Abstract
Introduction
Urgent hospital readmissions within 30 days of discharge after surgery are a measure of the quality of health and social care. This study aims to identify the characteristics of patients at higher risk of readmission and the main reasons for readmission, stratified by type of surgery.
Methods
This cross-sectional study analysed the medical records of patients over 60 years of age in 2022 who had undergone surgery. Records came from hospitals covering an area of 890,000 inhabitants in Northern Italy (ULSS Marca Trevigiana). Risk factors for readmission included demographic characteristics, hospitalisation details, comorbidities, and procedures. Readmission rates and 95% CI were calculated by risk factor, type of intervention and reason for readmission. A logistic model was used to estimate the OR of readmission, adjusting for potential confounders.
Results
The overall 30-day readmission rate was 3.8% (3.5–4.3), with the highest rates after gastrointestinal surgery (49.7 per 1,000 admissions) and the lowest after skin-soft tissue surgeries (15.5 per 1,000 admissions). Multivariate analysis identified dementia (OR = 3.19), end-stage kidney disease or dialysis (OR = 2.84), and metastatic cancer (OR = 2.65) as strong predictors of readmission. Advanced age (75+), male gender, primary cancer, and anemia were also independent predictors. Infection was the main reason for readmission. Other significant causes were hemorrhage, thrombosis/embolism, and intestinal obstruction.
Conclusions
The study highlights the importance of identifying risk factors for readmission to improve transitions of care. Targeted interventions for high-risk populations, particularly those with dementia, renal disease, or cancer, are essential to improve postoperative outcomes and alleviate the burden of unplanned readmissions on healthcare systems.
Introduction
Readmission after hospitalization is a critical aspect posing issues for patients, healthcare services, and social services. In the US, one in 7 patients are readmitted within 30 days following major surgery using Medicare claims data. Among these, 70.5% were rehospitalized for a medical condition, though 10% were likely to have been planned [1].
While medical patients are frequently readmitted for the same diagnosis with which they were discharged, surgical patients are more likely to be readmitted with a surgical complication that varies by patient factors and procedure type [2].
Factors influencing readmission after surgery are vast and can generally be summarized into biologic (e.g., comorbidities, frailty), procedure-related (e.g. duration of surgery, experience of surgeon [3]), socio-economic, and demographic (ethnicity, age) [4].
Readmission rate can only be useful as a hospital quality measure to the extent that readmissions could both be predicted and potentially prevented by actions over which hospitals have some influence [2]. It has been long debated whether surgical readmissions are predictable and thereby preventable [4].
Studies need to focus on targeting the clinical modifiable risk factors and discharge planning and education, which may help to prevent 30-day readmissions [5]. Although postoperative readmissions are difficult to predict at the time of discharge, preoperative factors are the most important to drive the prediction [2, 6].
Nonetheless, other postoperative, yet modifiable factors play a role in the readmission risk, among which the discharge setting. In this light the implementation of a thorough post-acute care program, including timely home- or facility-based clinical follow-up and rehabilitation, can prevent readmission occurrence [7, 8].
This study aims to understand both (a) risk factors for readmission within 30 days of discharge after surgical procedure in patients over 60 years old, and (b) the main reasons for readmission, stratified by type of surgery. This data could help healthcare professionals and policy makers to develop strategies for continuous quality improvement and tailored clinical risk management activities.
Methods
We followed STROBE guidelines for the reporting of this cross-sectional study [9].
Sample
The database relies on data from ordinary admissions, obtained from Hospital Discharge Records (SDO), which occurred in the year 2022 on a served population of 890,000 (ULSS 2 Health Authority “Marca Trevigiana”). To the purpose of the present study, only surgical index admissions in patients over 60 were included. Readmission was defined as a new hospital urgent - not programmed - admission within 30 days of discharge from the index admission.
We excluded: (1) index admissions ending with discharge to another hospital or with death of patient. (2) where the index admission was surgical but no intervention was eventually performed (only diagnostic procedures).
Hospital discharge records of index admissions were screened to collect data on potential risk factors of readmissions. In particular, we derived data on:
Patient demographic characteristics (age, gender).
Admission characteristics (length of stay, hospital, type of discharge - home, nursing come, home care).
Patient conditions and comorbidities (Table 1).
Procedures (Table 1).
Table 1.
ICD 9 codes for risk factors
| Risk factor | ICD 9 Codes | Reason for readmission | ICD 9 Codes | Intervention type | ICD-9 Codes |
|---|---|---|---|---|---|
| Dementia | 290–294 | Infection | 99,591; 5990; 7806; 9985.X; 038.X; 0384.X; 5672.X; 4804.X; 486; 7855.2; 4402.4; 482.X; 485; 507.X; 99,590; 0084.X; 4660; 9966.X; 9981.X; 041.X; 043.X; 1125; 421.X; 682.X, 7300.X; 7854 | CARDIOVASCULAR | 004X, 005X, 006X, 35X, 36X, 37X, 38X, 39X |
| Alcohol-related disease | 5710–5712;34,831; 34,982 | Wound complications | 998.3; 998.8 | ORTHOPEDIC | 007X, 008X, 009X, 76X, 77X, 78X, 79X, 80X, 81X, 82X, 83X, 84X |
| Bedridden | V4984; 7282; 7994; 2639; 707 | AKI | 584.X | NEURO | 01X, 02X, 03X, 04X, 05X |
| Diabetes | 250 | Heart failure | 428.X | ENDOCRINE | 06X, 07X |
| Dialysis or end-stage kidney disease | 5855–5856, V560-568; 3942, 3927; 3995 | Hemorrage | 998.1X; 285.1; 5997; 5310.X; 569.3; 431; 4590; 5688.1; 578.X; 6266; 7827; 7847 | EYE | 08X, 09X, 10X, 11X, 12X, 13X, 14X, 15X, 16X |
| Transplant | V420-V429 [excl. V4289] | Thrombosis/Embolism | 4151.X; 434.X; 451.X | ENT | 18X, 19X, 20X, 21X, 22X, 23X, 24X, 25X, 26X, 27X, 28X, 29X |
| Epilepsy | 345 | Coronary Syndrome/Myocardial Infarction | 410.X; 4111; 4140.X; 413.X | THORACIC | 30X, 31X, 32X, 33X, 34X |
| Obesity | 278 | Pleural effusion/Pneumothorax/Respiratory Failure | 5188.X; 5119; 512.X; | EMATOLYMPHATIC | 40X, 41X |
| Transfusion | 990–999 | Fluid and electrolyte disorders | 275.X; 276.X | GI | 42X, 43X, 44X, 45X, 46X, 47X, 48X, 49X, 50X, 51X, 52X, 53X, 54X |
| Anemia | 280–285 | Pancreatic or Hepatic | 57X.X | UROLOGIC | 55X, 56X, 57X, 58X, 59X, 60X, 61X, 62X, 63X, 64X |
| COVID | 48,041; 04311; 04321; 51,971 | Intestinal occlusion | 560.X | GYNECOLOGICAL | 65X, 66X, 67X, 68X, 69X, 70X, 71X, 72X, 73X, 74X, 75X |
| Stoma | V44, V55, 57xx | - | - | SKIN-SOFT TISSUES | 85X, 86X |
| COPD | 490–496 | - | - | - | - |
| Cancer | 140–209 | - | - | - | - |
| Myeloma | 20,300 | - | - | - | - |
| Pneumonia | 480–486; 4870 | - | - | - | - |
| UTI | 599; 590XX; 5950 | - | - | - | - |
Type of surgery was coded on the basis of ICD-9-CM intervention code categories defined by the Italian Healthcare Ministery [10], as in Table 1.
Reasons for readmission were defined according to main diagnosis at readmission (Table 1).
Statistical analysis
Difference in distribution of risk factors between readmitted and non-readmitted patients was tested using chi-square test for categorical variables while for continuous variables t-test was applied to verify mean differences by groups.
Rate of readmission was calculated dividing the number of readmissions and dividing by the number of index admissions, then multiplied by 1,000. 95% Binomial confidence intervals were used. Non-overlapping confidence intervals were considered statistically significant differences.
Mixed effects multiple logistic regression was used to assess the effect of individual predictors on probability of readmission, considering nesting in hospitals and correcting for age and gender.
Statistical tests were two-sided and a p-value less than 0.05 was considered statistically significant. All analyses were performed using R version 4.2.3 (R Foundation for Statistical Computing, Vienna, Austria).
Ethics
The dataset was pseudo-anonymized before analysis. The study protocol was approved by the competent ethics committee for the area (Prot. N. 0022516/24; 07/11/2024).
Results
A total number of 9020 index admissions occurred. Readmissions occurred less than 30 days after a first admission were 349. Median time to readmission was 9 days. Mortality during the readmission was 15.19%.
Overall 30-day readmission rate was 38.7 [34.9–42.9] (Table 2). Readmission was most common after gastro-intestinal procedures (49.7 [CI 40.3–61.1]) and least common after skin-soft tissue surgery (15.5 [CI = 8.2–29.1]).
Table 2.
Rate [CI] (Number) of readmission by type of surgery and risk factor
| Variable | Cardiovascular | GI | Orthopedic | Other | Skin-Soft Tissues | Urologic | Total |
|---|---|---|---|---|---|---|---|
| Age − 75+ | 60.7* [47.7–76.9] (63) | 68.8* [51.8–90.8] (45) | 63.7* [51.2–79.0] (76) | 44.2 [28.5–68.0] (19) | 11.6 [3.2–41.2] (2) | 43.6 [27.7–67.8] (18) | 57.2* [50.3–64.9] (223) |
| SEX - F | 32.4 [20.8–50.0] (19) | 47.6 [34.4–65.4] (35) | 36.5 [28.1–47.3] (54) | 28.3 [19.4–41.1] (26) | 15.5 [7.9–30.3] (8) | 19.8 [7.7–49.8] (4) | 32.9 [28.0-38.5] (146) |
| SEX - M | 45.4 [35.8–57.3] (66) | 51.3 [39.0-67.2] (49) | 52.8 [38.0-72.9] (34) | 44.1 [30.3–63.9] (26) | 15.2 [0.8–81.0] (1) | 31.1 [21.4–44.8] (27) | 44.3* [38.8–50.7] (203) |
| DISCHARGE - HOME | 35.5 [28.2–44.7] (69) | 46.0 [36.7–57.4] (73) | 29.9 [22.6–39.5] (47) | 33.0 [25.1–43.4] (49) | 15.7 [8.3–29.5] (9) | 26.4 [18.3–37.9] (28) | 33.5 [29.8–37.6] (275) |
| DISCHARGE - NURSING HOME | 134.6* [66.8-252.7] (7) | 69.8 [24.0-186.1] (3) | 44.4 [27.9–69.9] (17) | 76.9 [3.9-333.1] (1) | - | 200.0 [10.3-624.5] (1) | 58.1* [40.8–82.2] (29) |
| DISCHARGE - HOME CARE | 187.5 [101.9-319.4] (9) | 133.3 [69.1-241.7] (8) | 141.2* [96.7-201.5] (24) | 166.7 [47.0-448.0] (2) | - | 333.3 [96.8–700.0] (2) | 150.0* [114.0-194.8] (45) |
| DEMENTIA | 214.3* [75.7-475.9] (3) | - | 235.3* [124.4–400.0] (8) | - | - | - | 180.3* [103.8-294.7] (11) |
| DIABETES | 52.0 [30.6–86.9] (13) | 43.5 [14.9-120.2] (3) | 66.7 [28.8-146.8] (5) | - | - | - | 48.1 [31.6–72.3] (21) |
| DIALYSIS OR END-STAGE KD | 145.5* [75.6-261.6] (8) | 100.0 [5.1-404.2] (1) | - | - | - | - | 111.1* [59.6-197.9] (9) |
| TRANSPLANT | 34.5 [1.8-171.8] (1) | - | - | - | - | - | 16.1 [0.8–85.9] (1) |
| ANEMIA | 87.0 [34.3-203.2] (4) | 60.0 [20.6-162.2] (3) | 94.3* [71.3-123.9] (45) | 66.7 [3.4-298.2] (1) | - | 153.8* [43.3-422.3] (2) | 91.2* [70.7-116.9] (55) |
| STOMA | 62.5 [17.3-201.5] (2) | 87.0 [40.5–177.0] (6) | - | 176.5* [83.5-335.1] (6) | - | 107.1 [37.1–272.0] (3) | 103.7* [65.7-159.7] (17) |
| CANCERa. PRIMARY | 187.5* [65.9-430.1] (3) | 75.8* [51.8-109.4] (25) | 176.5* [61.9-410.3] (3) | 65.1* [41.1-101.8] (17) | 13.7 [5.9–31.7] (5) | 32.3 [20.5–50.5] (18) | 46.0 [36.6–57.6] (71) |
| CANCERb. METASTATIC | - | 136.4 [79.8-223.4] (12) | 142.9 [7.3-513.1] (1) | 50.8 [17.4-139.2] (3) | 16.9 [0.9–90.0] (1) | 500.0 [25.6-974.4] (1) | 82.9 [53.1-127.3] (18) |
| PNEUMONIA | 96.8 [33.5–249.0] (3) | 87.0 [24.2–268.0] (2) | 111.1 [31.0-328.0] (2) | 200.0* [70.5-451.9] (3) | - | - | 112.4* [62.2-194.6] (10) |
| UTI | 181.8* [51.4–477.0] (2) | - | 88.2 [30.5-229.6] (3) | 333.3 [17.1-792.3] (1) | - | - | 101.7* [47.4-204.6] (6) |
| LENGTH OF STAY − 15 + days | 109.5* [73.4-160.2] (22) | 113.5* [78.7-161.2] (26) | 75.8* [56.4-101.2] (41) | 122.6* [73.1-198.6] (13) | 83.3 [4.3-353.9] (1) | 23.3 [1.2-120.6] (1) | 91.9* [76.4-110.1] (104) |
| DISCHARGE_DAY - Weekday | 41.6 [33.8–51.2] (85) | 49.7 [40.3–61.1] (84) | 41.4 [33.7–50.7] (88) | 34.5 [26.4–44.9] (52) | 15.5 [8.2–29.1] (9) | 28.9 [20.5–40.8] (31) | 38.7 [34.9–42.9] (349) |
| Total | 41.6 [33.8–51.2] (85) | 49.7 [40.3–61.1] (84) | 41.4 [33.7–50.7] (88) | 34.5 [26.4–44.9] (52) | 15.5 [8.2–29.1] (9) | 28.9 [20.5–40.8] (31) | 38.7 [34.9–42.9] (349) |
(*) indicate risk factors significantly associated with higher rates of readmission
Across all intervention types, significant unadjusted risk factors for higher readmission rates included advanced age (75+) (57.2 [50.3–64.9; n = 223]), male gender (44.3 [38.8–50.7; n = 203]), discharge to home care (150.0 [114.0-194.8; n = 45]), dementia (180.3 [103.8-294.7; n = 11]), dialysis or end-stage kidney disease (111.1 [59.6-197.9; n = 9]), anemia (91.2 [70.7-116.9; n = 55]), prolonged hospital stays (15 + days) (91.9 [76.4-110.1; n = 104]), pneumonia (112.4, [62.2–194.6; n = 10]), presence of a stoma (103.7 [65.7-159.7; n = 17]).
Patients with dementia had significantly higher rates of readmission after cardiovascular and orthopedic surgery, respectively 214.3 [75.7-475.9; n = 3] and 235.3 [124.4–400.0; n = 8]. Patients with dialysis or end-stage kidney disease experienced a significantly higher readmission rate after cardiovascular interventions (145.5 [75.6-261.6; n = 8). Primary cancer was associated with significantly higher rates of readmission after cardiovascular, GI, and orthopedic surgery (respectively 187.5 [65.9-430.1; n = 3], 75.8 [51.8-109.4; n = 25], and 176.5 [61.9-410.3; n = 3]). Metastatic cancer had higher rates of readmission after GI surgery (136.4 [79.8-223.4; n = 12]). Anemia was also associated with significantly elevated readmission rates after orthopedic surgery (94.3 [71.3-123.9; n = 45]). Patients with UTI had higher rates of readmission after cardiovascular surgery (181 [51.4–477.0; n = 2]).
Table 3 shows rates and proportions of readmission by cause and type of intervention. Infection is the leading cause of readmission, accounting for 32.7% of all readmissions. Rates of readmission for infection were higher after orthopedic (18.4 [13.5–25.0]), gastrointestinal (14.2 [9.6–21.0]), and urologic (12.1 [7.1–20.7]) surgery. Coronary syndrome and myocardial infarction accounts for 23.5% of readmissions after cardiovascular surgery, with a rate of 9.8 [6.3–15.1]. Orthopedic interventions have a higher chance of readmission for venous thromnboembolism (VTE) (rate = 8.0 [5.0-12.8]), while gastrointestinal procedures reveal substantial rates for intestinal occlusion (8.3 [4.9–13.8]) and hemorrhage (7.7 [4.5–13.1]).
Table 3.
Rate of readmission by type of surgery and main cause of readmission
| Main cause of readmission | Cardiovascular | GI | Orthopedic | Other | Skin-Soft Tissues | Urologic | Total |
|---|---|---|---|---|---|---|---|
| Rate [CI] (N; Column %) | Rate [CI] (N; Column %) | Rate [CI] (N; Column %) | Rate [CI] (N; Column %) | Rate [CI] (N; Column %) | Rate [CI] (N; Column %) | Rate [CI] (N; Column %) | |
| Infection | 8.3 [5.2–13.3] (17; 20) | 14.2 [9.6–21.0] (24; 28.6) | 18.4 [13.5–25.0] (39; 44.3) | 11.9 [7.6–18.8] (18; 34.6) | 5.2 [1.8–15.0] (3; 33.3) | 12.1 [7.1–20.7] (13; 41.9) | 12.6 [10.5–15.2] (114; 32.7) |
| Heart Failure | 6.4 [3.7–10.9] (13; 15.3) | 0.6 [0.0-3.3] (1; 1.2) | 2.8 [1.3–6.1] (6; 6.8) | - | - | 1.9 [0.5–6.8] (2; 6.5) | 2.4 [1.6–3.7] (22; 6.3) |
|
Fluid and Electrolyte Disorders |
1.0 [0.3–3.6] (2; 2.4) | 0.6 [0.0-3.3] (1; 1.2) | 1.4 [0.5–4.1] (3; 3.4) | 1.3 [0.4–4.8] (2; 3.8) | - | - | 0.9 [0.4–1.7] (8; 2.3) |
|
Coronary Syndrome Myocardial Infarction |
9.8 [6.3–15.1] (20; 23.5) | - | - | - | - | - | 2.2 [1.4–3.4] (20; 5.7) |
| Thrombosis/Embolism | - | 0.6 [0.0-3.3] (1; 1.2) | 8.0 [5.0-12.8] (17; 19.3) | 1.3 [0.4–4.8] (2; 3.8) | - | 0.9 [0.0-5.3] (1; 3.2) | 2.3 [1.5–3.6] (21; 6) |
|
Pleural Effusion Pneumothorax Respiratory Failure |
- | 3.0 [1.3–6.9] (5; 6) | 0.9 [0.3–3.4] (2; 2.3) | 4.0 [1.8–8.6] (6; 11.5) | 1.7 [0.1–9.7] (1; 11.1) | - | 1.6 [0.9–2.6] (14; 4) |
| Pancreatic or Hepatic | 0.5 [0.0-2.8] (1; 1.2) | 1.8 [0.6–5.2] (3; 3.6) | 0.5 [0.0-2.7] (1; 1.1) | 0.7 [0.0-3.7] (1; 1.9) | - | - | 0.7 [0.3–1.5] (6; 1.7) |
| Intestinal Occlusion | 0.5 [0.0-2.8] (1; 1.2) | 8.3 [4.9–13.8] (14; 16.7) | 0.5 [0.0-2.7] (1; 1.1) | - | - | - | 1.8 [1.1–2.9] (16; 4.6) |
| Hemorrage | 4.4 [2.3–8.4] (9; 10.6) | 7.7 [4.5–13.1] (13; 15.5) | 1.9 [0.7–4.8] (4; 4.5) | 5.3 [2.7–10.4] (8; 15.4) | 1.7 [0.1–9.7] (1; 11.1) | 6.5 [3.2–13.4] (7; 22.6) | 4.7 [3.4–6.3] (42; 12) |
| AKI | 1.5 [0.5–4.3] (3; 3.5) | 2.4 [0.9–6.1] (4; 4.8) | 0.9 [0.3–3.4] (2; 2.3) | - | - | 0.9 [0.0-5.3] (1; 3.2) | 1.1 [0.6-2.0] (10; 2.9) |
| Wound Rupture | - | 1.8 [0.6–5.2] (3; 3.6) | 0.9 [0.3–3.4] (2; 2.3) | 1.3 [0.4–4.8] (2; 3.8) | 5.2 [1.8–15.0] (3; 33.3) | - | 1.1 [0.6-2.0] (10; 2.9) |
| Other | 9.3 [6.0-14.5] (19; 22.4) | 8.9 [5.4–14.6] (15; 17.9) | 5.2 [2.9–9.2] (11; 12.5) | 8.6 [5.0-14.7] (13; 25) | 1.7 [0.1–9.7] (1; 11.1) | 6.5 [3.2–13.4] (7; 22.6) | 7.3 [5.8–9.3] (66; 18.9) |
| Total | 41.6 [33.8–51.2] (85) | 49.7 [40.3–61.1] (84) | 41.4 [33.7–50.7] (88) | 34.5 [26.4–44.9] (52) | 15.5 [8.2–29.1] (9) | 28.9 [20.5–40.8] (31) | 38.7 [34.9–42.9] (349) |
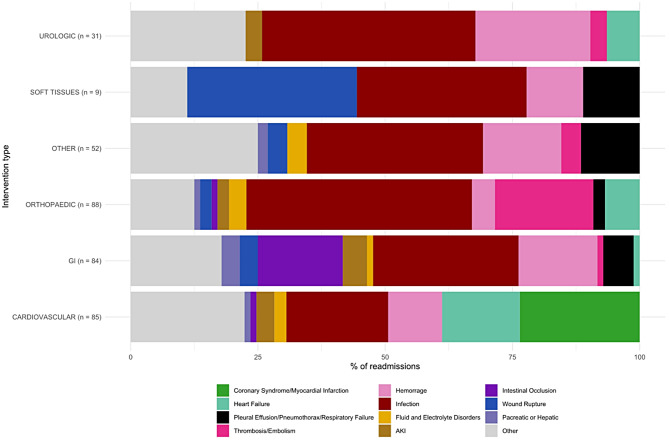
Figure 1 shows that the most frequent reasons for readmission after cardiovascular surgery include coronary syndrome/myocardial infarction (23.5%), and heart failure (15.2%). Other significant contributors are infection (20.0%), and hemorrhage (10.5%). In GI surgery, infection and intestinal occlusion are the primary reasons for readmission, accounting for a large proportion of cases (28.6% and 16.7%, respectively), followed by hemorrage (15.4%). For orthopedic surgery, infections (44%), Thrombosis/embolism (19.3%) and heart failure (6.8%) are the main causes of readmission. In skin-soft tissue surgery, infections account for 33.3% of readmissions, as well as wound ruptures. For urologic surgery, infections are the primary reason for readmission (41.9%), while hemorrhage accounts for 22.5%. For the other surgeries, a substantial proportion of readmissions are attributed to infection (34.6%), hemorrage (15.4%), and respiratory complications (11.5%).
Fig. 1.
Most frequent reasons for readmission by type of surgery
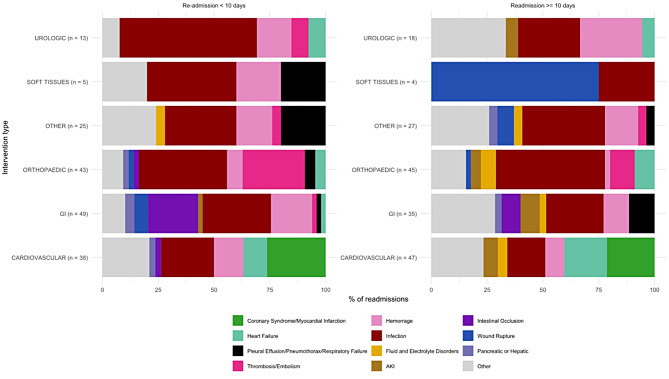
As in Fig. 2, fluid and electrolyte disorders tend to appear after more than 10 days, as well as acute kidney injury, and their combined frequency exceeds 5% in orthopedic surgery, GI surgery and cardiovascular surgery. Infections are common both in the first 10 days and after 10 days, but tend to be more frequent in the first days, except for orthopedic surgery where 48.9% of readmissions after 10 days were for infection, compared to only 39.5% before 10 days. Wound rupture is more frequent after 10 days for skin-soft tissue surgery, after which 3 / 4 of readmissions between 10 and 30 days are for this main reason. Thrombosis also tends to be more common in the first days following orthopedic surgery (27.9%) and then declines in frequency after 10 days (11.1%). Intestinal occlusion after gastro-intestinal surgery is also more common in the first 10 days after discharge (22.4% vs. 8.6%).
Fig. 2.
Time effect on type of readmission
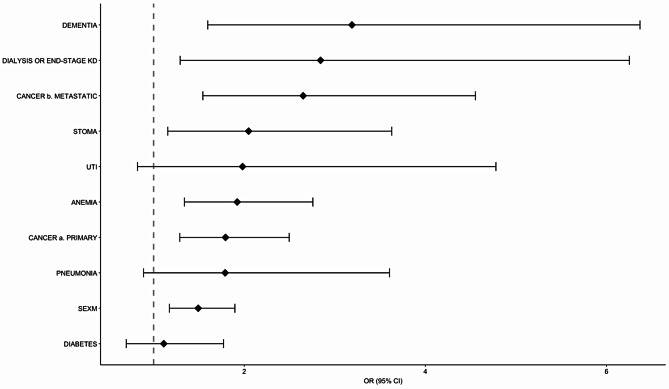
Figure 3 shows that, after correcting for type of intervention and age of patient, dementia [OR = 3.19; CI 1.60–6.37], dialysis or end-stage kidney disease [OR = 2.84; CI 1.29–6.25], and metastatic cancer [OR = 2.65; CI 1.54–4.55] are significantly associated with higher odds of readmission. Patients with stomas also exhibit a significantly higher risk of readmission [OR = 2.05; CI 1.16–3.63], as do those with anemia [OR = 1.92; CI 1.34–2.76] and primary cancer [OR = 1.79; 1.29–2.50]. Males are also at greater risk of readmission [OR = 1.49; CI 1.17–1.90].
Fig. 3.
Multiple mixed-effects logistic regression; DV = Readmission yes/no. Odds Ratios and 95% CI of readmission. Adjusted for gender, age, intervention type, hospital (random effect)
Discussion
We found an overall rate of readmission of 3.9% [CI 3.5–4.3%], highest after GI surgery and lowest after skin-soft tissue surgery. The most important risk factors for readmission were dementia, CKD or dialysis, metastatic or primary cancer, presence of a stoma and anemia. Male gender and age were also associated with a higher risk of readmission. Our data also showed that the most common reason for readmission was infection for all types of surgery. Readmissions for haemorrhage or hematoma were also relatively common, especially GI and skin-soft tissue surgery. Venous Thromboemolism (VTE) requiring readmission was relatively frequent after orthopedic surgery and, to a lesser extent, urologic and general surgery. Intestinal occlusion or post-operative ileus were more frequent after general surgery while wound complications, excluded infections, were a common reason for readmission, especially after skin-soft tissue surgery - mainly breast surgery. Coronary syndromes and heart failure were more common after cardiovascular interventions.
The overall rate of readmission in our sample was lower than expected from international literature which reports overall 30-day readmission rates of 11–13% [2, 11, 12], and unplanned readmission rate of 5.7% [13]. However, rates differ by surgical specialty and specific intervention, approach or priority (elective or urgent) [13–29].
Literature has identified numerous risk factors for readmission, depending on surgical specialty and specific intervention. According to Gani et al., the majority of the variation in readmission was attributable to patient-related factors (82.8%) while surgical subspecialty accounted for 14.5% of the variability, and individual surgeon-level factors accounted for 2.8% [6].
Age and male gender were associated to readmission rates in our sample. While age is consistently associated with increased risk in all types of surgery, literature is not consistent on the effect of sex on readmission rate, depending on surgery types [27, 30–32]. Dementia was strongly associated with readmission in our sample. Khan et al., focusing on hip fracture surgery, found that neurological disorders as the strongest predictors for readmission [14]. Geriatric conditions are associated with adverse surgical outcomes; thus, a comprehensive evaluation of treatment goals and communication of realistic risk estimates are essential to guide individualized decision making [33]. Anemia was another independent predictor of readmission according to our data. In vascular surgery, chronic anemia was found to be a risk factor for readmission with infection [34]. For orthopedic patients, bleeding disorder and low pre-operative hematocrit were each independently associated with readmissions risk [15]. Patients with metastatic cancer are also at higher risk of readmission, both according to our study and to international literature [32, 35]. Literature also agrees on the fact that renal disease (CKD) or dialysis are predictors of readmission in cardiac surgery [29, 31], vascular surgery [27], general surgery [24], and both elective and urgent [15] orthopedic surgery [20].
In terms of causes of readmission, our findings on infection being the most common is confirmed by literature [34, 36–38]. Woelber et al. [39] found that the overall proportion of surgical procedures leading to surgical site infection was 10%, of which 60% appeared after discharge. Readmissions for infection are of particular concern and mainly include surgical site infections, sepsis, pneumonia, and urinary tract infection [15]. Efforts to identify best therapeutical options (surgical approach, antimicrobial prophylaxis, wound care, rehabilitation, prognostic scores, patient education) to avoid infectious complications after surgical interventions are very common in literature [40–46].
Hemorrage was also relatively common as cause of readmission in our hospitals. Morris et al. report that in orthopedic, general and vascular surgery, bleeding accounted on average for 5% of readmissions [2]. Bleeding may also occur after ENT surgery, as confirmed by literature [47]. VTE was the second cause of readmission after orthopedic surgery in our area, with some cases occurring after urologic surgery and general surgery. According to literature, VTE occurs in a spectrum of severity ranging from an incidental finding to serious readmission-requiring events [48]. In the US, after orthopedic surgery, the most common reason for readmission after surgical site complication was thromboembolism [49, 50]. Schmid et al. investigated the causes of readmission after urologic interventions and found that VTE was the most common causes of readmission after radical prostatectomy [26]. 30-day incidence of VTE after cancer-related surgery are around 0.5-2% [51–54], which is consistent with our findings for general surgery.
Ileus paraliticus was a major player for readmission after GI surgery in our patients. Incidence of ileus varies according to specific intervention, approach (laparotomic, laparoscopic, robot-assisted) [55], and even side of intervention [56], and the extent of the resection [57]. According to Merkow et al., obstruction or ileus was the second most common reason for readmission (10.3%), especially after gastrointestinal and gynecological procedures [13]. We observed rarer cases of intestinal complications after orthopedic surgery, consistent with what is reported in literature [58].
Literature also confirms our findings for local non-infectious complications, which are more common as main causes of readmission after skin-soft tissue surgery: breast cancer surgery is generally associated with low rates of surgical morbidity with postoperative complications often regarding local complications such as seroma, infection, hematoma, mastectomy flap necrosis, wound dehiscence [59]. As in our findings, local issues such as wound and prosthetic complications are reported in literature for orthopedic surgery [15, 60] and less frequently for general surgery [24, 61, 62].
Conclusions
Our findings highlight that surgical readmissions are often driven by patient-related factors such as comorbidities (e.g., dementia, CKD, cancer, anemia) which expose to common post-operative complications like infection, bleeding, VTE, and ileus.
The effort to reduce readmissions after surgery should be threefold: firstly, healthcare policy should address modifiable risk factors at population level since it is established by literature that patient-level factors contribute most to readmission [4]. At hospital level, we should analyse patient’s risk factors (even before the procedure is performed, if planned) to address specific needs and be sure the patient has the appropriate care when discharged.
Secondly, we should focus on enriching post-discharge transitional care [2]. Early post-discharge follow-up visits and follow up with primary care (nurse, GP and other healthcare operators as needed) may reduce readmission rate. Surgical units should verify that patients have a support network for post-discharge care. If not, they should coordinate with primary care and social services in advance to arrange a protected discharge plan. This plan could involve home care or temporary residential care with rehabilitation options, as needed.
Finally, addressing the single causes of readmission is essential. For example, in the case of infections, it is important to ensure that the patient is discharged with the appropriate antibiotic therapy, easy to administer, and that the patient is able to recognize the signs of infection and to contact the healthcare provider in case of need. In case of orthopedic surgery, it is important to ensure that the patient is able to recognize the signs of thrombosis, but also that anticoagulation therapy is provided at discharge at least to cover the immediate post-discharge days.
Strengths and limits
The major limit of the study is the use of administrative datasets which may not be as accurate as clinical data. However, this is also the strength of the study, which makes the attempt to use available data to drive healthcare policy.
Author contributions
G.S. performed statistical analysis and wrote the results, prepared tables and figures. A.B. conceptualized the research and statistical methods, and wrote the introduction and discussion. M.M. and M.F. helped with the developement of the research question, worked for approval from ethical committee and reviewed the manuscript. G.A., P.C. and L.R. contributed to reviewing the results and writing introduction and discussion.
Funding
Funding was obtained from the project Prin_Progetti di Ricerca di Rilevante Interesse Nazionale - Bando 2020, Prot. 2020KHSSKE SOcial and health Frailty as determinants of Inequality in Aging. (SOFIA), by IRCSS San Camillo.
Data availability
The data supporting the findings of this study are held by the Marca Trevigiana Local Health Authority and were used under license for the present work, but they are not publicly available. These data are nonetheless available from the corresponding author on reasonable request and subject to permission being obtained by the Authority.
Declarations
Ethical approval
The dataset was pseudo-anonymized before analysis. The study protocol was approved by the competent ethics committee for the area (Prot. N. 0022516/24; 07/11/2024).
Consent to participate
Requirement for informed consent to participate has been waived by the relevant Ethics Committee (impracticable to obtain).
Consent for publication
Not applicable. The submission does not contain any data from an individual person.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Morris MS, Graham LA, Richman JS, Hollis RH, Jones CE, Wahl T, et al. Postoperative 30-day readmission: time to focus on what happens outside the hospital. Ann Surg. 2016;264:621–31. 10.1097/SLA.0000000000001855. [DOI] [PubMed] [Google Scholar]
- 3.Weller WE, Rosati C, Hannan EL. Relationship between surgeon and hospital volume and readmission after bariatric operation. J Am Coll Surg. 2007;204:383–91. 10.1016/j.jamcollsurg.2006.12.031. [DOI] [PubMed] [Google Scholar]
- 4.W T, H M. How to predict 30-Day readmission. Adv Surg. 2018;52. 10.1016/j.yasu.2018.03.015. [DOI] [PubMed]
- 5.Mary A. Prevention of 30-Day readmission after coronary artery bypass surgery. Home Healthc now. 2017;35:326–34. 10.1097/NHH.0000000000000555. [DOI] [PubMed] [Google Scholar]
- 6.Gani F, Lucas DJ, Kim Y, Schneider EB, Pawlik TM. Understanding variation in 30-Day surgical readmission in the era of accountable care: effect of the patient, surgeon, and surgical subspecialties. JAMA Surg. 2015;150:1042–9. 10.1001/jamasurg.2015.2215. [DOI] [PubMed] [Google Scholar]
- 7.Zhao R, Cheng L, Zheng Q, Lv Y, Wang Y-M, Ni M, et al. A smartphone application-based remote rehabilitation system for post-total knee arthroplasty rehabilitation: A randomized controlled trial. J Arthroplast. 2024;39:575–e5818. 10.1016/j.arth.2023.08.019. [DOI] [PubMed] [Google Scholar]
- 8.Chiang Y-W, Chang Y-J, Huang H-J, Hsieh C-P, Lu Y-H. Does post acute care reduce the mortality of octogenarian and nonagenarian patients undergoing hip fracture surgery? BMC Geriatr. 2024;24:322. 10.1186/s12877-024-04936-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296. 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salute M. della. Manuale ICD-9-CM versione italiana 2007 n.d.
- 11.Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med. 2013;369:1134–42. 10.1056/NEJMsa1303118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Postel M, Frank PN, Barry T, Satou N, Shemin R, Benharash P. The cost of preventing readmissions: why surgeons should lead the effort. Am Surg. 2014;80:1003–6. [PubMed] [Google Scholar]
- 13.Merkow RP, Ju MH, Chung JW, Hall BL, Cohen ME, Williams MV, et al. Underlying reasons associated with hospital readmission following surgery in the united States. JAMA. 2015;313:483–95. 10.1001/jama.2014.18614. [DOI] [PubMed] [Google Scholar]
- 14.Khan MA, Hossain FS, Dashti Z, Muthukumar N. Causes and predictors of early re-admission after surgery for a fracture of the hip. J Bone Joint Surg Br Volume. 2012;94:690–7. 10.1302/0301-620X.94B5.28933. [DOI] [PubMed] [Google Scholar]
- 15.Martin CT, Gao Y, Pugely AJ. Incidence and risk factors for 30-Day readmissions after hip fracture surgery. Iowa Orthop J. 2016;36:155–60. [PMC free article] [PubMed] [Google Scholar]
- 16.Paxton EW, Inacio MCS, Singh JA, Love R, Bini SA, Namba RS. Are there modifiable risk factors for hospital readmission after total hip arthroplasty in a US healthcare system?? Clin Orthop Relat Res. 2015;473:3446–55. 10.1007/s11999-015-4278-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doumouras AG, Saleh F, Hong D. 30-Day readmission after bariatric surgery in a publicly funded regionalized center of excellence system. Surg Endosc. 2016;30:2066–72. 10.1007/s00464-015-4455-8. [DOI] [PubMed] [Google Scholar]
- 18.McNeely C, Markwell S, Vassileva CM. Readmission after inpatient percutaneous coronary intervention in the medicare population from 2000 to 2012. Am Heart J. 2016;179:195–203. 10.1016/j.ahj.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 19.Shah SP, Xu T, Hooker CM, Hulbert A, Battafarano RJ, Brock MV, et al. Why are patients being readmitted after surgery for esophageal cancer? J Thorac Cardiovasc Surg. 2015;149. 10.1016/j.jtcvs.2015.01.064. [DOI] [PubMed]
- 20.Chen J, Zhang F, Liu C-Y, Yuan Q-M, Di X-S, Long S-W, et al. Impact of chronic kidney disease on outcomes after total joint arthroplasty: a meta-analysis and systematic review. Int Orthop. 2020;44:215–29. 10.1007/s00264-019-04437-4. [DOI] [PubMed] [Google Scholar]
- 21.Poupore AK, Stem M, Molena D, Lidor AO. Incidence, reasons, and risk factors for readmission after surgery for benign distal esophageal disease. Surgery. 2016;160:599–606. 10.1016/j.surg.2016.04.037. [DOI] [PubMed] [Google Scholar]
- 22.Kerwel TG, Leichtle SW, Asgeirsson T, Hendren SK, Cleary RK, Luchtefeld MA. Risk factors for readmission after elective colectomy: postoperative complications are more important than patient and operative factors. Dis Colon Rectum. 2014;57:98–104. 10.1097/DCR.0000000000000007. [DOI] [PubMed] [Google Scholar]
- 23.Al-Mazrou AM, Suradkar K, Mauro CM, Kiran RP. Characterization of readmission by day of rehospitalization after colorectal surgery. Dis Colon Rectum. 2017;60:202–12. 10.1097/DCR.0000000000000734. [DOI] [PubMed] [Google Scholar]
- 24.Van Butsele J, Bislenghi G, D’Hoore A, Wolthuis AM. Readmission after rectal resection in the ERAS-era: is a loop ileostomy the Achilles heel? BMC Surg. 2021;21:267. 10.1186/s12893-021-01242-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dan Z, YiNan D, ZengXi Y, XiChen W, JieBin P, LanNing Y. Thirty-Day readmission after radical gastrectomy for gastric cancer: A Meta-analysis. J Surg Res. 2019;243:180–8. 10.1016/j.jss.2019.04.076. [DOI] [PubMed] [Google Scholar]
- 26.Schmid M, Chiang HA, Sood A, Campbell L, Chun FK-H, Dalela D, et al. Causes of hospital readmissions after urologic cancer surgery. Urol Oncol. 2016;34:e2361–11. 10.1016/j.urolonc.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 27.Smith SL, Matthews EO, Moxon JV, Golledge J. A systematic review and meta-analysis of risk factors for and incidence of 30-day readmission after revascularization for peripheral artery disease. J Vasc Surg. 2019;70:996–e10067. 10.1016/j.jvs.2019.01.079. [DOI] [PubMed] [Google Scholar]
- 28.Benuzillo J, Caine W, Evans RS, Roberts C, Lappe D, Doty J. Predicting readmission risk shortly after admission for CABG surgery. J Card Surg. 2018;33:163–70. 10.1111/jocs.13565. [DOI] [PubMed] [Google Scholar]
- 29.Kwok CS, Chatterjee S, Bagur R, Sharma K, Alraies MC, Fischman D, et al. Multiple unplanned readmissions after discharge for an admission with percutaneous coronary intervention. Catheterization Cardiovasc Interventions: Official J Soc Cardiac Angiography Interventions. 2021;97:395–408. 10.1002/ccd.28797. [DOI] [PubMed] [Google Scholar]
- 30.Koechlin L, Miazza J, Gahl B, Santer D, Vöhringer L, Berdajs D, et al. Sex differences in readmission rate after cardiac surgery. Front Cardiovasc Med. 2023;10:1273785. 10.3389/fcvm.2023.1273785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sabe SA, Sabe MA, Kennedy KF, Sellke FW, Ehsan A. Risk factors for heart failure readmission after cardiac surgery. JACC Adv. 2023;2:100599. 10.1016/j.jacadv.2023.100599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alyabsi MS, Alqarni AH, Almutairi LM, Algarni MA, Alshammari KM, Almutairi A, et al. The 30-day hospital readmission and mortality after surgery in colorectal cancer patients. BMC Gastroenterol. 2022;22:434. 10.1186/s12876-022-02516-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oresanya LB, Lyons WL, Finlayson E. Preoperative assessment of the older patient: a narrative review. JAMA. 2014;311:2110–20. 10.1001/jama.2014.4573. [DOI] [PubMed] [Google Scholar]
- 34.Melvin JC, Smith JB, Kruse RL, Vogel TR. Risk factors for 30-Day hospital Re-Admission with an infectious complication after Lower-Extremity vascular procedures. Surg Infect. 2017;18:319–26. 10.1089/sur.2016.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu W, Wells CI, McGuinness M, Varghese C, Keane C, Liu C, et al. Characterising nationwide reasons for unplanned hospital readmission after colorectal cancer surgery. Colorectal Disease: Official J Association Coloproctology Great Br Irel. 2023;25:861–71. 10.1111/codi.16467. [DOI] [PubMed] [Google Scholar]
- 36.Hahnel J, Burdekin H, Anand S. Re-admissions following hip fracture surgery. Ann R Coll Surg Engl. 2009;91:591–5. 10.1308/003588409X432374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palubicka A, Jaworski R, Wekwejt M, Swieczko-Zurek B, Pikula M, Jaskiewicz J, et al. Surgical site infection after breast surgery: A retrospective analysis of 5-Year postoperative data from a single center in Poland. Med (Kaunas Lithuania). 2019;55:512. 10.3390/medicina55090512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Olsen MA, Nickel KB, Fox IK, Margenthaler JA, Ball KE, Mines D, et al. Infect Control Hosp Epidemiol. 2015;36:907–14. 10.1017/ice.2015.108. Incidence of Surgical Site Infection Following Mastectomy With and Without Immediate Reconstruction Using Private Insurer Claims Data. [DOI] [PMC free article] [PubMed]
- 39.Woelber E, Schrick EJ, Gessner BD, Evans HL. Proportion of surgical site infections occurring after hospital discharge: A systematic review. Surg Infect. 2016;17:510–9. 10.1089/sur.2015.241. [DOI] [PubMed] [Google Scholar]
- 40.de Wijkerslooth EML, Boerma E-JG, van Rossem CC, van Rosmalen J, Baeten CIM, Beverdam FH, et al. 2 days versus 5 days of postoperative antibiotics for complex appendicitis: a pragmatic, open-label, multicentre, non-inferiority randomised trial. Lancet (London England). 2023;401:366–76. 10.1016/S0140-6736(22)02588-0. [DOI] [PubMed] [Google Scholar]
- 41.Smith S, Abuhassanian I, Attia J, Carroll R, Lott N, Hampton J, et al. Antiseptic skin agents to prevent surgical site infection after clean implant surgery: subgroup analysis of the NEWSkin Prep trial. Surg Infect. 2023;24:818–22. 10.1089/sur.2023.250. [DOI] [PubMed] [Google Scholar]
- 42.Edmiston CE, Leaper DJ. Prevention of orthopedic prosthetic infections using Evidence-Based surgical site infection care bundles: A narrative review. Surg Infect. 2022;23:645–55. 10.1089/sur.2022.146. [DOI] [PubMed] [Google Scholar]
- 43.Wang L-H, Fang F, Lu C-M, Wang D-R, Li P, Fu P. Safety of fast-track rehabilitation after Gastrointestinal surgery: systematic review and meta-analysis. World J Gastroenterol. 2014;20:15423–39. 10.3748/wjg.v20.i41.15423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson RB, Farooque Y. Risks and prevention of surgical site infection after hernia mesh repair and the predictive utility of ACS-NSQIP. J Gastrointest Surgery: Official J Soc Surg Aliment Tract. 2022;26:950–64. 10.1007/s11605-022-05248-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grummet JP, Weerakoon M, Huang S, Lawrentschuk N, Frydenberg M, Moon DA, et al. Sepsis and ’superbugs’: should we favour the transperineal over the transrectal approach for prostate biopsy? BJU Int. 2014;114:384–8. 10.1111/bju.12536. [DOI] [PubMed] [Google Scholar]
- 46.Gillespie BM, Thalib L, Harbeck E, Tobiano G, Kang E, Tobiano S, et al. Effectiveness of discharge education for patients undergoing general surgery: A systematic review and meta-analysis. Int J Nurs Stud. 2023;140:104471. 10.1016/j.ijnurstu.2023.104471. [DOI] [PubMed] [Google Scholar]
- 47.Østvoll E, Sunnergren O, Stalfors J. Increasing readmission rates for hemorrhage after tonsil surgery: A longitudinal (26 Years) National study. Otolaryngology–Head and neck surgery. Official J Am Acad Otolaryngology-Head Neck Surg. 2018;158:167–76. 10.1177/0194599817725680. [DOI] [PubMed] [Google Scholar]
- 48.Rhoads C, Emara AK, Pumo T, Pan X, Zhou G, Koroukian S, et al. What are the drivers of readmission for serious venous thromboembolic events after primary total knee arthroplasty?? An analysis of 862,915 patients. J Knee Surg. 2023;36:1141–9. 10.1055/s-0042-1750063. [DOI] [PubMed] [Google Scholar]
- 49.Minhas SV, Kester BS, Lovecchio FC, Bosco JA. Nationwide 30-Day readmissions after elective orthopedic surgery: reasons and implications. J Healthc Quality: Official Publication Natl Association Healthc Qual. 2017;39:34–42. 10.1097/JHQ.0000000000000045. [DOI] [PubMed] [Google Scholar]
- 50.Metoxen AJ, Ferreira AC, Zhang TS, Harrington MA, Halawi MJ. Hospital readmissions after total joint arthroplasty: an updated analysis and implications for Value-Based care. J Arthroplast. 2023;38:431–6. 10.1016/j.arth.2022.09.015. [DOI] [PubMed] [Google Scholar]
- 51.Mallick S, Aiken T, Varley P, Abbott D, Tzeng C-W, Weber S, et al. Readmissions from venous thromboembolism after complex Cancer surgery. JAMA Surg. 2022;157:312–20. 10.1001/jamasurg.2021.7126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jarvis CA, Bonney PA, Ding L, Tang AM, Giannotta SL, Kim AW, et al. Readmission with venous thromboembolism after surgical treatment by primary cancer site. Surg Oncol. 2020;35:268–75. 10.1016/j.suronc.2020.09.013. [DOI] [PubMed] [Google Scholar]
- 53.DeWane MP, Davis KA, Schuster KM, Maung AA, Becher RD. Venous Thromboembolism-Related readmission in emergency general surgery patients: A role for prophylaxis on discharge?? J Am Coll Surg. 2018;226:1072–e10773. 10.1016/j.jamcollsurg.2018.03.021. [DOI] [PubMed] [Google Scholar]
- 54.Schlick CJR, Liu JY, Yang AD, Bentrem DJ, Bilimoria KY, Merkow RP, Pre-Operative. Intra-Operative, and Post-Operative factors associated with Post-Discharge venous thromboembolism following colorectal Cancer resection. J Gastrointest Surgery: Official J Soc Surg Aliment Tract. 2020;24:144–54. 10.1007/s11605-019-04354-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gómez Ruiz M, Espin-Basany E, Spinelli A, Cagigas Fernández C, Bollo Rodriguez J, María Enriquez Navascués J, et al. Early outcomes from the minimally invasive right colectomy anastomosis study (MIRCAST). Br J Surg. 2023;110:1153–60. 10.1093/bjs/znad077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Grass F, Lovely JK, Crippa J, Ansell J, Hübner M, Mathis KL, et al. Comparison of recovery and outcome after left and right colectomy. Colorectal Disease: Official J Association Coloproctology Great Br Irel. 2019;21:481–6. 10.1111/codi.14543. [DOI] [PubMed] [Google Scholar]
- 57.Emile SH, Horesh N, Garoufalia Z, Gefen R, Zhou P, Dasilva G, et al. Predictors and impact of ileus on outcomes after laparoscopic right colectomy: A Case-Control study. Am Surg. 2024;90:3054–60. 10.1177/00031348241260275. [DOI] [PubMed] [Google Scholar]
- 58.Klasan A, Putnis SE, Heyse TJ, Madzarac G, Gotterbarm T, Neri T, Ileus. Gastrointestinal bleeding and Clostridium difficile colitis after hip and knee Replacement - a systematic review. Surg Technol Int. 2020;37:377–84. [PubMed] [Google Scholar]
- 59.Al-Hilli Z, Wilkerson A. Breast surgery: management of postoperative complications following operations for breast Cancer. Surg Clin North Am. 2021;101:845–63. 10.1016/j.suc.2021.06.014. [DOI] [PubMed] [Google Scholar]
- 60.Bovonratwet P, Chen AZ, Shen TS, Ondeck NT, Islam W, Ast MP, et al. What are the reasons and risk factors for 30-Day readmission after outpatient total hip arthroplasty?? J Arthroplast. 2021;36:S258–63. 10.1016/j.arth.2020.10.011..e1. [DOI] [PubMed] [Google Scholar]
- 61.Jensen KK, Oma E, van Ramshorst GH, Nordholm-Carstensen A, Krarup P-M. Abdominal wound dehiscence is dangerous: a nationwide study of 14,169 patients undergoing elective open resection for colonic cancer. Hernia: J Hernias Abdom Wall Surg. 2022;26:75–86. 10.1007/s10029-020-02350-z. [DOI] [PubMed] [Google Scholar]
- 62.Kenig J, Richter P, Lasek A, Zbierska K, Zurawska S. The efficacy of risk scores for predicting abdominal wound dehiscence: a case-controlled validation study. BMC Surg. 2014;14:65. 10.1186/1471-2482-14-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Olsen MA, Nickel KB, Fox IK, Margenthaler JA, Ball KE, Mines D, et al. Infect Control Hosp Epidemiol. 2015;36:907–14. 10.1017/ice.2015.108. Incidence of Surgical Site Infection Following Mastectomy With and Without Immediate Reconstruction Using Private Insurer Claims Data. [DOI] [PMC free article] [PubMed]
Data Availability Statement
The data supporting the findings of this study are held by the Marca Trevigiana Local Health Authority and were used under license for the present work, but they are not publicly available. These data are nonetheless available from the corresponding author on reasonable request and subject to permission being obtained by the Authority.