Abstract
Background
With the rapid advancement of digital transformation, digital health literacy (DHL) has emerged as a crucial determinant influencing health outcomes and health inequalities among older adults. However, empirical evidence on how DHL affects health inequalities remains relatively limited. This study aims to investigate the association between DHL and health inequalities while analyzing the potential mechanisms through which DHL exerts its influence via mechanism testing among older adults in China.
Methods
From June to November 2024, a multicenter cross-sectional study was conducted by five research groups from four universities in China. DHL was assessed using the eHEALS scale, while health inequalities were measured using an index of relative deprivation. Multivariate regression models examined the association between DHL and health inequalities. The Baron and Kenny stepwise regression method was used to examine the mediating effect, and bias-corrected bootstrap resampling with 5000 iterations was applied to calculate 95% confidence intervals (95% CI) to confirm the significance of the mediating effect.
Results
Overall, 8696 valid individuals were included. DHL demonstrated a significant positive association with self-rated health (SRH) (coef = 0.015, P < .01) and a significant negative association with health inequalities (coef = −0.016, P < .01). DHL indirectly reduced health inequalities through the mediating effects of alleviating depressive symptoms (coef = −0.005, 95%CI: −0.0066, −0.0045) and promoting physical activity (coef = −0.001, 95%CI: −0.0020, −0.0011), respectively. However, the role in promoting health service utilization and regulating unhealthy behaviors was not significant. Bootstrap tests confirmed the significance of the mediating role.
Conclusion
DHL was associated with health inequalities and mitigates them by alleviating depressive symptoms and promoting physical activity. It is recommended that while bridging the digital divide, more attention could be paid to DHL and the translation of competencies among older adults to reduce health disparities and promote equitable aging.
Keywords: Digital health literacy, health inequalities, mediating effect, older adults, capability theory, multicenter study
Introduction
Population aging has emerged as a defining global demographic trend, with the World Health Organization (WHO) predicting that the number of individuals aged 60 years and older will double to 2.1 billion by 2050. 1 As the world's second most populous country, China is witnessing a continuous increase in its older population, experiencing an unprecedented rate of population aging. 2 This demographic shift not only heightens the demand for health services but also presents the complex challenge of sustaining and enhancing the health, well-being, and quality of life of older adults.3,4 However, the health status of older adults is uneven, and these disparities are increasingly accentuated by a combination of social determinants, such as socio-economic status, level of education, and geographic differences, resulting in so-called health inequalities.5–7 Health inequalities refer to systematic and avoidable differences in health status or outcomes that can be observed between different populations, among social groups within the same population, or across populations ranked by social status.8,9 These inequalities not only undermine social equity but also have extensive negative implications for both individual and societal well-being. Consequently, addressing health inequalities among older adults has become a critical focus of social and public health policy and research.
An important social transformation accompanying population aging is the increasing digitization of society. According to the 55th Statistical Report on Internet Development in China, by the end of 2024, the number of Internet users in China reached 1.1 billion, with an Internet penetration rate of 78.6%. Notably, the proportion of Internet users aged 50 and above has risen to 34.1%, indicating a deeper integration of digital technologies among middle-aged and older adults. 10 However, substantial disparities in digital technology usage persist among older adults.11,12 For older adults, the popularization of the Internet has brought convenience but has also exposed them to the challenges of the digital divide. The debate regarding the impact of digital technology on the health of the older population remains contentious, with differing perspectives on its potential positive and negative effects.13–16 Nevertheless, it is an irrefutable fact that “digital” is increasingly emerging as a critical determinant of health inequities within this group.17–19
The Three-Level Digital Divide Theory posits the existence of three distinct levels of digital disparity: the access divide, the usage divide, and the outcomes divide.20–23 This theory has elicited widespread concern regarding the social inequalities engendered by digital disparities. However, as digital technologies continue to penetrate and interact with social realities, the access divide appears to be narrowing, 24 while the usage divide and the outcomes divide persist, especially among vulnerable groups. Furthermore, the limitations of research that has disproportionately focused on the access divide have become increasingly evident. First, the physical aspect of the access divide has been overemphasized, with existing research predominantly relying on a dichotomous perspective of “to have or not to have” (e.g., whether or not one has access to the Internet), thereby ignoring the actual capacity of individuals to utilize the Internet. Second, current research often adheres to the arbitrary logic of technological determinism, which assumes that real value and health capital accumulation can be generated by ensuring access. However, digital technologies are embedded in specific social structures and cultural environments, leading to significant differences in the perceived functions, motivations for use, and health benefits of technologies among various social groups. 25
This context underscores the significance of digital health literacy (DHL), which is recognized as a key factor in achieving health outcomes and promoting equitable access to health services.26–30 DHL is defined as the ability to seek, find, understand, and evaluate health information from the digital environment and translate it into health knowledge and actions that can be applied to address or solve health problems.31,32 Compared to traditional health literacy, DHL places more emphasis on information processing and judgment in a digitally mediated environment, including understanding and using online healthcare delivery platforms, social media health messaging and remote health monitoring tools, etc. Research indicated that DHL is significantly associated with health-related behaviors, health management skills, health service utilization, and quality of life among older adults.28,33–35 However, empirical evidence on how DHL affects health inequalities in the older population remains relatively limited. Therefore, we conducted this study to explore the association between DHL and health inequalities and further analyzed the potential mechanisms of DHL's role through mechanism testing.
Theoretical analysis and research hypotheses
Amartya Sen's capability theory
The capability theory, developed by Amartya Sen, provides a novel analytical perspective for understanding digital technology use and health inequalities. The theory posits that measuring an individual's well-being should not focus solely on the resources available to them, but should examine whether the individual can transform resources into beneficial health outcomes.36–38 In this study, the theory breaks through the previously discussed over-focus on physical access and use and arbitrary technological determinism and instead focuses on how individuals convert digital health resources into actual health outcomes. In other words, only when DHL is improved can digitalization bring about higher levels of health outcomes and more equitable health opportunities for older adults.
Research has demonstrated that acquiring skills in retrieving, judging, and applying health information online can empower individuals with greater autonomy and decision-making power for disease prevention and health management.39–41 DHL is significantly and positively associated with personal health outcomes, as evidenced by improved self-rated health, disease course control, and quality of life. 25 So we proposed the hypothesis:
H1: DHL is positively associated with self-rated health among older adults
Health inequalities are the result of a combination of social structural disadvantages, unequal distribution of resources, and individual differences in ability. 5 In the digital age, despite government efforts to allocate healthcare resources at the macro level, individuals with limited DHL continue to face challenges in using available digital health resources for the translation and improvement of health outcomes, exacerbating existing health disparities. 42 So, we hypothesize:
H2: DHL is negatively associated with health inequalities among older adults
However, the impact of DHL on health inequalities may not be all directly accomplished, and there are still potential mediating pathways to be explored. Previous studies showed that DHL significantly increased willingness to exercise for health,43–45 and evidence from China and Denmark further confirmed that DHL was positively correlated with physical activity levels.46,47 Additionally, the interventions based on digital health have also been shown to improve physical mobility, reduce the risk of falls, and improve HRQoL.48,49 Thus, we posit that DHL could make it easier for older adults to access and externalize scientific exercise instruction and advice into physical activity, which in turn would improve their health and alleviate health inequalities. So, we hypothesize:
H3-1: DHL could alleviate health inequalities by promoting physical activity
One Hungary study suggested that DHL is associated with healthcare utilization. 50 Reviewed studies also have highlighted the growing adoption of digital health technologies and the Internet for services such as online appointment scheduling, virtual consultations with healthcare providers, and access to health-related information. 25 Those with higher levels of DHL are more likely to utilize health information in the online medium as a judge of their illness and thus complete disease control and management earlier, resulting in more beneficial health outcomes. Therefore, we predicted that digital health literacy can improve healthcare utilization to alleviate health inequalities.
H3-2: DHL could alleviate health inequalities by increasing utilization of health services
DHL is an expansion of health literacy in the digital environment, where health literacy enhancement enhances an individual's health awareness, risk perception, and self-regulation, thereby promoting healthy behaviors. Studies have reported the association between DHL and healthy lifestyles.39,51 A study in China found the enhancement of DHL reduces smoking behavior among community residents, 52 and another smartwatch-based smoking cessation intervention study reported that digital health warning message prompts could motivate them to smoking cessation. 53 Thus, we hypothesized:
H3-3: DHL could alleviate health inequalities by curbing unhealthy behaviors
Many studies have shown that digital technology use is strongly associated with mental health, yet conclusions about this effect are controversial. However, there is consensus in numerous studies regarding the protective effects of DHL on mental health.54–56 In large-scale surveys of older adults in the United States and Asia, DHL was associated with reductions in depressive symptoms 57 and anxiety. 58 DHL is a reflective measure of the ability to utilize digital technology to address health issues. Higher DHL groups are more likely to use online information resources to resolve their negative feelings or seek mental health service. 59 Thus, we hypothesize that:
H3-4: DHL could alleviate health inequalities by suppressing depressive symptoms
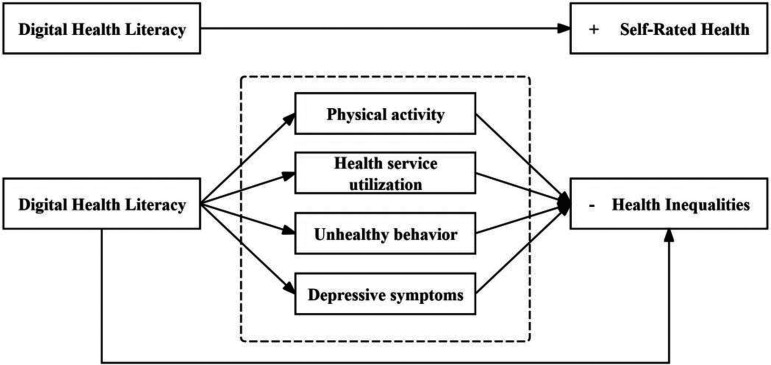
In summary, the framework of this study is shown in Figure 1.
Figure 1.
The framework of this study.
Methods
Study design
A multicenter cross-sectional study was conducted in collaboration with five research groups from four universities in China. All research groups implemented a standardized study protocol simultaneously to ensure methodological consistency. A multi-stage sampling strategy was employed to guarantee representativeness. First, 1–2 provinces were randomly selected from each of the eastern, central, and western regions of China to account for regional economic and social differences. Within each selected province, 1–2 prefectural cities or counties were chosen based on their levels of economic development to reflect the diversity within the province. Subsequently, cluster sampling was applied in these regions, with communities (or rural villages) designated as the primary sampling units. Whole cohort enrollment was used for older adults who met the inclusion criteria in the selected communities and villages.
The required sample size was calculated based on the proportion formula: , where n is the sample size, Z is the Z-score corresponding to the desired confidence level, p is the estimated proportion, and d is the allowable margin of error. Our study was prepared and initiated in 2023. We determined the P-value based on the latest Statistical Report on the Internet Development Situation in China (Issue 51) published by the China Internet Network Information Center (CNNIC) at the time, which showed that the Internet penetration rate of Chinese older adults was 54.5%. 60 We set the margin of error ( ) at 0.012, with a Z-score of 1.96 corresponding to a 95% confidence level. Based on these parameters, the calculated minimum sample size was 6616 participants. To account for potential non-response and invalid samples, an additional 20% was added, resulting in a final target sample size of 7940 participants.
Data collection and participants
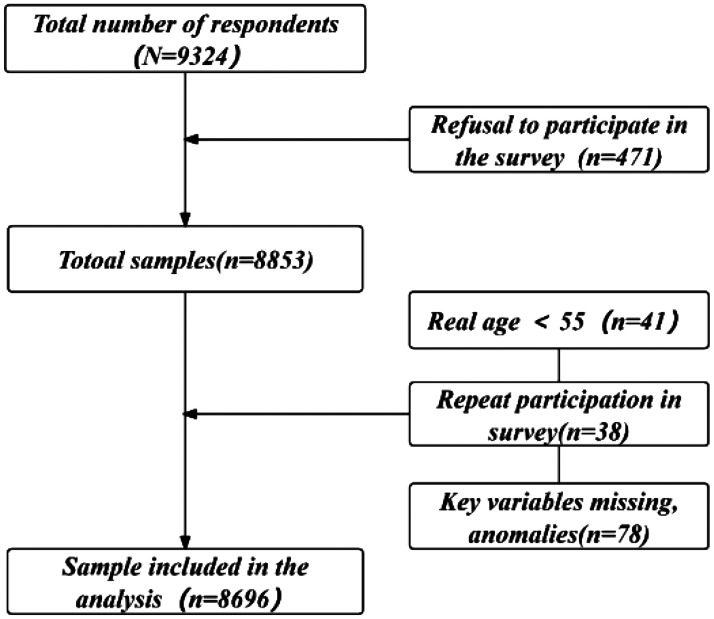
The data collection process was conducted from June to November 2024 by trained enumerators who coordinated with village councils or community workers. After obtaining the participants’ agreement and written informed consent, trained investigators conducted one-on-one interviews using paper-based questionnaires in the homes of older adults. The survey covered various domains, including demographic and socioeconomic characteristics, health status, mental health, health behaviors, and DHL. To ensure data accuracy and reliability, the survey team leader rigorously reviewed each questionnaire for completeness and quality upon submission. Eligibility criteria for participation were: (1) permanent residents who had lived in the study area for 6 months or more; (2) age ≥ 55 years; (3) aware of and able to cooperate with the investigation. Exclusion criteria: (1) Those not living in the community or separated from their households for any reason during the survey period. (2) Older adults with terminal illnesses. (3) Older adults who refused to participate. The final study encompassed six prefectural-level cities under four provinces (Hubei (central China), Shandong (east coast of China), Jiangsu (eastern China), and Guangxi Zhuang Autonomous Region (western China)), including 45 rural and 11 urban communities. Samples with refusal to participate, duplicate measurements, and missing key variables were excluded, resulting in a final sample size of 8696. For further details, refer to Figure 2.
Figure 2.
Participant enrollment procedure.
Variable
Dependent variable
Self-rated health (SRH). SRH is widely used in research in health-related fields to measure an individual's overall health status and has been shown in several studies to be strongly correlated with objective health outcomes, including morbidity and mortality, with good validity and reliability in different countries and across different sociodemographic groups.61–64 In this study, SRH was measured using a single question, “How would you currently rate your health?” Participants were asked to respond on a 5-point Likert scale (1 for very poor, 2 for poor, 3 for fair, 4 for good, and 5 for very good). This approach is consistent with established health research methodologies and facilitates comparability with existing studies.
Health inequalities. Referring to Zhu and Wu's study,42,65 the relative deprivation (RD) index was employed to assess health inequalities at the individual level. This index was derived from an individual's SRH. According to the theory of relative deprivation, older adults with poorer health status are more likely to experience greater relative deprivation due to the accumulation of health disadvantages, thereby exacerbating their exposure to health inequalities.
According to Kakwani's research, 66 the index is calculated as follows: Assuming that H is a group containing n samples of the older adults, the distribution vector H = (h1, h2, h3, …, hn−1, hn), h1 ≤ h2 ≤ h3 ≤…hn, can be obtained as the distribution vector of SRH for the group, based on the SRH in order from smallest to largest. In comparing the j individual to the i individual, the relative deprivation of health for the ith individual can be expressed as follows:
| (1) |
In equation (1), the average health relative deprivation index for the i individual, representing the health inequalities, is calculated by summing over j and dividing the result by the mean SRH value of all older adults within the group, as follows:
| (2) |
In equation (2), denotes the mean value of SRH of all older adults in group H. denotes the mean value of samples exceeding in older adults group H, and is the ratio of the number of samples with SRH exceeding in group H to the total sample.
Independent variable
DHL. DHL was assessed using an 8-item scale developed by Norman and Skinner, 31 with the Chinese version revised and validated by Ma, 67 demonstrating strong reliability and validity. Items are rated on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree), yielding a total score between 8 and 40, where higher scores indicate greater DHL. The original scale Cronbach's alpha was 0.88, 31 and in this study Cronbach's alpha was 0.986, indicating good internal consistency and reliability of the instrument.
Intermediate variable
Physical activity. Physical activity was assessed by asking older adults to recall the frequency of their exercise sessions per week over the past year, using the following question: “In the past year, how many times a week did you exercise?”
Unhealthy behavior. Unhealthy behaviors encompass smoking and alcohol abuse. Participants’ responses to the questions, answered as “no” or “yes,” were assigned values of 0 and 1, respectively. These values were then summed, resulting in a total score for unhealthy behaviors that ranged from 0 to 2.
Health service utilization. Health service utilization was assessed by aggregating responses to two questions: “In the past year, did you receive outpatient care?” and “In the past year, were you hospitalized?” Responses were coded as 0 for “no” and 1 for “yes,” yielding a total score that ranges from 0 to 2.
Depressive symptoms. Depressive symptoms were utilized to reflect the mental health of older adults and were assessed using the Center for Epidemiologic Studies Depression Scale-10 (CESD-10). The reliability of the CESD-10 has been well-established among Chinese older adults.68,69 The CESD-10 measures the depression level of the respondents through 10 items, each item ranging from 0 to 3 points, with positive items, reverse scored, and the total score ranging from 0 to 30 points, with higher scores reflecting higher levels of depression. In this study, Cronbach's alpha was 0.885, indicating good internal consistency and reliability of the instrument.
Covariate variable. The set of variables that are to be controlled for in this study encompasses gender, age, hukou, education, marital status, living status, retirement, monthly income, chronic disease, insurance status, and regional disparity.
Statistical analysis and modeling
In the descriptive statistical analysis, continuous variables were summarized as mean ± standard deviation (M ± SD), while categorical variables were presented as frequencies and percentages (n, %). Since the measurement of health inequalities was based on SRH, examining whether DHL influences SRH is a logical prerequisite for constructing the health inequalities index. Consequently, this study first investigated the effect of DHL on SRH before analyzing the relationship between DHL and health inequalities. Given the ordinal nature of the SRH variables, an ordered probit regression (O-Probit) model was employed to assess the association between DHL and SRH.
| (3) |
In equation (3), represents latent continuous variable representing the underlying level of self-rated health; DHL is the key independent variable, digital health literacy; represents a series of control variables. , … are coefficients to be estimated; is the error term, assumed to follow a standard normal distribution N(0,1).
The observed ordinal variable is categorized based on thresholds , depending on the value of . Here , , , are threshold parameters to be estimated, satisfying the condition < < < .
| (4) |
Additionally, the ordinary least squares (OLS) model was utilized to estimate the relationship between DHL and health inequalities. In the OLS model, the dependent variable is , and the key independent variable is . represents a series of control variables. is an error term capturing the unobserved factor for the ith unit of observation. The model is specified as follows:
| (5) |
In the mechanism analysis stage, the Baron and Kenny stepwise method was applied to test the significance of the mediating variables, and bias-corrected Bootstrap resampling with 5000 iterations was used to calculate confidence intervals.
| (6) |
| (7) |
| (8) |
The regression equations (6)–(8) collectively test the mediating effect in three sequential steps. The first step tests the total effect of DHL on health inequalities, the second step tests the effect of DHL on the Med variable, and the third step places both the DHL and Med variables into the regression equation and observes the change in the regression coefficient of DHL and the significance of the two variables. All statistical tests were two-tailed, with a significance level set at P < .05. Data analyses were performed using Stata Version 17.0.
Results
Descriptive statistical variables
The average age of participants was 70.90 years (SD = 8.45), with the majority aged between 71 and 80. Among the participants, 42.41% (n = 3688) were male and 57.59% (n = 5008) were female, while 48.45% (n = 4213) had middle education. In terms of residency, 47.32%(n = 4115)lived in urban areas, and 52.68% (n = 4581) lived in rural areas. Regarding health status, 47.91% (n = 4166) reported good SRH. 67.64% (n = 5882) had one chronic disease, while 31.93% (n = 2777) reported multiple comorbidities. The average health inequalities among participants was 0.12 (SD = 0.14), with a DHL score of 20.22 (SD = 10.59) and a CESD-10 score of 5.72 (SD = 5.54). Detailed information can be found in Table 1.
Table 1.
Descriptive statistical analysis of variables.
| Variable | Type/M ± SD | n (%)/(Max, Min) |
|---|---|---|
| Gender | Male | 3688(42.41) |
| Female | 5008(57.59) | |
| Age (year) | 55–60 | 1022(11.75) |
| 61–65 | 1250(14.37) | |
| 66–70 | 2091(24.05) | |
| 71–80 | 3151(36.24) | |
| >80 | 1182(13.59) | |
| Hukou | Urban | 4115(47.32) |
| Rural | 4581(52.68) | |
| Education | No formal education | 1414(16.26) |
| Low education | 2698(31.03) | |
| Middle education | 4213(48.45) | |
| High education | 371(4.27) | |
| Marital status | Unmarried | 73(0.84) |
| Married or partnered | 6858(78.86) | |
| Divorced or widowed | 1765(20.3) | |
| Living status | Living alone | 1201(13.81) |
| Living with spouse | 4215(48.47) | |
| Living with spouse and children | 2288(26.31) | |
| Living with children | 810(9.31) | |
| Others | 182(2.09) | |
| Retirement | Retired | 6898(79.32) |
| Retired, still working | 1412(16.24) | |
| Employed | 386(4.44) | |
| Chronic disease | None | 37(0.43) |
| Only 1 chronic | 5882(67.64) | |
| Multimorbidity | 2777(31.93) | |
| Monthly income (yuan) | No income | 1273(14.64) |
| 1–1000 | 2338(26.89) | |
| 1001–2000 | 1122(12.9) | |
| 2001–5000 | 2832(32.57) | |
| 5001–10,000 | 807(9.28) | |
| >10,000 | 324(3.73) | |
| Health insurance | No | 163(1.87) |
| Yes | 8533(98.13) | |
| Pension insurance | No | 604(6.95) |
| Yes | 8092(93.05) | |
| SRH | Bad | 98(1.13) |
| Poor | 584(6.72) | |
| Fair | 2818(32.41) | |
| Good | 4166(47.91) | |
| Excellent | 1030(11.84) | |
| Number of children | 1.96 ± 0.2 | (0,2) |
| Health inequalities | 0.12 ± 0.14 | (0, 0.72) |
| DHL | 20.22 ± 10.59 | (8, 40) |
| Physical activity | 3.74 ± 3.33 | (0,21) |
| Unhealthy behaviors | 0.35 ± 0.63 | (0,2) |
| Health service utilization | 0.58 ± 0.70 | (0,2) |
| Depressive symptoms | 5.72 ± 5.54 | (0,30) |
Note: SRH, self-rated health; DHL, digital health literacy.
Correlation analysis among main study variables
To explore the association among the main study variables and to make a preliminary assessment of potential multicollinearity, Pearson correlation analysis was conducted. As shown in Table 2, all pairwise correlation coefficients were below 0.5 in absolute value, indicating weak to moderate relationships. These results suggest a low risk of multicollinearity among the core variables and support the appropriateness of proceeding with the subsequent regression analysis.
Table 2.
Correlation between main variables.
| Variables | Health inequalities | DHL | Depressive symptoms | Physical activity | Unhealthy behaviors | Health service utilization |
|---|---|---|---|---|---|---|
| Health inequalities | 1.000 | |||||
| DHL | −0.160*** | 1.000 | ||||
| Depressive symptoms | 0.319*** | −0.053*** | 1.000 | |||
| Physical activity | −0.153*** | 0.072*** | −0.280*** | 1.000 | ||
| Unhealthy behaviors | −0.037*** | 0.046*** | −0.016 | −0.045*** | 1.000 | |
| Health service utilization | 0.259*** | −0.108*** | −0.031*** | 0.073*** | −0.059*** | 1.000 |
Note: DHL, digital health literacy; *** P < .01, ** P < .05, * P < .10.
Regression analysis of DHL on SRH and health inequalities
To assess the multicollinearity among the independent variables, we conducted variance inflation factor (VIF) diagnostics in the full regression model. The results indicated that the maximum VIF was 2.47, the minimum was 1.02, and the mean VIF was 1.39, all well below the commonly accepted threshold of 10. These findings indicate that multicollinearity is unlikely to bias the estimates in our analysis. To enhance the interpretability of regression coefficients, we scaled the health inequalities by multiplying them by 10, which does not affect the direction or significance of the relationships but ensures coefficients are easier to interpret. Table 3 shows the results of the O-Probit and OLS regression, which indicate that DHL demonstrates a significant positive effect on SRH (coef = 0.015, P < .01) and a significant negative association with health inequalities (coef = −0.016, P < .01). Specifically, compared to urban, rural older adults had higher levels of SRH (coef = 0.247, P < .01) and lower health inequalities (coef = −0.133, P < .05). Education level was significantly positively associated with SRH and showed a gradient effect (e.g., coef = 0.195, P < .05 for high education), but no significant results were found for health inequalities. Living with spouse is associated with lower SRH (coef = −0.129, P < .05) and higher health inequalities (coef = 0.208, P < .01) while living in other non-standard arrangements (e.g., with relatives or in nursing homes) further exacerbate health inequalities (coef = 0.404, P < .01). Health insurance availability enhances SRH (coef = 0.286, P < .01) and reduces health inequalities (coef = −0.271, P < .05). Age and gender did not reveal statistical differences in either model.
Table 3.
DHL baseline regression for SRH and health inequalities.
| Variables | Model 1 | Model 2 |
|---|---|---|
| SRH | Health inequalities | |
| DHL | 0.015***(0.001) | −0.016***(0.002) |
| Gender: female (ref: male) | −0.017(0.025) | 0.028(0.029) |
| Age: 61–65 (ref: 55–60) | 0.057(0.048) | −0.066(0.049) |
| 66–70 | 0.060(0.045) | −0.061(0.048) |
| 71–80 | −0.014(0.045) | 0.016(0.047) |
| >80 | −0.071(0.054) | 0.119*(0.062) |
| Hukou: rural (ref: urban) | 0.247***(0.049) | −0.133**(0.055) |
| Education: low education (ref: no formal education) | 0.072*(0.038) | −0.092*(0.049) |
| Middle education | 0.112***(0.044) | −0.100*(0.055) |
| High education | 0.195**(0.077) | −0.117(0.088) |
| Marital status: married or partnered (ref: unmarried) | 0.548***(0.167) | −0.319(0.199) |
| Divorced or widowed | 0.401**(0.164) | −0.132(0.196) |
| Living status: living with spouse (ref: living alone) | −0.129**(0.059) | 0.208***(0.072) |
| Living with spouse and children | 0.034(0.061) | 0.043(0.074) |
| Living with children | 0.043(0.052) | 0.043(0.066) |
| Other (living with relatives, nursing homes) | −0.196*(0.101) | 0.404***(0.135) |
| Retirement: retired, still working (ref: retired, not working) | 0.030(0.040) | −0.021(0.048) |
| Employed | 0.290***(0.066) | −0.145**(0.064) |
| Chronic: only 1 chronic (ref: no) | 0.124(0.185) | −0.168(0.212) |
| Multimorbidity | −0.550***(0.186) | 0.600***(0.214) |
| Monthly income: 1–1000 (ref: no income) | 0.116***(0.042) | −0.097*(0.052) |
| 1001–2000 | 0.182***(0.053) | −0.173***(0.065) |
| 2001–5000 | 0.223***(0.054) | −0.169***(0.065) |
| 5001–10,000 | 0.310***(0.065) | −0.248***(0.077) |
| >10,001 | 0.375***(0.084) | −0.314***(0.094) |
| Health insurance: yes (ref: no) | 0.286***(0.095) | −0.271**(0.126) |
| Pension insurance: yes (ref: no) | −0.027(0.056) | −0.314***(0.094) |
| Number of children | −0.651***(0.078) | −0.045(0.067) |
| Province: Guangxi (ref: Shandong) | −0.478***(0.061) | 0.460***(0.070) |
| Jiangsu | −0.038(0.051) | 0.065(0.060) |
| Hubei | −0.475***(0.041) | 0.450***(0.052) |
| Constant | — | 1.529***(0.334) |
| Observations | 8696 | 8696 |
| Pseudo R2/R2 | 0.072 | 0.124 |
Note: SRH, self-rated health; DHL, digital health literacy. Robust standard errors in parentheses. *** P < .01, ** P < .05, * P < .10.
Mechanisms of DHL's effect on health inequalities
Table 4 demonstrates the regression results between the different mediating variables respectively with DHL. DHL exhibits a significant negative association with depressive symptoms (coef = −0.061, P < .01) and a significant positive association with physical activity (coef = 0.024, P < .01). The association between DHL and unhealthy behaviors and health service utilization was not significant.
Table 4.
The effect of DHL on the intermediate variable.
| Variable | Depressive symptoms | Physical activity | Unhealthy behavior | Health service utilization |
|---|---|---|---|---|
| DHL | −0.061***(0.006) | 0.024***(0.004) | 0.001(0.001) | −0.000(0.001) |
| Covariate variable | Control | Control | Control | Control |
| Constant | 14.326***(1.332) | 2.179***(0.714) | 0.626***(0.125) | 0.428***(0.165) |
| Observations | 8696 | 8696 | 8696 | 8696 |
| R2 | 0.244 | 0.156 | 0.284 | 0.187 |
Note: DHL, digital health literacy. Covariate variable: gender, age, Hukou, education, marital status, living status, retirement, monthly income, chronic disease, insurance status, number of children, and regional disparity. Robust standard errors in parentheses; *** P < .01, ** P < .05, * P < .10.
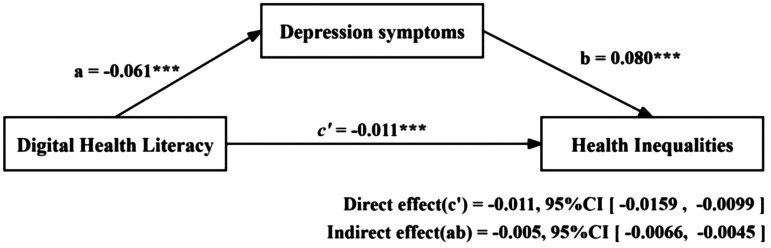
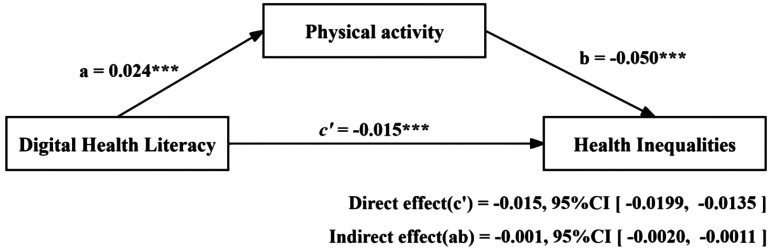
The Baron and Kenny stepwise method was employed to assess the mediating role of depressive symptoms and physical activity in the relationship between DHL and health inequalities. Table 5 and Figures 3 and 4 present the results of the mediation analysis. After controlling for covariates, DHL was found to be significantly negatively associated with health inequalities (Model 2: coef = −0.016, P < .01), and the relationship was attenuated but still significant after accounting for mediating variables (Model 4: coef = −0.011, P < .01 Model 6: coef = −0.015, P < .01). Bootstrap tests were used to further verify the significance of the mediating effects. Table 6 reports the bias-corrected nonparametric percentile confidence intervals for depressive symptoms and physical activity. DHL indirectly reduces health inequalities by suppressing depressive symptoms (coef = −0.005, 95%CI: −0.0066, −0.0045) and promoting physical activity (coef = −0.001, 95%CI: −0.0020, −0.0011), accounting for 31.25% and 6.25% of the total effect, respectively.
Table 5.
The mediating role of mediating variables (depressive symptoms, physical activity between DHL and health inequalities).
| Variables | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 |
|---|---|---|---|---|---|
| Health inequalities | Depressive symptoms | Health inequalities | Physical activity | Health inequalities | |
| DHL | −0.016***(0.002) | −0.061***(0.006) | −0.011***(0.002) | 0.024***(0.004) | −0.015***(0.002) |
| Depressive symptoms | 0.080***(0.004) | ||||
| Physical activity | −0.050***(0.005) | ||||
| Gender: female (ref: male) | 0.028(0.029) | 0.184(0.113) | 0.013(0.028) | 0.178**(0.071) | 0.037(0.029) |
| Age: 61–65 (ref: 55–60) | −0.066(0.049) | −0.331(0.213) | −0.039(0.049) | 0.095(0.125) | −0.061(0.049) |
| 66–70 | −0.061(0.048) | −0.322(0.204) | −0.035(0.047) | 0.318***(0.119) | −0.045(0.048) |
| 71–80 | 0.016(0.047) | −0.081(0.202) | 0.022(0.047) | 0.08(0.116) | 0.020(0.047) |
| >80 | 0.119*(0.062) | 0.129(0.248) | 0.109*(0.060) | −0.473***(0.146) | 0.095(0.062) |
| Hukou: rural (ref: urban) | −0.133**(0.055) | 1.083***(0.227) | −0.219***(0.053) | −0.058(0.131) | −0.136**(0.055) |
| Education: low education (ref: no formal education) | −0.092*(0.049) | 0.110(0.163) | −0.101**(0.046) | 0.103(0.109) | −0.087*(0.048) |
| Middle education | −0.100*(0.055) | −0.358*(0.188) | −0.071(0.051) | 0.282*(0.125) | −0.086(0.054) |
| High education | −0.117(0.088) | −0.125(0.346) | −0.107(0.084) | 0.420**(0.204) | −0.095(0.087) |
| Marital: married or partnered (ref: unmarried) | −0.319(0.199) | 2.724***(0.847) | −0.537***(0.191) | −0.541(0.395) | −0.346*(0.195) |
| Divorced or widowed | −0.132(0.196) | 3.277***(0.847) | −0.395**(0.189) | −0.497(0.384) | −0.157(0.192) |
| Living status: living with spouse (ref: living alone) | 0.208***(0.072) | −0.184(0.271) | 0.223***(0.069) | −0.351**(0.163) | 0.190***(0.072) |
| Living with spouse and children | 0.043(0.074) | 0.203(0.278) | 0.027(0.071) | −0.181(0.168) | 0.034(0.074) |
| Living with children | 0.043(0.066) | 0.361(0.237) | 0.014(0.062) | −0.675***(0.143) | 0.009(0.065) |
| Other (living with relatives, nursing homes) | 0.404***(0.135) | 1.049**(0.502) | 0.320***(0.124) | −0.663**(0.265) | 0.370***(0.132) |
| Retirement: retired, still working (ref: retired) | −0.021(0.048) | 0.243(0.163) | −0.040(0.046) | −0.029(0.117) | −0.022(0.048) |
| Employed | −0.145**(0.064) | 2.577***(0.327) | −0.351***(0.064) | −0.982***(0.172) | −0.194***(0.064) |
| Chronic: only 1 chronic (ref: no) | −0.168(0.212) | −1.784**(0.748) | −0.025(0.182) | 0.203(0.480) | −0.158(0.209) |
| Multimorbidity | 0.600***(0.214) | −0.124(0.751) | 0.610***(0.183) | −0.259(0.481) | 0.587***(0.210) |
| Monthly income: 1–1000 (ref: no income) | −0.097*(0.052) | −1.232***(0.164) | 0.002(0.049) | 0.382***(0.120) | −0.078(0.052) |
| 1001–2000 | −0.173***(0.065) | −1.238***(0.208) | −0.074(0.061) | 0.936***(0.149) | −0.126*(0.065) |
| 2001–5000 | −0.169***(0.065) | −1.219***(0.224) | −0.071(0.062) | 0.270*(0.149) | −0.155**(0.065) |
| 5001–10,000 | −0.248***(0.077) | −1.518***(0.266) | −0.127*(0.072) | 0.089(0.183) | −0.244***(0.076) |
| >10001 | −0.314***(0.094) | −1.174***(0.338) | −0.220**(0.087) | −0.172(0.238) | −0.323***(0.093) |
| Health insurance: yes (ref: no) | −0.271**(0.126) | −0.537(0.469) | −0.228*(0.118) | −0.668***(0.238) | −0.304**(0.125) |
| Pension insurance: yes (ref: no) | −0.314***(0.094) | 0.052(0.208) | −0.049(0.063) | −0.084(0.140) | −0.049(0.067) |
| Number of children | −0.045(0.067) | −5.438***(0.413) | 0.667***(0.082) | 1.168***(0.163) | 0.290***(0.076) |
| Province: Guangxi (ref: Shandong) | 0.460***(0.070) | 7.032***(0.272) | −0.104(0.073) | −1.922***(0.166) | 0.363***(0.070) |
| Jiangsu | 0.065(0.060) | 2.025***(0.210) | −0.097*(0.057) | 0.889***(0.146) | 0.110*(0.060) |
| Hubei | 0.450***(0.052) | 3.308***(0.168) | 0.185***(0.049) | −1.621***(0.121) | 0.369***(0.052) |
| Constant | 1.529***(0.334) | 14.326***(1.332) | 0.381(0.305) | 2.179***(0.714) | 1.639***(0.328) |
| Observations | 8696 | 8696 | 8696 | 8696 | 8696 |
| R 2 | 0.124 | 0.244 | 0.204 | 0.156 | 0.137 |
Note: DHL, digital health literacy. Robust standard errors in parentheses. *** p < 0.01, ** P < .05, * P < .10.
Figure 3.
The mediating effect of depressive symptoms in the relationship between DHL and health inequalities.
Figure 4.
The mediating effect of physical activity in the relationship between DHL and health inequalities.
Table 6.
Nonparametric percentile confidence intervals corrected for bias in depressive symptoms and physical activity.
| Variable | Observed coefficient | Bootstrap Std Err | 95% CI | |
|---|---|---|---|---|
| Paths | LLCI | ULCI | ||
| Depressive symptoms | ||||
| Indirect effect | −0.005 | 0.001 | −0.0066 | −0.0045 |
| Direct effect | −0.011 | 0.002 | −0.0159 | −0.0099 |
| Total effect | −0.016 | 0.002 | −0.0209 | −0.0148 |
| Physical activity | ||||
| Indirect effect | −0.001 | 0.000 | −0.0020 | −0.0011 |
| Direct effect | −0.015 | 0.002 | −0.0199 | −0.0135 |
| Total effect | −0.016 | 0.002 | −0.0211 | −0.0147 |
Discussion
As digital technology continues to reshape healthcare accessibility and health management, DHL has emerged as a crucial factor influencing health and equity among older adults. This study uniquely integrated the Capability Theory, utilizing data from a large multicenter survey conducted in China, to elucidate the correlations and mechanisms of action between DHL and health inequities affecting older adults.
First, the DHL score of the older adults surveyed in this study was 20.22 (SD = 10.59), which is higher than a survey in Jinan, China, 39 but lower than the findings from a study in Sweden. 70 This may be related to the level of economic development of the survey area and the source of the sample. Although the level of digitization in China has developed rapidly in recent years, there is still a gap with developed countries. In the O-Probit regression model, the results indicated that social determinants of health—such as urban/rural distribution, educational level, monthly income, and possession of health insurance—remain key variables influencing health outcomes. Notably, after controlling for these factors, the positive association between DHL and SRH remained significant, which supports Hypothesis 1. Several current studies have suggested the inclusion of digital factors as new social determinants,18,19 and this study similarly supports this finding. DHL is not only a reflection of the digital factor, but also the ability to use the digital health resource to translate into health benefits. Older adults with higher DHL are better equipped to utilize digital health resources, which enhances their health management and disease prevention efforts, ultimately leading to improved health outcomes.
Second, our findings indicated a significant negative correlation between DHL and health inequalities, thereby corroborating Hypothesis 2. This aligns with the findings of the current study. 29 DHL, as one of the capabilities to convert digital health resources into health capital, enabled disadvantaged groups to access and utilize resources such as telemedicine, online health education, and online appointments more smoothly, thus alleviating to some extent the health inequalities caused by economic, educational, and geographical differences. For example, it has been reported that China's Internet healthcare services have developed rapidly, transforming the traditional face-to-face healthcare service model. 71 This evolution has alleviated the time and space constraints faced by disadvantaged patients in rural and remote areas, thereby promoting the equalization of healthcare resources. 72 Notably, DHL played a significant role in this process. Research has demonstrated that individuals with higher levels of DHL are more likely to utilize telemedicine services to compensate for the scarcity of traditional healthcare resources, which is particularly crucial for those residing in remote or resource-limited areas. 73
Third, our study found that DHL mitigated health inequalities in older adults by promoting physical activity and suppressing depressive symptoms, but had a non-significant mediating effect on unhealthy behavioral constraints and promotion of health service utilization. These findings supported H3-1 and H3-4 and rejected H3-2 and H3-3. Bootstrap tests indicated that depressive symptoms partially mediated the relationship between DHL and health inequalities, accounting for 31.25% of the total effect, and physical activity likewise played a partial mediating role, accounting for 6.25% of the total effect. Older adults with higher DHL are more likely to use useful information on the internet to detoxify their negative emotions, such as online counseling, which can be effective in alleviating depression and loneliness among those living alone.57,59 Meanwhile, the use of digital technology has expanded advances in psychological treatments. A systematic review study supported the effectiveness of information technology-based cognitive behavioral therapy (ICBT) in improving depression in older adults and may lead to better outcomes in improving tweed geriatric mental health. 74 This research finding underscores the potential of DHL to mitigate health inequalities by enhancing mental well-being among older adults.
Moreover, DHL was significantly associated with physical activity, which was consistent with the results of previous studies. 47 Kim's findings indicated that cognitive abilities in DHL, including the understanding, interpretation, processing, and application of information, were crucial for enhancing YouTube users’ willingness to engage in active exercise. 44 This study further corroborated this conclusion within the older population and expanded on the role of DHL in mitigating health inequalities. This extension underscores the academic significance of the research. However, the mediating role of physical activity in addressing health inequalities is low (only 6.25%), indicating that more support is needed to combine with a healthy diet, and scientific exercise planning to amplify this role.
DHL represents an emerging capability in the field of digital health. However, our findings indicate that its impact on the regulation of unhealthy behaviors is not significant. This may stem from the tendency of individuals to selectively apply health knowledge based on their personal preferences, risk perceptions, and socio-cultural backgrounds, a phenomenon that is particularly pronounced among older adults. Among the various unhealthy behaviors, nicotine addiction from cigarette smoking is particularly concerning, as many older adults have maintained this habit for decades, rendering behavioral regulation through DHL challenging. A Chinese study revealed that moderate levels of health literacy alone may be inadequate to facilitate the adoption of tobacco control behaviors. 75 Additionally, social and cultural factors play a crucial role; for example, among Chinese older adults, smoking and drinking are often perceived as social activities that facilitate group cohesion.76–78 Such social norms may exert a stronger influence on behavior than individual health knowledge. Furthermore, it has been suggested that smoking and drinking are self-selected deviant behaviors, with individuals in better health and possessing greater health knowledge tending to believe that they can manage the associated risks. 79
Additionally, the relationship between DHL and health service utilization was not significant, contrary to the findings of Bíró É, who noted that DHL was negatively correlated with services such as specialists and general practitioners. 50 The reason for the conflicting conclusions may be due to sample selection issues. Most of the older adults in this study suffered from chronic diseases, and regular visits to health facilities for prescriptions and testing have become a part of chronic disease management for older adults in China, which may explain one reason why DHL is not related to health service utilization. In addition, since the measurement of health service utilization in this study was by outpatient services and inpatient services, and the measurement of Internet telemedicine services was not considered, its substitution effect on real health service utilization may have been missed.
While DHL is significantly associated with health promotion and the alleviation of health inequalities, its impact may still be constrained by external environmental and social structural factors. For example, differences between urban and rural areas in terms of the accessibility of digital health resources, health care delivery systems, and network infrastructure may result in the health-promoting effects of DHL varying across populations. Therefore, while promoting DHL enhancement, attention needs to be paid to social structural barriers to ensure that different social groups can enjoy digital health dividends equitably.
Based on the findings of this study, we advocate for continued research into the remaining potential mechanisms by which DHL promotes health among the older population and mitigates health inequalities. Government agencies and social organizations should actively explore measures and strategies to enhance DHL among older adults while continuing to expand public welfare initiatives such as “mobile classrooms” and “digital literacy” programs. Furthermore, future research could focus on leveraging digital health initiatives to maximize the potential of DHL and improve health outcomes for older adults. Additionally, while enhancing DHL, it is crucial to consider the development of network infrastructure in economically disadvantaged areas to ensure equitable access to the necessary resources for effective DHL implementation.
Conclusion
The results indicated that higher DHL is positively associated with better SRH and simultaneously mitigated health inequalities. Additionally, mediation analyses revealed that digital health literacy not only affects health inequalities through direct pathways but also indirectly by promoting physical activity and reducing depressive symptoms. These findings underscore the urgent need to enhance digital health literacy among older adults to reduce health disparities and promote equitable aging.
Limitations
This study has several limitations that should be acknowledged. First, as a cross-sectional study, the findings can only establish associations rather than causal relationships. The observed associations between DHL and health outcomes among older adults may be influenced by unmeasured confounders, such as pre-existing health conditions, social support, or healthcare access, thereby limiting the ability to infer causality. Future research should employ longitudinal designs with repeated follow-up assessments to strengthen causal inference and track the dynamic effects of digital health literacy on health disparities over time. Second, self-reported measures of health outcomes, including self-rated health and psychological well-being, may be subject to recall bias and social desirability bias. Although validated instruments were utilized, incorporating objective health indicators (e.g., biomarkers, and medical diagnoses) could complement self-reported data and provide a more comprehensive understanding of health inequalities. Considering the multidimensional nature of health, future research should adopt multidimensional measures for both health outcomes and health inequalities to enhance the stability and comprehensiveness of assessment. Third, it should be noted that due to the complex interactions that may exist among the mediating variables, the mediating mechanism test employed in this study focuses on the independent mediating role, necessitating further validation of the intricate relationships among the multivariate variables in question.
Despite these limitations, this study offers valuable insights into the role of digital health literacy in influencing health outcomes and inequalities among older adults. The findings underscore the necessity for targeted interventions and policy initiatives aimed at enhancing digital health literacy within this demographic. By emphasizing competence and its translation into health outcomes, the study advocates for bridging the digital divide as a means to further advance health equity.
Acknowledgements
We would like to express our profound gratitude to the staff at all levels of communities and village councils for their coordination and cooperation during the on-site survey, and to every researcher for their hard work.
Footnotes
ORCID iD: Gangrui Tan https://orcid.org/0009-0001-3490-6762
Ethical considerations: This study was approved by the Medical Ethics Committee of Zhongda Hospital, Affiliated with Southeast University (No. 2024ZDSYLL294-Y01). Written informed consent was obtained from all participants prior to the survey.
Author contributions: Gangrui Tan contributed to data analytics as well as the drafting and revision of the manuscript. Jianqian Chao was responsible for the research design and provided critical revisions that added significant intellectual content. Shengxuan Jin contributed to the manuscript revision and coordinated the work and data collection efforts. Yanqian Wu, Leixia Wang, Yongqi Du, Shishuo Yang, and Beibei Yang all contributed to the revision of the research design and assisted with data collection. All authors reviewed and approved the final version of the manuscript.
Funding: This study was supported by the Major Project of the National Social Science Fund of China (No: 23 & ZD188).
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: As this study is a major ongoing research project of the National Social Science Fund of China (NSSFC), relevant data are highly confidential and not publicly available. Data used only to support the results of this study are available upon request from the corresponding author.
Guarantor: JQC.
References
- 1.WHO. Ageing and health, https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed 1 February 2025).
- 2.Ministry of Civil Affairs, National Office for the Elderly. 2022 National Development Bulletin on Aging Departmental Dynamics, https://www.gov.cn/lianbo/bumen/202312/content_6920261.htm (accessed 17 August 2024).
- 3.Harper S. The capacity of social security and health care institutions to adapt to an ageing world. Int Soc Secur Rev 2010; 63: 177–196. [Google Scholar]
- 4.Ye P, Jin Y, Er Y, et al. A scoping review of national policies for healthy ageing in mainland China from 2016 to 2020. Lancet Reg Health, West Pac 2021; 12: 100168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marmot M. Social determinants of health inequalities. Lancet 2005; 365: 1099–1104. [DOI] [PubMed] [Google Scholar]
- 6.Shang XT, Wei ZH. Socio-economic inequalities in health among older adults in China. Public Health 2023; 214: 146–152. [DOI] [PubMed] [Google Scholar]
- 7.Marmot M, Friel S, Bell R, et al. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet (Lond Engl) 2008; 372: 1661–1669. [DOI] [PubMed] [Google Scholar]
- 8.McCartney G, Popham F, McMaster R, et al. Defining health and health inequalities. Public Health 2019; 172: 22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. Health inequities and their causes, https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes (accessed 1 February 2025).
- 10.China Internet Network Information Center (CNNIC). The 55th Statistical Report on China’s Internet Development. China Internet Network Information Center (CNNIC), January 2025.
- 11.Tappen RM, Cooley ME, Luckmann R, et al. Digital health information disparities in older adults: a mixed methods study. J Racial Ethn Health Disparities 2021; 9: 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swed O, Sheehan CM, Butler JS. The digital divide and veterans’ health: differences in self-reported health by internet usage. Armed Forces Soc 2020; 46: 238–258. [Google Scholar]
- 13.Cui K, Zou W, Ji X, et al. Does digital technology make people healthier: the impact of digital use on the lifestyle of Chinese older adults. BMC Geriatr 2024; 24: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang L, Li S, Ren Y. Does internet use benefit the mental health of older adults? Empirical evidence from the China health and retirement longitudinal study. Heliyon 2024; 10: e25397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y, Liu K, Zhang X, et al. Does digital infrastructure improve public health? A quasi-natural experiment based on China’s broadband policy. Soc Sci Med 2024; 344: 116624. [DOI] [PubMed] [Google Scholar]
- 16.Chai Y, Xian G, Wang M, et al. Aging wisely: the impact of internet use on older adults’ mental health. J Affect Disord 2024; 364: 139–145. [DOI] [PubMed] [Google Scholar]
- 17.Estrela M, Semedo G, Roque F, et al. Sociodemographic determinants of digital health literacy: a systematic review and meta-analysis. Int J Med Inf 2023; 177: 105124. [DOI] [PubMed] [Google Scholar]
- 18.Gallifant J, Celi LA, Pierce RL. Digital determinants of health: opportunities and risks amidst health inequities. Nat Rev, Nephrol 2023; 19: 749–750. [DOI] [PubMed] [Google Scholar]
- 19.Chidambaram S, Jain B, Jain U, et al. An introduction to digital determinants of health. PLOS Digit Health 2024; 3: e0000346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cullen R. Addressing the digital divide. Online Inf Rev 2001; 25: 311–320. [Google Scholar]
- 21.Hargittai E. Second-level digital divide: differences in people’s online skills. First Monday. Epub ahead of print 1 April 2002. DOI: 10.5210/fm.v7i4.942.
- 22.van Deursen AJAM, Helsper EJ. The third-level digital divide: who benefits most from being online? In: Communication and information technologies annual, pp.29–52. Emerald Group Publishing Limited.
- 23.van Dijk Jan AGM. The digital divide, 2019.
- 24.Neter E, Brainin E. Ehealth literacy: extending the digital divide to the realm of health information. J Med Internet Res 2012; 14: e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Badr J, Motulsky A, Denis J-L. Digital health technologies and inequalities: a scoping review of potential impacts and policy recommendations. Health Policy 2024; 146: 105122. [DOI] [PubMed] [Google Scholar]
- 26.van Kessel R, Hrzic R, O’Nuallain E, et al. Digital health paradox: international policy perspectives to address increased health inequalities for people living with disabilities. J Med Internet Res 2022; 24: e33819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.WHO. WHO releases first guideline on digital health interventions, https://www.who.int/news/item/17-04-2019-who-releases-first-guideline-on-digital-health-interventions (accessed 5 February 2025).
- 28.Boriani G, Maisano A, Bonini N, et al. Digital literacy as a potential barrier to implementation of cardiology tele-visits after COVID-19 pandemic: the INFO-COVID survey. J Geriatr Cardiol: JGC 2021; 18: 739–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Azzopardi-Muscat N, Sørensen K. Towards an equitable digital public health era: promoting equity through a health literacy perspective. Eur J Public Health 2019; 29: 13–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Campanozzi LL, Gibelli F, Bailo P, et al. The role of digital literacy in achieving health equity in the third millennium society: a literature review. Front Public Health 2023; 11: 1109323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res 2006; 8: e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ban S, Kim Y, Seomun G. Digital health literacy: a concept analysis. DIGITAL HEALTH 2024; 10: 20552076241287894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kemp E, Trigg J, Beatty L, et al. Health literacy, digital health literacy and the implementation of digital health technologies in cancer care: the need for a strategic approach. Health Promot J Aust 2021; 32: 104–114. [DOI] [PubMed] [Google Scholar]
- 34.Cho O-H, Kim H, Cho Y. Attitudes and digital health literacy mediate the relationship of digital information accessibility with intention for digital healthcare service use in patients with multiple myeloma: a cross-sectional study. Eur J Oncol Nurs 2025; 74: 102786. [DOI] [PubMed] [Google Scholar]
- 35.Xie H, Wu D, Zhou Y, et al. Use of new-media health information among the elderly and its effect on their health and health management. BMC Public Health 2024; 24: 2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sen A. Inequality reexamined. Harvard University Press, https://book.douban.com/subject/1997368/ (1992, accessed 6 February 2025).
- 37.Sen A. Commodities and capabilities. Delhi ; New York : Oxford University Press, http://archive.org/details/commoditiescapab00amar (1999, accessed 6 February 2025).
- 38.Sen A. Development as freedom. New York: Alfred Knopf, 1999. [Google Scholar]
- 39.Cui G-H, Li S-J, Yin Y-T, et al. The relationship among social capital, eHealth literacy and health behaviours in Chinese elderly people: a cross-sectional study. BMC Public Health 2021; 21: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhu X, Yang F. The association among eHealth literacy, depressive symptoms and health-related quality of life among older people: a cross-section study. Int J Older People Nurs 2023; 18: e12497. [DOI] [PubMed] [Google Scholar]
- 41.Kim K, Shin S, Kim S, et al. The relation between eHealth literacy and health-related behaviors: systematic review and meta-analysis. J Med Internet Res 2023; 25: e40778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wu M, Xue Y, Ma C. The association between the digital divide and health inequalities among older adults in China: nationally representative cross-sectional survey. J Med Internet Res 2025; 27: e62645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Conard S. Best practices in digital health literacy. Int J Cardiol 2019; 292: 277–279. [DOI] [PubMed] [Google Scholar]
- 44.Kim J, Youm H, Kim S, et al. Exploring the influence of YouTube on digital health literacy and health exercise intentions: the role of parasocial relationships. Behav Sci 2024; 14: 282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li Z, Wang Y, Li X, et al. Research on the Correlation between Digital Health Literacy and Physical Health Status in Middle-Aged and Elderly Adults:Based on the Mediating Effect of Physical Exercise Behavior. China Sport Science and Technology 2023; 59: 44–51.
- 46.Zangger G, Mortensen SR, Tang LH, et al. Association between digital health literacy and physical activity levels among individuals with and without long-term health conditions: data from a cross-sectional survey of 19,231 individuals. DIGITAL HEALTH 2024; 10: 20552076241233158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wei Y, Zhou Y. The mediating impact of exercise frequency and duration on the relationship between digital health literacy and health among older adults: a cross-sectional study. Medicine (Baltimore) 2024; 103: e39877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Solis-Navarro L, Gismero A, Fernández-Jané C, et al. Effectiveness of home-based exercise delivered by digital health in older adults: a systematic review and meta-analysis. Age Ageing 2022; 51: afac243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mclaughlin M, Delaney T, Hall A, et al. Associations between digital health intervention engagement, physical activity, and sedentary behavior: systematic review and meta-analysis. J Med Internet Res 2021; 23: e23180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bíró É, Vincze F, Nagy-Pénzes G, et al. Investigation of the relationship of general and digital health literacy with various health-related outcomes. Front Public Health 2023; 11: 1229734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tang H, Yuan D, Wang M, et al. Sequential mediating role of digital participation and health lifestyle in the relationship between socioeconomic status and depression of older adults. Beijing xue xue bao Yi xue ban = J Peking Univ, Health sci 2024; 56: 230–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yu-rong J, Qin W-Z, Jiao Z. Association of e-health literacy with lifestyle among 18–59 years old residents in taian city. Chin J Public Health 2021; 37: 1323–1327. [Google Scholar]
- 53.Stone C, Essery R, Matthews J, et al. Presenting and evaluating a smartwatch-based intervention for smoking relapse (StopWatch): feasibility and acceptability study. JMIR Form Res 2024; 8: e56999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Quansah F, Ankomah F, Agormedah EK, et al. COVID-digital health literacy and subjective well-being of students in Ghana: mediation-moderation analyses. Health Sci Rep 2022; 5: e916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ning L, Zheng Z, Liu M, et al. Profiles of digital health literacy among university students and its association with mental health during the COVID-19 pandemic: a latent profile analysis. DIGITAL HEALTH 2024; 10: 20552076231224596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rivadeneira MF, Salvador C, Araujo L, et al. Digital health literacy and subjective wellbeing in the context of COVID-19: a cross-sectional study among university students in Ecuador. Front Public Health 2022; 10: 1052423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nutakor JA, Zhou L, Larnyo E, et al. Impact of health information seeking behavior and digital health literacy on self-perceived health and depression symptoms among older adults in the United States. Sci Rep 2024; 14: 31080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Leung AYM, Parial LL, Tolabing MC, et al. Sense of coherence mediates the relationship between digital health literacy and anxiety about the future in aging population during the COVID-19 pandemic: a path analysis. Aging Ment Health 2022; 26: 544–553. [DOI] [PubMed] [Google Scholar]
- 59.Zhang X, Lewis S, Chen X, et al. Technology use and attitudes towards digital mental health in people with severe mental health problems: a survey study in China. Front Psychiatry 2023; 14: 1261795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.CNNIC. The 51st Statistical Report on the Development of the Internet in China, https://www.cnnic.net.cn/n4/2023/0303/c88-10757.html (2 March 2023, accessed 29 May 2023).
- 61.Mossey JM, Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health 1982; 72: 800–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 2009; 69: 307–316. [DOI] [PubMed] [Google Scholar]
- 63.Dong W, Li Y, Wang Z, et al. Self-rated health and health-related quality of life among Chinese residents, China, 2010. Health Qual Life Outcomes 2016; 14: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pan Y, Pikhartova J, Bobak M, et al. Reliability and predictive validity of two scales of self-rated health in China: results from China health and retirement longitudinal study (CHARLS). BMC Public Health 2022; 22: 1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhu M-L, Kang Z. Can Long⁃term Care Insurance Alleviate Health Inequality? —Evidences from CHARLS. Insurance Studies 2024; 90–100.
- 66.Kakwani N. The relative deprivation curve and its applications. J Bus Econom Statist 1984; 2: 384–394. [Google Scholar]
- 67.Ma Z, Wu M. The psychometric properties of the Chinese eHealth literacy scale (C-eHEALS) in a Chinese rural population: cross-sectional validation study. J Med Internet Res 2019; 21: e15720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen H, Mui AC. Factorial validity of the center for epidemiologic studies depression scale short form in older population in China. Int Psychogeriatr 2014; 26: 49–57. [DOI] [PubMed] [Google Scholar]
- 69.Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry 1999; 14: 608–617. [DOI] [PubMed] [Google Scholar]
- 70.Ghazi SN, Berner J, Anderberg P, et al. The prevalence of eHealth literacy and its relationship with perceived health status and psychological distress during COVID-19: a cross-sectional study of older adults in blekinge, Sweden. BMC Geriatr 2023; 23: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.People’s Daily (PRC newspaper). Making ‘telemedicine’ fair and efficient. China Government Network, https://www.gov.cn/zhengce/2019-04/26/content_5386421.htm (2019, accessed 10 February 2025).
- 72.Zhao B-Y, Huang L, Cheng X, et al. Digital health literacy and associated factors among internet users from China: a cross-sectional study. BMC Public Health 2024; 24: 908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ji H, Dong J, Pan W, et al. Associations between digital literacy, health literacy, and digital health behaviors among rural residents: evidence from zhejiang, China. Int J Equity Health 2024; 23: 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Qiu Y, Wu M, Liu J, et al. Effectiveness of information technology-based cognitive behavioral therapy on depression and anxiety symptoms among older adults: systematic review and meta-analysis. Gen Hosp Psychiatry 2024; 93: 9–19. [DOI] [PubMed] [Google Scholar]
- 75.Wang L, Li Y, Li L, et al. Association of health literacy with smoking behavior among Chinese men. Health Promot Int 2023; 38: daad113. [DOI] [PubMed] [Google Scholar]
- 76.Lee Y-H, Chang Y-C, Liu C-T, et al. Correlates of alcohol consumption and alcohol dependence among older adults in contemporary China: results from the Chinese longitudinal healthy longevity survey. J Ethn Subst Abuse 2020; 19: 70–85. [DOI] [PubMed] [Google Scholar]
- 77.Chang Y-C, Lee Y-H, Chiang T, et al. Associations of smoking and alcohol consumption with loneliness, depression, and loss of interest among Chinese older males and females. Int J Ment Health Addict 2024; 22: 1047–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Li C, Long C, Zhang M, et al. The influence of alcohol consumption on tobacco use among urban older adults: evidence from western China in 2017. Sustainability 2022; 14: 7752. [Google Scholar]
- 79.Yanbi H, Diyang Z, Ji S. Self-selection or situational stratification? A quasi-experimental study of health inequalities. Social Study 2022; 37: 92–113. [Google Scholar]