Abstract
Background
Older patients frequently experience delays in discharge post-hip fracture surgery. Our study aimed to describe the sociodemographic and clinical characteristics of patients who had a surgical repair for a hip fracture and to examine the associations between these characteristics and delayed discharge (> 6 days post-surgery) for frail vs. non frail patients.
Methods
We conducted a retrospective population-based cohort study using routinely collected health administrative data housed at ICES. The study population included all individuals aged 50 to 105 years with a hip fracture who had a surgical repair in Ontario, Canada between January 1, 2015, and December 31, 2021. We used descriptive statistics and multivariable logistic regression models to characterize the association of patient socio-demographics, baseline health, and characteristics of the acute care episode with delayed discharge between non-frail and frail groups.
Results
We included 74,838 patients, with a mean age of 80.9 (SD 10.7) years, among which 37,234 (49.8%) had a delayed discharge. Some factors increased the odds of delayed discharge in both non-frail and frail groups included prior location in complex continuing care (non-frail OR 1.64, 95% CI 1.14,2.35, P = 0.007; frail OR 2.33, 95% CI 1.70,3.21, P < 0.0001), as well as prior residence in the community with home care (non-frail OR 9.71, 95% CI 8.89,10.6, P < 0.0001; frail OR 13.8, 95% CI 12.0,15.8, P < 0.0001), or without home care (non-frail OR 5.81, 95% CI 5.35,6.32, P < 0.0001; frail OR 4.60, 95% CI 4.14,5.11, P < 0.0001) compared to long-term care as well as residing in a neighbourhood with a higher Racialized and Newcomer Populations Index quintile (non-frail OR 1.45, 95% CI 1.37,1.55, P < 0.0001; frail OR 1.90, 95% CI 1.68,2.16, P < 0.0001). Factors that reduced the odds of delayed discharge in both non-frail and frail groups included individuals living in rural areas (non-frail OR 0.44, 95% CI 0.42,0.47, P < 0.0001; frail OR 0.41, 95% CI 0.36,0.46, P < 0.0001), or having previous fragility fractures (non-frail OR 0.44, 95% CI 0.40,0.49, P < 0.0001; frail OR 0.56, 95% CI 0.51,0.62, P < 0.0001). However, patients in the non-frail group were more likely to be delayed for the presence of comorbidities including mood or mental health conditions (OR 1.22, 95% CI 1.16,1.28, P < 0.0001), stroke (OR 1.46, 95% CI 1.28,1.67, P < 0.0001), chronic obstructive pulmonary disease (OR 1.35, 95% CI 1.24,1.47, P < 0.0001), dementia (OR 1.41, 95% CI 1.34,1.48, P < 0.0001), or diabetes (OR 1.26, 95% CI 1.20,1.32, P < 0.0001). Factors that reduced the odds of delayed discharge in the non-frail group were female sex (OR 0.87, 95% CI 0.83,0.90, P < 0.0001), or having cancer (OR 0.94, 95% CI 0.90,0.98, P = 0.0089).
Conclusion
Delayed discharge was common after hip fracture surgery in both the non-frail and frail groups. Preoperative residential status, comorbidities and sociodemographic factors are associated with delayed discharge. These data can help to inform strategies to improve timely discharge from acute care and the overall outcomes of the older adult hip fracture population.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-025-08747-0.
Keywords: Hip fracture, Older adults, Surgery, Discharge
Introduction
Hip fractures in older adults are the most common fractures requiring admission to hospital and are associated with poor outcomes, including significant disability and increased mortality [1, 2]. Delays in discharge and longer length of stay in acute care for patients who underwent surgical repair for a hip fracture may increase long-term complications and negative health outcomes (such as functional decline) [3]. Unnecessary hospital bed days while waiting to access care that is appropriate for the patient’s current needs are also costly to the health care system and occurs most frequently among older adults because of the interplay between numerous individual, organizational, and system-level factors. Patient flow challenges may lead to cancellation of other surgical procedures and longer waitlists [4–7]. Reducing delays in discharge could contribute to an increase in system-level efficiencies, better experiences and outcomes for post-surgery hip fracture patients.
Best practice guidelines recommend that patients who had a hip fracture and who underwent surgical repair receive active rehabilitation following their acute care stay, with rehabilitation beginning no later than six days following surgery [8–11]. Despite this clear and growing evidence, factors related to delayed discharge from acute care exist. There are many challenges that contribute to these delays, yet organizational structures and health care providers’ roles in influencing these decisions are not always clear [12]. Timely discharge can be complex as it requires collaborative efforts from multiple health care providers in both acute and sub-acute care settings. The lack of clearly defined roles among different providers and in siloed settings can lead to a lack of oversight to ensure patients receive timely rehabilitative care [12].
Understanding the differences between patients who do or do not experience delayed discharge at a population level could help prioritize strategies and solutions to provide optimal care to this older population. In our study, we aimed to describe the sociodemographic and clinical characteristics of patients who underwent surgical repair for a hip fracture in Ontario, Canada and examine the associations between patients’ characteristics and delayed discharge (defined as greater than 6 days between date of surgery and discharge from acute care).
Methods
Study design and setting
We conducted a retrospective population-based cohort study using routinely collected health administrative data in Ontario, Canada, housed at ICES (formerly known as the Institute for Clinical Evaluative Sciences). Our protocol was published elsewhere [13]. We report our findings using the REporting of studies Conducted using Observational Routinely collected health Data (RECORD) reporting guideline [14]. Use of data was authorized under Sect. 45 of the Ontario’s Personal Health Information Protection Act. As such, this study did not require any further ethics approval.
Data sources
The following health administrative databases were used: the Discharge Abstract Database (DAD), which contains clinical and administrative individual-level data on admissions to acute care hospitals– where surgeries for hip fractures always occur and where rehabilitation at times begin; the Registered Persons Database (RPDB), which contains sociodemographic characteristics for all individuals who are eligible for health insurance coverage; the National Rehabilitation Reporting System (NRS), used to identify individuals receiving inpatient rehabilitation; the Continuing Care Reporting System (CCRS), used to identify individuals residing in long-term care and complex continuing care– both potential sites of rehabilitation; the Home Care Database, used to identify individuals who received publicly funded home care services; the Same Day Surgery database (SDS), which contains data on same day surgeries; the Ontario Mental Health Reporting System (OMHRS), which contains data on admissions to adult designated inpatient mental health beds; the ICES Physician Database (IPDB), which contains information on Ontario physicians; the Ontario Drug Benefit (ODB) program database, which contains prescription medication claims for those covered under the provincial drug program; the Drug List (DIN), which contains drug identification numbers; the Ontario Census (CENSUS) and the Postal Code Conversion File, which contain geographic identifiers and neighborhood-level information based on census data; and the Ontario Marginalization Index, which identifies census-based geographic information on the extent of marginalization within communities. These datasets were linked at the individual level using unique encoded identifiers.
Study cohort
The study cohort included all individuals with a hip fracture (ICD-10-CA: S72.0, S72.1, or S72.2) aged 50 to 105 who underwent surgical repair (defined by a presence of at least one of the following codes from the Canadian Classification of Health Interventions (CCI): 1VA53 (implantation of internal device, hip joint); 1VA74 (fixation, hip joint), 1VA80 (repair, hip joint); 1VC74 (fixation, femur); or 1VC80 (repair, femur) between January 1, 2015, and December 31, 2021. We excluded people with a hip fracture diagnosis that was not the most responsible diagnosis (MRDx) as well as any diagnosis of pathological fractures (ICD-10-CA M8445). In the case of multiple hip fractures, we only kept the first hip fracture incident. We also excluded those with missing or invalid data for birth date, sex or postal code, non-Ontario residents at the admission date, or those who stayed in hospital > 365 days.
Variables of interest
We determined individuals’ sociodemographic characteristics at the admission date. Sociodemographic characteristics included age, sex, geographical location (e.g., rurality), prior residence (i.e., home without home care, home with home care, long-term care, complex continuing care), neighbourhood income quintile, and the Racialized and Newcomer Populations Index from the Ontario Marginalization Index. A two-year lookback window from the admission date was used to determine pre-existing comorbidities. Comorbidities (e.g., cancer, mood-disorder/ mental health, renal disease, stroke, congestive heart failure, cardiovascular disease, chronic obstructive pulmonary disease, dementia, diabetes) were identified using the Health System Performance Research Network multimorbidity macro [15]. The preoperative frailty index (pFI), derived using 30 variables (e.g., comorbidities, socio-demographics, location of residence, etc.), was calculated using a validated, accumulating deficits frailty index [16]. Characteristics of the acute episode of care included the following: surgery day of the week; total number of days spent in hospital; number of days from hospital admission to surgery; and number of days spent in ICU and in Alternative Levels of Care (ALC).
The primary outcome was delayed discharge, defined as a discharge from acute care greater than 6 days post-surgery following best practice guidelines [8–11].
Statistical analyses
Descriptive analyses were performed on the characteristics of individuals and of their acute episode of care. Means and standard deviations, and medians and interquartile ranges, were used to summarize continuous variables; counts and proportions were used to summarize categorical variables. We performed multivariable logistic regression to identify factors associated with delayed discharge. All variables included in the model were pre-specified, checked for collinearity, and selected if previous literature and/or clinical expertise substantiated a potential association with delayed discharge. Factors included in the model comprised of patient’s socio-demographics characteristics (i.e., age, sex, prior residence, neighborhood income, rurality, and Racialized and Newcomer Populations Index), presence of various comorbidities at hospitalization, and characteristics of the acute care episode (i.e., number of days in hospital before surgery, surgery day of the week, and surgery type). We grouped the variable surgery day of the week as a binary variable, whether surgery occurred on Sunday/Monday (i.e., post-surgery day 6 falling on Saturday/Sunday) because this could delay discharge to the following Monday. The only continuous variables in the model were age and number of days in hospital before surgery– age did not meet the linearity assumption and was modelled using restricted cubic splines (RCS) with knots at the 25th, 50th, and 75th percentile; days in hospital before surgery met the linearity assumption and therefore did not require transformation. Only complete cases were included in the analyses– a reduction of only 893 patients (1.2% of cohort). We conducted sub-analyses based on the frailty status dichotomized as non-frail (pFI < = 0.21) and frail (pFI > 0.21) groups. All analyses were performed on SAS Version 9.4 and statistical significance calculated at an alpha < 0.05.
Results
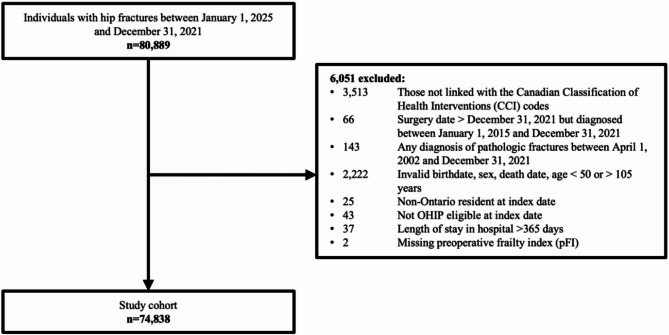
During the study period, 74,838 patients met the inclusion criteria (Fig. 1).
Fig. 1.
Study cohort creation
Sociodemographic and clinical characteristics
Among patients who had a hip fracture and who underwent surgical repair, the mean age was 80.9 (standard deviation [SD] 10.7), 68.1% were female, and 20.3% were considered frail. Most patients (n = 48,194, 64.4%) were admitted from the community without home care, and 86.4% of the hip fractures (n = 64,653) occurred in individuals living in urban areas.
In the non-frail group, the mean age was 80.6 (SD 11.0) and 69.3% were female whereas in the frail group the mean age was slightly higher at 82.4 (SD 9.4, P < 0.0001) and 63.2% were female (P < 0.0001). Patients who were frail (n = 4,914, 32.3%) also lived in poorer neighborhoods (P < 0.0001).
There were also differences in comorbidities between the groups with higher proportions in the frail group for dementia (n = 5,656, 37.2%, P < 0.0001), diabetes (n = 6,000, 39.5%, P < 0.0001), mood and other mental health conditions (n = 4,912, 32.3%, P < 0.0001), cancer (n = 3,622, 23.8%, P < 0.0001) and congestive heart failure (n = 4,216, 27.7% P < 0.0001). Further details on the cohort characteristics are in Table 1.
Table 1.
Sociodemographic and clinical characteristics of all patients who had a hip fracture and who underwent surgical repair
| Characteristics | Total (N = 74,838) |
Non-Frail pFI < = 0.21 (N = 59,637) |
Frail pFI > 0.21 (N = 15,201) |
P-value |
|---|---|---|---|---|
| Sociodemographic | ||||
| Age - mean (SD) | 80.9 (10.7) | 80.6 (11.0) | 82.4 (9.4) | < 0.0001 |
| Median (IQR*) | 83 (74–89) | 83.0 (74.0–89.0) | 84.0 (77.0–89.0) | < 0.0001 |
| Sex - n (%) | ||||
| Female | 50,943 (68.1%) | 41,337 (69.3%) | 9,606 (63.2%) | < 0.0001 |
| Location of Residence Prior to Hospitalization - n (%) | ||||
| Long Term Care | 7,597 (10.2%) | 4,537 (7.6%) | 3,060 (20.1%) | < 0.0001 |
| Complex Continuing Care | 359 (0.5%) | 173 (0.3%) | 186 (1.2%) | |
| Community with home care | 18,688 (25.0%) | 16,183 (27.1%) | 2,505 (16.5%) | |
| Community without home care | 48,194 (64.4%) | 38,744 (65.0%) | 9,450 (62.2%) | |
| Nearest Census Based Neighbourhood Income Quintile (Q) - n (%) | ||||
| Q1 (lowest) | 19,323 (25.8%) | 14,409 (24.2%) | 4,914 (32.3%) | < 0.0001 |
| Q2 | 16,488 (22.0%) | 12,705 (21.3%) | 3,783 (24.9%) | |
| Q3 | 14,096 (18.8%) | 11,369 (19.1%) | 2,727 (17.9%) | |
| Q4 | 12,562 (16.8%) | 10,590 (17.8%) | 1,972 (13.0%) | |
| Q5 (highest) | 11,959 (16.0%) | 10,264 (17.2%) | 1,695 (11.2%) | |
| Missing - n (%) | 410 (0.5%) | 300 (0.5%) | 110 (0.7%) | |
| Rural - n (%) | ||||
| Urban | 64,653 (86.4%) | 51,823 (86.9%) | 12,830 (84.4%) | < 0.0001 |
| Rural | 9,792 (13.1%) | 7,525 (12.6%) | 2,267 (14.9%) | |
| Missing | 393 (0.5%) | 289 (0.5%) | 104 (0.7%) | |
| Racialized and Newcomer Populations Quintile (Q) - n (%) | ||||
| Q1 (lowest) | 16,540 (22.1%) | 12,966 (21.7%) | 3,574 (23.5%) | < 0.0001 |
| Q2 | 16,624 (22.2%) | 13,293 (22.3%) | 3,331 (21.9%) | |
| Q3 | 14,868 (19.9%) | 11,999 (20.1%) | 2,869 (18.9%) | |
| Q4 | 13,718 (18.3%) | 11,079 (18.6%) | 2,639 (17.4%) | |
| Q5 (highest) | 12,196 (16.3%) | 9,658 (16.2%) | 2,538 (16.7%) | |
| Missing | 892 (1.2%) | 642 (1.1%) | 250 (1.6%) | |
| Clinical characteristics | ||||
| Comorbidities - n (%) | ||||
| Dementia | 16,978 (22.7%) | 11,322 (19.0%) | 5,656 (37.2%) | < 0.0001 |
| Diabetes | 16,344 (21.8%) | 10,344 (17.3%) | 6,000 (39.5%) | < 0.0001 |
| Mood Disorder & other Mental Health Conditions | 15,308 (20.5%) | 10,396 (17.4%) | 4,912 (32.3%) | < 0.0001 |
| Cancer | 14,110 (18.9%) | 10,488 (17.6%) | 3,622 (23.8%) | < 0.0001 |
| Congestive Heart Failure | 7,006 (9.4%) | 2,790 (4.7%) | 4,216 (27.7%) | < 0.0001 |
| Renal | 6,250 (8.4%) | 3,055 (5.1%) | 3,195 (21.0%) | < 0.0001 |
| Acute Myocardial Infarction | 5,434 (7.3%) | 3,310 (5.6%) | 2,124 (14.0%) | < 0.0001 |
| Chronic Obstructive Pulmonary Disease | 5,364 (7.2%) | 2,668 (4.5%) | 2,696 (17.7%) | < 0.0001 |
| Chronic Coronary Disease | 5,093 (6.8%) | 3,076 (5.2%) | 2,017 (13.3%) | < 0.0001 |
| Cardiac Arrythmia | 5,065 (6.8%) | 3,289 (5.5%) | 1,776 (11.7%) | < 0.0001 |
| Stroke | 2,311 (3.1%) | 1,066 (1.8%) | 1,245 (8.2%) | < 0.0001 |
| Fall - n (%) | 4,045 (5.4%) | 1,710 (2.9%) | 2,335 (15.4%) | < 0.0001 |
| Any Previous Fragility Fracture (Humerus, Wrist, Spine, or Hip) - n (%) | 5,102 (6.8%) | 2,369 (4.0%) | 2,733 (18.0%) | < 0.0001 |
| Humerus Fracture | 528 (0.7%) | 181 (0.3%) | 347 (2.3%) | < 0.0001 |
| Wrist Fracture | 27 (0.0%) | 11 (0.0%) | 16 (0.1%) | < 0.0001 |
| Spinal Fracture | 385 (0.5%) | 108 (0.2%) | 277 (1.8%) | < 0.0001 |
| Hip Fracture | 4,251 (5.7%) | 2,115 (3.5%) | 2,136 (14.1%) | < 0.0001 |
| Malignant Neoplasm - n (%) | 3,972 (5.3%) | 1,825 (3.1%) | 2,147 (14.1%) | < 0.0001 |
*IQR (interquartile range)
Acute episode of care characteristics
The median total length of stay in acute care was 8.0 days for both the non-frail (IQR = 5.0–13.0) and frail (IQR = 5.0–15.0) groups (P < 0.0001). The median length of stay post-surgery in acute care for the non-frail group was 6.0 days (IQR = 4.0–11.0) and for the frail group was 7.0 days (IQR = 4.0–14.0; P < 0.0001). Of the 59,637 patients in the non-frail group, 48.8% (n = 29,123) experienced a delayed discharge (> 6 days post-surgery). Of the 15,201 patients in the frail group, 53.4% (n = 8,111) had a delayed discharge (Table 2).
Table 2.
Acute episode of care characteristics of all patients who had a hip fracture and who underwent surgical repair
| Characteristics | Total (N = 74,838) |
Non-Frail pFI < = 0.21 (N = 59,637) |
Frail pFI > 0.21 (N = 15,201) |
P-value |
|---|---|---|---|---|
| Acute episode of care | ||||
| Surgery Day of the Week - n (%) | ||||
| Monday/Sunday | 21,635 (28.9%) | 17,239 (28.9%) | 4,396 (28.9%) | 0.9756 |
| Other days | 53,203 (71.1%) | 42,398 (71.1%) | 10,805 (71.1%) | |
| Total length of stay, Mean (SD) | 12.1 (16.7) | 11.7 (16.2) | 13.9 (18.7) | < 0.0001 |
| Median (IQR)* | 8.0 (5.0–13.0) | 8.0 (5.0–13.0) | 8.0 (5.0–15.0) | < 0.0001 |
| # of days between Acute Admission and Surgery dates, Mean (SD) | 1.3 (2.8) | 1.2 (2.3) | 1.5 (4.2) | < 0.0001 |
| Median (IQR) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | < 0.0001 |
| # of days between Surgery and Acute Discharge dates, Mean (SD) | 10.9 (16.3) | 10.5 (15.8) | 12.3 (17.9) | < 0.0001 |
| Median (IQR) | 6.0 (4.0–12.0) | 6.0 (4.0–11.0) | 7.0 (4.0–14.0) | < 0.0001 |
| Admission to ICU (Intensive Care Unit) - n (%) | 4,514 (6.0%) | 2,963 (5.0%) | 1,551 (10.2%) | < 0.0001 |
| Admission to Alternate Level of Care (ALC) - n (%) | 23,159 (30.9%) | 18,490 (31.0%) | 4,669 (30.7%) | 0.4912 |
|
Delayed Discharge > 6 days between Surgery & Acute Hospital Discharge - n (%) |
37,234 (49.8%) | 29,123 (48.8%) | 8,111 (53.4%) | < 0.0001 |
*IQR (interquartile range)
Table 3 shows the results from the logistic regression modelling of the outcome of delayed discharge for frail and non-frail groups.
Table 3.
Adjusted odds ratio for delayed discharge for frail and non-frail groups (n = 73,947*)
| Non-Frail pFI < = 0.21 | Frail pFI > 0.21 | |||
|---|---|---|---|---|
| Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
| Age | 1.04(1.03,1.05) | < 0.0001 | 1.00(0.98,1.01) | 0.6725 |
| Age RCS1** | 1.03(1.01,1.06) | 0.0011 | 1.05(1.00,1.10) | 0.0679 |
| Age RCS2 | 0.79(0.68,0.92) | 0.0021 | 0.75(0.54,1.04) | 0.0801 |
| Age RCS3 | 1.59(1.03,2.45) | 0.0348 | 1.71(0.69,4.22) | 0.246 |
| Sex (reference = Male) | 0.87(0.83,0.90) | < 0.0001 | 0.94(0.87,1.02) | 0.1184 |
| Prior Residence (reference = Long-term care (LTC)) | ||||
| Complex Continuing Care | 1.64(1.14,2.35) | 0.007 | 2.33(1.70,3.21) | < 0.0001 |
| Community with home care | 9.71(8.89,10.6) | < 0.0001 | 13.8(12.0,15.8) | < 0.0001 |
| Community without home care | 5.81(5.35,6.32) | < 0.0001 | 4.60(4.14,5.11) | < 0.0001 |
| Income (reference = Q1 (lowest)) | ||||
| Q2 | 0.94(0.89,0.99) | 0.0135 | 1.13(1.03,1.25) | 0.0103 |
| Q3 | 0.91(0.86,0.96) | 0.0006 | 1.14(1.02,1.27) | 0.0175 |
| Q4 | 0.88(0.83,0.93) | < 0.0001 | 1.10(0.97,1.24) | 0.1234 |
| Q5 (highest) | 0.83(0.79,0.88) | < 0.0001 | 1.12(0.98,1.27) | 0.0892 |
| Rurality (reference = Urban) | ||||
| Rural | 0.44(0.42,0.47) | < 0.0001 | 0.41(0.36,0.46) | < 0.0001 |
| Racialized and Newcomer Populations (reference = Q1 (lowest)) | ||||
| Q2 | 1.22(1.16,1.29) | < 0.0001 | 1.14(1.03,1.28) | 0.0157 |
| Q3 | 1.27(1.20,1.34) | < 0.0001 | 1.42(1.26,1.59) | < 0.0001 |
| Q4 | 1.37(1.29,1.45) | < 0.0001 | 1.71(1.52,1.94) | < 0.0001 |
| Q5 (highest) | 1.45(1.37,1.55) | < 0.0001 | 1.90(1.68,2.16) | < 0.0001 |
| Cancer (reference = No) | 0.94(0.90,0.98) | 0.0089 | 1.03(0.95,1.13) | 0.442 |
| Mood disorder / mental health (reference = No) | 1.22(1.16,1.28) | < 0.0001 | 1.06(0.97,1.15) | 0.1766 |
| Renal (reference = No) | 1.38(1.27,1.49) | < 0.0001 | 1.46(1.33,1.60) | < 0.0001 |
| Stroke (reference = No) | 1.46(1.28,1.67) | < 0.0001 | 1.11(0.97,1.26) | 0.1304 |
| Congestive heart failure (CHF) (reference = No) | 1.17(1.08,1.28) | 0.0003 | 1.12(1.02,1.22) | 0.0118 |
| Cardiovascular Disease (CVD) (reference = No) | 1.00(0.95,1.05) | 0.9663 | 0.95(0.88,1.03) | 0.2441 |
| Chronic obstructive pulmonary disease (COPD) (reference = No) | 1.35(1.24,1.47) | < 0.0001 | 1.07(0.97,1.18) | 0.1866 |
| Dementia (reference = No) | 1.41(1.34,1.48) | < 0.0001 | 0.91(0.84,0.99) | 0.026 |
| Diabetes (reference = No) | 1.26(1.20,1.32) | < 0.0001 | 1.04(0.96,1.12) | 0.3316 |
| Any previous fragility fractures (reference = No) | 0.44(0.40,0.49) | < 0.0001 | 0.56(0.51,0.62) | < 0.0001 |
| Preoperative wait time (days) | 1.16(1.14,1.18) | < 0.0001 | 1.14(1.11,1.17) | < 0.0001 |
| Surgery on Sunday or Monday | 1.00(0.97,1.04) | 0.8151 | 1.08(0.99,1.16) | 0.074 |
*Missing data in rurality, income, or Racialized and Newcomer Populations Index (n = 893)
**RCS (restricted cubic splines)
Factors that increased the odds of delayed discharge (both groups)
For both non-frail and frail groups, factors that increased the odds of delayed discharge were patients’ prior location in complex continuing care (non-frail OR 1.64, 95% CI 1.14,2.35, P = 0.007; frail OR 2.33, 95% CI 1.70,3.21, P < 0.0001), as well as prior residence in the community with home care (non-frail OR 9.71, 95% CI 8.89,10.6, P < 0.0001; frail OR 13.8, 95% CI 12.0,15.8, P < 0.0001), or without home care (non-frail OR 5.81, 95% CI 5.35,6.32, P < 0.0001; frail OR 4.60, 95% CI 4.14,5.11, P < 0.0001) compared to long-term care as well as patients residing in a neighbourhood with a higher Racialized and Newcomer Populations Index quintile (non-frail OR 1.45, 95% CI 1.37,1.55, P < 0.0001; frail OR 1.90, 95% CI 1.68,2.16, P < 0.0001). Individuals who were more likely to have a delayed discharge had the comorbidities of renal disease (non-frail OR 1.38, 95% CI 1.27,1.49, P < 0.0001; frail OR 1.46, 95% CI 1.33,1.60, P < 0.0001), or congestive heart failure (non-frail OR 1.17, 95% CI 1.08,1.28, P = 0.0003; frail OR 1.12, 95% CI 1.02,1.22, P = 0.0118), and waited longer preoperative for surgery (non-frail OR 1.16, 95% CI 1.14,1.18, P < 0.0001; frail OR 1.14, 95% CI 1.11,1.17, P < 0.0001).
Factors that reduced the odds of delayed discharge (both groups)
Factors that reduced the odds of delayed discharge in both non-frail and frail groups included individuals living in rural areas (non-frail OR 0.44, 95% CI 0.42,0.47, P < 0.0001; frail OR 0.41, 95% CI 0.36,0.46, P < 0.0001), or having previous fragility fractures (non-frail OR 0.44, 95% CI 0.40,0.49, P < 0.0001; frail OR 0.56, 95% CI 0.51,0.62, P < 0.0001).
Factors that increased the odds of delayed discharge (non-frail group only)
In the non-frail group, factors that increased the odds of delayed discharge were the presence of comorbidities including mood or mental health conditions (OR 1.22, 95% CI 1.16,1.28, P < 0.0001), stroke (OR 1.46, 95% CI 1.28,1.67, P < 0.0001), chronic obstructive pulmonary disease (OR 1.35, 95% CI 1.24,1.47, P < 0.0001), dementia (OR 1.41, 95% CI 1.34,1.48, P < 0.0001), or diabetes (OR 1.26, 95% CI 1.20,1.32, P < 0.0001).
Factors that reduced the odds of delayed discharge (non-frail group only)
Factors that reduced the odds of delayed discharge in the non-frail groups were female sex (OR 0.87, 95% CI 0.83,0.90, P < 0.0001), or having cancer (OR 0.94, 95% CI 0.90,0.98, P = 0.0089). Compared to the frail group, the non-frail group’s income in the second (OR 0.94, 95% CI 0.89,0.99, P = 0.0135) and the middle (OR 0.91, 95% CI 0.86,0.96, P = 0.0006) quintiles were less likely to have a delayed discharge compared to the frail group’s income in the second (OR 1.13, 95% CI 1.03,1.25, P = 0.0103) and the middle (OR 1.14, 95% CI 1.02,1.27, P = 0.0175) quintiles who were more likely to have a delayed discharge.
Discussion
Despite the existence of best practice guidelines, delayed discharge of patients who had a surgical repair for a hip fracture remains common. In our study, we found 49.8% (n = 37,234) of the patients experiencing a delayed discharge with 48.8% (n = 29,123) in the non-frail group and 53.3% (n = 8,111) in the frail group. We also found that patients in both frail and non-frail groups that had a prior residence in the community with or without home care, who lived in a neighbourhood with a higher Racialized and Newcomer Populations Index or who had pre-existing comorbidities (i.e., renal disease or congestive heart failure) were significantly more likely to have a delayed discharge. In hospital, patients with a longer preoperative wait time, or a fixation repair using intramedullary nail also had increased odds of having a delayed discharge. However, individuals living in rural areas or having any previous fragility fractures decreased the odds of having a delayed discharge by about half.
We also found that patients in the non-frail group, which we assumed would be more medically fit than the frail group, were more likely to be delayed because of the presence of comorbidities including mood or mental health conditions, stroke, chronic obstructive pulmonary disease, dementia, or diabetes compared to the frail group. This may be indicative of possible system level factors related to delayed discharge for this population, such as gaps in coordination of care transitions from acute to community care, inadequate management of delirium after surgery, lack of available home care services, and social supports. It is also possible that the older individuals in the frail group experienced more in hospital deaths and were therefore excluded from our study cohort. Alternatively, factors that reduced the odds of delayed discharge in the non-frail group were being female or having cancer.
Factors associated with prior residence/location of care and rurality
In this study, in both non-frail and frail groups, patients that were from the community, especially patients who were receiving home care (i.e., lower levels of independence), had much higher odds of having a delayed discharge whereas patients living in long-term care prior to their acute care admission were less likely to experience a delay in discharge back to their previous residence in long-term care. This is consistent with a study by Ryder and colleagues [17] which found that patients living in geriatric care institutions prior to admission were primarily discharged back to long-term care. Long-term care patients, typically return to their long-term care homes because they are appropriately resourced to take these patients back whereas people in the community with home care have such higher odds of a delayed discharge. These are likely the people where a hip fracture pushes them over the edge to transition to long-term care, and the process of waiting for a long-term care placement takes a long time. This may also be related to gaps in availability of necessary home care supports to return home. If the patient is relocating to a retirement home, there may also be gaps in obtaining placement in a retirement home, as well as home care services required to supplement the private retirement home supports.
Our study also found that patients from rural areas were less likely to have a delayed discharge, this may be partly because patients in rural settings experience a quicker discharge because they are not waiting for a rehabilitation bed due to the limited access to rehabilitation in rural settings. Previous studies have found that rural older adults are less likely to receive inpatient rehabilitation compared to their urban counterparts and are more likely to be discharged home without any rehabilitation [18–20]. This supports our findings of disparities in access to rehabilitation for rural older adults. Future research is needed to better understand the systemic issues and identify potential solutions to improve rehabilitation access for rural older adults who had a surgical repair for a hip fracture.
Factors associated with comorbidities
Patients with pre-existing comorbidities (i.e., renal disease, congestive heart failure) in both non-frail and frail groups were more likely to have a delayed discharge. However, additional comorbidities (i.e., mood disorder/ mental health, stroke, chronic obstructive pulmonary disease, dementia, or diabetes) in the non-frail group also increased the odds of a delayed discharge. A previous review showed that there was a positive correlation between comorbidities and the length of stay of patients with hip fractures [21]. Patients with comorbidities are more likely to have complications or require additional care, so they would require a longer hospital stay for treatment and care [22, 23]. Patients with multiple comorbidities may experience a decline in their independence with self-care, requiring more time than others to progress towards independence and needing more support at home. For high-risk groups (i.e., multiple comorbidities), early intervention should be taken to avoid postoperative complications and to reduce the length of hospital stay.
Factors associated with the hospital episode of care
In both the non-frail and frail groups, preoperative waiting time greater than 48 h was a contributing factor for delayed discharge. Best practice suggests that hip fracture surgery should occur within 48 h of admission [24]. Consistent with previous research, the waiting time before surgery influences the overall length of stay in hospital [25]. Studies found that early surgery can improve mobility, reduce the risk of delirium and other post-surgery complications [26–27]. Research has also shown that longer length of stay in hospital can lead to adverse health outcomes in patients later in life [28–30]. The unnecessary prolonged length of stay of patients can also lead to inefficient use of health care resources [31].
Strengths and limitations
We used comprehensive population-level health administrative databases to study the factors to delayed discharge for a large cohort of non-frail and frail patients who had a hip fracture and who underwent surgical repair. However, these databases rely on routinely collected data that could be subject to misclassification biases because these data were not originally collected for research purposes. Although system level factors are often substantial barriers to timely discharge, in this study, we were only able to identify patient and episode-level factors. Future work should look at clustering the analyses at the hospital level to help account for hospital variations. Furthermore, the group who experienced a delay in discharge might be heterogeneous; to attempt to address this issue, we have stratified our analysis based on non-frail and frail groups.
Implications for future practice and research
Overall, older adults following a hip fracture require a comprehensive care plan including timely rehabilitation [32]. Previous research has demonstrated some improvements in the reduction of overall hospital stays for older patients with hip fractures [33–35]. The results of this study underscore the lack of awareness of existing guidelines as well as the system pressures that delay safe discharge and the importance of providing a clear pathway that can help providers predict or flag patients at greater risk of delayed discharge [36]. Earlier planning for this patient population can prevent unnecessary discharge delays. Orthogeriatric care models, which involve collaborative management by orthopedic surgeons, geriatricians, and a multidisciplinary team, promote earlier mobilization and rehabilitation [37]. These models can improve hip fracture outcomes by reducing mortality, and complications [38]. By addressing comorbidities, preventing complications, and optimizing post-operative recovery, orthogeriatric care leads to shorter hospital stays and more timely discharges.
Previous work as part of the enhanced recovery after surgery program for elective total hip replacement has achieved positive results (i.e., shorten length of stay, reduction of costs) for older patients with a hip fracture [39–41]. Future work to minimize delays in discharge for the hip fracture population without compromising their health could apply lessons from the enhanced recovery after surgery program, focusing on a multidisciplinary approach to early planning and management to address the barriers to delayed discharge.
Conclusion
Using population-level administrative health data, this study provided a better understanding of the key factors related to delayed discharge from acute care for the post-surgery hip fracture population. This has important implications for clinical care across acute and sub-acute care settings to better meet the needs of patients who underwent surgical repair for a hip fracture at the health care system level. These results can help to support decision makers in planning strategies for the best management of hip fractures to shorten the acute care length of stay, reduce the cost of hospitalization, and thus make more efficient use of health service resources. Future research should implement and evaluate targeted strategies to improve the barriers to discharge for the post-surgery older hip fracture population.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
This study was supported by ICES, an independent, non-profit research institute funded by an annual grant from the MOH and MLTC. This study also received funding from the Innovation Fund of the Alternative Funding Plan for the Academic Health Sciences Centres of Ontario [BAM-22-001]. Parts of this material are based on data and information compiled and provided by: CIHI, Ontario Ministry of Health, Ontario Health, and Statistics Canada. These datasets were linked using unique encoded identifiers and analyzed at ICES. This research used data adapted from the Statistics Canada Postal Code OM Conversion File (PCCF), which is based on data licensed from Canada Post Corporation, and/or data adapted from the Ontario Ministry of Health Postal Code Conversion File, which contains data copied under license from ©Canada Post Corporation and Statistics Canada.Adapted from Statistics Canada, PCCF, October 2023. This does not constitute an endorsement by Statistics Canada of this product.We thank the Toronto Community Health Profiles Partnership for providing access to the Ontario Marginalization Index.We thank IQVIA Solutions Canada Inc. for use of their Drug Information File.The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Author contributions
CB, WL, SS, SP. CW, LT, DIM, PEB, VFM, SP and PT conceived the original idea. CB, WL, SS, SP, CW, LT, DIM designed the study and interpreted the results. AYD and MT performed the statistical analyses. CB, WL, AYD, MT, CW and PT reviewed and verified the results of the analyses. CB drafted the manuscript. All authors (CB, WL, SS, SP, AYD, MT, FDE, CW, LT, DIM, PEB, VFM, SP, SGF, BL, JW, CV, SS, AT, KP, SJTG, AS, and PT) reviewed and provided feedback and approved the final version of the manuscript.
Funding
Not applicable.
Data availability
The data set from this study is held securely in coded form at ICES. While data sharing agreements prohibit ICES from making the data set publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS. The full data set creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Declarations
Ethics approval and consent to participate
This project was conducted under Sect. 45 and approved by the ICES Privacy and Compliance Office. ICES is a prescribed entity under Sect. 45 of Ontario’s Personal Health Information Protection Act. Section 45 authorizes ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, allocation of resources to or planning for all or part of the health system.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Parker M, Johansen A. Hip fracture. BMJ (Clinical Res ed). 2006;333(7557):27–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag. 2014;10:937–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lim J. Big Data-Driven determinants of length of stay for patients with hip fracture. Int J Environ Res Public Health. 2020;17(14):E4949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Becchi MA, Pescetelli M, Caiti O, et al. Characteristics of patients in a ward of academic internal medicine: implications for medical care, training programmes and research. Intern Emerg Med. 2010;5(3):205–13. 10.1007/s11739-009-0325-5. [DOI] [PubMed] [Google Scholar]
- 5.Edirimanne S, Roake JA, Lewis DR. Delays in discharge of vascular surgical patients: a prospective audit. ANZ J Surg. 2010;80:443–6. 10.1111/j.1445-2197.2009.05130.x. [DOI] [PubMed] [Google Scholar]
- 6.Foer D, Ornstein K, Soriano TA, et al. Nonmedical factors associated with prolonged hospital length of stay in an urban homebound population. J Hosp Med. 2012;7(2):73–8. [DOI] [PubMed] [Google Scholar]
- 7.Mohammed A. Audit of orthopaedic bed utilisation. Health Bull. 2001;59(6):353–5. [PubMed] [Google Scholar]
- 8.Health Quality Ontario. Quality Standards. Hip fracture care for people with fragility fractures. Toronto, ON: health quality Ontario. 2017. Available: https://www.hqontario.ca/portals/0/documents/evidence/quality-standards/qs-hip-fracture-clinical-guide-en.pdf
- 9.Health Quality Ontario & Ministry of Health and Long-Term Care. Quality-Based procedures: clinical handbook for hip fracture. Toronto, ON: Health Quality Ontario, 2013. Available: https://www.health.gov.on.ca/en/pro/programs/ecfa/docs/qbp_hipfracture.pdf
- 10.Reyes BJ, Mendelson DA, Mujahid N, Mears SC, Gleason L, Mangione KK, Nana A, Mijares M, Ouslander JG. Postacute management of older adults suffering an osteoporotic hip fracture: A consensus statement from the international geriatric fracture society. Geriatr Orthop Surg Rehabil. 2020;11:2151459320935100. 10.1177/2151459320935100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence. Hip fracture overview. 2020. Available: http://pathways.nice.org.uk/pathways/hip-fracture
- 12.Backman C, Harley A, Papp S, French-Merkley V, Beaulé PE, Poitras S, Dobransky J, Squires JE. Barriers and enablers to early identification, referral and access to geriatric rehabilitation Post-Hip fracture: A Theory-Based descriptive qualitative study. Geriatr Orthop Surg Rehabil. 2022;13:21514593211047666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Backman C, Shah S, Webber C, Turcotte L, McIsaac DI, Papp S, Harley A, Beaulé P, French-Merkley V, Berdusco R, Poitras S, Tanuseputro P. Postsurgery paths and outcomes for hip fracture patients (POST-OP HIP PATHS): a population-based retrospective cohort study protocol. BMJ Open. 2022;12(12):e065599. 10.1136/bmjopen-2022-065599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The reporting of studies conducted using observational Routinely-collected health data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mondor L, Maxwell CJ, Bronskill SE, et al. The relative impact of chronic conditions and Multimorbidity on health-related quality of life in Ontario long-stay home care clients. Qual Life Res. 2016;25:2619–32. [DOI] [PubMed] [Google Scholar]
- 16.McIsaac DI, Wong CA, Huang A, Moloo H, van Walraven C. Derivation and Validation of a Generalizable Preoperative Frailty Index Using Population-based Health Administrative Data. Ann Surg. 2019;270(1):102–108. 10.1097/SLA.0000000000002769. PMID: 29672410. [DOI] [PubMed]
- 17.Ryder T, Close J, Harris I, et al. Patient and hospital factors influencing discharge destination following hip fracture. Australas J Ageing. 2021;40(3):e234–43. [DOI] [PubMed] [Google Scholar]
- 18.Vincent C, Jones A, Tanuseputro P, et al. Comparison of discharge destination post hip fracture among rural vs. Urban dwelling older adults: A retrospective cohort study. Can Geriatr J. 2024;27(3):383–4. [Google Scholar]
- 19.Backman C, Li W, Shah S, et al. Factors influencing initial rehabilitation type after hip fracture surgery: A retrospective cohort study. J Am Med Dir Assoc Published Online March. 2025;19. 10.1016/j.jamda.2025.105521. [DOI] [PubMed]
- 20.Liu X, Seidel JE, McDonald T, et al. Rural-Urban disparities in realized Spatial access to general practitioners, orthopedic surgeons, and physiotherapists among people with osteoarthritis in Alberta, Canada. Int J Environ Res Public Health. 2022;19(13):7706. 10.3390/ijerph19137706. Published 2022 Jun 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olthof M, Stevens M, Bulstra SK, et al. The association between comorbidity and length of hospital stay and costs in total hip arthroplasty patients: a systematic review. J Arthroplast. 2014;29(5):1009–14. [DOI] [PubMed] [Google Scholar]
- 22.Wong RMY, Zu Y, Chau WW, et al. High Charlson comorbidity index score is associated with early fracture-related complication for internal fixation of neck of femur fractures. Sci Rep. 2022;12(1):4749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Charlesworth CJ, Smit E, Lee DSH, et al. Polypharmacy among adults aged 65 years and older in the united States: 1988–2010. J Gerontol Ser Biol Sci Med Sci. 2015;70(8):989–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182:1609–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muhm M, Walendowski M, Danko T, et al. Length of hospital stay for patients with proximal femoral fractures: influencing factors. Der Unfallchirurg. 2016;119(7):560–9. [DOI] [PubMed] [Google Scholar]
- 26.Tang C, Fu SP. Effect of surgical timing of femoral intertrochanteric fractures on 1-year postoperative mortality in elderly. Zhongguo Gu Shang. 2017;30(7):602–6. [DOI] [PubMed] [Google Scholar]
- 27.He W, You Y, Sun K, et al. Admission delay is associated with worse surgical outcomes for elderly hip fracture patients: a retrospective observational study. World J Emerg Med. 2020;11(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ek S, Meyer AC, Hedström M, et al. Hospital length of stay after hip fracture and it’s association with 4-month mortality-exploring the role of patient characteristics. J Gerontol Ser Biol Sci Med Sci. 2022;77(7):1472–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.heikh HQ, Alnahhal A, Aqil A, et al. Length of hospital stay following hip fracture and risk of 30 and 90 day mortality in a united Kingdom cohort. Acta Orthop Belg. 2021;87(4):607–17. [DOI] [PubMed] [Google Scholar]
- 30.Gurger M. Factors impacting 1-year mortality after hip fractures in elderly patients: a retrospective clinical study. Niger J Clin Pract. 2019;22(5):648–51. [DOI] [PubMed] [Google Scholar]
- 31.Ntuli M, Filmalter CJ, White Z, et al. Length of stay and contributing factors in elderly patients who have undergone hip fracture surgery in a tertiary hospital in South Africa. Int J Orthop Trauma Nurs. 2020;37:100748. [DOI] [PubMed] [Google Scholar]
- 32.Pitzul KB, Wodchis WP, Carter MW, Kreder HJ, Voth J, Jaglal SB. Post-acute pathways among hip fracture patients: a system-level analysis. BMC Health Serv Res. 2016;16:275. 10.1186/s12913-016-1524-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nikkel LE, Kates SL, Schreck M et al. Length of hospital stay after hip fracture and risk of early mortality after discharge in new York State: retrospective cohort study. BMJ (Clinical Res ed). 2015;351. [DOI] [PMC free article] [PubMed]
- 34.Rasu RS, Zalmai R, Karpes Matusevich AR, et al. Shorter length of hospital stay for hip fracture in those with dementia and without a known diagnosis of osteoporosis in the USA. BMC Geriatr. 2020;20(1):523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rajamaki B, Koponen M, Hartikainen S, et al. Length of hospital stay after hip fracture and readmission rates of persons with and without Alzheimer’s disease: a matched cohort study. BMC Geriatr. 2020;20(1):214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cao H, Yu J, Chang Y, et al. Construction and validation of a risk prediction model for delayed discharge in elderly patients with hip fracture. BMC Musculoskelet Disord. 2023;24:66. 10.1186/s12891-023-06166-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Van Heghe A, Mordant G, Dupont J, Dejaeger M, Laurent MR, Gielen E. Effects of orthogeriatric care models on outcomes of hip fracture patients: A systematic review and Meta-Analysis. Calcif Tissue Int. 2022;110(2):162–84. 10.1007/s00223-021-00913-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dakhil S, Thingstad P, Frihagen F, Johnsen LG, Lydersen S, Skovlund E, et al. Orthogeriatrics prevents functional decline in hip fracture patients: report from two randomized controlled trials. BMC Geriatr. 2021;21(1):208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vendittoli PA, Pellei K, Desmeules F, et al. Enhanced recovery short-stay hip and knee joint replacement program improves patients outcomes while reducing hospital costs. Orthop Traumatol Surg Res. 2019;105:1237–43. [DOI] [PubMed] [Google Scholar]
- 40.Frassanito L, Vergari A, Nestorini R, et al. Enhanced recovery after surgery (ERAS) in hip and knee replacement surgery: description of a multidisciplinary program to improve management of the patients undergoing major orthopedic surgery. Musculoskelet Surg. 2020;104(1):87–92. [DOI] [PubMed] [Google Scholar]
- 41.Ding ZC, Xu B, Liang ZM, et al. Limited influence of comorbidities on length of stay after total hip arthroplasty: experience of enhanced recovery after surgery. Orthop Surg. 2020;12(1):153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data set from this study is held securely in coded form at ICES. While data sharing agreements prohibit ICES from making the data set publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS. The full data set creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.