1. BACKGROUND
Cardiovascular disease (CVD) is a major cause of death among individuals with diabetes, 1 and comprehensive treatment—including the management of glucose, lipids and blood pressure—is essential to prevent complications. 2 , 3 While previous studies have emphasized medication adherence, they often overlook individuals who discontinue or irregularly attend medical care. 4 Large‐scale claims databases now allow assessment of adherence to physician visits even among those who do not consistently seek care, as long as they maintain insurance coverage. Such individuals are typically categorized as lost to follow‐up in hospital‐ or registry‐based studies and have been excluded from prior analyses. Notably, many individuals with newly diagnosed diabetes do not initiate follow‐up, 5 , 6 and even among those who begin follow‐up after health checkups, approximately 20%–30% discontinue. 7 Evidence on adherence to physician visits is important because poor adherence has been linked to adverse outcomes such as dialysis or infection. 8 , 9 , 10 A study revealed that more than half of patients on dialysis with diabetes had previously discontinued diabetes care, with over two‐thirds doing so for more than 5 years. 11 Therefore, the true impact of overall adherence to diabetes care—focusing on physician visits for diabetes care—on CVD complications remains unclear. This study aimed to examine whether good adherence to diabetes care is associated with a lower risk of CVD, using a nationwide administrative database with annual health checkup data and adjustment for various risk factors.
2. METHODS
We conducted a retrospective cohort study using the JMDC claims database, which includes health checkups and insurance claims from working‐age individuals in Japan. We included individuals aged 20–60 years with HbA1c ≥6.5% at a checkup, essential biomarker data and continuous insurance coverage during both the 12‐month look‐back and 12‐month exposure periods around the baseline checkup. Individuals with a history of outcomes or diseases closely related to or predisposing to CVD were excluded (Table S1). Follow‐up began at the end of the exposure period and continued until the earliest occurrence of an event, death or censoring (Figure S1).
Good adherence was defined as no gaps in physician visits for diabetes care exceeding 6 months during the 1‐year exposure period. Although this cutoff was used in a previous study 7 and is considered acceptable among individuals with diabetes who maintain good control of blood pressure and lipid levels without medication, 12 we performed sensitivity analyses using alternative definitions (see Supplementary Methods).
The primary outcome was a composite of CVD events, including myocardial infarction, stroke or death. Secondary outcomes included each component of the primary outcome and microvascular complications such as kidney failure requiring dialysis, surgery for diabetic retinopathy and limb amputation (Table S2).
Propensity‐score overlap weighting was used to adjust for confounders. Adjusted variables included sex, age, body mass index, blood pressure, waist circumference, HbA1c, lipid profiles, liver enzymes, serum creatinine, urinary protein, smoking, alcohol use, behavioural changes (transtheoretical model), sleep, diet and physical activity. These cover most of Life's Essential 8, defined by the American Heart Association as influential in CVD development. 13 Cox regression was used to estimate weighted hazard ratios. We also estimated the absolute risk reduction at 2 years of follow‐up and performed competing risks and sensitivity analyses (see Supplementary Methods).
3. RESULTS
From checkups conducted between 2008 and 2023, we included a total of 95 788 individuals after excluding 43 196 (Figure S2). Of these, 11 065 (11.6%) exhibited poor adherence to physician visits (Table S3). After applying overlap weighting, covariate distributions were confirmed to be balanced (Table S4).
During a mean follow‐up period of 3.1 years, 2982 individuals experienced the composite outcome. In the weighted analysis, we observed 257 events over 24 705 person‐years (10.4 per 1000 person‐years) among individuals with good adherence, and 216 events over 25 301 person‐years (8.5 per 1000 person‐years) among those without good adherence (Figure 1). After multivariable adjustment, good adherence was associated with a lower risk of the composite outcome (HR = 0.82; 95% CI: 0.72–0.93; p = 0.002) (Table 1). At 2 years of follow‐up, the estimated event risk was 1.61% among individuals with good adherence and 1.94% among those without good adherence, yielding an absolute risk reduction of 0.33%. Good adherence was also associated with reduced risks of stroke (HR = 0.76; 95% CI: 0.63–0.91) and microvascular complications, including limb amputation (HR = 0.33; 95% CI: 0.12–0.87).
FIGURE 1.
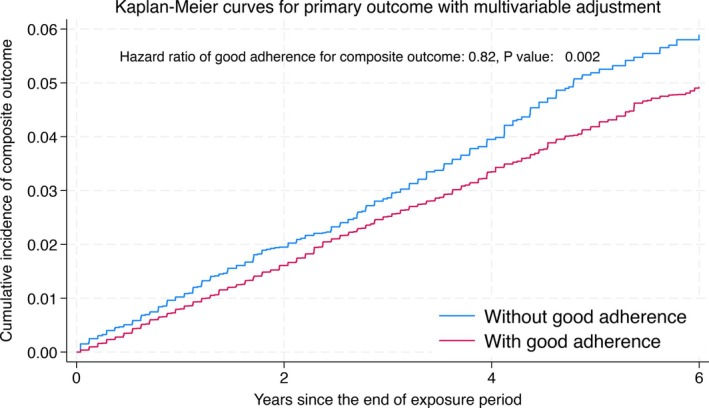
Kaplan–Meier curves for the cumulative incidence of the composite outcome, comparing individuals with and without good adherence to diabetes care. The analysis was adjusted using overlap weighting based on propensity scores. Individuals with good adherence had a lower risk of the composite outcome (hazard ratio = 0.82, p = 0.002).
TABLE 1.
Results for the primary and secondary outcomes.
| Analysis type | Outcome | HR of good adherence | 95% CI | p value |
|---|---|---|---|---|
| Primary | Composite | 0.82 | (0.72, 0.93) | 0.002 |
| Secondary | Myocardial infarction | 0.88 | (0.73, 1.05) | 0.142 |
| Stroke | 0.76 | (0.63, 0.91) | 0.003 | |
| Death | 0.75 | (0.50, 1.11) | 0.151 | |
| Kidney failure | 0.78 | (0.47, 1.31) | 0.343 | |
| Surgery for retinopathy | 0.89 | (0.75, 1.05) | 0.167 | |
| Limb amputation | 0.33 | (0.12, 0.87) | 0.025 | |
| Coronary surgery | 0.84 | (0.68, 1.04) | 0.118 | |
| Surgery for cerebral artery or tissue‐type plasminogen activator administration | 0.49 | (0.30, 0.81) | 0.006 |
| Outcome | SHR of good adherence | 95% CI | p value | |
|---|---|---|---|---|
| Competing‐risks analysis | Myocardial infarction | 0.88 | (0.73, 1.05) | 0.144 |
| Stroke | 0.76 | (0.63, 0.91) | 0.003 |
Abbreviations: CI, confidence interval; HR, hazard ratio; SHR, sub‐distribution hazard ratio.
Results of the stratified and sensitivity analyses are presented in Table S5 and Figure S4. Stratified analyses showed stronger associations among adults aged ≥51 years and those with HbA1c < 7.0%. Multiple sensitivity analyses supported the robustness of the primary findings (Table S5).
In supplementary analyses, we observed changes in biomarkers at the next checkups, stratified by adherence status. After applying overlap weighting with inverse probability of censoring weights (Table S6), the weighted results showed that individuals with good adherence had more favourable changes in HbA1c, triglycerides, low‐density lipoprotein cholesterol and blood pressure compared to those without good adherence (Table S7).
4. CONCLUSIONS
Using a large‐scale administrative claims database, we found that better adherence to diabetes care was associated with a lower incidence of CVD events, death and microvascular complications. These findings are consistent with prior research, including a randomized controlled trial in Japan 3 and a nationwide program in Korea. 2
Although the exact mechanisms remain uncertain, individuals with good adherence demonstrated improved HbA1c, blood pressure, triglycerides and low‐density lipoprotein cholesterol after the exposure period (Table S7). These sustained improvements in biomarkers—well‐known risk factors for CVD 3 —likely contributed to the lower event rates. Poor adherence may lead to clinical inertia, 14 reducing opportunities for timely intensification of blood pressure and lipid management, potentially increasing CVD risk.
The stratified analyses further support the clinical relevance of these findings. First, good adherence was associated with slightly greater benefits in older individuals, possibly due to accumulated effects over time, as adherence status tended to remain stable, particularly among those with good adherence. Moreover, the benefit appeared more pronounced in individuals with lower HbA1c levels, potentially because physicians treating those with HbA1c ≥ 7.0% may have prioritised glycaemic control over non‐glycaemic risk factors. This finding may underscore the importance of achieving HbA1c < 7%, as recommended in diabetes guidelines worldwide. 15
We acknowledge several limitations. First, the study may be subject to selection bias because we used an employer‐based insurance database in Japan, which may limit the generalisability of the findings to other populations or insurance systems. Second, although we adjusted for >50 confounders, residual confounding by unmeasured factors—such as socioeconomic status or dietary salt/sugar intake—may have resulted in misclassification. Third, as an observational study, causal inference is limited, and the specific effects of medication adherence or lipid and blood pressure management cannot be estimated. Future prospective studies are warranted to evaluate these effects separately. Fourth, the limited number of events in subgroup analyses may have led to insufficient power, potentially contributing to the lack of statistically significant results. Lastly, time‐varying confounding may have influenced our results despite our sensitivity analyses, including a per‐protocol approach.
In this observational study, we found an association between good adherence to diabetes care and a lower incidence of CVD or death. While our findings suggest the potential value of adherence in preventing adverse outcomes, the effectiveness of behavioural interventions remains to be established. Future interventional studies are warranted to examine whether promoting adherence can improve clinical outcomes.
AUTHOR CONTRIBUTIONS
A.O., Y.O., H.Y. and S.Y. conceived and designed the study, performed the statistical analysis and wrote, edited and reviewed the manuscript. R.I., Y.H., K.I.K., M.N., T.Y. and T.K. contributed to the discussion and interpretation of the data and edited and reviewed the manuscript. All authors have approved the final manuscript for publication. S.Y. is the guarantor of this work and, as such, had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
CONFLICT OF INTEREST STATEMENT
A.O., Y.O., R.I., S.Y., K.I.K. and T.K. are members of the Department of Prevention of Diabetes and Lifestyle‐Related Diseases, which is a cooperative program between The University of Tokyo and Asahi Mutual Life Insurance Company. Y.O. is currently employed by the Asahi Mutual Life Insurance Company, and K.I.K. was previously employed by the Asahi Mutual Life Insurance Company.
PEER REVIEW
The peer review history for this article is available at https://www.webofscience.com/api/gateway/wos/peer-review/10.1111/dom.16479.
Supporting information
Data S1. Supporting information.
ACKNOWLEDGEMENTS
This study was supported by Grants for young researchers from Japan Association for Diabetes Education and Care (2024‐YNG‐031).
Okada A, Otsuka Y, Inoue R, et al. Adherence to physician visits for diabetes care and cardiovascular disease risk: A retrospective cohort study using an administrative claims database. Diabetes Obes Metab. 2025;27(8):4590‐4593. doi: 10.1111/dom.16479
Akira Okada and Yusuke Ostuka contributed equally to this article as co‐first authors.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from JMDC. Inc. Restrictions apply to the availability of these data, which were used under license for this study. Data could be available with the permission of JMDC Inc.
REFERENCES
- 1. Weir MR. Cardiovascular risk reduction in type 2 diabetes: what the non‐specialist needs to know about current guidelines. Diabetes Obes Metab. 2024;26(S5):14‐24. [DOI] [PubMed] [Google Scholar]
- 2. Huh JH, Kwon S, Kim GO, Kim BY, Ha KH, Kim DJ. Long‐term effectiveness of the National Diabetes Quality Assessment Program in South Korea. Diabetes Care. 2023;46(9):1700‐1706. [DOI] [PubMed] [Google Scholar]
- 3. Ueki K, Sasako T, Okazaki Y, et al. Effect of an intensified multifactorial intervention on cardiovascular outcomes and mortality in type 2 diabetes (J‐DOIT3): an open‐label, randomised controlled trial. Lancet Diabetes Endocrinol. 2017;5(12):951‐964. [DOI] [PubMed] [Google Scholar]
- 4. Evans M, Engberg S, Faurby M, Fernandes J, Hudson P, Polonsky W. Adherence to and persistence with antidiabetic medications and associations with clinical and economic outcomes in people with type 2 diabetes mellitus: a systematic literature review. Diabetes Obes Metab. 2022;24(3):377‐390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Matsumura H, Sugiyama T, Sakata N, et al. Proportion of subsequent clinic visits among persons without regular clinic visits who were screened as having hyperglycemia: a retrospective cohort study. J Diabetes Investig. 2023;14(5):695‐706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Okada A, Hashimoto Y, Goto T, et al. A machine learning‐based predictive model to identify patients who failed to attend a follow‐up visit for diabetes care after recommendations from a national screening program. Diabetes Care. 2022;45(6):1346‐1354. [DOI] [PubMed] [Google Scholar]
- 7. Okada A, Ono S, Yamaguchi S, et al. Association between nutritional guidance or ophthalmological examination and discontinuation of physician visits in patients with newly diagnosed diabetes: a retrospective cohort study using a nationwide database. J Diabetes Investig. 2021;12(9):1619‐1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li H, Tian S, Chen T, et al. Newly diagnosed diabetes is associated with a higher risk of mortality than known diabetes in hospitalized patients with COVID‐19. Diabetes Obes Metab. 2020;22(10):1897‐1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Uchihara M, Sugiyama T, Bouchi R, et al. Association of acute‐to‐chronic glycemic ratio and outcomes in patients with COVID‐19 and undiagnosed diabetes mellitus: a retrospective nationwide cohort study. J Diabetes Investig. 2023;14(4):623‐629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Okada A, Yamaguchi S, Ono S, et al. Modification effect of receipt of diabetes care on the association between COVID‐19 infection and HbA1c level during the first year of the coronavirus pandemic using a nationwide population‐based database. J Diabetes Investig. 2024;15(7):953‐963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arakawa Y, Ishida Y, Higa A, Tana T, Iseki K. Clinical characteristics of diabetic patients who were started on dialysis at the age of <60 years: a questionnaire‐based study conducted in Okinawa. Nihon Toseki Igakkai Zasshi. 2019;52(2):93‐100. [Google Scholar]
- 12. Morrison F, Shubina M, Turchin A. Encounter frequency and serum glucose level, blood pressure, and cholesterol level control in patients with diabetes mellitus. Arch Intern Med. 2011;171(17):1542‐1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lloyd‐Jones DM, Allen NB, Anderson CAM, et al. Life's essential 8: updating and enhancing the American Heart Association's construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation. 2022;146(5):e18‐e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Augustin A, Coutts L, Zanisi L, et al. Impact of therapeutic inertia on long‐term blood pressure control. Hypertension. 2021;77(4):1350‐1359. [DOI] [PubMed] [Google Scholar]
- 15. Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2022;65(12):1925‐1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information.
Data Availability Statement
The data that support the findings of this study are available from JMDC. Inc. Restrictions apply to the availability of these data, which were used under license for this study. Data could be available with the permission of JMDC Inc.


