Abstract
Background
Head injury (HI) causes a wide range of psychological symptoms, such as cognitive deficits and mood changes, leading to significant disability. Although a few studies have explored the prevalence of HI in India. However, none of the meta-analytical studies reported the estimation of the prevalence of HI in India based on cross-sectional community surveys.
Summary
A systematic review search was conducted on journal hosting sites, namely EBSCOhost, Google Scholar, Ovid, PubMed, and Web of Science, complying with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Cross-sectional Indian studies reporting the prevalence of HI in India were included in the present study. The risk of bias was assessed using the Risk of Bias Tool for Prevalence Studies. The meta-analysis was conducted using ‘meta’ and ‘dmetar’ packages through R software (4.4.0). A total of 17 studies surveyed 85,720 people, of whom 921 suffered from HI. The results showed an HI prevalence of 25.7 per thousand people in India. Subgroup analysis revealed a higher prevalence of HI among females (91.1 per 1,000) in comparison to males (85.1 per 1,000). Additionally, subgroup analysis of domicile revealed a higher HI prevalence among those from urban areas (29.5 per 1,000) than among those from rural areas (22.4 per 1,000).
Key Message
This study highlights the substantial burden of HI in India and the associated disparities in gender and domicile. The findings will be helpful to health professionals and policymakers in making informed decisions regarding the preventive aspects of HI in India.
Keywords: Head injury, prevalence, India, systematic review, meta-analysis
Introduction
Head injury (HI) is a mechanical insult to the scalp, skull, or brain that may result from contact with a physical force or from sudden acceleration or deceleration movements. 1 HI may be classified into three types, namely mild, moderate, and severe, according to predetermined scores from the Glasgow Coma Scale (GCS). It may lead to potential impairments in a variety of symptoms, such as physical, emotional, and cognitive sequelae. 2 Individuals with HI may develop neurodegenerative diseases, leading to permanent disability in later life.3–5 Research shows a high global incidence of HI in regions like Southeast Asia and the Western Pacific. 6 HI is found to be the most prevalent in low- and middle-income countries (LMIC) in comparison to high-income countries. 7 Despite this, a marked scarcity of high-quality community-based studies exists in LMIC due to issues such as underreporting of cases, absence of clear case definitions and inadequate reporting mechanisms.8, 9
In the recent decade, India has experienced rapid urbanisation and motorisation, leading to a rise in HI cases from road traffic accidents (RTA).10, 11 Additionally, this situation is further exacerbated by factors such as poor compliance with road safety regulations (e.g., helmet use and adherence to traffic signals). 12 Furthermore, a delay in the first line of treatment and rehabilitative efforts contributes to poorer outcomes for HI survivors. A global burden of disease study 13 found that over a quarter of the world’s trauma deaths occur in India, of which 80% were caused by RTA. Therefore, consideration should be given to this large percentage of people.
A review of the literature revealed only a few studies focusing on India in their investigation of the prevalence of HI. For example, Damara 14 conducted a meta-analysis on mortality due to HI in LMICs, including only two Indian studies. Similarly, Khan 15 studied the prevalence of HI in older adults in LMICs, but the focus was limited to Tamil-speaking populations. None of the above-mentioned studies employed community-based surveys to study the prevalence of HI in India. For instance, a study by Damara et al. 14 was on hospital-based surveys only. Additionally, there is a dearth of meta-analytical studies conducted to estimate the prevalence of HI in India, especially using community-based cross-sectional surveys. Therefore, the aim of this study was to perform a systematic literature review and perform a meta-analysis to estimate the pooled prevalence of HI in India based on community-based cross-sectional surveys, and further to examine the different socio-demographic characteristics associated with the occurrence of HI.
Methods
This study adhered to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. 16
Information Sources and Search Strategy
A literature search was conducted in the Ebscohost, Google Scholar, Ovid, PubMed, and Web of Science databases, published up to February 2024. Studies in the English language were eligible for screening. The search strategy included the following keywords:
‘Epidemiology’ OR ‘Prevalence’ OR ‘Incidence’ OR ‘Risk’ OR ‘Burden’ OR ‘Case fatality’ OR ‘Mortality’, AND ‘Concussion’ OR ‘Brain injur*’ OR ‘Head injur*’ ‘Traumatic brain injur*’ OR ‘Craniocerebral injur*’ OR ‘Contusion’ OR ‘Laceration’ OR ‘Skull fracture’ OR ‘Axonal injur*’ AND ‘India’.
Eligibility Criteria
To be eligible for inclusion, studies must include (a) patients with injury to the head (b) studies carried out in India (c) studies reporting HI due to RTA, workplace injury and fall, (d) community-based cross-sectional survey conducted in the general population and (e) studies providing numerical data on the total sample surveyed and the identified cases of HI. Articles were excluded if they reported HI due to non-traumatic causes, such as poisoning and stroke. Articles reporting combined injuries to the mandible or spine in addition to the head were excluded. Finally, studies were excluded if they reported HI in a particular population or due to an event, such as prisoners, victims of abuse, and disaster victims.
Data Selection and Extraction Process
The titles and abstracts of the articles were screened independently by two authors (SA and JR) according to the eligibility criteria. Duplicate articles were identified manually, and full-text screening was followed by the exclusion of the final article. The name of the author(s), year, location, study design, study period, measurement tool, domicile (urban/rural), injury site, total sample size, and number of HI cases were extracted from the article and entered into an Excel sheet. Furthermore, the proportion of individuals with HI relative to the total surveyed population was extracted for the meta-analysis.
Risk of Bias
The Risk of Bias Tool for Prevalence Studies by Hoy and colleagues was used to assess the risk of bias. 17 This tool consists of 10 items for evaluating the external and internal validity of the included studies. The interpretation of the tool’s scores followed Macaulay’s recommendations, with scores below five categorised as high risk of bias, scores from 6 to 7 as moderate risk of bias, and scores from 8 to 10 as low risk of bias. 18
Data Synthesis
The meta-analysis was performed using R software (4.4.0) employing ‘dmetar’, 19 ‘meta’, 20 and ‘xlsx’ 21 packages. The random-effects model was chosen for conducting the current meta-analysis due to heterogeneity across the reported findings on the prevalence of HI in India. Furthermore, the ‘metaprop()’ function was used to estimate the prevalence of HI. Furthermore, a heterogeneity analysis was performed for each demographic comparison. Forest plots of the included studies were generated using the ‘forest’ function. The visual representation for publication bias was curated using Egger’s test through the ‘regtest()’ function. 22
Results
Study Selection
A total of 1,758 articles were identified from databases. Ebscohost, Google Scholar, Ovid, PubMed, and Web of Science (see Figure 1 for the PRISMA flow diagram). A total of 233 duplicate records were screened. Further, articles were screened based on the title and abstract search. Further, a search was refined on the basis of full-text search based on pre-set inclusion and exclusion criteria. Ninety-one papers were excluded, of which 40 articles did not provide data on HI, 21 articles focused on veterans of war belonging to the United States and United Kingdom, 12 studies were review studies or systematic reviews, 12 studies belonged to other South Asian countries, and 6 studies were not community-based surveys.
Figure 1. PRISMA Flowchart Demonstrating the Study Selection Process.

Risk of Bias Assessment
Table 1 depicts the interpretation of the risk of bias of each included study. The results indicated that 35% of the included studies were scored as low risk of bias, 65% of the included studies were scored as moderate risk of bias, and none of the included studies were scored as high risk of bias.
Table 1. Source Studies in Meta-analysis of TBI in India.
| Author Name | Year | Location | Study Design | Study Period | Case Ascertainment | Site | Total | Cases | Risk of Bias |
| Babu et al. | 2022 | Bangalore, Karnataka | Cross-sectional study | * | Custom-made questionnaire | Head and Neck | 675 | 24 | Low risk |
| Banerjee et al. | 2016 | Hooghly district, West Bengal | Cross-sectional study | 11.2015–02.2016 | Interview, Parent Supervision Attributes Profile Questionnaire (PSAPQ) | Head | 163 | 13 | Moderate risk |
| Basak et al. | 2020 | Siliguri, West Bengal | Cross-sectional study | 05.2016–04.2017 | Operational Definition, Custom-made questionnaire | Head and Neck | 780 | 70 | Moderate risk |
| Dandona et al. | 2010 | Godavari district, Andhra Pradesh | Cross-sectional study | 10.2007–05.2008 | Interview, ICD-10 | Head | 3686 | 12 | Moderate risk |
| Dandona et al. | 2006 | Hyderabad, Telangana | Cross-sectional study | 04.2004–11.2004 | Interview, Custom-made questionnaire | Head and Neck | 34,696 | 128 | Moderate risk |
| Das et al. | 2020 | Purba Bardhaman district, West Bengal | Cross-sectional study | 07.2018–06.2019 | Operational Definition, Interview | Head | 555 | 2 | Low risk |
| Gosalia et al. | 2019 | Rajkot, Gujarat | Cross-sectional study | 01.2014–12.2014 | Operational Definition, Interview, Custom-made questionnaire | Head | 2367 | 39 | Low risk |
| Inbaraj et al. | 2017 | Vellore, Tamil Nadu | Cross-sectional study | 03.2013–08.2013 | Interview, Custom-made questionnaire | Head | 1600 | 16 | Low risk |
| Indira et al. | 2016 | Chidambaram, Tamil Nadu | Cross-sectional study | 11.2015–08.2016 | Operational Definition, Interview, Custom-made questionnaire | Head | 200 | 0 | Moderate risk |
| Khan et al. | 2015 | α | Cross-sectional study | 2003–2007 | Operational Definition, Interview | Head | 2003 | 150 | Moderate risk |
| Kumar et al. | 2014 | Delhi | Cross-sectional study | 03.2013–04.2013 | Operational Definition, Custom-made questionnaire | Head | 192 | 2 | Moderate risk |
| Lahare et al. | 2023 | Chhattisgarh | Cross-sectional study | 01.2022–06.2022 | Interview, Custom-made questionnaire | Head | 312 | 32 | Moderate risk |
| Pathak et al. | 2020 | Ujjain, Madhya Pradesh | Cross-sectional study | * | Operational Definition, Interview, Training Educating and Advancing Collaboration in Health on Violence and Injury Prevention (TEACH-VIP 2) | Head | 6308 | 300 | Low risk |
| Rajak et al. | 2022 | Burnpur, West Bengal | Cross-sectional study | 11.2019–03.2020 | Operational Definition, Custom-made questionnaire | Head | 505 | 37 | Moderate risk |
| Tripathy et al. | 2015 | Chandigarh | Cross-sectional study | 03.2011–10.2012 | Interview, Hindi Mini Mental Status Examination (HMSE), Physical examination | Head and Neck | 300 | 9 | Low risk |
| Verma & Tewari | 2004 | Delhi | Cross-sectional study | * | Interview, Operational Definition | Head | 30,554 | 76 | Moderate risk |
| Zaidi et al. | 2013 | Aligarh | Cross-sectional study | 08.2006–07.2007 | Custom-made questionnaire | Head | 824 | 11 | Moderate Risk |
Notes: All included studies are mentioned in alphabetical order.
* denotes study period not mentioned; α denotes location not mentioned.
Prevalence of HI in India
The present meta-analysis included 17 studies from India, encompassing a total surveyed population of 85,720, of which 921 sustained HI.15, 23–38 The estimated prevalence of HI in India was found as 25.7 per 1,000 population (95% CI: 12.5 to 43.2 per 1,000 population). The heterogeneity analysis (Q = 1391.93, df = 16, p < .001) and I 2 value (98.9%) suggest the presence of significant heterogeneity across the studies, reflecting varying patterns of HI prevalence across India (see Figure 2 for more details).
Figure 2. Forest Plot Representing the Studies Included in the Prevalence of HI in India.

Prevalence of HI as per Socio-demographic Characteristics
Table 2 presents the prevalence of HI in India according to sociodemographic characteristics. A comparison of 12 urban and 6 rural-based studies (Figure 3) revealed that those residing in urban areas suffered more from HI (29.5 per 1,000 population, 95% CI: 12 to 54.1 per 1,000 population) than their rural counterparts (22.4 per 1,000 population, 95% CI: 5 to 50.7 per 1,000 population). Subgroup analysis indicated no significant difference between rural and urban populations (Q = 0.18, df = 1, p = .67).
Table 2. Prevalence of TBI as per Domicile, Age and Sex.
| No of Studies | Prevalence | 95% CI | Tau 2 | Q | I 2 | Subgroup Differences | |
| Domicile | |||||||
| Urban | 12 | 0.0295 | 0.0120, 0.0541 | 0.0112 | 734.05 | 98.5% | Q = 0.18, df = 1, p = .67 |
| Rural | 6 | 0.0224 | 0.0050, 0.0507 | 0.0083 | 129.15 | 96.1% | |
| Sex | |||||||
| Male | 4 | 0.0851 | 0.0032, 0.2525 | 0.0535 | 199.14 | 98.5% | Q = 0.01, df = 1, p = .94 |
| Female | 4 | 0.911 | 0.0074, 0.2451 | 0.0436 | 104.94 | 97.1% |
Figure 3. Forest Plot Representing the Included Studies as per Domicile.

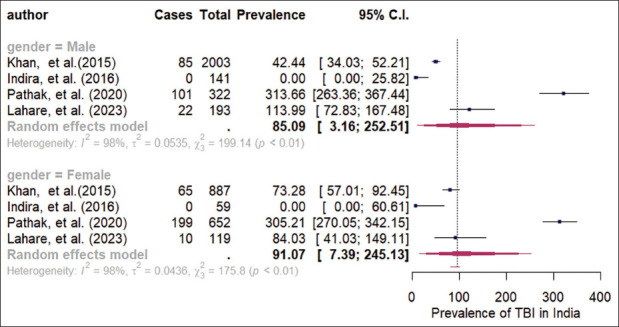
Furthermore, upon comparing the prevalence of HI between males and females (Figure 4), the prevalence among females (91.1 per 1,000 population, 95% CI: 7.4 to 245.1 per 1,000 population) was found to be slightly higher than that among males (85.1 per 1,000 population, 95% CI: 3.2 to 252.5 per 1,000 population). Subgroup analysis showed no significant difference between the genders (Q = 0.01, df = 1, p = .94).
Figure 4. Forest Plot Representing the Included Studies as Per Gender.
Publication Bias
The funnel plot is a visual representation of the potential existence of publication biases related to the inclusion of studies for the current prevalence estimation. Studies with small sample sizes and non-significant results have very little chance of being published, so it is also uncommon for those studies to be excluded from the current meta-analysis. The asymmetry in the funnel plot also suggests the presence of possible publication bias in the study (Figure 5). The Egger’s regression test was used to assess the symmetry in the funnel plot, using the regtest() function of ‘dmetar’ package. 22 The regression model’s intercept, β0 = 7.59 (95% CI: 2.5–12.67), was found to be statistically significant (t = 2.93, p = .01). This result implies that there is publication bias present in this study and the standard errors of the studies that are part of the funnel plot are asymmetric.
Figure 5. Funnel Plot Representing Publication Bias Among the Included Studies.

Discussion
The present systematic review and meta-analysis is the first comprehensive research record estimated pooled prevalence of HI in India. The estimated prevalence of HI in India is about 25.7 per 1,000 persons, and women sustained HI more than men. The estimated prevalence of HI in this study is consistent with the prevalence rates reported for other LMICs. For instance, the prevalence of HI was found to be 49 per thousand population in Puerto Rico, 15 whereas in Ghana, it was reported as 33 per thousand population 39 followed by the Republic of China with 4.4 per thousand population. 40 In contrast, the HI prevalence in the United States of America ranges between 120 and 182 per thousand persons.41–43 Similarly, a large community-based survey conducted in Ethiopia reported an HI prevalence of 397 per thousand population. 44
The lower estimated prevalence of HI in India compared to other developed western countries can be attributed to the fact that Indian states did not have a record of a comprehensive health care system for various types of head injuries, including the milder forms of HI caused by RTAs, violence, falls and natural disasters. 6 Although HI in India is mainly attributed to factors such as urbanisation, densely packed infrastructure, RTAs, and interpersonal violence etc. 9 Surprisingly, HI in female participants were more than in their male counterparts, which is contradictory to a study conducted in India, which reported that men sustained HI more than women. 13 There are manifold reasons that may be attributed to these contradictory findings. For instance, while performing sensitivity analysis in the present study, it was noted that there are two influential studies comprised for overall prevalence estimation of HI and gender-based subgroup comparisons,15, 35 and both of these influential studies focused mainly on older (over 60 years) and younger (under 18 years) participants. In these age groups, HI is often caused by falls rather than by RTA, therefore, women may suffer more from HI than men. Further, women who participate in sports and activities are at greater risk of being injured by HI than men. 45 Furthermore, large proportions of survivors of domestic violence and intimate partner violence are women who may sustain head injuries more than men. 46
A comparison of rural and urban populations showed that urban residents sustained HI more than rural residents. This finding was consistent with the findings of previous research in India.12, 47 The urban residents may be at a higher risk of HI than their rural counterparts because of denser infrastructure, leading to a higher number of RTAs. 47 Moreover, urban HI survivors have easy access to health care services compared to their rural counterparts, which increases their chances of being screened and identified as having a case of HI than the rural ones. 12 The present finding is contradictory to the findings of a meta-analysis that found more HI was experienced by people in rural areas than by those in urban areas. 48 Although most of the studies included in this meta-analysis were carried out in developed countries, 48 where rural areas have a higher incidence of road-related brain injuries than rural India; therefore, these contradictory findings may occur in the present study.
Significant heterogeneity was observed in the included studies for this prevalence estimate as well as possible publication bias was present in this study. The heterogeneity across findings of included studies could be attributed to the use of different psychometric tools and methods for diagnosing cases of HI in the community by the different researchers.
This study is pioneering in estimating the prevalence of HI in India based on community-based cross-sectional surveys, offering both theoretical and practical contributions. For instance, findings of the current study will help policymakers to make informed decisions regarding implementing rehabilitation services. As even milder forms of HI can lead to various cognitive and affective consequences, which may persist for several months to years.49, 50 Therefore, there is a critical need for comprehensive treatment and care services for TBI patients in India. However, such services remain fragmented and inadequate, particularly in the management of neuropsychological symptoms associated with HI. 12 The present study also highlighted one of the significant challenges related to the lack of well-documented health care records for non-RTA causes of TBI. This gap in documentation hampers accurate estimation of the true prevalence of head injuries across the population; therefore, findings may not fully capture the actual burden of HI in India.
Although this meta-analytical study is the first to attempt to estimate the prevalence of HI in India. However, a few limitations must be noted while interpreting the present findings, first, since the included studies were community-based, the primary method of data collection in majority of the studies were custom-made questionnaires and interviews, only a few studies used standardised measurement tools for assessing HI, such as the GCS or neuroimaging scans, therefore, this was also a major limitation of the study. Furthermore, few studies have been conducted in geographically limited areas, such as small villages or particular districts. Therefore, findings have limited generalisability to the broader population of HI patients.
Conclusion
India faces a significant public health challenge with HI, similar to the rest of the world. This study revealed that females and urban residents were at a higher risk of HI than males and rural residents in India. This study highlights the need to strengthen road safety legislation, improve trauma health and rehabilitation services for patients with HI in India.
Statement of Ethics
There were no human participants in this study; therefore, ethical approval was not required.
Abbreviations
HI: Head injury
LMIC: Low- and middle-income country
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines
RTA: Road traffic accidents
Authors’ Contributions
Saishree was responsible for the original draft preparation, review and editing, methodology development, data curation, and conceptualization of the study. Jay Kumar Ranjan contributed to formal analysis, investigation, methodology, supervision, and manuscript review and editing. H.S. Asthana provided support in supervision, methodology, and manuscript review and editing. Nityanand Pandey contributed to supervision, methodology, and critical review and editing of the manuscript. All authors have read and approved the final manuscript.
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This research was supported by the University Grants Commission (UGC) through the Junior Research Fellowship (JRF) awarded to the first author. The authors thank for their assistance and support.
ORCID iD: Jay Kumar Ranjan  https://orcid.org/0000-0002-5948-9360
https://orcid.org/0000-0002-5948-9360
Informed Consent
Informed consent was not applicable.
References
- 1.VandenBos GR. APA Dictionary of Psychology . American Psychological Association, 2007. [Google Scholar]
- 2.Jain S and Iverson LM.. Glasgow Coma Scale. StatPearls , https://www.ncbi.nlm.nih.gov/books/NBK513298/ (2023, accessed 4 April 2025). [PubMed]
- 3.Balabandian M, Noori M, Lak B, et al. Traumatic brain injury and risk of Parkinson’s disease: A meta-analysis. Acta Neurol Belg 2023; 123(4): 1225–1239. DOI: 10.1007/S13760-023-02209-X [DOI] [PubMed] [Google Scholar]
- 4.Collaborators G 2019 D. The burden of dementia due to Down syndrome, Parkinson’s disease, stroke, and traumatic brain injury: A systematic analysis for the Global Burden of Disease Study 2019. Neuroepidemiology 2021; 55(4): 286. DOI: 10.1159/000515393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Russell ER, Lyall DM and Stewart W.. HEalth And Dementia outcomes following Traumatic Brain Injury (HEAD-TBI): Protocol for a retrospective cohort study. BMJ Open 2023; 13(7): e073726. DOI: 10.1136/BMJOPEN-2023-073726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan B, Anderson DB, Chen L, et al. Global, regional and national burden of traumatic brain injury and spinal cord injury, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. BMJ Open 2023; 13(10): e075049. DOI: 10.1136/bmjopen-2023-075049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allen BC, Cummer E and Sarma AK.. Traumatic brain injury in select low- and middle-income countries: A narrative review of the literature. J Neurotrauma 2023; 40(7–8): 602–619. DOI: 10.1089/neu.2022.0068 [DOI] [PubMed] [Google Scholar]
- 8.Kamalakannan S, Gudlavalleti Aashrai SV, Murthy Gudlavalleti V, et al. Challenges in understanding the epidemiology of acquired brain injury in India. Ann Indian Acad Neurol 2015; 18(1): 66. DOI: 10.4103/0972-2327.151047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dasic D, Morgan L, Panezai A, et al. A scoping review on the challenges, improvement programs, and relevant output metrics for neurotrauma services in major trauma centers. Surg Neurol Int 2022; 13: 171. DOI: 10.25259/SNI_203_2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kar M, Sahu C, Singh P, et al. Prevalence of traumatic brain injury and associated infections in a trauma center in Northern India. J Glob Infect Dis 2023; 15(4): 137–143. DOI: 10.4103/jgid.jgid_66_23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maas AIR, Menon DK, Adelson PD, et al. Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. Lancet Neurol 2017; 16(12): 987–1048. DOI: 10.1016/S1474-4422(17)30371-X [DOI] [PubMed] [Google Scholar]
- 12.Jain C, Devi BI, Bhat DI, et al. Current status of traumatic brain injury in India. Indian J Neurotrauma . DOI: 10.1055/s-0044-1789260 [Google Scholar]
- 13.James SL, Theadom A, Ellenbogen RG, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18(1): 56–87. DOI: 10.1016/S1474-4422(18)30415-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Damara FA, Muchamad GR, Anton A, et al. Epidemiological pattern of traumatic brain injury in the COVID-19 pandemic: A systematic review and meta-analysis. World Neurosurg 2022; 161: e698–e709. DOI: 10.1016/j.wneu.2022.02.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khan A, Prince M, Brayne C, et al. Lifetime prevalence and factors associated with head injury among older people in low and middle income countries: A 10/66 study. PLoS One 2015; 10(7): e0132229. DOI: 10.1371/journal.pone.0132229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst Rev 2021; 10(1): 89. DOI: 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 2012; 65(9): 934–939. DOI: 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 18.Macaulay S, Dunger DB and Norris SA.. Gestational diabetes mellitus in Africa: A systematic review. PLoS One 2014; 9(6): e97871. DOI: 10.1371/journal.pone.0097871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harrer M, Cuijpers P, Furukawa TA, et al. Doing meta-analysis with R: A hands-on Guide . 2021. DOI: 10.1201/9781003107347 [Google Scholar]
- 20.Balduzzi S, Rücker G and Schwarzer G.. How to perform a meta-analysis with R: A practical tutorial. Evid Based Ment Health 2019; 22(4): 153–160. DOI: 10.1136/ebmental-2019-300117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dragulescu A and Arendt C.. xlsx: Read, Write, Format Excel 2007 and Excel 97/2000/XP/2003 Files . Published online 2020. [Google Scholar]
- 22.Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315(7109): 629–634. DOI: 10.1136/BMJ.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verma P and Tewari K.. Epidemiology of road traffic injuries in Delhi: Result of a survey. Reg Health Forum WHO South-East Asia Reg 2003; 8. [Google Scholar]
- 24.Babu YRM, Uthkarsh PS and A G.. Road traffic injuries among schoolchildren from rural and urban districts of South India. Indian J Med Spec 2022; 13(1): 29–32. DOI: 10.4103/injms.injms_71_21 [Google Scholar]
- 25.Banerjee S, Paul B, Bandyopadhyay K, et al. Domestic unintentional injury of 1 to 5-year-old children in a rural area of West Bengal, India: A community-based study. Tanzan J Health Res 2016; 18(3). DOI: 10.4314/thrb.v18i3.6 [Google Scholar]
- 26.Basak M, Biswas R, Bhattacherjee S, et al. Prevalence and pattern of childhood injuries in Siliguri City, West Bengal, India. Indian J Public Health 2020; 64(1): 39. DOI: 10.4103/ijph.IJPH_401_18 [DOI] [PubMed] [Google Scholar]
- 27.Dandona R, Kumar GA, Raj TS, et al. Patterns of road traffic injuries in a vulnerable population in Hyderabad, India. Inj Prev 2006; 12(3): 183–188. DOI: 10.1136/ip.2005.010728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dandona R, Kumar GA, Ivers R, et al. Characteristics of non-fatal fall injuries in rural India. Inj Prev 2010; 16(3): 166–171. DOI: 10.1136/ip.2009.023663 [DOI] [PubMed] [Google Scholar]
- 29.Das S, Roy RN, Das DK, et al. Community based assessment of unintentional injuries in a community development block of Purba Bardhaman District, West Bengal. Ethiop J Health Sci 2021; 31(2). DOI: 10.4314/ejhs.v31i2.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gosalia VV, Thakrar DV and Chudasama RK.. Epidemiological profile of injuries in urban and urban slum areas of Rajkot city, India: A community based study. Int J Community Med Public Health 2019; 6(4): 1652. DOI: 10.18203/2394-6040.ijcmph20191400 [Google Scholar]
- 31.Inbaraj LR, Rose A, George K, et al. Incidence and impact of unintentional childhood injuries: A community based study in rural South India. Indian J Pediatr 2017; 84(3): 206–210. DOI: 10.1007/s12098-016-2260-6 [DOI] [PubMed] [Google Scholar]
- 32.Inbaraj NC. Prevalence and pattern of sports injuries among the university students of physical education, Southern India. J Med Sci Clin Res 2016; 4(10): 13434–13440. DOI: 10.18535/jmscr/v4i10.107 [Google Scholar]
- 33.Kumar V, Mangal A, Yadav G, et al. Prevalence and pattern of sport injuries among college students in Delhi, India. Saudi J Sports Med 2014; 14(2): 109. DOI: 10.4103/1319-6308.142360 [Google Scholar]
- 34.Lahare VK, Verma N, Chandrakar A, et al. A community-based cross-sectional study on the epidemiology of injuries in Raipur City, Chhattisgarh. Cureus . Published online; July 14, 2023. DOI: 10.7759/cureus.41868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pathak A, Agarwal N, Mehra L, et al. Incidence, risk and protective factors for unintentional, nonfatal, fall-related injuries at home: A community-based household survey from Ujjain, India. Pediatr Health Med Ther 2020; 11: 65–72. DOI: 10.2147/PHMT.S242173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rajak R, Chattopadhyay A and Maurya P.. Accidents and injuries in workers of iron and steel industry in West Bengal, India: Prevalence and associated risk factors. Int J Occup Saf Ergon 2022; 28(4): 2533–2540. DOI: 10.1080/10803548.2021.2012021. [DOI] [PubMed] [Google Scholar]
- 37.Tripathy NK, Jagnoor J, Patro BK, et al. Epidemiology of falls among older adults: A cross sectional study from Chandigarh, India. Injury 2015; 46(9): 1801–1805. DOI: 10.1016/j.injury.2015.04.037 [DOI] [PubMed] [Google Scholar]
- 38.Zaidi S, Khan Z and Khalique N.. Injury pattern in children: A population-based study. Indian J Community Health 2013; 25: 45–51. [Google Scholar]
- 39.Baiden F, Anto-Ocrah M, Adjei G, et al. Head injury prevalence in a population of injured patients seeking care in Ghana, West Africa. Front Neurol 2022; 13. DOI: 10.3389/fneur.2022.917294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sun D, Jiang B, Ru X, et al. Prevalence and altered causes of traumatic brain injury in China: A nationwide survey in 2013. Neuroepidemiology; 2020; 54(2): 106–113. DOI: 10.1159/000501911 [DOI] [PubMed] [Google Scholar]
- 41.Karamian A, Lucke-Wold B and Seifi A.. Prevalence of traumatic brain injury in the general adult population of the USA: A meta-analysis. Neuroepidemiology . Published online; August 22, 2024: 1–10. DOI: 10.1159/000540676 [DOI] [PubMed] [Google Scholar]
- 42.Schneider ALC, Wang D, Ling G, et al. Prevalence of self-reported head injury in the United States. N Engl J Med 2018; 379(12): 1176–1178. DOI: 10.1056/NEJMc1808550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frost RB, Farrer TJ, Primosch M, et al. Prevalence of traumatic brain injury in the general adult population: A meta-analysis. Neuroepidemiology 2013; 40(3): 154–159. DOI: 10.1159/000343275 [DOI] [PubMed] [Google Scholar]
- 44.Tesfaw A, Eshetu M, Teshome F, et al. Prevalence of head injury among trauma patients at Debre Tabor Comprehensive Specialized Hospital, North Central Ethiopia. Open Access Surg 2021; 14: 47–54. DOI: 10.2147/OAS.S321404 [Google Scholar]
- 45.Mikolić A, van Klaveren D, Oude Groeniger J, et al. Differences between men and women in treatment and outcome after traumatic brain injury. J Neurotrauma . Published online October 19, 2020: neu. 2020.7228. DOI: 10.1089/neu.2020.7228 [DOI] [PubMed] [Google Scholar]
- 46.Manoranjan B, Scott T, Szasz OP, et al. Prevalence and perception of intimate partner violence-related traumatic brain injury. J Head Trauma Rehabil 2022; 37(1): 53–61. DOI: 10.1097/HTR.0000000000000749 [DOI] [PubMed] [Google Scholar]
- 47.Daugherty J, Sarmiento K, Waltzman D, et al. Traumatic brain injury–related hospitalizations and deaths in urban and rural counties—2017. Ann Emerg Med 2022; 79(3): 288–296.e1. DOI: 10.1016/j.annemergmed.2021.09.433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chequer de Souza J, Dobson GP, Lee CJ, et al. Epidemiology and outcomes of brain trauma in rural and urban populations: A systematic review and meta-analysis. Brain Inj 2024; 38(12): 953–976. DOI: 10.1080/02699052.2024.2361641 [DOI] [PubMed] [Google Scholar]
- 49.Chaurasiya A, Ranjan JK, Pandey N, et al. Clinical and affective correlates of cognitive functioning in complicated mild and moderate traumatic brain injury patients belonging to rural areas. J Neurosci Rural Pract 2020; 12: 177. DOI: 10.1055/s-0040-1715083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chaurasiya A, Pandey N, Ranjan JK, et al. Neurocognitive and affective sequelae following complicated mild and moderate traumatic brain injury: A case series. Neurol India 2021; 69(1): 56–61. DOI: 10.4103/0028-3886.310110 [DOI] [PubMed] [Google Scholar]


