Abstract
Background
The Optimal Screening for Prediction of Referral and Outcome-Yellow Flag (OSPRO-YF) is a questionnaire that helps assess multiple psychological domains. The primary purpose of this study was to evaluate the effect of body region (shoulder and elbow) and sex on baseline OSPRO-YF scores. The secondary purpose was to evaluate the association of age on baseline OSPRO-YF scores for both shoulder and elbow patients.
Methods
242 subjects completed 1) a demographic survey and 2) the 17-item OSPRO-YF. The OSPRO-YF estimates the individual scores of 11 psychological patient-reported outcome measures. To assess the effects of body region and sex on the OSPRO-YF, 1 multivariate generalized linear model was conducted. To assess the association of age on the OSPRO-YF, 11 simple linear regressions were conducted for each subscale of the OSPRO-YF.
Results
Patients with elbow pain exhibit higher fear avoidance behavior than those reporting with shoulder pain. Patients with elbow pain also presented with lower self-efficacy with respect to pain and rehabilitation. There was no significant main effect for sex nor was there a significant interaction for body region and sex. When controlling for both sex and BMI within the elbow cohort, age was significantly associated with the Tampa Scale of Kinesiophobia and the State-Trait Anger Expression Inventory.
Conclusion
Patients reporting with elbow pain seem to experience psychological barriers. By establishing psychological awareness in clinical settings, providers will be able to provide a patient-specific plan of care that accounts for these barriers.
Keywords: Psychological distress, Upper extremity, Musculoskeletal shoulder, Musculoskeletal elbow, OSPRO-YF, Negative mood, Positive affect, Fear avoidance
Psychological factors have been shown to impact patient recovery following a variety of musculoskeletal (MSK) health conditions.32,56,60 These factors often include maladaptive pain beliefs, negative affective reactions, and poor coping strategies.17,45 The prevalence of psychological distress in MSK disorders is well-studied in the knee, hip, and low back pain patient populations.4,16,39 Not only are these psychological factors present in patients suffering from MSK-related pathologies, but individuals undergoing knee or hip replacement with psychological factors identified preoperatively were at a higher risk for development of postoperative chronic pain.16 In addition, baseline psychological-related constructs have been found to predict postsurgical pain at both the 3-month and 6-month timepoints following knee arthroplasties.54 Furthermore, illness perception and pain catastrophizing were associated with patient-reported outcome measures (PROMs) at 12 months in a low back pain population.40 Preoperative fear of movement in patients with low back pain underdoing lumbar fusion surgery was significantly associated with postoperative movement behaviors such as sedentary behavior.29 While the majority of psychological determinants arise from the hip, knee, and spine literature,20,26,43 it is important to not neglect the prevalence and impact of these determinants in patient populations suffering from shoulder and elbow conditions. In fact, ineffective coping strategies and pain catastrophizing are associated with greater symptom intensity and magnitude of disability in patients with shoulder disorders.47 Similarly, patients with rotator cuff pathology who document poor self-perceived scores of negative mood or coping have increased shoulder pain and functional limitations.49 Minimal work in this area has been documented in patients with elbow pain. Although, researchers have found that individuals with tennis elbow have lower scores on common psychological domains when compared to a healthy cohort.1 Certainly, more work needs to be conducted on the impact of psychological distress on pain level and functional outcomes in a variety of ages among patients who present with both shoulder and elbow pain.
Patient-reported outcome measures (PROMs) in the form of self-report questionnaires are an effective way to assess psychological factors affecting a patient.10,61 However, the number of PROMs that can be used to assess psychological constructs can be overwhelming. Researchers suggest that several PROMs examine the same constructs, making it difficult to pick the most relevant outcome.10 A systematic review examining the use of psychologically related PROMs among physiotherapists found 7 psychological questionnaires used in practice centered around fear avoidance behavior, depression, and self-efficacy constructs.15 The fear avoidance questionnaire assesses patient beliefs with regards to the effect of physical activity and work.63 There are preferred measures for examining depression and anxiety in individuals with MSK pain; for depression, these include but are not limited to the following: Patient Health Questionnaire-9 (PHQ-9) and Depression subscale of the Hospital Anxiety Depression Scale; for anxiety, these include but are not limited to the following: State-Trait Anxiety Inventory (STAI), and Pain Anxiety Symptom Scale.5 Self-efficacy is defined as a person's confidence or belief in their capacity to achieve goals or perform activities.3 In the MSK literature, self-efficacy is often described in the context of pain, meaning the capacity to achieve a goal or perform an activity in the presence of symptoms or pain and is often measured using the Pain Self-Efficacy Questionnaire (PSEQ).48 The constructs mentioned above certainly only scratch the surface in terms of those that are currently available for assessing psychological distress. This can become problematic in a psychologically informed orthopedic practice needing to screen for multiple domains of psychological distress without questionnaire burden.
The Optimal Screening for Prediction of Referral and Outcome–Yellow Flag (OSPRO-YF) is one questionnaire that helps to assess multiple domains related to negative mood, fear avoidance, and positive affect or coping.38 The OSPRO-YF was developed because pain-associated psychological distress is not routinely performed as a standard part of orthopedic practice and has been shown to play a role in the recovery of orthopedic injuries. The OSPRO -YF is comprised of 17 questions, which allow scores to be estimated from 11 commonly utilized patient questionnaires within the negative mood, fear avoidance, and positive affect or coping domains.38 The OSPRO-YF was established in neck, low back, shoulder, and knee populations.38 Despite the known psychological distresses that accompany MSK conditions, few researchers have incorporated this outcome tool to help identify patients with elbow or shoulder pain suffering from psychological stressors. One study conducted on patients with rotator cuff pathology found that higher fear-avoidance beliefs were associated with worse reported pain.37 Additionally, preoperative psychological distress, measured via the OSPRO-YF is prevalent in patients with rotator cuff tears who undergo surgical management.49 Patients undergoing shoulder surgery with higher preoperative and postoperative OSPRO-YF total scores had poor Patient-Reported Outcomes Measurement Information System pain interference and depression scores.33 These few studies are specific to the shoulder; to our knowledge, no study has investigated OSPRO-YF scores in a patient population experiencing elbow pain and compared scores to patients with shoulder pain. In fact, it is not uncommon for upper extremity injuries to be grouped together and analyzed which can hinder a clinician’s ability in choosing appropriate measurements tools that best represent the patient’s characteristics and diagnosis.42 Therefore, the primary purpose of this study is to evaluate the effect of body region (shoulder and elbow) and sex on baseline OSPRO-YF scores in patients with shoulder and elbow pain. The secondary purpose was to evaluate the association of age on baseline OSPRO-YF scores for both shoulder and elbow patients. It is hypothesized that there will be differences between body region and sex and significant relationships between age and baseline OSPRO-YF scores on both the shoulder and elbow cohorts.
Materials and methods
Study design
Data for this study were retrospectively pulled from a single-surgeon database within a multisurgeon prospective clinical data registry. Prospective data collection started in September 30th, 2022, and is currently ongoing. OSPRO-YF data were collected between September 30th 2022 and May 16th 2023. All data were collected at the participant's initial patient visit using REDCap (Research Electronic Data Capture; Vanderbilt University, Nashville, TN, USA) electronic data capture tools hosted by UTHealth's School of Biomedical Informatics.24,25 REDCap is a secure, web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources.24,25 All participants read and signed an electronic informed consent or assent form approved by The University of Texas Health Science Center at Houston (IRB approval #: HSC-MH-21-1041) prior to enrollment in the study.35
Participants
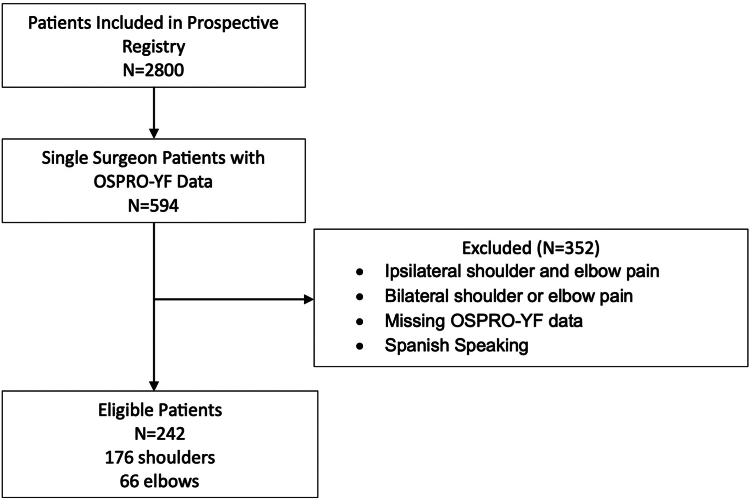
Participants included a total of 242 subjects (Figure 1) reporting with either shoulder or elbow pathology to a single surgeon in this clinical registry. 176 subjects reported shoulder pathology (89 males and 87 females, average age 51 ± 16 years; average height 170 ± 10 cm; average weight 83 ± 21 kgs; 70% Caucasian), while 66 subjects reported elbow pathology (42 males and 24 females, average age 45 ± 15 years; average height 175 ± 10 cm; average weight 88 ± 24 kgs; 80% Caucasian). Supplementary Appendix S1 provides the breakdown of initial encounter diagnosis for all included patients in both the shoulder and elbow cohorts. To meet inclusion criteria for this study, patients had to be between the ages of 18 and 90 years old and present with a primary complaint of either shoulder or elbow pain. Any subject between the ages of 18 and 90 years was included in the study, as the primary surgeon treats a wide variety of shoulder and elbow pathologies lending the practice to a mixture of different age ranges. Participants were excluded from this study if he or she complained of ipsilateral shoulder and elbow pain, bilateral shoulder or elbow pain, or English was not the primary speaking and reading language.
Figure 1.
Flowchart of screened, excluded, and included subjects. OSPRO-YF, Optimal Screening for Prediction of Referral and Outcome-Yellow Flag.
Procedures
All subjects reported to one board-certified, fellowship-trained orthopedic surgeon clinic (JG). Prior to meeting with the surgeon each subject completed a series of questionnaires: 1) a demographic survey and 2) the 17-item OSPRO-YF survey. The OSPRO-YF incorporates 3 different versions of a 7-question, 10-question, or 17-question scale related to 3 different domains as follows: negative mood, positive affect, and fear avoidance. This study incorporated the 17-item version, which has 85% accuracy, the highest of the 3 scales.38 The 17-item OSPRO-YF questionnaire estimates the individual scores of 11 PROMs and provides yellow flag indicators for each outcome via a regression model.38 Within the negative mood domain, estimated individual scores for the PHQ-9, STAI, and State-Trait Anger Expression Inventory (STAXI) are generated. Within the positive affect domain estimated scores on the PSEQ, Self-Efficacy for Rehabilitation (SER), and Chronic Pain Acceptance Questionnaire (CPAQ) are generated. Within the fear avoidance domain, estimated scores on the Fear Avoidance Beliefs Questionnaires (FABQ) (physical activity and work subscale [FABQ-W]), Pain Catastrophizing Scale, Tampa Scale of Kinesiophobia (TSK), and Pain Anxiety Symptom Scale.38 The interpretation of these 11 outcome measures can be found in Table I.
Table I.
Interpretation of the 11 patient outcomes scores that are predicted from the OSPRO-YF.
| Outcome measure | Psychological construct | Score range | Score interpretation |
|---|---|---|---|
| Negative mood | |||
| PHQ-9 | Depression | 0-27 | Higher score = elevated depression symptoms |
| STAI | Anxiety | 20-80 | Higher score = elevated anxiety symptoms |
| STAXI | Anger | 10-40 | Higher score = elevated levels of anger |
| Positive affect | |||
| PSEQ | Pain-related self-efficacy | 0-60 | Higher score = elevated or stronger levels of pain-related self-efficacy |
| SER | Self-efficacy for rehabilitation | 0-120 | Higher score = elevated self-efficacy during rehabilitation |
| CPAQ | Pain acceptance | 0-120 | Higher score = elevated levels of pain acceptance |
| Fear avoidance | |||
| FABQ-PA | Fear avoidance | 0-24 | Higher score = elevated levels of fear avoidance |
| FABQ-W | Fear avoidance | 0-42 | Higher score = elevated levels of fear avoidance |
| PCS | Pain catastrophizing | 0-52 | Higher score = elevated levels of pain catastrophizing |
| TSK-11 | Fear of movement | 11-44 | Higher score = elevated fear of movement |
| PASS-20 | Pain-related anxiety | 0-100 | Higher score = elevated symptoms of pain-related anxiety |
PHQ-9, Patient Health Questionnaire; STAI, State-Trait Anxiety Inventory; STAXI, State-Trait Anger Expression Inventory; PSEQ, Pain Self-Efficacy Questionnaire; SER, Self-Efficacy For Rehabilitation; CPAQ, Chronic Pain Acceptance Questionnaire; FABQ, Fear Avoidance Beliefs Questionnaires (FABQ) (physical activity (FABQ-PA) and work subscale (FABQ-W)); PSC, Pain Catastrophizing Scale; TSK-11, Tampa Scale Of Kinesiophobia; PASS-20, Pain Anxiety Symptom Scale; OSPRO-YF, Optimal Screening for Prediction of Referral and Outcome-Yellow Flag.
Statistical analysis
In order to assess the effects of body region and sex on the OSPRO-YF, one multivariate generalized linear model was conducted. All assumptions were met in order to run this statistical test: linearity, homoskedasticity, normality, independence of errors, and independence of independent variables. Body regions and sex were categorized as predictor variables, while the 11 predicted OSPRO-YF scores were considered the dependent variables. An alpha level of P < .05 was considered significant for the multivariate multiple regression, P values reaching < .01 were also documented within the results. To help guide the magnitude of the effect, the results partial eta squared (ηp2) statistics were provided. Partial eta squared statistics can be interpreted as 0.01 as a small effect, 0.06 as a medium effect, and 0.14 as large effect.12
To assess the effects of age on the OSPRO-YF, 11 simple linear regressions were conducted for each subscale of the OSPRO-YF for both the shoulder and elbow, where age was the predictor variable and OSPRO-YF subscales were the dependent variables. The R2 value was used to interpret how much of the variance in the dependent variable is explained by the independent variable (age). All assumptions were met in order to run this statistical test: independence of observations, continuous independent and dependent variables, no significant outliers, and normality. With the wide variety of age ranges in both the shoulder and elbow cohort, other potential cofounders, such as sex and BMI, were held constant.
The reliability of the OSPRO-YF in a pathological shoulder population has been previously documented in the literature.52 To our knowledge, this is the first study examining the OSPRO-YF in a pathological elbow population; thus, test-retest reliability for the total OSPRO score (sum of all 17-item questions), each of the subscales negative mood (sum of items 1-6), fear avoidance (sum of items 7-12) and positive affect (sum of items 13-17), and each of the predicted scores from the 11 outcomes were investigated.6 Test-retest reliability was analyzed using the Intraclass Correlation Coefficient (ICC2,1), with 95% confidence intervals on 45 patients undergoing elbow surgery. The analysis compared the 6-week OSPRO score to the 12-week OSPRO score. Reliability was interpreted as excellent (ICC values > 0.90), good (ICC values = 0.75-0.90), and moderate (ICC values = 0.5-0.75).51 All data were analyzed using statistical package SPSS version 29 (IBM Corp., Armonk, NY, USA).
Results
The test-retest reliability results are presented in Table II. In summary, the reliability for the 11 subscales generated moderate-to-good results in all but one subscale, PSEQ. When analyzing the reliability of the 3 psychological constructs, all but the positive affect construct revealed accepted reliability.
Table II.
Test-retest reliability across different OSPRO-YF scores.
| Reliability construct | ICC (95% CI) | Interpretation |
|---|---|---|
| Total OSPRO score | 0.71 (0.43-0.85) | Moderate |
| Negative mood subscale score | 0.78 (0.59-0.88) | Good |
| Fear-avoidance subscale score | 0.66 (0.34-0.82) | Moderate |
| Positive affect subscale score | 0.43 (−0.33-0.68) | Poor |
| PHQ-9 | 0.82 (0.67-0.90) | Good |
| STAI | 0.75 (0.54-0.85) | Good |
| STAXI | 0.82 (0.67-0.90) | Good |
| PSEQ | 0.44 (0.002-0.69) | Poor |
| SER | 0.66 (0.37-0.81) | Moderate |
| CPAQ | 0.64 (0.37-0.80) | Moderate |
| FABQ-PA | 0.67 (0.31-0.88) | Moderate |
| FABQ-W | 0.53 (0.13-0.74) | Moderate |
| PCS | 0.78 (0.59-0.88) | Good |
| TSK-11 | 0.72 (0.49-0.85) | Moderate |
| PASS-20 | 0.70 (0.45-0.84) | Moderate |
PHQ-9, Patient Health Questionnaire; STAI, State-Trait Anxiety Inventory; STAXI, State-Trait Anger Expression Inventory; PSEQ, Pain Self-Efficacy Questionnaire; SER, Self-Efficacy for Rehabilitation; CPAQ, Chronic Pain Acceptance Questionnaire; FABQ, Fear Avoidance Beliefs Questionnaires (FABQ) (physical activity (FABQ-PA) and work subscale (FABQ-W)); PSC, Pain Catastrophizing Scale; TSK-11, Tampa Scale of Kinesiophobia; PASS-20, Pain Anxiety Symptom Scale; OSPRO-YF, Optimal Screening for Prediction of Referral and Outcome-Yellow Flag.
Body region had a significant effect on FABQ-W, F (1, 203) = 7.400, P = .007, ηp2 = 0.035. In addition, body region had a significant effect on PSEQ, F (1, 203) = 4.532, P = 0.034, ηp2 = 0.022. Body region also had a significant effect on the SER subscale, F (1, 203) = 6.129, P = .014, ηp2 = 0.030. There was no significant main effect for sex nor was there a significant interaction for body region and sex on the OSPRO-YF (Table III).
Table III.
Means and (standard deviations) for the main effects of body region and sex on the OSPRO subscales.
| Outcome measure | Body region |
Sex |
||
|---|---|---|---|---|
| Elbow | Shoulder | Men | Women | |
| FABQ-W | 14.862∗∗ (10.573) | 11.002∗∗ (8.344) | 12.174 (8.933) | 11.909 (9.379) |
| PHQ-9 | 4.922 (3.516) | 4.512 (3.876) | 4.321 (3.666) | 4.931 (3.884) |
| STAI | 35.038 (8.717) | 33.636 (8.267) | 34.292 (8.941) | 33.741 (7.850) |
| STAXI | 13.672 (2.751) | 13.991 (3.224) | 14.040 (3.162) | 13.768 (3.047) |
| FABQ-PA | 16.565 (6.295) | 15.659 (6.451) | 16.531 (6.145) | 15.262 (6.631) |
| PCS | 15.415 (9.467) | 16.182 (9.956) | 16.211 (10.125) | 15.735 (9.521) |
| TSK-11 | 24.128 (5.724) | 24.599 (5.719) | 24.146 (5.786) | 24.804 (5.642) |
| PASS-20 | 34.949 (18.921) | 33.882 (18.533) | 32.695 (19.058) | 35.673 (18.087) |
| PSEQ | 35.205∗ (12.643) | 38.982∗ (11.553) | 38.556 (11.717) | 37.360 (12.199) |
| SER | 93.660∗ (23.760) | 100.436∗ (16.200) | 98.971 (18.980) | 98.240 (18.547) |
| CPAQ | 65.092 (16.673) | 68.326 (16.271) | 69.435 (15.143) | 65.434 (17.438) |
PHQ-9, Patient Health Questionnaire; STAI, State-Trait Anxiety Inventory; STAXI, State-Trait Anger Expression Inventory; PSEQ, Pain Self-Efficacy Questionnaire; SER, Self-Efficacy for Rehabilitation; CPAQ, Chronic Pain Acceptance Questionnaire; FABQ, Fear Avoidance Beliefs Questionnaires (FABQ) (physical activity (FABQ-PA) and work subscale (FABQ-W)); PSC, Pain Catastrophizing Scale; TSK-11, Tampa Scale of Kinesiophobia; PASS-20, Pain Anxiety Symptom Scale; OSPRO, Optimal Screening for Prediction of Referral and Outcome.
∗P < .05, ∗∗P < .01.
When controlling for both sex and BMI within the elbow cohort, age was significantly associated with TSK-11 F (3, 62) = 3.022, P = .03, R2 = 0.12 and STAXI F (3, 62) = 3.051, P = .03, R2 = 0.13. Table IV provides the Beta coefficients for model significance. When considering the shoulder cohort, age was not associated with any of the OSPRO-YF subscales.
Table IV.
Summary of significant predictors of OSPRO-YF subscales when considering age and holding sex and BMI constant.
| Beta coefficients | Standard error | P value | |
|---|---|---|---|
| TSK-11 | |||
| Intercept | 28.42 | 3.491 | |
| Age | −0.127 | 0.045 | .007 |
| STAXI | |||
| Intercept | 17.861 | 1.922 | |
| Age | −0.073 | 0.025 | .005 |
TSK-11, Tampa Scale of Kinesiophobia; STAXI, State-Trait Anger Expression Inventory; OSPRO-YF, Optimal Screening for Prediction of Referral and Outcome-Yellow Flag.
Discussion
This study sought to determine how body region, sex, and age effect baseline predicted OSPRO-YF scores. The hypothesis for both aims was partially supported as certain psychological measures seem to be associated with body region and age. Breaking down the results by psychological constructs (negative mood, positive affect, and fear avoidance), positive affect and fear avoidance seem to be affected by body region. More specifically, those presenting to clinic with elbow pain exhibit higher fear-avoidance behavior than those reporting with shoulder pain. Those with elbow pain also presented with lower PSEQ and SER scores when compared to the shoulder cohort, meaning the elbow cohort had lower self-efficacy with respect to pain and rehabilitation.13,58 Sex had no association with the predicted OSPRO-YF scores. While body region did not seem to affect any of the negative mood constructs, interestingly, patients reporting with shoulder or elbow pain, despite his or her sex, reported PHQ-9 scores ranging from 0-4 to 5-9, signifying minimal-to-mild depression, respectively.34 When analyzing the elbow cohort only, a 1-year increase in age was associated with a 0.127 and 0.073 decrease in TSK-11 and STAXI score, respectively. Meaning, as age increases, the fear of movement (TSK-11) and anger (STAXI) seem to diminish. In fact, 12% and 13% of the variability in TSK-11 and STAXI scores can be explained by age while keeping sex and BMI constant. Equations, using age, can be used to predict a patients TSK-11 and STAXI score; however, it should be noted that other variables are also responsible for the variability in these scores based on the R2 values presented in the results.
Negative mood construct
The results of our study are similar to other published studies investigating constructs specific to negative mood. Across multiple pain conditions (low back, neck, shoulder, and knee) PHQ-9 and STAI-T (trait portion of the STAI) did not differ7; additionally, PHQ-9 did not differ between sexes in those undergoing total joint arthroplasty.55 In addition, our average baseline PHQ-9 score of 4.512 in patients presenting with shoulder pain and 4.922 in patients presenting with elbow pain is similar to the range of PHQ-9 scores in shoulder pain population in the literature (3.13-4.63).7,30 A PHQ-9 score of 10 or greater is indicative of major depressive disorder and is used in many orthopedic studies as a baseline threshold for depression.8,27,34 It is informative to see minimal-to-mild depressive scores in this painful shoulder and elbow population. These baseline traits are important to assess in order to ensure optimal patient treatment strategy and outcomes.
Emotional regulation is an important determinant of well-being.23 Anger is a common emotional expression and is examined in the literature using the STAXI.18 There is evidence to support that aging is associated with improvements in emotional regulation and that older adults report lower levels of anger in everyday life when compared to the younger counterpart.22,36,46,53 It is a finding that would agree with the results of this study in individuals with elbow pain. While very few studies have assessed the effect of anger in MSK-related injures using the STAXI, the relationship of pain and anger has been investigated; however, the results are mixed. Authors have determined that appropriate anger regulation is associated with better pain outcomes in patients with low back pain.41 While another study conducted on patients >64 years old who had undergone a hip or knee replacement found no relationship between pain and state and trait anxiety.14
Positive affect construct
Self-efficacy describes the level of confidence a person has in their ability to achieve a desired outcome.48 The PSEQ explores an individual's beliefs in their ability to perform activities and manage pain effectively.48 Higher pain self-efficacy scores have been associated with less disability, pain, fatigue, and emotional distress in patients with MSK pain.44 While the elbow pain cohort had lower self-efficacy than patients presenting with shoulder pain, both scores were below 40, which may indicate low levels of pain self-efficacy.9 The PSEQ scores presented in this study seem to be in a similar range to those suffering from MSK pain.13 Low levels of pain self-efficacy have been documented across different shoulder cohorts,62 In fact, shoulder pain patients with a high pain self-efficacy reduce the risk of continued pain and disability at 6 months.9 The authors of this study were unable to find any existing literature on the elbow with regards to the PSEQ. However, the PSEQ-2 is associated with limitations 2-4 weeks after elbow fractures.31
The SER assess a person's ability to perform or succeed in a rehabilitation protocol and was initially developed for postoperative knee and hip surgeries.58 Baseline SER values are not established for either a shoulder or elbow population. The SER scale has been studied in a population undergoing anterior cruciate ligament (ACL) reconstruction. Higher self-efficacy reported within 4 weeks after ACL reconstruction was associated with better knee impairment resolution at 12 weeks.11 While not all the patients in our study underwent a surgical intervention the SER scores are higher when compared to baseline SER scores in patients undergoing ACL reconstructions.11 Further investigation is certainly required regarding SER scores in patients presenting with shoulder and elbow pain to fully characterize their value in clinical practice.
It is important to note the poor-to-moderate test-retest reliability scores in the PSEQ, SER, and positive affect subscale score within our study. A systematic review reporting on the measurement properties of the PSEQ in patients with MSK disorders document a weighted mean ICC of 0.86, ranging from 0.75 (moderate) to 0.93 (excellent).13
Fear avoidance
Fear-avoidance beliefs and pain experiences are significantly associated with one another, especially in chronic pain cases.19 This interaction between fear and pain leads to disability.19 Currently, there is no literature comparing the differences in FABQ scores between those with shoulder and elbow pathologies; these conditions are more commonly grouped together and analyzed as upper extremity injuries.28 Range of motion (ROM) demands at the elbow may be one possible explanation for the higher FABQ-W scores when compared to the shoulder cohort. More specifically, ROM in the elbow is critical for performing important activities of daily living, such as personal care, eating, and drinking, whereas full ROM in the shoulder is less important.50 If more elbow ROM and activity is needed for important activities of daily living than shoulder ROM, it may be likely for patients with elbow pain to have fear-avoidance behavior when the tasks they need to complete on a daily basis require full use of the elbow.
Kinesiophobia, the fear of movement or reinjury, as measured using the TSK-11, is another component of the fear avoidance construct. Many studies have been conducted using the TSK-11 in various MSK body regions, and the authors are unaware of a specific correlation between the TSK-11 and age in and elbow cohort, while several authors suggest no association between fear avoidance beliefs and age, a finding that is the same in this study.21 We do know that pain catastrophizing and depression are predictors of TSK in Dutch patients with chronic low back pain.57 This same study found no significant correlations between TSK and age.57 Similarly, other researchers have investigated kinesiophobia and associated factors in older patients with orthopedic conditions, such as total knee arthroplasty, finding no correlation between TSK and age.2 While the correlation was present in the study within the elbow cohort, the explained variance is low, meaning other variables may be more strongly predictive of TSK-11 scores in this upper extremity population.
This study is not without limitations. The patient population was diverse in that initial encounter diagnosis was variable in between patients within both the shoulder and elbow cohorts. The cohort included patients who were treated both operatively and nonoperatively; however, all data were collected prior to any surgical decision being made. Future research should consider surgical intervention as a factor when investigating psychological distress as it is not unreasonable to hypothesize that patient's surgical intervention might display different psychological profiles when compared to a nonsurgical cohort. The effect of psychological profiles on treatment success and long-term outcomes must also be considered. The reliability metrics for the positive affect construct for the elbow cohort ranged between poor and moderate. The lower ICCs in our study could be a direct result of the time frame in which the reliability results were collected, as the patient's attitude towards their new or updated treatment plan could have been altered. The racial profile of subjects in this study was over 70% White, and as a result, these baseline characteristics cannot be generalized across different races. Future studies should seek to assess baseline characteristics in a more racially diverse patient population. Patient medical history was not included within the study; therefore, variables such as prior history of depression or anxiety, medications, and alcohol or drug use were not included within the final analysis. Lastly, this study was comprised of more shoulder pain patients than elbow pain patients. However, this is to be expected as the MSK pain literature would support higher prevalence of shoulder pain when compared to elbow pain.59
Conclusion
The positive affect and fear avoidance domains of the OSPRO-YF seem to differ by body region. Patients presenting to clinic with elbow pain exhibit higher fear-avoidance behavior than those reporting with shoulder pain. Additionally, those with elbow pain also had lower self-efficacy with respect to pain and rehabilitation. While body region did not seem to affect any of the negative mood constructs, patients reporting with shoulder or elbow pain reported minimal-to-mild depression. Patients reporting with elbow pain seem to experience psychological barriers that may interfere with treatment prognosis. As such, these constructs of positive affect and fear avoidance should be further evaluated in patients suffering from elbow-related health conditions. By establishing psychological awareness in clinical settings, providers will be able to provide a comprehensive and patient-specific plan of care that accounts for these barriers.
Disclaimers
Funding: No grant funding was associated with this manuscript.
Conflicts of interest: James Gregory provides Arthrex/Stryker research support, consulting payments and Sparta Biomedical stock/stock options. None of these influence the contents discussed within this manuscript. The other authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article. No financial biases exist for any author in relation to this study.
Footnotes
The University of Texas Health Science Center at Houston (IRB approval #: HSC-MH-21-1041) approved this study.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2025.02.006.
Supplementary Data
References
- 1.Aben A., De Wilde L., Hollevoet N., Henriquez C., Vandeweerdt M., Ponnet K., et al. Tennis elbow: associated psychological factors. J Shoulder Elbow Surg. 2018;27:387–392. doi: 10.1016/j.jse.2017.11.033. [DOI] [PubMed] [Google Scholar]
- 2.Bakırhan S., Unver B., Elibol N., Karatosun V. Fear of movement and other associated factors in older patients with total knee arthroplasty. Ir J Med Sci. 2023;192:2217–2222. doi: 10.1007/s11845-022-03214-4. [DOI] [PubMed] [Google Scholar]
- 3.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Adv Behav Res Ther. 1978;1:139–161. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 4.BenDebba M., Torgerson W.S., Long D.M. Personality traits, pain duration and severity, functional impairment, and psychological distress in patients with persistent low back pain. Pain. 1997;72:115–125. doi: 10.1016/s0304-3959(97)00020-1. [DOI] [PubMed] [Google Scholar]
- 5.Bijker L., Sleijser-Koehorst M., Coppieters M., Cuijpers P., Scholten-Peeters G. Preferred self-administered questionnaires to assess depression, anxiety and somatization in people with musculoskeletal pain–a modified delphi study. J Pain. 2020;21:409–417. doi: 10.1016/j.jpain.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Butera K.A., George S.Z., Lentz T.A. Psychometric evaluation of the optimal screening for prediction of referral and outcome yellow flag (OSPRO-YF) tool: factor structure, reliability, and validity. J Pain. 2020;21:557–569. doi: 10.1016/j.jpain.2019.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Butera K.A., Lentz T.A., Beneciuk J.M., George S.Z. Preliminary evaluation of a modified start back screening tool across different musculoskeletal pain conditions. Phys Ther. 2016;96:1251–1261. doi: 10.2522/ptj.20150377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Catanzano A.A., Bastrom T.P., Bartley C.E., Yaszay B., Upasani V.V., Newton P.O. Depression screening in pediatric orthopedic surgery clinics and identifying patients at-risk. J Pediatr Orthop. 2024;10:1097. doi: 10.1097/BPO.0000000000002635. [DOI] [PubMed] [Google Scholar]
- 9.Chester R., Khondoker M., Shepstone L., Lewis J.S., Jerosch-Herold C. Self-efficacy and risk of persistent shoulder pain: results of a classification and regression tree (CART) analysis. Br J Sports Med. 2019;53:825–834. doi: 10.1136/bjsports-2018-099450. [DOI] [PubMed] [Google Scholar]
- 10.Chiarotto A., Terwee C.B., Ostelo R.W. Choosing the right outcome measurement instruments for patients with low back pain. Best Pract Res Clin Rheumatol. 2016;30:1003–1020. doi: 10.1016/j.berh.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Chmielewski T.L., George S.Z. Fear avoidance and self-efficacy at 4 weeks after ACL reconstruction are associated with early impairment resolution and readiness for advanced rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2019;27:397–404. doi: 10.1007/s00167-018-5048-6. [DOI] [PubMed] [Google Scholar]
- 12.Cohen J. 2nd edition. Lawrence Erlbaum; New York, NY: 1988. Stastical power analysis for the behavioral sciences. [Google Scholar]
- 13.Dube M.O., Langevin P., Roy J.S. Measurement properties of the pain self-efficacy questionnaire in populations with musculoskeletal disorders: a systematic review. Pain Rep. 2021;6 doi: 10.1097/PR9.0000000000000972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feeney S.L. The relationship between pain and negative affect in older adults: anxiety as a predictor of pain. J Anxiety Disord. 2004;18:733–744. doi: 10.1016/j.janxdis.2001.04.001. [DOI] [PubMed] [Google Scholar]
- 15.Fennelly O., Blake C., Desmeules F., Stokes D., Cunningham C. Patient-reported outcome measures in advanced musculoskeletal physiotherapy practice: a systematic review. Musculoskeletal Care. 2018;16:188–208. doi: 10.1002/msc.1200. [DOI] [PubMed] [Google Scholar]
- 16.Fernández-de-Las-Peñas C., Florencio L.L., de-la-Llave-Rincón A.I., Ortega-Santiago R., Cigarán-Méndez M., Fuensalida-Novo S., et al. Prognostic factors for postoperative chronic pain after knee or hip replacement in patients with knee or hip osteoarthritis: an umbrella review. J Clin Med. 2023;12:6624. doi: 10.3390/jcm12206624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferreira-Valente A., Queiroz-Garcia I., Pais-Ribeiro J., Jensen M.P. Pain diagnosis, pain coping, and function in individuals with chronic musculoskeletal pain. J Pain Res. 2020;13:783–794. doi: 10.2147/JPR.S236157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forgays D.G., Forgays D.K., Spielberger C.D. Factor structure of the state-trait anger expression inventory. J Pers Assess. 1997;69:497–507. doi: 10.1207/s15327752jpa6903_5. [DOI] [PubMed] [Google Scholar]
- 19.Gatchel R.J., Neblett R., Kishino N., Ray C.T. Fear-avoidance beliefs and chronic pain. J Orthop Sports Phys Ther. 2016;46:38–43. doi: 10.2519/jospt.2016.0601. [DOI] [PubMed] [Google Scholar]
- 20.Gatchel R.J., Polatin P.B., Mayer T.G. The dominant role of psychosocial risk factors in the development of chronic low back pain disability. Spine. 1995;20:2702–2709. doi: 10.1097/00007632-199512150-00011. [DOI] [PubMed] [Google Scholar]
- 21.González Aroca J., Díaz Á.P., Navarrete C., Albarnez L. Fear-avoidance beliefs are associated with pain intensity and shoulder disability in adults with chronic shoulder pain: a cross-sectional study. J Clin Med. 2023;12:3376. doi: 10.3390/jcm12103376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gross J.J., Carstensen L.L., Pasupathi M., Tsai J., Götestam Skorpen C., Hsu A.Y. Emotion and aging: experience, expression, and control. Psychol Aging. 1997;12:590. doi: 10.1037//0882-7974.12.4.590. [DOI] [PubMed] [Google Scholar]
- 23.Gross J.J., John O.P. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- 24.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O'Neal L., et al. The redcap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hopman-Rock M., Odding E., Hofman A., Kraaimaat F.W., Bijlsma J.W. Physical and psychosocial disability in elderly subjects in relation to pain in the hip and/or knee. J Rheumatol. 1996;23:1037–1043. [PubMed] [Google Scholar]
- 27.Hoshino E., Ohde S., Rahman M., Takahashi O., Fukui T., Deshpande G.A. Variation in somatic symptoms by patient health questionnaire-9 depression scores in a representative Japanese sample. BMC Public Health. 2018;18:1–10. doi: 10.1186/s12889-018-6327-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Inrig T., Amey B., Borthwick C., Beaton D. Validity and reliability of the fear-avoidance beliefs questionnaire (FABQ) in workers with upper extremity injuries. J Occup Rehabil. 2012;22:59–70. doi: 10.1007/s10926-011-9323-3. [DOI] [PubMed] [Google Scholar]
- 29.Jakobsson M., Hagströmer M., Lotzke H., von Rosen P., Lundberg M. Fear of movement was associated with sedentary behaviour 12 months after lumbar fusion surgery in patients with low back pain and degenerative disc disorder. BMC Musculoskelet Disord. 2023;24:874. doi: 10.1186/s12891-023-06980-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Janela D., Costa F., Molinos M., Moulder R.G., Lains J., Francisco G.E., et al. Asynchronous and tailored digital rehabilitation of chronic shoulder pain: a prospective longitudinal cohort study. J Pain Res. 2022;15:53–66. doi: 10.2147/JPR.S343308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jayakumar P., Teunis T., Vranceanu A.-M., Moore M.G., Williams M., Lamb S., et al. Psychosocial factors affecting variation in patient-reported outcomes after elbow fractures. J Shoulder Elbow Surg. 2019;28:1431–1440. doi: 10.1016/j.jse.2019.04.045. [DOI] [PubMed] [Google Scholar]
- 32.Khatib Y., Madan A., Naylor J.M., Harris I.A. Do psychological factors predict poor outcome in patients undergoing TKA? A systematic review. Clin Orthop Relat Res. 2015;473:2630–2638. doi: 10.1007/s11999-015-4234-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim B.I., Wu K.A., Luo E.J., Morriss N.J., Cabell G.H., Lentz T.A., et al. Correlation between the optimal screening for prediction of referral and outcome yellow flag tool and patient-reported legacy outcome measures in patients undergoing shoulder surgery. JSES Int. 2024;8:1115–1121. doi: 10.1016/j.jseint.2024.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lawrence C.E., Dunkle L., McEver M., Israel T., Taylor R., Chiriboga G., et al. A REDCap-based model for electronic consent (eConsent): moving toward a more personalized consent. J Clin Transl Sci. 2020;3:345–353. doi: 10.1017/cts.2020.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lawton M.P., Kleban M.H., Rajagopal D., Dean J. Dimensions of affective experience in three age groups. Psychol Aging. 1992;7:171. doi: 10.1037//0882-7974.7.2.171. [DOI] [PubMed] [Google Scholar]
- 37.Lemaster N.G., Hettrich C.M., Jacobs C.A., Heebner N., Westgate P.M., Mair S., et al. Which risk factors are associated with pain and patient-reported function in patients with a rotator cuff tear? Clin Orthop Relat Res. 2021;479:1982–1992. doi: 10.1097/CORR.0000000000001750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lentz T.A., Beneciuk J.M., Bialosky J.E., Zeppieri G., Jr., Dai Y., Wu S.S., et al. Development of a yellow flag assessment tool for orthopaedic physical therapists: results from the optimal screening for prediction of referral and outcome (OSPRO) cohort. J Orthop Sports Phys Ther. 2016;46:327–343. doi: 10.2519/jospt.2016.6487. [DOI] [PubMed] [Google Scholar]
- 39.Lentz T.A., George S.Z., Manickas-Hill O., Malay M.R., O’Donnell J., Jayakumar P., et al. What general and pain-associated psychological distress phenotypes exist among patients with hip and knee osteoarthritis? Clin Orthop Relat Res. 2020;478:2768. doi: 10.1097/CORR.0000000000001520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Løchting I., Garratt A.M., Storheim K., Werner E.L., Grotle M. The impact of psychological factors on condition-specific, generic and individualized patient reported outcomes in low back pain. Health Qual Life Out. 2017;15:1–9. doi: 10.1186/s12955-017-0593-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lombardo E.R., Tan G., Jensen M.P., Anderson K.O. Anger management style and associations with self-efficacy and pain in male veterans. J Pain. 2005;6:765–770. doi: 10.1016/j.jpain.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 42.MacDermid J.C., Valdes K., Szekeres M., Naughton N., Algar L. The assessment of psychological factors on upper extremity disability: a scoping review. J Hand Ther. 2018;31:511–523. doi: 10.1016/j.jht.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 43.Marks R. Physical and psychological correlates of disability among a cohort of individuals with knee osteoarthritis. Can J Aging. 2007;26:367–377. doi: 10.3138/cja.26.4.367. [DOI] [PubMed] [Google Scholar]
- 44.Martinez-Calderon J., Flores-Cortes M., Morales-Asencio J.M., Fernandez-Sanchez M., Luque-Suarez A. Which interventions enhance pain self-efficacy in people with chronic musculoskeletal pain? A systematic review with meta-analysis of randomized controlled trials, including over 12,000 participants. J Orthop Sports Phys Ther. 2020;50:418–430. doi: 10.2519/jospt.2020.9319. [DOI] [PubMed] [Google Scholar]
- 45.Martinez-Calderon J., Jensen M.P., Morales-Asencio J.M., Luque-Suarez A. Pain catastrophizing and function in individuals with chronic musculoskeletal pain. Clin J Pain. 2019;35:279–293. doi: 10.1097/AJP.0000000000000676. [DOI] [PubMed] [Google Scholar]
- 46.McConatha J.T., Leone F.M., Armstrong J.M. Emotional control in adulthood. Psychol Rep. 1997;80:499–507. doi: 10.2466/pr0.1997.80.2.499. [DOI] [PubMed] [Google Scholar]
- 47.Menendez M.E., Baker D.K., Oladeji L.O., Fryberger C.T., McGwin G., Ponce B.A. Psychological distress is associated with greater perceived disability and pain in patients presenting to a shoulder clinic. J Bone Joint Surg Am. 2015;97:1999–2003. doi: 10.2106/JBJS.O.00387. [DOI] [PubMed] [Google Scholar]
- 48.Nicholas M.K. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. 2007;11:153–163. doi: 10.1016/j.ejpain.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 49.Okafor C., Levin J.M., Boadi P., Cook C., George S., Klifto C., et al. Pain associated psychological distress is more strongly associated with shoulder pain and function than tear severity in patients undergoing rotator cuff repair. JSES Int. 2023;7:544–549. doi: 10.1016/j.jseint.2023.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oosterwijk A.M., Nieuwenhuis M.K., van der Schans C.P., Mouton L.J. Shoulder and elbow range of motion for the performance of activities of daily living: a systematic review. Physiother Theory Pract. 2018;34:505–528. doi: 10.1080/09593985.2017.1422206. [DOI] [PubMed] [Google Scholar]
- 51.Portney L.G., Watkins A.L. Prentice Hall; Philadelphia, PA: 2000. Foundations of clinical research applications to practice. [Google Scholar]
- 52.Razmjou H., Palinkas V., Robarts S., Kennedy D. Psychometric properties of the OSPRO–YF screening tool in patients with shoulder pathology. Physiother Can. 2021;73:26–36. doi: 10.3138/ptc-2019-0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schieman S. Age and anger. J Health Soc Behav. 1999;43:273–289. [PubMed] [Google Scholar]
- 54.Terradas-Monllor M., Ruiz M.A., Ochandorena-Acha M. Postoperative psychological predictors for chronic postsurgical pain after a knee arthroplasty: a prospective observational study. Phys Ther. 2023;104 doi: 10.1093/ptj/pzad141. [DOI] [PubMed] [Google Scholar]
- 55.Trinh J.Q., Carender C.N., An Q., Noiseux N.O., Otero J.E., Brown T.S. Resilience and depression influence clinical outcomes following primary total joint arthroplasty. J Arthoplasty. 2021;36:1520–1526. doi: 10.1016/j.arth.2020.11.032. [DOI] [PubMed] [Google Scholar]
- 56.Vissers M.M., Bussmann J.B., Verhaar J.A., Busschbach J.J., Bierma-Zeinstra S.M., Reijman M. Psychological factors affecting the outcome of total hip and knee arthroplasty: a systematic review. Semin Arthritis Rheum. 2012;41:576–588. doi: 10.1016/j.semarthrit.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 57.Vlaeyen J.W., Kole-Snijders A.M., Boeren R.G., Van Eek H. Fear of movement/(re) injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62:363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 58.Waldrop D., Lightsey O.R., Jr., Ethington C.A., Woemmel C.A., Coke A.L. Self-efficacy, optimism, health competence, and recovery from orthopedic surgery. J Couns Psychol. 2001;48:233. [Google Scholar]
- 59.Walker-Bone K., Palmer K.T., Reading I., Coggon D., Cooper C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum. 2004;51:642–651. doi: 10.1002/art.20535. [DOI] [PubMed] [Google Scholar]
- 60.Wertli M.M., Held U., Lis A., Campello M., Weiser S. Both positive and negative beliefs are important in patients with spine pain: findings from the occupational and industrial orthopaedic center registry. Spine J. 2018;18:1463–1474. doi: 10.1016/j.spinee.2017.07.166. [DOI] [PubMed] [Google Scholar]
- 61.Westman A.E., Boersma K., Leppert J., Linton S.J. Fear-avoidance beliefs, catastrophizing, and distress: a longitudinal subgroup analysis on patients with musculoskeletal pain. Clin J Pain. 2011;27:567–577. doi: 10.1097/AJP.0b013e318219ab6c. [DOI] [PubMed] [Google Scholar]
- 62.White R.J., Olds M., Cadogan A., Betteridge S., Sole G. Shoulder pain, disability and psychosocial dimensions across diagnostic categories: profile of patients attending shoulder physiotherapy clinics. NZ J Physiother. 2022;50:6–13. doi: 10.15619/NZJP/50.1.02. [DOI] [Google Scholar]
- 63.Williamson E. Fear avoidance beliefs questionnaire (FABQ) Aust J Physiother. 2006;52:149. doi: 10.1016/s0004-9514(06)70052-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.