Abstract
Background
Short-term cold spells and heat events are commonly considered risk factors for cardiovascular disease (CVD). This study quantitatively examined the effects of country-specific "climate-patterned temperature" (TMP), measured as long-term mean temperature, on global CVD incidence.
Methods
Recently published country-specific data on CVD incidence and TMP were analysed for statistical correlations at the population level using Microsoft Excel and SPSS. Confounding effects of humidity, aging, GDP PPP, obesity prevalence, and urbanization were controlled. Fisher r-to-z transformation compared correlation coefficients.
Results
Pearson's r and nonparametric analyses revealed a significant inverse correlation between TMP and CVD incidence worldwide (r = −0.646 and −0.574, respectively, p < 0.001). This relationship remained significant after controlling for confounders in a partial correlation model (r = −0.584, p < 0.001). Multiple linear regression showed TMP as a significant and independent predictor of CVD incidence (Beta = −0.384, p < 0.001). Stepwise regression identified aging as the most influential factor (R2 = 0.591), with TMP and GDP PPP following, increasing R2 to 0.731 and 0.747, respectively. Humidity, obesity prevalence, and urbanization were not significant predictors. TMP had a stronger predictive effect on CVD incidence in high-income countries compared to low- and middle-income countries (z = 1.96 and 2.28 in Pearson's r and nonparametric models, respectively, p < 0.05).
Conclusions
Long-term lower mean temperature (TMP) is a significant and independent risk factor for CVD worldwide, particularly in developed countries. TMP should be considered in epidemiological studies of CVD.
Keywords: Cardiovascular disease incidence, Cold temperature, Climate-patterned temperature, Long-term pattern of mean value of temperature, Population health
Highlights
-
•
Lower average ambient temperatures link to higher rates of heart disease worldwide.
-
•
Cold climate impacts heart disease risk, even with lifestyle factors controlled.
-
•
Cold climates predict heart disease more strongly in wealthier countries.
-
•
Considering temperature can improve heart disease prevention in colder regions.
1. Introduction
Cardiovascular diseases (CVDs) are chronic conditions with lifelong implications, affecting the heart and blood vessels [1]. Globally, CVD caused 17.9 million deaths in 2019, marking a 24 % increase since 1990 [2]. CVD represents over 60 % of the lifetime risk for global morbidity and mortality [1]. Over the past three decades, CVD has rapidly emerged as the leading cause of mortality worldwide [2]. While numerous studies underscored the escalating burden of CVD on healthcare systems, some indicated an overall declining trend in global CVD incidence and mortality [3,4]. This emphasizes the urgent need for enhanced understanding and prevention of CVD, making it a crucial public health priority in both developed and developing countries [5].
CVDs have multiple aetiologies driving the worldwide increase of CVD incidence [6]. Therefore, approaches to diagnosing and preventing CVD which have traditionally focused on the assessment and treatment of lifelong key risk factors should also consider both genetic and environmental factors [6,7]. Family linkage studies have shown that CVD development involves strong genetic underpinnings [8]. It has been well-established that at a population level, ageing [9], urban living [10,11], obesity and overweight [[12], [13], [14]] and economic affluence [15,16] have been recognized as the major environmental risk factors for CVD.
It is well-known that variations in ambient temperature change have been associated with increased CVD mortality worldwide because of the human biological response to extremes of thermal environments [[17], [18], [19]]. The rationale for the associations is that ambient temperature change can cause blood vessels to contract or dilate which may lead to fluctuations in blood pressure [18,20], cardiac hypertrophy [20], increased blood viscosity [21], and subsequently CVDs [22,23]. A number of studies have examined the role of extreme temperatures in contributing to CVDs, for example coronary heart disease [24], ischemic heart disease [25], myocardial infarction [24], cerebrovascular disease [26], heart failure [25], stroke [24,25], and total CVDs [17,18].
Weather refers to short-term atmospheric conditions. Severe weather changes, such as heat waves and cold spells have adverse effects on human health, which have been extensively associated with CVD mortality at population level in a large body of research [[27], [28], [29], [30], [31], [32]]. For example, in the past decades, severe heat waves have shown significant impacts on excess mortality, such as incidents in Chicago (1995), France and broadly Europe (2003). In contrast, cold spells leading to large numbers of deaths have occurred in Czech Republic (1987) and Moscow (2006).
Meteorologically, climate-patterned temperature, indicated by the averaged temperature over a specific region for 30 years or more (TMP), reflects a temperature pattern aligned with the long-term climate features of the area. Compared to short-term weather changes, for example extreme heat and cold spells, TMP has not been systematically associated with CVD development. Given the complexity of CVD pathology, this study has identified a number of opportunities to reflect on biases in the existing research literature:
-
1.
Curiously, a large number of studies, rather than considering the total CVD impact, have focused on individual CVDs, such as coronary heart disease [24], myocardial infarction [24], cerebrovascular disease [26], heart failure [25], stroke [24,25] and their association with short-term temperature changes. These studies have provided more reliable and consistent data, recognizing potential variations in the temperature's impact on specific cardiovascular diseases (CVDs) and their temperature-dependent susceptibility. Nonetheless, each CVD demonstrated interconnections with other types of CVDs, representing comorbidities [33], which may lead to excessive incidence. As the cumulative incidence of total CVDs has consistently been documented at the population level [2] there is an opportunity to examine the impact of temperature on the comprehensive incidence of CVDs.
-
2.
Previous studies have tended to consider the impact of short periods of time such as days to weeks of temperature extremes without consideration of the impact of much longer durations of exposure [25], e.g. across decades. This may not have allowed the authors to explore if the long-term temperature (climatically patterned) had a predicting role in CVD morality or incidence.
-
3.
The associations between extreme temperature and CVDs have been examined within relatively small regions, with no study examining the relationship across-country environments [25,32]. Due to regional CVD variation, analyses of only small regions may restrict insight into the association between extreme temperature change and total CVD mortality [34].
-
4.
Previous studies have also not considered a range of major confounding factors when exploring the relationship between extreme temperature and CVD risk [4,25,35].
Moreover, the Earth's temperature has increased by an average of 0.06 °C per decade since 1850, with a more rapid rise observed in recent decades [36]. Concurrently, with the recent accelerated temperature increase, some studies have suggested an overall decline in both CVD incidence and CVD mortality worldwide [3,4]. These findings challenged the notion that global warming is a culprit in increasing modern disease burden, including CVD development.
Given the above potential study biases and challenges in explaining the temperature- CVD relationship in previous research, in this cross-sectional study it was hypothesized that countries with long-term patterns of lower mean temperature (TMP) had greater cardiovascular disease incidence rates. This hypothesis was examined through analysing the statistical correlation between TMP and total CVD incidence at population level. The well-established potential confounding factors for the TMP – CVD relationship, such as humidity, ageing, economic affluence, obesity and urban living were incorporated into the data analyses for exploring the independent and significant role of TMP in predicting CVD incidence.
2. Material and method
2.1. Data sources and selection
To analyze the role of TMP in determining CVD incidence worldwide, the statistical role of TMP in determining CVD incidence was analysed at three levels, i.e. confounded TMP-CVD correlation, independent role of TMP in determining CVD and revealing TMP as the second most influential factor for CVD incidence. The country level data published by several international organizations were captured for achieving these study goals in this ecological study. Referencing previous studies [37,38], the role of TMP in determining CVD incidence was examined with the following variables:
The dependent variable is the country specific CVD incidence rate. Published by the Institute for Health Metrics and Evaluation of the University of Washington [39,40], the estimate of CVD incidence rate is expressed as the number of newly diagnosed CVD cases per 100,000 in 2017. We could not include the ICD codes in our dataset for subsequent analysis because they are not provided by IHME when they published their CVD data.
The independent variable is the country specific long-term pattern of mean value of temperature (Celsius, average yearly temperature for 30 years, 1988–2017, TMP hereafter) [41,42]. For each country/population, TMP was downloaded from the World Bank Group Climate Change Knowledge Portal [41]. The average temperature for 30 years was then calculated. The rationale for capturing this independent variable is that, typically, meteorological science adopts the average of a temperature over a period of 30 years or more for indexing a genuine temperature pattern for a region [42].
CVDs encompass multiple aetiologies, involving risk factors such as smoking, obesity, blood pressure, serum lipids, fasting glucose, dietary pattern, physical activity, diabetes, age, and kidney dysfunction [43,44]. These factors may compete with low TMP in contributing to CVD incidence. Due to data availability constraints at the population level, not all relevant risk factors were accessible for our ecological study. A literature review identified some key variables recognized as significant CVD risk factors throughout the lifespan [45]. These were included in our data analyses as potential confounders.
-
1)
Humidity indexed with average annual precipitations for the same period (1988–2017) which was also used for calculating the climate-patterned temperature (TMP) [41].
The stress temperature threshold for CVD pathogenesis remains uncertain and likely varies across different regions, however can be considered alongside humidity [46]. For instance, stress temperature thresholds may become higher when humidity is lower, and vice versa [46]. In other words, the combination of effects of the specific sets of temperature and humidity may have different effects on CVD pathogeneses [46].
Published by the United Nations, an increasing average life expectancy may indicate a higher level of healthcare service, nutritional improvements and a decrease in infectious disease mortality. Individuals aged 65 or older are more susceptible to CVD diseases due to a reduced capacity for thermoregulation and low physiological tolerance to ambient temperature changes [9,48,49]. Additionally, elderly people are more likely to have developed pre-existing conditions of CVDs such as hypertension, diabetes mellitus, hyperlipidaemia and coronary artery disease and obesity [50]. Cold stressors may be worse for the elderly because of co-morbidities and lower capacity for adaptive responses to unfavourable external stimulus [17,51].
-
3)
GDP PPP expressed in per capita purchasing power parity (US dollars) in 2014 published by the World Bank [15,16].
GDP PPP as a major indicator of socioeconomic status determines not only people's access to primary healthcare services that include CVD screening [16,52], but also their affordability to maintain comfortable temperature ranges through access to heating and cooling technologies [53].
-
4)
Obesity prevalence rate (adult) in 2014 published by the WHO Global Health Observatory (GHO) [54].
Obesity prevalence indicates the percentage of population aged 18+ with BMI ≥30 kg/m2 [54]. Posing multifactorial health challenges, obesity contributes directly to CVD incidence, and indirectly contributes to CVD comorbidities, such as hypertension, type 2 diabetes, dyslipidaemia, and atherosclerosis in both adults and children [[12], [13], [14]].
-
5)
Urbanization is expressed with the percentage of a population living within urban areas in 2014, as published by the World Bank [15].
Urbanization often entails a high level of education and healthcare services, yet may also encourage poor lifestyle choices, such as lack of physical exercise and social engagement, more intake of less nutritional food, high levels of gluten and processed meats, salt, fat, sugar and alcohol and lower vegetable consumption. Urban lifestyle has been recognized as a complex risk factor for chronic diseases, including CVDs [10,11,55].
The World Bank Group maintains a powerful database including collections of time series data on a variety of topics, such as socioeconomics, health, climate and demography [56] with 217 geographic locations/territories contributing their data. For the purposes of this paper, regardless of the political independent sovereign, geographic location/territory is interchangeably called country or population [57].
Firstly, a list of 217 geographic country locations was downloaded and all the above 7 variables were matched against each country. We considered each country/population an individual study subject for each data analysis model. However, not all the geographic locations/territories provided information for all relevant variables in the World Bank database. Therefore, the numbers of countries/population included for our analyses may differ in the different data analysis models used.
The diagnosis of CVD as a health condition may be a consequence of delay in the presentation of risk factors. In other words, CVD presentation may only occur after a cumulative exposure to the risk factors, including the independent variable (TMP) and potential confounding variables (humidity, ageing, GDP PPP, obesity and urbanization). For instance, if a population is exposed to higher GDP PPP, CVD incidence in this population may not increase immediately, but over several years. Therefore, country specific data on ageing, GDP PPP, obesity and urbanization were backdated 3 years from 2017 to account for an accumulation of confounding effects on CVD incidence. To represent the potential influences of climate, the long-term climate pattern of temperature and concurrent humidity were then incorporated for data analyses.
2.2. Data analysis
To examine the statistical TMP-CVD relationship for illustrating the role of TMP in predicting CVD incidence, the analysis proceeded in 5 steps after referring to the previous studies authored by You et al. [[58], [59], [60]].
-
1)
Bing© was used to integrate countries and their respective TMPs into the world geographic map in Microsoft Excel® 2016, and each country was colour saturated depending on their TMP values. Intuitively, the TMPs of different countries can be visualised depending on the darkness of colour and their latitudes.
With the raw data, scatter plots were also prepared for exploring and visualizing the correlation between TMP and CVD incidence in Excel (Microsoft® 2016). Scatter plots allowed an observation of correlation between TMP and CVD incidence and an examination of the variable distributions and data quality, such as identifying any major outliers. In this study, Greenland was identified as an outlier (TMP = - 18.36 °C, CVD incidence = 1590.84 per 100,000) and was removed from the following data analyses.
Before running correlation analyses, all above 7 variables were log-transformed to reduce possible curvilinearity of regressions and data non-homoscedasticity due to their abnormal distributions. The TMPs in the Russian Federation (-3.92 °C) and Canada (-3.59 °C) were below zero. The negatives cannot be log-transformed for exploring the best fit trendline because logarithmic, polynomial and power trendlines could not be drawn and visualised. Therefore, 5 °C was added to TMP for each country for identifying the best trendline between TMP and CVD incidence.
-
2.
Bivariate correlations (Pearson's and nonparametric) were used to quantify the strength and direction of the correlations between all variables. This common approach cross-checks aligning correlations with a-priori data and allowed us to ensure data quality. This allowed us for example, to check if the potential confounding variables were properly chosen.
-
3.
Partial correlation of Pearson's moment-product correlation was performed to examine the correlation between TMP and CVD incidence while the competing variables (humidity, ageing, GDP PPP and urbanization) were kept statistically constant.
TMP was first incorporated as an independent variable for predicting CVD incidence while humidity, ageing, GDP PPP, obesity and urbanization were kept constant. Then, TMP was kept statistically constant to explore the independent predicting effects of humidity, ageing, GDP PPP, obesity and urbanization on CVD incidence respectively. This examined how much TMP can explain each independent variable influencing CVD incidence.
-
4
Standard multiple linear regression (enter model) was conducted to analyze the respective predictive effects of humidity, ageing, GDP PPP, obesity and urbanization on CVD incidence. Subsequently, stepwise linear regression was performed to select the predictor(s) having the best influencing effects on CVD incidence.
To see if and how much TMP affected the predicting effects of humidity, ageing, GDP PPP, obesity and urbanization on CVD incidence in both enter and stepwise models, TMP was added and omitted as one of predicting variables for both multiple linear regression analyses.
-
5.The 217 countries were also grouped by different classification criteria; exploring the regional relationships between TMP and CVD with Pearson's r and nonparametric tests:
-
a)The World Bank income classifications: high income, upper middle income, low-middle income and low income; In response to the WHO's estimate that 75 % of CVD deaths occur in low- and middle-income countries (LMIC) [2] these countries were combined for creating another country grouping. Pearson's r and nonparametric tests were conducted for exploring the correlation between TMP and CVD incidence. Fisher's r-to-z transformation was applied for comparing the bivariate correlations of TMP to CVD in LMIC and high-income countries.
-
b)The developed and developing countries defined with the United Nations' common practice [61]. As a further response to the above WHO statement, Fisher's r-to-z transformation was applied to compare the Pearson's r and nonparametric correlations between TMP and CVD incidence in developed countries and in the developing countries.
-
c)Countries with a strong contrast in geographic distributions of income levels and/or cultural backgrounds.
-
a)
We analysed these correlations in 8 country groupings: Asia Cooperation Dialogue (ACD) [62]; the Asia-Pacific Economic Cooperation (APEC) [63]; the Arab World [64], countries with English as the official language (informed through government websites), Latin America [65], Latin America and the Caribbean (LAC) [65], the Organisation for Economic Co-operation and Development (OECD) [66] and Southern African Development Community (SADC) [67].
Bivariate correlations (Pearson's r and nonparametric rho), Pearson's moment-product partial correlation and multiple linear regressions were performed with log-transformed data in SPSS v. 28 (Chicago Il USA) [68]. The significance was reported when p was below 0.05, but the stronger significance levels, such as p < 0.01 and p < 0.001 were also indicated in this study. Regression analysis criteria were set at probability of F to enter ≤0.05 and probability of F to remove ≥0.10.
3. Results
Fig. 1 showed that most of the countries with low TMP are located in Europe and North America with high latitudes (north). Worldwide, the lowest TMP was in Greenland (-18.36) which was 47.89 °C lower than highest TMP in Burkina Faso (29.53). Worldwide, the mean of CVD incidence rate was 19.52 (Fig. 1). Fig. 1 also showed that most LMICs are in warmer regions, while high-income countries are in colder areas.
Fig. 1.
The world map of patterned temperature (TMP) for all countries.
Data source & definition: Climatically temperature pattern (TMP), °C, average yearly temperature for 30 years, 1988–2017, the World Bank Group CCKP.Both variables were not log-transformed for correlation analysis.
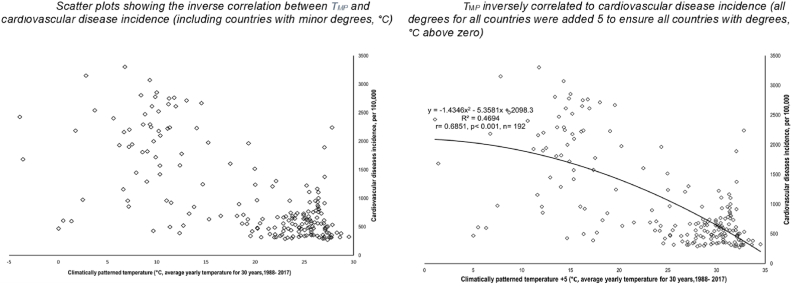
Fig. 2.1 and 2.2 revealed that, worldwide, TMP displayed a strong, negative, and significant correlation to CVD incidence rate. Both figures demonstrated that the TMP-CVD incidence relationship did not produce J-, V- or U-shaped trendlines. However, there appeared to be an outlier in the data which is Greenland (TMP = - 18.36 °C, CVD incidence = 1590.84 per 100,000, Fig. 2.1). After removing the outlier, the best fit TMP -CVD trendline was polynomial regression line (R2 = 0.4694 (r = − 0.6851), p < 0.001, n = 192, Fig. 2.2).
Fig. 2.
The relationship between temperature pattern (TMP, °C) and cardiovascular incidence rate.
Data source & definition: Climatically temperature pattern (TMP), °C, average yearly temperature for 30 years, 1988–2017, the World Bank Group CCKP; Cardiovascular disease (CVD) incidence rate (per 100,000) 2017, the Institute for Health Metrics and Evaluation. Both variables were not log-transformed for correlation analysis.
Table 1 showed that, worldwide, TMP was in a strong, negative and significant correlation to the variable of CVD incidence in both Pearson's r and nonparametric analyses (r = − 0.646, p < 0.001 and r = − 0.574, p < 0.001 respectively). Additionally, in both data analysis models, CVD incidence was significant and produced moderate to strong, positive correlations to ageing, GDP PPP, obesity and urbanization respectively (r range: 0.428–0.820, p < 0.001). However, humidity nearly showed nil correlation to CVD incidence. This suggested that humidity may not have a major role in determining the incidence of CVD.
Table 1.
Pearson's r and nonparametric correlation matrix between all variables.
| CVD incidence | Humidity | TMP | Ageing e [65] | GDP PPP | Obesity % | Urbanization | |
| CVD incidence | 1 | −0.014 | −0.646∗∗∗ | 0.764∗∗∗ | 0.734∗∗∗ | 0.428∗∗∗ | 0.526∗∗∗ |
| Humidity | −0.133 | 1 | 0.027 | 0.008 | −0.164∗ | −0.190∗∗∗ | −0.155∗ |
| TMP | −0.574∗∗∗ | 0.180∗∗∗ | 1 | −0.391∗∗∗ | −0.392∗∗∗ | −0.186∗ | −0.217∗∗∗ |
| Ageing e [65] | 0.782∗∗ | −0.061 | −0.399∗∗ | 1 | 0.811∗∗∗ | 0.362∗∗∗ | 0.556∗∗∗ |
| GDP PPP | 0.775∗∗∗ | −0.202∗∗∗ | −0.373∗∗∗ | 0.820∗∗∗ | 1 | 0.502∗∗∗ | 0.720∗∗∗ |
| Obesity % | 0.473∗∗∗ | −0.212∗∗ | −0.146∗∗ | 0.388∗∗∗ | 0.483∗∗∗ | 1 | 0.546∗∗∗ |
| Urbanization | 0.555∗∗∗ | −0.154∗ | −0.209∗∗∗ | 0.604∗∗∗ | 0.757∗∗∗ | 0.584∗∗∗ | 1 |
Pearson r (above diagonal) and nonparametric (below diagonal) correlations were reported.
Significance levels: ∗P < 0.05, ∗∗∗P < 0.001. Number of country range (sample size): 176–209.
Data source & definition: Climatically temperature pattern (TMP), °C, average yearly temperature for 30 years, 1988–2017, the World Bank Group CCKP; Cardiovascular disease (CVD) incidence rate (per 100,000) 2017, the Institute for Health Metrics and Evaluation; Ageing indexed with life expectancy at 65 year old in 2014, United Nations; Per capita GDP PPP, measured with the per capita purchasing power parity (PPP) value of all final goods and services produced within a territory in a given year, the World Bank 2014; Urbanization, measured with the percentage of population living in urban area, the World Bank 2014; Obesity prevalence, measured with the percentage of population aged 18+ with BMI equal to or over 30 kg/m2, the World Health Organization 2014. All data were log-transformed for correlation analysis.
Table 2 suggested that TMP is a significant risk factor for CVD incidence regardless of co-variates (humidity, ageing, GDP PPP, obesity and urbanization) influencing CVD incidence (r = 0.584, p < 0.001). However, when TMP was statistically kept constant, humidity, ageing, obesity and urbanization showed significant correlations to CVD incidence (r = 0.728, 0.685, 0.410 and 0.518 respectively, p < 0.001).
Table 2.
Partial correlations between cardiovascular disease incidence and independent variable when temperature pattern was included as the independent and confounder respectively.
| Variables | TMP partially correlated to CVDs | TMP kept constant statistically, other variables partially correlated to CVDs | ||||
| r | p | df | r | p | df | |
| TMP | −0.584 | <0.001 | 169 | – | – | – |
| Humidity | – | – | – | 0.728 | <0.001 | 189 |
| Ageing e [65] | – | – | – | 0.685 | <0.001 | 177 |
| GDP PPP | – | – | – | 0.004 | 0.952 | 189 |
| Obesity % | – | – | – | 0.410 | <0.001 | 177 |
| Urbanization | – | – | – | 0.518 | <0.001 | 189 |
All the data were log-transformed for correlation analysis.
- Included as the confounding factor.
Data source & definition: Climatically temperature pattern (TMP), °C, average yearly temperature for 30 years, 1988–2017, the World Bank Group CCKP; Cardiovascular disease (CVD) incidence rate (per 100,000) 2017, the Institute for Health Metrics and Evaluation; Ageing indexed with life expectancy at 65 year old in 2014, United Nations; Per capita GDP PPP, measured with the per capita purchasing power parity (PPP) value of all final goods and services produced within a territory in a given year, the World Bank 2014; Urbanization, measured with the percentage of population living in urban area, the World Bank 2014; Obesity prevalence, measured with the percentage of population aged 18+ with BMI equal to or over 30 kg/m2, the World Health Organization 2014.
Table 3 showed that when TMP was not added as a predicting variable in the multiple linear regression (enter), ageing and GDP PPP were the only two variables significantly influencing CVD incidence (Beta = 0.486 and 0.346 respectively). When TMP was added as a predicting variable, TMP, ageing and GDP PPP were the only 3 variables having a significant influence on CVD incidence (Beta = - 0.384, 0.410 and 0.235 respectively). Regardless of TMP being a predicting variable or not, humidity, obesity and urbanization showed very weak or almost no correlation to CVD incidence.
Table 3.
Multiple linear regression analyses sorting significant predictors of cardiovascular disease incidence.
| 3-1: ENTER | TMP not added | TMP added | |||
|---|---|---|---|---|---|
| Variables Entered | Beta | Sig. | Beta | Sig. | |
| TMP | Not applicable | Not applicable | −0.387 | <0.001 | |
| Ageing e [65] | 0.486 | <0.001 | 0.410 | <0.001 | |
| GDP PPP | 0.346 | <0.001 | 0.235 | <0.010 | |
| Humidity | 0.042 | 0.400 | 0.033 | 0.413 | |
| Obesity % | 0.080 | 0.165 | 0.077 | 0.106 | |
| Urbanization | −0.050 | 0.488 | −0.038 | 0.522 | |
| 3-2: STEPWISE | TMP not added | TMP added | |||
| Rank | Variables entered | Adjusted R square | Rank | Variables entered | Adjusted R square |
| 1 | Ageing e [65] | 0.591 | 1 | Ageing e [65] | 0.591 |
| 2 | GDP PPP | 0.626 | 2 | TMP | 0.731 |
| TMP | Not added | 3 | GDP PPP | 0.747 | |
| Humidity | Non-significant | Humidity | Non-significant | ||
| Obesity % | Non-significant | Obesity % | Non-significant | ||
| Urbanization | Non-significant | Urbanization | Non-significant | ||
Stepwise multiple linear regression modelling is reported. Contribution of variables is listed in order of how much they contribute to cardiovascular disease incidence.
All the data were log-transformed for correlation analysis.
Data source & definition: Climatically temperature pattern (TMP), °C, average yearly temperature for 30 years, 1988–2017, the World Bank Group CCKP; Cardiovascular disease (CVD) incidence rate (per 100,000) 2017, the Institute for Health Metrics and Evaluation; Ageing indexed with life expectancy at 65 year old in 2014, United Nations; Per capita GDP PPP, measured with the per capita purchasing power parity (PPP) value of all final goods and services produced within a territory in a given year, the World Bank 2014; Urbanization, measured with the percentage of population living in urban area, the World Bank 2014; Obesity prevalence, measured with the percentage of population aged 18+ with BMI equal to or over 30 kg/m2, the World Health Organization 2014.
In the subsequent multiple linear regression (stepwise), when TMP was not added as a predicting variable, ageing and GDP PPP were placed first and second most significant predicting variables for CVD incidence respectively (Table 2, Table 3). When TMP was added as a predicting variable, it was placed second to have the greatest influence on the CVD incidence (significantly increasing R2 from 0.591 to 0.731). Ageing and GDP PPP were placed first and third most influential predictors for CVD incidence (Table 2, Table 3).
In both enter and stepwise models, humidity, obesity and urbanization were weak predictors of CVD incidence.
Table 4 indicated that, in general TMP inversely correlated to CVD incidence in different country groupings, even when the strength of the correlation and significance levels varied. One of the highlights of the findings was that TMP retained a significantly stronger inverse correlation to CVD incidence in high-income countries compared to low- and middle-income countries (LMIC) (z = 1.96 and 2.28, p < 0.050 in Pearson's r and nonparametric respectively).
Table 4.
Temperature pattern (TMP) determined cardiovascular disease incidence in different country groupings.
| Country groupings | Pearson r | p | Nonparametric | p |
| Worldwide (n = 192) | −0.646∗∗ | <0.001 | −0.574∗∗ | <0.001 |
| World Bank income classifications | ||||
| High Income, n = 62 | −0.724∗∗ | <0.001 | −0.681∗∗ | <0.001 |
| Low Income, n = 28 | −0.395∗∗ | <0.050 | −0.361∗ | 0.059 |
| Low Middle Income, n = 48 | −0.419∗∗ | 0.050 | −0.343∗ | <0.050 |
| Upper Middle Income, n = 54 | −0.652∗∗ | <0.001 | −0.401∗∗ | <0.010 |
| Low- and middle-income countries (LMIC), n = 130 | −0.542∗∗ | <0.001 | −0.440∗∗ | <0.001 |
| Fisher r-to-z transformation | High vs LMIC: z = 1.96, p < 0.050 | High vs LMIC: z = 2.28, p < 0.050 | ||
| United Nations common practice | ||||
| Developed, n = 48 | −0.385∗∗ | 0.010 | −0.209 | 0.154 |
| Developing, n = 144 | −0.296∗∗ | <0.001 | −0.246∗∗ | <0.010 |
| Countries grouped with various factors | ||||
| English as Official Language, n = 51 | −0.561∗∗ | <0.001 | −0.131 | 0.358 |
| Asia-Pacific Economic Cooperation, n = 19 | −0.658∗∗ | <0.010 | −0.535∗ | <0.050 |
| Organisation for Economic Co-operation and Development, n = 37 | −0.519∗∗ | <0.001 | −0.328∗ | <0.050 |
| Arab World, n = 21 | −0.256 | 0.262 | −0.512∗ | <0.050 |
| Asia Cooperation Dialogue, n = 33 | −0.146 | 0.416 | −0.029 | 0.871 |
| Southern African Development Community, n = 16 | 0.021 | <0.050 | −0.041 | 0.880 |
| Latin America, n = 31 | −0.144 | 0.440 | −0.088 | 0.638 |
| Latin America and Caribbean, n = 34 | −0.295 | 0.090 | 0.172 | 0.331 |
All the data were log-transformed for correlation analysis.
Data source & definition: Climatically temperature pattern (TMP), °C, average yearly temperature for 30 years, 1988–2017, the World Bank Group CCKP; Cardiovascular disease (CVD) incidence rate (per 100,000) 2017, the Institute for Health Metrics and Evaluation.
4. Discussion
There has been much interest in examining the role of low temperature and increasing CVD incidence. Current literature suggests that short term cold temperatures (cold spells) have detrimental effects on CVDs in a number of studies [69,70]. With multiple data analysis models, our study uniquely suggested that low temperature had negative impact on CVD progenesis at three levels:
-
1.
Consistent with previous studies into the low temperature-CVD relationship, the inverse correlation between TMP and CVD incidence in this study suggested that countries with lower TMP may have higher CVD incidence rates.
-
2.
Low TMP independently predicted CVD incidence once the potential confounding effects of humidity, ageing, GDP PPP, obesity and urbanization on the low temperature-CVD relationship were removed from the model.
-
3.
Second to GDP PPP, TMP showed its significantly detrimental effects on CVD progenesis. Statistically, humidity, obesity and urbanization had insignificant or negligible influence on CVD pathogenesis.
In metrological science, "weather" refers to the short-term atmospheric conditions in a specific location, typically observed over a period of less than 30 years. Rapid low temperature changes (i.e. cold spells) have been extensively and almost unanimously postulated as a CVD risk factors due to increases of blood pressure [20,71], blood viscosity [21], platelet [21,71] and red cells counts [72]. It has also been associated with individual CVD types, such as cardiac hypertrophy [20]. However, a large majority of these studies were focused on revealing the risk of short-term low temperature conditions on different individual CVD types in specific locations. For example, the impact of winter temperatures on acute myocardial infarction and recurrent myocardial infarction was studied in Stockholm County, Sweden, from 1990 to 2002 [73]. Similarly, elevated cardiovascular disease risk factors, such as raised systolic blood pressure, were examined across 10 diverse regions in China between 2004 and 2008 [74].
In contrast, the independent variable in our study is the country-specific mean temperature value over 30 years (TMP). It was informed by the prevailing climate conditions of geographic location of each country, also called “climate-patterned temperature”. Our literature review showed that there has been no substantial research into the detrimental effects of long-term, low climate-patterned temperature on CVDs. As Earth's temperature has been on the rise over the past decades researchers have naturally focused on investigating the correlation between global warming and human health challenges, such as CVDs [75]. Arguably, CVD epidemiology studies have observed a global decrease in both CVD incidence and mortality [3,4]. This suggests a potential protective role of overall global warming in mitigating CVD pathogenesis. This suggestion is compatible with our study findings that countries with higher climate-patterned temperature may have lower CVD incidence rates.
Our analysis incorporated CVD incidence rate as the dependent variable, deviating from previous studies that predominantly used CVD mortality. CVD mortality, representing death due to CVDs, is an indicator of the adverse risk effects of cold temperature encompassing phases before diagnosis and subsequent clinical and non-clinical treatments. Mortality may not accurately predict the negative impact of cold temperature on CVD development, as the temperature-CVD relationship might be confounded by complex bio-psycho-social interventions which were associated with other important factors like economic status, urban advantages, and aging. However, these factors were often omitted in prior research. The inclusion of CVD incidence rate in our study offers a superior risk indicator, capturing new cases over a specified period for the population and less impacted by the complexities of pre-treatment or post-treatment effects.
Concerns have been raised about previous studies suggesting that low (cold) temperature might be seen as a precipitating factor rather than a long-term predisposing factor for CVDs [76]. Since CVDs often exhibit delayed onset, the impact of low temperature and other risk factors may take decades to manifest as symptomatic CVD. Previous studies often correlated mortality to CVD risk during periods of extremely cold temperatures, potentially missing the delayed effects. Liu, Yavar and Sun noted that deaths in such studies may result from the challenge of adapting to abrupt temperature drops rather than a pure "cold effect." This implies that individuals without a history of CVD or comorbidities are less likely to exhibit fatal effects from short-term cold temperatures [76]. Additionally, prior research lacked an exploration of the relationship between cold temperature and CVD mortality based on continuous variables. By investigating the TMP representing temperature pattern over a 30-year period (1988–2017) as a potential risk factor for CVDs, this was considered more representative of the accumulated and delayed effects of climate-patterned temperature (TMP) preceding any CVD incidence in 2017. The data analyses explored the statistical relationship between TMP and CVD incidence, challenging the notion that low temperature is merely a short-term precipitating factor.
We have comprehensively incorporated the impacts of global warming into our data analyses concerning the TMP-CVD relationship. It's crucial to recognize that global warming does not uniformly elevate temperatures in every country and at all times. The extent of warming varies geographically and temporally, with some countries experiencing significantly different patterns of temperature change [77,78].
Given prior research indicating more pronounced lagged effects in low temperatures, it is probable that the underestimation is more significant for cold conditions than for heat [[79], [80], [81], [82]]. This potential discrepancy is reflected in our scatter plots, demonstrating a non-linear TMP- CVD correlation without distinct platform or any J-, V-, or U-shaped patterns (Fig. 1). This may suggest that there was no threshold TMP worldwide, which is contrary to previous study findings [17,51,83,84]. Additionally, the shape of the trendline indicates a lack of bias in data quality. Furthermore, Earth's temperature has been rising due to global warming, coinciding with an overall decline in both CVD incidence and mortality worldwide [3,4]. This suggests that regional heatwaves may pose a significant risk for CVD mortality in limited areas for short periods. However, the risk from heatwaves may be minimal compared to the overall benefits of Earth's temperature increase for decreasing CVD mortality and incidence.
This study has provided a comprehensive analysis of a range of variables when exploring the correlation between TMP and CVD incidence rate. Adjustments for humidity, but also other well-established major confounders, such as ageing [50,52], GDP PPP [16,52,53], obesity [[12], [13], [14],52] and urban living [10,11,55] were made. In addition to the independent predicting effects of TMP on CVD incidence, simple and multiple regression were also applied to quantify the statistical explanation of TMP on CVD incidence. For instance, simple regression (scatter plots), revealed that, worldwide, TMP explained 46.94 % of CVD variance (R2 = 0.4694, Fig. 2.2). Multiple regression identified that TMP was placed the second most important variable increasing R2 to 0.731 (Table 2, Table 3). This suggested that TMP added 14 % of explanation for CVD incidence variation after ageing (59.1 %).
TMP was strongly correlated to CVD in high-income countries compared to LMIC. This showed that TMP may not be significant contributor to the WHO estimate that LMIC countries account for 75 % of CVD deaths worldwide [2]. The inverse correlation of TMP to CVD incidence was also observed in different country groupings. There is a growing interest in examining the different contributing effects of low temperature on CVDs in LMIC and high-income countries [2]. In this study, both the bivariate correlations (Pearson's r and non-parametric) revealed that TMP displayed a stronger correlation to CVD incidence in high-income countries compared to LMIC (z = 1.96 and 2.28, p < 0.050 respectively). This may be explained by emerging economies in LMIC over the past 30–40 years alleviating the detrimental effects of low TMP on CVD pathogenesis. For example, heating systems and access to better healthcare service has become more affordable and available to greater numbers of populations in LMIC countries.
5. Strengths and limitations
Our study uniquely contributes to the literature regarding the correlation between cold spells and CVDs.
-
1.
Instead of temporal temperature variations, “climate-patterned temperature” measured with long-term pattern of mean temperature value (30 years, TMP) has been correlated to CVD incidence [41,42]. This variable offers valuable insights into the long-term regional climate playing a crucial role in comprehending climate dynamics, evaluating the potential impacts of climate change, and making well-informed decisions in the field of public health such as CVDs.
-
2.
Almost all previous studies into the temperature-CVD relationship included CVD mortality rate as the dependent variable. However, CVD mortality as an end point measure may not be an accurate indicator of CVD development risk. By using CVD incidence to explore the temperature-CVD relationship instead of CVD mortality, we potentially increase the accuracy of our findings in this study relating to CVD development risk.
-
3.
The ecological study approach adopted in this study offered the advantage of incorporating more variables for data analysis compared to individual-based studies. Leveraging this, we included 5 potential confounding factors in our analyses to elucidate the independent role of TMP in predicting CVD incidence. While the variables explained a large majority of CVD variance (74.7 %), residual variance remains unexplained, constrained by data availability and quality, limiting the inclusion of additional variables in our analyses.
-
4.
Instead of referencing particular cities or other limited regions, this study quantified the worldwide role of climate-patterned temperature in determining CVD incidence risk depending on the potential confounding factors (humidity, ageing, GDP PPP, obesity and urbanization) and independent of these factors.
However, there are several important limitations to note.
-
1.
It is neither ethical nor logistically feasible to randomize populations to different levels of climate-patterned temperature (TMP), socioeconomic status, ageing, humidity, obesity and urbanization to determine which population would have greater CVD incidence rate. The nature of the study approach based on the population level cross-sectional dataset makes this subject to two intrinsic fallacies: 1) Correlation does not imply causation; 2) The correlations observed in this study may not necessarily hold true at an individual level.
However, this study has attempted to obtain accurate correlation between TMP and CVD incidence through accessing and incorporating more variables for analysing their intrinsic relationships. For instance, consideration of metrological science and incorporated long-term climate-patterned temperature (TMP), instead of short-term temperature changes as the independent variable. Additionally, several potential major confounding variables for analysing if and how much they affected the relationship between TMP and CVD incidence were considered.
-
2.
The data included in this study are the estimates of a broader population that cannot be entirely sampled. Therefore, the population level data published by IHME, WHO, United Nations and World Bank may be crude. Additioanlly, random errors may have been present in the collection and aggregation of the original data.
-
3.
The genetic background of CVD is significant and may heavily influence CVD incidence. However, due to data unavailability, the confounding effects of genetic background while we analysed the TMP- CVD incidence relationship could not be excluded.
-
4.
There are different sub-types of CVDs, and they may be affected by low temperature in different ways. We could not differentiate sub-types for analysis of their individual correlations to TMP.
6. Conclusion
This study suggested that low climate-patterned temperature (long-term pattern of low mean temperature, TMP) may be a significant and independent risk factor for CVD incidence worldwide. It also revealed that low TMP may be a more significant contributor for increasing CVD incidence rate in high-income countries. Thus, climate-patterned temperature should be incorporated for studying the effects of temperature on CVD prediction for optimal results.
CRediT authorship contribution statement
Wenpeng You: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. Jacob Sevastidis: Conceptualization, Formal analysis, Funding acquisition, Investigation, Resources, Validation, Visualization, Writing – review & editing. Frank Donnelly: Conceptualization, Funding acquisition, Investigation, Resources, Validation, Visualization, Writing – review & editing.
Ethics approval and consent to participate
All the variables incorporated into this study were freely extracted from the websites of international organizations, such as United Nation agencies and IHME. The whole set of the data involve the use of non-identifiable, pre-existing data about human beings. The individual person or their community cannot be traced as per the data. Therefore, they carry negligible ethical risk and there is no requirement for ethical approval or written informed consent from participation.
Availability of data and materials
All the data included in our data analyses are freely available from the United Nation agencies' online repositories which are open to the public. The data sources have been described in the section of “Materials and Methods”. There is no need to obtain formal permission to use the data for non-commercial purpose which is compliant with the agency's public permission in their terms and conditions.
Consent for publication
The authors approved the final manuscript for publishing.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgments
The authors express their appreciation to Ms Turi Christensen from the Institute for Health Metrics and Evaluation of the University of Washington for locating and downloading the data.
Handling editor: D Levy
List of abbreviations
- TMP
Climate-patterned temperature, calculated with long-term pattern of lower mean value of temperature for 30 years in this study
- CVD
Cardiovascular disease
- GDP PPP
Gross domestic product (purchasing power parity)
- Life e [65]
Life expectancy at 65 years old
- UN
United Nations
- WHO
World Health Organization
- IHME
Institute for Health Metrics and Evaluation of University of Washington
References
- 1.Mozaffarian D., Benjamin E.J., Go A.S., Arnett D.K., Blaha M.J., Cushman M., et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation (New York, N. Y.) 2016;133(4):e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.WHO. Cardiovascular Diseases (CVDs) 2021. [Google Scholar]
- 3.Amini M., Zayeri F., Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Public Health. 2021;21(1):1–12. doi: 10.1186/s12889-021-10429-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mensah G.A., Wei G.S., Sorlie P.D., Fine L.J., Rosenberg Y., Kaufmann P.G., et al. Decline in cardiovascular mortality: possible causes and implications. Circ. Res. 2017;120(2):366–380. doi: 10.1161/CIRCRESAHA.116.309115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roth G.A., Mensah G.A., Johnson C.O., Addolorato G., Ammirati E., Baddour L.M., et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vasan R.S., Benjamin E.J. The future of cardiovascular epidemiology. Circulation (New York, N. Y.) 2016;133(25):2626–2633. doi: 10.1161/CIRCULATIONAHA.116.023528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Said M.A., Verweij N., van der Harst P. Associations of combined genetic and lifestyle risks with incident cardiovascular disease and diabetes in the UK Biobank Study. JAMA Cardiol. 2018;3(8):693–702. doi: 10.1001/jamacardio.2018.1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vrablik M., Dlouha D., Todorovova V., Stefler D., Hubacek J.A. Genetics of cardiovascular disease: how far are we from personalized CVD risk prediction and management? Int. J. Mol. Sci. 2021;22(8):4182. doi: 10.3390/ijms22084182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NHS National health service: cardiovascular disease official website. 2022. https://www.nhs.uk/conditions/cardiovascular-disease/#:∼:text=age%20%E2%80%93%20CVD%20is%20most%20common,cholesterol%20and%20high%20blood%20pressure
- 10.You W., Henneberg M. Meat consumption providing a surplus energy in modern diet contributes to obesity prevalence: an ecological analysis. BMC Nutrition. 2016;2(1):1–11. [Google Scholar]
- 11.Smith S., Ralston J., Taubert K. The World Heart Federation; Geneva: 2012. Urbanization and Cardiovascular Disease- Raising Heart-Healthy Children in Today's Cities.https://world-heart-federation.org/wp-content/uploads/2017/05/FinalWHFUrbanizationLoResWeb.pdf [Available from: [Google Scholar]
- 12.Schwartz M.W., Seeley R.J., Zeltser L.M., Drewnowski A., Ravussin E., Redman L.M., et al. Obesity pathogenesis: an endocrine society scientific statement. Endocr. Rev. 2017;38(4):267–296. doi: 10.1210/er.2017-00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Unamuno X., Gómez‐Ambrosi J., Rodríguez A., Becerril S., Frühbeck G., Catalán V. Adipokine dysregulation and adipose tissue inflammation in human obesity. Eur. J. Clin. Invest. 2018;48(9) doi: 10.1111/eci.12997. [DOI] [PubMed] [Google Scholar]
- 14.Powell-Wiley T.M., Poirier P., Burke L.E., Després J.-P., Gordon-Larsen P., Lavie C.J., et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation (New York, N. Y.) 2021;143(21):e984–e1010. doi: 10.1161/CIR.0000000000000973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Bank. Indicators | Data 2018 [2 January 2018]. Available from: https://data.worldbank.org/indicator.
- 16.Gaziano T.A., Bitton A., Anand S., Abrahams-Gessel S., Murphy A. Growing epidemic of coronary heart disease in low-and middle-income countries. Curr. Probl. Cardiol. 2010;35(2):72–115. doi: 10.1016/j.cpcardiol.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen H., Zhang X. Influences of temperature and humidity on cardiovascular disease among adults 65 years and older in China. Front. Public Health. 2023;10 doi: 10.3389/fpubh.2022.1079722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh A., Mizdrak A., Daniel L., Blakely T., Baker E., Fleitas Alfonzo L., et al. Estimating cardiovascular health gains from eradicating indoor cold in Australia. Environ. Health. 2022;21(1):54. doi: 10.1186/s12940-022-00865-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woodward A. Heat, cold and climate change. J. Epidemiol. Community Health. 2014;68(7):595–596. doi: 10.1136/jech-2014-204040. [DOI] [PubMed] [Google Scholar]
- 20.Sun Z. Cardiovascular responses to cold exposure. Front. Biosci. Elite. 2010;2(2):495–503. doi: 10.2741/e108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goggins W.B., Chan E.Y., Yang C., Chong M. Associations between mortality and meteorological and pollutant variables during the cool season in two Asian cities with sub-tropical climates: Hong Kong and Taipei. Environ. Health. 2013;12(1):1–10. doi: 10.1186/1476-069X-12-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muntner P., Whittle J., Lynch A.I., Colantonio L.D., Simpson L.M., Einhorn P.T., et al. Visit-to-visit variability of blood pressure and coronary heart disease, stroke, heart failure, and mortality: a cohort study. Ann. Intern. Med. 2015;163(5):329–338. doi: 10.7326/M14-2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhai L., Ma X., Wang J., Luan G., Zhang H. Effects of ambient temperature on cardiovascular disease: a time-series analysis of 229288 deaths during 2009-2017 in Qingdao, China. Int. J. Environ. Health Res. 2022;32(1):181–190. doi: 10.1080/09603123.2020.1744532. [DOI] [PubMed] [Google Scholar]
- 24.Bai L., Li Q., Wang J., Lavigne E., Gasparrini A., Copes R., et al. Increased coronary heart disease and stroke hospitalisations from ambient temperatures in Ontario. Heart. 2018;104(8):673–679. doi: 10.1136/heartjnl-2017-311821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alahmad B., Khraishah H., Royé D., Vicedo-Cabrera A.M., Guo Y., Papatheodorou S.I., et al. Associations between extreme temperatures and cardiovascular cause-specific mortality: results from 27 countries. Circulation (New York, N. Y.) 2023;147(1):35–46. doi: 10.1161/CIRCULATIONAHA.122.061832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Y., Li S., Pan X., Tong S., Jaakkola J.J., Gasparrini A., et al. The effects of ambient temperature on cerebrovascular mortality: an epidemiologic study in four climatic zones in China. Environ. Health. 2014;13:1–12. doi: 10.1186/1476-069X-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stewart S., Keates A.K., Redfern A., McMurray J.J. Seasonal variations in cardiovascular disease. Nat. Rev. Cardiol. 2017;14(11):654–664. doi: 10.1038/nrcardio.2017.76. [DOI] [PubMed] [Google Scholar]
- 28.Moghadamnia M.T., Ardalan A., Mesdaghinia A., Keshtkar A., Naddafi K., Yekaninejad M.S. Ambient temperature and cardiovascular mortality: a systematic review and meta-analysis. PeerJ. 2017;5 doi: 10.7717/peerj.3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lu P., Xia G., Zhao Q., Xu R., Li S., Guo Y. Temporal trends of the association between ambient temperature and hospitalisations for cardiovascular diseases in Queensland, Australia from 1995 to 2016: a time-stratified case-crossover study. PLoS Med. 2020;17(7) doi: 10.1371/journal.pmed.1003176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peters A., Schneider A. Cardiovascular risks of climate change. Nat. Rev. Cardiol. 2021;18(1):1–2. doi: 10.1038/s41569-020-00473-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McMichael A.J. Globalization, climate change, and human health. N. Engl. J. Med. 2013;368(14):1335–1343. doi: 10.1056/NEJMra1109341. [DOI] [PubMed] [Google Scholar]
- 32.Yoneyama K., Nakai M., Higuma T., Teramoto K., Watanabe M., Kaihara T., et al. Weather temperature and the incidence of hospitalization for cardiovascular diseases in an aging society. Sci. Rep. 2021;11(1):1–11. doi: 10.1038/s41598-021-90352-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kendir C., van den Akker M., Vos R., Metsemakers J. Cardiovascular disease patients have increased risk for comorbidity: a cross-sectional study in The Netherlands. Eur. J. Gen. Pract. 2018;24(1):45–50. doi: 10.1080/13814788.2017.1398318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu J., Varghese B.M., Hansen A., Zhang Y., Driscoll T., Morgan G., et al. Heat exposure and cardiovascular health outcomes: a systematic review and meta-analysis. Lancet Planet. Health. 2022;6(6):e484–e495. doi: 10.1016/S2542-5196(22)00117-6. [DOI] [PubMed] [Google Scholar]
- 35.Achebak H., Devolder D., Ballester J. Trends in temperature-related age-specific and sex-specific mortality from cardiovascular diseases in Spain: a national time-series analysis. Lancet Planet. Health. 2019;3(7):e297–e306. doi: 10.1016/S2542-5196(19)30090-7. [DOI] [PubMed] [Google Scholar]
- 36.NOAA . Clim. Change: Global Temp. 2024. https://www.climate.gov/news-features/understanding-climate/climate-change-global-temperature#:∼:text=According%20to%20NOAA's%202023%20Annual,0.20%C2%B0%20C)%20per%20decade [Available from: [Accessed 24 December 2024] [Google Scholar]
- 37.You W., Henneberg M. 2022. Worldwide, Economic Affluence Was in Significantly Stronger Correlation to Obesity Prevalence Rate in Males than in Females. [Google Scholar]
- 38.You W., Feng S., Donnelly F. Total meat (flesh) supply may be a significant risk factor for cardiovascular diseases worldwide. Food Sci. Nutr. 2023;11(6):3203–3212. doi: 10.1002/fsn3.3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nichols E., Szoeke C.E., Vollset S.E., Abbasi N., Abd-Allah F., Abdela J., et al. Global, regional, and national burden of Alzheimer's disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(1):88–106. doi: 10.1016/S1474-4422(18)30403-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.IHME . Global Burden of Disease Study 2019 (GBD 2019) Results. Institute for Health Metrics and Evaluation (IHME); Seattle, United States: 2020. Global burden of disease collaborative network.http://ghdx.healthdata.org/gbd-results-tool [Google Scholar]
- 41.World Bank . The World Bank Group; 2021. Climate Change Knowledge Portal (CCKP): Average Yearly Temperature (1988-2017, Celsius)https://climateknowledgeportal.worldbank.org/ [Available from: [Google Scholar]
- 42.IPCC. Annex VII: Glossary. In: Matthews JBR, V , Möller R, van Diemen JS, Fuglestvedt V, Masson-Delmotte C, Méndez S, et al., editors. In Climate Change 2021: the Physical Science Basis Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change [Masson-Delmotte, V, P Zhai, A Pirani, SL Connors, C Péan, S Berger, N Caud, Y Chen, L Goldfarb, MI Gomis, M Huang, K Leitzell, E Lonnoy, JBR Matthews, TK Maycock, T Waterfield, O Yelekçi, R Yu, and B Zhou (eds)]. Cambridge University Press, Cambridge, United Kingdom and New York, NY, USA2021. p. 2215–2256.
- 43.Urtamo A., Jyväkorpi S.K., Kautiainen H., Pitkälä K.H., Strandberg T.E. Major cardiovascular disease (CVD) risk factors in midlife and extreme longevity. Aging Clin. Exp. Res. 2020;32:299–304. doi: 10.1007/s40520-019-01364-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bays H.E., Agarwala A., German C., Satish P., Iluyomade A., Dudum R., et al. Ten things to know about ten cardiovascular disease risk factors–2022. Am. J. Preventive Cardiol. 2022;10 doi: 10.1016/j.ajpc.2022.100342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burkart K.G., Brauer M., Aravkin A.Y., Godwin W.W., Hay S.I., He J., et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the Global Burden of Disease Study. Lancet. 2021;398(10301):685–697. doi: 10.1016/S0140-6736(21)01700-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Asseng S., Spänkuch D., Hernandez-Ochoa I.M., Laporta J. The upper temperature thresholds of life. Lancet Planet. Health. 2021;5(6):e378–e385. doi: 10.1016/S2542-5196(21)00079-6. [DOI] [PubMed] [Google Scholar]
- 47.United Nations . The 2017 Revision. DVD Edition. 2017. Department of economic and social affairs population division: world population prospects.https://population.un.org/wpp/Download/Standard/Mortality/ [Available from: [Google Scholar]
- 48.Fleg J.L., Strait J. Age-associated changes in cardiovascular structure and function: a fertile milieu for future disease. Heart Fail. Rev. 2012;17:545–554. doi: 10.1007/s10741-011-9270-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rodgers J.L., Jones J., Bolleddu S.I., Vanthenapalli S., Rodgers L.E., Shah K., et al. Cardiovascular risks associated with gender and aging. J. Cardiovascul. Dev. Dis. 2019;6(2):19. doi: 10.3390/jcdd6020019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vu A., Rutherford S., Phung D. Heat health prevention measures and adaptation in older populations—a systematic review. Int. J. Environ. Res. Publ. Health. 2019;16(22):4370. doi: 10.3390/ijerph16224370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klompmaker J.O., Laden F., James P., Sabath M.B., Wu X., Schwartz J., et al. Effects of long-term average temperature on cardiovascular disease hospitalizations in an American elderly population. Environ. Res. 2023;216 doi: 10.1016/j.envres.2022.114684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Levenson J.W., Skerrett P.J., Gaziano J.M. Reducing the global burden of cardiovascular disease: the role of risk factors. Prev. Cardiol. 2002;5(4):188–199. doi: 10.1111/j.1520-037x.2002.00564.x. [DOI] [PubMed] [Google Scholar]
- 53.Costello A., Abbas M., Allen A., Ball S., Bell S., Bellamy R., et al. Managing the health effects of climate change: lancet and university college London Institute for global health commission. Lancet. 2009;373(9676):1693–1733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 54.WHO Global Health Observatory . World Health Organization; 2022. The Data Repository.http://www.who.int/gho/database/en/ [Available from: [Google Scholar]
- 55.Diet W.H.O. vol.916. WHO technical report series; Geneva: 2003. (Nutrition and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation). [Google Scholar]
- 56.World Bank . The World Bank Group, © 2016; 2017. https://data.worldbank.org/indicator/SP.DYN.TFRT (Fertility Rate, Total (Births Per Woman)). [Google Scholar]
- 57.World Bank . The World Bank; 2022. https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries (How Does the World Bank Classify Countries?). [Google Scholar]
- 58.You W., Donnelly F. Physician care access plays a significant role in extending global and regional life expectancy. Eur. J. Intern. Med. 2022;(103):62–68. doi: 10.1016/j.ejim.2022.06.006. [DOI] [PubMed] [Google Scholar]
- 59.You W., Henneberg R., Henneberg M. Healthcare services relaxing natural selection may contribute to increase of dementia incidence. Sci. Rep. 2022;12(1):1–10. doi: 10.1038/s41598-022-12678-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.You W., Henneberg R., Henneberg M. Advanced healthcare services leading to relax natural selection may have been contributing to global and regional increase of dementia incidence. Res. Square. 2021 Version 1. [Google Scholar]
- 61.United Nations Statistics Division Composition of macro geographical (continental) regions, geographical sub-regions, and selected economic and other groupings: United Nations. 2013. http://unstats.un.org [Available from:
- 62.Asia Cooperation Dialogue Member countries. 2018. http://www.acddialogue.com
- 63.Asia-Pacific Economic Cooperation Member economies-asia-pacific economic cooperation. 2015. http://www.apec.org
- 64.World Bank . The World Bank; 2015. http://data.worldbank.org/region/ARB (Arab World | Data). [Google Scholar]
- 65.The United Nations Educational Scientific and Cultural Organization. UNESCO Regions-Latin America and the Caribbean; 2022. http://www.unesco.org [Google Scholar]
- 66.OECD List of OECD member countries. 2015. http://www.oecd.org
- 67.South Africa Development Community Southern African development community: member states. 2015. http://www.sadc.int
- 68.You W., Donnelly F. Although in shortage, nursing workforce is still a significant contributor to life expectancy at birth. Public Health Nurs. 2022;40(2):229–242. doi: 10.1111/phn.13158. [DOI] [PubMed] [Google Scholar]
- 69.Fan J.-F., Xiao Y.-C., Feng Y.-F., Niu L.-Y., Tan X., Sun J.-C., et al. A systematic review and meta-analysis of cold exposure and cardiovascular disease outcomes. Front. Cardiovasc. Med. 2023;10 doi: 10.3389/fcvm.2023.1084611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ryti N.R., Mäkikyrö E.M., Antikainen H., Hookana E., Junttila M.J., Ikäheimo T.M., et al. Risk of sudden cardiac death in relation to season-specific cold spells: a case–crossover study in Finland. BMJ Open. 2017;7(11) doi: 10.1136/bmjopen-2017-017398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Eldwood P., Beswick A., O'Brien J.R., Renaud S., Fifield R., Limb E., et al. Temperature and risk factors for ischaemic heart disease in the Caerphilly prospective study. Heart. 1993;70(6):520–523. doi: 10.1136/hrt.70.6.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Keatinge W., Coleshaw S., Cotter F., Mattock M., Murphy M., Chelliah R. Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombosis in winter. Br. Med. J. (Clin. Res. Ed.) 1984;289(6456):1405–1408. doi: 10.1136/bmj.289.6456.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rocklöv J., Forsberg B., Ebi K., Bellander T. Susceptibility to mortality related to temperature and heat and cold wave duration in the population of Stockholm County, Sweden. Glob. Health Action. 2014;7(1) doi: 10.3402/gha.v7.22737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yang L., Li L., Lewington S., Guo Y., Sherliker P., Bian Z., et al. Outdoor temperature, blood pressure, and cardiovascular disease mortality among 23 000 individuals with diagnosed cardiovascular diseases from China. Eur. Heart J. 2015;36(19):1178–1185. doi: 10.1093/eurheartj/ehv023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Aitken W.W., Brown S.C., Comellas A.P. Climate change and cardiovascular health. J. Am. Heart Assoc. 2022;11(24) doi: 10.1161/JAHA.122.027847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu C., Yavar Z., Sun Q. Cardiovascular response to thermoregulatory challenges. Am. J. Physiol. Heart Circ. Physiol. 2015;309(11):H1793–H1812. doi: 10.1152/ajpheart.00199.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.NASA World of change: global temperatures. 2022. https://earthobservatory.nasa.gov/world-of-change/global-temperatures
- 78.Huntingford C., Jones P.D., Livina V.N., Lenton T.M., Cox P.M. No increase in global temperature variability despite changing regional patterns. Nature. 2013;500(7462):327–330. doi: 10.1038/nature12310. [DOI] [PubMed] [Google Scholar]
- 79.Rocklöv J., Forsberg B. The effect of temperature on mortality in Stockholm 1998—2003: a study of lag structures and heatwave effects. Scand. J. Publ. Health. 2008;36(5):516–523. doi: 10.1177/1403494807088458. [DOI] [PubMed] [Google Scholar]
- 80.Dang T.N., Seposo X.T., Duc N.H.C., Thang T.B., An D.D., Hang L.T.M., et al. Characterizing the relationship between temperature and mortality in tropical and subtropical cities: a distributed lag non-linear model analysis in Hue, Viet Nam, 2009–2013. Glob. Health Action. 2016;9(1) doi: 10.3402/gha.v9.28738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yang J., Ou C.-Q., Ding Y., Zhou Y.-X., Chen P.-Y. Daily temperature and mortality: a study of distributed lag non-linear effect and effect modification in Guangzhou. Environ. Health. 2012;11(1):1–9. doi: 10.1186/1476-069X-11-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bao J., Wang Z., Yu C., Li X. The influence of temperature on mortality and its Lag effect: a study in four Chinese cities with different latitudes. BMC Public Health. 2016;16:1–8. doi: 10.1186/s12889-016-3031-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hashizume M., Wagatsuma Y., Hayashi T., Saha S.K., Streatfield K., Yunus M. The effect of temperature on mortality in rural Bangladesh—a population-based time-series study. Int. J. Epidemiol. 2009;38(6):1689–1697. doi: 10.1093/ije/dyn376. [DOI] [PubMed] [Google Scholar]
- 84.Chung J.-Y., Honda Y., Hong Y.-C., Pan X.-C., Guo Y.-L., Kim H. Ambient temperature and mortality: an international study in four capital cities of East Asia. Sci. Total Environ. 2009;408(2):390–396. doi: 10.1016/j.scitotenv.2009.09.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data included in our data analyses are freely available from the United Nation agencies' online repositories which are open to the public. The data sources have been described in the section of “Materials and Methods”. There is no need to obtain formal permission to use the data for non-commercial purpose which is compliant with the agency's public permission in their terms and conditions.