Abstract
Objective:
Acromioclavicular (AC) joint instability remains a challenging clinical problem, particularly in chronic cases where both vertical and horizontal stability must be restored. Traditional techniques have limitations in addressing multidirectional instability and minimizing implant-related complications.
The aim of this study was to evaluate the clinical and radiological outcomes of a combined coracoclavicular (CC) ligament and transacromial capsule reconstruction technique in patients with chronic AC joint instability.
Methods:
A retrospective study was performed on 40 patients who underwent AC joint reconstruction at a single center from 2019 to 2023. Radiological outcomes (clavicle-coracoid distance) were evaluated preoperatively, immediately postoperatively, and at the last follow-up (6 months). Functional results were assessed using the Constant, American Shoulder and Elbow Surgeons score (ASES), and Disabilities of the Arm, Shoulder, and Hand (DASH) score. Data were analyzed using SPSS v28.0. T-tests and repeated measures of Analysis of Variance (ANOVA) were employed to compare outcomes, with significance set at P < .05.
Results:
The preoperative mean CC distance was 20.3 ± 3.4 mm. Early postoperative measurements showed a significant reduction in CC distance, with a mean of 9.5 ± 1.5 mm in the capsule reconstruction group compared to 10.5 ± 1.6 mm in the non-reconstruction group (P = .053). At the 6-month follow-up, the late postoperative CC distance was maintained at 10.1 ± 1.6 mm in the reconstruction group, while it increased to 14.4 ± 2.0 mm in the non-reconstruction group (P < .001). The mean ASES score was 87.1 ± 8.1. The mean Constant score was 86.2 ± 7.6. Pain levels, evaluated using the Visual Analog Scale (VAS), decreased from a mean of 5.8 ± 1.2 preoperatively to 2.1 ± 1.0 postoperatively, indicating significant pain relief and improved functionality. No hardware failure or infection was noted. About 12.5% of patients experienced short-term anterior knee pain.
Conclusion:
The results of this study demonstrate that combined CC ligament and transacromial capsule reconstruction improves radiographic outcomes by maintaining the clavicle-coracoid distance and enhances functional scores (ASES and Constant) in patients with chronic AC joint instability. Addressing both vertical and horizontal instability appears to contribute to better short-term clinical recovery. Further studies with larger sample sizes and longer follow-up are needed to confirm these findings.
Level of evidence:
Level III (Retrospective Comparative Study).
Keywords: Acromioclavicular joint reconstruction, chronic AC joint injuries, coracoclavicular ligament reconstruction, semitendinosus tendon autograft, transacromial capsule reconstruction
Highlights
Early postoperative mobilization is feasible with this technique, allowing patients to begin rehabilitation as early as the first postoperative day.
The combined reconstruction approach provides enhanced horizontal and vertical joint stability compared to conventional techniques.
Patients demonstrated significantly improved functional outcomes, reflected by higher ASES and Constant scores in the reconstruction group.
The clavicle-coracoid distance was effectively maintained at the six-month follow-up, with statistically significant differences favoring the reconstruction group.
The technique is associated with a low complication rate and offers advantages in biological compatibility due to the use of autologous grafts.
.
Introduction
The acromioclavicular (AC) joint is fundamental for shoulder function, bridging the clavicle and scapula to aid in important upper limb activities. Injuries frequently occur in active individuals due to trauma or falls.1,2 The AC joint’s significance in diagnosis and treatment is underscored by its support of 3 key ligaments: the AC, coracoclavicular (CC) and coracoacromial ligaments. These ligaments provide vertical support and maintain stability under varying stresses.3 The joint’s gliding motion enhances shoulder flexibility and power, facilitating reaching, lifting and throwing activities.4 With over 40% of shoulder injuries attributed to AC joint issues, the necessity for preventive measures in sports medicine is evident.5
The Rockwood classification categorizes AC joint separations from mild sprains (type I) to complete dislocations with associated ligament damage (type VI).1 While types I and II are generally managed conservatively, more severe injuries (types III-VI) often require surgical intervention to restore anatomical alignment and joint stability.3 Surgical techniques such as the Weaver–Dunn procedure, CC ligament reconstructions using synthetic or autograft materials and TightRope systems have been developed.6 However, challenges like reduction loss, hardware failure and persistent pain persist, emphasizing the need for more reliable solutions.7-9
The semitendinosus tendon is used in a modified method to reconstruct CC ligaments and the AC joint capsule, enhancing joint stability by integrating ligament reconstruction with soft tissue repair. This biocompatibility approach minimizes complications such as infection or adverse foreign body responses associated with synthetic materials. Unlike the technique first described by Mazzocca et al in 2004,10 which required 2 acromial tunnels, this approach uses a single tunnel, potentially reducing risks of deltoid weakness, postoperative pain and acromial fractures. Similar techniques using free tendon grafts and low-profile implants for chronic AC joint instability have also been described by Kraus et al (2019)11 and Dittrich et al (2020).12 Previous studies have reported a complication rate of approximately 20% for the modified Weaver–Dunn procedure, which relies on coracoacromial ligament transfer without addressing horizontal instability.7,13 In contrast, double endobutton techniques have shown higher success rates with functional improvement rates exceeding 85%, but they are associated with hardware-related complications such as migration and irritation.14 Additionally, hook plates, while effective in achieving initial stability, demonstrate a loss of reduction rate of up to 16% and require secondary surgery for implant removal.15
This study aims to describe the modified surgical technique, evaluate its clinical and radiological outcomes and compare its efficacy with existing methods. By integrating ligament and capsule reconstruction through a biocompatible approach, the technique seeks to improve functional recovery and minimize donor site morbidity, offering a reproducible solution for managing complex AC joint injuries.
Material and methods
This comprehensive retrospective study involved 40 patients who underwent surgical reconstruction of the AC joint utilizing semitendinosus tendon grafts between 2019 and 2023 at a single medical institution. The same skilled surgeon performed all surgical procedures to ensure consistency in technique and outcomes. This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Ethical approval was obtained from the Dokuz Eylul University Local Ethics Committee (Approval No: 2025/04-10 Date: 5.02.2025). Written informed consent was obtained from all patients before participation and all patient data were anonymized to ensure confidentiality and compliance with ethical standards. This retrospective cohort study was conducted and reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. No financial incentives or conflicts of interest influenced the study design, data collection or analysis.
The surgical interventions involved using either a hook plate or an endobutton system based on a shared decision-making process with the patients. This approach ensured that all available techniques were thoroughly explained to the patients, allowing them to make informed decisions without surgeon bias. Specifically, hook plates were used in 9 patients, of whom 6 underwent reconstruction, while endobutton systems were used in 28 patients, with reconstruction performed in 15 cases. Additionally, in 3 patients, reconstruction was performed without an implant. Notably, all hook plates were removed within 3-6 months postoperatively. All patients presented with injuries at least 1 month old, which qualifies all cases as chronic. This delay was attributable to the institution being a tertiary referral center, where patients often first sought care at external facilities. The subsequent referral process to the center, combined with preoperative evaluations and scheduling, typically extended the time to surgical intervention to approximately 1 month.
To evaluate the outcomes of the surgical interventions, radiological assessments were systematically conducted at 4 distinct stages: prior to the operation (preoperative), immediately post-operative (day 0), 6 months after the surgery (corresponding with the time of implant removal) and during the final follow-up appointment. The CC distance, a critical measurement for assessing the reduction and stability of the joint, was meticulously measured at each of these time points to provide a comprehensive understanding of the surgical results and joint functionality.
Statistical analysis
The statistical analysis utilized IBM SPSS Statistics for Windows, Version 28.0 (IBM SPSS Corp.; Armonk, NY, USA) to systematically evaluate patient demographics and clinical outcomes. Descriptive statistics included means, medians, standard deviations, minimum and maximum values for continuous variables, and frequencies and percentages for categorical variables. A power analysis was performed before data analysis to assess the sufficiency of the sample size and detect significant differences. Based on the observed effect size (Cohen’s d = 2.37) for the primary outcome (late postoperative CC distance), the achieved power was calculated as >95% using Gpower V 3.1.9.7, confirming that the sample size was sufficient for between-group comparisons. The normality of data distribution was evaluated through the Kolmogorov–Smirnov and Shapiro–Wilk tests. In light of these findings: the independent samples t-test was utilized to compare 2 independent groups. Repeated Measures ANOVA was employed for longitudinal comparisons, utilizing the Huynh–Feldt correction when the assumption of sphericity was not met. A P-value of lower than .05 was considered statistically significant.
Surgical technique
Patient selection
This technique was applied to patients with chronic AC joint separations classified as Rockwood types III-VI. The inclusion criteria were patients with significant functional impairment, pain, and radiographic evidence of joint instability. Exclusion criteria included active infections, pediatric population, severe osteoporosis, or prior surgical interventions at the AC joint. Each patient provided informed consent after being briefed about the procedure and its potential risks and benefits.
Preoperative preparation
All patients underwent standard preoperative x-rays (Figure 1), and MRI was performed selectively in cases with suspected additional soft tissue injuries. A complete assessment of shoulder range of motion, strength, and neurovascular status was performed. The unilateral knee was also evaluated to ensure its suitability for graft harvesting.
Figure 1.
Preoperative shoulder AP x-ray.
Surgical technique
1. Anesthesia and positioning
The procedure was performed under general anesthesia, with the patient placed in a beach chair position. The operative shoulder and unilateral knee were prepped and draped sterilely.
2. Tendon harvesting
A 4-cm longitudinal incision was made over the pes anserine to harvest the semitendinosus tendon. After careful dissection and release of its distal attachment, the tendon was extracted using a tendon stripper, cleaned of muscle tissue, and prepared on the back table. It was folded longitudinally, reinforced with non-absorbable sutures and pre-tensioned with a 25 N load for 10 minutes to minimize postoperative elongation. The graft was kept hydrated in sterile saline-soaked gauze until implantation.
3. Acromioclavicular joint exposure
A transverse incision was made over the AC joint. The joint capsule and deltotrapezial fascia were carefully dissected to expose the joint while maintaining soft tissue integrity.
4. Reduction and fixation
Anatomic reduction of the AC joint was achieved through open manipulation. In many cases, temporary reduction was achieved by introducing a K-wire from the acromion to the clavicle, allowing reconstruction to proceed without the need for permanent implants. The absence of permanent implants such as hook plates or endobuttons offers a significant benefit by avoiding hardware-related complications, such as migration, irritation, or the need for secondary removal surgeries, while still providing sufficient support for the graft during the early phases of healing.
For patients with greater functional demands, such as athletes, more secure fixation methods were used to ensure long-term stability and support early rehabilitation. Endobutton systems or hook plates were selectively utilized to protect the graft from excessive stress during the critical remodeling period. By maintaining reduction and supporting the graft, they allow controlled early mobilization, which is particularly beneficial for patients needing to return to high activity levels.
5. Coracoclavicular ligament reconstruction
Before tunnel placement, the coracoid process is carefully exposed using blunt dissection to separate it from the surrounding soft tissues while meticulously preserving the adjacent neurovascular structures. Once adequately exposed, a Satinsky clamp is used to pass from medial to lateral beneath the coracoid process. The suture attached to one end of the graft is then pulled through, looping the graft securely around the inferior aspect of the coracoid. This step ensures the graft is positioned correctly and anchored before proceeding to bone tunnel creation.
Accurate placement of bone tunnels is crucial for replicating the anatomical configuration of the CC ligaments. Complex osteological measurements serve as a guide rather than absolute markers to assist in locating the insertions of the conoid and trapezoid ligaments. A cannulated reamer guide pin is used for tunnel creation. The conoid tunnel is positioned approximately 45 mm from the distal clavicle, along its posterior half, ensuring placement near the ligament’s posterior footprint. The guide pin is angled at approximately 45° to match the ligament’s oblique orientation, and a 6 or 7-mm reamer is used to create a 15-16 mm-long tunnel while avoiding cortical breach. For the trapezoid ligament, the tunnel is created more anteriorly, approximately 15 mm from the conoid tunnel and centered within the clavicle. Two guide pins are placed initially to ensure accurate alignment, followed by reaming through the entire width of the clavicle.
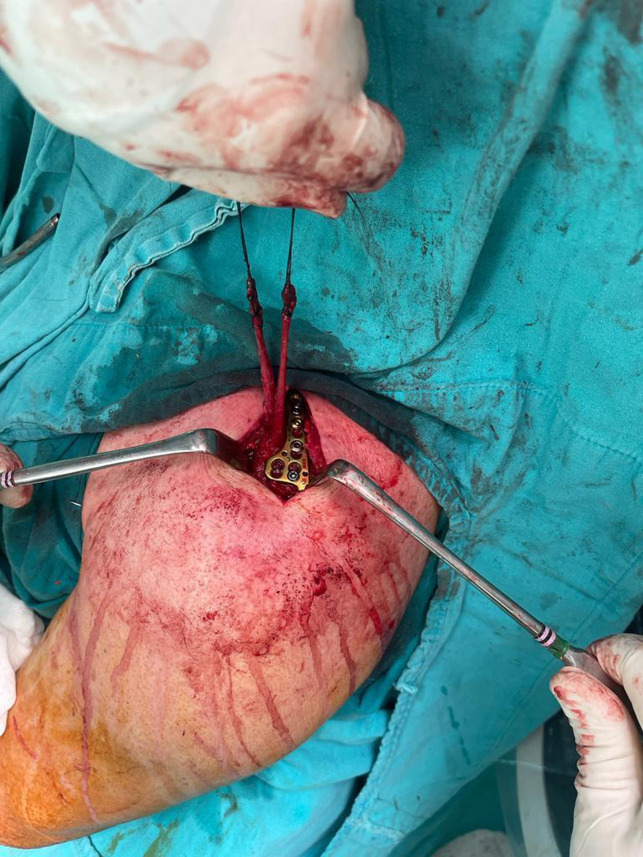
A semitendinosus tendon graft was then threaded through these tunnels in a looped configuration, specifically designed in an “8” shape (Figure 2). This configuration effectively mimics the natural architecture and function of the CC ligaments, which are vital for maintaining the stability of the AC joint. To ensure that the graft was securely anchored in place, various fixation methods were employed including interference screws, endobuttons or cortical fixation devices. Each option provides robust stabilization, which is essential for the success of graft integration and overall joint stability. After the reconstruction was completed, great care was taken to ensure that the graft was under the appropriate tension. Additionally, the surgical team focused on restoring the anatomical relationships of the surrounding structures, which ensures that the shoulder can move freely and effectively postoperatively.
Figure 2.
The image shows the semitendinosus tendon graft passed through meticulously drilled bone tunnels in the coracoid process and distal clavicle, forming an “8” loop configuration. This setup mimics the native coracoclavicular ligament architecture, ensuring robust stabilization of the acromioclavicular joint.
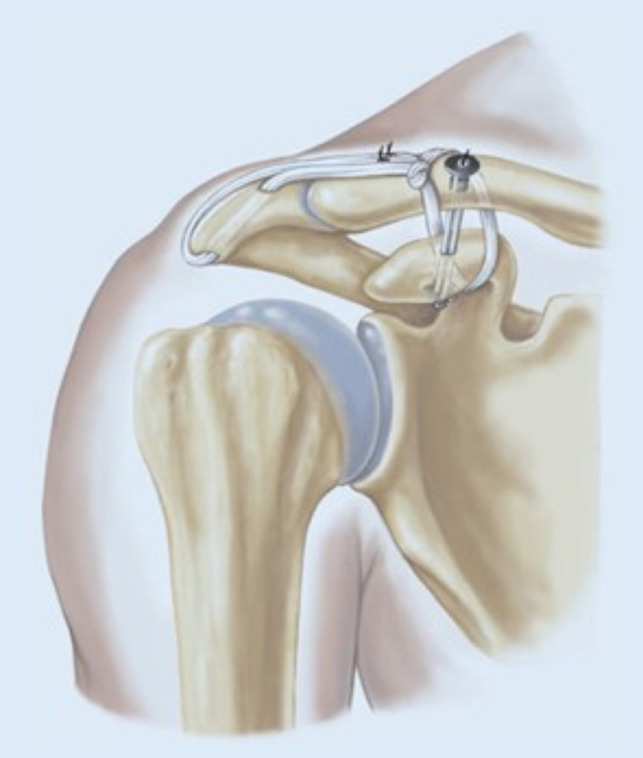
6. Joint capsule reconstruction (Transacromial technique)
A transacromial tunnel was created laterally using a cannulated drill, ensuring an appropriate length to accommodate the semitendinosus graft while leaving a safe margin at the anterior edge of the acromion. Then, the anterior segment of the graft, which had been securely looped over the clavicle, was passed through the acromial tunnel using non-absorbable sutures (2-0 Ti-cron). Care was taken to protect the surrounding soft tissues during this step. The graft was then looped posteriorly over the acromion and brought back to the clavicle, where it was securely tied to the anterior graft segment using additional non-absorbable sutures.
The process of capsule reconstruction (Figures 3 and 4) is meticulously undertaken by using the residual segment of the graft after the initial surgical procedure, involving careful suturing of the graft through a tunnel created and directed laterally within the acromion bone. Following this intricate suturing process, the graft is methodically secured over the acromion to ensure a robust connection with both the surrounding capsule and the remaining segment of the tendon that is anchored to the clavicle, using non-absorbable sutures that are specifically chosen for their durability and strength (Figures 3 and 4). This critical surgical step is meticulously designed and executed with the primary aim of significantly enhancing the stability and integrity of the AC joint, which is essential for maintaining proper shoulder function and biomechanics.
Figure 3.
The image illustrates the residual graft segment being secured through a laterally directed acromial tunnel. The graft is sutured to the capsule and anchored to the clavicle using durable, non-absorbable sutures, enhancing AC joint horizontal stability and structural integrity.
Figure 4.
Schematic illustration depicting the surgical technique for acromioclavicular (AC) joint reconstruction. The image demonstrates the semitendinosus tendon graft looped in an “8” configuration through bone tunnels in the coracoid process and distal clavicle, effectively mimicking the natural coracoclavicular ligament structure to restore vertical and horizontal joint stability.12
7. Final fixation and closure
The reconstructed joint was evaluated under fluoroscopy to confirm proper alignment and stability. A critical aspect of AC and CC joint reconstruction is the meticulous repair of the deltotrapezial fascia. To achieve this, the previously created fascial flaps were closed using absorbable sutures in a modified Mason-Allen interrupted pattern. Typically, 6 or 7 sutures were placed and the knots were securely tied on the posterior aspect of the trapezius. This closure technique ensured complete coverage of the grafts and the clavicle, reinforcing the structural integrity of the surgical site. If additional reinforcement was deemed necessary, the deltoid fascia was anchored through small drill holes in the anterior cortex of the clavicle. While concerns exist regarding the potential risk of iatrogenic fractures due to multiple clavicular tunnels, biomechanical data suggest that the presence of screws in these drill holes minimizes any significant reduction in load-to-failure strength.16
The subdermal tissue was carefully approximated using 2-0 or 3-0 absorbable sutures, ensuring optimal healing and minimizing the risk of wound complications. Skin closure was performed with either running 2-0 Prolene or interrupted nylon sutures, employing an eversion technique to promote a well-healed scar. The patient was placed in a supportive sling, maintaining the arm in neutral external rotation with slight upward force to optimize graft healing and shoulder stability.
Postoperative protocol
Patients were immobilized in a supportive shoulder sling to ensure comfort and protect the surgical site during the initial healing phase. However, unlike older reconstruction techniques, this advanced method may offer superior stability and reliability, allowing for an accelerated rehabilitation protocol.12,16 Passive shoulder range of motion exercises were initiated immediately after surgery to prevent stiffness and promote early joint mobility without compromising graft integrity.
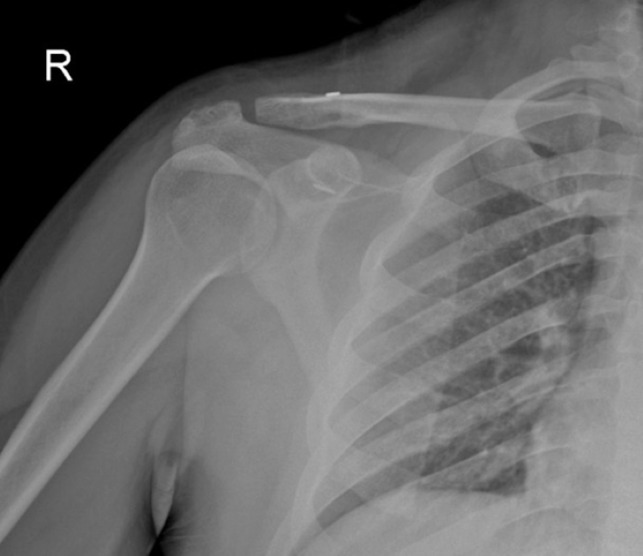
At the 3-week mark, active motion exercises were introduced to enhance mobility and restore functional shoulder movement progressively. Patients underwent x-ray imaging (Figure 5) to assess the control the joint’s stability and ensure proper graft positioning. Strengthening exercises targeting the shoulder and surrounding musculature were incorporated into the rehabilitation program at 6 weeks postoperatively. This gradual progression aimed to ensure optimal graft remodeling and soft tissue healing, ultimately enabling patients to return to their full range of daily and athletic activities by the 3-month milestone.
Figure 5.
Postoperative shoulder AP x-ray. Following surgical reconstruction, this x-ray demonstrates the acromioclavicular joint in a fully reduced position. The imaging was performed during the routine 3-week follow-up to assess the stability and alignment of the joint. The anatomical reduction of the acromioclavicular joint is well-maintained, with no evidence of displacement or subluxation, confirming the surgical intervention’s success and the graft’s integrity.
Results
Patient demographics and baseline characteristics
This technique was performed on 40 patients (35 male, 5 female) with a mean age of 42.1 years (18-72). Most injuries were the result of high-energy trauma, such as sports-related falls (60%) and motor vehicle accidents (30%). The average time from injury to surgery was 6 weeks (4-12 weeks), with chronic cases representing 100% of the cohort.
The distribution of Rockwood classifications (Table 1) between the reconstruction (YES) and non-reconstruction (NO) groups revealed no statistically significant difference (P = .526, Fisher’s exact test). This indicates that the Rockwood classification did not directly influence the decision to perform reconstruction.
Table 1.
Distribution of Rockwood classification by group
| Rockwood classification | 3A | 3B | 4 | 5 | Total |
|---|---|---|---|---|---|
| Reconstructıon No | 2 (12.5%) | 0 | 7 (43.8%) | 7 (43.8%) | 16 (100.0%) |
| Reconstructıon Yes | 2 (8.3%) | 2 (8.3%) | 6 (25.0%) | 14 (58.3%) | 24 (100.0%) |
| Total | 4 (10.0%) | 2 (5.0%) | 13 (32.5%) | 21 (52.5%) | 40 (100.0%) |
The relationship between the Rockwood classification (3A, 3B, 4, 5) and the reconstruction status (NO/YES) was analyzed using Fisher’s exact test. The resulting P-value was found to be .526, indicating that there is no statistically significant association between the Rockwood classification and whether reconstruction was performed (P > .05).
Radiographic outcomes
Radiological measurements were performed by an experienced radiologist and orthopedist who were blinded to the details of the study. Postoperative imaging revealed successful anatomical reduction in 97.5% (39/40) of cases. Follow-up shoulder AP x-rays at 6 months (after hook plate removal) confirmed maintained reduction without significant displacement of more than 5 mm in 92.5% of patients. The remaining 10% showed mild subluxation, though without functional impairment. All 3 patients with subluxation in the group had no capsule reconstruction, while the 24 patients who underwent transacromial capsule reconstruction showed no failures.
In the preoperative period, no statistically significant difference was observed between the non-reconstruction (−) and reconstruction (+) groups in terms of the clavicle-coracoid distance (P = .461). The mean values were 20.6 ± 3.54 mm and 19.8 ± 3.74 mm, respectively. In the early postoperative period, the CC distance did not show a statistically significant difference between the non-reconstruction (−) and reconstruction (+) groups (P = .053). However, it indicates a difference close to reaching statistical significance. The mean values were determined as 10.5 ± 1.57 mm in the non-reconstruction −) group and 9.52 ± 1.42 mm in the reconstruction (+) group (Tables 2 and 3).
Table 2.
Descriptive statistics for coracoclavicular distance
| Measurement | Reconstruction (YES)—Mean ± SD | Reconstruction (NO)—Mean ± SD | Reconstruction (YES)—Median (Min-Max) | Reconstruction (NO)—Median (Min-Max) |
|---|---|---|---|---|
| Preop CC distance | 19.8 ± 3.74 | 20.6 ± 3.54 | 21.0 (11.0-26.0) | 20.9 (14.5-26.7) |
| Early PO CC distance | 9.52 ± 1.42 | 10.5 ± 1.57 | 9.60 (7.0-12.4) | 10.2 (8.2-13.3) |
| Late PO CC distance | 10.1 ± 1.62 | 14.4 ± 2.03 | 10.1 (7.0-13.0) | 14.1 (10.9-19.0) |
Table 3.
Statistical analysis of coracoclavicular distance
| AC reconstruction | Statistic | df | P | |
|---|---|---|---|---|
| Preop CC distance | Student’s t | 0.744 | 38.0 | .461 |
| Early PO CC distance | Student’s t | 2.000 | 38.0 | .053 |
| Late PO CC distance | Student’s t | 7.519 | 38.0 | <.001 |



| ||||
In the late postoperative period (6 months), a statistically significant difference in the CC distance was identified between the 2 groups (P < .001). The mean distance in the non-reconstruction (−) group was 14.4 ± 2.03 mm, while it was 10.1 ± 1.62 mm in the reconstruction (+) group (Tables 2 and 3). This finding indicates that the reconstruction (+) group demonstrated a reduced clavicle-coracoid distance in the late postoperative period. This result suggests that performing a capsule reconstruction alongside the tendon reconstruction may be a key factor in improving long-term outcomes. No evidence of hardware failure or graft loosening was observed in any case.
Functional outcomes
The preoperative VAS scores did not show a statistically significant difference between the reconstruction (YES) and non-reconstruction (NO) groups (P = .391). This suggests that both groups experienced similar pain levels before the intervention, highlighting comparable baseline conditions (Table 4). Postoperative VAS scores revealed a significant difference between the 2 groups (P < .001). Patients in the reconstruction group (YES) reported substantially lower pain levels than those in the non-reconstruction group. This result indicates that the surgical intervention improved joint stability and significantly enhanced patient comfort and pain management.
Table 4.
Preoperative and postoperative VAS scores comparison
| AC reconstruction | Statistic | P | |
|---|---|---|---|
| Preop VAS (mean 5.9 ± 1.6) | Mann–Whitney U | 161.0 | .391 |
| Postop VAS (mean 1.88 ± 1.45) | Mann–Whitney U | 11.0 | <.001 |


| |||
The mean ASES score was significantly higher in the reconstruction group (YES: 93.04 ± 5.64) compared to the non-reconstruction group (NO: 82.0 ± 6.16, P < .001). This indicates that patients who underwent reconstruction experienced markedly better functional outcomes, reflecting improved pain relief and shoulder performance in daily activities. Similarly, the reconstruction group demonstrated superior results in the Constant score (YES: 92.88 ± 4.91) compared with the non-reconstruction group (NO: 79.9 ± 8.95, P < .001). This finding underscores the positive impact of reconstruction on shoulder strength, range of motion, and functional stability. The DASH scores, measuring disability, were significantly lower in the reconstruction group (YES: 2.93 ± 2.35) compared to the non-reconstruction group (NO: 12.6 ± 5.98, P < .001). A lower DASH score in the reconstruction group indicates better recovery and reduced functional impairment (Table 5).
Table 5.
Functional outcomes comparison (ASES, Constant, DASH scores)
| Outcome Measure | Group | n | Mean | Median | SD | SE |
|---|---|---|---|---|---|---|
| ASES score | No reconstruction | 16 | 82.0 | 83.3 | 6.16 | 1.54 |
| Reconstruction | 24 | 93.04 | 94.16 | 5.64 | 1.15 | |
| Constant score | No reconstruction | 16 | 79.9 | 80.0 | 8.95 | 2.24 |
| Reconstruction | 24 | 92.88 | 93.00 | 4.91 | 1.00 | |
| DASH score | No reconstruction | 16 | 12.6 | 11.4 | 5.98 | 1.49 |
| Reconstruction | 24 | 2.93 | 2.30 | 2.35 | 0.48 | |



| ||||||
Table 6 demonstrates the comparison of clinical and radiological outcomes between patients treated with hook plates and those treated with endobutton systems. In this subgroup analysis, no statistically significant differences were observed in preoperative, early postoperative, or late postoperative clavicle-coracoid (CC) distances, ASES scores, Constant scores, or postoperative VAS scores between the 2 groups (P > .05 for all). However, patients treated with endobutton systems exhibited significantly lower DASH scores compared to the hook plate group (P = .001), indicating better subjective functional outcomes. These results suggest that while implant type did not substantially affect objective radiological parameters or overall functional scores,
Table 6.
Comparison of outcomes between hook plate and endobutton groups
| Outcome measure | Hook plate (Mean ± SD) | Endobutton (Mean ± SD) | P |
|---|---|---|---|
| Preoperative CC distance (mm) | 20.5 ± 3.8 | 20.1 ± 3.6 | .642 |
| Early postoperative CC distance (mm) | 10.0 ± 1.5 | 9.4 ± 1.4 | .315 |
| Late postoperative CC distance (mm) | 11.2 ± 1.8 | 10.0 ± 1.5 | .212 |
| ASES score | 85.4 ± 6.2 | 89.8 ± 5.9 | .083 |
| Constant score | 84.1 ± 7.8 | 90.2 ± 5.1 | .075 |
| DASH score | 11.2 ± 5.1 | 4.1 ± 2.9 | .001 |
| Postoperative VAS score | 2.3 ± 1.1 | 1.9 ± 0.9 | .224 |
Table 7 summarizes the results of the multivariate linear regression analysis evaluating predictors of late postoperative clavicle-coracoid (CC) distance. Reconstruction status was identified as the only significant independent predictor, with patients who underwent reconstruction demonstrating a significantly smaller late postoperative CC distance (P < .001). In contrast, implant type (hook plate versus endobutton), age, and sex were not significantly associated with late postoperative CC distance (P > .05 for all variables). These findings suggest that the surgical reconstruction itself, rather than the choice of implant or patient demographics, is the key factor influencing radiological outcomes at follow-up.
Table 7.
Regression analysis results for predictors of late postoperative CC distance
| Variable | Estimate (B) | Standard error | P |
|---|---|---|---|
| Implant type (Hook Plate vs. Endobutton) | 0.0264 | 0.743 | .972 |
| Reconstruction (Yes vs. No) | −3.984 | 0.654 | <.001 |
| Age | 0.021 | 0.032 | .517 |
| Sex | 0.103 | 0.629 | .872 |
Complications
There are no cases of infection, neurovascular injury, or significant donor site morbidity. Three patients (12.5%) reported mild anterior knee pain following semitendinosus harvesting, which resolved within 3 months. Mild subluxation (5-10 mm) was observed in 3 patients in the group where the double endobutton technique was used without transacromial capsule reconstruction.
Discussion
In this study, the clinical and radiological outcomes of a combined CC ligament and transacromial capsule reconstruction technique for chronic AC joint instability were evaluated.
The major findings are: combined capsule and ligament reconstruction significantly improved radiological stability (maintenance of CC distance) and functional outcomes (ASES, Constant, DASH scores); implant type (hook plate vs. endobutton) did not significantly affect late CC distance or functional outcomes but DASH scores were superior in the endobutton group; and capsule reconstruction contributed to improved multidirectional stability beyond traditional CC-only techniques. Chronic AC joint injuries are generally defined as those persisting beyond 3 weeks, where biological healing potential is limited due to soft tissue degeneration and ligament retraction.17 This is particularly important in chronic and delayed cases, where residual horizontal instability has been shown to critically impair long-term outcome.18,19
The incorporation of transacromial capsule reconstruction alongside CC ligament repair resulted in superior maintenance of CC distance at 6 months (mean 10.1 ± 1.6 mm vs. 14.4 ± 2.0 mm in the non-capsule group; < 0.001) and significantly better functional outcomes (ASES 93.0 ± 5.6 vs. 82.0 ± 6.2; Constant 92.8 ± 4.9 vs. 79.9 ± 8.9; DASH 2.9 ± 2.3 vs. 12.6 ± 6.0). These findings align with recent reports by Rosso et al. (2021) and Dittrich et al. (2020), who emphasized the importance of addressing horizontal instability in chronic AC joint separations.7,12 Similarly, Rupp et al. (2022) noted that solely reconstructing the CC ligaments fails to restore horizontal stability, resulting in higher failure rates.8 Additionally, Aliberti et al. (2020) demonstrated in their systematic review that horizontal instability of the AC joint is a major determinant of poor functional outcomes if not properly addressed.18 Recent biomechanical studies also showed that restoring capsular integrity dramatically reduces anterior-posterior translation forces across the joint, thereby enhancing overall shoulder kinematics.20,21 The results reinforce the notion that anatomical, capsular-supported techniques provide biomechanically superior stabilization, particularly in chronic injuries.
Subgroup analysis revealed no statistically significant differences in radiological (CC distance) or most functional outcomes (ASES, Constant, VAS) between hook plate and endobutton groups (P > .05), although DASH scores favored endobuttons (4.1 ± 2.9 vs. 11.2 ± 5.1, P = .001). This finding is consistent with the observations of Berthold et al (2022)22 and Reyniers et al (2023),23 who reported that hardware choice may influence subjective comfort but does not independently determine objective stability. Furthermore, the regression analysis demonstrated that only the presence of capsule reconstruction—not implant type—was predictive of better late CC distance, supporting the conclusions by Cerciello et al (2022)24 regarding the dominant role of biological reconstruction over hardware selection. Similarly, Chen et al (2021)25 highlighted that factors like graft tensioning and tunnel positioning have a greater impact on postoperative maintenance of reduction than the specific type of fixation device used.
By reconstructing the anterior and posterior capsule rather than focusing solely on vertical stabilization, this technique created a functional dynamic envelope that resists anterior, posterior, superior, and inferior translations.16 This approach contrasts with traditional methods and aligns with the biomechanical insights of Bi et al (2023)21 and Hohmann et al (2023),26 who stressed the importance of restoring native multidirectional stability for optimal joint function. The network meta-analysis by Yan et al (2023)19 further supports the idea that procedures targeting multiple planes of instability yield superior functional and radiological outcomes compared to isolated vertical stabilization techniques.
This study demonstrates that combining CC ligament and transacromial capsule reconstruction results in superior clinical and radiological outcomes for chronic AC joint instability, compared to CC-only approaches. This method also appears advantageous for revision cases where previous surgeries failed to adequately address multidirectional instability or where fibrosis and anatomical distortions complicate standard techniques.13,27 Its robust biomechanical properties and biological compatibility support long-term joint stability and function. Strengths of the study include a well-defined chronic injury cohort, the application of subgroup and regression analyses, and the focus on multidirectional stability. However, limitations include the relatively small sample size (n = 40), 6-month follow-up duration, and absence of direct comparison with fully arthroscopic techniques. Future multicenter, randomized studies with larger cohorts, and longer follow-up are needed to confirm the long-term efficacy of combined capsule and ligament reconstruction, particularly in comparison with emerging minimally invasive approaches.27,28
This study demonstrates that combining CC ligament and transacromial capsule reconstruction improves radiological stability and functional outcomes in patients with chronic AC joint instability. Addressing both vertical and horizontal instability appears to contribute to better short-term recovery. Further studies with larger cohorts and longer follow-up are needed to confirm these preliminary findings.
Table 8.
Advantages and disadvantages of the surgical technique
| Advantages | Disadvantages |
|---|---|
| Provides superior horizontal and vertical stability, reducing subluxation risk | Potential risk of graft elongation over time if not correctly tensioned |
| Mimics the native biomechanics of the AC joint, restoring physiological function | Mild donor site morbidity (12.5% knee pain cases), typically resolving within 3 months |
| Low complication rate, with no observed infections or graft failures | Requires tendon harvesting, leading to potential donor site discomfort |
| Utilizes autologous semitendinosus tendon, enhancing biocompatibility and reducing rejection risk | Increased surgical complexity compared to single ligament reconstruction |
| Demonstrated superior maintenance of clavicle-coracoid distance over time (P < .001) | Technically demanding, requiring experience in anatomical reconstruction |
| Can be performed without permanent implants, avoiding hardware-related complications | |
| Allows earlier functional rehabilitation due to enhanced joint stability |
Table 9.
Abbreviations
| Abbreviation | Full Term |
|---|---|
| AC | Acromioclavicular |
| CC | Coracoclavicular |
| AP | Anteroposterior |
| DASH | Disabilities of the Arm, Shoulder, and Hand |
| ASES | American Shoulder and Elbow Surgeons Score |
| VAS | Visual Analog Scale |
| MRI | Magnetic resonance imaging |
| ANOVA | Analysis of Variance |
| SPSS | Statistical Package for the Social Sciences |
| PO | Postoperative |
| SD | Standard deviation |
| CI | Confidence Interval |
| K-wire | Kirschner wire |
Funding Statement
The authors declared that this study has received no financial support.
Footnotes
Ethics Committee Approval: This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Ethical approval was obtained from the Dokuz Eylul University Ethics Committee (Approval No: 2025/04-10 Date: 5.02.2025).
Informed Consent: Written informed consent was obtained from the patients who agreed to take part in the study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – O.B., B.D.; Design – B.D., I.N.E.; Supervision – M.H.O., O.B.; Resources – B.D., M.H.O.; Materials – B.D., I.N.E.; Data Collection and/or Processing – B.D., I.N.E.; Analysis and/or Interpretation – B.D., I.N.E.; Literature Search – O.B., M.H.O.; Writing Manuscript – B.D., O.B.; Critical Review – B.D., O.B, M.H.O.
Declaration of Interests: Onur Başçı is an Associate Editor at Acta Orthopaedica et Traumatologica Turcica, however, his involvement in the peer-review process was solely as an author. The other authors have no conflict of interest to declare.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.
References
- 1. Eschler A Rösler K Rotter R Gradl G Mittlmeier T Gierer P. . Acromioclavicular joint dislocations: radiological correlation between Rockwood classification system and injury patterns in human cadaver species. Arch Orthop Trauma Surg. 2014;134(9):1193 1198. (doi: 10.1007/s00402-014-2045-1) [DOI] [PubMed] [Google Scholar]
- 2. Martetschläger F Kraus N Scheibel M Streich J Venjakob A Maier D. . The diagnosis and treatment of acute dislocation of the acromioclavicular joint. Dtsch Arztebl Int. 2019;116(6):89 95. (doi: 10.3238/arztebl.2019.0089) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Reid D Polson K Johnson L. . Acromioclavicular joint separations Grades I-III: a review of the literature and development of best practice guidelines. Sports Med. 2012;42(8):681 696. (doi: 10.2165/11633460-000000000-00000) [DOI] [PubMed] [Google Scholar]
- 4. Grutter PW Petersen SA. . Anatomical acromioclavicular ligament reconstruction: a biomechanical comparison of reconstructive techniques of the acromioclavicular joint. Am J Sports Med. 2005;33(11):1723 1728. (doi: 10.1177/0363546505275646) [DOI] [PubMed] [Google Scholar]
- 5. Gowd AK, Liu JN, Cabarcas BC. Current concepts in the operative management of acromioclavicular dislocations: a systematic review and meta-analysis of operative techniques. Am J Sports Med. 2019;47(11):2745 2758. (doi: 10.1177/0363546518795147) [DOI] [PubMed] [Google Scholar]
- 6. Cook JB Tokish JM. . Surgical management of acromioclavicular dislocations. Clin Sports Med. 2014;33(4):721 737. (doi: 10.1016/j.csm.2014.06.009) [DOI] [PubMed] [Google Scholar]
- 7. Rosso C, Martetschläger F, Saccomanno MF. High degree of consensus achieved regarding diagnosis and treatment of acromioclavicular joint instability among ESA-ESSKA members. Knee Surg Sports Traumatol Arthrosc. 2021;29(7):2325 2332. (doi: 10.1007/s00167-020-06286-w) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rupp MC, Kadantsev PM, Siebenlist S. Low rate of substantial loss of reduction immediately after hardware removal following acromioclavicular joint stabilization using a suspensory fixation system. Knee Surg Sports Traumatol Arthrosc. 2022;30(11):3842 3850. (doi: 10.1007/s00167-022-06978-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Çarkçı E Polat AE Gürpınar T. . The frequency of reduction loss after arthroscopic fixation of acute acromioclavicular dislocations using a double-button device, and its effect on clinical and radiological results. J Orthop Surg Res. 2020;15(1):136. (doi: 10.1186/s13018-020-01674-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mazzocca AD, Conway JE, Johnson S. The anatomic coracoclavicular ligament reconstruction. Oper Tech Sports Med. 2004;12(1):56 61. (doi: 10.1053/j.otsm.2004.04.001) [DOI] [Google Scholar]
- 11. Kraus N Hann C Minkus M Maziak N Scheibel M. . Primary versus revision arthroscopically-assisted acromio- and coracoclavicular stabilization of chronic AC-joint instability. Arch Orthop Trauma Surg. 2019;139(8):1101 1109. (doi: 10.1007/s00402-019-03153-3) [DOI] [PubMed] [Google Scholar]
- 12. Dittrich M Wirth B Freislederer F Bellmann F Scheibel M. . Arthroscopically assisted stabilization of chronic bidirectional acromioclavicular joint instability using a low-profile implant and a free tendon graft. Obere Extrem. 2020;15(2):118 121. (doi: 10.1007/s11678-020-00576-y) [DOI] [Google Scholar]
- 13. Chang HM, Wang CH, Hsu KL. Does Weaver–Dunn procedure have a role in chronic acromioclavicular dislocations? A meta-analysis. J Orthop Surg Res. 2022;17(1):95. (doi: 10.1186/s13018-022-02995-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Boileau P Gastaud O Wilson A Trojani C Bronsard N. . All-arthroscopic reconstruction of severe chronic acromioclavicular joint dislocations. Arthroscopy. 2019;35(5):1324 1335. (doi: 10.1016/j.arthro.2018.11.058) [DOI] [PubMed] [Google Scholar]
- 15. Kienast B Thietje R Queitsch C Gille J Schulz AP Meiners J. . Mid-term results after operative treatment of rockwood grade III-V acromioclavicular joint dislocations with an AC-hook-plate. Eur J Med Res. 2011;16(2):52 56. (doi: 10.1186/2047-783X-16-2-52) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Banffy MB Uquillas C Neumann JA ElAttrache NS. . Biomechanical evaluation of a single- versus double-tunnel coracoclavicular ligament reconstruction with acromioclavicular stabilization for acromioclavicular joint injuries. Am J Sports Med. 2018;46(5):1070 1076. (doi: 10.1177/0363546517752673) [DOI] [PubMed] [Google Scholar]
- 17. Tauber M. . Management of acute acromioclavicular joint dislocations: current concepts. Arch Orthop Trauma Surg. 2013;133(7):985 995. (doi: 10.1007/s00402-013-1748-z) [DOI] [PubMed] [Google Scholar]
- 18. Aliberti GM Kraeutler MJ Trojan JD Mulcahey MK. . Horizontal instability of the acromioclavicular joint: a systematic review. Am J Sports Med. 2020;48(2):504 510. (doi: 10.1177/0363546519831013) [DOI] [PubMed] [Google Scholar]
- 19. Yan Y, Liao M, Lai H. Comparison of effectiveness and safety in treating acute acromioclavicular joint dislocation with five different surgical procedures: a systematic review and network meta-analysis. Orthop Surg. 2023;15(8):1944 1958. (doi: 10.1111/os.13731) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Morikawa D, Huleatt JB, Muench LN. Posterior rotational and translational stability in acromioclavicular ligament complex reconstruction: a comparative biomechanical analysis in cadaveric specimens. Am J Sports Med. 2020;48(10):2525 2533. (doi: 10.1177/0363546520939882) [DOI] [PubMed] [Google Scholar]
- 21. Bi AS, Robinson J, Anil U. Treatment options for acute Rockwood type III-V acromioclavicular dislocations: a network meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2023;32(6):1146 1158. (doi: 10.1016/j.jse.2023.01.039) [DOI] [PubMed] [Google Scholar]
- 22. Berthold DP, Muench LN, Dyrna F. Current concepts in acromioclavicular joint (AC) instability – a proposed treatment algorithm for acute and chronic AC-joint surgery. BMC Musculoskelet Disord. 2022;23(1):1078. (doi: 10.1186/s12891-022-05935-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reynıers P De Mulder T Ruette P Van Raebroeckx A. . Long-term follow-up in a single-bundle arthroscopic acromioclavicular joint reconstruction after Rockwood III to VI dislocation. Acta Orthop Belg. 2023;89(1):156 161. (doi: 10.52628/89.1.7586) [DOI] [PubMed] [Google Scholar]
- 24. Cerciello S, Corona K, Morris BJ. Hybrid coracoclavicular and acromioclavicular reconstruction in chronic acromioclavicular joint dislocations yields good functional and radiographic results. Knee Surg Sports Traumatol Arthrosc. 2022;30(6):2084 2091. (doi: 10.1007/s00167-021-06790-7) [DOI] [PubMed] [Google Scholar]
- 25. Chen K Xu B Lao YJ Yang Y. . Risk factors related to the loss of reduction after acromioclavicular joint dislocation treated with the EndoButton device. Ann Transl Med. 2021;9(4):345 345. (doi: 10.21037/atm-21-404) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hohmann E Tetsworth K. . Clinical outcomes for grades III-V acromioclavicular dislocations favor double-button fixation compared to clavicle hook plate fixation: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2023;33(7):2831 2846. (doi: 10.1007/s00590-023-03492-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ranne JO Kainonen TU Kanto KJ Lehtinen JT Niemi PT Scheinin H. . Tendon graft through the coracoid tunnel versus under the coracoid for coracoclavicular/acromioclavicular reconstruction shows no difference in radiographic or patient-reported outcomes. Arch Orthop Trauma Surg. 2024;144(8):3491 3501. (doi: 10.1007/s00402-024-05461-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sircana G, Saccomanno MF, Mocini F. Anatomic reconstruction of the acromioclavicular joint provides the best functional outcomes in the treatment of chronic instability. Knee Surg Sports Traumatol Arthrosc. 2021;29(7):2237 2248. (doi: 10.1007/s00167-020-06059-5) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.



 Content of this journal is licensed under a
Content of this journal is licensed under a