Abstract
Hematopoietic progenitor kinase 1 (HPK1) is a negative regulator of T-cell signaling. Inhibition of HPK1 with small molecules has been shown to reinvigorate the immune system toward fighting tumours in preclinical models, thus it holds promise as a therapeutic strategy in cancer immunotherapy. Herein we report a series of pyrazine carboxamide pyrazoles as selective inhibitors of HPK1. Key to our approach was the development of late-stage functionalisation chemistry which allowed for rapid SAR generation. Through these efforts, we discovered difluoroethyl pyrazole 16a, an in vivo tool which elicited the desired pharmacodynamic response in mice. Further, we describe the optimization of synthetic chemistry which could support preclinical studies of a member of this series of substituted pyrazoles.
Late-stage pyrazole functionalization was used to rapidly explore SAR and led to the identification of a potent HPK1 inhibitor.
Introduction
Few technologies have altered the cancer treatment landscape to the extent of immune checkpoint inhibitors.1 Treatment with antibodies inhibiting PD-1/PD-L1 or CTLA4 elicits a therapeutic response in a number of patients with solid tumours.2,3 Despite this success, large patient populations either do not respond4,5 to checkpoint inhibitors or relapse6,7 following treatment. As a result, there is a continued need to discover alternate mechanisms to harness a patient's immune system in cancer therapy. One particularly exciting target in this regard is hematopoietic progenitor kinase 1 (HPK1).8–11 Upon recognition of an antigen by a T cell through the T cell receptor (TCR), HPK1 phosphorylates serine 376 on SLP76. This phosphorylation event causes the LAT signalosome to dissociate, preventing further downstream signalling. It is hypothesized that inhibition of HPK1 should prevent phosphorylation of SLP76, reactivate T cell signalling, and enhance T cell activity. Initial studies in HPK1 kinase-dead mice have validated this hypothesis by improving T cell signalling and anti-tumour activity.12 As a result, many drug discovery programmes have been initiated towards small molecule HPK1 inhibitors to enhance immune function.13
Recently there have been numerous reports of tools validating this therapeutic approach in animal models, and several companies have progressed assets into the clinic.14–49 Notable examples of HPK1 inhibitors (1–4)19,37,48,49 from the literature are shown in Fig. 1a. The genesis of our medicinal chemistry program has been described recently.50 Two advanced compounds are shown in Fig. 1b. As previously noted, the utilization of the C3 methyl pyrazole (5 and 6) in the solvent channel of the HPK1 ATP binding site imparted significant selectivity gains against kinases within the MAPK family. In addition, the change to cyclopropyl at the 5-position of the pyrazine core improved the solubility of compound 6 compared to its methylamino analogue 5 (50 μM vs. 13 μM in simulated fed state intestinal fluid).
Fig. 1. (a) Previously reported HPK1 inhibitors. (b) Key C3-methyl pyrazole-containing compounds discovered through our medicinal chemistry program with an inset showing our hypothesis for pyrazole N1-substitution. (c) This work: multiple approaches to pyrazole synthesis enable the discovery and development of new analogues.
With compound 6 in hand, we recognized that compounds bearing both the methylated pyrazole and cyclopropyl group should be both selective and more soluble, thus addressing two of the key challenges in this series. Based on the X-ray co-crystal structure of 5 with HPK1 in Fig. 1b (inset), we hypothesized there was space for growth off N1 of the pyrazole. Building off that position would give us the chance to improve potency through interactions with Asp101, push on the p-loop of HPK1 to improve selectivity, and further tune physicochemical properties. Herein, we detail the development of synthetic chemistry that enabled the late-stage functionalization of intermediate 7, the evaluation of an advanced lead which was discovered through this chemistry manifold, and the route development which enabled the large-scale delivery of these methylated pyrazole HPK1 inhibitors (Fig. 1c).
Results and discussion
We deemed a late-stage functionalization strategy to be the most efficient for evaluating a diverse series of N1 substituents within the C3-methyl pyrazole scaffold. However, such an approach is not without its inherent challenges. In a putative alkylation of densely functionalized, free pyrazole-containing intermediate 7, there are multiple possible reactive sites in addition to the pyrazole, including the primary carboxamide, diarylamine, and azabenzimidazole (Scheme 1a). In the event the pyrazole moiety could be selectively targeted, mixtures of regioisomeric products are possible via competitive alkylation of N2. Nonetheless, this strategy remained appealing to us, as literature precedent supported N1 alkylation as the major product,51,52 while the undesired N2 isomers could also be isolated and evaluated in our assays. Moreover, 7 could be used as a nucleophile in multiple different reaction paradigms, allowing us to quickly generate structural diversity. A preliminary experiment with symmetrical 8 provided selective alkylation of the pyrazole to deliver 9 in 70% yield, giving us confidence in the approach (Scheme 1b).
Scheme 1. Late-stage pyrazole functionalization: conceptualization and proof-of-concept.
Intermediate 7 was synthesized in six steps from commercially available pyrazine dichloride 10 (Scheme 2). Regioselective Suzuki–Miyaura cross-coupling of the C5-chloride delivered 11 in good yield. Sandmeyer fluorination followed by SNAr with SEM-protected aminopyrazole 12 (as a mixture of pyrazole regioisomers) provided 13, which was carried crude into another Suzuki–Miyaura cross-coupling with diethanolamine boronate ester (BDEA)5314 to deliver 15 in 58% yield over three steps. Lastly, aminolysis of the methyl ester followed by SEM cleavage in a two-step, one-pot procedure provided 7·HCl in 96% yield. This efficient route allowed us to rapidly generate gram quantities of 7 in five linear synthetic steps with an overall yield of 37%.
Scheme 2. Synthesis of intermediate 7.
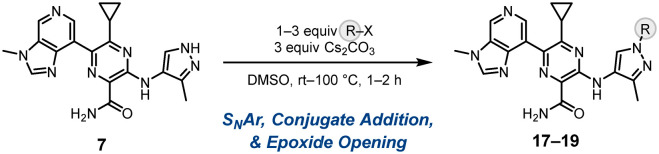
With 7 in hand and after some modest optimization, we identified mild, basic conditions that allowed us to diversify the pyrazole scaffold through four different reaction types (Fig. 2). Direct alkylation with primary and secondary alkyl (pseudo)-halides furnished over 60 analogues 16 with yields ranging from 17–90% and rr values ranging from 1 : 1 to 3 : 1. Additionally, SNAr with 2-fluoropyridine delivered N1-arylated 17 in modest yield and rr, while 1,4-addition to α,β-unsaturated electrophiles was exploited to access two compounds 18, also in good yields and rrs. Lastly, we envisaged that epoxide opening could provide compounds with differentiated solubility properties owing to the pendent alcohol in products 19. As such, we utilized this late-stage approach to generate eight analogues in moderate to good yields and regioselectivities by reaction with both linear substituted and bicyclic epoxides. All these transformations were generally found to exhibit clean reaction profiles in which the pyrazole was selectively functionalized over other reactive sites, though in some cases, carboxamide functionalization was detected in low quantities. Moreover, pyrazole regioselectivity was confirmed in each reaction paradigm by 1H-1H ROESY experiments, in which the key nOes between the pyrazole aryl C–H and alkyl C–H signals on the nascent substituent were observed in the N1 regioisomer. The desired N1-regiosiomer was often found to be major, albeit modestly. Regioisomers were most commonly separated using SFC with a chiral stationary phase, though flash chromatography could be used to separate them in some instances.
Fig. 2. Late-stage diversification of 7via alkylation, SNAr, conjugate addition, and epoxide opening under basic conditions. Yields are reported after column chromatography, and rr values were measured either based on crude 1H NMR or based on SFC with a chiral stationary phase. Conditions: (a) 1 equiv. 7, 1–3 equiv. electrophile, 1–3 equiv. Cs2CO3, DMSO or DMF, rt–100 °C. (b) 1 equiv. 7, 1.5 equiv. α,β-unsaturated electrophile, 0.75 equiv. DBU, DMSO, rt.
This late-stage pyrazole functionalization was a highly efficient way to quickly generate 74 diverse analogues, allowing us to rapidly evaluate the SAR around pyrazole N1-substitution and test our design hypotheses. Alkylation provided the largest set of pyrazole compounds for biological testing, several of which are detailed in Table 1. As a reference, N1-methylated pyrazole 6 provided important improvements in solubility and selectivity compared to compound 5 (Fig. 1b). Selectivity, in particular, has been a challenge across a number of HPK1 programs, as inhibition of off-target kinases can have an antagonistic effect on T-cell signaling,54–56 thus cancelling out the effects of HPK1 inhibition. Methyl pyrazole 6 showed good potency both in a biochemical ADP-Glo assay measuring HPK1 inhibition and an assay in primary human T-cells measuring increases in IL-2 secretion. At the highest concentrations of the assay in primary human T-cells, 6 showed some decreases in IL-2 secretion. Additionally, despite significant improvements, 6 carried a risk for poor absorption at higher doses. Thus, we hoped our late-stage alkylation approach would reveal compounds with improved profiles. Indeed, N1-difluoroethyl pyrazole 16a, which was designed to push on the flexible p-loop of HPK1,22 improved selectivity versus LCK, maintained excellent potency, and improved stability in HLM. As a result, it was profiled further as an in vivo tool to understand pharmacokinetic/pharmaco-dynamic relationships.
Table 1. Evaluation of N1-alkylated pyrazoles generated through late-stage alkylation.

| ||||||||
|---|---|---|---|---|---|---|---|---|
| Compound | R | HPK1 ADP-Glo IC50 (nM) | GLK ADP-Glo IC50 (nM) | LCK ADP-Glo IC50 (nM) | IL-2 EC50 (nM) | log D7.4 | Aq. solubility (μM) | HLM (μl min−1 mg−1) |
| 6 | Me | <3 | 91 | 5100 | 66 | 2.4 | 7.3 | <5.6b |
| 16a |

|
<3 | 158 | 17 400 | 72 | 2.6 | 13 | <3.0 |
| 16b |

|
<3 | 50 | 2200 | 101 | 2.1 | 51 | 13 |
| 16c |

|
<4a | 321 | 13 000 | 139 | 1.9 | 31 | 248 |
| 16d |

|
<3 | 137 | 3400 | 1980 | 1.3 | >1000 | 15 |
The average of two runs: <3 nM and 5 nM.
The average of three runs: <3.0, 6.7, and 7.2 μL min−1 mg−1.
We also explored several other avenues to enhance solubility within the late-stage alkylation library. For example, oxetane 16b was envisioned to lower log D relative to 6 and 16a, while morpholine 16c was designed to test the effect of basic functionality. Pyrrolidinone 16d was intended to disrupt crystal packing. These strategies all worked with varying levels of success, the most impressive being the >100-fold solubility gain realized with pyrrolidinone 16d. Despite increases in solubility, 16b–d were notably less potent and therefore not explored further. Many other analogues were evaluated as part of the late-stage alkylation library, but unfortunately none were as compelling as those highlighted here.
While our most promising functionalized pyrazoles came from alkylation, we also accessed a wide range of chemical space through late-stage SNAr (17), conjugate addition (18), and epoxide opening reactions (19). Select analogues that we synthesized using those strategies are shown in Table 2. Pyridine 17 lost biochemical potency and was thus not tested in our T-cell assay. Nitrile 18—which was synthesized through conjugate addition after a failed attempt at direct alkylation with 3-bromopropionitrile—maintained potency and showed reasonable solubility at the expense of metabolic stability. Lastly, alcohols 19a–c displayed reasonable profiles but were neither as potent nor selective as our leads 6 or 16a.
Table 2. Evaluation of N1-functionalized pyrazoles generated through late-stage SNAr, conjugate addition, & epoxide opening.
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Compound | R | HPK1 ADP-Glo IC50 (nM) | GLK ADP-Glo IC50 (nM) | LCK ADP-Glo IC50 (nM) | IL-2 EC50 (nM) | log D7.4 | Aq. solubility (μM) | HLM (μl min−1 mg−1) |
| 17 |

|
13 | 927 | 47 800 | N/A | 3.9 | 7 | <3.0 |
| 18 |

|
<3 | 118 | 5800 | 107 | 2.0 | 16 | 8.1 |
| 19a |

|
<3 | 611 | 4600 | 246 | 2.0 | 22 | <3.0 |
| 19b |

|
<3 | 410 | 2500 | 193 | 2.5 | 18 | 30 |
| 19c |

|
<3 | 276 | 6500 | 190 | 1.9 | 13 | <3.0 |
Given that difluoroethyl pyrazole 16a showed good potency and selectivity with very little diminished IL-2 secretion at high concentrations in our T-cell assay (Fig. 3)—as well as good physicochemical properties—we intended to profile it further in a variety of safety and pharmacokinetic experiments. As such, more material was required. While late-stage alkylation of 7 was highly effective to deliver the initial quantities of this lead compound, we deemed that it would not be suitable for delivering larger batches, owing in large part to the need to separate the N1- and N2-alkylated pyrazole regioisomers by preparative SFC in the final step. For the next batch of 16a, we opted for the route shown in Scheme 3, beginning with the alkylation of nitropyrazole 20 on 5 g scale.51 Difluoroethyl 21 was isolated in 55% yield following regioisomer separation by chiral SFC. Hydrogenation of 21 furnished aminopyrazole 22, which was used directly in an SNAr reaction with fluoropyrazine 23, which was prepared from intermediate 11 using a Sandmeyer fluorination as shown in Scheme 2, to deliver 24 in 91% yield. Suzuki–Miyaura cross coupling with BDEA ester 14 provided 25, which was converted to carboxamide 16a in 66% yield over two steps.
Fig. 3. Profile of 16a in the T-cell assay.
Scheme 3. Gram-scale re-synthesis of 16a.
Strategically, performing the alkylation and SFC separation early in the sequence was more efficient and less wasteful of our pyrazine- and azabenzimidazole-based intermediates, and it allowed us to rapidly deliver multi-gram quantities of 16a for additional profiling. However, preparative SFC was still required to efficiently separate the N1- and N2-pyrazole regioisomers. Moreover, we discovered through our work on related compounds50 that alkylated nitropyrazoles, like 21, are potentially explosive and therefore pose safety risks. To mitigate these key issues with an eye toward future larger-scale deliveries of 16a, we envisioned an alternate strategy involving a bespoke pyrazole synthesis. We hypothesized this could proceed via condensation of a hydrazine with an α,β-unsaturated β-keto ester that would be highly regioselective and therefore preclude the need for SFC (Scheme 4).57 We were able to demonstrate the reaction between 26 and difluoroethyl hydrazine 27 to deliver 28 in 62% yield and >20 : 1 rr following ester saponification. Aminopyrazole 22 could then be accessed through a Curtius rearrangement/deprotection sequence that was exemplified for another lead compound in this series. Although we never exemplified this sequence to deliver large quantities of 16a, our previous publication50 shows that the approach is indeed viable for related N1-alkylated pyrazoles with high levels of regioselectivity on large scale.
Scheme 4. Bespoke pyrazole synthesis via cyclocondensation.
Table 3 presents an overview of the safety and pharmacokinetic data acquired for 16a. The compound showed no liabilities in CYP reversible and time-dependent inhibition experiments and was also found to be clean in a series of ion channel inhibition assays. Furthermore, 16a had low intrinsic clearance in both human and rat hepatocytes. It was found to have high intrinsic permeability and a moderate efflux ratio, as assessed in separate Caco-2 assays. In vivo pharmacokinetic experiments were performed in rat and mouse. At low doses, reasonable absorption was observed in both species. Moderate clearance was observed, which was well-predicted by in vitro parameters, indicating that metabolism is primarily hepatic.
Table 3. Profile of 16a across various physicochemical, in vitro, and in vivo assays.
| CYP panel IC50: 1A2, 2C9, 2C19, 2D6, 3A4 (μM) | >30 all |
| CYP panel TDI: 1A2, 2C9, 2C19, 2D6, 3A4 (% inhibition) | <20 all |
| Cardio panel IC50: hERG, NaV1.5, IKs, Ito Kv4.3 (μM) | >20 all |
| Human Heps CLint [(μL min−1)/(106 cells)] | <1.0 |
| Rat Heps CLint [(μL min−1)/(106 cells)] | 4.5 |
| Human plasma protein binding (% free) | 7.2 |
| Caco2 Papp (10−6 cm s−1) | 82 |
| Caco2 efflux ratio | 14 |
| Mouse PK: oral bioavailability (%)/CL (mL min−1 kg−1)/Vss (L kg−1)/t1/2 (h) | 14/23/0.80/2.6 |
| Rat PK: oral bioavailability (%)/CL (mL min−1 kg−1)/Vss (L kg−1)/t1/2 (h) | 60/20/1.2/2.0 |
The feasibility of using 16a as a tool for in vivo PK/PD experiments was assessed through single dose pharmacokinetic experiments in mice. As shown in Fig. 4, 16a had favorable exposure at 30 mg kg−1. As such, the compound was taken forward into a single dose PK/PD study. Mice were given a single oral dose of 30 mg kg−1, and pSLP76 levels were measured at 2, 6, 16, and 24 hours. Maximal pSLP76 inhibition was observed 6 hours following oral dosing with sustained inhibition through the 24-hour time point. Having displayed a strong in vivo pharmacodynamic response, 16a was thus found to have the potential to serve as a tool for studying the effects of selective HPK1 inhibition.
Fig. 4. (a) Pharmacokinetic profile of 16a in mice. C57BL/6 mice were given a single dose of 16a at 1 mg kg−1 intravenously or 30 mg kg−1 by oral gavage. Plasma concentration was monitored over 8 or 24 hours. Data points are individual animals, and solid lines are geometric means. (b) Pharmacodynamic response in mice to a single oral dose of 16a given at 30 mg kg−1. Plasma levels of pSLP76 were measured at 0, 2, 6, 16, and 24 hours.
Conclusions
We have described our medicinal chemistry approach towards the optimization of a series of pyrazine carboxamide HPK1 inhibitors bearing a pyrazole-derived solvent tail. Our initial hypothesis was born from an analysis of X-ray crystal structures showing extra space available in the HPK1 binding site for elaborated pyrazole substituents that could allow us to tune kinase selectivity and physicochemical properties. To test this hypothesis, we developed a selective, late-stage pyrazole functionalization strategy to rapidly access a variety of substituents off N1 of the pyrazole. Upon evaluating many analogues which addressed the physicochemical and selectivity concerns of the initial leads, we selected N1-difluoroethyl pyrazole 16a for further evaluation. We therefore developed a more scalable route to this key compound that mitigated some issues with the late-stage alkylation approach and delivered the first multigram batch to supply in vivo PK/PD studies. Upon oral dosing at 30 mg kg−1 in mice, we observed significant reductions in pSLP76, consistent with inhibition of HPK1 in vivo. The work presented here in serves as an example of how synthetic chemistry can enable the rapid discovery and subsequent development of candidate drug-quality compounds.
Materials and methods
In vivo studies were performed at AstraZeneca in accordance with the Animal Care and Use guidelines approved by the AstraZeneca Institutional Animal Care and Use Committee. Mouse PK studies used a formulation of 0.5% HPMC and 0.1% Tween in water. Rat PK studies used a formulation of 95/5 SBE-B-CD (30% w/v in water)/5% DMSO. The dosing volume for all PK studies was 5 mL kg−1. For the PK/PD study, MC38 cells were injected subcutaneously into the right flank of female Balb/cmice (Envigo). 16a was dosed via oral administration once, using a dosing volume of 10 mL kg−1 and a formulation of Labrasol/40% v/v Kolliphor HS15 solution/water 45.0/27.5/27.5 at a concentration of up to 15 mg mL−1; once tumors reached an average tumor volume of 75 mm3. Mice were maintained in a controlled, pathogen-free environment at 20 to 25 °C, 40–70% humidity, and 12 h light/dark cycle. pSLP76 was detected by western blotting from tumor lysates and normalized to total SLP76 signal. Cell Signaling Technology antibodies #76384 and #4958 were used for detection of pSLP76 and total SLP76, respectively. pSLP76 inhibition was inferred by comparing signal from tumors in vehicle mice vs. compound dosed mice.
Author contributions
All authors were involved in the conception, execution, and/or data analysis of the experiments presented in this manuscript. AJM and LAM prepared the manuscript. All authors have given approval to the final version of the manuscript.
Conflicts of interest
The authors declare the following competing financial interest(s): all authors are current or former employees of AstraZeneca and may currently have or have had a financial stake in the performance of AstraZeneca.
Supplementary Material
Acknowledgments
The authors would like to thank Dr Robert Ziegler for helpful discussions.
Electronic supplementary information (ESI) available. See DOI: https://doi.org/10.1039/d5md00309a
Data availability
The data supporting this article have been included as part of the ESI.† Crystallographic data for 5 bound to HPK1 has been deposited at the PDB under accession code 9QT6 and can be obtained from https://www.wwpdb.org/.
Notes and references
- Ribas A. Wolchok J. D. Science. 2018;359:1350–1355. doi: 10.1126/science.aar4060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D. S. Mellman I. Immunity. 2013;39:1–10. doi: 10.1016/j.immuni.2013.07.012. [DOI] [PubMed] [Google Scholar]
- Waldman A. D. Fritz J. M. Lenardo M. J. Nat. Rev. Immunol. 2020;20:651–668. doi: 10.1038/s41577-020-0306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D. S. Mellman I. Nature. 2017;541:321–330. doi: 10.1038/nature21349. [DOI] [PubMed] [Google Scholar]
- Haslam A. Prasad V. JAMA Netw. Open. 2019;2:e192535. doi: 10.1001/jamanetworkopen.2019.2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma P. Hu-Lieskovan S. Wargo J. A. Ribas A. Cell. 2017;168:707–723. doi: 10.1016/j.cell.2017.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowicki T. S. Hu-Lieskovan S. Ribas A. Cancer J. 2018;24:47–53. doi: 10.1097/PPO.0000000000000303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawasdikosol S. Zha R. Yang B. Burakoff S. Immunol. Res. 2012;54:262–265. doi: 10.1007/s12026-012-8319-1. [DOI] [PubMed] [Google Scholar]
- Alzabin S. Pyarajan S. Yee H. Kiefer F. Suzuki A. Burakoff S. Sawasdikosol S. Cancer Immunol., Immunother. 2010;59:419–429. doi: 10.1007/s00262-009-0761-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling P. Meyer C. F. Redmond L. P. Shui J.-W. Davis B. Rich R. R. Hu M. C. T. Wange R. L. Tan T.-H. J. Biol. Chem. 2001;276:18908–18914. doi: 10.1074/jbc.M101485200. [DOI] [PubMed] [Google Scholar]
- Shui J.-W. Boomer J. S. Han J. Xu J. Dement G. A. Zhou G. Tan T.-H. Nat. Immunol. 2007;8:84–91. doi: 10.1038/ni1416. [DOI] [PubMed] [Google Scholar]
- Hernandez S. Qing J. Thibodeau R. H. Du X. Park S. Lee H.-M. Xu M. Oh S. Navarro A. Roose-Girma M. Newman R. J. Warming S. Nannini M. Sampath D. Kim J. M. Grogan J. L. Mellman I. Cell Rep. 2018;25:80–94. doi: 10.1016/j.celrep.2018.09.012. [DOI] [PubMed] [Google Scholar]
- Linney I. D. Kaila N. Expert Opin. Ther. Pat. 2021;31:893–910. doi: 10.1080/13543776.2021.1924671. [DOI] [PubMed] [Google Scholar]
- Zhou L. Wang T. Zhang K. Zhang X. Jiang S. Eur. J. Med. Chem. 2022;244:114819. doi: 10.1016/j.ejmech.2022.114819. [DOI] [PubMed] [Google Scholar]
- Sokolsky A. Vechorkin O. Hummel J. R. Styduhar E. D. Wang A. Nguyen M. H. Ye H. F. Liu K. Zhang K. Pan J. Ye Q. Atasoylu O. Behshad E. He X. Conlen P. Stump K. Ye M. Diamond S. Covington M. Yeleswaram S. Yao W. ACS Med. Chem. Lett. 2023;14:116–122. doi: 10.1021/acsmedchemlett.2c00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan B. K. Seward E. Lainchbury M. Brewer T. F. An L. Blench T. Cartwright M. W. Chan G. K. Y. Choo E. F. Drummond J. Elliott R. L. Gancia E. Gazzard L. Hu B. Jones G. E. Luo X. Madin A. Malhotra S. Moffat J. G. Pang J. Salphati L. Sneeringer C. J. Stivala C. E. Wei B. Wang W. Wu P. Heffron T. P. ACS Med. Chem. Lett. 2022;13:84–91. doi: 10.1021/acsmedchemlett.1c00473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vara B. A. Levi S. M. Achab A. Candito D. A. Fradera X. Lesburg C. A. Kawamura S. Lacey B. M. Lim J. Methot J. L. Xu Z. Xu H. Smith D. M. Piesvaux J. A. Miller J. R. Bittinger M. Ranganath S. H. Bennett D. J. DiMauro E. F. Pasternak A. ACS Med. Chem. Lett. 2021;12:653–661. doi: 10.1021/acsmedchemlett.1c00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu E. C. Methot J. L. Fradera X. Lesburg C. A. Lacey B. M. Siliphaivanh P. Liu P. Smith D. M. Xu Z. Piesvaux J. A. Kawamura S. Xu H. Miller J. R. Bittinger M. Pasternak A. ACS Med. Chem. Lett. 2021;12:459–466. doi: 10.1021/acsmedchemlett.0c00672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degnan A. P. Kumi G. K. Allard C. W. Araujo E. V. Johnson W. L. Zimmermann K. Pearce B. C. Sheriff S. Futran A. Li X. Locke G. A. You D. Morrison J. Parrish K. E. Stromko C. Murtaza A. Liu J. Johnson B. M. Vite G. D. Wittman M. D. ACS Med. Chem. Lett. 2021;12:443–450. doi: 10.1021/acsmedchemlett.0c00660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malchow S. Korepanova A. Panchal S. C. McClure R. A. Longenecker K. L. Qiu W. Zhao H. Cheng M. Guo J. Klinge K. L. Trusk P. Pratt S. D. Li T. Kurnick M. D. Duan L. Shoemaker A. R. Gopalakrishnan S. M. Warder S. E. Shotwell J. B. Lai A. Sun C. Osuma A. T. Pappano W. N. ACS Chem. Biol. 2022;17:556–566. doi: 10.1021/acschembio.1c00819. [DOI] [PubMed] [Google Scholar]
- Stumpf A. Xu D. Ranjan R. Angelaud R. Gosselin F. Org. Process Res. Dev. 2023;27:523–529. doi: 10.1021/acs.oprd.2c00384. [DOI] [Google Scholar]
- Gallego R. A. Bernier L. Chen H. Cho-Schultz S. Chung L. Collins M. Del Bel M. Elleraas J. Costa Jones C. Cronin C. N. Edwards M. Fang X. Fisher T. He M. Hoffman J. Huo R. Jalaie M. Johnson E. Johnson T. W. Kania R. S. Kraus M. Lafontaine J. Le P. Liu T. Maestre M. Matthews J. McTigue M. Miller N. Mu Q. Qin X. Ren S. Richardson P. Rohner A. Sach N. Shao L. Smith G. Su R. Sun B. Timofeevski S. Tran P. Wang S. Wang W. Zhou R. Zhu J. Nair S. K. J. Med. Chem. 2023;66:4888–4909. doi: 10.1021/acs.jmedchem.2c02038. [DOI] [PubMed] [Google Scholar]
- Wang M. S. Wang Z. Z. Li Z. L. Gong Y. Duan C. X. Cheng Q. H. Huang W. Yang G. F. J. Med. Chem. 2023;66:611–626. doi: 10.1021/acs.jmedchem.2c01551. [DOI] [PubMed] [Google Scholar]
- Zhu Q. Chen N. Tian X. Zhou Y. You Q. Xu X. J. Med. Chem. 2022;65:8065–8090. doi: 10.1021/acs.jmedchem.2c00172. [DOI] [PubMed] [Google Scholar]
- Wu F. Li H. An Q. Sun Y. Yu J. Cao W. Sun P. Diao X. Meng L. Xu S. Eur. J. Med. Chem. 2023;254:115355. doi: 10.1016/j.ejmech.2023.115355. [DOI] [PubMed] [Google Scholar]
- Shi H. Tang H. Li Y. Chen D. Liu T. Chen Y. Wang X. Chen L. Wang Y. Xie H. Xiong B. Eur. J. Med. Chem. 2023;248:115064. doi: 10.1016/j.ejmech.2022.115064. [DOI] [PubMed] [Google Scholar]
- Toure M. Johnson T. Li B. Schmidt R. Ma H. Neagu C. Lopez A. U. Wang Y. Guler S. Xiao Y. Henkes R. Ho K. Zhang S. Chu C. L. Gundra U. M. Porichis F. Li L. Maurer C. K. Fang Z. Musil D. DiPoto M. Friis E. Jones R. Jones C. Cummings J. Chekler E. Tanzer E. M. Huck B. Sherer B. Bioorg. Med. Chem. 2023;92:117423. doi: 10.1016/j.bmc.2023.117423. [DOI] [PubMed] [Google Scholar]
- Zhou L. Ye X. Wang K. Shen H. Wang T. Zhang X. Jiang S. Xiao Y. Zhang K. Bioorg. Chem. 2023;138:106682. doi: 10.1016/j.bioorg.2023.106682. [DOI] [PubMed] [Google Scholar]
- Zeng S. Zeng M. Yuan S. He L. Jin Y. Huang J. Zhang M. Yang M. Pan Y. Wang Z. Chen Y. Xu X. Huang W. Bioorg. Chem. 2023;139:106728. doi: 10.1016/j.bioorg.2023.106728. [DOI] [PubMed] [Google Scholar]
- Zhang J. Li Y. Tang H. Zhou Q. Tong L. Ding J. Xie H. Xiong B. Liu T. Bioorg. Chem. 2023;140:106811. doi: 10.1016/j.bioorg.2023.106811. [DOI] [PubMed] [Google Scholar]
- Xie C. Liu B. Song Z. Yang Y. Dai M. Gao Y. Yao Y. Ding C. Ai J. Zhang A. J. Med. Chem. 2023;66:16201–16221. doi: 10.1021/acs.jmedchem.3c01571. [DOI] [PubMed] [Google Scholar]
- Setsu G. Goto M. Ito K. Taira T. Miyamoto M. Watanabe T. Taniguchi T. Umezaki Y. Nakazawa Y. Uesugi S. Mori K. Horiuchi T. Obuchi W. Minami M. Shimada T. Wada C. Yoshida T. Higuchi S. Eur. J. Pharmacol. 2023;961:176184. doi: 10.1016/j.ejphar.2023.176184. [DOI] [PubMed] [Google Scholar]
- Feng D. Liu B. Chen Z. Xu J. Geng M. Duan W. Ai J. Zhang H. J. Biomol. Struct. Dyn. 2024;43(8):4152–4164. doi: 10.1080/07391102.2024.2301754. [DOI] [PubMed] [Google Scholar]
- Chen L. Zhang B. Zhou P. Duan Y. He C. Zhong W. Wang T. Xu S. Chen J. Yao H. Xu J. Bioorg. Chem. 2024;153:107814. doi: 10.1016/j.bioorg.2024.107814. [DOI] [PubMed] [Google Scholar]
- Zhang Z. Guo L. Zhao M. Pan H. Dong Z. Wang L. Yang X. Zhang Z. Wu M. Chang Y. Yang Y. Sun L. Liu S. Zhu R. Zheng H. Dai X. Zhang X. Jiang C. Zhu Z. Zhang Y. Liu D. J. Med. Chem. 2024;67:18682–18698. doi: 10.1021/acs.jmedchem.4c01906. [DOI] [PubMed] [Google Scholar]
- Peng J. Ding X. Shih P.-Y. Meng Q. Ding X. Zhang M. Aliper A. Ren F. Lu H. Zhavoronkov A. Eur. J. Med. Chem. 2024;279:116877. doi: 10.1016/j.ejmech.2024.116877. [DOI] [PubMed] [Google Scholar]
- Tellis J. C. Wei B. Siu M. An L. Chan G. K. Chen Y. Du X. Gazzard L. Hu B. Kiefer J. Kakiuchi-Kiyota S. Lainchbury M. Linehan J. L. Luo X. Malhotra S. Mendonca R. Pang J. Ran Y. Sethuraman V. Seward E. Sneeringer C. Su D. Wang W. Wu P. Moffat J. G. Heffron T. P. Choo E. F. Chan B. K. ACS Med. Chem. Lett. 2024;15:1606–1614. doi: 10.1021/acsmedchemlett.4c00319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng J. Ding X. Chen C. X. Zhao P. Ding X. Zhang M. Aliper A. Ren F. Lu H. Zhavoronkov A. J. Med. Chem. 2024;67:21520–21544. doi: 10.1021/acs.jmedchem.4c02421. [DOI] [PubMed] [Google Scholar]
- Wu M. Wu Y. Jin Y. Mao X. Zeng S. Yu H. Zhang J. Jin Y. Wu Y. Xu T. Chen Y. Wang Y. Yao X. Che J. Huang W. Dong X. J. Med. Chem. 2024;67:13852–13878. doi: 10.1021/acs.jmedchem.4c00644. [DOI] [PubMed] [Google Scholar]
- Xu J. Li Y. Chen X. Yang J. Xia H. Huang W. Zeng S. Bioorg. Chem. 2024;153:107866. doi: 10.1016/j.bioorg.2024.107866. [DOI] [PubMed] [Google Scholar]
- Zeng S. Jin Y. Xia H. Shang Y. Li Y. Wang Z. Huang W. Bioorg. Chem. 2024;143:107016. doi: 10.1016/j.bioorg.2023.107016. [DOI] [PubMed] [Google Scholar]
- Zeng S. Wu M. Jin Y. Ye Y. Xia H. Chen X. Che J. Wang Z. Wu Y. Dong X. Chen Y. Huang W. Eur. J. Med. Chem. 2024;267:116206. doi: 10.1016/j.ejmech.2024.116206. [DOI] [PubMed] [Google Scholar]
- Qiu X. Liu R. Ling H. Zhou Y. Ren X. Zhou F. Zhang J. Huang W. Wang Z. Ding K. Eur. J. Med. Chem. 2024;269:116310. doi: 10.1016/j.ejmech.2024.116310. [DOI] [PubMed] [Google Scholar]
- Fu S. Wei J. Li C. Zhang N. Yue H. Yang A. Xu J. Dong K. Xing Y. Tong M. Shi X. Xi Z. Wang H. Hou Y. Zhao Y. Bioorg. Chem. 2024;148:107454. doi: 10.1016/j.bioorg.2024.107454. [DOI] [PubMed] [Google Scholar]
- Duan Y. Guo Z. Zhong W. Chen J. Xu S. Liu J. Xu J. Future Med. Chem. 2024;16:2431–2450. doi: 10.1080/17568919.2024.2420630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu F. Li H. Li W. Zhang L. An Q. Sun J. Zhang Q. Sun Y. Xu L. Yu J. Diao X. Li J. Meng L. Xu S. Bioorg. Med. Chem. 2025;119:118079. doi: 10.1016/j.bmc.2025.118079. [DOI] [PubMed] [Google Scholar]
- Mao J. Zhou L. Wu Y. Wang K. Ye X. Wang T. Yang J. Tong J. Miao Q. Jiang S. Xiao Y. Zhang K. Bioorg. Chem. 2025;156:108158. doi: 10.1016/j.bioorg.2025.108158. [DOI] [PubMed] [Google Scholar]
- Gallego R. A. Cho-Schultz S. Del Bel M. Dechert-Schmitt A.-M. Donaldson J. S. He M. Jalaie M. Kania R. Matthews J. McTigue M. Tuttle J. B. Risley H. Zhou D. Zhou R. Ahmad O. K. Bernier L. Berritt S. Braganza J. Chen Z. Cianfrogna J. A. Collins M. Costa Jones C. Cronin C. N. Davis C. Dress K. Edwards M. Farrell W. France S. P. Grable N. Johnson E. Johnson T. W. Jones R. Knauber T. Lafontaine J. Loach R. P. Maestre M. Miller N. Moen M. Monfette S. Morse P. Nager A. R. Niosi M. Richardson P. Rohner A. K. Sach N. W. Timofeevski S. Tucker J. W. Vetelino B. Zhang L. Nair S. K. J. Med. Chem. 2024;67:22002–22038. doi: 10.1021/acs.jmedchem.4c01930. [DOI] [PubMed] [Google Scholar]
- Kaila N., Linney I., Whittaker B., Ward S., Wishart G., Feyfant E., Greenwood J., Leffler A., Cote A., Albanese S., Severance D., Briggs M., Carreiro S., Ciccone D., Lazari V., Leit S., Loh C., Tummino P., McElwee J., Rocnik J., Ashwell M., Collis A., Boiko S., Daigle S. and Srivastava B., presented in part at ACS Fall National Meeting, Colorado, USA, Denver, August 2024 [Google Scholar]
- Shields J. D. Baker D. Balazs A. Y. S. Bommakanti G. Casella R. Cao S. Cook S. Escobar R. A. Fawell S. Gibbons F. D. Giblin K. A. Goldberg F. W. Gosselin E. Grebe T. Hariparsad N. Hatoum-Mokdad H. Howells R. Hughes S. J. Jackson A. Reddy I. K. Kettle J. G. Lamont G. M. Lamont S. Li M. Lill S. O. N. Mele D. A. Metrano A. J. Mfuh A. M. Morrill L. A. Peng B. Pflug A. Proia T. A. Rezaei H. Richards R. Richter M. Robbins K. J. Martin M. S. Schimpl M. Schuller A. G. Sha L. Shen M. Sheppeck J. E. II M. S. Stokes S. Song K. Sun Y. Tang H. Wagner D. J. Wang J. Wang Y. Wilson D. M. Wu A. Wu C. Wu D. Wu Y. Xu K. Yang Y. Yao T. Ye M. Zhang A. X. Zhang H. Zhai X. Zhou Y. Ziegler R. E. Grimster N. P. J. Med. Chem. 2025;68(4):4582–4595. doi: 10.1021/acs.jmedchem.4c02631. [DOI] [PubMed] [Google Scholar]
- Huang A. Wo K. Lee S. Y. C. Kneitschel N. Chang J. Zhu K. Mello T. Bancroft L. Norman N. J. Zheng S.-L. J. Org. Chem. 2017;82:8864–8872. doi: 10.1021/acs.joc.7b01006. [DOI] [PubMed] [Google Scholar]
- Degorce S. L. Boyd S. Curwen J. O. Ducray R. Halsall C. T. Jones C. D. Lach F. Lenz E. M. Pass M. Pass S. Trigwell C. J. Med. Chem. 2016;59:4859–4866. doi: 10.1021/acs.jmedchem.6b00203. [DOI] [PubMed] [Google Scholar]
- Inglesby P. A. Agnew L. R. Carter H. L. Ring O. T. Org. Process Res. Dev. 2020;24:1683–1689. doi: 10.1021/acs.oprd.0c00296. [DOI] [Google Scholar]
- Chuang H.-C. Lan J.-L. Chen D.-Y. Yang C.-Y. Chen Y.-M. Li J.-P. Huang C.-Y. Liu P.-E. Wang X. Tan T.-H. Nat. Immunol. 2011;12:1113–1118. doi: 10.1038/ni.2121. [DOI] [PubMed] [Google Scholar]
- Chuang H.-C. Tsai C.-Y. Hsueh C.-H. Tan T.-H. Sci. Adv. 2018;4:eaat5401. doi: 10.1126/sciadv.aat5401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May-Dracka T. L. Arduini R. Bertolotti-Ciarlet A. Bhisetti G. Brickelmaier M. Cahir-McFarland E. Enyedy I. Fontenot J. D. Hesson T. Little K. Lyssikatos J. Marcotte D. McKee T. Murugan P. Patterson T. Peng H. Rushe M. Silvian L. Spilker K. Wu P. Xin Z. Burkly L. C. Bioorg. Med. Chem. Lett. 2018;28:1964–1971. doi: 10.1016/j.bmcl.2018.03.032. [DOI] [PubMed] [Google Scholar]
- Meazza G., Sillani L., Mereghetti P. and Forgia D., WO2015097658A1, 2015
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting this article have been included as part of the ESI.† Crystallographic data for 5 bound to HPK1 has been deposited at the PDB under accession code 9QT6 and can be obtained from https://www.wwpdb.org/.










