Abstract
Background:
Lesbian, gay, bisexual, transgender, queer, intersex, aromantic and asexual (LGBTQIA+) communities in the United States experience higher rates of alcohol use than the general population. While experiencing intimate partner violence (IPV) is thought to lead to increased alcohol use in LGBTQIA+ people, little research has investigated the temporal relationship between IPV and alcohol use in this population.
Methods:
Data from two annual questionnaires of The Population Research in Identity and Disparities for Equality Study (The PRIDE Study) longitudinal cohort (n=3,783) were included. Overall IPV and three sub-types (physical, sexual, and emotional) - measured in 2021 using the extended Hurt, Insult, Threaten, Scream (E-HITS) screening tool - was examined as a predictor of Alcohol Use Disorders Identification Test (AUDIT) score in 2022 using multivariable linear regression to assess linear and quadratic associations. Models were adjusted for sociodemographic characteristics and history of alcohol use.
Results:
One-quarter (24.7%) of respondents reported experiencing past-year IPV in 2021. The mean AUDIT score in 2022 was 3.52 (SD = 4.13). In adjusted models, both linear (B: 0.26, 95% CI: 0.14, 0.38) and quadratic (B: −0.03, 95% CI: −0.04, −0.01) terms for overall IPV were significantly associated with next-year AUDIT score. These patterns were mirrored in each IPV sub-type, were not attenuated when accounting for relationship characteristics, and were heterogeneous across gender identity groups.
Conclusions:
These results provide evidence of a temporal relationship between IPV and alcohol use in LGBTQIA+ communities, suggesting that efforts to prevent and mitigate IPV may help reduce alcohol use disparities in this population.
Keywords: Intimate partner violence, Alcohol use, Sexual and gender minority people, LGBTQIA+, PRIDE study
1. Introduction
Intimate partner violence (IPV) is a significant public health issue in lesbian, gay, bisexual, transgender, queer or questioning, intersex, aromatic and asexual (LGBTQIA+) communities in the United States (US; Whitfield et al., 2021). Defined as any action within a romantic relationship that causes physical, sexual, or emotional harm, as many as 61.1% of sexual minority women and 37.3% of sexual minority men in the US have experienced IPV, compared to 35% and 29% of heterosexual women and men, respectively (Leemis et al., 2022). Moreover, findings from a recent systematic review and meta-analysis show transgender people are more than twice as likely to experience IPV than their heterosexual, cisgender counterparts (Peitzmeier et al., 2020). To address this disproportionate public health burden, the US White House released its first National Action Plan to End Gender-based Violence in 2023, which calls for more research into the health impacts of IPV specifically in these communities to develop novel interventions tailored to LGBTQIA+ relationships (The White House, 2023).
Minority stress is thought to be a significant driver of negative health outcomes (including IPV) in LGBTQIA+ populations (Decker et al., 2018; Edwards et al., 2015; Swann et al., 2022). The Minority Stress Model posits that health disparities among LGBTQIA+ people exist in part due to the stress from navigating discrimination, prejudice, and stigma experienced due to their minority identity (Brooks, 1981; Hendricks and Testa, 2012; Meyer and Frost, 2013; Meyer, 2003). In response to the excess proximal (e.g., internalized homo- and trans-negativity) and distal (e.g., hate crimes, discrimination) stress of existing as an LGBTQIA+ person in a society dominated by cisgender, heterosexual men (i.e., cisheteropatriarchy), LGBTQIA+ people may use substances such as alcohol to cope (Flentje et al., 2020). Among potential stress-response behaviors, alcohol use is one of the most widely researched behaviors, and evidence indicates a disproportionately high rate of alcohol use and binge drinking among LGBTQIA+ communities (Dyar et al., 2020; Gosling et al., 2022; Hatzenbuehler, 2009; Hoy-Ellis, 2023; Lee et al., 2016; Wolfe et al., 2021). LGBTQIA+ adults are also significantly more likely to be diagnosed with an alcohol use disorder than their cisgender, heterosexual counterparts (Hughto et al., 2021; Krueger et al., 2020). Some LGBTQIA+ people may adopt alcohol use to self-manage other effects of minority stress, such as depressive symptoms (Tebbe and Budge, 2022).
Despite LGBTQIA+ people having both high rates of alcohol use and IPV, little research has investigated the temporal relationship between IPV and alcohol use in these populations. IPV is often found to be associated with alcohol use in specific LGBTQIA+ subgroups (e.g., cisgender sexual minority men, cisgender sexual minority women; Basting et al., 2023; Davis et al., 2016; Kimmes et al., 2019; King et al., 2022), but current knowledge of the role that IPV plays in alcohol use among LGBTQIA+ people is limited by cross-sectional designs and a preponderance of evidence focusing on cisgender men who have sex with men (Kim and Schmuhl, 2021; Porsch et al., 2022). A broader limitation within the IPV literature is the binary way in which IPV is commonly analyzed, especially in sexual and gender minority communities (Follingstad and Ryan, 2013; Smith et al., 2015). Previous research recommends modeling changes in substance use as both a constant process (i. e., a linear relationship) as well as one that includes gradual acceleration or deceleration in use (i.e., a curvilinear relationship) to capture the complex and dynamic aspects of both violence and substance use (Ahmadabadi et al., 2019; Brown et al., 2009; Cafferky et al., 2018), but the more nuanced effect of the continuum of IPV experiences remains largely unexplored in LGBTQIA+ people. Together, these issues pre-clude researchers from drawing causal inferences and developing effective, evidence-informed interventions for alcohol use for LGBTQIA+ communities that are inclusive of theeffects their relationship experiences may have on their substance use behaviors.
While we know of no studies examining the temporal relationship between IPV and increases in alcohol use in LGBTQIA+ people, substantial evidence finds that experiencing IPV leads to increased alcohol use among cisgender women in relationships with cisgender men (La Flair et al., 2012; Ogden et al., 2022). Feminist examinations of these results find that likely mechanisms for increased alcohol use include structural factors such as gender inequality and coping from the stress of abuse. Given similar structural forces through which oppression moves in queer communities (i.e., minority stress), even despite different interpersonal factors within these relationships compared to heterosexual ones, LGBTQIA+ couples may turn to alcohol to self-manage the effects of minority stress and IPV (Stubbs and Szoeke, 2022; White et al., 2023).
The purpose of this study was to identify the temporal relationships between IPV experiences among LGBTQIA+ people and subsequent alcohol use. We hypothesize that LGBTQIA+ people who report past-year IPV will have higher rates of alcohol use in the subsequent year and that the frequency of violence will have a dose-response effect across LGBTQIA+ communities. This may begin to illustrate the role of IPV in alcohol use disparities among LGBTQIA+ people, add more rigorous evidence on which to build effective interventions for the reduction of substance use in LGBTQIA+ communities broadly, and contribute to the successful completion of the US National Action Plan to reduce IPV.
2. Methods
2.1. Study design and participants
The PRIDE Study (www.pridestudy.org) is a community-engaged, prospective, online cohort study of LGBTQIA+ adults, described previously (Lunn, Capriotti, et al., 2019; Lunn, Lubensky, et al., 2019). Briefly, The PRIDE Study began recruitment in 2017 through LGBTQIA+ community events, partners, organizations, and social media. Eligible participants had to be age ≥18 years, reside in the US or its territories, identify as LGBTQIA+ or another gender and/or sexual minority person, and be comfortable with reading and understanding English. All participants provided informed consent through the web-based portal. Upon enrollment, participants are invited to complete the lifetime and current annual health and experiences questionnaire with annual invitations to complete subsequent annual questionnaires. For this study, we included participants who completed the 2021 (administered July 2021-May 2022) and 2022 (administered June 2022-May 2023) annual questionnaires (The PRIDE Study, 2024), hereafter referred to by the year that their administration began. The PRIDE Study was approved by the [BLINDED FOR REVIEW] Institutional Review Boards.
2.2. Exposures
The primary exposure is the Extended-Hurt, Insulted, Threaten, Scream (E-HITS) (Chan et al., 2010; Iverson et al., 2015) scale reported in the 2021 annual questionnaire. The E-HITS is a 5-item screening tool that assesses for past-year IPV by asking participants: “Over the last 12 months, how often did your partner: (1) physically hurt you?, (2) insult you or talk down to you?, (3) threaten you with harm?, (4) scream or curse at you?, and (5) force you to have sexual activities?” Responses are scored on a 5-point scale (1 = never to 5 = frequently), resulting in summed score ranging from 5 to 25 (Cronbach’s alpha = 0.71). We classified the E-HITS items into three subtypes which measured physical (items 1 and 3), sexual (item 5), and emotional (items 2 and 4) past-year IPV. The total scores for physical and emotional IPV ranged from 2 to 10. While E-HITS subscales have not been formally validated, previous psychometric data using cisgender, female participants found no statistical differences between the sensitivity and specificity of the E-HITS compared to the ‘gold standard’ Conflict Tactics Scale-2 in detecting IPV overall or its sub-types, providing preliminary justification for using the E-HITS to screen for IPV typology (Iverson et al., 2015).
2.3. Outcome
The main outcome of interest is the Alcohol Use Disorders Identification Test (AUDIT) (Saunders et al., 1993) scale reported in the 2022 annual questionnaire. The AUDIT is a 10-item screening tool that assesses the level of alcohol consumption and dependence in the past year. Items for the AUDIT include the quantity and frequency of drinking and heavy drinking (items 1–3); impaired control over drinking, increased salience of drinking, and morning drinking (items 4–6); and resulting problems from alcohol, such as guilt after drinking, blackouts, alcohol-related injuries, and whether others are concerned about the participant’s drinking (items 7–10). Participants respond to each item on a 5-point scale (0 = Never to 4 = Daily or almost daily), except for items 9 and 10 which are scored with values of 0 (No), 2 (Yes, but not in the past year), and 4 (Yes, during the last year). The total scores range from 0 to 40 (Cronbach’s alpha = 0.78).
2.4. History of alcohol use
We used two self-reported measures from the 2021 annual questionnaire to assess history of alcohol use: past-year alcohol use and alcohol use disorder. Participants are asked “How often did you have a drink containing alcohol in the PAST YEAR?” Responses were based on an ordinal scale from “Never” (0) to “4 or more times a week” (4). We dichotomized past-year alcohol use as any or never. Baseline alcohol use disorder was identified using the following question: “Do you currently have any of the following conditions that have been diagnosed by a health care provider?” Participants who selected “Alcoholism or Alcohol Use Disorder” were categorized to have experienced alcohol use disorder at baseline.
2.5. Relationship variables
Questions on participants’ current relationship status were obtained in the 2021 annual questionnaire. Participants were asked the following question: “Are you currently in a relationship?” Those who answered “yes” were asked about their general satisfaction with their current romantic relationships: “In general, how satisfied are you with your current romantic relationship(s)?” Responses were on a 5-point Likert scale, ranging from 0 (Very dissatisfied) to 4 (Very satisfied).
2.6. Socio-demographics
We included the following socio-demographic characteristics in our analysis from the 2021 questionnaire: age (continuous), ethnoracial identity with the option to select multiple responses (American Indian or Alaska Native; Asian; Black, African American or African; Hispanic, Latino, or Spanish; Middle Eastern or North African; Native Hawaiian or other Pacific Islander; White; and Another), education level (high school or less, some college, 4-year degree, master’s degree, and doctorate/professional degree), employment (yes/no), individual income ($0–20,000, $20,001–50,000, $50,001–100,000, and $100,001+), and Census region (Northeast, Midwest, South, and West). Gender identity was assessed using a question “What is your current gender identity?” with the option to select multiple responses (agender, cisgender man, cisgender woman, genderqueer, man, non-binary, questioning, transgender man, transgender woman, Two-spirit, woman, and another write-in response). We then used a two-step procedure (Tate, Ledbetter and Youssef, 2013) to cross-classify participants’ responses to gender identity and sex assigned at birth (female or male) into the following gender groups: cisgender men, cisgender women, gender diverse individuals assigned female at birth, gender diverse individuals assigned male at birth, transgender men, and transgender women. Sexual orientation was assessed using a question “What is your current sexual orientation” with the option to select multiple responses (asexual, bisexual, gay, lesbian, pansexual, queer questioning, same-gender loving, heterosexual, Two-spirit, and another write-in response. These responses were grouped into the following categories: asexual, bisexual, gay or lesbian, pansexual, queer, heterosexual, multiple options selected, or endorsed only another sexual orientation, same-gender loving, or questioning.
2.7. Statistical analysis
We first described key participant characteristics for the overall sample using descriptive statistics. To assess associations between past-year IPV in 2021 and subsequent AUDIT scores reported in 2022 annual questionnaire, we fitted separate linear regression models for each exposure and used a sandwich estimator to obtain robust standard errors. To test our hypothesis regarding the association of IPV frequency on alcohol use, IPV was modeled as both linear and quadratic terms. The best fitting models were determined using the likelihood ratio test comparing linear and quadratic models. Adjusted models accounted for age, gender groups, sexual orientation groups, education, employment, individual income, history of alcohol use, and Census region. To improve model fit, we mean-centered overall E-HITS and its subtypes. Socio-demographics and history of alcohol use of participants who were excluded due to missing E-HITS or AUDIT are reported in Supplemental Table 1. Among the analytic sample, missing data for covariates ranged between 0.03% (education level or employment) and 1.9% (past-year alcohol use), which was accounted for using multiple imputation by chained equations. Using the mice package (van Buuren and Groothuis-Oudshoorn, 2011), we generated and pooled across 20 imputed data sets to obtain a single estimate and 95% confidence interval (CI).
While currently being in a relationship was not a prerequisite for inclusion in the analysis, relationship status is an important marker of IPV; those currently in a relationship were more likely to report IPV and more severe forms of IPV than those who were not currently in a relationship (Carvalho et al., 2011; Sutton and Dawson, 2021). We conducted a sensitivity analysis by restricting the sample to those who reported currently being in a relationship and included relationship satisfaction as a covariate in these models. There may be important gender differences in IPV victimization and how it is associated with alcohol use within the LGBTQIA+ community (Caldwell et al., 2012; Reuter et al., 2017), but limited research has focused on these differences (Scott et al., 2023). Thus, we stratified our results by the gender groups mentioned above. We used R version 4.2.1 to perform all analyses (R Core Team, 2022). Interpretation of the data is based on an evaluation of magnitude, direction, and precision of the observed associations. Therefore, some significant results include zero due to rounding
3. Results
A total of 4495 participants initiated both the 2021 and 2022 annual questionnaires. Of these, we included all individuals who self-reported their gender identity and sexual orientation (n = 4488). We excluded 705 participants with any missing E-HITS or AUDIT items. Distribution of socio-demographics and history of alcohol use were similar between included participants and those excluded due to missing E-HITS and AUDIT items (Supplemental Table 1). However, a higher proportion of excluded participants had missing values for education level, employment, income, and past-year alcohol use, and a lower proportion identified as White. The final analytic sample for this analysis was 3783.
Sample characteristics are summarized in Table 1. The mean current age was 39.1 years (standard deviation [SD] = 14.9). Approximately 49% of participants were transgender or gender diverse, and 47% endorsed multiple sexual orientations. Most participants (92%) identified as White, which included 3107 people who only reported White (82.1% of sample) and 371 participants who selected White in addition to another ethnoracial identity (9.8% of sample). Participants predominately reported having at least a four-year college degree (78%) and being currently employed (73%); however, 58% reported an individual income of less than $50,000. Participants were also geographically diverse with a higher proportion of individuals currently residing in the Pacific region (33%). Two-thirds (66%) reported currently being in a relationship, and among those, 57% reported being satisfied or very satisfied with their current relationship. At baseline (2021), about 79% reported past-year alcohol use, and 4% reported alcohol use disorder. The mean overall E-HITS score was 5.65 (SD = 1.60). Approximately one-quarter (24.7%) of respondents reported experiencing past-year IPV in 2021. Among subtypes, 3.5% reported physical IPV with a mean score of the two physical IPV items of 2.06 (SD = 0.42). One-fifth (20.4%) reported sexual IPV using its relevant single item measure (M=1.32, SD = 0.73), and 23.9% reported emotional IPV with the mean of these two items of 2.54 (SD = 1.24). In the subsequent 12 months (2022 annual questionnaire), the mean AUDIT score was 3.52 (SD = 4.13).
Table 1.
Baseline participant characteristics, intimate partner violence (IPV), history of alcohol use, and AUDIT score at 1-year follow-up, The PRIDE Study 2021–2022.
| Total (n = 3783) | |
|---|---|
| Current age (years), mean (SD) | 39.1 (14.9) |
| Gender identity,a no. (%) | |
| Agender | 208 (5.5) |
| Cisgender man | 643 (17.0) |
| Cisgender woman | 892 (23.6) |
| Genderqueer | 548 (14.5) |
| Man | 784 (20.7) |
| Non-binary | 980 (25.9) |
| Questioning | 179 (4.7) |
| Transgender man | 518 (13.7) |
| Transgender woman | 214 (5.7) |
| Two-spirit | 40 (1.1) |
| Woman | 810 (21.4) |
| Another gender identity | 257 (6.8) |
| Gender groups, no. (%) | |
| Cisgender man | 929 (24.6) |
| Cisgender woman | 998 (26.4) |
| Gender diverse, assigned female at birth | 954 (25.2) |
| Gender diverse, assigned male at birth | 138 (3.6) |
| Transgender man | 541 (14.3) |
| Transgender woman | 223 (5.9) |
| Sexual orientation,a no. (%) | |
| Asexual | 440 (11.6) |
| Bisexual | 1148 (30.3) |
| Gay | 1290 (34.1) |
| Lesbian | 841 (22.2) |
| Pansexual | 602 (15.9) |
| Queer | 1738 (45.9) |
| Questioning | 88 (2.3) |
| Same-gender loving | 173 (4.6) |
| Heterosexual | 73 (1.9) |
| Two-spirit | 29 (0.8) |
| Another sexual orientation | 163 (4.3) |
| Sexual orientation groups, no. (%) | |
| Asexual | 110 (2.9) |
| Bisexual | 306 (8.1) |
| Gay or Lesbian | 1123 (29.7) |
| Pansexual | 96 (2.5) |
| Queer | 310 (8.2) |
| Heterosexual | 35 (0.9) |
| Multiple options selected | 1780 (47.1) |
| Endorsed only Another sexual orientation, Same-gender loving, or Questioning | 23 (0.6) |
| Ethnoracial identity,a,b no. (%) | |
| American Indian or Alaska Native | 107 (2.8) |
| Asian | 173 (4.6) |
| Black, African American or African | 138 (3.6) |
| Hispanic, Latino or Spanish | 227 (6.0) |
| Middle Eastern or North African | 54 (1.4) |
| Native Hawaiian or other Pacific Islander | 8 (0.2) |
| White | 3478 (91.9) |
| Another ethnoracial identity | 59 (1.6) |
| Education level, no. (%) | |
| High school or less | 142 (3.8) |
| Some college | 707 (18.7) |
| 4-year college graduate | 1322 (34.9) |
| Advanced degree | 1611 (42.6) |
| Missing | 1 (0.0) |
| Current employment, no. (%) | |
| No | 1004 (26.5) |
| Yes | 2778 (73.4) |
| Missing | 1 (0.0) |
| Individual income, no. (%) | |
| $0–20,000 | 1095 (28.9) |
| $20,001–50,000 | 1109 (29.3) |
| $50,001–100,000 | 990 (26.2) |
| $100,001+ | 563 (14.9) |
| Missing | 26 (0.7) |
| Current Census region, no. (%) | |
| Northeast | 776 (20.5) |
| Midwest | 770 (20.4) |
| South | 962 (25.4) |
| West | 1253 (33.1) |
| Missing | 22 (0.6) |
| Currently in relationship, no. (%) | |
| No | 1261 (33.3) |
| Yes | 2496 (66.0) |
| Missing | 26 (0.7) |
| Relationship satisfaction (n = 2496), no. (%) | |
| Very dissatisfied | 49 (1.3) |
| Dissatisfied | 111 (2.9) |
| Neutral | 189 (5.0) |
| Satisfied | 857 (22.7) |
| Very satisfied | 1289 (34.1) |
| Experienced any IPV, no. (%) | 936 (24.7) |
| Physical IPV, no. (%) | 133 (3.5) |
| Sexual IPV, no. (%) | 772 (20.4) |
| Emotional IPV, no. (%) | 904 (23.9) |
| Overall E-HITS, mean (SD) | 5.65 (1.60) |
| Physical E-HITS, mean (SD) | 2.06 (0.42) |
| Sexual E-HITS, mean (SD) | 1.32 (0.73) |
| Emotional E-HITS, mean (SD) | 2.54 (1.24) |
| Past-year alcohol use, no. (%) | 3005 (79.4) |
| Self-reported alcohol use disorder diagnosis, no. (%) | 136 (3.6) |
| AUDIT, mean (SD) | 3.52 (4.13) |
SD, standard deviation; E-HITS, Extended-Hurt, Insulted, Threaten, Scream; IPV, intimate partner violence, AUDIT, Alcohol Use Disorders Identification Test.
Participants could select multiple responses; thus, the sum of percentages is greater than 100%.
Approximately 11% selected multiple ethnoracial identities.
In adjusted models, both linear (B: 0.26, 95% CI: 0.14, 0.38) and quadratic (B: −0.03, 95% CI: −0.04, −0.01) terms for overall IPV were significantly associated with AUDIT scores (Table 2). This indicates a linear increase, but at a lower rate after E-HITS scores exceed 10 points. indicates our (see Fig. 1a). Among IPV subtypes for the overall sample, patterns of associations with AUDIT largely reflected those of overall IPV, with AUDIT scores increasing with respect to all subtypes, but at a lower rate at higher E-HITS scores. Sexual IPV (Fig. 1b) showed the largest association with AUDIT (linear B: 1.47, 95% CI: 0.39, 2.55 & quadratic B: −0.55, 95% CI: −0.94, −0.16), followed by physical IPV (linear B: 0.57, 95% CI: −0.02, 1.15 & quadratic B: −0.12, 95% CI: −0.25, 0.01) and emotional IPV (linear B: 0.36, 95% CI: 0.18, 0.55 & quadratic b: −0.07, 95% CI: −0.11, −0.02) (Fig. 1c and d).
Table 2.
Adjusted associations between intimate partner violence (IPV) and its subtypes with AUDIT scores among the total sample, The PRIDE Study, 2021–2022 (n = 3783).
| Adjusted B | 95% CI | P-valuea | ||
|---|---|---|---|---|
| Overall intimate partner violence | E-HITS | 0.26 | 0.14, 0.38 | <0.001 |
| E-HITS2 (quadratic) | −0.03 | −0.04, −0.01 | ||
| Types of intimate partner violence | Physical E-HITS | 0.57 | −0.02, 1.15 | 0.073 |
| Physical E-HITS2 | −0.12 | −0.25, 0.01 | ||
| Sexual E-HITS | 1.47 | 0.39, 2.55 | 0.005 | |
| Sexual E-HITS2 | −0.55 | −0.94, −0.16 | ||
| Emotional E-HITS | 0.36 | 0.18, 0.55 | 0.003 | |
| Emotional E-HITS2 | −0.07 | −0.11, −0.02 |
Models adjusted for age, gender identity groups, sexual orientation groups, education level, employment, individual income, baseline Census region, past-year alcohol use and baseline self-reported alcohol use disorder diagnosis. All E-HITS measures were mean centered.
Abbreviations: AUDIT, Alcohol Use Disorders Identification Test; E-HITS, Extended-Hurt, Insulted, Threaten, Scream; CI, confidence interval.
Compared models with and without quadratic term by pooling the likelihood-ratio test across multiply imputed data sets.
Fig. 1.
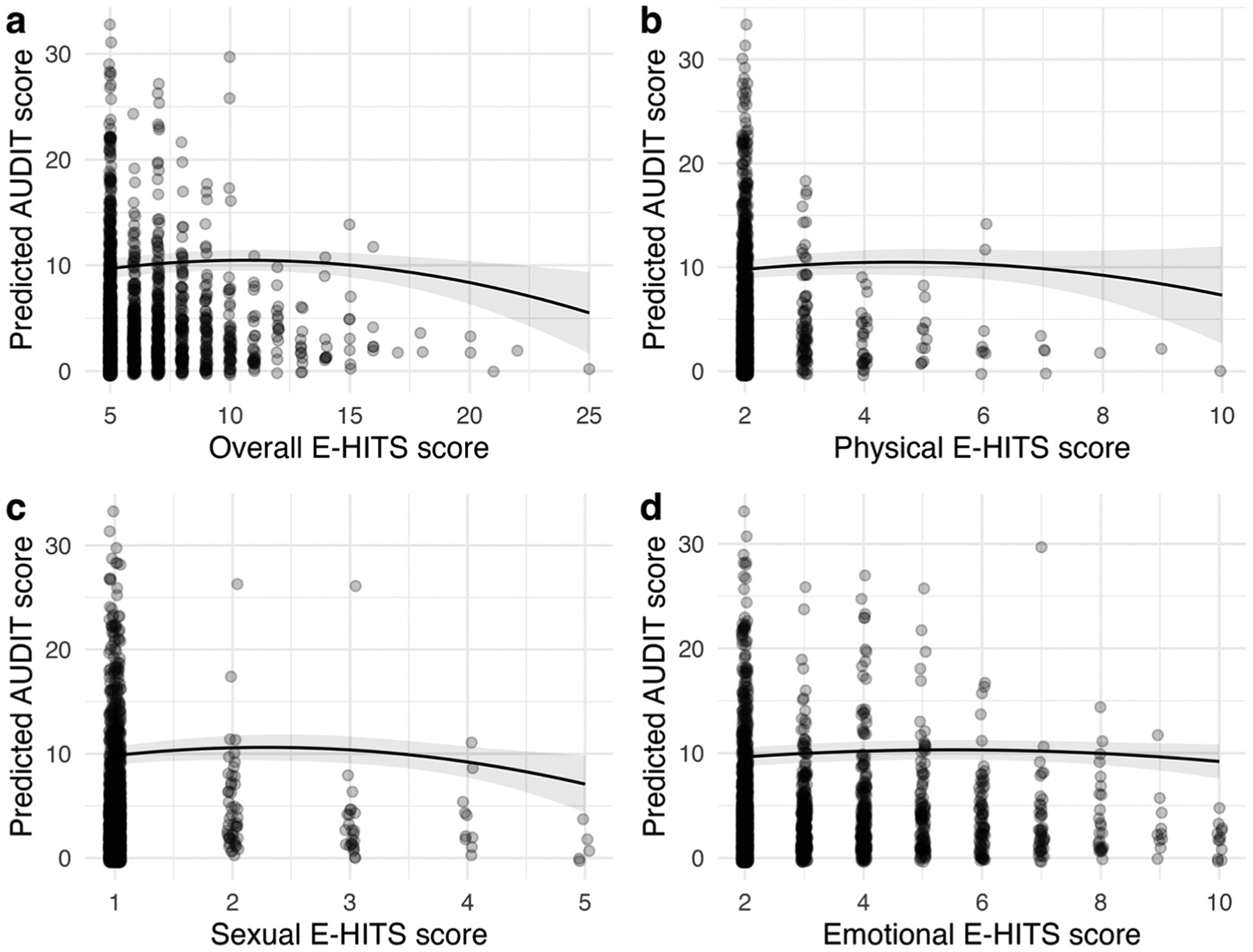
Model-predicted AUDIT scores at 1-year follow-up for a) overall E-HITS, b) physical E-HITS, c) sexual E-HITS, and d) emotional E-HITS. Fitted lines indicate predicted AUDIT scores, gray bands indicate 95% confidence intervals, black dots indicate raw AUDIT scores of individual participants. AUDIT, Alcohol Use Disorders Identification Test, E-HITS, Extended-Hurt, Insulted, Threaten, Scream.
Among participants with available information on current relationship status (n = 3757), there were few differences in sociodemographic characteristics, IPV, and history of alcohol use by current relationship status (Supplemental Table 2). Sensitivity analysis indicated that results did not substantially change after accounting for relationship status and satisfaction (Supplemental Table 3). Upon stratifying by gender groups, we observed considerable variation in the associations of past-year IPV and its subtypes with AUDIT (Supplemental Figure 1–4, Supplemental Table 4). Nonlinear patterns of associations were not consistent across gender identity groups or IPV typology. Among cisgender men, we observed these nonlinear associations for overall IPV (linear: B: 0.57, 95% CI: 0.28, 0.87 & quadratic: B: −0.05, 95% CI: −0.09, −0.01) and emotional IPV (linear: B: 0.75, 95% CI: 0.34, 1.16 & quadratic: B: −0.11, 95% CI: −0.21, 0.00,). For cisgender women, we observed nonlinear associations for physical IPV (linear: B: 2.28, 95% CI: 0.32, 4.24 & quadratic: B: −0.81, 95% CI: −1.58, −0.04) and sexual IPV (linear: B: 5.52, 95% CI: 2.45, 8.79 & quadratic: B: −2.15, 95% CI: −3.53, −0.78). For transgender men, we observed nonlinear associations for emotional IPV (linear: B: 0.56, 95% CI: 0.05, 1.07 & quadratic: B: −0.12, 95% CI: −0.24, 0.00). We did not observe significant associations between past-year IPV with subsequent AUDIT for other gender identity groups and IPV typology.
4. Discussion
The results of this study provide some of the first data on the temporal relationship between IPV and alcohol use among LGBTQIA+ people in the US. While previous work with cisgender, heterosexual women suggests that the stress resulting from IPV may result in incident increases in alcohol use (Abbey et al., 2004; Ogden et al., 2022), this relationship was largely unexplored in LGBTQIA+ relationships prior to this study. The results reported here add to the evidence concerning the role of IPV in substance use among LGBTQIA+ people and provide insight into potential points of intervention for the reduction of alcohol use in these communities and adding to the goals of the National Action Plan.
The results indicate that reporting any of the measured forms of violence in the past year is related to a subsequent higher AUDIT score of 0.26 points. When broken down by typology, experiencing sexual violence had the strongest relationship with alcohol use and was related to greater AUDIT scores (1.47 points per sexual E-HITS point, recalling that E-HITS is a measure of the frequency of violence). Experiencing physical violence was associated with greater AUDIT scores of more than half of a point (0.57), while reporting emotional violence resulted in higher AUDIT scores of more than a third of a point (0.36). These are consistent with studies of cisgender, heterosexual women, in which findings indicated increases in alcohol use in the year following IPV (La Flair et al., 2012; Ogden et al., 2022). However, the differential effects by typology should be interpreted with caution given the fact that the E-HITS scale is designed as a screening tool for IPV and is not reflective of the full breadth of violence types experienced by LGBTQIA+ populations. Together, these findings suggest that preventing IPV and mitigating its harms could be part of multi-pronged strategies to decrease future alcohol use in LGBTQIA+ communities.
Conditioning on relationship status and satisfaction did not significantly attenuate the results found in the larger sample, a null funding which has important implications for future IPV research. One common limitation of IPV research in LGBTQIA+ populations is that samples are limited to those who reported currently being in a relationship (Juwono et al., 2023; Mustanski et al., 2019). However, those who were not currently in a relationship may have recently experienced IPV and, in fact, may not be in a relationship for precisely that reason. This sub-analysis suggests that inclusion criteria for IPV-related research should be agnostic to current relationship status. Individual-level interventions designed to understand patterns of relationships (e.g., partner selection, communication skills, relationship functioning) may help those not currently in a relationship to be more mindful about future relationships, reducing their propensity to enter a(nother) violent relationship. While these types of individual interventions may provide some support, future work should concentrate on the context in which IPV occurs in order to change broader social norms (e.g., minority stress) that undergird the perpetration of relationship violence.
In this study, we explored the relationship between IPV and alcohol use with linear and quadratic functions. There was a dose-response relationship between IPV and alcohol use until a value of approximately 10 points on the E-HITS scale. While the E-HITS ranges from 5 to 25, there are important variations in how a value of 10 can be calculated (e.g., one person may endure frequent emotional violence accompanied by infrequent physical or sexual violence while another may endure rare instances of all five forms of violence measured). This initial glimpse into the dynamic relationship between IPV and alcohol use suggests that LGBTQIA+ people who experience lower scores on the E-HITS show increased levels of alcohol use, whereas those who have higher E-HITS scores show a more marginal effect on alcohol use beyond that already observed with mild-to-moderate alcohol use. There are several potential explanations for this finding. First, though we controlled for history of alcohol use at baseline, those who experience chronic IPV may already cope with these added stressors through heavier alcohol use, rendering alcohol use increases over the subsequent year marginal in nature. Second, those who experience more frequent IPV may turn to substances other than alcohol to cope with the additional stress of experiencing IPV. Previous studies suggest that men who have sex with men who report severe or frequent IPV have higher rates of illicit substance use (e.g., Wu et al., 2015) than those who report less frequent or severe IPV (e.g., Gezinski et al., 2021). Third, frequent instances of IPV often lead to the termination of a relationship, while less frequent instances of IPV are often endured for longer periods of time (Ackerman and Field, 2011; Gelles, 1976; Raghavan et al., 2005; Rhatigan et al., 2011), potentially compounding stress and leading to greater increases in alcohol use. Thus, reporting less frequent IPV may be indicative of more chronic violence and longer-term changes to the couple’s relationship (e.g., breakdown in communication patterns, additional life stressors) that together lead to increased alcohol use. Interventions targeting IPV and alcohol should make a concerted effort to include those experiencing IPV less frequently but are enduring IPV less often as part of a broader constellation of relationship dysfunction (Bresin et al., 2023). Importantly, this pattern varied by gender groups, meaning LGBTQIA+ should not be treated as a monolith for intervention development. Among gender groups, we saw a similar curvilinear pattern for cisgender men regarding overall and emotional IPV, for cisgender women for physical and sexual IPV, and for transgender men for emotional IPV. As these complex pathways are just now starting to be analyzed, additional research on how IPV may impact substance use patterns is needed within the diverse identities that comprise the LGBTQIA+ community. This may lead to a better understanding of the mechanisms between IPV and alcohol use, as well as how violence and alcohol use fit into diverse couples’ broader relationship contexts.
4.1. Strengths and limitations
While this study contains important strengths - including its longitudinal design, robust methods, geographically diverse sample, and theoretical grounding - there are important limitations to note. First, the measure of IPV, the E-HITS scale, is an IPV screener and is not meant to capture the full experience of IPV among LGBTQIA+ individuals. There are important forms of violence (e.g., “outing” or threatening to “out” someone, making fun of a partner based on gender expression) that fall outside the traditional measures of IPV and remain unaccounted for in most studies of IPV in these communities. Additionally, while preliminary evidence suggests the E-HITS can be used to screen for specific typologies of violence, this is not psychometrically validated in SGM people. Second, we did not control for other drug use or polydrug use, only alcohol use. LGBTQIA+ people may turn to (multiple) substances other than alcohol to cope with the stressors of existing as an LGBTQIA+ person in a cisheteropatriarchal society, as well as the other stressors due to their other intersectional identities (e.g., race-, ethnicity- socio-economic-based) that they may face. Future studies may query other substance use in relation to IPV. Even without accounting for other substance use, it is important to understand how IPV is related to alcohol use specifically given its ubiquitous nature in the US and high rates of use among these communities. Third, while The PRIDE Study is a diverse sample in many ways, certain racial and ethnic minority communities are underrepresented in this sub-sample, and white participants are overrepresented compared to those excluded for data missingness. As such, this study may not be generalizable to all LGBTQIA+ sub-groups. Finally, given that E-HITS was only included in The PRIDE Study beginning in 2021, we were only able to model the relationship between IPV on alcohol use across the two most recent years of the study. E-HITS only screens for IPV victimization; mounting evidence suggests queer relationships may have significant rates of bidirectional violence, meaning both members of a dyad perpetrate and experience IPV (Kirschbaum et al., 2023; Machado et al., 2024). We may therefore be missing the full spectrum of violence occurring in many participants’ relationships, which could have implications for alcohol use and intervention development. As The PRIDE Study cohort continues, we will be able to draw longer-term inferences on the effects of IPV on alcohol use and may be able to assess additional violence-related constructs.
5. Conclusion
Our results suggest that many (~25%) LGBTQIA+ participants in The PRIDE study are affected by IPV, and this was related to alcohol use. Consistent with the Minority Stress Model, these results point to the need for additional research that can elucidate the means by which interpersonal and individual interventions can prevent and mitigate the harms of IPV.
This analysis represents a first step toward understanding the role of IPV in alcohol use among a marginalized and under-resourced population. By adding rigor to the existing evidence base, we aim to begin understanding the temporal relationship between violence and individual alcohol use outcomes. Our results demonstrate that experiencing IPV is related to increased alcohol use across a wide range of sexual and gender identities, providing a foundation on which to conduct additional analyses in specific communities that may yield important results for intervention development. Though exploratory in nature, this study is among the first to show the temporal relationship between IPV and alcohol use in LGBTQIA+ communities, paving the way for future interventions that include preventing and mitigating IPV as a component of broader interventions designed to reduce alcohol use disparities in LGBTQIA+ communities, achieve the goals of the National Action Plan (The White House, 2023), and lead to greater health equity for this population.
Supplementary Material
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.drugalcdep.2024.111342.
Acknowledgments
The PRIDE Study is a community-engaged research project that serves and is made possible by LGBTQIA+ community involvement at multiple points in the research process, including the dissemination of findings. We acknowledge the courage and dedication of The PRIDE Study participants for sharing their stories; the careful attention of PRIDEnet Participant Advisory Committee (PAC) members for reviewing and improving every study application; and the enthusiastic engagement of PRIDEnet Ambassadors and Community Partners for bringing thoughtful perspectives as well as promoting enrollment and disseminating findings. For more information, please visit pridestudy.org
The authors would also like to acknowledge the contributions of the Early-Stage Investigator program at UCSF School of Nursing, including Dr. Oscar Beltran, Dr. John Gilmore, Dr. Briana Last, Dr. Briana McGeough, and Dr. Elliott Tebbe.
Funding
This study was co-funded by the National Institute on Drug Abuse and the Office of Research on Women’s Health through R01DA052016 to AF. Data collected for analysis in this publication was supported by the National Institutes of Health under Award Number 5P50AA005595. Dr. Annesa Flentje’s work on this project was partially supported by K24DA057874 from the National Institute on Drug Abuse. Research reported in this article was partially funded through a Patient-Centered Outcomes Research Institute [www.pcori.org; PPRN-1501-26848] to Dr. Mitchell R. Lunn. The statements in this article are solely the responsibility of the authors and do not necessarily represent the views of Patient-Centered Outcomes Research Institute, its Board of Governors or Methodology Committee, or the National Institutes of Health.
Footnotes
CRediT authorship contribution statement
Zubin Dastur: Investigation, Project administration, Writing – review & editing. Micah E. Lubensky: Investigation, Project administration, Writing – review & editing. Nguyen Khai Tran: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. Dalton Scott: Writing – original draft, Writing – review & editing. Nicholas Metheny: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Annesa Flentje: Funding acquisition, Investigation, Project administration, Supervision, Writing – review & editing. Mitchell R. Lunn: Funding acquisition, Investigation, Resources, Supervision, Writing – review & editing. Juno Obedin-Maliver: Funding acquisition, Investigation, Project administration, Supervision, Writing – review & editing.
Declaration of Competing Interest
Dr. Lunn has received consulting fees from Hims, Inc and from Folx Health that fall outside the scope of the submitted work. Dr Obedin-Maliver has received consulting fees from Folx Health, Hims, Inc, and Ibis Reproductive Health outside the scope of the submitted work. No other authors have disclosures to report.
References
- Ahmadabadi Z, Najman JM, Williams GM, Clavarino AM, d’Abbs P, Smirnov A, 2019. Intimate partner violence in emerging adulthood and subsequent substance use disorders: findings from a longitudinal study. Addiction 114 (7), 1264–1273. 10.1111/add.14592. [DOI] [PubMed] [Google Scholar]
- Abbey A, Zawacki T, Buck PO, Clinton AM, McAuslan P, 2004. Sexual assault and alcohol consumption: What do we know about their relationship and what types of research are still needed? Aggression and violent behavior 9, 271–303. 10.1016/S1359-1789(03)00011-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackerman J, Field L, 2011. The gender asymmetric effect of intimate partner violence on relationship satisfaction. Violence and victims 26, 703–724. 10.1891/0886-6708.26.6.703. [DOI] [PubMed] [Google Scholar]
- Basting EJ, Medenblik AM, Garner AR, Sullivan JA, Romero GJ, Shorey RC, Stuart GL, 2023. Intimate partner violence perpetration among sexual minority young adults: associations with alcohol use, PTSD symptoms, internalized homophobia, and heterosexist discrimination, 08862605231197152 J. Interpers. Violence 10.1177/08862605231197152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresin K, Nicholas JK, Cowand AL, Alacha HF, Rodriguez AM, Parrott DJ, 2023. The effects of sexual and gender minority stress on relationship functioning: a meta-analysis. Pers. Relatsh, pere.12511 10.1111/pere.12511. [DOI] [Google Scholar]
- Brooks VR, 1981. Minority stress and lesbian women. Heath. [Google Scholar]
- Brown EC, Catalano RF, Fleming CB, Haggerty KP, Abbott RD, 2009. Adolescent Substance Use Outcomes in the Raising Healthy Children Project: A Two-part Latent Growth Curve Analysis. [DOI] [PubMed]
- van Buuren S, Groothuis-Oudshoorn K, 2011. mice: Multivariate imputation by chained equations in R. J. Stat. Softw 45 (3), 1–67. 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- Cafferky BM, Mendez M, Anderson JR, Stith SM, 2018. Substance use and intimate partner violence: a meta-analytic review. Psychol. Violence 8 (1), 110–131. 10.1037/vio0000074. [DOI] [Google Scholar]
- Carvalho AF, Lewis RJ, Derlega VJ, Winstead BA, Viggiano C, 2011. Internalized sexual minority stressors and same-sex intimate partner violence. J. Fam. Violence 26 (7), 501–509. 10.1007/s10896-011-9384-2. [DOI] [Google Scholar]
- Caldwell JE, Swan SC, Woodbrown VD, 2012. Gender differences in intimate partner violence outcomes. Psychology of violence 2, 42. [Google Scholar]
- Chan C, Chan Y, Au A, Cheung G, 2010. Reliability and validity of the “extended—hurt, insult, threaten, scream” (E-hits) screening tool in detecting intimate partner violence in hospital emergency departments in Hong Kong. Hong Kong J. Emerg. Med 17 (2), 109–117. 10.1177/102490791001700202. [DOI] [Google Scholar]
- Davis A, Kaighobadi F, Stephenson R, Rael C, Sandfort T, 2016. Associations between alcohol use and intimate partner violence among men who have sex with men. LGBT Health 3 (6), 400–406. 10.1089/lgbt.2016.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker M, Littleton HL, Edwards KM, 2018. An updated review of the literature on LGBTQ+ intimate partner violence. Curr. Sex. Health Rep 10 (4), 265–272. 10.1007/s11930-018-0173-2. [DOI] [Google Scholar]
- Dyar C, Sarno EL, Newcomb ME, Whitton SW, 2020. Longitudinal associations between minority stress, internalizing symptoms, and substance use among sexual and gender minority individuals assigned female at birth. J. Consult. Clin. Psychol 88 (5), 389–401. 10.1037/ccp0000487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards KM, Sylaska KM, Neal AM, 2015. Intimate partner violence among sexual minority populations: a critical review of the literature and agenda for future research. Psychol. Violence 5 (2), 112–121. 10.1037/a0038656. [DOI] [Google Scholar]
- Flentje A, Heck NC, Brennan JM, Meyer IH, 2020. The relationship between minority stress and biological outcomes: a systematic review. J. Behav. Med 43 (5), 673–694. 10.1007/s10865-019-00120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Follingstad DR, Ryan KM, 2013. Contemporary issues in the measurement of partner violence. Sex Roles 69 (3–4), 115–119. 10.1007/s11199-013-0298-8. [DOI] [Google Scholar]
- Gelles RJ, 1976. Abused wives: Why do they stay. Journal of Marriage and the Family 38, 659–668. 10.2307/350685. [DOI] [Google Scholar]
- Gezinski LB, Gonzalez-Pons KM, Rogers MM, 2021. Substance use as a coping mechanism for survivors of intimate partner violence: implications for safety and service accessibility. Violence Women 27 (2), 108–123. 10.1177/1077801219882496. [DOI] [PubMed] [Google Scholar]
- Gosling H, Pratt D, Montgomery H, Lea J, 2022. The relationship between minority stress factors and suicidal ideation and behaviours amongst transgender and gender non-conforming adults: a systematic review. J. Affect. Disord 303, 31–51. 10.1016/j.jad.2021.12.091. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, 2009. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol. Bull 135 (5), 707–730. 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks ML, Testa RJ, 2012. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the minority stress model. Prof. Psychol. Res. Pract 43 (5), 460–467. 10.1037/a0029597. [DOI] [Google Scholar]
- Hoy-Ellis CP, 2023. Minority stress and mental health: a review of the literature. J. Homosex 70 (5), 806–830. 10.1080/00918369.2021.2004794. [DOI] [PubMed] [Google Scholar]
- Hughto JMW, Quinn EK, Dunbar MS, Rose AJ, Shireman TI, Jasuja GK, 2021. Prevalence and co-occurrence of alcohol, nicotine, and other substance use disorder diagnoses among US transgender and cisgender adults. JAMA Netw. Open 4 (2), e2036512. 10.1001/jamanetworkopen.2020.36512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iverson KM, King MW, Gerber MR, Resick PA, Kimerling R, Street AE, Vogt D, 2015. Accuracy of an intimate partner violence screening tool for female VHA patients: a replication and extension. J. Trauma. Stress 28 (1), 79–82. 10.1002/jts.21985. [DOI] [PubMed] [Google Scholar]
- Juwono S, Anato JLF, Kirschbaum AL, Metheny N, Dvorakova M, SkakoonSparling S, Moore DM, Grace D, Hart TA, Lambert G, Lachowsky NJ, Jollimore J, Cox J, Maheu-Giroux M, 2023. Prevalence, determinants, and trends in the experience and perpetration of intimate partner violence among a cohort of gay, bisexual, and other men who have sex with men in Montréal, Toronto, and Vancouver, Canada (2017–2022) [Preprint]. Epidemiology. 10.1101/2023.07.24.23293112. [DOI] [PubMed] [Google Scholar]
- Kim C, Schmuhl M, 2021. Assessment of research on Intimate Partner Violence (IPV) among sexual minorities in the United States. Trauma Violence Abus. 22 (4), 766–776. 10.1177/1524838019881732. [DOI] [PubMed] [Google Scholar]
- Kimmes JG, Mallory AB, Spencer C, Beck AR, Cafferky B, Stith SM, 2019. A meta-analysis of risk markers for intimate partner violence in same-sex relationships. Trauma Violence Abus. 20 (3), 374–384. 10.1177/1524838017708784. [DOI] [PubMed] [Google Scholar]
- King KA, Yockey RA, Vidourek RA, 2022. Transgender individuals and psychological intimate partner violence: a national study. J. Fam. Violence 37 (2), 289–300. 10.1007/s10896-020-00219-4. [DOI] [Google Scholar]
- Kirschbaum AL, Metheny N, Skakoon-Sparling S, Grace D, Yakubovich AR, Cox J, Palachi A, Sang JM, O’Campo P, Tan DHS, Hart TA, 2023. Syndemic factors and lifetime bidirectional intimate partner violence among gay, bisexual, and other sexual minority men. LGBT Health 10 (S1), S89–S97. 10.1089/lgbt.2023.0117. [DOI] [PubMed] [Google Scholar]
- Krueger EA, Fish JN, Upchurch DM, 2020. Sexual orientation disparities in substance use: investigating social stress mechanisms in a national sample. Am. J. Prev. Med 58 (1), 59–68. 10.1016/j.amepre.2019.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Flair LN, Bradshaw CP, Storr CL, Green KM, Alvanzo AAH, Crum RM, 2012. Intimate partner violence and patterns of alcohol abuse and dependence criteria among women: a latent class analysis. J. Stud. Alcohol Drugs 73 (3), 351–360. 10.15288/jsad.2012.73.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JH, Gamarel KE, Bryant KJ, Zaller ND, Operario D, 2016. Discrimination, mental health, and substance use disorders among sexual minority populations. LGBT Health 3 (4), 258–265. 10.1089/lgbt.2015.0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leemis Ruth W., Norah Friar, Khatiwada S, Chen MS, Kresnow M, Smith SG, Caslin S, Basile KC, 2022. The National Intimate Partner and Sexual Violence Survey: 2016/2017 Report on Intimate Partner Violence. Center for Disease Control and Prevention. 〈https://www.cdc.gov/violenceprevention/pdf/nisvs/nisvsreportonipv_2022.pdf〉. [Google Scholar]
- Lunn MR, Capriotti MR, Flentje A, Bibbins-Domingo K, Pletcher MJ, Triano AJ, Sooksaman C, Frazier J, Obedin-Maliver J, 2019. Using mobile technology to engage sexual and gender minorities in clinical research. PLOS ONE 14 (5), e0216282. 10.1371/journal.pone.0216282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunn MR, Lubensky M, Hunt C, Flentje A, Capriotti MR, Sooksaman C, Harnett T, Currie D, Neal C, Obedin-Maliver J, 2019. A digital health research platform for community engagement, recruitment, and retention of sexual and gender minority adults in a national longitudinal cohort study–—the PRIDE study. J. Am. Med. Inform. Assoc 26 (8–9), 737–748. 10.1093/jamia/ocz082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machado A, Sousa C, Cunha O, 2024. Bidirectional violence in intimate relationships: a systematic review. Trauma Violence Abus. 25 (2), 1680–1694. 10.1177/15248380231193440. [DOI] [PubMed] [Google Scholar]
- Meyer IH, 2003. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol. Bull 129 (5), 674–697. 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer Ilan H., Frost David M., 2013. Minority stress and the health of sexual minorities. Handbook of Psychology and Sexual Orientation. Oxford University Press, pp. 252–266. [Google Scholar]
- Mustanski B, Morgan E, D’Aquila R, Birkett M, Janulis P, Newcomb ME, 2019. Individual and network factors associated with racial disparities in HIV among young men who have sex with men: results from the RADAR cohort study. JAIDS J. Acquir. Immune Defic. Syndr 80 (1), 24–30. 10.1097/QAI.0000000000001886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden SN, Dichter ME, Bazzi AR, 2022. Intimate partner violence as a predictor of substance use outcomes among women: a systematic review. Addict. Behav 127, 107214 10.1016/j.addbeh.2021.107214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peitzmeier SM, Malik M, Kattari SK, Marrow E, Stephenson R, Agénor M, Reisner SL, 2020. Intimate partner violence in transgender populations: systematic review and meta-analysis of prevalence and correlates. Am. J. Public Health 110 (9), e1–e14. 10.2105/AJPH.2020.305774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porsch LM, Xu M, Veldhuis CB, Bochicchio LA, Zollweg SS, Hughes TL, 2022. Intimate partner violence among sexual minority women: a scoping review. Trauma Violence Abus. 152483802211228 10.1177/15248380221122815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghavan C, Swan SC, Snow DL, Mazure CM, 2005. The Mediational Role of Relationship Efficacy and Resource Utilization in the Link Between Physical and Psychological Abuse and Relationship Termination. Violence Against Women 11, 65–88. 10.1177/1077801204271514. [DOI] [PubMed] [Google Scholar]
- R Core Team, 2022. R: A Language and Environment for Statistical Computing (4.2.1) [Computer software]. R Foundation for Statistical Computing. 〈https://www.r-project.org/〉. [Google Scholar]
- Reuter TR, Newcomb ME, Whitton SW, Mustanski B, 2017. Intimate partner violence victimization in LGBT young adults: Demographic differences and associations with health behaviors. Psychology of violence 7, 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhatigan DL, Stewart C, Moore TM, 2011. Effects of Gender and Confrontation on Attributions of Female-Perpetrated Intimate Partner Violence. Sex Roles 64, 875–887. 10.1007/s11199-011-9951-2. [DOI] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M, 1993. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction 88 (6), 791–804. 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Scott S, Pulice-Farrow L, Do Q, Brunett K, Balsalm K, et al. , 2023. Intimate Partner Violence in Transgender and Nonbinary Relationships: Actor-Partner Associations with Relationship Satisfaction, Dyadic Coping, and Partner Support. LGBT Health 10 (S1). 10.1089/lgbt.2023.0112. [DOI] [PubMed] [Google Scholar]
- Smith J, Mulford C, Latzman NE, Tharp AT, Niolon PH, Blachman-Demner D, 2015. Taking stock of behavioral measures of adolescent dating violence. J. Aggress. Maltreatment Trauma 24 (6), 674–692. 10.1080/10926771.2015.1049767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubbs A, Szoeke C, 2022. The effect of intimate partner violence on the physical health and health-related behaviors of women: a systematic review of the literature. Trauma Violence Abus. 23 (4), 1157–1172. 10.1177/1524838020985541. [DOI] [PubMed] [Google Scholar]
- Sutton D, Dawson M, 2021. Differentiating characteristics of intimate partner violence: do relationship status, state, and duration matter? J. Interpers. Violence 36 (9–10), NP5167–NP5191. 10.1177/0886260518795501. [DOI] [PubMed] [Google Scholar]
- Swann G, Dyar C, Baidoo L, Crosby S, Newcomb ME, Whitton SW, 2022. Intersectional minority stress and intimate partner violence: the effects of enacted stigma on racial minority youth assigned female at birth. Arch. Sex. Behav 51 (2), 1031–1043. 10.1007/s10508-021-01958-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate CC, Ledbetter JN, Youssef CP, 2013. A two-question method for assessing gender categories in the social and medical sciences. J. Sex Res 50 (8), 767–776. 10.1080/00224499.2012.690110. [DOI] [PubMed] [Google Scholar]
- Tebbe EA, Budge SL, 2022. Factors that drive mental health disparities and promote well-being in transgender and nonbinary people. Nat. Rev. Psychol 1 (12), 694–707. 10.1038/s44159-022-00109-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The PRIDE Study, 2024. PRIDE Study Tools. 〈http://www.pridestudy.tools/datadetails〉.
- The White House, 2023. U.S. National Plan to End Gender-Based Violence: Strategies for Action. The White House. 〈https://www.whitehouse.gov/wp-content/uploads/2023/05/National-Plan-to-End-GBV.pdf〉. [Google Scholar]
- White SJ, Sin J, Sweeney A, Salisbury T, Wahlich C, Montesinos Guevara CM, Gillard S, Brett E, Allwright L, Iqbal N, Khan A, Perot C, Marks J, Mantovani N, 2023. Global prevalence and mental health outcomes of intimate partner violence among women: a systematic review and meta-analysis. Trauma Violence Abus. 152483802311555 10.1177/15248380231155529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitfield DL, Coulter RWS, Langenderfer-Magruder L, Jacobson D, 2021. Experiences of intimate partner violence among lesbian, gay, bisexual, and transgender college students: the intersection of gender, race, and sexual orientation. J. Interpers. Violence 36 (11–12), NP6040–NP6064. 10.1177/0886260518812071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe HL, Biello KB, Reisner SL, Mimiaga MJ, Cahill SR, Hughto JMW, 2021. Transgender-related discrimination and substance use, substance use disorder diagnosis and treatment history among transgender adults. Drug Alcohol Depend. 223, 108711 10.1016/j.drugalcdep.2021.108711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu E, El-Bassel N, McVinney LD, Hess L, Fopeano MV, Hwang HG, Charania M, Mansergh G, 2015. The association between substance use and intimate partner violence within Black male same-sex relationships. J. Interpers. Violence 30 (5), 762–781. 10.1177/0886260514536277. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


