Abstract
Background: Pilonidal sinus is a chronic inflammatory condition that typically occurs in the sacrococcygeal region and rarely in other locations. Scalp pilonidal sinus is extremely uncommon, making this case noteworthy as it expands the differential diagnosis for scalp nodular lesions. Case presentation: A 16-year-old girl presented with a persistent fluid-draining nodule on the top of her head, present for over a decade. She had a history of scalp injury at birth. Examination revealed a 1×2 cm mobile, tough nodule with a central opening and sparse surrounding hair. Imaging showed a gas density under the scalp but no bone involvement. The nodule was surgically excised. Histopathology confirmed pilonidal sinus, showing embedded hair, sebaceous gland involvement, and inflammatory cell infiltration. The patient recovered fully, with no recurrence or complications during three years of follow-up. Conclusions: This rare case of pilonidal sinus on the scalp highlights the importance of considering it in the differential diagnosis of scalp nodular lesions, particularly in patients with a history of trauma. It emphasizes the need for surgical treatment and careful follow-up to prevent recurrence.
Keywords: Pilonidal sinus, scalp nodules, sacrococcygeal region
Introduction
Pilonidal sinus disease is a chronic inflammatory condition characterized by the presence of a sinus or cyst containing hair [1]. While it is commonly found in the sacrococcygeal region, pilonidal sinus has also been reported in other ectopic locations such as the chin, neck, face, umbilicus, and scalp. Scalp pilonidal sinus is particularly rare due to the scalp’s dry and tough tissue, which typically resists hair entrapment [2]. However, trauma can serve as a predisposing factor for hair engulfment and subsequent sinus formation.
The rarity of scalp pilonidal sinus often leads to misdiagnosis. Common differential diagnoses include sebaceous cysts, lipomas, abscesses, and benign or malignant scalp tumors. This diagnostic ambiguity can result in delayed treatment or inappropriate management, complicating the patient’s condition. Recognizing the unique clinical and histopathologic features of pilonidal sinus is essential for accurate diagnosis and effective treatment.
This report presents a unique case of pilonidal sinus located on the top of the scalp, adding to the limited literature on this rare condition. By describing the clinical presentation, diagnostic challenges, and surgical management of this case, we aim to enhance awareness of scalp pilonidal sinus and emphasize its inclusion in the differential diagnosis of scalp nodules. The findings underscore the importance of a thorough clinical and histologic examination, enabling timely and accurate diagnosis of similar cases in clinical practice.
Case presentation
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of People’s Hospital of Kaihua. Written informed consent was obtained from the patient’s legal guardian for participation in this study. Written informed consent for publication of the case details and related images was obtained from the patient’s legal guardian.
A 16-year-old female student presented with a 10-year history of a recurrent fluid-draining nodule on the top of her head. She reported a history of scalp trauma at birth caused by a sharp instrument. On physical examination, a white, mobile, firm nodule measuring approximately 1×2 cm was observed on the scalp. The nodule had a central opening (0.2 cm in diameter) with sparse hair around it, and a foul-smelling fluid could be expressed upon pressure (Figure 1).
Figure 1.

Gross appearance of lesion.
Cranial computed tomography (CT) revealed a gas density shadow under the scalp at the site of the nodule, without any underlying bone abnormalities (Figure 2). The initial clinical diagnosis was a scalp tumor. Under local anesthesia, the nodule was excised using a fusiform incision extending to the periosteum. Histopathologic analysis revealed characteristic features of a pilonidal sinus. Under low magnification (Figure 3A), an expanded cystic cavity was observed within the dermis, displaying sinus tract-like morphology. Higher magnification highlighted specific structural details: the cyst wall exhibited epidermoid-like structures, with keratinous material occupying the cavity and focally connected sebaceous glands identified along the wall (Figure 3B). Additionally, hair shafts were present within the cystic cavity, accompanied by a mild infiltration of lymphocytes around the cyst wall (Figure 3C). These findings were consistent with the diagnosis of a pilonidal sinus, confirming this rare presentation on the scalp.
Figure 2.
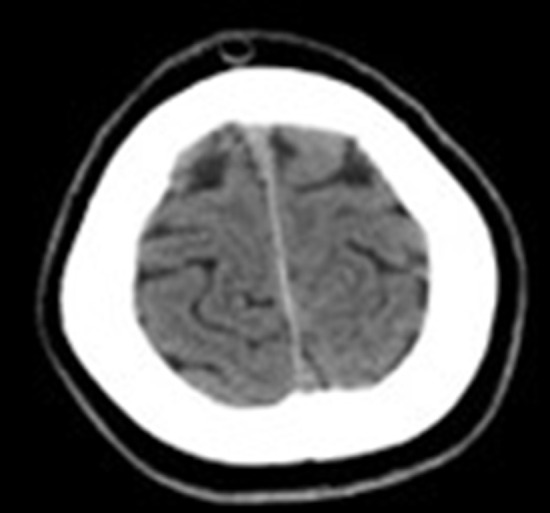
Computed tomography (CT) findings of lesion before surgery.
Figure 3.
Pathologic features of pilonidal sinus. A. Under low-power magnification, an expanded cystic cavity is observed within the dermis, exhibiting sinus tract-like changes. B. The cyst wall exhibits epidermoid-like structures, with keratinous material visible within the cavity and focally connected sebaceous glands identified along the wall (H&E stain, ×100). C. Hair structures are identified within the cystic cavity, with a mild infiltrate of lymphocytes surrounding the cyst wall (H&E stain, ×200).
Postoperative recovery was uneventful, with complete wound healing within a week. The patient remained symptom-free with no recurrence during a three-year follow-up period.
Discussion
Pilonidal disease was first described in 1833 by Mayo, who identified a hair-containing cyst located just below the coccyx. In 1880, Hodge coined the term “pilonidal” derived from the Latin words pilus (hair) and nidus (nest). The term now encompasses a spectrum of clinical presentations, ranging from asymptomatic hair-containing cysts and sinuses to symptomatic, recurrent abscesses, most commonly affecting the sacrococcygeal region [2].
The etiology of pilonidal sinus disease remains controversial, with both congenital and acquired theories proposed [3-5]. The congenital theory suggests that pilonidal sinus arises from residual epithelial tissues or skin depressions present at birth. In contrast, another theory posits that pilonidal sinuses are acquired from granulomatous reactions triggered by trauma, iatrogenic injury, chronic irritation by foreign bodies, or persistent infection [6,7].
While the scalp is a densely hairy region, its tough and dry tissue typically prevents hair penetration, making pilonidal sinus in this area exceedingly rare. However, mechanical or surgical trauma may create an entry point for hairs to become embedded within scalp tissue [2]. In our case, the patient’s history of scalp trauma from a sharp instrument injury at birth likely facilitated hair penetration, serving as the primary factor in pilonidal sinus development.
Although pilonidal sinus commonly occurs in the sacrococcygeal region, reports of extra-sacrococcygeal locations, including the scalp, are scarce [3,7-10]. After reviewing the literature, only eight documented cases of scalp pilonidal sinus were identified, five in the occipital region [1,11-14] and two in the posterior auricular area [2,15,16] (see Table 1). To our knowledge, a pilonidal sinus located at the vertex of the scalp has not been previously reported, making this case unique.
Table 1.
Cases of scalp pilonidal sinus
| Author | Year | Age (Years) | Gender | Location | History of Trauma | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| Moyer DG [12] | 1972 | 13 | M | Occipital area | Yes | Surgical excision | No recurrence |
| Kosaka M et al. [13] | 2007 | 4 | M | Occipital area | Yes | Surgical excision | No recurrence |
| Chiu MW et al. [11] | 2008 | 70 | F | Occipital area | Yes | Surgical excision | Unclear |
| Ak Nalbant O et al. [2] | 2011 | 31 | M | Post-auricle area | Unclear | Surgical excision | No recurrence |
| Kansal A et al. [15] | 2016 | 42 | F | Post-auricle area | Yes | Surgical excision | No recurrence |
| Destek S et al. [16] | 2016 | 46 | M | Post-auricle area | Yes | Surgical excision | No recurrence |
| El Mehdi M et al. [14] | 2022 | 4 | F | Occipital area | Yes | Surgical excision | Unclear |
| Gao Y et al. [1] | 2022 | 19 | M | Occipital area | NO | Surgical excision | No recurrence |
In conclusion, our report highlights a rare presentation of pilonidal sinus disease involving the vertex of the scalp. Although uncommon, pilonidal sinus should be considered in the differential diagnosis of persistent nodular masses or chronic sinus lesions of the scalp, especially in patients with a history of scalp trauma or surgical procedures. Further studies are warranted to enhance diagnostic accuracy and explore strategies to reduce postoperative recurrence in pilonidal sinus disease.
Acknowledgements
The authors would like to thank Dr. Wengen He for providing clinical support during the preparation of this report.
Disclosure of conflict of interest
None.
References
- 1.Gao Y, Hui Y, Liu H, An B, Liu F. Pilonidal cyst of the scalp. J Surg Case Rep. 2023;2023:rjad493. doi: 10.1093/jscr/rjad493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ak Nalbant O, Nalbant E. Pilonidal sinus of the scalp: a case report and review of the literature of head and neck localization. Med J Trak Univ. 2010 [Google Scholar]
- 3.Yokoyama T, Nishimura K, Hakamada A, Isoda KI, Yamanaka KI, Kurokawa I, Mizutani H. Pilonidal sinus of the supra-auricle area. J Eur Acad Dermatol Venereol. 2007;21:257–258. doi: 10.1111/j.1468-3083.2006.01831.x. [DOI] [PubMed] [Google Scholar]
- 4.Adhikari BN, Khatiwada S, Bhattarai A. Pilonidal sinus of the cheek: an extremely rare clinical entity-case report and brief review of the literature. J Med Case Rep. 2021;15:64. doi: 10.1186/s13256-020-02561-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dettmer M, Degiannis K, Braun-Münker M, Doll D, Maak M. The origin of pilonidal sinus disease - 10 wrong theories and one recent discovery. Albanian J Trauma Emerg Surg. 2023;7:1296–1299. [Google Scholar]
- 6.Nepomuceno H, Abrajano C, Chiu B. Pilonidal granuloma formation after an incision and drainage procedure is associated with retained hair within the sinus - a case series. Int J Surg Case Rep. 2024;125:110500. doi: 10.1016/j.ijscr.2024.110500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Sullivan MJ, Kirwan WO. Post-traumatic pilonidal sinus of the face. Br J Dermatol. 2000;143:1353. doi: 10.1046/j.1365-2133.2000.03937.x. [DOI] [PubMed] [Google Scholar]
- 8.Oudit D, Ellabban M, Eldafl D, Crawford L, Juma A. Pilonidal sinus of the chin. Plast Reconstr Surg. 2005;115:2153–4. doi: 10.1097/01.prs.0000165474.33353.8a. [DOI] [PubMed] [Google Scholar]
- 9.Meher R, Sethi A, Sareen D, Bansal R. Pilonidal sinus of the neck. J Laryngol Otol. 2006;120:e5. doi: 10.1017/S0022215105001490. [DOI] [PubMed] [Google Scholar]
- 10.Doll D, Petersen S. Trauma is not a common origin of pilonidal sinus. Dermatol Surg. 2008;34:283–4. doi: 10.1111/j.1524-4725.2007.34057.x. [DOI] [PubMed] [Google Scholar]
- 11.Chiu MW, Abrishami P, Sadeghi P. Letter: pilonidal cyst of the scalp. Dermatol Surg. 2008;34:1294–5. doi: 10.1111/j.1524-4725.2008.34279.x. [DOI] [PubMed] [Google Scholar]
- 12.Moyer DG. Pilonidal cyst of the scalp. Arch Dermatol. 1972;105:578–9. [PubMed] [Google Scholar]
- 13.Kosaka M, Kida M, Mori H, Kamiishi H. Pilonidal cyst of the scalp due to single minor trauma. Dermatol Surg. 2007;33:505–507. doi: 10.1111/j.1524-4725.2007.33102.x. [DOI] [PubMed] [Google Scholar]
- 14.El Mehdi M, El Gueouatri M, Yafi I, Zinedinne S, Benlaassel O, El Atiqi O, Amrani MD, Benchamkha Y. Pilonidal cyst of the scalp following a single minor trauma. Ann Chir Plast Esthet. 2022;67:261–263. doi: 10.1016/j.anplas.2022.06.009. [DOI] [PubMed] [Google Scholar]
- 15.Kansal A, Jain R, Jain S, Munjal K. A rare case of recurrent pilonidal sinus of scalp. Int Surg J. 2016:1669–1671. [Google Scholar]
- 16.Destek S, Gul VO, Ahioglu S. Rare type cranial postauricular pilonidal sinus: a case report and brief review of literature. Case Rep Surg. 2017;2017:5791972. doi: 10.1155/2017/5791972. [DOI] [PMC free article] [PubMed] [Google Scholar]



