Abstract
Background
Absence from work after breast cancer diagnosis may be part of the burden of disease for women with cancer, but little research has addressed this. We examined work absences of 4 weeks or more among women who had had breast cancer during the 3 years after diagnosis and compared their absences with those of women who had never had cancer.
Methods
Our 2 target study groups were women in Quebec 18–59 years of age who were working when they first received therapy for breast cancer between November 1996 and August 1997 and similarly aged women randomly selected from provincial health care files who had never had cancer and were working at the time of diagnosis in women who had cancer. We interviewed 646 women who had had breast cancer (73% of those eligible) and 890 women in the comparison group (51% of those eligible) by telephone 3 years after first diagnosis.
Results
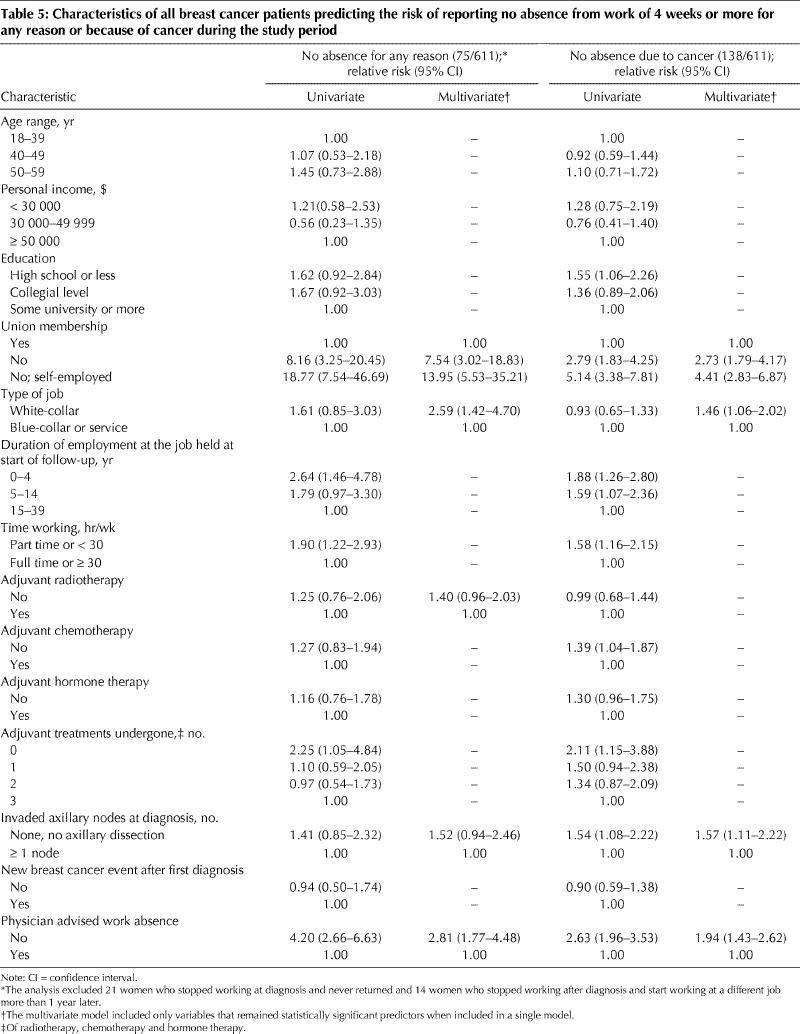
One year after diagnosis, 85% (459/541) of breast cancer survivors who remained free of disease during the 3-year study period were absent from work for 4 weeks or more compared with 18% (156/881) of healthy women (geometric mean total duration 5.6 v. 1.7 months, p < 0.001). By the third year, disease-free women were not absent more than women in the comparison group; however, more women who had experienced any new cancer event continued to be absent from work and to be absent from work for longer periods of time. Receiving adjuvant chemotherapy prolonged absence duration (9.5 v. 5.4 months among women not receiving chemotherapy). Compared with survivors belonging to a union, those who did not belong to a union (multivariate relative risk [RR] 7.54, 95% confidence interval [CI] 3.02–18.83) and those who were self-employed (RR 13.95, 95% CI 5.53–35.21) were more likely to report no work absence.
Interpretation
Most of the women with breast cancer took time off work (almost 6 months on average) after receiving the diagnosis. Three years after diagnosis, breast cancer survivors who remained disease-free — a large proportion of women with nonmetastatic breast cancer — were not absent from work more often or for longer periods of time than other working women.
Work experience after breast cancer is still a new aspect of cancer survivorship research. The results of recent studies have shown that most women who have had breast cancer return to work.1,2,3,4 However, apart from information about the percentage of breast cancer survivors who have returned to work by a specified time,5,6,7 little is known about the natural history of absence from work after breast cancer. Only 1 study has examined duration of absence from work, with a mixed group of cancer patients in the Netherlands as the study population.8
Absence rather than the disease itself may be the source of problems reported by some former patients when they return to work. Although legislation protects workers in Canada from unjustified job termination after sick leave,9 a prolonged absence can result in a reorganization of tasks or coincide with the end of a contract that is not renewed, particularly among women without job security. For self-employed workers, taking time off can mean the loss of contracts or of a professional network, and it often means no income during the absence.10 Also, the aggressive management of breast cancer in recent years, which involves multiple modalities, may increase the time away from work for initial treatment or because of side effects.8
We compared absence from work during the 3 years after first diagnosis among breast cancer survivors and women who had never had cancer. The comparison group, which was composed of women subject to similar labour market forces, made it possible to determine the amount of absence from work that could be directly attributed to breast cancer and how long absence due to breast cancer continued after the initial treatment phase. We also investigated the characteristics of breast cancer survivors that were associated with duration of absence and with not being absent from work during the 3-year period after diagnosis.
Methods
The study participants and procedures have been described fully elsewhere.1 In brief, we used the Quebec Tumour Registry to identify consecutive women 18–59 years of age in whom breast cancer was newly diagnosed between November 1996 and August 1997. To assemble a population-based comparison group, we selected from the files of the Régie de l'assurance maladie du Québec (RAMQ) a random sample of women in the same age range who were living in the province of Quebec at the same time that breast cancer was diagnosed in the patients but who had never had cancer. All breast cancer survivors had to be employed in the month of diagnosis, and women in the comparison group had to be employed during the same month (± 1) that breast cancer was diagnosed among survivors.
Because neither the RAMQ nor the Tumour Registry holds information on individual employment status, this could be assessed only when each woman was contacted directly. Potentially eligible subjects were contacted by letter. The letter requested the woman's signed permission to be contacted by a study team member, who would verify employment status at diagnosis (or similar period for women in the comparison group).
The follow-up period began for both breast cancer survivors and women in the comparison group in the month and year that breast cancer was first diagnosed in the survivor group. The follow-up period ended at the time of the interview 3 years after diagnosis. The mean duration of follow-up was comparable in both groups (41 ± 2 months).
Participants were interviewed by telephone. Women's work history during the 3-year period was assessed using a method adapted from one previously validated among Quebec women.11 Information on working conditions (number of hours worked per week, type of job, whether the woman was self-employed or a union member years employed in the job, income) was obtained for the job held at the start of follow-up and the one held at the end. We then asked whether the woman had been absent from work for 4 consecutive weeks or more since the start of follow-up. Women answering “yes” were asked about the number of such absences, their start date and duration, and the main reason for each absence.12 Sociodemographic and personal characteristics and health problems were ascertained. Because diagnosis and treatment could have occurred in any of more than 80 hospitals across Quebec, access to medical records was not feasible. Thus, at the end of the interview, we asked breast cancer survivors about initial disease management, nodal status, and recurrence during the study period. We have previously shown that survivors' recall of key features of their therapy and prognosis is almost perfect.13,14 Survivors were also asked whether their treating physician had advised them to take time off from work for treatment.
Because employment status was unknown when we first contacted potential participants, we used information from the 1996 Canada census on the proportions of women employed in Quebec between 18 and 59 years of age in 5-year strata to determine how many letters would have been sent had we been able to send letters to employed women only. The adjusted numbers of letters were used as the denominators for calculating study participation in the 2 study groups.
When possible, outcomes were assessed separately for survivors who remained disease-free during follow-up and for women who experienced any new breast cancer event (local, regional or distant recurrence, or a new primary breast cancer in the other breast) in the same period. Generalized linear models were used for analysis of continuous variables. Generalized linear models with a log link and binomial distribution for errors were used for the analysis of categorical data. This analysis is similar to logistic regression but provides a true relative risk instead of an odds ratio.15
Total duration of absence was calculated by summing the duration of all absences from work of 4 weeks or more, including those taken for vacation. Periods without work because of unemployment were not considered as absence from work. Because the number and duration of absences were not normally distributed, analyses were performed on log-transformed data, and least-square means were transformed back to the original scale. Thus, geometric means are presented. The confounding effects of age, belonging to a union, being self-employed, living with a partner, years of employment at the job held at the start of follow-up, personal income, number of hours worked per week, type of job, comorbid conditions, and total duration of employment during follow-up were evaluated. If the crude and adjusted estimates differed by more than 10%, the factor was considered a confounder and included in the model.
Because some absence from work is expected after a cancer diagnosis, we identified survivor characteristics that increased the likelihood of having no absence from work of 4 weeks or more. To ensure that women classified as having no absence had not been absent for fewer than 4 weeks on 1 or more occasions, we verified our classification by asking breast cancer survivors whether they had continued working during the treatment period. Sociodemographic, work and treatment characteristics were chosen a priori as potential predictors of not having been absent. All characteristics were entered simultaneously into a single multivariate model and removed 1 by 1 according to highest p value, until those with a p value of 0.10 or less remained. A similar strategy using the same potential predictors was used to identify characteristics of survivors with longer absences. To ensure that all absences possibly related to cancer were captured, these models were performed on both absences because of cancer and absences for any reason. This approach allowed us to capture such absences as those of women whose cancer was diagnosed while on vacation, and who reported vacation as the main reason for absence but also mentioned cancer.
This study was approved by the Commission d'accès à l'information du Québec and the Ethics Committee of the Hôpital du Saint-Sacrement.
Results
We sent letters about the study to 1504 breast cancer survivors and 2921 women in the comparison group who were eligible on the basis of age. We calculated that 885 of these survivors and 1745 of the women in the comparison group would have been working at the time of the survivors' diagnoses. Thus, overall participation among eligible women was estimated as 73% (646/885) among survivors and 51% (890/1745) among women in the comparison group.
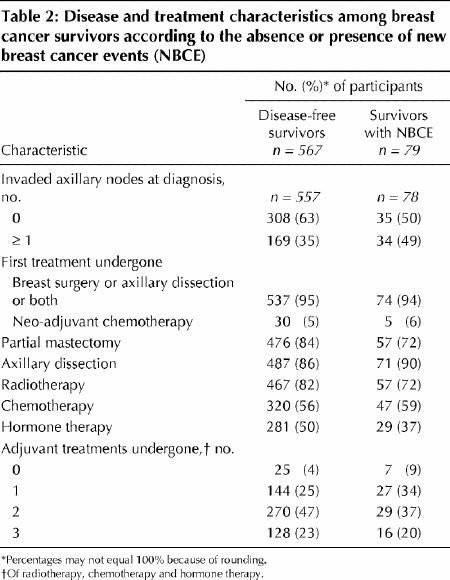
Characteristics at the start of follow-up were similar for the 2 study groups (Table 1). Table 2 shows the disease and treatment characteristics of survivors who remained disease-free and those who experienced new breast cancer events after first diagnosis in the follow-up period.
Table 1
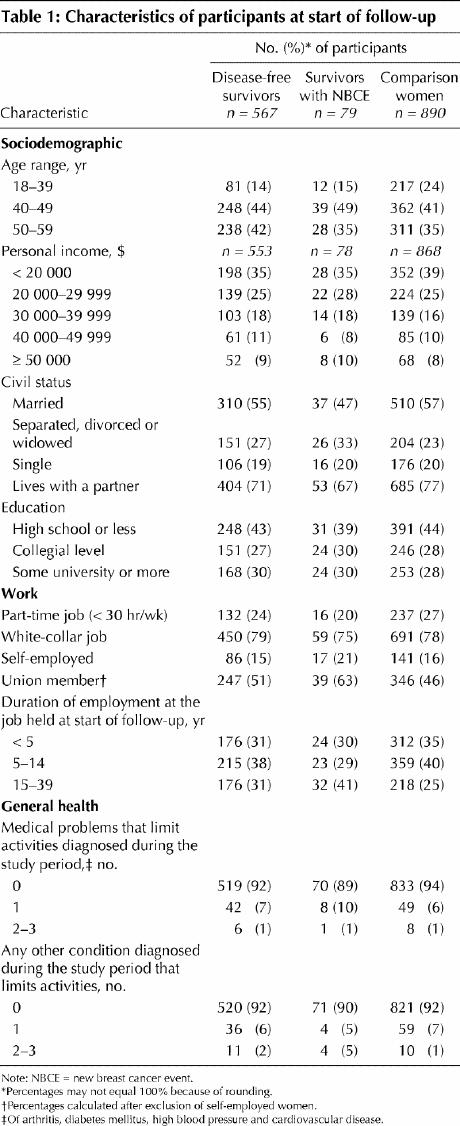
Table 2
Survivors worked a mean of 35 (standard deviation [SD] 13) hours per week, whereas women in the comparison group worked a mean of 34 (SD 11) hours per week. More than 90% of survivors and women in the comparison group reported having no activity-limiting medical problems during the study period. The mean delay between surgery and the start of adjuvant radiotherapy or chemotherapy was 5.5 (SD 3.8) weeks for women who had chemotherapy only or chemotherapy and radiotherapy and 12.3 (SD 7.5) weeks for women who received radiotherapy only (data not shown).
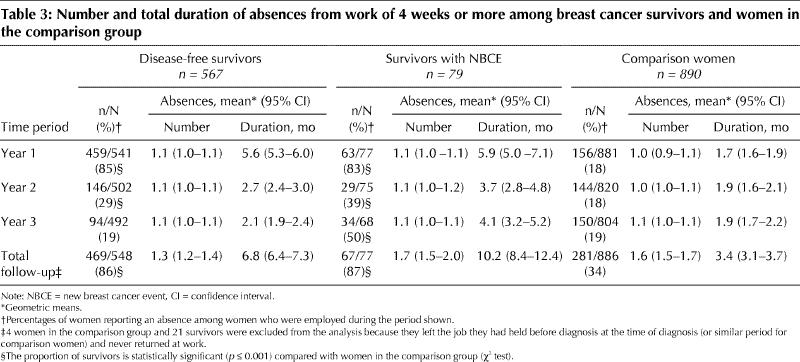
Of disease-free survivors, 85% reported at least 1 absence from work of 4 weeks or more for any reason during the first year after diagnosis, with a geometric mean total duration of 5.6 months (Table 3). In contrast, 18% (p < 0.001) of women in the comparison group reported at least 1 absence during the same period, with a mean total duration of 1.7 months (p < 0.001). In the third year after diagnosis, disease-free survivors were no more likely to have been off work than women in the comparison group. Among survivors with new cancer events, absences during the first year were comparable with those of disease-free survivors, but the duration of their absences remained longer than those of women who had never had cancer through to the end of follow-up. Absence specifically because of breast cancer during the 3-year follow-up was, on average, longer among survivors with new breast cancer events than among disease-free survivors (9.8 v. 5.9 months) (data not shown). These crude results were not substantially changed by adjustment for potential confounders.
Table 3
Among survivors, 81% began their first absence after diagnosis — the one most likely to be related to breast cancer — within 1 month. This first absence lasted less than 4 months for 26% of the women, 4–6 months for 24%, 7–12 months for 37% and 13 months or longer for 12%.
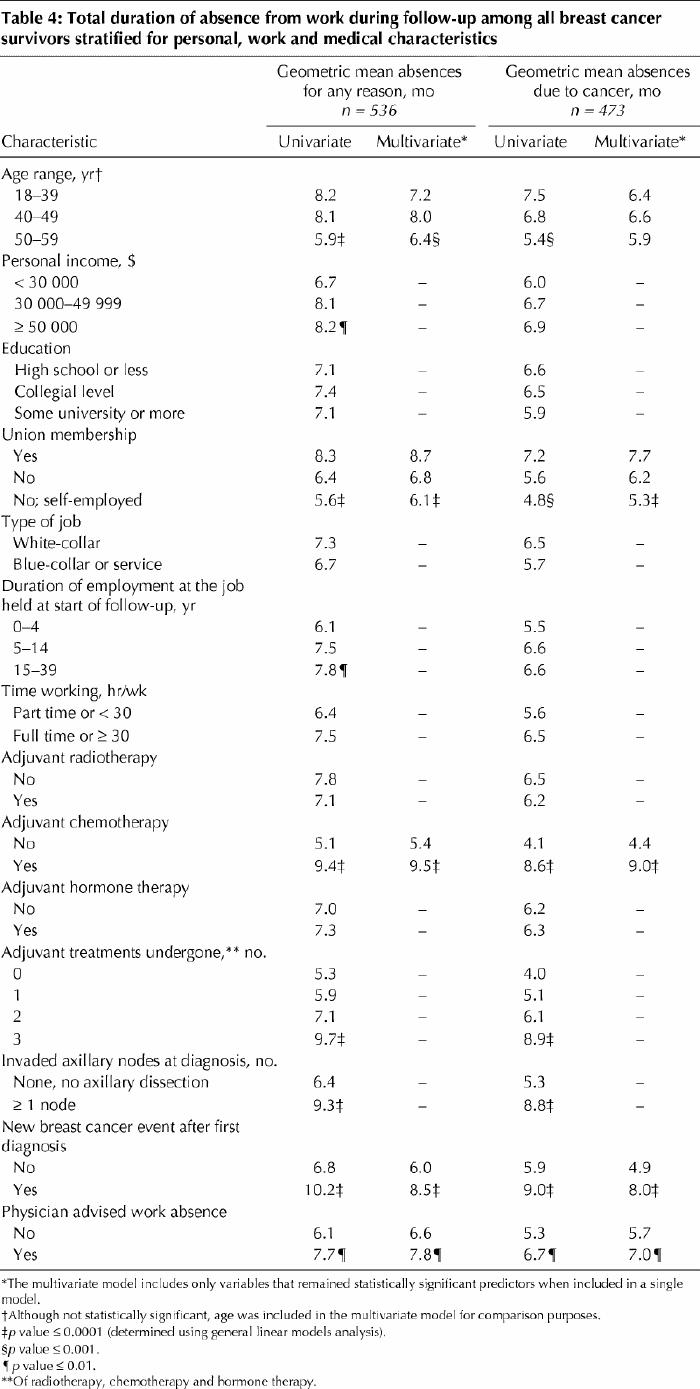
In the multivariate analysis, age less than 50 years, belonging to a union, chemotherapy, new cancer events during follow-up and physician advising absence from work all significantly increased absence duration for any reason (Table 4). Receiving chemotherapy and the number of adjuvant treatments received had the greatest influence on duration. Characteristics predicting absence duration for cancer only were similar.
Table 4
Two percent of women belonging to a union, 15% of those who did not belong to a union and 34% of self-employed workers reported no absence from work during follow-up. Compared with women belonging to a union, those who did not belong to a union (multivariate relative risk [RR] 7.54, 95% confidence interval [CI] 3.02–18.83) and those who were self-employed (RR 13.95, 95% CI 5.53– 35.21) were more likely to report no absence from work (Table 5). Having a white-collar job and not receiving a recommendation to take time from work from the physician also increased the likelihood of reporting no absence from work. Not having radiotherapy and no invaded axillary nodes were borderline predictors of reporting no absence from work (p = 0.08). Characteristics predicting no absence because of cancer were similar.
Table 5
Interpretation
Most breast cancer patients took time off work in the first year after diagnosis, and the time taken was, on average, almost 6 months. This represents a considerable excess attributable to disease when compared with similarly aged women who had never had cancer. In contrast to previous studies that reported only percentages of breast cancer patients at work or that had a shorter follow-up,5,6,8 we were able to show that, among survivors who remained free of disease, the excess of absence had considerably declined by year 2, and, by year 3, these women were not absent from work more often or for longer periods than other working women in Quebec. However, for patients who experienced new cancer events, overall absences remained in excess compared with healthy women throughout the 3-year follow-up. Women who belonged to a union or who had a blue-collar or service industry jobs were those most likely to be absent for some period. For those taking time off, chemotherapy in particular, multimodal adjuvant treatment and belonging to a union generally increased absence duration.
Because this study is population-based, we collected information about women from all socioeconomic strata and from urban, suburban and rural areas. As well, we have previously shown that study participants were very similar to Quebec women generally in terms of geographic distribution and key work charcteristics.1 The course of treatment for cancer patients in this study closely resembled that of other complete series of Quebec women we have identified at diagnosis.16,17 Thus, our results likely represent work absence among all working women with breast cancer who undergo its multimodal treatment.
Because absences were assessed retrospectively, we took several steps to minimize possible recall bias. We used evidence-based interview techniques to help participants recall events chronologically.18,19 Since information bias due to memory problems is more of a problem for reporting frequent events,18,19 we asked about absences of 4 consecutive weeks or more, which are not frequent and thus easier to remember. Although women in the comparison group did not have a breast cancer diagnosis to index their recall of absences, the events that caused absences of 4 weeks or more (vacation, illness, work conflicts, lockouts and deferred salary leave) were all memorable and thus probably as easy to remember for them as for breast cancer survivors. Apart from the final questions for patients only, interviews were worded identically for both groups in the study. Finally, evidence that we were successful in measuring absences comes from the stability of both the percentages of women in the comparison group reporting absences of 4 weeks or more and the duration of those absences for each year of follow-up. On a population level, it is reasonable to assume that events resulting in such absences are probably evenly distributed from 1 year to the next.
Although the positive and negative consequences of being absent from work on health, quality of life and work situation remain to be assessed, our results suggest some hardship in relation to job absence for certain breast cancer survivors. Being able to take time off work for breast cancer treatment does not appear to be an option equally available to all working women with this disease. Self-employed women or those not belonging to a union were much less likely to take time off work for initial treatments, even though their treatments resembled those of women who did take time off. These women may not feel able to take time off because their income decreases or stops when they are absent. Even some who do take time off work may experience financial burden because of the length of absence from work. For 74% of survivors, absence durations exceeded the 15-week federal employment insurance available during periods of illness, although an unknown proportion of women may have had access to additional disability insurance. Nonetheless, given that salary loss represents the greatest and most worrisome financial cost of breast cancer for some women,10 work absence likely represents a negative aspect of the cancer experience.
Supplementary Material
Acknowledgments
Financial support for this study was provided by research grants from the Canadian Breast Cancer Research Alliance and the Fondation Québécoise du Cancer. Elizabeth Maunsell and Chantal Brisson were National Health Research and Development Program National Health Research Scholars at the time this work was originally planned and funded, and are (E. Maunsell) or were (C. Brisson) Investigators of the Canadian Institutes of Health Research. Mélanie Drolet holds a PhD Fellowship Award from the Fonds de recherche en santé du Québec.
Footnotes
An abridged version of this article appeared in the Sept. 27, 2005, issue of CMAJ.
This article has been peer reviewed.
Contributors: Elizabeth Maunsell, as the principal investigator, had overall responsibility for all aspects of the study, including its conception and design, the acquisition, analysis and interpretation of data and drafting the manuscript. Mélanie Drolet contributed to the acquisition, analysis and interpretation of data and drafted the manuscript. Myrto Mondor conducted the analysis. Jacques Brisson, Chantal Brisson, BenoÎt Mâsse and Luc Deschênes contributed to the conception and design of the study and to the interpretation of data. All of the authors revised the manuscript critically for important intellectual content and approved the final version.
We thank Ninon Bourque (deceased), Director General of Communications, Department of Fisheries and Oceans, Ottawa and founding member of the Canadian Breast Cancer Network, for her invaluable contribution as part of the investigator group that planned and obtained funding for this study. We also thank the women who so generously gave their time to participate in this research.
Competing interests: None declared.
Correspondence to: Dr. Elizabeth Maunsell, Unité de recherche en santé des populations, Hôpital du Saint-Sacrement, 1050, chemin Sainte-Foy, Québec QC G1S 4L8; fax 418 682-7949; elizabeth.maunsell@uresp.ulaval.ca
References
- 1.Maunsell E, Drolet M, Brisson J, Brisson C, Masse B, Deschenes L. Work situation after breast cancer: results from a population-based study. J Natl Cancer Inst 2004;96:1813-22. [DOI] [PubMed]
- 2.Bradley CJ, Bednarek HL, Neumark D. Breast cancer and women's labor supply. Health Serv Res 2002;37:1309-28. [DOI] [PMC free article] [PubMed]
- 3.Bloom JR, Stewart SL, Chang S, Banks PJ. Then and now: quality of life of young breast cancer survivors. Psychooncology 2004;13:147-60. [DOI] [PubMed]
- 4.Ganz PA, Coscarelli A, Fred C, Kahn B, Polinsky ML, Petersen L. Breast cancer survivors: psychosocial concerns and quality of life. Breast Cancer Res Treat 1996;38:183-99. [DOI] [PubMed]
- 5.Bushunow PW, Sun Y, Raubertas RF, Rosenthal S. Adjuvant chemotherapy does not affect employment in patients with early-stage breast cancer. J Gen Intern Med 1995;10:73-6. [DOI] [PubMed]
- 6.Satariano WA, DeLorenze GN. The likelihood of returning to work after breast cancer. Public Health Rep 1996;111:236-41. [PMC free article] [PubMed]
- 7.Spelten ER, Sprangers MA, Verbeek JH. Factors reported to influence the return to work of cancer survivors: a literature review. Psychooncology 2002;11:124-31. [DOI] [PubMed]
- 8.Spelten ER, Verbeek JH, Uitterhoeve AL, Ansink AC, van der Lelie J, de Reijke TM, et al. Cancer, fatigue and the return of patients to work: a prospective cohort study. Eur J Cancer 2003;39:1562-7. [DOI] [PubMed]
- 9.Commission des normes du travail du Québec. Absence pour cause de maladie ou d'accident. Available: www.cnt.gouv.qc.ca/fr/normes/maladie.asp (accessed 1 Sept 2005).
- 10.Lauzier S, Maunsell E, De Koninck M, Drolet M, Hebert-Croteau N, Robert J. Conceptualization and sources of costs from breast cancer: findings from patients and caregivers focus group. Psychooncology 2005;14:351-60. [DOI] [PubMed]
- 11.Brisson C, Vezina M, Bernard PM, Gingras S. Validity of occupational histories obtained by interview with female workers. Am J Ind Med 1991;19:523-30. [DOI] [PubMed]
- 12.Dibbs R, Lutz D, Kaminsky B. “Questionnaire” de l'interview sur le travail. Ottawa: Statistics Canada; 1997. Available: www.statcan.ca/francais/research/75F0002MIF/75F0002MIF1997008.pdf (accessed 2 Sept 2005).
- 13.Maunsell E, Drolet M, Ouhoummane N, Robert J. Breast cancer survivors accurately reported key treatment and prognostic characteristics. J Clin Epidemiol 2005;58:364-9. [DOI] [PubMed]
- 14.McGinn T, Wyer PC, Newman TB, Keitz S, Leipzig R, Guyatt G, et al. Tips for learners of evidence-based medicine: 3. Measures of observer variability (kappa statistic). CMAJ 2004;171:1369-73. [DOI] [PMC free article] [PubMed]
- 15.Skov T, Deddens J, Petersen MR, Endahl L. Prevalence proportion ratios: estimation and hypothesis testing. Int J Epidemiol 1998;27:91-5. [DOI] [PubMed]
- 16.Maunsell E, Brisson J, Deschênes L, Frasure-Smith N. Randomized trial of a psychologic distress screening program after breast cancer: effects on quality of life. J Clin Oncol 1996;14:2747-55. [DOI] [PubMed]
- 17.Dorval M, Guay S, Mondor M, Mâsse B, Falardeau M, Robidoux A, et al. Couples who get closer after breast cancer: frequency and predictors in a prospective investigation. J Clin Oncol 2005;23:3588-96. [DOI] [PubMed]
- 18.Foddy W. Constructing questions for interviews and questionnaires. Cambridge (UK): Cambridge University Press; 1993.
- 19.Sudman S, Bradburn N, Schwarz N. Thinking about answers: the application of cognitive processes to survey methodology. San Francisco: Jossey-Bass Publishers; 1996.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


