Abstract
Purpose
Current literature interchangeably uses the terms “middle” and “medial” for the middle collateral artery (MCA). However, the term “medial” implies that the artery is positioned on the medial aspect of the arm, which may lead to misunderstandings in medical education or interdisciplinary communication. Our purpose is to provide anatomic and historical support for the use of the original “middle collateral artery” terminology.
Methods
We reviewed a 300-year history of anatomy texts to elucidate the origin of the MCA nomenclature. In three cadaveric specimens, the MCA was dissected following latex infusion and its vascular contribution to three pedicled flaps was demonstrated. In three additional specimens, the arms were imaged with computed tomography and three-dimensional reconstruction following barium sulfate infusion.
Results
The term “middle” collateral artery predates the term “medial” collateral artery by 80 years. The origin of the term “medial” collateral artery is likely a mistranslation of the predecessor Latin term, “arteria collateralis media.” Our cadaveric dissections and computed tomography imaging confirmed that the MCA’s course is on the posterolateral side of the arm between the anterolateral-positioned radial collateral artery and the medial-positioned superior ulnar collateral artery.
Conclusion
The term “medial” collateral artery is an anatomic misnomer. “Middle” collateral artery, its original name, accurately reflects its posterolateral position in the arm between the radial collateral artery and superior ulnar collateral artery. We recommend that authors use the term “middle” collateral artery based on its anatomical position and recommend discontinuation of the term “medial” collateral artery in the scientific literature.
Clinical Relevance
Given the MCA’s surgical significance in reconstructive flaps, nonanatomic labeling of the MCA as “medial” may lead to misunderstandings in medical education and surgical site identification. Replacing a misnomer with an anatomically accurate name would improve professional communication and teaching.
Key words: Computed tomography, Medial collateral artery, Middle collateral artery, Pedicle flap, Profunda brachii
The “medial” collateral artery (MCA) is one of two terminal branches of the profunda brachii artery. The MCA descends toward the elbow between the radial collateral artery (RCA), which lies more anterior, and the superior and inferior ulnar collateral arteries (SUCA and IUCA), which lie more medial.1
Despite its location in the posterolateral aspect of the arm, the MCA has been interchangeably referred to as the “middle” or “medial” collateral artery in various modern textbooks and scientific publications.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 When considering the validity of either name, it is important to examine the anatomical course of the artery. The term “medial” is an anatomic term that refers to a structure’s location with respect to the midline of the body in its anatomical position.14,15 In the upper extremity, the term is used in reference to the humerus or the olecranon, especially if the arm is abducted 90° or more from the torso. When considering the “medial” collateral artery’s relationship to the humerus, its course is entirely on the posterolateral side of the arm.1
The MCA most commonly originates from the terminus of the profunda brachii near the radial groove, where the profunda bifurcates into the MCA and RCA.16, 17, 18 Although variations in the MCA’s origin have been reported in the literature, these variations do not alter its downstream course.19 Anatomical texts of the 21st century describe the MCA as traveling posterior to the lateral intermuscular septum along the medial head of the triceps to the posterior side of the lateral epicondyle of the humerus, where the MCA then anastomoses with the interosseous recurrent artery and contributes to the olecranon articular rete.20,21 For context, the RCA follows the radial nerve anterolaterally in the arm before dividing into the anterior RCA (ARCA) and posterior RCA (PRCA).20, 21, 22 The ARCA follows the radial nerve to the anterior aspect of the arm, whereas the PRCA travels through the intermuscular septum and between the brachialis and triceps.19,20,22, 23, 24 The SUCA and IUCA arise from the brachial artery and descend along the medial arm with the ulnar nerve.1,22 Because the MCA is positioned between the radial and ulnar collateral arteries, the term “middle collateral artery” is both descriptive and anatomic.
Confusion arises when modern academic literature refers to the same structure as either the “middle” and “medial” collateral artery. The purpose of our study was to research the origin and derivation of the terms “middle collateral artery” and “medial collateral artery,” and to use anatomic dissections and high-resolution imaging to provide an anatomic basis for resolution of this controversy. We hypothesize that the MCA lies on the posterolateral aspect of the humerus throughout its course and between the radial and ulnar collateral arteries, thus justifying its original and correct name as the MCA.
Materials and Methods
Literature review
We conducted a literature review examining the history of the MCA nomenclature in texts and manuscripts spanning the 18th to 21st centuries. Using variations of the MCA’s terminology as keywords in online databases, 49 relevant scientific articles and anatomy textbooks were identified that referenced the MCA’s anatomy. These texts were reviewed to understand the vascular anatomy of the region and the chronological changes in the MCA’s terminology. Foreign language texts were translated using a combination of manual and automatic translation programs.
Anatomic study
Six upper extremities were analyzed for the anatomic portion of this study; three of these were examined through latex-infused cadaveric dissections, and three separate specimens were examined through computed tomography with barium sulfate contrast. Two of the specimens were men, and four were women (mean age 74.5 years, range 64–89 years). None of the specimens had known anatomical abnormalities or evidence of prior injury. Ethical approval was not sought for the present study because it is a cadaveric study. This study was completed in accordance with the Helsinki Declaration as revised in 2013.
In three specimens, 150 mL of latex injection medium (470024-612; Ward’s Blue) was infused into the brachial artery at the shoulder using a vessel cannula, which was secured by suture into the divided proximal end of the brachial artery. Leakage of latex was limited by applying gauze to the exposed vessels of the proximal musculature. The cannulated specimens were placed on ice for 24 hours before dissection. Through a posterolateral arm and proximal forearm incision, the triceps tendon was divided to separate the lateral and long heads and expose the medial triceps. The MCA was dissected and traced from its profunda brachii origin to the anconeus, and the RCA and SUCA were also dissected out to provide anatomical context. To simulate a clinical scenario, either the anconeus, medial triceps, or “extreme” lateral arm reconstructive flaps were raised on the posterolateral side of the arm, pedicled on the MCA as the blood supply.
In three additional upper extremities, 225 ml of barium sulfate solution (40% BaSO4 Varibar Thin Liquid, and 60% saline) was infused into the brachial artery at the shoulder. As with the latex infusion, a vessel cannula was secured into the brachial artery and gauze was used to help prevent leakage of the barium sulfate. After infusion, these cannulated specimens were imaged with high-resolution computed tomography (CT). CT was performed with a slice thickness of 0.6 mm and the following pararmeters:140 kVp, 140 mA, and a 512 × 512 matrix. Three-dimensional image reconstruction and volume rendering was performed to visualize the MCA in relation to neighboring anatomic structures. Displacement measurements were taken on the three-dimensional reconstructions; calibration of the programmed measurement tool was confirmed by comparing the measured length of the arm with the program’s measurement of the arm. From a posterior view of the arm, the displacement was measured between the MCA origin and the bottom edge of the lateral epicondyle. The displacement was also measured between the origin of the RCA and its bifurcation into the ARCA and PRCA.
Results
Literature review
The 1800 German anatomy text, Lehrbuch der Anatomie des Menschen designated the MCA as the “arteria collateralis radialis prima” and the RCA as the “arteria collateralis radialis secunda.”25 Prior anatomical texts from 18th century Europe did not separately identity the MCA, but instead referred to both the MCA and the RCA as “satellites arteriae brachialis” of the profunda brachii.25, 26, 27
The Latin name “[arteria] collateralis media” (translation: middle collateral artery) first appeared in Krause’s 1838 Handbuch der Menschlichen Anatomie. Krause (1838) described the artery as coursing down the middle of the triceps.28 After this, the term was used repeatedly in anatomical texts throughout the remainder of the 19th century.29, 30, 31, 32, 33, 34 A 1842 German text used the term “mittlere nebenpulsader,” which translates to “middle secondary artery.”34 The first use of the English term “middle collateral artery” appeared in 1904, along with the original Latin name “arteria collateralis media.”35 Thereafter, several other anatomical texts published this name as well.36, 37, 38 The first identifiable use of the term “medial collateral” artery was in 1918.39 Future texts repeated the term, including the 1921 publication of Morris's Human Anatomy: A Complete Systematic Treatise by English and American Authors, even though its previous two editions in 1907 and 1914 used the term “middle collateral artery.”40, 41, 42 Since then, either term has been used in 20th and 21st century scientific literature.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 In 1998, the Terminologia Anatomica termed this artery the “medial collateral artery”; however, in 2019, the second edition replaced it with “middle collateral artery.”43 Despite this change, numerous recent papers have continued to solely use the “medial collateral” term.44, 45, 46
Cadaveric dissections and computed tomography
MCA identification was confirmed in all six specimens by the MCA’s vascularization of the anconeus and medial triceps as well as by the proximity of the artery’s anatomic origin to the radial nerve and radial groove in the humerus. The other collateral arteries of the arm were also identified for context. The RCA was identified on the anterolateral aspect of the arm and lateral to the MCA; at an average of 3.44 cm (standard deviation [SD], 2.03 cm), it branched into the ARCA and PRCA. The SUCA branched off the brachial artery and traveled down the medial aspect of the arm. In all six cadaveric specimens, the profunda brachii bifurcated into its terminal branches, the MCA and RCA, near the radial groove on the posterolateral humerus. After its origin, the MCA’s course was entirely on the posterolateral arm, coursing down the humerus to the anconeus near the lateral epicondyle. As shown in Figure 1, the three specimens exemplify the course of the MCA posterolateral to the lateral epicondyle and olecranon. The average distance between the MCA origin and the lateral epicondyle in these three specimens was 14.61 cm (SD 1.25 cm). The three cadaveric dissections demonstrate the MCA’s course along the medial triceps toward the anconeus and demonstrate its practical utility in the vascularization of posterior arm reconstructive flaps (Figure 2, Figure 3, Figure 4).
Figure 1.
A–C Three-dimensional renderings of three right upper-extremity CT scans with contrast that illustrate the vascular anatomy of the posterolateral arm. Postprocessing coloring was used to highlight MCA, RCA, and profunda brachii in yellow, red, and blue, respectively.
Figure 2.
Dissection of the MCA and its neighboring structures in a right upper extremity with a demonstration of the anconeus reconstructive flap using the MCA as the blood supply.
Figure 3.
A Dissection of the MCA and its neighboring structures in a left upper extremity (flipped image). B This is followed by a corresponding demonstration of the medial triceps reconstructive flap over the olecranon. The MCA provides pedicled blood supply for the flap.
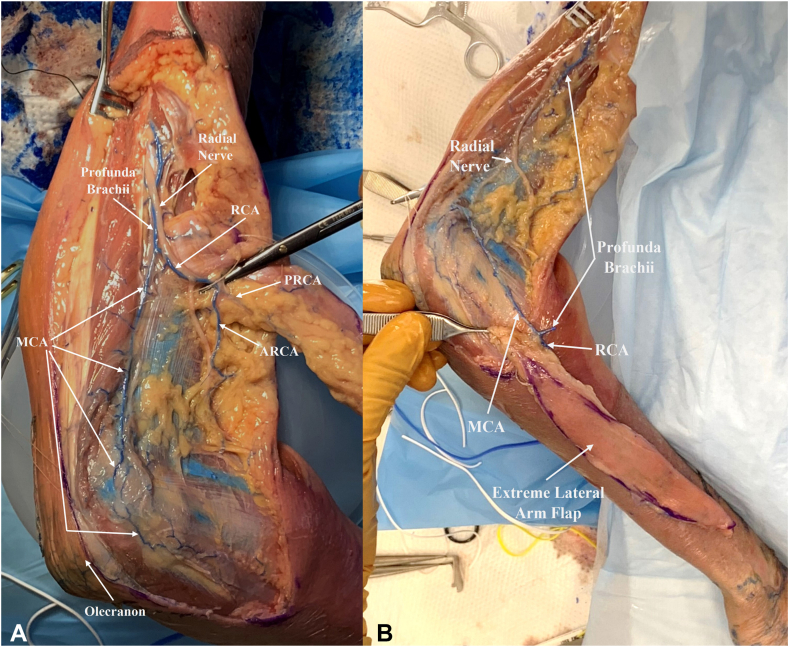
Figure 4.
A Dissection of the MCA and its neighboring structures in a right upper extremity. B This is followed by rotation of the “extreme” lateral arm reconstructive flap to the posterolateral forearm. Blood flows retrograde through the MCA from its anastomosis at the anconeus and flows anterograde through the RCA to supply the skin flap.
Discussion
Although the reasoning behind the introduction of the term “medial” for the MCA is unknown, it is likely that its origin was a mistranslation of the original Latin term “media”, and the error was perpetuated. This is supported by the fact that the mid-19th century name, “mittlere nebenpulsader,” and early 20th century name, “middle collateral artery,” both preceded the name “medial collateral artery” by nearly a century. The medial collateral artery mistranslation may have assimilated into the anatomic lexicon due the MCA’s oft cited association with the medial triceps.8,39,40 The Bulletin of the Johns Hopkins Hospital suspected a similar mistranslation of the term “media” in 1907 regarding the articular arteries in the knee, noting that the terms “medialis” and “media” could have been incorrectly translated to “medial” instead of “middle” in these cases.47
In addition to the issue of a potential mistranslation, our dissections demonstrate that the term “medial collateral artery” is anatomically incorrect. The MCA coursed entirely along the posterolateral side of the humerus. In context, the RCA was anterolaterally-positioned while the UCAs were medial to the MCA. Based on the 19th century German text that originated the Latin term “arteria collateralis media,” it may be inferred that the name referred to the MCA’s course in the middle of the other two collateral arteries of the arm. This is contextualized with the adjacent descriptions of the RCA and UCAs, which have been explained to run on the “outer” and “inner” sides of the arm respectively.28 Our cadaveric dissections and CT imaging demonstrated the consistent posterolateral anatomy of the MCA and corroborated its anatomic description as the middle collateral artery.
This mistranslated and inaccurate “medial collateral” term persisted throughout the 20th and 21st century and was incorporated as the official term for the artery in the first edition of the Terminologia Anatomica in 1998.48 Although the latest edition of the Terminologia Anatomica in 2019 replaced “medial collateral artery” with “middle collateral artery,” this nomenclature issue continues to stay relevant because recent papers since then continue to publish the misleading “medial collateral” name.17,44, 45, 46
Clarifying the name of the MCA is important for surgical reconstruction and medical education. Because of its robust blood supply to the posterior arm, the MCA is useful in planning soft tissue coverage for traumatic defects about the elbow. In particular, it is one of the main vascular pedicles of the “extreme” lateral arm flap, a retrograde island flap that can be used to provide soft tissue coverage to the ipsilateral forearm and wrist.19 The MCA also supplies the anconeus flap, which can cover defects over the posterior and lateral elbow, such as the radiohumeral joint, radioulnar joint, distal triceps tendon, and olecranon.4,5,11 Similarly, the MCA’s vascularization of the medial head of the triceps allows for the use of the medial head as a pedicled flap for elbow injuries and as a free flap.2,3,10 Our cadaveric harvests of three posterior arm flaps pedicled on the MCA demonstrate the MCA’s involvement in reconstruction and its surgical significance to the elbow and upper-extremity surgeon. Nonanatomic labeling of the MCA as “medial” may lead to misunderstandings in medical education and surgical site identification. Replacing a misnomer with an anatomically accurate name would improve professional communication and teaching.
Although no prior study has thoroughly examined the nomenclature issue, some sources have also commented that the “medial collateral” name is inappropriate. Though the authors’ reasoning wasn’t provided, Kachlik et al48 noted that the Terminologia Anatomica’s use of the term “medial collateral artery” in 1998 appeared incorrect and recommended the term “middle collateral artery” instead. Similarly, after describing the MCA’s posterolateral position in the 2017 Atlas of Upper Extremity Trauma: A Clinical Perspective, Eglseder commented that the name “medial collateral artery” was “erroneous” and preferred the use of its original name, the “middle collateral artery.”49 These prior comments support our contention that there is sufficient anatomic and historical support for discarding the erroneous “medial collateral artery” terminology in favor of its original name, “middle collateral artery.”
Although modern academic literature continues to use multiple terms for the MCA, we aim to encourage an update to the accepted nomenclature. We conclude that “middle collateral artery” adheres to the artery’s original name and accurately reflects the artery’s position in the upper arm between the RCA and the UCAs, whereas “medial collateral artery” is an anatomic misnomer for its posterolateral position and is a potential mistranslation. Therefore, we recommend the use of the original “middle” collateral artery terminology and recommend that the term “medial” collateral artery be discontinued going forward.
Conflicts of Interest
No benefits in any form have been received or will be received related directly to this article.
Acknowledgments
We would like to thank the Hospital for Special Surgery Simulation Learning & Training Center for providing cadavers.
References
- 1.Doyle J.R. Lippincott Williams & Wilkins; 2003. Surgical Anatomy of the Hand and Upper Extremity; pp. 245–246. [Google Scholar]
- 2.Delgove A., Weigert R., Casoli V. Evaluation of donor site morbidity after medial triceps brachii free flap for lower limb reconstruction. Arch Orthop Trauma Surg. 2017;137:1659–1666. doi: 10.1007/s00402-017-2780-1. [DOI] [PubMed] [Google Scholar]
- 3.Delgove A., Weigert R., Casoli V. A new local muscle flap for elbow coverage-the medial triceps brachii flap: anatomy, surgical technique, and preliminary outcomes. J Shoulder Elbow Surg. 2018;27:733–738. doi: 10.1016/j.jse.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 4.Elhassan B., Karabekmez F., Hsu C.C., Steinmann S., Moran S. Outcome of local anconeus flap transfer to cover soft tissue defects over the posterior aspect of the elbow. J Shoulder Elbow Surg. 2011;20:807–812. doi: 10.1016/j.jse.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 5.Luchetti R., Atzei A., Brunelli F., Fairplay T. Anconeus muscle transposition for chronic lateral epicondylitis, recurrences, and complications. Tech Hand Up Extrem Surg. 2005;9:105–112. doi: 10.1097/01.bth.0000160514.70744.42. [DOI] [PubMed] [Google Scholar]
- 6.Magden O., Tayfur V., Edizer M. Arterial anatomy of anconeus muscle flap. J Exp Clin Med. 2010;27:24–25. [Google Scholar]
- 7.Moran S. Lippincott Williams & Wilkins; 2016. Master Techniques in Orthopaedic Surgery: Soft Tissue Surgery. [Google Scholar]
- 8.Morrey B.F., Sotelo J.S., Morrey M.E. 5th ed. Elsevier Health Sciences; 2017. Morrey's The Elbow and Its Disorders E-Book; p. 23. [Google Scholar]
- 9.Paulsen F., Waschke J. One Volume, English. Elsevier Health Sciences; 2019. Sobotta Clinical Atlas of Human Anatomy; p. 108. [Google Scholar]
- 10.Piquilloud G., Villani F., Casoli V. The medial head of the triceps brachii. Anatomy and blood supply of a new muscular free flap: the medial triceps free flap. Surg Radiol Anat. 2011;33:415–420. doi: 10.1007/s00276-010-0739-9. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt C.C., Kohut G.N., Greenberg J.A., Kann S.E., Idler R.S., Kiefhaber T.R. The anconeus muscle flap: its anatomy and clinical application. J Hand Surg Am. 1999;24:359–369. doi: 10.1053/jhsu.1999.0359. [DOI] [PubMed] [Google Scholar]
- 12.Ward P.J. Elsevier Health Sciences; 2021. Netter's Integrated Musculoskeletal System: Clinical Anatomy Explained; p. 254. [Google Scholar]
- 13.Yamaguchi K., Sweet F.A., Bindra R., Morrey B.F., Gelberman R.H. The extraosseous and intraosseous arterial anatomy of the adult elbow. J Bone Joint Surg Am. 1997;79:1653–1662. doi: 10.2106/00004623-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Orthopaedic Surgeons (AAOS), Elling B., Elling K.M. In: Anatomy & Physiology for the Prehospital Provider. 2nd ed. AAOS Elling B., Elling K.M., editors. Jones & Bartlett Publishers; 2014. Human anatomy and physiology: an overview; p. 6. [Google Scholar]
- 15.McConnell T.H., Hull K.L. Essentials of Anatomy & Physiology. Enhanced Edition. Jones & Bartlett Learning; 2020. Human Form, Human Function; p. 213. [Google Scholar]
- 16.Bertelli J.A., Goklani M.S., Hill E. Anatomy of profunda brachial artery in the axilla and its relationship with the radial nerve: fresh-cadaver anatomical study and clinical observations. J Hand Surg Am. 2024;49(3):278.e1–278.e7. doi: 10.1016/j.jhsa.2022.06.025. [DOI] [PubMed] [Google Scholar]
- 17.Breeland G., Alshuqayfi H.A. StatPearls Publishing; 2021. Anatomy, Shoulder and Upper Limb, Profunda Brachii Artery. [PubMed] [Google Scholar]
- 18.Strauch B., Vasconez L.O., Herman C.K., Lee B.T. Vol 2. 4th ed. Lippincott Williams & Wilkins; 2015. Grabb's Encyclopedia of Flaps: Upper Extremities, Torso, Pelvis, and Lower Extremities. [Google Scholar]
- 19.Casoli V., Kostopoulos E., Pélissier P., Caix P., Martin D., Baudet J. The middle collateral artery: anatomic basis for the “extreme” lateral arm flap. Surg Radiol Anat. 2004;26:172–177. doi: 10.1007/s00276-003-0206-y. [DOI] [PubMed] [Google Scholar]
- 20.Blondeel P.N., Morris S.F., Hallock G.G., Neligan P.C. 2nd ed. CRC Press; 2013. Perforator Flaps: Anatomy, Technique, & Clinical Applications; pp. 304–317. [Google Scholar]
- 21.Standring S. 42nd ed. Elsevier Health Sciences; 2021. Gray's Anatomy E-Book: The Anatomical Basis of Clinical Practice; p. 922. [Google Scholar]
- 22.Wei F., Mardini S. 2nd ed. Elsevier Health Sciences; 2016. Flaps and Reconstructive Surgery E-Book; pp. 93–94. [Google Scholar]
- 23.Kokkalis Z.T., Papanikos E., Mazis G.A., Panagopoulos A., Konofaos P. Lateral arm flap: indications and techniques. Eur J Orthop Surg Traumatol. 2019;29:279–284. doi: 10.1007/s00590-019-02363-0. [DOI] [PubMed] [Google Scholar]
- 24.Strauch B., Yu H. 2nd ed. Thieme; 2011. Atlas of Microvascular Surgery: Anatomy and Operative Techniques; p. 12. [Google Scholar]
- 25.Hildebrandt F. 2nd ed. Schulbuchh; 1800. Lehrbuch der Anatomie des Menschen; p. 107. [Google Scholar]
- 26.Winslow JB. An Anatomical Exposition of the Structure of the Human Body. Translated from the French Original by G. Douglas. 4th ed. 1756:45.
- 27.Winslow JB. An Anatomical Exposition of the Structure of the Human Body. Translated from the French Original by G. Douglas. 6th ed. 1772:60.
- 28.Krause C.F.T. Handbuch der menschlichen Anatomie. Hahn. 1838:746. [Google Scholar]
- 29.Billings J.S. The National Medical Dictionary: Including English, French, German, Italian, and Latin Technical Terms Used in Medicine and the Collateral Sciences, and a Series of Tables of Useful Data. Lea Bros. & Company. 1890:196. [Google Scholar]
- 30.Bock C.E. Anatomisches Taschenbuch: Enthaltend die Anatomie des Menschen. Volckmar. 1841:206. [Google Scholar]
- 31.Henle J. Handbuch der systematischen Anatomie des Menschen: Handbuch der Gefässlehre des Menschen. Friedrich Vieweg und Sohn. 1868:137–138. [Google Scholar]
- 32.Henle J. Handbuch der Systematischen Anatomie des Menschen. Friedrich Vieweg und Sohn. 1876:141–142. [Google Scholar]
- 33.Hollstein L. Lehrbuch der Anatomie des Menschen. Schroeder. 1852:478. [Google Scholar]
- 34.Wilson E. Compendium der Anatomie des Menschen: Mit 150 in dem Text eingedruckten Abbildungen. Schröder. 1842:358. [Google Scholar]
- 35.Barker L.F., Lewis D.D.W., Revell D.G. J. B. Lippincott; 1904. A Laboratory Manual of Human Anatomy; p. 84. [Google Scholar]
- 36.Davis G.G. 3rd ed. J. B. Lippincott; 1915. Applied Anatomy; p. 274. [Google Scholar]
- 37.Gray H. Lea & Febiger; 1918. Anatomy of the Human Body; p. 591. [Google Scholar]
- 38.University of Illinois (Urbana-Champaign Campus) College of Medicine Dept of Anatomy Studies from the Dept. of Anatomy, University of Illinois College of Medicine. https://www.google.com/books/edition/Studies_from_the_Dept_of_Anatomy_Univers/Amk2AQAAMAAJ?hl=en&gbpv=0
- 39.Cunningham D.J. 5th ed. William Wood; 1918. Cunningham's Text-Book of Anatomy; p. 918. [Google Scholar]
- 40.Morris S.H. 6th ed. P. Blakiston; 1921. Morris' Human Anatomy: A Complete Systematic Treatise; p. 615. [Google Scholar]
- 41.Morris H, McMurrich JP. Human Anatomy: A Complete Systematic Treatise by English and American Authors. 4th ed. Blakiston; 1907:1348.
- 42.Morris S.H. 5th ed. P. Blakiston's Son & Company; 1914. Morris's Human Anatomy: A Complete Systematic Treatise by English and American Authors; p. 576. [Google Scholar]
- 43.Federative International Programme for Anatomical Terminology (FIPAT) 2nd ed. 2019. Terminologia Anatomica; p. 205. FIPAT.library.dal.ca; 2019:205. [Google Scholar]
- 44.Cutler H.S., Kelly D., Gross B., et al. Increased articular exposure of the lateral elbow joint with the anconeus approach compared to the Kocher approach: a cadaver study. Arch Orthop Trauma Surg. 2021;141:917–923. doi: 10.1007/s00402-020-03489-1. [DOI] [PubMed] [Google Scholar]
- 45.Martin J., Taqatqeh F., Dragu A., et al. Thumb reconstruction after radical tumor resection using free osteocutaneous lateral arm flap with secondary humerus fracture-a case report. Arch Orthop Trauma Surg. 2023;143(3):1725–1729. doi: 10.1007/s00402-022-04623-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Welle K., Prangenberg C., Hackenberg R.K., Gathen M., Dehghani F., Kabir K. Surgical anatomy of the radial nerve at the dorsal region of the humerus: a cadaveric study. J Bone Joint Surg Am. 2022;104(13):1172–1178. doi: 10.2106/JBJS.21.00482. [DOI] [PubMed] [Google Scholar]
- 47.Johns Hopkins Hospital Bulletin of the Johns Hopkins Hospital. The Hospital. 1907:456. [Google Scholar]
- 48.Kachlik D., Musil V., Baca V. Contribution to the anatomical nomenclature concerning upper limb anatomy. Surg Radiol Anat. 2017;39:405–417. doi: 10.1007/s00276-016-1749-z. [DOI] [PubMed] [Google Scholar]
- 49.Eglseder W.A. Springer; 2017. Atlas of Upper Extremity Trauma: A Clinical Perspective; p. 287. [Google Scholar]