Abstract
Hyperkalemia can lead to life-threatening arrhythmias, regardless of serum potassium levels. The electrocardiogram morphology lacks sensitivity and specificity in indicating the severity of hyperkalemia. Here, we present a case of an elderly woman with a history of end-stage renal disease on hemodialysis who developed sinus arrest due to moderate hyperkalemia without typical electrocardiographic findings of hyperkalemia, with subsequent restoration of sinus rhythm after correcting the electrolytic disturbance. The case highlights the importance of clinicians maintaining a high degree of suspicion for electrocardiographic abnormalities related to hyperkalemia, even in the absence of typical ECG findings, to ensure accurate diagnosis and timely intervention.
Keywords: hyperkalemia; sinus arrest, cardiac; case report
Introduction
Hyperkalemia, defined as a serum potassium level exceeding 5.5 mmol/l, is a common electrolyte disturbance associated with potentially severe cardiac arrhythmias [1]. Chronic kidney disease (CKD) is the most frequent cause of hyperkalemia. While the prevalence in the general population is 2%-3%, it may increase to 40%-50% in elderly patients with CKD [2].
Hyperkalemia is categorized based on serum potassium levels as mild (5.5-6.5 mmol/l), moderate (6.5-7.5 mmol/l), and severe (>7.5 mmol/l) [3]. Elevated serum potassium levels in the blood can be detected through a surface electrocardiogram (ECG). Typically, the ECG shows peaked and tall T-waves with serum potassium at 5.5-6.5 mmol/l, a disappearance of P-waves when levels reach 6.5-7.5 mmol/l, a widened QRS complex at 7-8 mmol/l, and eventually a sine wave pattern when serum potassium exceeds 8 mmol/l. It is also noted that sinus arrest, significant intraventricular conduction delay, ventricular tachycardia, and ventricular fibrillation may occur at potassium levels above 10 mmol/l [4]. Nevertheless, typical ECG changes are not always evident. In addition, hyperkalemia can cause life-threatening arrhythmias, regardless of serum potassium level. The severity of clinical symptoms is influenced not only by serum potassium levels but also by the speed of onset, accompanying electrolyte disturbances, medications, and other existing health conditions. In patients with CKD, variations in calcium levels could influence the ECG’s ability to predict hyperkalemia. Additionally, advanced age and diabetes are associated with a decreased likelihood of peaked T waves caused by hyperkalemia [4]. Herein, we present a case of sinus arrest due to moderate hyperkalemia in an elderly patient with CKD.
Case report
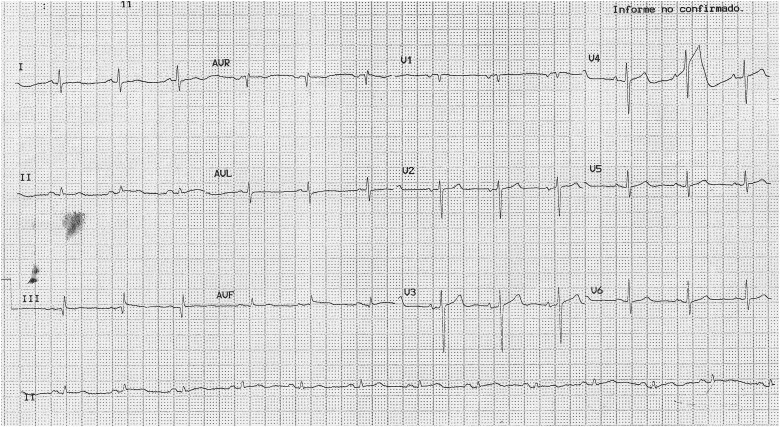
An 82-year-old woman was admitted to the Emergency Department with a three-day history of weakness and dyspnea. She had a 20-year history of hypertension and type 2 diabetes, as well as a 5-year history of end-stage renal disease on hemodialysis. Her medications included telmisartan 40 mg twice daily, prazosin 1 mg twice daily, calcitriol 0.25 mcg twice daily, linagliptin 5 mg/day, furosemide 40 mg/day, and erythropoietin 4000 units two times weekly. There was no history of use of negative chronotropic drugs. On presentation, her vital signs were as follows: blood pressure, 158/72 mmHg; pulse, 37 beats per minute; and peripheral capillary oxygen saturation level, 95% on room air. Physical examination revealed a somnolent patient presenting with bradycardia. No other abnormalities were observed. Initial laboratory tests were as follows: hematocrit 41.1% (normal range [NR] 39—59), blood urea nitrogen 58 mg/dL (NR 8—21), creatinine 3.14 mg/dL (NR 0.55—1.3), sodium 119 mmol/l (NR 135—145), potassium 6.15 mmol/l (NR 3.5—5.1), calcium 8.6 mg/dL (NR 8.4—10.2), magnesium 2.23 mg/dL (NR 1.6—2.5). Arterial blood gas analysis showed pH 7.35 (NR 7.35—7.45), pO2 85 mm Hg (NR 83—108), pCO2 41 mm Hg (NR 35—48), and HCO3- 22.6 mmol/l (NR 22—28). A 12-lead ECG tracing revealed bradycardia at 38 beats per minute without sinus activity (Fig. 1).
Figure 1.
Sinus arrest at 38 bpm with junctional escape rhythm and retrograde atrial activation (black dots). No typical manifestations of hyperkalemia are observed.
Initially, the patient received pharmacological treatment for hyperkalemia with 120 mg of furosemide, 2 g of calcium gluconate, 7 U of intravenous insulin with 25 mL of 50% dextrose and 10 mg of salbutamol. She had a urine output of 240 mL during the first two hours after the diuretic administration. However, her bradycardia persisted alongside elevated potassium levels (6.58 mmol/l) and a slight serum sodium level (121 mmol/l) improvement. Therefore, emergent hemodialysis was performed, resulting in a drop of serum potassium to 4.87 mmol/l and the restoration of normal sinus rhythm without any other ECG abnormality (Fig. 2). She was then transferred to the ward for further care because her hyponatremia continued (122 mmol/l). During hospitalization, she was treated with hemodialysis and loop diuretic, restoring near normal serum sodium level (133 mmol/l), with the recovery of consciousness, and there was no further evidence of bradyarrhythmia. Electrophysiology was consulted and attributed her ECG findings to hyperkalemia, given the rapid resolution of her cardiac rhythm abnormalities with correction of the potassium and the absence of electrocardiographic findings indicating atrioventricular conduction system disease or infra-Hisian disease. Hyperkalemia and hyponatremia were attributed to irregular adherence to her hemodialysis schedule. At discharge, the patient was counseled on the importance of strict adherence to her dialysis schedule and was scheduled to follow up with the nephrologist to avoid another episode of hyperkalemia. No further episodes of sinus arrest were observed during the follow-up.
Figure 2.
Sinus rhythm at 76 beats per minute, normal atrioventricular conduction. Note the absence of other conduction disturbances, such as bundle branch block.
Discussion
The myocardium is the primary organ affected by hyperkalemia, and the increased serum potassium leads to conduction abnormalities and impaired myocardial contraction. Sinus arrest caused by hyperkalemia is usually related only to severe cases (i.e. K+ > 8.0 mmol/l) because the tissue of the sinoatrial node and bundle of His is more resistant to hyperkalemia than atrial or ventricular myocardium [5]. In our case, it is postulated sinus arrest was precipitated by moderate hyperkalemia because the correction of this electrolyte imbalance led to the rapid reappearing of sinus activity, suggesting that hyperkalemia was the most important triggering factor of the event. Hyponatremia may have contributed to the occurrence of sinus arrest because low serum sodium increases the sensitivity of cardiac tissues to the effects of hyperkalemia [6]. Conversely, while hyponatremia is linked to sinus arrest [7] and atrioventricular block [8, 9], such cases are exceptional and have been found with serum sodium levels below 105 mmol/l.
For the management of high serum potassium levels, hemodialysis is the preferred choice for those facing life-threatening hyperkalemia [10]. In this case, the patient had elevated serum potassium associated with sinus arrest and did not adequately respond to medical treatment. This led to emergent hemodialysis, resulting in the normalization of potassium levels and restoration of sinus rhythm. Other medical treatments for hyperkalemia, such as the newer potassium binders like zirconium cyclosilicate and sodium bicarbonate [10], were not used for this case.
Our case is similar to other reports documenting that a modest elevation in serum potassium levels can lead to sinus arrest. Sakemi et al. report the case of a 55-year-old man with end-stage renal disease undergoing hemodialysis who developed sinus arrest at a serum potassium level of about 7.5 mmol/l without other typical ECG changes [11]. Lee et al. describe a case of sinus arrest in a patient who developed exercise-induced hyperkalemia (5.5 mmol/l) during treatment with both verapamil and a beta-blocking agent [12]. Mehta et al. presented a case of sinus arrest with a serum potassium level of 5.5 mmol/l in an elderly woman with a history of CKD [13]. Bonvini et al. documented a case of sinus arrest related to moderate hyperkalemia (6.4 mmol/l) in a 54-year-old woman using negative chronotropic drugs as antihypertensive treatment (diltiazem and atenolol) [14]. Mahana et al. report a case of sinus arrest due to moderate hyperkalemia (7.2 mmol/l) in a 55-year-old woman with a history of end-stage renal disease on hemodialysis treated with negative chronotropic drugs (metoprolol and amlodipine) [15].
The action potential of the sinus node differs significantly from that of the contractile myocardium. Sinus node cells display spontaneous diastolic depolarization, leading to a positive ‘pacemaker potential,’ which triggers an action potential when the threshold potential is reached. Diastolic depolarization during phase 4 of the sinus node action potential constitutes the fundamental pacemaker potential and underlies sinus node automaticity. This phenomenon represents the primary distinction between the sinus node and the myocardial tissue [16]. The electrophysiological consequences of hyperkalemia result from significant changes in cells' excitability and conduction velocity. As the extracellular concentration of potassium increases, transmembrane permeability rises, leading to potassium influx into the cells. This alters the transmembrane potential gradient, reduces the magnitude of the resting potential, and decreases the velocity of phase 0 of the action potential. The influx of potassium shortens the action potential, resulting in delayed conduction between myocytes. Ultimately, these changes slow down conduction. These conduction abnormalities lead to various electrocardiographic changes observed in hyperkalemia. As serum levels rise beyond normal ranges, there is suppression of sinoatrial and atrioventricular conduction, causing sinoatrial and atrioventricular blocks, often accompanied by escape beats [17].
Although experimental studies link hyperkalemia to predictable ECG abnormalities, these changes are not reliably sensitive or specific in clinical settings. The characteristic peaked T waves, considered the earliest and most common ECG sign of hyperkalemia, are present in only 22% of hyperkalemic patients [6]. Even when ECG alterations suggest hyperkalemia, they often lack specificity. A retrospective study of 305 hospitalized patients revealed that those with moderate hyperkalemia (6.0–7.0 mmol/l) showed ECG patterns similar to normokalemic individuals. Approximately 25% of normokalemic patients exhibited at least one ECG abnormality typically associated with hyperkalemia, such as peaked T waves, widened QRS complexes, or first-degree AV block, underscoring the limited specificity of these findings. Peaked T waves were noticeably more frequent than in normokalemic patients, only in cases of severe potassium elevation (>7.0 mmol/l) [18]. Martinez-Vea et al. found that ECGs showed no characteristic changes, even when potassium levels exceeded 8 mmol/l [19]. Furthermore, ECG changes in patients do not consistently follow the usual patterns observed in experimental hyperkalemia studies; instead, hyperkalemia can produce ST elevations, rate-dependent bundle branch blocks, or T wave pseudonormalization [20, 21]. Consequently, diagnosing hyperkalemia through the ECG is a challenge, and physicians should have a high degree of suspicion for electrocardiographic abnormalities related to hyperkalemia, even if ECG findings are not typical.
In summary, hyperkalemia can lead to life-threatening arrhythmias, regardless of serum potassium levels. However, diagnosing hyperkalemia using an ECG at presentation can be challenging. Therefore, physicians should initiate treatment promptly, considering the patient's clinical context —such as renal dysfunction, use of negative chronotropic medications, interactions with other electrolyte imbalances like hyponatremia and hypocalcemia, latent sinus node dysfunction, and pre-existing myocardial ischemia— in the presence of electrocardiographic changes that could be caused by hyperkalemia.
Acknowledgements
None.
Contributor Information
Antonio Cortés-Ortíz, Department of Cardiology, Hospital Regional de Alta Especialidad de Zumpango, Estado de México, Mexico.
José Antonio Trujillo-Espinosa, Department of Internal Medicine, Hospital Regional de Alta Especialidad de Zumpango, Estado de México, Mexico.
José Antonio Hernández-Lozada, Department of Internal Medicine, Hospital Regional de Alta Especialidad de Zumpango, Estado de México, Mexico.
Abraham Edgar Gracia-Ramos, Department of Internal Medicine, Hospital Regional de Alta Especialidad de Zumpango, Estado de México, Mexico; Department of Internal Medicine, Hospital General, Centro Médico Nacional La Raza, Instituto Mexicano del Seguro Social, Mexico City, Mexico.
Authors’ Contributions
All authors listed in this manuscript made substantial contributions to data acquisition, analysis, or interpretation and were involved in critically drafting or revising this article for important intellectual content. All authors approved the final version of the manuscript.
Conflict of interest
Abraham Edgar Gracia-Ramos serves as an Executive Editor of the Oxford Medical Case Reports journal. The authors were not involved in the editorial process for the manuscript, and appropriate steps were taken to ensure that authors were blinded to the review process.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical Approval
Ethical approval was not required for this study.
Consent
The patient provided written informed consent for this publication.
Guarantor
Antonio Cortés-Ortíz is the guarantor of this article.
References
- 1. Lindner G, Burdmann EA, Clase CM. et al. Acute hyperkalemia in the emergency department: a summary from a kidney disease: improving global outcomes conference. Eur J Emerg Med 2020;27:329–37. 10.1097/MEJ.0000000000000691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kovesdy CP. Management of hyperkalaemia in chronic kidney disease. Nat Rev Nephrol 2014;10:653–62. 10.1038/nrneph.2014.168 [DOI] [PubMed] [Google Scholar]
- 3. Weiss JN, Qu Z, Shivkumar K. Electrophysiology of Hypokalemia and Hyperkalemia. Circ Arrhythm Electrophysiol 2017;10:e004667. 10.1161/CIRCEP.116.004667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Campese VM, Adenuga G. Electrophysiological and clinical consequences of hyperkalemia. Kidney Int Suppl 2016;6:16–9. 10.1016/j.kisu.2016.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dittrich KL, Walls RM. Hyperkalemia: ECG manifestations and clinical considerations. J Emerg Med 1986;4:449–55. 10.1016/0736-4679(86)90174-5 [DOI] [PubMed] [Google Scholar]
- 6. Surawicz B. Relationship between electrocardiogram and electrolytes. Am Heart J 1967;73:814–34. 10.1016/0002-8703(67)90233-5 [DOI] [PubMed] [Google Scholar]
- 7. Zou S, Zhang Q, Gao S. et al. Electrocardiogram manifestations of hyponatraemia. CVJA 2022;33:61–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kottwitz J, Akdis D, Duru F. et al. Severe hyponatremia leading to complete atrioventricular block. Am J Med 2016;129:e243–4. 10.1016/j.amjmed.2016.05.033 [DOI] [PubMed] [Google Scholar]
- 9. Karabag T, Kalayci B, Sayin MR. et al. Atrioventricular conduction defect associated with severe hyponatremia. Clujul Med 2018;91:342–5. 10.15386/cjmed-846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rafique Z, Peacock F, Armstead T. et al. Hyperkalemia management in the emergency department: an expert panel consensus. JACEP Open 2021;2:e12572. 10.1002/emp2.12572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sakemi T, Ikeda Y, Rikitake O. Tonic convulsion associated with sinus arrest due to Hyperkalemia in a chronic Hemodialysis patient. Nephron 1996;73:370–1. [DOI] [PubMed] [Google Scholar]
- 12. Lee TH, Salomon DR, Rayment CM. et al. Hypotension and sinus arrest with exercise-induced hyperkalemia and combined verapamil/propranolol therapy. Am J Med 1986;80:1203–4. 10.1016/0002-9343(86)90688-1 [DOI] [PubMed] [Google Scholar]
- 13. Mehta NJ, Chhabra VK, Khan IA. Sinus arrest or sinoventricular conduction in mild hyperkalemia. J Emerg Med 2001;20:163–4. 10.1016/S0736-4679(00)00295-X [DOI] [PubMed] [Google Scholar]
- 14. Bonvini RF, Hendiri T, Anwar A. Sinus arrest and moderate hyperkalemia. Ann Cardiol Angeiol 2006;55:161–3. 10.1016/j.ancard.2005.10.001 [DOI] [PubMed] [Google Scholar]
- 15. Mahana I, Rosenfeld BL, Hadadi CA. et al. Uncommon ECG changes as a manifestation of Hyperkalemia. Am J Med 2022;135:1330–2. 10.1016/j.amjmed.2022.07.005 [DOI] [PubMed] [Google Scholar]
- 16. Murphy C, Lazzara R. Current concepts of anatomy and electrophysiology of the sinus node. J Interv Card Electrophysiol 2016;46:9–18. 10.1007/s10840-016-0137-2 [DOI] [PubMed] [Google Scholar]
- 17. Diercks DB, Shumaik GM, Harrigan RA. et al. Electrocardiographic manifestations: electrolyte abnormalities. J Emerg Med 2004;27:153–60. 10.1016/j.jemermed.2004.04.006 [DOI] [PubMed] [Google Scholar]
- 18. Varga C, Kálmán Z, Szakáll A. et al. ECG alterations suggestive of hyperkalemia in normokalemic versus hyperkalemic patients. BMC Emerg Med 2019;19:33. 10.1186/s12873-019-0247-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Martinez-Vea A, Bardají A, Garcia C. et al. Severe hyperkalemia with minimal electrocardiographic manifestations. J Electrocardiol 1999;32:45–9. 10.1016/S0022-0736(99)90020-1 [DOI] [PubMed] [Google Scholar]
- 20. Montague BT, Ouellette JR, Buller GK. Retrospective review of the frequency of ECG changes in Hyperkalemia. Clin J Am Soc Nephrol 2008;3:324–30. 10.2215/CJN.04611007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wróbel P, Jaroszyński A. Pseudonormalisation of the ECG in a patient with life-threatening hyperkalemia. Folia Cardiologica 2021;16:338–42. [Google Scholar]