Abstract
Background
A cross sectional survey was carried out on 120 hospitalised geriatric patients aged 60 and above in Hospital Universiti Kebangsaan Malaysia, Kuala Lumpur to investigate their nutrient intakes and food preferences.
Methods
Food intakes were recorded using a one day weighed method and diet recall. Food preferences were determined using a five point hedonic score. Food wastages and factors affecting dietary adequacy were also investigated.
Results
The findings indicated that the mean intakes of energy and all nutrients investigated except for vitamin C and fluid were below the individual requirement for energy, protein and fluid, and the Malaysian Recommendation of Dietary Allowances (RDA) for calcium, iron, vitamin A, thiamin, riboflavin, niacin and acid ascorbic. In general, subjects preferred vegetables, fruits and beans to red meat, milk and dairy products. There was a trend of women to have a higher percentage for food wastage. Females, diabetic patients, subjects who did not take snacks and subjects who were taking hospital food only, were more likely to consume an inadequate diet (p < 0.05 for all values).
Conclusions
Food service system in hospital should consider the food preferences among geriatric patients in order to improve the nutrient intake. In addition, the preparation of food most likely to be rejected such as meat, milk and dairy products need some improvements to increase the acceptance of these foods among geriatric patients. This is important because these foods are good sources of energy, protein and micronutrients that can promote recovery from disease or illness.
Background
Ageing is related to the deterioration of some physiological and health functions, thus, elderly people are more susceptible to various diseases and illnesses. Nutrition plays an important role in preventing diseases and promoting recovery from illnesses [1,2]. Besides diseases and hospital environment [1], food preferences [2] are also main factors affecting the food intake of geriatric patients. Thus, hospital menu should be planned according to the preferences of geriatric patients to ensure that they eat what is served to them [2]. Studies on food intakes and habits among Malaysian elderly living in rural areas [3,4] reported that although the subjects had regular meal pattern, the dietary intake was inadequate. Most of studies conducted among hospitalised elderly people in Western countries [5-7] and Malaysia [8] reported that malnutrition as assessed using anthropometric and biochemical indicators is common.
With respect to food preferences, elderly people are more likely to stick to their traditional food rather than new food products as a result of rapid development in food industries [9-12]. However, some elderly people may change their food preferences due to health reasons [13] and food belief [13,3]. Ageing is associated with a shift from diet with high in calories, sugar and meat to diet with rich in fruits and vegetables [14-16]. However, avoidance of certain fruits and vegetables due to food beliefs had been reported in a proportion of rural elderly Malays [3].
It appeared that there was a need to investigate the adequacy of dietary intake and food preferences among our hospitalised geriatric patients. Therefore, this study aimed to investigate the food intakes and preferences and also factors influencing dietary adequacy among hospitalised geriatric patients. The study was also undertaken as a basis for improving the nutrient intake of patients in order to accelerate recovery from disease and hopefully to reduce the length of hospital stay.
Materials and methods
The study was carried out cross-sectionally over weekdays at Hospital Universiti Kebangsaan Malaysia, Kuala Lumpur from August to November 1999. Data were not collected during weekends or public holidays because there may be changes in visiting hours and food habits and thus interfere with the usual food intakes over the weekdays. The inclusion criteria were geriatric patients aged 60 and above, newly admitted to medical and surgical wards with no critical illnesses, not nil by mouth, not on ventilator, not on test diets such as Vannillyl Mandelic Acid Test Diet, not on parenteral or enteral feeding and not fasting for operation or examination procedure. Eligible subjects were randomly selected from the hospital admission list daily. Subjects were then identified in the ward and gave their consent to participate in the study. On the next day, a clinical nutritionist interviewed the subjects to obtain information on social and medical backgrounds and also food preferences. Food preferences were determined using a five point hedonic score [17]. The food items were adapted from the list of commonly consumed foods among Malaysian elderly [18,19]. Some of the medical information were obtained from medical records. The anthropometric measurements included weight and height were taken afterwards according to the standard techniques [20]. A one day food intake was evaluated using a weighed record for lunch and dinner using Soehnle Digital Scales to the nearest 0.01 kg. Diet recall was performed to estimate intake for breakfast and in-between meals. The diet recalls were carried out at least four times to increase the reliability of the data since memory fades with age. During the last interview to recall the dietary intake, subjects were asked about the acceptance towards hospital foods including presentation, smell, taste, texture, portion size, hygiene, temperature and timing. Information on the use of special products and intravenous fluid were also recorded.
Nutrient intake was analysed using a DIET4 program which is based on the Malaysian Food Tables [21] and compared to the individual requirements for calories [22], protein [22], fluid [23] and the Malaysian RDA for calcium, ferum, vitamin A, thiamin, riboflavin, niacin and ascorbic acid [24]. Data were analysed using the Statistical Package for Social Sciences version 7.5. In order to determine differences for continuous data, the independent t-test was used for parametric data, whilst, the Mann-Whitney test was used for non-parametric data. The chi-squared test was used to explore factors influencing dietary adequacy.
Results and discussion
A total of 129 eligible subjects were initially recruited but 120 completed the study (response rate of 93%). Among the reasons of non-response were complaints of tired and pain, early discharge and unable to communicate. Of the 120 subjects, 55% were females and 82.5% aged 60 to 74 years. The age range was 60 to 94 years, with mean 67.8. The ethnic composition of the subjects of 50.8% Malays, 37.5% Chinese and 11.7% Indian was closed to the national ratio [25].
Table 1 presents the sociodemographic and health characteristics of the subjects. Women were more likely to be widowed (p < 0.05), had not received formal education (p < 0.05) and unemployed with no pensions (p < 0.05). With respect to the medical profiles, majority of the subjects stayed for 7 days or less in the ward (65.8%) and had been diagnosed with less than three types of diseases (59.2%). The most common diagnosis was diseases of the nervous system and sensory organ included cataracts, glaucoma and diabetic retinopathy (35.0%), and cancer (20.8%). Earlier studies had also indicated that cataracts [26] and cancer [27] are among the most common reasons for admission among elderly people. Therapeutic diet was prescribed to 60.6% of females and 48.3% of males, with diabetic diet being the most likely to be ordered (42.4%) followed by low salt diet (19.7%). Only 16.7% took vitamin and mineral supplements. Approximately half of the subjects had normal Body Mass Index, but nearly 17% had chronic energy deficiency and 28% were overweight.
Table 1.
Sociodemographic, health & medical characteristics of subjects.
| Characteristics | Male (n = 54) | Female (n = 66) | Total (n = 120) | |||
| n | % | n | % | n | % | |
| Demographic & socioeconomic: | ||||||
| widowed | 4 | 7.4 | 33* | 50.0 | 37 | 30.8 |
| no schooling | 2 | 3.7 | 34* | 51.5 | 36 | 30.0 |
| unemployed with no pensions | 15 | 27.8 | 61* | 92.4 | 76 | 63.3 |
| Medical: | ||||||
| multiple pathology (≥ 3 diagnosis) | 22 | 40.7 | 27 | 40.9 | 49 | 40.8 |
| therapeutic diet | 26 | 48.3 | 40 | 60.6 | 66 | 54.9 |
| Health: | ||||||
| visual problem | 43 | 79.6 | 56 | 84.8 | 99 | 82.5 |
| loss of appetite | 39 | 72.2 | 37 | 56.1 | 76 | 63.3 |
| Wearing denture | 16 | 29.3 | 35* | 53.0 | 51 | 42.5 |
| smoker or ex-smoker | 34 | 62.9 | 6* | 9.1 | 40 | 33.3 |
| food beliefs | 44 | 81.5 | 60 | 90.9 | 104 | 86.7 |
| self- perceived poor health | 29 | 53.8 | 28 | 42.4 | 57 | 47.5 |
| chronic energy deficiency (BMI < 18.5) | 10 | 18.5 | 11 | 16.7 | 21 | 17.5 |
| overweight (BMI ≥ 25.0) | 11 | 20.4 | 23 | 34.8 | 34 | 28.3 |
*p < 0.05 (Chi-squared test); BMI-Body mass index.
As reported among elderly Malays in rural areas [3], the mean intake for energy and all the investigated nutrients of this hospitalised elderly were below the recommendation except for ascorbic acid and fluid, as shown in Table 2. The intakes of energy, micronutrients and fluid were inadequate for more than 2/3 of the subjects.
Table 2.
Intakes of energy and micronutrients among hospitalised geriatric patients.
| Nutrients (unit) | Mean (SD) | Men (n = 54) | Female (n = 66) | Requirement | % subjects with intake less than requirement |
| Energy (kcal) | 1144 (480) | 1326 (488) | 995 (422)* | Individuala | 85.8 |
| Protein (g) | 44.2 (23.3) | 51.4 (25.7) | 38.3 (19.5)* | Individuala | 69.2 |
| Vitamin A (mg RE) | 401.7 (232.5) | 447.3 (225.4) | 364.4 (233.2)* | 750b | 93.3 |
| Thiamin (mg) | 0.65 (0.39) | 0.77 (0.48) | 0.55 (0.27)* | 0.8b | 71.7 |
| Riboflavin (mg) | 0.80 (0.50) | 0.90 (0.52) | 0.71 (0.48)* | 1.2b | 83.3 |
| Niacin (mg NE) | 9.6 (6.4) | 11.9 (7.1) | 7.8 (5.2)* | 13b | 76.7 |
| Acid ascorbic (mg) | 33.9 (31.4) | 36.6 (33.2) | 31.8 (29.8) | 30b | 63.3 |
| Calcium (mg) | 354.2 (319.8) | 350.6 (239.0) | 357.1 (375.0) | 450b | 77.5 |
| Iron (mg) | 7.6 (4.6) | 8.4 (4.4) | 6.8 (4.7) | 9b | 74.2 |
| Fluid (ml) | 1504 (871) | 1757 (1135) | 1296 (490)* | Individualc | 65.0 |
*p < 0.05, significant at 2 tailed (independent sample t-test) aIndividual requirement based on weight and height. b Malaysian RDA. c Individual fluid requirement based on age.
In general, the food preferences for both sexes are quite similar (Table 3). They preferred vegetables, fruits, legumes, rice, cereal, bread and noodles and fish rather than red meat and milk and dairy products. The food preferences may be influenced by health and disease states. With ageing, there was an increase in the intake of fruits and vegetables and a decrease in the consumption of red meat [14]. In our study the score was analysed using food group not individual food items, thus, specific food dislike may not be detected. For example, the score was the highest for vegetable food group, but a few types of vegetables such as white carrot, swamp cabbage and long beans with the lowest score was not showed. These type of foods were also avoided due to traditional food belief and were regarded as 'cold food'. A study on food preferences is more accurate if using the score for individual food item [28-31] but too many food items may burden the elderly subjects especially those with diseases or illnesses. As reported in the earlier study [3], a high proportion of the hospitalised elderly (86.7%) also had avoided a wide range of foods that are traditionally belief as bad for health mainly regarded as 'cold' as discussed earlier or being omitted from the diet due to health reasons such as diabetic, hypertensive and gastritis.
Table 3.
Food preferencesa among hospitalised geriatric patients as assessed using Hedonic Score [mean (sd)]
| Men (n = 54) | Women (n = 66) | ||
| Food Group | Mean (SD) | Food Group | Mean (SD) |
| 1. Vegetables | 3.67 (0.52) | 1. Vegetables | 3.67 (0.56) |
| 2. Fruits | 3.67 (0.85) | 2. Fruits | 3.44 (1.02) |
| 3. Legumes | 3.48 (0.55) | 3. Legumes | 3.27 (0.70) |
| 4. Rice, cereal, bread and noodles | 3.44 (0.34) | 4. Rice, cereal, bread and noodles | 3.25 (0.53) |
| 5. Fish and seafood | 3.14 (0.56) | 5. Fish and seafood | 3.06 (0.62) |
| 6. Fat and oil | 3.15 (0.60) | 6. Egg | 2.97 (0.82) |
| 7. Dessert | 3.15 (0.74) | 7. Dessert | 2.94 (0.74) |
| 8. Eggs | 3.10 (0.72) | 8. Fat and oil | 2.78 (0.58) |
| 9. Beverage | 2.97 (0.54) | 9. Beverage | 2.80 (0.54) |
| 10. Milk and dairy products | 2.91 (0.56) | 10. Milk and dairy products | 2.69 (0.72) |
| 11. Meat and chicken | 2.76 (0.75) | 11. Meat and chicken | 2.56 (0.62) |
afood preferences based on five point hedonic score, from the highest score to the lowest score in ascending order.
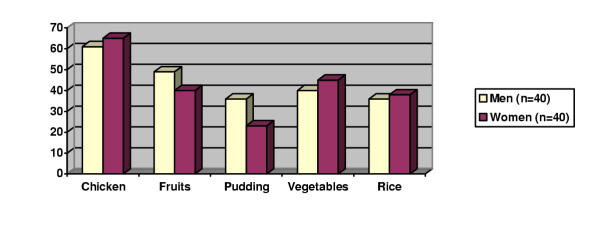
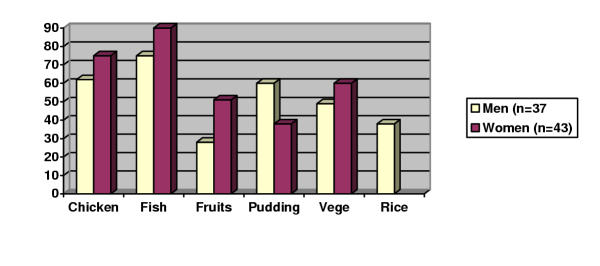
Approximately 81% of the subjects consumed foods both served by the hospital (hospital foods) and also those bought outside or brought by relatives (non-hospital foods); 14% consumed hospital foods only and 5% consumed non-hospital foods only. Food wastage analysis of hospital food served for lunch and dinner was carried out among a sub sample of 80 subjects, as shown in Figure 1 and Figure 2, respectively. The percentage of food wastage varied among dishes and sexes, ranged from 20% to 90%. It appeared that the food wastage was the highest for main dish such as chicken and fish, and more common in women for most of the food items (only weight of the edible parts being presented). Other studies also reported that food wastage was high among hospitalised patients, with more than 40% of hospital foods were wasted [32,33].
Figure 1.
Percentage of food wastage during lunch Note: fish was not included in lunch because fish was only served during dinner.
Figure 2.
Percentage of food wastage during dinner
Table 4 presents the results of analysis of acceptance towards hospital food services among subjects who were on normal and therapeutic diets. Both groups rated high score, thus expressed their satisfaction for food hygiene and meal times. They were in agreement in giving low rating for taste, appearance and temperature of hot foods. Complaint on food temperature is so common among hospitalised patients [34,35].
Table 4.
Acceptance on the quality of food services* in hospital rated by subjects receiving normal diet and therapeutic diet
| Rating by subjects (normal diet) (n = 54) | Rating by subjects (therapeutic diet) (n = 66) |
| 1. Food hygiene | 1. Food hygiene |
| 2. Time for lunch | 2. Time for breakfast |
| 3. Time for breakfast | 3. Time for lunch |
| 4. Temperature of cold food | 4. Food portion |
| 5. Food portion | 5. Time for dinner |
| 6. Food texture | 6. Texture of food |
| 7. Time for dinner | 7. Temperature of cold food |
| 8. Taste | 8. Appearance of food |
| 9. Appearance of food | 9. Taste of food |
| 10. Temperature of hot food | 10. Temperature of hot food |
* Item presented according to score from the highest (most acceptable) to the lowest (least likely to be accepted)
It was found that females, diabetic patients, subjects who did not take snacks and subjects who were only taking hospital food were more likely to consume an inadequate diet (p < 0.05 for all parameters), as shown in Table 5. Interestingly more women consumed inadequate diet and the percentage of food wastage was also slightly higher in women as compared to men. The findings indicated that besides three main meals and afternoon snack that being served at the moment of the study; midmorning tea and supper should also be served to increase the calories and micronutrients intakes. Diabetics were more likely to consume inadequate diet probably because they tend to limit food intake in order to achieve good control of blood glucose or diabetic diet is simply not palatable. There is a need to impart a wholesome nutrition education for diabetic patients.
Table 5.
Factors affecting dietary adequacy
| Dietary adequacya | |||||
| Factors | Yes | No | p value | ||
| n | % | n | % | ||
| Sociodemographic | |||||
| Female | 21 | 42.9 | 45 | 63.4 | 0.026* |
| no schooling | 10 | 20.4 | 26 | 36.6 | 0.057 |
| Health | |||||
| have chewing problem | 10 | 20.4 | 26 | 36.6 | 0.057 |
| without teeth | 6 | 12.2 | 19 | 26.8 | 0.054 |
| Eating pattern in hospital | |||||
| did not take snacks | 2 | 4.1 | 15 | 21.1 | 0.008* |
| taking only hospital food | 2 | 4.1 | 15 | 21.1 | 0.008* |
| eating alone during every main meal | 39 | 79.6 | 65 | 91.5 | 0.058 |
| Medical | |||||
| from surgical ward | 26 | 53.1 | 50 | 70.4 | 0.052 |
| undergone operation | 10 | 20.4 | 26 | 36.6 | 0.057 |
| under diabetic diet | 6 | 12.2 | 22 | 31.0 | 0.017* |
afive or more nutrients from the eight selected nutrients are more than 2/3 RDA; *p < 0.05 (Chi-squared test)
Conclusions
In conclusion, there is a concern towards dietary inadequacy among hospitalised elderly patients, with the diabetics, females and those consuming hospital food only are at a higher risk of malnutrition. Their nutrient intake can be increased by taking into consideration their food preferences, giving snacks or in between meals and improving the food service with respect to temperature, smell and appearance of food being served.
Competing interests
None declared.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
We would like to acknowledge the assistance given by staffs at Department of Dietetics and Food Services, Medical and Surgical Wards, Admission and Discharge Unit, and also SAJIBUMI of Hospital Universiti Kebangsaan Malaysia. We are indebted to the elderly subjects participated in this study. This study was supported by UKM Grant N2/99.
Contributor Information
Suzana Shahar, Email: suzanas@medic.ukm.my.
Kan Yin Chee, Email: suzanas@medic.ukm.my.
Wan Chak Pa' Wan Chik, Email: wan-chak@mail.hukm.ukm.my.
References
- Morley JE, Miller DK. Malnutrition in the elderly. Hosp Pract (off Ed) 1992;27:95–98. doi: 10.1080/21548331.1992.11705455. [DOI] [PubMed] [Google Scholar]
- Grows E, Rossouw JE, Labadarios D, Eck M. The nutrient intake of a group of older South African hospitalized persons. J Am Diet Assoc. 1989;89:255–257. [PubMed] [Google Scholar]
- Suzana S, Earland J, Suriah AR. Dietary intakes and food habits among rural elderly Malays. Asia Pacific J Clin Nutr. 2000;9:122–129. doi: 10.1046/j.1440-6047.2000.00147.x. [DOI] [PubMed] [Google Scholar]
- Suriah AR, Zainorni MJ, Shafawi S, Mimie SS, Zarina N, Wan Zainuddin WA, Zalifah MK. Nutrient intake among elderly in southern Penisular Malaysia. Mal J Nutr. 1996;2:11–19. [PubMed] [Google Scholar]
- Asplund K, Axelsson K, Norberg A, Eriksson S. Malnutrition in hospitalized elderly patients. In: RK Chandra, editor. Nutrition, immunity and illness in the elderly. New York: Pergamon Press.; 1985. pp. 213–227. [Google Scholar]
- Constans T, Bacq Y, Bréchot JF, Giwilmot JL, Choutet P, Lamisse F. Protein-energy malnutrition in elderly medical patients. J Am Geriat Soc. 1992;40:263–268. doi: 10.1111/j.1532-5415.1992.tb02080.x. [DOI] [PubMed] [Google Scholar]
- Williams R, Boyce T. Protein malnutrition in elderly Navajo patients. J Am Geriatr Soc. 1989;37:397–406. doi: 10.1111/j.1532-5415.1989.tb02634.x. [DOI] [PubMed] [Google Scholar]
- Suzana S, Wong F. Malnutrition among hospitalised geriatric patients. Research Highlights UKM. 2001.
- Chau P, Lee HS, Tseng R, Downes J. Dietary habits, health beliefs, and food practices of elderly Chinese women. J Am Diet Assoc. 1990;90:579–580. [PubMed] [Google Scholar]
- Fujita Y. Nutritional requirements of the elderly: A Japanese view. Nutr Rev. 1992;50:449–453. doi: 10.1111/j.1753-4887.1992.tb02501.x. [DOI] [PubMed] [Google Scholar]
- Krondl M, Lau D, Yurkiw MA, Coleman H. Food used and perceived food meaning of the elderly. J Am Diet Assoc. 1982;80:523–529. [PubMed] [Google Scholar]
- SENECA Food patterns of elderly Europeans. Eur J Clin Nutr. pp. S86–S100. [PubMed]
- Schlettwein-Gsell D. Nutrition and the quality of life: a measure for the outcome of nutritional intervention? Am J Clin Nutr. 1992;55:1263S–1266S. doi: 10.1093/ajcn/55.6.1263S. [DOI] [PubMed] [Google Scholar]
- Drewnowski A. Impact of aging on eating behaviors, food choices, nutrition and health status. Abstrak Concerence on Nutrition and Healthy Aging in Asia Singapura, 6–7 Julai 1991. [PubMed]
- Fujita Y, Ebisawa H. Dietary habits and nutritional problems of the elderly in Japan. Proceeding 6th Asian Congress of Nutrition Kuala Lumpur. 16–19 September 1991.
- Popkin BM, Haines PS, Patterson E. Dietary changes in older American, 1977–1987. Am J Clin Nutr. 1992;55:823–830. doi: 10.1093/ajcn/55.4.823. [DOI] [PubMed] [Google Scholar]
- Randall E, Sanjur D. Food preferences – their conceptualization and relationship to consumption. Ecology Food Nut. 1981;11:151–161. [Google Scholar]
- Suzana S. Nutritional status of rural elderly Malays: an exploration of social and health factors to develop a screening tool for identifying individuals at high risk of undernutrition and consuming an inadequate diet. PhD Thesis University of Sheffield, United Kingdom. 1998.
- Zalifah K. Status pemakanan dan penentuan nilai ambang rasa manis dan masin di kalangan warga tua diabetik dan bukan diabetik. Tesis ijazah sarjana Universiti Kebangsaan Malaysia. 1999.
- Fidanza F. Anthropometric methodology. In: F Fidanza, editor. Nutritional status assessment. London: Chapman & Hall; 1991. pp. 1–62. [Google Scholar]
- Tee ES, Ismail MN, Mohd A. Nutrient composition of Malaysian foods. Kuala Lumpur, ASEAN Sub-Committee on Protein-Food Habits Research and Development. 1988.
- Claudia VS, Lagua T. Nutrition and diet therapy dictionary. 3 1991. [Google Scholar]
- Randall H. Fluid, electrolyte, and fluid base balance. Surg Clin North Am. 1976;56:1019. doi: 10.1016/s0039-6109(16)41030-3. [DOI] [PubMed] [Google Scholar]
- Teoh T. Recommended daily dietary intakes for peninsular Malaysia. Med J Malaysia. 1975;30:38–42. [PubMed] [Google Scholar]
- Department of Statistics Laporan Am Banci Penduduk Jilid 2. Kuala Lumpur, Department of Statistics. 1991.
- Srinivas P, Poi PJH, Ebrahim S. Pattern of medical admissions among the elderly: a prospective review in University Hospital, Kuala Lumpur. Med J Malaysia. 1996;51:210–214. [Google Scholar]
- Lim G. Surgical problems among the elderly in Malaysia. Med J Malaysia. 1997;52:217–221. [PubMed] [Google Scholar]
- Dobell E, Chan M, Williams P, Allman M. Food preferences and food habits of patients with chronic renal failure undergoing dialysis. J Am Diet Assoc. 1993;93:1129–1135. doi: 10.1016/0002-8223(93)91644-6. [DOI] [PubMed] [Google Scholar]
- Meiselman HL, Waterman D. Food preferences of enlisted personnel in the armed forces. J Am Diet Assoc. 1978;73:621–629. [PubMed] [Google Scholar]
- Vickers ZM, Nielsen SS, Theologides A. Food preferences of patients with cancer. J Am Diet Assoc. 1981;79:441–445. [PubMed] [Google Scholar]
- Williams G. Food preferences of 500 inpatients in an Australian teaching hospital. J Food Nutr. 1988;45:34–40. [Google Scholar]
- Barton AD, Beigg CL, Macdonald IA, Allison P. High food wastage and low nutritional intakes in hospital patients. Clin Nutr. 2000;19:445–449. doi: 10.1054/clnu.2000.0150. [DOI] [PubMed] [Google Scholar]
- Edwards J, Nash A. Catering services. Measuring the wasteline. Health Service J. 1997;107:26–27. [PubMed] [Google Scholar]
- DeLuco D, Cremer M. Consumers' perception of hospital food and dietary services. J Am Diet Assoc. 1990;90:1711–1715. [PubMed] [Google Scholar]
- Lau C, Gregoire MB. Quality ratings of a hospital food service department by inpatients and postdischarge patients. J Am Diet Assoc. 1998;98:1303–1307. doi: 10.1016/S0002-8223(98)00291-0. [DOI] [PubMed] [Google Scholar]