Abstract
Stroke is a leading cause of morbidity and mortality worldwide, and dietary patterns have emerged as a significant modifiable factor in stroke prevention. The Mediterranean diet, characterized by high intake of fruits, vegetables, whole grains, nuts, olive oil, and fish, has been widely recognized for its cardiovascular benefits. However, its specific impact on stroke risk requires further elucidation. We conducted a comprehensive meta-analysis of 30 studies, including both cohort and case–control designs, to evaluate the relationship between adherence to the Mediterranean diet and the risk of stroke. A systematic search was performed across multiple databases, and a random-effects model was used to estimate pooled hazard ratios (HRs) with 95% confidence intervals (CIs). Heterogeneity was assessed using the I2 statistic, and publication bias was examined through funnel plots and Egger’s regression test. Additionally, trial sequential analysis was conducted to determine the adequacy of the sample size. The meta-analysis revealed a significant reduction in stroke risk among individuals adhering to the Mediterranean diet, with a pooled HR of 0.88 (95% CI: 0.84–0.91). Notably, a significant heterogeneity was detected (I2 = 34%). The Z-score plot from trial sequential analysis confirmed that the sample sizes were sufficient to draw definitive conclusions. However, a potential publication bias was identified. The case–control studies confirmed a highly significant effect (HR = 0.54, 95% CI: 0.4–0.73). The funnel plots in both settings hinted at the presence of a potential publication bias, supported by a significant Egger’s test. Our findings provide robust evidence supporting the protective effect of the Mediterranean diet against stroke. Despite the presence of some heterogeneity and potential publication bias, the cumulative evidence suggests that promoting the Mediterranean diet could serve as an effective public health strategy for stroke prevention. Further research is recommended to explore the underlying mechanisms and to assess the diet’s impact across diverse populations.
Keywords: Meta-analysis, Case–control, Stroke prevention, Dietary intervention, Diet
Introduction
Stroke is a leading cause of morbidity and mortality globally, with significant public health implications [1–3]. As an age-related disease, the incidence and prevalence of stroke increase sharply with advancing age, making it a growing concern in aging populations across the globe [1–3]. The aging demographics in many parts of the world are expected to significantly exacerbate the stroke burden, underscoring the urgent need for effective prevention strategies. In the USA, stroke is the fifth leading cause of death, accounting for approximately 1 in every 19 deaths [1]. Each year, around 795,000 Americans suffer a stroke, with nearly 610,000 of these being first or new strokes [4–6]. In Europe, the situation is equally concerning, with stroke being the second leading cause of death and a leading cause of adult disability [7]. The European Union alone witnesses more than 1 million strokes annually, a figure that is expected to rise as the population ages [7]. The prevalence of stroke underscores its significant impact, with nearly 7 million adults in the USA living with the aftermath of a stroke, many of whom endure chronic disabilities that severely diminish their quality of life. Similarly, in Europe, millions of individuals are affected by stroke, resulting in profound personal and societal costs [7]. The economic impact of stroke is staggering, with the total cost in the EU estimated at around €45 billion annually, including healthcare expenses, informal care, and productivity losses. These statistics highlight the critical need for effective prevention strategies that can mitigate the growing burden of stroke.
Traditionally, the primary risk factors for stroke have included hypertension, smoking, and diabetes [3, 6]. However, recent research has increasingly focused on the role of dietary patterns in stroke prevention [3], with particular emphasis on the Mediterranean diet [8–15]. This diet, characterized by a high intake of fruits, vegetables, whole grains, legumes, nuts, olive oil, and fish [16], has gained widespread recognition for its cardiovascular benefits [17–20]. Unlike other dietary approaches, the Mediterranean diet emphasizes monounsaturated fats, moderate alcohol consumption, and minimal intake of red meat. These dietary components are associated with a range of health benefits [21–29], particularly in reducing the risk of cardiovascular diseases. Emerging studies have highlighted the potential protective effects of the Mediterranean diet against stroke, yet the magnitude of this association and the underlying mechanisms remain to be fully clarified. Some epidemiological studies have demonstrated a significant inverse relationship between adherence to the Mediterranean diet and stroke risk, particularly ischemic stroke [8–15]. However, variations in the diet's effectiveness based on sex, age, and population subgroups have been observed, suggesting the need for a more nuanced understanding of its protective effects [8–15]. There is evidence suggesting that the protective effects of the Mediterranean diet may vary by sex, potentially due to differences in hormonal regulation and cardiovascular physiology. For instance, women may experience greater benefits from the diet’s anti-inflammatory properties during postmenopause, a period associated with increased vascular inflammation. These findings underscore the need for sex-specific analyses in future research to tailor dietary interventions more effectively. One critical area that warrants further exploration is the variation in the composition of the “Mediterranean diet” across different countries. The traditional Mediterranean diet is not a monolithic entity but rather a collection of dietary habits that vary significantly across the Mediterranean region [30–35]. These regional differences could contribute to the heterogeneity observed in studies assessing the diet’s impact on stroke risk. Moreover, the confounding effects of other aspects of the Mediterranean lifestyle, such as physical activity levels, social interactions, and overall lifestyle habits, further complicate the ability to draw definitive conclusions. These lifestyle factors, integral to the Mediterranean way of life, may synergistically enhance the diet’s protective effects, making it challenging to isolate the diet's specific impact on stroke prevention.
Given these complexities, the goal of this study was to conduct a comprehensive meta-analysis that synthesizes data from a diverse range of studies to clarify the relationship between adherence to the Mediterranean diet and stroke risk. By systematically analyzing these studies, this meta-analysis aims to provide robust evidence on the effectiveness of the Mediterranean diet in stroke prevention, accounting for potential sources of heterogeneity and confounding factors.
Methods
Study selection
A comprehensive search for relevant studies was conducted in the PubMed, Web of Science, and Google Scholar databases from 1990 until 2024. The search utilized keywords combined as detailed in Table 1: “Mediterranean diet” or “dietary patterns,” in combination with “stroke,” “cerebrovascular disease,” or “ischemic—or hemorrhagic stroke.” The literature search was limited to full-text publications without language restrictions. Additionally, the reference lists of identified articles and related previous meta-analyses were reviewed to uncover any further studies.
Table 1.
List of keyword combinations for research on the relationship between Mediterranean diet adherence and stroke risk
| Combination | Keywords |
|---|---|
| 1 | “Mediterranean Diet” AND “Stroke” |
| 2 | “Mediterranean Diet” AND “Cerebrovascular Disease” |
| 3 | “Mediterranean Diet” AND “Ischemic Stroke” |
| 4 | “Mediterranean Diet” AND “Hemorrhagic Stroke” |
| 5 | “Dietary Patterns” AND “Stroke” |
| 6 | “Dietary Patterns” AND “Cerebrovascular Disease” |
| 7 | “Dietary Patterns” AND “Ischemic Stroke” |
| 8 | “Dietary Patterns” AND “Hemorrhagic Stroke” |
Eligibility criteria
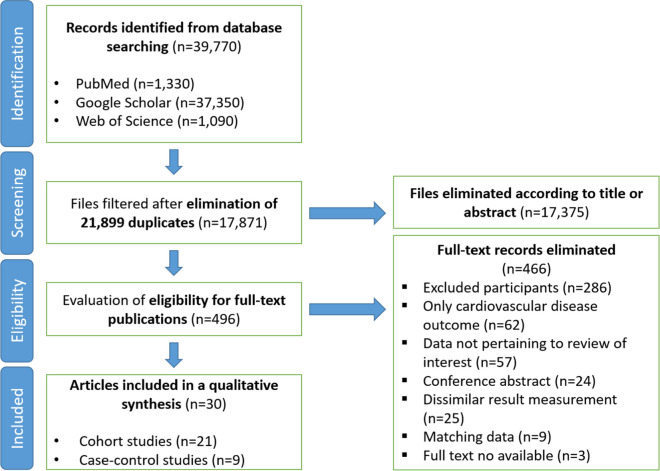
Two independent reviewers (AL, MF) screened all records and included studies that met the criteria listed in Table 2. In addition, Fig. 1 presents the study selection process for the meta-analysis.
Table 2.
Eligibility criteria for study selection
| Criterion | Description |
|---|---|
| Study population | Adults adhering to the Mediterranean diet (with comparisons to those following other dietary patterns or general populations) |
| Exposure of interest | Adherence to the Mediterranean diet, assessed through dietary questionnaires or other validated measures |
| Reported estimates | Studies reporting relative risk (RR), hazard ratios, or odds ratios and 95% confidence intervals (CIs) for stroke risk, or where these could be calculated from provided data |
| Outcome | Incidence of stroke, including subtypes such as ischemic stroke and hemorrhagic stroke |
| Study design | Observational studies, including cohort or case–control designs. In cases of duplicate studies from the same population, the study with the longest follow-up period was included |
Fig. 1.
Flow diagram illustrating the article selection process
Evaluating the overall effect
We conducted our statistical analysis using an updated approach available through the web platform at https://metaanalysisonline.com. To estimate pooled hazard ratios (HR), odds ratios (OR), and their 95% confidence intervals (CI), we employed a random-effects model. We used forest plots to visualize the results of individual studies and their aggregate effect, offering a comprehensive view of data variability and the overall effect size. To assess heterogeneity among the included studies, we applied the chi-squared test and calculated the I2 statistic.
Analysis of publication bias
Funnel plots were constructed to evaluate the relationship between study effect estimates and their precision, which also allowed us to examine the potential presence of publication bias. Egger’s regression test was performed to statistically assess the significance of any observed bias.
Assessing sample size adequacy
To determine the adequacy of the sample size, we performed a trial sequential analysis (TSA). The a priori required information size (APIS) was calculated assuming a 10% relative risk reduction, with a two-sided α of 5% and a statistical power (1 – β) of 80%. TSA was executed using Stata 17.0 with the metacoumbounds package. A Z-curve plot was generated to depict the relationship between actual cumulative sample size (AIS), time, and cumulative Z-scores. This analysis was crucial in determining whether the existing sample size was adequate to draw conclusive inferences or if further studies would be needed to solidify the findings.
Results
Identification of studies
In the initial phase of our systematic review, a total of 39,770 records were identified across multiple databases, including PubMed (n = 1330), Google Scholar (n = 37,350), and Web of Science (n = 1090). After removing 21,899 duplicates, 17,871 unique records were subjected to a title and abstract screening. This process led to the exclusion of 17,375 records that did not meet our inclusion criteria. Subsequently, the full texts of 496 articles were assessed for eligibility. During this stage, 466 articles were excluded for various reasons, such as studies only focused on cardiovascular disease (n = 62), or other methodological issues like lack of pertinent data (n = 57) or being a conference abstract only (n = 24). Ultimately, 30 articles were included in the qualitative synthesis, comprising 21 cohort studies and nine case–control studies (see Fig. 1).
Cohort studies
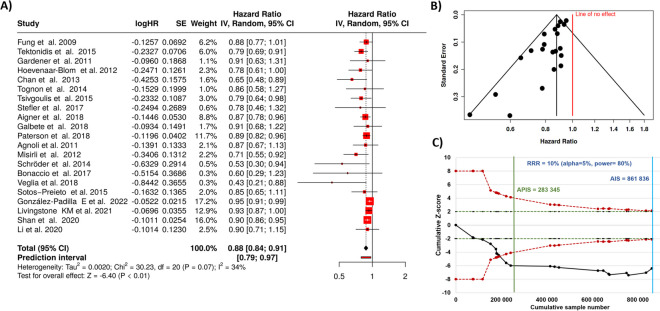
All together 21 studies were analyzed [36–56]. Based on the analysis performed using random-effects model with inverse variance method to compare the hazard rate (HR), there is a statistical difference, the summarized hazard rate is 0.88 with a 95% confidence interval of 0.84—0.91. The test for overall effect shows a significance at p < 0.05.
Notably, a noteworthy heterogeneity was detected (p = 0.07), suggesting inconsistent effects in magnitude and/or direction. The I2 value indicates that 34% of the variability among studies arises from heterogeneity rather than random chance (as shown in Fig. 2A).
Fig. 2.
Results for all cohort studies comparing Mediterranean diet and stroke risk. There is a highly significant reduction in stroke incidence with a total HR of 0.88 (A). On the other hand, the funnel plot indicates a potential publication bias (B). The Z-score plot of cohort studies investigating the correlation indicates that no additional studies are needed to get a definitive conclusion (C). SE, standard error; CI, confidence interval; IV, inverse variance; APIS, a priori information size; AIS, actual information size; RRR, relative risk ratio
The funnel plot indicates a potential publication bias. Egger’s test supports the presence of funnel plot asymmetry (intercept: − 1.35, 95% CI: − 1.86 to − 0.84, t: − 5.209, p-value: 0, see Fig. 2B).
The trial sequential analysis, as depicted in the Z-score plot in Fig. 2C, demonstrated that the total cumulative sample size (n = 861,836) was higher than the sample number necessary to draw definitive conclusions (n = 283,345).
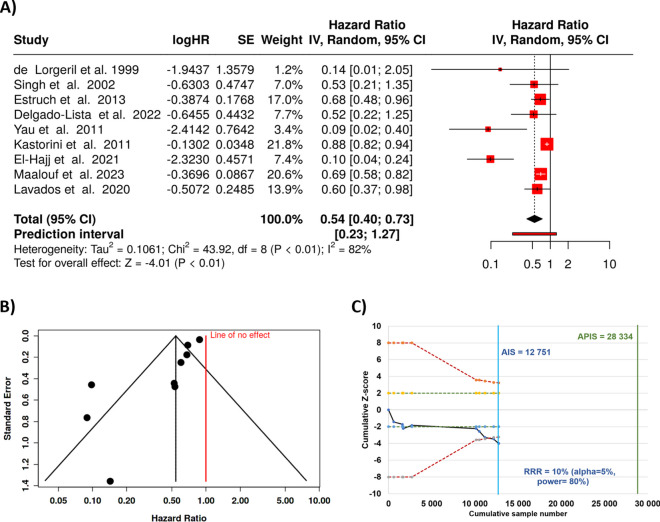
Case–control analysis
When combining all case–control studies, we were able to analyze all together nine trials [57–65]. Based on the analysis using random-effects model with the inverse variance method to compare the hazard rate, we observed a robust statistical difference, the summarized hazard rate was 0.54 with a 95% confidence interval of 0.4–0.73. In addition, the test for overall effect also supports significance at p < 0.05.
On the other hand, a significant heterogeneity was detected (< 0.01), suggesting varying effects in scale and/or direction. The I2 value indicates that 82% of the unpredictability among trials stems from heterogeneity relatively to random chance (see Fig. 3A).
Fig. 3.
Case–control studies comparing Mediterranean diet and the risk of stroke. The forest plots show a highly marked effect with a HR of 0.54 (A). The funnel plot indicates a potential publication bias (B). Z-score plot of case–control studies investigating the correlation between obesity and colorectal cancer indicates the necessity of further studies to establish a definitive conclusion (C). SE, standard error; CI, confidence interval; IV, inverse variance; APIS, a priori information size; AIS, actual information size; RRR, relative risk ratio
Similar to the incidence studies, the funnel plot points to a likely publication bias. The performed Egger’s test supports the existence of funnel plot unevenness (intercept: − 2.35, 95% CI: − 3.46 to − 1.24, t: − 4.135, p-value: 0.004, Fig. 3B).
The total number of cases included in the case–control analysis (n = 12,751) did not reach the a priori information size required for statistical significance (n = 28,334). This indicates that in this setting the current sample size is insufficient to draw definitive conclusions, necessitating further research to validate these findings. The Z-score plot utilizing all case–control studies which investigated the correlation between Mediterranean diet is provided in Fig. 3C.
Discussion
This meta-analysis provides comprehensive evidence that adherence to the Mediterranean diet is associated with a significant reduction in stroke risk. The pooled hazard ratio of 0.88 from cohort studies indicates that individuals who closely follow the Mediterranean diet have a 12% lower risk of stroke compared to those who do not. This finding aligns with existing literature that has consistently highlighted the cardiovascular benefits of the Mediterranean diet, particularly its role in reducing the risk of ischemic stroke.
One of the key strengths of this study is its large sample size, which includes data from over 860,000 participants in the cohort studies and 12,751 participants in the case–control studies. The trial sequential analysis confirmed that the cumulative sample size of the cohort studies was sufficient to draw definitive conclusions, thereby strengthening the validity of our findings. However, it is important to acknowledge the significant heterogeneity observed in both the cohort (I2 = 34%) and case–control studies (I2 = 82%), which suggests variability in the effects of the Mediterranean diet on stroke risk across different populations and study designs.
The observed heterogeneity could be attributed to several factors [66], including differences in the definition and composition of the “Mediterranean diet” across studies. The Mediterranean diet is not a standardized dietary pattern but rather a collection of dietary habits that vary significantly across the Mediterranean region and beyond [67]. While the Mediterranean diet is characterized by core components, regional variations—such as the emphasis on specific foods like olive oil in Greece versus fish in Southern Italy—may influence its overall impact. Many Mediterranean countries are moving away from the traditional Mediterranean dietary pattern, while Northern European and other countries globally are increasingly adopting a Mediterranean-like diet [68, 69]. Outside of the Mediterranean region, adherence to the Mediterranean diet often reflects adaptations to local food availability and cultural preferences. In non-Mediterranean countries, olive oil is frequently substituted with other unsaturated fats, such as canola oil, while nuts and seeds are emphasized due to their availability. Similarly, the consumption of fatty fish, a key component of the Mediterranean diet, is adapted based on regional seafood options. These substitutions may impact the overall efficacy of the diet, as the bioactive compounds and nutrient profiles of alternative foods may differ. These compositional variations further contribute to the heterogeneity observed in studies examining the diet’s protective effects against stroke. These regional differences could lead to variations in the observed protective effects against stroke. Additionally, the confounding effects of other lifestyle factors integral to the Mediterranean way of life, such as physical activity, social interactions, and overall lifestyle habits, may also contribute to the heterogeneity. These factors are known to synergistically enhance the diet’s protective effects, making it challenging to isolate the specific impact of diet alone on stroke prevention. The need for standardized definitions and adherence measures in future studies is emphasized. Furthermore, the presence of potential publication bias, as indicated by the funnel plots and Egger’s test, suggests that studies with positive results might be overrepresented in the literature, which could inflate the perceived benefits of the Mediterranean diet. This limitation highlights the importance of future research, particularly in underrepresented populations and contexts. The case–control studies included in this meta-analysis demonstrated a pronounced effect (HR = 0.54), suggesting that the Mediterranean diet could be particularly beneficial in specific populations or under certain conditions. However, while the cohort studies demonstrated sufficient sample sizes, the case–control studies did not meet the a priori information size requirement, indicating the need for larger, well-designed studies to confirm these findings. The significant heterogeneity and the fact that the total sample size did not reach the a priori information size required for statistical significance indicate that these findings should be interpreted with caution. Further research with larger and more diverse cohorts is needed to confirm these results and to better understand the conditions under which the Mediterranean diet is most effective in reducing stroke risk.
The molecular and cellular mechanisms by which the Mediterranean diet exerts its vasoprotective effects, thereby reducing the risk of stroke, are likely multifaceted and interconnected [17, 20, 34, 70–73]. These effects are mediated through anti-atherogenic, antioxidative, anti-inflammatory, and anti-aging pathways, providing valuable insights into how the Mediterranean diet promotes healthy brain aging. Atherosclerosis, a chronic condition characterized by plaque buildup in arterial walls, is a key cause of ischemic stroke. The Mediterranean diet exerts potent anti-atherogenic effects, in part, by improving lipid metabolism [72]. Rich in monounsaturated fats from olive oil, the diet has been shown to reduce low-density lipoprotein (LDL) cholesterol while increasing high-density lipoprotein (HDL) cholesterol [72, 74–80]. Elevated LDL cholesterol is a major risk factor for atherosclerosis as it promotes plaque formation, whereas HDL cholesterol is protective. By improving lipid profiles, the Mediterranean diet reduces the likelihood of plaque formation and progression within arteries [81–85]. Additionally, the diet is high in omega-3 polyunsaturated fatty acids (PUFAs) from fish and nuts, which lower triglycerides and stabilize atherosclerotic plaques [86]. Omega-3 PUFAs inhibit pro-inflammatory gene expression and reduce inflammation in arterial walls, helping prevent plaque rupture, which is critical in stroke prevention [87]. Furthermore, the diet’s antioxidant-rich foods, including fruits, vegetables, and olive oil, help prevent LDL oxidation, a key event in atherosclerosis [75, 77, 88]. Oxidized LDL is more readily taken up by macrophages, forming foam cells that accelerate plaque development. By reducing oxidative LDL damage, the Mediterranean diet slows atherogenesis.
Aging-induced microvascular impairment is a critical factor in the pathogenesis of ischemic brain damage [89]. As individuals age, there is a gradual reduction in microvascular density, known as microvascular rarefaction, which compromises the ability of small blood vessels to supply oxygen and nutrients to brain tissue. This can be exacerbated by other cardiovascular risk factors, such as obesity, hypertension, and hyperhomocysteinemia. This reduction in microvascular density, coupled with aging-related endothelial dysfunction and impaired cerebral blood flow (CBF) regulation, exacerbates the brain’s vulnerability during ischemic events. Endothelial dysfunction impairs vasodilation and promotes vasoconstriction, which further limits blood flow to areas at risk during stroke [89]. Additionally, the brain’s ability to regulate CBF in response to metabolic demands becomes compromised with age [90], making it more difficult to preserve tissue in the peri-infarct region during ischemia [91]. The Mediterranean diet may play a significant role in mitigating these effects and improving microvascular function in the brain. By protecting against microvascular impairment, the Mediterranean diet may help lessen the extent of ischemic damage during stroke, ultimately reducing stroke severity and improving outcomes.
Hypertension is another major stroke risk factor, and the Mediterranean diet aids in regulating blood pressure [92–95]. The diet promotes potassium intake while reducing sodium consumption, essential for maintaining healthy blood pressure. In addition, the Mediterranean diet enhances NO bioavailability, promoting endothelium-mediated vasodilation and lowering blood pressure [96–100]. Better endothelial function not only aids in blood pressure regulation but also reduces the risk of clot formation, further lowering stroke risk [101]. The Mediterranean diet’s emphasis on whole foods, healthy fats, and nutrient balance supports weight management [102], which is also important for blood pressure control and stroke prevention, as obesity-related metabolic syndrome is a known risk factor for both.
The Mediterranean diet’s anti-inflammatory properties are another key factor in stroke prevention [103, 104]. Chronic inflammation drives the progression of atherosclerosis and other vascular diseases, with inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6) linked to plaque instability and rupture [105–107]. The Mediterranean diet’s rich content of omega-3 fatty acids, polyphenols, and fiber lowers systemic inflammation, reducing these markers and mitigating the inflammatory processes that contribute to vascular disease [103, 104]. Polyphenols, including resveratrol, activate endogenous antioxidant defenses, such as Nrf2-regulated antioxidative responses and SIRT1-mediated cellular stress resilience pathways [108, 109], and reduce both mitochondria-derived and NADPH oxidase derived ROS production, attenuating cellular oxidative stress and inhibiting redox sensitive pro-inflammatory signaling mechanism. Omega-3 fatty acids shift immune cells toward an anti-inflammatory state, reducing their contribution to atherosclerosis [110, 111]. Additionally, the diet’s fiber content promotes gut health, fostering the production of short-chain fatty acids [112–114], which have systemic anti-inflammatory effects.
The Mediterranean diet also exerts anti-aging effects, further enhancing its role in reducing stroke risk [18, 115]. Aging contributes to the development of atherosclerosis [116] and stroke through mechanisms such as oxidative stress, heightened state of inflammation [105–107], mitochondrial dysfunction [117–120], and cellular senescence [121]. The Mediterranean diet reduces oxidative stress, a key factor in vascular aging, by providing antioxidants that neutralize ROS [17, 122–124]. This protects the endothelium from oxidative macromolecular damage and its downstream consequences as well from activation of redox sensitive pro-inflammatory, pro-atherogenic pathways. Oxidative stress impairs endothelial function by depleting NO, leading to vasoconstriction and a higher risk of thrombosis. By preserving NO availability and reducing ROS levels, the Mediterranean diet promotes endothelial health contributing to protection against stroke.
Mitochondrial dysfunction, characterized by dysregulated expression of the mitochondrial electron transport chain, reduced energy production, increased ROS generation and decreased mitochondrial antioxidant defenses, accelerates aging and contributes to both macrovascular diseases [125, 126] and microvascular pathologies [127] and endothelial functional impairment [128]. The Mediterranean diet enhances mitochondrial efficiency and promotes biogenesis through components like polyphenols [18, 115]. Omega-3 fatty acids also help maintain mitochondrial function and membrane integrity [115, 129], reducing oxidative damage associated with aging. Additionally, the anti-inflammatory and antioxidant properties of the Mediterranean diet likely help reduce the accumulation of senescent cells [18, 122], which secrete pro-inflammatory factors contributing to the pathogenesis of atherosclerosis [116, 130–134]. Autophagy, a process by which cells remove damaged components and recycle them for energy, plays a key role in aging and vascular health [135–138]. Components of the Mediterranean diet have been shown to enhance autophagy [139–141], promoting cellular repair and reducing the buildup of damaged proteins and organelles that contribute to cellular aging. In conclusion, the Mediterranean diet exerts its vasoprotective effects through a combination of anti-atherogenic, antioxidative, anti-inflammatory, and anti-aging mechanisms. These interconnected processes—improved lipid metabolism, blood pressure regulation, enhanced endothelial function, reduced inflammation, and support of mitochondrial health—contribute to the diet’s ability to prevent atherosclerosis and reduce the risk of stroke.
The Mediterranean diet’s protective effects may also be mediated through epigenetic mechanisms [18, 142–144]. Key components of the diet have been shown to influence gene expression by modulating epigenetic markers, including DNA methylation and histone acetylation [142]. These modifications play a crucial role in regulating pathways associated with inflammation, oxidative stress, and vascular function. For example, polyphenols like resveratrol can activate SIRT1, a histone deacetylase linked to improved endothelial function and reduced oxidative damage [145, 146]. By targeting fundamental pathways involved in epigenetic regulation of cellular aging processes, the Mediterranean diet provides an additional layer of protection against stroke and other age-related diseases [143, 144].
The protective effects of the Mediterranean diet, as demonstrated by the findings of this meta-analysis, have substantial public health implications. The consistent evidence supporting the Mediterranean diet’s role in reducing stroke risk highlights its potential as a powerful preventive strategy. Given the significant burden of stroke, particularly in countries like Hungary [1–3], where stroke mortality rates are among the highest in Europe, promoting adherence to the Mediterranean diet could become a pivotal element in public health initiatives aimed at reducing stroke incidence and mortality. According to the World Health Organization, stroke is the third leading cause of death in the country, with an age-standardized mortality rate that underscores the severity of the problem [1–3]. The high prevalence of stroke in Hungary reflects broader issues related to unhealthy aging, particularly poor dietary habits, which are key contributors to the country’s cardiovascular disease burden [147–152]. In response to this crisis, the Semmelweis Study—a prospective workplace cohort study—was initiated to investigate the underlying causes of unhealthy aging and to develop targeted interventions [153]. One such intervention is the Semmelweis-EUniWell Workplace Health Promotion Program, which seeks to address the specific causes of unhealthy aging, with a focus on improving dietary habits. By clarifying the relationship between the Mediterranean diet and stroke risk, this meta-analysis offers critical insights that will inform the development and refinement of both the Semmelweis Study and the Workplace Health Promotion Program. Integrating the Mediterranean diet into such national programs has the potential to address dietary inadequacies, particularly in the workplace setting, where interventions can reach large segments of the population.
In conclusion, this meta-analysis presents compelling evidence that adherence to the Mediterranean diet is associated with a substantial reduction in stroke risk. While the results are encouraging, further research is necessary to address the observed heterogeneity and investigate the mechanisms underlying the diet’s protective effects. Continued exploration in this area will be crucial for developing tailored dietary recommendations and public health strategies to mitigate the global burden of stroke.
Funding
Open access funding provided by Semmelweis University. This work was supported by grants from the National Institute on Aging (RF1AG072295, R01AG055395, R01AG068295; R01AG070915), the National Institute of Neurological Disorders and Stroke (R01NS100782), the National Cancer Institute (R01CA255840). This work was also supported by TKP2021-NKTA-47, implemented with the support provided by the Ministry of Innovation and Technology of Hungary from the National Research, Development and Innovation Fund, financed under the TKP2021-NKTA funding scheme; by funding through the National Cardiovascular Laboratory Program (RRF-2.3.1–21-2022–00003) and by the National Laboratory for Drug Research and Development (PharmaLab, RRF-2.3.1–21-2022–00015) provided by the Ministry of Innovation and Technology of Hungary from the National Research, Development and Innovation Fund; by the Semmelweis Momentum Programme; Project no. 135784 implemented with the support provided from the National Research, Development and Innovation Fund of Hungary, financed under the K20 funding scheme and the European University for Well-Being (EUniWell) program (grant agreement number: 101004093/ EUniWell/EAC-A02-2019 / EAC-A02-2019–1). The computational infrastructure of A5 Genetics Ltd (Kutaso, Hungary) was used for the study. This work was also supported by the EKÖP-2024–2 and EKÖP-2024–9 New National Excellence Program of the Ministry for Culture and Innovation from the source of the National Research, Development and Innovation Fund. The funding sources had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the American Heart Association, or the Presbyterian Health Foundation. We acknowledge the inspiration drawn from early studies by Artúr Görgey [154]. The 4o version of ChatGPT, developed by OpenAI, was used as a language tool to refine our writing and enhancing the clarity of our work. The support of ELIXIR Hungary is acknowledged.
Declarations
Competing interests
Dr. Balázs Győrffy serves as Associate Editor for GeroScience. Dr. Zoltan Ungvari serves as Editor-in-Chief for GeroScience and has personal relationships with individuals involved in the submission of this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zoltan Ungvari, Mónika Fekete, and Péter Varga contributed equally to this manuscript.
References
- 1.“Global Burden of Disease Stroke Risk Factor Collaborators:” Global, regional, and national burden of stroke and its risk factors, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 2024;23:973–1003. 10.1016/S1474-4422(24)00369-7 [DOI] [PubMed]
- 2.Wu S, Liu M. Global burden of stroke: dynamic estimates to inform action. Lancet Neurol. 2024;23:952–3. 10.1016/S1474-4422(24)00363-6. [DOI] [PubMed] [Google Scholar]
- 3.Chen X, Zheng J, Wang J, Wang H, Shi H, Jiang H, Shan P, Liu Q. Global burden and cross-country inequalities in stroke and subtypes attributable to diet from 1990 to 2019. BMC Public Health. 2024;24:1813. 10.1186/s12889-024-19337-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salerno P, Motairek I, Dong W, Nasir K, Fotedar N, Omran SS, Ganatra S, Hahad O, Deo SV, Rajagopalan S, Al-Kindi SG. County-level socio-environmental factors associated with stroke mortality in the United States: a cross-sectional study. Angiology. 2024;33197241244814. 10.1177/00033197241244814 [DOI] [PMC free article] [PubMed]
- 5.Kazi DS, Elkind MSV, Deutsch A, Dowd WN, Heidenreich P, Khavjou O, Mark D, Mussolino ME, Ovbiagele B, Patel SS, Poudel R, Weittenhiller B, Powell-Wiley TM, Joynt Maddox KE, American HA. Forecasting the economic burden of cardiovascular disease and stroke in the United States through 2050: a presidential advisory from the American Heart Association. Circulation. 2024;150:e89–101. 10.1161/CIR.0000000000001258. [DOI] [PubMed] [Google Scholar]
- 6.Joynt Maddox KE, Elkind MSV, Aparicio HJ, Commodore-Mensah Y, de Ferranti SD, Dowd WN, Hernandez AF, Khavjou O, Michos ED, Palaniappan L, Penko J, Poudel R, Roger VL, Kazi DS, American HA. Forecasting the burden of cardiovascular disease and stroke in the United States through 2050-prevalence of risk factors and disease: a Presidential Advisory From the American Heart Association. Circulation. 2024;150:e65–88. 10.1161/CIR.0000000000001256. [DOI] [PubMed] [Google Scholar]
- 7.Soto A, Guillen-Grima F, Morales G, Munoz S, Aguinaga-Ontoso I. Trends in mortality from stroke in the European Union, 1996–2015. Eur J Neurol. 2021;28:182–91. 10.1111/ene.14517. [DOI] [PubMed] [Google Scholar]
- 8.Saulle R, Lia L, De Giusti M, La Torre G. A systematic overview of the scientific literature on the association between Mediterranean Diet and the Stroke prevention. Clin Ter. 2019;170:e396–408. 10.7417/ct.2019.2166. [DOI] [PubMed] [Google Scholar]
- 9.Chen GC, Neelakantan N, Martin-Calvo N, Koh WP, Yuan JM, Bonaccio M, Iacoviello L, Martinez-Gonzalez MA, Qin LQ, van Dam RM. Adherence to the Mediterranean diet and risk of stroke and stroke subtypes. Eur J Epidemiol. 2019;34:337–49. 10.1007/s10654-019-00504-7. [DOI] [PubMed] [Google Scholar]
- 10.Liyanage T, Ninomiya T, Wang A, Neal B, Jun M, Wong MG, Jardine M, Hillis GS, Perkovic V. Effects of the Mediterranean diet on cardiovascular outcomes—a systematic review and meta-analysis. PLoS One. 2016;11:e0159252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sebastian SA, Padda I, Johal G. Long-term impact of Mediterranean diet on cardiovascular disease prevention: a systematic review and meta-analysis of randomized controlled trials. Curr Probl Cardiol. 2024;49:102509. [DOI] [PubMed] [Google Scholar]
- 12.Grosso G, Marventano S, Yang J, Micek A, Pajak A, Scalfi L, Galvano F, Kales SN. A comprehensive meta-analysis on evidence of Mediterranean diet and cardiovascular disease: are individual components equal? Crit Rev Food Sci Nutr. 2017;57:3218–32. [DOI] [PubMed] [Google Scholar]
- 13.Kontogianni MD, Panagiotakos DB. Dietary patterns and stroke: a systematic review and re-meta-analysis. Maturitas. 2014;79:41–7. [DOI] [PubMed] [Google Scholar]
- 14.Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N. Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol. 2013;74:580–91. [DOI] [PubMed] [Google Scholar]
- 15.Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2019;58:173–91. 10.1007/s00394-017-1582-0. [DOI] [PubMed] [Google Scholar]
- 16.Godos J, Scazzina F, Paterno Castello C, Giampieri F, Quiles JL, Briones Urbano M, Battino M, Galvano F, Iacoviello L, de Gaetano G, Bonaccio M, Grosso G. Underrated aspects of a true Mediterranean diet: understanding traditional features for worldwide application of a “Planeterranean” diet. J Transl Med. 2024;22:294. 10.1186/s12967-024-05095-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tosti V, Bertozzi B, Fontana L. Health Benefits of the Mediterranean Diet: metabolic and molecular mechanisms. J Gerontol A Biol Sci Med Sci. 2018;73:318–26. 10.1093/gerona/glx227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shannon OM, Ashor AW, Scialo F, Saretzki G, Martin-Ruiz C, Lara J, Matu J, Griffiths A, Robinson N, Lilla L, Stevenson E, Stephan BCM, Minihane AM, Siervo M, Mathers JC. Mediterranean diet and the hallmarks of ageing. Eur J Clin Nutr. 2021;75:1176–92. 10.1038/s41430-020-00841-x. [DOI] [PubMed] [Google Scholar]
- 19.Rees K, Takeda A, Martin N, Ellis L, Wijesekara D, Vepa A, Das A, Hartley L, Stranges S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2019;3:CD009825. 10.1002/14651858.CD009825.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corella D, Coltell O, Macian F, Ordovas JM. Advances in understanding the molecular basis of the Mediterranean diet effect. Annu Rev Food Sci Technol. 2018;9:227–49. 10.1146/annurev-food-032217-020802. [DOI] [PubMed] [Google Scholar]
- 21.Ungvari Z, Fekete M, Fekete JT, Grosso G, Ungvari A, Gyorffy B. Adherence to the Mediterranean diet and its protective effects against colorectal cancer: a meta-analysis of 26 studies with 2,217,404 participants. Geroscience. 2024. 10.1007/s11357-11024-01296-11359. 10.1007/s11357-024-01296-9 [DOI] [PMC free article] [PubMed]
- 22.Godos J, Ferri R, Lanza G, Caraci F, Vistorte AOR, Yelamos Torres V, Grosso G, Castellano S. Mediterranean diet and sleep features: a systematic review of current evidence. Nutrients. 2024;16:282. 10.3390/nu16020282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nucci D, Nardi M, Cinnirella A, Campagnoli E, Maffeo M, Perrone PM, Shishmintseva V, Grosso FM, Castrofino A, Castaldi S, Romano L, Gianfredi V. Adherence to Mediterranean diet and risk of pancreatic cancer: systematic review and meta-analysis. Int J Environ Res Public Health. 2023;20:2403. 10.3390/ijerph20032403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Godos J, Grosso G, Ferri R, Caraci F, Lanza G, Al-Qahtani WH, Caruso G, Castellano S. Mediterranean diet, mental health, cognitive status, quality of life, and successful aging in southern Italian older adults. Exp Gerontol. 2023;175:112143. 10.1016/j.exger.2023.112143. [DOI] [PubMed] [Google Scholar]
- 25.Godos J, Castellano S, Ferri R, Caraci F, Lanza G, Scazzina F, Alanazi AM, Marx W, Galvano F, Grosso G. Mediterranean diet and chronotype: data from Italian adults and systematic review of observational studies. Exp Gerontol. 2023;181:112284. 10.1016/j.exger.2023.112284. [DOI] [PubMed] [Google Scholar]
- 26.Godos J, Ferri R, Caraci F, Cosentino FII, Castellano S, Galvano F, Grosso G. Adherence to the Mediterranean diet is associated with better sleep quality in Italian adults. Nutrients. 2019;11:976. 10.3390/nu11050976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marventano S, Godos J, Platania A, Galvano F, Mistretta A, Grosso G. Mediterranean diet adherence in the Mediterranean healthy eating, aging and lifestyle (MEAL) study cohort. Int J Food Sci Nutr. 2018;69:100–7. 10.1080/09637486.2017.1332170. [DOI] [PubMed] [Google Scholar]
- 28.Grosso G, Pajak A, Mistretta A, Marventano S, Raciti T, Buscemi S, Drago F, Scalfi L, Galvano F. Protective role of the Mediterranean diet on several cardiovascular risk factors: evidence from Sicily, southern Italy. Nutr Metab Cardiovasc Dis. 2014;24:370–7. 10.1016/j.numecd.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 29.Grosso G, Mistretta A, Marventano S, Purrello A, Vitaglione P, Calabrese G, Drago F, Galvano F. Beneficial effects of the Mediterranean diet on metabolic syndrome. Curr Pharm Des. 2014;20:5039–44. 10.2174/1381612819666131206112144. [DOI] [PubMed] [Google Scholar]
- 30.Svezia B, Cabiati M, Matteucci M, Passino C, Pe ME, Lionetti V, Del Ry S. Tuscany Sangiovese grape juice imparts cardioprotection by regulating gene expression of cardioprotective C-type natriuretic peptide. Eur J Nutr. 2020;59:2953–68. 10.1007/s00394-019-02134-x. [DOI] [PubMed] [Google Scholar]
- 31.Lionetti V, Tuana BS, Casieri V, Parikh M, Pierce GN. Importance of functional food compounds in cardioprotection through action on the epigenome. Eur Heart J. 2019;40:575–82. 10.1093/eurheartj/ehy597. [DOI] [PubMed] [Google Scholar]
- 32.Casieri V, Matteucci M, Cavallini C, Torti M, Torelli M, Lionetti V. Long-term intake of pasta containing barley (1–3)beta-D-glucan increases neovascularization-mediated cardioprotection through endothelial upregulation of vascular endothelial growth factor and parkin. Sci Rep. 2017;7:13424. 10.1038/s41598-017-13949-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agostini S, Chiavacci E, Matteucci M, Torelli M, Pitto L, Lionetti V. Barley beta-glucan promotes MnSOD expression and enhances angiogenesis under oxidative microenvironment. J Cell Mol Med. 2015;19:227–38. 10.1111/jcmm.12442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andreo-Lopez MC, Contreras-Bolivar V, Munoz-Torres M, Garcia-Fontana B, Garcia-Fontana C. Influence of the Mediterranean diet on healthy aging. Int J Mol Sci. 2023;24:4491. 10.3390/ijms24054491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castello A, Rodriguez-Barranco M, de Larrea NF, Jakszyn P, Dorronsoro A, Amiano P, Chirlaque MD, Colorado-Yohar S, Guevara M, Moreno-Iribas C, Pollan M, Sanchez MJ. Adherence to the Western, Prudent and Mediterranean dietary patterns and colorectal cancer risk: findings from the Spanish Cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Spain). Nutrients. 2022;14:3085. 10.3390/nu14153085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation. 2009;119:1093–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gardener H, Wright CB, Gu Y, Demmer RT, Boden-Albala B, Elkind MS, Sacco RL, Scarmeas N. Mediterranean-style diet and risk of ischemic stroke, myocardial infarction, and vascular death: the Northern Manhattan Study. Am J Clin Nutr. 2011;94:1458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hoevenaar-Blom MP, Nooyens AC, Kromhout D, Spijkerman AM, Beulens JW, Van Der Schouw YT, Bueno-de-Mesquita B, Verschuren WM. Mediterranean style diet and 12-year incidence of cardiovascular diseases: the EPIC-NL cohort study. PLoS One. 2012;7:e45458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chan R, Chan D, Woo J. The association of a priori and a posterior dietary patterns with the risk of incident stroke in Chinese older people in Hong Kong. J Nutr Health Aging. 2013;17:866–74. [DOI] [PubMed] [Google Scholar]
- 40.Tognon G, Lissner L, Sæbye D, Walker KZ, Heitmann BL. The Mediterranean diet in relation to mortality and CVD: a Danish cohort study. Br J Nutr. 2014;111:151–9. [DOI] [PubMed] [Google Scholar]
- 41.Tektonidis TG, Åkesson A, Gigante B, Wolk A, Larsson SC. A Mediterranean diet and risk of myocardial infarction, heart failure and stroke: a population-based cohort study. Atherosclerosis. 2015;243:93–8. [DOI] [PubMed] [Google Scholar]
- 42.Tsivgoulis G, Psaltopoulou T, Wadley VG, Alexandrov AV, Howard G, Unverzagt FW, Moy C, Howard VJ, Kissela B, Judd SE. Adherence to a Mediterranean diet and prediction of incident stroke. Stroke. 2015;46:780–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stefler D, Malyutina S, Kubinova R, Pajak A, Peasey A, Pikhart H, Brunner EJ, Bobak M. Mediterranean diet score and total and cardiovascular mortality in Eastern Europe: the HAPIEE study. Eur J Nutr. 2017;56:421–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aigner A, Becher H, Jacobs S, Wilkens LR, Boushey CJ, Le Marchand L, Haiman CA, Maskarinec G. Low diet quality and the risk of stroke mortality: the multiethnic cohort study. Eur J Clin Nutr. 2018;72:1035–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Galbete C, Kröger J, Jannasch F, Iqbal K, Schwingshackl L, Schwedhelm C, Weikert C, Boeing H, Schulze MB. Nordic diet, Mediterranean diet, and the risk of chronic diseases: the EPIC-Potsdam study. BMC Med. 2018;16:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paterson KE, Myint PK, Jennings A, Bain LK, Lentjes MA, Khaw K-T, Welch AA. Mediterranean diet reduces risk of incident stroke in a population with varying cardiovascular disease risk profiles. Stroke. 2018;49:2415–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Agnoli C, Krogh V, Grioni S, Sieri S, Palli D, Masala G, Sacerdote C, Vineis P, Tumino R, Frasca G. A priori–defined dietary patterns are associated with reduced risk of stroke in a large Italian cohort. J Nutr. 2011;141:1552–8. [DOI] [PubMed] [Google Scholar]
- 48.Misirli G, Benetou V, Lagiou P, Bamia C, Trichopoulos D, Trichopoulou A. Relation of the traditional Mediterranean diet to cerebrovascular disease in a Mediterranean population. Am J Epidemiol. 2012;176:1185–92. [DOI] [PubMed] [Google Scholar]
- 49.Schröder H, Salas-Salvadó J, Martínez-González MA, Fíto M, Corella D, Estruch R, Ros E. Baseline adherence to the Mediterranean diet and major cardiovascular events: Prevención con Dieta Mediterránea trial. JAMA Intern Med. 2014;174:1690–2. [DOI] [PubMed] [Google Scholar]
- 50.Bonaccio M, Di Castelnuovo A, Pounis G, Costanzo S, Persichillo M, Cerletti C, Donati MB, de Gaetano G, Iacoviello L, Investigators M-SS. High adherence to the Mediterranean diet is associated with cardiovascular protection in higher but not in lower socioeconomic groups: prospective findings from the Moli-sani study. Int J Epidemiol. 2017;46:1478–87. [DOI] [PubMed] [Google Scholar]
- 51.Veglia F, Baldassarre D, de Faire U, Kurl S, Smit AJ, Rauramaa R, Giral P, Amato M, Di Minno A, Ravani A. A priori-defined Mediterranean-like dietary pattern predicts cardiovascular events better in north Europe than in Mediterranean countries. Int J Cardiol. 2019;282:88–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, Willett WC, Rimm EB, Hu FB. Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation. 2015;132:2212–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.González-Padilla E, Tao Z, Sánchez-Villegas A, Álvarez-Pérez J, Borné Y, Sonestedt E. Association between adherence to Swedish Dietary Guidelines and Mediterranean Diet and Risk of Stroke in a Swedish Population. Nutrients. 2022;14(6):1253. 10.3390/nu14061253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Livingstone KM, Abbott G, Bowe SJ, Ward J, Milte C, McNaughton SA. Diet quality indices, genetic risk and risk of cardiovascular disease and mortality: a longitudinal analysis of 77 004 UK Biobank participants. BMJ Open. 2021;11:e045362. 10.1136/bmjopen-2020-045362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shan Z, Li Y, Baden MY, Bhupathiraju SN, Wang DD, Sun Q, Rexrode KM, Rimm EB, Qi L, Willett WC, Manson JE, Qi Q, Hu FB. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med. 2020;180:1090–100. 10.1001/jamainternmed.2020.2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li J, Guasch-Ferré M, Chung W, Ruiz-Canela M, Toledo E, Corella D, Bhupathiraju SN, Tobias DK, Tabung FK, Hu J. The Mediterranean diet, plasma metabolome, and cardiovascular disease risk. Eur Heart J. 2020;41:2645–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Delgado-Lista J, Alcala-Diaz JF, Torres-Peña JD, Quintana-Navarro GM, Fuentes F, Garcia-Rios A, Ortiz-Morales AM, Gonzalez-Requero AI, Perez-Caballero AI, Yubero-Serrano EM, Rangel-Zuñiga OA, Camargo A, Rodriguez-Cantalejo F, Lopez-Segura F, Badimon L, Ordovas JM, Perez-Jimenez F, Perez-Martinez P, Lopez-Miranda J. Long-term secondary prevention of cardiovascular disease with a Mediterranean diet and a low-fat diet (CORDIOPREV): a randomised controlled trial. Lancet. 2022;399:1876–85. 10.1016/s0140-6736(22)00122-2. [DOI] [PubMed] [Google Scholar]
- 58.Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–90. [DOI] [PubMed] [Google Scholar]
- 59.Singh RB, Dubnov G, Niaz MA, Ghosh S, Singh R, Rastogi SS, Manor O, Pella D, Berry EM. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): a randomised single-blind trial. Lancet. 2002;360:1455–61. 10.1016/s0140-6736(02)11472-3. [DOI] [PubMed] [Google Scholar]
- 60.de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99:779–85. [DOI] [PubMed] [Google Scholar]
- 61.Yau WY, Hankey GJ. Which dietary and lifestyle behaviours may be important in the aetiology (and prevention) of stroke? J Clin Neurosci. 2011;18:76–80. 10.1016/j.jocn.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 62.Kastorini CM, Milionis HJ, Ioannidi A, Kalantzi K, Nikolaou V, Vemmos KN, Goudevenos JA, Panagiotakos DB. Adherence to the Mediterranean diet in relation to acute coronary syndrome or stroke nonfatal events: a comparative analysis of a case/case-control study. Am Heart J. 2011;162:717–24. 10.1016/j.ahj.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 63.El-Hajj M, Salameh P, Rachidi S, Al-Hajje A, Hosseini H. Adherence to the Mediterranean diet decreases the risk of stroke in the Lebanese population: a case-control study. Pharm Pract (Granada). 2021;19:2157. 10.18549/PharmPract.2021.1.2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Maalouf E, Hallit S, Salameh P, Hosseini H. Eating behaviors, lifestyle, and ischemic stroke: a Lebanese case-control study. Int J Environ Res Public Health. 2023;20(2):1487. 10.3390/ijerph20021487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lavados PM, Mazzon E, Rojo A, Brunser AM, Olavarría VV. Pre-stroke adherence to a Mediterranean diet pattern is associated with lower acute ischemic stroke severity: a cross-sectional analysis of a prospective hospital-register study. BMC Neurol. 2020;20:252. 10.1186/s12883-020-01824-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tong TYN, Imamura F, Monsivais P, Brage S, Griffin SJ, Wareham NJ, Forouhi NG. Dietary cost associated with adherence to the Mediterranean diet, and its variation by socio-economic factors in the UK Fenland Study. Br J Nutr. 2018;119:685–94. 10.1017/S0007114517003993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moreiras-Varela O. The Mediterranean diet in Spain. Eur J Clin Nutr. 1989;43(Suppl 2):83–7. [PubMed] [Google Scholar]
- 68.Van Diepen S, Scholten AM, Korobili C, Kyrli D, Tsigga M, Van Dieijen T, Kotzamanidis C, Grammatikopoulou MG. Greater Mediterranean diet adherence is observed in Dutch compared with Greek university students. Nutr Metab Cardiovasc Dis. 2011;21:534–40. 10.1016/j.numecd.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 69.da Silva R, Bach-Faig A, Raido Quintana B, Buckland G, de Almeida MDV, Serra-Majem L. Worldwide variation of adherence to the Mediterranean diet, in 1961–1965 and 2000–2003. Public Health Nutr. 2009;12:1676–84. 10.1017/S1368980009990541. [DOI] [PubMed] [Google Scholar]
- 70.Gundogdu A, Nalbantoglu OU. The role of the Mediterranean diet in modulating the gut microbiome: a review of current evidence. Nutrition. 2023;114:112118. 10.1016/j.nut.2023.112118. [DOI] [PubMed] [Google Scholar]
- 71.Martucci M, Ostan R, Biondi F, Bellavista E, Fabbri C, Bertarelli C, Salvioli S, Capri M, Franceschi C, Santoro A. Mediterranean diet and inflammaging within the hormesis paradigm. Nutr Rev. 2017;75:442–55. 10.1093/nutrit/nux013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Grosso G, Mistretta A, Frigiola A, Gruttadauria S, Biondi A, Basile F, Vitaglione P, D’Orazio N, Galvano F. Mediterranean diet and cardiovascular risk factors: a systematic review. Crit Rev Food Sci Nutr. 2014;54:593–610. 10.1080/10408398.2011.596955. [DOI] [PubMed] [Google Scholar]
- 73.Fernandez de la Puente M, Hernandez-Alonso P, Canudas S, Marti A, Fito M, Razquin C, Salas-Salvado J. Modulation of telomere length by Mediterranean diet, caloric restriction, and exercise: results from PREDIMED-Plus study. Antioxidants (Basel). 2021;10(10):1596. 10.3390/antiox10101596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wolff E, Vergnes MF, Portugal H, Defoort C, Amiot-Carlin MJ, Lairon D, Nicolay A. Cholesterol-absorber status modifies the LDL cholesterol-lowering effect of a Mediterranean-type diet in adults with moderate cardiovascular risk factors. J Nutr. 2011;141:1791–8. 10.3945/jn.111.141333. [DOI] [PubMed] [Google Scholar]
- 75.Hernaez A, Castaner O, Goday A, Ros E, Pinto X, Estruch R, Salas-Salvado J, Corella D, Aros F, Serra-Majem L, Martinez-Gonzalez MA, Fiol M, Lapetra J, de la Torre R, Lopez-Sabater MC, Fito M. The Mediterranean Diet decreases LDL atherogenicity in high cardiovascular risk individuals: a randomized controlled trial. Mol Nutr Food Res. 2017;61(9):1601015. 10.1002/mnfr.201601015. [DOI] [PubMed] [Google Scholar]
- 76.Bedard A, Corneau L, Lamarche B, Dodin S, Lemieux S. Sex differences in the impact of the Mediterranean diet on LDL particle size distribution and oxidation. Nutrients. 2015;7:3705–23. 10.3390/nu7053705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Barona J, Jones JJ, Kopec RE, Comperatore M, Andersen C, Schwartz SJ, Lerman RH, Fernandez ML. A Mediterranean-style low-glycemic-load diet increases plasma carotenoids and decreases LDL oxidation in women with metabolic syndrome. J Nutr Biochem. 2012;23:609–15. 10.1016/j.jnutbio.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mediterranean diet delivers a punch to LDL cholesterol. Mayo Clin Health Lett. 2011;29:4. 10.1007/s11306-019-1579-1 [PubMed]
- 79.Zhu C, Sawrey-Kubicek L, Beals E, Hughes RL, Rhodes CH, Sacchi R, Zivkovic AM. The HDL lipidome is widely remodeled by fast food versus Mediterranean diet in 4 days. Metabolomics. 2019;15:114. 10.1007/s11306-019-1579-1. [DOI] [PubMed] [Google Scholar]
- 80.Sanllorente A, Soria-Florido MT, Castaner O, Lassale C, Salas-Salvado J, Martinez-Gonzalez MA, Subirana I, Ros E, Corella D, Estruch R, Tinahones FJ, Hernaez A, Fito M. A lifestyle intervention with an energy-restricted Mediterranean diet and physical activity enhances HDL function: a substudy of the PREDIMED-Plus randomized controlled trial. Am J Clin Nutr. 2021;114:1666–74. 10.1093/ajcn/nqab246. [DOI] [PubMed] [Google Scholar]
- 81.Rodriguez-Garcia E, Ruiz-Nava J, Santamaria-Fernandez S, Fernandez-Garcia JC, Vargas-Candela A, Yahyaoui R, Tinahones FJ, Bernal-Lopez MR, Gomez-Huelgas R. Implications of the Mediterranean diet and physical exercise on the lipid profile of metabolically healthy obese women as measured by nuclear magnetic resonance spectroscopy ((1)H NMR). Chem Phys Lipids. 2018;213:68–75. 10.1016/j.chemphyslip.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 82.Estruch R, Camafort M. The Mediterranean diet and plasma lipid profile. Rev Esp Cardiol (Engl Ed). 2015;68:279–81. 10.1016/j.rec.2014.11.021. [DOI] [PubMed] [Google Scholar]
- 83.Di Lorenzo L, Vimercati L, Pipoli A, Manghisi NM, Lampignano L, Caputi A, De Maria L, Zupo R, De Pergola G. Interplay between adherence to the Mediterranean diet and lipid profile: a comparative survey between day-time healthcare and non-healthcare female workers. Front Public Health. 2021;9:649760. 10.3389/fpubh.2021.649760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Delgado M, Gutierrez A, Cano MD, Castillo MJ. Elimination of meat, fish, and derived products from the Spanish-Mediterranean diet: effect on the plasma lipid profile. Ann Nutr Metab. 1996;40:202–11. 10.1159/000177915. [DOI] [PubMed] [Google Scholar]
- 85.Bedard A, Corneau L, Vohl MC, Dodin S, Lemieux S. Effect of the Mediterranean diet on the lipid-lipoprotein profile: is it influenced by the family history of dyslipidemia? J Nutrigenet Nutrigenomics. 2014;7:177–87. 10.1159/000374116. [DOI] [PubMed] [Google Scholar]
- 86.Harper CR, Jacobson TA. Beyond the Mediterranean diet: the role of omega-3 Fatty acids in the prevention of coronary heart disease. Prev Cardiol. 2003;6:136–46. 10.1111/j.1520-037x.2003.1332.x. [DOI] [PubMed] [Google Scholar]
- 87.Calder PC. The role of marine omega-3 (n-3) fatty acids in inflammatory processes, atherosclerosis and plaque stability. Mol Nutr Food Res. 2012;56:1073–80. 10.1002/mnfr.201100710. [DOI] [PubMed] [Google Scholar]
- 88.Fito M, Guxens M, Corella D, Saez G, Estruch R, de la Torre R, Frances F, Cabezas C, Lopez-Sabater MDC, Marrugat J, Garcia-Arellano A, Aros F, Ruiz-Gutierrez V, Ros E, Salas-Salvado J, Fiol M, Sola R, Covas MI, Investigators PS. Effect of a traditional Mediterranean diet on lipoprotein oxidation: a randomized controlled trial. Arch Intern Med. 2007;167:1195–203. 10.1001/archinte.167.11.1195. [DOI] [PubMed] [Google Scholar]
- 89.Toth P, Tarantini S, Csiszar A, Ungvari Z. Functional vascular contributions to cognitive impairment and dementia: mechanisms and consequences of cerebral autoregulatory dysfunction, endothelial impairment, and neurovascular uncoupling in aging. Am J Physiol Heart Circ Physiol. 2017;312:H1–20. 10.1152/ajpheart.00581.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Iadecola C. The neurovascular unit coming of age: a journey through neurovascular coupling in health and disease. Neuron. 2017;96:17–42. 10.1016/j.neuron.2017.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dalkara T, Arsava EM. Can restoring incomplete microcirculatory reperfusion improve stroke outcome after thrombolysis? J Cereb Blood Flow Metab. 2012;32:2091–9. 10.1038/jcbfm.2012.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.van Soest AP, Beers S, van de Rest O, de Groot LC. The Mediterranean-Dietary Approaches to Stop Hypertension Intervention for Neurodegenerative Delay (MIND) diet for the aging brain: a systematic review. Adv Nutr. 2024;15:100184. 10.1016/j.advnut.2024.100184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kokkinos P, Panagiotakos DB, Polychronopoulos E. Dietary influences on blood pressure: the effect of the Mediterranean diet on the prevalence of hypertension. J Clin Hypertens (Greenwich). 2005;7:165–70. 10.1111/j.1524-6175.2005.04079.x. (quiz 171-162). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen H, Dhana K, Huang Y, Huang L, Tao Y, Liu X, van Lent DM, Zheng Y, Ascherio A, Willett W, Yuan C. Association of the Mediterranean Dietary Approaches to Stop Hypertension Intervention for Neurodegenerative Delay (MIND) diet with the risk of dementia. JAMA Psychiatry. 2023;80:630–8. 10.1001/jamapsychiatry.2023.0800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Charles RL, Rudyk O, Prysyazhna O, Kamynina A, Yang J, Morisseau C, Hammock BD, Freeman BA, Eaton P. Protection from hypertension in mice by the Mediterranean diet is mediated by nitro fatty acid inhibition of soluble epoxide hydrolase. Proc Natl Acad Sci U S A. 2014;111:8167–72. 10.1073/pnas.1402965111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yubero-Serrano EM, Fernandez-Gandara C, Garcia-Rios A, Rangel-Zuniga OA, Gutierrez-Mariscal FM, Torres-Pena JD, Marin C, Lopez-Moreno J, Castano JP, Delgado-Lista J, Ordovas JM, Perez-Martinez P, Lopez-Miranda J. Mediterranean diet and endothelial function in patients with coronary heart disease: an analysis of the CORDIOPREV randomized controlled trial. PLoS Med. 2020;17:e1003282. 10.1371/journal.pmed.1003282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Torres-Pena JD, Rangel-Zuniga OA, Alcala-Diaz JF, Lopez-Miranda J, Delgado-Lista J. Mediterranean diet and endothelial function: a review of its effects at different vascular bed levels. Nutrients. 2020;12(8):2212. 10.3390/nu12082212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Torres-Pena JD, Garcia-Rios A, Delgado-Casado N, Gomez-Luna P, Alcala-Diaz JF, Yubero-Serrano EM, Gomez-Delgado F, Leon-Acuna A, Lopez-Moreno J, Camargo A, Tinahones FJ, Delgado-Lista J, Ordovas JM, Perez-Martinez P, Lopez-Miranda J. Mediterranean diet improves endothelial function in patients with diabetes and prediabetes: a report from the CORDIOPREV study. Atherosclerosis. 2018;269:50–6. 10.1016/j.atherosclerosis.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 99.Shannon OM, Mendes I, Kochl C, Mazidi M, Ashor AW, Rubele S, Minihane AM, Mathers JC, Siervo M. Mediterranean diet increases endothelial function in adults: a systematic review and meta-analysis of randomized controlled trials. J Nutr. 2020;150:1151–9. 10.1093/jn/nxaa002. [DOI] [PubMed] [Google Scholar]
- 100.Rallidis LS, Lekakis J, Kolomvotsou A, Zampelas A, Vamvakou G, Efstathiou S, Dimitriadis G, Raptis SA, Kremastinos DT. Close adherence to a Mediterranean diet improves endothelial function in subjects with abdominal obesity. Am J Clin Nutr. 2009;90:263–8. 10.3945/ajcn.2008.27290. [DOI] [PubMed] [Google Scholar]
- 101.Capurso C, Massaro M, Scoditti E, Vendemiale G, Capurso A. Vascular effects of the Mediterranean diet part I: anti-hypertensive and anti-thrombotic effects. Vascul Pharmacol. 2014;63:118–26. 10.1016/j.vph.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 102.Dominguez LJ, Veronese N, Di Bella G, Cusumano C, Parisi A, Tagliaferri F, Ciriminna S, Barbagallo M. Mediterranean diet in the management and prevention of obesity. Exp Gerontol. 2023;174:112121. 10.1016/j.exger.2023.112121. [DOI] [PubMed] [Google Scholar]
- 103.Itsiopoulos C, Mayr HL, Thomas CJ. The anti-inflammatory effects of a Mediterranean diet: a review. Curr Opin Clin Nutr Metab Care. 2022;25:415–22. 10.1097/MCO.0000000000000872. [DOI] [PubMed] [Google Scholar]
- 104.Estruch R. Anti-inflammatory effects of the Mediterranean diet: the experience of the PREDIMED study. Proc Nutr Soc. 2010;69:333–40. 10.1017/S0029665110001539. [DOI] [PubMed] [Google Scholar]
- 105.Libby P. Inflammation and the pathogenesis of atherosclerosis. Vascul Pharmacol. 2024;154:107255. 10.1016/j.vph.2023.107255. [DOI] [PubMed] [Google Scholar]
- 106.Soehnlein O, Libby P. Targeting inflammation in atherosclerosis - from experimental insights to the clinic. Nat Rev Drug Discov. 2021;20:589–610. 10.1038/s41573-021-00198-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Libby P. The changing landscape of atherosclerosis. Nature. 2021;592:524–33. 10.1038/s41586-021-03392-8. [DOI] [PubMed] [Google Scholar]
- 108.Price NL, Gomes AP, Ling AJ, Duarte FV, Martin-Montalvo A, North BJ, Agarwal B, Ye L, Ramadori G, Teodoro JS, Hubbard BP, Varela AT, Davis JG, Varamini B, Hafner A, Moaddel R, Rolo AP, Coppari R, Palmeira CM, de Cabo R, Baur JA, Sinclair DA. SIRT1 is required for AMPK activation and the beneficial effects of resveratrol on mitochondrial function. Cell Metab. 2012;15:675–90. 10.1016/j.cmet.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Danz ED, Skramsted J, Henry N, Bennett JA, Keller RS. Resveratrol prevents doxorubicin cardiotoxicity through mitochondrial stabilization and the Sirt1 pathway. Free Radic Biol Med. 2009;46:1589–1597. S0891–5849(09)00154–3 [pii] 10.1016/j.freeradbiomed.2009.03.011 [DOI] [PubMed]
- 110.Simonetto M, Infante M, Sacco RL, Rundek T, Della-Morte D. A novel anti-inflammatory role of Omega-3 PUFAs in prevention and treatment of atherosclerosis and vascular cognitive impairment and dementia. Nutrients. 2019;11(10):2279. 10.3390/nu11102279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Laye S, Nadjar A, Joffre C, Bazinet RP. Anti-inflammatory effects of omega-3 fatty acids in the brain: physiological mechanisms and relevance to pharmacology. Pharmacol Rev. 2018;70:12–38. 10.1124/pr.117.014092. [DOI] [PubMed] [Google Scholar]
- 112.Seethaler B, Nguyen NK, Basrai M, Kiechle M, Walter J, Delzenne NM, Bischoff SC. Short-chain fatty acids are key mediators of the favorable effects of the Mediterranean diet on intestinal barrier integrity: data from the randomized controlled LIBRE trial. Am J Clin Nutr. 2022;116:928–42. 10.1093/ajcn/nqac175. [DOI] [PubMed] [Google Scholar]
- 113.Nagpal R, Neth BJ, Wang S, Craft S, Yadav H. Modified Mediterranean-ketogenic diet modulates gut microbiome and short-chain fatty acids in association with Alzheimer’s disease markers in subjects with mild cognitive impairment. EBioMedicine. 2019;47:529–42. 10.1016/j.ebiom.2019.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Joseph J, Depp C, Shih PB, Cadenhead KS, Schmid-Schonbein G. Modified Mediterranean diet for enrichment of short chain fatty acids: potential adjunctive therapeutic to target immune and metabolic dysfunction in schizophrenia? Front Neurosci. 2017;11:155. 10.3389/fnins.2017.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pollicino F, Veronese N, Dominguez LJ, Barbagallo M. Mediterranean diet and mitochondria: new findings. Exp Gerontol. 2023;176:112165. 10.1016/j.exger.2023.112165. [DOI] [PubMed] [Google Scholar]
- 116.Ungvari Z, Tarantini S, Sorond F, Merkely B, Csiszar A. Mechanisms of vascular aging, a geroscience perspective: JACC focus seminar. J Am Coll Cardiol. 2020;75:931–41. 10.1016/j.jacc.2019.11.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Madamanchi NR, Runge MS. Mitochondrial dysfunction in atherosclerosis. Circ Res. 2007;100:460–473. 100/4/460 [pii] 10.1161/01.RES.0000258450.44413.96 [DOI] [PubMed]
- 118.Sobenin IA, Zhelankin AV, Sinyov VV, Bobryshev YV, Orekhov AN. Mitochondrial aging: focus on mitochondrial DNA damage in atherosclerosis - a mini-review. Gerontology. 2015;61:343–9. 10.1159/000368923. [DOI] [PubMed] [Google Scholar]
- 119.Wang Y, Wang W, Wang N, Tall AR, Tabas I. Mitochondrial oxidative stress promotes atherosclerosis and neutrophil extracellular traps in aged mice. Arterioscler Thromb Vasc Biol. 2017;37:e99–107. 10.1161/ATVBAHA.117.309580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yu E, Calvert PA, Mercer JR, Harrison J, Baker L, Figg NL, Kumar S, Wang JC, Hurst LA, Obaid DR, Logan A, West NE, Clarke MC, Vidal-Puig A, Murphy MP, Bennett MR. Mitochondrial DNA damage can promote atherosclerosis independently of reactive oxygen species through effects on smooth muscle cells and monocytes and correlates with random-effect plaques in humans. Circulation. 2013;128:702–12. 10.1161/CIRCULATIONAHA.113.002271. [DOI] [PubMed] [Google Scholar]
- 121.Nyul-Toth A, Patai R, Csiszar A, Ungvari A, Gulej R, Mukli P, Yabluchanskiy A, Benyo Z, Sotonyi P, Prodan CI, Liotta EM, Toth P, Elahi F, Barsi P, Maurovich-Horvat P, Sorond FA, Tarantini S, Ungvari Z. Linking peripheral atherosclerosis to blood-brain barrier disruption: elucidating its role as a manifestation of cerebral small vessel disease in vascular cognitive impairment. Geroscience. 2024. 10.1007/s11357-024-01194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ali S, Davinelli S, Accardi G, Aiello A, Caruso C, Duro G, Ligotti ME, Pojero F, Scapagnini G, Candore G. Healthy ageing and Mediterranean diet: a focus on hormetic phytochemicals. Mech Ageing Dev. 2021;200:111592. 10.1016/j.mad.2021.111592. [DOI] [PubMed] [Google Scholar]
- 123.Dai J, Jones DP, Goldberg J, Ziegler TR, Bostick RM, Wilson PW, Manatunga AK, Shallenberger L, Jones L, Vaccarino V. Association between adherence to the Mediterranean diet and oxidative stress. Am J Clin Nutr. 2008;88:1364–70. 10.3945/ajcn.2008.26528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ambring A, Friberg P, Axelsen M, Laffrenzen M, Taskinen MR, Basu S, Johansson M. Effects of a Mediterranean-inspired diet on blood lipids, vascular function and oxidative stress in healthy subjects. Clin Sci (Lond). 2004;106:519–25. 10.1042/CS20030315. [DOI] [PubMed] [Google Scholar]
- 125.Ali MA, Gioscia-Ryan R, Yang D, Sutton NR, Tyrrell DJ. Cardiovascular aging: spotlight on mitochondria. Am J Physiol Heart Circ Physiol. 2024;326:H317–33. 10.1152/ajpheart.00632.2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ungvari Z, Tarantini S, Donato AJ, Galvan V, Csiszar A. Mechanisms of vascular aging. Circ Res. 2018;123:849–67. 10.1161/CIRCRESAHA.118.311378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sakamuri SS, Sure VN, Kolli L, Evans WR, Sperling JA, Bix GJ, Wang X, Atochin DN, Murfee WL, Mostany R, Katakam PV. Aging related impairment of brain microvascular bioenergetics involves oxidative phosphorylation and glycolytic pathways. J Cereb Blood Flow Metab. 2022;42:1410–24. 10.1177/0271678X211069266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tarantini S, Valcarcel-Ares NM, Yabluchanskiy A, Fulop GA, Hertelendy P, Gautam T, Farkas E, Perz A, Rabinovitch PS, Sonntag WE, Csiszar A, Ungvari Z. Treatment with the mitochondrial-targeted antioxidant peptide SS-31 rescues neurovascular coupling responses and cerebrovascular endothelial function and improves cognition in aged mice. Aging Cell. 2018;17. 10.1111/acel.12731 [DOI] [PMC free article] [PubMed]
- 129.Lalia AZ, Dasari S, Robinson MM, Abid H, Morse DM, Klaus KA, Lanza IR. Influence of omega-3 fatty acids on skeletal muscle protein metabolism and mitochondrial bioenergetics in older adults. Aging (Albany NY). 2017;9:1096–129. 10.18632/aging.101210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Grootaert MOJ, Moulis M, Roth L, Martinet W, Vindis C, Bennett MR, De Meyer GRY. Vascular smooth muscle cell death, autophagy and senescence in atherosclerosis. Cardiovasc Res. 2018;114:622–34. 10.1093/cvr/cvy007. [DOI] [PubMed] [Google Scholar]
- 131.Uryga AK, Bennett MR. Ageing induced vascular smooth muscle cell senescence in atherosclerosis. J Physiol. 2016;594:2115–24. 10.1113/JP270923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Childs BG, Baker DJ, Wijshake T, Conover CA, Campisi J, van Deursen JM. Senescent intimal foam cells are deleterious at all stages of atherosclerosis. Science. 2016;354:472–7. 10.1126/science.aaf6659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gray K, Kumar S, Figg N, Harrison J, Baker L, Mercer J, Littlewood T, Bennett M. Effects of DNA damage in smooth muscle cells in atherosclerosis. Circ Res. 2015;116:816–26. 10.1161/CIRCRESAHA.116.304921. [DOI] [PubMed] [Google Scholar]
- 134.Gardner SE, Humphry M, Bennett MR, Clarke MC. Senescent vascular smooth muscle cells drive inflammation through an interleukin-1alpha-dependent senescence-associated secretory phenotype. Arterioscler Thromb Vasc Biol. 2015;35:1963–74. 10.1161/ATVBAHA.115.305896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kim JW, Nam SA, Koh ES, Kim HW, Kim S, Woo JJ, Kim YK. The impairment of endothelial autophagy accelerates renal senescence by ferroptosis and NLRP3 inflammasome signaling pathways with the disruption of endothelial barrier. Antioxidants (Basel). 2024;13(8):886. 10.3390/antiox13080886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Marzoog BA. Endothelial cell aging and autophagy dysregulation. Cardiovasc Hematol Agents Med Chem. 2024. 10.2174/0118715257275690231129101408. [DOI] [PubMed] [Google Scholar]
- 137.Mai S, Brehm N, Auburger G, Bereiter-Hahn J, Jendrach M. Age-related dysfunction of the autophago-lysosomal pathway in human endothelial cells. Pflugers Arch. 2019;471:1065–78. 10.1007/s00424-019-02288-x. [DOI] [PubMed] [Google Scholar]
- 138.Han Q, Yu Y, Liu X, Guo Y, Shi J, Xue Y, Li Y. The role of endothelial cell mitophagy in age-related cardiovascular diseases. Aging Dis. 2024. 10.14336/AD.2024.0788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Tocci G, Biondi-Zoccai G, Forte M, Gallo G, Nardoianni G, Fiori E, D’Ambrosio L, Di Pietro R, Stefanini G, Cannata F, Rocco E, Simeone B, Sarto G, Schirone L, D’Amico A, Peruzzi M, Nocella C, Volpe M, Rubattu S. Effects of two-month treatment with a mixture of natural activators of autophagy on oxidative stress and arterial stiffness in patients with essential hypertension: a pilot study. Nutr Metab Cardiovasc Dis. 2023;33:2287–93. 10.1016/j.numecd.2023.07.026. [DOI] [PubMed] [Google Scholar]
- 140.Guo H, Chen Y, Liao L, Wu W. Resveratrol protects HUVECs from oxidized-LDL induced oxidative damage by autophagy upregulation via the AMPK/SIRT1 pathway. Cardiovasc Drugs Ther. 2013;27:189–98. 10.1007/s10557-013-6442-4. [DOI] [PubMed] [Google Scholar]
- 141.Chen ML, Yi L, Jin X, Liang XY, Zhou Y, Zhang T, Xie Q, Zhou X, Chang H, Fu YJ, Zhu JD, Zhang QY, Mi MT. Resveratrol attenuates vascular endothelial inflammation by inducing autophagy through the cAMP signaling pathway. Autophagy. 2013;9:2033–45. 10.4161/auto.26336. [DOI] [PubMed] [Google Scholar]
- 142.Gensous N, Garagnani P, Santoro A, Giuliani C, Ostan R, Fabbri C, Milazzo M, Gentilini D, di Blasio AM, Pietruszka B, Madej D, Bialecka-Debek A, Brzozowska A, Franceschi C, Bacalini MG. One-year Mediterranean diet promotes epigenetic rejuvenation with country- and sex-specific effects: a pilot study from the NU-AGE project. Geroscience. 2020;42:687–701. 10.1007/s11357-019-00149-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Hoffmann A, Meir AY, Hagemann T, Czechowski P, Muller L, Engelmann B, Haange SB, Rolle-Kampczyk U, Tsaban G, Zelicha H, Rinott E, Kaplan A, Shelef I, Stumvoll M, Bluher M, Liang L, Ceglarek U, Isermann B, von Bergen M, Kovacs P, Keller M, Shai I. A polyphenol-rich green Mediterranean diet enhances epigenetic regulatory potential: the DIRECT PLUS randomized controlled trial. Metabolism. 2023;145:155594. 10.1016/j.metabol.2023.155594. [DOI] [PubMed] [Google Scholar]
- 144.Mantilla-Escalante DC, Lopez de Las Hazas MC, Crespo MC, Martin-Hernandez R, Tome-Carneiro J, Del Pozo-Acebo L, Salas-Salvado J, Bullo M, Davalos A. Mediterranean diet enriched in extra-virgin olive oil or nuts modulates circulating exosomal non-coding RNAs. Eur J Nutr. 2021;60:4279–4293. 10.1007/s00394-021-02594-0 [DOI] [PubMed]
- 145.Bernier M, Wahl D, Ali A, Allard J, Faulkner S, Wnorowski A, Sanghvi M, Moaddel R, Alfaras I, Mattison JA, Tarantini S, Tucsek Z, Ungvari Z, Csiszar A, Pearson KJ, de Cabo R. Resveratrol supplementation confers neuroprotection in cortical brain tissue of nonhuman primates fed a high-fat/sucrose diet. Aging (Albany NY). 2016;8:899–916. 10.18632/aging.100942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Toth P, Tarantini S, Tucsek Z, Ashpole NM, Sosnowska D, Gautam T, Ballabh P, Koller A, Sonntag WE, Csiszar A, Ungvari ZI. Resveratrol treatment rescues neurovascular coupling in aged mice:role of improved cerebromicrovascular endothelial function and down-regulation of NADPH oxidas. Am J Physiol Heart Circ Physiol. 2014;306:H299–308. ajpheart.00744.2013 [pii]10.1152/ajpheart.00744.2013 [DOI] [PMC free article] [PubMed]
- 147.Bardos H, Llanaj E, Vincze F, Dioszegi J, Piko P, Kosa Z, Sandor J, Adany R. Diet quality as assessed by Healthy Eating Index-2015 among Hungarian Roma living in settlements of Northeast Hungary. Sci Rep. 2022;12:19213. 10.1038/s41598-022-23670-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Schreiberne Molnar E, Nagy-Lorincz Z, Nagy B, Bakacs M, Kis O, Sarkadi Nagy E, Martos E. [Hungarian Diet and Nutritional Status Survey - The OTAP2014 study. V. Vitamin intake of the Hungarian population]. Orv Hetil. 2017;158:1302–1313. 10.1556/650.2017.30832 [DOI] [PubMed]
- 149.Sarkadi Nagy E, Bakacs M, Illes E, Nagy B, Varga A, Kis O, Schreiberne Molnar E, Martos E. [Hungarian Diet and Nutritional Status Survey - OTAP2014. II. Energy and macronutrient intake of the Hungarian population]. Orv Hetil. 2017;158:587–597. 10.1556/650.2017.30718 [DOI] [PubMed]
- 150.Nagy B, Nagy-Lorincz Z, Bakacs M, Illes E, Sarkadi Nagy E, Martos E. [Hungarian Diet and Nutritional Status Survey - OTAP2014. III. Macroelement intake of the Hungarian population]. Orv Hetil. 2017;158:653–661. 10.1556/650.2017.30744 [DOI] [PubMed]
- 151.Nagy B, Nagy-Lorincz Z, Bakacs M, Illes E, Sarkadi Nagy E, Erdei G, Martos E. [Hungarian Diet and Nutritional Status Survey - The OTAP2014 study. IV. Microelement intake of the Hungarian population]. Orv Hetil. 2017;158:803–810. 10.1556/650.2017.30773 [DOI] [PubMed]
- 152.Erdei G, Kovacs VA, Bakacs M, Martos E. [Hungarian Diet and Nutritional Status Survey 2014. I. Nutritional status of the Hungarian adult population]. Orv Hetil. 2017;158:533–540. 10.1556/650.2017.30700 [DOI] [PubMed]
- 153.Ungvari Z, Tabak AG, Adany R, Purebl G, Kaposvari C, Fazekas-Pongor V, Csipo T, Szarvas Z, Horvath K, Mukli P, Balog P, Bodizs R, Ujma P, Stauder A, Belsky DW, Kovacs I, Yabluchanskiy A, Maier AB, Moizs M, Ostlin P, Yon Y, Varga P, Voko Z, Papp M, Takacs I, Vasarhelyi B, Torzsa P, Ferdinandy P, Csiszar A, Benyo Z, et al. The Semmelweis Study: a longitudinal occupational cohort study within the framework of the Semmelweis Caring University Model Program for supporting healthy aging. Geroscience. 2024;46:191–218. 10.1007/s11357-023-01018-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Görgey A. Über die festen, flüchtigen, fetten Säueren des Cocusnussöles. In: Sitzungsberichte der mathematisch-naturwissenschaftlichen Classe der k. Akademie der Wissenschaften in Wien. . Vienna: Akademie der Wissenschaften in Wien. ; 1848:208-227.