Abstract
Concerns about the relationship between social media use and adolescent mental health are growing, yet few studies focus on adolescents with clinical-level mental health symptoms. This limits our understanding of how social media use varies across mental health profiles. In this Registered Report, we analyse nationally representative UK data (N = 3,340, aged 11–19 years) including diagnostic assessments by clinical raters alongside quantitative and qualitative social media measures. As hypothesized, adolescents with mental health conditions reported spending more time on social media and were less happy about the number of online friends than adolescents without conditions. We also found hypothesized differences in social media use by condition type: adolescents with internalizing conditions reported spending more time on social media, engaging in more social comparison and experiencing greater impact of feedback on mood, alongside lower happiness about the number of online friends and lower honest self-disclosure. In contrast, those with externalizing conditions only reported higher time spent. These findings emphasize the need to consider diverse adolescent mental health profiles in policy and clinical practice.
Subject terms: Science, technology and society; Human behaviour; Epidemiology
Using a nationally representative UK sample of adolescents with clinical-level mental health symptoms, this Registered Report examined differences in social media use. The results suggest that adolescents with mental health conditions spent more time on social media and were less happy about online friends than adolescents without conditions.
Main
Adolescents around the world have experienced a decline in their mental health over the past decade1. Recent UK data suggests that one in six 7–16-year olds and one in four 17–19-year olds have a probable mental health condition, a clear rise from the one in nine and one in ten recorded in 2017, respectively2. As 48% of those with a mental health condition first experience relevant symptoms before the age of 18 years3, this increased mental health burden will negatively impact society and the economy, as well as adolescent and adult life4. Many have raised concerns that this trend has been caused, at least in part, by increased adolescent social media use, which has revolutionized how adolescents live, learn and interact: 93% of 12–17-year olds now report having a social media profile5.
To address these concerns, academic investigation of social media use and adolescent mental health has increased substantially in recent years6. Research teams have recruited adolescent populations in schools, universities or as part of broader community-based samples to identify cross-sectional and longitudinal links between increased smartphone or social media use and scores on questionnaires of depression7,8, anxiety9, disordered eating10 and other mental health symptoms10–12. These studies have primarily found small positive associations. Some researchers have used these to argue that there exists a causal link between social media use and mental health declines (that is, “screen time, perhaps especially social media, may have larger effects on adolescent girls’ mental health than on boys’ and that is indeed what we found, with social media significantly correlated with depressive symptoms […]”13 p. 13). Such arguments, in turn, have been used to call for restrictive policy regulations to limit smartphone and social media use in adolescent age groups14.
However, many researchers have also questioned the strength of the current evidence base and highlighted that existing studies do not support the idea that there is a causal relationship linking social media use to mental health. Indeed, the literature provides many conflicting results15. Researchers have not only debated about a lack of longitudinal or causal evidence16, but have also disagreed about what effect sizes matter17–19 and how to deal with the substantial individual differences present20,21, which have been linked to factors such as age22, gender23,24 and ethnicity25.
Across these topics of debate, however, researchers have largely overlooked how the kind of instruments used to measure mental health, as well as the populations being studied, limits their ability to draw meaningful inferences about the relationship of social media with adolescent mental health in the first place. So far, most studies have examined school- or community-based adolescent samples15,16,26, relating scores on mental health questionnaires (for example, the Hospital Anxiety and Depression Scale9,27) to time spent on social media. The rationale for doing so is that questionnaires capturing continuous clinical symptoms are informative when reasoning about social media use in relation to the whole spectrum of mental health, across types of severity and clinical presentation. However, this approach is not a suitable surrogate for studying links between social media and mental health in adolescents with versus without mental health conditions, for two main reasons. First, it reduces the complexity of clinical presentations to the tail end of variation in selected mental health symptoms among mostly healthy individuals. Second, it ignores the potentially important differences between those who endorse symptoms on a questionnaire and those who reach diagnostic criteria in standard clinical classifications. For example, an adolescent can score very highly on a questionnaire measuring depressive symptoms, but not meet the criteria for a diagnosis if the queried symptoms have only been present for a short time or if they are better explained by a different condition or situation.
To address this issue, select studies have moved beyond such an approach, dichotomizing symptom severity by applying cut-off scores to mental health questionnaires to reflect the presence or absence of a mental health diagnosis23. However, dichotomization does not solve many of the problems highlighted above and is known to have low sensitivity when predicting clinical diagnoses. Indeed, those with a mental health condition can score below the threshold on some scales28,29. In other words, although researchers would like to demonstrate the presence or absence of specific links between mental health conditions and social media use, the measures of psychopathology they employ might not be appropriate for these goals.
Importantly, the assumption that patterns of social media use found in non-clinical or community samples will generalize to those with mental health conditions has not yet been systematically tested. To our knowledge, only a few studies—most qualitative—have documented different social media use experiences in clinical adolescent populations, including those fulfilling stringent diagnostic criteria for a clinical condition, attending mental health services or being hospitalized for suicidal ideation and suicide attempts30–33. Adolescents in these studies reported both positive and negative social media experiences, such as enhanced social connection and trouble downregulating their use. Broadly speaking, these experiences aligned with established risk and protective factors previously linked to mental health in offline spaces and suggest there is no clear-cut positive or negative association between mental health and social media use. The studies also raise the idea that vulnerable youth might experience heightened emotional responses to social media use. However, this has not been directly assessed due to the lack of non-clinical comparison groups. Such comparisons are therefore necessary to identify differences in social media use between adolescents with and without mental health conditions.
Owing to the lack of research among young people with mental health conditions26, the important question of whether social media use varies across different types of conditions also remains unaddressed. For example, an adolescent with an internalizing condition (for example, generalized anxiety disorder or depressive disorder) might use and feel impacted by social media differently than an adolescent with an externalizing condition (for example, attention deficit hyperactivity disorder or conduct disorder). This is because, despite both groups presenting mental health symptoms at clinical levels, their experiences of psychopathology can be qualitatively different. Internalizing conditions involve negative emotionality towards the self, expressed through ruminative thought patterns, worries and social withdrawal34. On the contrary, externalizing conditions involve negative emotionality towards others, expressed through impulsivity, risk taking and disinhibition35. Studies that assess mental health with select questionnaires cannot comprehensively account for and investigate such clinical diversity. This is a substantial shortcoming, given the need for research to understand how social media use relates to the growing number of adolescents experiencing mental health symptoms at clinical levels.
This Registered Report provides critical data and evidence-based insights into how social media and mental health are related across adolescent populations who meet and do not meet diagnostic criteria for a wide range of mental health conditions. Given the cross-sectional nature of the data and planned analyses, the study results do not provide causal evidence. Hence, all reported coefficients indicate associations, with the possibility of bidirectional relationships and third variables affecting social media use, mental health or the relationship between the two. We analysed the nationally representative Mental Health of Children and Young People (MHCYP) study36, a cross-sectional survey carried out by National Health Service (NHS) Digital in 2017 that collected data from over 3,000 adolescents (11–19 years old) in England. In place of completing self-report measures of mental health, the participants in this study underwent multi-informant standardized diagnostic assessments evaluated by professional clinical raters for different mental health conditions (Table 1). We note that, in the stage 1 report, the terms ‘clinical and non-clinical population’ were used, but in stage 2 this was changed to ‘adolescents with and without mental health conditions’ to clarify that participants in this study were not recruited or diagnosed by a clinic, but instead underwent the mental health assessment as part of the MHCYP study.
Table 1.
Summary of our categorization of mental health conditions into internalizing and externalizing
| Grouping of mental health conditions | List of mental health conditions diagnosed in the DAWBA |
|---|---|
| Any | Separation anxiety disorder, generalized anxiety disorder, obsessive–compulsive disorder, specific phobia, social phobia, agoraphobia, panic disorder, post-traumatic stress disorder, other anxiety disorder, major depressive episode, other depressive episode, hyperkinetic disorder, other hyperactivity disorder, oppositional defiant disorder, conduct disorder (general, confined to family, unsocialized, socialized and other), attention deficit hyperactivity disorder, other disruptive behavioural disorders, any behavioural disorder, autism spectrum disorder, eating disorder, tic disorder, selective mutism, psychosis, body dysmorphic disorder, bipolar affective disorder, mania, attachment disorder, feeding disorder, sleep disorder and eliminating disorder. |
| Internalizing | Separation anxiety disorder, generalized anxiety disorder, obsessive–compulsive disorder, specific phobia, social phobia, agoraphobia, panic disorder, post-traumatic stress disorder, other anxiety disorder, body dysmorphic disorder, major depressive episode, other depressive episode and eating disorders. |
| Externalizing | Hyperkinetic disorder, other hyperactivity disorder, oppositional defiant disorder, conduct disorder (general, confined to the family, unsocialized, socialized and other), attention deficit hyperactivity disorder, other disruptive behavioural disorders and any behavioural disorder. |
| Excludeda from questions 2 and 3 | Autism spectrum disorder, tic disorder, psychotic disorders, mania and bipolar affective disorder. |
aWe exclude adolescents diagnosed with these conditions as they do not clearly map onto the symptomatology of either internalizing or externalizing diagnoses34,65. Further, because the diagnostic variance of mania and bipolar disorder accounted for by internalizing pathology is lower than most other internalizing disorders, such as anxiety and depression33, we decided to exclude these diagnoses from the internalizing category, together with autism spectrum disorder, tic disorder and psychotic disorders. DAWBA, Development and Wellbeing Assessment.
Further, to gain a comprehensive understanding of how social media use differs across adolescents with and without a mental health condition, we examined both quantitative and qualitative dimensions of social media use. Measuring only time spent provides a crude and simplistic estimate of social media use, conflating distinct analytical levels and missing a rich range of psychological factors such as appraisal and motivations that might vary as a function of mental health37. Researchers have therefore called for quantitative time-based measures of social media use to be complemented by more qualitative engagement-based measures capturing adolescents’ social media activities and their appraisal of them16,38–42. Such practice is, however, still relatively rare. In this Registered Report, we included both types of measures, namely, time spent on social media and dimensions of social media engagement that could incur mental health risks (that is, online social comparison, monitoring and impact of online feedback and lack of control over time spent online) or benefits (that is, online friendship, as well as opportunities for honest self-disclosure and authentic self-presentation). By complementing quantitative and qualitative dimensions of social media use, this work provides a more solid foundation for mechanistic research aimed at informing future targeted interventions, clinical practice and policy actions benefitting adolescent mental health.
We used existing literature on adolescents’ mental health in relation to both online and offline contexts (Table 2) to guide our hypotheses and analyses of the data along three lines of enquiry. Specifically, we evaluated whether social media use differs in adolescents with versus without a mental health condition (Question 1), with an internalizing or externalizing condition versus without a condition (Question 2) and with an internalizing versus externalizing condition (Question 3).
Table 2.
Review of key social media and mental health literature used to formulate the hypotheses of our study
| Social media use | Scientific literature | Relevant hypotheses | Key references |
|---|---|---|---|
|
Time spent on social media Item: “When you use social media sites or apps how much time in total do you spend using them on a typical school day/weekend?” |
Research on the relationship between social media use and mental health in different samples has yielded limited and conflicting results. On the one hand, studies have found that young people diagnosed with depression report spending more time on social media compared with non-clinical controls33. Further, studies that focus on excessive rather than average time spent on social media show comorbidity between anxiety, depression, attention deficit hyperactivity disorder and excessive time spent on social media72. However, in a sample of hospitalized adolescents with psychiatric conditions, the frequency of social media use and perception of overuse was not associated with clinical severity32. Additionally, in an independent clinical sample, using social media less, both overall and for messaging, was linked to higher levels of suicidal ideation over the next 30 days106. There is more work on community samples available (for example refs. 26,71) examining time spent on social media (mostly self-reported) and its relation to depression, anxiety and other indicators of mental health. Recent reviews and meta-analyses have reached a general agreement that associations are weak and positive (higher social media use is linked with higher levels of anxiety and depression8,15,107). Overall, despite mixed evidence, research therefore seems to suggest a small relationship between more time spent on social media and lower mental health, both when considering internalizing and externalizing symptoms. |
H1.1a: adolescents with any mental health condition will spend more time on social media than adolescents without a condition. H2.1a: adolescents with internalizing mental health conditions will spend more time on social media than adolescents without a condition. H2.3a: adolescents with externalizing mental health conditions will spend more time on social media than adolescents without a condition. H3.0a: adolescents with externalizing mental health conditions will not differ from adolescents with internalizing conditions in time spent on social media. |
Valkenburg et al.15 Cunningham et al.8 George et al.71 Gürbüz et al.33 Fassi et al.26 Hussain & Griffiths72 Hamilton et al.106 Riehm et al.107 Nesi et al.32 |
|
Online social comparison Item: “I compare myself to others on social media sites and apps” |
In offline contexts, social comparison provides means of gathering information about the social world. This is particularly important during adolescence when young people need to develop a sense of personal and social identity and adjust to bodily changes43. Despite social comparison being instrumental for maturation into adulthood, its exacerbation has been associated with poor mental health, particularly in relation to internalizing symptoms. For instance, adolescents with anxiety and eating disorders engage in less favourable and more frequent social comparisons than adolescents without these conditions44–48. Social media platforms offer continuous and more concrete opportunities for social comparison than offline contexts, for instance, by allowing people to browse others’ profiles without initiating social interaction52. Indeed, adolescents with a depression diagnosis reported unfavourably comparing themselves with others when using social media30. Similarly, among adolescents hospitalized for suicidal behaviour, 30% reported engaging in self-denigrating social comparisons, particularly body-related ones31. |
H1.1b: adolescents with any mental health condition will engage in more online social comparison than adolescents without a condition. H2.0b: adolescents with externalizing mental health conditions will not differ in online social comparison from adolescents without a condition. H2.1b: adolescents with internalizing mental health conditions engage in more online social comparison than adolescents without a condition. H3.1b: adolescents with internalizing mental health conditions will engage in more online social comparison than adolescents with externalizing conditions. |
Krayer et al.43 Corning et al.44 Goodman et al.45 Rao et al.48 Thwaites & Dagnan46 Troop et al.47 Pempek et al.52 Radovic et al.30 Weinstein et al.31 |
|
Perceived lack of control over time spent online Item: “In general, I spend more time on social media than I mean to” |
Difficulties in managing personal goal pursuit in the face of internal, interpersonal and environmental forces that could impede it have been closely linked to the symptomatology of different mental health conditions, particularly externalizing ones. For example, attention deficit hyperactivity disorder and conduct problems are characterized by lower levels of self-monitoring, self-instruction and goal setting53. Technological developments now allow individuals to access social media at any location or time of the day. Consequently, online platforms are not limited to a particular environment and repetitions of certain behaviours, such as opening an app or scrolling through one’s feed108, might result in adolescents feeling unable to reduce the time they spend online despite being motivated to do so. We expect difficulties in self-regulation and goal pursuit to also reflect in how adolescents with mental health conditions engage with social media. Indeed, in a sample of adolescent psychiatric inpatients, self-regulation of social media behaviour was associated with mental health symptoms109. Further, in qualitative interviews, 40% of inpatients hospitalized for suicidal behaviour reported trouble regulating social media use and feeling ‘addicted’31. |
H1.1c: adolescents with any mental health condition will be more likely to lack control over time spent online than adolescents without a condition. H2.0c: adolescents with internalizing mental health conditions will not differ in lack control over time spent online from adolescents without a condition. H2.3c: adolescents with externalizing mental health conditions will be more likely to lack control over time spent online than adolescents without a condition. H3.2c: adolescents with externalizing mental health conditions will be more likely to lack control over time spent online than adolescents with internalizing conditions. |
Strauman et al.53 Winds et al.109 Weinstein et al.31 Bayer et al.108 |
|
Monitoring of online feedback Item: “I monitor the amount of likes, comments and shares I get on social media” |
Adolescents and adults with depression, anxiety and eating disorders, among other internalizing conditions, have a higher tendency to seek feedback from others110,111, particularly when negative, and engage in more reassurance seeking55. Further, compulsivity in social media checking behaviours has been associated with anxiety, depression and problematic smartphone use112, therefore becoming a cause of clinical and developmental concern76. Consistent with these results, online feedback seeking has been associated with depressive symptoms in adolescent community samples54. This association holds even after accounting for the effects of the overall frequency of technology use, offline excessive reassurance seeking and prior depressive symptoms. |
H1.1d: adolescents with any mental health condition will be more likely to monitor online feedback than adolescents without a condition. H2.0d: adolescents with externalizing mental health conditions will not differ in monitoring online feedback from adolescents without a condition. H2.1d: adolescents with internalizing mental health conditions will be more likely to monitor online feedback than adolescents without a condition. H3.1d: adolescents with internalizing mental health conditions will be more likely to monitor online feedback than adolescents with externalizing conditions. |
Hames et al. 111 Gillet et al.55 Elhai et al.112 Barry et al.76 Nesi & Prinstein54 Clerkin et al.110 |
|
Perceived impact of online feedback Item: “The amount of likes, comments and shares I get on social media has an impact on my mood” |
Compared with people without a mental health condition, those with internalizing conditions (for example, depression113) tend to have biased perceptions and recall of interpersonal feedback. This bias is apparent in both their symptoms, such as negative beliefs about the self and worry, as well as neural markers, such as feedback- and error-related negativity56,57. Social media platforms offer continuous opportunities for exposure to feedback from peers and strangers. Further, feedback is often more quantifiable and permanent than when received offline (for example, the number of likes received and comments to old posts can be revisited). We therefore expect the biased perception of social feedback demonstrated by some clinical groups to occur and possibly be heightened in online contexts54. |
H1.1e: adolescents with any mental health condition will be more likely to feel impacted by online feedback than adolescents without a condition. H2.0e: adolescents with externalizing mental health conditions will not differ in feeling impacted by online feedback from adolescents without a condition. H2.1e: adolescents with internalizing mental health conditions will be more likely to feel impacted by online feedback than adolescents without a condition. H3.1e: adolescents with internalizing mental health conditions will be more likely to feel impacted by online feedback than adolescents with externalizing conditions. |
Gotlib113 Tobias & Ito56 Tucker et al.57 Nesi & Prinsten54 |
|
Online friendship Item: “I am happy with the number of friends I have on social media” |
In offline contexts, social connections are a protective factor against long-term adverse physical and emotional outcomes, particularly during adolescence114. In line with this evidence, young people with both internalizing and externalizing mental health conditions report difficulties with peers, having few friends and wanting to be alone58–60. Further, adolescents with internalizing conditions tend to be unhappy with their social status and adolescents with externalizing conditions tend to have trouble making and keeping friends, both online and offline73,75. |
H1.2f: adolescents with any mental health condition will be less happy about the number of online friends than adolescents without a condition. H2.2f: adolescents with internalizing mental health condition will be less happy about the number of online friends they have than adolescents without a condition. H2.4f: adolescents with externalizing mental health conditions will be less happy about the number of online friends they have than adolescents without a condition. H3.0f: adolescents with internalizing mental health conditions will be as happy about the number of online friends they have as adolescents with externalizing conditions. |
Viner et al.114 Asselmann et al.58 McBride & Preyde59 Sibley et al.60 Bagwell et al.75 Dawson et al.73 |
|
Honest online self-disclosure Item: “I can be honest with people on social media sites and apps about how I am feeling” |
Self-disclosure is a communication process by which one person reveals information about themselves to another115. The extent of self-disclosure has been associated with higher relationship quality, intimacy and well-being in offline contexts. In adolescent psychiatric inpatients, low levels of self-disclosure have been linked to suicidality, with anxiety and depression mediating this association61. The quality of self-disclosure also differs in people with low compared with high psychological distress. For instance, people that are less distressed tend to disclose more positive information whereas those high in distress tend to disclose more negative and less honest information62. This effect appears to also occur on social media platforms. For instance, depressed individuals are more likely to post darker, bluer and greyer images than people without depressive symptoms116. Communicating personal and emotional information increases the risk of embarrassment and rejection117, which is compounded by adolescents’ increased sensitivity to peer feedback and anxiety regarding negative social evaluations118. We expect this to be especially difficult for adolescents with internalizing conditions, as they must balance the rewards associated with self-disclosure119 with considerations of how that disclosure might be received by their peers. |
H1.2g: adolescents with any mental health condition will engage in less online honest self-disclosure than adolescents without a condition. H2.0g: adolescents with externalizing mental health conditions will not differ in online honest self-disclosure from adolescents without a condition. H2.2g: adolescents with internalizing mental health conditions will engage in less online honest self-disclosure than adolescents without a condition. H3.2g: adolescents with internalizing mental health conditions will engage in less online honest self-disclosure than adolescents with externalizing conditions. |
Sprecher & Hendrick115 Horesh & Apter61 Chen62 Reece & Danforth116 Omarzu117 Van den bos118 Vijayakumar et al.119 |
|
Authentic online self-presentation Item: “My social media profile is a true reflection of myself” |
Different internalizing conditions such as anxiety, depression and eating disorders are characterized by the internalization of an ideal self that, once compared with perceptions of the actual self, results in negative self-evaluations. Adolescents with these conditions therefore create perfectionistic self-presentations to combat negative self-narratives and project desirable images of themselves in the mind of others63,64,68–70. We expect this process to also occur online, given the multiple affordances offered by social media platforms to curate one’s image, such as deleting old posts, editing new posts and optimizing messages before sending. Hence, adolescents with a mental health condition, particularly if an internalizing condition, might be more likely to engage in impression management online to compensate for negative self-evaluations62. |
H1.2h: adolescents with any mental health condition will engage in less authentic online self-presentation than adolescents without a condition. H2.0h: adolescents with externalizing mental health conditions will not differ in authentic online self-presentation from adolescents without a condition. H2.2h: adolescents with internalizing mental health conditionswill engage in less authentic online self-presentation than adolescents without a condition. H3.2h: adolescents with internalizing mental health conditions will engage in less authentic online self-presentation than adolescents with externalizing conditions. |
Flett & Hewitt63 Jain & Sudhir64 O’Connor et al.70 Sassaroli et al.68 Calvo et al.69 Chen62 |
The social media items are reported in bold for clarity.
First, we expected adolescents with any mental health condition to report engaging with social media differently than those without a condition. For instance, gathering information about peers is particularly important during adolescence when young people develop a sense of personal and social identity43. However, high levels of upward social comparison (that is, comparisons with those believed to be of higher status than the self) have been associated with poorer mental health44–48. Previous work suggests that most social comparisons made on social media sites are upward rather than downward49, possibly because individuals tend to portray themselves in an ideal manner online50,51. Social media could further amplify these processes as platforms offer continuous and more concrete opportunities for comparing oneself with others, such as browsing profiles without initiating social interaction52. Indeed, engagement in self-denigrating online social comparisons was a common theme raised by adolescent psychiatric inpatients during qualitative interviews31. We therefore expected adolescents with a mental health condition to engage in more online social comparison than those without a condition (hypothesis H1.1b). Similarly (see Table 2 for a detailed overview of the literature in support of each hypothesis), we expected them to spend more time on social media8,15 (H1.1a), report more lack of control over time spent online31,53 (H1.1c), while also monitoring54,55 (H1.1 d) and feeling more impacted by online feedback56,57 (H1.1e).
In contrast, we expected adolescents with any condition to engage less with social media in ways that might be protective for their mental health. For instance, we hypothesized that adolescents with a mental health condition are less happy with the number of friends they have online than adolescents without a condition (H1.2f). This is because social connections protect against long-term adverse physical and emotional outcomes, particularly during adolescence48, and young people with mental health conditions often report difficulties with peers, having few friends and wanting to be alone58–60. Similarly, we expected adolescents with a mental health condition to engage in less honest online self-disclosure61,62 (H1.2g) and authentic online self-presentation63,64 (H1.2h) compared with adolescents without a condition (Table 2).
Second, we predicted social media use to vary between adolescents with different symptomatology, focusing specifically on how the social media use of adolescents with an internalizing or externalizing condition (Table 1) differed from those without a condition.
We know from the mental health literature that internalizing conditions involve negative self-views, rumination, worries and social withdrawal34,65. Notably, these symptoms could be relevant to how young people present themselves and engage with others on social media31,32,66. For instance, adolescents with internalizing conditions are more likely to notice discrepancies between their ideal and actual selves67 and may compensate for these discrepancies via impression management offline. We expect this process to also occur online, given the multiple affordances social media platforms offer to curate one’s image (for example, deleting old posts and editing new posts). Hence, we hypothesized that adolescents with internalizing conditions would be less likely to engage in authentic self-presentation on social media than adolescents without a mental health condition68–70 (H2.2h). Further (Table 2), we hypothesized that adolescents with internalizing conditions would spend more time on social media8,15,71 (H2.1a), engage in more online social comparison30 (H2.1b) and online feedback monitoring54 (H2.1d), feel more impacted by online feedback56 (H2.1e), be less happy about online friends (H2.2f) and engage in less honest self-disclosure62 (H2.2g) than those without a condition. In contrast, we did not expect a difference in whether they perceive a lack of control over the time they spend online (H2.0c)53.
Compared with internalizing conditions, externalizing conditions involve impulsivity, low self-monitoring and risk taking34,65. These symptoms could be reflected in how social media is used by these groups. Hence, we hypothesized that adolescents with externalizing conditions would be more likely than adolescents without a condition to spend more time on social media72 (H2.3a) and perceive they lack control over the time they spend online53 (H2.3c). Further, we expected them to also be more dissatisfied with their number of online friends73 (H2.4f). In contrast, we did not expect differences in the other dimensions of social media use (H2.0b,d,e,g,h; Table 2), since they primarily relate to symptoms of internalizing rather than externalizing conditions.
Our third question examined whether adolescents with internalizing conditions use social media differently than those with externalizing conditions. Specifically, we expected adolescents with internalizing conditions to report engaging in more online social comparison30 (H3.1b) and online feedback monitoring55 (H3.1d), feeling more impacted by online feedback56 (H3.1e), engaging in less honest self-disclosure61 (H3.2g) and less authentic self-presentation on social media69 (H3.2h) than those with externalizing conditions. In contrast, we expected adolescents with externalizing conditions to report having less control over the time they spend online53,73 compared to adolescents with internalizing conditions (H3.2c). Further, since adolescents with internalizing conditions tend to be unhappy with their social status74 and adolescents with externalizing conditions tend to have trouble making and keeping friends in both online and offline contexts73,75, we expect both groups to be similarly dissatisfied with their number of online friends (H3.0f). We also hypothesized that both groups would not differ in the amount of time they spend on social media (H3.0a), given that both adolescents with internalizing and externalizing symptoms have been reported to spend more time on social media than adolescents without these symptoms33,76.
Altogether, this study comprehensively maps and compares different dimensions of social media use in adolescents with and without mental health conditions. Hence, it will lay the foundation for future mechanistic and translational research studying which specific social media dimensions relate to mental health in different adolescent groups. This will be a crucial first step to inform translational research and clinical practice, as well as the design of targeted interventions and policies to improve children’s and adolescents’ mental health.
Results
Sample description
Our final sample included 3,340 young people (Table 3) aged 11–19 (mean 14.77, s.d. 2.48) years. The sample was 50% male and 50% female, 16% of participants had at least one mental health condition (N = 519), 8% had an internalizing condition (N = 282) and 3% had an externalizing condition (N = 104). Descriptive statistics split by social media items, sex and diagnostic groups are reported in Supplementary Tables 5–8 and Supplementary Figs. 3–5). Further, an overview of our hypotheses and results is provided in Supplementary Table 9.
Table 3.
Descriptive information by mental health condition
| Mental health category | N | Age mean | Age s.d. | Sex proportion (male) | SES* |
|---|---|---|---|---|---|
| No condition | 2,821 | 14.71 | 2.48 | 0.50 | 0.42 |
| Any condition | 519 | 15.10 | 2.45 | 0.47 | 0.41 |
| Externalizing | 104 | 14.27 | 2.04 | 0.72 | 0.45 |
| Internalizing | 282 | 15.94 | 2.35 | 0.28 | 0.40 |
| Other | 76 | 14.00 | 2.59 | 0.80 | 0.36 |
| Between comorbidity | 57 | 13.93 | 1.80 | 0.51 | 0.46 |
*The proportion of participants in the fourth quartile (the most deprived category based on the Index of Multiple Deprivation). SES, socioeconomic status.
Any mental health condition versus no condition
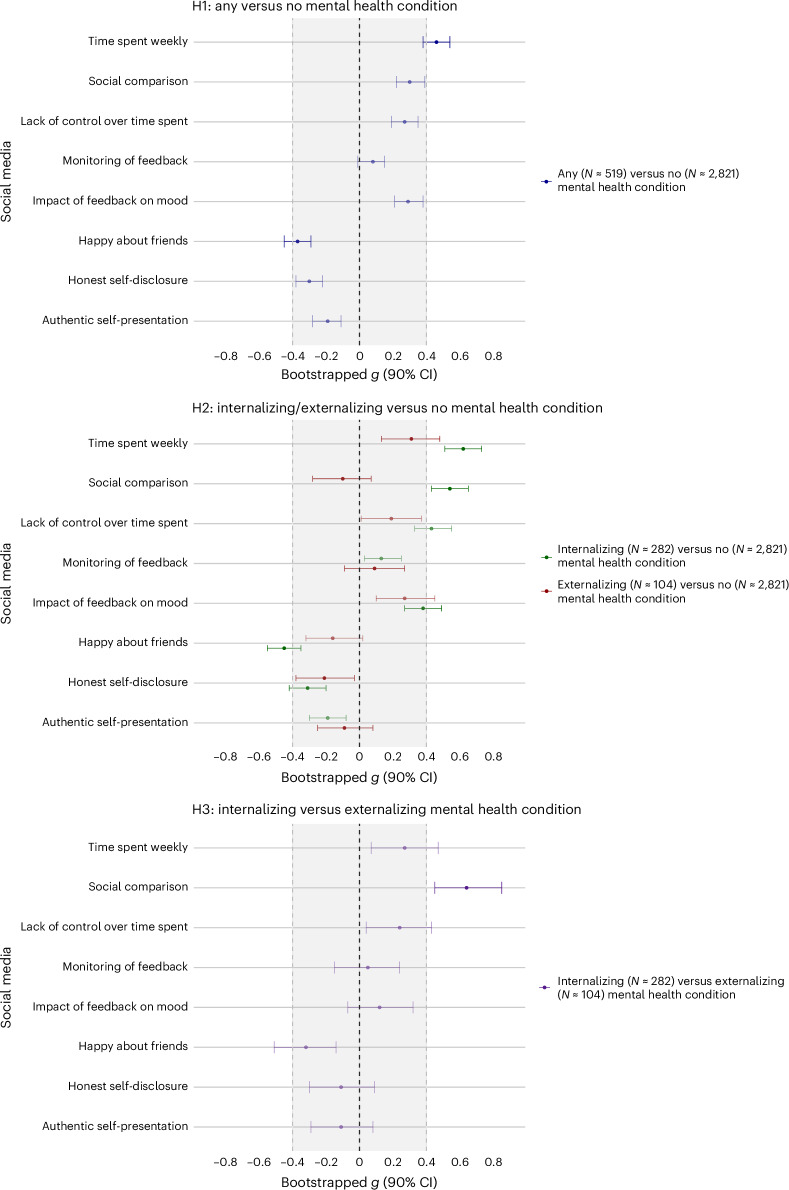
We first compared adolescents with versus without mental health conditions, irrespective of condition type (Fig. 1, H1). In line with our hypothesis, we found that adolescents with any mental health condition reported spending more time on social media than adolescents without a condition (H1.1a; g = 0.46 (90% confidence interval (CI) 0.38 to 0.54); NHST (null hypothesis significance testing): 𝛽 = 0.87, s.e.m. of 0.08, t = 10.48, P = 2.745 × 10−25; EQV (equivalence testing): t(633.8) = 1.21, P = 0.916). Specifically, differences were positive, statistically significant and non-equivalent. That is, we could not reject differences as large or larger than our preregistered equivalence bounds (smallest effect size of interest (SESOI), g = 0.4), indicating potentially meaningful differences between adolescents with and without a condition. On the contrary, the results did not support our hypothesis for online social comparison (H1.1b; g = 0.30 (90% CI 0.22 to 0.39); NHST: 𝛽 = 0.42, s.e.m. of 0.07, t = 6.52, P = 7.973 × 10−11; EQV: t(641.08) = −1.89, P = 0.026), lack of control over time spent online (H1.1c; g = 0.27 (90% CI 0.19 to 0.35); NHST: 𝛽 = 0.39, s.e.m. of 0.07, t = 5.52, P = 3.614 × 10−8; EQV: t (674.42) = −2.68, P = 0.002) and impact of online feedback on mood (H1.1e; g = 0.29 (90% CI 0.21 to 0.38); NHST: 𝛽 = 0.38, s.e.m. of 0.06, t = 6.36, P = 2.269 × 10−10; EQV: t(608.98) = −2.06, P = 0.016). For these dimensions of social media engagement, effect sizes were positive, statistically significant but equivalent (that is, they fell within the preregistered SESOIs). This indicates a difference that is too small to be theoretically meaningful between adolescents with and without a mental health condition. Last, for monitoring of online feedback, we found differences that were not statistically significant and also equivalent, indicating no statistically nor theoretically meaningful differences between adolescents with versus without a condition (H1.1d; g = 0.08 (90% CI −0.01 to 0.15) NHST: 𝛽 = 0.11, s.e.m. of 0.07, t = 1.55, P = 0.121; EQV: t (653.24) = −6.47, P = 0.000).
Fig. 1. Differences in social media use for the three group comparisons.
Top: hypothesis 1 (H1, any mental health condition versus no condition). Middle: hypothesis 2 (H2, internalizing/externalizing versus no condition). Bottom: hypothesis 3 (H3, internalizing versus externalizing condition). Data are presented as mean differences based on Hedges’s g effect size (g) and its corresponding 90% CI. The shaded area indicates the SESOI (g = 0.4, corresponding to d = 0.4). If the 90% CI lies completely within the SESOI, we concluded equivalence, and therefore no meaningful differences. Bolded effect sizes reflect comparisons that supported our hypotheses, while faded effect sizes reflect comparisons that did not support our hypotheses. The starting sample size includes social media users (N = 519 for adolescents with any mental health condition, N = 282 for internalizing conditions, N = 104 for externalizing conditions and N = 2,821 for no mental health condition). However, the exact sample sizes for each comparison are reported in Supplementary Tables 5 and 6 and differ for each dimension of social media use, given that we planned to analyse those separately.
We further hypothesized that adolescents with any mental health condition would score lower than adolescents without a condition on dimensions of social media use that could incur mental health benefits, namely, happiness about the number of online friendships (H1.2f), honest self-disclosure (H1.2g) and authentic self-presentation (H1.2h). In line with our hypothesis, we found lower happiness about the number of online friendships (H1.2f; g = −0.37 (90% CI −0.45 to −0.29); NHST: 𝛽 = −0.33, s.e.m. of 0.04, t = −8.23, P = 2.660 × 10−16; EQV: t(590.4) = 0.56, P = 0.277), for which the effect size was negative, statistically significant and non-equivalent (that is, large enough to be potentially meaningful). In contrast, we did not find differences in honest self-disclosure (H1.2g; g = −0.30 (90% CI −0.38 to −0.22); NHST: 𝛽 = −0.39, s.e.m. of 0.06, t = −6.37, P = 2.213 × 10−10; EQV: t(629.39) = 1.931, P = 0.028) and authentic self-presentation (H1.2h; g = −0.19 (90% CI −0.28 to −0.11); NHST: 𝛽 = −0.24, s.e.m. of 0.06, t = −3.98, P = 7.085 × 10−5; EQV: t(624.53) = 4.04, P = 0.000). In these cases, effect sizes were negative and statistically significant but equivalent, suggesting that differences between those with and without a mental health condition were too small to be theoretically meaningful.
Internalizing/externalizing conditions versus no condition
Our second question concerned the extent to which adolescents with internalizing or externalizing conditions differed in their social media use from adolescents without a condition (Fig. 1, H2).
Internalizing versus no condition
Our hypotheses were grounded in the mental health literature, which suggests that anxiety and depressive disorders are characterized by negative self-views, rumination, worries and social withdrawal. We expected these symptoms to be mirrored in adolescents’ online experiences. The results supported our hypotheses for time spent on social media (H2.1a; g = 0.62 (90% CI 0.51 to 0.73); NHST: 𝛽 = 1.12, s.e.m. of 0.11, t = 10.32, P = 1.609 × 10−25; EQV: t(317.39) = 3.21, P = 0.999), online social comparison (H2.1b; g = 0.54 (90% CI 0.43 to 0.65); NHST: 𝛽 = 0.76, s.e.m. of 0.08, t = 9.12, P = 1.304 × 10−19; EQV: t(318.57) = 2.11, P = 0.994) and the impact of online feedback (H2.1e; g = 0.38 (90% CI 0.27 to 0.49); NHST: 𝛽 = 0.51, s.e.m. of 0.08, t = 6.61, P = 4.494 × 10−11; EQV: t(306.67) = −0.27, P = 0.385), where we found positive, statistically significant, and non-equivalent effect sizes, suggesting potentially meaningful differences between adolescents with internalizing versus no condition. In contrast, the results did not support our hypothesis for monitoring of online feedback, where differences were not statistically significant and were also too small to be considered meaningful (H2.1d; g = 0.13 (90% CI 0.03 to 0.25); NHST: 𝛽 = 0.20, s.e.m. of 0.09, t = 2.13, P = 0.033; EQV: t(324.47) = −4.13, P = 0.000).
For those with internalizing conditions, we also hypothesized decreased levels of happiness about the number of online friendships (H2.2f), honest self-disclosure (H2.2g) and authentic self-presentation (H2.2h). Our hypotheses were confirmed for happiness about the number of online friendships (H2.2f; g = −0.45 (90% CI −0.55 to −0.35); NHST: 𝛽 = −0.40, s.e.m. of 0.05, t = −7.91, P = 3.49 × 10−15; EQV: t(304.45) = −0.69, P = 0.776) and honest self-disclosure (H2.2g; g = −0.31 (90% CI −0.42 to −0.20); NHST: 𝛽 = −0.41, s.e.m. of 0.08, t = −5.16, P = 2.670 × 10−7; EQV: t(314.2) = 1.32, P = 0.088), where we found negative, statistically significant and potentially meaningful differences. In other words, those with internalizing conditions scored lower than adolescents with no condition. In contrast, we did not find support for meaningful differences in authentic self-presentation (H2.2h; g = −0.19 (90% CI −0.30 to −0.08); NHST: 𝛽 = −0.25, s.e.m. of 0.08, t = −3.16, P = 0.002; EQV: t(310.64) = 3.08, P = 0.500 × 10−4), where the effect size was statistically significant but equivalent, and therefore too small to be considered meaningful. Last, we expected no differences in lack of control over time spent online for adolescents with internalizing versus no condition (H2.0c). The results did not support our hypothesis, showing positive, statistically significant and potentially meaningful differences (g = 0.43 (90% CI 0.33 to 0.55); NHST: 𝛽 = 0.60, s.e.m. of 0.09, t = 6.74, P = 1.91 × 10−11; EQV: t(336.39) = 0.489, P = 0.689).
Externalizing versus no condition
Externalizing conditions are characterized by impulsivity, low self-monitoring, and risk taking. We expected such symptoms to be reflected in how social media is used by this group. The results supported our hypotheses for time spent on social media (H2.3a; g = 0.31 (90% CI 0.13 to 0.48); NHST: 𝛽 = 0.58, s.e.m. of 0.17, t = 3.40, P = 0.001; EQV: t(105.73) = −0.83, P = 0.232), where we found positive differences that were statistically significant and large enough to be theoretically meaningful. The results did not support our hypotheses for the lack of control over time spent online (H2.3c; g = 0.19 (90% CI 0.01 to 0.37); NHST: 𝛽 = 0.27, s.e.m. of 0.15, t = 1.83, P = 0.068; EQV: t(100.39) = −2.01, P = 0.017) and happiness about the number of online friendships (H2.4f; g = −0.16 (90% CI −0.32 to 0.02); NHST: 𝛽 = −0.12, s.e.m. of 0.09, t = −1.39, P = 0.165; EQV: t(96.65) = 2.34, P = 0.023), where differences were not statistically significant and were too small to be meaningful.
Last, we expected no differences between adolescents with externalizing and no conditions in online social comparison (H2.0b), monitoring of online feedback (H2.0d), feeling impacted by online feedback (H2.0e), honest online self-disclosure (H2.0g) and authentic self-presentation (H2.0h). The results supported our hypotheses for online social comparison (H2.0b; g = −0.10 (90% CI −0.28 to 0.07); NHST: 𝛽 = −0.13, s.e.m. of 0.14, t = −0.97, P = 0.331; EQV: t(104.81) = 2.94, P = 0.000), monitoring of feedback (H2.0d; g = 0.09 (90% CI −0.08 to 0.27), NHST: 𝛽 = 0.13, s.e.m. of 0.16, t = 0.82, P = 0.410; EQV: t(97.07) = −2.92, P = 0.004), honest self-disclosure (H2.0g; g = −0.21 (90% CI −0.38 to −0.03), NHST: 𝛽 = −0.26, s.e.m. of 0.13, t = −2.01, P = 0.045; EQV: t(98.82) = 1.79, P = 0.040), and authentic self-presentation (H2.0h; g = −0.09 (90% CI −0.25 to 0.08), NHST: 𝛽 = −0.11, s.e.m. of 0.13, t = −0.85, P = 0.395; EQV: t(98.29) = 2.96, P = 0.003), as these effect sizes were not statistically significant and were also too small to be considered meaningful. In contrast, the results did not support our hypothesis for the impact of feedback on mood (H2.0e; g = 0.27 (90% CI 0.10 to 0.45), NHST: 𝛽 = 0.34, s.e.m. of 0.13, t = 2.71, P = 0.007; EQV: t(96.78) = −1.14, P = 0.120), where we found positive, significant and potentially meaningful differences.
Internalizing versus externalizing conditions
Our third question focused only on adolescents with a mental health condition and specifically examined whether those with an internalizing condition use social media differently than those with an externalizing condition (Fig. 1, H3).
The results supported our hypotheses for online social comparison (H3.1b; g = 0.64 (90% CI 0.45 to 0.85); NHST: 𝛽 = 0.89, s.e.m. of 0.16, t = 5.75, P = 0.000, EQV: t(203.72) = 2.187, P = 0.993), where we found positive differences that were statistically significant and large enough to be theoretically meaningful in adolescents with internalizing compared with externalizing conditions. In contrast, the results did not support our hypotheses for the monitoring of online feedback (H3.1d; g = 0.05 (90% CI −0.15 to 0.24); NHST: 𝛽 = 0.07, s.e.m. of 0.18, t = 0.40, P = 0.689, EQV: t(157.17) = −2.924, P = 0.002) and impact of online feedback on mood (H3.1e; g = 0.12 (90% CI −0.07 to 0.32); NHST: 𝛽 = 0.16, s.e.m. of 0.14, t = 1.12, P = 0.261, EQV: t(171.21) = −2.421, P = 0.008), where differences were not statistically significant and were too small to be meaningful.
We further hypothesized that adolescents with internalizing conditions would score lower than adolescents with externalizing conditions in lack of control over time spent online (H3.2c), honest self-disclosure (H3.2g) and authentic self-presentation (H3.2h). However, we found neither significant nor meaningful differences across these dimensions (H3.2g; g = −0.11 (90% CI −0.30 to 0.09); NHST: 𝛽 = −0.15, s.e.m. of 0.15, t = −0.99, P = 0.323, EQV: t(170.73) = 2.47, P = 0.004; H3.2h; g = −0.11 (90% CI −0.29 to 0.08); NHST: 𝛽 = −0.14, s.e.m. of 0.15, t = −0.93, P = 0.351, EQV: t(185.78) = 2.51, P = 0.005). Further, the results were inconclusive for lack of control over time spent online (H3.2c; g = 0.24 (90% CI 0.04 to 0.43); NHST: 𝛽 = 0.33, s.e.m. of 0.17, t = 1.98, P = 0.048, EQV: t(156.91) = −1.37, P = 0.080), where we did not find statistically significant differences nor we could reject meaningfully large effect sizes.
Last, we hypothesized that adolescents with internalizing conditions would not differ from adolescents with externalizing conditions in time spent on social media (H3.0a) and happiness in the number of online friendships (H3.0f). The results did not confirm our hypotheses. For time spent on social media, we found positive differences (internalizing higher than externalizing) that were statistically significant and potentially meaningful (H3.0a; g = 0.27 (90% CI 0.07 to 0.47); NHST: 𝛽 = 0.54, s.e.m. of 0.191, t = 2.76, P = 0.006, EQV: t(171.33) = −1.15, P = 0.1125). Further, we found that adolescents with internalizing conditions reported lower happiness about the number of online friends than adolescents with externalizing conditions. In this case, differences were negative, statistically significant and potentially meaningful (H3.0f; g = −0.32 (90% CI −0.51 to −0.14); NHST: 𝛽 = −0.29, s.e.m. of 0.10, t = −2.93, P = 0.003, EQV: t(206.5) = 0.707, P = 0.223).
Exploratory and sensitivity analyses
To extend our findings, we conducted four sets of sensitivity analyses. First, we included adolescents with between-group comorbidities in question 2, such as any internalizing condition with a comorbid externalizing condition, or vice versa, and compared them with those without a condition (Supplementary Tables 15 and 16). Second, we examined the association between mental health severity, conceptualized as the number of conditions (irrespective of diagnostic type), and social media use (Supplementary Table 17). Third, we focused on adolescents with specific conditions and compared their social media use with that of adolescents without a condition. In this case, we only tested conditions for which we were sufficiently powered, namely, major depressive disorder (N ≈ 86; Supplementary Table 18), generalized anxiety disorder (N ≈ 75; Supplementary Table 19) and social anxiety disorder (N ≈ 70; Supplementary Table 20). Last, we tested our hypotheses for time spent on social media separately for school days and weekends, rather than using a composite score (Supplementary Table 21).
Overall, the results were largely in line with our primary findings with a few exceptions. Namely, we found that adolescents with externalizing and between-group comorbidity (Supplementary Table 16) reported less honest self-disclosure than those without a condition. For the sensitivity analysis on mental health severity, we found that the number of conditions, irrespective of type, was associated with time spent on social media, social comparison, monitoring of feedback and impact of feedback on mood (Supplementary Table 17). Last, we did not find differences for time spent on weekdays versus weekends/holidays (Supplementary Table 21). We note that these sensitivity analyses were exploratory and conducted on relatively small sample sizes, which limits the robustness of these findings.
Discussion
In this Registered Report, we analysed differences in social media use between adolescents with and without mental health conditions in a UK sample of over 3,000 participants. Overall, we found significant and meaningful differences across both quantitative (time spent) and qualitative (for example, online social comparison and happiness about the number of online friends) dimensions of social media use.
Interestingly, the largest difference in social media use between those with and without mental health conditions was in the time spent on social media, with the former reporting higher usage. It is important to note that this measure was self-reported, which is known to have only a moderate correlation with objective measures such as sensing data77. This raises the question of whether those with mental health conditions perceive that they spend more time on social media or whether they actually do so. Further, we observed that adolescents with a mental health condition reported lower satisfaction with the number of their online friends. In offline contexts, social connections serve as a protective factor against long-term adverse physical and emotional outcomes, especially during adolescence. Our findings therefore suggest that the difficulties with peer relationships experienced by youth clinical groups offline may also be reflected in their online interactions. For the other dimensions of social media use examined, our results followed the hypothesized direction and were statistically significant (with the exception of monitoring of online feedback). However, the differences were not large enough to be considered meaningful. This might be explained by the relatively high threshold set as our SESOI, which was a moderate effect size grounded in literature on sleep and physical exercise, both established markers of psychopathology.
We next compared social media use between adolescents with a specific mental health condition (internalizing or externalizing) versus no condition. In this case, the results largely supported our hypotheses, whereby adolescents with internalizing conditions demonstrated higher time spent on social media, increased social comparison, greater impact of social media feedback on mood, lower satisfaction with the number of online friends and lower honest self-disclosure compared to those without a mental health condition. Unexpectedly, we also found that adolescents with internalizing conditions reported a higher lack of control over their time spent online, an engagement dimension that we had instead hypothesized would be more pronounced in those with externalizing conditions. For adolescents with externalizing conditions, the only meaningful difference when compared with those with no condition was increased time spent online, with no notable differences across other dimensions of social media use. These results might be explained by the fact that the dimensions of social media engagement used in this study were largely framed around internal experiences (that is, they enquired about one’s emotions and thoughts) that could be more effective indicators of internalizing rather than externalizing conditions.
Finally, by limiting our focus to only adolescents with mental health conditions, we compared those with internalizing to those with externalizing conditions. We found that adolescents with internalizing conditions engaged in higher online social comparison. This finding aligns with existing research indicating that adolescents with depressive and anxious symptomatology tend to unfavourably compare themselves with others on social media. Given that social media platforms provide continuous and concrete opportunities for social comparison—such as browsing others’ profiles without initiating social interaction52—social comparison may represent a critical mechanism associated with internalizing symptoms on social media. Further, adolescents with internalizing conditions were less happy about the number of their online friends. This may be because their tendency towards negative self-evaluation and social comparison leads them to make negative evaluations of their social status78. In contrast, adolescents with externalizing conditions might be less focused on social comparison and more on immediate social interactions, resulting in greater satisfaction with their online friendships.
Altogether, this study has three key strengths. First, the complex survey design, which utilized random probability sampling, produced a nationally representative UK sample. Second, all participants in the sample underwent a standardized multi-informant assessment by professional clinical raters. This method provided comprehensive information about participants’ mental health without only relying on self-reported questionnaires, self-diagnoses or mental health service use, measures that only capture a subset of individuals with mental health conditions79,80. Last, we examined both qualitative and quantitative aspects of social media use, offering insights beyond time spent into relevant engagement dimensions such as online social comparison and the impact of feedback on mood.
We also acknowledge some limitations of our study. First, regarding study design, we analysed raw associations from cross-sectional data. Therefore, no causal or directional inference can be drawn from these findings, including whether the onset of mental health conditions affects the examined dimensions of social media use or vice versa. Further, given the relatively small sample size in our externalizing group (N = 104) and the relatively large number of individuals with between-group comorbidities (N = 57), our findings concerning externalizing conditions should be interpreted with caution. Specifically, our question 2 and 3 results exclude adolescents with a relatively common clinical profile of comorbid externalizing and anxiety disorders. Additional work on how young people with this clinical profile use and experience social media is needed.
Further, although the sample was nationally representative, we cannot determine the extent to which our findings apply outside the UK. Given the socio-cultural factors influencing social media use and mental health conditions, replicating these results in other regions across both the Global North and Global South is crucial if generalizations are to be made25. We also acknowledge that the data were collected in 2017. While the examined dimensions of social media use remain relevant, the rapid evolution of platforms and user behaviours presents a potential limitation when applying our findings to current trends. Last, we acknowledge limitations regarding our measures. Specifically, we relied on self-reported social media data. Self-reports capture participants’ perceptions, such as online social comparison, that cannot be objectively or reliably measured otherwise. However, they often fail to accurately reflect actual patterns in usage, particularly when estimating time spent on social media77.
Future research should aim to replicate and expand on these findings in three key areas. First, studies using experimental and longitudinal designs are essential to clarify the temporal and causal dynamics linking various social media patterns to mental health conditions. Doing so would allow us to disentangle the within-person variation and directional relationship between social media use and mental health symptom presentation, onset or recovery. Second, regarding social media use, future studies could investigate other self-reported and clinically relevant aspects of engagement, such as time displacement from offline activities81, the similarity between perceived self on social media and offline82, as well as goal-directed social media use. Additionally, studies could assess differences in objective social media use, such as time spent on various apps, posting behaviours, active messaging and content exposure. Third, research involving adolescents with intellectual and learning disabilities is necessary to identify differences in this specific clinical group, which was not included in this study.
The results have implications for clinical practice. Specifically, we find key aspects of social media engagement that could inform the creation of guidelines for patient consultations and early intervention strategies. For example, this could include psychoeducation and cognitive-behavioural reappraisal techniques specifically aimed at online social comparison or the impact of social media feedback (for example, ‘likes’) on mood for adolescents with internalizing conditions.
Over the past years, there has been increasing concern that social media is negatively impacting young people’s mental health, but very little research has compared social media use in those with and without mental health conditions26. In one of the first studies of its kind, we find that young people with mental health conditions report engaging with social media in different ways from those without a condition. This highlights aspects of social media use that might present an increased risk to this already vulnerable group and provides a window for future research to ensure that the digital world is safe for all children regardless of mental health status.
Methods
Ethics information
The MHCYP 2017 survey was reviewed and approved by the West London and GTAC Research Ethics Committee (reference: 16/LO/0155) and the Health Research Authority Confidentiality Advisory Group (reference: 16/CAG/0016) in 2016. Both parents and children provided consent to take part in data collection and were compensated with a £10 voucher for their time. Parents of children under 16 years were interviewed first and permission was sought to interview their child afterwards; the child then provided assent. Conversely, 17–19-year olds were directly asked for their consent, with permission subsequently sought for their parents to be interviewed. Access to the data was granted to the research team by NHS Digital (DARS-NIC-424336-T7K7T-v0.6 r).
Design
The MHCYP study is one of a series of national surveys on the mental health of children and young people in England administered in 1999, 2004, 2017, 2021 and 2022. In this Registered Report, we analysed the 2017 wave collected between January and October 2017: the most recent wave to be made available to researchers as well as the first wave to collect comprehensive data on adolescents’ social media use and to include 17–19-year olds. We only analysed data from adolescents who reported being social media users aged 11–19 years, a total of 3,340 participants (50% male and 50% female) out of the full sample of 9,117. The survey was collected using a stratified probability sample of children and young people living in England who were registered with a general practitioner36. Data were collected via face-to-face interviews with adolescents and their parents. At the same time, if the family agreed, questionnaires were mailed to teachers (for the available data and key demographics see MHCYP 201736,83).
Measures
Time spent on social media
The study measured time spent on social media using two questionnaire items: “When you use social media sites or apps, how much time do you spend using them on a typical school day?” (SMTimeSpentS) and “When you use social media sites or apps how much time in total do you spend using them on a typical weekend or holiday day?” (SMTimeSpentW). Participants answered both questions on a nine-point Likert scale: 1, less than 30 min; 2, more than 30 min but less than an hour; 3, 1–2 h; 4, 2−3 h; 5, 3–4 h; 6, 4–5 h; 7, 5–6 h; 8, 6–7 h; 9, more than 7 h. A single variable reflecting average social media hours was created from these two variables (SMTimeSpent; see Supplementary Table 1 for more details). To do so, we first calculated the mean time in hours for each response. For example, if a participant responded “one to two hours”, we recoded this as 1.5 h. Participants that responded “more than seven hours” were recoded to 7.5 h, while participants that responded “less than 30 min” were recorded to 15 min (that is, 0.25 h). Weekday hours were then multiplied by 5, and weekend hours were multiplied by 2, and the products were summed and divided by 7 to establish a daily mean social media use variable, measured in hours. The SMTimeSpent variable was coded as continuous84.
In the survey, the questions regarding time spent on social media for both weekdays (SMTimeSpentS) and weekends (SMTimeSpentW) were only asked of adolescents who responded that they use social media sites daily or on most days on a previous questionnaire item (SMFreqofUse; 1, daily or most days). Hence, participants that reported a lower frequency of social media use (that is, SMFreqofUse; 2, a few times a week; 3, once a week; 4, a few times a month; 5, once a month; 6, less often than once a month) were not asked these questions. To handle the resulting missing data in the SMTimeSpent variable, we coded any adolescents who responded to the SMFreqofUse question that they use social media between “a few times a week” and “once a week” to 45 min (0.75 h) and adolescents that responded “a few times a month” and “less often than once a month” to 15 min (0.25 h) on the SMTimeSpent question (for more information about our approach to missing data, see Supplementary Table 2).
Social media engagement
We analysed seven qualitative dimensions of social media engagement measured with questionnaire items tapping into experiences associated with both risks and benefits to adolescent mental health. All measures (summarized with related literature in Table 2) were developed in consultation with a young person advisory group (see the Supplementary Methods for more information), where children and adolescents defined the dimensions of social media use most relevant to them. The measures related to mental health risks encompassed online social comparison (“I compare myself to others on social media”), lack of control over time spent online (“I spend more time on social media than I mean to”), monitoring of online feedback (“I monitor the amount of likes, comments and shares I get on social media”) and the impact of online feedback (“The amount of likes, comments and shares I get on social media has an impact on my mood”). On the contrary, the measures indicative of mental health benefits included online friendship (“I am happy with the number of friends I have on social media”), honest self-disclosure (“I can be honest with people on social media sites and apps about how I am feeling) and authentic self-presentation (“My social media profile is a true reflection of myself”).
Participants responded to these measures using a five-point Likert scale (1, disagree a lot; 2, disagree a little; 3, neither agree nor disagree; 4, agree a little; 5, agree a lot). We omitted the “Don’t know” responses and coded 1–5 responses as continuous, given research suggesting that five-point continuous classifications perform as well as or occasionally better than categorical classifications84. We performed a sensitivity analysis to test whether examining social media use on weekdays versus weekends/holidays separately, rather than as a weighted average, changed the main results.
Mental health conditions
Face-to-face interviewers completed the Development and Wellbeing Assessment (DAWBA)85 with parents and adolescents aged 11 years or over to establish mental health conditions. During the interview, participants were first led through the 25-item Strengths and Difficulties Questionnaire86 (Supplementary Table 3). Second, the interviewer administered the DAWBA, a diagnostic tool shown to have good validity87 and reliability88. The DAWBA uses structured and semi-structured questions to assess the presence and severity of symptoms for a wide range of DSM-5 or ICD-10 mental health disorders (Table 1). Each module starts with a few screening items, which, if answered negatively (indicative of the lack of symptoms), allow the interview to proceed to the next module with no loss of accuracy87 (for example, Supplementary Table 4). There is one exception: if a participant scores highly on the Strengths and Difficulties Questionnaire, the interviewer is directed to ask in-depth internalizing disorder DAWBA modules, even if participants screened negative on the initial questions.
After the initial screening items, the subsequent structured items in the DAWBA modules relate directly to diagnostic criteria in DSM-5 and ICD-10. They are close-ended questions about specific mental health symptoms (for example, “In the last 4 weeks, have there been times when you have been very sad, miserable, unhappy or tearful?”). If a participant responds positively to these structured items, they are subsequently asked open-ended questions about these problems (for example, “Please describe your mood—sadness or irritability—and your level of interest in things”). During the assessment, interviewers transcribe open-ended responses verbatim and are also able to add personal comments beneath each response.
A team of clinical raters assessed the DAWBA’s structured and qualitative information from all informants to decide whether an adolescent showed evidence of a DSM-5 or ICD-10 mental health condition that would warrant clinical treatment (Supplementary Figs. 1 and 2). To determine the presence of a condition, clinical raters (1) checked that the answers to structured comments were understood by the participants accurately; (2) interpreted any conflicts between child, parent and teacher responses and decided which assessment to prioritize; and (3) identified clinically impairing disorders that did not perfectly fit current operationalized diagnostic criteria or “not otherwise specified diagnosis” such as “other anxiety disorder”.
Overall, we coded information on mental health conditions into two separate variables: (1) a binary variable indicating the presence of any mental health condition (diagnosis or no diagnosis) and (2) a categorical variable for the type of condition (internalizing diagnosis, externalizing diagnosis or no diagnosis). We subdivided conditions identified via the diagnostic assessment into internalizing and externalizing using existing classifications of psychiatric diagnoses34,65 (Table 1). This distinction draws from transdiagnostic research showing that different conditions (for example, anxiety, depression and eating disorders) are often comorbid, share underlying core symptoms89 and can therefore be grouped to reflect clinical presentations with more validity34. Further, when we had enough power, we ran additional exploratory analyses examining responses to all social media questions (a–g) separately for individual conditions (specifically, major depressive disorder, generalized anxiety disorder and social anxiety disorder).
Comorbidity data were coded into two separate variables: (1) a binary variable indicating within-group comorbidity (any two diagnoses of either internalizing or externalizing: yes or no, for descriptive purposes only) and (2) a binary variable indicating internalizing–externalizing between-group comorbidity (any comorbid internalizing and externalizing diagnoses: yes or no). Individuals who showed between-group comorbidity were removed before the analysis of questions 2 and 3, given our goal to compare social media use between these groups. To increase the clinical utility of this work, we ran a sensitivity analysis for question 2, including people with between-group comorbidity.
Analysis plan
We conducted all statistical analyses in R version 4.3.1 (R Core Team, 2021), testing the association between time- and engagement-based measures of social media use and mental health conditions using equivalence tests and linear regression models90,91. To control for the type I error rate across multiple tests, we set a corrected alpha level of 0.0125, accounting for the false discovery rate across our four tested hypotheses for any given social media item92. Our analytical approach was based on regressions rather than analysis of variance, as the former allow for more diverse predictors, unbalanced groups and inclusion of covariates in potential exploratory analyses93. Below, we describe the statistical analyses we used to test our questions and hypotheses (see the Supplementary Information for more details). Further, the analysis code is available on OSF94.
Questions and hypotheses
Question 1: investigate whether adolescents with any mental health condition use social media differently than those without a condition
To address question 1, we tested the association between social media use and mental health conditions. Specifically, we estimated linear regression models with mental health condition as a binary predictor (two levels: diagnosis versus no diagnosis) and social media use as a continuous outcome. The no diagnosis group was set as the reference level for these analyses. Below, we report our null and directional hypotheses, first for dimensions of social media use expected to reflect mental health risks and second for dimensions expected to reflect mental health benefits in adolescents with versus without a condition.
H0(1.0): adolescents with any mental health condition will not differ from adolescents without a condition in (a) time spent on social media, (b) online social comparison, (c) lacking control over time spent online, (d) monitoring of online feedback, (e) feeling impacted by online feedback, (f) happiness about the number of online friendships, (g) honest online self-disclosure and (h) authentic self-presentation online.
H1(1.1): adolescents with any mental health condition will score higher than adolescents without a condition in (a) time on social media, (b) online social comparison, (c) lacking control over time spent online, (d) monitoring of online feedback and (e) feeling impacted by online feedback.
H1(1.2): adolescents with any mental health condition will score lower than adolescents without a condition in (f) happiness about the number of online friendships, (g) honest online self-disclosure and (h) authentic self-presentation online.
To examine whether social media use varies with mental health severity, we conducted sensitivity analyses to test for a linear effect of the number of diagnoses on the social media responses using linear regression models.
Question 2: investigate whether adolescents with an internalizing or externalizing condition use social media differently than those without a condition
After assessing differences in social media use in adolescents with versus without any mental health condition, we examined whether adolescents with internalizing or externalizing conditions use social media differently than adolescents without a condition. Hence, we conducted linear regression models with diagnostic category as a categorical predictor (three levels: internalizing diagnosis, externalizing diagnosis and no diagnosis) and social media use as a continuous outcome. To test our hypotheses, we examined comparisons between two levels of the diagnostic category variable, with no diagnosis set as the reference level. For hypotheses 2.0i, 2.1 and 2.2, we reported regression coefficients for internalizing versus no diagnosis, while for hypotheses 2.0e, 2.3 and 2.4 we reported coefficients for externalizing versus no diagnosis. The null hypotheses marked by ‘e’ or ‘i’ indicate that, for the considered comparison, the null hypothesis was our primary hypothesis. Hence, for those dimensions of social media use, we expected no difference between adolescents with internalizing or externalizing conditions and those without a condition. We used ‘e’ to indicate primary null hypotheses related to externalizing versus no condition and ‘i’ to indicate our primary null hypotheses related to internalising condition.
H0(2.0): adolescents with internalizing or externalizing conditions will not differ from adolescents without a condition in (a) time on social media, (b) online social comparisone, (c) lacking control over time spent onlinei, (d) monitoring of online feedbacke, (e) feeling impacted by online feedbacke, (f) happiness about the number of online friendships, (g) honest online self-disclosuree and (h) authentic self-presentation onlinee.
H1(2.1): adolescents with internalizing condition will score higher than adolescents without a condition in (a) time on social media, (b) online social comparison, (d) monitoring of online feedback and (e) feeling impacted by online feedback.
H1(2.2): adolescents with internalizing conditions will score lower than adolescents without a condition in (f) happiness about the number of online friendships, (g) honest online self-disclosure and (h) authentic self-presentation online.
H1(2.3): adolescents with externalizing conditions will score higher than adolescents without a condition in (a) time spent on social media and (c) lack of control over time spent online.
H1(2.4): adolescents with externalizing conditions will score lower than adolescents without a condition in (f) happiness about the number of online friendships.
Question 3: investigate whether adolescents with an internalizing mental health condition use social media differently than those with an externalizing condition
To address question 3, we examined how adolescents with internalizing conditions differed in social media engagement compared to adolescents with externalizing conditions. To this aim, we compared the internalizing and externalizing levels of the diagnostic category variable described in question 2, with internalizing as the reference level. Also, in this case, the null hypotheses marked by ‘c’ indicate our primary hypotheses. Hence, for those dimensions of social media use, we expected no difference between adolescents with internalizing and externalizing conditions.
H0 (3.0): adolescents with internalizing conditions will not differ from adolescents with externalizing conditions in (a) time on social mediac, (b) online social comparison, (c) lacking control over time spent online, (d) monitoring of online feedback, (e) feeling impacted by online feedback, (f) happiness about the number of online friendshipsc, (g) online self-disclosure and (h) authentic self-presentation online.
H1(3.1): adolescents with internalizing conditions will score higher than adolescents with externalizing conditions in (b) online social comparison, (d) monitoring of online feedback and (e) feeling impacted by online feedback.
H1(3.2): adolescents with internalizing conditions will score lower than adolescents with externalizing conditions in (c) lack of control over time spent online, (g) online self-disclosure and (h) authentic self-presentation online.
For all regression analyses, we treated the eight dimensions of social media use, including both time- and engagement-based measures, as separate outcomes predicted by information on mental health conditions as the only regressor. While it is common in research to use statistical control to remove confounding effects from a regression coefficient, appropriate control variables should be identified only after justifying a causal structure that includes the outcome, predictors and all theorized confounders. When the selected control variables are inappropriate or remain unjustified, controlling can result in biased regression estimates95. Further, recent literature warns against controlling for demographic factors such as sex without thought and instead prompts researchers to interrogate how this variable intersects with the predictors and outcomes under investigation96. In the present work, treating sex or age as a confounding variable would mean ignoring the possibility that there are meaningful sex or age differences in the examined relationships. As our goal is to investigate the overall association between social media use and mental health, we provided a descriptive account of the age and sex of adolescents included in each tested model rather than control for these demographics. For example, in question 1, age and sex of adolescents with any condition versus without a condition are reported for descriptive purposes (Table 3).
Equivalence testing
Given that null hypothesis significance testing does not allow a comprehensive interpretation of statistically non-significant results97, each model was complemented by equivalence tests97 using the bootstrapped two one-sided tests (TOST) with the ‘boot_T_TOST’ function from the TOSTER package91 to quantify support for the null hypothesis (H0(1–3)). This involves assessing whether the 90% CIs for the effect size lie inside prespecified equivalence bounds that indicate the SESOI. If the CIs lie inside the equivalence bounds, the effect size is interpreted as negligible. On the contrary, if the CIs spread outside the equivalence bounds, the effect size is considered meaningful in size. In this case, the 90% CIs are used rather than 95% because the effect size is tested against two equivalence bounds separately (that is, the upper and lower bound), reflecting (1 – 2α) × 100% (see the Supplementary Information for more details).
We established the equivalence bounds by identifying a theoretically meaningful SESOI (Cohen’s d = 0.4; refer to the Supplementary Methods for a detailed explanation). After an extensive scoping exercise to identify a suitable theoretical foundation, we determined that the most relevant benchmark for our research questions are everyday behaviours linked to mental health, such as sleep and physical activity. These behaviours, much like social media use, are a regular part of daily routines but, unlike social media use, they are well-established markers of psychopathology, based on both theory98–100 and matched empirical evidence101,102. Consequently, if the actual effect size of social media use is comparable to that observed for behaviours such as sleep and physical activity, we can confidently conclude that social media use also represents an everyday behaviour that exhibits meaningful group-level differences between clinical and non-clinical populations. The interpretation and analysis plan are presented separately for each hypothesis in the Supplementary Information.
Overall, we inferred support for the null hypotheses (that is, no meaningful difference in social media use between groups) if the 90% CI for this association lies within the equivalence bounds. Of note, while a theoretical SESOI based on everyday behaviours and their link to mental health served as our primary effect size of interest to allow for a clear confirmatory approach, we also identified secondary SESOIs based on the effect sizes that are practically and clinically meaningful. These secondary SESOIs play an important role in supporting the interpretation of our findings (as detailed in Supplementary Methods), ensuring the applicability of our study to both academic and practical domains.
Overall, we inferred support for the alternative hypotheses if (1) the coefficient for the association of social media use and our grouping variable for mental health diagnosis was significant, (2) the association followed the hypothesised direction and (3) the CIs for the association did not fall within the equivalence bounds. The interpretation and analysis plan are presented separately for each hypothesis in the Supplementary Information. Further, we detail the planned exploratory analyses in the Supplementary Methods.
Given that not all assumptions of linear models were met (Supplementary Table 9), we complemented our preregistered parametric analyses with exploratory nonparametric tests for all hypotheses (Supplementary Tables 10 and 11). We implemented the Brunner Munzel test based on the ‘brunner_munzel’ function for NHST and the ‘simple_htest’ function for equivalence testing from the TOSTER package in R91. This test, also known as the generalized Wilcoxon test, is a nonparametric test of stochastic equality between two samples that tests against the null hypothesis that for randomly selected values X (that is, social media score in the adolescents without a condition) and Y (that is, social media score in adolescents with a condition), the probability of X being greater than Y is equal to the probability of Y being greater than X. We documented all discrepancies (20% overall) between the parametric and nonparametric test results in Supplementary Tables 12–14.
Sampling plan
Inclusion criteria and sample size
We included all participants in the MHCYP 2017 survey aged between 11 and 19 years at the time of assessment who have answered any of the social media use questions with anything other than “don’t know”. Only individuals with diagnostic information, including the absence of a diagnosis, were included in the MHCYP dataset. Since we examined each social media use question separately, we included participants who answered at least one of the seven social media engagement questions or the question about time spent on social media. No specific documentation was available regarding the response rates for the social media questions. Given that the questionnaires were administered through interviews with professionals, we expected minimal missing data for the social media responses103. Hence, using a conservative estimate, we assumed a 5% missingness for our power calculations.
To address question 1, all adolescents with and without a condition were included in our analysis. Hence, in question 1, we included (1) participants with conditions other than internalizing or externalizing disorders (for example, autism spectrum disorder, tic disorder and psychotic disorders; Table 2); (2) participants with within-group comorbidity (multiple internalizing or externalizing diagnoses; for example, comorbid depressive and social anxiety disorder); and (c) participants with between-group comorbidity (both internalizing and externalizing conditions; for example, comorbid depressive and attention deficit hyperactivity disorder).
In contrast, for questions 2 and 3, we included (1) participants with internalizing or externalizing conditions only and (2) participants with within-group comorbidity (multiple internalizing or externalizing diagnoses). Hence, participants with other conditions or between-group comorbidity were excluded from the main analysis, given our goal to compare social media use in adolescents with externalizing and internalizing conditions. However, we ran sensitivity analyses to test the impact of including participants with between-group comorbidities in question 2.
On the basis of the summary demographics83, after accounting for potential missing data, we estimated the sample of complete cases to be around N = 3,854 (accounting for 5% missingness in the sample of N = 4,057, 11–19-year olds), approximately 15% of whom received at least one mental health diagnosis (N = 577). Available documentation83 suggests that approximately 19.2% of individuals with internalizing conditions have at least one comorbid externalizing condition, and approximately 28% of individuals with externalizing diagnoses have at least one comorbid internalizing diagnosis. This suggests approximately N = 370 with internalizing-only diagnoses and N = 199 with externalizing-only diagnoses.
Power calculations
We calculated the power by setting the SESOI (d = 0.4, refer to Supplementary Methods for a detailed explanation), the alpha level to 0.05 and the estimated sample size (estimated N = 3,854 based on existing MHCYP documentation). For the equivalence tests, power was calculated using the TOSTER package in R91,104. For the regression models, power was determined using the pwr package105 in R. The code for these calculations is available on the OSF94.
H0(1). We calculated the power for equivalence testing to detect a SESOI of d = 0.4 given at least N ≥ 577 individuals with a condition and N ≥ 3,277 individuals without a condition. The results indicate 100% power to reject the presence of effects that are larger than d = 0.4.
H1(1). We calculated the power to detect a statistical effect of condition on social media responses using linear regression. The results indicate 100% power to detect the SESOI (d = 0.4) with at least N ≥ 577 individuals with a condition and N ≥ 3,277 individuals without a condition.
H0(2). We calculated the power for equivalence testing to detect a SESOI of d = 0.4 given at least N ≥ 370 individuals with an internalizing only condition and N ≥ 3,277 with no condition. The results indicate 100% power to reject the presence of effects that are larger than d = 0.4. We calculated the power for equivalence testing to detect a SESOI of d = 0.4 given at least N > 199 individuals with an externalizing only condition and N > 3,277 with no condition. The results indicate 100% power to reject the presence of effects that are larger than d = 0.4.
H1(2). We calculated the power to detect a statistical effect of internalizing condition type (internalizing versus no condition) on social media responses using linear regression. The results indicate 100% power to detect the SESOI (d = 0.4) with at least N ≥ 370 individuals with an internalizing-only condition and N ≥ 3,277 with no condition. We calculated power to detect an effect of externalizing diagnosis type (that is, externalizing versus no condition) on social media responses using linear regression. The results indicate 100% power to detect the SESOI (d = 0.4) with at least N ≥ 199 individuals with an externalizing-only condition and N ≥ 3,277 with no condition.
H0(3). We calculated the power for equivalence testing to detect a SESOI of d = 0.4 given at least N ≥ 370 individuals with internalizing only and N ≥ 199 with externalizing only conditions. The results indicate 96% power to reject the presence of effects that are larger than d = 0.4.
H1(3). We calculated the power to detect a statistical effect of internalizing-only versus externalizing-only condition type on social media responses. The results indicate 99.8% power to the SESOI (d = 0.4) with at least N ≥ 370 individuals with internalizing only and N ≥ 199 with externalizing only conditions.
In addition to our a priori power calculations, we conducted power sensitivity analyses with the final sample size105. That is, we determined the smallest effect size that is observable with 95% power, given the corrected alpha of 0.0125 and our final sample size (Supplementary Table 22).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Supplementary Methods including Tables 1–4 and Figs. 1 and 2 and Results including Tables 5–22 and Figs. 3–5.
Source data
Statistical source data for Fig. 1.
Acknowledgements
The UK Medical Research Council DTP PhD programme (RG86932) funded L.F. The Jacobs Foundation (CERES SUAI/084 G114119), the UK Medical Research Council (MC_UU_00030/13) and a UKRI Future Leaders Fellowship (MR/X034925/1) funded A.M.F., L.F. and A.O. The Huo Family Foundation, and the ESRC (ES/Y010736/1 and ES/T008709/1) funded A.K.P. Both A.K.P. and A.O. were supported by the Economic and Social Research Council (ES/T008709/1). T.J.F. is supported by the National Institute for Health and Care Research (NIHR204413, NIHR153625 and NIHR202025), the Swedish Research Council for Health Working Life and Welfare (2022-01002_Forte), and the Medical Research Council (MC_PC_20052). All research at the Department of Psychiatry in the University of Cambridge is supported by the NIHR Cambridge Biomedical Research Centre (NIHR203312) and the NIHR Applied Research Collaboration East of England. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. T.J.F.’s research group receives funding from Place2Be, a third sector organisation that provides mental health training and intervention to UK schools. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. The MHCYP 2017 survey was funded by the Department of Health and Social Care, commissioned by NHS Digital, and carried out by the National Centre for Social Research, the Office for National Statistics and Youthinmind. We are very grateful to all the adolescents and families who took part in the study, the personnel for their help in recruiting them and the whole NHS Digital team that includes interviewers, technicians, research scientists, volunteers, managers, receptionists, nurses and the clinical raters. A special thank you to D. Lakens, M. Vuorre and A.R. Caldwell for their valuable advice on the statistical analyses.
Author contributions
We present author contributions according to the CRediT (Contributor Roles Taxonomy). L.F.: conceptualization, methodology, formal analysis, writing— original draft, writing—review and editing. A.M.F.: conceptualization, methodology, formal analysis, writing—review and editing. A.K.P.: methodology, writing—review and editing, supervision. T.J.F.: writing—review and editing, supervision, resources, project administration. A.O.: conceptualization, methodology, writing—original draft, writing—review and editing, supervision. Of note, none of the authors that conceptualized the analysis previously accessed the MHCYP dataset. For the purpose of open access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising from this submission.
Peer review
Peer review information
Nature Human Behaviour thanks Candice Biernesser, Johannes Breuer, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Data availability
The MHCYP dataset is held on behalf of NHS Digital by the UK Data Service. Restrictions apply to the availability of this data for privacy and ethical reasons, which were used under license for this study. Data access can be requested by applying to the Data Access Request Service (DARS; number: DARS-NIC-424336-T7K7T-v0.6). Researchers interested in accessing the data can find further information via the DARS website at https://digital.nhs.uk/services/data-access-request-service-dars/dars-guidance. Source data are provided with this paper.
Code availability
The analysis code can be found on the OSF94.
Competing interests
The authors declare no competing interests.
Footnotes
Protocol registration The Stage 1 protocol for this Registered Report was accepted in principle on 7 December 2023. The protocol, as accepted by the journal, is available via Figshare at https://figshare.com/s/730e3b0d4da82e9b6a46.
Change history
5/12/2025
In the version of the article initially published, in Table 3, the row labels "Internalizing" and "Externalizing" were switched and have now been corrected so that "Externalizing" corresponds with N = 104 and "Internalizing" corresponds with N = 282. Additionally, in the "Internalizing versus externalizing conditions" section, "s.e.m. of 0191" should have read "s.e.m. of 0.191". These corrections have been made to the HTML and PDF versions of the article.
Supplementary information
The online version contains supplementary material available at 10.1038/s41562-025-02134-4.
References
- 1.World Health Organization. Mental health of adolescents https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (2024).
- 2.NHS. Mental Health of Children and Young People in England in 2022 https://digital.nhs.uk/news/2022/rate-of-mental-disorders-among-17-to-19-year-olds-increased-in-2022-new-report-shows (2022).
- 3.Paus, T., Keshavan, M. & Giedd, J. N. Why do many psychiatric disorders emerge during adolescence? Nat. Rev. Neurosci.9, 947–957 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whiteford, H. A. et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet382, 1575–1586 (2013). [DOI] [PubMed] [Google Scholar]
- 5.Ofcom. Children's Media Use and Attitudes Reporthttps://www.ofcom.org.uk/__data/assets/pdf_file/0024/234609/childrens-media-use-and-attitudes-report-2022.pdf (2022).
- 6.Orben, A. Teenagers, screens and social media: a narrative review of reviews and key studies. Soc. Psychiatry Psychiatr. Epidemiol.55, 407–414 (2020). [DOI] [PubMed] [Google Scholar]
- 7.Yoon, S., Kleinman, M., Mertz, J. & Brannick, M. Is social network site usage related to depression? A meta-analysis of Facebook–depression relations. J. Affect. Disord.248, 65–72 (2019). [DOI] [PubMed] [Google Scholar]
- 8.Cunningham, S., Hudson, C. C. & Harkness, K. Social media and depression symptoms: a meta-analysis. Res. Child Adolesc. Psychopathol.49, 241–253 (2021). [DOI] [PubMed] [Google Scholar]
- 9.Woods, H. C. & Scott, H. #Sleepyteens: social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. J. Adolesc.51, 41–49 (2016). [DOI] [PubMed] [Google Scholar]
- 10.Wilksch, S. M., O’Shea, A., Ho, P., Byrne, S. & Wade, T. D. The relationship between social media use and disordered eating in young adolescents. Int. J. Eat. Disord.53, 96–106 (2020). [DOI] [PubMed] [Google Scholar]
- 11.Beeres, D. T., Andersson, F., Vossen, H. G. M. & Galanti, M. R. Social media and mental health among early adolescents in Sweden: a longitudinal study with 2-year follow-up (KUPOL Study). J. Adolesc. Health68, 953–960 (2021). [DOI] [PubMed] [Google Scholar]
- 12.Boer, M., Stevens, G., Finkenauer, C., de Looze, M. & van den Eijnden, R. Social media use intensity, social media use problems, and mental health among adolescents: investigating directionality and mediating processes. Comput. Hum. Behav.116, 106645 (2021). [Google Scholar]
- 13.Twenge, J. M., Joiner, T. E., Rogers, M. L. & Martin, G. N. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clin. Psychol. Sci.6, 3–17 (2018). [Google Scholar]
- 14.Wait until 8th https://www.waituntil8th.org/ (2024).
- 15.Valkenburg, P. M., Meier, A. & Beyens, I. Social media use and its impact on adolescent mental health: an umbrella review of the evidence. Curr. Opin. Psychol.44, 58–68 (2022). [DOI] [PubMed] [Google Scholar]
- 16.Odgers, C. L. & Jensen, M. R. Annual research review: adolescent mental health in the digital age: facts, fears, and future directions. J. Child Psychol. Psychiatry61, 336–348 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Orben, A. & Przybylski, A. K. The association between adolescent well-being and digital technology use. Nat. Hum. Behav.3, 173–182 (2019). [DOI] [PubMed] [Google Scholar]
- 18.Twenge, J. M., Haidt, J., Joiner, T. E. & Campbell, W. K. Underestimating digital media harm. Nat. Hum. Behav.4, 346–348 (2020). [DOI] [PubMed] [Google Scholar]
- 19.Orben, A. & Przybylski, A. K. Reply to: underestimating digital media harm. Nat. Hum. Behav.4, 349–351 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beyens, I., Pouwels, J. L., van Driel, I. I., Keijsers, L. & Valkenburg, P. M. The effect of social media on well-being differs from adolescent to adolescent. Sci. Rep.10, 10763 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johannes, N., Dienlin, T., Bakhshi, H. & Przybylski, A. K. No effect of different types of media on well-being. Sci. Rep.12, 61 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Orben, A., Przybylski, A. K., Blakemore, S.-J. & Kievit, R. A. Windows of developmental sensitivity to social media. Nat. Commun.13, 1649 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelly, Y., Zilanawala, A., Booker, C. & Sacker, A. Social media use and adolescent mental health: findings from the UK Millennium Cohort Study. EClinicalMedicine6, 59–68 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Booker, C. L., Kelly, Y. J. & Sacker, A. Gender differences in the associations between age trends of social media interaction and well-being among 10–15 year olds in the UK. BMC Public Health18, 321 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghai, S., Fassi, L., Awadh, F. & Orben, A. Lack of sample diversity in research on adolescent depression and social media use: a scoping review and meta-analysis. Clin. Psychol. Sci.11, 759–772 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fassi, L. et al. Social media use and internalizing symptoms in clinical and community adolescent samples: a systematic review and meta-analysis. JAMA Pediatr.178, 814–822 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand.67, 361–370 (1983). [DOI] [PubMed] [Google Scholar]
- 28.Boyd, J. H. Screening for depression in a community sample: understanding the discrepancies between depression symptom and diagnostic scales. Arch. Gen. Psychiatry39, 1195 (1982). [DOI] [PubMed] [Google Scholar]
- 29.Manea, L., Gilbody, S. & McMillan, D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. Can. Med. Assoc. J.184, E191–E196 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Radovic, A., Gmelin, T., Stein, B. D. & Miller, E. Depressed adolescents’ positive and negative use of social media. J. Adolesc.55, 5–15 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weinstein, E. et al. Positive and negative uses of social media among adolescents hospitalized for suicidal behavior. J. Adolesc.87, 63–73 (2021). [DOI] [PubMed] [Google Scholar]
- 32.Nesi, J., Wolff, J. C. & Hunt, J. Patterns of social media use among adolescents who are psychiatrically hospitalized. J. Am. Acad. Child Adolesc. Psychiatry58, 635–639.e1 (2019). [DOI] [PubMed] [Google Scholar]
- 33.Gurbuz, H., Demir, T., Ozcan, B., Kadak, M. & Poyraz, B. Use of social network sites among depressed adolescents. Behav. Inf. Technol.36, 517–523 (2017). [Google Scholar]
- 34.Eaton, N. R. et al. The structure and predictive validity of the internalizing disorders. J. Abnorm. Psychol.122, 86–92 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn (American Psychiatric Association, 2022).
- 36.NHS Digital. Mental Health of Children and Young Peoplehttps://files.digital.nhs.uk/20/1DEB0D/MHCYP%202017%20Appendix%20F%20-%20Project%20Instructions.pdf (2017).
- 37.Meier, A. & Reinecke, L. Computer-mediated communication, social media, and mental health: a conceptual and empirical meta-review. Commun. Res. 48, (2020).
- 38.Verbeij, T., Pouwels, J. L., Beyens, I. & Valkenburg, P. M. The accuracy and validity of self-reported social media use measures among adolescents. Comput. Hum. Behav. Rep.3, 100090 (2021). [Google Scholar]
- 39.Dumas, T. M., Tremblay, P. F., Ellis, W., Millett, G. & Maxwell-Smith, M. A. Does pressure to gain social media attention have consequences for adolescents’ friendship closeness and mental health? A longitudinal examination of within-person cross-lagged relations. Comput. Hum. Behav.140, 107591 (2023). [Google Scholar]
- 40.Frison, E. & Eggermont, S. Browsing, posting, and liking on Instagram: the reciprocal relationships between different types of Instagram use and adolescents’ depressed mood. Cyberpsychol. Behav. Soc. Netw.20, 603–609 (2017). [DOI] [PubMed] [Google Scholar]
- 41.Nesi, J., Miller, A. B. & Prinstein, M. J. Adolescents’ depressive symptoms and subsequent technology-based interpersonal behaviors: a multi-wave study. J. Appl. Dev. Psychol.51, 12–19 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li, J.-B. et al. Associations of intensity and emotional connection related to online social networking use on the risk of incident depression among Chinese adolescents: a prospective cohort study. J. Affect. Disord.308, 116–122 (2022). [DOI] [PubMed] [Google Scholar]
- 43.Krayer, A., Ingledew, D. K. & Iphofen, R. Social comparison and body image in adolescence: a grounded theory approach. Health Educ. Res.23, 892–903 (2007). [DOI] [PubMed] [Google Scholar]
- 44.Corning, A. F., Krumm, A. J. & Smitham, L. A. Differential social comparison processes in women with and without eating disorder symptoms. J. Couns. Psychol.53, 338–349 (2006). [Google Scholar]
- 45.Goodman, R. J., Samek, D. R., Wilson, S., Iacono, W. G. & McGue, M. Close relationships and depression: a developmental cascade approach. Dev. Psychopathol.31, 1451–1465 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thwaites, R. & Dagnan, D. Moderating variables in the relationship between social comparison and depression: an evolutionary perspective. Psychol. Psychother. Theory Res. Pract.77, 309–323 (2004). [DOI] [PubMed] [Google Scholar]
- 47.Troop, N. A. Social rank, rank-related life events and eating pathology. Eur. Eat. Disord. Rev.24, 75–77 (2016). [DOI] [PubMed] [Google Scholar]
- 48.Rao, P. A. et al. Social anxiety disorder in childhood and adolescence: descriptive psychopathology. Behav. Res. Ther.45, 1181–1191 (2007). [DOI] [PubMed] [Google Scholar]
- 49.Verduyn, P., Gugushvili, N., Massar, K., Täht, K. & Kross, E. Social comparison on social networking sites. Curr. Opin. Psychol.36, 32–37 (2020). [DOI] [PubMed] [Google Scholar]
- 50.Chou, H.-T. G. & Edge, N. “They are happier and having better lives than i am”: the impact of using Facebook on perceptions of others’ lives. Cyberpsychol. Behav. Soc. Netw.15, 117–121 (2012). [DOI] [PubMed] [Google Scholar]
- 51.Gonzales, A. L. & Hancock, J. T. Mirror, mirror on my Facebook wall: effects of exposure to Facebook on self-esteem. Cyberpsychol. Behav. Soc. Netw.14, 79–83 (2011). [DOI] [PubMed] [Google Scholar]
- 52.Pempek, T. A., Yermolayeva, Y. A. & Calvert, S. L. College students’ social networking experiences on Facebook. J. Appl. Dev. Psychol.30, 227–238 (2009). [Google Scholar]
- 53.Strauman, T. J. Self-regulation and psychopathology: toward an integrative translational research paradigm. Annu. Rev. Clin. Psychol.13, 497–523 (2017). [DOI] [PubMed] [Google Scholar]
- 54.Nesi, J. & Prinstein, M. J. Using social media for social comparison and feedback-seeking: gender and popularity moderate associations with depressive symptoms. J. Abnorm. Child Psychol.43, 1427–1438 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gillett, D. A. & Mazza, S. J. Clarifying a construct: an integrative functional model of reassurance-seeking behaviors. J. Ration. -Emot. Cogn. -Behav. Ther.36, 362–377 (2018). [Google Scholar]
- 56.Tobias, M. R. & Ito, T. A. Anxiety increases sensitivity to errors and negative feedback over time. Biol. Psychol.162, 108092 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tucker, D. M., Luu, P., Frishkoff, G., Quiring, J. & Poulsen, C. Frontolimbic response to negative feedback in clinical depression. J. Abnorm. Psychol.112, 667–678 (2003). [DOI] [PubMed] [Google Scholar]
- 58.Asselmann, E., Wittchen, H.-U., Lieb, R. & Beesdo-Baum, K. Sociodemographic, clinical, and functional long-term outcomes in adolescents and young adults with mental disorders. Acta Psychiatr. Scand.137, 6–17 (2018). [DOI] [PubMed] [Google Scholar]
- 59.McBride, S. & Preyde, M. Loneliness and social isolation in a sample of youth hospitalized for psychiatric illness. Child Adolesc. Soc. Work J.39, 157–166 (2022). [Google Scholar]
- 60.Sibley, M. H., Evans, S. W. & Serpell, Z. N. Social cognition and interpersonal impairment in young adolescents with ADHD. J. Psychopathol. Behav. Assess.32, 193–202 (2010). [Google Scholar]
- 61.Horesh, N. & Apter, A. Self-disclosure, depression, anxiety, and suicidal behavior in adolescent psychiatric inpatients. Crisis27, 66–71 (2006). [DOI] [PubMed] [Google Scholar]
- 62.Chen, H. Antecedents of positive self-disclosure online: an empirical study of US college students’ Facebook usage. Psychol. Res. Behav. Manag.10, 147–153 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Flett, G. L. & Hewitt, P. L. in Social Anxiety, 159–187 (Academic Press, 2014).
- 64.Jain, M. & Sudhir, P. M. Dimensions of perfectionism and perfectionistic self-presentation in social phobia. Asian J. Psychiatry3, 216–221 (2010). [DOI] [PubMed] [Google Scholar]
- 65.Krueger, R. F., McGue, M. & Iacono, W. G. The higher-order structure of common DSM mental disorders: internalization, externalization, and their connections to personality. Personal. Individ. Differ.30, 1245–1259 (2001). [Google Scholar]
- 66.Nesi, J. et al. Selfie appearance investment and peer feedback concern: multimethod investigation of adolescent selfie practices and adjustment. Psychol. Pop. Media10, 488–499 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Higgins, E. T. Self-discrepancy: a theory relating self and affect. Psychol. Rev.94, 319–340 (1987). [PubMed] [Google Scholar]
- 68.Sassaroli, S. et al. Perfectionism in depression, obsessive-compulsive disorder and eating disorders. Behav. Res. Ther.46, 757–765 (2008). [DOI] [PubMed] [Google Scholar]
- 69.Calvo, R. et al. Obsessive–compulsive personality disorder traits and personality dimensions in parents of children with obsessive–compulsive disorder. Eur. Psychiatry24, 201–206 (2009). [DOI] [PubMed] [Google Scholar]
- 70.O’Connor, R. C., Rasmussen, S. & Hawton, K. Predicting depression, anxiety and self-harm in adolescents: the role of perfectionism and acute life stress. Behav. Res. Ther.48, 52–59 (2010). [DOI] [PubMed] [Google Scholar]
- 71.George, M. J. et al. Young adolescents’ digital technology use, perceived impairments, and well-being in a representative sample. J. Pediatr.219, 180–187 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hussain, Z. & Griffiths, M. D. Problematic social networking site use and comorbid psychiatric disorders: a systematic review of recent large-scale studies. Front. Psychiatry9, 686 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dawson, A. E., Wymbs, B. T., Evans, S. W. & DuPaul, G. J. Exploring how adolescents with ADHD use and interact with technology. J. Adolesc.71, 119–137 (2019). [DOI] [PubMed] [Google Scholar]
- 74.Gillard, J. A. et al. Converging evidence for enduring perceptions of low social status in individuals in remission from depression. J. Affect. Disord.294, 661–670 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bagwell, C. L., Molina, B. S. G., Pelham, W. E. & Hoza, B. Attention-deficit hyperactivity disorder and problems in peer relations: predictions from childhood to adolescence. J. Am. Acad. Child Adolesc. Psychiatry40, 1285–1292 (2001). [DOI] [PubMed] [Google Scholar]
- 76.Barry, C. T., Sidoti, C. L., Briggs, S. M., Reiter, S. R. & Lindsey, R. A. Adolescent social media use and mental health from adolescent and parent perspectives. J. Adolesc.61, 1–11 (2017). [DOI] [PubMed] [Google Scholar]
- 77.Parry, D. A. et al. A systematic review and meta-analysis of discrepancies between logged and self-reported digital media use. Nat. Hum. Behav.5, 1535–1547 (2021). [DOI] [PubMed] [Google Scholar]
- 78.Allen, N. B. & Badcock, P. B. T. The social risk hypothesis of depressed mood: evolutionary, psychosocial, and neurobiological perspectives. Psychol. Bull.129, 887–913 (2003). [DOI] [PubMed] [Google Scholar]
- 79.Stuart, A. L. et al. Comparison of self-report and structured clinical interview in the identification of depression. Compr. Psychiatry55, 866–869 (2014). [DOI] [PubMed] [Google Scholar]
- 80.Mathai, J., Anderson, P. & Bourne, A. Comparing psychiatric diagnoses generated by the strengths and difficulties questionnaire with diagnoses made by clinicians. Aust. N. Z. J. Psychiatry38, 639–643 (2004). [DOI] [PubMed] [Google Scholar]
- 81.Valkenburg, P. M. & Peter, J. Social consequences of the internet for adolescents: a decade of research. Curr. Dir. Psychol. Sci.18, 1–5 (2009). [Google Scholar]
- 82.Bunker, C. J. & Kwan, V. S. Y. Similarity between perceived selves on social media and offline and its relationship with psychological well-being in early and late adulthood. Comput. Hum. Behav.152, 108025 (2024). [Google Scholar]
- 83.NHS. Mental Health of Children and Young People in England, 2017 https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2017/2017 (2017).
- 84.Rhemtulla, M., Brosseau-Liard, P, É. & Savalei, V. When can categorical variables be treated as continuous? A comparison of robust continuous and categorical SEM estimation methods under suboptimal conditions. Psychol. Methods17, 354–373 (2012). [DOI] [PubMed] [Google Scholar]
- 85.Youthinmind. Development and Well-Being Assessment (DAWBA) https://dawba.info/ (2012).
- 86.Youthinmind. Strengths and Difficulties Questionnaire (SDQ) https://www.sdqinfo.org/a0.html (2022).
- 87.Goodman, R., Ford, T., Richards, H., Gatward, R. & Meltzer, H. The development and well‐being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J. Child Psychol. Psychiatry41, 645–655 (2000). [PubMed] [Google Scholar]
- 88.Aebi, M. et al. The use of the development and well-being assessment (DAWBA) in clinical practice: a randomized trial. Eur. Child Adolesc. Psychiatry21, 559–567 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kamper-DeMarco, K. E., Shankman, J., Fearey, E., Lawrence, H. R. & Schwartz-Mette, R. A. Linking social skills and adjustment. Soc. Ski. Life Span 47–66 (2020).
- 90.Chambers, J. M. lm function—stats package (version 3.6.2). https://www.rdocumentation.org/packages/stats/versions/3.6.2/topics/lm (1992).
- 91.Caldwell, A. R. Exploring equivalence testing with the updated TOSTER R package (preprint). Open Science Framework10.31234/osf.io/ty8de (2022).
- 92.Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B Methodol.57, 289–300 (1995). [Google Scholar]
- 93.Judd, C. M., McClelland, G. H., & Ryan, C. S. Data Analysis: a Model Comparison Approach to Regression, ANOVA, and Beyond (Routledge, 2017).
- 94.Fassi et al. Registered Report: social media use in adolescents with and without mental health conditions. Open Science Framework,https://osf.io/s2dwu/?view_only=5acced2ddb884f9481d439a7746f4dd1 (2025).
- 95.Wysocki, A. C., Lawson, K. M. & Rhemtulla, M. Statistical control requires causal justification. Adv. Methods Pract. Psychol. Sci.5, 251524592210958 (2022). [Google Scholar]
- 96.Shapiro, J. R., Klein, S. L. & Morgan, R. Stop ‘controlling’ for sex and gender in global health research. BMJ Glob. Health6, e005714 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lakens, D. Equivalence tests: a practical primer for t tests, correlations, and meta-analyses. Soc. Psychol. Personal. Sci.8, 355–362 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Crone, D., Smith, A. & Gough, B. ‘I feel totally at one, totally alive and totally happy’: a psycho-social explanation of the physical activity and mental health relationship. Health Educ. Res20, 600–611 (2005). [DOI] [PubMed] [Google Scholar]
- 99.Knowlden, A. P., Sharma, M. & Bernard, A. L. A theory of planned behavior research model for predicting the sleep intentions and behaviors of undergraduate college students. J. Prim. Prev.33, 19–31 (2012). [DOI] [PubMed] [Google Scholar]
- 100.Rebar, A. L. & Taylor, A. Physical activity and mental health; it is more than just a prescription. Ment. Health Phys. Act.13, 77–82 (2017). [Google Scholar]
- 101.Mollayeva, T. et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med. Rev.25, 52–73 (2016). [DOI] [PubMed] [Google Scholar]
- 102.Ruscio, J. A probability-based measure of effect size: robustness to base rates and other factors. Psychol. Methods13, 19–30 (2008). [DOI] [PubMed] [Google Scholar]
- 103.Mirzaei, A., Carter, S. R., Patanwala, A. E. & Schneider, C. R. Missing data in surveys: key concepts, approaches, and applications. Res. Soc. Adm. Pharm.18, 2308–2316 (2022). [DOI] [PubMed] [Google Scholar]
- 104.Lakens, D., Scheel, A. M. & Isager, P. M. Equivalence testing for psychological research: a tutorial. Adv. Meth. Pract. Psychol. Sci.1, 259–269 (2018). [Google Scholar]
- 105.Champely, S. pwr package (version 1.3-0). https://cran.r-project.org/web/packages/pwr/pwr.pdf (2020).
- 106.Hamilton, J. L. et al. Social media use and prospective suicidal thoughts and behaviors among adolescents at high risk for suicide. Suicide Life Threat. Behav.51, 1203–1212 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Riehm, K. E. et al. Associations between time spent using social media and internalizing and externalizing problems among US youth. JAMA Psychiatry76, 1266–1273 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bayer, J. B., Anderson, I. A. & Tokunaga, R. S. Building and breaking social media habits. Curr. Opin. Psychol.45, 101303 (2022). [DOI] [PubMed] [Google Scholar]
- 109.Winds, K., Aebi, M. & Plattner, B. Problematic internet use among adolescent male and female psychiatric inpatients: a gender perspective. Child Psychiatry Hum. Dev. 10.1007/s10578-022-01408-6 (2022). [DOI] [PMC free article] [PubMed]
- 110.Clerkin, E. M., Smith, A. R. & Hames, J. L. The interpersonal effects of Facebook reassurance seeking. J. Affect. Disord.151, 525–530 (2013). [DOI] [PubMed] [Google Scholar]
- 111.Hames, J. L., Hagan, C. R. & Joiner, T. Interpersonal Processes in Depression. Annu. Rev. Clin. Psychol.9, 355–377 (2013). [DOI] [PubMed] [Google Scholar]
- 112.Elhai, J. D., Gallinari, E. F., Rozgonjuk, D. & Yang, H. Depression, anxiety and fear of missing out as correlates of social, non-social and problematic smartphone use. Addict. Behav.105, 106335 (2020). [DOI] [PubMed] [Google Scholar]
- 113.Gotlib, I. H. Perception and recall of interpersonal feedback: negative bias in depression. Cogn. Ther. Res.7, 399–412 (1983). [Google Scholar]
- 114.Viner, R. M. et al. Adolescence and the social determinants of health. Lancet379, 1641–1652 (2012). [DOI] [PubMed] [Google Scholar]
- 115.Sprecher, S. & Hendrick, S. S. Self-disclosure in intimate relationships: associations with individual and relationship characteristics over time. J. Soc. Clin. Psychol.23, 857–877 (2004). [Google Scholar]
- 116.Reece, A. G. & Danforth, C. M. Instagram photos reveal predictive markers of depression. EPJ Data Sci.6, 15 (2017). [Google Scholar]
- 117.Omarzu, J. A disclosure decision model: determining how and when individuals will self-disclose. Personal. Soc. Psychol. Rev.4, 174–185 (2000). [Google Scholar]
- 118.van den Bos, E., de Rooij, M., Miers, A. C., Bokhorst, C. L. & Westenberg, P. M. Adolescents’ increasing stress response to social evaluation: pubertal effects on cortisol and alpha-amylase during public speaking. Child Dev.85, 220–236 (2014). [DOI] [PubMed] [Google Scholar]
- 119.Vijayakumar, N. et al. Getting to know me better: an fMRI study of intimate and superficial self-disclosure to friends during adolescence. J. Pers. Soc. Psychol.118, 885–899 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Methods including Tables 1–4 and Figs. 1 and 2 and Results including Tables 5–22 and Figs. 3–5.
Statistical source data for Fig. 1.
Data Availability Statement
The MHCYP dataset is held on behalf of NHS Digital by the UK Data Service. Restrictions apply to the availability of this data for privacy and ethical reasons, which were used under license for this study. Data access can be requested by applying to the Data Access Request Service (DARS; number: DARS-NIC-424336-T7K7T-v0.6). Researchers interested in accessing the data can find further information via the DARS website at https://digital.nhs.uk/services/data-access-request-service-dars/dars-guidance. Source data are provided with this paper.
The analysis code can be found on the OSF94.