Abstract
Purpose
Chronic non-specific low back pain (CNLBP) is a complex and heterogeneous condition, and it is necessary to explore new treatment approaches. We evaluated whether the addition of dry cupping therapy to guideline‑based conventional therapy would further improve clinical outcomes in CNLBP.
Methods
Thirty-six patients with CNLBP were recruitedand randomly divided into two groups: the control group and the intervention group. The intervention group received cupping therapy in addition to the control group (core stabilization exercises, spinal manipulation and education) for 4 weeks. The primary outcome was the visual analog scale (VAS) for pain intensity. Secondary outcomes were the Roland Morris disability questionnaire (RMDQ), and pressure pain thresholds (PPT) at bilateral Shenshu (BL23), Qihaishu (BL24), and Dachangshu (BL25) acupuncture points.
Results
At week 4 the between‑group difference in resting pain was trivial (median difference 0.0 cm, 95% CI − 1.0 to 1.0). Neither clinically important nor statistically significant differences were detected in disability or PPTs. Both groups improved substantially from baseline.
Conclusion
In this randomized trial, adding dry cupping to conventional therapy offered no additional benefit over conventional therapy alone for pain, disability or PPT in CNLBP. Larger, multicentre trials with longer follow‑up and standardized negative pressures are warranted.
Trial registration: ChiCTR2300069398, http://www.chictr.org.cn, Registration Date: March 15, 2023.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12998-025-00588-x.
Keywords: Cupping, Chronic non-specific low back pain, Pain pressure threshold, Disability, Pain
Introduction
Chronic non-specific low back pain (CNLBP), defined as persistent lumbosacral discomfort lasting ≥ 12 weeks without identifiable pathological etiology, constitutes the predominant subtype of chronic low back pain (CLBP) [1]. This multifactorial condition, accounting for 80%-90% of CLBP cases globally, has emerged as the primary cause of disability among musculoskeletal disorders globally [2, 3]. Characterized by the absence of specific pathoanatomical correlates (e.g., infection, neoplasm, spinal fracture, or inflammatory arthropathy), CNLBP predominantly involves functional musculoskeletal dysfunction rather than structural pathology [4].
One study suggested that microdamage or fatigue in the lower back due to mechanical load during daily activities or work is a significant contributing factor to CNLBP [5]. Additionally, factors such as smoking, obesity, depression, and aging also increase the risk of CNLBP [2, 6].
The management of CNLBP is highly individualized, as not all patients respond uniformly to the same interventions [7]. No single treatment has been found to be universally effective, necessitating the use of evidence-based, multifaceted rehabilitation strategies to alleviate pain and reduce treatment costs [7]. In light of the limited efficacy and potential side effects of pharmacological treatments, non-pharmacological approaches such as physical rehabilitation, health education, and complementary therapies have gained prominence in the management of CNLBP [8, 9]. Core stabilization exercises enhance spinal stability and motor control [10], while spinal manipulation therapy reduces pain sensitivity through sensory and motor modulation [11, 12]. Although both are common, their variable outcomes highlight the need for complementary therapies to address diverse patient needs [13, 14].
Cupping therapy is a traditional Chinese treatment with a history of over 4000 years, including dry cupping therapy (utilizing controlled suction without epidermal disruption) and wet cupping therapy (combining vacuum application with subsequent therapeutic phlebotomy), which has emerged as a promising complementary treatment for CNLBP [15, 16]. Cupping therapy involves creating negative pressure on the skin using vacuum-sealed cups, and it has been widely utilized to alleviate pain and improve physical function [17]. The mechanisms by which cupping therapy exerts its effects are multifaceted and include both physiological and psychological pathways. From a physiological perspective, cupping therapy improves local blood circulation, promotes the removal of pain-inducing substances, and enhances the delivery of nutrients to the affected tissues [18]. It also stimulates mechanoreceptors and small-diameter nerves, leading to the release of endorphins and other neurotransmitters that block pain signals [19]. Moreover, the mechanical deformation caused by negative pressure can restore lumbar fascia sensory feedback, improving muscle coordination and spinal stability [20]. Beyond its physiological benefits, cupping therapy often provides psychological relaxation, which may contribute to its therapeutic effects [21, 22].
Despite its widespread use and reported safety, the efficacy of cupping therapy for CNLBP remains controversial due to a lack of high-quality evidence [13]. Previous research, such as studies examining the impact of cupping therapy on muscle stiffness in the triceps, has demonstrated its potential to modulate tissue properties and reduce stiffness [23]. These findings suggest that similar benefits may extend to other regions, including the lower back. Building on this foundation, our study aimed to investigate the short-term effects of adding cupping therapy to conventional rehabilitation in patients with CNLBP. Our hypothesis was that patients who received cupping therapy in addition to conventional therapy would experience improvements in pain, physical function, and pressure pain threshold (PPT) compared to those who received conventional therapy alone.
Materials and methods
Study design
This was a randomized, comparative trial with single-blind and parallel groups. Our trial design strictly adhered to the STRICTOC (Standards for reporting interventions in clinical trials of cupping) checklist, with full methodological compliance details documented in Online Appendix 1 [24]. The researchers involved in the study, with the exception of the experimental designer and therapists, were unaware of the participants' identities. Additionally, the participants in both groups were also kept unaware of the intervention provided to the other group. The study was registered at www.chictr.org.cn (Registration Date: March 15, 2023), and was approved by the Ethics Committee of Kunshan Rehabilitation Hospital (No. 2023-LYP-001).
Participants
Participants were recruited through posters and Wechat software. The study commenced in March 2023 and concluded in June 2023. The inclusion criteria for participants were as follows [25]: ages ranging from 18 to 48 years, chronic pain lasting for more than 3 months, pain between the costal margin and the transverse lines of the buttock, and pain scores (VAS) ranging from 3 to 8 points. The exclusion criteria included individuals who had received rehabilitation in the last three months, presence of dermatosis in the cupping area, painkillers for the last three months, history of previous spinal surgery, radiating pain, inflammatory or rheumatic diseases of the spine, severe pathological conditions of the spine, and other specific low back pain (LBP) with definitive underlying etiology. Physicians were involved throughout the recruitment process. They assessed participants and performed further diagnostic clarification and management if low back pain with red flag signs was identified.
Randomization
The randomization process was simple, with a researcher who was not involved in the subsequent research stages mixing prepared cards containing therapeutic regimens in an opaque jar. Enrolled patients were randomly assigned by drawing cards from the jar.
Blinding
This study was conducted with evaluator blinding. The participants were unaware of which group they had been assigned to. They were informed that there would be two different interventions but were not aware of the specific treatment measures in the other group. The evaluators who rated the variables were blinded as they did not know which intervention the participants had received, as they were not present during the individual interventions. Only the therapists were aware of the exact interventions.
Interventions
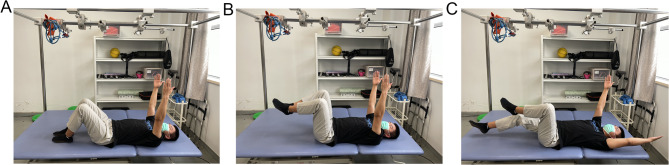
The participants had no prior experience with core stabilization training, spinal manipulation, or cupping therapy (Fig. 1). The spinal manipulation and partial core stabilization training were administered in the climate-controlled rehabilitation hall of Kunshan Rehabilitation Hospital, where ambient temperature was maintained at a constant 24 °C. This detailed description has been structured following the template for intervention description and replication (TIDieR) checklist to ensure replicability [26].
Fig. 1.
Dead bug. A Phase 1: Participants lay on their back with their knees bent and arms fully extended, and then alternated their arms constantly. B Phase 2: While performing the exercise from Phase 1, participants lifted their legs and held them. C Phase 3: Participants performed the dead bug exercise while alternating both their arms and legs
All participants received standardized pre-enrollment health education by a therapist, which included self-management of CNLBP, stretching, strengthening exercises, and the role of emotions and fear avoidance.
Control group (conventional therapy only).
Participants first received spinal manipulation administered by a therapist with over 3 years of professional experience [14], followed by therapist-guided core stability training [27], as detailed in the Online Appendix 2.
Intervention group (dry cupping + conventional therapy)
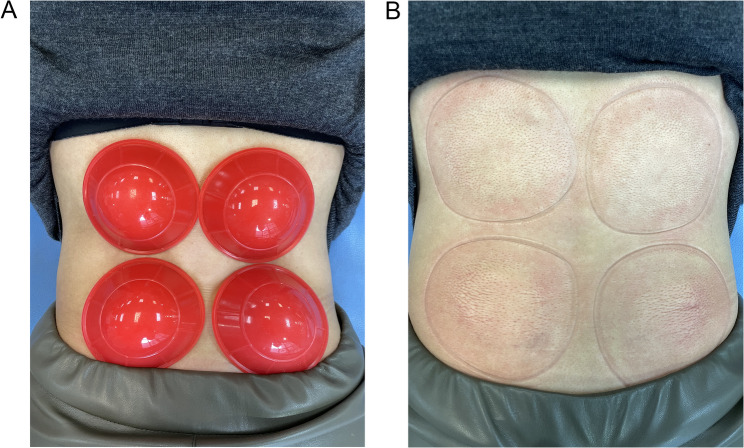
Participants in the intervention group received cupping therapy in addition to the standard treatment protocol administered to the control group. The cups used in this study are made of silicone and have an inner diameter of 5.5 cm and an outer diameter of 7.5 cm. Prior to treatment, the cups were sterilized using 70% alcohol. Subjects were positioned in a prone position on the treatment bed, allowing for the skin of the treatment area to be exposed. The therapist applied two cups in parallel on each side of the L1–L5 vertebral body and removes as much air from the cups as possible while adsorbing. Cupping therapy was performed twice a week with an interval of more than 3 days for a total of 4 weeks (Fig. 2A, 2B).
Fig. 2.
Cupping treatments. A Application of the silicone cups at the low back area. B Ten minutes after cupping
Blinding of participants
Participants attended scheduled rehabilitation sessions at the hospital, with staggered scheduling across groups to minimize inter-group contact. However, within-group concurrent training sessions might occur during the rehabilitation process.
Sample Size
The sample size calculation was conducted based on the results of the primary outcome, which was measured using the VAS. The sample size was determined using the G*Power 3.1 software, with a significance level (α) of 0.05 (two-sided) and a power (1-β) of 0.8, assuming an effect size of 1. The effect size of 1 was based on a similar study by Salemi et al. [28], the cupping group had a VAS mean of 2.25 with a standard deviation (SD) of 1.71, while the sham group had a mean of 4.59 (SD = 2.18). The calculated total sample size was 34 patients. To account for a potential loss rate of 15%, a total of 40 patients were enrolled in the study.
Outcome measures
The pain intensity, disability, and PPT of both groups of subjects were assessed at baseline (T0) and after 4 weeks of treatment (T4). We conducted an additional evaluation of the PPT of both groups of subjects 10 min after the first treatment (T1).
Primary outcome measures
The VAS was utilized to measure the self-reported pain intensity of the patients. The involved participants placing a marker on a 10-cm-long straight line that had stops at each end. The left stop represented no pain, while the right stop represented the worst pain imaginable [29]. MCID for VAS in LBP was 22.5 [30].
Secondary outcome measures
The Roland Morris disability questionnaire (RMDQ) was employed to evaluate functional disability resulting from low back pain. The RMDQ is a concise and user-friendly self-assessment tool designed to measure physical function in individuals with back pain. Its simplicity makes it suitable for monitoring the progress of individual patients in clinical settings. The questionnaire comprises 24 questions that specifically address routine activities of daily living. Each affirmative response is assigned 1 point, and the final score is determined by the total number of points, ranging from 0 to 24. Higher scores indicate greater levels of disability [31]. MCID for RMDQ was 3.5 [32].
The PPT was assessed using a pressure algometer (WD, WX-100, Wenzhou, China). A pressure algometer is a device that measures the force required to elicit a PPT. These devices have been shown to have high reliability and validity [33], and they also demonstrate acceptable intraexaminer reliability in terms of pressure rate application. The PPT measurements taken across multiple sessions showed reliable results without any significant differences [34]. Refer to the study by Volpato et al. [35], PPT was measured bilaterally at three specific points: BL23 (Shenshu), BL24 (Qihaishu), and BL25 (Dachangshu). Participants were instructed to say “yes” when they started feeling pain or discomfort. Once they said “yes,” the pressure was immediately stopped, and the meter was removed from the skin. The PPT threshold was evaluated three times and averaged.
Statistical analysis
The statistician remained blinded to group allocation throughout the data analysis process. Our study employed per-protocol analysis, with two participant withdrawals occurring in both the control and intervention groups. All remaining participants demonstrated full adherence to treatment protocols and completed all scheduled assessments, yielding complete datasets with no missing values.
Data analysis was performed using SPSS 22.0. The normality of continuous data was assessed using the Kolmogorov–Smirnov test. Normally distributed data were presented as mean ± standard deviation, while non-normally distributed data were presented as quartiles. Inter-group comparisons were conducted using the independent sample t-test, while intra-group comparisons were analyzed using the paired sample t-test. For non-normally distributed data, the Mann–Whitney test was employed. The Chi-square test was used to compare proportions in terms of sex. Significance was set at α = 0.05.
Results
Participant flow
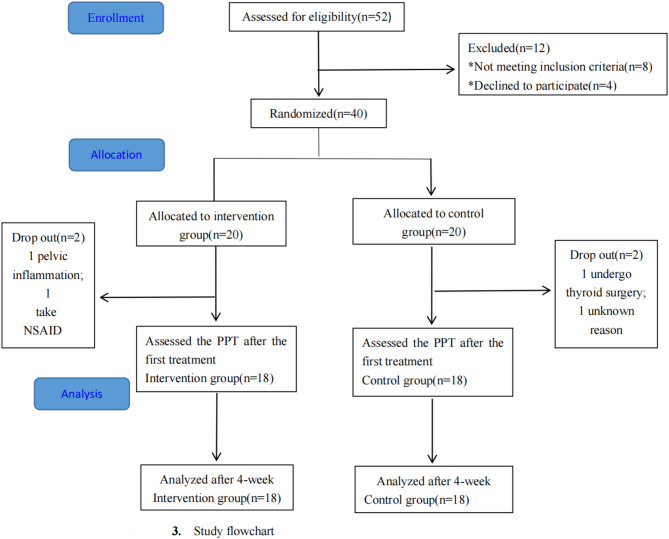
Patients were recruited at Kunshan Rehabilitation Hospital from March 2023 to June 2023, and the study intervention and follow-up assessments were scheduled to be completed by July 2023. The recruitment and assignment process are depicted in Fig. 3.
Fig. 3.
The flowchart of the study
A total of 52 eligible patients were screened, with 12 patients being excluded for not meeting the inclusion criteria (n = 8) or refusing to participate after being informed of the trial (n = 4). Finally, 40 patients were randomly assigned to either the control group or the intervention group. In the control group, one patient withdrew due to thyroidectomy, while the other did not provide a specific reason. In the intervention group, withdrawal occurred due to the sudden diagnosis of pelvic inflammatory disease and the use of nonsteroidal anti-inflammatory drugs for low back pain. Thirty‑six participants therefore completed the 4‑week protocol and were included in the per‑protocol analysis (Intervention n = 18; Control n = 18). Two intervention participants reported experiencing skin itchiness during cupping, but this sensation disappeared after the cups were removed. This acceptable adverse response persisted for two weeks. No other adverse events were documented.
Thirty-six patients with CNLBP, ranging in age from 18 to 48 years, including 6 males and 30 females, volunteered to participate in this study. The distribution of sex, age, height, weight, BMI, and duration of pain was similar between the two groups. The participants’ baseline demographic characteristics are provided in Table 1.
Table 1.
Baseline demographic and clinical variables
| Intervention group (n = 18) | Control group (n = 18) | P | |
|---|---|---|---|
| Age (years)b | 32.11 (7.05) | 35.83 (6.24) | 0.103 |
| Sex (male/female)a | 4/14 | 2/16 | 0.658 |
| Height (cm)b | 164.50 (6.01) | 163.28 (6.95) | 0.576 |
| Weight (kg)b | 62.72 (11.45) | 57.11 (9.31) | 0.116 |
| BMI (kg/m2)b | 23.07 (3.19) | 21.31 (2.37) | 0.070 |
| Pain duration (years)b | 5.50 (3.76) | 5.61 (3.78) | 0.930 |
| VASc | 5.00 (3.75, 7.25) | 4.00 (2.75, 6.25) | 0.323 |
| RMDQc | 5.00 (3.75, 7.00) | 4.00 (3.00, 5.25) | 0.214 |
BMI: body mass index. Data are presented as mean (SD), number of patients, and median (Q1, Q3); a Chi-square test (Fisher, 2side), bIndependent samples t test. cMann-Whitney U test
Effect of the intervention
Primary outcome
VAS
As shown in Table 2, a comparison of the VAS scores between the groups revealed no difference after 4 weeks of treatment (MD 0.00 95% CI − 1.00 to 1.00). However, compared to the baseline scores [control group: 4.00 (2.75, 6.25), intervention group: 5.00 (3.75, 7.25)], both groups experienced a significant reduction in VAS scores after 4 weeks of treatment [control group: 1.50 (0.75, 3.00), intervention group: 1.00 (0.00, 3.00)] (95% CI − 4.00 to − 1.50 and − 5.00 to − 2.00).
Table 2.
Pain intensity and disability
| Intervention group(n = 18) | Control group(n = 18) | CI 95% | Median difference intervention/control |
CI 95% (Median difference) | |
|---|---|---|---|---|---|
| VAS | |||||
| T0 | 5.00 (3.75, 7.25) | 4.00 (2.75, 6.25) | − 1.00 to 2.00 | 0.00( − 1.25, 4.00) | − 0.91 to 2.46 |
| T4 | 1.00 (0.00, 3.00) | 1.50 (0.75, 3.00) | − 1.00 to 1.00 | 0.00( − 1.00, 0.50) | − 1.34 to 1.12 |
| CI 95% | − 5.00 to − 2.00 | − 4.00 to − 1.50 | |||
| RMDQ | |||||
| T0 | 5.00 (3.75, 7.00) | 4.00 (3.00, 5.25) | − 1.00 to 2.00 | 0.00( − 1.25, 3.00) | − 0.60 to 2.16 |
| T4 | 1.00 (0.00, 3.25) | 1.00 (0.00, 2.00) | − 1.00 to 1.00 | 0.00( − 1.00, 1.00) | − 0.50 to 1.61 |
| CI 95% | − 4.50 to − 2.50 | − 4.00 to − 2.50 | |||
VAS Visual analog scale; RMDQ Roland Morris disability questionnaire. T0: Baseline; T4: at 4 weeks treatment. Data was presented as median (interquartile range). Mann–Whitney U test, Hodges-Lehmann 95% CI
Secondary outcomes
RMDQ
As shown in Table 2, a comparison of the RMDQ scores between the groups revealed no difference after 4 weeks of treatment (MD 0.00 95% CI − 1.00 to 1.00). However, the scores in each group significantly reduced from baseline [control group: 4.00 (3.00, 5.25), intervention group: 5.00 (3.75, 7.00)] to 4 weeks after treatment [control group: 1.00 (0.00, 2.00), intervention group: 1.00 (0.00, 3.25)] (95% CI − 4.00 to − 2.50 and − 4.50 to − 2.50).
PPT
A comparison of the PPT between the groups revealed no difference after 4-week interventions [95% CI: BL23 (L: − 0.63 to 1.88; R: − 0.44 to 1.99); BL24 (L: − 0.64 to 1.86; R: − 0.84 to 1.66); BL25 (L: − 0.65 to 1.81; R: − 0.65 to 1.92)]. However, compared to baseline, the PPT in the intervention group significantly increased after the 4 weeks of treatment [95% CI: BL23 (L: − 1.68 to − 0.52; R: − 1.48 to − 0.33); BL24 (L: − 1.76 to − 0.48; R: − 1.39 to − 0.18); BL25 (L: − 1.70 to − 0.73; R: − 1.76 to − 0.71)], while the PPT in the control group showed no statistical differences after the 4 weeks of treatment [95% CI: BL23 (L: − 1.05 to 0.29; R: − 0.89 to 0.25); BL24 (L: − 1.04 to 0.42; R: − 1.15 to 0.22); BL25 (L: − 1.17 to 0.52; R: − 0.93 to 0.54)]. Additionally, after the first treatment, the PPT in the intervention group was significantly higher than before treatment [95% CI: BL23 (L: − 1.70 to − 1.13; R: − 1.60 to − 0.72); BL24 (L: − 1.59 to − 0.96; R: − 1.65 to − 0.74); BL25 (L: − 1.94 to − 1.25; R: − 1.98 to − 1.10)], and it was also higher than that in the control group at the same time point [95% CI: BL23 (L: 0.03 to 2.26; R: 0.11 to 2.41); BL24 (L:0.01 to 2.25; R:0.15 to 2.51); BL25 (L:0.01 to 2.28; R:0.12 to 2.38)]. Please refer to Table 3 for further details.
Table 3.
Pressure pain threshold
| Group | Time | BL23 | BL24 | BL25 | |||
|---|---|---|---|---|---|---|---|
| Left | Right | Left | Right | Left | Right | ||
| Intervention group (n = 18) | T0 | 4.93 ± 1.52 | 5.26 ± 1.54 | 4.88 ± 1.51 | 5.01 ± 1.42 | 4.42 ± 1.42 | 4.45 ± 1.37 |
| T1 | 6.34 ± 1.71c | 6.42 ± 1.84c | 6.15 ± 1.68c | 6.20 ± 1.92c | 6.02 ± 1.78c | 5.92 ± 1.76c | |
| T4 | 6.03 ± 2.01b | 6.16 ± 1.91b | 5.99 ± 2.06b | 5.79 ± 2.02b | 5.63 ± 1.81b | 5.69 ± 2.01b | |
| Control group (n = 18) | T0 | 5.02 ± 1.49 | 5.07 ± 1.54 | 5.07 ± 1.73 | 4.92 ± 1.62 | 4.73 ± 1.57 | 4.86 ± 1.63 |
| T1 | 5.20 ± 1.57a | 5.16 ± 1.53a | 5.03 ± 1.62a | 4.87 ± 1.55a | 4.87 ± 1.56a | 4.72 ± 1.73a | |
| T4 | 5.40 ± 1.67 | 5.39 ± 1.68 | 5.38 ± 1.61 | 5.38 ± 1.64 | 5.05 ± 1.83 | 5.06 ± 1.77 | |
BL23: Shenshu; BL24: Qihaishu; BL25: Dachangshu. T0: baseline; T1: at the first treatment; T4: at 4 weeks treatment. Date was presented as mean (standard deviation); Independent samples t test and paired sample t test. Inter-group: aP < 0.05; intra-group (T4 vs T0): bP < 0.05; (T1 vs T0): cP < 0.05.
Discussion
This study investigated the short-term effects of adding cupping therapy to conventional rehabilitation in patients with CNLBP. Our primary objective was to compare the efficacy of conventional therapy alone versus conventional therapy supplemented with cupping therapy. Both groups exhibited significant improvements in pain intensity (VAS) and disability (RMDQ) after 4 weeks of treatment; however, no statistically significant differences were observed between the two groups.
The absence of between-group differences suggests that the addition of cupping therapy does not enhance the benefits of conventional treatment. Both groups received core stabilization exercises, spinal manipulation, and patient education, which are well-established interventions for CNLBP [36]. Our findings substantiate that the conventional therapeutic regimen integrating health education, core stabilization training, and spinal manipulation demonstrates statistically significant improvements in both pain mitigation and disability index reduction among patients with CNLBP, with clinically satisfactory short-term outcomes. These well-established integrative treatments may have minimized the additional impact of cupping therapy on short-term outcomes. Our findings are consistent with the previous study [21], which found that cupping therapy was not superior to sham interventions for improving pain, function, or quality of life in CNLBP patients. The overall effect of cupping therapy on the multifactorial nature of CNLBP appears to be limited.
Regarding secondary outcomes, the intervention group exhibited a transient improvement in PPT immediately after the first treatment session, suggesting an immediate neuromodulatory effect. The immediate PPT increase observed in the intervention group highlights the potential of cupping therapy to modulate pain sensitivity through immediate physiological effects. However, after 4 weeks of treatment, although the PPT in the intervention group remained higher than baseline, it was not significantly different from the control group. This may be attributed to the timing of the final assessment, conducted 3–5 days after the last treatment session, during which elevated PPT levels may have gradually returned to baseline, as observed by Suzuki et al. [37].
However, some studies have reported significant long-term benefits of cupping therapy for pain reduction and functional improvement. These findings diverge from our own observations. These discrepancies may be attributed to differences in study protocols and populations. For example, Volpato et al. [35] and Salemi et al. [28] only included single sessions of cupping and sham cupping in their studies, whereas we incorporated combination treatment in our trial. Additionally, cultural familiarity with cupping therapy among our Chinese participants could have influenced their response, potentially reducing the placebo effect compared to studies conducted in populations less exposed to this practice. Variability in the standardization of negative pressure applied during cupping, as well as differences in adjunctive treatments, may also explain the inconsistencies across studies.
In our study, two participants in the intervention group reported mild pruritus during moving cupping therapy sessions. These self-limiting reactions resolved spontaneously by the fourth treatment session without recurrence. This finding highlights the clinical imperative to thoroughly inform patients of potential transient cutaneous responses (e.g., erythema, pruritus) prior to treatment initiation, thereby optimizing safety profiles in manual therapy interventions.
In summary, while cupping therapy may provide immediate, short-term effects on pain sensitivity, our study demonstrates that it does not offer additional long-term benefits in pain relief or functional improvement when combined with conventional therapy.
Strengths and limitations
This study has significant implications for clinical practice, indicating that for patients with chronic nonspecific low back pain, the conventional treatment combining health education, core stabilization exercises, and spinal manipulation demonstrates sufficient therapeutic efficacy, thereby eliminating the necessity for supplementary cupping interventions. Our study had certain limitations. First, the utilization of silicone cups, while convenient and practical, limited the ability to precisely standardize the negative pressure applied during cupping therapy, potentially contributing to variability in treatment effects. Second, the follow-up period was relatively short, focusing on immediate and short-term outcomes without assessing the long-term sustainability of the observed benefits. Third, the intervention group received cupping therapy twice weekly, while the treatment group underwent spinal manipulation once per week. This discrepancy in total intervention times may introduce confounding effects on the outcomes. Additionally, while a sham control group could have provided a stronger control for placebo effects, it was not included due to the cultural familiarity of participants with cupping therapy, which could have compromised the blinding and validity of a sham intervention. Lastly, the single‑centre design and modest sample size resulted in limited statistical power and generalisability, particularly to older adults and other care settings. Future studies should employ standardized protocols to ensure consistent treatment application, extend follow-up periods to evaluate long-term effects, recruit larger and more diverse samples to improve generalizability, and incorporate appropriate control groups or innovative placebo designs to better distinguish the specific effects of cupping therapy.
Conclusion
The addition of dry cupping to standard rehabilitation for CNLBP did not yield greater improvements in pain or disability compared to conventional therapy alone over a four-week period. The improvements observed in both groups may reflect the general effectiveness of the core rehabilitation program rather than a distinct effect of cupping. Considering the study’s limitations, such as the modest sample size, single-center setting, short follow-up period, and absence of a sham control, further research through larger, multicenter studies with longer follow-up is needed before cupping can be considered for routine clinical use in this context.
Supplementary Information
Acknowledgements
We thank all participating patients for their cooperation and understanding. We thank the staff of Kunshan Rehabilitation Hospital for their publicity in the recruitment effort.
Author contributions
Study concept and design: Renjie Xu, Guangxu Xu. Data Management: Chengjie Yan. Interventions: Zhou Li, Chaochen Zhao and Jingming Ma. Statistical analysis: Yun Yang. Analyses and interpretation of data: Guangxu Xu and Chengjie Yan. Drafting the manuscript: Renjie Xu, Yun Yang and Chengjie Yan. All authors reviewed the manuscript.
Funding
This work was supported by the Science and Technology Bureau of Kunshan [Grant No. KS2252].
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Our study was approved by the Ethics Committee of Hospital (No. 2023-LYP-001) and all of the patients are voluntary to participate in this study.
Consent for publication
All the authors were informed about the trial and gave consent for publication. We confirm that written consent for publication has been obtained from all individuals whose personal data, images, or case details are included in this manuscript. Copies of the consent forms are available for editorial review upon request.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yun Yang and Guangxu Xu contributed equally to this work and are co-corresponding authors.
References
- 1.Bardin LD, King P, Maher CG. Diagnostic triage for low back pain: a practical approach for primary care. Med J Aust. 2017;206:268–73. [DOI] [PubMed] [Google Scholar]
- 2.Hurwitz EL, Randhawa K, Yu H, Côté P, Haldeman S. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J: Off Publ Eur Spine Soci, the Eur Spinal Deform Soci, Eur Sect Cerv Spine Res Soci. 2018;27:796–801. [DOI] [PubMed] [Google Scholar]
- 3.DALYs; G, Collaborators H. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England). 2016;388:1603–58. [DOI] [PMC free article] [PubMed]
- 4.Hayden JA, Ellis J, Ogilvie R, Malmivaara A, van Tulder MW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. 2021. 10.1002/14651858.CD009790.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coenen P, Kingma I, Boot CR, Bongers PM, van Dieën JH. Cumulative mechanical low-back load at work is a determinant of low-back pain. Occup Environ Med. 2014;71:332–7. [DOI] [PubMed] [Google Scholar]
- 6.Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet (London, England). 2017;389:736–47. [DOI] [PubMed] [Google Scholar]
- 7.Urits I, Burshtein A, Sharma M, Testa L, Gold PA, Orhurhu V, et al. Low back pain, a comprehensive review: pathophysiology, diagnosis, and treatment. Curr Pain Headache Rep. 2019;23:23. [DOI] [PubMed] [Google Scholar]
- 8.Burchert D. Back pain in the primary care setting: Non-specific back pain. Der Internist. 2021;62:24–33. [DOI] [PubMed] [Google Scholar]
- 9.Chiarotto A, Koes BW. Nonspecific low back pain. N Engl J Med. 2022;386:1732–40. [DOI] [PubMed] [Google Scholar]
- 10.Hlaing SS, Puntumetakul R, Khine EE, Boucaut R. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet Disord. 2021;22:998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bialosky JE, Beneciuk JM, Bishop MD, Coronado RA, Penza CW, Simon CB, et al. Unraveling the mechanisms of manual therapy: modeling an approach. J Orthop Sports Phys Ther. 2018;48:8–18. [DOI] [PubMed] [Google Scholar]
- 12.Onifer SM, Sozio RS, DiCarlo DM, Li Q, Donahue RR, Taylor BK, et al. Spinal manipulative therapy reduces peripheral neuropathic pain in the rat. NeuroReport. 2018;29:191–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet (London, England). 2018;391:2368–83. [DOI] [PubMed] [Google Scholar]
- 14.Thomas JS, Clark BC, Russ DW, France CR, Ploutz-Snyder R, Corcos DM. Effect of spinal manipulative and mobilization therapies in young adults with mild to moderate chronic low back pain: a randomized clinical trial. JAMA Netw Open. 2020;3: e2012589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aboushanab TS, AlSanad S. Cupping therapy: an overview from a modern medicine perspective. J Acupunct Meridian Stud. 2018;11:83–7. [DOI] [PubMed] [Google Scholar]
- 16.Mohamed AA, Zhang X, Jan YK. Evidence-based and adverse-effects analyses of cupping therapy in musculoskeletal and sports rehabilitation: a systematic and evidence-based review. J Back Musculoskelet Rehabil. 2023;36:3–19. [DOI] [PubMed] [Google Scholar]
- 17.Choi TY, Ang L, Ku B, Jun JH, Lee MS. Evidence map of cupping therapy. J Clin Med. 2021. 10.3390/jcm10081750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Bedah AMN, Elsubai IS, Qureshi NA, Aboushanab TS, Ali GIM, El-Olemy AT, et al. The medical perspective of cupping therapy: effects and mechanisms of action. J Tradit Complement Med. 2019;9:90–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rozenfeld E, Kalichman L. New is the well-forgotten old: The use of dry cupping in musculoskeletal medicine. J Bodyw Mov Ther. 2016;20:173–8. [DOI] [PubMed] [Google Scholar]
- 20.Qureshi NA, Ali GI, Abushanab TS, El-Olemy AT, Alqaed MS, El-Subai IS, et al. History of cupping (Hijama): a narrative review of literature. J Integrat Med. 2017;15:172–81. [DOI] [PubMed] [Google Scholar]
- 21.Almeida Silva HJ, Barbosa GM, Scattone Silva R, Saragiotto BT, Oliveira JMP, Pinheiro YT, et al. Dry cupping therapy is not superior to sham cupping to improve clinical outcomes in people with non-specific chronic low back pain: a randomised trial. J Physiother. 2021;67:132–9. [DOI] [PubMed] [Google Scholar]
- 22.Almeida Silva HJ, Avila MA, Castro KMS, Pinheiro YT, Lins CAA, Medeiros Barbosa G, et al. Exploring patient experiences of participating in a real and sham dry cupping intervention for nonspecific low back pain: a qualitative study. PLoS ONE. 2022;17(5): e0268656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Y, Mo PC, Jain S, Elliott J, Bleakney A, Lyu S, et al. Effect of durations and pressures of cupping therapy on muscle stiffness of triceps. Front Bioeng Biotechnol. 2022;10: 996589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X, Tian R, Lam WC, Duan Y, Liu F, Zhao C, et al. Standards for reporting interventions in clinical trials of cupping (STRICTOC): extending the CONSORT statement. Chin Med. 2020;15:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicol V, Verdaguer C, Daste C, Bisseriex H, Lapeyre É, Lefèvre-Colau MM, et al. Chronic low back pain: a narrative review of recent international guidelines for diagnosis and conservative treatment. J Clin Med. 2023;12(4):1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348: g1687. [DOI] [PubMed] [Google Scholar]
- 27.Kim CR, Park DK, Lee ST, Ryu JS. Electromyographic changes in trunk muscles during graded lumbar stabilization exercises. PM R. 2016;8:979–89. [DOI] [PubMed] [Google Scholar]
- 28.Salemi MM, Gomes V, Bezerra LMR, Melo TMS, Alencar GG, Montenegro I, et al. Effect of dry cupping therapy on pain and functional disability in persistent non-specific low back pain: a randomized controlled clinical trial. J Acupunct Meridian Stud. 2021;14:219–30. [DOI] [PubMed] [Google Scholar]
- 29.Yoo JH, Kim SE, Lee MG, Jin JJ, Hong J, Choi YT, et al. The effect of horse simulator riding on visual analogue scale, body composition and trunk strength in the patients with chronic low back pain. Int J Clin Pract. 2014;68:941–9. [DOI] [PubMed] [Google Scholar]
- 30.Park KB, Shin JS, Lee J, Lee YJ, Kim MR, Lee JH, et al. Minimum clinically important difference and substantial clinical benefit in pain, functional, and quality of life scales in failed back surgery syndrome patients. Spine (Phila Pa 1976). 2017;42:E474–81. [DOI] [PubMed] [Google Scholar]
- 31.Koç M, Bayar B, Bayar K. A comparison of back pain functional scale with roland morris disability questionnaire, oswestry disability index, and short form 36-health survey. Spine. 2018;43:877–82. [DOI] [PubMed] [Google Scholar]
- 32.Ostelo RW, de Vet HC. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005;19(4):593–607. [DOI] [PubMed] [Google Scholar]
- 33.Kinser AM, Sands WA, Stone MH. Reliability and validity of a pressure algometer. J Strength Cond Res. 2009;23:312–4. [DOI] [PubMed] [Google Scholar]
- 34.Balaguier R, Madeleine P, Vuillerme N. Is one trial sufficient to obtain excellent pressure pain threshold reliability in the low back of asymptomatic individuals? A Test-Retest Study. PLoS ONE. 2016;11: e0160866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Volpato MP, Breda ICA, de Carvalho RC, de Castro MC, Ferreira LL, Silva ML, et al. Single cupping thearpy session improves pain, sleep, and disability in patients with nonspecific chronic low back pain. J Acupunct Meridian Stud. 2020;13:48–52. [DOI] [PubMed] [Google Scholar]
- 36.George SZ, Fritz JM, Silfies SP, Schneider MJ, Beneciuk JM, Lentz TA, et al. Interventions for the management of acute and chronic low back pain: revision 2021. J Orthop Sports Phys Ther. 2021;51(11):CPG1–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suzuki H, Tahara S, Mitsuda M, Izumi H, Ikeda S, Seki K, et al. Current concept of quantitative sensory testing and pressure pain threshold in neck/shoulder and low back pain. Healthcare (Basel, Switzerland). 2022. 10.3390/healthcare10081485. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.