Abstract
Purpose
Heterotopic calcification (HC) is a rarely reported pathology of aberrant bone deposition in extraskeletal tissue, most commonly outside of the central nervous system. While some of these findings may be incidental and asymptomatic, patients with symptomatic cord compression due to HC require consideration for expedited surgical intervention. We present the first described pediatric case of HC of the cervical spine causing spinal cord compression in a patient presenting with acute weakness and paresthesias following a minor trauma.
Case report
An 11-year-old male with a history of long-standing spastic hemiplegia thought to be related to perinatal hypoxia presented acutely myelopathic after a minor trauma. Imaging revealed an extradural calcification of the upper cervical spine with severe spinal cord compression and a focal kyphotic deformity, considered most likely to represent a calcified meningioma, nerve sheath tumor, or heterotopic calcification. The patient was taken for decompression, mass resection, and laminoplasty, with final pathology revealing heterotopic calcification.
Conclusion
While HC can develop after traumatic insult, or as late sequelae of spontaneous hemorrhage or infection, involvement of the cervical spine in a child has not previously been reported. In the setting of severe spinal cord compression with motor deficits, decompression and complete resection are safe and feasible. Histological analysis of HC will demonstrate a zonal arrangement of peripheral spindle cells/fibrous tissue, myxoid/cartilaginous tissue, and an inner core of ossification. Close attention should be paid in infancy when there may be an unclear diagnosis for weakness or spasticity without full imaging of the neuroaxis.
Keywords: Pediatric spinal cord injury, Heterotopic calcification, Cervical spine, Heterotopic ossification, Central cord syndrome
Introduction
Heterotopic calcification (HC) is a pathology of aberrant bone deposition in extraskeletal tissue and remains rarely reported in the literature [1, 2]. The most common etiology stems from traumatic sequelae, followed by tumoral or genetic origins [3]. Varying levels of TGF-β, IL-1, IL-2, and leptin increase osteoblastic activity following traumatic insult leading to bone formation [4–8]. HC most commonly occurs surrounding joints and soft tissue, with no current reports of spinal cord involvement. Of note, while 10% of pediatric patients with traumatic spinal cord injury (SCI) can develop HC, this has been linked to progressive spasticity secondary to calcification of tissue outside of the central nervous system [8–10].
Other less commonly reported manifestations of atypical calcification in the spine include diffuse spinal dural calcifications in the setting of hyperparathyroidism and ligamentum flavum calcification [2–15]. While these findings may be incidental and asymptomatic, a patient with HC within the spinal canal can present with cord compression necessitating surgical decompression. Herein, we present a case of HC of the cervical spine causing spinal cord compression in a child with subtle underlying myelopathy presenting with acute weakness and paresthesias following minor trauma.
Case report
Presentation and perioperative management
An 11-year-old male with a history of right-sided spastic hemiparesis presented with central cord syndrome, including bilateral upper greater than lower extremity weakness and dysesthetic pain, after wrestling with an older sibling. Born at 36 weeks gestation via cesarean section, his childhood was notable for slow progression of motor milestones, left-sided preference for motor tasks, and right-sided spasticity, which was ultimately diagnosed as spastic cerebral palsy. He subsequently underwent extensive orthopaedic interventions to address the sequelae of presumed cerebral palsy, including serial bracing, femoral osteotomy, and tendon lengthening procedures. Imaging of the neural axis was never obtained, and no further workup was completed for his seemingly chronic underlying myelopathy.
During the index presentation to the emergency department, the dysesthetic pain resolved, but some numbness in his bilateral hands persisted. He was 4/5 strength in his right deltoid with a positive Hoffman sign. As was his baseline, he demonstrated ambulatory spastic quadriparesis with increased tone on the right side. A CT of the cervical spine demonstrated a large, calcified mass occupying the majority of the canal, causing focal kyphosis. MRI revealed a large extradural mass from C2 to C5 with heterogeneous enhancement, adjacent dural enhancement, and internal calcifications. There was displacement and severe compression of the spinal cord. No other lesions were identified throughout the neuroaxis.
Surgical intervention
After brief stabilization and artificial mean arterial pressure (MAP) elevation in the ICU, the patient was taken to the operating room for mass resection. Somatosensory and motor-evoked potentials were monitored and stable throughout the case. A midline incision was performed after localization, and laminectomy was completed from the bottom of C2 to the top of C5. A large, calcified mass was immediately visualized occupying the entirety of the dorsal spinal canal. Under the microscope, we began internally debulking the mass on the left side of the canal, away from the spinal cord. Because the majority of the mass was densely calcified, this was achieved by switching between the high-speed drill and the ultrasonic aspirator. Once all calcified material was removed, the spinal cord began to relax back toward the center of the canal. A capsular, fibrous portion of the tumor remained in the left lateral gutter. We visualized the left C3 and C4 nerve roots, neither of which were directly involved in the lesion. A single arterial pedicle of the lesion that arose from the left exiting C4 nerve root was cauterized and cut, allowing deliverance of the remaining soft tissue mass. There was no CSF leak. A laminoplasty was performed at C3–4. Postoperatively, supraphysiologic MAP goals were maintained for 72 hours. The motor exam improved to nearly full strength in the right upper extremity, with continued improvement in sensation. The patient was discharged home ambulatory on postoperative day 4 (Figs. 1, 2 and 3).
Fig. 1.

Preoperative non-contrast CT (above) and T2 MRI of cervical spine (sagittal and axial views) displaying a left eccentric calcified mass from C2 to C5 with severe spinal cord compression
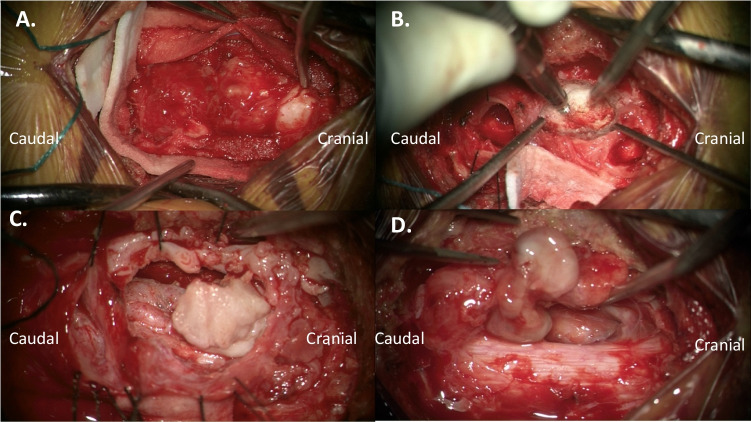
Fig. 2.
Intraoperative microscope images depicting (A) initial dissection visualizing pearly white ossified lesion at cranial portion; (B) utilization of burr for piecemeal debulking of lesions within the central canal; (C) mobilized lesion after debulking the cranial portion; and (D) re-expansion of the spinal cord along right side, with visualization of the capsular portion of the tumor adjacent to exiting C4 nerve root
Fig. 3.

Postoperative non-contrast CT of the cervical spine (sagittal and axial views) displaying gross total resection with expected pneumocephalus and re-expansion of spinal cord within the canal
Discussion
Histology/Immunohistochemical
Histologic evaluation of the mass demonstrated background fibrocartilaginous ligamentous tissue with a myxedematous degeneration (Fig. 4 A and B). There was a zonal transition in the foci of degeneration to hyaline cartilage with subsequent endochondral ossification (Fig. 4 C and D). From these areas, there was a gradual transition to lamellar bony trabeculae with fibrovascular marrow (Fig. 4E). Areas with hematopoietic marrow represented the oldest foci of degeneration within the lesion (Fig. 4).
Fig. 4.
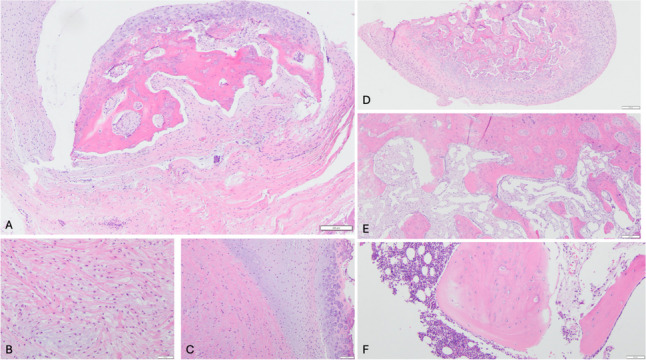
A Low-power view of ligamentous tissue with ossification. B High-power view of fibrocartilage with myxedematous degeneration. C High-power view of transition of degenerating cartilage (left) to endochondral ossification (right). D Low-power view of endochondral ossification. E Trabecular bone and fibrovascular marrow in maturing areas of lesion. F. Trabecular bone and hematopoietic marrow in the most mature foci in the lesion
Follow-up
Immediate postoperative MRI revealed a gross total resection with re-expansion of the spinal cord. XR at 2 weeks revealed kyphosis at C3–4, which progressed to nearly 50° by 6 weeks postoperatively. The patient subsequently underwent C2–5 anterior cervical discectomy and fusion and has recovered uneventfully continues to demonstrate slowly progressive neurologic improvement.
Conclusion
While HC can develop after traumatic insult, or as late sequelae of spontaneous hemorrhage or infection, involvement of the cervical spine in a child has not been described. We presented a unique case of HC within the cervical canal in a young patient with acute on chronic myelopathy, initially diagnosed as spastic hemiparesis from cerebral palsy. The inciting event was most likely a perinatal spinal hemorrhage that later calcified, though an epidural abscess following an indolent infection is also possible. In the setting of severe spinal cord compression with motor deficits, complete surgical resection is safe and feasible, and can result in gain of neurologic function despite chronic myelopathic changes. Histological specimens can reveal a zonal arrangement of peripheral spindle cells/fibrous tissue, myxoid/cartilaginous tissue, and an inner core of ossification. This is the first reported pediatric case of HC within the cervical spine presenting acutely as a spinal cord injury, with only two other reported cases of HC within the spine in adults (Table 1) [16, 17]. Close attention should be paid in infancy when there may be an unclear diagnosis for weakness or spasticity without complete neuroaxis imaging.
Table 1.
Heterotopic calcification case reports – spine
| Case report | Age/sex | Location | Final diagnosis |
|---|---|---|---|
| Weerakoon et al. [16] | 60F | L4/5 facet | Heterotopic calcification |
| Bellasri and Asri [17] | 35M | S1 nerve root | Neuritis ossificans* |
*Neuritis ossificans is described as heterotopic calcification involving nerve roots
Author contribution
T.Z. and P.R. wrote the main manuscript text. T.Z. and R.S prepared the figures and wrote the histology sections. M.D., B.G., and R.S. provided insightful edits. All authors provided edits and reviewed the manuscript.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tyler Zeoli, Email: Tyler.Zeoli@vumc.org.
Michael C. Dewan, Email: Michael.Dewan@vumc.org
References
- 1.Sun E, Hanyu-Deutmeyer AA (2024) Heterotopic ossification. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519029/ [PubMed]
- 2.Park J, Lee S, Joo KB (2014) Growing heterotopic calcification in the prevertebral space of a cervical spine as a late complication of irradiation: case report. Korean J Radiol 15(1):140–4. 10.3348/kjr.2014.15.1.140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silengo M, Defilippi C, Belligni E, Biamino E, Flex E, Brusco A, Ferrero GB, Tartaglia M, Hennekam RC (2013) Progressive extreme heterotopic calcification. Am J Med Genet A 161A(7):1706–1713. 10.1002/ajmg.a.35944 [DOI] [PubMed] [Google Scholar]
- 4.Upadhyay J, Farr OM, Mantzoros CS (2015) The role of leptin in regulating bone metabolism. Metabolism 64(1):105–113. 10.1016/j.metabol.2014.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang L, Tang X, Zhang H, Yuan J, Ding H, Wei Y (2011) Elevated leptin expression in rat model of traumatic spinal cord injury and femoral fracture. J Spinal Cord Med 34(5):501–509. 10.1179/2045772311Y.0000000034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gautschi OP, Toffoli AM, Joesbury KA, Skirving AP, Filgueira L, Zellweger R (2007) Osteoinductive effect of cerebrospinal fluid from brain-injured patients. J Neurotrauma 24(1):154–162. 10.1089/neu.2006.0166 [DOI] [PubMed] [Google Scholar]
- 7.Bidner SM, Rubins IM, Desjardins JV, Zukor DJ, Goltzman D (1990) Evidence for a humoral mechanism for enhanced osteogenesis after head injury. J Bone Joint Surg Am 72(8):1144–1149 [PubMed] [Google Scholar]
- 8.Dey D, Wheatley BM, Cholok D et al (2017) The traumatic bone: trauma-induced heterotopic ossification. Transl Res 186:95–111. 10.1016/j.trsl.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Kuijk AA, Geurts AC, van Kuppevelt HJ (2002) Neurogenic heterotopic ossification in spinal cord injury. Spinal Cord 40(7):313–326. 10.1038/sj.sc.3101309 [DOI] [PubMed] [Google Scholar]
- 10.Sullivan MP, Torres SJ, Mehta S, Ahn J (2013) Heterotopic ossification after central nervous system trauma: a current review. Bone Joint Res 2(3):51–57. 10.1302/2046-3758.23.2000152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takahashi T, Hanakita J, Minami M (2018) Pathophysiology of calcification and ossification of the ligamentum flavum in the cervical spine. Neurosurg Clin N Am 29(1):47–54. 10.1016/j.nec.2017.09.016 [DOI] [PubMed] [Google Scholar]
- 12.Malecki A, Pawloski J, Anzalone A, Shaftel K, Fadel HA, Lee I (2024) Compressive myelopathy from diffuse spinal dural calcifications in a patient with end-stage renal disease: illustrative case. J Neurosurg Case Lessons 7(9):CASE23641. 10.3171/CASE23641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rieth KG, Quindlen EA (1983) Calcified chronic spinal subdural hematoma demonstrated by computed tomography. Spine (Phila Pa 1976) 8(8):812–6. 10.1097/00007632-198311000-00002 [DOI] [PubMed] [Google Scholar]
- 14.Gebara NV, Heller GD, Phillips CD, Hatzoglou V (2015) MR findings of fibrodysplasia ossificans progressiva complicated by acute cord compression: case report and literature review. Radiol Case Rep 6(4):467. 10.2484/rcr.v6i4.467.PMID:27307924;PMCID:PMC4900023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pithon RFA, Bahia PRV, Marcondes J, Canedo N, Marchiori E (2019) Calcifying pseudoneoplasm of the neuraxis. Radiol Bras 52(5):342–343. 10.1590/0100-3984.2017.0171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weerakoon A, Sharp D, Chapman J, Clunie G (2011) Lumbar canal spinal stenosis due to axial skeletal calcinosis and heterotopic ossification in limited cutaneous systemic sclerosis: successful spinal decompression. Rheumatology 50(11):2144–2146. 10.1093/rheumatology/ker293 [DOI] [PubMed] [Google Scholar]
- 17.Bellasri S, Asri CE (2016) Neuritis ossificans: rare cause of sciatica. Pan African Medical Journal 25:170. 10.11604/pamj.2016.25.170.9937 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.