Abstract
Background
Hospital discharge against medical advice, especially among substance-abusing populations, is a frustrating problem for health care pro-viders. Because of the high prevalence of injection drug use among HIV- positive patients admitted to hospital in Vancouver, we explored the factors associated with leaving hospital against medical advice in this population.
Methods
We reviewed records for all HIV/AIDS patients admitted to St. Paul's Hospital, Vancouver, between Apr. 1, 1997, and Mar. 1, 1999. After identifying the first (“index”) admission during this period, we followed the patients' records for 1 year. Multivariate models were applied to identify the determinants of discharge against medical advice and to estimate the impact of such discharge on readmission rate, readmission frequency and length of stay in hospital.
Results
Of 981 index admissions among HIV/AIDS patients, 125 (13%) of the patients left the hospital against medical advice. Departure on the day on which welfare cheques were issued and a history of injection drug use were significant predictors of leaving against medical advice. After adjusting for sex, age, severity of illness, injection drug use and homelessness, we found that patients leaving against medical advice were readmitted more frequently than those who were formally discharged (frequency ratio 1.25, 95% confidence interval [CI] 1.11–1.42), were more likely to be readmitted with a related diagnosis within 30 days (odds ratio 5.00, 95% CI 3.04–8.24) and had significantly longer lengths of stay in the follow-up period.
Interpretation
Discharge against medical advice among HIV-positive patients was associated with frequent readmissions with the same diagnosis. Preventing such discharges is likely to benefit patients (by improving their health status) and the health care system (by reducing unnecessary readmissions).
Hospital discharge against medical advice has always been a frustrating problem for health care providers, in part because such premature discharge is often associated with multiple readmissions. This problem has been discussed in the literature since the early 1960s. Most of the early studies were conducted in US settings and focused on psychiatric patients,1,2,3,4,5,6,7,8,9,10,11,12,13,14 as well as patients admitted to other subspecialty or general medicine wards.15,16,17,18,19,20,21,22,23 Depending on the patient population and the type of treatment, the rate of discharge against medical advice has varied widely, ranging from 0.7% to 2.2% for general medical admissions and from 6% to 54% for psychiatric admissions.15,18,19,24,25,26
Although some studies had inconsistent findings on the role of sex and ethnicity in discharges against medical advice, there was general agreement that younger patients, those with substance abuse disorders, and those with prior discharges against medical advice were more likely to leave under these circumstances.6,7,8,9,15,17,18,19,20,22 In particular, among patients discharged against medical advice, the estimated prevalence of substance abuse ranged from 20% to over 50%.2,18,19,21,22,24,25
A high proportion of HIV-positive patients admitted to our institution are injection drug users, and we hypothesized that they would be more likely to leave hospital against medical advice than other HIV-positive risk groups. Therefore, we studied a cohort of HIV/AIDS patients who had been admitted to hospital to estimate the rate of hospital discharges against medical advice, to determine the factors associated with such discharge and to assess the impact of leaving hospital under these circumstances on hospital readmission rates.
Methods
This retrospective cohort study was based on all HIV-positive patients admitted to St. Paul's Hospital in Vancouver, the largest AIDS tertiary care centre in Canada, between Apr. 1, 1997, and Mar. 1, 1999, who survived to discharge. We obtained the data from discharge abstracts completed by the staff of the Medical Records Department. A discharge abstract is a patient-specific administrative record for the hospital stay, from the start of admission to discharge, transfer to another institution or death. The discharge abstract records a variety of patient characteristics, including injection drug use and medical and surgical procedures performed. The first admission of a particular patient during the study period, if the patient was discharged alive, was defined as the index admission. We followed each patient's records for 1 year after the index admission.
The study patients were classified into 2 groups according to the manner in which they were discharged from the index admission: discharge against medical advice or formal discharge. Characteristics of patients, including age, sex, housing status (homeless or not), injection drug use status and severity of underlying HIV disease, were obtained from the discharge abstract for the index admission. Patients were classified as homeless if they did not report a fixed address at admission. Because of the characteristics of the patient population at this hospital, all HIV-positive patients are routinely asked by the physician if they inject drugs. Patients in the study were classified as injection drug users or not according to their response to this question, as recorded by the physician during the index admission. From the diagnoses recorded on the discharge abstract, we identified patients with at least one diagnosis of AIDS or advanced HIV disease (International Classification of Diseases, 9th revision, codes 42.0–44.9), and we used this classification as a marker of disease severity. Data on CD4 cell counts were available for only 70% of the patients.
We examined readmission patterns for the 1-year follow-up period and estimated the rates of readmission within 30 days after discharge from the index admission, within 30 days with the same or related diagnoses as the index admission, and within 1 year. A physician [A.P.] reviewed in detail the discharge abstracts for the index admission and the subsequent admissions to compare diagnoses. Data were available on length of stay for each admission.
The day of the week on which patients were discharged was also available. In particular, we identified discharges occurring on “welfare Wednesdays” (the days on which welfare cheques were issued). At the time of the study, HIV-positive residents of British Columbia were eligible for a disability benefit (approximately $825 per month) that included “comfort money” for coffee, tobacco, and other such items ($85), support for accommodation ($350), and an allowance for meals and other expenses ($390). In addition, they could apply for a critical health benefit (Schedule C), which included an allowance for bottled water, vitamins and minerals, over-the-counter drugs and prescriptions. Because of the differences in the actual amounts received by individuals, it was difficult to determine the exact amount of benefits foregone during each patient's hospital stay, although it would have been a significant portion of their total monthly income.
We used bivariate and multivariate analyses. In the bivariate analysis, we compared categorical variables using the Mantel-Haenszel χ2 test and continuous variables using the Wilcoxon rank-sum test. Multiple logistic regression was performed for factors associated with leaving hospital against medical advice. We also investigated the effect on discharge status of interactions between variables (such as discharge on welfare Wednesday and injection drug use, discharge on welfare Wednesday and homelessness, and injection drug use and homelessness).
Several multivariate models were fitted to assess the effect of leaving against medical advice on utilization of hospital services. Multiple logistic regression was used to estimate the adjusted effect of leaving against medical advice on readmission patterns. Multiple linear regression was used to assess the determinants of length of stay, where length-of-stay variables were transformed to a logarithmic scale to satisfy the normality assumption of the model. Specifically, the variable for follow-up length of stay (y) was transformed to log (y + 1) because it included lengths of stay with the value zero. The multiple Poisson regression model was used to examine the adjusted effect of discharge against medical advice on readmission frequency during the follow-up period. Again, possible interactions between variables (such as homelessness and injection drug use, homelessness and discharge against medical advice, and injection drug use and discharge against medical advice) were investigated.
Results
Between Apr. 1, 1997, and Mar. 1, 1999, 981 HIV/AIDS patients were admitted to hospital and survived to discharge. The median age was 38 years (interquartile range 33–44), 213 (22%) were women, 57 (6%) were homeless at admission, 448 (46%) were injection drug users, and 355 (36%) had AIDS or advanced HIV.
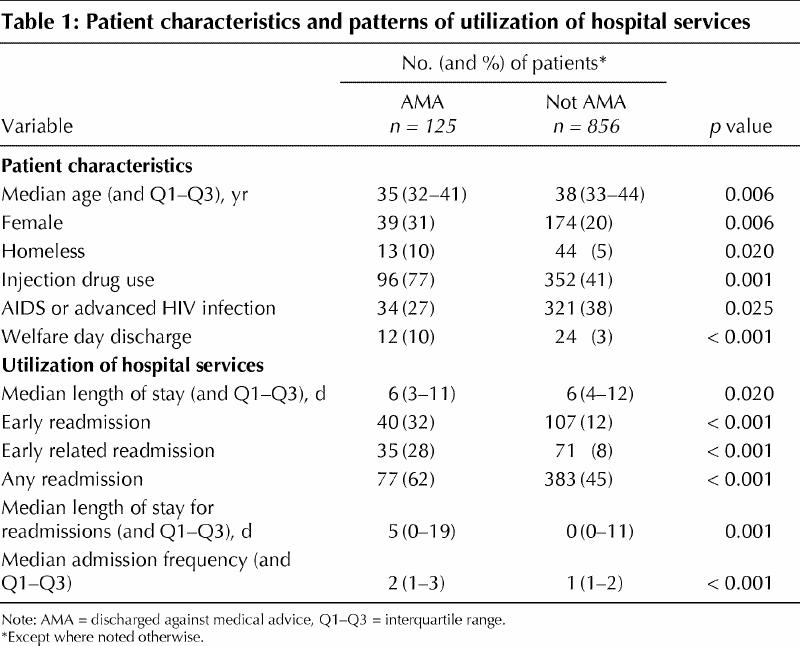
Table 1 shows the patients' characteristics and their utilization of hospital services according to whether they left hospital against medical advice. One hundred and twenty-five (13%) patients terminated the index admission by leaving against medical advice. The bivariate comparison showed that patients who left against medical advice were younger (median age 35 v. 38 years, p = 0.006), less likely to have a diagnosis of AIDS or advanced HIV (27% v. 38%, p = 0.025), and more likely to be female (31% v. 20%, p = 0.006), homeless (10% v. 5%, p = 0.020) and injection drug users (77% v. 41%, p = 0.001). The rate of discharge against medical advice for the index admission was substantially higher among injection drug users than among those who were not injection drug users (21% v. 5%, p < 0.0001). The rate of discharge against medical advice for subsequent admissions was also considerably higher among patients who left against medical advice after the index admission. More than 40% of patients who left against medical advice from the index admission and were subsequently readmitted left against medical advice again; this proportion was only 6% for those who were formally discharged from the index admission (p < 0.0001).
Table 1
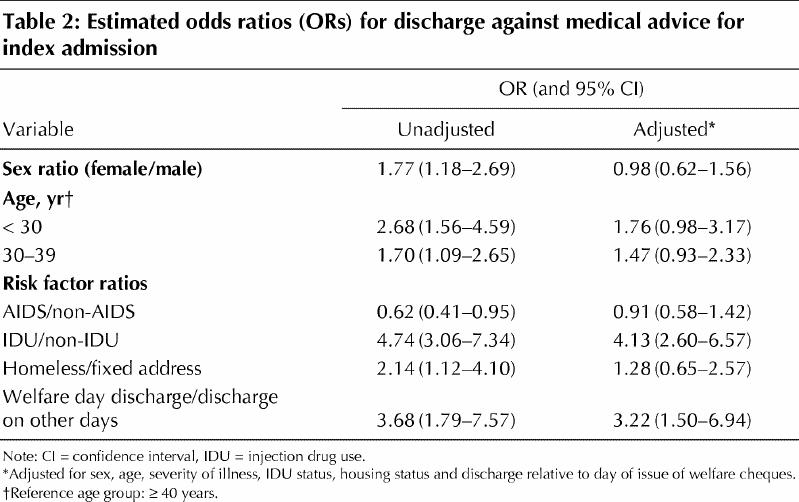
The bivariate and multivariate analyses showed that patients were more likely to leave the hospital against medical advice on days when welfare cheques were issued (adjusted odds ratio [OR] 3.22, 95% confidence interval [CI] 1.50–6.94) than on other days (Table 2). Injection drug users were more likely than those not using injection drugs to leave against medical advice (OR 4.13, 95% CI 2.60–6.57). Age, sex, severity of illness and housing status were not independent predictors of discharge against medical advice. Interactions between discharge on welfare Wednesdays, injection drug use and homelessness were not significant.
Table 2
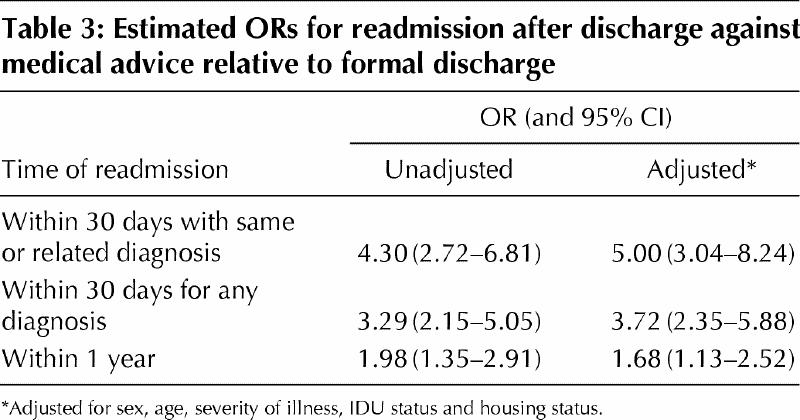
The unadjusted and adjusted ORs for hospital readmission patterns in relation to type of discharge are presented in Table 3. Leaving the hospital against medical advice was an independent predictor of readmission within 30 days, readmission with the same or related diagnoses within 30 days and readmission within 1 year. In particular, patients leaving against medical advice were 5 times more likely to be readmitted with related diagnoses within 30 days (adjusted OR 5.00, 95% CI 3.04–8.24).
Table 3
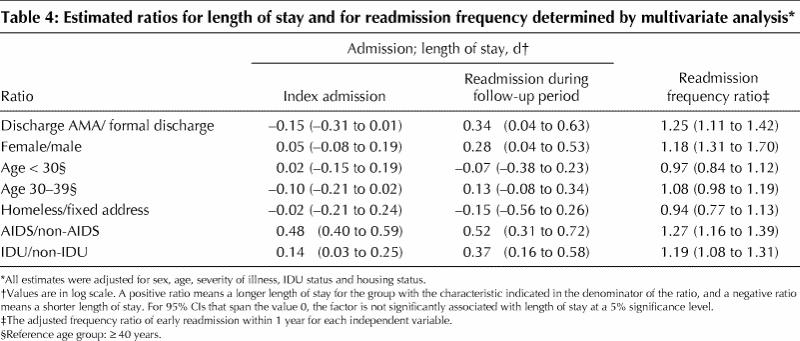
The results of multiple linear regression on the length-of-stay variables are presented in Table 4. After adjustment for sex, age, severity of illness, injection drug use status, and housing status and relative to HIV-positive patients who were formally discharged, patients who left against medical advice had a significantly longer length of stay in the follow-up period. The estimated ratio of length of stay (in log scale) in the follow-up period between the 2 groups was 0.34 (95% CI 0.04–0.63). Table 4 also presents the results of the multiple Poisson regression on frequency of readmission within 1 year. Patients leaving against medical advice were readmitted to hospital 1.25 times more frequently than patients who were discharged formally (adjusted frequency ratio 1.25, 95% CI 1.11–1.42). Interactions between variables such as homelessness and injection drug use or injection drug use and discharge against medical advice were not statistically significant in any of our multivariate analyses and hence were not included in the final models.
Table 4
Data on CD4 cell count within 6 months after admission was available for approximately 70% of the patients. The multivariate models shown in Tables 2-4 were refitted for this subgroup on the basis of CD4 counts instead of the diagnoses of AIDS or advanced HIV. The direction, magnitude and significance levels of these estimates were similar to those obtained with AIDS or advanced HIV as proxies for disease severity (data not shown).
Interpretation
Among HIV/AIDS patients who had been admitted to hospital, those who left against medical advice were more likely to be injection drug users and were more likely to leave on days when welfare cheques were issued. These patients were also readmitted more frequently. Often the readmission was for the same (or related) diagnosis as the previous admission. Length of stay in hospital was also significantly longer during subsequent admissions for patients who left against medical advice. The higher resource utilization during the follow-up period suggests that patients leaving under these circumstances may not have sufficiently recovered from their illness at the time of discharge because of incomplete treatment during the index admission.
Our finding that injection drug users were at greater risk of leaving hospital against medical advice is consistent with many earlier investigations.2,3,7,8,15,18,19,20,21,24,26,27 However, in our study, the 13% rate of discharge against medical advice was well above the rate typically reported for acute care hospitals (1.2%)16 and was similar to that for psychiatric patients (16%).9 In one study, homelessness was a factor associated with psychiatric patients leaving against medical advice,5 although this was not the case in our study. However, like other authors,6,18 we found that leaving hospital against medical advice was a predictor of subsequent discharge under these circumstances.
Chandrasena and Miller26 reported that patients leaving against medical advice or being absent without official leave were at higher risk of readmission in the short (1-week) and long (2-year) term. Their estimated readmission rates were modestly lower than ours, but the ORs for being readmitted were similar. In contrast, Tuchman and Lavell28 reported that leaving hospital against medical advice in the United States was not associated with more subsequent readmissions. They attributed this finding to the fact that the patients in their study were in lower socioeconomic groups and perhaps could not have afforded subsequent admissions, even if needed. One report that studied risk factors for early hospital readmission among patients with AIDS and pneumonia did not consider discharge against medical advice; however, patients leaving the hospital unaccompanied by family or friends were 4.8 times more likely to be readmitted within 14 days.29
In this retrospective analysis, we were unable to confirm whether individual patients were actually receiving welfare, but given our experience with this population, the likelihood is very high.30 A patient who otherwise receives a disability benefit of $825 a month would receive only $435 while in hospital. Patients want to maintain their welfare benefit level and may leave hospital against medical advice so they can pick up their welfare cheques in person and avoid losing the full disability benefit. In addition, patients may need access to cash and feel that they cannot wait until formal discharge. A redesign of the current procedure to allow full welfare payments to be redirected to people while they are in hospital might improve their health care utilization and outcomes. If the reported morbidity and mortality consequences of existing procedures are taken into account, the rationale for a careful redesign of welfare benefit policies in British Columbia becomes obvious.31
Our study has a number of limitations. First, we were unable to identify patients who were readmitted to another hospital or who died after discharge from the index admission. Second, we did not have CD4 cell counts for all patients. However, the subgroup analyses with CD4 cell counts suggested that our proxy variable (diagnosis of AIDS or advanced HIV) was an equally good marker of disease severity. Finally, no specific reasons were available for leaving against medical advice.
Given the higher resource utilization of HIV-positive patients who leave against medical advice, the development of effective strategies to encourage these patients to complete their treatment course in hospital may benefit both the patients (by improving their health status) and the health care system (by reducing unnecessary readmissions).
β See related article page 647
Footnotes
This article has been peer reviewed.
Contributors: Dr. Anis was the principal investigator for this study. Drs. Anis, Palepu, Schechter and O'Shaughnessy were responsible for the development of the hypothesis and the study design. Dr. Palepu reviewed the discharge abstracts to determine whether or not diagnoses of hospital admissions were related. Ms. Sun and Ms. Guh developed the statistical methodology and data linkage before statistical analysis of the data. The final manuscript was prepared by Dr. Anis, Ms. Sun, Ms. Guh and Dr. Palepu.
Acknowledgements: We gratefully acknowledge the assistance of Dianne Calbick, Dr. Alex Chan, Diane Skippen and Barbara Vinduska in research for and preparation of this manuscript.
Dr. Schechter is the recipient of a Canada Research Chair award and Dr. Palepu has a New Investigator Award from the Canadian Institutes of Health Research.
Competing interests: None declared.
Correspondence to: Dr. Aslam H. Anis, British Columbia Centre for Excellence for HIV/AIDS, St. Paul's Hospital, 570-1081 Burrard St., Vancouver BC V6Z 1Y6; fax 604 806-8778; anis@hivnet.ubc.ca
References
- 1.Daniels RS, Margolis OM, Carson RC. Hospital discharges against medical advice I: origin and prevention. Arch Gen Psychiatry 1963;8:120-30. [DOI] [PubMed]
- 2.Schlauch RW, Reigh P, Kelly MJ. Leaving the hospital against medical advice. N Engl J Med 1979;300:22-4. [DOI] [PubMed]
- 3.Pages KP, Russo JE, Wingerson DK, Ries RK, Roy-Byrne PP, Cowley DS. Predictors and outcome of discharge against medical advice from the psychiatric units of a general hospital. Psychiatr Serv 1998;49(9):1187-92. [DOI] [PubMed]
- 4.Smith HH. Discharge against medical advice (AMA) from an acute care private psychiatric hospital. J Clin Psychol 1982;38:550-4. [DOI] [PubMed]
- 5.Dalrymple AJ, Fata M. Cross–validating factors associated with discharges against medical advice. Can J Psychiatry 1993;38(4):285-9. [DOI] [PubMed]
- 6.Louks J, Mason J, Backus F. AMA discharges: prediction and treatment outcome. Hosp Community Psychiatry 1989;40:299-301. [DOI] [PubMed]
- 7.Crowe DB, Rosse RB, Sheridan MJ, Deutsch SI. Substance use diagnoses and discharge patterns among psychiatric inpatients. Hosp Community Psychiatry 1991; 42:403-5. [DOI] [PubMed]
- 8.Planansky K, Johnston R. A survey of patients leaving a mental hospital against medical advice. Hosp Community Psychiatry 1976;27:865-8. [DOI] [PubMed]
- 9.Akhtar S, Halfrinch J, Mestayer R. AMA discharges from a psychiatric inpatient unit. Int J Soc Psychiatry 1981;27:143-50. [DOI] [PubMed]
- 10.Cook CA, Booth BM, Blow FC, McAleenan KA, Bunn JY. Risk factors for AMA discharge from VA inpatient alcoholism treatment programs. J Subst Abuse Treat 1994;11:239-45. [DOI] [PubMed]
- 11.Moy E, Bartman D. Race and hospital discharge against medical advice. J Natl Med Assoc 1996;88:658-60. [PMC free article] [PubMed]
- 12.Endicott P, Watson B. Interventions to improve the AMA-discharge rate for opiate-addicted patients. J Psychosoc Nurs Ment Health Serv 1994;32:36-40. [DOI] [PubMed]
- 13.Letterie G, Markenson G, Markenson M. Discharge against medical advice in an obstetric unit. J Reprod Med 1993;38:370-4. [PubMed]
- 14.Dubow D, Propp D, Narasimhan K. Emergency department discharge against medical advice. J Emerg Med 1992;10:513-6. [DOI] [PubMed]
- 15.Weingart SN, Davis RB, Phillips RS. Patients discharged against medical advice from a general medicine service. J Gen Intern Med 1998;13:568-71. [DOI] [PMC free article] [PubMed]
- 16.Smith DB, Telles JL. Discharges against medical advice at regional acute care hospitals. Am J Public Health 1991;81:212-5. [DOI] [PMC free article] [PubMed]
- 17.Baile WF, Brinker JA, Wachspress JD, Engel BT. Signouts against medical advice from a coronary care unit. J Behav Med 1979;2:85-92. [DOI] [PubMed]
- 18.Jeremiah J, O'Sullivan P, Stein MD. Who leaves against medical advice? J Gen Intern Med 1995;10:403-5. [DOI] [PubMed]
- 19.Jankowski DB, Drum DE. Diagnostic correlates of discharge against medical advice. Arch Gen Psychiatry 1977;34:153-5. [DOI] [PubMed]
- 20.Saitz R, Ghali WA, Moskowitz MA. Characteristics of patients with pneumonia who are discharged from hospital against medical advice. Am J Med 1999; 107: 507-9. [DOI] [PubMed]
- 21.Jones AA, Himmelstein DU. Leaving a county hospital against medical advice [letter]. JAMA 1979;242:2758. [PubMed]
- 22.Ochitill HN, Havassy B, Byrd RC, Peters R. Leaving a cardiology service against medical advice. J Chronic Dis 1985;38:79-84. [DOI] [PubMed]
- 23.Cillis K, Russell V, Busby K. Factors associated with unplanned discharge from psychiatric day treatment programs. Gen Hosp Psychiatry 1997;19:355-61. [DOI] [PubMed]
- 24.Jeffer EK. Against medical advice: Part I, a review of the literature. Mil Med 1993; 158:69-73. [PubMed]
- 25.Chandrasena R. Premature discharges: a comparative study. Can J Psychiatry 1987; 32:259-63. [DOI] [PubMed]
- 26.Chandrasena R, Miller WC. Discharge AMA and AWOL: a new “revolving door syndrome.” Psychiatr J Univ Ottawa 1998;13:155-7. [PubMed]
- 27.Peres de los Cobos J, Trujols J, Ribalta E, Casas M. Cocaine use immediately prior to entry in an inpatient heroin detoxification unit as a predictor of discharges against medical advice. Am J Drug Alcohol Abuse 1997;23:267-79. [DOI] [PubMed]
- 28.Tuchman J, Lavell M. Psychiatric patients discharged with or against medical advice. J Clin Psychiatry 1962;18:177-80. [DOI] [PubMed]
- 29.Grant RW, Charlebois ED, Wachter RM. Risk factors for early readmission in patients with AIDS and pneumonia. J Gen Intern Med 1999;14:531-6. [DOI] [PMC free article] [PubMed]
- 30.Tyndall MW, Craib KJP, Currie S, Li K, O'Shaughnessy MV, Schechter MT. Impact of HIV infection on mortality in a cohort of injection drug users. J Acquir Immune Defic Syndr 2001;28:351-7. [DOI] [PubMed]
- 31.Verheul G, Singer SM, Christenson JM. Mortality and morbidity associated with the distribution of monthly welfare payments. Acad Emerg Med 1997;4(2):118-23. [DOI] [PubMed]


