Abstract
Background
Abstinence‐plus interventions promote sexual abstinence as the best means of preventing acquisition of HIV, but also encourage safer‐sex strategies (eg condom use) for sexually active participants.
Objectives
To assess the effects of abstinence‐plus programs for HIV prevention in high‐income countries.
Search methods
We searched 30 electronic databases (eg CENTRAL, PubMed, EMBASE, AIDSLINE, PsycINFO) ending February 2007. Cross‐referencing, hand‐searching, and contacting experts yielded additional citations.
Selection criteria
We included randomized and quasi‐randomized controlled trials evaluating abstinence‐plus interventions in high‐income countries (as defined by the World Bank). Interventions were any efforts that encouraged sexual abstinence as the best means of HIV prevention, but also promoted safer sex. Results were self‐reported biological outcomes, behavioral outcomes, and HIV knowledge.
Data collection and analysis
Three reviewers independently appraised 20070 citations and 325 full‐text papers for inclusion and methodological quality; 39 evaluations were included. Due to heterogeneity and data unavailability, we presented the results of individual studies instead of a meta‐analysis.
Main results
Studies enrolled 37724 North American youth; participants were ethnically diverse. Programs took place in schools (10), community facilities (24), both schools and community facilities (2), healthcare facilities (2), and family homes (1). Median final follow‐up occurred 12 months after baseline.
Results showed no evidence that abstinence‐plus programs can affect self‐reported sexually transmitted infection (STI) incidence, and limited evidence that programs can reduce self‐reported pregnancy incidence. Results for behavioral outcomes were promising; 23 of 39 evaluations found a significantly protective intervention effect for at least one behavioral outcome. Consistently favorable program effects were found for HIV knowledge.
No adverse effects were observed. Several evaluations found that one version of an abstinence‐plus program was more effective than another, suggesting that more research into intervention mechanisms is warranted.
Methodological strengths included large samples and statistical controls for baseline values. Weaknesses included under‐utilization of relevant outcomes, self‐report bias, and analyses neglecting attrition and clustered randomization.
Authors' conclusions
Many abstinence‐plus programs appear to reduce short‐term and long‐term HIV risk behavior among youth in high‐income countries. Evidence for program effects on biological measures is limited. Evaluations consistently show no adverse program effects for any outcomes, including the incidence and frequency of sexual activity. Trials comparing abstinence‐only, abstinence‐plus, and safer‐sex interventions are needed.
Keywords: Humans, Developed Countries, Sexual Abstinence, HIV Infections, HIV Infections/prevention & control, Randomized Controlled Trials as Topic, Safe Sex
Plain language summary
Abstinence‐plus programs for preventing HIV infection in high‐income countries (as defined by the World Bank)
Abstinence‐plus programs are widespread interventions that primarily target young people. On the premise that sexual abstinence is the best way to prevent HIV, abstinence‐plus interventions aim to prevent, stop, or decrease sexual activity; however, programs also promote condom use and other safer‐sexstrategies as alternatives for sexually active participants. Abstinence‐plus programs differ from abstinence‐only interventions, which promote abstinence as the exclusive means of HIV prevention without encouraging safer sex.
This review included 39 randomized and quasi‐randomized controlled trials comparing abstinence‐plus programs to various control groups (eg "usual care," no intervention). Although we conducted an extensive international search for trials, all included studies were conducted among youth in the US, Canada, and the Bahamas (total baseline enrolment=37724 participants). The included programs took place in schools, community centers, and healthcare facilities. We did not conduct a meta‐analysis because of missing data and variation in program designs.
Using various control groups, 24 of 39 evaluations showed a significantly protective intervention effect on at least one biological or behavioral outcome at short‐term, medium‐term, or long‐term follow‐up. Eight trials found no evidence that abstinence‐plus programs affect self‐reported sexually transmitted infection (STI) incidence and limited evidence that programs have a protective effect on self‐reported pregnancy incidence. Results for behavioral outcomes were inconsistent across studies. Findings in almost every trial assessing HIV‐related knowledge favored the intervention group over controls. No harms were observed for any outcome, including incidence and frequency of sexual activity.
Limitations for this review include underreporting of relevant outcomes, reliance on program participants to report their behaviors accurately, and methodological weaknesses in the trials.
Background
Although over two decades have passed since the first AIDS diagnosis, an effective and accessible HIV vaccine remains a distant hope. More than 7600 people died from AIDS‐related causes each day in 2005, while an estimated 38.6 million people worldwide were living with HIV (UNAIDS 2006). Poverty and structural violence, insufficient prevention efforts, and rapid viral evolution contribute to the spread of this "modern plague" (Farmer 2001); approximately 4.1 million new infections occurred in 2005 alone (UNAIDS 2006). In the absence of a vaccine, HIV prevention programs demand continued attention. The HIV pandemic is most devastating for middle‐ and low‐income nations, but new infections continue mounting even in countries with many resources for prevention (Jaffe 2004). The World Health Organization estimated in 2004 that 1.6 million people in high‐income countries were living with HIV (UNAIDS 2004); by 2005, 2.0 million individuals in North America, Western Europe, and Central Europe alone were living with HIV, and 65000 became newly infected in these three regions (UNAIDS 2006). The widespread availability of antiretroviral treatment (ART) allows many individuals in high‐income countries to live longer and healthier lives than their counterparts in resource‐poor countries, but ART is not a cure. Furthermore, even if ART could eliminate the virus, it would still be desirable to prevent the spread of HIV. Primary prevention efforts are still necessary in high‐income countries, particularly among high‐risk groups.
High‐income economies are defined by the World Bank by gross national income as those with a gross national income per capita of $10,726 or higher: Andorra, Antigua and Barbuda, Aruba, Australia, Austria, the Bahamas, Bahrain, Belgium, Bermuda, Brunei Darussalam, Canada, Cayman Islands, Channel Islands, Cyprus, Denmark, Faeroe Islands, Finland, France, French Polynesia, Germany, Greece, Greenland, Guam, Hong Kong (China), Iceland, Ireland, Isle of Man, Israel, Italy, Japan, Korea Rep., Kuwait, Liechtenstein, Luxembourg, Macao (China), Malta, Monaco, Netherlands, Netherlands Antilles, New Caledonia, New Zealand, Norway, Portugal, Puerto Rico, Qatar, San Marino, Saudi Arabia, Singapore, Slovenia, Spain, Sweden, Switzerland, United Arab Emirates, United Kingdom, United States, US Virgin Islands (World Bank 2007).
Sexual behavior outpaces drug injecting as the major cause of HIV infection in many high‐income countries. Studies from the United States suggest that over 70% of HIV‐positive men and women may remain sexually active, and a substantial percentage continue to engage in unprotected sex (Crepaz 2002). The rising prevalence of other sexually transmitted infections (STIs), such as gonorrhea and chlamydia, indicates increased risky sexual behavior in Australia, Western Europe, Japan, and the US. Although sex between men still accounts for most new infections in Australia, Canada, Denmark, Germany, Greece, New Zealand, and the US, evidence suggests that heterosexual sex is responsible for an increasing proportion of seroconversions (UNAIDS 2004). For example, according to UK figures, heterosexual sex accounted for 66% of all new infections in 2003 (AVERT 2005). Major risk groups vary by region (Rivers 2000), but evidence suggests that HIV is now disproportionately concentrated among youth, ethnic minority groups, men who have sex with men, women, and recent immigrants (UNAIDS 2006, Berry 2005, AVERT 2005). In the current socio‐epidemiological climate, primary prevention programs targeting sexual risk behavior are essential for all groups.
Description of the intervention Various behavioral interventions have proven effective in reducing HIV‐risk behaviors in high‐income countries, but a number of prevention strategies still require rigorous evaluation. Abstinence‐based programs are one such approach, consisting of abstinence‐plus and abstinence‐only approaches. The term "abstinence‐based" indicates that the interventions promote sexual abstinence as the best means of HIV infection prevention.
Abstinence‐plus interventions are conducted in a variety of formats, but all use a hierarchical approach to promote sexual abstinence and then safer sex for the prevention of HIV. These interventions convey the message that sexual abstinence is the best or safest behavior choice; interventions encourage both primary abstinence (remaining a virgin) and secondary abstinence (returning to abstinence after experiencing sex in the past). Recognizing that some participants do choose to have sex, abstinence‐plus programs then also encourage sexually active participants to use condoms, limit their number of sexual partners, or practice other safer‐sex behaviors. Abstinence‐plus interventions also typically include extensive information on sexually transmitted infections, pregnancy, contraception, and HIV.
Theoretical bases for abstinence‐plus programs have included social learning theory, the health belief model, the theory of reasoned action, and the theory of planned behavior, and social cognitive theory. The primary targets for abstinence‐based programs are youth, and although the interventions often occur in school settings, they are also implemented in community settings, after‐school groups, clinics, and via media‐based campaigns. These interventions often incorporate or address family involvement, school influences, and community norms as factors that influence behavior, but abstinence‐plus programs fundamentally encourage abstinence and safer sex as individual‐level choices.
Notably, abstinence‐plus programs differ from abstinence‐only programs. Abstinence‐only programs emphasize abstinence as the exclusive means of sexual risk reduction, without encouraging condom use, partner reduction, or other safer‐sex strategies as alternatives for sexually active participants. While abstinence‐only programs present participants with a strict dichotomy (abstinence or sexual activity), abstinence‐plus programs offer participants a pyramid of risk reduction behaviors, in which abstinence is promoted as the safest choice, but then followed by safer sex.
Terminology complicates the discussion of abstinence‐plus programs: programs differ in their specific definitions of "abstinence" and "sex," and possible definitions for these terms vary widely (Haglund 2002, Horan 1998, Pitts 2001, Remez 2000, Sanders 1999, Sonfield 2001). Furthermore, various terms have been used to describe abstinence‐plus interventions, including "comprehensive," "safer‐sex," and "abstinence‐oriented" approaches. Regardless of terminology, programs were included in this review if they used a sexual risk behavior hierarchy that promoted abstinence from any type of sexual activity as the best, but not the only means of preventing the sexual acquisition of HIV.
Why it is important to do this review Although a number of reviews have commented specifically on the intervention effects of abstinence‐only programs (NHS 1997, DiCenso 2002, Franklin 1997, Kirby 2001, Kirby 2006, and Thomas 2000), we have found very few that have specifically defined and discussed the effects of abstinence‐plus interventions. Instead, abstinence‐plus interventions are often reviewed alongside safer‐sex or abstinence‐only programs (eg in Kirby 2006, Jemmott 2000, Kim 1997, Pedlow 2003, Robin 2004), and it can be difficult to determine which programs use a hierarchy and which do not. Bennett 2005 and Manlove 2004 have both evaluated abstinence‐plus programs alongside abstinence‐only approaches, but these reviews focused on pregnancy prevention instead of HIV, and they were limited to programs for United States adolescents. Frost 1995 also evaluated abstinence‐plus programs for pregnancy prevention in US youth, but this was a narrative review without a systematic search strategy. Abstinence‐only and abstinence‐plus programs have been jointly reviewed in the developing world (O'Reilly 2004, O'Reilly 2006); this review found one abstinence‐only and nine abstinence‐plus program evaluations, grouped the evaluations for analysis, and concluded that the interventions had "no impacts on condom use" and a "minimal, but significant effect on abstinence." As yet, however, no reviews exist for high‐income countries. We believe that an international search, a focus on HIV‐related outcomes, and the separation of abstinence‐only from abstinence‐plus programs are required to understand the effects of abstinence‐based programs for HIV prevention in high‐income countries.
Beyond the scientific rationale for this review, a review of abstinence‐plus programs is politically important, not least because abstinence‐plus programs are popular and widespread. Abstinence‐plus programs with a youth focus are particularly common in the United States: a nationally representative US survey of 825 school districts in 1999 discovered that 69% of districts had a specific policy for teaching sex education; of these, 51% districts used abstinence‐plus programs and 35% used abstinence‐only programs (Landry 1999). (The remaining 14% presented abstinence as one option for HIV prevention, but did not state that abstinence was the preferred choice.) This estimate of abstinence‐plus program prevalence does not account for programs that take place outside school settings, and little is known regarding the uptake of abstinence‐plus programs in high‐income countries other than the US.
Abstinence‐based programs, including both abstinence‐only and abstinence‐plus interventions, are also the subject of continuing political debate. Abstinence‐only interventions are frequently criticized for promoting sexual abstinence as the exclusive prevention strategy; one criticism is that the omission of safer sex strategies makes abstinence‐only interventions ineffective or inapplicable to participants who do engage in sexual activity (DiClemente 1998, HRW 2002, Lancet 2004, Lancet 2002, Lancet 2006, Walgate 2004). In contrast, abstinence‐plus programs have been opposed on the grounds that promoting safer sex along with abstinence can "undermine the abstinence message" (Haskins 1997). Critics suggest that safer‐sex promotion can send confusing mixed messages to program participants, "implicitly condone sexual activity among teens," or make participants more likely to engage in sex (Rector 2002). It is also important to investigate whether the abstinence promotion component of abstinence‐plus programs detracts from the effectiveness of safer‐sex messages. By separately reviewing the evidence for abstinence‐only and abstinence‐plus interventions, we aim to address these criticisms directly.
To date, there has been no systematic analysis of the effects of abstinence‐plus programs on HIV prevention among all residents of high‐income countries. This review seeks to identify, synthesize, and evaluate the effects of abstinence‐plus interventions on HIV‐risk behavior and HIV transmission among participants in high‐income countries. This review is a complement to our previous review of abstinence‐only interventions (Underhill 2007b, Underhill 2005, Underhill 2006a, Underhill 2006b); it has also been published in abridged form (Underhill 2007a).
Objectives
To determine the effects of abstinence‐plus programs for preventing HIV infection among participants in high‐income countries.
The interventions were any planned efforts intended to increase rates of abstinence as the best means of HIV prevention, but also intended to increase safer‐sex behaviors such as condom use, partner reduction, or decreased frequency of unprotected sex. The participants were anyone in high‐income countries. Our primary outcome measures were HIV, other STIs, and pregnancy, although we included any trials that assessed a behavioral or biological outcome. We included studies comparing abstinence‐plus programs with the following interventions: no intervention; HIV‐unrelated programs comparable in time and format (ie "attention controls"; for example, these might include a program involving the same activities and the same number of sessions, but focused on abstinence from drugs, not sex); abstinence‐only HIV prevention programs; other abstinence‐plus HIV prevention programs; and HIV prevention programs that did not emphasize abstinence.
Methods
Criteria for considering studies for this review
Types of studies
We included only controlled interventions that evaluated the effects of abstinence‐plus programs designed to influence behavior change on at least one outcome measure related to HIV transmission. These included randomized and quasi‐randomized controlled trials. We defined quasi‐randomized controlled trials as those that approximated randomization by using a method of allocation that was unlikely to lead to consistent bias, such as flipping a coin or alternating participants. Limiting the review to randomized and quasi‐randomized controlled trials was practical because many of the primary outcomes were self‐reported, and random allocation is important to control for both known and unknown confounding. If a meta‐analysis had been feasible, we would have conducted a separate analysis on randomized controlled trials to assess the effects of methodological quality.
Types of participants
We included studies comprised of any participants that were conducted in high‐income countries, as defined by the World Bank (World Bank 2007). Participants did not need to be born in or hold citizenship in a high‐income country, but they must have been present in a high‐income country when the intervention took place. No exclusions were made by intervention setting (eg clinic, school, community center, faith‐based organization) or primary risk group. Because our focus was primary prevention, studies restricted to participants who were already HIV positive were excluded. No exclusions were made by gender, age, sexual orientation, language, occupation, racial or ethnic group, or other characteristics.
Types of interventions
"Abstinence" may be clinically defined as refraining from vaginal, anal, and oral sex. Given inconsistent definitions, this review included studies encouraging abstinence from any one or a combination of these behaviors. We made no exclusions by type of organization delivering the programs (eg schools, healthcare providers, community‐based organizations, faith‐based organizations).
Criteria for abstinence‐plus interventions included the following: 1. the intervention was a planned effort to encourage sexual abstinence or a return to sexual abstinence as the best means of HIV prevention; 2. specific outcomes of interest were presented; 3. HIV prevention was a stated goal of the intervention; 4. the program also promoted condom use, partner reduction, or any other safer‐sex behavior as an alternative to abstinence.
We included studies that used the following comparison groups: 1. no intervention; 2. attention control: interventions that were equal in format and time, but targeted HIV‐unrelated behaviors. For example, a comparison group might have received an intervention with the same number of sessions and the same activities, but the control intervention could have focused on refusing gang membership instead of abstaining from sexual activity; 3. interventions that did not encourage abstinence as a primary outcome (eg condom promotion programs, didactic HIV information sessions); 4. abstinence‐only programs; 5. comparisons between enhanced and non‐enhanced versions of the same program; 6. usual care as defined by the trialist.
Types of outcome measures
Studies reporting outcome measures directly related to HIV transmission (ie self‐reported risk behavior and biological outcomes) were included. Biological (primary) outcomes included the incidence of STIs, HIV, and pregnancy. Examples of risk behavior outcomes included condom use, number of sexual partners, and frequency of unprotected intercourse. If reports included a summary measure of sexual risk, authors were contacted for data on specific outcomes. Where possible, we also examined outcome measures relevant to HIV knowledge, adverse outcomes, program fidelity, cost‐effectiveness, and intervention acceptability.
Biological (primary) outcome measures
HIV incidence
STI incidence
Pregnancy incidence
Behavioral (secondary) outcome measures
Incidence and frequency of unprotected vaginal sex
Incidence and frequency of unprotected oral sex
Incidence and frequency of unprotected anal sex
Incidence and frequency of any vaginal sex
Incidence and frequency of any oral sex
Incidence and frequency of any anal sex
Number of sex partners
Use of male condoms
Use of female condoms
Abstaining from sex if condoms are not used
Duration of abstinence post‐intervention
Return to abstinence (for those who were previously sexually active)
Incidence of sexual initiation
Search methods for identification of studies
We refined our search strategy with recommendations from the Cochrane HIV/AIDS Review Group. No language restrictions were imposed, and translations were sought where necessary. No restrictions on journal of publication were imposed. No country names or other geographical terms were used in the search. Most databases were searched from 1980 onward. Full search strategies for each database are included in Table 1.
1. Search Strategies for Electronic Databases.
| Database | Years Searched | Strategy | Total Records |
| ADOLEC | Inception‐2007 | Inception ‐ 2005, Total Records Retrieved: 504 Search terms: ABSTINENCE [Words] and SEX [Words] and HIV [Words], SEX [Words] and POSTPONE [Words] or ABSTAIN [Words], VIRGIN [Words] or CHASTITY [Words] or CELIBATE [Words], SEX [Words] and EDUCATION [Words] and HIV [Words]. Examined all records. 2005‐2007, Total Records Retrieved: 87 Search terms: sex and education [Palavras] and hiv [Palavras] and 2005 or 2006 or 2007 [País, ano de publicação], abstain and sex, abstain and sex and hiv, postpone and sex, virgin or chaste or chastity or celibate. Examined all records. | 591 |
| AIDSLINE | 1980‐2007 | 1980‐2005, Total Unique Records Retrieved: 1450 #1 PT=RANDOMIZED CONTROLLED TRIAL #2 PT=CONTROLLED CLINICAL TRIAL #3 RANDOMIZED CONTROLLED TRIALS #4 RANDOM ALLOCATION #5 DOUBLE BLIND METHOD #6 SINGLE BLIND METHOD #7 PT=CLINICAL TRIAL #8 CLINICAL TRIALS OR CLINICAL TRIALS, PHASE I OR CLINICAL TRIALS, PHASE II OR CLINICAL TRIALS, PHASE III OR CLINICAL TRIALS, PHASE IV OR CONTROLLED CLINICAL TRIALS OR MULTICENTER STUDIES #9 (SINGL* OR DOUBL* OR TREBL* OR TRIPL*) NEAR6 (BLIND* OR MASK*) #10 CLIN* NEAR6 TRIAL* #11 CLIN* NEAR6 TRIAL* #12 PLACEBOS #13 RANDOM* #14 RANDOM* #15 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 #16 ANIMALS NOT (HUMAN AND ANIMALS) #17 #15 NOT #16 #18 SEXUAL ABSTINENCE [MESH] #19 ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED)) #20 #18 OR #19 #21 #17 AND #20 AND PY=1980‐2005 2005‐2007, Total Unique Records Retrieved: 16 #1 PT=RANDOMIZED CONTROLLED TRIAL #2 PT=CONTROLLED CLINICAL TRIAL #3 RANDOMIZED CONTROLLED TRIALS #4 RANDOM ALLOCATION #5 DOUBLE BLIND METHOD #6 SINGLE BLIND METHOD #7 PT=CLINICAL TRIAL #8 CLINICAL TRIALS OR CLINICAL TRIALS, PHASE I OR CLINICAL TRIALS, PHASE II OR CLINICAL TRIALS, PHASE III OR CLINICAL TRIALS, PHASE IV OR CONTROLLED CLINICAL TRIALS OR MULTICENTER STUDIES #9 (SINGL* OR DOUBL* OR TREBL* OR TRIPL*) NEAR6 (BLIND* OR MASK*) #10 CLIN* NEAR6 TRIAL* #11 CLIN* NEAR6 TRIAL* #12 PLACEBOS #13 RANDOM* #14 RANDOM* #15 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 #16 ANIMALS NOT (HUMAN AND ANIMALS) #17 #15 NOT #16 #18 SEXUAL ABSTINENCE [MESH] #19 ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED)) #20 #18 OR #19 #21 #17 AND #20 AND PY=2005‐2007 | 1465 |
| Bibliomap | 1887‐2007 | 1887‐2005, Total Unique Records Retrieved: 52 Search terms: EVALUATION AND SEXUAL HEALTH, ABSTINENCE AND SEX AND HIV, SEX AND (POSTPONE OR ABSTAIN), POSTPONE AND SEX, DELAY AND SEX, CHASTITY AND SEX, CHASTITY, VIRGIN, SEX AND EDUCATION AND HIV. 2005‐2007, Total Unique Records Retrieved: 154 abstinen* or abstain* or chastity or chaste or virgin* or celiba* or "sex education" | 206 |
| BIOSIS | 1969‐2007 | 1969‐2005, Total Unique Records Retrieved: 1061 (((ABSTINEN* or ABSTAIN* or postpon* or DELAY*) and SEX*) or CHASTITY or CHASTE or VIRGIN* or CELIBA* or (SEX* and EDUCAT*)) and (HIV* or AIDS*) and ((control* or trial* or random* or blind* or (clinical and trial*) or (research and design) or compar* or evaluation) not (animals not human)) 2005‐2007, Total Unique Records Retrieved: 185 #1(((ABSTINEN* or ABSTAIN* or postpon* or DELAY*) and SEX*) or CHASTITY or CHASTE or VIRGIN* or CELIBA* or (SEX* and EDUCAT*)) and (PY:BXCD = 2005‐2006) #2(HIV* or AIDS*) and (PY:BXCD = 2005‐2006) #3((control* or trial* or random* or blind* or (clinical and trial*) or (research and design) or compar* or evaluation) not (animals not human)) and (PY:BXCD = 2005‐2006) #4#1 and #2 and #3 and (PY:BXCD = 2005‐2006) *Records for 2007 were not yet available in Feb 2007. | 1246 |
| Catalog of US Government Publications | 1976‐2007 | 1976 ‐ 2005, Total Records Retrieved: 133 Search terms: Abstinence AND sex, (ABSTINEN* OR ABSTAIN* OR DELAY* OR POSTPON*) AND SEX, SEX* AND EDUCATION*, (SEX* AND EDUCATION*) AND (HIV* OR AIDS*). Examined all records. 2005‐2007, Total Records Retrieved: 295 Search terms: Abstinence AND sex, (ABSTINEN* OR ABSTAIN* OR DELAY* OR POSTPON*) AND SEX, SEX* AND EDUCATION*, (SEX* AND EDUCATION*) AND (HIV* OR AIDS*). Examined all records. | 428 |
| CENTRAL | 1980‐2007 | 1980‐2005, Total Unique Records Retrieved: 74 #1hiv OR hiv‐1* OR hiv‐2* OR hiv1 OR hiv2 OR (HIV INFECT*) OR (HUMAN IMMUNODEFICIENCY VIRUS) OR (HUMAN IMMUNEDEFICIENCY VIRUS) OR (HUMAN IMMUNE‐DEFICIENCY VIRUS) OR (HUMAN IMMUNO‐DEFICIENCY VIRUS) OR (HUMAN IMMUN* DEFICIENCY VIRUS) OR (ACQUIRED IMMUNODEFICIENCY SYNDROME) OR (ACQUIRED IMMUNEDEFICIENCY SYNDROME) OR (ACQUIRED IMMUNO‐DEFICIENCY SYNDROME) OR (ACQUIRED IMMUNE‐DEFICIENCY SYNDROME) OR (ACQUIRED IMMUN* DEFICIENCY SYNDROME) in All Fields in all products #2MeSH descriptor HIV Infections explode all trees in MeSH products #3MeSH descriptor HIV explode all trees in MeSH products #4MeSH descriptor Sexually Transmitted Diseases, Viral, this term only in MeSH products #5(#1 OR #2 OR #3 OR #4) #6MeSH descriptor Sexual Abstinence explode all trees in MeSH products #7ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED)) in All Fields in all products #8(#6 OR #7) #9(#5 AND #8), from 1980 to 2005 2005‐2007, Total Unique Records Retrieved: 138 #1(hiv OR hiv‐1* OR hiv‐2* OR hiv1 OR hiv2 OR (HIV INFECT*) OR (HUMAN IMMUNODEFICIENCY VIRUS) OR (HUMAN IMMUNEDEFICIENCY VIRUS) OR (HUMAN IMMUNE‐DEFICIENCY VIRUS) OR (HUMAN IMMUNO‐DEFICIENCY VIRUS) OR (HUMAN IMMUN* DEFICIENCY VIRUS) OR (ACQUIRED IMMUNODEFICIENCY SYNDROME) OR (ACQUIRED IMMUNEDEFICIENCY SYNDROME) OR (ACQUIRED IMMUNO‐DEFICIENCY SYNDROME) OR (ACQUIRED IMMUNE‐DEFICIENCY SYNDROME) OR (ACQUIRED IMMUN* DEFICIENCY SYNDROME)), from 2005 to 2007 #2MeSH descriptor HIV Infections explode all trees #3MeSH descriptor HIV explode all trees #4MeSH descriptor Sexually Transmitted Diseases, Viral explode all trees #5MeSH descriptor Sexual Abstinence explode all trees #6ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED)) #7(( #1 OR #2 OR #3 OR #4 ) AND ( #5 OR #6 )), from 2005 to 2007 | 212 |
| CHID | 1985‐2005 | Search terms: Abstinence, Sex Education, Abstinence and Sex, examined records, most were program manuals or propaganda materials, no visible evaluations, even when using the "professional" audience filter. Examined all records. *CHID was taken off‐line in September 2006. | 0 relevant |
| CINAHL | 1982‐2007 | 1982‐2005, Total Unique Records Retrieved: 4079 (((ABSTINEN* or ABSTAIN* or postpon* or DELAY*) and SEX*) or CHASTITY or CHASTE or VIRGIN* or CELIBA* or (SEX* and EDUCAT*)) and (HIV* or AIDS*) and ((control* or trial* or random* or blind* or (clinical and trial*) or (research and design) or compar* or evaluation) not (animals not human)) 2005‐2007, Total Unique Records Retrieved: 143 #1((((ABSTINEN$ or ABSTAIN$ or postpon$ or DELAY$) and SEX$) or CHASTITY or CHASTE or VIRGIN$ or CELIBA$ or (SEX$ and EDUCAT$)) and (HIV$ or AIDS$) and ((control$ or trial$ or random$ or blind$ or (clinical and trial$) or (research and design) or compar$ or evaluation) not (animals not human))).mp. [mp=title, subject heading word, abstract, instrumentation] #2(((ABSTINEN$ or ABSTAIN$ or postpon$ or DELAY$) and SEX$) or CHASTITY or CHASTE or VIRGIN$ or CELIBA$ or (SEX$ and EDUCAT$)).mp. [mp=title, subject heading word, abstract, instrumentation] #3(HIV$ or AIDS$).mp. [mp=title, subject heading word, abstract, instrumentation] #4((control$ or trial$ or random$ or blind$ or (clinical and trial$) or (research and design) or compar$ or evaluat$) not (animals not human)).mp. [mp=title, subject heading word, abstract, instrumentation] #52 and 3 and 4 #6limit 5 to yr="2005 ‐ 2007" | 4222 |
| CSA Illumina ‐ includes ASSIA, ERIC, Political Science Abstracts, Social Services Abstracts, and Sociological Abstracts | 1963‐2007 | Sociological Abstracts [1963‐], ERIC [1991‐], ASSIA [1987‐], Political Science Abstracts [1975‐], and Social Services Abstracts [1979‐]. Searched until Febuary 15, 2007 Total Unique Records Retrieved: 1179 1975‐2005, Total Unique Records Retrieved: 841 ((ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED))) and (HIV* or AIDS*)) and (randomized controlled trial OR controlled clinical trial OR randomized controlled trials OR random allocation OR double‐blind method OR single‐blind method OR clinical trial OR clinical trials OR random* OR research design OR comparative study OR evaluation NOT (animals NOT human)) 2005‐2007, Total Unique Records Retrieved: 338 (ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED))) and (HIV* or AIDS*) and (randomized controlled trial OR controlled clinical trial OR randomized controlled trials OR random allocation OR double‐blind method OR single‐blind method OR clinical trial OR clinical trials OR random* OR research design OR comparative study OR evaluation NOT (animals NOT human)), Date Range: 2005‐2007 | 1179 |
| DARE | 1991‐2007 | 1991‐2005, Total Unique Records Retrieved: 127 Search terms: HIV, ABSTINENCE, VIRGINITY, VIRGIN, POSTPON* SEX, AIDS 2005‐2007, Total Unique Records Retrieved: 122 Search terms: HIV, ABSTINENCE, VIRGINITY, VIRGIN, POSTPON* SEX, AIDS | 249 |
| Dissertation Abstracts International (UMI Proquest) | 1997‐2007 | 1 KEY(abstinence) or TI(abstinence) or AB(abstinence) 2 #1 and (KEY(hiv) or TI(hiv) or AB(hiv)) | 64 |
| EMBASE | 1974‐2007 | 1980‐2005, Total Unique Records Retrieved: 622 #1 ('human immunodeficiency virus infection'/exp) OR ('human immunodeficiency virus'/exp) OR (hiv:ti OR hiv:ab) OR ('hiv‐1':ti OR 'hiv‐1':ab) OR ('hiv‐2':ti OR 'hiv‐2':ab) OR ('human immunodeficiency virus':ti OR 'human immunodeficiency virus':ab) OR ('human immuno‐deficiency virus':ti OR 'human immuno‐deficiency virus':ab) OR ('human immunedeficiency virus':ti OR 'human immunedeficiency virus':ab) OR ('human immune‐deficiency virus':ti OR 'human immune‐deficiency virus':ab) OR ('acquired immune‐deficiency syndrome':ti OR 'acquired immune‐deficiency syndrome':ab) OR ('acquired immunedeficiency syndrome':ti OR 'acquired immunedeficiency syndrome':ab) OR ('acquired immunodeficiency syndrome':ti OR 'acquired immunodeficiency syndrome':ab) OR ('acquired immuno‐deficiency syndrome':ti OR 'acquired immuno‐deficiency syndrome':ab) #2 (random*:ti OR random*:ab) OR (factorial*:ti OR factorial*:ab) OR (cross?over*:ti OR cross?over:ab OR crossover*:ti OR crossover*:ab) OR (placebo*:ti OR placebo*:ab) OR (((doubl*:ti AND blind*:ti) OR (doubl*:ab AND blind*:ab))) OR (((singl*:ti AND blind*:ti) OR (singl*:ab AND blind*:ab))) OR (assign*:ti OR assign*:ab) OR (volunteer*:ti OR volunteer*:ab) OR ('crossover procedure'/de) OR ('double‐blind procedure'/de) OR ('single‐blind procedure'/de) OR ('randomized controlled trial'/de) OR (allocat*:ti OR allocat*:ab) #3 sexual AND 'abstinence'/exp #4 'abstinence'/de OR abstain* OR chastity OR chaste OR virgin* OR celiba* OR (sex* AND educat*) OR (sex* AND (marriage* OR married)) #5 #3 OR #4 #6 #1 AND #2 AND #5 #7 #1 AND #2 AND #5 AND [1980‐2005]/py 2005‐2007, Total Unique Records Retrieved: 83 #1exp human immunodeficiency virus infection/ or exp human immunodeficiency virus/ or hiv.ti,ab. or hiv‐1.ti,ab. or hiv‐2.ti,ab. or human immunodeficiency virus.ti,ab. or human immuno‐deficiency virus.ti,ab. or human immunedeficiency virus.ti,ab. or human immune‐deficiency virus.ti,ab. or acquired immune‐deficiency syndrome.ti,ab. or acquired immunedeficiency syndrome.ti,ab. or acquired immunodeficiency syndrome.ti,ab. or acquired immuno‐deficiency syndrome.ti,ab. #2(random$ or factorial or cross?over or crossover or placebo).ti,ab. or ((doubl$ and blind$).ti. or (doubl$ and blind$).ab.) or ((singl$ and blind$).ti. or (singl$ and blind$).ab.) or (assign$.ti. or assign$.ab.) or (volunteer$.ti. or volunteer$.ab.) or exp crossover procedure/ or exp double‐blind procedure/ or exp single‐blind procedure/ or exp randomized controlled trial/ or allocat$.ti,ab. #3exp abstinence/ and sex$.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] #4exp abstinence/ or abstain$.mp. or chastity.mp. or chaste.mp. or virgin$.mp. or celiba$.mp. or (sex$ and educat$).mp. or (sex$ and (marriage$ or married)).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] #53 or 4 #61 and 2 and 5 #7limit 6 to yr="2005 ‐ 2007" | 705 |
| EurasiaHealth Knowledge Multilingual Library | Inception‐2007 | Inception ‐ 2005, Total Records Retrieved: 452 Search terms: Abstinence, Abstain, Sexual health, AIDS, HIV, HIV Prevention. Examined all records. 2005‐2007, Total Records Retrieved: 488 Search terms: Abstinence, Abstain, Sexual health, AIDS, HIV, HIV Prevention. Examined all records. | 940 |
| HealthPromis | 1997‐2005 | Search Terms: HIV, AIDS, Abstinence. Examined all records. | 14 |
| OVID 2005 ‐ includes SIGLE and Global Health | 1973‐2005 | SIGLE (1980 ‐ May 28, 2005) and Global Health (1973 ‐ May 28, 2005) Total Unique Records Retrieved: 683 (((ABSTINEN* or ABSTAIN* or postpon* or DELAY*) and SEX*) or CHASTITY or CHASTE or VIRGIN* or CELIBA* or (SEX* and EDUCAT*)) and (HIV* or AIDS*) and ((control* or trial* or random* or blind* or (clinical and trial*) or (research and design) or compar* or evaluation) not (animals not human)) *Please see Ovid 2007 search for Global Health 2005‐2007. SIGLE was taken off line in 2005. | 683 |
| OVID 2007 ‐ includes AMED, BNI, HMIC, and Global Health | 2005‐2007 | AMED [2005‐], BNI [2005‐], HMIC [2005‐], and Global Health [2005‐], Searched February 15, 2007 Total Unique Records Retrieved: 118 #1(((ABSTINEN$ or ABSTAIN$ or postpon$ or DELAY$) and SEX$) or CHASTITY or CHASTE or VIRGIN$ or CELIBA$ or (SEX$ and EDUCAT$)).mp. [mp=ab, hw, ti, ot, bt] #2(HIV$ or AIDS$).mp. [mp=ab, hw, ti, ot, bt] #3((control$ or trial$ or random$ or blind$ or (clinical and trial$) or (research and design) or compar$ or evaluat$) not (animals not human)).mp. [mp=ab, hw, ti, ot, bt] #41 and 2 and 3 #5limit 4 to yr="2005 ‐ 2007" | 118 |
| PAIS 2007 | 2005‐2007 | 1972‐2005, see WebSpirs 2005 ‐ February 15, 2007 Total Unique Records Retrieved: 9 (ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED))) and (hiv* or aids*) and (randomized controlled trial OR controlled clinical trial OR randomized controlled trials OR random allocation OR double‐blind method OR single‐blind method OR clinical trial OR clinical trials OR random* OR research design OR comparative study OR evaluation NOT (animals NOT human)) | 9 |
| PsycINFO | 1887‐2007 | 1887‐2005, Total Unique Records Retrieved: 1146 ((ABSTINEN* or ABSTAIN* or postpon* or DELAY*) and SEX*) or CHASTITY or CHASTE or VIRGIN* or CELIBA* or (SEX* and EDUCAT*)) and (HIV* or AIDS*) and ((control* or trial* or random* or blind* or (clinical and trial*) or (research and design) or compar* or evaluation) not (animals not human)) 2005‐2007, Total Unique Records Retrieved: 99 #1((((ABSTINEN$ or ABSTAIN$ or postpon$ or DELAY$) and SEX$) or CHASTITY or CHASTE or VIRGIN$ or CELIBA$ or (SEX$ and EDUCAT$)) and (HIV$ or AIDS$) and ((control$ or trial$ or random$ or blind$ or (clinical and trial$) or (research and design) or compar$ or evaluation) not (animals not human))).mp. [mp=title, abstract, heading word, table of contents, key concepts] #2limit 1 to yr="2005 ‐ 2007" | 1245 |
| PubMed | 1980‐2007 | 1980‐2005, Total Unique Records Retrieved: 5164 #1 Search HIV Infections[MeSH] OR HIV[MeSH] OR hiv[tw] OR hiv‐1*[tw] OR hiv‐2*[tw] OR hiv1[tw] OR hiv2[tw] OR hiv infect*[tw] OR human immunodeficiency virus[tw] OR human immunedeficiency virus[tw] OR human immuno‐deficiency virus[tw] OR human immune‐deficiency virus[tw] OR ((human immun*) AND (deficiency virus[tw])) OR acquired immunodeficiency syndrome[tw] OR acquired immunedeficiency syndrome[tw] OR acquired immuno‐deficiency syndrome[tw] OR acquired immune‐deficiency syndrome[tw] OR ((acquired immun*) AND (deficiency syndrome[tw])) OR "Sexually Transmitted Diseases, Viral"[MeSH:NoExp] #2 Search SEXUAL ABSTINENCE [MESH] #3 Search ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED)) #4 Search #2 OR #3 #5 Search randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized controlled trials [mh] OR random allocation [mh] OR double‐blind method [mh] OR single‐blind method [mh] OR clinical trial [pt] OR clinical trials [mh] OR ("clinical trial" [tw]) OR ((singl* [tw] OR doubl* [tw] OR trebl* [tw] OR tripl* [tw]) AND (mask* [tw] OR blind* [tw])) OR ( placebos [mh] OR placebo* [tw] OR random* [tw] OR research design [mh:noexp] OR comparative study [mh] OR evaluation studies [mh] OR follow‐up studies [mh] OR prospective studies [mh] OR control* [tw] OR prospectiv* [tw] OR volunteer* [tw]) NOT (animals [mh] NOT human [mh]) #6Search #1 AND #4 AND #5 Field: All Fields, Limits: Publication Date from 1980 to 2005 2005‐2007, Total Unique Records Retrieved: 595 #1 Search HIV Infections[MeSH] OR HIV[MeSH] OR hiv[tw] OR hiv‐1*[tw] OR hiv‐2*[tw] OR hiv1[tw] OR hiv2[tw] OR hiv infect*[tw] OR human immunodeficiency virus[tw] OR human immunedeficiency virus[tw] OR human immuno‐deficiency virus[tw] OR human immune‐deficiency virus[tw] OR ((human immun*) AND (deficiency virus[tw])) OR acquired immunodeficiency syndrome[tw] OR acquired immunedeficiency syndrome[tw] OR acquired immuno‐deficiency syndrome[tw] OR acquired immune‐deficiency syndrome[tw] OR ((acquired immun*) AND (deficiency syndrome[tw])) OR "Sexually Transmitted Diseases, Viral"[MeSH:NoExp] Limits: Publication Date from 2005 to 2007 #2 Search SEXUAL ABSTINENCE [MESH] Limits: Publication Date from 2005 to 2007 #3 Search ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED)) Limits: Publication Date from 2005 to 2007 #4 Search #2 OR #3 Limits: Publication Date from 2005 to 2007 #5 Search randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized controlled trials [mh] OR random allocation [mh] OR double‐blind method [mh] OR single‐blind method [mh] OR clinical trial [pt] OR clinical trials [mh] OR ("clinical trial" [tw]) OR ((singl* [tw] OR doubl* [tw] OR trebl* [tw] OR tripl* [tw]) AND (mask* [tw] OR blind* [tw])) OR ( placebos [mh] OR placebo* [tw] OR random* [tw] OR research design [mh:noexp] OR comparative study [mh] OR evaluation studies [mh] OR follow‐up studies [mh] OR prospective studies [mh] OR control* [tw] OR prospectiv* [tw] OR volunteer* [tw]) NOT (animals [mh] NOT human [mh]) Limits: Publication Date from 2005 to 2007 #6 Search #1 AND #4 AND #5 Limits: Publication Date from 2005 to 2007 | 5759 |
| SciSearch (Web of Knowledge): Biomedical abstracts | 1974‐2007 | 1974‐2005, Total Unique Records Retrieved: 21 #1 topic=(((ABSTINEN* OR ABSTAIN*) and SEX*) OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*)) Database=Web of Science; Timespan=Latest 5 Years #2 topic=(HIV* OR AIDS*) Database=Web of Science; Timespan=Latest 5 Years #3 topic=((randomized SAME controlled) OR control* OR trial* OR random* OR double‐blind* OR single‐blind* OR (clinical AND trial*) OR (research SAME design) OR comparative OR evaluation NOT (animals NOT human)) Database=Web of Science; Timespan=Latest 5 Years #4 topic=((((ABSTINEN* OR ABSTAIN*) and SEX*) OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*)) and (HIV* OR AIDS*) and ((randomized SAME controlled) OR control* OR trial* OR random* OR double‐blind* OR single‐blind* OR (clinical AND trial*) OR (research SAME design) OR comparative OR evaluation NOT (animals NOT human))) 2005‐2007, Total Unique Records Retrieved: 66 #1 topic=(((ABSTINEN* OR ABSTAIN*) and SEX*) OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*)) Database=Web of Science; Timespan=Latest 5 Years #2 topic=(HIV* OR AIDS*) Database=Web of Science; Timespan=Latest 5 Years #3 topic=((randomized SAME controlled) OR control* OR trial* OR random* OR double‐blind* OR single‐blind* OR (clinical AND trial*) OR (research SAME design) OR comparative OR evaluation NOT (animals NOT human)) Database=Web of Science; Timespan=Latest 5 Years #4 topic=((((ABSTINEN* OR ABSTAIN*) and SEX*) OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*)) and (HIV* OR AIDS*) and ((randomized SAME controlled) OR control* OR trial* OR random* OR double‐blind* OR single‐blind* OR (clinical AND trial*) OR (research SAME design) OR comparative OR evaluation NOT (animals NOT human))) Database=Web of Science; Timespan=Latest 5 Years Examined records from 2005‐2007. | 87 |
| TROPHI | Inception‐2007 | Inception ‐ 2005, Total Records Retrieved: 176 Search terms: abstinence AND sex AND HIV, sex and (postpone or abstain), postpone AND sex, delay AND sex, chastity, virgin, sex education AND HIV, HIV OR AIDS. Examined all records. 2005‐2007, Total Records Retrieved: 200 Search terms: abstinence and sex, virgin, postpone sex, abstain, HIV. Examined all records from 2005‐2007. | 376 |
| WEBSPIRS 2005 ‐ includes AMED, BNI, RCN Journals, HMIC, PAIS, and SERFILE | 1972‐2005 | AMED [1985‐], BNI [1985‐], RCN [1985‐1996], HMIC [1983‐], SERFILE [Inception‐], and PAIS [1972‐], Searched May 28, 2005 Total Unique Records Retrieved: 94 (((ABSTINEN* or ABSTAIN* or postpon* or DELAY*) and SEX*) or CHASTITY or CHASTE or VIRGIN* or CELIBA* or (SEX* and EDUCAT*)) and (HIV* or AIDS*) and ((control* or trial* or random* or blind* or (clinical and trial*) or (research and design) or compar* or evaluation) not (animals not human)) *For 2005‐2007 searches of AMED, BNI, and HMIC, see the search of OVID. For 2005‐2007 searches of PAIS, see PAIS. RCN was searchable via BNI in 2007. | 94 |
Electronic Databases We searched the following electronic databases, ending February 15, 2007: 1. ADOLEC (Inception‐2007) 2. AIDSLINE (1980‐2007) 3. AMED (1985‐2007) 4. ASSIA (1987‐2007) 5. BiblioMap (1887‐2007) 6. BIOSIS (1969‐2007) 7. BNI (1985‐2007) 8. Catalog of US Government Publications (1976‐2007) 9. CENTRAL (Cochrane Central Register of Controlled Trials) (1980‐2007) 10. CHID (1985‐2005; went offline in 2005) 11. CINAHL (1982‐2007) 12. DARE (1991‐2007) 13. Dissertation Abstracts International (1997‐2007) 14. EMBASE (1974‐2007) 15. ERIC (1991‐2007) 16. EurasiaHealth Knowledge Multilingual Library (Inception‐2007) 17. Global Health Abstracts (1973‐2007) 18. HealthPromis (1997‐2005; went offline in 2005) 19. HMIC (1983‐2007) 20. PAIS (1972‐2007) 21. Political Science Abstracts (1975‐2007) 22. PsycINFO (1887‐2007) 23. PubMed (1980‐2007) 24. RCN (1985‐1996; updating ended in 1996) 25. SCISEARCH (Web of Knowledge) (1974‐2007) 26. SERFILE (Inception ‐ 2005; inaccessible in 2007) 27. SIGLE (1980‐2005; went offline in 2005) 28. Social Services Abstracts (1979‐2007) 29. Sociological Abstracts (1963‐2007) 30. TRoPHI (Inception‐2007)
Other relevant libraries of international agencies, especially those concerned with the prevention of HIV/AIDS (UNAIDS, USAID, WHO, UNFPA, World Bank, and Centers for Disease Control and Prevention) were searched. We made additional efforts to identify and acquire unpublished literature.
Hand‐Searching We hand‐searched various conference proceedings from 2000 onwards to identify unpublished reports. These included proceedings from the International AIDS Conference, the Conferences on Retroviruses and Opportunistic Infections, the US National HIV Prevention Conferences, the Abstinence Education Evaluation Conference, and the International Society of STD Research (ISSTDR).
Personal communication We contacted leading experts in the field of abstinence‐based programs to solicit potentially relevant unpublished papers, ongoing research, and suggestions for other contacts.
Cross References The reference lists of related reviews and all articles obtained were examined for additional citations.
Search Terms We searched with combinations of the following terms. MeSH terms (eg "Sexual Abstinence") were also identified and included. We did not include country names or program names, as they may not be specified in searchable headings.
Intervention terms: abstinence, abstain, chastity, chaste, virgin, celibacy, celibate, sex education, marriage, delay, postpone.
Study terms: randomized controlled trial, controlled clinical trial, random allocation, double‐blind, single‐blind, clinical trial, mask, comparative study, control, pre‐post controlled designs, comparison group, cohort study, comparative study, evaluation study, feasibility study, follow up studies.
HIV terms: HIV Infections, HIV, HIV‐1, HIV‐2, human immunodeficiency virus, human immunedeficiency virus, human immuno‐deficiency virus, human immune‐deficiency virus, AIDS, acquired immunodeficiency syndrome, acquired immunedeficiency syndrome, acquired immuno‐deficiency syndrome, acquired immune‐deficiency syndrome, sexually transmitted diseases.
PUBMED SAMPLE SEARCH STRATEGY #1 Search HIV Infections[MeSH] OR HIV[MeSH] OR hiv[tw] OR hiv‐1*[tw] OR hiv‐2*[tw] OR hiv1[tw] OR hiv2[tw] OR hiv infect*[tw] OR human immunodeficiency virus[tw] OR human immunedeficiency virus[tw] OR human immuno‐deficiency virus[tw] OR human immune‐deficiency virus[tw] OR ((human immun*) AND (deficiency virus[tw])) OR acquired immunodeficiency syndrome[tw] OR acquired immunedeficiency syndrome[tw] OR acquired immuno‐deficiency syndrome[tw] OR acquired immune‐deficiency syndrome[tw] OR ((acquired immun*) AND (deficiency syndrome[tw])) OR "Sexually Transmitted Diseases, Viral"[MeSH:NoExp] Limits: Publication Date from 1980 to 2007 #2 Search SEXUAL ABSTINENCE [MESH] Limits: Publication Date from 1980 to 2007 #3 Search ABSTINENCE OR ABSTAIN* OR CHASTITY OR CHASTE OR VIRGIN* OR CELIBA* OR (SEX* AND EDUCAT*) OR (SEX* AND (MARRIAGE* OR MARRIED)) Limits: Publication Date from 1980 to 2007 #4 Search #2 OR #3 Limits: Publication Date from 1980 to 2007 #5 Search randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized controlled trials [mh] OR random allocation [mh] OR double‐blind method [mh] OR single‐blind method [mh] OR clinical trial [pt] OR clinical trials [mh] OR ("clinical trial" [tw]) OR ((singl* [tw] OR doubl* [tw] OR trebl* [tw] OR tripl* [tw]) AND (mask* [tw] OR blind* [tw])) OR ( placebos [mh] OR placebo* [tw] OR random* [tw] OR research design [mh:noexp] OR comparative study [mh] OR evaluation studies [mh] OR follow‐up studies [mh] OR prospective studies [mh] OR control* [tw] OR prospectiv* [tw] OR volunteer* [tw]) NOT (animals [mh] NOT human [mh]) Limits: Publication Date from 1980 to 2007 #6 Search #1 AND #4 AND #5 Limits: Publication Date from 1980 to 2007
Data collection and analysis
Selection of studies All reviewers independently examined citations reviewed by the search strategy. KU obtained full‐text articles of potentially relevant papers. All reviewers independently assessed their eligibility using an eligibility form based on pre‐specified inclusion criteria. Reasons for excluding potentially relevant trials are specified in the "Characteristics of Excluded Studies." We contacted the authors for clarification when necessary. Disagreements were resolved by discussion and, if necessary, referral to the Cochrane HIV/AIDS Review Group.
Data extraction and management All reviewers independently extracted data on study design, participants, interventions, outcomes and methodological quality using pre‐designed data collection forms. Any disagreements were resolved by discussion and referral to the Cochrane HIV/AIDS Review Group if necessary.
The extracted data included the following measures: citation, study design, methodological criteria, inclusion and exclusion criteria, comparison group intervention, participant characteristics, trial setting, theoretical basis for intervention, elements of intervention, all relevant outcome measures, and results. We expected the trial settings to vary widely (eg schools, clinics, prisons, community centers, and churches), and examined this carefully when considering the heterogeneity of our data set. We also examined any process or cost‐effectiveness data reported, including training, monitoring, acceptability, costs, and sustainability.
Where reports were uncertain or included summary measures, authors were contacted for clarification. We noted any data that was consistently underreported, and highlighted this deficit along with future research needs in the discussion.
Assessment of methodological quality of included studies Depending on study design, we evaluated the following methodological components, since there is evidence that these may be associated with biased estimates of effects. 1. Similarity of the intervention and control groups (whether groups were treated equally except for the intervention). 2. Method of generation of the randomization sequence. 3. Generation of allocation concealment. 4. Blinding (participants, intervention staff, and outcome assessors). 5. Intention‐to‐treat analysis. 6. Loss to follow up. In our results and discussion sections, we highlight attrition as a particular limitation of any studies with a total dropout exceeding one third of baseline enrolment.
Measures of treatment effect To investigate the feasibility of a meta‐analysis, all eligible studies were summarized in RevMan to the fullest extent possible. All reviewers assisted in abstracting the data, with KU entering all data into RevMan and DO and PM checking all entries. Disagreements were resolved by discussion. A narrative synthesis was provided for all results, but we determined that a statistical meta‐analysis was not appropriate for this review due to differences in program and evaluation design, underreporting of key data, and inability to retrieve unpublished or missing data from authors. Had the studies been comparable and more completely reported, our meta‐analysis would have measured the weighted average effect size for each outcome measure, weighted mean differences (for continuous outcomes), odds ratios of effects (for dichotomous outcomes), and 95% confidence intervals. Odds ratios less than one would have expressed a protective intervention effect.
Unit of analysis issues Studies with multiple treatment groups A meta‐analysis was not conducted for this version of the review. However, had meta‐analysis been possible, we would have dealt with multiple treatment groups in the following way: When studies had more than 2 treatment groups, we planned to accept only 2 groups for the meta‐analysis. In keeping with procedures used by the US HIV/AIDS Prevention Research Synthesis project (Johnson 2002), we planned to take the arm with the greatest or most intense exposure (as identified by the trialist), compared to the arm with the least or least intense exposure, thereby giving each study the most favorable chance of yielding significant program effects. When different trial arms emphasized sexual abstinence to differing extents, we would have accepted the arm that emphasized abstinence the most, compared to the arm that emphasized abstinence the least.
Cross‐over trials We did not anticipate dealing with these trials in the review, and no cross‐over trials were recovered by the search. If we had identified any studies using this design, we would have analyzed only the follow‐up data from the period before the cross over.
Cluster randomized trials When studies use cluster randomization, analyzing the data at the level of the individual participant has two implications. First, p‐values may be artificially small, suggesting significant effects where none occurred (Higgins 2005). Second, the confidence intervals for these results may appear artificially narrow, which would cause the studies to receive disproportionately more weight in the context of a meta‐analysis (Donner 2002, Johnson 2002). The second concern was unimportant for this version of the review because no meta‐analysis was conducted. However, the first remained relevant because wherever possible, we reported the individual study results as calculated in RevMan.
In order to analyze cluster‐randomized trials appropriately in RevMan, we sought statistical guidance from the Cochrane HIV/AIDS Review Group and a number of external statistical experts. Before entering the results of cluster‐randomized studies into RevMan, we transformed outcome data according to the procedure in the Cochrane Handbook (Higgins 2005, supported in Adams 2004), dividing the number of events and number of participants by the design effect [1 + (1 ‐ m) * r]. We used the details provided by each study (total n and number of clusters) to calculate the average cluster size (m). After a sensitivity analysis, we decided upon consultation with the review group to report results using the intra‐class correlation coefficients (r) recommended in Johnson 2002. These were ICC=0.015 for school‐based studies and ICC=0.005 for community‐based studies (regardless of cluster size); these values were calculated respectively from school‐based studies of youth smoking behavior and community‐based studies of HIV prevention for men who have sex with men (Johnson 2002). Insufficient data were available for us to estimate a reliable ICC from the included studies.
Even with extensive statistical guidance, we acknowledge that the applicability of external values to this review is somewhat uncertain. For greater transparency, we report the results of cluster‐randomized trials analyzed both before and after controlling for clustering.
Dealing with missing data Missing data arose from two sources: participant attrition and missing statistics.
Attrition We preferred to accept studies with intention‐to‐treat analyses, which minimize attrition bias by imputing data for participants who drop out of the trial (Hollis 1999). However, we also accepted studies that used complete case analyses, but contacted authors for missing data. If a meta‐analysis had been possible, we would have conducted sensitivity analyses to investigate attrition as a source of heterogeneity and possible bias.
Missing statistics Where statistics were missing (eg numbers of participants per group, attrition rates, means and standard deviations, or percentages), we contacted primary study authors to supply the information. Where the information was unavailable due to data loss or non‐response, we reported the available results as stated in the trial report.
Assessment of heterogeneity If a meta‐analysis had been possible, we would have assessed heterogeneity using the chi square test of heterogeneity, visual inspection of the data, and the I2 statistic (Higgins 2002). The I2statistic determines the percentage of variability that is due to heterogeneity rather than sampling error, where a value greater than 50% suggests moderate heterogeneity. If any of these methods indicated heterogeneity, we would have investigated possible explanations, including clinical and methodological characteristics. Even when tests for heterogeneity were non‐significant, we planned to conduct subgroup analyses to explore other potential moderators.
Assessment of reporting biases If a meta‐analysis had been possible, we would have used funnel plots (plotting effect size against standard error) to detect potential bias. Additional analyses may have included the planned Egger regression approach with a weight‐function model. Asymmetry can be due to publication bias, but it can also arise from clinical and methodological heterogeneity. In the event that a relationship had been found, these sources of heterogeneity would also have been examined as possible explanations (Egger 1997).
Data synthesis If a meta‐analysis had been possible, we would have considered conducting analyses according to both fixed effects and random effects models. The random effects model would have been used where there was indication of heterogeneity and the source of such heterogeneity could not be explained. The random effects model would also have been used for analyses incorporating small numbers of studies, for which tests of heterogeneity may be underpowered. If there were no source of heterogeneity beyond differences in the observed covariates, we would have conduct both fixed effects and random effects analyses and investigated differences between the two procedures.
The narrative synthesis was conducted according to the following methods. First, we entered each individual study in RevMan. Secondly, we prepared the supplemental Charts of Effects appended to this review (see Appendix A). These charts are organized by outcome, and each chart shows the effects of individual studies according to RevMan analyses (where possible) or as reported in the primary study. The charts also integrate key methodological features of each study (eg control group, attrition), along with each study's definition of the outcome of interest (eg condom use was variously defined as condom use at last sex among sexually experienced participants, or condom use in the last month among sexually active participants). The charts were then explained in text format for the description of studies and results.
Sub‐group analyses If we had conducted a meta‐analysis, we would have stratified our analysis by intervention setting (eg school, clinic) and by participants' age, country, ethnicity, and socioeconomic status. Subgroup analyses would only have been conducted if data allowed, with the knowledge that using a number of subgroups can lead to statistically misleading conclusions.
Sensitivity analysis If we had conducted a meta‐analysis, we would have performed separate analyses for studies using complete case, per‐protocol, and intention‐to‐treat methods, with a sensitivity analysis to investigate disparities among the three groups.
Results
Description of studies
See Figure 1.
1.
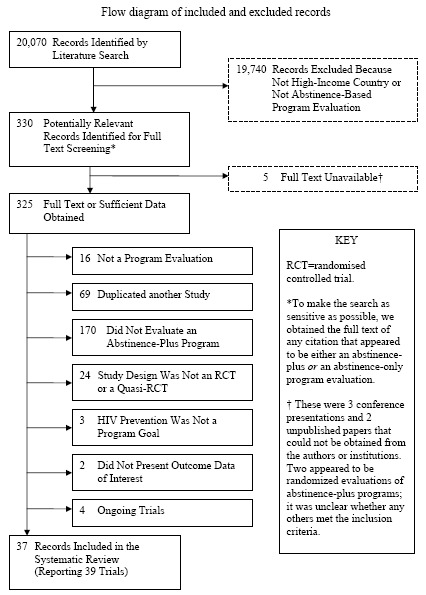
QUOROM Chart.
A total of 20070 citations were assessed for inclusion (of these, 19892 were recovered from electronic database searches ending February 2007, 99 were from hand‐searching, 17 were from personal contacts, and 62 were from cross‐referencing). After screening, 330 papers were deemed potentially relevant evaluation studies. Full text copies (or sufficient information) for 235 of these citations were obtained.
Of the 5 papers we could not obtain, 2 were conference abstracts of unclear relevance whose authors could not be located. One was an in‐press paper of unclear relevance that could not be obtained from the authors. Two appeared to be recently completed abstinence‐plus program trials, but reports were not available and could not be obtained from the trialists.
Of the 325 papers for which the full text (or sufficient study information) was obtained, 288 were excluded for the following reasons: 16 were not program evaluations, 69 duplicated another paper, 170 did not evaluate an abstinence‐plus intervention, 24 did not meet the criteria for study design, 3 evaluated abstinence‐plus interventions that did not list HIV prevention as a program goal, 2 did not present outcome data of interest, and 4 were ongoing or recently completed trials for which full reports were not yet available.
After these studies were excluded, analyses were limited to 37 separate papers (along with the papers that duplicated these reports), comprising 39 separate evaluations assessing the effects of abstinence‐plus programs. Two reports described 2 evaluations (Kennedy 2000a, Kennedy 2000b, McBride 2000a, McBride 2000b). Additionally, one trial (Philliber 2001) reported a 12‐site evaluation study but grouped the 12 sites for analysis, so this represents one evaluation.
Included Studies Detailed information about individual studies may be found in the Table of Included Studies.
Design Five of the included studies were quasi‐randomized controlled trials. Methods of allocation were reported in four studies, which used alternation (Danielson 1990), tossing a coin (Ferguson 1998), and assignment by even or odd birth date (McBride 2000a, McBride 2000b). We included these quasi‐randomized designs after determining that the randomization sequences, as described, were unlikely to lead to systematic bias between the treatment arms. Although baseline differences reached significance in two of these studies (Danielson 1990 and McBride 2000b), all four of these quasi‐randomized controlled trials controlled for baseline values in analyses.
The fifth quasi‐RCT (Moberg 1998) was a three‐arm trial, with arms receiving a one‐year intervention, a three‐year intervention, and usual care. This study used a stratified randomization sequence based on whether the included schools could feasibly deliver a one‐year or a three‐year program. Within each of those two categories, schools were then randomly assigned to deliver either the intervention or usual care. Specific procedures for random assignment within these categories were not reported.
The remaining 34 evaluations were randomized controlled trials, although method of randomization was rarely reported (see Methodological quality of included studies).
Twenty‐one trials randomized clusters of participants: units of randomization included schools (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Markham 2006, Moberg 1998, Wright 1997), classrooms (Kirby 1997, O'Donnell 2002), school districts (Weeks 1997), neighborhoods or communities (Dancy 2006, Ferguson 1998, Sikkema 2005, Wu 2003), community centers (DiIorio 2006, DiIorio 2007, Jemmott 2004), friendship groups (Stanton 1996), recruitment groups (Stanton 2006), and cohorts of 6‐10 participants (St Lawrence 1995b, St Lawrence 2002). The remaining 18 trials randomized individuals. Cluster‐randomization was commonly driven by the need to minimize potential contamination, along with the convenience of schools and other clustered units for program delivery.
Control groups for the evaluations varied as follows:
Controls in ten trials received usual care (Aarons 2000, Boekeloo 1999, Coyle 2004, Coyle 2006, Kirby 1997, Markham 2006, Moberg 1998, Philliber 2001, Weeks 1997, Wright 1997). Usual care consisted of the HIV/AIDS prevention services or sex education normally provided by the school system or community setting. These services may have included no treatment, abstinence‐only programs, safer‐sex interventions, condom promotion programs, or other abstinence‐plus programs, but very few details were provided to gauge what services usual care control groups actually received. This prevented a quantitative synthesis of trials with usual care controls.
Seven trials used a non‐intervention (no‐treatment) control group (Danella 2000, Danielson 1990, Hernandez 1990, Kennedy 2000a, Kennedy 2000b, McBride 2000a, McBride 2000b); in some cases the intervention was offered to the control group after completion of treatment.
Eleven trials used attention control groups, in which the control participants are exposed to the same types of program activities and exposure but with a different thematic focus (Dancy 2006, DiIorio 2007, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Jemmott 2004, St Lawrence 1999, Stanton 2000, Stanton 2006, Villarruel 2006). Four of these trials involved the same program developers (Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999). Attention control groups focused on concepts such as career planning and career opportunities (Jemmott 1992, Stanton 2000), general health (Dancy 2006, Hewitt 1998, Jemmott 1998, Jemmott 1999, Jemmott 2004, Villarruel 2006), anger management (St Lawrence 1999), and environmental education (Stanton 2006).
In four trials (Coyle 2001, DiIorio 2006, Sikkema 2005, Smith 1994), controls received an educational program, which we designated as an "information" control group. These interventions were generally brief and provided factual information about HIV and its transmission.
Fifteen trials compared several different versions of an abstinence‐plus intervention, sometimes in addition to a usual care, non‐intervention, attention control, or information control (Dancy 2006, DiIorio 2006, Ferguson 1998, Hewitt 1998, Jemmott 1998, Moberg 1998, O'Donnell 2002, Sikkema 2005, St Lawrence 1995a, St Lawrence 1995b, St Lawrence 2002, Stanton 1996, Stanton 2006, Weeks 1997, Wu 2003).
Hernandez 1990 was the only trial to compare identical formats of an abstinence‐plus program, an abstinence‐only program, and a safer‐sex program, along with a non‐intervention control. In a similar trial, Jemmott 1998 compared an abstinence‐plus program with a heavy emphasis on abstinence, an abstinence‐plus program with a heavy emphasis on condom skills, and an attention control focusing on general health.
Ten evaluations involved more than two treatment arms (Dancy 2006, DiIorio 2006, Hernandez 1990, Hewitt 1998, Jemmott 1998, Moberg 1998, Sikkema 2005, St Lawrence 2002, Weeks 1997, Wu 2003). Another evaluation evolved into a three‐arm design based on dosage when the host school system decided to expand the experimental program halfway through the evaluation; analyses were provided both by original assignment and by dosage received (0, 1, or 2 program years) (O'Donnell 2002).
Sample Size Together, the 39 studies enrolled approximately 37724 participants at baseline, with a median baseline enrolment of 535. Sample size at baseline ranged from 34 (St Lawrence 1995b) to 4512 (Wright 1997); one trial did not report the specific number enrolled at baseline, but this was approximated from the given attrition rates and number analyzed (Kirby 1997). Nine trials reported using a power calculation (DiIorio 2006, DiIorio 2007, Ferguson 1998, Jemmott 1998, Kennedy 2000a, Kennedy 2000b, Moberg 1998) or reported the statistical power attained by the sample size for each outcome at follow‐up (McBride 2000a, McBride 2000b); while it is likely that a majority of remaining trials used power calculations as well, these calculations were not reported.
After attrition at each study's longest follow‐up, the analyses reported in this review encompass approximately 25796 participants (with values imputed for trials using intention‐to‐treat analyses), for an overall attrition of 31.6%. This figure does not account for non‐response or under‐utilization of any specific outcome measure.
Setting Despite our international search for trials, all 39 studies took place in North America; 37 studies took place in the contiguous United States, 1 multi‐site study involved four Canadian provinces, and 1 trial took place in the Bahamas. US evaluation sites varied and are described in the Table of Included Studies; most trials were conducted in coastal areas. Of the trials that used multi‐site designs, all grouped participants from different sites together for analysis, and only Coyle 2001 reported group‐by‐location analyses. The majority of evaluations took place in urban settings; only one trial took place in an exclusively rural area (Stanton 2006).
The immediate program setting was usually a school or community center (32 trials). Other programs took place at health centers (Danielson 1990, St Lawrence 1995a), doctors' offices (Boekeloo 1999), a residential drug treatment center (St Lawrence 1995b, St Lawrence 2002), a juvenile reformatory (St Lawrence 1999), and family homes (Stanton 1996, Wu 2003).
Participants All participants were adolescents or young adults. Mean ages in individual trials ranged from 11.5 years (Coyle 2004) to 19.25 years (Hernandez 1990); the median of these mean ages was approximately 14.4 years. The majority of programs targeted pre‐secondary‐school youth; it has been suggested that programs promoting sexual abstinence may be more effective before participants make their sexual debut (DiClemente 1998). Specific data on participant inclusion criteria and target ages are provided in the Table of Included Studies.
Twenty‐nine trials enrolled primarily minority participants (Aarons 2000, Boekeloo 1999, Coyle 2001, Coyle 2004, Coyle 2006, Dancy 2006, DiIorio 2006, Ferguson 1998, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000b, Kennedy 2000a, Kirby 1997, Markham 2006, O'Donnell 2002, Philliber 2001, Sikkema 2005, Smith 1994, St Lawrence 1995a, St Lawrence 1999, Stanton 1996, Villarruel 2006, Weeks 1997, Wu 2003, Jemmott 2004, DiIorio 2007, Stanton 2000), of which 12 enrolled samples that were 97‐100% African‐American (Dancy 2006, DiIorio 2006, Ferguson 1998, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, St Lawrence 1995a, Stanton 1996, Wu 2003, DiIorio 2007, Stanton 2000). An additional study was conducted among participants of Bahamian ethnicity (Danella 2000). Twenty trials reported any information about participants' socioeconomic status (Aarons 2000, Coyle 2001, Coyle 2004, DiIorio 2006, DiIorio 2007, Ferguson 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Markham 2006, O'Donnell 2002, Philliber 2001, Sikkema 2005, Smith 1994, St Lawrence 1995a, Stanton 1996, Wu 2003, Dancy 2006, Stanton 2000, Weeks 1997), of which 18 indicated that participants were of lower SES than the general population (Aarons 2000, DiIorio 2006, DiIorio 2007, Ferguson 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Markham 2006, O'Donnell 2002, Philliber 2001, Sikkema 2005, Smith 1994, St Lawrence 1995a, Stanton 1996, Wu 2003, Dancy 2006, Stanton 2000, Weeks 1997). Indicators of SES included uptake of free/reduced lunch plans, neighborhood, receipt of Medicaid or public assistance, mothers' education, and living in a home with a working adult.
Thirty trials included both male and female participants. Four studies enrolled males only (Danielson 1990, DiIorio 2007, Jemmott 1992, St Lawrence 1999), and five studies enrolled females only (Dancy 2006, Danella 2000, Ferguson 1998, McBride 2000a, McBride 2000b).
Since participants in most studies were younger than the legal age of consent, parental consent procedures were relevant ethical concerns. Hernandez 1990 was limited to participants over the age of 18 and so did not require parental consent. Twenty‐eight studies required active parental consent for participation in the intervention and participation in data collection. Two studies required active parental consent, but only for participants under the age of 14 years (McBride 2000a, McBride 2000b). In three studies, the experimental interventions were delivered as part of a school curriculum; however, these three studies required active parental consent for participation in data collection procedures (Coyle 2004, Kirby 1997, and Moberg 1998). One study used passive consent procedures for participation in both the intervention and in data collection (Weeks 1997). Two evaluations were part of a 5‐evaluation design (Kennedy 2000a, Kennedy 2000b); the report for all five sites stated that parental consent was waived for two sites where the experimental program targeted sexually active youth. However, four of the five sites met this criterion, so it was unclear which two had waived the parental consent procedures. Type of consent was not determined for two trials (Jemmott 2004, Markham 2006).
Twenty‐two of the 39 included studies offered an incentive of some kind for participation in either the experimental program or the data collection process. The experimental programs in 11 evaluations were delivered as part of a school curriculum or as a means of earning course credit, creating an academic motivation for participation (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Hernandez 1990, Kirby 1997, Markham 2006, Moberg 1998, O'Donnell 2002, Weeks 1997, Wright 1997). At least 19 trials offered participants some type of material incentive (Danielson 1990, DiIorio 2007, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000a, Kennedy 2000b, McBride 2000a, McBride 2000b, Philliber 2001, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, Sikkema 2005, Stanton 1996, Stanton 2000, Villarruel 2006, Weeks 1997). Incentives included coupons, pizza parties, cash or gift certificates, and non‐monetary gifts. The experimental interventions frequently included end‐of‐program celebrations.
Interventions A number of similarities unified the 39 experimental interventions. Most importantly, every intervention promoted both sexual abstinence and condom or contraception use, and every intervention conveyed the message that abstinence is the best preventive choice. The use of this prevention hierarchy allows the grouping of these 39 programs in a systematic review. All but one of the programs (Hernandez 1990) targeted teenagers or adolescents. Every intervention conveyed information about HIV, STIs, the risks of sex, and different strategies for HIV prevention.
Within this rubric, however, there was a wide range of program designs. Reporting about intervention design and implementation was often limited, particularly for reporting on implementation fidelity. It was often extremely difficult to discern what proportion of the program was spent discussing and encouraging abstinence as opposed to condom use or other methods of risk reduction, which is a source of error for this review.
Notably, fifteen programs emphasized pregnancy prevention as much or more than HIV prevention (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Danielson 1990, DiIorio 2006, Ferguson 1998, Kirby 1997, Markham 2006, McBride 2000b, McBride 2000a, Moberg 1998, O'Donnell 2002, Philliber 2001, Smith 1994); the remaining programs exclusively targeted HIV prevention. Studies that were limited to pregnancy prevention were excluded because interventions focused only on pregnancy may exclusively emphasize the consequences of penile‐vaginal sex, while neglecting the risks of oral intercourse, anal intercourse, or same‐sex sexual activity.
Not all of the abstinence‐plus interventions maintained an exclusive topical focus on sexual risk behaviors. Several programs included activities such as scheduled community service (Coyle 2006, DiIorio 2006, O'Donnell 2002); tutoring, job assistance, college application assistance, healthcare and mentoring (Philliber 2001); education‐related field trips (DiIorio 2006); general nutrition and substance abuse (Moberg 1998); a 6‐week career mentorship placement (Smith 1994); and parental monitoring (Dancy 2006, DiIorio 2007, Stanton 2000, Wu 2003). However, sexual risk reduction via abstinence and condom use remained primary goals for all of these programs.
The delivering organizations were schools for 10 programs (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Hernandez 1990, Kirby 1997, Markham 2006, Moberg 1998, Weeks 1997, Wright 1997), community facilities for 24 programs (Dancy 2006, Danella 2000, DiIorio 2006, Ferguson 1998, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000b, Kennedy 2000a, McBride 2000b, McBride 2000a, Philliber 2001, Sikkema 2005, Smith 1994, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, St Lawrence 1995b, Stanton 1996, Villarruel 2006, Wu 2003, Jemmott 2004, DiIorio 2007), schools and community facilities for 2 programs (O'Donnell 2002, Stanton 2006), healthcare personnel for 2 programs (Boekeloo 1999, Danielson 1990), and staff visiting family homes in one program (Stanton 2000). Twelve programs were delivered in large groups or classroom format (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Ferguson 1998, Hernandez 1990, Kirby 1997, Markham 2006, Moberg 1998, O'Donnell 2002, Weeks 1997, Wright 1997), 24 were delivered in small groups (Dancy 2006, Danella 2000, DiIorio 2006, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000b, Kennedy 2000a, McBride 2000b, McBride 2000a, Philliber 2001, Sikkema 2005, Smith 1994, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, St Lawrence 1995b, Stanton 2006, Stanton 1996, Villarruel 2006, Wu 2003, Jemmott 2004, DiIorio 2007), two involved one‐on‐one delivery (Boekeloo 1999, Danielson 1990), and one was delivered to parent‐child dyads (Stanton 2000).
Program facilitators were adults only in 29 programs (Boekeloo 1999, Coyle 2004, Coyle 2006, Dancy 2006, Danella 2000, Danielson 1990, DiIorio 2006, Hewitt 1998, Jemmott 1992, Jemmott 1999, Kennedy 2000b, Markham 2006, McBride 2000b, McBride 2000a, Moberg 1998, O'Donnell 2002, Philliber 2001, Smith 1994, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, St Lawrence 1995b, Stanton 2006, Stanton 1996, Villarruel 2006, Weeks 1997, Wu 2003, Jemmott 2004, DiIorio 2007, Stanton 2000), both adults and peers in 6 programs (Aarons 2000, Coyle 2001, Ferguson 1998, Jemmott 1998, Sikkema 2005, Wright 1997), and peers only in 2 programs (Kennedy 2000a, Kirby 1997); two interventions were media‐based and facilitated by adults (Hernandez 1990, Stanton 2000). One evaluation randomized groups of intervention participants to receive the program from either peer leaders or adult leaders (Jemmott 1998). An additional evaluation tested "matching" hypotheses to determine the moderating effects of facilitator gender, facilitator ethnicity, and gender composition of the program delivery group among African‐American participants (Jemmott 1999).
Sixteen programs attempted to involve participants' parents to any degree (Boekeloo 1999, Coyle 2001, Dancy 2006, DiIorio 2006, Markham 2006, Moberg 1998, O'Donnell 2002, Philliber 2001, Sikkema 2005, Stanton 2006, Stanton 1996, Weeks 1997, Wright 1997, Wu 2003, DiIorio 2007, Stanton 2000). Strategies to encourage parental involvement included brochures and mailings, parent‐child homework assignments, curriculum advisory groups, parent meetings or orientations, and community advisory groups.
Program exposure ranged from a single half‐hour session with a physician (Boekeloo 1999) to an after‐school program that served youth for three hours each school day, 50 weeks per year for three years (approximately 2250 service hours, Philliber 2001). The median program exposure was 10.5 hours across trials. Nine trials evaluated single‐session programs (Boekeloo 1999, Danielson 1990, Hernandez 1990, Hewitt 1998, Jemmott 1992, Jemmott 1999, Kennedy 2000a, Kennedy 2000b, Stanton 2000); the remaining trials evaluated programs with multiple sessions.
All but five evaluations reported a theoretical basis for the intervention (with the exception of Danielson 1990, Ferguson 1998, Hernandez 1990, O'Donnell 2002, and Smith 1994). Theoretical bases included social cognitive theory, the theory of reasoned action, the theory of planned behavior, social influences theory, the information‐motivation‐behavioral skills model, and the health belief model.
Several programs are represented in multiple evaluations: eight studies evaluated variations of the Be Proud! Be Responsible! program (Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000b, Kennedy 2000a, Villarruel 2006, Jemmott 2004), four studies evaluated variations of Becoming a Responsible Teen (St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, St Lawrence 1995b), four studies evaluated variations of the Focus on Kids curriculum (Stanton 2006, Stanton 1996, Wu 2003, Danella 2000), and two studies evaluated the ImPACT parental monitoring intervention (Stanton 2000, Wu 2003).
Outcomes All outcomes were self‐reported, with the exception of one evaluation that was able in some cases to use medical records and staff reports to verify self‐reported pregnancy in the intervention group (Philliber 2001), and another evaluation that was able to use program records to assess the receipt of treatment for STIs (St Lawrence 1995b). The latter trial also attempted to medically evaluate STI incidence, but data were discarded due to specimen mishandling.
All outcomes were self‐reported. Eight studies used computers or audio computer assisted self interviewing (ACASI) technology to gather data (Dancy 2006, DiIorio 2007, Markham 2006, Sikkema 2005, Stanton 2006, Stanton 1996, Stanton 2000, Wu 2003). Recent investigations (with exceptions (Zellner 2005) have suggested that ACASI technology may minimize self‐report bias among adolescents (Gribble 1999, Romer 1997, Turner 1998), but there were too few ACASI studies in this review to observe systematic differences in results by data collection method.
The remaining trials assessed outcomes using written surveys or did not specify the exact method of data collection; one study collected outcome data by phone (Boekeloo 1999). Questionnaires were administered in both English and Spanish in at least six trials (Aarons 2000, Boekeloo 1999, Coyle 2004, Coyle 2006, Kirby 1997, Villarruel 2006), and in both English and French in another study (Wright 1997). Seven studies reported mailing questionnaires to participants who could not complete the surveys in the project setting (Coyle 2001, Coyle 2004, Coyle 2006, Danielson 1990, Kirby 1997, Moberg 1998, Weeks 1997), and four studies conducted make‐up surveys for participants who did not attend scheduled follow‐ups (Jemmott 1999, McBride 2000a, McBride 2000b, O'Donnell 2002).
Two studies described resistance from schools or parents to sexual behavior questions on the survey (Coyle 2004, Moberg 1998). Additionally, McBride 2000a and McBride 2000b were part of a six‐study evaluation, but three study sites geared towards participants younger than 14 years did not include behavioral questions in the survey (the remaining site did not evaluate an abstinence‐based program).
Twenty trials reported piloting the questionnaires with populations that approximated the study sample, either in the published trial report in or a supplemental paper (Aarons 2000, Boekeloo 1999, Coyle 2001, Coyle 2004, Coyle 2006, Danella 2000, Ferguson 1998, Hernandez 1990, Jemmott 1998, Jemmott 1999, Kennedy 2000a, Kennedy 2000b, Smith 1994, St Lawrence 1995a, St Lawrence 2002, Stanton 1996, Stanton 2000, Stanton 2006, Villarruel 2006, Wright 1997). An additional eleven studies reported using survey instruments that had been previously used or piloted elsewhere (Dancy 2006, Danielson 1990, DiIorio 2006, DiIorio 2007, Hewitt 1998, Jemmott 1992, Jemmott 2004, Sikkema 2005, St Lawrence 1995b, St Lawrence 1999, Wu 2003).
Twenty‐seven of the trial reports included a description of techniques used to improve the completeness and validity of self‐reported data. These included using ACASI technology to gather data (Dancy 2006, DiIorio 2007, Markham 2006, Sikkema 2005, Stanton 2006, Stanton 1996, Stanton 2000, Wu 2003); using anonymous questionnaires (Aarons 2000, Boekeloo 1999, Coyle 2001); identifying participants by code numbers or code names (Danielson 1990, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000a, Kennedy 2000b, Kirby 1997, St Lawrence 1995a, St Lawrence 1995b, St Lawrence 2002, Wright 1997); stressing the confidential nature of the survey during survey administration (Dancy 2006, Danielson 1990, Hernandez 1990, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000a, Kennedy 2000b, Moberg 1998, St Lawrence 2002, Stanton 2006, Wright 1997); physically separating participants from one another or from their parents during the survey (DiIorio 2006, Hernandez 1990, Hewitt 1998, Moberg 1998, Wright 1997, St Lawrence 1999, Stanton 2000); using survey administrators to offer reading assistance or read the survey aloud (Moberg 1998, St Lawrence 1999, St Lawrence 2002, Stanton 2006); using survey monitors who had not been involved in program delivery (Hewitt 1998, Villarruel 2006); asking participants to sign honesty agreements or honesty pledges (Dancy 2006, Jemmott 1998, Jemmott 1999); appealing to participants to answer honestly because the evaluation could be used to help similar young people (Hewitt 1998, Jemmott 1998, Jemmott 1999); and giving participants calendars to facilitate the recall of sexual behaviors (Jemmott 1998).
The primary trials reported outcome data in a range of formats; common formats included odds ratios with 95% confidence intervals, test statistics for ANCOVAs or ANOVAs, group means or percentages with p‐values from significance tests, and transformed group means with a statement of significance. Commonly missing data, which prevented the entry of many studies into RevMan, included numbers of participants per trial arm at follow‐up and standard deviations for group means.
We classified follow‐up assessments as short‐term (less than 6 months after baseline), medium‐term (from 6 up to 12 months), and long‐term (12 months or longer). Twenty‐two studies provided long‐term follow‐up data (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Danella 2000, Danielson 1990, DiIorio 2006, DiIorio 2007, Jemmott 1998, Jemmott 2004, Kirby 1997, Moberg 1998, O'Donnell 2002, Philliber 2001, Sikkema 2005, St Lawrence 1995a, St Lawrence 2002, Stanton 1996, Villarruel 2006, Weeks 1997, Wright 1997, Wu 2003), and the median final assessment time across studies was 12 months after baseline. We included short‐term outcome data for one ongoing study (Markham 2006); after the trial ends, long‐term results will be included in a review update. Because program duration ranged from one session to three years, follow‐up assessments took place at a wide variety of times after the end of the interventions. There were also differences across trials in the recall periods over which sexual behaviors were assessed (e.g., over the last three months, over the last year, ever). This variability also contributed to our decision to avoid a quantitative synthesis. Twenty trials provided sufficient data for partial or complete re‐analysis in RevMan (Boekeloo 1999, Dancy 2006, DiIorio 2006, Ferguson 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kirby 1997, McBride 2000b, McBride 2000a, Moberg 1998, Philliber 2001, Sikkema 2005, Smith 1994, St Lawrence 1995b, Stanton 2006, Stanton 1996, Villarruel 2006, Weeks 1997, Wu 2003).
Recall periods for follow‐up data varied, but participants were commonly asked to recall their behaviors over the past 1‐3 months. Outcomes such as pregnancy, STI incidence, number of partners, and "ever had sex" were evaluated over participants' lifetimes, while behaviors such as condom use, abstinence, and unprotected sex were assessed in the short‐term. Condom use outcome data were often collected for participants' last vaginal sex, even if this occurred before enrolment in the study.
The outcomes of greatest relevance to HIV risk (i.e., HIV infection, STI infection, and unprotected sexual behaviors) were under‐utilized, as indicated in Tables 3 and 4. No study assessed HIV incidence, and no study medically evaluated sexually transmitted infections (STI) or pregnancy. Seven trials assessed self‐reported STI or pregnancy incidence (Boekeloo 1999, Coyle 2006, Ferguson 1998, Kirby 1997, O'Donnell 2002, Philliber 2001, Wu 2003), which are vulnerable to floor effects (i.e., incidence levels are so low that studies may be underpowered to find significant differences between groups) and underreporting due to unknown status.
Every trial reported at least one behavioral outcome, and 24 studies assessed HIV‐related knowledge. The most commonly reported behavioral outcomes included frequency of unprotected vaginal sex (12 trials), incidence of sex (21 trials), frequency of recent sex (13 trials), number of sex partners (13 trials), condom use (26 trials), and sexual initiation (19 trials).
Nine trials assessed oral or anal sex acts (Boekeloo 1999, Jemmott 1992, Dancy 2006, Jemmott 1999, Markham 2006, St Lawrence 1995a, St Lawrence 1999, Wright 1997, Wu 2003), but three only reported these in summary measures of oral, anal, and vaginal intercourse (Boekeloo 1999, Markham 2006, Dancy 2006). In other trials, data on oral or anal sex were not assessed or could not be disaggregated from reports of "sex" or "intercourse." Only three trials reported specific definitions of "sex" (e.g., "a boy's penis in your vagina / your penis in a girl's vagina" (Hewitt 1998)), all of which signified vaginal intercourse (Hewitt 1998, Coyle 2004, Villarruel 2006); the remaining trial reports did not specify operationalized definitions. Given this trend, we classified results for nonspecific definitions of "sex" as vaginal sex. No trial reported same‐sex sexual behavior outcomes.
Five trials used risk behavior indices (Jemmott 1992, Jemmott 1999, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002); these were based on slightly different outcomes, as specified in Appendix A.
Excluded Studies Excluded studies consist of all evaluations produced by the search that evaluated abstinence‐plus programs using non‐randomized controlled, quantitative designs among any population group in high‐income countries. Cross‐sectional studies and comparisons of program participants against national survey samples were included. These abstinence‐plus programs could focus on preventing pregnancy or preventing HIV, and the studies could report any outcomes. Details of the excluded studies, including results for behavioral and biological outcomes only, are provided in the Table of Excluded Studies. The results mentioned in this table are those reported by the trialists, with no further analysis by the reviewers.
Ongoing Studies See the Table of Ongoing Studies. These studies were in progress or unavailable at the time of our search.
Risk of bias in included studies
Allocation Specific procedures for generating the allocation sequence were rarely reported. Four of the five quasi‐randomized controlled studies described the method of random allocation used: these included alternation (Danielson 1990), a coin flip (Ferguson 1998), and assignment by even or odd birth date (McBride 2000a, McBride 2000b). Of the 34 randomized controlled studies, only ten described how the allocation sequence was generated: procedures included computer‐generated randomization sequences (DiIorio 2006, Jemmott 1998, Jemmott 1999, Villarruel 2006), random numbers tables (Danella 2000, Markham 2006, Stanton 1996, Stanton 2000, Wu 2003), and having participants draw sealed envelopes from a bag, although procedures for preparing the envelopes and monitoring the envelope‐drawing were not described (Philliber 2001).
Similarly, procedures for concealing the allocation of intervention assignment were very rarely reported. Allocation concealment was not used in the four quasi‐randomized controlled trials described above (Danielson 1990, Ferguson 1998, McBride 2000a, McBride 2000b), so these studies received the "D" designation for allocation concealment. The lack of concealment may make these four studies especially prone to bias, but it did not appear that the direction of bias was consistent. Of the four studies, one found no significant effects (McBride 2000b), two found a protective effect on one of two outcomes (Danielson 1990, McBride 2000a), and one found two protective effects out of four outcomes (Ferguson 1998).
Of the 34 randomized controlled studies, only two reported strategies for concealing the allocation sequence from trialists and those recruiting participants into the study (Jemmott 1998, Stanton 2000). These were the only trials that received the "A" designation for allocation concealment, indicating that procedures were adequate. The remaining trials received the "B" or "D" designation, which indicated that allocation concealment was unclear. The trial that used sealed envelopes for random assignment (Philliber 2001) was also given the B designation because it was unclear how envelopes were prepared and offered to the participants.
The inadequate reporting of methods for generating and concealing the allocation sequence is a severe limitation of this data set. While procedures may have been adequate in every trial, unclear reporting leaves us uncertain whether trial results are vulnerable to selection bias.
Inadequate and clustered randomization sequences can heighten the potential for baseline differences. Of the 39 trials, 19 reported at least one significant group difference at baseline (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Danielson 1990, DiIorio 2006, DiIorio 2007, Jemmott 1998, Kennedy 2000a, Kennedy 2000b, Markham 2006, McBride 2000a, Moberg 1998, Philliber 2001, Smith 1994, St Lawrence 1995b, Stanton 2006, Weeks 1997, Wright 1997). Every one of these trials controlled for baseline differences in analyses.
Seven trials did not provide a clear statement of baseline equivalence (Danella 2000, Ferguson 1998, Hewitt 1998, Jemmott 1992, Jemmott 1999, Jemmott 2004, Stanton 1996); however, five of these used analytical procedures that would have controlled for baseline values (Ferguson 1998, Hewitt 1998, Jemmott 1992, Jemmott 1999, Jemmott 2004).
The remaining trials reported baseline equivalence for all measures assessed. Notably, one trial used a significance level of P<0.01 for these calculations (Kirby 1997), and another reported baseline equivalence only for sexual behaviors (O'Donnell 2002).
Deviations from random assignment were explicitly acknowledged in three studies: O'Donnell 2002, McBride 2000b, and Stanton 1996. In O'Donnell 2002, which evaluated a 2‐year program, administrators at the school sponsoring the intervention were "enthusiastic" about the program. In the program's second year, the school chose to devote additional resources to expand the program; simultaneously, scheduling concerns caused a smaller number of participants to leave the program and join the control group. As a consequence, 26% of the analyzed sample changed conditions midway through the trial, of which 69% moved from the control to the intervention group. Analyses were performed both by original assignment and according to dosage (similar to a treatment‐on‐the‐treated analysis). According to McBride 2000b, program dosage for the intervention group ranged from 0‐63 hours with a mean of 22 hours, while dosage for the control group ranged from 0‐29 hours with a mean of 0 hours. It is unclear who received the 29 hours of exposure in the control group, and an explanation was not offered in the published trial. It was also unclear how these data were used in analyses, although it appears that participants were analyzed in their originally assigned groups. In Stanton 1996, a supplementary report suggested that some control participants may have been exposed to at least some activities in the experimental program.
Blinding Given the nature of the interventions, as well as the time commitment involved, no participants were blind to their treatment arm assignment. The staff who delivered the interventions were also not blind to participants' assignments. An exception occurred in one trial that took place in a managed care setting (Boekeloo 1999): while the physicians who delivered the interventions did know who was in the treatment group, they were not told which of their other patients had been enrolled in the control group. Otherwise, the impossibility of blinding participants and intervention staff may have led to performance bias.
Contamination and threats to program differentiation may have arisen from two sources: when the same staff administered treatment of some kind to both the intervention and the control group (although it was often unclear whether this had happened), and when participants knew one another outside the context of the trial. The effect of these sources of error, however, may be more likely to bias findings in the direction of no effect than in the direction of significance.
The first source of contamination was clearly possible in at least four trials (Boekeloo 1999, Stanton 2000, St Lawrence 1995b, Wu 2003). However, in one of these trials (Boekeloo 1999), exit interviews showed that 11 of 13 intervention topics were discussed significantly more often in the intervention than in the control group. In two of the other trials (Stanton 2000, Wu 2003), the intervention was primarily media‐based and may therefore be less vulnerable to performance bias.
It was unclear whether facilitators for the experimental intervention and educational control program were the same in 11 other studies (Coyle 2001, DiIorio 2006, DiIorio 2007, Hernandez 1990, Philliber 2001, St Lawrence 1995a, St Lawrence 2002, Sikkema 2005, Stanton 1996, Stanton 2006, Weeks 1997). A few other studies may be vulnerable to contamination by personnel not directly involved in treating the control groups: In Ferguson 1998, which evaluated a peer counseling intervention, the peer leaders were instructed not to give counseling to members of the control group, although they may have lived close by; the potential for contamination may have been strong in this study. In Kirby 1997, the program was delivered in intervention classrooms by non‐school personnel; however, some teachers taught classrooms in both treatment arm and may have conveyed some of the relevant information to their control classes. In Moberg 1998, which had two active treatment arms, the same intervention facilitator helped to administer the program to schools in both active conditions. In O'Donnell 2002, staff for participants' service learning placements did not come in contact with the control participants; however, the same teachers may have had both control and intervention classrooms, and may have discussed community service with control classrooms as well. In Philliber 2001, control students often received tutoring or other services at the community centers that delivered the experimental intervention, potentially giving the staff a chance to deliver prevention messages as well.
The second source of contamination was more likely to be present in trials that randomized participants by individual or classroom, rather than by entire community center, school, or school district. The use of self‐referrals and word‐of‐mouth as recruitment in Kennedy 2000a and Kennedy 2000b suggested that participants knew one another outside the trial; given recruitment settings, participant sharing of information may have been likely in at least 15 other trials (Ferguson 1998, Hernandez 1990, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Philliber 2001, McBride 2000a, McBride 2000b, Smith 1994, St Lawrence 1999, Stanton 1996, Stanton 2000, Stanton 2006, Wu 2003).
The blinding of assessors and data collectors was not entirely crucial for this group of studies, because almost every study utilized written self‐reported questionnaires or ACASI technology for data collection. According to trial reports, assessors were blind to participants' assignments in four trials (Boekeloo 1999, Danielson 1990, Jemmott 1998, Jemmott 1999), along with the eight trials that used ACASI technology (Dancy 2006, DiIorio 2007, Markham 2006, Sikkema 2005, Stanton 2006, Stanton 1996, Stanton 2000, Wu 2003). St Lawrence 1995a, St Lawrence 1995b, and St Lawrence 2002 used roleplay assessments to evaluate participants' social skills, peer education skills, and/or anger management; those assessing the roleplays were blind to participants' assignment, but it was unclear whether staff who administered the written behavioral questionnaire to the participants were blind as well.
Follow‐up and exclusions Attrition rates at final follow‐up ranged from 0% (St Lawrence 1995b) to 55% (Weeks 1997), with a median rate of 20% of baseline enrolment. One study report indicated an attrition rate that did not appear to correspond to the number given for baseline enrolment (Danielson 1990); we calculated a more conservative rate using the figures given for number analyzed and number enrolled at baseline. Eight trials observed overall attrition rates that exceeded 33% at final follow‐up (Coyle 2004, Coyle 2006, Jemmott 2004, Kennedy 2000a, Kennedy 2000b, Sikkema 2005, Weeks 1997, Wright 1997); high attrition must be considered as a potential threat to internal and external validity.
Most of the trials with attrition exceeding 0% commented on the distribution of participant dropout. In 15 trials, attrition rates differed by at least one participant characteristic (Coyle 2001, Coyle 2004, Danielson 1990, Jemmott 1998, Jemmott 1999, Kennedy 2000a, McBride 2000a, McBride 2000b, O'Donnell 2002, Philliber 2001, Sikkema 2005, Villarruel 2006, Weeks 1997, Wright 1997, Wu 2003); in eleven of these studies, participants who left the trials reported riskier behaviors or more risk factors at baseline than those who were retained (Coyle 2001, Danielson 1990, Jemmott 1999, Kennedy 2000a, McBride 2000a, McBride 2000b, Philliber 2001, Sikkema 2005, Weeks 1997, Wright 1997, Wu 2003). Differential attrition between treatment arms was observed in six trials (Dancy 2006, Kennedy 2000b, Markham 2006, Moberg 1998, Stanton 2006, Weeks 1997), and attrition led to non‐equivalence at follow‐up for another study (Philliber 2001). A common source of attrition‐related uncertainty was the lack of specific data regarding numbers of participants with program non‐attendance only, survey non‐completion only, and both program non‐attendance and survey non‐completion.
Thirty‐four trials analyzed participants according to complete‐case procedures; that is, trials analyzed participants in the groups to which they had been originally allocated, but did not impute values for dropouts. This type of analysis may overestimate the possibility of observing a significantly protective effect, since in many studies dropouts had reported higher risk behaviors at baseline. Complete case analyses also do not account for differential rates of attrition between the intervention and control groups.
Of the remaining five trials, three analyzed participants according to intention‐to‐treat procedures: St Lawrence 1995b had no attrition, Weeks 1997 imputed values using random‐effects regression analyses, and Coyle 2004 imputed data for dropouts using a rich‐imputation model based on baseline peer norms, group, time, ethnicity, and group‐by‐time interaction. Analysis type could not be determined for one trial (Jemmott 2004). Finally, O'Donnell 2002 conducted several sets of analyses according to different principles, prompted by a large proportion of treatment arm crossovers in the second year of the trial. One set of analyses was conducted according to original assignment but without imputing data for dropouts; another was conducted according to treatment‐on‐the‐treated (TOT) principles (by number of years of program exposure) without imputing data for dropouts; and a third set was conducted according to TOT principles but with imputed data for dropouts based on the last value carried forward. However, at no time were results reported according to original assignment and accounting for dropouts, which would have qualified as intention‐to‐treat.
Selective reporting As described in the "Outcomes" section above, the included studies reported a range of outcomes, using different recall periods and aggregating outcomes such as vaginal, oral, and anal sex acts in different ways. This variability, which we also observed in our review of abstinence‐only programs for HIV prevention, suggests that no standard set of outcomes exists to evaluate behavioral HIV prevention interventions for this population. This lack of consensus hindered our ability to perform a meta‐analysis.
As stated above, a recurring source of ambiguity and selective reporting was the use of non‐specific outcome measures, such as "sexual intercourse," "sex," or "virginity," without clear definitions. Previous research suggests that these terms may be difficult to understand, and they have many different definitions among adolescents, adults, medical practitioners, program coordinators, and the general public (Haglund 2002, Horan 1998, Pitts 2001, Remez 2000, Sanders 1999, Sonfield 2001). In fact, only three trial reports reported defining "sex" for the purposes of the questionnaire (Coyle 2004, Hewitt 1998, Villarruel 2006); all three referred to vaginal sex. The remaining trials defined measures variously as "intercourse," "sexual intercourse," "vaginal, anal, and oral sexual activity," "sexual relations," "coitus," "casual sex," "anal intercourse," "had sex," "instances of completed sexual activity," "vaginal, anal, and oral intercourse," "virginity," "sex partners," and "partners." Given the ambiguity and range of meanings of these terms, more specific and operationalized definitions may be necessary to gauge HIV‐related risk.
A number of results were reported only among the subgroups of students who were sexually active, or who reported having ever had sex. These most commonly included condom use, number of partners, and frequency of vaginal sex. Conversely, sexual initiation (ie sexual debut) was often assessed only among participants who reported never having had vaginal sex at baseline. Outcome‐specific findings appear in Appendix A.
A few studies that enrolled both males and females reported at least one outcome separately by gender without providing overall summaries of effect (Aarons 2000, Coyle 2004, O'Donnell 2002). One trial (Aarons 2000) assessed condom use among males only.
As discussed in the "Outcomes" section, the trial results were reported in a variety of formats, many of which were unsuitable for meta‐analysis in RevMan due to missing data. Commonly missing data included numbers of participants per trial arm, percentages for dichotomous outcomes, and group means and standard deviations for continuous outcomes. We contacted investigators on multiple occasions to secure missing data; while many authors were helpful in providing additional information, statistical data were often unavailable due to data loss or non‐response.
Another limitation of this data set is the lack of statistical controls for cluster‐randomized data. When studies do not control for the clustered nature of data, they risk receiving disproportionate weight in a meta‐analysis; the analysis of clustered data on an individual level is also linked to Type I error ‐ that is, finding significant results when none exist. Of the 21 studies that randomized participants in clusters, 14 had statistical procedures in place to control for clustering in analyses (Coyle 2001, Coyle 2004, Coyle 2006, Dancy 2006, DiIorio 2006, DiIorio 2007, Jemmott 2004, Kirby 1997, Markham 2006, Moberg 1998, O'Donnell 2002, Sikkema 2005, St Lawrence 2002, Wu 2003). These included using confirmatory multilevel analyses, entering a fixed nested effect term into analyses, and running regression analyses that controlled for clustering. The remaining 7 cluster‐randomized studies (Aarons 2000, Ferguson 1998, St Lawrence 1995b, Stanton 1996, Stanton 2006, Weeks 1997, and Wright 1997) did not report statistical methods for dealing with clustered data, suggesting that they analyzed participants on an individual level.
When a number of different outcomes are analyzed, it is also appropriate to statistically control for the use of multiple statistical tests, thereby again minimizing the chance of Type I error. Only three of the 39 included studies used any kind of correction: St Lawrence 1995a and St Lawrence 1999 used a Bonferroni correction when considering the significance of statistical tests, and Weeks 1997 incorporated a Tukey adjustment into statistical analyses.
Finally, selective reporting also occurred in trials that did not report significance or sufficient data to calculate the significance of key results; this occurred in O'Donnell 2002 for pregnancy and all comparisons between the 2‐year and 1‐year program exposure conditions (group means were provided without significance tests or numbers of participants per trial arm); Hernandez 1990 for pairwise comparisons among the four trial arms; Weeks 1997 for HIV knowledge (analyses combined the two active treatment arms for comparison against the control group, but did not provide sufficient data to calculate pairwise comparisons at any time point); and St Lawrence 1995a for a number of post‐hoc comparisons at specific time points.
Other potential sources of bias Limitations of self‐report and behavioral outcome data The reliance on self‐reported data is an inevitable source of bias for studies evaluating sexual behavior. The limitations of self‐report for sexual behavior have been analyzed elsewhere with respect to adolescents (Alexander 1993, Binson 1998, Brener 2004, Catania 1996, Lauritsen 1997, Meston 1998, Newcomer 1988, Rosenbaum 2006, Zabin 1984). Self‐report biases may be heightened in evaluations of abstinence‐plus programs due to the programs' emphasis on abstinence. Recent survey data suggest that youth who take virginity pledges may be more likely to retract their sexual histories at a later date (Rosenbaum 2006); although virginity pledges are abstinence‐only, not abstinence‐plus interventions, any program that privileges abstinence may have a similar effect on self‐report. Furthermore, sexual behavior may not always correspond directly to HIV/STI risk (O'Leary 1997, Peterman 2000). The most robust data for abstinence‐plus program evaluations would be medical evaluations of HIV or STI incidence; however, due perhaps to the young age of the participants, resource limitations, or logistical complications, no study was able to evaluate outcomes in this way.
Heterogeneity in program design and implementation across trials A major source of bias in this review is a high degree of heterogeneity in the ways programs were designed and implemented across trials. Our inclusion criteria specified that we would accept evaluations of any programs that used a hierarchy to promote sexual abstinence as the best strategy, while also promoting safer‐sex strategies such as condom use and partner reduction as viable alternatives. However, we did not specify to what extent the programs should emphasize abstinence, relative to other prevention strategies. This is illustrated clearly in Jemmott 1998, in which one abstinence‐plus program acknowledged that condoms were effective for preventing HIV/AIDS, but spent the majority of the intervention promoting abstinence; the other abstinence‐plus program acknowledged that abstinence was the best strategy, but spent the majority of the intervention promoting condom use and providing condom skills training. Under our rubric, both of these were abstinence‐plus programs, despite their different program focuses. The proportions of program time spent on abstinence, condom use, and other subject material may vary widely within this review.
Finding relevant trials A related potential source of bias for this review as a whole is the fact that many other HIV/AIDS risk reduction programs might have used a hierarchy to privilege abstinence over other prevention strategies, but did not state this explicitly in the abstract or trial report. We may have missed these programs in our search; if trials did not state that sexual abstinence was a main target of the program, we excluded them from the review. Additionally, our search for abstinence‐plus programs was complicated to the controversial political climate surrounding such programs, along with confusion regarding the difference between abstinence‐only and abstinence‐plus designs. Trialists sometimes felt strongly about whether programs should be classified as "abstinence‐based," "abstinence‐plus," "comprehensive," or another designation, and it is possible that the many meanings for such terms led to the omission of relevant trials from this review.
Underreporting of implementation data The problems of assessing heterogeneity and finding all relevant abstinence‐plus programs were compounded by a general lack of information on program design and actual program implementation. The majority of studies reported little data to help reviewers gauge how programs were designed, what treatments the trialists intended for participants to receive, what was actually delivered by program facilitators, and what was actually taken up or attended by the participants. The underreporting of this information may be due to the limited space allocated to program design and implementation in published journals, but may also derive from ambiguity within the interventions themselves. The failure of many programs to provide specific definitions of "abstinence" and "sex" leaves them especially vulnerable to varying interpretations by participants and staff during program delivery. Differences in the ways that programs were designed, delivered, and taken up may make studies too heterogeneous to draw comparisons across trials; however, it was difficult to uncover these differences from the available data. This source of uncertainty contributed to our decision not to undertake a statistical meta‐analysis of the trial results.
All but four of the evaluations (Danella 2000, Danielson 1990, Ferguson 1998, Jemmott 2004) reported using strategies to monitor and/or promote implementation fidelity, that is, the extent to which programs were delivered by facilitators and taken up by participants as planned. Strategies for encouraging implementation fidelity included the following: keeping attendance and/or homework records; conducting exit interviews with participants after intervention delivery; observing whether intervention materials were received; using program manuals; providing facilitators with ongoing training, technical assistance, and support; using standard intervention media materials; stressing the importance of fidelity during facilitator training; having facilitators brainstorm and use standard responses to common program questions; having facilitators report which program activities were conducted; assessing the effect of different facilitator assignments on outcomes; conducting site visits or periodic observations of program staff; creating tapes of all program sessions, which were later evaluated by the principal investigator according to an activity checklist; having a trained observer monitor a sample of all program sessions; conducting debriefing sessions or intensive interviews with program staff and participants; granting program contracts only to organizations that appeared most likely to deliver the program with high fidelity; communicating with participants by phone or mail to encourage attendance; and providing makeup sessions for absent participants.
The use of these many different strategies shows that trialists recognize the importance of implementation fidelity. However, while the strategies for promoting adherence were frequently reported, the actual extent of implementation fidelity was rarely stated. For example, while many studies collected attendance data, the mean number of hours of participant attendance was rarely reported. While many studies required facilitators to report which program activities were completed, trial reports frequently did not state the percentage of program activities that were carried out as planned. Boekeloo 1999 was an exception to this trend; the results of participant exit surveys were reported in full, showing that there were indeed significant differences between the treatments administered to intervention and control groups. Several trials carried out supplementary analyses by program dosage (O'Donnell 2002, Stanton 1996, Stanton 2006), and degree of program implementation (Wright 1997).
Specific threats to program fidelity were observed in several studies. Danielson 1990 stated that only 85% of participants in the experimental group were "successfully scheduled" to receive the intervention. This report also noted a "major area‐wide media campaign about AIDS" that occurred during the project, possibly confounding effects. Moberg 1998 reported that a vocal community opposition group made it difficult for community‐based program activities to convey program messages related to sexual behavior; additionally, at one program site a member of the community opposition group attended every program session related to sexual behavior, potentially affecting program delivery.
Effects of interventions
Before presenting results, it is useful to enumerate the similarities of the interventions across studies. All programs used a HIV prevention hierarchy to privilege sexual abstinence over safer‐sex behaviors such as condom use, reducing the number of sexual partners, or decreasing the frequency of unprotected sex. However, all programs did include elements of both abstinence and safer‐sex promotion. All programs included extensive information about HIV, STIs, and the risks of sex, and most programs included some type of condom and/or communication skills training. Almost every program was delivered in a group setting, and all but two were delivered to participants in schools or community centers. All participants were North American youth, with 37 evaluations taking place in the United States. HIV prevention was a goal of every intervention. Every study evaluated at least one behavioral or biological outcome.
These many similarities made systematic review methodology an appropriate research strategy for assessing effectiveness. However, after a thorough investigation of the data set, we determined that a statistical synthesis of the given data would be uninformative for several reasons:
Heterogeneity: Despite the many similarities across trials enumerated above, sufficient clinical heterogeneity remained. There were differences among the 39 programs in terms of intervention design, delivery, exposure, staff, and extent of emphasis on abstinence. These differences may have made the programs unsuitable for aggregation, since a meta‐analysis aggregating disparate interventions may not provide useful insight regarding which specific program types are effective.
Furthermore, the evaluations utilized a number of different control groups, recall periods, and follow‐up times. Some outcomes were reported for different subgroups across studies (eg males, females, participants reporting sexual experience at baseline). Grouping such different comparisons together could have been misleading, but separating the evaluations into sub‐comparisons rendered the groupings too small for an informative meta‐analysis.
Data availability: Another major obstacle to meta‐analyzing these results was the under‐utilization and underreporting of primary outcomes. As noted earlier, biological outcomes and the most clinically relevant behavioral outcomes (ie unprotected vaginal, anal, and oral sex) were underreported. Furthermore, we were unable to enter data into RevMan for a number of trial comparisons due to incomplete reporting by primary trials. Data unavailability also made it difficult for us to assess publication bias.
Statistical reasons: Finally, there were several compelling statistical reasons why a meta‐analysis may have been misleading. As aforementioned, most trials used complete case analyses instead of intention‐to‐treat procedures. Meta‐analyzing a number of primary studies that did not account for dropouts may have compounded this error, particularly since dropouts often differed significantly from trial completers. Other statistical obstacles included accommodating cluster randomization, adjusting results to account for baseline differences, and handling trials with more than two arms, although these could have been overcome statistically had we decided to proceed with the meta‐analysis.
Three trials reported study‐specific ICC values, which we used in our analyses for those trials (DiIorio 2006, Sikkema 2005, Wu 2003). We were unable to obtain study‐specific intra‐class correlation coefficients or raw data for the remaining cluster‐randomized trials; we therefore followed the precedent of reporting results using intra‐class correlation coefficients of 0.015 for school‐based evaluations and 0.005 for community‐based evaluations (Johnson 2002).
Where analyses were impossible in RevMan, the results are reported as available in the primary studies. Results for each outcome are summarized in Appendix A. Throughout the following sections, "n" refers to the number of participants included in the analyses and is not necessarily equivalent to the number enrolled at baseline. Some totals are approximated due to non‐specific reporting in primary trials. No trial observed a significant adverse effect for any outcome. Biological outcomes STI incidence Two trials measured self‐reported STI diagnosis by a doctor or nurse, the closest proxy for HIV infection in this review (Boekeloo 1999, Kirby 1997). These studies reported data for 1700 participants at any follow‐up; neither found significantly protective intervention effects compared to usual care, although non‐significant findings at each study's longest follow‐up favored the abstinence‐plus programs.
A third trial (n=34) took place in a residential drug treatment center and assessed participants' receipt of STI treatment in the 2 months before and after the intervention (St Lawrence 1995b). A trend at short‐term follow‐up favored an abstinence‐plus program with behavior skills training over a program version without skills training, but results were not statistically significant.
No trial assessing STI incidence had an overall attrition rate exceeding 33% of baseline enrolment.
Pregnancy incidence Limited evidence suggested that abstinence‐plus programs can reduce pregnancy incidence. Seven trials assessed self‐reports of having or causing a pregnancy, with analyses representing 3672 participants (Boekeloo 1999, Coyle 2006, Ferguson 1998, Kirby 1997, O'Donnell 2002, Philliber 2001, Wu 2003). One trial (n=941) discovered a significantly protective effect at long‐term follow‐up compared to usual care (Philliber 2001), although subgroup analyses discovered significance among girls only (n=519). Another trial found that adding a parental monitoring intervention to a community‐based abstinence‐plus program led to a significantly protective effect on the incidence of pregnancy among all participants at 24‐month follow‐up (n=494; Wu 2003). Additional analyses favored the parental monitoring program without booster sessions over the parental monitoring program with booster sessions (n=295).
A third trial (n=195) did not report significance, but long‐term findings suggested that students who participated in an in‐school curriculum with community service were less likely to report a pregnancy than students who participated in the curriculum without service hours (O'Donnell 2002).
The remaining four studies found no significant effects compared to usual care (n=1990; Boekeloo 1999, Coyle 2006, Kirby 1997) or a non‐enhanced program version (without peer counseling, n=63; Ferguson 1998). Non‐significant findings in three trials favored abstinence‐plus programs over usual care at longest follow‐up (n=1987; Boekeloo 1999, Coyle 2006, Kirby 1997).
Two trials assessing pregnancy incidence had overall attrition rates exceeding 33% of baseline enrolment (Coyle 2006, Wu 2003).
Behavioral outcomes Incidence of unprotected vaginal sex Three trials reported participants' self‐reported incidence of unprotected vaginal sex (n approx 2495; Jemmott 2004, Jemmott 1998, DiIorio 2007). All three compared an abstinence‐plus program to an attention‐matched control group.
Two trials found significantly protective effects at 3‐month and 12‐month follow‐up, but not at 6‐month follow‐up. One assessed lifetime incidence of unprotected sex among participants who reported ever having had sex, and found protective effects among all participants (n<277; it was unclear how many participants were in this subgroup) (DiIorio 2007). The other trial assessed unprotected sex in the past 3 months, and found protective effects only among participants who had reported ever having had sex at baseline (n approx 69; Jemmott 1998). Subsequent analyses favored a condom‐focused abstinence‐plus program over an abstinence‐focused program for this subgroup (n=59, OR=0.23; 95% CI 0.05 to 0.95).
The remaining trial found no significant effect at 12‐month follow‐up (n=1707) (Jemmott 2004). It was unclear whether this outcome referred to incidence or frequency of unprotected vaginal sex, or whether it was reported among any particular subgroup of participants.
No trial assessing incidence of unprotected vaginal sex had an overall attrition rate exceeding 33% of baseline enrolment.
Frequency of unprotected vaginal sex Twelve trials assessed participants' self‐reported frequency of unprotected vaginal sex (n=4270; Coyle 2001, Coyle 2006, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000a, Kennedy 2000b, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, Villarruel 2006).
Significance tests in six trials (n=2704) indicated protective intervention effects compared to attention controls (n=762; Jemmott 1992, Jemmott 1998, Villarruel 2006), information about HIV (n=1371; Coyle 2001), usual care (n=412; Coyle 2006), and a non‐enhanced program version (without skills training and a motivation component (n=159; St Lawrence 2002) at any follow‐up. Subgroup analyses showed that protective effects in one study using an attention control were significant only among participants who had reported sexual experience at baseline (n=69; Jemmott 1998).
The remaining six trials (n=1353) found no significant effects at any time point compared to no treatment (n=212; Kennedy 2000a, Kennedy 2000b), attention‐matched controls (n=916; Hewitt 1998, Jemmott 1999, St Lawrence 1999), or a non‐enhanced program version without skills training (n=225, St Lawrence 1995a).
Three trials assessing frequency of unprotected vaginal sex had overall attrition rates exceeding 33% of baseline enrolment (Coyle 2006, Kennedy 2000a, Kennedy 2000b).
Frequency of unprotected oral sex The only trial to assess this outcome (n=225) took place in a community‐based organization, comparing the program to a non‐enhanced version without skills training (St Lawrence 1995a). This trial found significantly a protective effect according to a group‐by‐time interaction with assessments at 2, 8, and 14 months after baseline. Attrition in this trial did not exceed 33% of baseline enrolment.
Frequency of unprotected anal sex Two trials assessed participants' self‐reported frequency of unprotected anal sex (n=537), and both evaluated versions of the Becoming a Responsible Teen program (St Lawrence 1995a, St Lawrence 1999). One trial (n=225) took place in a community‐based organization, comparing the program to a non‐enhanced version without skills training (St Lawrence 1995a). This trial found significantly a protective effect according to a group‐by‐time interaction with assessments at 2, 8, and 14 months after baseline. The other trial (n=312) took place in a juvenile reformatory and found no significant program effects approximately seven months after baseline compared to an attention control (St Lawrence 1999). Attrition in these trials did not exceed 33% of baseline enrolment.
Combined incidence of vaginal, oral, or anal sex Four trials reported incidence of any recent oral, anal, or vaginal sex (n=5084; Boekeloo 1999, Markham 2006, St Lawrence 1995a, Wright 1997). Two trials found protective effects: one compared to usual care at five‐month follow‐up (n=1206; Markham 2006), and one compared with a non‐enhanced program version (without skills training) at 14‐month follow‐up (n=225; St Lawrence 1995a).
The remaining two trials found no significant effects compared to usual care (n=3653; Boekeloo 1999, Wright 1997). One of these trials assessing had an overall attrition rate exceeding 33% of baseline enrolment (Wright 1997).
Incidence of any vaginal sex Twenty‐one trials evaluated incidence of any (protected or unprotected) vaginal sex (n approx 13208; Boekeloo 1999, Coyle 2004, Danella 2000, Danielson 1990, Ferguson 1998, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000a, Kennedy 2000b, McBride 2000b, McBride 2000a, Moberg 1998, O'Donnell 2002, St Lawrence 2002, Stanton 2006, Villarruel 2006, Weeks 1997, Wu 2003, Stanton 2000).
Comparisons in five trials (n=2237) found significantly protective effects at any time point compared to no treatment (n=55; McBride 2000a), attention controls (n=356; Jemmott 1998), usual care (significant among males only, n=1412; Coyle 2004), or non‐enhanced program versions (one without community service, n=255, O'Donnell 2002; one without skills training and a motivational component, n=159, St Lawrence 2002).
The remaining 16 trials (n=9379) found no significant effects at any time point compared to no treatment (n=1890; Danella 2000, Danielson 1990, Kennedy 2000a, Kennedy 2000b, McBride 2000b), attention controls (n=2416; Hewitt 1998, Jemmott 1992, Jemmott 1999, Stanton 2000, Stanton 2006, Villarruel 2006), usual care (n=4445; Boekeloo 1999, Moberg 1998, Weeks 1997), and a non‐enhanced program version (n=628; Ferguson 1998, Wu 2003).
Three trials assessing incidence of vaginal sex had overall attrition rates exceeding 33% of baseline enrolment (Coyle 2004, Weeks 1997, Wu 2003).
Frequency of any vaginal sex Thirteen trials reported participants' frequency of recent vaginal sex (n=8524) (Boekeloo 1999, Coyle 2001, Coyle 2004, Coyle 2006, Hernandez 1990, Hewitt 1998, Jemmott 1992, Jemmott 1998, Kennedy 2000a, Kennedy 2000b, Kirby 1997, Smith 1994, Jemmott 2004).
Five trials (n=2169) observed significantly protective effects at any time point compared to attention controls (n=169; Jemmott 1992, Jemmott 1998), information about HIV (n=95; Smith 1994), or usual care (significant among all participants (n=493; Coyle 2006), or among males only (n=1412; Coyle 2004). Protective effects in one study using an attention control were significant only among participants who had reported sexual experience at baseline (n=69; Jemmott 1998).
The other eight trials (n=4371) found no significant effects compared to no treatment (n=618; Hernandez 1990, Kennedy 2000a, Kennedy 2000b), attention controls (n=1831; Hewitt 1998, Jemmott 2004), information about HIV (n=1371; Coyle 2001), and usual care (n=551; Boekeloo 1999, Kirby 1997).
Four trials assessing frequency of vaginal sex had overall attrition rates exceeding 33% of baseline enrolment (Coyle 2004, Coyle 2006, Kennedy 2000a, Kennedy 2000b).
Frequency of any oral sex One trial reported frequency of oral sex, comparing an abstinence‐plus program to an attention control; findings were non‐significant approximately seven months after baseline (n=312; St Lawrence 1999). Attrition in this trial did not exceed 33% of baseline enrolment.
Incidence of any anal sex Three trials reported incidence of anal sex (n=1091; Jemmott 1992, Jemmott 1999, Wu 2003). Two trials compared versions of the Be Proud! Be Responsible! program to attention controls: one found protective effects at 6‐month, but not 3‐month follow‐up (n=460; Jemmott 1999). The other found a protective effect at 3‐month follow‐up (n=117; Jemmott 1992).
The third trial included three arms comparing (1) the Focus on Kids program with parental monitoring and booster sessions, (2) Focus on Kids with parental monitoring but not booster sessions, and (3) Focus on Kids without parental monitoring or booster sessions. No significant effects were found for any pairwise comparison for incidence of anal sex at 24 months after baseline (n=494; Wu 2003). Final attrition in this trial exceeded 33% of baseline enrolment.
Frequency of any anal sex Two trials reported frequency of anal sex (n=590; Jemmott 1992, Jemmott 1999). Both compared versions of the Be Proud! Be Responsible! program to attention controls. One evaluation found a protective effect at six‐month, but not three‐month follow‐up (n=460) (Jemmott 1999). The other found no significant effect at three‐month follow‐up (n=117) (Jemmott 1992), which was the only assessment time. Neither trial had an overall attrition rate that exceeded 33% of baseline enrolment.
Incidence of "casual sex" One trial assessed the incidence of "casual sex" at 3.5‐month follow‐up (n=34) (St Lawrence 1995b); although results favored the addition of skills training to the Becoming a Responsible Teen program, findings did not reach significance in RevMan. There was no attrition in this trial.
Frequency of "casual sex" One trial assessed the frequency of casual sex approximately seven months after baseline (n=312), and found no significant effects compared to an attention control (St Lawrence 1999). Overall attrition in this trial did not exceed 33% of baseline enrolment.
Number of sex partners Thirteen trials assessed participants' number of sexual partners (Boekeloo 1999, Coyle 2001, Coyle 2004, Coyle 2006, Hernandez 1990, Jemmott 1992, Jemmott 1999, Kirby 1997, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, Villarruel 2006, Wright 1997). Any definition of "sexual partner" was accepted for this outcome. Analyses represent at least 7495 but fewer than 10513 participants; one large study restricted analyses to sexually experienced participants without reporting the size of this subgroup (Wright 1997).
Four evaluations (n=2236) found significantly protective effects at any follow‐up compared to attention controls (n=665 Jemmott 1992, Villarruel 2006), usual care (significant among males only, n=1412; Coyle 2004), or a non‐enhanced program version without skills training and a motivation component (n=159; St Lawrence 2002).
The remaining nine studies (3842<n<6860) found no significant effects compared to no treatment (n=388 Hernandez 1990), attention controls (n=792; Jemmott 1999, St Lawrence 1999), information about HIV (n=1371; Coyle 2001), usual care (1066<n<4084; Boekeloo 1999, Coyle 2006, Kirby 1997, Wright 1997), and a non‐enhanced program version without skills training (n=225; St Lawrence 1995a).
Three trials assessing number of sex partners had overall attrition rates exceeding 33% of baseline enrolment (Coyle 2004, Coyle 2006, Wright 1997).
Number of unprotected sex partners Two school‐based trials (n=1842) reported the number of partners with whom participants reported unprotected sex (Coyle 2001, Coyle 2006). One trial found significantly protective effects among all participants at 19‐month and 31‐month follow‐up, but not at seven‐month follow‐up (n=1371) compared to an information control (Coyle 2001); repeated measures analyses by gender showed that the effect was significant among males only (n=658).
The other trial found no significant effects at 6‐month, 12‐month, or 18‐month follow‐up compared to usual care (n=471) (Coyle 2006). Attrition in this trial exceeded 33% of baseline enrolment.
Number of oral sex partners One trial (Wright 1997) assessed participants' self‐reported number of lifetime oral sex partners, reporting non‐significant effects compared to usual care at long‐term follow‐up. Although group means favored the intervention group over controls at both 12‐month follow‐up (n<3018) and 24‐month follow‐up (n<2323), comparisons did not reach statistical significance at either point according to repeated‐measures ANOVAs. Overall attrition in this trial exceeded 33% of baseline enrolment.
Number of anal sex partners Three studies (Jemmott 1992, Jemmott 1999, Wright 1997) assessed participants' self‐reported number of anal sex partners. The number of participants analyzed at any time point was between 594 and 3612, but is uncertain because one study did not report the specific number analyzed. One study found a significantly protective effect compared to an attention control group at 6‐month follow‐up (n=460; Jemmott 1999); the remaining trials found no significant effects at 3‐month follow‐up compared to attention control (n=114, Jemmott 1992), or at 12‐month or 24‐month follow‐up compared to usual care (n<3018, Wright 1997). One trial assessing number of anal sex partners had an overall attrition rate exceeding 33% of baseline enrolment (Wright 1997).
Incidence of sex with a non‐monogamous partner One trial assessed sex in the past 2 months with a partner known to be non‐monogamous, among all participants. According to RevMan analyses, the effect did not reach significance when compared to a non‐enhanced program version (without skills training) at 3.5 months after baseline (n=34; St Lawrence 1995b). There was no attrition in this trial.
Number of sex partners known to be non‐monogamous Only St Lawrence 1999 assessed participants' number of partners known to be non‐monogamous, with analyses representing 312 participants at at least 7‐month follow‐up (6 months after release from a juvenile correctional facility, after receiving the intervention upon arrival at the facility). An abstinence‐plus program was compared to an attention control focusing on anger management, with no significant effects according to a MANOVA. Attrition in this trial did not exceed 33% of baseline enrolment.
Use of condoms Twenty‐six trials reported any measure of condom use (Aarons 2000, Boekeloo 1999, Coyle 2001, Coyle 2004, Coyle 2006, Danella 2000, DiIorio 2006, Hewitt 1998, Jemmott 1992, Jemmott 1998, Kennedy 2000a, Kennedy 2000b, Kirby 1997, Moberg 1998, Philliber 2001, Sikkema 2005, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, Stanton 2006, Stanton 1996, Villarruel 2006, Weeks 1997, Wright 1997, Wu 2003, Jemmott 2004). Analyses represent at least 5100, but fewer than 14641 participants; nine trials restricted this outcome to sexually experienced participants but did not report the size of this subgroup (Aarons 2000, Coyle 2004, Danella 2000, Hewitt 1998, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, Wright 1997, Jemmott 2004). No trial assessed the use of male and female condoms separately.
Fourteen studies (2640<n<5231) reported a significantly protective effect at any follow‐up compared to no treatment (n<500; Danella 2000), attention controls (378<n<2085; Jemmott 1992, Jemmott 1998, Jemmott 2004, Villarruel 2006), information about HIV (n=1436; Coyle 2001, DiIorio 2006, Sikkema 2005), usual care (n=515; Boekeloo 1999, Coyle 2006), or a non‐enhanced program version (without skills training [n<225; St Lawrence 1995a], without skills training and a motivation component [n<159; St Lawrence 2002], without delivering the intervention in friendship groups [n=71; Stanton 1996], without parental monitoring [n=240; Wu 2003]).
The remaining 12 trials (2432<n<9382) found no significant effects compared to no treatment (n=287; Kennedy 2000a, Kennedy 2000b), attention controls (271<n<707; Hewitt 1998, St Lawrence 1999, Stanton 2006), and usual care (1874<n<8388; Aarons 2000, Coyle 2004, Kirby 1997, Moberg 1998, Philliber 2001, Weeks 1997, Wright 1997).
Eight trials assessing condom use had overall attrition rates that exceeded 33% of baseline enrolment (Coyle 2004, Coyle 2006, Kennedy 2000a, Kennedy 2000b, Sikkema 2005, Weeks 1997, Wright 1997, Wu 2003).
An additional trial assessed the absolute number of times that participants used condoms at six‐week follow‐up, finding no significant effects in an ANOVA comparing abstinence‐plus, abstinence‐only, and safer‐sex programs against a no‐treatment control (n=388) (Hernandez 1990). A post‐hoc test found that safer‐sex program participants reported using condoms on significantly more occasions than abstinence‐plus program participants (n approx 194). However, this outcome did not accommodate possible differences in the number of times participants had sexual intercourse. Without this data, it is impossible to say whether this effect suggests benefit (e.g., fewer sex acts) or possible harm (e.g., a lower percentage of condom‐protected occasions).
Incidence of sexual initiation Nineteen trials assessed sexual initiation, virginity, or "ever had sex" (n approx 20367) (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Dancy 2006, DiIorio 2006, Ferguson 1998, Kirby 1997, Markham 2006, McBride 2000b, McBride 2000a, Moberg 1998, O'Donnell 2002, Philliber 2001, Sikkema 2005, Stanton 2006, Weeks 1997, Wright 1997, DiIorio 2007).
Four trials (n approx 1990) found a significantly protective program effect at any time point compared to usual care (significant among females only [n=271, Aarons 2000], or among males only [n=1412; Coyle 2004]), or a non‐enhanced program version (without community service [n=225; O'Donnell 2002] or without peer counseling [n=52; Ferguson 1998]).
The other 15 trials (n=16451) found no significant effects compared to no treatment (n=281; McBride 2000b, McBride 2000a), attention controls (n=1056; Dancy 2006, DiIorio 2007, Stanton 2006), information about HIV (n=3755; Coyle 2001, DiIorio 2006, Sikkema 2005), and usual care (n=11359; Coyle 2006, Kirby 1997, Markham 2006, Moberg 1998, Philliber 2001, Weeks 1997, Wright 1997).
Five trials assessing sexual initiation had overall attrition rates exceeding 33% of baseline enrolment (Coyle 2004, Coyle 2006, Sikkema 2005, Weeks 1997, Wright 1997).
Risk behavior index Five trials aggregated sexual risk behavior into an index for assessing intervention effects (n=1298). The definitions of these indices varied, and four of the five studies (n=966) discovered significantly protective effects at short‐term, medium‐term, or long‐term follow‐up, when programs were compared to an attention control at short‐term and medium‐term follow‐up (n=598, Jemmott 1992, Jemmott 1999) or non‐enhanced program versions (without skills training) at long‐term follow‐up (n=368, St Lawrence 1995a, St Lawrence 2002).
One trial found no significant effects compared to an attention control at approximately 7 months after baseline (n=312; St Lawrence 1999). No trial that used a risk behavior index had an overall attrition rate exceeding 33% of baseline enrolment.
Knowledge of HIV or STI facts Twenty‐four trials reported a measure of HIV/AIDS knowledge (n approx 20904) (Boekeloo 1999, Coyle 2001, Coyle 2004, Coyle 2006, Dancy 2006, Danella 2000, Danielson 1990, DiIorio 2006, Ferguson 1998, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000b, Kennedy 2000a, Kirby 1997, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, St Lawrence 1995b, Stanton 2006, Stanton 1996, Weeks 1997, Wright 1997). Definitions of knowledge varied.
Comparisons in twenty trials (n approx 19364) found that abstinence‐plus program participants reported significantly greater HIV/AIDS knowledge when compared to no treatment (n=2073; Danella 2000, Danielson 1990, Kennedy 2000a, Kennedy 2000b), attention controls (n approx 1915; Dancy 2006, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, St Lawrence 1999), information about HIV (n=4151; Coyle 2001, DiIorio 2006), usual care (n=10948; Boekeloo 1999, Coyle 2004, Coyle 2006, Kirby 1997, Weeks 1997, Wright 1997), and a different program version (n=277; Ferguson 1998, St Lawrence 1995a). In one trial, participants in a non‐enhanced program version (without peer counseling) demonstrated greater knowledge than participants in the enhanced version at 3‐month follow‐up (n=52; Ferguson 1998).
The four studies with non‐significant findings (n=1432) either compared an abstinence‐plus program to a non‐enhanced program version (without skills training [n=34, St Lawrence 1995b], without skills training and a motivational component [n=159, St Lawrence 2002], without delivering the program in friendship groups [n=301, Stanton 1996]) or used an attention control in an area with preexisting HIV education (n=938; Stanton 2006).
Six trials assessing knowledge had overall attrition rates exceeding 33% of baseline enrolment (Coyle 2004, Coyle 2006, Kennedy 2000a, Kennedy 2000b, Weeks 1997, Wright 1997).
Cost Seven trials reported any measure of program cost.
Cost data for the Safer Choices intervention in Coyle 2001 were reported in a separate paper (Wang 2000). According to the paper, the intervention was "cost‐effective and cost saving in most scenarios considered." The cost‐effectiveness evaluation estimated intervention costs, and then used the Bernoulli model to translate condom and contraceptive use data into an estimated number of prevented cases of HIV, other STIs, and pregnancy (and the corresponding medical and social costs averted). According to this analysis, the program cost 105,243 USD and prevented 0.12 cases of HIV, 24.37 cases of chlamydia, 2.77 cases of gonorrhea, 5.86 cases of pelvic inflammatory disease, and 18.5 pregnancies (assuming that 345 participants were sexually active). These averted case numbers suggested that for every 1 USD in program costs, 2.65 USD were saved in total medical and social costs (Wang 2000).
The intervention evaluated in Dancy 2006 was reportedly "cost‐effective," but no cost data were presented.
One trial based in non‐governmental organizations (Jemmott 2004) reported that the training of facilitators "need not be extraordinarily extensive or expensive" in order to achieve program effects. Specific cost data were not provided.
McBride 2000a and McBride 2000b reported that program sites received between 40,000 and 50,000 USD per year for program costs. These data were not translated into estimates of cost‐benefit.
Philliber 2001 reported cost data for program sites in New York City only (where 6 of the 12 program sites were located). In these settings, program costs per participant were 4,000 USD per year, averaging approximately 16 USD per day. These data were not translated into estimates of cost‐benefit.
Sikkema 2005 reported that the intervention "would need to avert only a small number of HIV infections to be cost‐saving to society." Specific cost data were not provided.
Participant Satisfaction Twenty‐three trials indicated any information about program acceptability or participant satisfaction. Where these data were available, evaluations consistently indicated high levels of acceptability and participant satisfaction (Coyle 2001, Coyle 2004, Coyle 2006, DiIorio 2007, DiIorio 2006, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, McBride 2000b, McBride 2000a, Moberg 1998, O'Donnell 2002, Philliber 2001, Smith 1994, St Lawrence 1995a, St Lawrence 1999, St Lawrence 2002, St Lawrence 1995b, Stanton 1996, Villarruel 2006, Wright 1997, Markham 2006). One trial reported organized resistance from a minority of community members, but the program was reportedly acceptable to the majority of stakeholders (Moberg 1998).
Discussion
Summary of main results The 39 included trials (n=37724) showed no evidence that abstinence‐plus programs increase HIV risk among youth participants in high‐income countries, and multiple evaluations found that the programs can decrease HIV risk. Twenty‐four trials (baseline n=20982) observed significantly protective program effects for behavioral outcomes (Aarons 2000, Boekeloo 1999, Coyle 2001, Coyle 2004, Coyle 2006, Danella 2000, DiIorio 2006, Ferguson 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Markham 2006, McBride 2000a, O'Donnell 2002, Sikkema 2005, Smith 1994, St Lawrence 1995a, St Lawrence 2002, Stanton 1996, Villarruel 2006, Wu 2003, Jemmott 2004, DiIorio 2007) and/or biological outcomes (Philliber 2001, Wu 2003), but protective effects were not consistent across all trials. The overwhelming majority of trials that assessed HIV/AIDS knowledge found significant results favoring abstinence‐plus program participants. No adverse program effects were reported for any outcome.
The results of this review may not generalize to all abstinence‐plus programs in all high‐income settings. The applicability of results must be appraised carefully given the methodological deficiencies of included trials, the relatively homogeneous nature of participants represented in this review (North American adolescents), the substantial heterogeneity across trials in the ways programs were designed and delivered, the under‐utilization of outcomes most relevant to HIV risk, and the frequent omission of methodological details and implementation information from primary trial reports.
Self‐reported biological outcomes Biological outcomes for this review were severely under‐utilized and limited to participants' self‐reported incidence of STI and pregnancy. Against usual care control groups, three program trials did not indicate that abstinence‐plus programs can significantly affect incidence or treatment of STI diagnosis at any time point (n=1734). While several programs appeared to have more promising effects on pregnancy incidence, findings across seven studies with various control groups (n=3672) were inconsistent and in once case hampered by the lack of a statistical test. No study observed a statistically significant iatrogenic effect for any biological outcome at any follow‐up time.
The evidence of biological effects is limited by the following: floor effects constrain the possibility of finding significant effects where prevalence is low; quantitative synthesis of the available results was determined to be uninformative; reporting bias or the lack of diagnosis may impede reliable self‐reports of STI and pregnancy (ie relying on diagnosis does not capture undiagnosed conditions, especially given that many STIs are asymptomatic); STI incidence, STI treatment, and especially pregnancy incidence have limited ability to indicate HIV risk; and significance was not provided for one study that may have had protective effects (O'Donnell 2002).
Self‐reported behavioral outcomes Every trial reported at least one behavioral outcome, although assessments of unprotected sexual behaviors continued to be remarkably under‐utilized. Unprotected sexual behavior outcomes for which significance was observed included incidence of unprotected vaginal sex; frequency of unprotected vaginal sex, frequency of unprotected oral sex; and frequency of unprotected anal sex. Other outcomes for which significance was observed included incidence of oral, anal or vaginal sex; incidence of vaginal sex; frequency of vaginal sex; incidence of anal sex; frequency of anal sex; number of partners; number of unprotected partners; number of anal sex partners; condom use; sexual initiation; and a risk behavior index. No harms were observed
Several outcomes were relevant to abstinent behavior (ie sexual initiation; the incidence of vaginal, oral, and anal sex; and the frequency of vaginal, oral, and anal sex). Results for these outcomes were mixed, suggesting that many, but not all abstinence‐plus programs may reduce the incidence or frequency of sexual activity. Importantly, no study observed any harms for these outcomes, suggesting abstinence‐plus programs did not hasten sexual initiation, nor did any program increase the incidence or frequency of sexual activity. Furthermore, no study observed an adverse program effect on condom use, suggesting that abstinence promotion messages did not undermine the safer‐sex components of abstinence‐plus programs.
Nine trials discovered that one abstinence‐plus program was significantly more effective than another program version (DiIorio 2006, Ferguson 1998, Jemmott 1998, O'Donnell 2002, Sikkema 2005, St Lawrence 1995a, St Lawrence 2002Stanton 1996, Wu 2003). These findings should prompt further investigation into intervention mechanisms and the generalizability of effects.
The evidence of behavioral effects is limited by several factors: quantitative synthesis of the available results was impossible; reporting bias or differing definitions of behavioral terms may impede reliable self‐reports of behavior; behavioral outcomes have limited ability to indicate HIV risk (Peterman 2000, O'Leary 1997); floor effects may constrain the possibility of finding significant change in participant populations with low levels of sexual activity; and five of the studies reporting behavioral outcomes had overall attrition rates exceeding 33%. The underreporting of key outcomes and the lack of implementation data made it difficult to identify the specific contexts, populations, and program characteristics that brought about the effects observed.
HIV/AIDS knowledge HIV/AIDS knowledge was one of the most commonly assessed outcomes in this review (24 trials, n approx. 20904), and all but four studies assessing this outcome found statistically significant protective effects at every follow‐up time. This review provides overwhelming evidence that abstinence‐plus programs consistently and significantly improve participants' knowledge of HIV/AIDS information, as compared to a variety of control groups at short‐term, medium‐term, and long‐term assessments.
Results for this outcome are particularly limited by heterogeneity in the ways studies defined HIV/AIDS knowledge. While some studies limited this outcome to knowledge of several basic transmission facts (eg Boekeloo 1999), others used extensive scales to assess a more thorough knowledge of HIV/AIDS biology, transmission, and prevention. HIV/AIDS knowledge scales were also frequently combined with knowledge of other reproductive health facts, STD‐related information, and information about pregnancy and contraception.
Acceptability: cost and participant satisfaction Insufficient cost data were available to assess the cost‐effectiveness of abstinence‐plus interventions. Where these data were collected (23 trials), participants' evaluations of the experimental programs consistently indicated high levels of program acceptability and participant satisfaction.
Additional results from recently completed trials At the time of this review, two replication trials of the Be Proud! Be Responsible! intervention had been completed, but we were unable to obtain complete results either from conference presentations or from the authors (Borawski 2007, Jemmott 2006). We do not believe that including these trials would have changed the results of this review.
One trial encompassed ten arms (baseline n=662), comparing an 8‐hour and a 12‐hour abstinence‐plus program to an abstinence‐only program, a safer‐sex program, and an attention control at 24‐month follow‐up (with and without booster sessions for each condition) (Jemmott 2006). Preliminary findings included logistic regression results for sexual initiation among baseline virgins, which found no significant difference between the 4 abstinence‐plus and the 2 abstinence‐only arms at 24‐month follow‐up (P=0.07). Similar analyses of sexual intercourse incidence among all participants appeared to favor the abstinence‐only intervention over the abstinence‐plus intervention arms, but significance was unclear (P=0.05). This contrasts with nineteen trials in this review that found protective or non‐significant effects (n approx 20367). Outcome data for all other comparisons, including results for condom use and unprotected sex, were unavailable at the time of this review.
The other trial took place among slightly older adolescents in US suburbs (Borawski 2007). Ten high schools were enrolled in the trial. Preliminary results suggested no significant behavioral effects at one‐year follow‐up when compared to an attention control (Kirby 2006), but specific information was not yet available.
No results were available for Brown 2002, Jemmott 2007, Markham 2007, and Tortolero 2007.
Quality of the evidence: Internal validity and methodological rigor Methodological quality was sometimes difficult to judge due to incomplete reporting of key methodological and clinical features. Reporting deficiencies may obscure important methodological strengths or weaknesses, and it was often difficult to obtain additional information by contacting the trialists due to data loss and non‐response.
As a group, the studies had several important strengths: large sample sizes, attention to long‐term follow‐up, stating a theoretical basis for the experimental intervention, describing the development of data collection instruments, using techniques to promote the validity of self‐reported data, controlling for baseline differences in statistical analyses, and reporting the causes and possible impacts of attrition.
However, these strengths were partially overshadowed by the following methodological weaknesses or ambiguities:
Underreporting of key methodological features: Few of the evaluations specified the procedures used for assigning participants, concealing the allocation sequence, blinding outcome assessors, or separating program facilitators between the intervention and control groups.
Missing data: Commonly missing values across studies included the number of participants per trial arm at baseline and follow‐up, means and standard deviations for continuous outcomes, percentages for dichotomous outcomes, effect sizes, and attrition analyses. Power calculations were rarely reported, although the median sample size was fairly large.
Attrition at last follow‐up: Dropout exceeded 33% in eight of the included studies. Only three trials used intention‐to‐treat analyses, which account for data missing due to attrition; instead, every trial used a complete case analysis. Missing data caused a number of problems during the review, especially with respect to quantitative synthesis and testing for publication bias.
Unit of analysis problems: Of the 21 trials that used cluster randomization, 14 statistically accommodated the unit of randomization. The other 7 studies are potentially vulnerable to Type I errors. Our inability to estimate reliable intraclass correlation coefficients from available study data is a possible source of bias for the review as a whole.
Limitations of outcome measures: All outcome data in this review (except STI treatment data for St Lawrence 1995b) are vulnerable to self‐report bias. While biological outcomes are the best indicators of HIV risk, there are obstacles to using these outcomes among youth populations. These include resistance from schools or parents, logistical difficulties, and floor effects (a recent study suggests that overall HIV prevalence in young adults in the US is 1.0 per 1000, Morris 2006). For these reasons, self‐reported behavioral outcomes were a necessary proxy for HIV risk, inevitably introducing self‐report bias. The results of this review highlight the need for a standardized set of outcome measures with unambiguous and explicit definitions, consistent follow‐up times and recall periods, and clinically meaningful implications for HIV risk. Reaching a consensus on a set of behavioral outcomes, follow‐up times, recall periods, subgroups of interest, and reporting formats would transform researchers' ability to make comparisons across primary trials. As this review demonstrates, behavioral outcomes of HIV prevention trials are often nonspecifically defined (particularly for terms known to have varying meanings, such as "sex," "virginity," or "partner"); different studies use differing follow‐up times and recall periods; the most clinically meaningful outcomes (eg STI incidence, incidence of unprotected vaginal sex) are rarely used; outcomes are rarely separated into oral, anal, and vaginal sex acts, which carry different levels of HIV risk; outcomes are reported for various subsets of participants across studies; and long‐term follow‐up data are often not collected. Long‐term follow‐up data are also particularly relevant for studies of youth sexual behavior, which is often characterized by intermittent periods of activity (Rotheram‐Borus 2000).
Insufficient reporting on program design and implementation: Incomplete reporting on the design and implementation of both experimental and control interventions has been previously noted as a limitation of behavioral HIV prevention trials (O'Leary 1997); ideally, reports of implementation should be sufficiently detailed to permit replication, or at least to permit reviewers to judge whether programs are similar enough to combine their evaluations in a systematic review (Montgomery 2005). Additionally, detailed reporting on implementation characteristics can allow the tracking of particular program components across studies, leading to the identification of potentially effective program characteristics. Few of the trials in this review reported this level of detail on intervention design, program delivery by staff, uptake by participants, and unique features of the trial context (eg concurrent media campaigns, community support or opposition to the program, prevalence of HIV in the specific target population, prevalence of structural risk factors). Journals may wish to consider dedicating more space to the reporting of key implementation data for studies of behavioral HIV prevention programs. Details on the treatment of control groups were rarely reported, although these are crucial to understand trial comparisons. To address the current debate over abstinence‐based programs, comparisons of abstinence‐plus programs against abstinence‐only interventions may provide the most relevant data. It is possible that studies with "usual care" control groups may have made some of these comparisons, but unclear reporting of what control group participants actually received made this difficult to determine.
Overall completeness and applicability of evidence External validity The objective of this review was to determine the effectiveness of abstinence‐plus programs for HIV prevention among all participants in high‐income countries. The evidence gathered by our search is somewhat able to address this objective, but the generalizability (external validity) of these results may not extend to all abstinence‐plus programs in all high‐income settings. The included studies most frequently evaluated community‐based abstinence‐plus programs among US ethnic minority adolescents who lived in low‐income urban areas. However, the application of this trial evidence in any high‐income setting must be considered carefully given the following limitations.
First, relatively little data were available for the biological outcomes of interest. Data were also insufficient to inform assessments of cost‐effectiveness, implementation fidelity, intervention mechanisms, and the effectiveness of specific program characteristics across studies. Program designs were consistent with the interventions described in our background research, but they may not represent the entire realm of abstinence‐plus approaches in high‐income countries. It is also important to note that most studies did not specify an exact definition of "abstinence" or "sex." With very few exceptions, it was unclear whether programs encouraged participants to abstain from vaginal, oral, and/or anal intercourse; the temporal element of abstinence was also frequently unclear (e.g., abstinence until marriage, until a one‐year delay in sexual initiation, until a committed relationship, or until an unspecified time in the future). This ambiguity may have allowed significant clinical heterogeneity across studies, and it hindered attempts to conduct subgroup analyses based on different definitions of abstinence.
Second, as in previous reviews, the results of this review are derived from studies enrolling North American youth. However, this is the first review to extensively search for abstinence‐plus program trials from all high‐income economies, including those outside North America. Alongside conclusions about program effectiveness, this review can also conclude that abstinence‐plus program trials in high‐income countries outside North America are rare or inaccessible by existing search methods. We cannot be certain which of these possibilities contributed to the lack of non‐North American evidence, but past reviews have suggested that abstinence‐based approaches are less common in high‐income countries beyond the US (Berne 1999, Jones 1985). Given the protective effects discovered by this review, some abstinence‐plus programs may be feasible beyond North America; however, program implementers in other regions must carefully research program acceptability and rigorously compare abstinence‐plus programs to existing HIV prevention strategies.
Third, even within the realm of North American adolescents and young adults, a number of vulnerable groups are not represented in these trials. For example, data were unavailable or could not be disaggregated for gay, lesbian, bisexual, or transgender youth; youth with disabilities; youth who have immigrated to the US; substance‐dependent youth; or homeless young people. It was not possible to carry out subgroup analyses by age, gender, program setting, program facilitator, SES, religiosity, sexual orientation, ethnicity, or other characteristics, although many of these may be important moderators of program effects. Age may be particularly critical: with mean ages ranging from 11.3 to 19.3, trials enrolled participants in many stages of sexual development. This variation may have affected the way abstinence‐based messages were presented and received across trials. Several regions of the US were underrepresented, particularly the South and Midwest, and there was a general lack of studies in rural areas.
Fourth, one of the most salient research deficits in this review is the lack of direct comparisons of abstinence‐plus against abstinence‐only, condom‐promotion, or safer‐sex programs. According to our criteria, Hernandez 1990 was the only study to provide this type of comparison. This study evaluated a one‐session intervention and was limited to short‐term follow‐up; results showed no significant differences between an abstinence‐plus program, an abstinence‐only program, a safer‐sex program, and a nonintervention control. Beyond these results, this review cannot directly address the differential effectiveness of abstinence‐plus and abstinence‐only strategies for HIV prevention.
Evidence in the practice context We prepared this review as a complement to our recent review of abstinence‐only programs for HIV prevention in high‐income countries. Despite these limitations, the evidence from this systematic review has crucial implications for public health policy and practice, particularly in the debate over abstinence‐only and abstinence‐plus HIV prevention strategies. As updated in February 2007, our review of abstinence‐only programs discovered 13 program trials from eight papers, which enrolled 15940 US adolescents. Trials consistently found no significant program effects on biological and behavioral outcomes when compared to various controls. One study observed short‐term and long‐term harms for STI incidence, pregnancy incidence, and frequency of vaginal sex compared to usual care (n=4652); these were not mirrored in other studies. An isolated protective effect was observed for incidence of recent sex (n approx 839, compared to usual care controls), but this was limited to short‐term follow‐up and offset by non‐significant findings in other trials. In sum, the review suggested that abstinence‐only interventions do not significantly decrease or exacerbate HIV risk among high‐income country participants.
In contrast, this review of abstinence‐plus programs suggests that numerous abstinence‐plus interventions can have significantly protective effects on multiple sexual risk behaviors when compared to various controls; furthermore, abstinence‐plus programs do not appear to have any adverse effects on behavioral or biological outcomes. Participants appeared to understand the hierarchical message of abstinence‐plus programs, as trials consistently reported significant program effects for HIV prevention knowledge. Importantly, no study observed adverse program effects for the incidence or frequency of sexual activity, suggesting that safer sex promotion did not encourage sex or undermine the abstinence message. Moreover, the promotion of abstinence did not appear to detract from the programs' condom promotion message, as many studies demonstrated protective short‐term and long‐term program effects on condom use.
Given that HIV risk in the US is elevated among low‐income and ethnic minority populations, we originally planned to conduct a priori subgroup analyses based on these characteristics. The lack of a quantitative synthesis made these comparisons difficult. However, a majority of trials discovered protective behavioral and biological program effects among the 29 trials that enrolled primarily ethnic minority participants, the 12 trials that enrolled primarily African‐American participants, and the 18 trials that reported enrolling economically disadvantaged participants. Although this review cannot provide definitive conclusions about the moderating effects of ethnicity or SES, these results suggest that some abstinence‐plus programs may be appropriate, acceptable, and effective for youth at elevated risk due to poverty or minority ethnicity. While a higher prevalence of sexual risk behavior and pregnancy may have facilitated the detection of significant effects in high‐risk groups, these trends might also indicate that abstinence‐plus programs are promising prevention strategies for some underserved youth populations.
Abstinence‐plus interventions are somewhat unique in their hierarchical basis; they promote abstinence as the best strategy, but also promote safer sex behaviors as secondary alternatives. As with other hierarchical interventions (eg the promotion of barrier methods for HIV prevention in women, investigated in Gollub 1996, Gollub 2000, Farr 1996, Fontanet 1998, Miller 2004, and Stein 1999), critics of abstinence‐plus programs have raised concerns over whether the addition of safer‐sex training can "undermine" the core abstinence message. Common questions include whether the hierarchy in abstinence‐plus programs can be understood, whether abstinence‐plus programs can decrease overall sexual risk behaviors, and whether presenting secondary alternatives might adversely affect the rate at which program participants practice abstinent behavior. The results of this review showed that participants of abstinence‐plus programs have consistently significant knowledge gains regarding HIV and its prevention, that some abstinence‐plus programs can decrease sexual risk behaviors overall, and the presentation of secondary alternatives did not adversely affect the rate at which programs participants engage in sexual activity.
Abstinence‐plus programs are currently excluded from a number of abstinence‐based program funding streams due to their explicit promotion of condom use; in light of the combined evidence from our reviews, it may be prudent to reconsider these resource allocation policies.
Summaries for stakeholders Findings in this review may apply to a number of stakeholders. Clinicians may be interested in the findings from Boekeloo 1999 and Danielson 1990, which each evaluated a one‐session intervention delivered by a health provider: Boekeloo 1999 found no significant effects for any outcome except condom use, which improved in the short‐term only. Danielson 1990 found no significant effects on the incidence of vaginal sex.
For educational stakeholders, the ten school‐based trials in this review (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Hernandez 1990, Kirby 1997, Markham 2006, O'Donnell 2002, Weeks 1997, Wright 1997) found no evidence for effects on STI, and no consistent evidence of effects on pregnancy. Behavioral outcomes were more commonly evaluated but inconsistent; six trials found a protective effect on at least one behavioral outcome (Aarons 2000, Coyle 2001, Coyle 2004, Coyle 2006, Markham 2006, O'Donnell 2002). Thus, although some school‐based abstinence‐plus programs have demonstrated protective effects, various others have not. Further investigation is required to understand the contexts and mechanisms behind the protective effects observed.
For families, several evaluations assessed the effects of a family‐based program or involved parents to a high degree (Dancy 2006, DiIorio 2006, DiIorio 2007, Stanton 2000, Wu 2003). Although no trial assessed STI, one found a significant effect on pregnancy (Wu 2003). Three found a protective effect on at least one behavioral outcome, including unprotected sex, condom use, and pregnancy (DiIorio 2006, DiIorio 2007, Wu 2003). Additionally, Weeks 1997 assessed the addition of parent‐child activities to an in‐school curriculum, but found low parental uptake of activities and no protective effects on behavioral outcomes.
Finally, community‐based or after‐school programs that took place outside the family were evaluated in 21 trials (Danella 2000, Ferguson 1998, Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Jemmott 2004, Kennedy 2000a, Kennedy 2000b, McBride 2000a, McBride 2000b, Moberg 1998, Philliber 2001, Sikkema 2005, Smith 1994, St Lawrence 1995a, St Lawrence 1995b, St Lawrence 1999, St Lawrence 2002, Stanton 1996, Villarruel 2006), of which 14 found a protective effect on at least one biological or behavioral outcome (Danella 2000, Ferguson 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Jemmott 2004, McBride 2000a, Philliber 2001, Sikkema 2005, Smith 1994, St Lawrence 1995a, St Lawrence 2002, Stanton 1996, Villarruel 2006). These protective interventions were often able to target specific risk groups, such as African‐American adolescents, low‐income urban youth, substance‐dependent adolescents, incarcerated youth, and youth at exceptionally high risk for pregnancy. It is possible that effects were more detectable among these populations because of less susceptibility to floor effects. Alternately, the specific tailoring of these programs may have made them more effective among their target participant groups. Unclear reporting and the under‐utilization of relevant outcomes made it difficult to assess the effects of contextual and program characteristics across studies; however, the results suggest that a number of community‐based abstinence‐plus programs can affect risk behavior.
Potential biases in the review process This review has a number of strengths. It is the first review to focus exclusively on abstinence‐plus programs for HIV prevention among any participants in high‐income countries. Our review adds to previous assessments of abstinence‐plus programs by virtue of its international scope; pre‐specified, systematic, and highly sensitive search for trial evidence; inclusion of published and unpublished literature; extensive methodological scrutiny of included studies; exclusive focus on behavioral and biological outcomes; pre‐reviewed protocol; independence from external funding; assessment of data on cost, participant satisfaction, and program implementation; and acceptance of only the most rigorous trial evidence (ie data from randomized and quasi‐randomized controlled trials).
However, there were several potential biases in the review process, which stem primarily from our search strategy. Despite our extensive search for unpublished and ongoing trials (which included searching grey literature, hand‐searching conference abstracts, and contacting experts), our review remains vulnerable to publication bias. This review does not include studies indexed after February 2007. Our search for unpublished literature was somewhat hampered by non‐response and the political connotations of terms such as "abstinence‐plus" and "abstinence‐based"; it is possible that additional unpublished evaluations of abstinence‐plus programs exist, but were not called to our attention due to political concerns or varying definitions of these terms. Additionally, our electronic search used an HIV filter, which means that it did not reliably uncover evaluations of abstinence‐plus programs focused exclusively on pregnancy or general STI prevention. Several randomized controlled evaluations of abstinence‐plus pregnancy prevention programs were recovered by cross‐referencing, but we classified these as excluded studies after determining that HIV prevention was not a stated goal. We suggest that users consult the pregnancy prevention literature for further evidence of the effectiveness of abstinence‐plus programs for preventing pregnancy.
While assessing trials for inclusion, it was frequently difficult or impossible to assess the extent to which interventions emphasized abstinence, or how they discussed condom use and/or other safer‐sex strategies. It is possible that we have omitted abstinence‐plus interventions that did not include any terms such as "postpone sex" or "abstain" in their titles or abstracts; key words for these evaluations may have been broad terms such as "sex education," "voluntary counseling," "hierarchical counseling," or "family life education." Including terms with this broad scope in our search strategy would have made the review unfeasible due to the large number of search hits, so we have accepted this as a limitation of the review. We welcome suggestions to correct any errors of omission in future updates.
Beyond the limitations of our search strategy, we were often unable to obtain relevant missing data, including methodological characteristics, clinical characteristics, and outcome data. This led to several systematic gaps in the review, such as the inability to enter a number of trials into RevMan or to assess publication bias. While we thank the trialists who did respond to our queries, data loss and non‐response frequently made it difficult to discover unreported information.
We also had difficulty finding a reliable intra‐class correlation coefficient when computing the design effect for cluster‐randomized trials. After seeking statistical guidance from the Cochrane HIV/AIDS group and a variety of external experts, we ran a sensitivity analysis with a range of possible ICC values and ultimately reported two sets of results for cluster‐randomized trials in Appendix A: one set unadjusted for cluster randomization, and one set with adjustments for clustering. This affected the significance of results for isolated pairwise comparisons in four trials, always in the direction of non‐significance: Dancy 2006 (sexual initiation, knowledge), Moberg 1998 (vaginal sex), Sikkema 2005 (sexual initiation), and Wu 2003 (anal sex).
Perhaps owing to software limitations and lack of access to the original data sets, our re‐analyzed results differed slightly from originally published results in Boekeloo 1999 (incidence of vaginal sex), Dancy 2006 (sexual initiation), Jemmott 1998 (incidence and frequency of unprotected vaginal sex), Jemmott 1999 (frequency of unprotected vaginal sex), Moberg 1998 (sexual initiation), Sikkema 2005 (condom use and sexual initiation), St Lawrence 1995b (incidence of casual sex, incidence of sex with a non‐monogamous partner, knowledge), Villarruel 2006 (incidence of vaginal sex), and Wu 2003 (pregnancy and incidence of vaginal sex). All but three differences were in the direction of non‐significant effects in our re‐analyzed version; re‐analyzed results were significant for incidence of unprotected vaginal sex in the trial by Jemmott 1998, condom use in the trial by Sikkema 2005, and pregnancy in Wu 2003.
We did not use a Bonferroni or other correction to control for multiple statistical tests. The results reported in this paper summarize 571 separate statistical comparisons (not including the second set of tests for cluster‐randomized trials). Of these, 156 tests attained statistical significance at a level of P<0.05 (far more than the 29 tests that may have been expected to attain significance by chance).
Finally, we must acknowledge the potential for bias due to dominant cultural norms: two reviewers (KU and DO) are originally from coastal areas of the United States, while the third (PM) is from the United Kingdom.
To see charts of each trial's effects, please refer to http://www.igh.org/Cochrane/charts.
Authors' conclusions
Implications for practice.
Given the methodological limitations of the evidence, the homogeneity of the trial populations, the under‐utilization of primary outcomes, and the heterogeneity in abstinence‐plus program designs, this review cannot draw unequivocal conclusions about all abstinence‐plus programs in all high‐income countries. We also cannot comment on program effectiveness in participant populations outside adolescents in North America.
Evidence suggests that abstinence‐plus programs do not consistently affect self‐reported STI or pregnancy incidence. However, when compared to a variety of control groups, a number of abstinence‐plus programs had significantly favorable effects on sexual behavior outcomes at short‐term, medium‐term, and long‐term. Consistently protective program effects were observed for the acquisition of HIV/AIDS knowledge at every follow‐up point.
Several program strategies for high‐risk groups appeared to have significantly favorable effects on multiple sexual behaviors, prompting further investigation and potential scale‐up of these interventions.
Where participation satisfaction data were collected, evaluations indicated high levels of abstinence‐plus program acceptability.
Implications for research.
Future research could address the following questions raised by this review:
Direct comparisons between abstinence‐plus programs and other program types (ie abstinence‐only, condom promotion, safer‐sex)
Intervention mechanisms
Program effectiveness among especially vulnerable groups (eg gay, lesbian, bisexual, or transgendered youth; youth with disabilities; recent immigrants; substance‐dependent youth; homeless youth)
Program effectiveness in settings outside North America
Mediating effects of implementation fidelity for existing programs
Effects of strategies to improve the validity of self‐report
Mediating effects of different program strategies, concepts, dosages, theoretical bases, formats, and facilitators. Moderating effects of program setting and participant characteristics.
Some evaluations indicated that different abstinence‐plus intervention strategies can have differential effects on behavior. Additional research is necessary to understand what contexts, populations, and program elements make these effects possible, as well as to clarify the generalizability of these findings.
Future research could consult the following methodological needs:
Improved reporting of key methodological, clinical, and statistical information (eg method of randomization, allocation concealment, procedures for blinding data collectors, numbers of participants per trial arm at follow‐up, attrition analyses, means and standard deviations for continuous outcomes). Use of the CONSORT statement (Moher 2001).
Standardized behavioral outcome measures with consistent follow‐up intervals, recall periods, and clinical meanings. Increased use of HIV, STI, and pregnancy as primary outcomes. Medical evaluation of HIV and STI (especially given recent studies suggesting that this may be acceptable among youth populations [Asbel 2006, Bowden 2005]). Disaggregation of oral, anal, and vaginal sex outcomes.
More complete reporting of implementation data (ie program design, program delivery, participant uptake, and trial context) for intervention and control arms
Analyses that account for dropouts (intention‐to‐treat) and unit of randomization
Correction for multiple statistical tests
Incorporation of cost‐effectiveness and participant satisfaction data
Provision of data sets for IPD (individual patient data) analyses
What's new
| Date | Event | Description |
|---|---|---|
| 28 October 2008 | Amended | Converted to new review format. |
History
Review first published: Issue 1, 2008
| Date | Event | Description |
|---|---|---|
| 13 November 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We thank Nandi Siegfried, Gail Kennedy, Tara Horvath, George Rutherford, and Mike Sweat for providing guidance on our protocol and/or support during the review process. We are grateful to Karishma Busgeeth for helping us to develop our search strategy and for carrying out searches of CENTRAL, PubMed, AIDSLINE, and EMBASE. We also thank the many experts who responded to our queries regarding unpublished and ongoing evaluations, the trialists who responded to our inquiries and sent manuscripts that we could not obtain in the UK, and the statistical experts who provided us with guidance about how to analyze cluster randomized trials. We also thank the Centre for Evidence‐Based Intervention and the Department of Social Policy and Social Work at the University of Oxford for internal support.
Data and analyses
Comparison 1. Boekeloo 1999: A+ vs. Usual Care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 STD diagnosis by doctor or nurse ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 STD diagnosis by doctor or nurse ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Pregnancy ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Pregnancy ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Vaginal Intercourse in past 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Vaginal Intercourse in past 3m ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Vaginal, Oral, or Anal Intercourse in past 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8 Vaginal, Oral, or Anal Intercourse in past 3m ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9 Condom use at last vaginal intercourse ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 10 Condom use at last vaginal intercourse ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected |
1.1. Analysis.
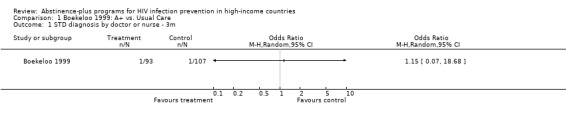
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 1 STD diagnosis by doctor or nurse ‐ 3m.
1.2. Analysis.
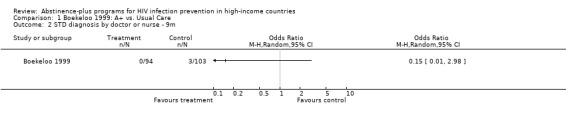
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 2 STD diagnosis by doctor or nurse ‐ 9m.
1.3. Analysis.
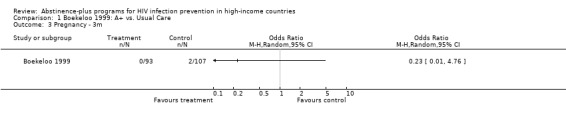
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 3 Pregnancy ‐ 3m.
1.4. Analysis.
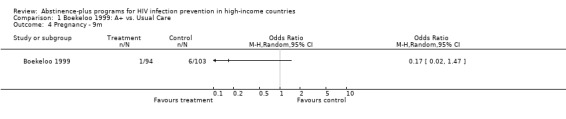
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 4 Pregnancy ‐ 9m.
1.5. Analysis.
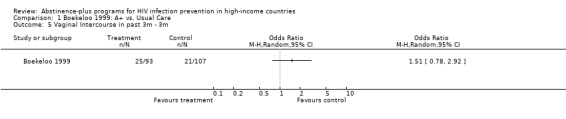
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 5 Vaginal Intercourse in past 3m ‐ 3m.
1.6. Analysis.
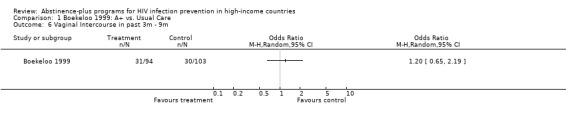
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 6 Vaginal Intercourse in past 3m ‐ 9m.
1.7. Analysis.
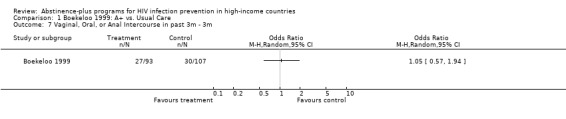
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 7 Vaginal, Oral, or Anal Intercourse in past 3m ‐ 3m.
1.8. Analysis.
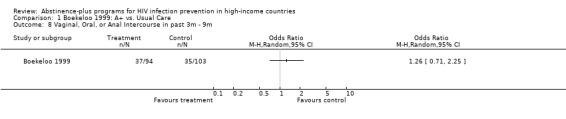
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 8 Vaginal, Oral, or Anal Intercourse in past 3m ‐ 9m.
1.9. Analysis.
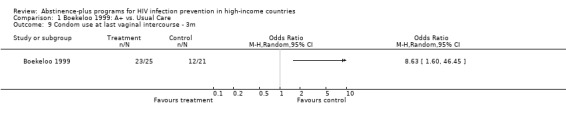
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 9 Condom use at last vaginal intercourse ‐ 3m.
1.10. Analysis.
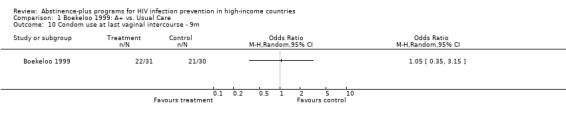
Comparison 1 Boekeloo 1999: A+ vs. Usual Care, Outcome 10 Condom use at last vaginal intercourse ‐ 9m.
Comparison 2. Dancy 2006: A+ Delivered by Mothers vs. A+ Delivered by Health Experts vs. Attention Delivered by Mothers.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Ever had sex ‐ 5m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Mothers vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Experts vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Mothers vs Experts | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Ever had sex ‐ 5m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Mothers vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Experts vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Mothers vs Experts | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Knowledge ‐ 5m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Mothers vs Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Experts vs control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Mothers vs Experts | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Knowledge 5m CLUSTER ADJUSTED | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Mothers vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Experts vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Mothers vs Experts | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
2.1. Analysis.
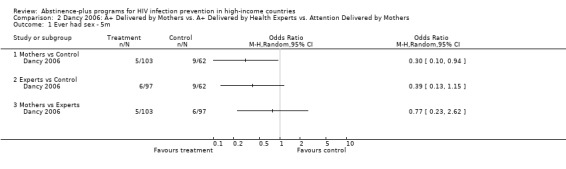
Comparison 2 Dancy 2006: A+ Delivered by Mothers vs. A+ Delivered by Health Experts vs. Attention Delivered by Mothers, Outcome 1 Ever had sex ‐ 5m.
2.2. Analysis.
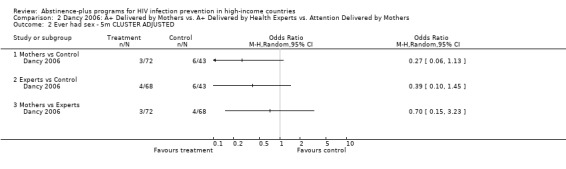
Comparison 2 Dancy 2006: A+ Delivered by Mothers vs. A+ Delivered by Health Experts vs. Attention Delivered by Mothers, Outcome 2 Ever had sex ‐ 5m CLUSTER ADJUSTED.
2.3. Analysis.
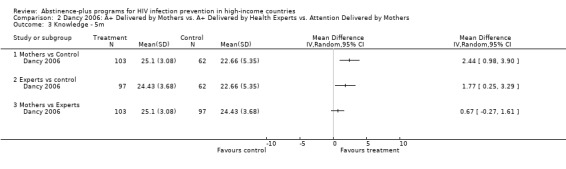
Comparison 2 Dancy 2006: A+ Delivered by Mothers vs. A+ Delivered by Health Experts vs. Attention Delivered by Mothers, Outcome 3 Knowledge ‐ 5m.
2.4. Analysis.
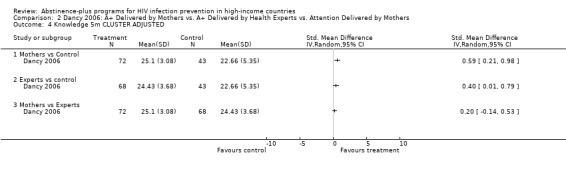
Comparison 2 Dancy 2006: A+ Delivered by Mothers vs. A+ Delivered by Health Experts vs. Attention Delivered by Mothers, Outcome 4 Knowledge 5m CLUSTER ADJUSTED.
Comparison 3. DiIorio 2006: A+ vs. Information.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Condom use at last sex ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 SCT vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 LSK vs control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 SCT vs LSK | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Condom use at last sex ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 SCT vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 LSK vs control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 SCT vs LSK | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Ever had sex ‐ 4m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 SCT vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 LSK vs control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 SCT vs LSK | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Ever had sex ‐ 4m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 SCT vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 LSK vs control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 SCT vs LSK | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Ever had sex ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 SCT vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 LSK vs control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 SCT vs LSK | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Ever had sex ‐ 12m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 SCT vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 LSK vs control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 SCT vs LSK | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Ever had sex ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 SCT vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 LSK vs control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 SCT vs LSK | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Ever had sex ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 SCT vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 LSK vs control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 SCT vs LSK | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
3.1. Analysis.
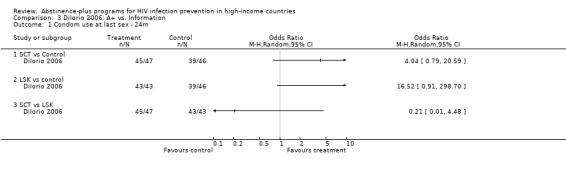
Comparison 3 DiIorio 2006: A+ vs. Information, Outcome 1 Condom use at last sex ‐ 24m.
3.2. Analysis.
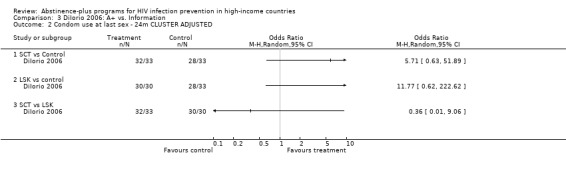
Comparison 3 DiIorio 2006: A+ vs. Information, Outcome 2 Condom use at last sex ‐ 24m CLUSTER ADJUSTED.
3.3. Analysis.
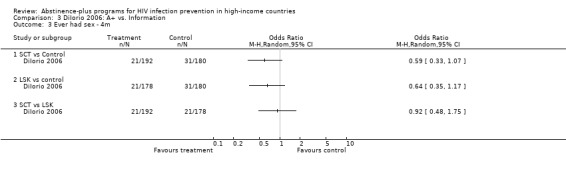
Comparison 3 DiIorio 2006: A+ vs. Information, Outcome 3 Ever had sex ‐ 4m.
3.4. Analysis.
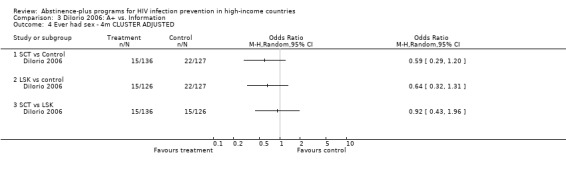
Comparison 3 DiIorio 2006: A+ vs. Information, Outcome 4 Ever had sex ‐ 4m CLUSTER ADJUSTED.
3.5. Analysis.
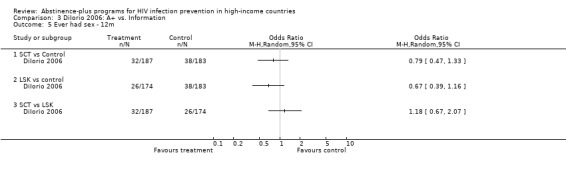
Comparison 3 DiIorio 2006: A+ vs. Information, Outcome 5 Ever had sex ‐ 12m.
3.6. Analysis.
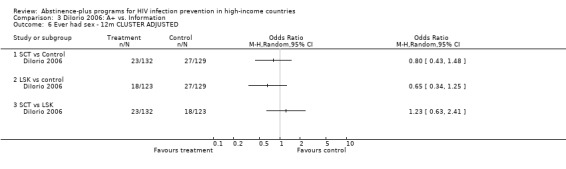
Comparison 3 DiIorio 2006: A+ vs. Information, Outcome 6 Ever had sex ‐ 12m CLUSTER ADJUSTED.
3.7. Analysis.
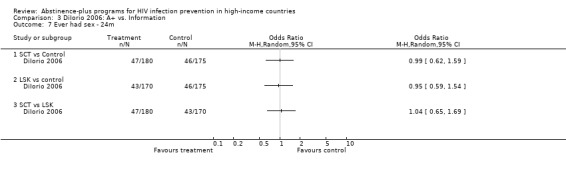
Comparison 3 DiIorio 2006: A+ vs. Information, Outcome 7 Ever had sex ‐ 24m.
3.8. Analysis.
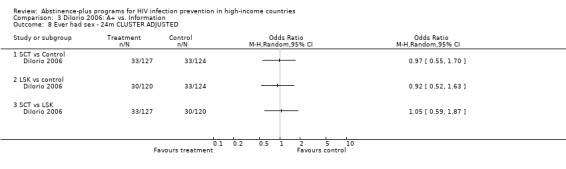
Comparison 3 DiIorio 2006: A+ vs. Information, Outcome 8 Ever had sex ‐ 24m CLUSTER ADJUSTED.
Comparison 4. Ferguson 1998: A+ with Peer Counseling vs. A+ without Peer Counseling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pregnancy ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Recent sex ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Recent sex ‐ 3m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Sex ever ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 All participants | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Sex ever ‐ 3m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 All participants | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
4.1. Analysis.
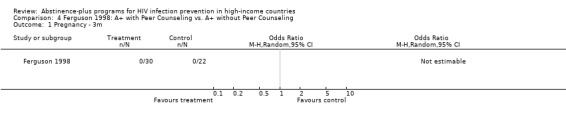
Comparison 4 Ferguson 1998: A+ with Peer Counseling vs. A+ without Peer Counseling, Outcome 1 Pregnancy ‐ 3m.
4.2. Analysis.
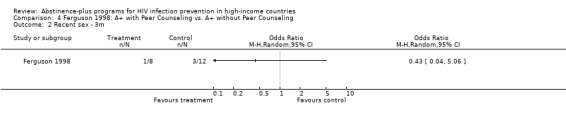
Comparison 4 Ferguson 1998: A+ with Peer Counseling vs. A+ without Peer Counseling, Outcome 2 Recent sex ‐ 3m.
4.3. Analysis.
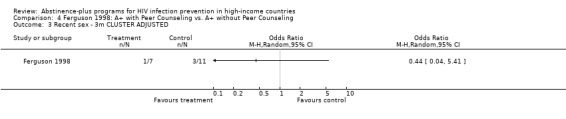
Comparison 4 Ferguson 1998: A+ with Peer Counseling vs. A+ without Peer Counseling, Outcome 3 Recent sex ‐ 3m CLUSTER ADJUSTED.
4.4. Analysis.
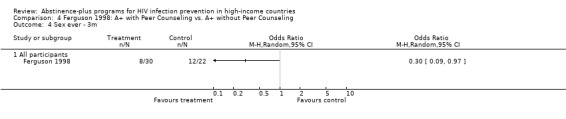
Comparison 4 Ferguson 1998: A+ with Peer Counseling vs. A+ without Peer Counseling, Outcome 4 Sex ever ‐ 3m.
4.5. Analysis.
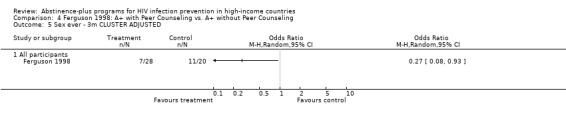
Comparison 4 Ferguson 1998: A+ with Peer Counseling vs. A+ without Peer Counseling, Outcome 5 Sex ever ‐ 3m CLUSTER ADJUSTED.
Comparison 5. Jemmott 1992: A+ vs. Attention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Frequency of unprotected intercourse in past 3m (days) ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Boys | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Sexual intercourse in past 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Boys | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Frequency of intercourse in past 3m (days) ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Boys | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Anal intercourse in past 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Boys | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Frequency of anal intercourse in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Boys | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Number of coital partners in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Boys | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Number of anal sex partners in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Boys | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Rated frequency of condom use in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Boys | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 HIV knowledge ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Boys | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
5.1. Analysis.
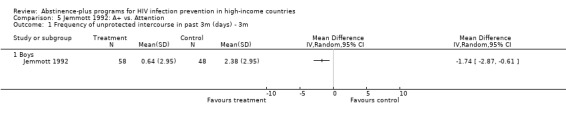
Comparison 5 Jemmott 1992: A+ vs. Attention, Outcome 1 Frequency of unprotected intercourse in past 3m (days) ‐ 3m.
5.2. Analysis.
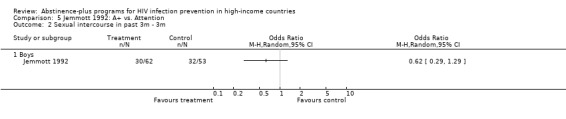
Comparison 5 Jemmott 1992: A+ vs. Attention, Outcome 2 Sexual intercourse in past 3m ‐ 3m.
5.3. Analysis.
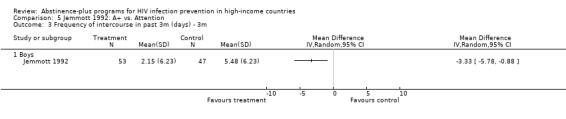
Comparison 5 Jemmott 1992: A+ vs. Attention, Outcome 3 Frequency of intercourse in past 3m (days) ‐ 3m.
5.4. Analysis.
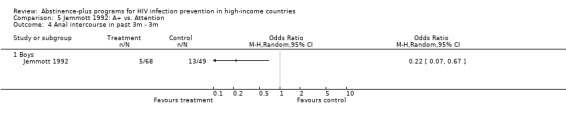
Comparison 5 Jemmott 1992: A+ vs. Attention, Outcome 4 Anal intercourse in past 3m ‐ 3m.
5.5. Analysis.
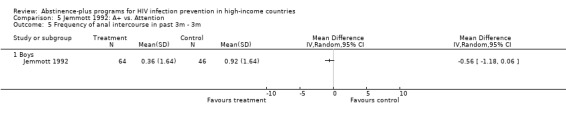
Comparison 5 Jemmott 1992: A+ vs. Attention, Outcome 5 Frequency of anal intercourse in past 3m ‐ 3m.
5.6. Analysis.
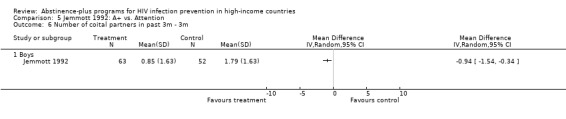
Comparison 5 Jemmott 1992: A+ vs. Attention, Outcome 6 Number of coital partners in past 3m ‐ 3m.
5.7. Analysis.
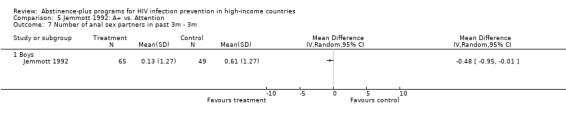
Comparison 5 Jemmott 1992: A+ vs. Attention, Outcome 7 Number of anal sex partners in past 3m ‐ 3m.
5.8. Analysis.
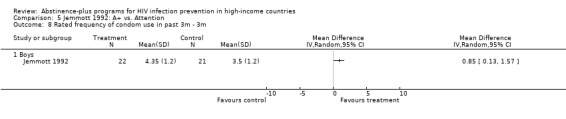
Comparison 5 Jemmott 1992: A+ vs. Attention, Outcome 8 Rated frequency of condom use in past 3m ‐ 3m.
5.9. Analysis.
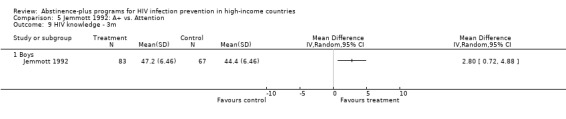
Comparison 5 Jemmott 1992: A+ vs. Attention, Outcome 9 HIV knowledge ‐ 3m.
Comparison 6. Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unprotected sex in past 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Unprotected sex in past 3m ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Unprotected sex in past 3m ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Unprotected sex in past 3m among sexually experienced ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Unprotected sex in past 3m among sexually experienced ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Unprotected sex in past 3m among sexually experienced ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 Condom v Abstinence | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Unprotected sex in past 3m among sexually inexperienced ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Unprotected sex in past 3m among sexually inexperienced ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Unprotected sex in past 3m among sexually inexperienced ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Frequency of unprotected sex in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Frequency of unprotected sex in past 3m ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Frequency of unprotected sex in past 3m ‐ 12m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Frequency of unprotected sex in past 3m among sexually experienced ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Frequency of unprotected sex in past 3m among sexually experienced ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Frequency of unprotected sex in past 3m among sexually experienced ‐ 12m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.4 Condom v. Abstinence | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Frequency of unprotected sex in past 3m among sexually inexperienced ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Frequency of unprotected sex in past 3m among sexually inexperienced ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 17.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Frequency of unprotected sex in past 3m among sexually inexperienced ‐ 12m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Sex in past 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 19.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Sex in past 3m ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 20.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 Sex in past 3m ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 21.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 Sex in past 3m among sexually experienced ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 22.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 22.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 23 Sex in past 3m among sexually inexperienced ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 23.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Frequency of intercourse in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 24.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 Frequency of intercourse in past 3m ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 25.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 Frequency of intercourse in past 3m ‐ 12m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 26.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 Frequency of intercourse in past 3m among sexually experienced ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 27.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 28 Frequency of intercourse in past 3m among sexually experienced ‐ 12m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 28.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 28.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 28.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 29 Frequency of intercourse in past 3m among sexually inexperienced ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 29.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 29.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 29.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 30 Frequency of intercourse in past 3m among sexually inexperienced ‐ 12m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 30.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 30.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 30.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 31 Consistent condom use in past 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 31.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 31.4 Condom v Abstinence | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 32 Consistent condom use in past 3m ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 32.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 32.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 32.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 33 Consistent condom use in past 3m ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 33.1 Abstinence v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 33.2 Condom v Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 33.3 Abstinence v Condom | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 34 Frequency of condom use in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 34.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 34.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 34.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 35 Frequency of condom use in past 3m ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 35.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 35.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 35.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 36 Frequency of condom use in past 3m ‐ 12m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 36.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 36.2 Condom v Abstinence | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 36.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 37 HIV knowledge at immediate post‐intervention ‐ 12m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 37.1 Abstinence v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 37.2 Condom v Control | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 37.3 Abstinence v Condom | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
6.1. Analysis.
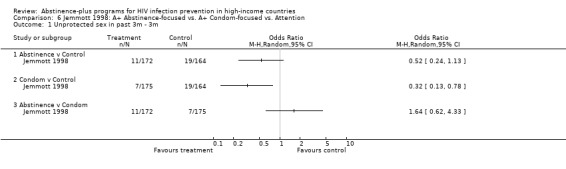
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 1 Unprotected sex in past 3m ‐ 3m.
6.2. Analysis.
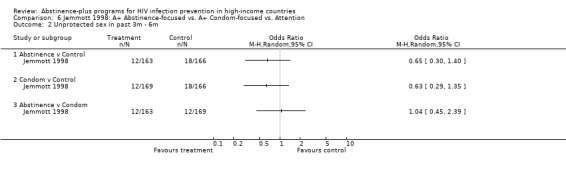
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 2 Unprotected sex in past 3m ‐ 6m.
6.3. Analysis.
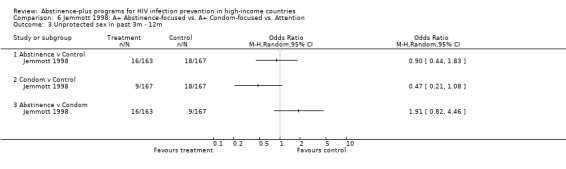
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 3 Unprotected sex in past 3m ‐ 12m.
6.4. Analysis.
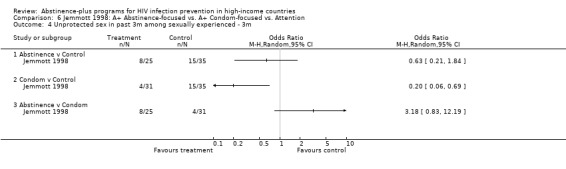
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 4 Unprotected sex in past 3m among sexually experienced ‐ 3m.
6.5. Analysis.
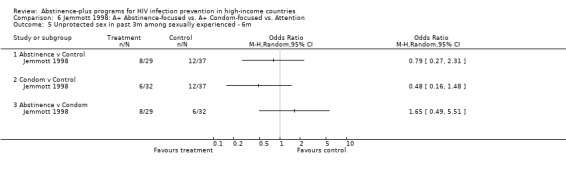
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 5 Unprotected sex in past 3m among sexually experienced ‐ 6m.
6.6. Analysis.
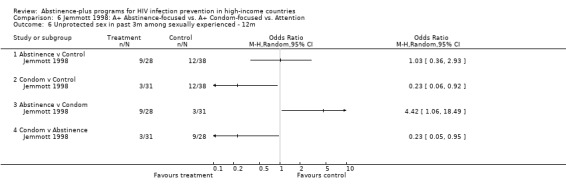
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 6 Unprotected sex in past 3m among sexually experienced ‐ 12m.
6.7. Analysis.
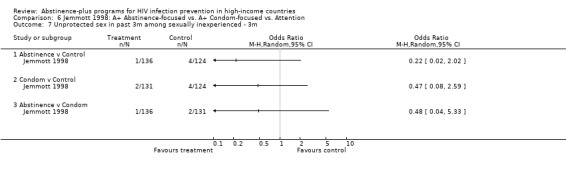
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 7 Unprotected sex in past 3m among sexually inexperienced ‐ 3m.
6.8. Analysis.
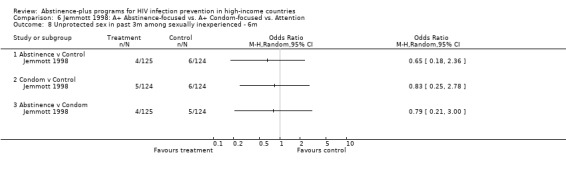
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 8 Unprotected sex in past 3m among sexually inexperienced ‐ 6m.
6.9. Analysis.
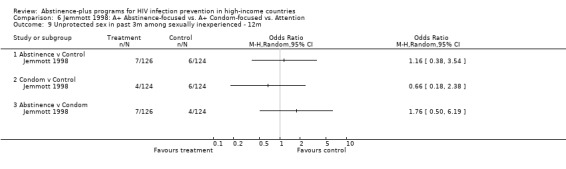
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 9 Unprotected sex in past 3m among sexually inexperienced ‐ 12m.
6.10. Analysis.
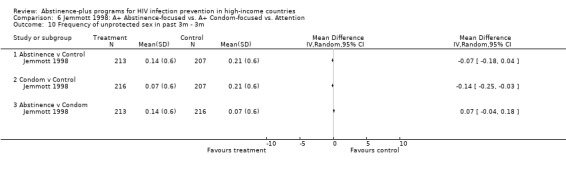
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 10 Frequency of unprotected sex in past 3m ‐ 3m.
6.11. Analysis.
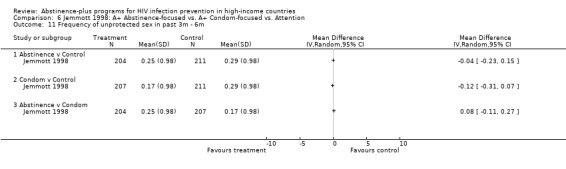
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 11 Frequency of unprotected sex in past 3m ‐ 6m.
6.12. Analysis.
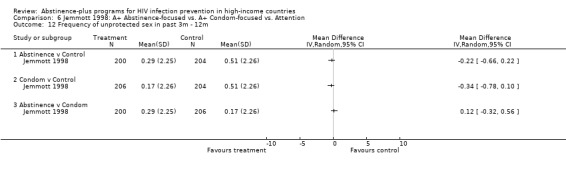
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 12 Frequency of unprotected sex in past 3m ‐ 12m.
6.13. Analysis.
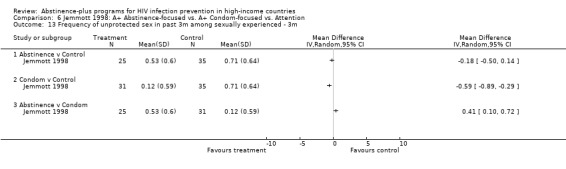
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 13 Frequency of unprotected sex in past 3m among sexually experienced ‐ 3m.
6.14. Analysis.
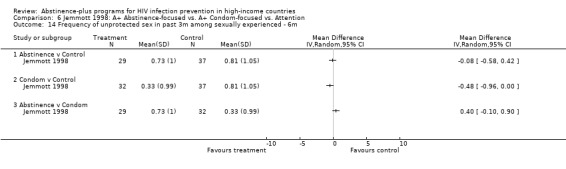
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 14 Frequency of unprotected sex in past 3m among sexually experienced ‐ 6m.
6.15. Analysis.
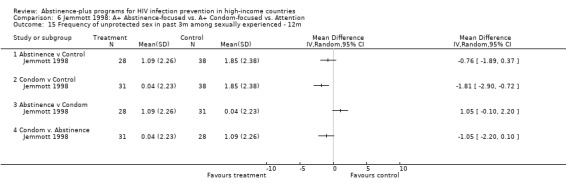
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 15 Frequency of unprotected sex in past 3m among sexually experienced ‐ 12m.
6.16. Analysis.
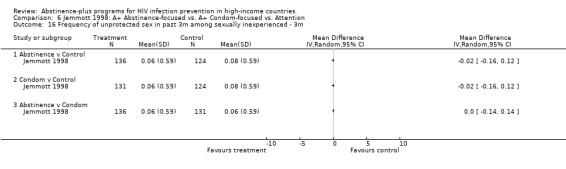
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 16 Frequency of unprotected sex in past 3m among sexually inexperienced ‐ 3m.
6.17. Analysis.
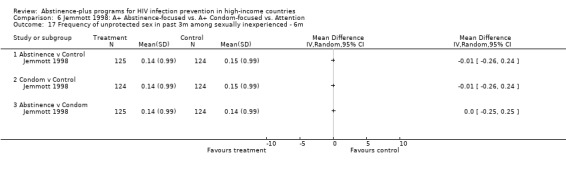
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 17 Frequency of unprotected sex in past 3m among sexually inexperienced ‐ 6m.
6.18. Analysis.
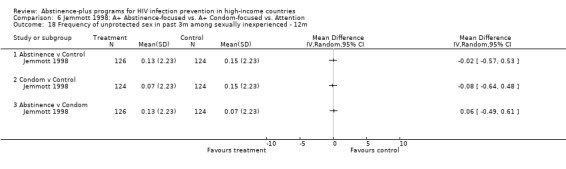
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 18 Frequency of unprotected sex in past 3m among sexually inexperienced ‐ 12m.
6.19. Analysis.
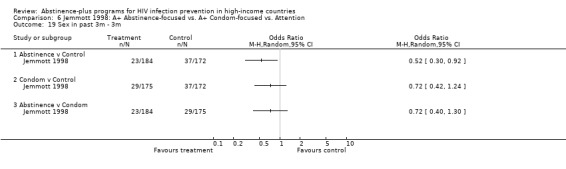
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 19 Sex in past 3m ‐ 3m.
6.20. Analysis.
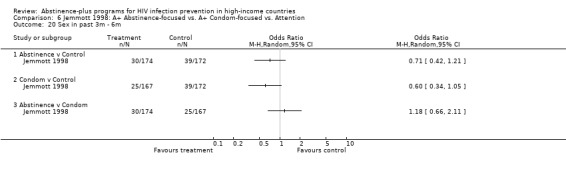
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 20 Sex in past 3m ‐ 6m.
6.21. Analysis.
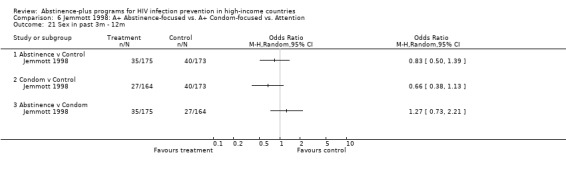
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 21 Sex in past 3m ‐ 12m.
6.22. Analysis.
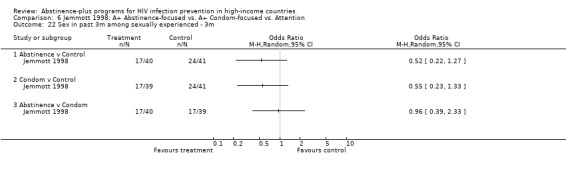
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 22 Sex in past 3m among sexually experienced ‐ 3m.
6.23. Analysis.
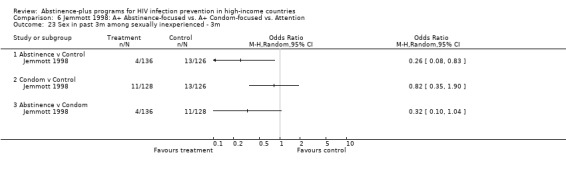
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 23 Sex in past 3m among sexually inexperienced ‐ 3m.
6.24. Analysis.
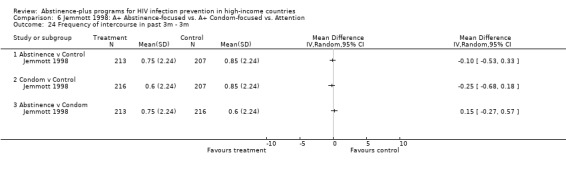
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 24 Frequency of intercourse in past 3m ‐ 3m.
6.25. Analysis.
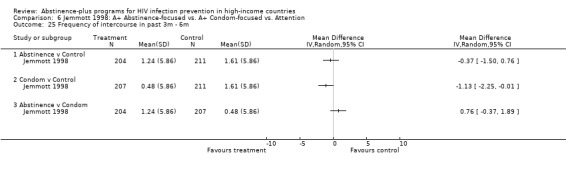
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 25 Frequency of intercourse in past 3m ‐ 6m.
6.26. Analysis.
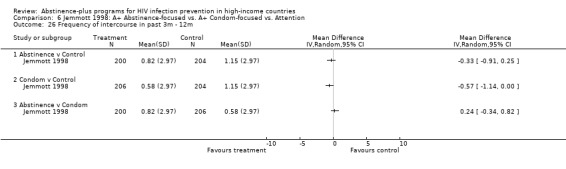
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 26 Frequency of intercourse in past 3m ‐ 12m.
6.27. Analysis.
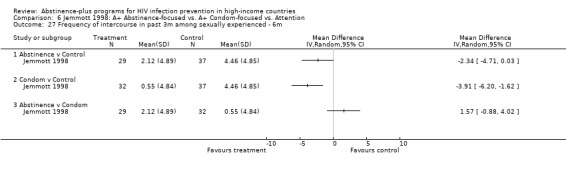
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 27 Frequency of intercourse in past 3m among sexually experienced ‐ 6m.
6.28. Analysis.
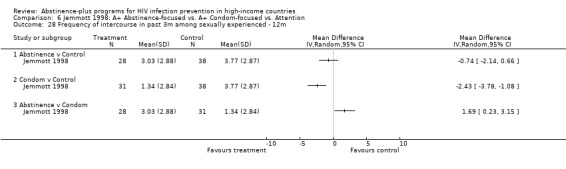
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 28 Frequency of intercourse in past 3m among sexually experienced ‐ 12m.
6.29. Analysis.
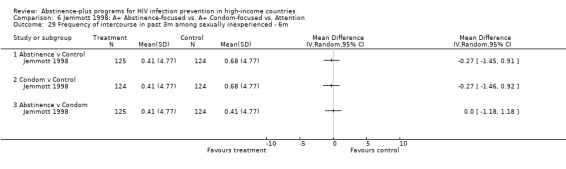
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 29 Frequency of intercourse in past 3m among sexually inexperienced ‐ 6m.
6.30. Analysis.
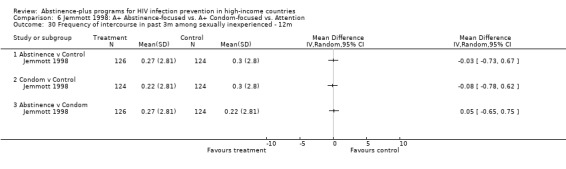
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 30 Frequency of intercourse in past 3m among sexually inexperienced ‐ 12m.
6.31. Analysis.
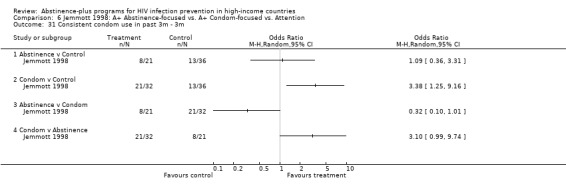
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 31 Consistent condom use in past 3m ‐ 3m.
6.32. Analysis.
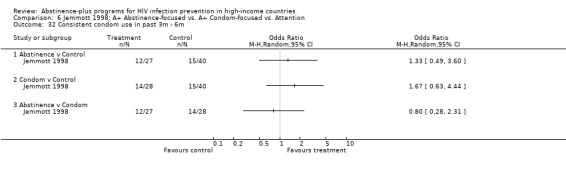
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 32 Consistent condom use in past 3m ‐ 6m.
6.33. Analysis.
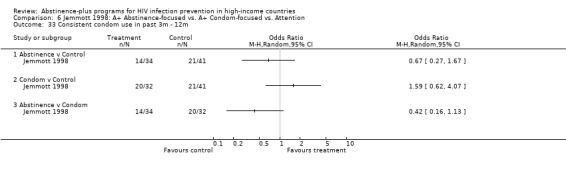
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 33 Consistent condom use in past 3m ‐ 12m.
6.34. Analysis.
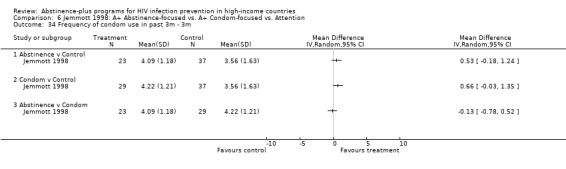
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 34 Frequency of condom use in past 3m ‐ 3m.
6.35. Analysis.
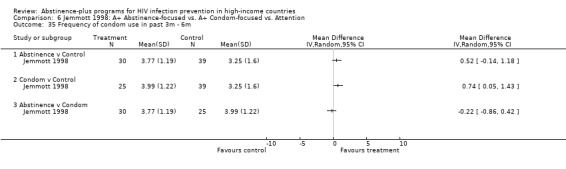
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 35 Frequency of condom use in past 3m ‐ 6m.
6.36. Analysis.
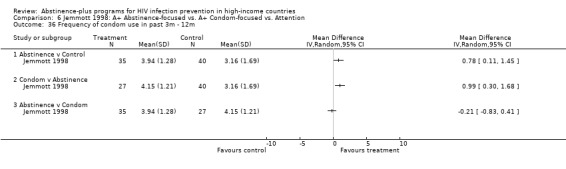
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 36 Frequency of condom use in past 3m ‐ 12m.
6.37. Analysis.
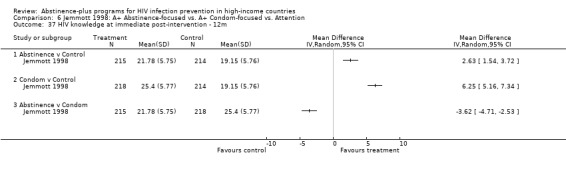
Comparison 6 Jemmott 1998: A+ Abstinence‐focused vs. A+ Condom‐focused vs. Attention, Outcome 37 HIV knowledge at immediate post‐intervention ‐ 12m.
Comparison 7. Jemmott 1999: A+ vs. Attention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Frequency of unprotected intercourse in past 3m (days) ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Frequency of unprotected intercourse in past 3m (days) ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Sexual intercourse in past 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Sexual intercourse in past 3m ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Anal intercourse in past 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Anal intercourse in past 3m ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Frequency of anal intercourse in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8 Frequency of anal intercourse in past 3m ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9 Number of coital partners in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10 Number of coital partners in past 3m ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11 Number of anal intercourse partners in past 3m ‐ 3m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12 Number of anal intercourse partners in past 3m ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
7.1. Analysis.
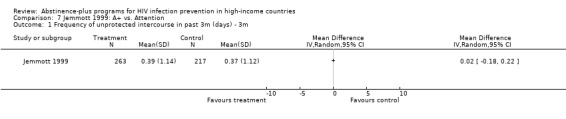
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 1 Frequency of unprotected intercourse in past 3m (days) ‐ 3m.
7.2. Analysis.
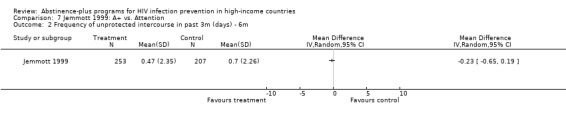
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 2 Frequency of unprotected intercourse in past 3m (days) ‐ 6m.
7.3. Analysis.
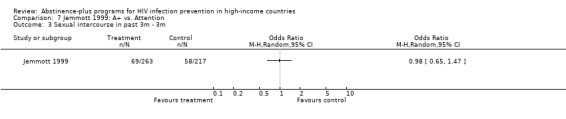
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 3 Sexual intercourse in past 3m ‐ 3m.
7.4. Analysis.
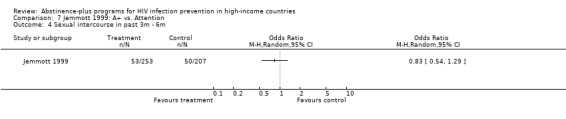
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 4 Sexual intercourse in past 3m ‐ 6m.
7.5. Analysis.
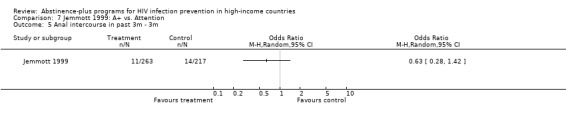
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 5 Anal intercourse in past 3m ‐ 3m.
7.6. Analysis.
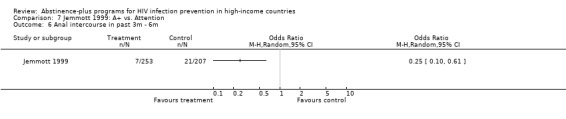
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 6 Anal intercourse in past 3m ‐ 6m.
7.7. Analysis.
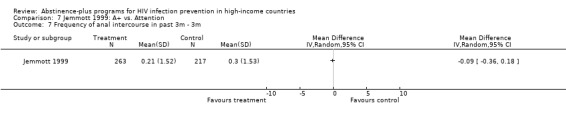
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 7 Frequency of anal intercourse in past 3m ‐ 3m.
7.8. Analysis.
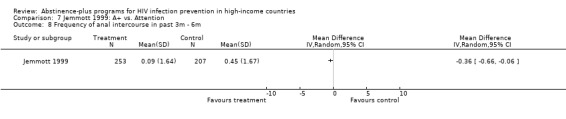
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 8 Frequency of anal intercourse in past 3m ‐ 6m.
7.9. Analysis.
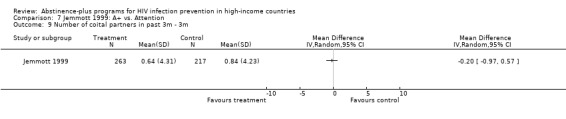
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 9 Number of coital partners in past 3m ‐ 3m.
7.10. Analysis.
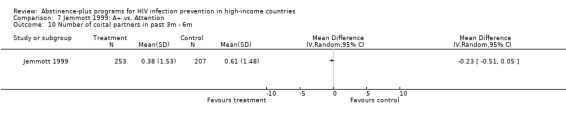
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 10 Number of coital partners in past 3m ‐ 6m.
7.11. Analysis.
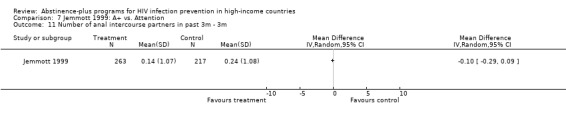
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 11 Number of anal intercourse partners in past 3m ‐ 3m.
7.12. Analysis.
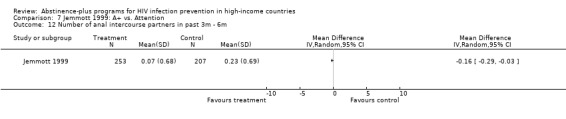
Comparison 7 Jemmott 1999: A+ vs. Attention, Outcome 12 Number of anal intercourse partners in past 3m ‐ 6m.
Comparison 8. Kirby 1997: A+ vs. Usual Care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 STD diagnosis ‐ 5m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 STD diagnosis ‐ 5m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 STD diagnosis ‐ 17m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 STD diagnosis ‐ 17m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Pregnancy ‐ 5m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Pregnancy ‐ 5m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Pregnancy ‐ 17m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8 Pregnancy ‐ 17m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9 Condom use at last sex ‐ 5m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 10 Condom use at last sex ‐ 5m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 11 Condom use at last sex ‐ 17m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 12 Condom use at last sex ‐ 17m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 13 Sexual initiation ‐ 5m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 14 Sexual initiation ‐ 5m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 15 Sexual initiation ‐ 17m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 16 Sexual initiation ‐ 17m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected |
8.1. Analysis.
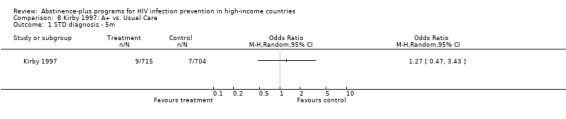
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 1 STD diagnosis ‐ 5m.
8.2. Analysis.
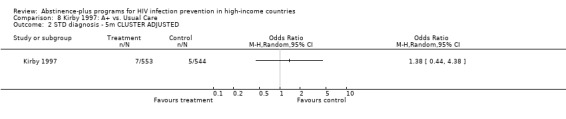
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 2 STD diagnosis ‐ 5m CLUSTER ADJUSTED.
8.3. Analysis.
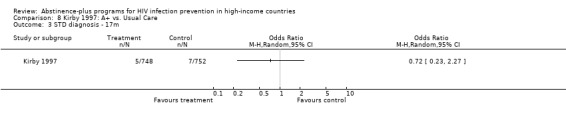
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 3 STD diagnosis ‐ 17m.
8.4. Analysis.
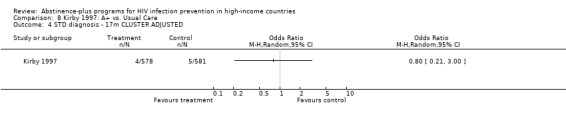
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 4 STD diagnosis ‐ 17m CLUSTER ADJUSTED.
8.5. Analysis.
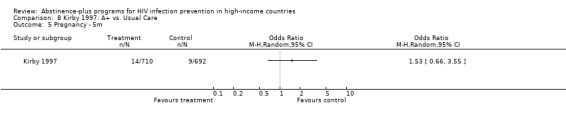
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 5 Pregnancy ‐ 5m.
8.6. Analysis.
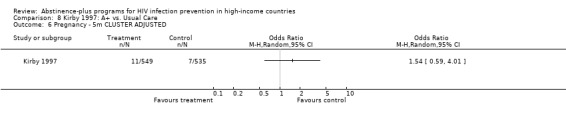
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 6 Pregnancy ‐ 5m CLUSTER ADJUSTED.
8.7. Analysis.
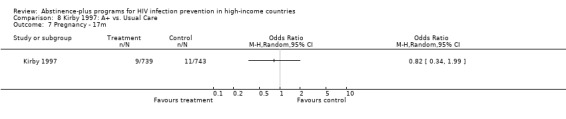
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 7 Pregnancy ‐ 17m.
8.8. Analysis.
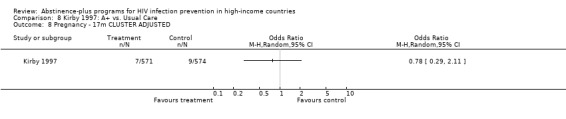
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 8 Pregnancy ‐ 17m CLUSTER ADJUSTED.
8.9. Analysis.
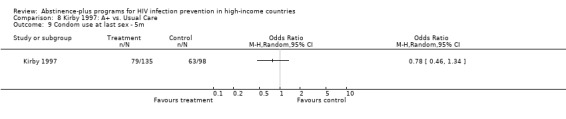
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 9 Condom use at last sex ‐ 5m.
8.10. Analysis.
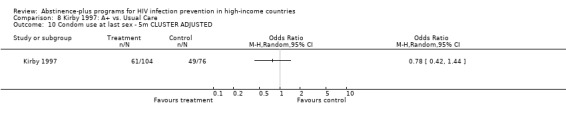
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 10 Condom use at last sex ‐ 5m CLUSTER ADJUSTED.
8.11. Analysis.
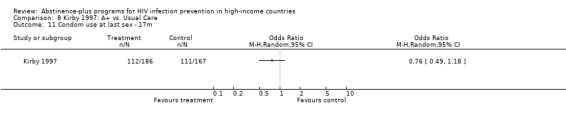
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 11 Condom use at last sex ‐ 17m.
8.12. Analysis.
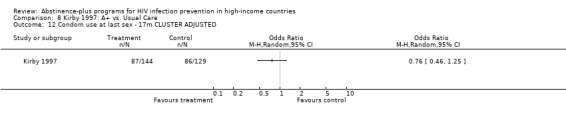
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 12 Condom use at last sex ‐ 17m CLUSTER ADJUSTED.
8.13. Analysis.
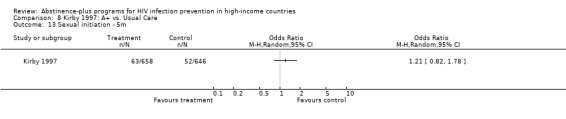
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 13 Sexual initiation ‐ 5m.
8.14. Analysis.
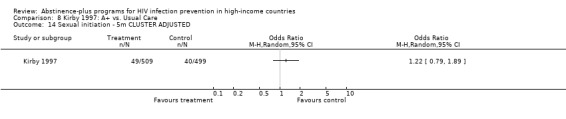
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 14 Sexual initiation ‐ 5m CLUSTER ADJUSTED.
8.15. Analysis.
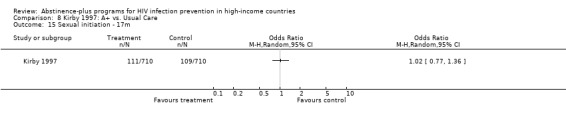
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 15 Sexual initiation ‐ 17m.
8.16. Analysis.
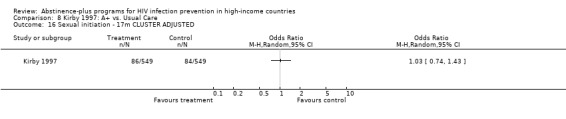
Comparison 8 Kirby 1997: A+ vs. Usual Care, Outcome 16 Sexual initiation ‐ 17m CLUSTER ADJUSTED.
Comparison 9. McBride 2000a: A+ vs. No Treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intercourse in past month ‐ 8m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Girls | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Intercourse ever ‐ 8m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Girls | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
9.1. Analysis.
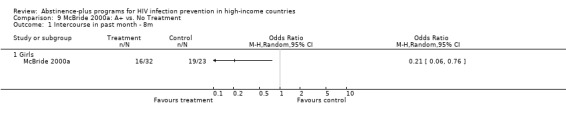
Comparison 9 McBride 2000a: A+ vs. No Treatment, Outcome 1 Intercourse in past month ‐ 8m.
9.2. Analysis.
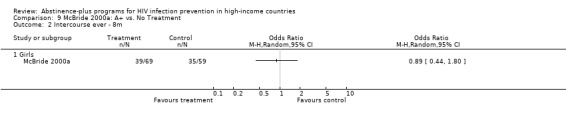
Comparison 9 McBride 2000a: A+ vs. No Treatment, Outcome 2 Intercourse ever ‐ 8m.
Comparison 10. McBride 2000b: A+ vs. No Treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intercourse in past month ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Girls | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Intercourse ever ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Girls | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
10.1. Analysis.
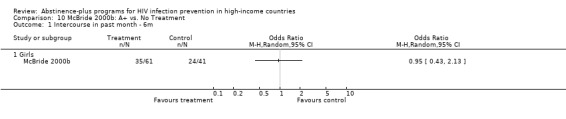
Comparison 10 McBride 2000b: A+ vs. No Treatment, Outcome 1 Intercourse in past month ‐ 6m.
10.2. Analysis.
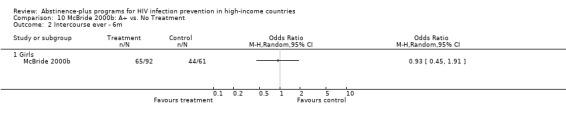
Comparison 10 McBride 2000b: A+ vs. No Treatment, Outcome 2 Intercourse ever ‐ 6m.
Comparison 11. Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recent sex ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Recent sex ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Recent sex ‐ 36m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Recent sex ‐ 36m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Recent sex ‐ 48m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Recent sex ‐ 48m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Consistent condom use ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Consistent condom use ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Consistent condom use ‐ 36m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Consistent condom use ‐ 36m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 10.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Consistent condom use ‐ 48m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 11.1 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Consistent condom use ‐ 48m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 12.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Ever had sex ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 13.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Ever had sex ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 14.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Ever had sex ‐ 36m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 15.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Ever had sex ‐ 36m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 16.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Ever had sex ‐ 48m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 17.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Ever had sex ‐ 48m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 18.1 Intensive vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Age‐Appropriate vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.3 Intensive vs Age‐Appropriate | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
11.1. Analysis.
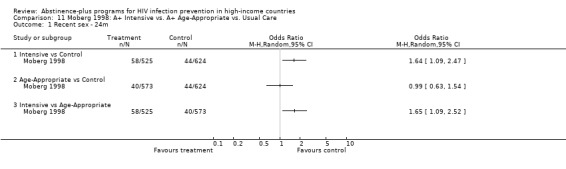
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 1 Recent sex ‐ 24m.
11.2. Analysis.
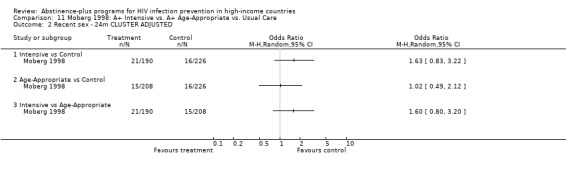
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 2 Recent sex ‐ 24m CLUSTER ADJUSTED.
11.3. Analysis.
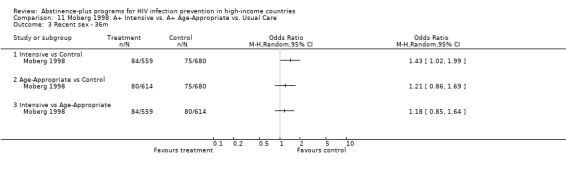
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 3 Recent sex ‐ 36m.
11.4. Analysis.
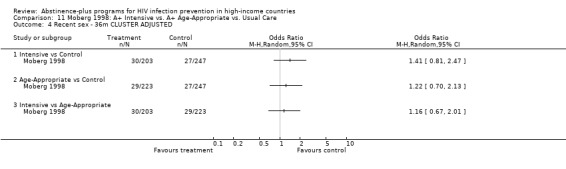
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 4 Recent sex ‐ 36m CLUSTER ADJUSTED.
11.5. Analysis.
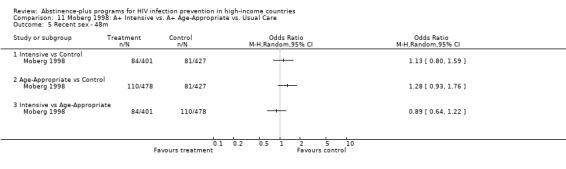
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 5 Recent sex ‐ 48m.
11.6. Analysis.
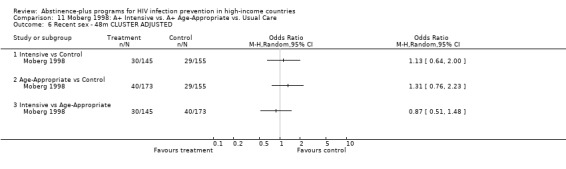
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 6 Recent sex ‐ 48m CLUSTER ADJUSTED.
11.7. Analysis.
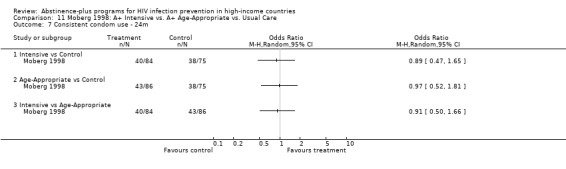
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 7 Consistent condom use ‐ 24m.
11.8. Analysis.
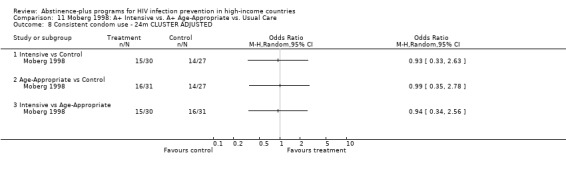
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 8 Consistent condom use ‐ 24m CLUSTER ADJUSTED.
11.9. Analysis.
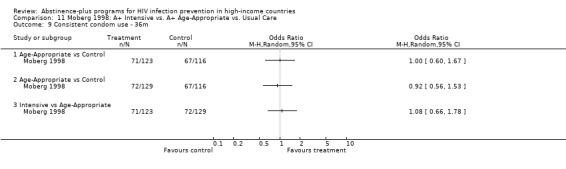
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 9 Consistent condom use ‐ 36m.
11.10. Analysis.
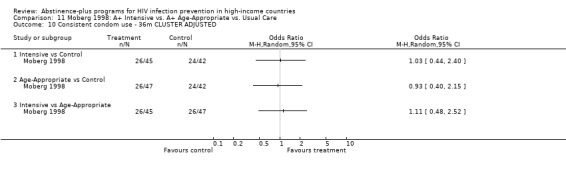
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 10 Consistent condom use ‐ 36m CLUSTER ADJUSTED.
11.11. Analysis.
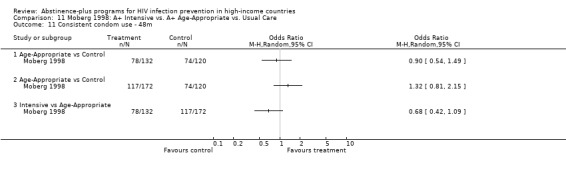
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 11 Consistent condom use ‐ 48m.
11.12. Analysis.
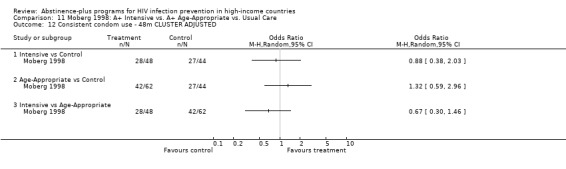
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 12 Consistent condom use ‐ 48m CLUSTER ADJUSTED.
11.13. Analysis.
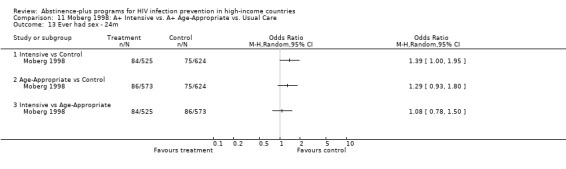
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 13 Ever had sex ‐ 24m.
11.14. Analysis.
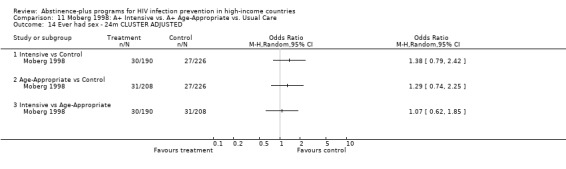
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 14 Ever had sex ‐ 24m CLUSTER ADJUSTED.
11.15. Analysis.
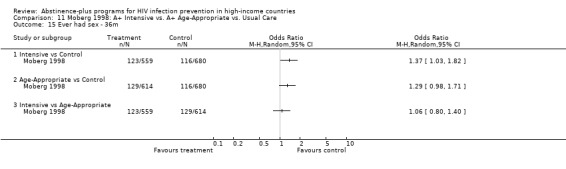
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 15 Ever had sex ‐ 36m.
11.16. Analysis.
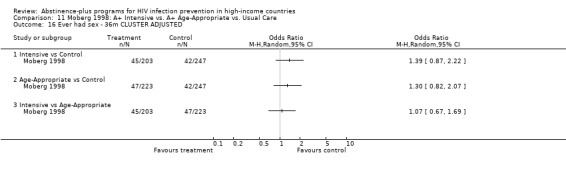
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 16 Ever had sex ‐ 36m CLUSTER ADJUSTED.
11.17. Analysis.
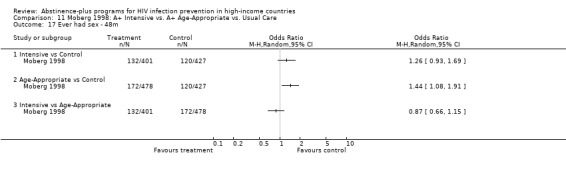
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 17 Ever had sex ‐ 48m.
11.18. Analysis.
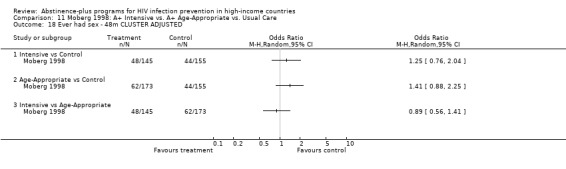
Comparison 11 Moberg 1998: A+ Intensive vs. A+ Age‐Appropriate vs. Usual Care, Outcome 18 Ever had sex ‐ 48m CLUSTER ADJUSTED.
Comparison 12. Philliber 2001: A+ vs. Usual Care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pregnancy ‐ 36m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 All participants | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Girls | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Boys | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Ever had vaginal sex ‐ 36m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 All participants | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Girls | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Boys | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Condom use at last sex among sexually experienced ‐ 36m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 All participants | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Girls | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Boys | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
12.1. Analysis.
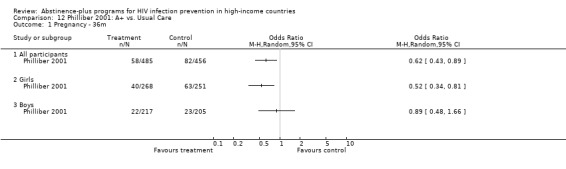
Comparison 12 Philliber 2001: A+ vs. Usual Care, Outcome 1 Pregnancy ‐ 36m.
12.2. Analysis.
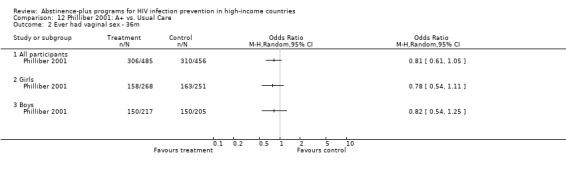
Comparison 12 Philliber 2001: A+ vs. Usual Care, Outcome 2 Ever had vaginal sex ‐ 36m.
12.3. Analysis.
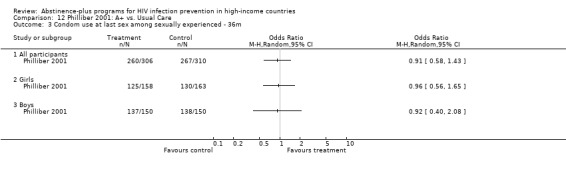
Comparison 12 Philliber 2001: A+ vs. Usual Care, Outcome 3 Condom use at last sex among sexually experienced ‐ 36m.
Comparison 13. Sikkema 2005: A+ Workshops and Community Involvement vs. A+ Workshops Only vs. Information.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Condom use among those ever having sex ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Workshop vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Community vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Workshop vs Community | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Condom use among those ever having sex ‐ 9m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Workshop vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Community vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Workshop vs Community | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Condom use among those ever having sex ‐ 18m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Workshop vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Community vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Workshop vs Community | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Condom use among those ever having sex ‐ 18m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Workshop vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Community vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Workshop vs Community | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Ever had sex among baseline virgins ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 Workshop vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Community vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Workshop vs Community | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Ever had sex among baseline virgins ‐ 9m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Workshop vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Community vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Workshop vs Community | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Ever had sex among baseline virgins ‐ 18m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Workshop vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Community vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Workshop vs Community | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Ever had sex among baseline virgins ‐ 18m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Workshop vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Community vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Workshop vs Community | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
13.1. Analysis.
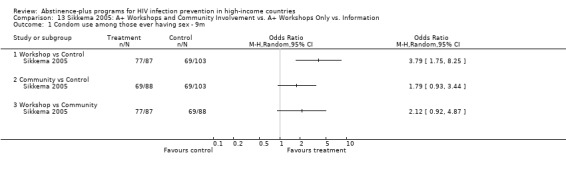
Comparison 13 Sikkema 2005: A+ Workshops and Community Involvement vs. A+ Workshops Only vs. Information, Outcome 1 Condom use among those ever having sex ‐ 9m.
13.2. Analysis.
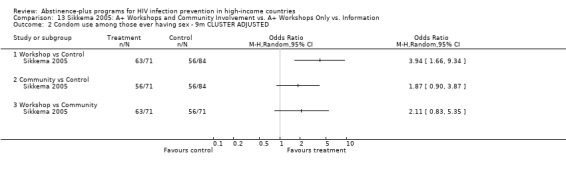
Comparison 13 Sikkema 2005: A+ Workshops and Community Involvement vs. A+ Workshops Only vs. Information, Outcome 2 Condom use among those ever having sex ‐ 9m CLUSTER ADJUSTED.
13.3. Analysis.
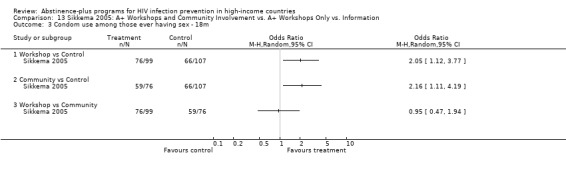
Comparison 13 Sikkema 2005: A+ Workshops and Community Involvement vs. A+ Workshops Only vs. Information, Outcome 3 Condom use among those ever having sex ‐ 18m.
13.4. Analysis.
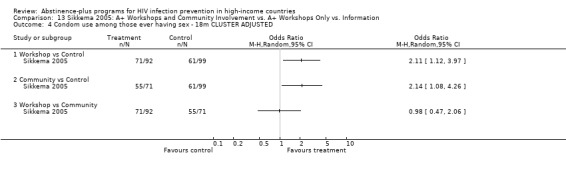
Comparison 13 Sikkema 2005: A+ Workshops and Community Involvement vs. A+ Workshops Only vs. Information, Outcome 4 Condom use among those ever having sex ‐ 18m CLUSTER ADJUSTED.
13.5. Analysis.
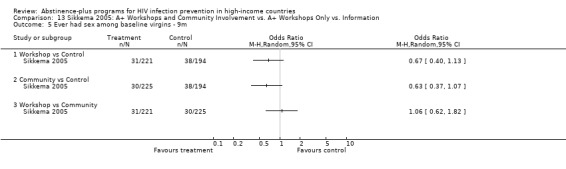
Comparison 13 Sikkema 2005: A+ Workshops and Community Involvement vs. A+ Workshops Only vs. Information, Outcome 5 Ever had sex among baseline virgins ‐ 9m.
13.6. Analysis.
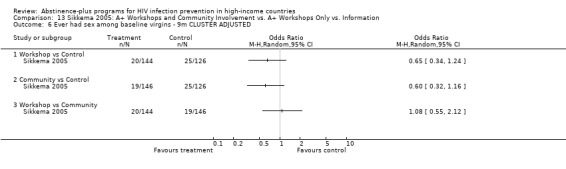
Comparison 13 Sikkema 2005: A+ Workshops and Community Involvement vs. A+ Workshops Only vs. Information, Outcome 6 Ever had sex among baseline virgins ‐ 9m CLUSTER ADJUSTED.
13.7. Analysis.
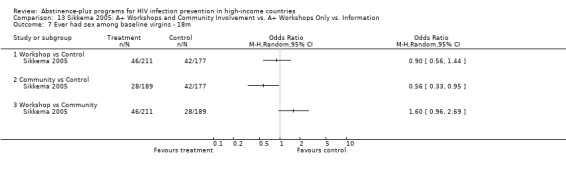
Comparison 13 Sikkema 2005: A+ Workshops and Community Involvement vs. A+ Workshops Only vs. Information, Outcome 7 Ever had sex among baseline virgins ‐ 18m.
13.8. Analysis.
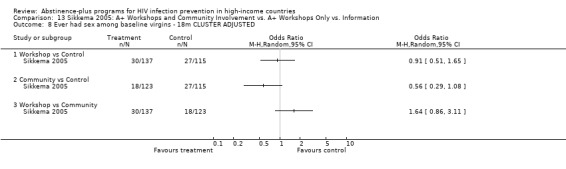
Comparison 13 Sikkema 2005: A+ Workshops and Community Involvement vs. A+ Workshops Only vs. Information, Outcome 8 Ever had sex among baseline virgins ‐ 18m CLUSTER ADJUSTED.
Comparison 14. Smith 1994: A+ vs. Information.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Absolute sexual frequency ‐ 6m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
14.1. Analysis.
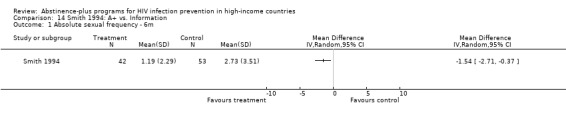
Comparison 14 Smith 1994: A+ vs. Information, Outcome 1 Absolute sexual frequency ‐ 6m.
Comparison 15. St Lawrence 1995b: A+ with Skills Training vs. A+ without Skills Training.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 STI treatment in past 2m ‐ 3.5m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 STI treatment in past 2m ‐ 3.5m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Casual sex in past 2m ‐ 3.5m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Casual sex in past 2m ‐ 3.5m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Sex with non‐monogamous partner in past 2m ‐ 3.5m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Sex with non‐monogamous partner in past 2m ‐ 3.5m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 HIV knowledge ‐ 3.5m | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8 HIV knowledge ‐ 3.5m CLUSTER ADJUSTED | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
15.1. Analysis.
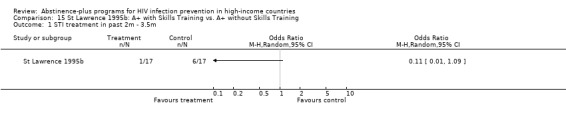
Comparison 15 St Lawrence 1995b: A+ with Skills Training vs. A+ without Skills Training, Outcome 1 STI treatment in past 2m ‐ 3.5m.
15.2. Analysis.
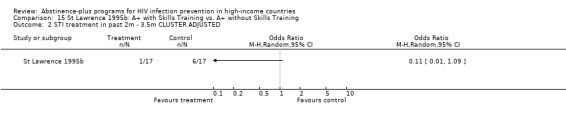
Comparison 15 St Lawrence 1995b: A+ with Skills Training vs. A+ without Skills Training, Outcome 2 STI treatment in past 2m ‐ 3.5m CLUSTER ADJUSTED.
15.3. Analysis.
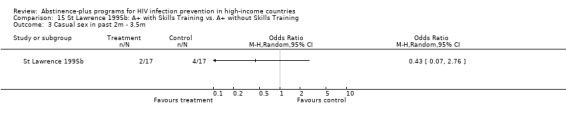
Comparison 15 St Lawrence 1995b: A+ with Skills Training vs. A+ without Skills Training, Outcome 3 Casual sex in past 2m ‐ 3.5m.
15.4. Analysis.
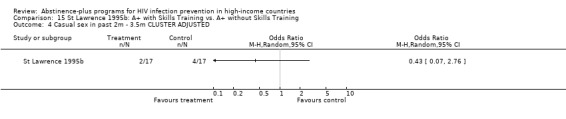
Comparison 15 St Lawrence 1995b: A+ with Skills Training vs. A+ without Skills Training, Outcome 4 Casual sex in past 2m ‐ 3.5m CLUSTER ADJUSTED.
15.5. Analysis.
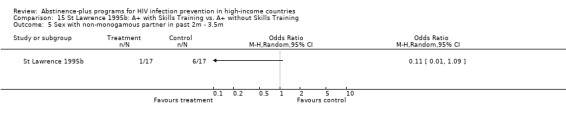
Comparison 15 St Lawrence 1995b: A+ with Skills Training vs. A+ without Skills Training, Outcome 5 Sex with non‐monogamous partner in past 2m ‐ 3.5m.
15.6. Analysis.
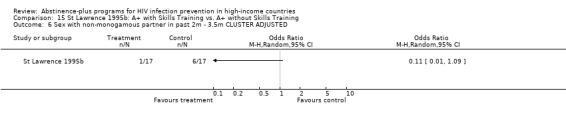
Comparison 15 St Lawrence 1995b: A+ with Skills Training vs. A+ without Skills Training, Outcome 6 Sex with non‐monogamous partner in past 2m ‐ 3.5m CLUSTER ADJUSTED.
15.7. Analysis.
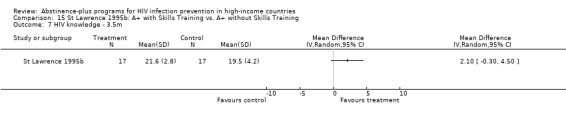
Comparison 15 St Lawrence 1995b: A+ with Skills Training vs. A+ without Skills Training, Outcome 7 HIV knowledge ‐ 3.5m.
15.8. Analysis.
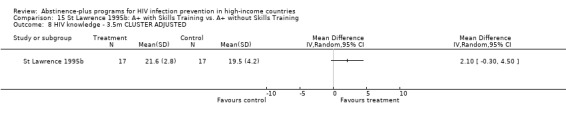
Comparison 15 St Lawrence 1995b: A+ with Skills Training vs. A+ without Skills Training, Outcome 8 HIV knowledge ‐ 3.5m CLUSTER ADJUSTED.
Comparison 16. Stanton 1996: A+ Intensive Delivered in Friendship Groups vs. A+ Non‐enhanced, No Friendship Group Delivery.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Condom use at last sex ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Condom use at last sex ‐ 6m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Condom use at last sex ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Condom use at last sex ‐ 12m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected |
16.1. Analysis.
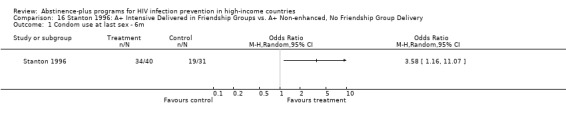
Comparison 16 Stanton 1996: A+ Intensive Delivered in Friendship Groups vs. A+ Non‐enhanced, No Friendship Group Delivery, Outcome 1 Condom use at last sex ‐ 6m.
16.2. Analysis.
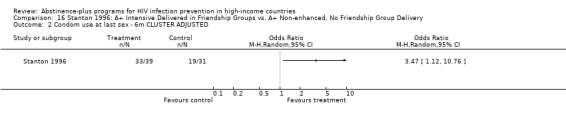
Comparison 16 Stanton 1996: A+ Intensive Delivered in Friendship Groups vs. A+ Non‐enhanced, No Friendship Group Delivery, Outcome 2 Condom use at last sex ‐ 6m CLUSTER ADJUSTED.
16.3. Analysis.
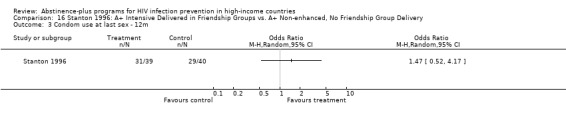
Comparison 16 Stanton 1996: A+ Intensive Delivered in Friendship Groups vs. A+ Non‐enhanced, No Friendship Group Delivery, Outcome 3 Condom use at last sex ‐ 12m.
16.4. Analysis.
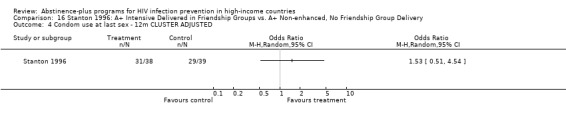
Comparison 16 Stanton 1996: A+ Intensive Delivered in Friendship Groups vs. A+ Non‐enhanced, No Friendship Group Delivery, Outcome 4 Condom use at last sex ‐ 12m CLUSTER ADJUSTED.
Comparison 17. Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recent sex ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Recent sex ‐ 3m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Recent sex ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Recent sex ‐ 6m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Recent sex ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Recent sex ‐ 9m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Condom use at last sex among sexually active ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8 Condom use at last sex among sexually active ‐ 3m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9 Condom use at last sex among sexually active ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 10 Condom use at last sex among sexually active ‐ 6m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 11 Condom use at last sex among sexually active ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 12 Condom use at last sex among sexually active ‐ 9m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 13 Ever had sex among baseline virgins ‐ 9m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 14 Ever had sex among baseline virgins ‐ 9m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected |
17.1. Analysis.
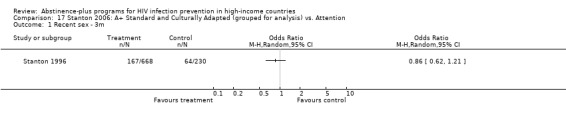
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 1 Recent sex ‐ 3m.
17.2. Analysis.
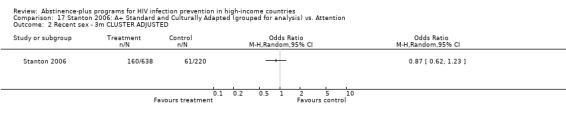
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 2 Recent sex ‐ 3m CLUSTER ADJUSTED.
17.3. Analysis.
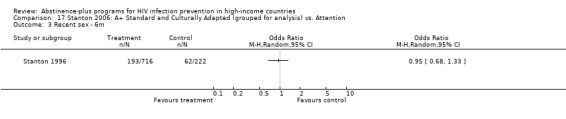
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 3 Recent sex ‐ 6m.
17.4. Analysis.
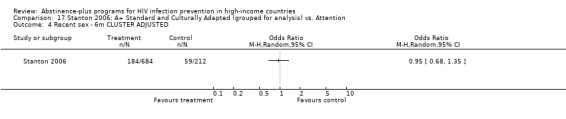
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 4 Recent sex ‐ 6m CLUSTER ADJUSTED.
17.5. Analysis.
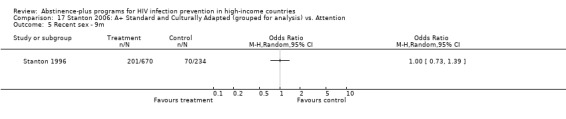
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 5 Recent sex ‐ 9m.
17.6. Analysis.
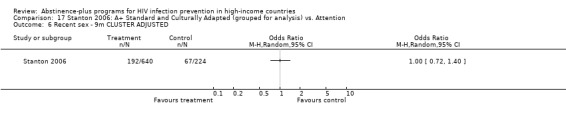
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 6 Recent sex ‐ 9m CLUSTER ADJUSTED.
17.7. Analysis.
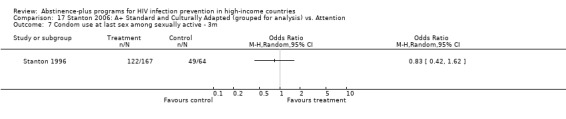
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 7 Condom use at last sex among sexually active ‐ 3m.
17.8. Analysis.
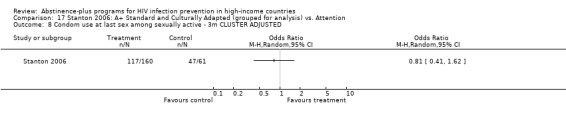
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 8 Condom use at last sex among sexually active ‐ 3m CLUSTER ADJUSTED.
17.9. Analysis.
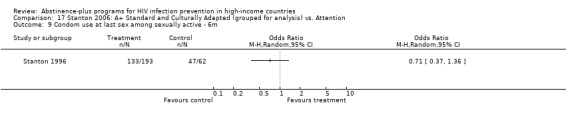
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 9 Condom use at last sex among sexually active ‐ 6m.
17.10. Analysis.
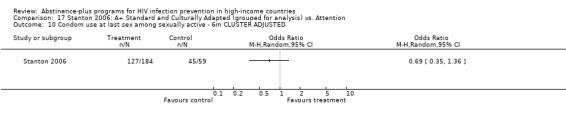
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 10 Condom use at last sex among sexually active ‐ 6m CLUSTER ADJUSTED.
17.11. Analysis.
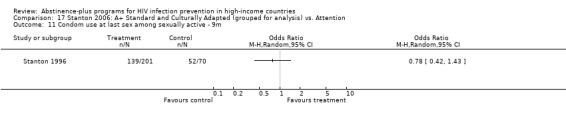
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 11 Condom use at last sex among sexually active ‐ 9m.
17.12. Analysis.
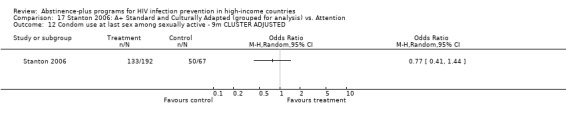
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 12 Condom use at last sex among sexually active ‐ 9m CLUSTER ADJUSTED.
17.13. Analysis.
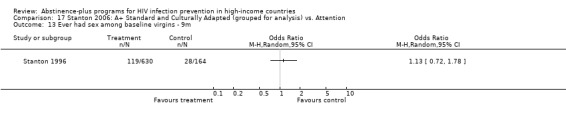
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 13 Ever had sex among baseline virgins ‐ 9m.
17.14. Analysis.
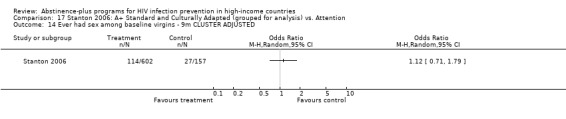
Comparison 17 Stanton 2006: A+ Standard and Culturally Adapted (grouped for analysis) vs. Attention, Outcome 14 Ever had sex among baseline virgins ‐ 9m CLUSTER ADJUSTED.
Comparison 18. Villarruel 2006: A+ vs. Attention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Sex in last 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Sex in last 3m ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3 Sex in last 3m ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Multiple partners in last 3m ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5 Multiple partners in last 3m ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6 Multiple partners in last 3m ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7 Consistent condom use in last 3m among sexually active at baseline ‐ 3m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8 Consistent condom use in last 3m among sexually active at baseline ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9 Consistent condom use in last 3m among sexually active at baseline ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected |
18.1. Analysis.
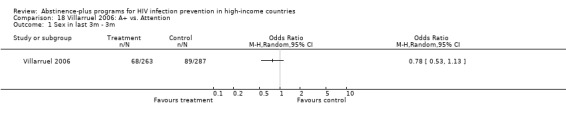
Comparison 18 Villarruel 2006: A+ vs. Attention, Outcome 1 Sex in last 3m ‐ 3m.
18.2. Analysis.
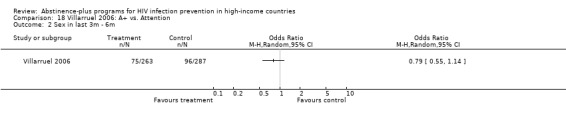
Comparison 18 Villarruel 2006: A+ vs. Attention, Outcome 2 Sex in last 3m ‐ 6m.
18.3. Analysis.
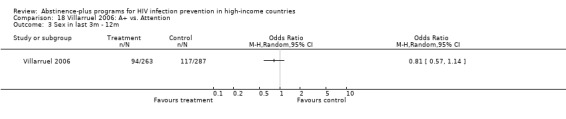
Comparison 18 Villarruel 2006: A+ vs. Attention, Outcome 3 Sex in last 3m ‐ 12m.
18.4. Analysis.
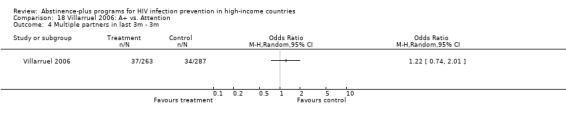
Comparison 18 Villarruel 2006: A+ vs. Attention, Outcome 4 Multiple partners in last 3m ‐ 3m.
18.5. Analysis.
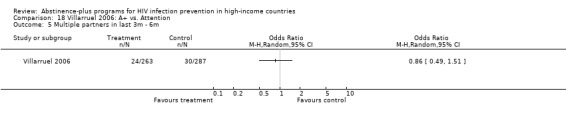
Comparison 18 Villarruel 2006: A+ vs. Attention, Outcome 5 Multiple partners in last 3m ‐ 6m.
18.6. Analysis.
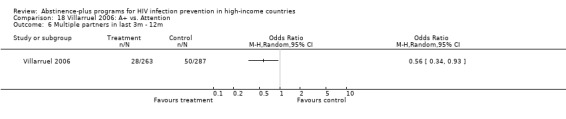
Comparison 18 Villarruel 2006: A+ vs. Attention, Outcome 6 Multiple partners in last 3m ‐ 12m.
18.7. Analysis.
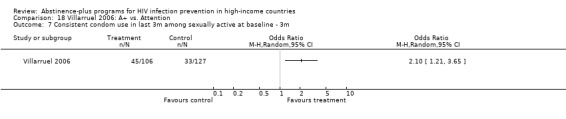
Comparison 18 Villarruel 2006: A+ vs. Attention, Outcome 7 Consistent condom use in last 3m among sexually active at baseline ‐ 3m.
18.8. Analysis.
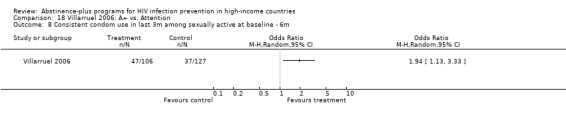
Comparison 18 Villarruel 2006: A+ vs. Attention, Outcome 8 Consistent condom use in last 3m among sexually active at baseline ‐ 6m.
18.9. Analysis.
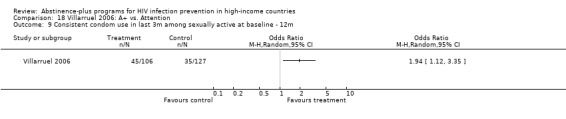
Comparison 18 Villarruel 2006: A+ vs. Attention, Outcome 9 Consistent condom use in last 3m among sexually active at baseline ‐ 12m.
Comparison 19. Weeks 1997: A+ with Parent Involvement vs. A+ without Parent Involvement vs. Usual Care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recent sex ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Non‐Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Parent vs Non‐Parent | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Recent sex ‐12m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Non‐Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Parent vs Non‐Parent | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Recent sex ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Non‐Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Parent vs Non‐Parent | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Recent sex ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Non‐Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Parent vs Non‐Parent | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Ever had sex ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Non‐Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Parent vs Non‐Parent | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Ever had sex ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Non‐Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Parent vs Non‐Parent | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Condom use at last sex ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Non‐Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 Parent vs Non‐Parent | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Condom use at last sex ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Non‐Parent vs Control | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Parent vs Non‐Parent | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
19.1. Analysis.
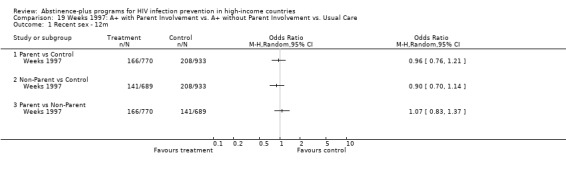
Comparison 19 Weeks 1997: A+ with Parent Involvement vs. A+ without Parent Involvement vs. Usual Care, Outcome 1 Recent sex ‐ 12m.
19.2. Analysis.
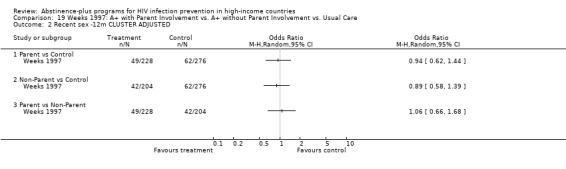
Comparison 19 Weeks 1997: A+ with Parent Involvement vs. A+ without Parent Involvement vs. Usual Care, Outcome 2 Recent sex ‐12m CLUSTER ADJUSTED.
19.3. Analysis.
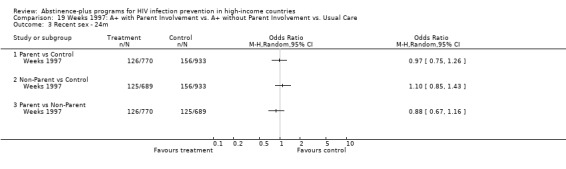
Comparison 19 Weeks 1997: A+ with Parent Involvement vs. A+ without Parent Involvement vs. Usual Care, Outcome 3 Recent sex ‐ 24m.
19.4. Analysis.
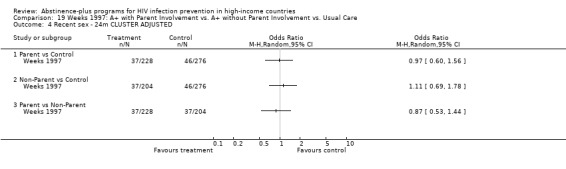
Comparison 19 Weeks 1997: A+ with Parent Involvement vs. A+ without Parent Involvement vs. Usual Care, Outcome 4 Recent sex ‐ 24m CLUSTER ADJUSTED.
19.5. Analysis.
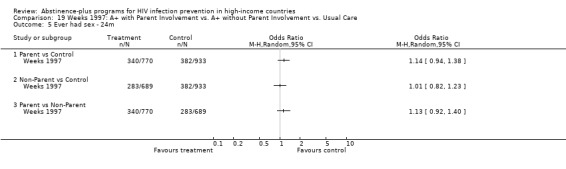
Comparison 19 Weeks 1997: A+ with Parent Involvement vs. A+ without Parent Involvement vs. Usual Care, Outcome 5 Ever had sex ‐ 24m.
19.6. Analysis.
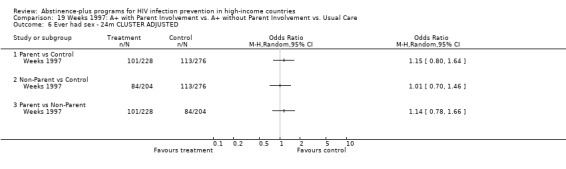
Comparison 19 Weeks 1997: A+ with Parent Involvement vs. A+ without Parent Involvement vs. Usual Care, Outcome 6 Ever had sex ‐ 24m CLUSTER ADJUSTED.
19.7. Analysis.
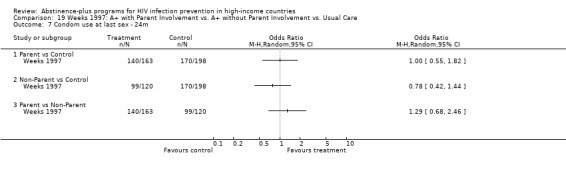
Comparison 19 Weeks 1997: A+ with Parent Involvement vs. A+ without Parent Involvement vs. Usual Care, Outcome 7 Condom use at last sex ‐ 24m.
19.8. Analysis.
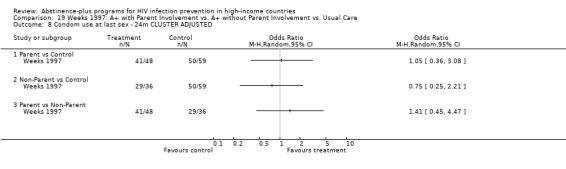
Comparison 19 Weeks 1997: A+ with Parent Involvement vs. A+ without Parent Involvement vs. Usual Care, Outcome 8 Condom use at last sex ‐ 24m CLUSTER ADJUSTED.
Comparison 20. Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pregnancy in past 6m ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pregnancy in past 6m ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Sex in the past 6m ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Sex in the past 6m ‐ 6m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Sex in the past 6m ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Sex in the past 6m ‐ 12m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Sex in the past 6m ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Sex in the past 6m ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Anal sex in past 6m ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Anal sex in past 6m ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 10.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Condom use at last sex among participants reporting sex in the past 6m ‐ 6m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 11.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Condom use at last sex among participants reporting sex in the past 6m ‐ 6m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 12.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Condom use at last sex among participants reporting sex in the past 6m ‐ 12m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 13.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Condom use at last sex among participants reporting sex in the past 6m ‐ 12m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 14.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Condom use at last sex among participants reporting sex in the past 6m ‐ 24m | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 15.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Condom use at last sex among participants reporting sex in the past 6m ‐ 24m CLUSTER ADJUSTED | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 16.1 FOK and ImPACT (with and without boosters) vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 FOK and ImPACT with boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 FOK and ImPACT without boosters vs. FOK only | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.4 FOK and ImPACT with boosters vs. FOK and ImPACT without boosters | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
20.1. Analysis.
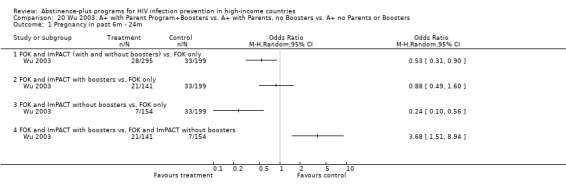
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 1 Pregnancy in past 6m ‐ 24m.
20.2. Analysis.
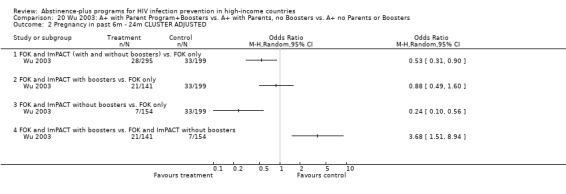
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 2 Pregnancy in past 6m ‐ 24m CLUSTER ADJUSTED.
20.3. Analysis.
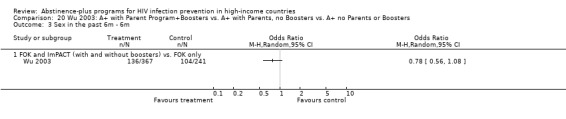
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 3 Sex in the past 6m ‐ 6m.
20.4. Analysis.
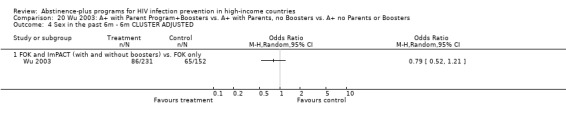
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 4 Sex in the past 6m ‐ 6m CLUSTER ADJUSTED.
20.5. Analysis.
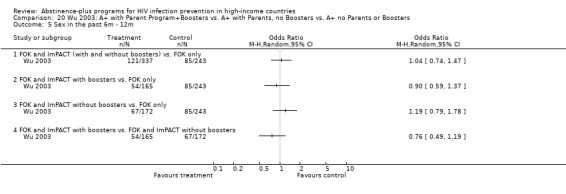
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 5 Sex in the past 6m ‐ 12m.
20.6. Analysis.
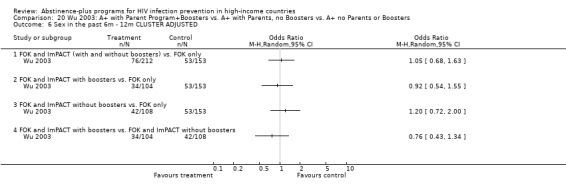
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 6 Sex in the past 6m ‐ 12m CLUSTER ADJUSTED.
20.7. Analysis.
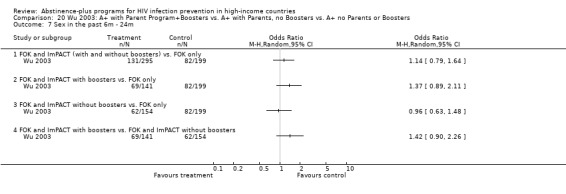
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 7 Sex in the past 6m ‐ 24m.
20.8. Analysis.
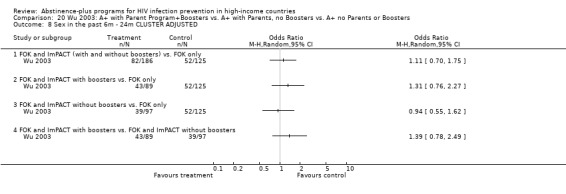
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 8 Sex in the past 6m ‐ 24m CLUSTER ADJUSTED.
20.9. Analysis.
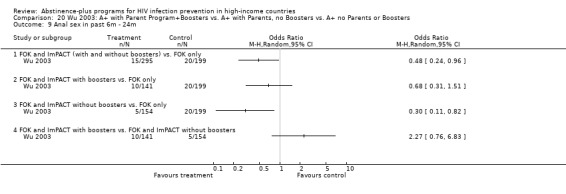
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 9 Anal sex in past 6m ‐ 24m.
20.10. Analysis.
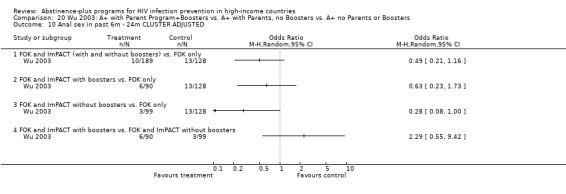
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 10 Anal sex in past 6m ‐ 24m CLUSTER ADJUSTED.
20.11. Analysis.
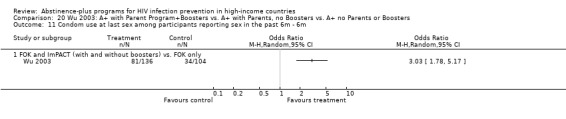
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 11 Condom use at last sex among participants reporting sex in the past 6m ‐ 6m.
20.12. Analysis.
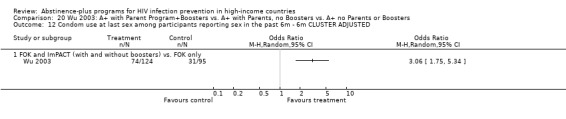
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 12 Condom use at last sex among participants reporting sex in the past 6m ‐ 6m CLUSTER ADJUSTED.
20.13. Analysis.
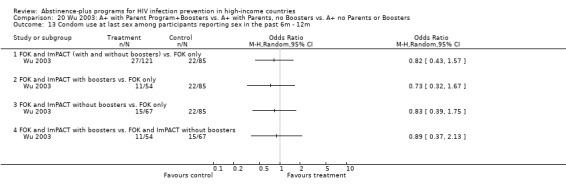
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 13 Condom use at last sex among participants reporting sex in the past 6m ‐ 12m.
20.14. Analysis.
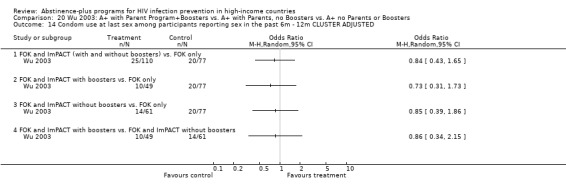
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 14 Condom use at last sex among participants reporting sex in the past 6m ‐ 12m CLUSTER ADJUSTED.
20.15. Analysis.
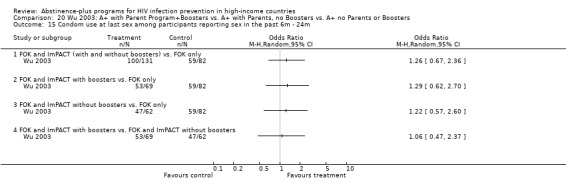
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 15 Condom use at last sex among participants reporting sex in the past 6m ‐ 24m.
20.16. Analysis.
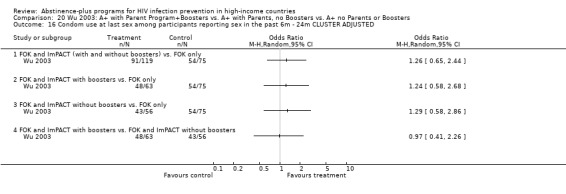
Comparison 20 Wu 2003: A+ with Parent Program+Boosters vs. A+ with Parents, no Boosters vs. A+ no Parents or Boosters, Outcome 16 Condom use at last sex among participants reporting sex in the past 6m ‐ 24m CLUSTER ADJUSTED.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aarons 2000.
| Methods | RCT, Abstinence‐plus vs. Usual Care. Unit of randomization: School, matched‐pair design based on class size, location, and racial distribution. Method of randomization: Not reported. Data collection: Self‐administered anonymous surveys completed in school. Assessment times: Baseline, 3m, 8m, and 15m. Complete case analysis. Attrition: 27.5% at 15m. No attrition analyses provided. Group equivalence: Baseline differences in ethnicity, SES, alcohol use, family structure and grades. Controlled for baseline values in multivariate analysis. |
|
| Participants | Washington, DC (USA) N = 582 students, 6 schools Mean age 12.8 yrs Ethnicity: 84% African‐American. Others primarily Latino. SES: 63% enrolled in federal free or reduced price lunch program. 48% Male. Notes on recruitment: 6 schools were diverse and close to affiliated clinics. Excluded students who were not in 7th grade at beginning of study, not in 8th grade in 1996‐1997 year, truant/suspended during consent process or questionnaire, or incapable of reading and comprehending questionnaire in English or Spanish. |
|
| Interventions | 1: "Postponing Sexual Involvement" with "Self Center." 7th‐grade students received 3 teacher‐led sessions on reproductive health and 5 peer‐led sessions on peer pressures and postponing sex. Small‐group discussions, formal instruction. Individual meetings were held with at‐risk students according to health screening survey. Brown‐bag lunch booster session in 8th grade. 8th‐grade assembly led by person with AIDS. Art contest on project themes.
Theoretical basis: Social cognitive theory.
Setting: junior high school classrooms.
Exposure: 8 class periods over 2m in 7th grade, approximately 2 hours of optional booster sessions recommended in 8th grade.
Staff: Full‐time health education professional in each school. Peer leaders were from the 10th and 11th grades of local high schools. 2: Usual care ‐ students received usual health curriculum as dictated by school. |
|
| Outcomes | Virginity Condom use at last intercourse among male participants |
|
| Notes | Funding: NIH Office of Research on Minority Health, National Institute of Child Health and Human Development. Not designed to track individual participants. Analyses did not control for clustering. Fidelity monitoring by attendance records. No data for cost or participant satisfaction. Schools received small monetary stipend for participation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Boekeloo 1999.
| Methods | RCT, Abstinence‐plus vs. Usual Care. Unit of randomization: Individual, stratified by health care provider. Method of randomization: Not reported. Data collection: Assessment immediately post‐intervention by face‐to‐face interview with female interviewer (unblinded). Assessments by phone using touch‐tone data collection administered by female interviewer (blinded) at follow‐ups. Assessment times: Immediate post‐intervention (exit interview), 3m, 9m. Complete case analysis. Attrition: 10% at 9m. No significant differences between the study groups at any follow‐up for gender, age group, state of residence, or practice site. Group equivalence: No baseline differences by gender, age group, state of residence, or practice site. |
|
| Participants | Washington, DC (USA) N = 219 adolescents, 19 physicians, 5 managed‐care sites Age: Intervention group 49% aged 12‐13 yrs, 51% aged 14‐15 yrs. Control group 57% aged 12‐13 yrs, 43% aged 14‐15 yrs. Ethnicity: 65% African‐American, 19% White, 3% Hispanic, 13% Other. SES: Not reported 50% Male. Notes on recruitment: Recruited all patients aged 12‐15 who were scheduled for a general care visit with any one of the 19 participating physicians. Participants were invited by phone and letter to take part in the study. |
|
| Interventions | 1: "Awareness, Skills, Self‐Efficacy/Self‐Esteem, and Social Support "(ASSESS). 1‐session intervention included an audiotaped risk assessment, where participants listened to the assessment and an educational program using a tape player and headset; participants then discussed their personal risks with a physician. Physician used a pyramid to illustrate sexual risks. Concepts included sexual history and safe‐sex behaviors, hierarchy of safe‐sex behaviors, refusal skills, condom skills, community resources, drug use, HIV/AIDS, pregnancy prevention, puberty, limiting partners, and alternatives to intercourse. Adolescent received 2 brochures about refusal and condom skills, 1 brochure about community resources. Parents received 2 brochures about addressing drugs and sexual risk with kids.
Theoretical basis: Social cognitive theory, theory of reasoned action.
Setting: Pediatrician's office.
Exposure: Risk assessment lasted 14 minutes, followed by 1‐session discussion with physician.
Staff: Licensed pediatrician. 2: Usual care ‐ participants attended general care visit from the same pediatricians, but did not participate in risk assessment exercise, receive brochures, or have the pyramid‐directed discussion. |
|
| Outcomes | STI diagnosis since last assessment Pregnancy since last assessment Oral, anal, or vaginal sex in the past 3m Vaginal sex in the past 3m Frequency of vaginal sex in the past 3m Number of lifetime vaginal sex partners Number of vaginal sex partners in the past 3m Condom use at last vaginal sex among participants reporting vaginal sex in the past 3m Know vaginal intercourse can transmit HIV Know oral intercourse can transmit HIV Know anal intercourse can transmit HIV Know condoms do not offer 100% protection |
|
| Notes | Funding: National Institute for Child Health and Human Development, Health Resources and Service Administration (Mid‐Atlantic AIDS Education Training Center Program Grant). No pre‐intervention assessment. Same facilitators conducted intervention and control‐group sessions. Fidelity monitoring through exit interviews with participants: participants reported the extent to which they had discussed intervention topics with the physicians. for all but 2 intervention topics, significantly higher percentages of intervention participants than control participants reported discussing the subject during their appointment. No data for cost or participant satisfaction. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Coyle 2001.
| Methods | RCT, Abstinence‐plus vs. Information about HIV and STIs.
Unit of randomization: School, stratified by state, used a matched‐pairs design based on an index of school characteristics. Method of randomization: Not reported. Data collection: Self‐report surveys completed in school and administered by trained data collectors (surveys were sent by mail if students unavailable in school). Assessment times: Baseline, 7m, 19m, and 31m. Complete case analysis. Attrition 21% at 31m. Dropouts were more likely to be older and male, less likely to live with both parents, reported more risk behavior at baseline, and had reported less favorable scores on psychosocial scales. Group equivalence: Baseline differences for 10 of 13 psychosocial variables. Intervention group also more likely to report ever having sex, being tested for HIV, and being tested for other STDs. Controlled for outcome‐specific covariates and baseline values in each analysis. |
|
| Participants | California and Texas (USA) N = 3869 students, 20 schools Age: All participants began study in 9th grade. for intervention group: 4.4% were 13 yrs, 57.2% were 14 yrs, 28.1% were 15 yrs, 8.6% were 16yrs, and 1.7% were 17yrs and older. for control group, respective percentages are 4.6%, 57.4%, 27.7%, 7.9%, and 2.4% Ethnicity: Intervention group: 13.5% Asian, 19.6% African‐American, 28.4% Latino, 30.2% Caucasian, 8% Other. Control group: 22.2%, 14.3%, 26.4%, 30.7%, 6.4% SES: Described as "diverse." 49.8% male in intervention group, 46.4% male in control group. Notes on recruitment: 10 schools were recruited in each state, chosen for diversity in ethnicity and SES, location in areas of country with high HIV rates, and close proximity to investigators. Excluded 95 students at intervention and control schools who were in 11th or 12th grades, and 346 students who left school during the 1993‐1994 school year and did not return the following year. Analyses were restricted to ninth‐graders who completed baseline survey in fall of 1993 and officially enrolled in second year of the intervention (fall 1994). |
|
| Interventions | 1: "Safer Choices." In‐school curriculum included 10 lessons in the 9th grade and 10 lessons in the 10th grade. Concepts included delaying sex, condom use, self‐efficacy, communication with parents and partners, peer norms, perceived risks of infection, and STI and HIV knowledge. Program also included 4 other components: school organization (school health promotion council); peer resources and school environment change (including student peer resource team activities and assemblies); parent education (newsletters, homework assignments); and school‐community linkages (community resource guides, local HIV+ speakers).
Theoretical basis: Social cognitive theory, social influence theory, models of school change.
Setting: Public high school classes.
Exposure: 20 class sessions over 2 academic years, additional activities varied by school.
Staff: Teachers, peer leaders, and guest speakers. 2: Information about HIV and STIs. Participants received five 50‐min class sessions focusing on HIV and STI knowledge. Small number of extracurricular activities varied by school. Unclear if this was an abstinence‐based intervention. Theoretical basis: Unclear. Setting: Public high school classes. Exposure: 5 class sessions over 1 academic year, additional activities varied by school. Staff: Unclear. |
|
| Outcomes | Frequency of intercourse without a condom in last 3m among participants reporting intercourse Number of times had sex in last 3m among sexually experienced participants Number of sex partners in last 3m among sexually experienced participants Number of sexual partners without a condom in last 3m among participants reporting intercourse Condom use at last intercourse among participants who reported vaginal sex in the past 3 months Sexual initiation among all participants HIV knowledge among all participants |
|
| Notes | Funding: Centers for Disease Control and Prevention Analyses controlled for clustering. Intervention schools received training and technical support for 1993‐1994 and 1994‐1995 years, reduced support in 1995‐1996. Subgroup analyses by gender, race, baseline virginity, and risk at baseline show significant protective effects for all risk groups, but on different variables. Cost data presented in separate paper. Interviews with school personnel suggest that the experimental program was well‐received |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Coyle 2004.
| Methods | RCT, Abstinence‐plus vs. Usual Care. Unit of randomization: School, stratified by district, matched‐pairs design based on index of school characteristics. Method of randomization: Not reported. Data collection: self‐report surveys completed in school and administered by trained data collectors (surveys were sent by mail if students unavailable in school). Assessment times: Baseline, 12m, 24m, and 36m. ITT analysis, rich‐imputation model to approximate outcomes for dropouts. Attrition: 9% at 12m, 12% at 24m, 36% in 36m. No differences in retention across groups. Attrition higher among boys, also higher among African‐Americans and Latinos than among Others and Whites. Group equivalence: No baseline differences by demographics. Intervention group more likely to report ever having had sex at baseline (differences diminished after controlling for baseline peer norms). Included baseline values as covariates in all analyses. |
|
| Participants | Northern California (USA)
N = 2829 students, 19 schools Mean age 11.5 yrs Ethnicity: 5.2% African‐American, 15.9% Asian, 59.3% Latino, 16.5% Caucasian, 3.1% Other. SES: Described as "diverse." 49.9% Male. Notes on recruitment: 19 middle schools (grades 6‐8) were recruited from 3 midsized districts, selected for diversity in ethnicity and SES. |
|
| Interventions | 1: "Draw the Line/Respect the Line." In‐school curriculum consisted of 20 in‐class lessons: 6th grade had 5 lessons on limit‐setting in nonsexual situations. 7th grade had 8 lessons on sexual limits. 8th grade had 7 lessons including HIV+ speaker, refusal and condom skills. Concepts included delaying intercourse, using condoms, personal limits, consequences of sex, skills to maintain limits, respecting others' limits, refusal skills. Activities integrated elements specific to Latino culture, and involved interactive classes, small group activities, an HIV+ speaker, a condom demonstration, and skills practice.
Theoretical basis: Social cognitive theory, social inoculation theory.
Setting: Junior high school classrooms.
Exposure: 20 class sessions over 3 years ‐ 5 in 6th grade, 8 in 7th grade, 7 in 8th grade.
Staff: Bilingual (Spanish/English) adult facilitators. 2: Usual Care ‐ usual school health curriculum as dictated by school. |
|
| Outcomes | Sex in the past 12m among all participants Number of times had sex in past 12m among all participants Number of sexual partners in last 12m among all participants Condom use at last sex among participants reporting vaginal sex in the past 12 months Ever had sex among all participants Knowledge about HIV and condoms among all participants |
|
| Notes | Funding: National Institute of Mental Health. Analyses restricted to the 2829 participants who completed the baseline survey. Analyses controlled for clustering. Long‐term follow‐up limited by high attrition. No cost data reported. Student feedback was used to improve program throughout implementation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Coyle 2006.
| Methods | RCT, Abstinence‐plus vs. Usual care. Unit of randomization: School. Method of randomization: Not reported. Data collection: Written self‐report surveys in English/Spanish. Often mailed or hand‐delivered to participants due to high turnover at schools. Assessment times: 6m, 12m, 18m Complete case analysis. Attrition: 45% at 6m, 53% at 12m, 58% at 18m. No differences across groups. Dropouts were more likely to have reported having sex in the previous 3 months and using a condom at last sex at baseline. Group equivalence at baseline: Significant baseline differences (intervention group slightly older than controls), but controlled in analyses. |
|
| Participants | Northern California (USA) N = 988 students at 24 alternative schools Mean age: 16.0 Ethnicity: 28% African‐American, 15% Asian American, 29% Hispanic/Latino, 12% White, 16% Other. SES: unclear 62% male Notes on recruitment: Recruited 13 schools. Participants had been referred to schools for discipline issues, substance use, and chronic absenteeism; schools are intended to help students make up lost credits in order to return to mainstream schools or get a GED. |
|
| Interventions | 1: All4You!: 26 hours over 6 weeks led by health educators. Included 13.5 hours of classroom instruction and 12.5 hours of community service as a classroom. No parent involvement. Lessons drawn from Be Proud! Be Responsible! and Safer Choices curricula.
Theoretical basis: Social cognitive theory, theory of reasoned action, theory of planned behavior.
Setting: Alternative school classrooms and service learning placements.
Exposure: 26 hours over 6 weeks
Staff: Health educators. 2: Usual care defined by schools ("typically consisted of outside presenters from local community‐based agencies"). |
|
| Outcomes | Been pregnant or caused a pregnancy since baseline among participants reporting sexual activity in the past 3 months Frequency of intercourse without a condom in last 3m among all participants Frequency of vaginal intercourse in the last 3m among all participants Number of lifetime sexual partners among all participants Number of sexual partners without a condom in last 3m among all participants Condom use at last sex among participants who report ever having had sex Sexual initiation among participants who reported being sexually inexperienced at baseline HIV and condom knowledge among all participants |
|
| Notes | Funding: Center for Disease Control and Prevention. Analyses controlled for clustering. Rehearsed project implementation at a pilot school. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Dancy 2006.
| Methods | RCT, Abstinence‐plus (led by mothers) vs. Abstinence‐plus (led by health experts) vs. Attention. Unit of randomization: Community. Method of randomization: Not reported. Data collection: ACASI assessment. Assessment times: 5 months after baseline. Complete case analysis. Attrition: 11% at 5 months. Attrition higher among mother‐led experimental group (1) and controls (3). Group equivalence at baseline: No group differences at baseline. |
|
| Participants | Chicago, IL (USA) N = 262 girls and their mothers in 3 communities. Mean age: 12.4 Ethnicity: 100% African‐American SES: low 0% male Notes on recruitment: Recruited mother‐daughter pairs by flyers, word‐of‐mouth, and face‐to‐face encounters with participants in community settings. |
|
| Interventions | 1: Mother‐Daughter Risk Reduction curriculum. Mothers undergo 12 weeks of training in small groups to learn curriculum from health experts. Then, mothers teach their daughters about HIV risk reduction in 6 small‐group classes. Each mother teaches a portion of the curriculum. Includes commitment to abstinence and mother‐child homework assignments.
Theoretical basis: Social cognitive theory, theory of reasoned action, community‐other mothers.
Setting: Community centers.
Exposure: 12 weeks of training for mothers; 12 hours over 6 weeks for girls.
Staff: Mothers of participants (who have been trained by health educators). 2: Heath Expert HIV Risk Reduction curriculum. 12 hours over 6 weeks, sessions delivered to girls alone by health experts. No mother‐daughter homework assignments or formalized agreement to practice sexual abstinence. 3: Attention. Mother Daughter Health Promotion curriculum. Same as 1, but focused on general nutrition and exercise instead of HIV. |
|
| Outcomes | Vaginal, oral, or anal intercourse ever among all participants HIV transmission knowledge among all participants |
|
| Notes | Funding: National Institute of Mental Health. Analyses controlled for clustered randomization. Practice sessions and technical support were provided for mother‐led groups (1 and 3). Small number of communities randomized (1 per treatment condition). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Danella 2000.
| Methods | RCT, Abstinence‐plus vs. No treatment. Unit of randomization: Individual. Method of randomization: Random numbers table. Data collection: Unclear whether it was ACASI or written self‐report. Assessment times: 2m, 6m, 12m. Complete case analysis. Attrition: Unclear. No attrition analyses reported. Group equivalence at baseline: Unclear. |
|
| Participants | Nassau, Bahamas. N = 500 girls Age range: 9‐17 years Ethnicity: 100% Bahamian SES: unclear 0% male Notes on recruitment: Recruited from schools, an STI clinic, and a community‐based program for expecting adolescent mothers. |
|
| Interventions | 1: Focus on Kids (Bahamian version). Led by adults, activities included lectures, skills‐building, videos, games, interactive activities. Concepts included HIV, alcohol, sexual harassment, and "sweethearting." Adapted from original FOK curriculum based on group discussion and consensus with community stakeholders.
Theoretical basis: Social cognitive theory, protection motivation theory
Setting: Group settings in community centers
Exposure: 15 hours over 10 weeks with graduation ceremony, booster session after 6 months.
Staff: Adults. 2: No treatment (delayed receipt of the experimental program). |
|
| Outcomes | Sexual intercourse in past 6m among all participants Condom use at last sex among sexually active participants AIDS knowledge (75% or more correct) |
|
| Notes | Funding: World AIDS Foundation. Data extracted from a conference presentation and a partially completed report. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Danielson 1990.
| Methods | Quasi‐RCT, Abstinence‐plus vs. Nonintervention. Unit of randomization: Individual. Method of randomization: Alternation. Data collection: Self‐report surveys completed in the medical office examining room or other private room, administered by blind study personnel; some follow‐ups completed by mail. Assessment times: Baseline and 12m. Complete case analysis for most data; sexual activity status was imputed as "not active in the previous year" if other data did not indicate sexual activity. Attrition: 19.9% at 12m. Approximately 1% more was lost from control group than from intervention group. Attrition was associated with having had sex at baseline, performing poorly in school, being in a higher grade at school, having less perceived family wealth, not having a father in the home, having friends who had had sex, having girlfriend, and having low level of heterosexual intimacy. Group equivalence: Baseline differences in parental education and employment. Used logistic regression to control for confounders of a range of variables; missing confounding values were replaced by estimated values (mode or median). |
|
| Participants | Portland, OR and Vancouver, WA (USA) n = 1195 Age range: 15‐18yrs Ethnicity: Predominantly white, <5% African‐American, <4% Asian. SES: 85% reported having father who was employed full‐time; 44% reported that their father had graduated from college. 100% Male Notes on recruitment: Recruited by phone among men aged 15‐18 who received ambulatory care at participating medical offices between June 1985‐November 1986, who anticipated being in the area for one year. |
|
| Interventions | 1: "Reproductive Health Counseling for Young Men." Goals: promote abstinence and contraception. Healthcare practitioner introduced 30‐min slide‐tape program, which participant viewed privately in an exam room. Program included explicit photos and information regarding anatomy, fertility, hernia, testicular self‐examination, STIs, AIDS, contraception, abstinence, couple communication, and access to health services. Healthcare provider and participant had individual consultation after the program, which focused on contraception and was guided by the participant's interests. Consultation included question‐and‐answer time, discussing values and motivations, condom practice, modeling and rehearsing communication skills, providing explicit advice, and encouraging abstinence, consistent contraceptive use, condom use, and STI recognition.
Theoretical basis: Not reported.
Setting: Medical examination room.
Exposure: 1 hour.
Staff: 5 nurse practitioners, 3 physician's assistants, and 2 registered nurses. 2: Nonintervention. Control participants received the reproductive health counseling session after 12m follow‐up. |
|
| Outcomes | Sexual activity (i.e., reporting intercourse, intercourse with a female partner, or intercourse with someone the participant didn't know well) in last 12 months among all participants AIDS knowledge among all participants Data on condom use were collected, but confounded with other methods of contraception. |
|
| Notes | Funding: Office of Family Planning, Department of Health and Human Services; National Institutes of Health Biomedical Research Support Grant. Participants received $15 stipend for transportation costs. N's are unclear; 1449 youth agreed to participate, and "scheduling was successfully completed" for n = 1195. However, the report states that 82% were followed up at 12 months, which consisted of 994 follow‐up surveys. According to this data, total baseline enrollment should be n = 1212. We re‐computed attrition considering the given baseline enrollment figure of n = 1195 and the number of participants with usable follow‐up data n = 971. Threats to intervention fidelity: an external community‐wide AIDS prevention campaign began midway through the intervention. Study reports that 85% of intervention participants were "successfully scheduled for a health consultation," suggesting that 15% of the intervention group did not receive the intervention; it is unclear whether these participants were excluded from analyses. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
DiIorio 2006.
| Methods | RCT, Abstinence‐plus (based on social cognitive theory) vs. Abstinence‐plus (based on Life Skills theory) vs. Information. Unit of randomization: Community center. Method of randomization: Computer‐generated sequence. Data collection: Unclear whether assessments used ACASI or written surveys; mothers and children were surveyed in separate rooms. Assessment times: 4m, 12m, 24m Complete case analysis. Attrition: 5.5% at 4m, 6.5% at 12m, 9.8% at 24m. No attrition analyses reported. Group equivalence at baseline: Baseline differences (group 2 was significantly older than groups 1 and 3), but controlled in analyses. |
|
| Participants | Atlanta, GA (USA) N = 582 participants and their mothers, at 11 community centers. ("110 mothers had more than 1 adolescent with whom they participated in the study") Mean age: 12.2 Ethnicity: 97.9% African‐American SES: low 60% male Notes on recruitment: Recruited mother/child units through Boys and Girls Clubs of Metro Atlanta. |
|
| Interventions | 1: Keepin' it R.E.A.L. Based on social cognitive theory. Led by adult facilitators, attended by mothers and adolescents. Focused on adolescent development and communication, peer influences, condoms, contraceptives, HIV. Activities included games, videos, discussions, role‐plays, skits, demonstrations, and homework.
Theoretical basis: Social cognitive theory.
Setting: Community centers.
Exposure: 14 hours in 7 sessions over 14 weeks.
Staff: Adult facilitators. 2: Keepin' it R.E.A.L., but based on life skills theory instead of social cognitive theory. Same exposure and activities as before, but focused on the idea that problem behaviors co‐occur within adolescents and are based on common underlying psychological attributes. Discussions addressed many at‐risk behaviors (smoking, alcohol/drugs, violence, and early sex). Included community service and educational field trips. Mothers explore parenting problems. 3: Information. Mothers and adolescents attend a 1‐hour HIV prevention session that included a videotape and a discussion of risk and prevention. |
|
| Outcomes | Condom use at last sex among participants who have ever had sex Percentage of time condoms used in past 30 days among participants who have ever had sex Percentage of time condoms used in past 3 months among participants who have ever had sex Percentage of time condoms used in past 6‐12 months among participants who have ever had sex Ever had sex among all participants HIV knowledge among all participants |
|
| Notes | Funding: National Institute of Mental Health Analyses controlled for clustering within community centers. But it was unclear how this trial accommodated clustering within treatment arms. It appeared that at least 220 of the 582 randomized youth were siblings. Reported ICC for community center level. Implementation monitoring included facilitator training, weekly meetings with facilitators, and 20% of sessions were videotaped and evaluated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
DiIorio 2007.
| Methods | RCT, Abstinence‐plus vs. Attention. Unit of randomization: Community center. Method of randomization: Unclear. Data collection: ACASI Assessment times: 3m, 6m, 12m Complete case analysis. Attrition: Approx 20% at 12m (unclear at 3m and 6m). Attrition did not differ by group. Group equivalence at baseline: Baseline differences (percentage of participating fathers living with their respective adolescent), controlled in analyses. |
|
| Participants | Atlanta, GA (USA) N = 277 boys at 7 community centers. Mean age: 12.7 Ethnicity: 97% African‐American SES: low 100% male Notes on recruitment: Recruited father/son units through Boys and Girls Clubs of Metro Atlanta. Father figures were eligible if they were 18 or older, were identified by the mother as a significant influence in the adolescent's life, had at least a one‐year relationships with the adolescent, and the mother and son agreed together that the person would serve as a father figure. |
|
| Interventions | 1: R.E.A.L. MEN. Led by adult facilitators, 6 sessions attended by fathers, 1 session attended by fathers and sons. Focused on adolescent development and communication, peer influences, condoms, HIV, parental monitoring. Delivered in groups, included lectures, discussions, role‐plays, games, and videos. Included end‐of‐intervention party.
Theoretical basis: Social cognitive theory.
Setting: Community centers.
Exposure: 14 hours in 7 session over 7 weeks.
Staff: Adult facilitators. 2: Attention. Same format as experimental, but focused on nutrition and exercise. |
|
| Outcomes | Ever had sex without a condom among participants who have ever had sex Ever had sex among all participants |
|
| Notes | Funding: Unclear. Incentives included $25 for completing each assessment, and non‐monetary project materials (mugs, T=shirts). Analyses controlled for clustering. Appeared to be only one son per father. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Ferguson 1998.
| Methods | Quasi‐RCT, Abstinence‐plus enhanced (with peer counseling) vs. Abstinence‐plus non‐enhanced (without peer counseling). Unit of randomization: Neighborhood. Method of randomization: Coin toss. Data collection: Written multiple‐choice survey. Assessment times: Baseline, immediately post‐intervention, and 3m follow‐up. Complete case analysis; participants with any missing data were excluded from the study. Attrition: 17% at 3m; all who dropped out relocated to other counties. Attrition differed between groups ‐ 26.7% in control group, 9.1% in experimental group. Group equivalence: Test of baseline significance not provided. Analyses used repeated‐measures ANOVAs to incorporate baseline data. |
|
| Participants | Charlottesville, VA (USA) N = 63 participants, 4 neighborhoods Age range: 12‐16 yrs, mean ages by neighborhood were 13.0 or 13.5 yrs Ethnicity: 100% African‐American. SES: Neighborhoods had average household incomes ranging between $9,337 and $18,937 (125% of federal poverty level) 0% Male. Notes on recruitment: Study recruited African‐American females between ages of 12 and 16 who had successfully completed the Monticello community pregnancy prevention program, resided in one of the four target neighborhoods, were not pregnant, and had never given birth to a child. Participants were assigned to groups based on neighborhood of residence. |
|
| Interventions | 1: Peer Counseling Intervention: 8‐week supplement to the "Monticello Area Community Action Agency (MCAA) Camp Horizon Adolescent Pregnancy Prevention Program." 2 program hours per week delivered to groups of participants in classroom setting. Activities included culturally specific peer counseling, informal discussions, roleplays, communication skills, celebration of Kwanza principles, singing spirituals, and attending gospel music festivals. Goals included preventing pregnancy, delaying sex, increasing knowledge, and maintaining or increasing contraceptive use. Concepts included Afrocentricity, ethnicity, sex, sexuality, "the African American value system," academic and career development, leadership, and life management skills.
Theoretical basis: Not reported.
Setting: After‐school program; location unclear.
Exposure: 2 hours per week for 8 weeks.
Staff: Peer leaders from the same Monticello program; received 10‐week training program. 2: Same curriculum as above, but without the peer counseling component. All activities were directed by the investigator. Theoretical basis: Not reported. Setting: After‐school program; location unclear. Exposure: 2 hours per week for 8 weeks. Staff: the investigator (PhD and RN). |
|
| Outcomes | Pregnancy Sexual intercourse at least once in past 4 weeks among all participants "Ever being sexually active" among all participants Knowledge of reproduction, STDs, and contraception among all participants |
|
| Notes | Funding: Not reported. Analyses did not control for clustering. Some peer counselors lived in or around control‐group neighborhoods, but were instructed not to give counseling to participants in the control group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Hernandez 1990.
| Methods | RCT, Abstinence‐plus vs. Abstinence‐only vs. Safe‐sex vs. Nonintervention. Unit of randomization: Individual. Method of randomization: Not reported. Data collection: Confidential written questionnaire in a group setting. Assessment times: Baseline and 1.5m. Complete case analysis. Attrition: 5% at 1.5m. Attrition analyses not provided. Group equivalence: No statistically significant baseline differences. |
|
| Participants | North Carolina (USA) N = 410 Mean age: 19.25 yrs Ethnicity: 85% white. SES: Not reported. 55% Male. Notes on recruitment: 410 unmarried students aged 18‐21 from state universities were recruited from an introductory psychology course. Participation in the study was an option to fulfill research requirements in the course. |
|
| Interventions | 1: Abstinence‐plus intervention ("Protection"). One session. Concepts included abstinence, the biology and symptoms of AIDS, transmission, prevention, explicit instructions on condom use and discussing safe sex with partners. Participants received a 7‐page written health education program written by the Duke University Student Health Service and the American College Health Association ("Making Sex Safer"). They then watched a video entitled "AIDS: You're Not Immune" from the Alpha Theta fraternity. Participants received a brochure from HERO entitled "Safer Sex for Men and Women Concerned About AIDS."
Theoretical basis: Not reported.
Setting: College classroom.
Exposure: 45 minutes.
Staff: Media‐based, unclear what staff facilitated the program. 2: Abstinence‐only intervention ("Abstinence"). One session. Format, setting, theoretical basis, exposure, and staff same as above. Concepts included abstinence, the biology and symptoms of AIDS, transmission, and prevention. the intervention did not promote condom use or discussing safe sex with partners. Participants received a 7‐page written health education program (adapted from the North Carolina Board of Education senior high school AIDS curriculum); they then watched the video "AIDS: What everyone should know" (from Aims Media in Los Angeles). They also received a brochure about AIDS transmission and prevention (from the Fort Bragg Dependents' School System). 3: Safe‐sex intervention ("Decision"). Format, staff, exposure, theory, and setting as above, but the intervention "presented safe sex and described it as an alternative to abstinence." the written curriculum was adapted from the American Red Cross AIDS program for senior high school students. the video was "Letter from Brian," from the American Red Cross. the brochure "AIDS: the Facts" was also from the American Red Cross. 4: Nonintervention control. |
|
| Outcomes | Number of times used condoms in past 6 weeks Number of times had sex in past 6 weeks Number of sex partners in the past 6 weeks |
|
| Notes | Funding: Not reported. All interventions were based on pre‐existing programs. This was the only study to enroll participants older than adolescence. Condom use outcome measured the number of times participants used condoms, not the proportion of sexual acts that were protected. No data for cost or participant satisfaction. Participants received course research credits for participation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Hewitt 1998.
| Methods | RCT, Abstinence‐plus (Africentric) vs. Abstinence‐plus (Generic) vs. Attention Control. Unit of randomization: Individual. Method of randomization: Not reported. Data collection: Self‐report questionnaire, completed in group settings in classrooms, administered by project assistants who were not intervention facilitators. Code numbers to protect confidentiality. Assessment times: Baseline, immediately post‐intervention, and 3m. Complete case analysis. Attrition: 4% at 3m. Attrition analyses not reported. Group equivalence: No explicit statement of baseline differences was provided. Controlled for baseline values as covariates in analyses. |
|
| Participants | Philadelphia, PA (USA) N = 124 Mean age 13.19 yrs Ethnicity: 100% African‐American. SES: Not reported. 38.7% Male. Notes on recruitment: Adolescents in 7th through 9th grade were recruited via 6 community‐based organizations. 15 Hispanic adolescents also participated in the intervention, but analyses were limited to African‐American participants. Participants were paid for participating in the intervention and 3m follow‐up. |
|
| Interventions | 1: "Healthy Living" (Generic). Delivered in small groups of 7‐8 adolescents. Designed to increase knowledge about STIs and AIDS and the belief that abstinence as a teen is the best way for adolescents to prevent HIV. Condom use was mentioned, but abstinence was emphasized. Concepts included STI/HIV information, goal beliefs, self‐efficacy, information on needle‐sharing risks, limit‐setting, goal‐setting, and identifying obstacles to goals. Activities included videos, roleplays, small group discussions, games, exercises, and skill building activities.
Theoretical basis: Theory of planned behavior, social cognitive theory.
Setting: School (not during school time).
Exposure: 1 session, 5 hours long.
Staff: Each group led by 1 adult or 2 peer facilitators. Staff for all 3 arms included 9 adults (mean age 41.5 years, 100% African‐American), and 18 high school seniors (mean age 17.07 years, all but one African‐American). All had prior experience with small group facilitation. 2: "Healthy Living ‐ Harambee" (Africentric). Format, exposure, theory, staff, concepts, activities, and setting same as above, but program was designed to have an Africentric focus. Rooms were decorated with a map of Africa and posters to reinforce African cultural pride, facilitators wore traditional African clothing or colors, activities integrated four African/African‐American proverbs. HIV prevention methods were delivered in a way that stressed communalism, mutual cooperation, community empowerment, and cultural relevance; HIV prevention was presented as a collective and individual responsibility. 3: Name not reported. the intervention included the same activities, format, staff, setting, and exposure as the intervention condition, but focused on general health instead of HIV. Concepts included heart disease, cancer, and hypertension. Discussions did not include any topics related to HIV or AIDS. Activities included videos, discussions, games, exercises, and skill‐building activities for nutrition and aerobic exercise. |
|
| Outcomes | Log‐transformed number of days participants reported unprotected vaginal sex in the past 3m among all participants Vaginal intercourse in last 3m among all participants Log‐transformed number of days participants reported having vaginal sex in last 3m among all participants Frequency of condom use in past 3m scored on Likert scale 1 (never) ‐ 5 (always) among participants reporting vaginal sex in the past 3m Knowledge of AIDS, STDs, HIV, and pregnancy among all participants |
|
| Notes | Funding: Not reported. Intervention based on Be Proud! Be Responsible!, similar to Jemmott 1992, Jemmott 1998, Jemmott 1999, Jemmott 2004, Kennedy 2000a, Kennedy 2000b. Study was a Ph.D. dissertation, advised by the first study author from Jemmott 1992, Jemmott 1998, and Jemmott 1999. Participants were given $45 for participating ‐ $20 for intervention and $25 for 3m assessment. Lacked explicit statement of baseline differences. No cost data reported. Participant evaluations were consistently and significantly higher for the Generic than the Africentric condition. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Jemmott 1992.
| Methods | RCT, Abstinence‐plus vs. Attention Control. Unit of randomization: Individual, stratified by age. Method of randomization: Not reported. Data collection: Self‐report questionnaires administered in group setting by program staff. Assessment times: Baseline, immediately post‐intervention, and 3m. Complete case analysis. Attrition: 4% at 3m. Attrition did not differ by condition. Group equivalence: No explicit statement of baseline differences. Controlled for baseline values as covariates in analyses. |
|
| Participants | Philadelphia, PA (USA) N = 157 Mean Age 14.64 yrs SES: "Low income" communities. Ethnicity: 100% African‐American. 100% Male. Notes on recruitment: Invited outpatients at medical clinic (formed 44% of sample), students in grades 10‐12 at assemblies at local high schools (32%), and youth at a local community center (24%). Participants were paid for participating in intervention and for 3m follow‐up. |
|
| Interventions | 1: Be Proud! Be Responsible!. Out‐of‐school program delivered in small groups in one 5‐hr session. Aims to weaken problematic attitudes toward risky behavior. Concepts included abstinence, condom use, and factual AIDS information. Activities included videos, games, exercises, roleplays, and condom demonstration.
Theoretical basis: Theory of reasoned action.
Setting: School (on Saturday).
Exposure: 1 session, 5 hours long.
Staff: African‐American adults (mean age 36.2 yrs), including men and women with backgrounds in sex education, nursing, counseling, or social work. 2: Attention Control. Same exposure, activities, and staff as above (different facilitators were trained separately to deliver each program type), but focused on career opportunities. Delivered in small groups in one 5‐hour session. Discussions focused on career planning, career analysis. Activities included videos, games, and a value‐awareness exercise. |
|
| Outcomes | Number of days respondent did not use condom during coitus in past 3m among all participants Coitus in past 3 months among all participants Number of days participant had coitus in past 3m among all participants Incidence of heterosexual anal sex in past 3m among all participants Number of days respondent had heterosexual anal sex in past 3m among all participants Number of coital partners in past 3m among all participants Number of female anal sex partners in past 3m among all participants Frequency of condom use in past 3m scored on Likert scale from 1 (never) to 5 (always) among sexually active Risk behavior index among all participants (averaged z scores from behaviors in previous 3m, including coitus, multiple sexual partners, condom use, and heterosexual anal intercourse) AIDS knowledge among all participants |
|
| Notes | Funding: American Foundation for AIDS, National Institute of Child Health and Human Development. Intervention based on Be Proud! Be Responsible! program, similar to Hewitt 1998, Jemmott 1998, Jemmott 1999, Jemmott 2004, Kennedy 2000a, Kennedy 2000b. No explicit statement of baseline differences. Follow‐ups showed no within‐group differences in knowledge, attitudes, intentions, and behavioral outcomes by facilitator. No cost data provided. Participants in both conditions rated programs highly for enjoyment, their learning from the activities, and the feeling that the programs will help them in the future. No differences between groups except that those in AIDS intervention considered themselves more likely to recommend the program to others. Participants were paid $40 for participating: $15 for intervention and $25 for follow‐up attendance. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Jemmott 1998.
| Methods | RCT, Abstinence‐plus (Abstinence‐focused) vs. Abstinence‐plus (Condom‐focused) vs. Attention Control. Unit of randomization: Individual. Method of randomization: Computer‐generated and blind. Data collection: Confidential self‐report questionnaires administered by blinded proctors in group settings (school rooms with blackboards). Participants signed agreements to answer truthfully. Assessment times: Baseline, immediately post‐intervention, 3m, 6m, and 12m. Complete case analysis. Attrition: 3.5% at 3m, 5.6% at 6m, 7.4% at 12m. 1.8% did not attend both intervention sessions, but remained in the analysis. Attrition did not differ significantly by intervention group. Returnees at 3m follow‐up scored significantly higher in baseline condom prevention beliefs than non‐returnees; returnees at 6m follow‐up scored significantly higher in baseline abstinence prevention beliefs than non‐returnees; and returnees at 6m follow‐up scored significantly lower in baseline condom‐use knowledge than non‐returnees. These variables did not interact with the intervention to affect outcome measures, according to hierarchical multiple regression analyses. Group equivalence: Condom‐focused group had significantly greater condom use knowledge than other two groups at baseline (p = 0.02). This was controlled for in analyses for which it proved a significant predictor. No other baseline differences on pre‐intervention measures of conceptual variables, sexual behavior, or demographics between abstinence‐plus and control group. All analyses controlled for baseline values. |
|
| Participants | Philadelphia, PA (USA) N = 659 Mean age: 11.8 yrs Ethnicity: 100% African‐American. SES: "low‐income" communities. 47% Male. Notes on recruitment: Recruited youth from 6th and 7th grade classrooms in 3 middle schools (made announcements in assemblies, classrooms, and cafeterias, and sent letters to parents and guardians). Participants were paid for participating in intervention and for each follow‐up assessment. |
|
| Interventions | 1: "Making a Difference," Abstinence‐focused. Out‐of‐school program delivered in small groups of 6‐8 participants. Designed to increase knowledge of HIV, strengthen beliefs supporting abstinence, and increase self‐efficacy and skills to resist pressures to have sexual intercourse. the interventions "acknowledged that condoms can reduce risks, but emphasized abstinence to eliminate the risks of pregnancy and STIs, including HIV." Concepts included factual information, self‐efficacy, refusal skills, community pride and responsibility. Activities included videos, discussions, games, brainstorming, experiential exercises, and skill‐building.
Theoretical basis: Social cognitive theory, Theory of reasoned action, theory of planned behavior.
Setting: School (on Saturday)
Exposure: Two 4‐hour sessions on consecutive Saturdays.
Staff: 25 African‐American adults (mean education: master's degree), and 45 peers (mean age: 15.6 yrs). Each facilitator was randomly assigned to only one intervention and trained separately. Adults facilitated groups alone, and youth facilitated in pairs. 2: "Making Proud Choices", Condom‐focused. Format, theory, setting, exposure, staff composition, activities, and concepts same as above. Designed to increase knowledge of HIV, enhance hedonistic beliefs about condom use, and increase self‐efficacy and skills to use condoms. the interventions "indicated that abstinence is the best choice but emphasized the importance of using condoms to reduce the risk of pregnancy and STIs, including HIV." Concepts and activities were the same as above. 3: Attention Control. Format, theory, setting, exposure, staff composition, and activities same as above. Instead of addressing HIV risks, intervention focused on general health concepts, including information about cardiovascular disease, stroke, and cancers. the intervention promoted healthy diet skills, aerobic exercise, and breast/testicular self‐exams, and the program discouraged smoking. |
|
| Outcomes | Incidence of unprotected intercourse in past 3 months among all participants Number of days on which the participant had sex without a condom in the past 3m among all participants Sexual intercourse in past 3 months among all participants Adjusted mean frequency of intercourse in past 3m among all participants Mean frequency of condom use on Likert scale from 1 (never) to 5 (always) in past 3m among all participants reporting vaginal sex in past 3m Consistent condom use in past 3m among sexually active Knowledge about HIV risk reduction among all participants |
|
| Notes | Funding: National Institute of Mental Health. Intervention based on Be Proud! Be Responsible! program, similar to Hewitt 1998, Jemmott 1992, Jemmott 1999, Jemmott 2004, Kennedy 2000a, Kennedy 2000b. Fidelity monitoring: Facilitators recorded the intervention activities that they completed, which ranged from 89% to 100%, with a mean of 99%. Percentage of activities implemented did not differ among the groups. Trainers monitored the intervention delivery. No cost data provided. Participants rated all interventions highly for enjoyment, which did not differ between treatment conditions. Participants with peer facilitators liked the interventions and their facilitators significantly more than did those with adult facilitators. Participants were paid $100 for participating: $40 for intervention and $20 for each follow‐up attendance. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Jemmott 1999.
| Methods | RCT, Abstinence‐plus vs. Attention Control. Unit of randomization: Individual, stratified by gender and age. Method of randomization: Assignment by computer‐generated random number sequences. Data collection: Self‐report questionnaires administered by program staff, included honesty appeal based on social responsibility. Assessment times: Baseline, immediately post‐intervention, 3m, and 6m. Complete case analysis. Attrition: 3.2% at 3m, 7.3% at 6m. Attrition did not differ significantly by group. Returnees at 6m more likely to have had high pre‐intervention hedonistic beliefs about condoms, to have not reported coitus in the previous 3m at baseline, and to be younger than non‐returnees. Group equivalence: No explicit statement of baseline differences. Controlled for baseline values as covariates in analyses. |
|
| Participants | Trenton, NJ (USA) N = 496 Mean age 13.2 yrs Ethnicity: 100% African‐American. SES: Drawn from low‐income area (44.1% area households with children under 18 yrs are female‐headed, 67.8% of these are under 125% of federal poverty level). 46.2% Male. Notes on recruitment: Recruited from public schools via announcements in 7th and 8th grade assemblies and lunch periods. Participants were paid for taking part in the intervention and for follow‐up assessments. |
|
| Interventions | 1: "Be Proud! Be Responsible!" Out‐of‐school program delivered in small groups of 6‐8 participants. Concepts included abstinence, knowledge of STI and HIV risks, condom skills, hedonistic beliefs about condom use, condom negotiation, and risks of sharing drug paraphernalia. Activities included group discussions, games, videos, experiential exercises, skill‐building activities.
Theory: Social cognitive theory, theory of reasoned action, theory of planned behavior.
Setting: School (on Saturday)
Exposure: One 5‐hour session.
Staff: Adults (mean age: 36 yrs, had bachelor's degree or above, backgrounds in health education, counseling, nursing, social work). Staff were varied systematically to either match or differ from the gender and race of participants. Participant groups were also systematically varied to be either mixed or same‐sex. 2: Attention Control. Same format, theory, exposure, activities, setting, and staff as intervention, but focused on general (non‐sexual) health. Structurally equivalent to the intervention, delivered in small groups of 6‐8 participants. Concepts included heart disease, stroke, hypertension, cancers, and factual info on diet, exercise, and smoking cessation. Activities included group discussions, videos, games, diet analysis, pulse monitoring, and skill‐building. Separate facilitators delivered each intervention. |
|
| Outcomes | Number of days on which the participant had sex without a condom in the past 3m among all participants Coitus in past 3m among all participants Incidence of anal intercourse in past 3m among all participants Number of days respondent had anal sex in past 3m among all participants Number of coital partners in past 3m among all participants Number of anal sex partners in past 3m among all participants Sexual behavior index among all participants in past 3m (based on log unprotected sex, log number of partners, log frequency of anal sex, and log number of anal sex partners) HIV risk‐reduction knowledge among all participants |
|
| Notes | Funding: National Institute of Child Health and Human Development, National Institute of Mental Health. Intervention based on Be Proud! Be Responsible! program, similar to Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 2004, Kennedy 2000a, Kennedy 2000b. There was little effect on behavioral outcomes to support the hypotheses that matching facilitators to participants by gender and/or race leads to a more protective intervention effect. Mixed evidence was found for the effects of delivering the intervention to single‐gender (rather than mixed‐gender) participant groups. No cost data provided. Participant satisfaction was high for all groups, did not differ significantly by whether facilitators matched participants' gender or ethnicity for facilitator. Satisfaction also did not differ significantly by whether participants received the intervention in single‐sex or mixed‐gender groups. Participants were paid $60 for participation ‐ $20 for intervention, $20 for each follow‐up assessment attendance. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Jemmott 2004.
| Methods | RCT, Abstinence‐plus vs. Attention. Unit of randomization: Community center. Method of randomization: Unclear. Data collection: Unclear, but probably written surveys. Assessment times: baseline, 3m, 6m, 12m. Complete case analysis. Attrition: 9% missed every follow‐up. No attrition analyses. Group equivalence at baseline: No explicit statement of equivalence, but analyses controlled for baseline behaviors. |
|
| Participants | NJ and Philadelphia, PA (USA) N = 3448 randomized in 86 NGOs, 1707 participants randomly selected for assessment. Mean age: 14.8 Ethnicity: 83% African‐American, 13% Latino,1% white SES: unclear 43% male Notes on recruitment: Youth recruited through community‐based organizations. |
|
| Interventions | 1: "Be Proud! Be Responsible!" Out‐of‐school program delivered in small groups of 6‐8 participants. Concepts included abstinence, knowledge of STI and HIV risks, condom skills, hedonistic beliefs about condom use, condom negotiation, and risks of sharing drug paraphernalia. Activities included group discussions, games, videos, experiential exercises, skill‐building activities.
Theory: Social cognitive theory, theory of reasoned action, theory of planned behavior.
Setting: School (on Saturday)
Exposure: One 5‐hour session.
Staff: Adults (mean age: 37.6 yrs, 95% had some college). 82% African‐American, 9% Latino, 7% white. 2: Attention. Same format as experimental, but focused on general health, not HIV. |
|
| Outcomes | "Unprotected coitus" "Frequency of coitus" Frequency of condom use, most likely among participants reporting sex in the past 3m Consistent condom use, most likely among participants reporting sex in the past 3m Condom use at last sex, most likely among participants reporting ever had sex |
|
| Notes | Funding: Unclear. Analyses controlled for clustering. Replication trial of Be Proud! Be Responsible!, but the first to evaluate the program as implemented by non‐governmental organization staff. Intervention based on Be Proud! Be Responsible! program, similar to Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Kennedy 2000a, Kennedy 2000b. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kennedy 2000a.
| Methods | RCT, Abstinence‐plus vs. Nonintervention.
Unit of randomization: Individual. Method of randomization: Not reported. Data collection: Self‐report written questionnaire. Questionnaires delivered in group settings; unique identifiers based on demographic information were used instead of participant names. Questionnaire administrators told participants that responses were voluntary and confidential, and trial staff encouraged honesty. Assessment times: for the intervention group ‐ baseline (T1), immediately after the intervention (T2, same day as T1), and 1‐month follow‐up (T3). for the control group ‐ T2 and T3. Complete case analysis. Attrition: 48.3%. Attrition higher in intervention group (52.7%) than in comparison group (42.9%). Dropouts reported significantly more sex in the past 30 days (p<0.05), lower intentions to use condoms during future sex among sexually active participants (p<0.05), and less skills in negotiating safer sex (p<0.01) than participants who were retained. Group equivalence: At baseline, intervention group scored significantly higher than control group on condom‐use intentions (p < 0.05). All analyses used multivariate ANOVAs. |
|
| Participants | Sacramento, CA (USA) n = 735 Mean age: 15.29 yrs Ethnicity: 24.9% White, 18.1% African‐American, 38.6% Hispanic, 18.4% Other. SES: Not reported 45.3% Male Notes on recruitment: Participants were recruited by self‐referral, coalition members, and community‐based organizations that served youth. the target participant group was sexually active adolescents aged 14‐18 who use condoms inconsistently, but adolescents who were not target audience members were not excluded. Participants were given $10‐15 in gift certificates as compensation for time and expenses for completing follow‐up questionnaires. |
|
| Interventions | 1: "Prevention Marketing Initiative Local Demonstration Project" (PMI), based on "Be Proud! Be Responsible" intervention. Tailored to fit target population of sexually active adolescents aged 14‐18 who use condoms inconsistently (videos and materials specific to African‐American adolescents were removed). Workshop activities included group discussions, games, lectures, videos, condom demos, roleplays, and other interactive exercises. Added emphasis on condoms as prevention against pregnancy and STIs in addition to HIV. Details of HIV biology were replaced with information about local services. Also added pledge to talk about HIV prevention to friends, urged condom carrying. Introduced self‐reward for safer behavior.
Theoretical basis: Theory of reasoned action.
Exposure: Ranged from 5‐9 hours, often took place in one day.
Setting: Community settings "ranging from detention centers to church basements."
Staff: "Near peers," trained by personnel who had received "training‐of‐trainer" instruction in "Be Proud! Be Responsible!". Most facilitators were women. 2: No intervention: wait‐list control. |
|
| Outcomes | Number of times participants had sex without a condom in the past 30 days, among "sexually active" participants Sex in the past 30 days, among "sexually active" participants Number of times participants had sex in the past 30 days, among "sexually active" participants Condom use at last sex, among "sexually active" participants HIV/AIDS knowledge among all participants |
|
| Notes | Funding: Not reported. Intervention based on Be Proud! Be Responsible! program, similar to Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Jemmott 2004, Kennedy 2000b. This evaluation is part of a 5‐site study, which also included Kennedy 2000b; each site evaluated a different version of the intervention. Fidelity monitoring: periodic observations and site visits by PMI staff. Facilitators noted distractions, omissions, and concerns after each workshop. Parental consent was waived in two of the five sites, although it is unclear whether this study was one of them. Participants received $10‐15 in gift certificates after participating in the follow‐up assessment. No cost or participation satisfaction data reported. the report stated that there was no organized community resistance to the programs. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kennedy 2000b.
| Methods | RCT, Abstinence‐plus vs. Nonintervention. Unit of randomization: Individual. Method of randomization: Not reported. Data collection: Self‐report written questionnaire. Questionnaires delivered in group settings; unique identifiers based on demographic information were used instead of participant names. Questionnaire administrators told participants that responses were voluntary and confidential, and trial staff encouraged honesty. Assessment times: for the intervention group ‐ baseline (T1), immediately after the intervention (T2, same day as T1), and 1‐month follow‐up (T3). for the control group ‐ T2 and T3. Complete case analysis. Attrition: 43.9% at 1 month. Attrition higher in intervention group (53.7%) than in comparison group (25.7%). Attrition analyses not provided, although "some differential attrition across conditions" was observed in the 5‐site design. Higher risk participants (e.g., those who were sexually active and/or reported lower levels of condom use and condom intentions) were "relatively unlikely" to be retained. Group equivalence: At baseline, intervention group participants scored significantly higher on abstinence beliefs, self‐efficacy, and talking to parents about HIV‐related risks (p < 0.05 for all comparisons). |
|
| Participants | Nashville, TN (USA) n = 535 Mean age: 14.43 yrs Ethnicity: 0.3% White, 77.4% African‐American, 16.9% Hispanic, 5.4% Other. SES: Not reported 40.7% Male Notes on recruitment: Participants were recruited by self‐referral, coalition members, and community‐based organizations that served youth. the target participant group was sexually active African‐Americans aged 12‐15 living in low‐income housing who want to avoid pregnancy and STIs, as well as sexually inactive African‐Americans age 12‐15 living in low‐income housing. Adolescents who were not target audience members were not excluded. Participants were given $10‐15 in gift certificates as compensation for time and expenses for completing follow‐up questionnaires. |
|
| Interventions | 1: "Prevention Marketing Initiative Local Demonstration Project" (PMI), based on Jemmotts' "Be Proud! Be Responsible" intervention. Tailored to fit target population of African‐Americans aged 12‐15 living in low‐income housing. Workshop activities included group discussions, games, lectures, videos, condom demos, roleplays, and other interactive exercises. Added emphasis on condoms as prevention against pregnancy and STIs in addition to HIV, added emphasis on the benefits of delaying sex and abstinence. Details of HIV biology were replaced with information about local services. Participants were also asked to interview an adult about what it had been like to be a teenager. Parents were offered a 1‐hour session.
Theoretical basis: Theory of reasoned action.
Exposure: Ranged from 5‐9 hours, often took place in one day.
Setting: Community settings "ranging from detention centers to church basements."
Staff: Trained by personnel who had received "training‐of‐trainer" instruction in "Be Proud! Be Responsible!", had several years of experience working with youth. Most facilitators were women. 2: No intervention: wait‐list control. |
|
| Outcomes | Number of times participants had sex without a condom in the past 30 days, among "sexually active" participants Sex in the past 30 days, among "sexually active" participants Number of times participants had sex in the past 30 days, among "sexually active" participants Condom use at last sex, among "sexually active" participants HIV/AIDS knowledge among all participants |
|
| Notes | Funding: Not reported. Intervention based on Be Proud! Be Responsible! program, similar to Hewitt 1998, Jemmott 1992, Jemmott 1998, Jemmott 1999, Jemmott 2004, Kennedy 2000a. This evaluation is part of a 5‐site study, which also included Kennedy 2000a; each site evaluated a different version of the intervention. Fidelity monitoring: periodic observations and site visits by PMI staff. Facilitators noted distractions, omissions, and concerns after each workshop. Parental consent was waived in two of the five sites, although it is unclear whether this study was one of them. Participants received $10‐15 in gift certificates after participating in the follow‐up assessment. No cost or participation satisfaction data reported. the report stated that there was no organized community resistance to the programs. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kirby 1997.
| Methods | RCT, Abstinence‐plus vs. Usual Care. Unit of randomization: Classroom. Method of randomization: Not reported. Data collection: Confidential self‐report surveys in English or Spanish completed in class at baseline and 5m. At 17m, students were pulled from their classes during prearranged times and administered the survey on school premises. Several students were surveyed after school or by mail. Assessment times: Baseline, 5m, 17m. Complete case analysis. Attrition: 27% at 5m, 23% at 17m. Among youth lost for any reason, similar proportions were lost from treatment and control groups. Group equivalence: No baseline differences at the .01 significance level |
|
| Participants | Los Angeles, CA (USA) n = approx 2099 participants, 102 classrooms, 6 schools. (Number of baseline participants approximated from given attrition rates and number of participants analyzed.) Mean age: 12.3yrs. Ethnicity: 64% Latino, 13% Asian, 9% African‐American, 5% White. SES: Not reported. 46% Male. Notes on recruitment: 6 middle schools in Hollywood‐Wilshire and Central areas of LA were recruited. Nearly all 7th grade teachers participated, including 102 classrooms. 99% of included students were in 7th grade. |
|
| Interventions | 1: "Project SNAPP (Skills and kNowledge for AIDS and Pregnancy Prevention)." This intervention was delivered in addition to school's regular health education curriculum. Objectives were to prevent unintended pregnancy and HIV by delaying onset of intercourse (primary goal) and increasing condom use. Concepts included social influences, assertive communication, resistance skills, myths about HIV and pregnancy, risk recognition, barriers to abstinence and condom use, community resources. Activities included demonstrations, discussions, roleplays, games, large and small group activities, question and answer activities, personal stories of educators, making personal decisions.
Theoretical basis: Social learning theory, health belief model.
Setting: Middle school classes.
Exposure: 8 sessions over 2 weeks.
Staff: 3 males and 7 females ranging in age from 15 to 22. 5 were teen mothers, 2 were HIV+. 2: Usual care: School's regular curriculum only, without additional SNAPP program. |
|
| Outcomes | Ever been told by a doctor or nurse that had an STD, among all students who had never been diagnosed with STD at baseline Ever been pregnant or gotten someone pregnant, among all participants never reporting a pregnancy at baseline Number of times had sex in previous 3 months among sexually experienced participants Number of people with whom participants had sex in past 12m, among sexually experienced participants Condom use at last sex, among participants who report ever having sex Sexual initiation among participants who reported being sexually inexperienced at baseline Change in knowledge among all participants |
|
| Notes | Funding: California Wellness Foundation. No specific statement of baseline enrollment n. Analyses used a Bonferroni correction to control for multiple statistical tests. Analyses were conducted on the level of individual participants; had significant effects been found, confirmatory multi‐level analyses would have controlled for clustering. Fidelity monitoring: Peer leaders received ongoing training and supervision. Unclear if baseline differences existed at the p < 0.05 significance level. No cost data or participant satisfaction data provided. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Markham 2006.
| Methods | RCT, Abstinence‐plus vs. Usual care. Unit of randomization: School. Method of randomization: Random numbers table. Data collection: ACASI Assessment times: baseline, 5m (ongoing assessments at 18 and 24m) Complete case analysis. Attrition: 8%, dropout higher in experimental arm. Group equivalence at baseline: Baseline differences (ethnicity), controlled in analyses. |
|
| Participants | Houston, TX (USA) N = 1307 students at 10 middle schools. Mean age: 12.5 Ethnicity: 44% African‐American, 42% Hispanic, 15% other. SES: low 43% male Notes on recruitment: Schools were recruited; participants were in 7th grade. |
|
| Interventions | 1: It's Your Game, Keep it Real." 12 sessions in 7th grade and 10 sessions in 8th grade. Includes classroom sessions and 4 individual CD‐ROM based assignments to individually tailor prevention messages. Focused on HIV and pregnancy. Included parent‐child homework.
Theoretical basis: Social cognitive theory.
Setting: Middle schools.
Exposure: 22 hours over 2 years
Staff: Adults. 2: Usual care defined by schools. |
|
| Outcomes | Any type of intercourse in the past 3 months among all participants Sexual initiation among all participants |
|
| Notes | Funding: National Institute of Mental Health. Analyses controlled for clustering. Ongoing trial; future assessments at 18 and 24 months. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
McBride 2000a.
| Methods | Quasi‐RCT, Abstinence‐plus vs. Nonintervention. Unit of randomization: Individual. Method of randomization: Group assignment was based on whether a participant had an even or odd birth date. Data collection: Self‐report surveys administered in group settings; individuals were surveyed later if absent for test. Format of these makeup surveys is unclear. Assessment times: Baseline and 8m. Complete case analysis. Attrition: 20% at 8m. Those lost to follow‐up were less likely to have mothers with high‐school education, more likely to have mostly Ds and Fs, more likely to have repeated a grade. Group equivalence: Treatment group significantly older at baseline (15.1 yrs treatment, 14.4 yrs control). Controlled for baseline values in analyses. |
|
| Participants | Washington state (USA) N = 166 Mean age: Treatment group 15.1 yrs, Control group 14.7 yrs. Ethnicity: This site was part of a 6‐site evaluation, in which 3 sites enrolled teenagers. for all 3 teenage sites combined, nonwhite participants constituted a mean 26% of the sample. SES: Not reported. 0% Male. Notes on recruitment: Agencies got funding from state to provide pregnancy prevention projects. Females aged 12‐17 were referred by school counselors, family planning clinics, and social service agencies because they were perceived to be at high risk for early sex and pregnancy. |
|
| Interventions | 1: Name not reported. Objectives were to provide education, support, and referrals to young women at risk for early sexual activity or pregnancy. Concepts included self‐esteem, sexuality, pregnancy, STIs, identifying and avoiding risky behavior, life planning, communication, decision‐making. Activities included weekly group meetings, individual sessions according to needs, referrals, identification of community resources, and some social events.
Theoretical basis: "Client‐centered approach," which included information and coping skills.
Setting: Middle schools and high schools.
Exposure: Weekly group meetings. Participants received mean 31 hours, median 25 hours, range 0‐140 hours over the 8 months.
Staff: Health and sexuality educators employed by Planned Parenthood. 2: Nonintervention control. Controls had 0 hours exposure. |
|
| Outcomes | Intercourse in past month among all participants Ever had intercourse among all participants |
|
| Notes | Funding: State of Washington Department of Health. This evaluation was one site in a 6‐site trial that also included McBride 2000b. of the remaining four sites, three enrolled younger participants and did not evaluate behavioral outcomes; one enrolled teenagers and did not appear to evaluate an abstinence‐based intervention. Coupons and pizza parties were used at some evaluation sites to help secure parental consent. Each program site received $40,000‐$50,000 per year (USD) to implement the program. Focus groups and word‐of‐mouth recruitment strategies suggested program acceptability and participant satisfaction. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
McBride 2000b.
| Methods | Quasi‐RCT, Abstinence‐plus vs. Nonintervention. Unit of randomization: Individual. Method of randomization: Group assignment was based on whether a participant had an even or odd birth date. Data collection: Self‐report surveys administered in group settings; individuals were surveyed later if absent for test. Format of these makeup surveys is unclear. Assessment times: Baseline and 6m. Complete case analysis. Attrition: 32% at 6m. Those lost to follow‐up were less likely to have mothers with high‐school education, more likely to have mostly Ds and Fs, more likely to have repeated a grade. Group equivalence: No baseline differences. Controlled for baseline values in analyses. |
|
| Participants | Washington state (USA) N = 232 Mean age: This site was part of a 6‐site evaluation, of which 3 sites enrolled teenagers. for all 3 teenage sites combined, mean age = 15.4 yrs. Ethnicity: for all three sites, nonwhite participants constituted a mean 26% of the sample. SES: Not reported. 0% Male. Notes on recruitment: Agencies got funding from state to provide pregnancy prevention projects. Females aged 12‐17 were referred by school counselors, family planning clinics, and social service agencies because they were perceived to be at high risk for early sex and pregnancy. |
|
| Interventions | 1: Name not reported. Objectives were to empower young women, to improve their self‐esteem, and to help avoid early pregnancy by offering support, care, and safe place. Concepts included consequences of sexual behavior, family and friendships, healthy relationships, decision‐making, stress management. Activities included weekly group sessions, worksheets, videos, guest speakers, referrals, individual mentors 1 hr per week.
Theoretical basis: "Client‐centered approach," which included information and coping skills.
Setting: Schools and other community‐based settings.
Exposure: Weekly group meetings, 1hr per week mentoring. Participants received mean 22 hours, median 17 hours, range 0‐63 hours over the 6 months.
Staff: health and sexuality educators and social workers with local health department. 2: Nonintervention control. Mean exposure 0 hrs, but reported exposure for this group ranged from 0‐29 hours. |
|
| Outcomes | Intercourse in past month among all participants Ever had intercourse among all participants |
|
| Notes | Funding: State of Washington Department of Health. This evaluation was one site in a 6‐site trial that also included McBride 2000a. of the remaining four sites, three enrolled younger participants and did not evaluate behavioral outcomes; one enrolled teenagers and did not appear to evaluate an abstinence‐based intervention. Coupons and pizza parties were used at some evaluation sites to help secure parental consent. Each program site received $40,000‐$50,000 per year (USD) to implement the program. Focus groups and word‐of‐mouth recruitment strategies suggested program acceptability and participant satisfaction. It is unclear why controls received program exposure ranging 0‐29 hours. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Moberg 1998.
| Methods | Quasi‐RCT, Abstinence‐plus (delivered in 1 year) vs. Abstinence‐plus (delivered over 3 years) vs. Usual Care. Unit of randomization: School, stratified into 2 levels based on whether they could feasibly deliver a 1‐year or 2‐year program, then stratified into 3 levels by reported student substance use. Method of randomization: Not reported. Data collection: Self‐administered surveys completed either in class or by mail. Assessment times: Baseline, 1yr, 2yrs, 3yrs, and 4yrs. Complete case analysis. Attrition: 8% in 7th grade, 14% in 8th grade, 20% at 9th grade, and 32% at 10th grade for all 3 arms. Intensive program participants were underrepresented at 10th‐grade follow‐up. Group equivalence: No baseline differences by "most demographic characteristics," by several scales measuring relevant health attitudes and behaviors, or by alcohol, tobacco, and marijuana use. Parental education was significantly lower in the Age‐Appropriate group than in the Intensive or control groups; significantly fewer control participants reported having working mothers than the two intervention groups. Analyses controlled for baseline values of all outcomes. |
|
| Participants | Wisconsin (USA) N = 2483 participants, 21 schools. Age: 6th grade at pretest (approx 11.5 yrs). At 9th grade posttest, 68% were 14 yrs and 29% were 15 yrs. Ethnicity: 96% White, 4% Other. SES: 86% have fathers working full time, 52% have mothers working full time. 48% Male. Notes on recruitment: Schools in small cities and towns were recruited, and randomization was stratified based on whether the schools indicated that they could provide a one‐year intervention (Intensive) or three‐year intervention (Age‐Appropriate). Within each of these 2 categories, schools were randomly assigned to either receive the intervention or serve as a control. |
|
| Interventions | 1: "Healthy for Life" ‐ Intensive. Objectives were that students would not have sex, and that when students do eventually have sex, they will use protection to avoid pregnancy and STIs. Concepts included understanding social situations, developing refusal skills, clarifying parental values, media analysis, communicating with parents and opposite sex, body image, responsibility for health behaviors, risks of early sex, sexuality facts, birth control information, and anonymous questions. Activities included in‐class lessons, parent‐child homework assignments, home mailings to parents, refusal skill raining, peer leaders, health advocacy, media analysis, public commitments to health, and student feedback. Only one program lesson in the sexuality unit concerned condom use, with more emphasis on abstinence. Some community activities took place, but these did not generally deal with sex because of community resistance.
Theoretical basis: Social influences theory.
Setting: Middle school classrooms.
Exposure: 54 lessons over 12 weeks in 7th grade.
Staff: Healthy for Life teachers that were hired, trained, and supervised by research team. Each HFL teachers was paired with participating school teacher. Material was presented by both teachers, but HFL teachers commonly presented more of the sexuality education lessons. Each classroom elected 3 peer leaders from the class to deliver approximately one third of the curriculum. 2: "Healthy for Life" ‐ Age Appropriate. All details same as above, except that the 54 class sessions were delivered over the course of 3 years (grades 6‐8). Program exposure occurred for 4 weeks during each year of middle school. 3: Usual care health education programming as dictated by the schools. Sometimes these included prevention‐oriented curriculum like Quest, Values and Choices, and Here's Looking at You 2000. Healthy for Life was delivered to control schools for a subsequent cohort of students. |
|
| Outcomes | Sexual intercourse in the past month among all participants Consistent condom use among participants reporting sexual intercourse ever Ever had sexual intercourse among all participants |
|
| Notes | Funding: National Institute on Drug Abuse; Robert Wood Johnson Foundation. Program fidelity was challenged by community opposition groups, which required the omission of sexuality messages from many planned community‐wide program activities. In one classroom, a member of the community opposition group attended every program lesson with content related to sexuality. Fidelity monitoring by teacher logs regarding implementation of each lesson, observation by trained observer of a sample of all implementations, and intensive interviews with program staff, teachers, administrators, and students. Cost data not provided. Focus groups and feedback surveys suggested that the Age‐Appropriate group tired of program messages after the third program year. Analyses controlled for unit of randomization. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
O'Donnell 2002.
| Methods | RCT, Abstinence‐plus enhanced (with community service) vs. Abstinence‐plus non‐enhanced (without community service).
Unit of randomization: Classroom. Method of randomization: Not reported. Data collection: Self‐report questionnaires completed in school. Assessment times: Baseline, 6m, 3.9yrs. Complete case and Treatment‐on‐the‐treated analyses. Complete case analyses excluded the 52 students who deviated from assigned randomization sequence after the program's first year, but grouped participants by original assignments. Treatment‐on‐the‐treated analyses grouped participants based on years of program exposure, but used carry‐forward data to approximate outcomes for dropouts. No analysis imputed data for dropouts AND analyzed participants in their original trial arms (which would have been intention‐to‐treat). Attrition: 23.5% at 3.9yrs. Attrition was higher among boys, but dropouts' reports of sexual initiation and recent sex did not differ at baseline from returnees (controlling for gender). Conducted carry‐forward analysis to confirm results and still found significant effects for initiation and recent sex. Group equivalence: No significant baseline differences in sexual behavior. Analyses were performed on change scores controlling for gender, ethnicity, and sexual initiation at baseline. |
|
| Participants | Brooklyn, NY (USA) N = 225 students, 18 classrooms. Mean age: 12.4 yrs. Ethnicity: 71% African‐American, 26% Latino, 3% other. SES: "economically disadvantaged" area 40.5% Male. Recruitment notes: Included 7th grade class of a public middle school in 1994; only those who completed the 1994 baseline survey were eligible for follow‐up assessment in 1998. Originally, the study included a usual care group that did not receive the in‐school curriculum or community service, but this control group was not randomly assigned. |
|
| Interventions | 1: "Reach for Health" with Community Youth Service (CYS) component. In‐class curriculum with mandatory extracurricular community volunteer service in nursing homes, daycare centers, and local clinics. Concepts included risks of unprotected sex, violence, and substance use. Service program focused on learning about service organizations, setting goals, and considering students' own attitudes about other groups. Activities included in‐class instruction, interactive activities, communication skills, goal‐setting, in‐class debriefing on service experiences, and volunteer service in nursing homes, community health centers, childcare facilities.
Theoretical basis: Not stated.
Setting: Public middle schools, volunteer service in various community locations.
Exposure: Curriculum consisted of 40 class sessions in 7th grade and 34 in 8th grade. 10 of these classes each year focused on healthy sexuality. CYS component consisted of 3hrs/week in service placements over 7th and 8th grades (approximately 90 service hours per year).
Staff: Middle school health teachers and placement site staff. 2: Reach for Health, without CYS component. In‐class curriculum as in condition 1, but no extracurricular volunteer component. Control students received the same 40 Reach for Health class sessions in 7th grade and the same 34 sessions in 8th grade. 10 of these classes each year focused on healthy sexuality. |
|
| Outcomes | Pregnancy among all participants not reporting pregnancy at baseline Sex in the past 30 days among all participants Ever had sex among all participants |
|
| Notes | Funding: National Institute of Child Health and Human Development. Analyses controlled for clustering. After year 1 of the program, the school expanded the CYS component to more students. This led to 32 students transferring into the intervention group and 16 transferring to the control group because CYS did not fit their schedules. Analyses were divided into youth receiving 2 program years, youth receiving 1 program year (i.e., those who transferred in or out after year 1), and no‐exposure controls. Fidelity monitoring by monthly site visits, observations of placement activities, and tracking attendance at placements and completion of classroom lessons. Technical assistance was provided to schools. Complete case analyses using original baseline assignments also showed trends towards protective effects on sexual initiation and recent sex, p < 0.10. A nonrandomized, usual care control group existed for the 6m assessment. RFH‐CYS participants (condition 1) were significantly less likely to report recent intercourse (last 3m) that control students. RFH‐only participants (condition 2) did not differ significantly from controls in reports of recent intercourse. Data for cost and participant satisfaction were not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Philliber 2001.
| Methods | RCT, Abstinence‐plus vs. Usual Care. Unit of randomization: Individual. Method of randomization: Sealed envelopes drawn by participants. Data collection: Annual self‐report surveys, knowledge tests, attendance records, and medical records (medical records for intervention group only). Assessments were scheduled at centers. Participants who did not attend scheduled assessments received phone calls and home visits. Assessment times: Baseline, 1yr, 2yrs, 3yrs. Complete case analysis. Attrition: 19.1% at 3yrs. Gender, age, and baseline sex were related to program attendance. At 36m, more program teens did not live with either parent and fewer were Latino; 70% of intervention group participants were still involved at some level in the program. Group equivalence: Baseline equivalence for demography, SES, grades, family relationships, and previous participation in after‐school programs. |
|
| Participants | 12 sites in New York, Maryland, Texas, Florida, Oregon, and Washington (USA) N = 1163 Mean age: 14.3 yrs. Age range 13‐15yrs. Ethnicity: 42.5% African‐American, 3% Caribbean Black, 29.0% Hispanic, 5.5% White, 3.5% Asian, 14.0% Multi‐Ethnic, 2% Other. SES: 53.5% of participants' families had no adult employed, received entitlements, or both. 45.0% Male. Notes on recruitment: Recruited individuals by community mailings, flyers, and outreach in schools and community. Paid youth for completing assessments. Eligible if not enrolled in ongoing structured after‐school program with a regular meeting schedule, aged 13‐15 on July 1, 1997 (for New York sites), or aged 13‐15 on January 1, 1998 (for other sites). Ineligible if pregnant, already parents, or enrolled in another youth program. Participants received cash, metro cards, T‐shirts, walkmans, bookbags, etc for attending assessments. |
|
| Interventions | 1: "Children's Aid Society Carrera Program." After‐school program meeting daily during the school year, including free medical care and summer booster sessions. Concepts included job assistance, sex education, arts, sports, mental health, medical care, and pregnancy prevention. Activities and services included Job Club, academic component, weekly arts classes, weekly family life and sexuality education, weekly mental health discussion groups, individual counseling as needed, annual medical exam, STI testing, free condoms.
Theoretical basis: Not reported.
Setting: Community centers.
Exposure: 3 hrs per day during school year, summer booster sessions and mentoring. Program lasted all 3 years.
Staff: Healthcare workers, full‐time coordinator at each site. 2: Usual care ‐ usual youth center offerings (generally occurred at the same community centers, but the Carrera program was not offered to control participants). Exposure varied. Most community centers offered some recreational activities, homework help, and drop‐in centers. None had health care services on site. |
|
| Outcomes | Became pregnant or caused pregnancy among all participants Condom use at last sex among all participants who reported having had sex Ever had sex among all participants |
|
| Notes | Funding: Charles Stuart Mott Foundation, Robin Hood Foundation. Unclear how sealed envelopes were prepared. Monitored participant attendance; attended mean 12 hours per month. Cost data included for 6 New York sites: Carrera program cost $4000 per year for each teen enrolled ‐ $16 per participant per day. Logs suggest that program nonattendance by participants was usually not voluntary, and that sometimes parents would punish their children by making them miss program days. Participants received cash, metro cards, T‐shirts, Walkmans, bookbags, etc for participating in data collection. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Sikkema 2005.
| Methods | RCT, Abstinence‐plus (enhanced) vs. Abstinence‐plus (non‐enhanced) vs. Information Unit of randomization: Housing development. Method of randomization: Not reported. Data collection: ACASI. Assessment times: Baseline, 9m, 18m Complete case analysis. Attrition: 26% at 9m, 35% at 18m. Attrition higher among riskier participants (older, had lived in developments for less time, more likely to have had sex, used tobacco, used alcohol, used illicit drugs, and to have had a STI). Attrition did not differ between trial arms. Group equivalence at baseline: No significant baseline differences. |
|
| Participants | Sites in Milwaukee and Racine (WI), Roanoke (VA), Seattle and Tacoma (WA) N = 1172 youth in 15 housing developments. Mean age=14.5 Ethnicity: 51% African‐American, 20% Asian, 10% East African, 3% White, 3% Hispanic, 3% Ukrainian, 2% Russian, 1% Native American, 5% Other SES: low 50% male Notes on recruitment: Participants recruited through housing developments via written announcements, phone contacts, and door‐to‐door recruitment. |
|
| Interventions | 1: Community involvement. Participants attended workshops: small group program delivered in same‐gender groups. Included brochures, free condoms, skills training, HIV/STI education, sexual negotiation skills, condom use skills, personal pride, and self‐respect. After the workshops, participants received 2 follow‐up sessions, formed a Teen Health Project Leadership Council (THPLC) with natural opinion leaders, had a number of THPLC‐led activities and events, and received sessions offered to parents. Attendance rate was 86.2% (percentage of participants attending any sessions).
Theoretical basis: social cognitive theory, theory of reasoned action, theory of planned behavior, social learning theory
Setting: Community centers
Exposure: 6 hours over 2 weekly sessions.
Staff: Ault leaders. 2: Workshops only. Same as 1, but program ended with the workshops. Small group program delivered in same‐gender groups. Included brochures, free condoms, skills training, HIV/STI education, sexual negotiation skills, condom use skills, personal pride, and self‐respect. No parent involvement. Attendance rate was 87.2% (percentage of participants attending any sessions). 3: Information. Participants were invited to one AIDS education session that included a video, condoms, and educational brochures. Attendance rate was 15%. |
|
| Outcomes | Condom use at last sex among participants reporting ever having had sex Sexual initiation among participants who reported being sexually inexperienced at baseline Additional data collected, but not reported: HIV/AIDS knowledge Number of partners STD incidence |
|
| Notes | Funding: National Institute of Mental Health. Analyses controlled for clustering. Reported ICC. Participants received $15 per survey completion. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Smith 1994.
| Methods | RCT, Abstinence‐plus (written materials with skills training and multiple sessions) vs. Information (written materials on contraception and sexual decision‐making). Unit of randomization: Individual. Method of randomization: Not reported. Data collection: Self‐report written questionnaire completed in school. Assessment times: Baseline, immediate post‐intervention, 6 months. Complete case analysis. Attrition: 20.8%. Attrition more likely in experimental group (18 intervention participants compared to 7 controls), significance not reported. Group equivalence: No baseline differences. |
|
| Participants | New York, NY (USA) N = 120. Mean age: 15.1 yrs. Ethnicity: 43.3% African‐American, 30.8% West Indian, 22.5% Hispanic, 3.3% Other. SES: Inner city school. 25.8% Male. Notes on recruitment: All consenting member of the 1989 freshman class at an inner‐city Queens high school were recruited. |
|
| Interventions | 1: "Teen Incentives Program." 6‐month after‐school program with three phases. Phase I: weekly meeting in small group of 10‐20 youth. Concepts: self‐esteem, communication, social skills, decision‐making, academic performance, career planning, parent relationships, peer influences, substance abuse, sexuality, STIs, pregnancy, and sexual responsibility. Phase II: 6‐week career mentorship that involved spending time with a healthcare professional. Exposure unclear. Phase III: practicing skills in small‐group format, including role‐playing, writing, and acting out skits. Exposure unclear.
Theoretical basis: Not stated.
Setting: School and mentorship placement.
Exposure: 6 months total. 8 weekly 1‐hour sessions in Phase I, 6 weeks of mentorship in Phase II, Phase III unclear.
Staff: Not stated. 2: Abstinence‐plus non‐enhanced. Participants were put on waiting list and given minimum intervention in the form of written materials on contraception and sexual decision making. |
|
| Outcomes | Absolute sexual frequency ‐ instances of completed sexual activity during past 2m, among all participants | |
| Notes | Funding: Not reported. No data provided for cost or participant satisfaction. Potential for contamination was not addressed (all participants attended school together, but were randomized as individuals). Little information was provided about actual intervention (e.g., exposure, staff). No fidelity monitoring reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
St Lawrence 1995a.
| Methods | RCT, Abstinence‐plus enhanced (multiple sessions with skills training) vs. Abstinence‐plus non‐enhanced (one session without skills training). Unit of randomization: Individual. Method of randomization: Not reported. Data collection for sexual behaviors: Self‐report questionnaire administered in written format. Code numbers used to protect participants' confidentiality. Sexual assertion and peer education skills were assessed using roleplays. Assessment times: Baseline, 2m (immediately post‐intervention), 8m, and 14m. ITT analysis, imputed values for dropouts based on mean values for intervention condition at the same assessment. Attrition: 8.5% at 12m, primarily due to relocation. No significant differences between those retained and lost. Group equivalence: No baseline differences between intervention conditions. |
|
| Participants | Jackson, MS (USA) N = 246 Mean age: 15.3yrs. Ethnicity: 100% African‐American. SES: 82% of patients at the health center received Medicaid. 28% Male. Notes on recruitment: Collaborated with public health service center serving low‐income minority participants, and gave brochures to all African‐American patients between 14‐18yrs who had no active symptoms of AIDS. Participants were paid $5 per hour for participation. |
|
| Interventions | 1: "Becoming a Responsible Teen" with behavioral skills training. Weekly sessions at a community healthcare facility, delivered in groups of 5‐15 youth. Concepts included HIV/AIDS information, the continuum of risky activities, the relevance of HIV to African‐American communities, communication skills, abstinence, condom use, values and decisions, the prevalence of teen sex, and risk recognition. Activities included roleplays, skills training, condom practice, games, communication skills, HIV+ youth speakers from community, identifying social support mechanisms, and personally identifying positive life changes.
Theory: Social learning theory, self‐efficacy theory.
Setting: Community healthcare facility.
Exposure: 1 session per week (90‐120 mins) for 8 wks.
Staff: Male‐female pair of adult facilitators. 2: Non‐enhanced program version: "Becoming a Responsible Teen" without behavioral skills training. One‐time session provided information and advised abstinence, but program was limited in exposure and did not focus on skills for communication or condom use. Delivered in groups of 5‐15 youth. Concepts included information about HIV/AIDS, abstinence, continuum of risky activities, relevance of HIV to African‐American communities. Activities included didactic instruction, games, group discussion. Delivered in small groups of 5‐15 youth. Setting: Community healthcare facility. Exposure: One 2‐hour session. Staff: male‐female pair of adult facilitators. |
|
| Outcomes | Log(10) frequency of unprotected vaginal intercourse in past 2m among all participants Log(10) frequency of unprotected oral intercourse in past 2m among all participants Log(10) frequency of unprotected anal intercourse in past 2m among all participants Incidence of vaginal, oral, or anal intercourse in past 2 months among all participants Number of partners in past 2m among all participants Percentage of condom‐protected intercourse occasions in past 2m among participants reporting oral, anal, or vaginal intercourse Overall sexual behavior including number of sex partners, percentage of condom‐protected intercourse occasions, and log‐transformed frequencies of unprotected vaginal intercourse, condom‐protected vaginal intercourse, unprotected oral intercourse, unprotected anal intercourse, and condom‐protected anal intercourse AIDS knowledge test among all participants |
|
| Notes | Funding: National Institute of Mental Health. Bonferroni correction used to control for multiple statistical tests. No cost data provided. Participant satisfaction high for the experimental group; all participants indicated that they would recommend the program to their friends. Rigorous fidelity monitoring: All sessions were audiotaped and evaluated for adherence by the project director. Makeup sessions were provided for absent participants. Participants were paid $5 per hour for participation, and they received a T‐shirt and certificate for program attendance. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
St Lawrence 1995b.
| Methods | RCT, Abstinence‐plus enhanced (multiple sessions with skills training) vs. Abstinence‐plus non‐enhanced (one session without skills training). Unit of randomization: Cohort. Method of randomization: Not reported. Data collection for sexual behavior: Written self‐report questionnaire. Program records assessed STI treatment in past 2 months. Code names used to protect participants' confidentiality. Social skills assessed using roleplays. Assessment times: Baseline, 3.5m (2m after intervention ended). Intention‐to‐treat analysis. Attrition: 0%. Group equivalence: Intervention participants had lower scores on the Internal subscale of the Health Locus of Control Scale, attitudes toward HIV, condom attitudes, self‐efficacy, and perceptions of vulnerability to HIV. Controlled using repeated‐measures ANOVAs. |
|
| Participants | Jackson, MS (USA) N = 34 youth, 6 cohorts. Mean age: 15.6 yrs. Ethnicity: 84% white, 16% African‐American. SES: Not reported. 73% Male. Notes on recruitment: Participants were recruited from a residential treatment facility for substance‐dependent youths; none declined to participate. |
|
| Interventions | 1: Somewhat based on "Becoming a Responsible Teen" with behavioral skills training. Weekly sessions delivered in small groups. Concepts included HIV/AIDS information, abstinence, the risk continuum, risk education. Activities included roleplays, skills training, rehearsal, condom practice, games, communication and partner negotiation skills, assertiveness, and "contracts" to change behaviors.
Theory: Cognitive‐behavioral theory.
Setting: Residential drug treatment center.
Exposure: 1 session per week (90mins) for 6 wks.
Staff: Three adult group leaders. 2: Non‐enhanced program version. Same as above, but without skills training, roleplays, skills practice, or contract to change behaviors. Theory: Cognitive‐behavioral theory. Setting: Residential drug treatment center. Exposure: 1 session per week (90mins) for 6 wks. Staff: Three adult group leaders. |
|
| Outcomes | STI treatment in the past 2 months among all participants Casual sex in the past 2 months among all participants Sex in the past 2 months with a partner known to be non‐monogamous among all participants AIDS knowledge test among all participants |
|
| Notes | Funding: National Institute of Mental Health and National Institute of Drug Abuse. No controls for clustering or multiple statistical tests. No cost data provided. Participant satisfaction was high and did not differ between groups. Rigorous fidelity monitoring: All sessions were audiotaped and evaluated for adherence by the project director. Makeup sessions were provided for absent participants. Mean attendance was 5.8 of the 6 sessions. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
St Lawrence 1999.
| Methods | RCT, Abstinence‐plus vs. Attention Control.
Unit of randomization: Individual. Method of randomization: Unclear. Data collection for sexual behavior: paper‐and‐pencil measures administered weekly. Participants were spaced in a large room and given copies of the instrument on clipboards; questions were projected on a screen and explained orally. Condom skills were assessed in a private room by demonstration using a model. STI incidence was biologically evaluated at baseline, but this was not repeated at 6‐month follow‐up due to the mishandling of laboratory specimens. Unclear procedures for collecting behavior data at 6‐month follow‐up. Assessment times: Baseline, immediate post‐intervention, >7 months after baseline (the program lasted 1 month after baseline, and participants were evaluated 6 months after their release from the reformatory; release times varied). Complete case analysis. No data appeared to be imputed for participants who dropped out of the study entirely. If participants completed follow‐up assessments but were missing data for a given response, missing data were replaced with the mean value for the participant's group at that assessment time. Attrition: 13.6% at 6 months after discharge. 12 of the dropouts withdrew from the study while still at the facility; explanations were not provided for other sources of attrition. No significant differences were found between the participants who were followed up and the participants who dropped out after release from the reformatory. Group equivalence: No baseline differences on demographic, cognitive‐mediating, or behavioral measures, according to MANOVA. |
|
| Participants | Mississippi (USA) N = 361. Mean age: 15.8 (SD = 0.7). Ethnicity: 69.9% African‐American, 28.0% White, Native American 0.2%, Hispanic 1.9%. SES: unclear. 100% Male. Notes on recruitment: Participants were in the custody of the Department of Youth services. In loco parentis consent was provided by the custodial agency. Participants were recruited during the first orientation week after entering the state reformatory. Inclusion criteria were informed consent and no obvious physical or mental impairment that would preclude participation in a small group intervention. 8 youth were ineligible because they were housed in a separate high‐security unit. |
|
| Interventions | 1: Shortened version of "Becoming a Responsible Teen" with skills practice, delivered in groups of 10‐12. Included one informational session about HIV and other STIs. Skills training and practice was provided for five skills: correct condom use, refusal of unwanted sexual initiations, partner negotiation for condom use prior to sex, information provision to peers, and self‐reinforcement for adaptive behaviors. Activities included small‐group instruction, observing group leaders practice skills, watching peer role models on videos, and practicing skills in dyads.
Theory: Cognitive‐behavioral theory.
Setting: Private classroom in a state juvenile reformatory.
Exposure: 6 one‐hour sessions. 2 sessions were provided per week in the second, third, and fourth weeks after entering the facility.
Staff: Adult group leaders. 2: Attention control focusing on anger management, delivered in groups of 10‐12. the program was based on the Positive Adolescent Choices Training (PACT) program. Included information about anger management skills. Skills training was provided for six components: giving positive feedback, giving negative feedback, accepting criticism, resisting peer pressure, solving problems, and conflict resolution. Activities included small‐group instruction, observing group leaders practice skills, watching peer role models on videos, and practicing skills in dyads. Theory not reported. |
|
| Outcomes | Unprotected vaginal intercourse frequency in past 3m among all participants Unprotected anal intercourse frequency in past 3m among all participants Oral intercourse frequency in past 3m among all participants Number of casual sex encounters since baseline among all participants Number of sex partners in past 3m among all participants Number of non‐monogamous partners since baseline among all participants Percentage of condom‐protected intercourse occasions in past 3m among participants reporting intercourse Summary of sexual behaviors (including log‐transformed frequencies of unprotected vaginal sex, condom‐protected vaginal sex, unprotected anal sex, condom‐protected anal sex, oral sex, and number of partners) AIDS knowledge test among all participants |
|
| Notes | Funding: CDC Division of Sexually Transmitted Disease Prevention, Mississippi State Department of Health, Levi Strauss Company. Bonferroni correction used to control for multiple statistical tests. Participants in both interventions rated the programs highly for comfort with staff (mean 9 out of 10), value of the program (9.2), and enjoyment (9.1); evaluations did not differ between the two programs. Cost data not provided. Participants received $25 and a T‐shirt for completing the final follow‐up assessment. Fidelity monitoring: 97% completed interventions and the immediate post‐test assessment. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
St Lawrence 2002.
| Methods | RCT, Abstinence‐plus enhanced (education with skills training and "motivational component) vs. Abstinence‐plus enhanced (education with skills training only) vs. Abstinence‐plus non‐enhanced (education only). Unit of randomization: Cohort of 6‐10 adolescents. Method of randomization: Not reported. Data collection for sexual behavior: Written self‐report questionnaire. Code names used to protect participants' confidentiality. Investigators traveled to participants' locales to administer assessments, paid participants $25 for 6m and $35 for 12m assessments. All measures administered orally as an accompaniment to the written questionnaire (read aloud by staff person at all assessments, used overhead projector at baseline), adolescents responded on their personal copy of the survey. Anger management and social skills assessed using roleplays. Assessment times: Baseline, immediately post‐intervention, 6m, and 12m. Complete case analysis. Attrition: 3% at 6m, 11% at 12m for all three arms. Attrition due to inability to locate participants; further analyses not provided. Group equivalence: No significant baseline differences by group. |
|
| Participants | Mississippi (USA) N = 161 youth, 24 cohorts. Mean age 16.0 yrs. Ethnicity: 75% White, 22% African‐American, 1% Hispanic, 2% Native American. SES: Not reported. 68% Male. Notes on recruitment: Recruited participants over a 3‐year period in the only 3 Mississippi residential drug treatment programs serving adolescents. Adolescents admitted to facilities were drawn from throughout Mississippi and were diagnosed as substance‐dependent. Randomization occurred after 3‐week detoxification period. Participants were paid $25 for 6‐month and $35 for 12‐month follow‐up assessments. |
|
| Interventions | 1: Somewhat based on "Becoming a Responsible Teen," Information‐Motivation‐Behavioral Skills Training version (IMB). After 3 weeks of detoxification, participants received the intervention during their remaining 4 weeks of residential drug treatment. the intervention was delivered several times each week in small groups of 6‐10 adolescents, and activities were conducted apart from the treatment facility by staff members who were not involved in the drug treatment program. Concepts included STIs, HIV/AIDS, problem solving, condom skills, expressing self, refusal skills, partner negotiation, peer education, risk sensitization, anger management. Activities included instruction, games, group discussion, condom skills practice, negotiation and refusal skills practice, practice in providing information to peers, problem‐solving, and anger management skills. Towards the end of the intervention, participants received pictures of themselves digitized to reflect their own faces in end‐stage AIDS (the "motivation" component). the participants were then told that they new everything they needed to know to prevent HIV. Participants received T‐shirt and certificate upon completion.
Theoretical basis: Information‐Motivation‐Behavioral Skills model.
Setting: Off‐site space linked to residential drug treatment facility.
Exposure: Twelve 90‐min sessions provided over 4 weeks (3 sessions per week). Provided over first 28 of 30 days post‐detoxification in residential drug treatment.
Staff: Co‐led by one male and one female facilitator. Facilitators had degrees in psychology and received training and supervision from the lead investigator. 2: Information‐Behavioral Skills Training version (IB). Same as above, including all skills training, EXCEPT that participants did not receive a digitally altered photograph of themselves in end‐stage AIDS. 3: Information‐only version (I). Same as IMB and IB, but no skills training or digitally enhanced photograph were provided. Concepts included STIs, AIDS, values, birth control, drinking/driving, peer pressure, drug education, smoking, gangs, weapons, and stress. Activities included games, group discussion, and instruction. Participants received T‐shirt and certificate upon completion. |
|
| Outcomes | Unprotected vaginal intercourse frequency in past 3m among all participants Percentage abstinent during past 3m among all participants Number of sex partners in past 3m among all participants Percentage of condom‐protected intercourse occasions in past 3m among participants reporting intercourse AIDS knowledge test among all participants |
|
| Notes | Funding: Not reported. Analyses did not control for unit of randomization. Participants were paid $25 for 6m and $35 for 12m assessments. It is unclear whether the personnel delivering each intervention were the same. Rigorous fidelity monitoring: All intervention sessions audiotaped and monitored. the principal investigator then compared each session against a study checklist, and checked off each element as it was presented. Cost data not provided. Participants ranked each condition equally highly for satisfaction. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Stanton 1996.
| Methods | RCT, Abstinence‐plus (enhanced) vs. Abstinence‐plus (non‐enhanced) Unit of randomization: Friendship group, stratified into pairs by gender, age, and median sexual experience. Method of randomization: Random numbers table Data collection: ACASI Assessment times: baseline, 6m, 12m Complete case analysis. Attrition: 27% at 12m follow‐up. Attrition did not differ by trial arm. Group equivalence at baseline: Unclear whether groups were equivalent at baseline; repeated measures analyses used to accommodate baseline values where possible. |
|
| Participants | Baltimore, MD (USA) N = 383 youth in 75 naturally occurring friendship groups. Median age: 11.3 Ethnicity: 100% African‐American SES: low 56% male Notes on recruitment: Recruited through community contacts (who received stipends for helping to identify eligible youth). Groups consisted of 3‐10 same‐gender friends who were within 3 years of age of each other, with no youth being outside the age range of 9‐15. |
|
| Interventions | 1: Focus on Kids. 7 weekly community‐based sessions plus a day‐long session/party at a campsite. Delivered by adults to naturally formed, single‐sex friendship groups. Included cultural components, decision‐making, communication, negotiation skills, discussion of peer condom use, family trees, and HIV/AIDS. Activities included small group discussions, lectures, videos, games, roleplays, acting, storytelling, arts and crafts, and community projects. Phone calls and reminders were used to encourage attendance.
Theoretical basis: Social cognitive theory, protection motivation theory
Setting: Community recreation center meeting room
Exposure: 10.5 hours over 7 weekly sessions.
Staff: Pair of interventionists (from a pool of 25), at least one was gender‐matched to the group. 2: Non‐enhanced. Youths were invited to attend weekly sessions at community sites, each of which included a video about AIDS and a discussion. Condoms were provided. No effort was made to deliver the intervention through natural friendship groups, and no cultural component was included. |
|
| Outcomes | Condom use at last sex among participants reporting sex in the past 6 months AIDS knowledge among all participants |
|
| Notes | Funding: National Institute of Mental Health, Agency for Health Care and Research, National Institutes of Health. Analyses did not specify procedures to control for clustering. Participants received $20 for completing all surveys. Same intervention evaluated in Danella 2000, Stanton 2006, and Wu 2003. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Stanton 2000.
| Methods | RCT, Abstinence‐plus vs. Attention Unit of randomization: Parent‐youth dyad Method of randomization: Random numbers table. Data collection: ACASI Assessment times: baseline, 2m, 6m, 9m, 12m Complete case analysis. Attrition: 12% at 2m, 17% at 6m, 20% at 9m, 25% at 12m. No group differences in attrition. Group equivalence at baseline: No significant baseline differences. |
|
| Participants | Baltimore, MD (USA) N = 237 dyads, each consisting of 1 youth and 1 parent. Median age: 13.6 Ethnicity: 100% African‐American SES: low 51% male Notes on recruitment: Recruited through community contacts, identified through community residents. One child and one parent per household were eligible. |
|
| Interventions | 1: ImPACT (Informed Parents and Children Together). Video‐based intervention that included a 22‐min video about parent‐youth communication and monitoring (emphases: monitoring youth, talking with them about sex, conveying facts about AIDS, condom skills, encouraging youth to be abstinent or to use condoms, and emphasizing how drugs and alcohols can lead to risky sexual behaviors). After the video, adult facilitator led the parent‐child dyad in discussion, role‐plays, and condom skills practice.
Theoretical basis: Social cognitive theory
Setting: Family homes
Exposure: 1.25 hours in one session
Staff: Adult facilitator 2: Attention. Goal for IT! Same format as intervention, but focused on goal‐setting and career opportunities instead of HIV. No condom skills or condom demonstration. |
|
| Outcomes | Sex in the past 2m among all participants (at 2m follow‐up) Sex in the past 6m among all participants (at 6m and 12m follow‐up) |
|
| Notes | Funding: National Institute of Mental Health. Same intervention evaluated in Wu 2003. Participants received a copy of the videos. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Stanton 2006.
| Methods | RCT, Abstinence‐plus (culturally adapted) vs. Abstinence‐plus (standard) vs. Attention Unit of randomization: Recruitment group Method of randomization: Not reported Data collection: written surveys (n=740) or ACASI (n=391) Assessment times: baseline, 3m, 6m, 9m Complete case analysis. Attrition: 21% at 3m, 17% at 6m, 20% at 9m. Attrition higher in abstinence‐plus arms than in attention control arm. Group equivalence at baseline: Significant baseline differences (intervention youth were less likely to be sexually active, had greater knowledge of HIV, but had lower perceived self‐efficacy regarding condom use). Controlled in analyses. |
|
| Participants | 12 Rural counties in WV (USA) N = 1131 youth in 110 recruitment groups. Mean age: approx. 14.3 Ethnicity: primarily white SES: unclear 42% male Notes on recruitment: Groups recruited through community facilitators, received interventions through school systems or community‐based organizations. |
|
| Interventions | 1: Focus on Kids. Approximately 12 hours delivered by adults to naturally formed, single‐sex friendship groups. Included cultural components, decision‐making, communication, negotiation skills, and HIV/AIDS. Activities included games, discussions, videos, family tree discussions, homework. Concepts included decision making, goal setting, communication, negotiation, relationships, abstinence, safer sex, drugs, alcohol, drug‐selling. Adapted from original FOK after focus group sessions with stakeholders. Some intervention‐group participants (n=617) received a culturally enhanced version (family tree activities were changed to reflect local culture, more factual information was included, and 2 exercises on goal setting and future planning were added).
Theoretical basis: Social cognitive theory, protection motivation theory
Setting: Schools or community‐based organizations.
Exposure: 8 sessions if delivered in schools; 1 day or 2 half‐days if delivered by community‐based organizations.
Staff: Pair of adult facilitators. Sometimes delivered long‐distance via interactive televised format. Facilitators were in their 20s‐60s, white and African‐American, and worked as teachers, ministers, community‐center directors, liaison officers, faculty members, graduate students, and housewives. 2. Attention control. Same format, but focused on environmental health. Adapted from Council from Environmental Health curriculum "Water Education for Teachers." No discussion of HIV. |
|
| Outcomes | Sex in the past 6m among all participants Frequency of condom use (Likert scale 1‐5) among participants reporting sex in the past 6m Condom use at last sex among participants reporting sex in the past 6m Ever had sexual intercourse among baseline virgins HIV/AIDS knowledge among all participants |
|
| Notes | Funding: National Institute of Mental Health Same intervention evaluated in Danella 2000, Stanton 1996, and Wu 2003. Analyses did not specify procedures to control for clustering. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Villarruel 2006.
| Methods | RCT, Abstinence‐plus vs. Attention Unit of randomization: Individual Method of randomization: Computer‐generated sequence Data collection: Written English/Spanish surveys Assessment times: baseline, 3m, 6m, 12m Complete case analysis. Attrition: 18.4% at 12m (unclear at 3m and 6m). Attrition higher among Spanish speakers. Group equivalence at baseline: No baseline differences. |
|
| Participants | Philadelphia, PA (USA) N = 656 Mean age: 14.9 Ethnicity: of those analyzed, 100% Latino SES: unclear 45% male Notes on recruitment: Eligible if they self‐reported being Latino and were aged 13‐18 years. 45% born outside mainland US |
|
| Interventions | 1: Cuidate! (Based on Be Proud! Be Responsible!). Tailored to Latino adolescents. 6 hours delivered by adults to small groups of participants. Included small‐group discussions, videos, interactive exercises, and skill‐building activities. Delivered in English and Spanish. Incorporated cultural aspects: familialism and gender‐role expectations. Presented abstinence and condom use as culturally accepted and effective ways to prevent HIV.
Theoretical basis: Theory of reasoned action, social cognitive theory, theory of planned behavior
Setting: Schools on Saturday
Exposure: 6 hours over 2 sessions
Staff: Adults 2: Attention. Same as above, but focused on health issues that affect Latinos. Concepts included diet, exercise, physical activity, cigarettes, alcohol, and drug use. Contextualized in Latino cultural values. |
|
| Outcomes | Number of days of unprotected sex in the past 3m among participants who reported being sexually active at baseline Vaginal intercourse in last 3m among all participants Multiple partners in the past 3m among all participants Consistent condom use in the past 3m among participants who reported being sexually active at baseline Condom use at last sex among participants who reported being sexually active at baseline Proportion of days of protected sex among participants who reported being sexually active at baseline |
|
| Notes | Funding: National Institute of Nursing Research It appeared that 103 youth were randomized and underwent the intervention, but were then eliminated because they were not Latino. It is unclear how these youth were included in the trial given the eligibility criteria. An additional 3 control participants were excluded because they did not undergo the intervention. Participants were compensated as much as $110 for participating, in addition to T‐shirts |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Weeks 1997.
| Methods | RCT, Abstinence‐plus enhanced (with assigned parent‐child activities) vs. Abstinence‐plus non‐enhanced (without assigned parent‐child activities) vs. Usual Care. Unit of randomization: School district. Method of randomization: Not reported. Data collection: Self‐report surveys completed in 7th (pretest) and 8th grades (12m post‐baseline, immediately post‐intervention) under the supervision of trained data collectors. 9th grade data (24m post‐baseline) were collected by telephone interviews (57%), and via mail survey (43%). Results did not differ by method of data collection. Assessment times: Baseline, immediate post‐intervention, 12m, 24m. ITT analysis, imputed data for dropouts using random‐effect regression analyses. Attrition: 30.2% in 8th grade, 48.6% in 9th grade for all three arms. 9th grade data were not used in this analysis because the attrition was greater than 1/3. Those lost to dropout had higher rates of sexual activity and licit drug use. Group equivalence: Groups were equivalent for gender and age at baseline. Significant differences by race (Intervention group more Hispanic, less African‐American). Controlled for gender, race, and attrition in analyses. |
|
| Participants | Chicago, IL (USA) N = 2392 students, 15 school districts. Mean age: 12.5 yrs. Ethnicity: 59.6% African‐American, 24.9% White, 10.1% Latino, 5.4% Other. SES: School districts considered at‐risk partly because of student poverty. 51.4% Male. Notes on recruitment: Participants were 7th grade students in 15 school districts recruited from large metropolitan area. These districts were among the 45 districts likely to be at greatest risk for high prevalence of HIV based on poverty, proportion of minority students, rates of reported STIs and pregnancies, school dropouts, and reading scores. Those who completed 9th grade survey got $10 gift certificate for local music/video store. |
|
| Interventions | 1: "Youth AIDS Prevention Project (YAPP)" with parent activities. In‐class curriculum with parent‐child homework assignments. Concepts included HIV Knowledge, pregnancy, STIs, enhanced decision‐making, resistance and negotiation skills, drug education, human sexuality, skill‐building, abstinence, and self‐efficacy. Activities included lectures, discussions, videos, small group exercises, roleplays, brainstorming, competitions, anonymous Q&A sessions, parent‐child homework assignments and scheduled parent meetings.
Theoretical basis: Social cognitive theory, social influences model of behavior change
Setting: Middle school classes.
Exposure: 10 in‐class lessons over 2 wks in 7th grade, 5 lesson booster sessions over 1 wk in 8th grade.
Staff: Masters‐level health educators. 2: YAPP‐ Non‐Parent. Same name, concepts, format, theoretical basis, exposure, setting, and staff as above, but without parent‐child homework assignments. 3: Basic, minimal AIDS education in compliance with state mandates. Varied by district. |
|
| Outcomes | Had sex once or more in past 30 days among all participants Condom use at last sex among participants reporting vaginal sex ever Ever had sex among all participants Overall AIDS knowledge among all participants |
|
| Notes | Funding: National Institute of Mental Health. Analyses did not control for clustering. Used Tukey adjustment to control for multiple statistical tests. Fidelity monitoring by attendance records and homework completion rates. Parental participation in curricular activities beyond assigned homework (e.g., parent meetings and parent networks) was low. Cost and participation satisfaction data were not provided. Participants who completed 9th grade survey got $10 gift certificate for a local music/video store. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Wright 1997.
| Methods | RCT, Abstinence‐plus vs. Usual Care. Unit of randomization: School, stratified by province, matched‐pairs design based on participant characteristics, participants' families' characteristics, and school characteristics. Method of randomization: Not reported. Data collection: Self‐report administered in school by teachers in French and English at baseline, immediately post‐intervention, and at grade 10 and grade 11. Code numbers to protect confidentiality. Complete case analysis. Questionnaires that were "inconsistent" were excluded. Attrition: 23.4% at post‐test, 33.1% at 12m, and 48.5% at 24m. This required us to exclude all but the immediate posttest results from these analyses. Attrition was higher among those reporting less intention to practice preventive behaviors, lower levels of peer norms supportive of preventive activity, worse relationships with parents, less positive attitudes towards people living with HIV, higher levels of perceived risk of acquiring an STI, less sexual experience, less alcohol use, fewer opposite‐sex sexual partners, less cannabis use, more previous class time on AIDS instruction, lower levels of church attendance, and more frequent class‐skipping and absence from class. Group equivalence: Baseline differences were found in knowledge, attitudes towards gay people and people living with HIV/AIDS, behavioral intentions, skills/self‐efficacy, and number of sexual partners of the same sex. Baseline equivalence for previous class time spent on HIV/AIDS, church attendance, absence from class, class time skipped, participant‐parent relationships, social integration, self‐esteem, perceived risk, worry, peer support, sexual experience ever, alcohol use, cannabis use, number of opposite‐sex partners, and condom use. Repeated measures ANOVAs controlled for baseline values. |
|
| Participants | Manitoba, New Brunswick, Nova Scotia, and Ontario (Canada) N = 4512 students, 123 classrooms, 8 schools, 4 provinces. Age range: 13‐16 yrs Ethnicity: Not reported. SES: Not reported. 42.2% Male. Notes on recruitment: Four provinces were selected in consultation with the Council of Ministeres of Education Canada advisory group. Two school jurisdictions chosen in each site and randomly assigned. Each school jurisdiction provided a minimum of 20 grade 9 classes (approximately 500 participants). Sites selected far apart to minimize contamination. |
|
| Interventions | 1: "Skills for Healthy Relationships." Conducted in French in New Brunswick and in English in other provinces. In‐class curriculum for 9th grade students based on knowledge acquisition, skills development, motivational supports, and attitude development. Program included 31 activities. Divided into 4 units: Transmission, Responsible Behavior‐abstinence, Responsible behavior‐safer sex, and Health‐Enhancing Supports. Concepts included abstinence, condom skills, HIV/AIDS knowledge, drug information, other STIs, HIV/AIDS activism, problem solving skills, communication, assertiveness, self‐efficacy, and AIDS‐related stigma. Activities included instruction, videos, teacher or peer demonstration, roleplays with peer leaders, behavior rehearsal, assertiveness skills, negotiation practice, refusal skills, skills modeling by peer leaders, practicing assertiveness with parents, and condom practice. Participants received a course grade based on two in‐class tests, class participation, and class activities.
Theoretical basis: Behavioral Change Interventions Model (developed specifically for this intervention, derived from Information‐Motivation‐Behavioral Skills model, Theory of reasoned action, theory of planned behavior, and self‐efficacy theory).
Setting: Grade 9 classrooms. Science classes, family life classes, personal development and relationship classes, and physical/health education classes.
Exposure: 20 hours.
Staff: 52 teachers, 1 peer leader per 4‐6 participants selected from classes. 2: Usual care ‐ Usual sexuality education curriculum as dictated by the schools. Content and teaching strategies varied across provinces and classes. Usually focused to a greater degree on information dissemination and didactic techniques. Skill development tended not to be a primary focus, peer leaders and parent activities were not used, and programs were on average shorter than 20 hours. |
|
| Outcomes | Vaginal, oral, or anal intercourse in past 2 months among all participants Number of vaginal sex partners ever among participants reporting vaginal sex Number of oral sex partners ever among participants reporting oral sex Number of anal sex partners ever among participants reporting anal sex Condom use at last sexual intercourse among participants reporting sexual intercourse in past 2 months Vaginal, oral, or anal intercourse ever among all participants HIV knowledge among all participants |
|
| Notes | Funding: National Health Research and Development Program; AIDS Prevention and Education Unit (National AIDS Contribution Program, National AIDS Strategy, Health Canada). Study was a Ph.D. dissertation. Analyses did not control for unit of randomization. Cost data were not provided. Participant satisfaction: 80% of experimental program participants indicated that it was excellent, very good, or good. 14% indicated that it was fair, 6% that it was poor. Teacher ratings were generally positive, but over 75% teachers reported that program was too long. 92% of administrators reported wanting to integrate the program into existing grade 9 course. ANCOVAs were conducted on all non‐significant outcomes to measure the impact of degree of program implementation. "Greater" program implementers reported significantly lower levels of sexual experience in the last 2 months and significantly fewer oral partners ever than controls. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Wu 2003.
| Methods | RCT, Abstinence‐plus (enhanced with boosters) vs. Abstinence‐plus (enhanced without boosters) vs. Abstinence‐plus (non‐enhanced without boosters) Unit of randomization: Recruitment site Method of randomization: Random numbers table Data collection: ACASI Assessment times: baseline, 6m, 12m, 24m Complete case analysis. Attrition: 26% at 6m, 29% at 12m, 40% at 24m. Attrition higher among males, older participants, and participants reporting higher rates of risk behaviors. No differences between trial arms. Group equivalence at baseline: No baseline differences. |
|
| Participants | Baltimore, MD N = 817 in 35 housing developments Mean age: 14 Ethnicity: 100% African‐American SES: low 42% male Notes on recruitment: Recruited from 35 housing developments, community centers, and recreation centers. |
|
| Interventions | 1: Focus on Kids, plus ImPACT, plus booster sessions. FOK: 10.5 hours over 7 weekly sessions plus one daylong session at a campsite. Delivered by adults to natural single‐sex friendship groups, included games, homework, discussion, and videos. Concepts included abstinence, safe sex, relationships, drugs/alcohol, drug selling, HIV, decision‐making, and goal setting. ImPACT: one‐session parent‐child monitoring intervention that was delivered by trial staff in family homes. Included a video, roleplays, and condom demonstration. Concepts included parental monitoring and HIV. Booster sessions for youth at 6 months and 12 months after baseline, re‐emphasized material from FOK curriculum.
Theoretical basis: Social cognitive theory, prevention motivation theory.
Setting: Community centers, family homes.
Exposure: 10.5 hours over 7 sessions, 1‐day campsite trip, 1.25‐hour session for parents and kids, and one‐session boosters after a delay of 6 months and 10 months.
Staff: Adults 2: FOK, plus ImPACT, but without booster sessions. Same as Group 1, but no booster sessions at 6 months or 10 months after baseline. 3. FOK only. Same as Group 1, but did not receive the ImPACT intervention or any boosters. |
|
| Outcomes | Been pregnant or caused a pregnancy in the past 6 months Sexual intercourse in the past 6 months among all participants Engaged in anal sex in past 6m among all participants Condom use at last sex among participants sexual intercourse in the past 6 months |
|
| Notes | Funding: National Institute of Mental Health Analyses controlled for clustering. Reported ICC. Same interventions evaluated in Danella 2000, Stanton 1996, Stanton 2000, and Stanton 2006. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Boyer 1997 | Nonrandom assignment of participants. Location: "Urban public high schools," funding from State of California. n = 695 enrolled, 513 analyzed Mean age: 14.4 yrs. Follow‐up: 4 weeks post‐intervention. Intervention: Abstinence‐plus enhanced (didactic information plus skills‐building activities) vs. Abstinence‐plus non‐enhanced (didactic information only). Interventions were delivered in physical education classes. the 3‐session experimental program included a mix of didactic instruction and skills‐building strategies; the 1‐session control received didactic information about HIV and prevention only. Findings: Analyses controlling for baseline differences showed a significant but small effect of the experimental intervention for STD knowledge. No significant impacts on condom use or number of sexual partners in the past month. |
| Caron 1998 | Nonrandom assignment of participants. Location: Quebec, Canada n = 144 analyzed Mean age: 14.8 yrs Follow‐up: 3 weeks post‐baseline Intervention: Abstinence‐plus vs. No Intervention. LifeSavers ‐ Two 50‐minute sessions presented by peer educators aged 15‐16. Programs presented the advantages of abstinence and condom use, discussed obstacles to abstinence or condom use, and presented strategies to reduce obstacles. Findings: No behavioral outcomes presented. |
| Caron 2004 | Nonrandom assignment of participants. Location: Quebec, Canada. n = In junior level sample, 945 enrolled, 698 analyzed. In senior level sample, 477 enrolled, 306 analyzed. Mean Age: 14.1 for junior sample, 15.9 for senior sample. Follow‐up: 9 months post‐intervention. Intervention: Abstinence‐plus vs. Usual care. Protection Express Program ‐ senior high school students worked as peer educators (25‐hour training), program was integrated into Moral and Religious Education classes. Peer educators worked in teams of 5 to develop and deliver educational presentation on postponing sex, assertiveness, equality in relationships, healthy relationships, and condom use. Presentations were judged by teachers and peers, and then presented to junior students. Evaluations assess senior students (the educators) and junior students (the audience who watched the programs). Findings: for junior students, no significant difference in condom use or postponing vaginal and anal sex in the past 3 months. for senior students, no significant difference in postponing vaginal and anal sex in the past 3 months. However, among senior students, experimental participants were more likely to use a condom consistently with their regular or occasional sexual partners (p < 0.01). Analyses used hierarchical model procedure and ANCOVAs. |
| Eisen 1992 | Focused on pregnancy prevention, not HIV prevention. Location: Texas and California n = 1444 enrolled, 888 analyzed. Ages: 13‐14yrs (29%), 15‐17yrs (67%), 18‐19yrs (4%). Follow‐up: 12m post‐intervention. Intervention: Abstinence‐plus vs. Usual Care. Teen Talk ‐ 12‐15hr classroom curriculum including factual instruction and group discussion. Findings: No significant difference between baseline virgins in experimental and comparison groups (n = 596) regarding percentage who maintained abstinence over the follow‐up year. |
| Fisher 2002 | Nonrandom assignment of participants. Location: Inner‐city areas in Connecticut n = 1577 enrolled, 1532 analyzed. Mean age: 14.8 yrs Follow‐up: 12m post‐intervention. Intervention: Abstinence‐plus (classroom intervention) vs. Abstinence‐plus (peer intervention) vs. Abstinence‐plus (combined classroom and peer intervention) vs. Usual care. Classroom Program ‐ 5 sessions delivered by regular high school teachers focusing on factual information, attitudes, motivation, skills, and skills practice. Peer Intervention ‐ Natural peer opinion leaders have 5‐min conversations with approximately 5 same‐sex friends and acquaintances over a 3‐week period. Combined ‐ Group gets both interventions. Findings: Analyses were limited to participants who indicated that they were sexually active. Condom use was ranked from 1 (never) to 5 (always). At 3m follow‐up, participants in combined and peer interventions reported significantly more condom use in the previous 3m than usual care controls. At 12m follow‐up, the classroom‐based program had a significantly protective effect for condom use when compared to usual care, but the combined and peer‐led groups had no significant effects compared to usual care. |
| Handler 1987 | Focused on pregnancy prevention, not HIV prevention. Location: Chicago, IL n = 63 enrolled, 53 analyzed. Mean age: 13.3 yrs Follow‐up: 13‐14m post‐baseline. Intervention: Abstinence‐plus vs. Usual Care. Peer Power Project ‐ program for 7th and 8th‐grade females, weekly meetings of groups (15 participants) delivered by a school counselor and a paid community aide. Programs are delivered during the last hour of the school day, 1 day per week, throughout the school year. Sessions focus on knowledge of sexual risks, contraception, educational/career opportunities, access to contraception and health care, and empowerment. Groups engage in community outreach activities, visit health and family planning facilities, have career‐related speakers and field trips, and give participants cultural/artistic enrichment opportunities. Findings: Among participants who had not engaged in sex at baseline, there were no significant differences in having had sexual intercourse at 12m follow‐up. Between pretest and posttest, 2 pregnancies occurred in the control group and one in the intervention group. |
| Herz 1986a | Nonrandom assignment of participants. Location: Chicago, IL n = 56 Mean age: 13.3 yrs Follow‐up: One week before end of program. Intervention: Abstinence‐plus vs. No intervention. In‐school curriculum consisted of one 40‐min session per week for 15 weeks. Activities included films, roleplays, communication skills building, group activities, didactic learning. Concepts included birth control, anatomy, nutrition, hygiene, and education/career goals. Attendance neared 100%. Findings: No biological or behavioral outcomes assessed. |
| Herz 1986b | Focused on pregnancy prevention, not HIV prevention. Location: Chicago, IL n = 55 Mean age: 12.9 yrs Follow‐up: 12 weeks post‐intervention. Intervention: Abstinence‐plus vs. No intervention. In‐school curriculum for 1 hour per week for 10 weeks. Activities included film on "saying no" and didactic presentation of facts about birth control and anatomy. Participants refused to engage in roleplay activities. Attendance averaged 95%. Findings: No biological or behavioral outcomes assessed. |
| Herz 1986c | Focused on pregnancy prevention, not HIV prevention. Location: Chicago, IL n = 61 Mean age: 12.8 yrs Follow‐up: Immediate post‐intervention. Intervention: Abstinence‐plus vs. No intervention. After‐school group for 1 hour per week for 11 weeks. Attendance per student averaged 46% of sessions. Activities included film on "saying no" and didactic presentation of facts about birth control and anatomy. Findings: No biological or behavioral outcomes assessed. |
| Howard 1990 | Nonrandom assignment of participants. Location: Atlanta, GA n = 536 analyzed. Age: 13‐14 at baseline Follow‐up: 12m post‐intervention. Intervention: Abstinence‐only vs. Usual Care. Postponing sexual involvement ‐ 5‐session in‐school curriculum presented by male‐female teams of older peer (high school) leaders. Supplemented general sexual health curriculum that included information about family planning and STDs. Findings: Among baseline virgins, program students were significantly more likely to postpone sexual intercourse than controls. Baseline non‐virgins did not change behaviors as a result of the program. for girls, fewer pregnancies observed among girls in experimental group than in control group. |
| Hubbard 1998 | Nonrandom assignment of participants. Location: "Southern Rural State" ‐ funding from Arkansas State Dept of Education. n = 212 analyzed. Age range: Grades 9‐10. (57% were aged 15‐16yrs) Follow‐up: 18m Intervention: Abstinence‐plus vs. Abstinence‐only and state‐approved curricula. Reducing the Risk ‐ 16‐lesson curriculum for students in grades 9‐12, led by adult teachers. Involves information on risks of unprotected sex, social influences, and skills‐building. Findings: Among baseline virgins, significantly fewer students in the abstinence‐plus group became sexually active at posttest than abstinence‐only and state‐curriculum controls. Among participants who became sexually active post‐intervention, significantly more abstinence‐plus participants reported using STD/HIV and pregnancy prevention than abstinence‐only and state‐curriculum controls. |
| Kennedy 2000c | Nonrandom assignment of participants. Location: Phoenix, AZ n = 465 enrolled, 213 analyzed. Mean age: 16.53 Follow‐up: 1 month Intervention: Abstinence‐plus vs. No intervention. Be Proud! Be Responsible! ‐ 1‐session intervention in small group format. Group discussions, games, mini‐lectures, videos, condom demonstrations, role‐plays. Group discussion of barriers to condom use. Information about local services. Tailored to sexually active adolescents aged 16‐19 who have used condoms at least once and who intend to use condoms. Findings: Significantly favor intervention group for knowledge in group x time interaction from repeated‐measures ANOVA (p = 0.0005, n = 196). Also significantly favored intervention group for condom use at last sex. No significant effects for frequency of unprotected sex in the past 30 days, incidence of sex in the past 30 days, or frequency of sex in the past 30 days. |
| Kennedy 2000d | Nonrandom assignment of participants, lack follow‐up data for controls. Location: Newark, NJ n = 406 enrolled, 358 analyzed. Mean age: 14.27 Follow‐up: 1 month for intervention group; used baseline data only for controls. Intervention: Abstinence‐plus vs. No intervention. Be Proud! Be Responsible! ‐ 1‐session intervention in small group format. Group discussions, games, mini‐lectures, videos, condom demonstrations, role‐plays. Discouraged young women from dating older men. Information about local services. Tailored for both sexually active and sexually inactive participants aged 13‐16. Findings: When follow‐up knowledge in for the intervention group was compared to baseline knowledge for the control group, a between‐groups t test significantly favored the intervention group (n = 322, p = 0.0001). Marginal increase in condom use at last sex among control participants. No significant differences in incidence of sex, frequency of sex, or frequency of unprotected sex in past 30 days. |
| Kirby 1991 | Nonrandom assignment of participants. Location: California n = 758 analyzed. Age: High school (14‐18yrs). Grade 9 (27%), 10 (56%), 11 (11%), 12 (6%) Follow‐up: 18m post‐baseline. Intervention: Abstinence‐plus vs. Usual Care. Reducing the Risk ‐ 15‐session in‐school curriculum taught by high school instructors focusing on social pressures and prevention skills. Pregnancy‐oriented. Findings: Among baseline virgins, significantly fewer intervention participants reported ever having sex at 18m. No significant differences in pregnancy outcomes for baseline virgins or baseline non‐virgins. Condom use outcomes confounded with outcomes for other contraceptives. |
| Krauss 2002 | No outcomes of interest. Location: New York, NY n = 240 Mean age: 10‐13 Follow‐up: 6 months Intervention: Abstinence‐plus vs. No treatment. Parent/Preadolescent Training for HIV prevention. Four 3‐hour sessions focusing on HIV, knowledge, parent‐child communication, risk identification, and interacting with people living with HIV/AIDS. Findings: No behavioral outcomes presented. |
| Lemieux 2003 | Nonrandom assignment of participants. Location: Appears to be urban area in Connecticut n = 306 Mean age: 9th‐12th grade Follow‐up: Immediate post‐intervention Intervention: Abstinence‐plus vs. Usual care. Music‐based HIV prevention program focused on information‐motivation‐behavioral skills theory and the natural opinion leader model. Findings: "Among participants who had ever been sexually active, increases in condom use were found." |
| Lieberman 2000 | Nonrandom assignment of participants. Location: New York City, NY n = 312 analyzed. Mean Age: 12.9yrs Follow‐up: 12m post‐baseline. Intervention: Abstinence‐plus vs. Usual care. Project IMPPACT ‐ In‐school presentations recruit small groups of students to discuss teen issues and life skills. Small groups discuss communication skills, support healthy communication, and create supportive peer groups. Meet in groups of 8‐12 for 12‐14 sessions over 1 semester for 1 class period per meeting. Attendance rate: 11.3 sessions per participant. Reported Findings: At 12m, no significant differences between groups in incidence of sexual initiation, condom use at last sex, or reported pregnancies for boys, girls, or combined. |
| Main 1994 | Nonrandom assignment of participants. Location: Colorado n = 979 analyzed. Mean age: 15 yrs Follow‐up: 6m post‐baseline Intervention: Abstinence‐plus vs. Usual Care. Based on Get Real About AIDS. 15‐session skills‐based curriculum taught by health, physical education, science, and study skills teachers. Sessions focused on HIV knowledge, determinants of risky behavior, vulnerability to HIV, and skills to manage and avoid risk. Findings: At 6m follow‐up, no significant differences in onset of sexual intercourse among participants who reported never having had sex at baseline. Sexually active participants in the intervention schools reported significantly fewer partners in the last 2 months and significantly greater frequency of using condoms than controls. No significant differences for sexually active students in frequency of sex in the past 2 months. HIV knowledge was significantly greater in the intervention group at post‐test. |
| McKay 2004 | Nonrandom assignment of participants. Location: Chicago, IL n = 564 Mean age: 4th‐5th grade Follow‐up: Immediate post‐intervention (control group data collected 1 year prior to intervention group data) Intervention: Abstinence‐plus vs. Usual care. Chicago HIV Prevention and Adolescent Mental Health Project. 12 weekly sessions focusing on sexual possibility situations, family communication, rules, monitoring, support, values, puberty, and HIV. Findings: No behavioral outcomes presented. |
| Merakou 2006 | Nonrandom assignment of participants. Location: Athens, Greece n = 900 Mean age: 15‐20 years Follow‐up: Immediate post‐intervention (6 months after baseline) Intervention: Abstinence‐plus vs. No treatment. Peer education program including Teen‐AIDS Club kiosk, posters, stamps, hats and T‐shirts, classroom presentations, and HIV prevention celebration. Findings: No significant effects for sexual initiation among all participants; the percentage initiating sex since baseline was higher in the intervention group. Non‐significant findings favored the intervention group for having sex at least once with a "one‐night partner" without using a condom, and for initiating condom use for the first time with a partner. |
| Noell 1997 | No outcomes of interest. Location: Oregon and California n = 327 middle school participants, 500 high school participants. Age range: Middle school (11‐14 yrs) and high school (14‐18 yrs). Follow‐up: 1 month post‐baseline Interventions: Abstinence‐plus vs. No intervention (wait list control). the Choice is Yours ‐ 1‐session (45‐90 min) teacher‐led program with an interactive videodisc, designed to provide information and skills to help sexual decision‐making. Each videodisc contains 1 or 2 extended scenarios with branching story lines; participants decided on choices for the couples in the video and saw the positive or negative outcomes of those choices. Findings: No behavioral or biological outcomes were presented. |
| O'Donnell 1999 | Nonrandom assignment of participants. Same study as O'Donnell 2002, but this paper reported outcomes for a usual care control group in addition to the two abstinence‐plus arms. Participants in the usual care control group were not randomly assigned. Location: New York City, NY n = 1061 Mean age: 12.2 in seventh grade, 13.3 in eighth grade Follow‐up: 6m Intervention: Abstinence‐plus enhanced (in‐school curriculum with community service) vs. Abstinence‐plus non‐enhanced (in‐school curriculum without community service) vs. Usual care. Reach for Health ‐ Community Youth Service program in the enhanced condition. Reach for Health program only in the non‐enhanced condition. See the Table of Included Studies for a description of the two active intervention arms. Findings: Pairwise or overall tests of significance at 6m assessment were not provided. Changes from baseline to 6m follow‐up are given for RFH‐CYS group (enhanced), then RFH group (non‐enhanced), then controls. Ever had sex (n = 1132): +4.4%, +3.4%, +8.2%. Sex in past 3 months (n = 1148): ‐0.4%, +3.4%, +5.3%. Sex without a condom in past 3 months among those reporting recent sex (n = 266): ‐15.9%, ‐12.7%, +3.0%. According to logistic regression analysis of recent sex at 6m follow‐up controlling for recent sex at baseline, gender, grade level, and clustering, the RFH‐CYS group reported significantly less recent sex than usual care controls (p < 0.05). Effect was not significant for curriculum only vs. controls. According to logistic regression analysis of Sexual Behavior Index at 6m follow‐up, controlling for gender, grade, and baseline index scores, participants in the RFH‐CYS group reported significantly less risk behavior than controls (p < 0.05). Effect was marginally significant for RFH‐only group vs. controls (p < 0.08). Sexual Behavior Index was scored according to the following values: 1 (virgin), 2 (past but not recent intercourse), 3 (recent sex but always protected by condoms and birth control), 4 (recent unprotected sex). |
| Peeler 2000 | Nonrandom assignment of participants. Location: Pullman, Washington n = 386 college students Age: College age (18‐22 yrs) Follow‐up: 15 weeks post‐baseline. Intervention: Abstinence‐plus (Self‐management Skills Training led by peer instructors) vs. Abstinence‐plus (Self‐management Skills Training led by peer instructors AND Peer Norms Challenge) vs. No intervention. Self Management Skills Training: 15 fifty‐minute sessions focusing on HIV facts, prevalence of HIV, risk factors, personal risk assessment, sexual communication, assertiveness, abstinence and alternatives to sex, condom use, condom acquisition, condom negotiation, patterns of sex, and sticking to a behavioral plan. Peer Norms Challenge session: replaced the final session of SMST; participants discussed perceptions and realities of peer norms for alcohol use. Findings: Analyses used 3 (group) x 2 (time) ANOVAs. Group x Time effects were significant for number of times participants used condoms in the last 2 months, with each intervention group reporting more condom use than the control group. No significant effects for "sexual activity level," "frequency of sexual intercourse" in the past 2 months. Data collected for incidence and frequency of vaginal, oral, and anal sex; percentage of condom‐protected vaginal intercourse occasions; and number of partners, but significance not specifically reported. |
| Peters 1998 | Nonrandom assignment of participants. Location: Houston, TX n = unclear Mean age: 9th‐12th grade Follow‐up: Immediate post‐intervention Intervention: Abstinence‐plus vs. No treatment. Project Alpha. Student newsletters provided stories about community and student role models who improved their efficacy to abstain from sex "until adulthood." Findings: No behavioral outcomes presented. |
| Siegel 2001 | Nonrandom assignment of participants. Location: Rochester, NY n = 2312 middle school participants, 1689 high school participants enrolled. Mean age: 13.2 (middle school), 17.4 (high school) Follow‐up: for middle school comparisons, 12m post‐intervention for usual care and RAPP adult‐led and peer‐led interventions, 6m post‐intervention for group taught by school district health educator. for high school comparisons, unclear ‐ "long‐term follow‐up" was defined as "beyond 3 to 6 months." Intervention: Abstinence‐plus (RAPP adult‐led by pairs of RAPP‐trained educators) vs. Abstinence‐plus (RAPP peer led) vs. Abstinence‐plus (RAPP taught by usual health teacher ‐‐ only included for comparisons among middle school participants) vs. Usual care. RAPP ‐ Rochester AIDS Prevention Project, 12‐session (in middle schools) or 10‐session (in high schools) project aimed to increase knowledge and skills. 2‐3 sessions were delivered per week. Based on theory of reasoned action, included general guidance and exercises for assertive communication and decision‐making, skills‐based activities concerning sexuality, pregnancy, STDs, and HIV. Small and large‐group exercises, roleplaying, homework. Findings: At immediate post‐intervention follow‐up, intervention groups reported more knowledge than usual care controls among both genders in both middle and high school comparisons. At long‐term follow‐up, knowledge gains remained significant only among middle school participants (both boys and girls). Sexual behavior was divided into "some sex," "risk sex," and "high risk sex." Using repeated measures ANOVAs, intervention group was not a statistically significant predictor of whether participants would report risk sex for middle school boys, middle school girls, high school boys, or high school girls. Intervention group was not a significant predictor for whether participants would report "some sex" among middle school boys, high school girls, or high school boys. Among middle school girls, intervention group was a significant predictor for reporting "some sex," with mean scores as follows (higher scores refer to safer behaviors): RAPP by regular health teacher 9.1, peer‐led RAPP 8.6, adult‐led RAPP 8.3, controls 8.4. Among middle school participants, a separate set of analyses included participants who reported abstinence at pre‐intervention. Logistic regressions were conducted separately by gender (664 females, 339 males). Outcome was transition to sexual activity. Compared to usual care controls, boys in the peer‐taught RAPP group were significantly less likely to initiate sexual activity (OR = 0.4, p = 0.03); same for males in the regular teacher‐taught group (OR = 0.4, p = 0.02). NS for the RAPP adult‐led condition (OR = 0.6, p = 0.12). NS for girls in every condition. When middle school analyses were limited to participants aged <13 at pre‐intervention who reported baseline abstinence, significant effects were observed for sexual initiation among boys in all 3 active conditions. NS for girls. |
| Smith 2000 | Nonrandom assignment of participants. Location: 2 counties in Georgia (USA) n = 86 enrolled (74 analyzed) in comparison between STAND leaders and control 10th‐graders; 241 enrolled (241 analyzed) in comparison between STAND program participants and control 9th/10th graders. Mean age: 15.7 for STAND leaders; 15.3 for STAND participants Follow‐up: 12m post‐baseline. Intervention: In the STAND leader comparisons, Abstinence‐plus (STAND leadership training) vs. Attention Control (generic leadership training without HIV emphasis) vs. Nonintervention. In the program participant comparisons, Abstinence‐plus (lived in county that received STAND intervention) vs. Nonintervention (lived in the county that did not have trained STAND leaders). STAND ‐ peer leaders receive 36‐hour training to influence peers and change cultural norms to encourage abstinence and risk‐reduction among sexually active peers. STAND leaders then serve as positive role models and have informal conversations with peers. Findings: Testing the effects of receiving STAND leadership training: Significance tests comparing groups not provided. At 12m follow‐up, Risk Behavior Knowledge among STAND leaders increased significantly more than among controls. At 12m follow‐up, 29% of baseline virgins in the STAND leader group had initiated sex, compared to 33% of baseline virgins in the control group. Among sexually active youth at 12m follow‐up, 77% of STAND leaders reported using a condom for every act of intercourse, vs. 47% of controls. STAND leaders reported a larger increase in the number of condom‐protected acts in the previous 3 months than controls (212.5% vs. 30.6%). There were no significant group differences in the number of unprotected acts of intercourse in the past 3m among non‐virgins at 12m follow‐up. 3 STAND leaders and 3 control participants reported having been pregnant or caused a pregnancy at 12m follow‐up. Among sexually active participants, significantly fewer STAND leaders than controls reported an STD diagnosis (p < 0.01). Testing the effects of having STAND peer leaders in the county: At 12m follow‐up, there were no significant differences in knowledge between participants in the counties that had STAND leaders and participants in the control counties. No significant differences for sexual initiation, condom use at last sex, or consistent condom use. Pregnancy rates for intervention and control county participants were 14% vs. 8%; rates of STD diagnosis were 2% vs. 0%. Among participants who had never had anal sex at baseline, rates of anal intercourse were 2.5% vs. 4.4%. Incidence of anal sex among all participants was 7.8% vs. 11.0%. Incidence of unprotected anal sex among all participants reporting anal sex was 46.1% vs. 12.5%. |
| Vincent 1987 | Nonrandom assignment of participants. Location: South Carolina (Denmark, Bamberg County) n = 1 county. Mean age: Program targeted females aged 14‐17 yrs. Follow‐up: Program implemented for 5 years. Intervention: Abstinence ‐plus vs. Usual Care. School/Community Program for Sexual Risk Reduction Among Teens. Sex education in all grades (K‐12) emphasizing decision‐making, postponing sex, and contraception; mini‐courses (10 hours) for clergy, church leaders, and parents; media campaign via radio and newspaper; community awareness activities. Compared to surrounding counties. Findings: Analyses compared EPR (Estimated Pregnancy Rate) of the target area to a non‐targeted area in the same county, and to 3 other counties in the state. Comparisons assessed changes in EPR between 1981‐1985. Annual EPRs declined sharply in the intervention area in 1984 and 1985, but remained relatively constant in the 3 comparison counties. In the period 1984‐1985, the EPR in the intervention area was significantly lower (p < 0.01) than the average EPRs in the other 4 groups. In 1987‐1988 (described in Koo 1994), pregnancy rate rose again in intervention area and did not differ significantly from rates in comparison counties. |
| Walter 1993 | Nonrandom assignment of participants. Location: New York City, NY n = 1316 at baseline, 867 at 3m follow‐up. Mean age: 15.7 yrs Follow‐up: 3m Intervention: Abstinence‐plus vs. No intervention. 6 in‐school sessions on consecutive days led by regular classroom teachers, focus on AIDS facts, misperceptions, personal values, delaying sexual intercourse, negotiating with partners, condom skills. Findings: Results significantly favored the intervention group at post‐test for AIDS knowledge. No effect on sexual abstinence. Significance not provided for other outcomes, but means favored intervention group for change in number of high‐risk partners, percentage reporting monogamy, percentage reporting consistent condom use, and STD incidence. Intervention group reported significantly more favorable outcomes on a behavioral risk index (p = 0.006). |
| Zabin 1986 | Nonrandom assignment of participants. Location: Baltimore, MD n = 3646 enrolled, 2950 at follow‐up. Data were collected at each time point from students currently present in the 4 included schools; individual participants were not tracked. Age range: Junior high school (grades 7‐8, ages 12‐14) and high school (grades 9‐12, ages 14‐18) Follow‐up: Approx 3 yrs, although years of program exposure varied depending on how long a student had been present in the school. Participants were divided into zero, one‐year, two‐year, and three‐year exposure groups for analysis. Intervention: Abstinence‐plus vs. Usual care. Self Center ‐ In‐school and after‐school program lasting all throughout a school year. A social worker and a nurse‐midwife (or nurse‐practitioner) were based in each intervention school. They made presentations at least once per year in each homeroom, offered group and individual counseling on school premises during the school day, provided reproductive health services (contraceptive counseling, pregnancy testing, referrals, etc.) at after‐school clinics near school premises. Clinics also offered individual and group counseling, education, and discussions. Emphasis on personal responsibility, goal‐setting, and communication. All services were free, and program lasted 3 school years. Findings: Sexual initiation data were limited to participants over age 15 who initiated intercourse during the three program years. Data for program participants with three years of exposure were compared to data from students who attended the intervention schools, but had never been exposed to the program (i.e., zero exposure). Trends suggest that three‐year participants delayed first sex compared to zero‐exposure participants; median delay of first sex was 7 months. Significance not stated. Pregnancy rates were compared for program schools vs. control schools. This comparison used the spring follow‐up data from the first school year as baseline data (instead of baseline, which was in the fall of the first school year), "in order to ensure strictly comparable age distributions." After 16m of exposure, increases in pregnancy rates were 13% for intervention girls and 50% for control girls. After 20m of program exposure, pregnancy rates for intervention girls fell 22.5%, and rates for control girls rose 39.5%. After 28m of program exposure, pregnancy rates for intervention girls fell 30.1%, while rates for control girls rose 57.6%. Data for these percentages were limited to sexually active females. Significance not stated. |
Characteristics of ongoing studies [ordered by study ID]
Jemmott 2006.
| Trial name or title | Promoting Health Among Teens (PHAT) Project |
| Methods | |
| Participants | 662 African American grade 6 and 7 students in Pennsylvania, US. Mean age=12.0 years. 47% Male. 23% reported having had sexual intercourse at baseline, 12% had sexual intercourse in past 3 months, and 0.3% reported same‐gender sexual activity. |
| Interventions | 10 trial arms: 1. 8‐hour "Making a Difference!" Abstinence‐Only Intervention. 2. Same as 1, with booster sessions. 3. 8‐hour Safer‐Sex Intervention. 4. Same as 3, with booster sessions. 5. 12‐hour Combined Abstinence/Safer Sex. 6. Same as 5, with booster sessions. 7. 8‐hour Combined Abstinence/Safer Sex 8. Same as 7, with booster sessions. 9. 8‐hour Health Promotion Intervention (Control condition) 10. Same as 9, with booster sessions. |
| Outcomes | Sexual debut, recent sex, consistent condom use, condom use at last sex. |
| Starting date | |
| Contact information | University of Pennsylvania |
| Notes | Funding: National Institute of Mental Health |
Jemmott 2007.
| Trial name or title | The Church and Family Health Promotion Program |
| Methods | |
| Participants | "African‐American parents and one of their 6th or 7th grade children" in 10 churches across Philadelphia, PA |
| Interventions | Unclear |
| Outcomes | Unclear |
| Starting date | |
| Contact information | University of Pennsylvania |
| Notes | Funding: Unclear |
Markham 2007.
| Trial name or title | All About Youth |
| Methods | |
| Participants | 1500 students in grade 7, from 38 middle schools in Houston, Texas |
| Interventions | 3 trial arms: 1. Abstinence‐only. Based on "It's Your Game ... Keep it real." Includes 22 lessons in 7th and 8th grade focusing on the federal components of abstinence‐only education. Includes instruction, group activities, and CD‐ROMs with individual activities. 2. Abstinence‐plus. Same format, but abstinence‐plus concepts. HIV, STI, and pregnancy prevention program, also based on "It's Your Game ... Keep it real." Includes 22 lessons in 7th and 8th grade focusing on peer relationships, refusal, puberty, body development, consequences of vaginal/oral/anal sex, limits, dating relationships, condoms, and contraceptives. Includes instruction, group activities, and CD‐ROMs with individual activities. 3. Usual care defined by schools. |
| Outcomes | Sexual initiation, proportion of sexually active students, knowledge, condom use, number of sex partners |
| Starting date | September 2006 |
| Contact information | University of Texas Houston School of Public Health |
| Notes | Funding: Centers for Disease Control and Prevention |
Tortolero 2007.
| Trial name or title | Safer Choices 2 |
| Methods | |
| Participants | 500 high‐risk students in 10 alternative schools in Houston TX. In Wave 1, schools were randomized to intervention or control. In Wave 2, the treatment conditions were crossed over between schools, and a new cohort was enrolled. |
| Interventions | 2 trial arms: 1. Safer Choices 2. Abstinence‐plus program based on social cognitive theory and social influences. Activities include modeling, videos, journals, making commitments, group activities, condom use skills, condom demonstration, and opinion polls. Concepts include relationships, condoms, sexual risks, condom negotiation, gender roles, personalizing risk. 2. Usual care defined by schools |
| Outcomes | Unprotected sex, number of sex partners, proportion currently sexually active, knowledge about HIV/AIDS, choosing not to have sex when participant does not want to. Use condoms correctly and consistently when having sex. Assessed at baseline, 6m, 12m, and 24m. |
| Starting date | |
| Contact information | University of Texas Houston School of Public Health |
| Notes | Funding: National Institute of Child Health and Human Development |
Contributions of authors
All authors contributed equally to conceiving and designing the review, screening studies for inclusion, appraising the quality of papers, extracting data from papers, drafting and editing the protocol and full review, and interpreting the data.
KU coordinated the review, undertook searches of electronic databases that were not searched by the Cochrane HIV/AIDS Group Trial Search Coordinator (ie all but CENTRAL, PubMed, AIDSLINE, and EMBASE), carried out the email search for unpublished literature, and organized the retrieval of papers.
KU and DO wrote to authors of papers for additional information.
KU and PM extracted and entered data on trial results into RevMan.
All authors have approved this manuscript.
Sources of support
Internal sources
Centre for Evidence‐Based Intervention, Oxford University, UK.
Department of Social Policy and Social Work, Oxford University, UK.
External sources
No sources of support supplied
Declarations of interest
None
Edited (no change to conclusions)
References
References to studies included in this review
Aarons 2000 {published and unpublished data}
- Aarons SJ, Jenkins RR, Raine TR, El‐Khorazaty MN, Woodward KM, Williams RL, Clark MC, Wingrove BK. Postponing sexual intercourse among urban junior high school students: a randomized controlled evaluation. J Adolesc Health 2000;27:236‐247. [DOI] [PubMed] [Google Scholar]
Boekeloo 1999 {published data only}
- Boekeloo BO, Shamus LA, Simmens SJ, Cheng TL, O'Connor K, D'Angelo LJ. A STD/HIV prevention trial among adolescents in managed care. Pediatrics 1999;103:107‐115. [DOI] [PubMed] [Google Scholar]
Coyle 2001 {published data only}
- Basen‐Engquist K, Coyle KK, Parcel GS, Kirby D, Banspach SW, Carvajal SC, Baumler E. Schoolwide effects of a multicomponent HIV, STD, and pregnancy prevention program or high school students. Health Educ Behav 2001;28(2):166‐185. [DOI] [PubMed] [Google Scholar]
- Coyle K, Basen‐Engquist K, Kirby D, Parcel G, Banspach S, Harrist R, Baumler E, Weil M. Short‐term impact of Safer Choices: a multicomponent school‐based HIV, other STD, and pregnancy prevention program. J School Health 1999;69(5):181‐188. [DOI] [PubMed] [Google Scholar]
- Coyle K, Basen‐Engquist K, Kirby D, et al. Safer Choices: reducing teen pregnancy, HIV, and STDs. Public Health Rep 2001;116(S1):82‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby DB, Baumler E, Coyle KK, Basen‐Engquist K, Parcel GS, Harrist R, Banspach SW. The "Safer Choices" intervention: its impact on the sexual behaviors of different subgroups of high school students. J Adolescent Health 2004;35:442‐452. [DOI] [PubMed] [Google Scholar]
Coyle 2004 {published data only}
- Coyle K, Kirby D, Marin BV, Gomez CA, Gregorich SE. Draw the line/respect the line: a randomized trial of a middle school intervention to reduce sexual risk behaviors. Am J Public Health 2004;94(5):843‐851. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coyle 2006 {published data only}
- Coyle KK, Kirby DB, Robin LE, Banspach SW, Baumler E, Glassman JR. All4You! A randomized trial of an HIV, other STDs, and pregnancy prevention intervention for alternative school students. AIDS Educ Prev 2006;18(3):187‐203. [0899‐9546 (Print)] [DOI] [PubMed] [Google Scholar]
Dancy 2006 {published data only}
- Dancy BL, Crittenden KS, Talashek ML. Mothers' effectiveness as HIV risk reduction educators for adolescent daughters. J Health Care Poor Underserved 2006;17(1):218‐39. [1049‐2089 (Print)] [DOI] [PubMed] [Google Scholar]
Danella 2000 {unpublished data only}
- Danella R, Galbraith J, Bain R, Brathwaite N. HIV/AIDS risk reduction intervention for adolescent girls in the Bahamas. International AIDS Conference. Durban, South Africa, 2000.
- Danella R, Galbraith J, Brathwaite N, Bain R, Sill A, and the Bahamas Focus on Youth Working Group. Focus on youth: A randomized, controlled effectiveness trial of an adapted "Programs That Work for HIV/AIDS Risk‐Reduction" intervention for adolescent girls in the Bahamas Unpublished.
Danielson 1990 {published data only}
- Danielson R, Marcy S, Plunkett A, Wiest W, Greenlick MR. Reproductive health counseling for young men: what does it do?. Fam Plann Perspect 1990;22(3):115‐121. [PubMed] [Google Scholar]
DiIorio 2006 {published data only}
- DiIorio C, Denzmore P, Wang DT, Lipana J, Resnicow K, Rogers‐Tillman G, Dudley WN, Marter D. Keepin' it R.E.A.L.: A mother‐adolescent HIV prevention program. In: Pequegnat W, Szapocznik J editor(s). Working with Families in the Era of HIV/AIDS. London: Sage Publications, Ltd., 2000. [Google Scholar]
- DiIorio C, Resnicow K, McCarty F, De AK, Dudley WN, Wang DT, Denzmore P. Keepin' it R.E.A.L.! Results of a mother‐adolescent HIV prevention program. Nurs Res 2006;55(1):43‐51. [0029‐6562 (Print)] [DOI] [PubMed] [Google Scholar]
- DiIorio C, Resnicow K, Thomas S, Dongqing T, Dudley WN, Marter D, Lipana J. Keepin' it R.E.A.L.! Program description and results of baseline assessment. Health Educ Behav 2002;29(1):104‐23. [DOI] [PubMed] [Google Scholar]
DiIorio 2007 {unpublished data only}
- Denzmore P, DiIorio C, Williams P, Brown T, Bailey R, Wang T, McCarty F. Maintaining fidelity to a curriculum in multigroup intervention studies: The R.E.A.L. MEN project, a HIV prevention intervention behavioral study. Natl HIV Prev Conf. Atlanta, GA, 2003.
- DiIorio C, Denzmore P, Williams P, McCarty F, Wang Q, Qi J, Bedell R. An HIV prevention program for fathers and their sons. International AIDS Conference. Barcelona, Spain, 2002.
- DiIorio C, McCarty F, Resnicow K, Lehr S, Denzmore P. R.E.A.L. MEN: A group randomized trial of an HIV prevention program for adolescent males. Am J Public Health 2007:In press. [DOI] [PMC free article] [PubMed]
Ferguson 1998 {published data only}
- Ferguson SF. Peer counseling in a culturally specific adolescent pregnancy prevention program. J Health Care Poor U 1998;9(3):322‐40. [DOI] [PubMed] [Google Scholar]
Hernandez 1990 {published data only}
- Hernandez JT, Smith FJ. Abstinence, protection, and decision‐making: experimental trials on prototypic AIDS programs. Health Educ Res 1990;5(3):309‐320. [Google Scholar]
Hewitt 1998 {unpublished data only}
- Hewitt N. Africentricity, HIV behavioral intervention, and HIV risk associated behavior among African American adolescents: a randomized controlled trial. Doctoral Dissertation at Princeton University 1998.
Jemmott 1992 {published data only}
- Jemmott JB III, Jemmott LS, Fong GT. Reductions in HIV risk‐associated sexual behavior among Black male adolescents: effects of an AIDS prevention intervention. 1992 82;3:372‐377. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jemmott 1998 {published data only}
- Jemmott JB III, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk‐reduction interventions for African‐American adolescents: a randomized controlled trial. JAMA 1998;279(19):1529‐1536. [DOI] [PubMed] [Google Scholar]
Jemmott 1999 {published data only}
- Jemmott JB III, Jemmott LS, Fong GT, McCafree K. Reducing HIV risk‐associated sexual behavior among African American adolescents: testing the generality of intervention effects. American Journal of Community Psychology 1999;27(2):161‐187. [DOI] [PubMed] [Google Scholar]
Jemmott 2004 {unpublished data only}
- Jemmott JB, III, Jemmott LS, Fong GT, Hines PM. Evaluation of an HIV/STD risk reduction intervention implemented by Non‐Governmental Organizations (NGOs): A randomized controlled cluster trial. International AIDS Conference. Bangkok, Thailand, 2004.
- Jemmott JI. HIV in ethnic minority populations. Current epidemiology and intervention approaches for HIV/AIDS among drug users. Bethesda, MD, 2004.
Kennedy 2000a {published data only}
- Kennedy MG, Mizuno Y, Hoffman R, Baume C, Strand J. The effect of tailoring a model HIV prevention program for local adolescent target audiences. AIDS Educ Prev 2000;12(3):225‐38. [PubMed] [Google Scholar]
Kennedy 2000b {published data only}
- Kennedy MG, Mizuno Y, Hoffman R, Baume C, Strand J. The effect of tailoring a model HIV prevention program for local adolescent target audiences. AIDS Educ Prev 2000;12(3):225‐38. [PubMed] [Google Scholar]
Kirby 1997 {published data only}
- Kirby D, Korpi M, Adivi C, Weissman J. An impact evaluation of Project SNAPP: an AIDS and pregnancy prevention middle school program. AIDS Educ Prev 1997;9(Supplement A):44‐61. [PubMed] [Google Scholar]
Markham 2006 {unpublished data only}
- Markham CM, Tortolero S, Peskin M, Shegog R, Addy R, Baumler E, McKirahan N, Spooner K, Escobar‐Chaves L, Thiel M. Short‐term impact evaluation of "It's your game, keep it real": A multimedia HIV/STI and pregnancy prevention intervention for middle school youth. American Public Health Association 134th Annual Meeting and Exposition. Boston, MA, 2006.
McBride 2000a {published data only}
- McBride D, Gienapp A. Using randomized designs to evaluate client‐centered programs to prevent adolescent pregnancy. Fam Plann Perspect 2000;32(5):227‐235. [PubMed] [Google Scholar]
McBride 2000b {published data only}
- McBride D, Gienapp A. Using randomized designs to evaluate client‐centered programs to prevent adolescent pregnancy. Fam Plann Perspect 2000;32(5):227‐235. [PubMed] [Google Scholar]
Moberg 1998 {published data only}
- Moberg DP, Piper DL. The Healthy for Life project: sexual risk behavior outcomes. AIDS Educ Prev 1998;10(2):128‐148. [PubMed] [Google Scholar]
- Piper DL, Moberg DP, King MJ. The Healthy for Life project: behavioral outcomes. The Journal of Primary Prevention 2000;21(1):47‐73. [Google Scholar]
O'Donnell 2002 {published data only}
- O'Donnell L, Stueve A, O'Donnell C, Duran R, San Doval A, Wilson RF, Haber D, Perry E, Pleck JH. Long‐term reductions in sexual initiation and sexual activity among urban middle schoolers in the Reach for Health service learning program. J Adolesc Health 2002;31:93‐100. [DOI] [PubMed] [Google Scholar]
- O'Donnell L, Stueve A, San Doval A, Duran R, Haber D, Atnafou R, Johnson N, Grant U, Murray H, Juhn G, Tang J, Piessens P. The effectiveness of the Reach for Healthy community youth service learning program in reducing early and unprotected sex among urban middle school students. Am J Public Health 1999;89(2):176‐181. [DOI] [PMC free article] [PubMed] [Google Scholar]
Philliber 2001 {published data only}
- Philliber S, Kaye J, Herrling S. The national evaluation of the Children's Aid Society Carrera‐Model program to prevent teen pregnancy. Accord, NY: Philliber Research Associates, 2001. [Google Scholar]
- Philliber S, Williams Kaye J, Herrling S, West E. Preventing pregnancy and improving health care access among teenagers: an evaluation of the Children's Aid Society‐Carrera program. Perspect Sex Reprod Health 2002;34(5):244‐251. [PubMed] [Google Scholar]
Sikkema 2005 {published data only}
- Sikkema KJ, Anderson ES, Kelly JA, Winett RA, Gore‐Felton C, Roffman RA, Heckman TG, Graves K, Hoffmann RG, Brondino MJ. Outcomes of a randomized, controlled community‐level HIV prevention intervention for adolescents in low‐income housing developments. AIDS 2005;19(14):1509‐16. [0269‐9370 (Print)] [DOI] [PubMed] [Google Scholar]
Smith 1994 {published data only}
- Smith, MAB. Teen incentives program: evaluation of a health promotion model for adolescent pregnancy prevention. J Health Education 1994;25(1):24‐9. [DOI] [PubMed] [Google Scholar]
St Lawrence 1995a {published data only (unpublished sought but not used)}
- Lawrence JS, Brasfield TL, Jefferson KW, Alleyne E, O'Bannon RE III, Shirley A. Cognitive‐behavioral intervention to reduce African American adolescents' risk for HIV infection. J Consult Clin Psychol 1995;63(2):221‐237. [DOI] [PubMed] [Google Scholar]
St Lawrence 1995b {published data only}
- St. Lawrence JS, Jefferson KW, Alleyne E, Brasfield TL. Comparison of education versus behavioral skills training interventions in lowering sexual HIV‐risk behavior of substance‐dependent adolescents. J Consult Clin Psychol 1995;63(1):154‐7. [DOI] [PubMed] [Google Scholar]
St Lawrence 1999 {published data only}
- Lawrence JS, Crosby RA, Belcher L, Yazdani N, Brasfield T. Sexual risk reduction and anger management interventions for incarcerated male adolescents: a randomized controlled trial of two interventions. J Sex Educ Ther 1999;24(1&2):9‐17. [Google Scholar]
St Lawrence 2002 {published data only (unpublished sought but not used)}
- Lawrence JS, Crosby R, Brasfield TL, O'Bannon RE III. Reducing STD and HIV risk behavior of substance‐dependent adolescents: a randomized controlled trial. J Consult Clin Psychol 2002;70(4):1010‐1021. [PubMed] [Google Scholar]
Stanton 1996 {published and unpublished data}
- Galbraith J, Ricardo I, Stanton B, Black M, Fiegelman S, Kaljee L. Challenges and rewards of involving community in research: an overview of the "Focus on Kids" HIV risk reduction program. Health Educ Behav 1996;23(3):383‐94. [DOI] [PubMed] [Google Scholar]
- Stanton BF, Li X, Ricardo I, Galbraith J, Feigelman S, Kaljee L. A randomized, controlled effectiveness trial of an AIDS prevention program for low‐income African‐American youths. Archives of Pediatrics and Adolescent Medicine 1996;150(4):363‐72. [DOI] [PubMed] [Google Scholar]
Stanton 2000 {published and unpublished data}
- Li X, Stanton B, Galbraith J, Burns J, Cottrell L, Pack R. Parental monitoring intervention: Practice makes perfect. J Nat Med Assoc 2002;94:364‐70. [PMC free article] [PubMed] [Google Scholar]
- Stanton B, Li X, Galbraith J, Cornick G, Fiegelman S, Kaljee L, Zhou Y. Parental underestimates of adolescent risk behavior: a randomized controlled trial of a parental monitoring intervention. J Adolesc Health 2000;26:18‐26. [DOI] [PubMed] [Google Scholar]
Stanton 2006 {published and unpublished data}
- Stanton B, Cottrell L, Li X, et al. The complex business of adapting effective interventions to new populations. An urban to rural transfer. Psychosocial Workshop. Philadelphia, PA, 2005. [DOI] [PubMed]
- Stanton B, Harris C, Cottrell L, Li XM, Gibson C, Guo JT, Pack R, Galbraith J, Pendleton S, Wu Y, Burns J, Cole M, Marshall S. Trial of an urban adolescent sexual risk‐reduction intervention for rural youth: A promising but imperfect fit. J Adolesc Health 2006;38:55.e25‐55.e36. [DOI] [PubMed] [Google Scholar]
Villarruel 2006 {published data only}
- Villarruel AM, Jemmott JB, III, Jemmott LS. A randomized controlled trial testing an HIV prevention intervention for Latino youth. Arch Pediatr Adolesc Med 2006;160(8):772‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarruel AM, Jemmott LS, Jemmott JB, 3rd. Designing a culturally based intervention to reduce HIV sexual risk for Latino adolescents. J Assoc Nurses AIDS Care 2005;16(2):23‐31. [1055‐3290 (Print)] [DOI] [PubMed] [Google Scholar]
- Villarruel AM, Jemmott LS, Jemmott JB, Eakin BL. Recruitment and retention of Latino adolescents to a research study: lessons learned from a randomized clinical trial. J Spec Pediatr Nurs 2006;11(4):244‐50. [1539‐0136 (Print)] [DOI] [PubMed] [Google Scholar]
Weeks 1997 {published data only}
- Levy SR, Perhats C, Weeks K, Handler A, Zhu C, Flay BR. Impact of a school‐based AIDS prevention program on risk and protective behavior for newly sexually active students. J School Health 1995;65(4):145‐151. [DOI] [PubMed] [Google Scholar]
- Weeks K, Levy SR, Gordon AK, Handler A, Perhats C, Flay BR. Does parental involvement make a difference? The impact of parent interactive activities on students in a school‐based AIDS prevention program. AIDS Educ Prev 1997;9(Supplement A):90‐106. [PubMed] [Google Scholar]
- Weeks K, Levy SR, Zhu C, Perhats C, Handler A, Flay BR. Impact of a school‐based AIDS prevention program on young adolescents' self‐efficacy skills. Health Educ Res 1995;10(3):329‐344. [Google Scholar]
Wright 1997 {unpublished data only}
- Wright NP. Effects of a high school sexuality education program. Doctoral Dissertation at Queen's University 1997.
Wu 2003 {published and unpublished data}
- Stanton B, Cole M, Galbraith J, Li X, Pendleton S, Cottrell L, Marshall S, Wu Y, Kaljee L. Randomized trial of a parent intervention: Parents can make a difference in long‐term adolescent risk behaviors, perceptions, and knowledge. Arch Pediatr Adolesc Med 2004;158:947‐55. [DOI] [PubMed] [Google Scholar]
- Wu Y, Burns JJ, Stanton BF, Li X, Harris CV, Galbraith J, Wei L. Influence of prior sexual risk experience on response to intervention targeting multiple risk behaviors among adolescents. J Adolesc Health 2005;36(1):56‐63. [1054‐139X (Print)] [DOI] [PubMed] [Google Scholar]
- Wu Y, Stanton B, Galbraith J, Kaljee L, Cottrell L, Li X, Harris C, D'Alessandri D, Burns J. Sustaining and broadening intervention impact: A longitudinal randomized trial of 3 adolescent risk reduction approaches. Pediatrics 2003;111(1):32‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Boyer 1997 {published data only}
- Boyer CB, Shafer M. Evaluation of a knowledge‐ and cognitive‐behavioral skills‐building intervention to prevent STDs and HIV infection in high school students. Adolescence 1997;32(125):25‐40. [PubMed] [Google Scholar]
Caron 1998 {published data only}
- Caron F, Otis J, Pilote F. Evaluation of an AIDS peer education program on multiethnic adolescents attending an urban high school in Quebec, Canada. Journal of HIV/AIDS Prevention and Education for Adolescents and Children 1998;2(1):31‐53. [Google Scholar]
Caron 2004 {published data only}
- Caron F, Godin G, Otis J, Lambert LD. Evaluation of a theoretically based AIDS/STD peer education program on postponing sexual intercourse and on condom use among adolescents attending high school. Health Educ Res 2004;19(2):185‐97. [DOI] [PubMed] [Google Scholar]
Eisen 1992 {published data only}
- Eisen M, Zellman GL. A health beliefs field experiment: Teen Talk. In: Miller BC, Card JJ, Paikoff RL, Peterson JL editor(s). Preventing Adolescent Pregnancy: Model Programs and Evaluations. Sage Publications, 1992:220‐264. [Google Scholar]
- Eisen M, Zellman GL, McAlister AL. Evaluating the impact of a theory‐based sexuality and contraceptive education program. Fam Plann Perspect 1990;22(6):261‐271. [PubMed] [Google Scholar]
Fisher 2002 {published data only}
- Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information‐motivation‐behavioral skills model‐based HIV risk behavior change intervention for inner‐city high school youth. Health Psychol 2002;21(2):177‐86. [PubMed] [Google Scholar]
Handler 1987 {published data only}
- Handler AS. An evaluation of a school‐based adolescent pregnancy prevention program. Dissertation, Univ. of Illinois at Chicago 1987.
Herz 1986a {published data only}
- Herz EJ, Reis JS, Barbera‐Stein L. Family life education for young teens: an assessment of three interventions. Health Educ Quart 1986;13(3):201‐21. [DOI] [PubMed] [Google Scholar]
Herz 1986b {published data only}
- Herz EJ, Reis JS, Barbera‐Stein L. Family life education for young teens: an assessment of three interventions. Health Educ Quart 1986;13(3):201‐21. [DOI] [PubMed] [Google Scholar]
Herz 1986c {published data only}
- Herz EJ, Reis JS, Barbera‐Stein L. Family life education for young teens: an assessment of three interventions. Health Educ Quart 1986;13(3):201‐21. [DOI] [PubMed] [Google Scholar]
Howard 1990 {published data only}
- Howard M, McCabe JA. An information and skills approach for younger teens: Postponing Sexual Involvement program. In: Miller BC, Card JJ, Paikoff RL, Peterson JL editor(s). Preventing Adolescent Pregnancy: Model Programs and Evaluations. Sage Publications, 1992:83‐109. [Google Scholar]
- Howard M, McCabe JB. Helping teenagers postpone sexual involvement.. Fam Plann Perspect 1990;22(1):21‐26. [PubMed] [Google Scholar]
Hubbard 1998 {published data only}
- Hubbard BM, Giese ML, Rainey J. A replication study of reducing the risk, a theory‐based sexuality curriculum for adolescents. J Sch Health 1998;68(6):243‐247. [DOI] [PubMed] [Google Scholar]
Kennedy 2000c {published data only}
- Kennedy MG, Mizuno Y, Hoffman R, Baume C, Strand J. The effect of tailoring a model HIV prevention program for local adolescent target audiences. AIDS Educ Prev 2000;12(3):225‐38. [PubMed] [Google Scholar]
Kennedy 2000d {published data only}
- Kennedy MG, Mizuno Y, Hoffman R, Baume C, Strand J. The effect of tailoring a model HIV prevention program for local adolescent target audiences. AIDS Educ Prev 2000;12(3):225‐38. [PubMed] [Google Scholar]
Kirby 1991 {published data only}
- Kirby D, Barth RP, Leland N, Fetro JV. Reducing the Risk: impact of a new curriculum on sexual risk‐taking. Fam Plann Perspect 1991;23(6):253‐263. [PubMed] [Google Scholar]
Krauss 2002 {published data only}
- Krauss BJ, Godfrey CC, Day JO, Pride J. Now I can learn about HIV: Effects of a parent training on children's practical HIV knowledge and HIV worries: A randomized trial in an HIV‐affected neighborhood. International AIDS Conference. Barcelona, Spain, 2002.
- Krauss BJ, Yee D, Tiffany J, Davis WR, Reardon D, DeJesus J, Garcia E, Rivera C, Daniels T, Velez R, Godfrey CC, Goldsamt L, Almeyda L, Bula E, Jones Y, Pride J, Pierre‐Louis M, Troche E, O'Day J. Saving our children from a silent epidemic: The Path program for parents and preadolescents. In: Pequegnat W, Szapocznik J editor(s). Working with Families in the Era of HIV/AIDS. London: Sage Publications, Ltd., 2000:89‐112. [Google Scholar]
Lemieux 2003 {published data only}
- Lemieux A. Designing, implementing, and evaluating a music‐based HIV prevention intervention for urban adolescents. Doctoral Dissertation at University of Connecticut 2003:171.
Lieberman 2000 {published data only}
- Lieberman LD, Gray H, Wier M, Fiorentino R, Maloney P. Long‐term outcomes of an abstinence‐based, small‐group pregnancy prevention program in New York City schools. Fam Plann Perspect 2000;32(5):237‐245. [PubMed] [Google Scholar]
Main 1994 {published data only}
- Main DS, Iverson DC, McGloin J, Banspach SW, Collins JL, Rugg DL, Kolbe LJ. Preventing HIV infection among adolescents: evaluation of a school‐based program. Prev Med 1994;23:409‐17. [DOI] [PubMed] [Google Scholar]
McKay 2004 {published data only}
- McKay MM, Chasse K, Paikoff R, McKinney L, Baptiste D, Coleman D, Madison S, Bell CC. Family‐level impact of the CHAMP family program: A community collaborative effort to support urban families and reduce youth HIV risk exposure. Fam Proc 2004;43(1):79‐93. [DOI] [PubMed] [Google Scholar]
- McKay MM, Coleman D, Paikoff R, Baptiste D, Madison S, Scott R. Preventing HIV risk exposure in urban communities: The CHAMP family program. In: Pequegnat W, Szapocznik J editor(s). Working with Families in the Era of HIV/AIDS. London: Sage Publications, Ltd., 2000. [Google Scholar]
Merakou 2006 {published data only}
- Merakou K, Kourea‐Kremastinou J. Peer education in HIV prevention: an evaluation in schools. Eur J Public Health 2006;16(2):128‐32. [1101‐1262 (Print)] [DOI] [PubMed] [Google Scholar]
Noell 1997 {published data only}
- Noell J, Ary D, Duncan T. Development and evaluation of a sexual decision‐making and social skills program: "The Choice is Yours ‐ Preventing HIV/STDs". Health Educ Behav 1997;24(1):87‐101. [DOI] [PubMed] [Google Scholar]
O'Donnell 1999 {published data only}
- O'Donnell L, Stueve A, San Doval A, Duran R, Haber D, Anafou R, et al. The effectiveness of the Reach for Health community youth service learning program in reaching early and unprotected sex among urban middle school students. Am J Pub Health 1999;89(2):176‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peeler 2000 {published data only}
- Peeler C. An analysis of the effects of a course designed to reduce the frequency of high‐risk sexual behavior and heavy drinking. Pullman, WA: Washington State University, 2000. [Google Scholar]
Peters 1998 {published data only}
- Peters RJ. Project Alpha: a culturally appropriate approach to adolescent male sex education. Doctoral Dissertation at University of Texas School of Public Health 1998:148.
Siegel 2001 {published data only}
- Aten MJ, Siegel DM, Enaharo M, Auinger P. Keeping middle school students abstinent: outcomes of a primary prevention intervention. J Adolesc Health 2002;31:70‐8. [DOI] [PubMed] [Google Scholar]
- Siegel DM, Aten MJ, Enaharo M. Long‐term effects of a middle school and high school‐based human immunodeficiency virus sexual risk prevention intervention. Arch Pediatr Adolesc Med 2001;155:1117‐26. [DOI] [PubMed] [Google Scholar]
- Siegel DM, Aten MJ, Roghmann KJ, Enaharo M. Early effects of a school‐based human immunodeficiency virus infection and sexual risk prevention intervention. Arch Pediatr Adolesc Med 1998;152:961‐70. [DOI] [PubMed] [Google Scholar]
Smith 2000 {published data only}
- Smith MU, Dane FC, Archer ME, Devereaux RS, Katner HP. Students Together Against Negative Decisions (STAND): evaluation of a school‐based sexual risk reduction intervention in the rural South. AIDS Educ Prev 2000;12(1):49‐70. [PubMed] [Google Scholar]
Vincent 1987 {published data only}
- Koo HP, Dunteman GH, George C, Green Y, Vincent M. Reducing adolescent pregnancy through a school‐ and community‐based intervention: Denmark, South Carolina revised. Fam Plann Perspect 1994;26(5):206‐11+17. [Google Scholar]
- Vincent ML, Clearie AF, Schluchter MD. Reducing adolescent pregnancy through school and community‐based education. JAMA 1987;257(24):3382‐86. [PubMed] [Google Scholar]
Walter 1993 {published data only}
- Walter HJ, Vaughan RD. AIDS risk reduction among a multiethnic sample of urban high school students. JAMA 1993;270(6):725‐30. [PubMed] [Google Scholar]
Zabin 1986 {published data only}
- Zabin LS, Hirsch MB, Smith EA, Streett R, Hardy JB. Evaluation of a pregnancy prevention program for urban teenagers. Fam Plann Perspect 1986;18(3):119‐26. [PubMed] [Google Scholar]
References to studies awaiting assessment
Borawski 2007 {unpublished data only}
- Borawski E, Hayman L, Adams‐Davis K, Landis C. Taking Be Proud! Be Responsible! to the suburbs. http://www.case.edu/affil/healthpromotion/projects/be_proud_proj.html 2007.
Brown 2002 {unpublished data only}
- Brown EJ, Jemmott LS. Mother‐son HIV risk‐reduction program. The Advancing Nursing Practice Excellence: State of the Science. Washington, DC, 2002.
- Jemmott LS, Jemmott JB, III, Howard M, Outlaw FH, Brown EJ, Hopkins BH. Strengthening the bond: The Mother‐Son Health Promotion Project. In: Pequegnat W, Szapocznik J editor(s). Working With Families in the Era of HIV/AIDS. London: Sage Publications, Ltd., 2000. [Google Scholar]
References to ongoing studies
Jemmott 2006 {unpublished data only}
- Jemmott JB, III, Jemmott LS, Fong GT. Efficacy of an abstinence‐only intervention over 24 months: A randomized controlled trial with young adolescents. International AIDS Conference. Toronto, Canada, 2006. [DOI] [PMC free article] [PubMed]
Jemmott 2007 {unpublished data only}
- Jemmott LS, Jemmott JB, III, Hutchinson MK, Icard LD, Gipson W. The Church and Family Health Promotion Program. http://www.nursing.upenn.edu/healthdisparities/churchprogram.asp 2007.
Markham 2007 {unpublished data only}
- Markham, C. SIP 4‐04 Evaluation of Abstinence‐Only and Abstinence‐Plus Program to Prevent HIV, STD, and Pregnancy Among Middle School Students. United States National Institute of Health 2007; Vol. http://clinicaltrials.gov/ct/show/NCT00167505?order=1.
Tortolero 2007 {published data only}
- Tortolero S, Markham CM, Parcel GS, Peters RJ, Escobar‐Chaves SL, Basen‐Engquist K, Lewis HL. Using intervention mapping to adapt an effective HIV, sexually transmitted disease, and pregnancy prevention program for high‐risk minority youth. Health Promot Pract 2005;6(3):286‐98. [DOI] [PubMed] [Google Scholar]
Additional references
Adams 2004
- Adams G, Gulliford MC, Ukoumunne OC, Eldridge S, Chinn S, Campbell MJ. Patterns of intra‐cluster correlation from primary care research to inform study design and analysis. J Clin Epidemi 2004;57:785‐94. [DOI] [PubMed] [Google Scholar]
Alexander 1993
- Alexander CS, Somerfield MR, Ensminger ME, Johnson KE, Kim YJ. Consistency of adolescents' self‐report of sexual behavior in a longitudinal study. Journal of Youth and Adolescence 1993;22(5):455‐71. [Google Scholar]
Asbel 2006
- Asbel LE, Newbern EC, Salmon M, Spain CV, Goldberg M. School‐based screening for Chlamydia trachomatis and Neisseria gonorrhoeae among Philadelphia public high school students. Sex Transm Dis 2006;33(10):614‐620. [DOI] [PubMed] [Google Scholar]
AVERT 2005
- AVERT. UK HIV/AIDS FAQs. AVERT 2005; Vol. Retrieved 26 April 2005 from http://www.avert.org/aidsfaqs.htm.
Bennett 2005
- Bennett SE, Assefi NP. School‐based teenage pregnancy prevention programs: a systematic review of randomized controlled trials. J Adolesc Health 2005;36:72‐81. [DOI] [PubMed] [Google Scholar]
Berne 1999
- Berne L, Huberman B. European approaches to adolescent sexual behavior and responsibility. Washington DC: Advocates for Youth, 1999. [Google Scholar]
Berry 2005
- Berry S. AIDS in America. AVERT 2005; Vol. Retrieved 26 April 2005 from http://www.avert.org/aids‐america.htm.
Binson 1998
- Binson D, Catania JA. Respondents' understanding of the words used in sexual behavior questions. Public Opinion Quarterly 1998;62:190‐208. [Google Scholar]
Bowden 2005
- Bowden FJ, O'Keefe EJ, Primrose R, Currie MJ. Sexually transmitted infections, blood‐borne viruses and risk behaviour in an Australian senior high school population‐The SHLiRP study. Sex Health 2005;2(4):229‐36. [1448‐5028 (Print)] [DOI] [PubMed] [Google Scholar]
Brener 2004
- Brener N, Grunbaum J, Kann L, McManus T, Ross J. Assessing health risk behaviors among adolescents: the effect of question wording and appeals for honesty. J Adolesc Health 2004;35:91‐100. [DOI] [PubMed] [Google Scholar]
Catania 1996
- Catania JA, Binson D, Canchola J, Pollack LM, Hauck W. Effects of interviewer gender, interviewer choice, and item wording on responses to questions concerning sexual behavior. Public Opinion Quarterly 1996;60(3):345‐75. [Google Scholar]
Crepaz 2002
- Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: A review of social, psychological, and medical findings. AIDS 2002;16:135‐149. [DOI] [PubMed] [Google Scholar]
DiCenso 2002
- DiCenso A, Guyatt G, Willan A, Griffith L. Interventions to reduce unintended pregnancies among adolescents: Systematic review of randomised controlled trials. British Medical Journal 2002;324:1426‐1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
DiClemente 1998
- DiClemente RJ. Preventing sexually transmitted infections among adolescents: a clash of ideology and science. JAMA 1998;279(19):1574‐5. [DOI] [PubMed] [Google Scholar]
Donner 2002
- Donner A, Klar N. Issues in the meta‐analysis of cluster randomized trials. Statistics in Medicine 2002;21:2971‐80. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey‐Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Farmer 2001
- Farmer P. Infections and Inequalities: The Modern Plagues. Berkeley, CA: University of California Press, 2001. [Google Scholar]
Farr 1996
- Farr G, Castro L, Disantostefano R, Claassen E, Olguin F. Use of spermicide and impact of prophylactic condom use among sex workers in Santa Fe de Bogota, Columbia. Sex Transm Dis 1996;23(3):206‐12. [DOI] [PubMed] [Google Scholar]
Fontanet 1998
- Fontanet A, Saba J, Chandelying V, Sakondhavat C, Bhiraleus P, Rugpao S. Protection against sexually transmitted diseases by granting sex workers in Thailand the choice of using the male or female condom: results from a randomized controlled trial. AIDS 1998;12(14):1851‐9. [DOI] [PubMed] [Google Scholar]
Franklin 1997
- Franklin C, Grant D, Corcoran J, Miller PO, Bultman L. Effectiveness of prevention programs for adolescent pregnancy: a meta‐analysis. Journal of Marriage and the Family 1997;59(3):551‐67. [Google Scholar]
Frost 1995
- Frost J, Forest J. Understanding the impact of effective teenage pregnancy prevention programs. Fam Plann Perspect 1995;27:188‐95. [PubMed] [Google Scholar]
Gollub 1996
- Gollub E, French P, Latka M, Johns L, Blum L, O'Donnell J, Stein A. The women's safer sex hierarchy: initial responses to counseling on women's methods of STD/HIV prevention at an STD clinic. Int Conf AIDS. Vancouver, Canada, 1996.
Gollub 2000
- Gollub E, French P, Loundou A, Latka M, Rogers C, Stein Z. A randomized trial of hierarchical counseling in a short, clinic‐based intervention to reduce the risk of sexually transmitted diseases in women. AIDS 2000;14:1249‐55. [DOI] [PubMed] [Google Scholar]
Gribble 1999
- Gribble J, Miller H, Rogers S, et al. Interview mode and measurement of sexual behaviors: Methodological issues. J Sex Res 1999;36(1):16‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haglund 2002
- Haglund K. Sexually abstinent African American adolescent females' descriptions of abstinence. Journal of Nursing Scholarship 2002;35(3):231‐236. [DOI] [PubMed] [Google Scholar]
Haskins 1997
- Haskins R, Bevan CS. Abstinence education under welfare reform. Children and Youth Services Review 1997;19(5/6):465‐484. [Google Scholar]
Higgins 2002
- Higgins J, Thompson S. Quantifying heterogeneity in meta‐analysis. Statistics in Medicine 2002;21(11):1538‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2005
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5. The Cochrane Library, Issue 3. John Wiley & Sons, Ltd, 2005. [Google Scholar]
Hollis 1999
- Hollis S, Campbell F. What is meant by intention‐to‐treat analysis?. BMJ 1999;319:670‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Horan 1998
- Horan P, Phillips J, Hagen N. The meaning of abstinence for college students. Journal of HIV/AIDS Prevention and Education for Adolescents and Children 1998;2:51‐66. [Google Scholar]
HRW 2002
- Human Rights Watch. Ignorance only: HIV/AIDS, human rights, and abstinence‐only programs in the United States. New York, NY: Human Rights Watch, 2002. [Google Scholar]
Jaffe 2004
- Jaffe H. Whatever happened to the U.S. AIDS epidemic?. Science 2004;305:1243‐1244. [DOI] [PubMed] [Google Scholar]
Jemmott 2000
- Jemmott JB III, Jemmott LS. HIV risk reduction behavioral interventions with heterosexual adolescents. AIDS 2000;14(Supplement 2):S40‐S52. [PubMed] [Google Scholar]
Johnson 2002
- Johnson W, Semaan S, Hedges L, Ramirez G, Mullen P, Sogolow E. A protocol for the analytical aspects of a systematic review of HIV prevention research. J Acquir Immune Defic Syndr 2002;30:S62‐72. [PubMed] [Google Scholar]
Jones 1985
- Jones E, Forrest J, Goldman N, Henshaw S, Lincoln R, Rosoff J, et al. Teenage pregnancy in developed countries: Determinants and policy implications. Fam Plann Perspect 1985;17(2):53‐63. [PubMed] [Google Scholar]
Kim 1997
- Kim N, Stanton B, Li X, Dickersin K, Galbraith J. Effectiveness of the 30 adolescent AIDS‐risk reduction interventions: a quantitative review. J Adolesc Health 1997;20:204‐215. [DOI] [PubMed] [Google Scholar]
Kirby 2001
- Kirby D. Emerging answers: Research findings on programs to reduce teen pregnancy. Washington DC: National Campaign to Prevent Teen Pregnancy, 2001. [Google Scholar]
Kirby 2006
- Kirby D, Laris BA, Rolleri L. The impact of sex and HIV education programs in schools and communities on sexual behaviors among young adults. Research Triangle Park, NC: Family Health International, YouthNet Program, 2006. [Google Scholar]
Lancet 2002
- Editorial. Abstinence, monogamy, and sex. Lancet 2002;360(9327):97. [PubMed] [Google Scholar]
Lancet 2004
- Editorial. Is it churlish to criticize Bush over his spending on AIDS?. Lancet 2004;364(9431):303‐4. [DOI] [PubMed] [Google Scholar]
Lancet 2006
- Editorial. HIV prevention needs an urgent cure. Lancet 2006;367(9518):1213. [DOI] [PubMed] [Google Scholar]
Landry 1999
- Landry DJ, Kaeser L, Richards CL. Abstinence promotion and the provision of information about contraception in public school district sexuality education policies. Fam Plann Perspect 1999;31(6):280‐6. [PubMed] [Google Scholar]
Lauritsen 1997
- Lauritsen JL, Swicegood CG. The consistency of self‐reported initiation of sexual activity. Fam Plann Perspect 1997;29(5):215‐21. [PubMed] [Google Scholar]
Manlove 2004
- Manlove J, Papillo AR, Ikramullah E. Not yet: programs to delay first sex among teens. Washington, DC: National Campaign to Prevent Teen Pregnancy, 2004. [Google Scholar]
Meston 1998
- Meston CM, Heiman JR, Trapnell PD, Paulhus DL. Socially desirable responding and sexuality self‐reports. Journal of Sex Research 1998;35(2):147‐57. [Google Scholar]
Miller 2004
- Miller L, Murphy S, Clark L, Hamburger M, Moore J. Hierarchical messages for introducing multiple HIV prevention options: promise and pitfalls. AIDS Educ and Prev 2004;16(6):509‐25. [DOI] [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman D for the CONSORT Group. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. Lancet 2001;357(9263):1191‐4. [PubMed] [Google Scholar]
Montgomery 2005
- Montgomery P, Gardner F, Operario D, Mayo‐Wilson E, Tamayo S, Underhill K. The Oxford implementation Reporting Index: the development of an indicator of treatment fidelity in systematic reviews of psycho‐social interventions (Poster). Cochrane Collaboration Colloquium. Melbourne, Australia, 2005.
Morris 2006
- Morris M, Handcock M, Miller W, et al. Prevalence of HIV infection among young adults in the United States: results from the Add Health study. Am J Public Health 2006;96(6):1091‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Newcomer 1988
- Newcomer S, Udry JR. Adolescents' honesty in a survey of sexual behavior. J Adolesc Res 1988;3(3/4):419‐23. [Google Scholar]
NHS 1997
- NHS Centre for Reviews and Dissemination. Preventing and reducing the adverse effects of unintended teenage pregnancies. Effective Health Care 1997;3(1):1‐12. [Google Scholar]
O'Leary 1997
- O'Leary A, DiClemente RJ, Aral SO. Reflections on the design and reporting of STD/HIV behavioral intervention research. AIDS Educ Prev 1997;9(Supplement 1):1‐14. [PubMed] [Google Scholar]
O'Reilly 2004
- O'Reilly K, Medley A, Dennison J, Schmid GP, Sweat MD. Systematic review of the impact of abstinence‐only programmes on risk behavior in developing countries. eJIAS. 2004; Vol. 1(1):TuPeC4899.
O'Reilly 2006
- O'Reilly K, Medley A, Dennison J, Sweat MD. Systematic review of the impact of abstinence‐only programmes on risk behavior in developing countries (1990‐2005). International AIDS Conference. Toronto, Canada, 2006.
Pedlow 2003
- Pedlow C, Carey M. HIV sexual risk‐reduction interventions for youth: A review and methodological critique of randomized controlled trials. Behavior Modification 2003;27:135‐190. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peterman 2000
- Peterman TA, Lin LS, Newman DR, et al. Does measured behavior reflect STD risk? An analysis of data from a randomized controlled behavioral intervention study. Sex Transm Dis 2000;27(8):446‐51. [DOI] [PubMed] [Google Scholar]
Pitts 2001
- Pitts M, Rahman Q. Which behaviors constitute "having sex" among university students in the UK?. Archives of Sexual Behavior 2001;30(2):169‐76. [DOI] [PubMed] [Google Scholar]
Rector 2002
- Rector R. The effectiveness of abstinence education programs in reducing sexual activity among youth. Washington DC: Heritage Foundation, 2002. [Google Scholar]
Remez 2000
- Remez L. Oral sex among adolescents: Is it sex or is it abstinence?. Family Planning Perspectives 2000;32(6):298‐304. [PubMed] [Google Scholar]
Rivers 2000
- Rivers K, Aggleton P. HIV prevention in industrialized countries. In: Peterson J, DiClemente R editor(s). HIV Prevention Handbook. London: Kluwer Academic/Plenum Publishers, 2000. [Google Scholar]
Robin 2004
- Robin L, Dittus P, Whitaker D, et al. Behavioral interventions to reduce incidence of HIV, STD, and pregnancy among adolescents: A decade in review. Journal of Adolescent Health 2004;34:3‐26. [DOI] [PubMed] [Google Scholar]
Romer 1997
- Romer D, Hornik R, Stanton B, et al. "Talking" computers: A reliable and private method to conduct interviews on sensitive topics with children. J Sex Res 1997;34(1):3‐9. [Google Scholar]
Rosenbaum 2006
- Rosenbaum J. Reborn a virgin: adolescents' retracting of virginity pledges and sexual histories. Am J Public Health 2006;96(6):1098‐103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rotheram‐Borus 2000
- Rotheram‐Borus MJ, O'Keefe Z, Kracker R, Foo HH. Prevention of HIV among adolescents. Prevention Science 2000;1(1):15‐30. [DOI] [PubMed] [Google Scholar]
Sanders 1999
- Sanders S, Reinisch J. Would you say you "had sex" if...?. Journal of the American Medical Association 1999;281(3):275‐277. [DOI] [PubMed] [Google Scholar]
Sonfield 2001
- Sonfield A, Gold RB. States' implementation of the Section 510 abstinence education program, FY 1999. Family Planning Perspectives 2001;33(4):166‐171. [PubMed] [Google Scholar]
Stein 1999
- Stein Z, Saez H, El‐Sadr W, Healton C, Mannuheimer S, Messeri P, Scimeca M, Devanter N, Zimmerman R, Betne P. Safer sex strategies for women: The hierarchical model in methadone treatment clinics. J Urban Health 1999;76(1):62‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2000
- Thomas M. Abstinence‐Based Programs for Prevention of Adolescent Pregnancies. Journal of Adolescent Health 2000;26:5‐17. [DOI] [PubMed] [Google Scholar]
Turner 1998
- Turner C, Ku L, Rogers S, Lindberg L, Pleck J, Sonenstein F. Adolescent sexual behavior, drug use, and violence: New survey technology detects elevated prevalence among U.S. males. Science 1998;280(May 8):867‐73. [DOI] [PubMed] [Google Scholar]
UNAIDS 2004
- UNAIDS/WHO. 2004 Report on the Global AIDS Epidemic: 4th Global Report. Geneva: UNAIDS, 2004. [Google Scholar]
UNAIDS 2006
- UNAIDS. Report on the global AIDS epidemic. Geneva, Switzerland: UNAIDS/WHO, 2006. [Google Scholar]
Underhill 2005
- Underhill K, Montgomery P, Operario D. Abstinence‐based programs for HIV infection prevention in high‐income countries. Cochrane Database of Systematic Reviews 2005;3:Art. No.: CD005421. [DOI] [PMC free article] [PubMed] [Google Scholar]
Underhill 2006a
- Underhill K, Montgomery P, Operario D. Systematic review of abstinence‐only and abstinence‐plus programs for the prevention of HIV infection in high‐income countries. International AIDS Conference. Toronto, Canada, 2006.
Underhill 2006b
- Underhill K, Montgomery P, Operario D. Systematic review of abstinence‐only programmes for the prevention of HIV infection in high‐income countries. 1st International Workshop on HIV Transmission. Toronto, Canada: Virology Education, 2006.
Underhill 2007a
- Underhill K, Operario D, Montgomery P. Systematic review of abstinence‐plus HIV prevention programs in high‐income countries. PLoS Medicine 2007;4(9):e275. [DOI] [PMC free article] [PubMed] [Google Scholar]
Underhill 2007b
- Underhill K, Montgomery P, Operario D. Sexual abstinence only programmes to prevent HIV infection in high income countries: Systematic review. BMJ 2007;335(7613):248. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walgate 2004
- Walgate R. Bush's AIDS plan criticised for emphasising abstinence and forbidding condoms. BMJ 2004;329(7459):192. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2000
- Wang L, Davis M, Robin L, Collins J, Coyle K, Baumler E. Economic evaluation of Safer Choices: a school‐based human immunodeficiency virus, other sexually transmitted diseases, and pregnancy prevention program. Arch Pediatr Adolesc Med 2000;154(10):1017‐24. [DOI] [PubMed] [Google Scholar]
World Bank 2007
- World Bank. High Income Economies. World Bank Vol. Retrieved 15 February 2007 from http://www.worldbank.org.
Zabin 1984
- Zabin LS, Hirsch MB, Smith EA, Hardy JB. Adolescent sexual attitudes and behavior: are they consistent?. Fam Plann Perspect 1984;16(4):181‐5. [PubMed] [Google Scholar]
Zellner 2005
- Zellner J. HIV risk behavior and high risk youth: Can audio‐CASI and bogus pipeline increase the accuracy of reports?. Doctoral Dissertation at Alliant International University. San Diego, CA, 2005.
References to other published versions of this review
Underhill PLoS
- Underhill K, Operario D, Montgomery P. Systematic review of abstinence‐plus HIV prevention programs in high‐income countries.. PLoS Medicine 2007 Sept. 18;4(9):e275. [DOI] [PMC free article] [PubMed] [Google Scholar]


