Abstract
Background and Objectives:
Though research indicates that certain aspects of adverse neighborhood conditions may influence weight development in childhood and adolescence, it is unknown if the Child Opportunity Index (COI), a composite measure of 29 indicators of neighborhood conditions, is associated with weight outcomes in adolescence. We hypothesized that lower COI would be associated with higher overweight and obesity in cross-sectional and longitudinal modeling in a national sample of 9- and 10-year-olds and that this association would be different by sex.
Methods:
Using data from the Adolescent Brain Cognitive Development (ABCD) study (n=11,857), we examined the cross-sectional association between COI quintile and overweight and obesity in 9- and 10-year-olds. Additionally, we used hazard ratios to examine incident overweight and obesity across three waves of data collection.
Results:
Due to the interaction between sex and COI (p<0.05), we present sex-specific models. There was a stepwise bivariate association, in which higher COI was associated with lower obesity prevalence. This pattern held in multilevel models, with a stronger association in females. In models adjusted for individual and household characteristics, female adolescents in the lowest quintile COI neighborhoods had 1.81 (95% confidence interval [CI]: 1.32, 2.48) times the odds of obesity compared to those in the highest quintile. In longitudinal models, the COI was associated with incident obesity in females only: adjusted HR=4.27 (95% CI: 1.50, 12.13) for lowest compared to highest COI.
Conclusions:
Neighborhood opportunity is associated with risk of obesity in pre-adolescence into mid-adolescence. Females may be particularly influenced by neighborhood conditions.
Introduction
Pre-adolescent and adolescent obesity are associated with adverse emotional, social, and physical health outcomes in the short- and long-term.1,2 Pre-pandemic national data showed that 20.7% of 6 to 11-year-olds and 22.2% of 12 to 19-year-olds had obesity, and this contrasts with a prevalence of 12.7% among 2 to 5-year-olds.3 These numbers indicate the importance of understanding weight development and its modifiable causes during the transition to early adolescence and through the adolescent and young adult periods. Due to its multifactorial etiology, including obesogenic environment, genetic and epigenetic factors, hormonal and developmental changes, psychological, and behavioral factors4, reversal of obesity that is present in adolescence is uncommon5 and treatment is complex.1,4 Further, given that the current research literature shows inconsistent evidence for what factors may be associated with obesity during adolescence,6 there is an urgent need for additional research to identify potential causes and avenues for both prevention and interventions to prevent and reduce overweight among children and adolescents.
Research studies from a wide range of disciplines indicate the importance of place-based economic, physical, and social conditions for child development, including a focus on overweight and obesity in childhood and adolescence.7–9 The Child Opportunity Index (COI) is a 29-item indicator of “the context of neighborhood-based conditions and resources … that influence children’s healthy development and long-term outcomes”(p. 1693).10 The COI includes aspects of the built environment (access to healthy food, access to green space, and walkability) and the social environment (including both economic and educational aspects, such as employment rate, homeownership rate, and high school graduation rate). Previous work has shown associations between the COI and food insecurity11, asthma morbidity,12 mortality,13 and life expectancy at birth.14 In addition, there is growing evidence that the distinct developmental trajectories experienced by girls and boys during adolescence may be differentially influenced by place-based exposures such as those measured by the COI. Physiologically, adolescents of different sexes are exposed to different endocrine signals; while socially, adolescents are increasingly gendered in their communities. It is hypothesized that the combined effect of these internal and external experiences causes exposure to the same neighborhood environments to differentially affect adolescent girls versus boys.
To date, only a few studies have examined the COI in relation to metabolic outcomes among adolescents, and results are inconsistent. Additionally, extant literature shows conflicting evidence for sex differences in associations between COI and weight outcomes. In a cohort from Eastern Massachusetts (n=743), there was no association between the overall COI with measures of adiposity (percentage body fat, fat mass index, and trunk fat mass index) in early adolescence (mean age, 13.1 years).15 In a sample in New York state, among 9-year-olds (but not at ages 12 and 15), higher COI was associated with lower BMI for females, but not males.16 Males, instead, showed similar BMI at age 9 across levels of the COI, but slower increases in BMI through age 15 within higher COI neighborhoods. Finally, combining data from 54 cohorts in the Environmental Influences on Child Health Outcomes (ECHO) program (n=20,677), higher neighborhood opportunity, assessed during the prenatal period and throughout childhood, was associated with lower mean BMI trajectory and lower risk of obesity from childhood to adolescence, with larger associations at older ages of outcome assessment.17 Notably, the ECHO study17 did not find evidence for sex differences, which contrasts previous work that has shown that neighborhood factors, particularly economic factors, may be more strongly associated with obesity among girls compared to boys.18–20
To advance our understanding of how neighborhood conditions may influence weight and weight development in early adolescence, we examined these associations in a large cohort of 9–10-year-olds in the Adolescent Brain Cognitive Development (ABCD) Study. We hypothesized that lower COI would be associated with higher rates of obesity at ages 9–10 and over 2 years of follow-up. Based on prior literature and because girls and boys have different growth trajectories in this peripubertal period, we conducted analyses separated by sex.
Methods
Study Population
The Adolescent Brain Cognitive Development (ABCD) Study is an ongoing study that began with 11,878 nine and ten year old children, along with their parents/guardians, focusing on psychological and neurobiological development from pre-adolescence to young adulthood.21 Participants were recruited between September 2016 and October of 2018 through school-based sampling in 21 catchment areas, whose racial/ethnic composition reflect the racial/ethnic composition of the United States.21 To participate in the ABCD study, parent/guardians provided informed written consent and children provided written assent. We used data available in Version 4, and excluded subjects who did not have BMI data, resulting in 11,857 subjects for cross-sectional analysis. Subjects with follow-up information from year 1 and/or year 2 were included in our longitudinal analysis (n=6353). This analysis was considered non-human subjects research by our Institutional Review Board (IRB) since it relies on de-identified secondary data. The ABCD Study itself was approved by the University of California San Diego Institutional Review Board, and each data collection site also had approval from their local IRB.
Exposure: Child Opportunity Index
The Child Opportunity Index (COI) 2.0 is a composite index of 29 census-tract indicators that measure neighborhood conditions that are relevant to healthy child development and long-term outcomes.10 Data from many public sources, including the Census Bureau, the Department of Education, and the Environmental Protection Agency, are collated and scaled to create the COI score.22 Neighborhood data from 2015 were used to construct the COI variables used in this anaysis. COI percentile scores are created by ranking all census tracts in the US according to their COI z-score, with each group containing 1 percent of the US child population, and the resulting groups receiving a COI score from 1, lowest opportunity, to 100, highest opportunity.10 These scores are commonly used in quintiles based on national data10, and this is the approach we use in our analyses. In addition to an overall score, the COI components can be divided into three subgroups, focused on (1) education, (2) health and environment, and (3) social and economic conditions.
Outcomes
Measures of height and weight were collected using standardized measurements following CDC guidelines23 at each in-person, annual data collection.24,25 We calculated body mass index (BMI) (kg/m2) and converted this to age- and sex-specific percentiles based on the CDC 2000 Growth Chart SAS code.26 We excluded outliers with biologically implausible BMI z-scores of less than −4 or greater than 8. We categorized percentile scores into three categories: not overweight/obesity (less than or equal to 85), overweight (greater than 85 and less than or equal to 95) and obesity (greater than 95). For longitudinal analysis, our primary outcome was new onset obesity among those who did not have obesity in the prior wave. In sensitivity analyses, we examined new onset overweight or obesity among those categorized as not overweight/obesity in the prior wave.
Covariates
Consistent with prior literature on neighborhood characteristics and BMI, we include covariates that are associated with COI and may predict adolescent weight outcomes. All covariates were reported during the baseline, in-person study visit. We operationalized these variables in a manner consistent with prior studies reporting on ABCD data.24,25 The primary caregiver of the pre-adolescent reported on the child’s sex at birth (male, female), birthweight, race and ethnicity, pubertal status, and current use of stimulant medication. A single variable for race and ethnicity, conceptualized as social constructs, was included as a covariate to control for differences in lived experience that were not measured by other variables in our model. Pubertal status was assessed through caregiver report on the Pubertal Development Scale.27 Current use of stimulant medication was operationalized based on parent report of all prescription medication taken within the past 2 weeks28 (see Table 1 for details).
Table 1.
Child, family, and neighborhood characteristics for overall sample and stratified by sex.
| Full Sample | Females | Males | ||||
|---|---|---|---|---|---|---|
| n=11,857 | n=5,672 | n=6,185 | ||||
|
|
||||||
| n or mean | % or SD | n or mean | % or SD | n or mean | % or SD | |
| Child Opportunity Index 1 | ||||||
| 1st (lowest) | 1,943 | 16 | 940 | 17 | 1,003 | 16 |
| 2nd | 1,501 | 13 | 763 | 13 | 738 | 12 |
| 3rd | 1,754 | 15 | 867 | 15 | 887 | 14 |
| 4th | 2,830 | 24 | 1,355 | 24 | 1,475 | 24 |
| 5th (highest) | 3,829 | 32 | 1,747 | 31 | 2,082 | 34 |
| Child Characteristics | ||||||
| Weight category at baseline | ||||||
| Not overweight/obesity | 8,083 | 68 | 3,899 | 69 | 4,184 | 68 |
| Overweight | 1,801 | 15 | 861 | 15 | 940 | 15 |
| Obesity | 1,973 | 17 | 912 | 16 | 1,061 | 17 |
| Age (years) | 9.9 | 0.6 | 9.9 | 0.6 | 9.9 | 0.7 |
| Race/ethnicity | ||||||
| White | 6,180 | 52 | 2,895 | 51 | 3,285 | 53 |
| Black | 1,783 | 15 | 894 | 16 | 889 | 14 |
| Hispanic | 2,459 | 21 | 1,184 | 21 | 1,275 | 21 |
| Asian | 260 | 2.2 | 132 | 2.3 | 128 | 2.1 |
| Native American | 38 | 0.3 | 25 | 0.4 | 13 | 0.2 |
| Multiracial | 1,067 | 9 | 510 | 9 | 557 | 9 |
| Other | 70 | 0.6 | 32 | 0.6 | 38 | 0.6 |
| Birthweight (kg) | 3.18 | 0.67 | 3.11 | 0.66 | 3.25 | 0.68 |
| Puberty status at baseline | ||||||
| Prepuberty | 3,348 | 28 | 1,490 | 26 | 1,858 | 30 |
| Early puberty | 4,499 | 38 | 1,571 | 28 | 2,928 | 47 |
| Midpuberty | 3,693 | 31 | 2,413 | 43 | 1,280 | 21 |
| Late/post puberty | 317 | 2.7 | 198 | 3.5 | 119 | 1.9 |
| Current use of stimulant medication2 | ||||||
| No | 11,196 | 94 | 5,491 | 97 | 5,705 | 92 |
| Yes | 661 | 5.6 | 181 | 3.2 | 480 | 7.8 |
|
Parent and Family
Characteristics |
||||||
| Family structure | ||||||
| Partnered parent | 8,715 | 74 | 4,134 | 73 | 4,581 | 74 |
| Single parent | 3,142 | 26 | 1,538 | 27 | 1,604 | 26 |
| Parent nativity | ||||||
| US-born | 9,764 | 82 | 4,685 | 83 | 5,079 | 82 |
| Foreign-born | 2,093 | 18 | 987 | 17 | 1,106 | 18 |
| Parent education | ||||||
| Post-graduate degree | 4,054 | 34 | 1,947 | 34 | 2,107 | 34 |
| Bachelor degree | 3,027 | 26 | 1,427 | 25 | 1,600 | 26 |
| Some college | 3,080 | 26 | 1,451 | 26 | 1,629 | 26 |
| HS/GED or less | 1,696 | 14 | 847 | 15 | 849 | 14 |
| Household financial strain3 | ||||||
| 0 | 9,276 | 78 | 4,456 | 79 | 4,820 | 78 |
| 1 | 1,076 | 9.1 | 519 | 9.2 | 557 | 9 |
| 2 | 703 | 5.9 | 334 | 5.9 | 369 | 6 |
| 3 or more | 802 | 6.8 | 363 | 6.4 | 439 | 7.1 |
| Household income to needs ratio (INR)4 | ||||||
| less than 1 | 1,999 | 17 | 973 | 17 | 1,026 | 17 |
| 1 to less than 2 | 2,008 | 17 | 964 | 17 | 1,044 | 17 |
| 2 to less than 4 | 2,905 | 25 | 1,386 | 24 | 1,519 | 25 |
| 4 to less than 6 | 1,846 | 16 | 865 | 15 | 981 | 16 |
| 6 to 14 | 3,099 | 26 | 1,484 | 26 | 1,615 | 26 |
COI quintiles are based on the nationwide distribution.
The medications classified as stimulants in this study were methylphenidate, dextroamphetamine, dexmethylphenidate, amphetamine, Evekeo®, Adderall®, Vyvanse®, Concerta®, Focalin®, Quillivant®, Ritalin®, and Metadate®.
Financial strain was created as a sum score of seven items on the Parent-Reported Financial Adversity Questionnaire, and coded as a four category variable (no financial strain, one financial strain, two financial strains, three or more financial strains).
Household income to needs ratio was calculated by dividing gross income over federal poverty level. We categorized income-to-needs ratio into five categories.
Caregiver education was defined as the highest level of education attained by either the primary caregiver or their partner. Family structure was coded as a binary variable, differentiating between primary caregivers who were married or living with a partner versus those who were single. Parent nativity status was also coded as a binary variable: if either the primary or secondary caregiver was foreign-born, the participant was classified as having a foreign-born parent; otherwise, participants were categorized as having US-born parents. Income-to-needs ratio (INR) was calculated as household income divided by the federal poverty line for the household size. Thus, a INR value above 1 indicates being above the poverty threshold, while a INR value below 1 indicates being below the poverty threshold.29 We categorized INR into five categories. Last, financial strain was created as a sum score of seven items on the Parent-Reported Financial Adversity Questionnaire30, and coded as a four-category variable.
Statistical Analysis
We first examined the distribution of participants’ characteristics stratified by weight status and sex. Next, we conducted multi-level logistic regression to account for the clustering of individuals within study site. We examined whether the Child Opportunity Index was associated with a greater risk of obesity or overweight at baseline. We present sex-specific models, based both on prior literature and an observed statistically significant interaction (p<0.05) between sex and COI. In model 1, we adjusted for interview age. Next, we added covariates that are potentially important confounders of the association between COI and BMI: race/ethnicity, parent nativity, family structure, birth weight, parental education, income-to-needs ratio, and financial adversity (model 2). The last model added two covariates that may be confounders or mediators of the association between COI and BMI: parental reported puberty status and stimulant medication usage (model 3). We evaluated model fit by considering the Null Deviance and Residual Deviance results. Next, we examined whether the Child Opportunity Index at baseline was associated with a higher risk of incident obesity over the follow-up period using Cox proportional hazard models (‘survival’ package) with random effects to account for clustering by study site, including only children with BMIs classified as not overweight/obesity and overweight at baseline (n=6,353). We used the same model building approach and stratified all analyses by sex. We used the Global Schoenfeld test to confirm that models were not in violation of the proportional odds assumption. Analyses were conducted in R, using the lme4, mclogit, and survival packages.
To account for missing data, we used multiple imputations by chained equations using the MICE R package.31 We generated 10 imputed datasets, analyzed each imputed dataset, and combined the results across imputations using Rubin’s rules.
In sensitivity analyses, we examined the cross-sectional and longitudinal associations (same models as described above) between each of the three subscales of the COI (education, health, and social and economic domains) and overweight and obesity. Finally, for longitudinal modeling, we created an additional outcome of incident overweight or obesity (as a combined variable).
Results
As shown in Table 1, 15% of the sample had overweight and 17% had obesity at baseline, with similar levels among females and males. Approximately half of the sample was non-Hispanic white, nearly 20% was Hispanic, and 15% was non-Hispanic black. Approximately one third (32%) of the sample lived in neighborhoods classified into the highest quintile of the COI, while 16% resided in the lowest quintile of the COI. For both males and females, there was a stepwise cross-sectional association between COI and obesity in which higher COI was associated with lower obesity prevalence, ranging from a high of 31% of females with obesity in the 1st (lowest) COI to a low of 6.9% of females with obesity in the 5th (highest) COI (Table 2). Interactions between sex and COI quintiles were significant at p<.05 across models, thus we present sex-specific results.
Table 2.
Weight category at baseline by quintile of the Child Opportunity Index
| Child Opportunity Index Quintile1 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1st (very low) | 2nd (Low) | 3rd (Moderate) | 4th (High) | 5th (Very high) | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Females (n=5672) | ||||||||||
| Not overweight/obesity | 446 | 51 | 388 | 60 | 482 | 65 | 888 | 74 | 1,347 | 81 |
| Overweight | 150 | 17 | 117 | 18 | 124 | 17 | 167 | 14 | 200 | 12 |
| Obesity | 271 | 31 | 146 | 22 | 137 | 18 | 139 | 12 | 114 | 6.9 |
| Males (n=6185) | ||||||||||
| Not overweight/obesity | 506 | 53 | 375 | 59 | 498 | 64 | 936 | 70 | 1,515 | 78 |
| Overweight | 167 | 18 | 102 | 16 | 135 | 17 | 195 | 15 | 262 | 13 |
| Obesity | 274 | 29 | 161 | 25 | 145 | 19 | 206 | 15 | 174 | 8.9 |
COI quintiles are based on the nationwide distribution.
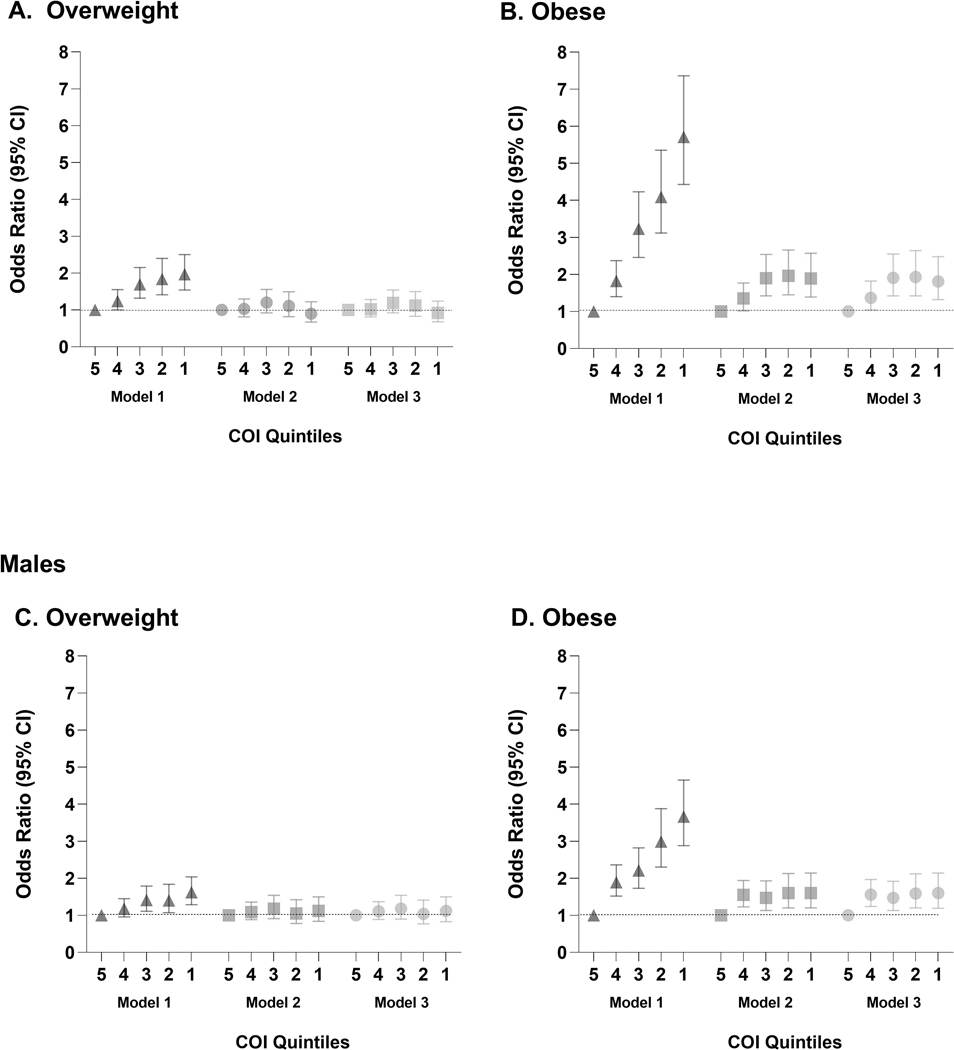
Figure 1 displays results of models examining the cross-sectional association between COI and overweight and obesity. For both males and females, there was an association between the overall COI and overweight in Model 1, which was reduced to insignificance with the addition of confounding factors in Models 2 and 3. However, for obesity, the association remained, even in fully adjusted models. Female adolescents in the lowest quintile COI neighborhoods had 1.81 (95% confidence intervals [CI]: 1.32, 2.48) times the odds of obesity compared to female adolescents in the highest quintile neighborhoods. Females in the 2nd and 3rd lowest quintiles faced similar odds of obesity, with a slightly lower odds for the 4th quintile (Odds Ratio (OR)=1.37, 95% CI: 1.04, 1.82) compared to the highest quintile. Males in the lowest COI quintile neighborhoods had 1.60 times the odds of obesity (95% CI: 1.19, 2.14) compared to males in the highest quintile neighborhoods; this association was largely the same for quintiles 2, 3, and 4.
Figure 1.
Odds ratios and 95% confidence intervals for overweight and obesity status at baseline by Child Opportunity Index quintile, stratified by sex. Model 1 is adjusted for age of subject at interview. Model 2 is adjusted for age, race/ethnicity, birth weight, parent nativity, family structure, parental education, financial strain, and household INR. Model 3 is adjusted for age, race/ethnicity, birth weight, parent nativity, family structure, parental education, financial strain, household INR, puberty, and stimulant medication.
In models to estimate incident obesity in adolescents between the ages of 10 and 13 (Table 3), females in the lowest COI quintile had HR=4.06 (95% CI: 1.74, 9.49) times the risk of incident obesity compared to females in the highest COI quintile when adjusting only for age (Model 1). Likewise, females in the 2nd lowest quintile had hazard ratio of incident obesity (HR)=3.07 (95% CI: 1.26, 7.51); quintiles 3 and 4 did not show an association. These associations held even after adjustment for additional child and family characteristics (see Models 2 and 3, Table 3). Among males, there was no association between COI and new-onset obesity in either simple or fully adjusted models (Table 3).
Table 3.
Hazard ratio (HR) and 95% confidence intervals (CI) for new onset obesity among participants who were not overweight/obesity at baseline, using the COI overall score (n=6353). Stratified by sex.
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | ||||
| Females (n=3036) | |||||||||
| Child Opportunity Index Quintile 1 | |||||||||
| 1st (lowest) | 4.06 | 1.74 | 9.49 | 4.18 | 1.50 | 11.70 | 4.27 | 1.50 | 12.13 |
| 2nd | 3.07 | 1.26 | 7.51 | 2.87 | 1.06 | 7.78 | 2.79 | 1.01 | 7.68 |
| 3rd | 1.52 | 0.56 | 4.14 | 1.42 | 0.50 | 4.04 | 1.36 | 0.47 | 3.92 |
| 4th | 1.09 | 0.43 | 2.74 | 1.10 | 0.42 | 2.86 | 1.09 | 0.42 | 2.84 |
| 5th (highest) | 1.00 | 1.00 | 1.00 | ||||||
| Males (n=3317) | |||||||||
| Child Opportunity Index Quintile 1 | |||||||||
| 1st (lowest) | 1.86 | 0.87 | 3.94 | 0.78 | 0.30 | 2.03 | 0.76 | 0.30 | 1.95 |
| 2nd | 1.66 | 0.71 | 3.88 | 0.96 | 0.38 | 2.45 | 0.94 | 0.37 | 2.38 |
| 3rd | 1.59 | 0.75 | 3.34 | 1.12 | 0.51 | 2.47 | 1.07 | 0.48 | 2.37 |
| 4th | 1.63 | 0.87 | 3.07 | 1.29 | 0.67 | 2.47 | 1.25 | 0.65 | 2.42 |
| 5th (highest) | 1.00 | 1.00 | 1.00 | ||||||
HR; Hazard Ratio, CI; Confidence Interval
COI quintiles are based on the nationwide distribution.
Model 1 is adjusted for age of subject at interview.
Model 2 adjusts for: age, race/ethnicity, birth weight, parent nativity, family structure, parental education, financial strain, household INR.
Model 3 adjusts for: age, race/ethnicity, birth weight, parent nativity, family structure, parental education, financial strain, household INR, puberty, stimulant medication.
Sensitivity Analyses
Results using scores for the COI sub-scales separately displayed similar patterns to those observed for the full COI score for baseline (Supplemental Table 1) and longitudinal analyses (Supplemental Table 2). There was no evidence for an association between neighborhood opportunity and incident overweight or obesity (as a combined variable) (Supplemental Table 3).
Discussion
At ages 9–10, low neighborhood opportunity, as measured by the COI, was associated with a higher prevalence of obesity, and this association was stronger among females. An elevated prevalence of obesity was observed for every quintile of COI compared to the highest quintile. Over the follow up period, girls in low COI neighborhoods continued to be at elevated risk of developing obesity. Interestingly, each sub-domain of the COI scale showed similar effect estimates, emphasizing the importance of future work to better understand specific aspects of neighborhood contexts that can be prioritized for intervention. These analyses advance prior research by using a large, population-based cohort of pre-adolescents followed prospectively into adolescence, with objective measures of body weight and height. We also use a comprehensive assessment of neighborhood context designed to reflect compounding forms of advantage that shape opportunities for healthy child development.
Our results add to the literature documenting that neighborhood disadvantage is associated with current and future obesity in adolescence and early adulthood.9,19,32 Our finding that the association is stronger among females compared to males is consistent with studies showing specific aspects of the neighborhood environment may be particularly important for girls in this age range.8,9 For example, neighborhood parks and playgrounds had a stronger association with BMI and obesity rates among 10–17 year old females compared to males33 and supermarket availability in the neighborhood had a longitudinal association with lower BMI in females, but not in males.34 However, different aspects of the neighborhood, such as physical activity resources, may have a stronger impact on boys’ weight.8 As emphasized earlier, the COI incorporates many aspects of the neighborhood environment. Our results of stronger effects among girls suggest that global measures of neighborhood may be more relevant for future research focused on girls.
Neighborhood conditions may influence adolescent weight through many pathways, including physical activity and access to health-promoting resources (parks, safe walking trails, healthy food), behavior and behavioral norms, and stress response pathways.19,35–38 These pathways may also explain sex-based differences in these associations. Within behavioral pathways, it is possible that in less advantaged neighborhoods, threats to girls’ personal safety may lead them to spend more time indoors.19 Additionally, parents may be more protective of girls, thus limiting their outdoor recreational time to a greater degree than boys. For stress response pathways, greater exposure to stress, whether actual or perceived, can have a continuous impact on activating the stress response in the body, which may result in chronic disengagement from physical activity, an increased inclination towards consuming unhealthy foods, and physiological dysregulation characterized by the accumulation of visceral fat.39–41 It is possible that adverse neighborhood conditions are perceived as more stressful or less safe for young girls compared to boys, thus elevating their chronic stress exposure or limiting activities, which may lead to adiposity.
It is important to keep in mind that the children in this cohort were ages 9 and 10 at baseline. Our results may be specific to this very special time in early adolescence when children may be more likely to spend time in their neighborhood compared to younger children and compared to older adolescents and young adults.33 Additionally, young adolescents are likely exerting more control over their own eating and activity levels compared to younger children. A third consideration is that girls are more likely to have started puberty at this age, compared to boys, and previous research has linked low COI with younger pubertal development among girls16, though we were able to control for pubertal status in our models. In one of the few studies to present sex-specific findings for an age group similar to ours, Singh et al7 reported from the National Survey of Children’s Health that females aged 10–11 years old seemed to be particularly sensitive to their environment, with young girls from less advantaged neighborhoods being two to four times more likely to have overweight or obesity compared to young girls from more advantaged neighborhoods, and these findings were stronger compared to males of this same age. In another study, higher COI was associated with lower BMI for females only at age 9, but lower BMI for males at ages 12 and 15, which the authors propose may be due to adaptive calibration in which biological processes are accelerated in unpredictable environments, especially for females.16
Strengths of our study include the large cohort recruited from 21 locations across the country, the ability to study outcomes prospectively, controlling for many important confounding factors, and use of the COI which incorporates many aspects of the neighborhood. Several limitations should also be noted. First, we rely on BMI percentile scores to categorize individuals into categories of not overweight/obesity, overweight, and obesity. BMI is an imperfect measure of adiposity and body composition, and while it may not be sufficient as a single measure in clinical settings for dispensing medical advice to individuals, it is considered a good measure of population health and is strongly correlated with dual x-ray absorptiometry (DEXA), which is considered the gold standard.42 Related, and as discussed extensively in the literature43, the BMI percentile does not represent the same body fatness across subgroups of the population. A second limitation is that our longitudinal sample is smaller and represents a more socioeconomically-advantaged group of children compared to the cross-sectional data (see Supplemental Table 4). This under-representation of socioeconomically disadvantaged participants at the third assessment would lead to under-estimates of the association between COI and obesity, therefore we suspect our results may be conservative. Wide confidence intervals with the HR estimates indicate a degree of imprecision in the calculated prospective association between COI and development of obesity, likely due to the limited time frame (2 years of follow-up) for development of new onset overweight/obesity. As the ABCD study continues, it will be important to include a longer follow-up timeframe. Third, although we adjusted for a range of covariates, there is the possibility of unmeasured confounding. We acknowledge that larger societal forces, including structural racism and historical and current housing and zoning policies that determine where people live and the potentially obesogenic environment in which they live, are critical factors in understanding the associations between neighborhood context and obesity outcomes, but are beyond the scope of this analysis. Finally, ABCD V.4 did not provide a tract-level identifier for clustering, thus we may be overestimating the precision of our estimates. In future research, it will be important to better understand whether the sex differences are specific to the pre- and early adolescent period captured within the developmental period covered by our data. In addition, our results indicate that the COI was associated with obesity, but not overweight; future research is needed to understand if different mechanisms place not overweight/obesity children at risk of transitioning to overweight.
Conclusion
Neighborhood opportunity may influence prevalence of obesity in pre-adolescence and risk of new onset obesity in early adolescence. Females may be particularly influenced by neighborhood conditions. The COI is a wide-ranging measure of neighborhood quality, and though it cannot identify specific pathways for intervention, may be useful for policymakers or program administrators who allocate resources spatially. The COI may help decision-makers make more equitable investments that are informed by multi-dimensional, spatial inequities. Likewise, pediatricians could use this information as a screening tool, to probe for potential health risks and barriers to accessing health care or other services, and to make additional clinical or non-clinical referrals.44
Supplementary Material
Implications and Contribution:
Using a wide-ranging measure of neighborhood quality, this analysis finds that 9 and 10 year old children who resided in lower opportunity neighborhoods had elevated levels of obesity in cross-sectional analysis. In prospective analysis, lower opportunity neightborhoods were associated with higher risk of new onset obesity among females only.
Acknowledgment:
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9-10 and follow them over 10 years into early adulthood. The ABCD Study® is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in the analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from DOI 10.15154/1523041. Additional support for this work was made possible from NIEHS R01-ES032295 and R01-ES031074.
Funding/Support.
Support for this research was provided by the following: the CZI/Silicon Valley Community Foundation to the Center on the Developing Child at Harvard University; the W. K. Kellogg Foundation; T32GM007753 and T32GM144273 (both from the National Institute of General Medical Sciences).
Abbreviations:
- ABCD
Adolescent Brain Cognitive Development
- CI
confidence interval
- COI
Child Opportunity Index
- INR
Income-to-needs ratio
Footnotes
Conflict of Interest Disclosures: None
Contributor Information
Karen A. Ertel, Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health; Department of Biostatistics and Epidemiology, School of Public Health and Health Sciences, University of Massachusetts Amherst.
Sakurako S. Okuzono, Department of Social & Behavioral Sciences, Harvard T.H. Chan School of Public Health.
Logan Nicole Beyer, Department of Social and Behavioral Sciences, Harvard T. H. Chan School of Public Health; Harvard Medical School.
Kedie Pintro, Department of Epidemiology, Harvard T. H. Chan School of Public Health.
Adolfo G. Cuevas, Department of Social and Behavioral Sciences, New York University School of Global Public Health; Center for Anti-racism, Social Justice, and Public Health.
Natalie Slopen, Department of Social and Behavioral Sciences, Harvard T. H. Chan School of Public Health; Center on the Developing Child, Harvard University..
References
- 1.Steinbeck KS, Lister NB, Gow ML, Baur LA. Treatment of adolescent obesity. Nature Reviews Endocrinology. 2018;14(6):331–344. [DOI] [PubMed] [Google Scholar]
- 2.Reilly JJ, Methven E, McDowell ZC, et al. Health consequences of obesity. Arch Dis Child. Sep 2003;88(9):748–52. doi: 10.1136/adc.88.9.748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stierman B, Afful J, Carroll MD, et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. 2021; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardel MI, Atkinson MA, Taveras EM, Holm J-C, Kelly AS. Obesity treatment among adolescents: a review of current evidence and future directions. JAMA pediatrics. 2020;174(6):609–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gordon-Larsen P, The NS, Adair LS. Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity. 2010;18(9):1801–1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Narciso J, Silva AJ, Rodrigues V, et al. Behavioral, contextual and biological factors associated with obesity during adolescence: A systematic review. PloS one. 2019;14(4):e0214941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health affairs. 2010;29(3):503–512. [DOI] [PubMed] [Google Scholar]
- 8.Daniels KM, Schinasi LH, Auchincloss AH, Forrest CB, Roux AVD. The built and social neighborhood environment and child obesity: A systematic review of longitudinal studies. Preventive Medicine. 2021;153:106790. [DOI] [PubMed] [Google Scholar]
- 9.Kim Y, Cubbin C, Oh S. A systematic review of neighbourhood economic context on child obesity and obesity-related behaviours. Obesity reviews. 2019;20(3):420–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Acevedo-Garcia D, Noelke C, McArdle N, et al. Racial And Ethnic Inequities In Children’s Neighborhoods: Evidence From The New Child Opportunity Index 2.0. Health Affairs. 2020;39(10):1693–1701. [DOI] [PubMed] [Google Scholar]
- 11.Ho BJ, Rucker A, Boyle MD, Badolato GM, Goyal MK. Relationship Between Food Insecurity and Neighborhood Child Opportunity Index. The Journal of pediatrics. 2022; [DOI] [PubMed] [Google Scholar]
- 12.Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping Neighborhood Health Geomarkers To Clinical Care Decisions To Promote Equity In Child Health. Health Affairs. 2017;36(6):999–1005. doi: 10.1377/hlthaff.2016.1425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Slopen N, Cosgrove C, Acevedo-Garcia D, Hatzenbuehler ML, Shonkoff JP, Noelke C. Neighborhood opportunity and mortality among children and adults in their households. Pediatrics. 2023;151(4):e2022058316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shanahan KH, Subramanian SV, Burdick KJ, Monuteaux MC, Lee LK, Fleegler EW. Association of Neighborhood Conditions and Resources for Children With Life Expectancy at Birth in the US. JAMA Network Open. 2022;5(10):e2235912-e2235912. doi: 10.1001/jamanetworkopen.2022.35912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aris IM, Rifas-Shiman SL, Jimenez MP, et al. Neighborhood Child Opportunity Index and Adolescent Cardiometabolic Risk. Pediatrics. Feb 2021;147(2)doi: 10.1542/peds.2020-018903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thorpe D, Klein DN. The Effect of Neighborhood-level Resources on Children’s Physical Development: Trajectories of Body Mass Index and Pubertal Development and the Influence of Child Biological Sex. Journal of youth and adolescence. 2022;51(5):967–983. [DOI] [PubMed] [Google Scholar]
- 17.Aris IM, Perng W, Dabelea D, et al. Associations of Neighborhood Opportunity and Social Vulnerability With Trajectories of Childhood Body Mass Index and Obesity Among US Children. JAMA Network Open. 2022;5(12):e2247957-e2247957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee H, Harris K, Gordon-Larsen P. Life course perspectives on the links between poverty and obesity during the transition to young adulthood. Popul Res Policy Rev. 2009;28:505–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kranjac AW, Boyd C, Kimbro RT, Moffett BS, Lopez KN. Neighborhoods matter; but for whom? Heterogeneity of neighborhood disadvantage on child obesity by sex. Health & Place. 2021;68:102534. [DOI] [PubMed] [Google Scholar]
- 20.Kowaleski-Jones L, Wen M. Community and child energy balance: differential associations between neighborhood environment and overweight risk by gender. International journal of environmental health research. 2013;23(5):434–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garavan H, Bartsch H, Conway K, et al. Recruiting the ABCD sample: Design considerations and procedures. Developmental cognitive neuroscience. 2018;32:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Noelke C, McArdle N, Baek M, Huntington N, Huber R, Hardy E, Acevedo Garcia D. Child Opportunity Index 2.0 Technical Documentation. 2020. diversitydatakids.org/researchlibrary/research-brief/how-we-built-it [DOI] [PubMed] [Google Scholar]
- 23.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital and health statistics Series 11, Data from the national health survey. 2002/May// 2002;(246):1–190. [PubMed] [Google Scholar]
- 24.Barch DM, Albaugh MD, Avenevoli S, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Developmental cognitive neuroscience. 2018;32:55–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palmer CE, Sheth C, Marshall AT, et al. A Comprehensive Overview of the Physical Health of the Adolescent Brain Cognitive Development Study Cohort at Baseline. Front Pediatr. 2021;9:734184. doi: 10.3389/fped.2021.734184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. The SAS Program for CDC Growth Charts that Includes the Extended BMI Calculations. Accessed June 15, 2022. https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm
- 27.Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. J Youth Adolesc. Apr 1988;17(2):117–33. doi: 10.1007/bf01537962 [DOI] [PubMed] [Google Scholar]
- 28.Gray JC, Schvey NA, Tanofsky-Kraff M. Demographic, psychological, behavioral, and cognitive correlates of BMI in youth: Findings from the Adolescent Brain Cognitive Development (ABCD) study. Psychol Med. Jul 2020;50(9):1539–1547. doi: 10.1017/s0033291719001545 [DOI] [PubMed] [Google Scholar]
- 29.Rakesh D, Zalesky A, Whittle S. Assessment of Parent Income and Education, Neighborhood Disadvantage, and Child Brain Structure. JAMA Network Open. 2022;5(8):e2226208-e2226208. doi: 10.1001/jamanetworkopen.2022.26208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barch DM, Albaugh MD, Baskin-Sommers A, et al. Demographic and mental health assessments in the adolescent brain and cognitive development study: Updates and age-related trajectories. Dev Cogn Neurosci. Dec 2021;52:101031. doi: 10.1016/j.dcn.2021.101031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. Journal of statistical software. 2011;45:1–67. [Google Scholar]
- 32.Burdette AM, Needham BL. Neighborhood environment and body mass index trajectories from adolescence to adulthood. Journal of Adolescent Health. 2012;50(1):30–37. [DOI] [PubMed] [Google Scholar]
- 33.Fan M, Jin Y. Do neighborhood parks and playgrounds reduce childhood obesity? American Journal of Agricultural Economics. 2014;96(1):26–42. [Google Scholar]
- 34.Chen H-J, Wang Y. Changes in the neighborhood food store environment and children’s body mass index at peripuberty in the United States. Journal of Adolescent Health. 2016;58(1):111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sullivan SM, Peters ES, Trapido EJ, Oral E, Scribner RA, Rung AL. Assessing mediation of behavioral and stress pathways in the association between neighborhood environments and obesity outcomes. Preventive medicine reports. 2016;4:248–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.D’Agostino EM, Zhao AY, Zewdie HY, et al. Associations Between Neighborhood Opportunity and Indicators of Physical Fitness for New York City Public School Youth. Childhood Obesity. 2023; [DOI] [PubMed] [Google Scholar]
- 37.Ghazaryan A, Park S, Onufrak SJ, Carlson AC, Rhone A, Roy K. Characteristics Associated With Purchasing Sugar-Sweetened Beverages and Bottled Water Among US Households, 2015. Journal of the Academy of Nutrition and Dietetics. 2024;124(1):28–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zewdie HY, Zhao AY, Ogletree SS, et al. Longitudinal associations between neighborhood child opportunity and physical fitness for New York City public school youth. American Journal of Epidemiology. 2023:kwad101. [DOI] [PubMed] [Google Scholar]
- 39.Rutters F, La Fleur S, Lemmens S, Born J, Martens M, Adam T. The hypothalamic-pituitary-adrenal axis, obesity, and chronic stress exposure: foods and HPA axis. Current obesity reports. 2012;1:199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mouchacca J, Abbott GR, Ball K. Associations between psychological stress, eating, physical activity, sedentary behaviours and body weight among women: a longitudinal study. BMC Public Health. Sep 11 2013;13:828. doi: 10.1186/1471-2458-13-828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Björntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. May 2001;2(2):73–86. doi: 10.1046/j.1467-789x.2001.00027.x [DOI] [PubMed] [Google Scholar]
- 42.Sun Q, Van Dam RM, Spiegelman D, Heymsfield SB, Willett WC, Hu FB. Comparison of dual-energy x-ray absorptiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors. American journal of epidemiology. 2010;172(12):1442–1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Flegal KM, Ogden CL. Childhood obesity: are we all speaking the same language? Advances in nutrition (Bethesda, Md). 2011;2(2):159S–166S. doi: 10.3945/an.111.000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bazemore AW, Cottrell EK, Gold R, et al. “Community vital signs”: incorporating geocoded social determinants into electronic records to promote patient and population health. J Am Med Inform Assoc. Mar 2016;23(2):407–12. doi: 10.1093/jamia/ocv088 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.