Abstract
Background
Diabetes affects various body systems, increasing the risk of complications.
Objectives
This study assessed the impact of clinical pharmacist-associated education on diabetes self-care practices and glycemic control in Sudanese individuals with Type 2 Diabetes Mellitus (T2DM).
Design and methods
This quasi-experimental study with no control group recruited 110 adults with T2DM from a diabetes clinic over 12 months using simple random sampling. We collected data through interviews and calls. Participants received 12 educational videos covering diabetes management. The intervention was video-based and delivered over 5 months. We analyzed data using SPSS version 28.
Results
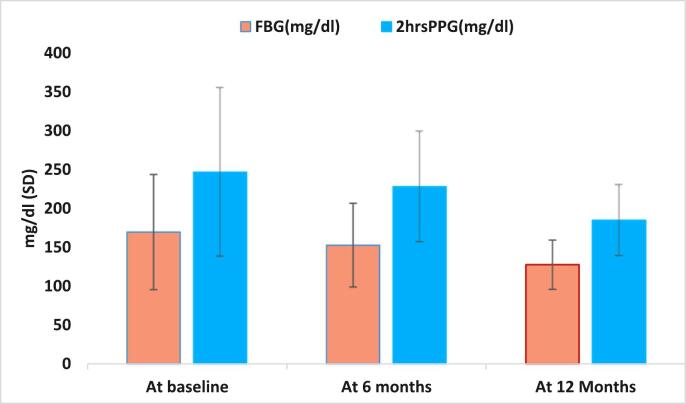
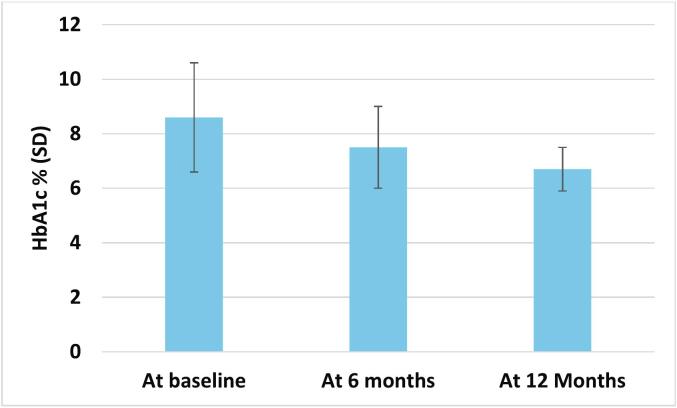
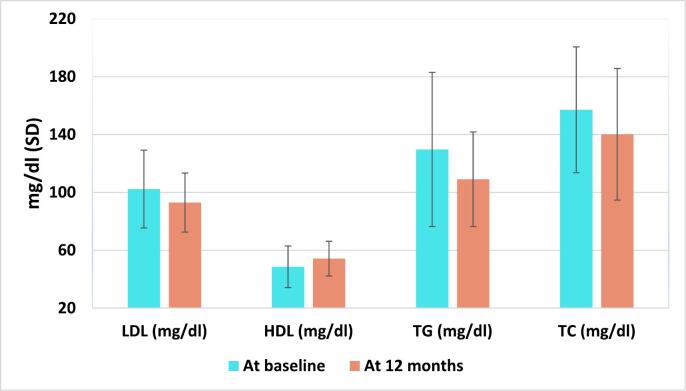
The mean age of participants was 56.2 ± 10.3 years. Self-care practices significantly improved over time. Fasting blood glucose (FBG) levels decreased by 16.7 mg/dL at 6 months (p = 0.009) and 41.9 mg/dL at 12 months (p < 0.001). Two-hour postprandial glucose levels dropped by 18.7 mg/dL at 6 months (p = 0.006) and 61.8 mg/dL at 12 months (p < 0.001). HbA1c levels decreased by 1 % at6 months (p < 0.001) and 1.9 % at 12 months (p < 0.001). The effect size (Cohen's d) was increased from 0.26 at 6 months to 0.74 at 12 months. Similarly, it was increased for 2hrsPPG from 0.2 at 6 months to 0.74 at 12 months. For HbA1c, it was increased from 0.62 at 6 months to 1.25 at 12 months, indicating clinically meaningful improvement in long-term glycemic control following the pharmacist intervention. LDL decreased by 9.2 mg/dL at 12 months (p < 0.001), and HDL increased by 5.5 mg/dL at 12 months (p = 0.002). Changes in BUN and serum creatinine were insignificant.
Conclusion
Clinical pharmacist education improved diabetes self-care practices and metabolic outcomes, including glycemic control and lipid profiles, demonstrating its role in achieving therapeutic goals for patients with T2DM.
Keywords: Self-care practices, Clinical pharmacist, Glycemic parameters, Diabetes control, Education
Highlights
-
•
Diabetes education is the cornerstone of management of diabetes.
-
•
Clinical pharmacist have a crucial role in controlling diabetes mellitus especially in the developing countries.
-
•
This study showed significant improvement in diabetes parameters following clinical pharmacist intervention.
1. Introduction
The prevalence of diabetes in Sudan has increased significantly over the last two decades, driven by rising obesity, sedentary lifestyles, and excessive carbohydrate intake.1, 2, 3 Poorly managed type 2 diabetes mellitus (T2DM) can lead to serious complications, disability, and early death, with increased risks of heart attack, stroke, nephropathy, retinopathy, and neuropathy.4, 5, 6, 7, 8, 9 Effective management aims to lower glycated hemoglobin (HbA1c), as each 1 % reduction significantly reduces the risk of major complications.10 Diabetes care involves both pharmacological and non-pharmacological strategies, emphasizing adherence and self-management as key components.11 While insulin is essential for type 1 diabetes, it is used in T2DM when other treatments fail to maintain glycemic control.12 Intensive insulin therapy and oral hypoglycemics have proven effective in improving outcomes in T2DM.12,13The American Diabetes Association (ADA) emphasizes several factors in selecting T2DM medications, including efficacy, weight impact, hypoglycemia risk, administration route, cardiovascular and renal effects, cost, and potential side effects. For instance, congestive heart failure is associated with pioglitazone or rosiglitazone use.13 Despite pharmacological interventions, many patients remain uncontrolled, highlighting the importance of non-pharmacological measures.14 Nutrition therapy must be individualized and evidence-based. A dietician evaluates the patient's current dietary habits and collaborates to develop a tailored nutrition-care plan.15,16 Medical nutrition therapy (MNT), as defined by the CDC and ADA, is a cornerstone of T2DM management, with proven benefits for HbA1c and other outcomes.17,18 The ADA's evidence-based dietary recommendations and 2020 guidelines also advocate regular physical activity, aerobic exercises, and flexibility training to improve metabolic control.19
Weight reduction is prioritized in T2DM care, particularly for overweight or obese patients. Losing at least 5 % of body weight improves glycemic control and cardiovascular health.19,20 Weight loss can be achieved through lifestyle modifications, medications, or bariatric surgery.20
Psychological health is another critical component of diabetes care. T2DM patients face a heightened risk of psychological distress, which can negatively impact adherence and health outcomes.19,21 Interventions like cognitive-behavioral therapy (CBT), motivational interviewing (MI), and client-centered therapy (CCT) have been effective in addressing diabetes distress.19,21 Smoking cessation is also vital, with counselling and treatment playing essential roles in reducing associated risks.19
Self-management refers to a patient-driven approach to managing diabetes through informed decisions and specific behaviors, often in collaboration with healthcare providers.22,23 Diabetes Self-Management Education and Support (DSMES) is a globally recognized cornerstone of quality diabetes care, aimed at equipping individuals with the knowledge, skills, and confidence needed to manage their condition effectively through structured education and personalized support.24 In Sudan, where access to specialist care and DSMES is limited, pharmacist-led interventions offer a practical, cost-effective, and scalable solution. By utilizing the accessibility and expertise of pharmacists, DSMES can be more consistently and equitably delivered, empowering patients to take control of their health and reducing the risk of complications. The ADA incorporates DSMES programs as one of six core elements in its chronic care model, with proven benefits for metabolic control, prognosis, and quality of life (QoL).19,23,25
Effective diabetes self-care involves lifestyle changes, including exercise, weight control, dietary adjustments, blood glucose monitoring, and proper medication use. In Sudan, traditional diets rich in starch make dietary control challenging for many T2DM patients.26 This underscores the need for tailored interventions that consider cultural and dietary habits. Clinical pharmacists play a vital role in T2DM management by optimizing therapies, resolving drug-related issues, and improving patient education and adherence, which enhances outcomes and reduces healthcare costs.27,28 They support patients through education on glucose monitoring, physical assessments, and adherence tools, with studies confirming the effectiveness of pharmacist-led interventions in improving glycemic control.29, 30, 31 Barriers to effective diabetes care in Sudan include limited access to specialists, poor continuity of care, low health literacy, inadequate adherence, and insufficient counselling.
Given pharmacists' accessibility; especially in community settings, they are well-positioned to provide regular education, support, and task-shifted care. Implementing pharmacist-led interventions could fill critical gaps in Sudan's diabetes care system, offering cost-effective and continuous support that improves patient outcomes in a resource-limited environment. Few studies have focused on Sudanese healthcare settings, where pharmacists' roles in chronic illness management are still underexplored. We have recently shown that pharmacist lead intervention in Sudan is associated with improving knowledge, attitude, patients' quality of life, treatment satisfaction and medication adherence.27,32,33
Despite the presence of specialized diabetes centers in Khartoum, pharmacist-managed clinics, this is the first study in Sudan to implement and assess a video-based diabetes education program led by clinical pharmacists, representing a novel, culturally tailored approach in a resource-limited setting and enables scalable, low-cost education delivery. This study aimed to evaluate the impact of clinical pharmacist education on diabetes self-care and glycemic control in Sudanese adults with Type 2 Diabetes.
2. Methods
2.1. Study design
This study was a quasi-experimental pre-post interventional study without a control group.
2.2. Study site
The study was conducted at a diabetes clinic located at Omdurman Military Hospital (OMH). OMH is a secondary healthcare hospital located in Khartoum state and contains about 704 beds. The clinic provides services for T1DM and T2DM, and it contains an outpatient clinic that receives patients with diabetes two times per week. The clinic staff includes: diabetes physician, dietician, specialist nurse and pharmacist.
2.3. Study population
Adult individuals with T2DM attend the diabetes clinic at OMH.
2.4. Study period
We collected the data from January 2021 to January 2022.
2.5. Inclusion and exclusion criteria
Individuals with T2DM aged more than 18 years (adult, older adult) of both sexes and attending the outpatient clinic were eligible for the study. We excluded any pregnant patients with diabetes, patients currently using diabetogenic medications and any patients who were unable to communicate from the study.
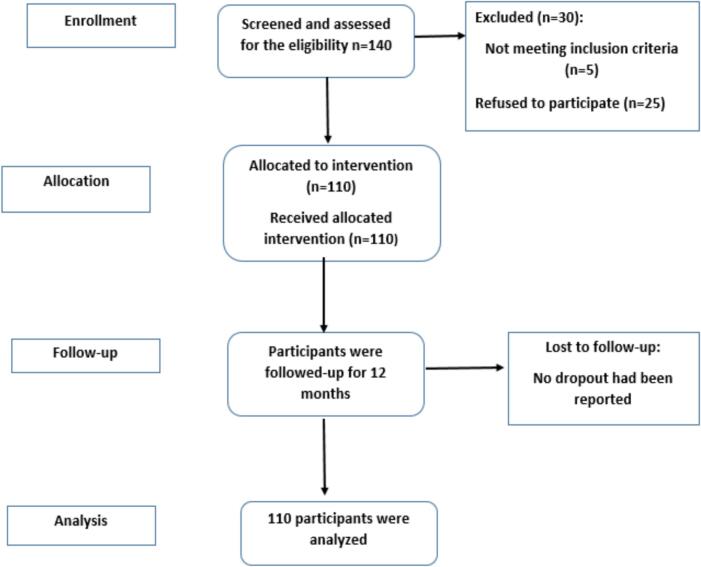
A total of 140 adult patients with T2DM attending the outpatient diabetes clinic at Omdurman Military Hospital (OMH) were initially assessed for eligibility. Of these, 30 individuals were excluded; 15 did not meet the inclusion criteria and 15 declined to participate. A final sample of 110 eligible participants was enrolled in the study. All 110 enrolled participants completed the full 12-month follow-up period. There were no dropouts or losses to follow-up during the study, reducing the risk of attrition bias (Fig. 1).
Fig. 1.
Flow of participants through each stage of the study.
2.6. Sample size and sampling techniques
We calculated the sample size using OpenEpi based on the following parameters: a confidence level of 95 % (α = 0.05), a statistical power of 80 % to detect a true effect, and a margin of error of 5 %. The estimated sample size was 105; but we recruited 110 patients accounting for any drop out as the study progressed. Participants were selected using simple random sampling. Each eligible patient attending the clinic was assigned a number, and numbers were randomly drawn to select participants until the target sample size was reached.
2.7. Data collection tool and method
We collected the data over 12 months through face-to-face interviews and telephone calls. We scheduled six sessions throughout the period of data collection, during which we collected the baseline information of the participants, provided the participants with the educational materials and recorded the laboratory results at baseline, during the follow-up period and at the end of the study. Laboratory investigations were requested and performed at the discretion of each patient's Primary Care Physician (PCPs). Patients were managed by their assigned PCPs per usual care plus clinical pharmacist education. We provided twelve educational videos covered all information about diabetes mellitus to the participants over five months. We blinded both data collectors and biostatisticians to the study condition assignment to reduce assessment bias. They were not informed about the content or timing of the educational program provided to participants. The blinding ensured that data collection, entry, and analysis were carried out objectively, without effect of participants' exposure to the intervention.
The self-care questionnaire used in this study was based on a previously validated tool by Farag et al.,34 which demonstrated strong internal consistency in a Sudanese population (Cronbach's alpha = 0.869). For the present study, the questionnaire was further reviewed to ensure its relevance, clarity, and cultural appropriateness for the specific cohort at Omdurman Military Hospital. The instrument was translated from English to Arabic using a forward–backward translation process conducted by bilingual clinical pharmacy experts. The translated version was then reviewed by an expert panel comprising two clinical pharmacists, a diabetologist, and a public health specialist to ensure semantic and conceptual equivalence. A pilot test was conducted with 10 patients from the same clinical setting who were not included in the final study sample. Feedback was collected on item clarity, language simplicity, and cultural appropriateness. Minor linguistic and formatting adjustments were made accordingly. The pilot confirmed that the instrument was well-understood and acceptable to participants with varied literacy levels, supporting its use in the main study.
The questionnaire consisted of three sections; section one included the socio-demographic data and the medical history of the participants. The second section consisted of questions assessing the participants' self-care practices towards DM.34 Section three consisted of the laboratory investigations that included glycemic parameters (FBG, 2hrsPPG, HbA1c), lipid profile (HDL, LDL, TG, TC).
2.8. Intervention (education)
In this phase, we provided the educational materials to the participants in the form of videos sent throughout the period of intervention. The educational videos were primarily delivered via WhatsApp, a widely used mobile messaging platform in Sudan, ensuring ease of access and minimal technical barriers. Participants who did not have access to WhatsApp or smartphones were offered the videos through in-person file transfer during clinic visits. This flexible, multimodal delivery approach ensured that all participants, regardless of digital literacy or internet availability, could access the content. Participants were instructed to view each video at their convenience and were encouraged to rewatch the materials as needed. We distributed 12 videos over a 5-month period. Participant engagement with the videos was monitored through self-report during scheduled follow-up phone calls and clinic visits. In each session, participants were asked whether they had watched the assigned videos, how many times, and whether they found the content understandable and useful. While no digital viewing logs were used due to technological limitations in the setting, this self-reported feedback was recorded to assess adherence to the educational component. Participants were also encouraged to ask questions and share reflections related to video content, further reinforcing engagement and comprehension. Participants received 4 videos in the first month, and 2 videos each month for the next 4 months. Each video was in MP4 format and lasted from 4 to 7 min.. Before full distribution, the videos had been piloted with a small sample of the target population to ensure clarity, cultural relevance, and engagement. We did minor improvements to content and design based on pilot feedback. All videos were linguistically and culturally tailored including locally relevant language, examples, and illustrations to ensure that they related to the intended Arabic-speaking population. To reduce the potential of contamination from non-study staff or other educational sources, the educational videos was exclusively given by the principal investigator. Furthermore, we carried out data collection independently through planned interviews and follow-up calls, limiting participants' exposure to unintentionally diabetes education throughout the intervention. Although the study did not specifically assess exposure to external sources, the structured and consistent nature of the intervention reduced the likelihood of contamination. In those videos, we provided detailed information about diabetes such as:
-
•
Diabetes mellitus pathophysiology, blood glucose goals, HbA1c goals, management of hyperglycemic and hypoglycemic episodes and how to avoid them.
-
•
Information regarding DM medications includes the mode and time of use, possible contraindications, possible side effects, and managing them.
-
•
The importance of patients' adherence to their healthy diet, medications and physician's instructions.
-
•
Counselling regarding lifestyle modifications, including exercise, weight management, diet modifications, and how to count daily calories.
-
•
The importance of self-care activities to manage their diabetes, including self-monitoring of their blood glucose, foot care, eye care, management of diabetes during sick days, diabetes and special conditions (like diabetes and sexual life, diabetes and infection, diabetes in the elderly patients, etc.).
2.9. Outcome measures
We measured HbA1c, Fasting blood glucose (FBG) and two hours postprandial blood glucose (2hrsPPG) at baseline, 6 months, and 12 months for all participants. In addition, we measured lipid profile and renal function tests for all participants at baseline and at 12 months. Glycemic parameters (FBG, 2hrsPPG, and HbA1c) were measured at baseline, 6 months, and 12 months to allow for more frequent monitoring of short-term and intermediate-term changes in glucose control, which are direct indicators of diabetes management effectiveness and sensitive to educational interventions. In contrast, lipid profile and renal function parameters were assessed only at baseline and at 12 months. This is because meaningful changes in lipid levels and renal biomarkers typically require a longer duration to manifest and are less sensitive to short-term behavioral or educational interventions. Participants continued to receive routine medical care from their assigned primary care physicians throughout the study period. Any adjustments in antidiabetic medications including dose changes or additions of new agents were made at the discretion of the treating physicians, independent of the study team. No protocol-driven medication adjustments were implemented as part of the intervention.
2.10. Data analysis
We analyzed the data by using the Statistical Package for the Social Sciences (SPSS) version 28. We performed descriptive statistics to describe the data and inferential statistics to determine any significant difference between the outcome variables at two and three points. We performed paired sample t-test to compare the mean difference of lipid and renal function parameters at baseline and 12 months. In addition, We performed repeated measure ANOVA to compare the mean difference of FBG, 2hrsPPG and HbA1c levels at baseline, 6 months and 12 months. We have addressed data of the baseline laboratory values using multiple imputation in SPSS, with the assumption of missing at random (MAR). We created five imputed datasets using the Full Conditional Specification (FCS) approach. Analyses were performed individually and pooled using Rubin's rules to control for variability and provide robust, unbiased estimates.
We presented the data as mean differences, with 95 % confidence intervals (CIs) and p-values. Statistical significance was determined at the level of α = 0.05, with p-values less than 0.05 considered significant.
3. Results
3.1. Baseline characteristics of the participants
3.1.1. Socio-demographic characteristics of the participants at baseline
The sample size in this study was 110 participants. 68.2 % of the participants were females. The mean age of the participants was 56.2 (±10.3) years. 84.5 % of them were married and 44.5 % have completed their education till the university level. The mean BMI was 30.1(±5.6) kg/m2. The mean systolic pressure among the participants was 123.2(7.2) mmHg, while the mean diastolic pressure was 80.4 (±5.2) mmHg. The median (Interquartile range, IQR) duration since DM diagnosis for the total participants was 9 (5–16) years (Table 1).
Table 1.
Baseline information of the participants (n = 110).
| Socio-demographic characteristics | Responses | N | % |
|---|---|---|---|
| Gender | Males | 35 | 31.8 |
| Females | 75 | 68.2 | |
| Marital status | Unmarried | 17 | 15.5 |
| Married | 93 | 84.5 | |
| Age | Mean (±SD) | 56.2(±10.3) | |
| Educational level | Illiterate | 17 | 15.5 |
| Primary school | 27 | 24.5 | |
| Secondary school | 49 | 44.5 | |
| Bachelor degree | 16 | 14.5 | |
| Postgraduate level | 1 | 0.9 | |
| BMI: | Underweight | 0 | 0 |
| Normal | 16 | 14.5 | |
| Overweight | 43 | 39.1 | |
| Obese | 51 | 46.4.1 | |
| BMI | Mean (±SD) | 30.1(5.6) | |
| SBP (mmHg), | Mean (SD) | 123.2(7.2) | |
| SBP N (%) | Uncontrolled | 14 | 12.7 |
| Controlled | 96 | 87.3 | |
| DBP (mmHg) | Mean (SD) | 80.4(5.2) | |
| DBP N (%) | Uncontrolled | 25 | 22.7 |
| Controlled | 85 | 77.3 | |
| Duration since DM diagnosis | Median(IQR) | 9(5–16) | |
| Duration since DM diagnosis | 1–5 | 27 | 24.5 |
| 6–10 | 31 | 28.2 | |
| 11–15 | 23 | 20.9 | |
| 16–20 | 17 | 15.5 | |
| > 20 years | 12 | 10.9 | |
SD: standard deviation, BMI: body mass index, DBP: Diastolic blood pressure, SBP: Systolic Blood Pressure. DM: diabetes mellitus.
3.1.2. Family and social history and diabetes-associated complications of the participants at baseline
Most participants had a family history of diabetes (66.4 %), and more than half of them had a history of hypertension (51.8 %). Most participants in this study have never been alcoholic abusers (94.5 %) or smokers (93.4 %). More than 50 % of participants suffered from episodes of recurrent hyper or/and hypoglycemia, tooth decay, retinopathy, and peripheral neuropathy. Among them, tooth decay was the most reported complication (70.9 %) (Table 2).
Table 2.
Family and social history and Diabetes-associated complications of the participants at baseline (n = 110).
| Variables | Responses | N | % | |
|---|---|---|---|---|
| Family history in first-degree relatives | Diabetes | Yes | 73 | 66.4 |
| No | 37 | 33.6 | ||
| Hypertension | Yes | 57 | 51.8 | |
| No | 53 | 48.2 | ||
| Dyslipidemia | Yes | 38 | 34.5 | |
| No | 72 | 65.5 | ||
| Social history | Alcohol | Never | 104 | 94.5 |
| I stopped | 6 | 5.5 | ||
| Smoking | Never | 99 | 90.0 | |
| I stopped | 11 | 10.0 | ||
| Complications | History of renal diseases | – | 8 | 7.3 |
| History of cardiac diseases | – | 13 | 11.8 | |
| Episodes of recurrent hyper or/and hypoglycemia | – | 63 | 57.3 | |
| Tooth decay | – | 78 | 70.9 | |
| Peripheral neuropathy | – | 59 | 53.6 | |
| Retinopathy | – | 65 | 59.1 |
Cig: cigarette.
Cardiac problems: Ischemic heart diseases, heart failure, heart valves replacement, stroke, TIA, atherosclerosis.
Renal problems: renal stones, acute kidney injury, chronic kidney diseases, benign prostatic hyperplasia.
3.2. Participant's self-care practices towards diabetes at baseline and 12 months
At baseline, more than one third (38.2 %) of participants reported that they have glucometers in their houses. The majority of the participants (76.4 %) checked their blood glucose periodically in the labs. 56.4 % of them reported that they examined their feet. 70.9 % of them were doing exercise. 72.7 % reported that they have a proper meal plan recommended by their doctor. After 12 months, 44.5 % of the participants had glucometers in their houses, and the majority of them 77.2 % checked their blood glucose by themselves. The participants showed improvement towards their adherence to physical exercise, foot and eye care at the end of the study when compared baseline (Table 3).
Table 3.
Diabetes-related self-care practices at baseline and after 12 months (n = 110).
| Practice | Responses | Before |
After |
||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Having a glucometer at home | Yes | 42 | 38.2 | 49 | 44.5 |
| No | 68 | 61.8 | 61 | 55.5 | |
| If yes, check blood sugar with a glucometer by the patient? | Yes | 35 | 83.3 | 38 | 77.5 |
| No | 7 | 16.7 | 11 | 22.5 | |
| The place where the blood sugar is tested | In the lab | 84 | 76.4 | 76 | 69.1 |
| In home by glucometer | 3 | 2.7 | 9 | 8.2 | |
| Both | 23 | 20.9 | 25 | 22.7 | |
| The frequency of testing blood sugar level | Once a month | 47 | 42.7 | 43 | 39.1 |
| Once a week | 6 | 5.5 | 9 | 8.2 | |
| Twice a week | 10 | 9.1 | 9 | 8.2 | |
| Every 2 months | 8 | 7.3 | 9 | 8.2 | |
| Every day | 3 | 2.7 | 3 | 2.7 | |
| Twice a month | 4 | 3.6 | 5 | 4.5 | |
| On need | 9 | 8.1 | 5 | 4.5 | |
| Every 3 months | 23 | 21.0 | 27 | 24.5 | |
| Doing physical exercise | Yes | 78 | 70.9 | 94 | 85.5 |
| No | 32 | 29.1 | 16 | 14.5 | |
| Frequency of doing physical exercise /week | Median (IQR) | 7 (4–7) | 7 (4–7) | ||
| Examining feet | Yes | 62 | 56.4 | 91 | 82.7 |
| No | 48 | 43.6 | 19 | 17.3 | |
| If yes, the frequency of examining feet | Once per year | 1 | 1.6 | 0 | 0 |
| Twice per month | 4 | 6.5 | 7 | 7.7 | |
| Once per week | 7 | 11.3 | 13 | 14.3 | |
| Once per day | 45 | 72.6 | 56 | 61.5 | |
| Sometimes | 0 | 0 | 5 | 5.5 | |
| Monthly | 2 | 3.2 | 6 | 6.6 | |
| Twice a week | 3 | 4.8 | 4 | 4.4 | |
| Applying moisturizing lotion on feet | Yes | 93 | 84.5 | 93 | 84.5 |
| No | 9 | 8.2 | 8 | 7.3 | |
| Sometimes | 8 | 7.3 | 9 | 8.2 | |
| Inspection of the shoes before putting on | Yes | 88 | 80.0 | 91 | 82.7 |
| No | 15 | 13.6 | 5 | 4.5 | |
| Sometimes | 7 | 6.4 | 14 | 12.7 | |
| Checking eyes in the hospital | Yes | 65 | 59 | 79 | 71.8 |
| No | 45 | 41 | 31 | 28.2 | |
| If yes, the frequency of checking eyes in the hospital | Once per year | 29 | 44.6 | 35 | 44.3 |
| Once per month | 9 | 13.8 | 13 | 16.5 | |
| Once per 3 months | 14 | 21.6 | 19 | 24 | |
| When I complain | 2 | 3.1 | 1 | 1.3 | |
| Every 6 months | 6 | 9.2 | 7 | 8.9 | |
| Since I had DM | 4 | 6.2 | 4 | 5 | |
| 6 times /year | 1 | 1.5 | 0 | 0 | |
| Telling the health care provider about diabetes before taking any other medicine | Yes | 105 | 95.5 | 110 | 100 |
| No | 5 | 4.5 | 0 | 0 | |
| Having a proper meal plan recommended by the doctor? | Yes | 80 | 72.7 | 101 | 91.8 |
| No | 30 | 27.3 | 9 | 8.2 | |
3.3. Biochemical changes among the participants
3.3.1.1. HbA1c, FBG and 2hrsPPG levels at baseline, 6 month, and 12 month-periods
A pairwise comparison using the Bonferroni correction showed that the mean difference in FBG level from baseline to 6 months fell by 16.7 mg/dl (CI, 3.5–30, p = 0.009) and from baseline to 12 months, it fell by 41.9 mg/dl (CI 28.4–55.5, p < 0.001).
Moreover, the mean difference in 2hrsPPG level from baseline to 6 months fell by 18.7 mg/dl (CI, 2.4–39.8, p = 0.006) and from baseline to 12 months, it fell by 61.8 (CI 42.3–81.4, p < 0.001). On the other hand, the mean difference in HbA1c level from baseline to 6 months fell by 1 % (CI, 0.6–1.5, p < 0.001) and from baseline to 12 months, it fell by 1.9 % (CI 1.5–2.2, p < 0.001). Hence the results of the repeated measure ANOVA indicate a significant time effect for FBG, 2hrsPPG and HbA1c levels among the three time points (Table 4, Fig. 2, Fig. 3). The intervention showed various degrees of clinical significance for the primary outcomes. The effect size of FBG was minimal at 6 months (Cohen's d = 0.26), but increased to a medium-to-large effect by 12 months (d = 0.74), indicating a gradual but considerable improvement in FBG level. Similarly, the effect size for 2hrsPPG at 6 months was (d = 0.20), but was increased to 0.74 at 12 months indicating improved postprandial control with time. In contrast, HbA1c revealed a moderate effect at 6 months (d = 0.62), which increased to a large effect at 12 months (d = 1.25), indicating a considerable and clinically meaningful improvement in long-term glycemic control following the pharmacist-led educational intervention. To assess the overall clinical relevance of the intervention, we calculated a composite outcome which is defined as the proportion of participants achieving a ≥ 1 % reduction in HbA1c from baseline. At 6 months, 61.8 % of participants reached this target, which increased to 78.2 % by 12 months. This summary measure reflects a substantial and sustained glycemic improvement attributable to the pharmacist-led video intervention.
Table 4.
Pairwise comparisons of the mean difference of the glycemic parameters, lipid profile and renal function parameters at different time points.
| Laboratory data | Mean (±SD) at baseline | Mean (±SD) At 6 months |
Mean difference baseline-6 months (95 %, CI) |
P value |
Mean (±SD) at 12 months |
Mean difference baseline-12 months (95 %, CI) |
P value |
|---|---|---|---|---|---|---|---|
| FBG(mg/dl) | 169.4 (±74) | 152.6(±53.8) | 16.7 (3.5–30) | 0.009 | 127.5(31.7) | 41.9 (28.4–55.5) | <0.001 |
| 2hrsPPG(mg/dl) | 246.5(±108.6) | 227.8 (±71.3) | 18.7 (2.4–39.8) | 0.006 | 184.6 (45.9) | 61.8 (42.3–81.4) | <0.001 |
| HbA1C (%) | 8.6(±2) | 7.5 (±1.5) | 1(0.6–1.5) | <0.001 | 6.7 (0.8) | 1.9 (1.5–2.2) | <0.001 |
| LDL(mg/dl) | 102.3 (±26.9) | – | – | – | 93(±20.4) | 9.2(3–15) | 0.003 |
| HDL(mg/dl) | 48.6(±14.4) | – | – | – | 54.2(±12) | −5.5(2–8.9) | 0.002 |
| TG(mg/dl) | 129.7 (±53.3) | – | – | – | 109.1(±32.7) | 20.6(10.4–30.9) | <0.001 |
| TC (mg/dl) | 157.1 (±43.5) | – | – | – | 140.2(±45.5) | 16.9(7.8–26) | <0.001 |
| BUN(mg/dl) | 23.7 (±7) | – | – | – | 23.4(±6.5) | 0.3(−1.5–2) | 0.706 |
| Scr(mg/dl) | 0.7 (±0.2) | – | – | – | 0.7(±0.2) | 0.02(−0.04–0.08) | 0.508 |
SD: standard deviation, CI: Confidence interval, FBG: fasting blood glucose, 2hrsPPG: 2 h postprandial glucose, HbA1c: glycosylated hemoglobin, LDL: low-density lipoprotein, HDL: high-density lipoprotein, TG: triglyceride level, TC: total cholesterol level. BUN: blood urea nitrogen, Scr: serum creatinine. Note: p value of less than 0.05 considered as a statistically significant.
Fig. 2.
Comparison of the mean (SD) of FBG and 2hrsPPG at baseline, 6 month months and 12 month of the study. FBG: fasting blood glucose, 2hrsPPG: 2 h postprandial glucose. SD: standard deviation. p < 0.009 at 6 months, and p < 0.001 at 12 months.
Fig. 3.
Comparison of the mean (SD) of HbA1c at baseline, 6 month months and 12 month of the study, HbA1c: glycosylated hemoglobin, SD: standard deviation. p < 0.001 at 6 and 12 months.
3.3.1.2. Lipid profile and renal function parameters at baseline and 12 month-periods
The Mean difference of the LDL level from baseline to 12 months for participants fell by 9.2 mg/dl (CI, 3–15, p < 0.001) while the mean difference of the HDL level from baseline to 12 months for the participants increased by 5.5 mg/dl (CI, 2–8.9, P = 0.002). However BUN and Scr revealed a statistically insignificant results (Table 4, Fig. 4).
Fig. 4.
Comparison of the lipid parameters at baseline and 12 month of the study. LDL: low-density lipoprotein, HDL: high-density lipoprotein, TG: triglyceride level, TC: total cholesterol, SD: standard deviation. p < 0.001 at 12 months.
The statistical analysis demonstrates no significant association between the improvement of patients' self-care practices and either the duration of diabetes (p = 0.384) or sex (p = 0.936), suggesting that these demographic factors do not appear to influence patients' engagement in self-care behaviors. Additionally, no significant relationship was found between sex and glycemic control, as measured by HbA1c, at both baseline (p = 0.444) and after 12 months (p = 0.132), indicating comparable glycemic outcomes between male and female patients. Notably, despite the result was statistically insignificant, a linear trend was identified between diabetes duration and baseline HbA1c levels (p = 0.08), implying that longer disease duration is associated with poorer glycemic control at the time of assessment. However, this association was not maintained after 12 months (p = 0.985), suggesting that effective clinical management may mitigate the negative impact of longer diabetes duration on glycemic outcomes. Although most variables did not demonstrate statistically significant associations, the observed trend between diabetes duration and baseline glycemic control highlights the need for targeted early interventions in patients with longstanding diabetes.
4. Discussion
Pharmacists play a crucial role in diabetes management, screening high-risk patients, setting treatment goals, and assessing health status. A strong family history of diabetes is a significant risk factor for T2DM. In our study, 66.4 % of participants reported a family history of diabetes, consistent with findings by Bukhsh et al. (59.2 %).35 However, other studies showed lower rates, such as 47 % in a Sudanese study36 and 44.2 % in the interventional group in a study by Al Mazroui et al.,37 Pharmacists educate patients on glucometer use, foot care, blood pressure monitoring, and lipid management while promoting adherence to care standards.29 This study assessed the impact of pharmacist-led education on self-care, including exercise, weight management, diet, and self-monitoring of blood glucose (SMBG). The proportion of participants owning glucometers increased by 8 %, with most still preferring laboratory tests for reliability. During the COVID-19 pandemic, participants relied more on home monitoring due to fears of visiting laboratories.
Regular exercise is critical for T2DM management. Over 70 % of participants exercised regularly, improving by 14.6 % from baseline. Comparable studies reported similar trends, such as 62.3 % in Ahmed et al.38 and 46.9 % in Farag et al.,34 Conversely, Al-Maskari et al. reported higher rates (83.4 %).39 Foot care adherence also improved, rising from 56 % to over 80 %, aligning with Al-Maskari et al.'s findings (81 %).39 Eye care adherence increased from 59 % to 71.8 %, consistent with Sudanese findings (45.1 %).34Dietary counselling was common, with nearly 75 % of participants receiving advice on meal plans, aligning with studies by Farag et al. and Al-Maskari et al.,34,39 However, adherence to these recommendations remains an area of concern. Overall, participants demonstrated improved self-care practices over time, underscoring the positive impact of pharmacist-led educational programs.
Notably, FBG levels significantly improved over the study period. The mean reduction from baseline to six months was 16.7 mg/dL (p = 0.009) and 41.9 mg/dl at 12 months (p < 0.001). Comparable studies reported similar improvements, such as a 24.2 mg/dL reduction in Tabassum et al.,40 21.4 mg/dl in Mourao et al.,41 and 36.7 mg/dl in George et al.,42 These findings indicate a significant time effect on FBG reduction. The mean reduction in 2hrPPG was 18.7 mg/dl at six months (p = 0.006) and 61.8 mg/dl at 12 months (p < 0.001). This aligns with Tabassum et al., who reported a 30 mg/dl decrease,40 and Malathy et al., who observed a 33 mg/dl reduction.43 HbA1c levels improved significantly, with a mean reduction of 1 % at six months (p < 0.001) and 1.9 % at 12 months (p < 0.001). This aligns with findings from other studies showing reductions of 1–1.7 %.44, 45, 46,and These reductions significantly lower the risks of heart attack (26.6 %), stroke (22.8 %), and other diabetes-related complications (70.3 %).10 The findings of this study are consistent with and go beyond those of major meta-analyses. For example, Santschi et al. (2012) and Wang et al. (2020) found that pharmacist-led therapies reduced HbA1c by an average of 0.76 % and 0.85 %, respectively. In comparison, this research found a higher 1.9 % decrease, most likely due to its persistent, culturally tailored video-based method. Improvements in FBG and 2hrPPG were also greater than previously reported.47,48
Our study also showed improvement in lipid profile. For instance, LDL cholesterol decreased by 9.2 mg/dl (p = 0.003), consistent with Cohen et al. (9.4 mg/dl)49 and Chan et al. (6.5 mg/dL).50 HDL cholesterol improved by 5.5 mg/dl, agreeing with Wishah et al.44 and Al Mazroui et al.,37 However, some studies reported no significant HDL improvement.45,50, 51, 52. Variations in results could be attributed to differences in interventions, sample sizes, and study durations.
Pharmacists can deliver Diabetes Self-Management Education and Support (DSMES), equipping patients with the skills and confidence needed to manage their condition effectively. For instance, regular counselling by pharmacists helps patients understand: diabetes and impact on their life and health, how to interpret blood glucose readings, the impact of diet and exercise and early warning signs of complications. Ultimately, this education fosters self-efficacy, enabling patients to make informed decisions, engage in goal-setting, and assume active roles in managing their health. Studies show that pharmacist-led DSMES interventions significantly increase patients' diabetes knowledge, perceived control, and self-care behavior.53
In addition Pharmacists can help in increasing adherence for diabetes medication as they can address common barriers to adherence such as: misunderstanding of prescriptions, concerns about side effects, forgetfulness or lack of routine, cultural beliefs or myths around medication, clarify treatment plans and reinforce the importance of consistent use as well as provide tools like pill organizers or reminder systems. Evidence confirm that pharmacist interventions lead to significant improvements in medication adherence, with corresponding improvements in clinical outcomes such as HbA1c.54
The above initiative if implemented well can help in decreasing health care cost. Pharmacist-led educational interventions have demonstrated cost-effectiveness by improving clinical outcomes and reducing the need for more expensive healthcare services. For instance, Zhu et al. (2023) showed that in a systematic review assessing the cost-effectiveness of pharmacist involvement in diabetes management, that pharmacist care is more cost-effective compared to standard care, primarily due to better glycemic control and enhanced patient compliance.55
In addition, Hendrie et al. (2014) assessed the cost-effectiveness of a pharmacist-led Diabetes Management Education Program (DMEP) and found that it significantly reduced the number of glycemic episodes in patients with type 2 diabetes mellitus. The program was determined to be cost-effective, with patients expressing willingness to pay more than the cost to avoid hypoglycemic episodes.24
Comparisons with studies from other LMICs support the potential of pharmacist-led and video-based interventions. In Pakistan, Bukhsh et al. demonstrated that pharmacist-led education significantly improved HbA1c levels and diabetes self-care practices, although the intervention was delivered face-to-face rather than through video content.56 In Nigeria, David et al. implemented a pharmacist-led program that enhanced both glycemic control and medication adherence among patients with type 2 diabetes.57 Similarly, in Egypt, El-Haga et al. found that structured diabetes education improved patients' knowledge and self-care behaviors regarding self-administration of insulin injections among diabetic patients, though it was conducted through direct group sessions.58 Unlike these studies, our intervention used culturally tailored mobile videos, offering a scalable, low-cost solution that may be more feasible in settings with limited healthcare workforce availability and high patient loads.It is important to point out that the alternative causes for the observed improvements in glycemic control and self-care practices may exist in addition to pharmacist-led education. Regression to the mean is an important concern, since persons with initially poor glycemic control may normally improve with time without intervention. In addition, increased clinic visits and regular interaction with healthcare professionals during the study period may have improved adherence and awareness, regardless of the educational videos. The Hawthorne effect, in which people change their behavior just because they are being observed, may have also had a role. Finally, seasonal factors, medication adjustments by primary care providers or enhanced access to lab testing during the 12 months might influence the observed results. While the findings suggest that pharmacist-led video education may be a sustainable and feasible method for diabetes care in low-resource settings like Sudan, the lack of a control group limits the ability to draw definitive causal inferences. The improvements observed could have been influenced by other factors such as regression to the mean, increased clinical engagement, seasonal variations, or the Hawthorne effect. The use of pre-recorded, culturally adapted videos reduces continuing expenditures and pressure on overloaded healthcare systems, and assures constant delivery of educational materials. Videos may be readily transmitted through mobile devices or local networks, making them available even in remote areas. Leveraging pharmacists, who are frequently more accessible than physicians, improves continuity of treatment and makes better use of existing human resources. This scalable strategy provides an effective way for improving diabetes outcomes in similar underserved locations. To improve diabetes care in low-resource settings, policies should integrate pharmacists into multidisciplinary teams, establish national pharmacist-led DSMES programs using culturally appropriate video tools, encourage task-shifting to expand pharmacists' roles, and provide long-term funding and training for efficiently implementing these interventions. Despite the promising outcomes of this study, several implementation barriers must be acknowledged to ensure successful scale-up. One of the primary challenges is limited internet access, particularly in rural or underserved areas where mobile data coverage may be unreliable or unaffordable. Although WhatsApp was used for video delivery due to its widespread use, some participants required alternative formats such as in-person file transfers highlighting the need for flexible, hybrid delivery methods. Participant literacy also presents a barrier, as comprehension of educational content may vary based on health literacy levels. While efforts were made to use culturally appropriate and simplified language in the videos, some individuals may still require additional support or face difficulties with self-directed learning. Furthermore, cultural resistance to pharmacist-led counselling could limit uptake. In some settings, pharmacists may be viewed primarily as dispensers rather than educators, which can affect patient trust or engagement with pharmacist-driven education. To address these challenges, future scale-up efforts should incorporate community sensitization campaigns, infrastructure support for digital access, and tailored strategies to overcome literacy and cultural barriers.
5. Strengths and limitations
-
•
The study's strengths include a low dropout rate (<2 %) and the individualized nature of interventions, which helped minimize contamination. A unique aspect of this study is that it is one of the pioneering efforts in this field in Sudan and demonstrated that clinical pharmacist-led education can improve diabetes self-care practices and metabolic outcomes. However, the study also has the following limitations:
-
•
The lack of a control group reduces its internal validity and limits causal interpretation.
-
•
External variables, such as natural changes over time, frequent testing, or unrelated treatments, may have contributed to the observed improvements.
-
•
There is also a possibility that recall bias occurred during participant recruitment, which could influence self-reported results and increase the likelihood of inaccurate reporting or social desirability bias.
-
•
Furthermore, conducting the study in a single center may limit the generalizability of the findings to broader populations.
-
•
Extending the study duration beyond 12 months could allow for a more comprehensive assessment of metabolic parameters related to diabetes control.
6. Conclusion and recommendations
Clinical pharmacists significantly improve diabetes management by enhancing self-care practices and achieving therapeutic goals in T2DM patients. This study highlights their essential role in improving glycemic control, lipid profiles, and overall diabetes care. The findings provide robust evidence supporting the integration of pharmacists in T2DM care in Sudan. To improve diabetes care in low-resource settings, national guidelines should incorporate clinical pharmacists into primary diabetes care, pharmacist-led DSMES programs using culturally appropriate video tools should be established, furthermore, encouraging task-shifting to expand pharmacists' roles, and providing long-term funding and training for efficiently implementing these interventions are critical issues. The next steps should include a well-designed randomized controlled trial (RCT) to strengthen causal evidence of the intervention's effectiveness. The proposed RCT could employ a cluster randomization approach at the clinic level to prevent contamination between intervention and control groups. Participants in the intervention arm would receive the same culturally tailored video-based education from clinical pharmacists, while those in the control arm would receive standard care without additional educational support. The trial should include a longer follow-up period; ideally 18 to 24 months to assess the sustainability of improvements in glycemic control, self-care behaviors, and secondary outcomes such as lipid profiles and healthcare utilization. Medication titration and adherence should be closely tracked through electronic health records or pharmacy refill data to account for treatment changes. Following this, a cost-effectiveness analysis should be conducted to evaluate the financial benefits of scaling pharmacist-led video education. Given the rising adoption of mobile health technologies, this asynchronous, low-cost video intervention offers a scalable and replicable model for delivering diabetes self-management education across other low- and middle-income countries. Finally, a multi-site implementation study would help evaluate the feasibility, scalability, and real-world impact of this intervention across diverse geographic and healthcare settings.
CRediT authorship contribution statement
Safaa Badi: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Data curation, Conceptualization. Sara Zainelabdein Suliman: Writing – review & editing, Methodology, Investigation, Conceptualization. Rayan Almahdi: Writing – review & editing, Software, Methodology, Conceptualization. Mohammed A. Aldomah: Writing – original draft, Formal analysis, Data curation, Conceptualization. Habab Khalid Elkheir: Writing – review & editing, Validation, Supervision, Conceptualization. Mohamed Izham Mohamed Ibrahim: Writing – original draft, Visualization, Supervision, Methodology, Conceptualization. Mohamed H. Ahmed: Writing – original draft, Visualization, Investigation, Conceptualization.
Consent for publication
Our manuscript doesn't contain any individual person's data to be published.
Ethics approval and consent to participate
We performed this study in line with the principles of the Declaration of Helsinki. We obtained the ethical approval from Omdurman Islamic University (OIU/FPGS-Jan-2020) and Omdurman Military Hospital (GDMS/April-2021). The ethics committees reviewed and approved the use of educational video materials as part of the intervention. We obtained a written informed consent from the participants before being recruited into the study after explaining the main aim of the study. The facts and basis of the study, risks and benefits anticipated, the confidentiality and voluntary nature of the study were demonstrated to the participants by the principal investigator.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We are grateful for all participants in this study and all staff helped in this study.
Contributor Information
Safaa Badi, Email: Safaabadi30@gmail.com.
Mohamed Izham Mohamed Ibrahim, Email: mohamedizham@qu.edu.qa.
Data availability
The video contents and datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Elmadhoun W.M., Noor S.K., Ibrahim A.A.A., Bushara S.O., Ahmed M.H. 2016. Prevalence of Diabetes Mellitus and its Risk Factors in Urban Communities of North Sudan : Population-Based Study. [DOI] [PubMed] [Google Scholar]
- 2.El-sayed E.F., et al. Diabetes & Metabolic Syndrome: Clinical Research & Reviews Sugar intake in Sudanese individuals was associated with some features of the metabolic syndrome: population based study. Diabetes Metab Syndr Clin Res Rev. 2017;3(12):1–6. doi: 10.1016/j.dsx.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Ali Y.A., Almobarak A.O., Awadalla H., Elmadhoun W.M., Ahmed M.H. Obesity among Sudanese adults with diabetes: a population-based survey. Ann Transl Med. 2017;5(12):1–8. doi: 10.21037/atm.2017.05.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Almobarak A.O., Awadalla H., Osman M., Ahmed M.H. Prevalence and predictive factors for heart failure among Sudanese individuals with diabetes: population based survey. 2018;2:1–8. [Google Scholar]
- 5.Almobarak A., Badi S., Elmadhoun W., Tahir H., Ahmed M. The prevalence and risk factors of stroke among Sudanese individuals with diabetes: cross-sectional survey. Brain Circ. 2020;6(1):26. doi: 10.4103/bc.bc_15_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Almobarak A.O., Elmak N., Sulaf I., Sulaiman A.A., Ahmed M.H., Diabetes complications in Sudanese individuals with type 2 diabetes : overlooked problems in sub-Saharan Africa?. Diabetes Metab Syndr Clin Res Rev. 11. Suppl 2, S1047–S1051. [DOI] [PubMed]
- 7.Elwali E.S., Almobarak A.O., Hassan M.A., Mahmooud A.A., Awadalla H., Ahmed M.H. Frequency of diabetic retinopathy and associated risk factors in Khartoum, Sudan: population based study. Int J Ophthalmol. 2017;10(6):948–954. doi: 10.18240/ijo.2017.06.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed M.H., Elwali E.S., Awadalla H., Almobarak A.O. The relationship between diabetic retinopathy and nephropathy in Sudanese adult with diabetes: population based study. Diabetes Metab Syndr Clin Res Rev. 2017;11:S333–S336. doi: 10.1016/j.dsx.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed M.H., Awadalla H., Elmadhoun W.M. Prevalence and risk factors for acute coronary syndrome among sudanese individuals with diabetes: a population- based study. 2017;8(5):184–189. doi: 10.14740/cr616w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stratton I.M., et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. Br Med J. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shareef J., Fernandes J., Samaga L. Evolving role of clinical pharmacist in the management of diabetes mellitus. Int J Res Med Sci. 2015;3(6):1305–1308. [Google Scholar]
- 12.Rang H.P., Ritter J.M., Flower R.J., Henderson G. 9th ed. Elsevier; London: 2018. Rang and Dales’s Pharmacology. [Google Scholar]
- 13.Diabetes A. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetesd2021. Diabetes Care. 2021;44(January):S111–S124. doi: 10.2337/dc21-S009. [DOI] [PubMed] [Google Scholar]
- 14.Leite R.G.O.F., et al. Effectiveness of non-pharmacological strategies in the management of type 2 diabetes in primary care: a protocol for a systematic review and network meta-analysis. BMJ Open. 2020;10(1):1–7. doi: 10.1136/bmjopen-2019-034481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franz M.J., Macleod J. Success of nutrition-therapy interventions in persons with type 2 diabetes: challenges and future directions. Diabetes, Metab Syndr Obes Targets Ther. 2018;11:265–270. doi: 10.2147/DMSO.S141952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pastors J.G., Warshaw H., Daly A., Franz M., Kulkarni K. The evidence for the effectiveness of medical nutrition therapy in diabetes management. Diabetes Care. 2002;25(3):608–613. doi: 10.2337/diacare.25.3.608. [DOI] [PubMed] [Google Scholar]
- 17.CDC . Centers for Disease Control and Prevention; 2018. Medical Nutrition Therapy | Reimbursement and Sustainability | DSMES Toolkit | Diabetes | CDC.https://www.cdc.gov/diabetes/dsmes-toolkit/reimbursement/medical-nutrition-therapy.html [Online]. Available: [Accessed: 26-Jun-2021] [Google Scholar]
- 18.Evert A.B., et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. 2019;42(5):731–754. doi: 10.2337/dci19-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson E.L., et al. Standards of medical care in diabetes—2020 abridged for primary care providers. Clin Diabetes. 2020;38(1):7. doi: 10.2337/cd20-as01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Franz M.J., Boucher J.L., Rutten-Ramos S., VanWormer J.J. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. J Acad Nutr Diet. 2015;115(9):1. doi: 10.1016/j.jand.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 21.Chapman A., et al. Psychological interventions for the management of glycemic and psychological outcomes of type 2 diabetes mellitus in China: a systematic review and meta-analyses of randomized controlled trials. Front Public Health. 2015;3(November):1. doi: 10.3389/fpubh.2015.00252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Royal college of nursing . Royal college of nursing; 2019. Self-Care.https://www.rcn.org.uk/clinical-topics/public-health [Online]. Available: [Accessed: 26-Jun-2021] [Google Scholar]
- 23.Fajriyah N., Firmanti T.A., Mufidah A., Septiana N.T. A diabetes self-management education/support (DSME/S) program in reference to the biological, psychological and social aspects of a patient with type 2 diabetes mellitus: a systematic review. J Ners. 2019;14(3):55–56. [Google Scholar]
- 24.Hendrie D., Miller T.R., Woodman R.J., Hoti K., Hughes J. Cost-effectiveness of reducing glycaemic episodes through community pharmacy management of patients with type 2 diabetes mellitus. J Prim Prev. 2014 Dec;35(6):439–449. doi: 10.1007/s10935-014-0368-x. [DOI] [PubMed] [Google Scholar]
- 25.Odgers-Jewell K., Ball L.E., Kelly J.T., Isenring E.A., Reidlinger D.P., Thomas R. Effectiveness of group-based self-management education for individuals with type 2 diabetes: a systematic review with meta-analyses and meta-regression. Diabet Med. 2017;34(8):1027–1039. doi: 10.1111/dme.13340. [DOI] [PubMed] [Google Scholar]
- 26.Abdalla E.A.M., Abdulraheem N.A., Mohammed A.A. Lifestyle patterns associated with overweight and obesity among adults in Jabra Area in Khartoum State - Sudan: a community based study. World Wide J Multidiscipl Ina Res Dev WWJMRD. 2016;2(12):21–24. [Google Scholar]
- 27.Misita C.P. Clinical pharmacists in outpatient diabetes care: essential members of the multidisciplinary team. Clin Diabetes. 2013;31(4):162–165. [Google Scholar]
- 28.Badi S., et al. The impact of clinical pharmacist diabetes education on medication adherence in patients with type 2 diabetes mellitus: an interventional study from Khartoum, Sudan. J Persnalized Med. 2024;14(47) doi: 10.3390/jpm14010074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Palain S.P., Chhetri A., Prabhu M., Rajan S. Role of pharmacist in counseling diabetes patients. Internet Aust J Pharm. 2024;4(1):5. [Google Scholar]
- 30.Shrivastava S.R.B.L., Shrivastava P.S., Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12(14) doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stämpfli D., Baumgartner P., Boeni F., Bedouch P., Lampert M.L., Hersberger K.E. Translation and validation of a tool to assess the impact of clinical pharmacists’ interventions. Int J Clin Pharmacol. 2019;41(1):56–64. doi: 10.1007/s11096-018-0755-0. [DOI] [PubMed] [Google Scholar]
- 32.Badi S., Suliman S.Z., Almahdi R., et al. The impact of diabetes education by clinical pharmacist on quality of life and treatment satisfaction of Sudanese individuals with type II diabetes mellitus: randomized, double-blind, controlled trial. J Prim Care Community Health. 2024;15 doi: 10.1177/21501319241279681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Badi S., Suliman S.Z., Almahdi R., et al. The impact of the clinical pharmacist-led diabetes education on the knowledge and attitude of individuals with type II diabetes mellitus: an interventional study. Pharm (Basel, Switzerland) 2024;12(5) doi: 10.3390/pharmacy12050151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farag O.E., et al. Knowledge and self-care activities among Sudanese individuals with diabetes: a cross sectional survey. J Hosp Manag Heal Policy. 2020;4(March):2. [Google Scholar]
- 35.Bukhsh A., et al. Association of diabetes-related self-care activities with glycemic control of patients with type 2 diabetes in Pakistan. Patient Prefer Adherence. 2018;12:2377–2385. doi: 10.2147/PPA.S177314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Balla S.A. Prevalence of diabetes, knowledge and attitude of rural population towards diabetes and hypoglycaemic event, Sudan 2013. Am J Heal Res. 2014;2(6):356. [Google Scholar]
- 37.Al Mazroui N.R., Kamal M.M., Ghabash N.M., Yacout T.A., Kole P.L., McElnay J.C. Influence of pharmaceutical care on health outcomes in patients with type 2 diabetes mellitus. Br J Clin Pharmacol. 2009;67(5):547–557. doi: 10.1111/j.1365-2125.2009.03391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bin Ahmed I., et al. Level of diabetic patients’ knowledge of diabetes mellitus, its complications and management in Saudi Arabia. Arch Pharma Pr. 2019;10(4):80–86. [Google Scholar]
- 39.Al-Maskari F., El-Sadig M., Al-Kaabi J.M., Afandi B., Nagelkerke N., Yeatts K.B. Knowledge, attitude and practices of diabetic patients in the United Arab Emirates. PloS One. 2013;8(1):1–8. doi: 10.1371/journal.pone.0052857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tabassum N.F., Himanandini N., Fathima M., Sankeerthna M., Vanjari N.K., Bandaru S.S. Effectiveness of clinical pharmacist directed-diabetes management. J Diabetes Mellit. 2019;9(3):137–145. [Google Scholar]
- 41.Mourão A.O.M., et al. Pharmaceutical care program for type 2 diabetes patients in Brazil: a randomised controlled trial. Int J Clin Pharmacol. 2013;35(1):79–86. doi: 10.1007/s11096-012-9710-7. [DOI] [PubMed] [Google Scholar]
- 42.George A.K., Jewel V.G., Manohar M., Kumar S.P., Muneerudeen J. Impact of patient counselling on knowledge, attitude, practices of patients with type 2 diabetes mellitus at a tertiary care teaching hospital. Asian J Pharm Clin Res. 2017;10(5):293–296. [Google Scholar]
- 43.Malathy R., Narmadha M.P., Ramesh S., Alvin J.M., Dinesh B.N. Effect of a diabetes counseling programme on knowledge, attitude and practice among diabetic patients in Erode district of South India. J Young Pharm. 2011;3(1):65–72. doi: 10.4103/0975-1483.76422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wishah R.A., Al-Khawaldeh O.A., Albsoul A.M. Impact of pharmaceutical care interventions on glycemic control and other health-related clinical outcomes in patients with type 2 diabetes: randomized controlled trial. Diabetes Metab Syndr Clin Res Rev. 2015;9(4):271–276. doi: 10.1016/j.dsx.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 45.Lim K., Lim Phei Ching. Evaluation of a pharmacist-managed diabetes medication therapy adherence clinic. Clin Pharm Pract. 2010;8(4):250–254. doi: 10.4321/s1886-36552010000400008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee X.Y., et al. Impact of pharmacist-managed diabetes medication therapy adherence clinic (DMTAC) in government health clinics. Malaysian J Pharm Sci. 2015;13(1):43–51. [Google Scholar]
- 47.Santschi V., Chiolero A., Paradis G., Colosimo A.L., Burnand B. Pharmacist interventions to improve cardiovascular disease risk factors in diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. 2012;35(12):2489–2497. doi: 10.2337/dc12-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Y., Yeo Q.Y., Ko Y., Lee J.Y. A systematic review and meta-analysis of pharmacist-led diabetes management programs on clinical outcomes and patients’ self-management. BMJ Open. 2020;10 [Google Scholar]
- 49.Cohen L.B., Taveira T.H., Khatana S.A.M., Dooley A.G., Pirraglia P.A., Wu W.C. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ. 2011;37(6):801–812. doi: 10.1177/0145721711423980. [DOI] [PubMed] [Google Scholar]
- 50.Chan C.W., Siu S.C., Wong C.K.W., Lee V.W.Y. A pharmacist care program: positive impact on cardiac risk in patients with type 2 diabetes. J Cardiovasc Pharmacol Ther. 2012;17(1):57–64. doi: 10.1177/1074248410396216. [DOI] [PubMed] [Google Scholar]
- 51.Farsaei S., Sabzghabaee A.M., Zargarzadeh A.H., Amini M. Effect of pharmacist-led patient education on glycemic control of type 2 diabetics: a randomized controlled trial. J Res Med Sci. 2011;16(1):43–49. [PMC free article] [PubMed] [Google Scholar]
- 52.Spencer-Bonilla G., et al. A systematic review and meta-analysis of trials of social network interventions in type 2 diabetes. BMJ Open. 2017;7(8):1–11. doi: 10.1136/bmjopen-2017-016506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Christy A., Fernanda F., Insani W.N., Abdulah R. Pharmacist-led digital health interventions for patients with diabetes: a systematic review. J Multidiscip Healthc. 2025 Jan 11;18:101–112. doi: 10.2147/JMDH.S494584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pringle J.L., Boyer A., Conklin M.H., McCullough J.W., Aldridge A. The Pennsylvania project: pharmacist intervention improved medication adherence and reduced health care costs. Health Aff (Millwood) 2014 Aug;33(8):1444–1452. doi: 10.1377/hlthaff.2013.1398. [PMID: 25092847] [DOI] [PubMed] [Google Scholar]
- 55.Zhu J., Zhou Y., Wang G. Cost-effectiveness of pharmacist care in diabetes management: a systematic review. Diabetes Ther. 2024 Jan;15(1):61–76. doi: 10.1007/s13300-023-01505-2. Epub 2023 Nov 14. PMID: 37957464; PMCID: PMC10786784.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bukhsh A., Khan T.M., Lee S.W.H., Lee L.H., Chan K.G., Goh B.H. Efficacy of pharmacist based diabetes educational interventions on clinical outcomes of adults with type 2 diabetes mellitus: a network meta-analysis. Front Pharmacol. 2018;9:339. doi: 10.3389/fphar.2018.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.David E.A., Soremekun R.O., Abah I.O., Aderemi-Williams R.I. Impact of pharmacist-led care on glycaemic control of patients with uncontrolled type 2 diabetes: a randomised controlled trial in Nigeria. Pharm Pract (Granada) 2021 Jul-Sep;19(3):2402. doi: 10.18549/PharmPract.2021.3.2402. Epub 2021 Aug 14. PMID: 34457094; PMCID: PMC8370187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mohamed E.I.E., Mohamed A.T.M., Ali H.G.E., Abd El Rahman R.M.M., Elgazzar S.E. Effect of structured educational program on diabetic patients’ knowledge, attitude, and practices regarding self-administration of insulin injection. Egypt. J Health Care. 2024 Jun;15(2):18. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The video contents and datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.