Abstract
Introduction
Data-Driven Decision Making (DDDM) plays a pivotal role in healthcare, specifically patient management. This review aims to provide a comprehensive understanding of the technologies used in DDDM and provide a framework of how DDDM is involved in patient management.
Methodology
This study follows the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) framework, studies from Web of Science, Pubmed, and Embase are screened for consideration. The inclusion criteria are outlined to identify studies on patient management utilizing DDDM.
Result
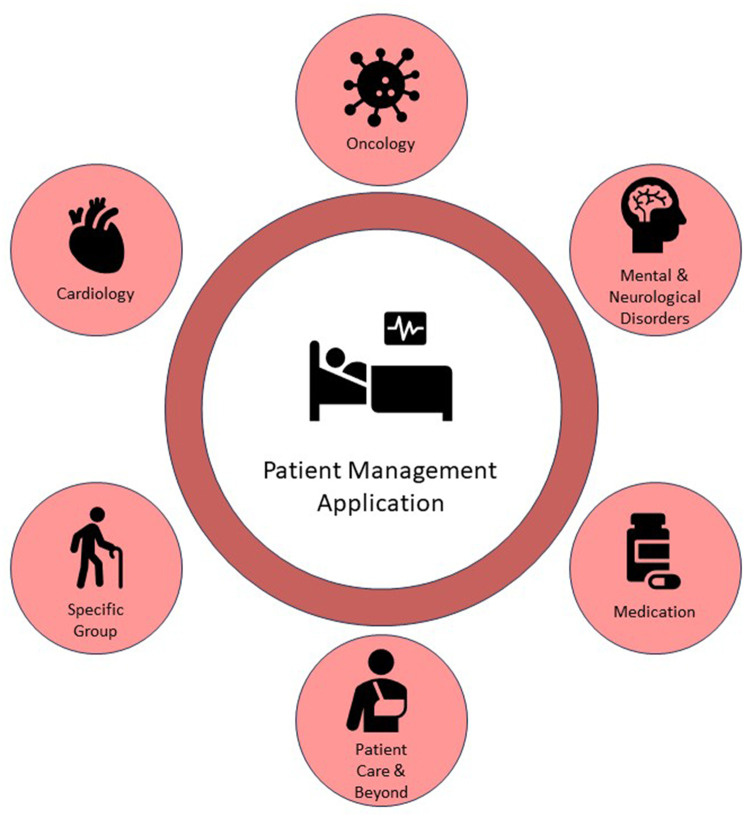
The studies included in the review explore DDDM in patient management from data-driven approaches to decision making methods. In the former, artificial intelligence, together with other methods, is the dominant method utilized. As a comparison, the decision support system, Markov decision process, and shared decision making are exploited in the latter. Disease diagnosis and treatment was the most common area of patient management application along with precision medicine, patient care, nursing, and other related fields of patient management. A framework of how DDDM is involved in patient management was identified.
Conclusion
While challenges such as data quality and interpretability exist, advantages of DDDM lie in unprecedented personalization, streamlined decision-making, and the potential for a future where technology complements healthcare expertise for more effective and patient-centered care. DDDM is not only a useful option for patient management but also to many other aspects of healthcare and the systems around healthcare.
Keywords: Data-driven decision making, Patient management, Deep learning, Oncology, Precision medicine
Introduction
Data-Driven Decision Making (DDDM) is a revolution in itself that has touched almost all the domains of life such as economy, industry, and medical science. Growing numbers of organizations are applying DDDM to tackle complex issues, make critical decisions, and enhance performance [1], In finance, retail, and technology, the integration of data-driven approaches increases operational efficiency, enhances customer value, and fosters innovation [2] The effectiveness of DDDM is central to its ability to gather and analyze large datasets to obtain useful information that can be used to make strategic decisions and enhance adaptability.
The consequences of DDDM are most important in the healthcare sector. Formerly, the management of complexity, variability, and limited standardization were major challenges to traditional healthcare management approaches. Many of these models are inadequate for the management of the patient’s holistic needs, resulting in time wastage and suboptimal results [3] In response, healthcare is slowly but steadily being transformed by technological advancement, big data analysis, and the growing need for effective and sensitive healthcare.
DDDM is bringing about a change in the way that patients are handled, moving away from generic and often reactive care to one that is more specific, timely, and patient-focused. Healthcare professionals can now take a holistic view of the patient with the help of digital information such as EHRs, patient input, genomic data, and telemetry to provide highly specific treatments. For example, Reinforcement Learning (RL), a form of artificial intelligence, has been used effectively in the dynamic modeling of dosing kinetics for antiarrhythmic drugs and thus an improvement in patient-specific treatments [4] In the same manner, the combination of RL with the clustering method was used to personalize the management of diabetes by properly suggesting the most suitable treatment options for every patient based on their specific characteristics [5].
Other technologies, such as deep learning have also greatly enhanced the diagnostic speed and treatment results. For instance, neural network-based deep learning models have assisted in enhancing the clinical decision-making process by providing an efficient analysis of the EHRs data which has resulted in improved accuracy of patient diagnosis [6] Furthermore, Random Forest models, which are another form of machine learning, have been used effectively in orthopedic surgery to predict post-operative patient recovery and outcomes, which helps clinicians manage patient care actively [7].
The advantages of DDDM are wide-ranging and applicable to most fields of healthcare. This paper presents how predictive analytics enabled by DDDM has enhanced the patient risk classification for heart failure and enhanced the chances of reducing hospital readmission in cardiology [8] In the field of neurological and mental health, DDDM has helped in precise predictive modeling to help clinicians to determine the probability of a decline in the quality of life of patients with traumatic brain injury and in the utilization of therapeutic resources [9] Moreover, DDDM has improved nursing practice. Prediction models developed with the help of data help the nurses identify the patients who are at risk of developing complications and thus help in the effective allocation of resources and development of better care plans to ensure that the patient receives optimal care.
This structured review aims to provide a comprehensive understanding of the most up-to-date methodologies driving the evolution of DDDM in the healthcare landscape. Providing a new framework of how DDDM is involved in patient management. As the review unfolds, it illuminates the transformative potential of DDDM and its pivotal role in shaping the future of patient management. The rest of this paper is organized as follows. Section II demonstrates the methodology of the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) framework utilized in this review. Section III displays the results collected in Sect. II and analyzes them into different categories based on the DDDM methodology utilized and the patient management filed of application. Section V Summarized the content discussed in previous sections and provided insights of future potentials of DDDM in patient management.
Methodology
Research design
The research design sets the foundation for this systematic review, which aims to explore the role and impact of data-driven decision making in patient care. In accordance with best practices in systematic review methodology, this study follows the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) framework. This framework ensures that the review is conducted in a systematic and transparent manner, enhancing its rigor and reliability. A systematic review is an established research method for synthesizing and summarizing existing literature on a specific topic. It involves a rigorous and structured process of searching, selecting, and analyzing relevant studies to answer well-defined research questions. In this case, the focus is on understanding how data-driven decision making influences patient care.
Data sources and search strategy
The credibility and comprehensiveness of this systematic review depend on the data sources and search strategy employed. To gather a rich and representative dataset, we conducted a comprehensive search of relevant literature from various sources.
The primary databases chosen for this systematic review include PubMed, Web of Science, and Embase. These databases were selected for their central role in the field of healthcare research and their reputation for providing a wealth of relevant research studies. In addition to the primary databases, the author considered outside literature sources and expert recommendations. This broader approach ensures that the review captures a wide spectrum of relevant studies, including those that might not be indexed in the primary databases.
Developing an effective search strategy was a critical aspect of this systematic review. It involved the use of a combination of relevant keywords and Boolean operators to create a search query that would yield a comprehensive and well-rounded selection of articles which is shown in Table 1 The search strategy includes terms related to data-driven decision making, patient care, healthcare, and related concepts. Furthermore, to maintain the relevance and currency of the data, the search is intentionally limited to articles published from 2013 to the present. This time frame ensures that the review focuses on the most recent studies, aligning with contemporary practices and technologies in healthcare. The initial search yields a substantial number of publications, totaling 4,149. The next steps in the systematic review process involve refining this initial set to ensure that only the most relevant and high-quality studies are included in the analysis. The authors made substantial efforts to include unpublished data and grey literature searches in order to minimize publication bias. The authors systematically searched repositories such as medRxiv, SSRN, and relevant conference proceedings to identify potentially relevant unpublished studies and preprints. All search procedures including those involving grey literature were documented in detail and this significantly reduced potential biases and enhanced the reproducibility and credibility of the systematic review findings.
Table 1.
Search query utilizing relevant keywords and boolean operators
| Web of science (3503) | PubMed (371) | Embase (275) |
|---|---|---|
| ((TS=(data-driven OR data-centered)) AND (TS=(patient management OR patient care OR diagnosis OR disease)) AND (TS=(decision making OR decision support system))) AND (PY=(2013–2023)) NOT DT = (EDITORIAL MATERIAL OR NOTE OR LETTER) | ((data-driven[MH]) OR (data-driven[TIAB]) OR (data centered[MH]) OR (data centered[TIAB])) AND ((patient management[MH]) OR (patient management[TIAB]) OR (patient care[TIAB]) OR (patient care[MH]) OR (diagnosis[MH]) OR (diagnosis[TIAB]) OR (disease[MH]) OR (disease[TIAB])) AND ((decision making[TIAB]) OR (decision making[MH]) OR (decision support system[MH]) OR (decision support system[TIAB])) AND (”2013”[DP]: “2023”[DP]) | (‘data-driven’:ti,ab,kw OR data centered:ti,ab,kw) AND (‘patient management’:ti,ab,kw OR ‘patient care’:ti,ab,kw OR ‘diagnosis’:ti,ab,kw OR disease:ti,ab,kw) AND (‘decision making’:ti,ab,kw OR ‘decision support system’:ti,ab,kw) AND [2013–2023]/py |
Inclusion vs. exclusion criteria
Inclusion and exclusion criteria serve as the guiding principles for selecting studies to be included in the systematic review. These criteria were developed collaboratively by the research team to ensure a clear and rigorous selection process. The criteria encompass various elements, including the types of studies, target populations, interventions, comparators, outcomes, and study designs. These are collectively known as the PICOS criteria and provide a structured approach to defining the scope of the review. PICOS framework used to define the inclusion and exclusion criteria for the study: Population (P): Patients from a variety of healthcare contexts. Intervention (I): The implementation of Data-Driven Decision Making techniques (such as artificial intelligence, machine learning, reinforcement learning, deep learning, decision support systems, Markov decision processes, and shared decision making) in the management of patients. Comparison (C): A comparator was not always necessary but where available, studies that compared data driven approaches to more conventional decision making approaches were of interest. Outcomes (O): Clinical outcomes, diagnostic accuracy, treatment efficacy, patient satisfaction, or any other measurable effects on the patient management process. Study Design (S): Both the qualitative and quantitative original research articles were considered for review. Review articles, editorials, letters and studies conducted in a language other than English were excluded. The reasons for these criteria were to limit the review to only strong empirical evidence of DDDM use in patient care in order to increase the relevance and usefulness of the findings.
The initial set of 4,149 publications is refined through a selection process led by the researcher. During this process, the researcher screens each article based on the criteria outlined above. The aim is to ensure that the final selection comprises studies that closely align with the research questions and objectives of the systematic review.
Selection process
Following the inclusion and exclusion criteria in Sect. 2.3, after removing 427 duplicate publications, 3722 publications are screened for consideration. 3602 publications excluded based on inclusion/exclusion criteria, and 120 publications are assessed for eligibility. 61 publications were removed as they are not closely relevant to patient management or DDDM, 5 publications from outside sources are relevant and added to the reference list, yielding a total of 64 publications included in the end. The selection process is shown in Fig. 1 An independent reviewer performed a systematic study selection and eligibility assessment to reduce selection bias and improve methodological rigor. The current study contains a defined approach to handle disagreements that emerge during study selection. The authors documented all unclear cases regarding the application of inclusion criteria before achieving consensus through multiple discussions. The consensus-based approach followed a structured process to achieve transparency while reducing bias and improving decision consistency and systematic review credibility.
Fig. 1.
PRISMA selection process
Data collection
A systematic approach to data collection is fundamental for maintaining consistency and accuracy in a systematic review. To facilitate this, the researcher develops a standardized data extraction form. This form serves as a structured tool for capturing essential data from the selected studies. The data extraction form is designed to cover critical aspects of each study, ensuring that no relevant information is overlooked. In the context of this review, it captures information related to data process methodology, decision-making methodology, and the contributions of data-driven decision making to patient care. These elements are at the core of the research questions and objectives.
Data extraction is a meticulous process that requires attention to detail. The researcher systematically goes through each selected study, extracting the necessary information, and recording it in the data extraction form. This step ensures that the review’s findings are based on accurate and comprehensive data from the selected studies, the extracted data of the publications is shown in Table 2.
Table 2.
Publications with methods applied
| Author & Year | Data-driven Method | Decision Making Contribution | Patient Management Field | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ML | RL | DL | RF | ODD | DS | MDP | SDM | PC | DDT | PM | |
| Ba et al. [10] | ✓ | ✓ | ✓ | ✓ | |||||||
| Bauer-Staeb et al. [11] | ✓ | ✓ | ✓ | ||||||||
| Bayati et al. [8] | ✓ | ✓ | |||||||||
| Bennett et al. [12] | ✓ | ✓ | ✓ | ||||||||
| Bizzo et al. [13] | ✓ | ✓ | ✓ | ||||||||
| Boloori et al. [14] | ✓ | ✓ | ✓ | ||||||||
| Brown et al. [15] | ✓ | ✓ | ✓ | ||||||||
| Buchlak et al. [16] | ✓ | ✓ | ✓ | ||||||||
| Bucholc et al. [17] | ✓ | ✓ | ✓ | ||||||||
| Buyer et al. [18] | ✓ | ✓ | |||||||||
| Casano et al. [19] | ✓ | ✓ | ✓ | ||||||||
| Castieira et al. [20] | ✓ | ✓ | ✓ | ||||||||
| Choi et al. [21] | ✓ | ✓ | ✓ | ||||||||
| Chuang et al. [22] | ✓ | ✓ | ✓ | ✓ | |||||||
| Comito et al. [6] | ✓ | ✓ | ✓ | ||||||||
| Divard et al. [23] | ✓ | ✓ | ✓ | ||||||||
| Escandell-Montero et al. [24] | ✓ | ✓ | ✓ | ||||||||
| Faller et al. [25] | ✓ | ✓ | ✓ | ||||||||
| Fischer et al. [26] | ✓ | ✓ | ✓ | ||||||||
| Fontana et al. [27] | ✓ | ✓ | ✓ | ✓ | |||||||
| Fu et al. [28] | ✓ | ✓ | |||||||||
| Gehrung et al. [29] | ✓ | ✓ | |||||||||
| Gultepe et al. [30] | ✓ | ✓ | ✓ | ||||||||
| Guo et al. [31] | ✓ | ✓ | |||||||||
| Hasimbegovic et al. [32] | ✓ | ✓ | |||||||||
| Hendriks et al. [33] | ✓ | ✓ | ✓ | ||||||||
| Heuvel et al. 2020 | ✓ | ✓ | ✓ | ✓ | |||||||
| Hu et al. [34] | ✓ | ✓ | ✓ | ||||||||
| Jafari-Marandi et al. [35] | ✓ | ✓ | ✓ | ||||||||
| Jayakumar et al. [36] | ✓ | ✓ | ✓ | ||||||||
| Kaur et al. [37] | ✓ | ✓ | ✓ | ||||||||
| Kharazmi et al. [38] | ✓ | ✓ | ✓ | ||||||||
| Klann et al. [39] | ✓ | ✓ | ✓ | ||||||||
| Kondylakis et al. [40] | ✓ | ✓ | ✓ | ||||||||
| Kriegova et al. [41] | ✓ | ✓ | ✓ | ||||||||
| Levy et al. [4] | ✓ | ✓ | |||||||||
| Li et al. [42] | ✓ | ✓ | ✓ | ||||||||
| Mannini et al. [43] | ✓ | ✓ | ✓ | ||||||||
| Müller et al. [44] | ✓ | ✓ | ✓ | ||||||||
| Nagamine et al. [45] | ✓ | ✓ | |||||||||
| Niraula et al. [46] | ✓ | ✓ | ✓ | ✓ | |||||||
| Oh et al. [5] | ✓ | ✓ | ✓ | ||||||||
| Park et al. [47] | ✓ | ✓ | ✓ | ||||||||
| Pinsky et al. [48] | ✓ | ✓ | ✓ | ||||||||
| Podell et al. [9] | ✓ | ✓ | ✓ | ||||||||
| Prasad et al. [49] | ✓ | ✓ | ✓ | ||||||||
| Raj et al. [50] | ✓ | ✓ | ✓ | ||||||||
| Saravi et al. [51] | ✓ | ✓ | ✓ | ||||||||
| Schell et al. [52] | ✓ | ✓ | ✓ | ||||||||
| Shapey et al. [53] | ✓ | ✓ | ✓ | ||||||||
| Shi et al. 2021 | ✓ | ✓ | |||||||||
| Singh et al. [54] | ✓ | ✓ | ✓ | ||||||||
| Stoitsas et al. [7] | ✓ | ✓ | ✓ | ||||||||
| Suresh et al. [55] | ✓ | ✓ | ✓ | ||||||||
| Szlejf et al. [56] | ✓ | ✓ | |||||||||
| Tsoukalas et al. [57] | ✓ | ✓ | ✓ | ||||||||
| Valdes et al. [58] | ✓ | ✓ | ✓ | ||||||||
| Valente et al. [59] | ✓ | ✓ | ✓ | ||||||||
| Verboven et al. [60] | ✓ | ✓ | ✓ | ||||||||
| Wu et al. [61] | ✓ | ✓ | ✓ | ||||||||
| Xue et al. [62] | ✓ | ✓ | ✓ | ||||||||
| Yee et al. [63] | ✓ | ✓ | ✓ | ||||||||
| Zhai et al. [64] | ✓ | ✓ | ✓ | ||||||||
| Zhang et al. [65] | ✓ | ✓ | ✓ | ||||||||
Data analysis
Data analysis is the phase where the systematic review begins to uncover insights and patterns from the selected studies. The analysis process will employ a qualitative method that aims to analyze the articles based on the information extracted from the previous section. The analysis of qualitative data is a nuanced and interpretative process. Qualitative data often consists of text-based information, such as interview transcripts or open-ended survey responses. Thematic analysis is the chosen method for examining this data.
Thematic analysis is a systematic and iterative process that involves identifying, analyzing, and reporting patterns or themes within the qualitative data. The aim is to uncover recurring ideas, concepts, and insights related to DDDM in patient care. A thematic analysis was used to identify, interpret, and report patterns in the qualitative data extracted from the included studies. The reviewer first read and re-read the data to get a good understanding of the content. After the familiarization stage, the reviewer systematically coded the extracted data segments, identifying key concepts and ideas related to DDDM methodologies and patient management. The coded data segments were then examined and grouped to form initial themes, each representing significant recurring patterns observed across the studies. The preliminary themes were then reviewed and refined in an iterative manner to ensure coherence, internal consistency, and clear differentiation. Each of the identified themes was explicitly defined and described, with relevant examples taken from the analyzed studies. This systematic and transparent thematic analysis approach contributed significantly to the quality, meaning, and clarity of the qualitative synthesis in this systematic review.
In summary, the methodological framework of this systematic review is robust, transparent, and comprehensive. It adheres to the PRISMA-P guidelines, employs clear inclusion and exclusion criteria, and follows a structured data collection and analysis process. By meticulously adhering to these methods, the systematic review aims to provide valuable insights into the role and impact of DDDM in patient care, contributing to the ongoing advancement of healthcare practices and decision-making processes. To minimize potential publication bias, this review incorporated external sources, expert recommendations, and grey literature, capturing unpublished or non-database-indexed studies. Additionally, dual-reviewer involvement throughout the study selection and data extraction processes enhanced methodological rigor and reduced selection bias. Systematic resolution of reviewer conflicts further strengthened the reliability and validity of the review’s findings, ensuring trustworthiness and actionable insights for practitioners and researchers alike.
Results
The results are the qualitative analysis of the articles selected in Sect. II, the overall structure from data-driven approach to decision-making methods to patient management application is shown in Fig. 2.
Fig. 2.
Overall structure from data-driven approach to decision-making methods to patient management application
Artificial intelligence based data-driven approach
The use of AI in DDDM within hospital management has ushered in a new era of efficiency and effectiveness in healthcare operations. AI systems, fueled by deep learning algorithms, have the capacity to process vast and complex datasets, encompassing electronic health records, medical imaging, patient demographics, and real-time monitoring data. By harnessing this wealth of information, healthcare administrators can gain deeper insights into patient trends, resource utilization, and clinical outcomes.
These advanced AI applications not only enhance the efficiency and cost-effectiveness of hospital management but also contribute significantly to patient-centric healthcare. By leveraging AIs analytical prowess, hospitals can provide more tailored and effective care, leading to improved patient satisfaction and overall health outcomes. As AI technology continues to evolve, it holds the promise of even greater advancements in DDDM within hospital management, ultimately reshaping the landscape of healthcare delivery.
Reinforcement learning
Reinforcement learning (RL) is a branch of AI that operates on the principle of training algorithms to make sequential decisions in dynamic and evolving environments. The fundamental concept revolves around an agent interacting with an environment, taking actions, receiving feedback in the form of rewards or penalties, and adjusting its strategy to maximize cumulative rewards over time. The key objective of RL is to learn a policy-a mapping of states to actions-that enables the agent to make decisions that optimize long-term outcomes. This learning process involves exploration, where the agent discovers the consequences of different actions, and exploitation, where it leverages learned knowledge to make decisions. RL algorithms, inspired by behavioral psychology and neuroscience, have demonstrated remarkable success in various fields, including healthcare.
In the domain of DDDM, RL has demonstrated transformative applications, contributing to adaptive and personalized interventions. Notably, RL has been employed in the management of antiarrhythmic medication dofetilide, accurately predicting dosing decisions with 96.1% accuracy [4] and aligning seamlessly with the adaptive nature of DDDM. The integration of EHRs and  -means clustering in a cluster-applied deep reinforcement learning model for type 2 diabetes mellitus treatment showcases RLs ability to navigate complex patient profiles, essential in DDDM for continuously adapting to individual patient characteristics [5] The intensive care unit (ICU) setting, with its dynamic and time-sensitive nature, has been a focus for RL applications, such as electrolyte repletion for critically ill patients. Using RL for electrolyte repletion has drastically cut down the need for magnesium and potassium replacements by 60%, normalized the timing of interventions in all three electrolytes (potassium, magnesium, and phosphate) and skewed them towards oral replacement as opposed to the intravenous route [49]. By developing an AI tool that recommends patient-tailored electrolyte repletion strategies, RL contributes to optimizing decisions in situations that demand dynamic responses, a key aspect of DDDM. The combination of RL with supervised learning in treating Coronary Heart Disease demonstrates its potential in dynamic treatment strategies, allowing for a comprehensive understanding of disease progression [30] Exploring RL for hypotension treatment in the ICU, a study employs RL to identify decision regions for treatment strategies, providing an interpretable framework crucial in DDDM scenarios [65] RLs application in anemia treatment in hemodialysis patients further exemplifies its contribution to DDDM by achieving optimal patient outcomes through dynamic adaptation [24].
-means clustering in a cluster-applied deep reinforcement learning model for type 2 diabetes mellitus treatment showcases RLs ability to navigate complex patient profiles, essential in DDDM for continuously adapting to individual patient characteristics [5] The intensive care unit (ICU) setting, with its dynamic and time-sensitive nature, has been a focus for RL applications, such as electrolyte repletion for critically ill patients. Using RL for electrolyte repletion has drastically cut down the need for magnesium and potassium replacements by 60%, normalized the timing of interventions in all three electrolytes (potassium, magnesium, and phosphate) and skewed them towards oral replacement as opposed to the intravenous route [49]. By developing an AI tool that recommends patient-tailored electrolyte repletion strategies, RL contributes to optimizing decisions in situations that demand dynamic responses, a key aspect of DDDM. The combination of RL with supervised learning in treating Coronary Heart Disease demonstrates its potential in dynamic treatment strategies, allowing for a comprehensive understanding of disease progression [30] Exploring RL for hypotension treatment in the ICU, a study employs RL to identify decision regions for treatment strategies, providing an interpretable framework crucial in DDDM scenarios [65] RLs application in anemia treatment in hemodialysis patients further exemplifies its contribution to DDDM by achieving optimal patient outcomes through dynamic adaptation [24].
In conclusion, RL stands at the forefront of revolutionizing patient management within the realm of DDDM. Its ability to adapt and make sequential decisions aligns seamlessly with the complex and evolving nature of healthcare scenarios. The applications of RL in predicting dosing decisions, personalized treatment recommendations for diabetes, and optimizing strategies in critical care settings highlight its efficacy in navigating the intricacies of patient care. The synergy of RL with electronic health records, clustering techniques, and supervised learning demonstrates its potential to enhance clinical decision making and provide personalized interventions. As healthcare continues to embrace data-driven approaches, RL emerges as a pivotal technology, contributing to more adaptive, personalized, and effective strategies in patient management, ultimately improving outcomes and shaping the future of precision medicine.
Deep learning
Deep learning, a subset of AI, operates on the principles of neural networks inspired by the human brain. It involves the use of complex algorithms and layered neural structures to analyze and learn patterns from vast datasets. In the context of healthcare, deep learning models can process diverse and intricate health data, enabling them to make predictions, classifications, and decisions. These models often leverage techniques such as convolutional neural networks (CNNs) for image analysis, recurrent neural networks (RNNs) for sequence data, and attention mechanisms for focused information processing [42].
Applying deep learning in the realm of DDDM can significantly transform patient management in healthcare. By harnessing the power of deep learning, healthcare systems can optimize decision support, diagnosis, and treatment strategies. For instance, the integration of deep learning in clinical decision support systems allows for the extraction of valuable insights from EHRs and various medical data sources. Precision and recall reached approximately 90% in predicting correct patient diagnosis from EHR data. This facilitates more accurate disease diagnosis, personalized treatment recommendations, and improved overall patient care [6] Moreover, deep learning plays a pivotal role in predictive analytics, enabling healthcare professionals to anticipate patient health outcomes and plan interventions accordingly. Predictive models, often based on RNNs or long short-term memory networks, can analyze temporal patterns in patient data, offering valuable insights into potential health issues. Resulting in 57% reduction in manual pathology workload [29] This foresight enhances preventive measures and timely interventions, contributing to better health outcomes. The integration of deep learning in patient management also extends to image-based diagnostics. CNNs excel in tasks such as medical imaging analysis, where they can accurately detect anomalies and assist in the early diagnosis of conditions. This capability is particularly valuable in fields like radiology, pathology, and dermatology, where visual information is crucial for decision making [31].
In conclusion, the application of deep learning in DDDM significantly enhances patient management in healthcare. By leveraging the capabilities of deep learning models, healthcare professionals can extract meaningful insights from complex data, leading to improved diagnostic accuracy, personalized treatment strategies, and proactive health management. The integration of deep learning technologies in healthcare systems underscores the transformative potential of AI in revolutionizing patient care. This technological evolution paves the way for more efficient and personalized healthcare delivery, with ongoing advancements promising even greater strides in the future.
Random forest
Random Forest, a potent machine learning algorithm, operates on the principle of ensemble learning, combining multiple decision trees to enhance predictive accuracy and robustness. Its integration into patient management processes represents a notable advance in healthcare, particularly within the Internet of Things (IoT) framework, offering a comprehensive approach to healthcare delivery. This section delves into the transformative applications of Random Forest within DDDM, highlighting its impact on patient outcomes and the challenges associated with its implementation.
The applications of Random Forest in healthcare extend to various domains, showcasing its efficacy in predictive modeling and decision support. In the study by Pavleen Kaur et al. [37], the IoT-driven Random Forest demonstrated high accuracy in disease prediction, emphasizing its potential for remote patient monitoring. Despite the positive outcomes, the study raises critical concerns regarding data security and privacy, calling for nuanced approaches in implementing IoT-based systems. Orthopedic surgery, specifically total joint arthroplasty, sees the application of Random Forest models for predicting patient outcomes [27] However, challenges related to data generalizability and the need for model customization are brought to light. Similarly, another research [63] focuses on using Random Forest for upper limb spasticity assessment, presenting an automated system that significantly outperforms other classifiers. The study introduces a novel Logical-SVM-RF classifier, aiming to reduce variability in clinical assessments. In forecasting patient recovery profiles post-trauma, research explores the application of Random Forest [7] The study underscores the importance of key predictors and advocates for an interdisciplinary approach to patient rehabilitation. Additionally, another research [23] compares the predictive performance of an AI-based system using Random Forest with transplant physicians, showcasing its potential as a valuable decision support tool.
In conclusion, Random Forest and machine learning collectively contribute to enhancing patient management, providing more accurate predictions and personalized treatments. However, the studies emphasize the need to address challenges related to data security, privacy, and the necessity for tailored approaches in diverse healthcare settings. Looking forward, the continued integration of Random Forest in DDDM holds promise for improved patient outcomes, necessitating ongoing efforts to refine models, address challenges, and foster interdisciplinary collaboration for comprehensive healthcare solutions.
Machine learning
Machine learning, a subset of AI, operates by leveraging algorithms to analyze data, learn from their patterns, and make informed decisions or predictions. In the context of healthcare, machine learning algorithms process vast amounts of medical data-from patient records to clinical studies-to identify trends, diagnose diseases, predict outcomes, and recommend treatments. This approach is particularly valuable in DDDM in patient care, where the ability to quickly and accurately process complex information can significantly enhance patient outcomes and optimize healthcare delivery.
In the realm of patient management, machine learning offers transformative solutions. For instance, research developed an AI framework that uses Markov decision processes and dynamic decision networks to improve healthcare delivery, demonstrating its potential in reducing costs and enhancing patient outcomes [12] Another research employed machine learning to predict prolonged ICU stays, integrating vital sign data with clinical information to optimize ICU resource allocation [20] Other research utilized machine learning to aid clinical decisions for COVID-19 patients, enhancing predictions for patient discharge, disease severity, and mortality [19] Research applied machine learning in radiotherapy treatment planning, showcasing its ability to match patients with suitable historical treatment plans [58] Another research combined machine learning with the Evidence Reasoning approach for diagnosing thyroid nodules, ensuring accuracy and interpretability [28] Other research demonstrated the application of machine learning in thyroid nodule diagnosis and cognitive impairment screening, providing accurate and actionable insights for healthcare professionals [56] Finally, research introduced an AI-powered tool for cardiovascular health management in cancer survivors, predicting disease risk and offering personalized care suggestions [15]
These studies highlight the critical role of machine learning in DDDM within patient care, offering innovative approaches to diagnosing, treating, and managing various health conditions. By harnessing the power of machine learning, healthcare providers can make more informed decisions, tailor treatments to individual patient needs, and ultimately improve the quality and efficiency of patient care.
Other data-driven approaches
The realm of DDDM in patient management encompasses various methodologies, extending beyond the realm of AI. While AI-based approaches dominate, other data-driven methods such as big data analysis, regression analysis, and similar models play a crucial role, especially in scenarios where constructing AI algorithms may prove challenging. Within personalized medicine, ethical considerations are paramount, particularly concerning black box algorithms, a big data approach [26] These algorithms, while providing treatment recommendations, lack transparency and interpretability, raising concerns about accountability and biases.
A broader application of data-driven methods is evident in predicting patient outcomes, as seen in a study focusing on estimating readmission risks for heart failure patients [8] The predictive model, leveraging extensive EHR data, outperforms traditional risk indicators, demonstrating the potential for precise and cost-effective post-discharge care. Such approaches unveil unexpected predictive factors, emphasizing the advantage of comprehensive EHR data in constructing models. In the context of clinical decision making, case similarity analysis emerges as a valuable tool, supporting diagnostic and treatment decisions [18] This retrospective analysis of patient cases identifies crucial diagnostic features through the  K-correlation coefficient [54] The method allows for individualized diagnostic assessments, potentially reducing waiting times for treatment proposals and enhancing the efficacy of treatment methods. However, the need for larger and more diverse datasets is acknowledged for further validation. The synergy of process mining and multi-criteria decision making provides insights into operational patterns and bottlenecks, with applications in ophthalmology patient management [54] Actionable insights, such as preferences for certain operating theatres and identified bottlenecks, lead to recommendations for improvements. The proposed “Design for process-mining” introduces a novel concept for decentralized data collection, aiming to enhance the process mining and decision-making process. Precision medicine’s reliance on data-driven methods is showcased in a model utilizing Formal Concept Analysis for health trajectory management [4] This model, realized through a Clinical Decision-making Tool, automates the analysis of modifiable factors impacting a patient’s health trajectory. It successfully predicts the probability of future events, providing patients with a sense of control over their health outcomes. However, the model’s need for further validation across diverse datasets and clinical contexts is acknowledged.
K-correlation coefficient [54] The method allows for individualized diagnostic assessments, potentially reducing waiting times for treatment proposals and enhancing the efficacy of treatment methods. However, the need for larger and more diverse datasets is acknowledged for further validation. The synergy of process mining and multi-criteria decision making provides insights into operational patterns and bottlenecks, with applications in ophthalmology patient management [54] Actionable insights, such as preferences for certain operating theatres and identified bottlenecks, lead to recommendations for improvements. The proposed “Design for process-mining” introduces a novel concept for decentralized data collection, aiming to enhance the process mining and decision-making process. Precision medicine’s reliance on data-driven methods is showcased in a model utilizing Formal Concept Analysis for health trajectory management [4] This model, realized through a Clinical Decision-making Tool, automates the analysis of modifiable factors impacting a patient’s health trajectory. It successfully predicts the probability of future events, providing patients with a sense of control over their health outcomes. However, the model’s need for further validation across diverse datasets and clinical contexts is acknowledged.
In conclusion, these diverse applications collectively underscore the transformative potential of DDDM in patient management. Whether addressing ethical considerations, predicting patient outcomes, supporting clinical decisions, optimizing operational processes, or guiding health trajectories, these methodologies exhibit promise. Each approach also recognizes its limitations, emphasizing the necessity for ongoing research and validation to unlock their full potential.
Decision making methods
Decision making in patient management is complex and faces many challenges such as the complexity of the condition of patients, the difficulty of finding the optimal solution, and the uncertainty of how patients will react to different choices. Thus, the method of decision making is crucial for people to find the optimal solution. Three methods of decision making are dominant across the research, which are decision support system, Markov decision process, and shared decision making.
Decision support system
A Decision Support System (DSS) in healthcare is an advanced tool designed to enhance the decision-making capabilities of healthcare professionals. It integrates various data sources like EHRs, clinical trials, imaging data, and guidelines to provide comprehensive insights into a patient’s condition. By utilizing machine learning and other AI-based approaches, DSSs analyze this data to offer personalized recommendations, ranging from disease diagnosis to treatment strategies. The primary aim is to improve patient outcomes, increase healthcare delivery efficiency, and enhance overall patient management.
Research utilizes machine learning techniques to predict mortality risk in sepsis patients, validating the association between serum lactate levels and increased mortality risk and demonstrating the potential of SVM classification to predict mortality risk using a limited set of features. This approach is particularly promising for non-ICU settings where comprehensive data may not be readily available [29] In parallel, a novel DSS for detecting and localizing skin vascular structures in dermoscopy images, based on the Stacked Sparse Autoencoder, outperforms other techniques in accuracy for vessel detection tasks. The system’s effectiveness depends on factors like patch size and image quality, with optimal performance achieved using images meeting specific guidelines [38] Developed as a CDSS, the system for diagnosing and predicting the severity of Alzheimer’s disease utilizes cognitive functioning assessment scores and MRI data, with the Kernel Ridge Regression model showing high prediction accuracy. The integration of cognitive scores and neuroimaging data is found to enhance the accuracy of Alzheimer’s disease diagnosis and severity prediction [17] Focused on developing a DSS to improve patient management in the context of Antimicrobial Resistance, the digital tool amalgamates hospital data with clinical rules, providing a precision-guided system for antibiotic selection. The potential of such tools to enhance patient management is highlighted, with improvements noted in clinical outcomes and reductions in inappropriate antibiotic use [44] Aimed at creating a CDSS for individualized treatment plans for Rifampicin Resistant Tuberculosis patients in resource-limited settings, the system developed using a hybrid model of machine learning techniques and expert input shows promise but also indicates the need for further research to assess its accuracy in real-life clinical settings [60].
These studies collectively emphasize the significant role of DSS in healthcare, demonstrating the potential of these systems to improve diagnostic accuracy, treatment planning, and overall patient care, marking a substantial advancement in healthcare decision making and patient outcomes.
Markov decision process
The Markov Decision Process (MDP) is a mathematical framework extensively used in healthcare for modeling decision-making where outcomes are influenced by both random events and the decisions of healthcare professionals. This approach is particularly valuable in patient management, where decisions are fraught with uncertainties and varying outcomes. MDP is characterized by its states, actions, transitions, and rewards. States represent the various conditions or scenarios of a patient, encompassing health status, treatment history, and other relevant factors. Actions refer to the possible interventions or treatments available in each state. Transitions are the probabilities of moving from one state to another based on the action taken, capturing the uncertainty in how a patient’s condition might evolve following a particular intervention. Rewards denote the values indicating the desirability of each state-action pair, considering factors like treatment efficacy, side effects, and costs. The goal of MDP is to find an optimal policy and a mapping of states to actions, which maximize the expected cumulative reward over time. This policy serves as a decision-making guide for healthcare professionals, indicating the best course of action for each patient state.
In healthcare research, MDP has been applied in various contexts. For example, MDP was utilized within a Reinforcement Learning framework to optimize anemia treatment in hemodialysis patients. Their approach, which combined the Fitted Q-Iteration algorithm with regression trees, improves patient outcomes by increasing the proportion of patients with adequate hemoglobin levels and reducing drug usage [24] Another research employed an ambiguous partially observable MDP to manage post-transplant medications, balancing the risk of organ rejection against the onset of new diabetes after transplantation. This model provides robust decision-making strategies that improve life expectancy and reduce medical expenditures by considering uncertainties and individual patient risk factors [14] MDP was used to optimize discharge policies for Alternate Level of Care patients to long-term care facilities. Their approach, which uses machine learning techniques to estimate health state transition probabilities, demonstrates the potential of MDP in resource allocation and patient-centered care. The index policy derived from MDP outperforms other policies in reducing hospital costs [22] An MDP model was used to develop a Poisson regression model to approximate optimal treatment decisions. This approach provides a more computationally efficient and clinically acceptable alternative to traditional MDP optimization, outperforming current clinical practices in terms of health outcomes [52]
Despite its effectiveness, MDP in healthcare faces challenges such as data dependency and limited dimensionality. Researchers address these by optimizing and extending MDP models or employing alternative models better suited to specific situations. For instance, the Poisson regression model in the study by Schell et al. offers a more efficient and clinically relevant alternative to traditional MDP optimization. In conclusion, MDPs offer a powerful tool for healthcare decision making, enabling the development of personalized treatment plans and optimizing resource allocation. By considering uncertainties and long-term consequences, MDPs help healthcare professionals navigate complex patient care scenarios, ultimately improving patient outcomes.
Shared decision making
Shared decision making (SDM) in healthcare is a collaborative process where healthcare providers and patients work together to make decisions about the patient’s treatment plan. This approach respects the patient’s right to be fully informed about their options and to have an active role in their own care. Recent research explores various methods to enhance SDM, particularly through the integration of technology and data analysis.
Research pioneers the use of process mining and the PROMETHEE II method to illuminate operational patterns, providing a foundation for more informed and DDDM. The incorporation of multi-criteria decision-making tools, such as PROMETHEE II, facilitates collaborative decisions in patient care [54] Another research develops an AI-enabled decision aid for knee osteoarthritis patients, showcasing how data-driven technologies enhance the quality of shared decision making. This tool integrates patient-reported outcome measures and personalized estimations, positively impacting decision quality, patient satisfaction, and functional outcomes [36] Finally, research proposes a clinical trial focusing on an AI-powered clinical decision aid for managing cardiovascular risks in cancer survivors, emphasizing the evolving landscape where data and shared decision making converge for improved patient outcomes [15].
These studies underscore the growing importance of integrating technology and data analysis in SDM. By leveraging process mining, AI, and decision-making methods, healthcare providers can enhance the quality of patient care, align treatments with guidelines, and respect patients’ preferences and values. This approach not only improves patient outcomes but also fosters a more patient-centered healthcare system.
Disease diagnosis and treatment
DDDM has various applications in patient management, including disease diagnosis and treatment, precision medicine, patient care, and beyond, shown in Fig. 3 In the realm of disease diagnosis and treatment, the application of advanced data-driven methodologies holds significant promise for improving patient outcomes. Leveraging comprehensive datasets and sophisticated analytical tools, healthcare professionals can enhance the accuracy and efficiency of disease diagnosis and treatment strategies.
Fig. 3.
Applications of DDDM in patient management
Oncology
Within the realm of oncology, a transformative shift is evident as DDDM takes center stage in patient management. Pioneering efforts, such as the translation of the Dutch national breast cancer guideline into data-driven Clinical Decision Trees, underscore the strides made in simplifying intricate guidelines into personalized, actionable care plans [33] This innovative approach represents a significant advancement, marking the departure from conventional one-size-fits-all interventions to a more tailored and patient-centric model in oncology.
Another crucial facet of this paradigm shift is observed in the integration of structured reporting tools and AI systems for standardizing oncologic imaging assessments [13] The advent of Computer-Assisted Reporting and Decision Support modules not only enhances guideline adherence but also streamlines clinical decision support, showcasing the potential to revolutionize patient management across diverse cancer types. This integration signifies a departure from traditional methods, bringing forth a new era of efficiency and precision in oncological diagnostics. In the domain of treatment recommendations, a notable stride is witnessed with the C3R model, a deep learning-based decision support system tailored for colorectal cancer [47] This model’s adaptability to real-world data and high accuracy challenges the limitations of rule-based systems, emphasizing the necessity for personalized decision making in the complex landscape of oncology. Diagnostic strategies are also evolving, with research focusing on enhancing thyroid cancer diagnoses through data-driven approaches. One study introduces a novel multi-criteria decision making model, which utilizes a fusion of weights and reliabilities to model thyroid cancer diagnosis [62] Another proposes a comprehensive framework for improving thyroid cancer diagnoses using big data, showcasing the potential of DDDM in enhancing medical diagnoses in oncology [28] Further advancements in oncology decision support are exemplified by an approach employing similarity analysis of medical cases to support clinical decision making in head and neck cancer [18] Retrospective analysis of patient cases and the use of the  K-correlation coefficient highlight the potential of DDDM in improving diagnostic accuracy. Additionally, a study combines the Radial Basis Function Network algorithm and decision trees to improve breast cancer classification accuracy using mammogram images [55] The high accuracy rate of this algorithm demonstrates the effectiveness of combining different algorithms in medical imaging and cancer diagnosis. Another research emphasizes the need to incorporate decision-making goals into data analytics for breast cancer diagnosis, introducing the LS-SOED method that optimizes diagnosis outcomes [35].
K-correlation coefficient highlight the potential of DDDM in improving diagnostic accuracy. Additionally, a study combines the Radial Basis Function Network algorithm and decision trees to improve breast cancer classification accuracy using mammogram images [55] The high accuracy rate of this algorithm demonstrates the effectiveness of combining different algorithms in medical imaging and cancer diagnosis. Another research emphasizes the need to incorporate decision-making goals into data analytics for breast cancer diagnosis, introducing the LS-SOED method that optimizes diagnosis outcomes [35].
These studies illuminate the transformative journey of oncology towards DDDM in patient management. Through the amalgamation of advanced technologies and analytical methodologies, oncology is evolving towards a future characterized by personalized, precise, and patient-centric cancer care, ultimately enhancing outcomes for individuals navigating the complexities of cancer treatment.
Cardiology
Cardiology, the branch of medicine dealing with disorders of the heart and blood vessels, is increasingly leveraging DDDM to enhance patient care. This approach utilizes vast amounts of medical data to inform treatment strategies, improve diagnostic accuracy, and personalize patient care. Recent research in this field has demonstrated the potential of various data-driven methods and technologies in transforming cardiology practices.
An Artificial Intelligence Clinical Decision Support System incorporating machine learning has been designed to enhance heart failure diagnosis, demonstrating substantial concordance with expert diagnoses [21] Moving to predictive modeling, a study utilized HER data to create a model estimating readmission risks in heart failure patients, outperforming traditional risk indicators [8] Analyzing EHRs through a data-driven methodology, researchers provided a comprehensive understanding of heart failure, facilitating targeted interventions and personalized care strategies for more effective patient management [45] Investigating treatment decisions, a study explored the decision-making process for transcatheter aortic valve replacement and isolated surgical aortic valve replacement in young high-risk patients, identifying key factors guiding physicians in treatment selection [32] In hypertension management, a machine learning model recommending antihypertensive medications based on individual patient characteristics outperformed the standard-of-care approach, emphasizing the superiority of robust learning procedures [34] Expanding into cardiovascular care for cancer survivors, an AI-powered clinical decision aid tool was proposed to provide early detection of cardiovascular risks, stratify risk levels, and offer tailored recommendations aligned with guidelines and expert insights [15] Venturing into predictive modeling, cardiorespiratory instability in critically ill patients was forecasted, leveraging high-frequency data and advanced signal processing techniques, exhibiting commendable performance in predicting clinically relevant events [48].
Collectively, these studies underscore the transformative influence of DDDM in cardiology, steering the field towards a future characterized by more personalized, accurate, and effective patient care, ultimately improving overall outcomes and treatment experiences.
Mental and neurological disorders
Mental and neurological disorders present unique challenges in patient management due to their complexity and the need for personalized care. Recent research has focused on leveraging DDDM models to enhance the diagnosis, treatment, and management of these disorders. These models utilize vast amounts of clinical data, advanced analytics, and machine learning algorithms to provide insights that can guide healthcare professionals in making informed decisions.
Examining the effectiveness of cognitive behaviour therapy and counselling for depression in primary care settings, a study found that treatment outcomes could be improved by allocating treatment based on baseline characteristics, emphasizing the potential of personalized therapy approaches in treating depression [11] In traumatic brain injury patients, a predictive algorithm was developed to estimate the thirty-day mortality risk using physiological parameters like intracranial pressure and cerebral perfusion pressure, demonstrating strong predictive power and potential optimization of management strategies [50] For patients undergoing Deep Brain Stimulation surgery, a DSS for predicting discharge disposition was evaluated, utilizing preoperative clinical data to aid in planning and decision making for patients with neurological disorders [16] Another study introduced a data-centric approach integrating genomics, phenotypic characteristics, and treatment response data to guide decisions in neurological disorders, enhancing predictive accuracy in diagnosis and therapy tailoring [17] In patients with severe acquired brain injuries, machine learning models were developed to predict tracheostomy decannulation probability and timing, providing valuable information for clinical decision making and improving in-hospital care organization [43] Additionally, a triage decision support tool was developed to quantify the risk of early neurologic decline in traumatic brain injury patients, It utilizes machine learning models which base on clinical and physiological data collected during the first hour of hospital resuscitation [9].
These studies collectively highlight the significant role of DDDM in enhancing the management of mental and neurological disorders. By utilizing advanced technologies and analytical methods, healthcare professionals can navigate complex situations, balance trade-offs, and ultimately optimize patient outcomes by selecting the most appropriate interventions and care strategies.
Specific groups
The application of DDDM across various healthcare sectors, including pediatric occupational therapy, elderly care, hepatocellular carcinoma treatment, and pediatric preventive care. These demonstrate its transformative impact on enhancing patient outcomes and optimizing healthcare delivery.
In elderly care, a Machine Learning Assisted Integrated Data-driven Framework (MLA-IDDF) is discussed for improving performance of wearable medical devices, enhancing the accuracy of physiological data collection and signal recovery crucial for elderly health monitoring [10] The MLA-IDDF method shows improved signal recovery accuracy and compression ratios, offering a more efficient and accurate approach to elderly care monitoring. Additionally, addressing delayed discharge in elderly patients involves proposing a prediction-driven decision-making framework for efficient discharge to Long-Term Care facilities. This framework considers individual patient characteristics and health trajectories, with the proposed index policy demonstrating improved efficiency and cost savings compared to traditional discharge policies [22] Finally, research was developed to explore the importance of DDDM in treating particularly older individuals with hepatocellular carcinoma treatment, highlighting the need for personalized treatment approaches and shared decision making considering individual patient characteristics such as age, tumor size, and physiological reserve [53] In pediatric healthcare, the use of DDDM in pediatric occupational therapy focuses on systematic outcome measurement and accountability, leading to marked improvements in addressing challenges faced by children with Autism Spectrum Disorder [25] For pediatric preventive care, the focus is on using Bayesian networks, leveraging observational data from EHR to develop a patient-tailored prioritization system for risk assessments and physician prompts. This approach aims to improve the delivery of pediatric preventive services by tailoring recommendations based on individual patient risks [39].
These studies collectively underscore the significant role of DDDM in enhancing patient care across various medical fields, showcasing the potential of advanced technologies and analytical methods in healthcare.
Precision medicine
Precision medicine, revolutionizing patient management by tailoring treatments to individual patient conditions, is prominently shaping healthcare across diverse medical domains. The transformative impact of this approach is evident in studies utilizing data-driven methodologies to fine-tune treatment strategies for specific patient cohorts.
In the realm of type-2 diabetes mellitus, a study exemplifies the prowess of precision medicine [5] Through the development of a Cluster-applied Deep Q Network model, the utilization of EHRs enables the creation of personalized treatment recommendations [5] The superiority of this model over other reinforcement learning models in mitigating fasting plasma glucose levels and diabetes-related complications underscores the potential of precision medicine in optimizing diabetes care. Delving into precision medicine applications in Parkinson’s Disease, another study employs Next-Generation Sequencing technologies to pinpoint patient-specific mutations [66] This comprehensive approach, integrating genetic insights with environmental factors and digital phenotyping, promises a nuanced and personalized paradigm for Parkinson’s Disease treatment. The concept of healthcare fusion, as introduced by Zhai et al., emphasizes the integration of diverse data types and stakeholders in precision medicine. Particularly beneficial in Alzheimer’s disease and ovarian cancer, this approach facilitates early disease detection and precise prescription strategies [64] Contributing a model of Health Trajectory management using Formal Concept Analysis for Total Knee Arthroplasty patients, Fischer et al. automate the analysis of modifiable factors, providing multiple decision paths to influence health outcomes [41] In discussing the ethical dimensions of personalized medicine, a study addresses challenges related to black box algorithms, integration of non-medical data, and the management of incidental findings in EHRs [26] Presenting a data-driven approach for predicting rational medication dosages in pediatric medicine, the proposed hybrid learning model blends physiological and indication features, exhibiting precise dosage prediction capabilities [61], highlighting the adaptability of precision medicine across diverse patient demographics.
Collectively, these studies illustrate the strides made in precision medicine, emphasizing its potential to deliver personalized and effective treatment plans rooted in individual patient data. This approach not only elevates patient outcomes but also propels the evolution of patient-centered care practices across various medical specialties.
Patient care, nursing and beyond
The application of DDDM in healthcare goes beyond disease diagnosis and treatment, reaching into critical domains such as patient care, nursing, and broader healthcare management. This transformative approach utilizes comprehensive datasets and advanced analytical methodologies to optimize healthcare delivery, enhance patient experiences, and streamline clinical workflows.
In patient care, DDDM is reshaping how healthcare providers address the holistic well-being of individuals. By leveraging data encompassing patient demographics, medical histories, and real-time monitoring, healthcare professionals can tailor interventions to individual characteristics. This personalized approach not only improves treatment outcomes but also fosters a more patient-centric care experience, enhancing overall satisfaction [15] Resource optimization is a key facet of DDDM in patient care. Machine learning models predicting patient admission rates enable hospitals to allocate resources effectively, contributing to improved patient flow and enhanced healthcare service delivery. Proactive DDDM also extends to chronic disease management, where remote patient monitoring utilizing wearable devices and real-time data analysis allows for prompt intervention, improving outcomes and reducing the burden on healthcare facilities [64].
In nursing, DDDM empowers healthcare professionals with tools and insights that enhance decision-making and contribute to the overall quality of patient care. Predictive analytics models assist nurses in forecasting patient outcomes and identifying potential risks, allowing for proactive interventions and personalized care plans. The application of DDDM in nursing extends to evidence-based practice, where real-time insights into best practices, treatment effectiveness, and patient outcomes inform decision-making and improve the quality of care delivered by nurses. Moreover, DDDM can transform workforce management and resource allocation in nursing. Data-driven tools optimize nurse staffing levels based on patient acuity, workload, and historical data patterns, ensuring a balanced workload and contributing to more efficient nursing operations.
Beyond patient care and nursing, DDDM is making significant contributions to healthcare management, administration, and policy-making. In healthcare administration, predictive analytics models forecast patient admissions, allowing hospitals to adjust staffing levels and allocate resources effectively for cost-effective and patient-centric care [49] DDDM is also playing a pivotal role in healthcare policy-making. Analyzing population health data and epidemiological trends facilitates informed decisions about public health initiatives, resource allocation, and preventive measures. Data-driven insights contribute to the development of evidence-based policies that address the specific needs of diverse populations, improving overall community health. Furthermore, in healthcare quality management, DDDM enhances the monitoring and evaluation of healthcare services. Analysis of patient outcomes, adherence to clinical guidelines, and performance metrics enables healthcare organizations to identify areas for improvement, implement targeted interventions, and ensure the delivery of high-quality care [41].
In conclusion, the integration of DDDM in patient care, nursing, and broader healthcare management signify a transformative shift towards more efficient, effective, and patient-centric healthcare delivery. As technology continues to evolve, the adoption of data-driven methodologies will be crucial for healthcare professionals and organizations to navigate the complexities of the modern healthcare landscape and provide optimal care to individuals and communities.
Discussion
Interpretation of results
The integration of Data-Driven Decision Making (DDDM) is changing patient management in different healthcare contexts and is considered a major step toward a patient-centered, optimal, and effective healthcare delivery system. The outcomes of this systematic review reflect the critical role that DDDM approaches such as reinforcement learning, deep learning, random forest models, and decision support systems play in enhancing clinical decision-making, diagnostic precision, and treatment outcome. For instance, reinforcement learning has helped the management of chronic diseases like diabetes by developing patient-specific dosage regimens and treatment plans. In the same way, the application of deep learning techniques has greatly enhanced diagnostic procedures in oncology through the analysis of images to detect cancers at an early stage and with higher accuracy than conventional methods. The random forest algorithms have shown great potential in the field of postoperative outcome prediction models thus improving the decision-making process and management of resources in surgical care. Also, Decision Support Systems (DSS) have greatly impacted clinical workflows by streamlining treatment guidelines in areas such as cardiology, neurology, and infectious diseases. Patient data, clinical guidelines, and machine learning are combined and presented by DSS to offer potential solutions, which may lead to better patient results, decreased variability in care, and improved healthcare costs.
Limitations
However, there are still numerous limitations. The quality and the representativeness of the healthcare data are still an issue. Missing data or sampling error can result in wrong or maintenance of inequality in decision-making in clinical practice. Moreover, many of the current machine learning models, including those that are based on deep learning and reinforcement learning, are not easily understandable. These problems are a challenge to clinical adoption because healthcare professionals need understandable explanations of the automated decisions that they wish to incorporate into practice. Furthermore, ethical and privacy issues are major constraints, especially with the growth of IoT devices in patient care and data collection in real time. IoT-based systems are more prone to security risks and data leakage and thus pose a significant risk to data integrity, ownership, access control, and adherence to data protection policies. These problems have to be solved in order to make sure that patients and healthcare professionals can trust the data and technologies that are used in the management of their health. The study also has some methodological limitations such as publication bias, study design heterogeneity, and different patient populations. Although the systematic review method was quite rigorous in reducing bias, grey literature was included and two researchers extracted data independently, there may still be some residual bias which may affect the generalization of the review results.
Future outlook
Future work should focus on overcoming these limitations by improving the data collection process to achieve a higher response rate and data completeness, especially in vulnerable groups. The development of explainable AI and interpretable machine learning models is crucial to increase the understanding, usage, and integration of DDDM tools by clinicians in patient care. Research on federated learning, which allows model training without compromising patient data privacy, also presents promising directions for the future. However, such cooperation is crucial between healthcare professionals, data scientists, and policy makers. Such partnerships would be useful in the development of overall governance frameworks that address the ethical and governance aspects of using and sharing data, including the issues of privacy and security. Long-term clinical effectiveness, cost-effectiveness and patient experience of the DDDM tools should also be investigated as part of the next studies to increase the evidence for their use.
Conclusion
This systematic review shows that Data-Driven Decision Making (DDDM) improves patient management through better, more precise and individualized healthcare in various specialties. The techniques that have applied advanced methodologies such as deep learning, reinforcement learning, and sophisticated decision support systems have shown great potential in enhancing the accuracy of diagnosis, clinical results, and treatment efficacy. Specifically, DDDM-inspired strategies have resulted in a significant improvement in the predictive accuracy of chronic diseases, reduction of the healthcare workers’ workload, increased treatment personalization, and the ability to distinguish clinically important biomarkers of complex diseases. However, the widespread adoption of such models is hindered by several critical issues, including the quality of data, the understandability of the analytical methods used, and issues concerning the privacy and security of patients’ information, especially in the context of IoT-enabled healthcare. These limitations can be overcome through methodological refinement, the use of more transparent algorithms, and the development of robust ethical frameworks. In the future, the cooperation of healthcare providers, technologists, researchers, and policymakers is vital. Such cooperation can develop responsible guidelines, support ethical governance, and promote the development of strong technological integration into clinical practice. Further research and targeted funding are expected to sustain the potential of DDDM methodologies which can serve as the basis for shifting healthcare systems around the world to more personalized, effective, and equitable patient care. Therefore, the integration of DDDM can be improved in the following ways to enhance the decision-making process, improve the current healthcare delivery system and enhance the quality of health services and treatment across the world. Moreover, future studies should include the assessment of the cost-effectiveness and the sustainability of the implemented DDDM technologies in various healthcare contexts. In taking these steps, the potential of DDDM can be best realized, leading to innovation and the universal acceptance of the approach. Thus, healthcare systems will not only provide better patient results but also develop strong data-driven systems that can help manage new healthcare issues in a data-rich environment.
Acknowledgements
The author would like to show his appreciation to Dr. Baruch Fischhoff, Dr. Kevin Jarbo, and Dr. Qiang Luo, for some useful discussions.
Abbreviations
- DDDM
Data-driven decision making
- PRISMA-P
Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols
- EHR
Electronic Health Record
- AI
Artificial Intelligence
- RL
Reinforcement Learning
- CNN
Convolutional Neural Network
- RNN
Recurrent Neural Network
- ML
Machine Learning
- DSS
Decision Support System
- MDP
Markov Decision Process
- SDM
Shared Decision Making
- MLA-IDDF
Machine Learning Assisted Integrated Data-driven Framework
- ICU
Intensive Care Unit
- IoT
Internet of Things
Author contributions
GL, the sole author of this manuscript, acknowledges responsibility for all aspects of the research presented.
Funding
The author received no specifc funding for this study.
Data availability
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author declares no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Basile LJ, Carbonara N, Pellegrino R, Panniello U. Business intelligence in the healthcare industry: The utilization of a data-driven approach to support clinical decision making. Technovation. 2023;120(102482) 166–4972. https://www.sciencedirect.com/science/article/pii/S0166497222000293 [Google Scholar]
- 2.Brynjolfsson E, McElheran K. The rapid adoption of data-driven decision-making. Am. Econ. Rev. 2016;0002-8282. 106(5):133–39. 10.1257/aer.p20161016. 128th Annual Meeting of the American-Economic-Association, San Francisco, CA, JAN. [Google Scholar]
- 3.Cresswell K, Callaghan M, Khan S, Sheikh Z, Mozaffar H, Sheikh A. Investigating the use of data-driven artificial intelligence in computerised decision support systems for health and social care: A systematic review. Health Inf. J. 2020;26(3):2138–47. 10.1177/1460458219900452. [DOI] [PubMed] [Google Scholar]
- 4.Levy AE, Biswas M, Weber R, Tarakji K, Chung M, Noseworthy PA, Newton-Cheh C, Rosenberg MA. Applications of machine learning in decision analysis for dose management for dofetilide. PLoS One. 2020;14(12):1–13, 12. 10.1371/journal.pone.0227324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oh SH, Lee SJ, Park J. Effective data-driven precision medicine by cluster-applied deep reinforcement learning. Knowl-Based Syst. 2022;256(109877);950–7051. https://www.sciencedirect.com/science/article/pii/S0950705122009704 [Google Scholar]
- 6.Comito C, Falcone D, Forestiero A. Ai-driven clinical decision support: Enhancing disease diagnosis exploiting patients similarity. IEEE Access. 2022;10:6878–88. 10.1109/ACCESS.2022.3142100. [Google Scholar]
- 7.Stoitsas K, Bahulikar S, de Munter L, de Jongh MAC, Jansen MAC, Jung MM, van Wingerden M, Van Deun K. Clustering of trauma patients based on longitudinal data and the application of machine learning to predict recovery. Sci. Rep. 2022. 2045-2322. 12(1):16990. 10.1038/s41598-022-21390-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bayati M, Braverman M, Gillam M, Mack KM, Ruiz G, Smith MS, Horvitz E. Data-driven decisions for reducing readmissions for heart failure: General methodology and case study. PLoS One. 2014. 9:1–9. 10.1371/journal.pone.0109264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Podell J, Yang S, Miller S, Felix R, Tripathi H, Parikh G, Miller C, Chen H, Kuo Y-M, Lin CY, Hu P, Badjatia N. Rapid prediction of secondary neurologic decline after traumatic brain injury: A data analytic approach. Sci. Rep. 2023;13(1):403, 2045–322. 10.1038/s41598-022-26318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ba T, Li S, Wei Y. A data-driven machine learning integrated wearable medical sensor framework for elderly care service. Measurement. 2021;167(108383):263–2241. https://www.sciencedirect.com/science/article/pii/S0263224120309192 [Google Scholar]
- 11.Bauer-Staeb C, Griffith E, Faraway JJ, Button KS. Personalised psychotherapy in primary care: Evaluation of data-driven treatment allocation to cognitive–behavioural therapy versus counselling for depression. BJPsych Open. 2023;9(2):e46. 10.1192/bjo.2022.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bennett CC, Hauser K. Artificial intelligence framework for simulating clinical decision-making: A markov decision process approach. Artif. Intel. Med. 2013. 57(1):933–3657, 9–19. https://www.sciencedirect.com/science/article/pii/S0933365712001510 [DOI] [PubMed] [Google Scholar]
- 13.Bizzo BC, Almeida RR, Alkasab TK. Computer-assisted reporting and decision support in standardized radiology reporting for cancer imaging. JCO Clin. Cancer Inf. 2021. 5:426–434. 10.1200/CCI.20.00129. [DOI] [PubMed] [Google Scholar]
- 14.Boloori A, Saghafian S, Chakkera HA, Cook CB. Data-driven management of post-transplant medications: An ambiguous partially observable markov decision process approach. Manuf & Service Operations Manag. 2020;22(5):1066–87. 10.1287/msom.2019.0797. [Google Scholar]
- 15.Brown S, Chung B, Doshi K, et al. Patient similarity and other artificial intelligence machine learning algorithms in clinical decision aid for shared decision-making in the prevention of cardiovascular toxicity (pact): A feasibility trial design. Cardio-Oncology. 2023;9(7). 10.1186/s40959-022-00151-0. [DOI] [PMC free article] [PubMed]
- 16.Buchlak QD, Kowalczyk M, Leveque J-C, Wright A, Farrokhi F. Risk stratification in deep brain stimulation surgery: Development of an algorithm to predict patient discharge disposition with 91.9 % accuracy. J. Clin. Neurosci. 2018;57(967–5868):26–32. https://www.sciencedirect.com/science/article/pii/S0967586818304971 [DOI] [PubMed] [Google Scholar]
- 17.Bucholc M, Ding X, Wang H, Glass DH, Wang H, Prasad G, Maguire LP, Bjourson AJ, McClean PL, Todd S, Finn DP, Wong-Lin K. A practical computerized decision support system for predicting the severity of alzheimer’s disease of an individual. Expert Syst. Appl. 2019;130(957–4174):157–71. https://www.sciencedirect.com/science/article/pii/S0957417419302520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buyer J, Oeser A, Grieb N, Dietz A, Neumuth T, Stoehr M. Decision support for oropharyngeal cancer patients based on data-driven similarity metrics for medical case comparison. Diagnostics. 2022;12(4):2075–4418. https://www.mdpi.com/2075-4418/12/4/999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Casano N, Santini SJ, Vittorini P, Sinatti G, Carducci P, Mastroianni CM, Ciardi MR, Pasculli P, Petrucci E, Marinangeli F, Balsano C. Application of machine learning approach in emergency department to support clinical decision making for sars-cov-2 infected patients. J. Integr. Bioinform. 2023;20(2):20220047. 10.1515/jib-2022-0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Castiñeira D, Schlosser KR, Geva A, Rahmani AR, Fiore G, Walsh BK, Smallwood CD, Arnold JH, Santillana M. Adding continuous vital sign information to static clinical data improves the prediction of length of stay after intubation: A data-driven machine learning approach. Respir. Care. 2020. ISSN 0020-1324. 65(9):1367–77. https://rc.rcjournal.com/content/65/9/1367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choi D-J, Park JJ, Ali T, Lee S. Artificial intelligence for the diagnosis of heart failure. NPJ Digit. Med. 2020;3(1):54. 10.1038/s41746-020-0261-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chuang Y, Zargoush M, Ghazalbash S, Samiedaluie S, Kuluski K, Guilcher S. From prediction to decision: Optimizing long-term care placements among older delayed discharge patients. Prod. Oper. Manag. 2023;32(4):1041–58. 10.1111/poms.13910. [Google Scholar]
- 23.Divard G, Raynaud M, Tatapudi VS, Abdalla B, Bailly E, Assayag M, Binois Y, Cohen R, Zhang H, Ulloa C, Linhares K, Tedesco HS, Legendre C, Jouven X, Montgomery RA, Lefaucheur C, Aubert O, Loupy A. Comparison of artificial intelligence and human-based prediction and stratification of the risk of long-term kidney allograft failure. Commun. Med. (Lond). 2022;2(1):150. 10.1038/s43856-022-00201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Escandell-Montero P, Chermisi M, Martínez-Martínez JM, Gómez-Sanchis J, Barbieri C, Soria-Olivas E, Mari F, Vila-Francés J, Stopper A, Gatti E, Martín-Guerrero JD. Optimization of anemia treatment in hemodialysis patients via reinforcement learning. Artif. Intel. Med. 2014;62(1):933–3657, 47–60. https://www.sciencedirect.com/science/article/pii/S0933365714000840 [DOI] [PubMed] [Google Scholar]
- 25.Faller P, Hunt J, van Hooydonk E, Mailloux Z, Schaaf R. Application of data-driven decision making using ayres sensory Integration\textregistered with a child with autism. Am. J. Occup. Ther. 2015;70(1):272–9490. p70012200201–09. 10.5014/ajot.2016.016881. [DOI] [PubMed]
- 26.Fischer T, Brothers K, Erdmann P, Langanke M. Clinical decision-making and secondary findings in systems medicine. BMC Med Ethics. 2016;17(1):32. 10.1186/s12910-016-0113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fontana MA, Lyman S, Sarker GK, Padgett DE, MacLean CH. Can machine learning algorithms predict which patients will achieve minimally clinically important differences from total joint arthroplasty? Clin. Orthop. & Relat. Res. 2019;477(6):1267–79. 10.1097/CORR.0000000000000687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fu C, Xu C, Xue M, Liu W, Yang S. Data-driven decision making based on evidential reasoning approach and machine learning algorithms. Appl. Soft. Comput. 2021. 110(107622):1568–4946. https://www.sciencedirect.com/science/article/pii/S1568494621005433. [Google Scholar]
- 29.Gehrung M, Crispin-Ortuzar M, Berman AG, O’Donovan M, Fitzgerald RC, Markowetz F. Triage-driven diagnosis of barrett’s esophagus for early detection of esophageal adenocarcinoma using deep learning. Nat. Med. 2021;27:833–41. 10.1038/s41591-021-01287-9. [DOI] [PubMed] [Google Scholar]
- 30.Gultepe E, Green JP, Nguyen H, Adams J, Albertson T, Tagkopoulos I. From vital signs to clinical outcomes for patients with sepsis: A machine learning basis for a clinical decision support system. J. Am. Med. Inf. Assoc. 2013. 21(2):1067–5027, 315–25. 10.1136/amiajnl-2013-001815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guo H, Li J, Liu H, He J. Learning dynamic treatment strategies for coronary heart diseases by artificial intelligence: Real-world data-driven study. Bmc Med. Inform. Decis. 2022;22(1):1472–6947, 39. 10.1186/s12911-022-01774-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hasimbegovic E, Papp L, Grahovac M, Krajnc D, Poschner T, Hasan W, Andreas M, Gross C, Strouhal A, Delle-Karth G, Grabenwöger M, Adlbrecht C, Mach M. A sneak-peek into the physician’s brain: A retrospective machine learning-driven investigation of decision-making in tavr versus savr for young high-risk patients with severe symptomatic aortic stenosis. J. Personalized Med. 2021;11(11). ISSN 2075-4426. https://www.mdpi.com/2075-4426/11/11/1062 [DOI] [PMC free article] [PubMed]
- 33.Hendriks MP, Verbeek XA, van Vegchel T, van der Sangen MJ, Strobbe LJ, Merkus JW, Zonderland HM, Smorenburg CH, Jager A, Siesling S. Transformation of the national breast cancer guideline into data-driven clinical decision trees. JCO Clin. Cancer Inf. 2019. 3(3):1–14. 10.1200/CCI.18.00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hu Y, Huerta J, Cordella N, Mishuris RG, Paschalidis IC. Personalized hypertension treatment recommendations by a data-driven model. Bmc Med. Inform Decis. 2023;23(1:1472–6947, 44. 10.1186/s12911-023-02137-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jafari-Marandi R, Davarzani S, Gharibdousti MS, Smith BK. An optimum ann-based breast cancer diagnosis: Bridging gaps between ann learning and decision-making goals. Appl. Soft Comput. 2018. 72(1568–4946):108–20. https://www.sciencedirect.com/science/article/pii/S1568494618304484 [Google Scholar]
- 36.Jayakumar P, Moore MG, Furlough KA, Uhler LM, Andrawis JP, Koenig KM, Aksan N, Rathouz PJ, Bozic KJ. Comparison of an artificial intelligence–enabled patient decision aid vs educational material on decision quality, shared decision-making, patient experience. Funct. Outcomes Adults Knee Osteoarthr: Randomized Clin. Trial JAMA Network Open. 2021;4(2):2574–3805. e2037107–2037107. 10.1001/jamanetworkopen.2020.37107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaur P, Kumar R, Kumar M. A healthcare monitoring system using random forest and internet of things (iot). Multimedia Tools Appl. 2019;78(14):1573–7721. 19905–16. 10.1007/s11042-019-7327-8. [Google Scholar]
- 38.Kharazmi P, Zheng J, Lui H, Wang ZJ, Lee TK. A computer-aided decision support system for detection and localization of cutaneous vasculature in dermoscopy images via deep feature learning. J. Med. Syst. 2018;42(2):33. 10.1007/s10916-017-0885-2. [DOI] [PubMed] [Google Scholar]
- 39.Klann JG, Anand V, Downs SM. Patient-tailored prioritization for a pediatric care decision support system through machine learning. J. Am. Med. Inf. Assoc. 2013;20(e2). 1067–5027. e267–74. 10.1136/amiajnl-2013-001865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kondylakis H, Axenie C, Bastola D(, DG, Katehakis, Kouroubali A, Kurz D, Larburu N, Macía I, Maguire R, Maramis C, Marias K, Morrow P, Muro N, Núñez-Benjumea FJ, Rampun A, Rivera-Romero O, Scotney B, Signorelli G, Wang H, Tsiknakis M, Zwiggelaar R. Status and recommendations of technological and data-driven innovations in cancer care: Focus group study. J. Med. Internet Res. 2020;22(12:e22034. 1438–8871. https://www.jmir.org/2020/12/e22034 [DOI] [PMC free article] [PubMed]
- 41.Kriegova E, Kudelka M, Radvansky M, Gallo J. A theoretical model of health management using data-driven decision-making: The future of precision medicine and health. J. Transl. Med. 2021;19(1). 1479–5876. 68. 10.1186/s12967-021-02714-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li X, Dvornek NC, Zhuang J, Ventola P, Duncan JS. Brain biomarker interpretation in asd using deep learning and fmri. In: Frangi AF, Schnabel JA, Davatzikos C, Alberola-López C, Fichtinger G, editors. Medical image computing and computer assisted intervention– MICCAI 2018. Cham: Springer International Publishing; 2018. p. 206–14. ISBN 978-3-030-00931-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mannini A, Hakiki B, Liuzzi P, Campagnini S, Romoli A, Draghi F, Macchi C, Carrozza MC. Data-driven prediction of decannulation probability and timing in patients with severe acquired brain injury. Comput. Met. Programs Biomed. 2021;209(106345):0169–2607. https://www.sciencedirect.com/science/article/pii/S0169260721004193 [DOI] [PubMed] [Google Scholar]
- 44.Müller L, Srinivasan A, Abeles SR, Rajagopal A, Torriani FJ, Aronoff-Spencer E. A risk-based clinical decision support system for patient-specific antimicrobial therapy (ibiogram): Design and retrospective analysis. J. Med. Internet Res. 2021;23(12):e23571. 1438–8871. https://www.jmir.org/2021/12/e23571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nagamine T, Gillette B, Kahoun J, Burghaus R, Lippert J, Saxena M. Data-driven identification of heart failure disease states and progression pathways using electronic health records. Sci. Rep. 2022;12(1). 2045–2322. 17871. 10.1038/s41598-022-22398-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Niraula D, Sun W, Jin J, Dinov ID, Cuneo K, Jamaluddin J, Matuszak MM, Luo Y, Lawrence TS, Jolly S, Haken RKT, Naqa IE. A clinical decision support system for ai-assisted decision-making in response-adaptive radiotherapy (arclids). Sci. Rep. 2023;13(1):5279. 2045–322. 10.1038/s41598-023-32032-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Park J-H, Baek J-H, Sym SJ, Lee KY, Lee Y. A data-driven approach to a chemotherapy recommendation model based on deep learning for patients with colorectal cancer in Korea. Bmc Med. Inform. Decis. 2020;1472-6947. 20(1):241. 10.1186/s12911-020-01265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pinsky MR, Dubrawski A, Clermont G. Intelligent clinical decision support. Sensors. 2022. ISSN 1424-8220. 22(4). https://www.mdpi.com/1424-8220/22/4/1408 [DOI] [PMC free article] [PubMed]
- 49.Prasad N, Mandyam A, Chivers C, Draugelis M, Hanson CW, Engelhardt BE, Laudanski K. Guiding efficient, effective, and patient-oriented electrolyte replacement in critical care: An artificial intelligence reinforcement learning approach. J. Personalized Med. 2022;12(5):2075–4426. https://www.mdpi.com/2075-4426/12/5/661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Raj R, Wennervirta JM, Tjerkaski J, Luoto TM, Posti JP, Nelson DW, Takala R, Bendel S, Thelin EP, Luostarinen T, Korja M. Dynamic prediction of mortality after traumatic brain injury using a machine learning algorithm. NPJ Digit. Med. 2022;5(1):96. 2398–6352. 10.1038/s41746-022-00652-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Saravi B, Hassel F, Ülkümen S, Zink A, Shavlokhova V, Couillard-Despres S, Boeker M, Obid P, Lang GM. Artificial intelligence-driven prediction modeling and decision making in spine surgery using hybrid machine learning models. J. Personalized Med. 2022;12(4):2075–4426. https://www.mdpi.com/2075-4426/12/4/509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schell GJ, Marrero WJ, Lavieri MS, Sussman JB, Hayward RA. Data-driven markov decision process approximations for personalized hypertension treatment planning. MDM Policy Pract. 2016;1(1):2381468316674214. 10.1177/2381468316674214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shapey IM, Malik HZ, de Liguori Carino N. Data driven decision-making for older patients with hepatocellular carcinoma. Eur. J. Surg. Oncol. 2021, 47(3):748–7983. 576–82. 10.1016/j.ejso.2020.05.023. [DOI] [PubMed] [Google Scholar]
- 54.Singh S, Verma R, Koul S. A data-driven approach to shared decision-making in a healthcare environment. OPSEARCH. 2022. ISSN 0975-0320. 59(2):732–46. 10.1007/s12597-021-00543-3. [Google Scholar]
- 55.Suresh A, Udendhran R, Balamurgan M. Hybridized neural network and decision tree based classifier for prognostic decision making in breast cancers. Soft. Comput. 2020. 24(11):1433–7479. 7947–53. 10.1007/s00500-019-04066-4. [Google Scholar]
- 56.Szlejf C, Batista A, Bertola L, Lotufo P, Benseãor I, Filho AC, Suemoto C. Data-driven decision making for the screening of cognitive impairment in primary care: A machine learning approach using data from the elsa-brasil study. Braz J. Med. Biol. Res. 2023;56(e12475):100–879X. 10.1590/1414-431X2023e12475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tsoukalas A, Albertson T, Tagkopoulos I. From data to optimal decision making: A data-driven, probabilistic machine learning approach to decision support for patients with sepsis. JMIR Med. Inf. 2015;3(1):e11. 2291–9694. http://medinform.jmir.org/2015/1/e11/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Valdes G, Charles IS, B. JC, Lin A, Yom SS, Pattison AJ, Carpenter CM, Solberg TD. Clinical decision support of radiotherapy treatment planning: A data-driven machine learning strategy for patient-specific dosimetric decision making. Radiother Oncol. 2017. 125(3):167–8140. 392–97. 10.1016/j.radonc.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 59.Valente F, Paredes S, Henriques J, Rocha T, de Carvalho P, Morais J. Interpretability, personalization and reliability of a machine learning based clinical decision support system. Data Min Knowl. Discov. 2022. ISSN 1573-756X. 36(3):1140–73. 10.1007/s10618-022-00821-8. [Google Scholar]
- 60.Verboven L, Calders T, Callens S, Black J, Maartens G, Dooley KE, Potgieter S, Warren RM, Laukens K, Van Rie A. A treatment recommender clinical decision support system for personalized medicine: Method development and proof-of-concept for drug resistant tuberculosis. Bmc Med. Inform Decis. 2022;22(1):1472–6947. 56. 10.1186/s12911-022-01790-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu M, Hong L, Zhao Y, Chen L, Wang J. Dosage prediction in pediatric medication leveraging prescription big data. IEEE Access. 2019;7:94285–92. 10.1109/ACCESS.2019.2928457. [Google Scholar]
- 62.Xue M, Cao P, Hou B, Liu W. Data-driven decision-making with weights and reliabilities for diagnosis of thyroid cancer. Int. J. Mach. Learn Cybern. 2022;13(8):2257–2271. 1868–808X. 10.1007/s13042-022-01521-x. [Google Scholar]
- 63.Yee J, Low CY, Hashim NM, Zakaria NAC, Johar K, Othman NA, Chieng HH, Hanapiah FA. Clinical spasticity assessment assisted by machine learning methods and rule-based decision. Diagnostics. 2023;13(4):2075–4418. https://www.mdpi.com/2075-4418/13/4/739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhai K, Yousef MS, Mohammed S, Al-Dewik NI, Qoronfleh MW. Optimizing clinical workflow using precision medicine and advanced data analytics. Processes. 2023;11(3):2227–9717. https://www.mdpi.com/2227-9717/11/3/939 [Google Scholar]
- 65.Zhang K, Wang H, Du J, Chu B, Arévalo AR, Kindle R, Celi LA, Doshi-Velez F. An interpretable rl framework for pre-deployment modeling in icu hypotension management. NPJ Digit. Med. 2022. 2398-6352. 5(1):173. 10.1038/s41746-022-00708-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.van den Heuvel L, Dorsey RR, Prainsack B, Post B, Stiggelbout AM, Meinders MJ, Bloem BR. Quadruple decision making for parkinson’s disease patients: Combining expert opinion, patient preferences, scientific evidence, and big data approaches to reach precision medicine. J. Appl. Psychol Parkinson’s Disease. 2020. 10(1877–718X):223–31. 10.3233/JPD-1917121. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.