15.2(41) | 84.8(229) | 270 | ||
| Tertiary Education | 11.6(157) | 88.4(1192) | 1349 | ||
| Partner’s Education | 1.573 | 0.210 | |||
| At Most Secondary Education | 14.6(38) | 85.4(223) | 261 | ||
| Tertiary Education | 11.8(160) | 88.2(1198) | 1358 | ||
| Occupation | 8.467* | 0.011 | |||
| Not Working | 15.7(22) | 84.3(118) | 140 | ||
| Business/Self-Employed | 13.3(82) | 86.7(535) | 617 | ||
| Civil Servants | 13.9(23) | 86.1(143) | 166 | ||
| Private Org./Professionals | 11.6(57) | 88.4(433) | 490 | ||
| Health Workers | 6.8(14) | 93.2(192) | 206 | ||
| Partner’s Occupation | 10.449* | 0.034 | |||
| Student/Not Working | 13.0(28) | 87.0(188) | 216 | ||
| Business/Self-Employed | 14.6(68) | 85.4(399) | 467 | ||
| Civil Servants | 9.7(16) | 90.3(149) | 165 | ||
| Private Organisations/Professionals | 12.5(79) | 87.5(551) | 630 | ||
| Health Workers | 5.0(7) | 95.0(134) | 141 | ||
| Monthly Income | 0.453 | 0.929 | |||
| Less than $19.99 | 9.1(7) | 90.9(70) | 77 | ||
| $19.99—$32.65 | 9.3(5) | 90.7(49) | 54 | ||
| $33.32—$65.97 | 11.6(10) | 88.4(76) | 86 | ||
| ≥ $66.63 | 9.0(8) | 91.0(81) | 89 | ||
| Partner’s Monthly Income | 1.219 | 0.749 | |||
| Less than $19.99 | 10.0(2) | 90.0(18) | 20 | ||
| $19.99—$32.65 | 8.7(2) | 91.3(21) | 23 | ||
| $33.32—$65.97 | 11.9(7) | 88.1(52) | 59 | ||
| ≥ $66.63 and above | 7.0(8) | 93.0(107) | 115 | ||
| Religion | 15.294* | 0.001 | |||
| Christianity | 10.7(137) | 89.3(1149) | 309 | ||
| Islam | 18.8(58) | 81.2(251) | 1286 | ||
| Others | 12.5(3) | 87.5(21) | 24 | ||
| Desire for more children | |||||
| Yes | 12.9(94) | 87.1(634) | 728 | 3.556 | 0.169 |
| No | 10.9(83) | 89.1(679) | 762 | ||
| Not Sure | 16.3(21) | 83.7(108) | 129 | ||
| Number of Additional Children Desired | |||||
| None | 10.8(89) | 89.2(737) | 826 | 7.600 | 0.022* |
| One | 16.4(58) | 83.6(295) | 353 | ||
| 2 and above | 11.6(51) | 88.4(389) | 440 | ||
| Number of Previous Pregnancies | |||||
| None | 13.7(10) | 86.3(63) | 73 | 0.889 | 0.828 |
| 1–2 | 11.6(90) | 88.4(686) | 776 | ||
| 3–4 | 13.0(87) | 87.0(584) | 671 | ||
| 5 + | 11.1(11) | 88.9(88) | 99 | ||
| Number of miscarriages | |||||
| None | 12.5(134) | 87.5(938) | 1072 | 0.247 | 0.884 |
| 1–2 | 11.6(55) | 88.4(419) | 474 | ||
| + | 12.3(9) | 87.7(64) | 73 | ||
| Number of Children Alive | |||||
| None | 11.9(10) | 88.1(74) | 84 | 1.089 | 0.664 |
| 1–2 | 11.6(94) | 88.4(713) | 807 | ||
| 3–4 | 13.2(86) | 86.8(565) | 651 | ||
| 5 + | 10.4(8) | 89.6(69) | 77 | ||
| Number of Children Ever Born (CEB) | |||||
| None | 16.1(9) | 83.9(47) | 56 | 0.875 | 0.831 |
| 1–2 | 12.2(73) | 87.8(526) | 599 | ||
| 3–4 | 12.2(84) | 87.8(604) | 688 | ||
| 5 + | 11.6(32) | 88.4(244) | 276 | ||
*p < 0.05
About 13.0% (94) of the 728 women who had at least three surviving children were not using a long-term contraceptive method. The logistic regression presented in Table 3 shows the factors influencing the non-use of long-term contraceptive methods among women who had at least three (≥ 3) surviving children. In the unadjusted model, factors influencing the non-use of long-term methods include education and religion (p < 0.05). The data showed that the likelihood of non-use of long-term contraceptive methods was significantly lower among women who had tertiary education (uOR = 0.539, 95% C. I = 0.338–0.859, p = 0.009) compared to their counterparts with at most secondary education. Likewise, the risk of non-use of long-term methods among Christian women with at least three surviving children was 59% lower (uOR = 0.410, 95% C. I = 0.258–0.652, p < 0.001) than that of Muslim women. However, in the adjusted model, only religion was found to be the predictor of non-use of long-term contraceptive methods among women with at least three surviving children.
Table 3.
Logistic Regression Analysis of the Determinants of Use of Non-use of Long-Term Contraceptive Method among Women who have at least three Surviving Children
| Background Characteristics | Unadjusted Odds Ratio (uOR) | Adjusted Odds Ratio (aOR) | ||
|---|---|---|---|---|
| uOR (95% C.I) | p-value | aOR (95% C.I) | p-value | |
| Age | ||||
| 15–34 (Ref. Cat.) | 1.000 | 1.000 | ||
| 35 + | 1.351(0.820–2.227) | 0.238** | 1.436(0.859–2.402) | 0.168 |
| Education | ||||
| ≤ Secondary (Ref. Cat.) | 1.000 | 1.000 | ||
| Tertiary | 0.539(0.338–0.859) | 0.009* | 0.712(0.365–1.390) | 0.320 |
| Partner’s Education | ||||
| ≤ Secondary (Ref. Cat.) | 1.000 | 1.000 | ||
| Tertiary | 0.664(0.404–1.093) | 0.108** | 1.231(0.605–2.506) | 0.566 |
| Ethnicity | ||||
| Yoruba (Ref. Cat.) | 1.000 | |||
| Others | 0.801(0.458–1.400) | 0.436 | ||
| Religion | ||||
| Islam (Ref. Cat.) | 1.000 | 1.000 | ||
| Christianity | 0.410(0.258–0.652) | < 0.001* | 0.439(0.265–0.726) | < 0.001* |
| Others | 0.394(0.048–3.214) | 0.384 | 0.399(0.047–3.366) | 0.399 |
| Miscarriage | ||||
| No (Ref. Cat.) | 1.000 | 1.000 | ||
| Yes | 1.300(0.840–2.012) | 0.240** | 1.335(0.854–2.089) | 0.205 |
| Number of Previous Pregnancies | ||||
| 3–4 (Ref. Cat.) | 1.000 | |||
| 5 + | 0.866(0.443–1.692) | 0.866 | ||
| Occupation | ||||
| Not Working | 1.174(0.469–2.943) | 0.731 | ||
| Business/Self-Employed | 1.014(0.648–1.588) | 0.951 | ||
| CS/Professionals (Ref. Cat.) | 1.000 | |||
| Partner’s Occupation | ||||
| Not Working | 1.608(0.783–3.301) | 0.196** | 1.552(0.740–3.254) | 0.245 |
| Business/Self-Employed | 1.580(0.995–2.507) | 0.052* | 1.414(0.847–2.363) | 0.186 |
| CS/Professionals (Ref. Cat.) | 1.000 | 1.000 | ||
*p < 0.05; **p < 0.25; CS: Civil Servants
Exploring the modern contraceptive types, reasons for discontinuation, service-level challenges, and how the facility is mitigating the challenges
Availability of contraceptive methods
The availability of varieties of contraceptive methods at the health facility will provide the care providers the opportunity to provide counselling services on different methods rather than focusing on the ones they have at a particular time. This will in addition avail the potential users the opportunity to make choices. The healthcare provider [HCP] at the study site noted that;
“The facility offered both reversible and non-reversible contraceptive methods. The irreversible methods available at the facility are vasectomy and bilateral tubal ligation which are mainly used for limiting childbearing, but the methods are barely used at the facility. Other long-acting methods which can last from 5 to 12 years are available at the facility and these include IUD, implant, and short-acting methods that can last for 2-3 months are also available for access at the facility. Implants are the most used long-acting contraceptive product at the facility, but women limiting and those spacing predominantly use long-acting methods at the facility” (Assistant Nursing Officer, UCH Fertility Centre).
Reasons for discontinuation of contraceptive methods
Women often discontinue the use of a particular contraceptive method and switch to another method or completely disengage from using any contraceptive method. Aside from their intention to have more children, they do this if they are uncomfortable with a method or have some complications and health conditions associated with the use of a method. The health care worker provided insight into the reasons for discontinuation of contraceptive methods based on her experience and interaction with women at her facility.
Women’s preference for long-acting methods over short-acting methods is based on two main factors (i) ease and convenience of use and (ii) immediate return to fertility after stoppage or discontinuation of use. Maybe because it’s reversible and convenient. Just put it there, let me use it for as long as I want and I pull it out. And the return to fertility is immediate. That’s the beautiful thing about implants. So, that’s why the majority tends to use implant IUDs” (Assistant Nursing Officer, UCH Fertility Centre).
From the modern contraceptive general perspective, the data showed that career development amongst women, family economy dynamics and the consciousness to have a specific number of children that their families could cater for were factors promoting the use of modern contraceptives. In addition, women had growing awareness of the importance of the number of children in their lives and family outcomes. Hence, they were more ready than before to control their births. This growth of awareness also supported the growing clientele size at the facility.
“Well, the economic situation is a factor now. Gone are the days when people used to have as many children as possible. But now with the recession, with the economic situation, more women have that awareness that they should have children that they can conveniently cater for. And that increases the clientele for family planning. Then apart from that, I think another factor is that most women tend to be career women now unlike those days when they used to be just sitting at home, full housewife or trading. But now most women tend to be career. So, for their career to progress, they have to be conscious of how often they get pregnant”
(Assistant Nursing Officer, UCH Fertility Centre).
Religion, beliefs, traditions, perspectives and backgrounds have been expressed by clients as factors mitigating the use of modern contraceptives, but sentiments attributed to these factors were being eroded by the increasing awareness and sensitisation of women on the need for FP, especially across social media and other media channels. The argument was that more women were aware of contraceptive methods and how they are used, but lacked the theoretical foundation of how the methods work. The review of records showed that Catholic women were well-represented FP clients in the facility, despite the objection and aversion of this religious domination to FP. Activities to promote the use of FP at the facility are;
“In the facility, we do in-house training. Sometimes we call in the support staff, the security, cleaners, and especially the junior cadres to educate them on the need for family planning. We also visit the clinics where you can have access to nursing mothers. For instance, women attending immunization clinics at the college are the target audience. They are the people that need family planning. We go there to health-educate them. We also give out education in the postnatal clinic, that’s six weeks after delivery. So, we are sensitizing them, in-house” (Assistant Nursing Officer, UCH Fertility Centre).
FP is a unit that is expected to provide all FP services at the health facility and this often requires staff to discharge specific services to clients including outreach programs. However, mass migration of healthcare workers out of the country is likely to pose a challenge. Consequently, manpower deficit may have a strong influence on the delivery of FP services at the tertiary health facilities in Nigeria as much as other primary and secondary facilities. Another big challenge often reported at health facilities in Nigeria is the lack of training to equip staff with contemporary knowledge of FP technology and services provision. Some FP providers lack the requisite skills and expertise to handle modern contraceptive procedures such as IUDs and implants. The healthcare provider’s voice about this construct;
“The shortage of manpower is a big factor. We used to be very plenty, but now it’s like just two people doing the work of 12 staff” The low manpower strength at the facility increases the workload on them and their productivity. This system-level challenge affects the capacity of the centre’s manpower to meet the needs of clients. The community outreach services have been impaired too. The structure of low manpower cuts across the primary and secondary FP centres which increases the workload and stress on staff at the UCH facility being a tertiary health institution. If you go to a health centre where the so-called experts cannot provide some method because of their expertise, they tend to tilt their health education towards what they have and what they can provide. It’s not all. Unlike when all the options are available” (Assistant Nursing Officer, UCH Fertility Centre).
Service-level challenges arising from family planning service delivery
One of the service-related challenges is complication that may arise from the use of FP, particularly the long-acting and permanent methods e.g., poorly inserted Implants. Other challenges might result from contraceptive failure or the inability of women to conceive when they decide to do so. However, most of these challenges are often from the primary and secondary health facilities arising from poor clients’ management.
“Being a teaching hospital, every problem from every other centre comes here. Yeah. So, when they create a problem, it will end at our table. And we don’t have any choice but to attend to them. We do our best and we’ve been trying to control such situations so that it doesn’t go out of hand. However, there have been no cases of litigation or lawsuits, because the facility adheres to the national and international Standard Operational Procedure. Clients younger than age 18 were attended to under the support of a guardian. In cases of partner’s insubordination, we handle such situations so that it doesn’t escalate to the level of lawsuits or litigations” (Assistant Nursing Officer, UCH Fertility Centre).
Efforts to mitigate challenges
There was no record of litigation or lawsuits because the facility delivered family planning services using an approved Standard Operational Procedure [SOP], a national protocol to which the facility adheres to. For instance, clients younger than 18 years of age were attended to under the support of a guardian. Also, in cases of partner insubordination, the healthcare workers leverage their experience in communicating and addressing such disturbances.
“So, some of them will come with their wife with all sorts of reactions. But, you know, as professionals, we know how to handle them. So, most cases, we handle such situations that it doesn’t escalate to the level of lawsuits or litigations” (Assistant Nursing Officer, UCH Fertility Centre).
Contraceptive failure was a major problem managed at the centre which largely involved clients transferred from other primary, secondary and private health facilities. Hence, the facility deployed inter-agency collaboration to improve the health outcomes of clients. For instance, the facility worked with HIV/AIDS programs and agencies to manage contraceptive failure in clients on Anti-retroviral (ARV) medications by identifying and replacing contraceptive products whose potency was lowered by ARVs.
Reasons for preference for SACMs instead of LACMs among high fertility women
The 1988 Nigeria Population Policy and the revised editions of the policy emphasized that the number of children per family is limited to four. Therefore, if a woman has had at least four children, the expectation is that she should use contraceptives to limit rather than to space childbirth. In such circumstances, long-acting or permanent methods would have been appropriate for such women. However, the National Guideline for FP Services allows clients to choose their preferred contraceptive method after being advised by professionals. High fertility clients (having at least 4 surviving children) are at liberty to use any method, since the service providers cannot impose a particular method on them. Their choice and decision to use a particular method might have been informed by various factors including socioeconomic, cultural, and peer interactions. The healthcare provider said that;
“Well, one thing about family planning is that we don’t force our methods on anybody. If a high-fertility woman decides to use a short-term method, this can also limit the number of children they will bear as long as they adhere to it and are not defaulting. It’s okay because it’s their choice. And they know the reason why they chose that method. So, there are some people like that” (Assistant Nursing Officer, UCH Fertility Centre).
Focus Group Discussion [FGD] with Highly Fertile Women using short-term contraceptive methods
The ages of eight (8) sexually active, fecund women with 4 or more living births who participated in the interview ranged from 35 to 49 years. Two of the women were 35–39 years, 4 were 40–44 years, and 2 were 45–49 years. All the women were aware of different short-term and long-term contraceptive methods some of which they had used for child spacing or limiting. The women had used contraceptive products for more than 10 years and their experience built over time improved their understanding of the functionalities of different contraceptive methods. However, these women generally used short-term methods instead of long-term methods. Amongst these women, 6 (75.0%) belonged to polygamous marriages or had multiple husbands at different points in their marital journey. 25% (n = 2) of these women had mixed genders amongst their living children and 5 (62.5%) indicated that were likely to have more children if their partners wanted it.
Reasons for choosing short-term contraceptive methods
The use of a particular method is strictly the choice of the clients not that of the service provider. However, the service provider has the responsibility to counsel the clients on the appropriate method. The women who participated in the FGD repeatedly mentioned that the reasons for their choice of short-term methods were fear of forgetting the elapsed timing of the long-term methods, the hygiene needs, the cost of maintenance, etc. The views of the participants were as follows;
“For the long-term method, one might feel there is still enough time which might make one forget. While for the short time method, you already know the span you can’t forget easily” (Participant 6)
“Also, the pills, I might forget to use them, that is why I opted for the injection since I was told it is every three months or two months. Then I opted for the two months, once it elapses, I renew it the next two months. Since I have my fifth child; am still using it” (Participant, 5).
“I have been using pills before giving birth and I am comfortable with it. Even when I started giving birth, I kept using it. Once I intend to give birth, I do stop using it and I am very comfortable with it and I have no complaints” (Participant, 4).
Two of the participants said they were afraid of injections but would prefer Oral Contraceptive Pills (OCPs). An implication is that they show sentiments towards products other than the ones they used and the interest they built concerning a particular product tended to affect their capacity to seek a change of method. From the perspectives expressed by participants, they showed immense confidence in short-term methods, especially for OCPs and injectables, because of the convenience, ease-of-use, partner’s choice, never fails, short renewal time, and memory lapses associated with the use of long-term methods and the short-term methods keep women within her fertility desires, even when long-acting reversible methods might offer a better advantage. The gender of living children was commonly reported by the women as one of the drivers for the use of short-acting methods. In some cases, women emphasised that their partners preferred they used short-term methods so that they could have children whenever they wanted since they had not achieved their preferred child’s gender.
“The private part own can fail, but you see that of the arm, I will forget, but I already have that of the pills at home. I do not forget at all. I have been using pills since I had my second child, and now I have five children in total. I like the pills because I do not make mistakes” (Participant 2).
"The reason for the choice of injection is that it is very convenient. I have heard a lot, I heard that implants (arm) bring about bleeding, while that of the private part can find its way into the private part. I have been using that of injection up until I had my fourth child. If I want to have another child, I can stop the injection method. The injection method is very convenient for me. If I am given a shot, the next shot would be the next three months. I also do set reminders for the next appointment. Since I have been using this injection method. It has been convenient for me and I am comfortable with it. These are the reasons why I prefer the injection method” (Participant 1).
“It has never failed me since I have been using even up until I welcomed my fourth child. It has never failed me that is why am using it” (Participant 2).
“I have four kids of which all are females, but I give birth through caesarean surgery. My husband still wants more kids, but for my health’s sake, I employ the short-term method. I cannot kill myself because I want to give birth. My husband is not aware, only my mother is aware” (Participant 6).
The role of partners in women’s choice of short-term methods
The role of men is essential to contraceptive adoption, choice, and use by their wives or female sexual partners. The cultural background of most Nigerian societies makes men the family head and, in this perspective, they are involved in all household decisions including those that affect their wives. Most participants claimed that they undertook their current contraceptive method without their husbands’ knowledge because they may demand more children. Hence, women’s lack of privacy for IUCD or Implants prompted them to use OCPs or injections which their husbands could rarely trace. Hence, the decision to choose a long-acting reversible method might be beyond women alone, therefore their husbands would have to be involved. However, some of the women claimed that their husbands selected the short-term method they are currently using.
“My husband does not give consent to the long-term method. He gave consent the last time we came together for me to be given Injection. He does not like the long-term method” (Participant 5)
“My husband likes children a lot. He also wanted a male that is why I opted for the short-term method, should in case he insists that we must have kids then I can easily stop it” (Participant 4)
Choice of non-reversible contraceptive methods
Non-reversible methods involve the use of surgical processes to induce contraception such as vasectomy (in men) and Bi-lateral Tubal Ligation [BTL] (in women). One of the participants showed interest in considering non-reversible contraception but was discouraged against it based on her age.
“I have tried to employ it after giving birth through caesarean surgery. Nevertheless, the doctor did not provide it for me due to my age. I was informed that there is a certain age that they can advise to go for such a service. However, due to my age as at my last birth, I was told I could not be offered the service” (Participant 3).
Discussion
Nigeria is a high-fertility country and every society across the country supports childbearing. Ibadan is a traditional society dominated by people who are adherent to their cultural identities including childbearing, particularly in marriage. Access to contraceptive commodities is not free in Nigeria. These commodities are often procured at the patent medicine store and health facilities out-of-pocket. The shame attached to buying contraceptives such as condoms, oral pills, etc. is still prevalent in Ibadan. This study examined modern contraceptive-type use among women who accessed family planning services at the University College Hospital Fertility Research Centre, Ibadan from 2018–2022.
The findings revealed that the trajectory of FP services uptake barely changed from 2018 and 2022 at the health facility. Although an upsurge in the number of clients at the FP clinic was found between 2018 and 2019, this followed a sharp downward trend in 2020 and consistently an increase from 2020 to 2022. The observed pattern of the number of clients accessing the FP clinic at the health facility could be attributed to the COVID-19 pandemic which prevented many patients from accessing the health facility in the year 2020, either due to the fear of contracting the disease at the health facility or lockdown policy and other non-pharmaceutical measures to mitigate the spread of the disease by the government at that time. The sudden and consistent increase in the number of FP clients at the health facility from 2020 to 2021 and 2021 to 2022 is evidence that COVID-19 was the reason for the observed pattern in FP clinic attendees. Many studies have isolated COVID-19 as the reason for low healthcare patronage during the year 2020 which was the peak year of the disease [12, 20]. Therefore, it is pertinent that government and FP planners devise strategies to get FP services across to women who require such during a pandemic situation in Nigeria. Best practices implemented for similar services in other settings during the pandemic can be adopted.
The study further revealed that about four-fifths of the women whose files were reviewed within the study period used long-term contraceptive methods. Although almost all the women used long-term reversible contraceptive methods, this finding is in agreement with the outcome of similar hospital-based studies previously conducted in Nigeria and elsewhere around the world where fecund women with 4 or more living children used long-term methods instead of short-term methods [28, 45]. However, the finding is inconsistent with the reported low prevalence of long-term contraceptive methods by national studies in Nigeria and East African countries [21, 30]. While our study was hospital-based and retrospective in design, the population-based and cross-sectional design approaches used for the nationally representative study could be attributed to the differences. The population-based study involved both users and non-users of contraceptive methods, while the current study focused on contraceptive users. Counselling received at the point of care can promote the use of long-term contraceptive methods among clients at the FP clinics. It is thus expected that the proportion of women who used long-acting methods in our hospital-based study would be higher than the proportion in the population-based studies.
Research is consistent with three to four or fewer children being the average number of children a woman bears in the southwest region, of Nigeria especially Ibadan, a setting where the evaluated health facility is cited which is one of the largest cities in the region [1]. Therefore, one would have expected that women who already have at least three surviving children accept to initiate a long-term contraceptive method instead of the short-term methods. The finding from this study showed that one in eight women who had at least three surviving children did not seek long-term contraceptive methods at the clinic. The issues associated with long-term methods including convenience, ease-of-use, partner’s choice, never fails, short renewal time and child’s gender preference as identified in the qualitative arm of this study might inform their preference for the short-term contraceptive uptake instead of long-term methods. Such reasons have been identified in earlier studies [6, 15, 30]. The multivariate analysis revealed religion as the sole predictor of non-use of long-term contraceptive methods among women with at least three surviving children. Women with at least three surviving children who were Christians had a higher likelihood of using long-term contraceptive methods compared to their Muslim counterparts. This finding perfectly aligns with expectations because there is a tendency that a higher proportion of Muslim women compared to Christians might have the intention to have another child soon [7, 16], therefore, they adopt short-term contraceptives for spacing rather than limiting births. Competition for children among wives could be another possible reason since polygamy is more pronounced among Muslims than Christians [4].
Aside from the socioeconomic issues, high-fertility women are at greater risk of pregnancy complications, disability, and other health conditions associated with further pregnancy [34]. Therefore, such women are expected to use long-term contraceptive methods to limit childbearing. Although the interviewed service provider opined that clients cannot be forced to use a method different from their preferred method, they can only provide counselling and technical guidance on the benefits of the recommended product. Therefore, it is not surprising that some high-fertility women who participated in this study mainly used short-term contraceptive methods. The main reasons provided by such women were convenience, ease of use, partner’s choice, never fails, short renewal time, and child’s gender preference. Side effects and lack of access were also highlighted as reasons for the non-use of long-term contraceptive methods. These factors have been reported in existing studies in Scotland [2], Ethiopia [6], Ghana [15], and Nigeria [8, 30, 41]. This finding has policy implications on fertility and maternal health. While long-term methods hardly fail, there is a noticeable failure rate for short-term methods. Government policy and interventions to promote the use of long-term contraceptive methods among high-fertility women are thus paramount in Nigeria. Addressing the issue of training and understaffing at the FP clinic due to the exodus of large healthcare workers out of the country as emphasised by the interviewed FP service provider can bridge the gap.
The strength of this study is the use of hospital-based data which provided an opportunity to explore the experience of women currently using contraceptives rather than the community-based study where non-users might claim that they are currently using a contraceptive method, thus enhancing the accuracy of our findings. The use of mixed-method design from the perspectives of the clients and service providers in understanding the barriers to the use of long-term methods among high-fertility women is another strength. However, using a single facility instead of including other facilities providing FP services in Ibadan makes the findings not generalisable to the entire community. However, UCH being a tertiary health facility provides healthcare services to most inhabitants of Ibadan and its environment. In most situations, the facility receives referrals from both the secondary and primary health facilities. Therefore, evaluating FP activities at the facility can provide a wider view of the FP services in Ibadan and its suburban communities. An assessment of how the supply of contraceptive products across multiple facilities affects the choice of contraceptive methods by women of reproductive age remains a grey area for further research.
Conclusions
There was a slightly increasing trend in the number of clients who accessed contraceptive services at the family planning clinic in UCH, Ibadan from 2018 to 2022. The majority of the clients demanded long-term contraceptive methods over the period. Religion was the main predictor of the use of long-term contraceptive methods among women with at least three surviving children. The main reasons ascribed by the high-fertility women for using the short-term methods were convenience, ease-of-use, partner’s choice, never fails, short renewal time, and child’s gender preference. Mass migration of healthcare workers out of the country and lack of training were reported by the service provider as the main challenges to accessing family planning services at the facility. Addressing these challenges can promote the use of contraception in the study area. More sensitisation on the need to embrace long-term reversible contraceptive methods among high-fertility women is essential.
Supplementary Information
Acknowledgements
We thank University College Hospital, Ibadan for granting the permission to review the relevant case file for this study. The support provided by the FP clinic officers is appreciated.
Abbreviations
- BTL
Bilateral Tubal Ligation
- CPR
Contraceptive prevalence Rate
- FGD
Focus Group Discussion
- FP
Family Planning
- HCP
Healthcare Provider
- IAMRAT
Institute for Advanced Medical Research and Training
- ICPD
International Conference on Population and Development
- IDI
In-depth Interview
- IUCDs
Intra-Uterine Contraceptive Devices
- KII
Key Informant Interview
- LACMs
Long-Acting Contraceptive Methods
- OCPs
Oral Contraceptives
- SACMs
Short-Acting Contraceptive Methods
- SDGs
Sustainable Development Goals
- SSA
Sub-Saharan Africa
- TFR
Total Fertility Rate
- UCH
University College Hospital
Authors’ contributions
Atoyebi A.O (AAO) and Adebowale Ayo Stephen (AAS) conceptualized the research idea and developed the study plan. AAS, AAO, and Okunlola M.A (OMA) wrote the introduction and method section. AAS, Olaoye O.S (AOS), and AAO conducted the data analysis and interpretation. AAS, OMA and PME wrote the discussion section while AAS produced the draft of the paper. The authors revised and approved the final draft. AAS is the guarantor of the paper.
Funding
Open access funding is provided by North-West University.
Data availability
The datasets analysed or generated from this study are not available for public use due to the need for confidentiality for sensitive information gathered. The secondary data were obtained through the review of hospital records of women accessing family planning services at a tertiary health institution. Permission to use such data will have to be granted by the hospital's management board. Therefore, its availability for public consumption might be limited. The primary data which was the qualitative aspect of the study shall be made available to the prospective users by the authors on request.
Declarations
Ethics approval and consent to participate
I confirm that all experiments were performed in accordance with relevant guidelines and regulations. The approval to conduct this study was granted by the ethical committee at the Institute for Advanced Medical Research and Training [IAMRAT] of the College of Medicine, University of Ibadan with approval number NHREC/05/012008a. Within the hospital system, the study gained approval for data collection and patient access by the Department of Obstetrics and Gynaecology, Faculty of Clinical Sciences, College of Medicine, University of Ibadan. This approval was needed to access the Family Planning Research Unit where patients’ case files are. For the qualitative part of the study, informed consent was obtained from the participants before the commencement of the study. The respondents were informed that they would not be subjected to any form of harm and that their involvement would not induce mental health risk on them, in compliance with the Declaration of Helsinki. We ensured that the secondary data from women’s case files were not commercialised or made accessible to unauthorised individuals who may use the information to the detriment of the women. The respondents were assured of the anonymity of the information they provided. The possible identifier that could be used to track each respondent to the information they provided was removed from the original data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abiodun OM, Balogun OR. Sexual activity and contraceptive use among young female students of tertiary educational institution in Ilorin. Nigeria Contraception. 2009;79:2. [DOI] [PubMed] [Google Scholar]
- 2.Adebowale A. Palamuleni M. Religion and ethnicity interaction as a predictor of male fertility in Nigeria: Evidence from a national representative sample. PLoS One. 2024;19:1. 10.1371/journal.pone.0296983 [DOI] [PMC free article] [PubMed]
- 3.Adebowale AS, Asa S, Abe JO, Oyinlola FF. Sex preference, religion, and ethnicity roles in fertility among women of childbearing age in Nigeria: Examining the links using zero-inflated Poisson regression model. Int J Stat Probab. 2019;8(6):91–106. [Google Scholar]
- 4.Adebowale, AS. Fagbamigbe FA. and Bamgboye EA. Contraceptive Use: Implication for Completed Fertility, Parity Progression and Maternal Nutritional Status in Nigeria. Afr J Reprod Health. 2011;15:4, pp. 60–67 [PubMed]
- 5.Adedini SA, Omisakin OA, Somefun OD. Trends, patterns and determinants of long-acting reversible methods of contraception among women in sub-Saharan Africa. PLoS ONE. 2019;14:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aduloju OP, Akintayo AA, Adefisan AS, Aduloju T. Utilization of Long-Acting Reversible Contraceptive (LARC) Methods in a tertiary hospital in southwestern Nigeria: A Mixed Methods Study. J Obstet Gynaecol India. 2021;71(2):173–80. 10.1007/s13224-020-01386-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aduloju OP. Uptake of family planning services at a new University Teaching Hospital in southwestern Nigeria. Trop J Obstet Gynaecol. 2013;30(1):119–25. [Google Scholar]
- 8.Aduloju OP, Akintayo AA, Adefisan AS, Aduloju T. Utilization of Long-Acting Reversible Contraceptive (LARC) Methods in a Tertiary Hospital in Southwestern Nigeria: A Mixed Methods Study. J Obstet Gynaecol India. 2021;71:173–80. 10.1007/s13224-020-01386-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahinkorah BO. Predictors of modern contraceptive use among adolescent girls and young women in sub-Saharan Africa: a mixed-effects multilevel analysis of data from 29 demographic and health surveys. Contracept Reprod Med. 2020;5:1–12. 10.1186/s40834-020-00138-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed SAKS, Ajisola M, Azeem K, Bakibinga P, Chen YF, Choudhury NN, Fayehun O, Griffiths F, Harris B, Kibe P, Lilford RJ, Omigbodun A, Rizvi N, Sartori J, Smith S, Watson SI, Wilson R, Yeboah G, Aujla N, Azam SI, Diggle PJ, Gill P, Iqbal R, Kabaria C, Kisia L, Kyobutungi C, Madan JJ, Mberu B, Mohamed SF, Nazish A, Odubanjo O, Osuh ME, Owoaje E, Oyebode O, Porto de Albuquerque J, Rahman O, Tabani K, Taiwo OJ, Tregonning G, Uthman OA, Yusuf R. Improving Health in Slums Collaborative. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob Health. 2020;5:e003042. 10.1136/bmjgh-2020-003042. [DOI] [PMC free article] [PubMed]
- 11.Ajzen I. The Theory of Planned Behaviour. Organisational Behaviour and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- 12.Akamike IC, Okedo-Alex IN, Eze II, Ezeanosike OB, Uneke CJ. Why does uptake of family planning services remain sub-optimal among Nigerian women? A systematic review of challenges and implications for policy. Contracept Reprod Med. 2020;30:1–13. 10.1186/s40834-020-00133-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anguzu R, Sempeera H, Sekandi JN. High parity predicts the use of long-acting reversible contraceptives in the extended postpartum period among women in rural Uganda. Contracept Reprod Med. 2018;3:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asegidew W, Tariku B, Kaba M, Getachew S, Ketsela K. Acceptance and positive attitude increased utilization of long acting and permanent family planning methods among reproductive age group women from Debre Berhan District, Ethiopia: quantitative and qualitative analysis. J Community Med Health Educ. 2017;7(2):541–72. [Google Scholar]
- 15.Awolude OA, Olagunju A. S: Convert contraceptive use amongst women of reproductive age in Ibadan Nigeria. Niger Med. 2019;28:1–16. [Google Scholar]
- 16.Bolarinwa OA, Nwagbara UI, Okyere J, Ahinkorah BO, Seidu AA, Ameyaw EK, Igharo V. Prevalence and predictors of long-acting reversible contraceptive use among sexually active women in 26 sub-Saharan African countries. Int Health. 2021;14:492–500. 10.1093/inthealth/ihab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bolarinwa OA and Olagunju OS: Knowledge and factors influencing long-acting reversible contraceptives use among women of reproductive age in Nigeria [version 3; peer review: 1 approved, 2 approved with reservations] Gates Open Research. 2020;3:7–16. 10.12688/gatesopenres.12902.3 [DOI] [PMC free article] [PubMed]
- 18.Bolarinwa OA, Ajayi KV, Okeke SR. Spatial distribution and multilevel analysis of factors associated with long-acting reversible contraceptive use among sexually active women of reproductive age in Nigeria. Arch Public Health. 2023;81:99. 10.1186/s13690-023-01110-6 [DOI] [PMC free article] [PubMed]
- 19.Braverman PK, Adelman WP, Alderman EM, Breuner CC, Levine DA, Marcell AV, O’Brien RF. Contraception for adolescents. Pediatrics. 2014;134:e1244–56. 10.1542/peds.2014-2299. [DOI] [PubMed] [Google Scholar]
- 20.Brunie A, Stankevitz K, Nwala AA, Nqumayo M, Chen M, Danna K, Afolabi K, Rademacher K. H: Expanding long-acting contraceptive options: a prospective cohort study of the hormonal intrauterine device, copper intrauterine device, and implants in Nigeria and Zambia. Lancet Glob Health. 2021;9:e1431–41. 10.1016/S2214-109X(21)00318-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coll CDVN, Ewerling F, Hellwig F, De Barros AJD. Contraception in adolescence: the influence of parity and marital status on contraceptive use in 73 low-and middle-income countries. Reprod Health. 2019;16:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeMaria, A.L., Sundstrom, B., Faria, A.A: Using the theory of planned behaviour and self-identity to explore women’s decision-making and intention to switch from combined oral contraceptive pill (COC) to long-acting reversible contraceptive (LARC). BMC Women’s Health. 2019;19:82.10.1186/s12905-019-0772-8 [DOI] [PMC free article] [PubMed]
- 23.Enyew EB, Tareke AA, Ngusie HS, Kasaye MD, Kebede SD, Feyisa MS. Long-acting family planning uptake and associated factors among women in the reproductive age group in East Africa: multilevel analysis. Front Glob Womens Health. 2005;6(2):1444784. 10.3389/fgwh.2025.1444784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fagbamigbe AF, Afolabi RF, Idemudia ES. Demand and unmet needs of contraception among sexually active in-union women in Nigeria: distribution, associated characteristics, barriers, and program implications. SAGE Open. 2018;8:2158244017754023. 10.1177/2158244017754023. [Google Scholar]
- 25.Glasier A, Scorer J, Bigrigg A. Attitudes of women in Scotland to contraception: a qualitative study to explore the acceptability of long-acting methods. J Fam Plann Reprod Health Care. 2008;34:213–7. 10.1783/147118908786000497. [DOI] [PubMed] [Google Scholar]
- 26.Hindin MJ, McGough LJ, Adanu RM. Misperceptions, misinformation and myths about modern contraceptive use in Ghana. J Fam Plann Reprod Health Care. 2014;40:30–5. 10.1136/jfprhc-2012-100464. [DOI] [PubMed] [Google Scholar]
- 27.Hosseini H, Torabi F, Bagi B. Demand for long acting and permanent contraceptive methods among Kurdish women in Mahabad. Iran J Biosoc Sci. 2014;46(6):776–85. [DOI] [PubMed] [Google Scholar]
- 28.Jumbo CH, Muhammad RB, Adewole ND, Isah DA, Offiong RA, Abdullahi HI. Uptake of long-acting reversible contraceptives in north-central Nigeria: a five-year review International. J Res Med Sci. 2021;9:1335–9. [Google Scholar]
- 29.Leite H, Lindsay C, Kumar M. COVID-19 outbreak: implications on healthcare operations’. TQM J. 2020;33:247–56. 10.1108/TQM-05-2020-0111. [Google Scholar]
- 30.Michael, T. O., Asa, S. S., Olubodun, T.: Trends and risk indicators for high fertility among Nigerian female youth aged 15–29 years: A pooled data analysis. Heliyon. 2024;10(18):e37946. 10.1016/j.heliyon.2024.e37946. [DOI] [PMC free article] [PubMed]
- 31.Montano DE, Kasprzyk D: Theory of reasoned action, the theory of planned behaviour, and the integrated behavioural model. In: Glanz K, Reimer BK, Lewis FM, editors. Health behaviour and health education. 2002, 3rd. San Francisco, CA: Jossey-Bass.
- 32.Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, Jones M, Kitchener E, Fox M, Johansson M, Lang E, Duggan A, Scott I, Albarqouni L. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11:e045343. 10.1136/bmjopen-2020-045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nyimbili , F., & Nyimbili , L.: Types of Purposive Sampling Techniques with Their Examples and Application in Qualitative Research Studies. British Journal of Multidisciplinary and Advanced Studies. 2024, 5 (1): 90–99. 10.37745/bjmas.2022.0419
- 34.Obembe TA, Odebunmi KO, Olalemi AD. Determinants of family size among men in slums of Ibadan Nigeria. Ann Ibadan Postgrad Med. 2018;16(1):12–22. [PMC free article] [PubMed] [Google Scholar]
- 35.Ohazurike, E., Olamijulo, JA, Ibisomi, L., Olorunfemi, G., Oluwole, AA: Predictors of discontinuation of subdermal levonorgestrel implants (Jadelle) at the Lagos University Teaching Hospital, Lagos, Nigeria: an analytic cohort study. Afr J Reprod Health. 2020;2:48–63. 10.29063/ajrh2020/v24i2.5 [DOI] [PubMed]
- 36.Otekunrin OA, Olasehinde LO, Oliobi CE, Otekunrin OA, Osuolale K. A: Exploring women’s preferences for attributes of long-acting reversible contraceptive (LARC) methods: A discrete choice experiment. Scientific African. 2023;19:e01499. 10.1016/j.sciaf.2022.e01499. [Google Scholar]
- 37.Oyediran KA. Fertility desires of Yoruba couples of South-western Nigeria. J Biosoc Sci. 2006;38(5):605–24. [DOI] [PubMed] [Google Scholar]
- 38.Population Reference Bureau: 2025 World Population Datasheet. 2023 [https://2023-wpds.prb.org/wp-content/uploads/2023/12/2023-World-Population-Data-Sheet-Booklet.pdf]
- 39.Sambah F, Aboagye RG, Seidu AA, Tengan CL, Salihu T. Ahinkorah, BO: Long-acting reversible contraceptives use among adolescent girls and young women in high fertility countries in sub-Saharan Africa. Reprod Health. 2022;19(209):221. 10.1186/s12978-022-01494-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, Burroughs H, Jinks C. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907. 10.1007/s11135-017-0574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sundstrom B, Billings D, Zenger KE. Keep calm and LARC on: a theory-based long-acting reversible contraception (LARC) access campaign. J Commun Healthc Strateg Media Engagem Glob Health. 2016;1:1–18. 10.1080/17538068.2016.1143165. [Google Scholar]
- 42.Thanel K, Garfinkel D, Riley C, Esch K, Girma W, Kebede T, et al. Leveraging long acting reversible contraceptives to achieve FP2020 commitments in sub-Saharan Africa: The potential of implants. PLoS ONE. 2018;13(4):e0195228. 10.1371/journal.pone.0195228. [DOI] [PMC free article] [PubMed]
- 43.Tibaijuka L, Odongo R. Welikhe, E: Factors influencing the use of long-acting versus short-acting contraceptive methods among reproductive-age women in a resource-limited setting. BMC Women’s Health. 2017;25:1–13. 10.1186/s12905-017-0382-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Waithaka MW, Gichangi P, Thiongo M: Assessing the magnitude of and factors associated to demand for long-acting reversible and permanent contraceptive methods among sexually active women in Kenya. medRxiv. 2020;10:1–18. 1101/2020.11.12.20230383.
- 45.Weldekiros ME, Tamire M, Berhane A, Gufue ZH, Tesfa FH. Utilization Status and Perceived Barriers Towards Long-Acting Reversible Contraceptives Among Female Youth College Students in Northern Ethiopia: A Mixed-Methods Study. Int J Womens Health. 2023;15:1107–23. 10.2147/IJWH.S413425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Westoff CF, Bietsch K. Religion and reproductive behaviour in sub-Saharan Africa. DHS Analytical Studies. No. 48. Rockville, Maryland, USA: ICF International; 2015.
- 47.Williams LA, Sun J, Masser B. Integrating self-determination theory and the theory of planned behaviour to predict intention to donate blood. Transfus Med. 2019;29(Suppl. S1):S59–S64. 10.1111/tme.12566. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analysed or generated from this study are not available for public use due to the need for confidentiality for sensitive information gathered. The secondary data were obtained through the review of hospital records of women accessing family planning services at a tertiary health institution. Permission to use such data will have to be granted by the hospital's management board. Therefore, its availability for public consumption might be limited. The primary data which was the qualitative aspect of the study shall be made available to the prospective users by the authors on request.