Abstract
Mitochondrial-supported bioenergetics decline and oxidative stress increases during aging. To address whether the dietary addition of acetyl-l-carnitine [ALCAR, 1.5% (wt/vol) in the drinking water] and/or (R)-α-lipoic acid [LA, 0.5% (wt/wt) in the chow] improved these endpoints, young (2–4 mo) and old (24–28 mo) F344 rats were supplemented for up to 1 mo before death and hepatocyte isolation. ALCAR+LA partially reversed the age-related decline in average mitochondrial membrane potential and significantly increased (P = 0.02) hepatocellular O2 consumption, indicating that mitochondrial-supported cellular metabolism was markedly improved by this feeding regimen. ALCAR+LA also increased ambulatory activity in both young and old rats; moreover, the improvement was significantly greater (P = 0.03) in old versus young animals and also greater when compared with old rats fed ALCAR or LA alone. To determine whether ALCAR+LA also affected indices of oxidative stress, ascorbic acid and markers of lipid peroxidation (malondialdehyde) were monitored. The hepatocellular ascorbate level markedly declined with age (P = 0.003) but was restored to the level seen in young rats when ALCAR+LA was given. The level of malondialdehyde, which was significantly higher (P = 0.0001) in old versus young rats, also declined after ALCAR+LA supplementation and was not significantly different from that of young unsupplemented rats. Feeding ALCAR in combination with LA increased metabolism and lowered oxidative stress more than either compound alone.
Harmon, Miguel, and others (1, 2) postulated that mitochondrial decay is a significant factor in aging, caused, in part, by the release of reactive oxygen species (ROS) as by-products of mitochondrial electron transport. Mitochondria are targets of their own oxidant by-products. The steady-state oxidative damage in mitochondria is high relative to other organelles, and the percentage of oxygen converted to superoxide increases with age (3–6). This leads to a vicious cycle of increasing mitochondrial damage, which adversely affects cell function (7), and results in a loss of ATP-generating capacity, especially in times of greater energy demand, thereby compromising vital ATP-dependent reactions. Cellular processes affected by mitochondrial decay include detoxification, repair systems, DNA replication, osmotic balance, and higher-order processes (7), such as cognitive function (7–9). Thus, preservation of mitochondrial function is important for maintaining overall health during aging (7). This theory is buttressed by the observation that caloric restriction, the only known regimen to increase mean life span in animals, maintains mitochondrial function and lowers oxidant production (7, 8, 10–12). A spartan diet of calorie restriction appears to be too unappealing to be widely adopted in humans, and thus other alternative regimens to improve or maintain normal mitochondrial activities have been sought.
Several dietary supplements, including the mitochondrial cofactor and antioxidant lipoic acid (LA), increase endogenous antioxidants or mitochondrial bioenergetics (13–15). Feeding old rats acetyl-l-carnitine (ALCAR), a mitochondrial metabolite, reverses the age-related decline in tissue carnitine levels and improves mitochondrial fatty acid β-oxidation in the tissues studied (15–18). ALCAR supplementation also reverses the age-related alterations in fatty acid profiles and loss in cardiolipin levels, an essential phospholipid required for mitochondrial substrate transport (15–17). We demonstrated that ALCAR supplementation reverses the age-associated decline in metabolic activity in rats, suggesting that ALCAR improves mitochondrial function and increases general metabolic activity (19, 20). ALCAR-induced improvement in metabolic parameters appear to be responsible for improving short-term memory deficits and cognitive function in elderly subjects given ALCAR (21, 22) and in old rats (9).
This increased metabolic activity may come at a price, however, because supplementing rats with high levels of ALCAR lowered hepatocellular antioxidant status (19). This ALCAR-induced antioxidant loss was not seen, however, in other organs (T.M.H. and D. Heath, unpublished work) or when lower doses were given (23). We also showed that giving high [1.5% (wt/vol)], but not lower [0.5% (wt/vol)], supplemental doses of ALCAR to old rats increased mitochondrial oxidant flux, suggesting that while high ALCAR supplementation may increase electron flow through the electron transport chain, it also heightens formation of ROS as a consequence. We thus hypothesized that ALCAR supplemented with an antioxidant may have the salutary effect of increasing mitochondrial function and general metabolic activity without a concomitant increase in oxidative stress. We chose LA as a cosupplement for two reasons: (i) it is a naturally occurring cofactor for mitochondrial α-keto acid dehydrogenases (24), which may aid in cellular glucose-dependent ATP production (25); and (ii) in its reduced form, LA is a potent antioxidant and also increases intracellular ascorbate and glutathione concentrations (15, 26). Thus, LA and ALCAR may act together to reverse age-related metabolic decline and also reduce indices of oxidative stress.
We show that the combined supplementation of ALCAR and LA (ALCAR+LA) reverses age-related metabolic decline, improves hepatocellular ascorbate levels, and lowers oxidant appearance and oxidative damage.
Materials and Methods
The following chemicals were used: EGTA, trypan blue, glutathione, heparin (sodium salt), and rhodamine 123 (R123) (Sigma); 2′7′-dichlorofluorescin diacetate (Molecular Probes); collagenase (type D) (Roche Molecular Biochemicals); and LA and meta-phosphoric acid (Fluka). ALCAR was a gift of Sigma Tau (Pomezia, Italy) and purchased from Aldrich. LA was a gift from Hans Tritschler, Asta Medica, Frankfurt. All other reagents were reagent grade or better. Double-distilled/deionized water was used throughout.
Rats (Fischer 344, virgin male, outbred albino) (3–5 mo) were obtained from Simonsen Laboratories (Gilroy, CA). Old rats (identical strain; 20–28 mo) were from the National Institute on Aging animal colonies. All animals were fed Purina rodent chow and water ad libitum. There was no discernable difference in food consumption in ALCAR vs. untreated rats. All animals were acclimatized at the Northwest Animal Facilities at the University of California at Berkeley for at least 1 week before experimentation.
ALCAR Supplementation.
Old and young rats were given a 1.5% (wt/vol; pH adjusted to ≈6) solution of ALCAR in their drinking water and allowed to drink ad libitum for 1 mo before death and hepatocyte isolation. Both young and old rats typically drank ≈20 ml/rat per day (data not shown), which provided a daily ALCAR dose of ≈0.75 g/kg body wt per day for old rats and 1.2 g/kg body wt per day for young rats. All animal experiments were done with appropriate Animal Use Committee clearances.
LA Supplementation.
Young and old rats were given LA [0.5% (wt/wt)] mixed into the AIN-93M chow (Dyets, Bethlehem, PA) for 2 weeks before death. Unsupplemented animals were fed Purina rodent chow and water ad libitum. The pellets were made into a mush and fed to some young and old rats for 2 weeks before cell isolation. Both young and old rats typically ate ≈15 g/rat per day (data not shown), which provides a daily LA dose of 0.12 g/kg body weight for young rats and 0.075 g/kg body weight for old rats.
Cell Isolation.
Liver tissue was dispersed into single cells by collagenase perfusion (27). Cell number was assessed by using a hemocytometer, and viability was determined by trypan blue exclusion. Viability was usually more than 90% in both age groups.
Flow Cytometry.
Hepatocytes (2.0 × 106 cells) were incubated with R123 (0.01 mg/ml) for 30 min at 37°C and then subjected to flow cytometry (described in ref. 20).
Assay of Oxidants with 2′7′-Dichlorofluorescin Diacetate.
Formation of oxidants in cells was determined by fluorescence over time by using 2′7′-dichlorofluorescin diacetate, a reduced, nonfluorescent derivative of fluorescein (28). Quadruplicate samples were routinely analyzed. Fluorescence was monitored by using a Cytofluor 2350 fluorescent measurement system (Millipore) with standard fluorescein filters and cytocalc software. Because the majority of cells from old rats consume oxygen at lower rates than cells from young animals (20), the rate of oxidant production was normalized to the level of oxygen consumed. Cellular oxygen consumption was measured by using a Yellow Springs Instruments 5300 oxygen electrode and monitor. Cells (4.0 × 106) were added to 3 ml of Krebs–Henseleit balanced salt medium supplemented with 1 mM glucose and 7 mM glutamate, pH 7.4, that had been previously equilibrated to 20°C, and oxygen consumption was monitored for at least 15 min.
Ascorbate Analysis.
Ascorbic acid analysis was performed as described (29). Briefly, samples were acidified with meta-phosphoric acid (10% wt/vol) and mixed with 50 μl of 200 mM Trizma buffer (Sigma), pH 9.0, giving a sample pH of about 2.5. The samples were placed in a chilled (2°C) auto sampler for analysis. The system used for separation was reversed-phase HPLC (Hewlett–Packard) with coulometric detection (ESA, Bedford, MA). The peak area corresponding to ascorbic acid was integrated by using Hewlett–Packard chemstation software and compared with a standard curve based on authentic material.
Malondialdehyde (MDA) Measurement.
Lipid peroxidation was assayed by using a gas chromatography-MS method for MDA (30, 31). Briefly, hepatocytes were lysed with PBS containing 2.8 mM butylated hydroxytoluene and 1% (wt/vol) SDS, pH 7.4. The protein-bound MDA was hydrolyzed with H2SO4. MDA was converted to a stable derivative by using pentafluorophenyl hydrazine (room temperature). The derivative was detected with a Hewlett–Packard 5890 Series II gas chromatograph interfaced to a 5989 MS system equipped with a J & W Scientific (Folsom, CA) DBWAX capillary column (15 m × 0.25 mm i.d., 0.25-μm film thickness) in the negative chemical ionization mode. The results were indexed to protein, which was measured by using the BCA protein assay kit (Pierce).
Activity Tests.
Ambulatory activity was monitored as described (18). Briefly, each night rats were moved from group housing to individual cages (48 cm l × 25 cm w × 20 cm h) at least 4 h before the quantification of ambulatory parameters. The room was on a 12 h light/dark cycle (lights on 6 a.m. to 6 p.m.). At 8 p.m. dim light illuminated the test subjects for video tracking. Quantification began at 9 p.m. and continued for 4 h. One hour later the low light turned off, and the room remained in total darkness until 6 a.m. when the standard light/dark cycle lighting began. A video signal from a camera suspended directly above the individual cages was fed directly into a Videomex-V (Columbus Instruments, Columbus, OH) computer running the multiple objects multiple zones software. The system quantified ambulatory activity parameters and was calibrated to report distance traveled in cm. In addition to total distance traveled, the time each subject spent in ambulatory (locomotor), stereotypic (grooming), and resting (nonmovement) activity was recorded and dumped in hourly segments to an IBM computer. This hourly data were recorded by the Videomex-V multiple objects multiple zones monitoring software. At 9 a.m. animals were removed from individual housing and returned to group housing. Before ALCAR+LA supplementation and for 2 consecutive nights, the ambulatory activity of each rat was recorded. After ALCAR+LA supplementation and for 2 consecutive nights, the same spontaneous locomotor parameters were determined. Each rat served as its own control.
Statistical Analysis.
Statistical significance was determined by using the paired two-tailed Student's t test or single factor ANOVA. Results are expressed as the mean ± SE.
Results
Measurement of Cellular and Physiological Parameters of Metabolic Activity.
To determine whether cosupplementation of ALCAR+LA improved general parameters of physiological activity, a series of experiments were performed to monitor indices of cellular and whole animal metabolism.
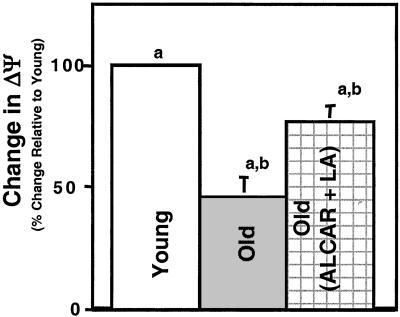
We previously showed significantly lower average mitochondrial membrane potential (ΔΨ) in the majority of hepatocytes from old rats compared with young rats, but a 1-mo feeding regimen of 1.5% (wt/vol) ALCAR reversed this decline in ΔΨ (19). For the present study, we also found a marked age-related decline in this key parameter of mitochondrial function (Fig. 1). Relative to mean fluorescence characteristics seen in hepatocytes from young unsupplemented animals, the average ΔΨ for hepatocytes from old rats was 53.8 ± 8.0% lower (n = 5), representing a significant loss (P = 0.02). Feeding ALCAR+LA to old rats markedly reversed this decline (Fig. 1). Old rats on the ALCAR+LA supplemented diet had an average ΔΨ that was only 22.8 ± 6.0% lower relative to young unsupplemented rats. Thus, dietary supplementation with ALCAR+LA partially restored the loss of mitochondrial ΔΨ although the improvement was not as great as previously observed with ALCAR alone (19).
Figure 1.
Dietary supplementation of ALCAR+LA partially reverses the age-related decline in average mitochondrial ΔΨ. Rats were fed ALCAR+LA as described, and average hepatocellular ΔΨ was assessed by using R123. Results showed that average ΔΨ was significantly lower in cells from old animals relative to young. However, ALCAR+LA supplementation significantly increased average ΔΨ over that seen in unsupplemented old rats. Columns denoted by the same letter are statistically different (P ≤ 0.05) from each other.
We previously showed in separate reports that ALCAR or LA supplementation increased hepatocellular and myocardial oxygen consumption, indicating that either compound was able to increase cellular metabolism (18, 19). Young and old rats were supplemented with or without ALCAR+LA before cell isolation, and this general parameter of metabolic rate was monitored by using an oxygen electrode. Hepatocellular oxygen consumption declined from 1.03 ± 0.17 (n = 5) to 0.54 ± 0.09 μmol/min per 106 cells (n = 5) in young versus old unsupplemented rats, a significant (P = 0.03) decline of 47.6% with age. These results are in agreement with our previous results and suggest that there is an age-related decline in hepatocellular metabolic rate. Oxygen consumption in hepatocytes from old rats treated with ALCAR+LA was 0.82 ± 0.07 μmol O2/min per 106 cells versus 0.95 ± 0.05 μmol/min per 106 in unsupplemented (n = 5) young rats (P = 0.02). Thus, feeding ALCAR+LA to old rats significantly reversed the age-related decline in hepatocellular oxygen consumption.
Ambulatory Activity.
To further explore whether ALCAR+LA generally improved metabolic rate on a whole animal basis, we studied ambulatory activity in animals fed with or without ALCAR+LA. Old rats exhibited a 3-fold decline in ambulatory activity in terms of overall movement and the amount of time spent in movement (Table 1). The speed of old animals when in movement was not different from that shown by young animals, suggesting that the age-related decline in activity was not caused by pain or the inability to move, but rather it reflected a general loss of metabolic activity.
Table 1.
Ambulatory activity in rats fed with or without ALCAR+LA
| Young | Old | Percent difference | |
|---|---|---|---|
| Ambulatory activity before ALCAR+LA supplementation | |||
| Distance (cm/h) | 528 ± 43 | 177 ± 19 | −66.5 |
| Ambulation (s) | 58 ± 5 | 20 ± 2 | −65.0 |
| Resting (s) | 1,463 ± 94 | 1,717 ± 73 | 17.4 |
| Speed (cm/s) | 9.1 ± 0.2 | 8.6 ± 0.2 | — |
| Ambulatory activity after ALCAR+LA supplementation | |||
| Distance (cm/h) | 693 ± 60 | 376 ± 23 | −45.7 |
| Ambulation (s) | 76 ± 7 | 43 ± 3 | −43.4 |
| Resting (s) | 1,397 ± 55 | 1,982 ± 60 | 41.8 |
| Speed (cm/s) | 9.2 ± 0.1 | 8.8 ± 0.1 | — |
| Percent change (pre- versus post-ALCAR+LA supplementation) | |||
| Distance | 31.3 | 112.4 | |
| Ambulation | 31.0 | 115.0 | |
| Resting | −4.5 | 15.4 | |
| Speed | 1.1 | 2.3 | |
Animals were then fed ALCAR+LA for 1 mo (in the case of LA 2 weeks) and again tested for ambulatory activity. Results show that ALCAR+LA significantly improved ambulatory activity in young and old animals. For the young animals, the amount of active time and the overall distance traveled increased by ≈31% when compared with their activity before ALCAR+LA supplementation. A much greater increase was observed in old rats. Ambulation and overall distance traveled more than doubled from 20 ± 2 s per movement and 177 ± 19 cm/h to 43 ± 3 s per movement and 376 ± 23 cm/h, respectively. This increase, although still not as good, on average, as young untreated rats, nevertheless represented a significant (P = 0.03) improvement versus that of old untreated animals. Thus, ALCAR+LA supplementation not only reverses the age-related decline in oxygen consumption, a cellular parameter of metabolic activity, but also increases ambulatory activity, a general physiological parameter of metabolic activity.
Antioxidant Status/Oxidative Stress.
We previously observed that feeding 1.5% (wt/vol) ALCAR alone to old rats, although markedly increasing metabolic activity through improved mitochondrial function, also resulted in heightened oxidant production and decreased low molecular weight antioxidant status. This finding was presumably caused by increased formation of ROS/reactive nitrogen species as by-products of heightened metabolic activity. To understand whether feeding ALCAR+LA could ameliorate this potential increase in oxidative stress, we measured ascorbic acid status, overall oxidant production, and markers of oxidative damage in freshly isolated hepatocytes taken from young and old rats fed with or without ALCAR+LA.
Hepatocytes from old rats had significantly lower ascorbate levels as compared with young rats (7.29 ± 2.97 versus 3.38 ± 0.67; P = 0.003) (Fig. 2), suggesting that liver antioxidant status may be compromised with age. We observed, as previously, that ALCAR supplementation at 1.5% (wt/vol) resulted in a further and significant decline in ascorbate levels beyond the observed age-related loss in this key antioxidant. However, ALCAR+LA supplementation reversed the ALCAR-induced and age-related loss of ascorbate such that there was no longer a significant difference (P = 0.3) in hepatocellular ascorbate values between ALCAR+LA-treated old rats and that of untreated young animals (Fig. 2).
Figure 2.
LA supplementation reverses the ALCAR-induced and age-related decline in hepatocellular ascorbate levels. Hepatocytes (1.0 × 106 cells) were hydrolyzed in 10% (wt/vol) metaphosphoric acid, and the ascorbate content in the supernatant was analyzed by HPLC with electrochemical detection (31). Results show that old rats had significantly lower hepatocellular ascorbate concentrations than cells isolated from young animals. For rats fed 1.5% (wt/vol) ALCAR, ascorbate levels in hepatocytes from both young and old rats were significantly lower than corresponding controls (not shown). Cosupplementation of LA with ALCAR negated both the age-related and ALCAR-induced decline in hepatocellular ascorbate concentrations. Columns denoted by the same letter are statistically different (P ≤ 0.05) from each other.
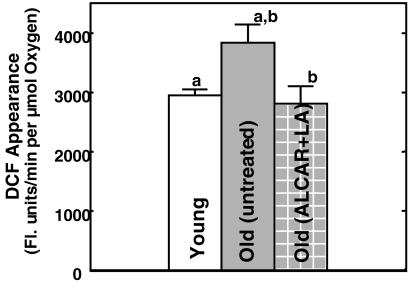
To further investigate whether ALCAR+LA actually affected oxidative stress parameters in old rats, hepatocellular oxidant production was monitored by using 2′,7′-dichlorofluorescin oxidation. This cell permeant dye becomes fluorescent when it is oxidized. Thus, general oxidant production can be monitored in cells by measuring the rate of increased fluorescence over time. Cells isolated from young and old rats exhibited a marked difference in fluorescence appearance (Fig. 3). Oxidant production increased over 30.8% with age from 2,942.3 ± 99.3 to 3,835.22 ± 303.6 fluorescence units/min per μmol O2 consumed per 106 cells. This finding is in agreement with our previously published results (18) and is consistent with lower antioxidant status and heightened mitochondrial oxidant production during aging. Addition of ALCAR+LA to the diet of old rats caused a significant decline in appearance of oxidants to 2,801.79 ± 308.0 fluorescence units/min per μmol O2 consumed per 106 cells, which was not different from untreated or ALCAR+LA-fed young rats. Thus, the combination of ALCAR with LA not only reverses the age-related increase in oxidants, but also the additional oxidants induced by high doses of ALCAR. These results suggest that ALCAR+LA supplementation not only improves metabolic rate and physiological activity, but does so without causing a concomitant increase in oxidants.
Figure 3.
ALCAR+LA supplementation lowers 2,′7′-dichlorofluorescin (DCF) appearance. Young and old rats were treated with or without ALCAR+LA, and hepatocytes were isolated as described. Cells (40,000) were incubated with dichlorofluorescin diacetate (20 μM, final concentration), and the rate of fluorescence appearance was measured by using a Cytofluor fluorescent plate reader (as described in Materials and Methods). Because of the difference in oxygen consumption characteristics, all rates of fluorescence were expressed in relation to oxygen consumption. Results show that ALCAR+LA supplementation significantly lowered the age-related increase in DCF appearance, indicating lower ROS and/or reactive nitrogen species in hepatocytes under this feeding regimen. Columns denoted by the same letter are statistically different (P ≤ 0.05) from each other.
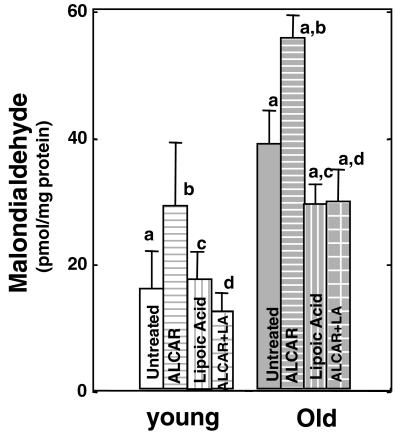
To further assess whether ALCAR+LA modulated age-related and ALCAR-induced oxidative stress, we also measured steady-state levels of MDA, a marker of lipid peroxidation (Fig. 4). Hepatocellular MDA levels in old untreated rats were more than 4-fold higher than the levels seen in young rats, a significant increase (P = 0.0001). Similar to results shown for oxidant production, we observed a small, but significant, increase in steady-state MDA levels in liver tissue from old rats fed ALCAR alone (Fig. 4); on average, a similar increase in young rats was not significant. These results again suggest that high ALCAR alone, although improving metabolism and cognitive function, also increased oxidative stress in the liver. When LA was given along with ALCAR, we observed that there was a significant decline in MDA levels (Fig. 4). Most importantly, hepatic MDA concentrations in old ALCAR+LA fed rats no longer statistically differed from those found in young untreated animals.
Figure 4.
ALCAR+LA supplementation significantly lowers the steady-state age-related accumulation of lipid peroxidation. MDA, a marker of lipid peroxidation, was measured by gas chromatography/MS as described (29, 30). Results show no statistical increase (P ≥ 0.05) in MDA levels with ALCAR, LA, or both supplements in liver tissue from young animals. MDA levels were significantly increased in liver from old rats relative to young controls, and ALCAR supplementation alone further increased hepatic MDA content over that of nonsupplemented old rats. LA alone and ALCAR+LA supplementation significantly decreased hepatic MDA content in livers from old rats. Columns denoted by the same letter are statistically different (P ≤ 0.05) from each other.
Discussion
We previously demonstrated that feeding old rats ALCAR markedly improves the average mitochondrial membrane potential, a key indicator of mitochondrial function, to a level no longer significantly different from that of young rats (18). This reversal of membrane potential appears to be caused, in part, by replenishment of carnitine, a betaine that shuttles fatty acids into the mitochondrion for β-oxidation. ALCAR administration also appears to reverse the age-related decline in cardiolipin levels. Cardiolipin is a key phospholipid cofactor for a number of mitochondrial substrate transporters as well as the protein complexes in the electron transport chain. Thus, age-related decline in cardiolipin could profoundly and adversely affect mitochondria.
Our results, in combination with studies by Hagen, Paradies, Gadaleta, and others (15, 16), clearly demonstrate that ALCAR improves metabolic function in a number of tissues, most likely by improving substrate and electron flux through mitochondria.
ALCAR does not, however, improve one aspect of mitochondrial decay in old rats, namely, the age-related increase in oxidants. Electron transfer through the mitochondrial electron transport chain becomes less efficient with age, which leads to increased oxidant leakage. ALCAR at the 1.5% level used in our initial experiments appears to increase electron flow through the electron transport chain, which further increases the appearance of ROS. In support of this concept, we observed higher oxidant appearance and lower hepatocellular antioxidant status after ALCAR supplementation (18). Feeding 1.5% ALCAR to old rats improved the age-related decline in metabolic rate, but increased oxidant appearance to a small, yet significant, degree. This ALCAR-induced increase in hepatocellular oxidative stress may be unique to the liver or caused by the relatively high levels of ALCAR used in this feeding study. In recent studies where old rats were fed 1.5% ALCAR, we did not observe any ALCAR-induced increased oxidative stress in the heart but saw a significant improvement in mitochondrial function and cellular metabolism (T.M.H., J. Suh, and D. Heath, unpublished results). In other studies using lower ALCAR doses [0.5% (wt/vol)], Liu et al. (22) noted no ALCAR-induced changes in parameters of oxidative stress in rat brain, yet found that this dose significantly improved cognitive function in aged animals (9). Thus, smaller doses of ALCAR may effectively improve metabolic function without higher oxidative stress.
The rationale for the present study was to determine whether other mitochondrial metabolites fed along with ALCAR could improve metabolic parameters and lower the age-related increase in oxidative stress. We chose to cosupplement LA with ALCAR because LA is easily taken up into a variety of tissues and can be reduced to a powerful antioxidant, dihydrolipoic acid (23). Even though LA/dihydrolipoic acid is quickly removed from most cells, this compound also induces cystine/cysteine uptake and can thereby increase glutathione synthesis (25). LA supplementation maintains and actually reverses the age-related decline in hepatocellular and myocardial ascorbate and glutathione levels, even when cells were incubated with tert-butylhydroperoxide, a model alkyl peroxide (32, 33). Thus, LA may not only act synergistically with ALCAR to improve mitochondrial-supported bioenergetics but may also improve general antioxidant status, which declines with age.
LA elicits other cell responses that may complement the actions of ALCAR on the cell. LA enhances glucose uptake by increasing glucose transporters at the surface of cells (24). It is also a cofactor for α-keto acid dehydrogenases found in the mitochondria, and its supplementation in the diet of aging animals may thus correct any age-associated decline in α-ketoglutarate dehydrogenase and pyruvate dehydrogenase caused by lost cofactors. Humphries and Szweda (34) showed that pyruvate dehydrogenase and α-ketoglutarate dehydrogenase can be modified by adduction with 4-hydroxy-nonenal (R. Moreau and T. M. Hagen, personal communication), rendering it unable to transfer acetyl groups. MDA and 4-hydroxy-nonenal also inactivate carnitine acyltransferase and decrease the binding affinity for substrates (35). Thus, LA may act synergistically with ALCAR to improve both fatty acid and glucose catabolism and energy production. Indeed, we have previously shown that LA alone also increases oxygen consumption and mitochondrial membrane potential, although not as effectively as ALCAR (14).
Supplementing the diet of old rats with ALCAR+LA significantly improves many of the most frequently encountered age-related changes in mammals—namely loss of energy metabolism, increased oxidative stress, decreased physical activity, and as shown in ref. 9, impaired cognitive function. This affect on cognitive function has been previously observed for both ALCAR and LA (36), but to our knowledge, has not been observed for the combination of the two supplements. How ALCAR and LA affect short-term memory is not well understood, but may be caused by a number of factors, including increased neurotransmitter production, improved mitochondrial function, and/or calcium handling by the neuron (20, 21, 36). We have also recently found that LA alone significantly reduces the age-related accumulation of iron and copper in the brain (J. H. Suh, personal communication). Thus, the LA component may also increase neuro-cognitive function by potentially lowering iron and copper-induced oxidative stress.
Presently, only short-term feeding regimens of ALCAR+LA have been given to aged animals. The present study suggests that long-term feeding experiments are warranted to monitor how effectively ALCAR+LA supplementation ameliorates oxidative stress, loss of metabolic function, and mild cognitive impairment seen in older animals. In this regard, it is of interest that many of the cellular effects of caloric restriction, which does increase lifespan, are also affected by ALCAR+LA supplementation.
Acknowledgments
We thank Steve Lawson (Linus Pauling Institute) for comments on this manuscript. This study was supported by National Institutes of Health Grants P30-ES01896 and AG17140, Ellison Medical Foundation Grant SS-0422–99, Department of Energy Grant 00ER62943, Bruce and Giovanna Ames Foundation grants (to B.N.A.), and National Institutes of Health Grant AG17141 (to T.M.H.).
Abbreviations
- ALCAR
acetyl-l-carnitine
- LA
lipoic acid
- MDA
malondialdehyde
- ROS
reactive oxygen species
References
- 1.Miquel J, Economos A C, Fleming J, Johnson J E. Exp Gerontol. 1980;15:575–591. doi: 10.1016/0531-5565(80)90010-8. [DOI] [PubMed] [Google Scholar]
- 2.Harmon D. J Am Geriatr Soc. 1972;20:145–147. doi: 10.1111/j.1532-5415.1972.tb00787.x. [DOI] [PubMed] [Google Scholar]
- 3.Sohal R S, Sohal B H. Mech Ageing Dev. 1991;57:187–202. doi: 10.1016/0047-6374(91)90034-w. [DOI] [PubMed] [Google Scholar]
- 4.Sohal R S, Sohal B H, Orr W C. Free Radical Biol Med. 1995;19:499–504. doi: 10.1016/0891-5849(95)00037-x. [DOI] [PubMed] [Google Scholar]
- 5.Perez-Campo R, Lopez-Torres M, Cadenas S, Rojas C, Barja G. J Comp Physiol. 1998;168:149–158. doi: 10.1007/s003600050131. [DOI] [PubMed] [Google Scholar]
- 6.Sastre J, Pallardo F V, Vina J. IUBMB Life. 2000;49:427–435. doi: 10.1080/152165400410281. [DOI] [PubMed] [Google Scholar]
- 7.Beckman K B, Ames B N. Physiol Rev. 1998;78:547–581. doi: 10.1152/physrev.1998.78.2.547. [DOI] [PubMed] [Google Scholar]
- 8.Shigenaga M K, Hagen T M, Ames B N. Proc Natl Acad Sci USA. 1994;91:10771–10778. doi: 10.1073/pnas.91.23.10771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu J, Head E, Gharib A M, Yuan W, Ingersoll R T, Hagen T M, Cotman C W, Ames B N. Proc Natl Acad Sci USA. 2002;99:2356–2361. doi: 10.1073/pnas.261709299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee C K, Klopp R G, Weindruch R, Prolla T A. Science. 1999;285:1390–1393. doi: 10.1126/science.285.5432.1390. [DOI] [PubMed] [Google Scholar]
- 11.Lee J, Yu B P, Herlihy J T. Free Radical Biol Med. 1999;26:260–265. doi: 10.1016/s0891-5849(98)00195-6. [DOI] [PubMed] [Google Scholar]
- 12.Merry B J. Ann NY Acad Sci. 2000;908:180–198. doi: 10.1111/j.1749-6632.2000.tb06646.x. [DOI] [PubMed] [Google Scholar]
- 13.Lass A, Forster M J, Sohal R S. Free Radical Biol Med. 1999;26:1375–1382. doi: 10.1016/s0891-5849(98)00330-x. [DOI] [PubMed] [Google Scholar]
- 14.Huertas J R, Martinez-Velasco E, Ibanez S, Lopez-Frias M, Ochoa J J, Quiles J, Parenti Castelli G, Mataix J, Lenaz G. Biofactors. 1999;9:337–343. doi: 10.1002/biof.5520090233. [DOI] [PubMed] [Google Scholar]
- 15.Hagen T M, Ingersoll R T, Lykkesfeldt J, Liu J, Wehr C M, Vinarsky V, Bartholomew J C, Ames B N. FASEB J. 1999;13:411–418. doi: 10.1096/fasebj.13.2.411. [DOI] [PubMed] [Google Scholar]
- 16.Paradies G, Petrosillo G, Gadaleta M N, Ruggierio F M. FEBS Lett. 1999;454:207–209. doi: 10.1016/s0014-5793(99)00809-1. [DOI] [PubMed] [Google Scholar]
- 17.Paradies G, Ruggierio F M, Petrosillo G, Gadaleta M N, Quagliarello E. FEBS Lett. 1994;350:213–215. doi: 10.1016/0014-5793(94)00763-2. [DOI] [PubMed] [Google Scholar]
- 18.Hagen T M, Wehr C M, Ames B N. Ann NY Acad Sci. 1998;854:214–223. doi: 10.1111/j.1749-6632.1998.tb09904.x. [DOI] [PubMed] [Google Scholar]
- 19.Hagen T M, Ingersoll R T, Wehr C M, Lykkesfeldt J, Vinarsky V, Bartholomew J C, Song M H, Ames B N. Proc Natl Acad Sci USA. 1998;95:9562–9566. doi: 10.1073/pnas.95.16.9562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hagen T M, Yowe D L, Bartholomew J C, Wehr C M, Do K L, Park J-Y, Ames B N. Proc Natl Acad Sci USA. 1997;94:3064–3069. doi: 10.1073/pnas.94.7.3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gorini A, D'Angelo A, Villa R F. Neurochem Res. 1999;24:617–624. doi: 10.1023/a:1021008306414. [DOI] [PubMed] [Google Scholar]
- 22.Imperato A, Ramacci M T, Angelucci L. Neurosci Lett. 1989;107:251–255. doi: 10.1016/0304-3940(89)90826-4. [DOI] [PubMed] [Google Scholar]
- 23.Liu, J., Atamna, H. & Ames, B. N. (2002) Ann. N.Y. Acad. Sci., in press. [DOI] [PubMed]
- 24.Bustamente J, Lodge J K, Marcocci L, Tritschler H J, Packer L, Rihn B H. Free Radical Biol Med. 1998;24:1023–1039. doi: 10.1016/s0891-5849(97)00371-7. [DOI] [PubMed] [Google Scholar]
- 25.Estrada D E, Ewart H S, Tsakiridis T, Volchuk A, Ramlal T, Tritschler H J, Klip A. Diabetes. 1996;45:1798–1804. doi: 10.2337/diab.45.12.1798. [DOI] [PubMed] [Google Scholar]
- 26.Han D, Handelman G, Marcocci L, Sen C K, Roy S, Kobuchi H, Tritschler H J, Flohe L, Packer L. Biofactors. 1997;6:321–338. doi: 10.1002/biof.5520060303. [DOI] [PubMed] [Google Scholar]
- 27.Moldeus P, Hogberg J, Orrenius S. Methods Enzymol. 1978;52:60–71. doi: 10.1016/s0076-6879(78)52006-5. [DOI] [PubMed] [Google Scholar]
- 28.LeBel C P, Ischiropoulos H, Bondy S C. Chem Res Toxicol. 1992;5:227–231. doi: 10.1021/tx00026a012. [DOI] [PubMed] [Google Scholar]
- 29.Lykkesfeldt J, Loft S, Poulsen H E. Anal Biochem. 1995;229:329–335. doi: 10.1006/abio.1995.1421. [DOI] [PubMed] [Google Scholar]
- 30.Yeo H C, Helbock H J, Chyu D W, Ames B N. Anal Biochem. 1999;220:391–396. doi: 10.1006/abio.1994.1355. [DOI] [PubMed] [Google Scholar]
- 31.Yeo H C, Liu J, Helbock H J, Ames B N. Methods Enzymol. 1999;300:70–78. doi: 10.1016/s0076-6879(99)00115-9. [DOI] [PubMed] [Google Scholar]
- 32.Lykkesfeldt J, Hagen T M, Vinarsky V, Ames B N. FASEB J. 1998;12:1183–1189. doi: 10.1096/fasebj.12.12.1183. [DOI] [PubMed] [Google Scholar]
- 33.Hagen T M, Vinarsky V, Wehr C M, Ames B N. Antioxid Redox Signalling. 2000;2:473–483. doi: 10.1089/15230860050192251. [DOI] [PubMed] [Google Scholar]
- 34.Humphries K M, Szweda L I. Biochemistry. 1998;37:15835–15841. doi: 10.1021/bi981512h. [DOI] [PubMed] [Google Scholar]
- 35.Liu J, Killilea D W, Ames B N. Proc Natl Acad Sci USA. 2002;99:1876–1881. doi: 10.1073/pnas.261709098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dimpfel W. Eur J Med Res. 1996;1:523–527. [PubMed] [Google Scholar]