Abstract
Background
Osteoporosis, a common metabolic bone condition primarily affecting geriatrics globally, weakens bones and raises fracture risk. Prior osteoporotic fractures heighten susceptibility to further fractures, notably hip fractures, impacting outcomes post-surgical management. Analyzing this link is vital for optimizing interventions for at-risk individuals. This study investigates these associations and suggests interventions for high-risk patients.
Methods
This study is a retrospective case-control analysis of 1234 patients who underwent hip fracture surgery. Hospital records from two teaching university hospitals and two major governmental hospitals in Jordan over a three-year period were reviewed. Data encompassed patient demographics, comorbidities, perioperative variables, and postoperative outcomes and complications.
Results
Of the 1234 patients, 124 (10%) had prior fragility fractures (PFF): 85 contralateral hip (68.5%), 25 distal radius (20.2%), and 18 proximal humerus fractures (14.5%). Patients with prior contralateral hip fractures had higher rates of hypertension (55.5% vs. 41.1%, p = 0.03) and dementia (3.5% vs. 2.1%, p = 0.09), with trends in diabetes (38.8% vs. 31.3%, p = 0.17) and ICU admissions (7.0% vs. 4.3%, p = 0.33) that were not statistically significant. Blood transfusion rates were comparable (35.3% vs. 33.4%, p = 0.82). Subgroup analysis showed that patients with prior proximal humerus fractures had significantly higher postoperative strong analgesic use (60.5% vs. 43.2%, p = 0.007) and increased rates of dementia compared to other subgroups. However, these findings were specific to this subgroup and cannot be generalized to all PFF patients. The one-year all-cause mortality rate was 10.6% for patients with PFF and 6.2% for those without (p = 0.22). Although not statistically significant, this trend may hold clinical relevance in understanding the prognosis of this high-risk subgroup.
Conclusion
patients with prior contralateral hip fractures exhibited higher chances of postoperative ICU admission and increased comorbidity rates. This highlights the necessity for tailored care for this subgroup.
Level of evidence
Level III, Retrospective cohort study.
Keywords: Hip fracture, Osteoporosis, Fragility fracture, Geriatric fractures, Proximal humerus fracture, Distal radius fracture
Introduction
Osteoporosis, a pervasive disease primarily affecting the elderly on a global scale, is categorized as a metabolic bone disorder characterized by a quantifiable reduction in bone mineral density (BMD), predominantly impacting trabecular bones within the skeletal system [1, 2]. According to the World Health Organization (WHO) criteria, osteoporosis manifests when BMD registers 2.5 standard deviations (SD) or more below the mean value observed in young, healthy individuals, indicated by a T-score of less than − 2.5 SD [3–5]. Osteoporosis has been consistently linked to a wide spectrum of fractures, with a particular focus on the vertebral columns, proximal humerus, distal radius, and hip [6–8]. Among these fractures, vertebral osteoporotic fractures and hip fractures have shown a high association with increased morbidity and mortality rates, especially among the geriatric population [9–11]. This highlights the significant impact that osteoporosis-related fractures can have on the overall health and well-being of elderly patients [12, 13].
Patients with a history of osteoporosis-related fractures present with compromised bone health compared to those with an intact bone status, necessitating a thorough examination of the consequences of pre-existing fragility fractures on outcomes and complications in hip fracture surgery [14, 15]. This assessment is crucial for unraveling the intricate relationship between prior osteoporotic events and subsequent health outcomes [16, 17]. By exploring the impact of prior fragility fractures on hip fracture patients, a more comprehensive understanding can be achieved regarding the potential amplification of complications and compromised recovery trajectories [18, 19].
Despite extensive research on osteoporosis and related fractures, a knowledge gap remains regarding the long-term impact of prior fragility fractures on postoperative outcomes in patients undergoing hip fracture surgery. Existing studies primarily focus on immediate fracture risk and general osteoporosis management, often overlooking how prior fractures can trigger a cascade of physiological, functional, and psychological consequences that adversely affect surgical recovery and complications. These fractures are not merely isolated events but indicators of systemic bone fragility, reduced muscle strength, and diminished functional reserve—factors that collectively compromise postoperative recovery [20–22]. Additionally, patients with a history of fragility fractures often present with comorbidities such as osteoporosis, cardiovascular disease, and cognitive decline, all of which elevate perioperative risks [23, 24]. This complex interplay of decreased bone quality, functional deterioration, and psychosocial challenges highlights the critical need for a deeper understanding of how prior fragility fractures influence surgical outcomes, particularly in hip fracture surgery.
This study addresses the gap in understanding the impact of different types of prior fragility fractures—such as contralateral hip, distal radius, and proximal humerus fractures—on postoperative outcomes. By delineating the complex interplay between osteoporosis and hip fractures, our research aims to inform targeted intervention strategies that optimize outcomes for high-risk geriatric patients predisposed to bone fragility.
Patients and methods
In this study, we employed a retrospective cohort study design, wherein we conducted a comprehensive review of hospital records pertaining to all patients included in the study.
This study involved a sample size of 1234 patients who underwent hip fracture surgery and were recruited from two leading teaching university hospitals and two major governmental hospitals in Jordan. A post hoc power analysis was conducted, revealing a statistical power of 0.85 (85%) to detect meaningful differences between groups, with an alpha level of 0.05 and a medium effect size (Cohen’s d = 0.5). The findings confirmed that the sample size of 1234 patients (124 with prior fractures and 1110 without) was adequate for identifying statistically significant differences.
The data collection spanned a period of three years, from January 2019 to December 2021. The inclusion criteria encompassed patients admitted with hip fractures involving the femur neck and intertrochanteric region, aged > 55 years, and treated using surgical interventions (fixation with either intramedullary nail or dynamic hip screw for intertrochanteric fractures and arthroplasty for femur neck fractures). Conversely, the exclusion criteria comprised patients falling outside the specified study timeframe, those who did not receive surgical treatment, individuals with pathological fractures, and those with fractures resulting from motor vehicle accidents.
While vertebral and distal femur fractures are osteoporosis-related injuries, they were excluded from this study due to very limited patient numbers and insufficient data, which could introduce bias and affect the reliability of our findings. Vertebral fractures are often underdiagnosed without routine imaging, and distal femur fractures are far less common compared to hip, distal radius, and proximal humerus fractures, making them less relevant to our research focus.
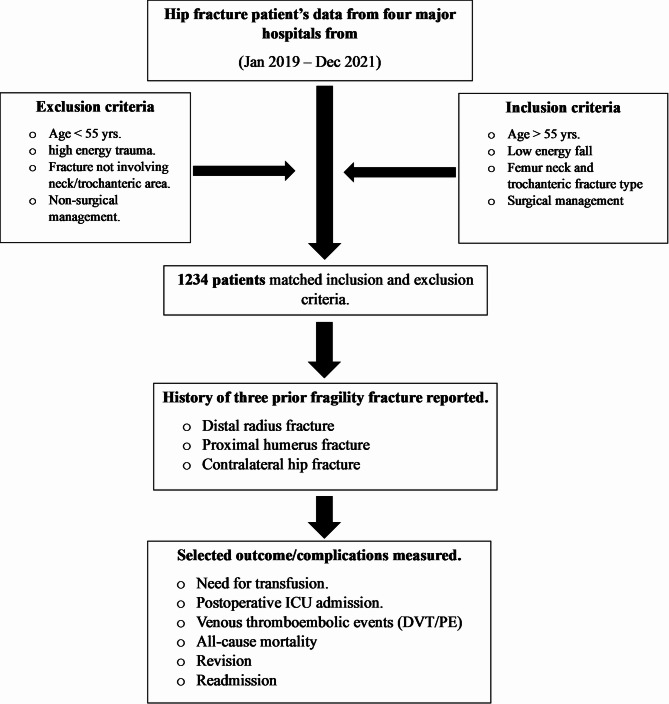
The collected data were systematically categorized into three distinct domains: the patient’s health profile and comorbidities, perioperative variables, and postoperative outcomes and complications. The first category encompassed a comprehensive range of data points, including age, gender, smoking status, a wide spectrum of comorbidities, and the patient’s prior history of osteoporosis-related fractures, with a specific focus on fractures involving the proximal humerus, distal radius, and the contralateral hip. The perioperative variables included the type of anesthesia used, the specific fracture type, the fixation method utilized, the operating surgeon, the duration of hospitalization, and the use of perioperative anticoagulants. Lastly, the postoperative outcomes and complications category included factors such as the need for blood transfusion, admission to the postoperative Intensive Care Unit (ICU), occurrences of postoperative thromboembolic events (including Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE)), all-cause mortality, readmission rates, and the need of revision procedures. Figure 1 is a flowchart of the study methodology.
Fig. 1.
Flow chart summary of the study methodology
Appropriate Institutional Review Board (IRB) for this study was obtained by the Mutah University Medical Research Office, IRB number (Approval number 123/2023). All participants involved in the research had consented to participate. To ensure ethical conduct, informed consent was obtained from all study participants, indicating their voluntary agreement to take part and their understanding of the study’s purpose. Throughout the study, adherence to ethical standards was maintained in accordance with the Code of Ethics outlined by the World Medical Association, as delineated in the Declaration of Helsinki. All patient data, including any identifying information, was securely protected.
Data for this study was analyzed using Microsoft Office Excel 2022® and the International Package of Social Sciences (SPSS)® version 23. Descriptive statistics were used to provide information about the sample. Independent samples t test was used to compare means between two categories variable. Chi square and Fisher’s Exact test were used to determine the relationship between categorical variables. A p value of less than or equal to 0.05 was considered significant.
Data normality was assessed using the Shapiro-Wilk test and visual inspection. T-tests were used for normally distributed data, Mann-Whitney U tests for non-normal data, and Chi-square or Fisher’s exact tests for categorical variables.
Results
A total of 1234 patients were included in this study, with 124 (10.0%) having a history of prior osteoporosis-related fragility fractures and 1110 (90.0%) having none. Among those with prior fractures, 85 (68.5%) had contralateral hip fractures, 25 (20.2%) had distal radius fractures, and 18 (14.5%) had proximal humerus fractures. Osteoporosis was significantly more prevalent among patients with prior fragility fractures (76.6% vs. 3.3%, p < 0.001), and bisphosphonate use was also expectingly associated with this group (4.8% vs. 1.7%, p = 0.033). While not statistically significant, trends indicated a higher proportion of females (60.5% vs. 52.5%) and non-smokers (75.0% vs. 71.4%) among those with prior fragility fractures compared to those without.
Variables with normal distribution, including patient age and length of hospital stay, were analyzed using independent samples t-tests. The analysis showed no significant differences between patients with and without prior fragility fractures for these variables (e.g., mean age: 77 vs. 75 years, p = 0.56; mean hospital stays: 7.5 vs. 7.4 days, p = 0.85), indicating comparable distributions across groups.
Overall, Table 1 underscores key demographic and clinical distinctions between patients with and without prior fragility fractures. Among those with fragility fractures, 31 patients (25.0%) had a history of cardiovascular disease compared to 341 patients (30.7%) without such fractures. Dementia (Alzheimer type) was present in 5 patients (4.0%) in the fragility fracture group versus 24 patients (2.2%) in the non-fragility group. Additionally, preoperative ICU admission was required for 4 patients (3.2%) with fragility fractures, compared to 27 patients (2.4%) without. These findings highlight important differences in patient health profiles that can inform clinical management decisions.
Table 1.
Comparison of health profiles between patients with and without history of fragility fractures. DM: diabetes mellitus, HTN: hypertension, preop: preoperative, ICU: intensive care unit. * Independent samples t test, ** fisher’s exact test
| Comparison | Patients without prior fragility fractures (n = 1110) n(%) |
Patients with prior fragility fractures (n = 124) n(%) |
(p-value) | |
|---|---|---|---|---|
| Age (yrs.) | Mean | 75 | 77 | 0.56* |
| Gender | Male | 527 (47.5%) | 49 (39.5%) | 0.055** |
| Female | 583 (52.5%) | 75 (60.5%) | ||
| Smoking | Smoker | 317 (28.6%) | 31 (25.0%) | 0.235** |
| Non-smoker | 793 (71.4%) | 93 (75.0%) | ||
| DM | Yes | 554 (49.9%) | 56 (45.2%) | 0.182** |
| No | 556 (50.1%) | 68 (54.8%) | ||
| HTN | Yes | 737 (66.4%) | 78 (62.9%) | 0.247** |
| No | 373 (33.6%) | 46 (37.1%) | ||
| Cardiovascular disease | Yes | 341 (30.7%) | 31 (25.0%) | 0.111** |
| No | 769 (69.3%) | 93 (75.0%) | ||
| Cerebrovascular disease | Yes | 206 (18.6%) | 19 (15.3%) | 0.226** |
| No | 904 (81.4%) | 105 (84.7%) | ||
| Endocrine disease | Yes | 47 (4.2%) | 5 (4.0%) | 0.574** |
| No | 1063 (95.8%) | 119 (96.0%) | ||
| Renal disease | Yes | 91 (8.2%) | 10 (8.1%) | 0.563** |
| No | 1019 (91.8%) | 122 (98.4%) | ||
| Dementia | Yes | 24 (2.2%) | 119 (96.0%) | 0.305** |
| No | 1086 (97.8%) | 5 (4.0%) | ||
| Osteoporosis | Yes | 37 (3.3%) | 95 (76.6%) | < 0.001** |
| No | 1073 (96.7%) | 29 (23.4%) | ||
| Bisphosphonate use | Yes | 19 (1.7%) | 6 (4.8%) | 0.033** |
| No | 1091 (98.3%) | 118 (95.2%) | ||
| Preop ICU need | Yes | 27 (2.4%) | 4 (3.2%) | 0.380** |
| No | 1083 (97.6%) | 120 (96.8%) | ||
The subgroup analysis of patients with prior fragility fractures revealed a similar mean age of 77 years across all subgroups. Among those with distal radius fractures, 18 (72.0%) were female, 20 (80.0%) were smokers, 23 (92.0%) had hypertension, and 5 (20.0%) had renal disease. In the proximal humerus fracture subgroup, 13 (72.3%) were female, 14 (77.7%) were smokers, 10 (55.5%) had hypertension, and 8 (44.5%) had diabetes. Patients with contralateral hip fractures included 47 (58.0%) females, 32 (39.5%) with diabetes, 47 (58.0%) with hypertension, and 3 (3.7%) requiring preoperative ICU admission due to an unstable medical condition. These findings highlight key demographic and clinical characteristics of each subgroup, offering insights into the variability within fragility fracture populations. A summary of these comparisons is provided in Table 2.
Table 2.
Summary of comparison between subgroups of patients with prior fragility fracture and their health profiles. DM: diabetes mellitus, HTN: hypertension, preop: preoperative, ICU: intensive care unit. * Independent samples t test, ** fisher’s exact test
| Comparison | Patients with prior fragility fractures (n = 124) |
p-value | |||
|---|---|---|---|---|---|
| Distal radius fracture (n = 25) |
Proximal humerus fracture (n = 18) |
Contralateral hip fracture (n = 81) |
|||
| Age (yrs.) | Mean | 77 | 76 | 77 | 0.96* |
| Gender | Male | 7 (28.0%) | 5 (27.8%) | 34 (42.0%) | 0.70** |
| Female | 18 (72.0%) | 13 (72.2%) | 47 (58.0%) | ||
| Smoking | Yes | 5 (20.0%) | 4 (22.2%) | 20 (24.7%) | 0.99** |
| No | 20 (80.0%) | 14 (77.8%) | 61 (75.3%) | ||
| DM | Yes | 14 (56.0%) | 8 (44.4%) | 32 (39.5%) | 0.17** |
| No | 11 (44.0%) | 10 (55.6%) | 49 (60.5%) | ||
| HTN | Yes | 23 (92.0%) | 10 (55.6%) | 47 (58.0%) | 0.03** |
| No | 2 (8.0%) | 8 (44.4%) | 34 (42.0%) | ||
| Cardiovascular disease | Yes | 8 (32.0%) | 2 (11.1%) | 22 (27.2%) | 0.37** |
| No | 17 (68.0%) | 16 (88.9%) | 59 (72.8%) | ||
| Cerebrovascular disease | Yes | 4 (16.0%) | 4 (22.2%) | 70 (86.4%) | 0.19** |
| No | 21 (84.0%) | 14 (77.8%) | 11 (13.6%) | ||
| Endocrine disease | Yes | 1 (4.0%) | 1 (5.6%) | 3 (3.7%) | 0.74** |
| No | 24 (96.0%) | 17 (94.4%) | 78 (96.3%) | ||
| Renal disease | Yes | 5 (20.0%) | 0 (0.0%) | 6 (7.4%) | 0.69** |
| No | 20 (80.0%) | 18 (100.0%) | 75 (92.6%) | ||
| Dementia | Yes | 2 (8.0%) | 0 (0.0%) | 77 (95.1%) | 0.09** |
| No | 23 (92.0%) | 18 (100.0%) | 4 (4.9%) | ||
| Preop ICU admission | Yes | 0 (0.0%) | 1 (5.6%) | 78 (96.3%) | 0.049** |
| No | 25 (100.0%) | 17 (94.4%) | 3 (3.7%) | ||
The comparison of outcomes and complications between patients with and without prior fragility fractures revealed no statistically significant differences; however, several findings may hold clinical relevance. The mean hospital stay was comparable between groups (7.5 vs. 7.4 days). Among patients with fragility fractures, 51 (41.1%) required postoperative blood transfusions, compared to 371 (33.4%) in those without fractures, suggesting a potential trend toward increased perioperative blood loss. Similarly, while venous thromboembolic events were rare (2.4% vs. 2.5%), and ICU admission rates remained slightly higher in the fragility fracture group (9.7% vs. 10.2%), these factors may still reflect an increased physiological burden in this population. Additionally, 16 patients (12.9%) with fragility fractures required readmission within one month, and one-year mortality was observed in 9 (7.3%), trends that, while not statistically significant, may indicate higher vulnerability in this subgroup. These findings underscore the need for heightened perioperative attention and tailored postoperative management for patients with prior fragility fractures. A summary of these comparisons is presented in Table 3. Comparison within the subgroups of patients with prior fragility fractures and patients without fragility fractures are demonstrated in Table 4.
Table 3.
Comparison between outcome/complications between patients with and without prior fragility fractures. readmission: readmission to hospital within one month of discharge regardless of the cause
| Comparison | Patients with prior fragility fracture compared with patients without fragility fracture | p-value | ||
|---|---|---|---|---|
| Prior fragility fracture (n = 124) |
No prior fragility fracture (n = 1110) |
|||
| Mean length of stay (days) | 7.5 | 7.4 | 0.85 | |
| Need for blood transfusion | 51 (41.1%) | 371 (33.4%) | 0.08 | |
| Thromboembolic events | 3 (2.4%) | 28 (2.5%) | 0.94 | |
| Postop ICU admission | 12 (9.7%) | 113 (10.2%) | 0.86 | |
| Postop opioids need | 75 (60.5%) | 664 (59.8%) | 0.93 | |
| Readmission | 16 (12.9%) | 116 (10.5%) | 0.40 | |
| Reason for readmission | Medical | 12 (9.7%) | 84 (7.6%) | 0.68 |
| Surgical | 4 (3.2%) | 32 (2.9%) | ||
| Need for revision | 5 (4.0%) | 33 (3.0%) | 0.51 | |
| Mortality | In-hospital | 3 (2.4%) | 23 (2.1%) | 0.10 |
| 1-month | 1 (0.8%) | 27 (2.4%) | 0.10 | |
| 3-month | 1 (0.8%) | 14 (1.3%) | 0.10 | |
| 6-month | 1 (0.8%) | 39 (3.5%) | 0.10 | |
| 1-yr | 9 (7.3%) | 36 (3.2%) | 0.10 | |
Table 4.
Subgroup analysis of patients with prior fragility fractures compared to patients without fragility fractures. DRF: distal radius fracture, PHF: proximal humerus fracture, HF: contralateral hip fracture. LOS: length of stay, ICU: intensive care unit. Non: patients with no prior fragility fractures. **: denotes statistically significant findings (p < 0.05)
| Comparison | Subgroup analysis between patients with and without prior history of fragility fractures | ||||||
|---|---|---|---|---|---|---|---|
| DRF | PHF | HF | |||||
| DRF (n = 25) |
Non (n = 1110) |
PHF (n = 18) |
Non (n = 1110) |
HF (n = 81) |
None (n = 1110) |
||
| Mean LOS (days) | 8.0 | 7.4 | 6.4 | 7.4 | 7.6 | 7.4 | |
| p = 0.96 | p = 0.98 | p = 0.90 | |||||
| Need for blood transfusion | 11 | 371 | 10 | 371 | 30 | 371 | |
| p = 0.29 | p = 0.05 | p = 0.82 | |||||
| Thromboembolic events | 2 | 28 | 1 | 28 | 0 | 28 | |
| p = 07 | p = 0.4 | p = 0.12 | |||||
| Postop ICU admission | 4 | 113 | 2 | 113 | 6 | 113 | |
| p = 0.32 | p = 0.88 | p = 0.33 | |||||
| Postop opioids need | 15 | 664 | 11 | 664 | 51 | 664 | |
| p = 0.99 | p = 0.98 | p = 0.007** | |||||
| Readmission | 5 | 116 | 3 | 116 | 8 | 116 | |
| p = 0.12 | p = 0.40 | p = 0.60 | |||||
| Need for revision | 1 | 33 | 0 | 33 | 4 | 33 | |
| p = 0.78 | p = 0.44 | p = 0.36 | |||||
| Death | Hospital | 2 | 23 | 1 | 23 | 0 | 23 |
| p = 0.32 | p = 0.32 | p = 0.33 | |||||
| 1-mo | 0 | 27 | 0 | 27 | 0 | 27 | |
| p = 0.18 | p = 0.19 | p = 0.17 | |||||
| 3-mo | 1 | 14 | 0 | 14 | 0 | 14 | |
| p = 0.37 | p = 0.31 | p = 0.25 | |||||
| 6-mo | 1 | 39 | 0 | 39 | 1 | 39 | |
| p = 0.41 | p = 0.44 | p = 0.39 | |||||
| 1-yr | 3 | 36 | 0 | 36 | 6 | 36 | |
| p = 0.29 | p = 0.21 | p = 0.22 | |||||
Patients with prior contralateral hip fractures exhibited a higher likelihood of postoperative ICU admission compared to those with proximal humerus and distal radius fractures (p = 0.04), suggesting a greater perioperative risk in this subgroup. Additionally, they had higher rates of diabetes (p = 0.17), hypertension (p = 0.03), cerebrovascular disease (p = 0.19), and dementia (p = 0.09), reflecting a more complex comorbidity profile. Compared to patients with other prior fractures, those with contralateral hip fractures also showed higher rates of postoperative blood transfusion (p = 0.82), ICU admission (p = 0.33), strong analgesic use (p = 0.007), need for revision surgery (p = 0.36), and one-year all-cause mortality (p = 0.22). While some of these differences were not statistically significant, they highlight clinically meaningful trends, reinforcing that patients with prior contralateral hip fractures represent a high-risk group requiring specialized perioperative care and close postoperative monitoring. A summary of these findings is presented in Table 4.
Discussion
The analysis of 1234 individuals indicated that almost 10% had previously had fractures associated with osteoporosis. These fractures included 85 hip fractures on the opposite side, 25 fractures in the distal radius, and 18 fractures in the proximal humerus. Patients who had previously had fractures due to fragility, with an average age of 77 years, showed specific patterns of comorbidity. Among them, 45.5% had diabetes and 25.1% had a history of cardiovascular disease. Specific demographic insights were revealed by subgroup analysis conducted within different fracture types. Postoperative outcomes showed little variations in the duration of hospital stay, with 41.1% of patients with fragility fractures needing blood transfusions, and just 0.02% having venous thromboembolic events. Out of the total number of patients, twelve individuals (0.09%) needed to be admitted to the Intensive Care Unit (ICU) after their surgery. Additionally, sixteen patients had to be readmitted within the first month after their operation. The one-year mortality rate for individuals who had previously had fragility fractures was 0.07%, providing valuable insights into the various ramifications of these injuries on future hip fractures.
The assessment of geriatric patients having hip fracture surgery focuses on the presence of several medical comorbidities. Bliemel et al. emphasize the correlation between neurological and kidney-related disorders and their effects on the overall state of health [20]. In addition, Liu et al. have identified a range of risk factors for death, including advanced age, male gender, cognitive impairment, delirium, cardiovascular and renal illnesses, malignancy, smoking, obesity, and suboptimal body weight [21]. Meltzer-Bruhn et al. emphasize the significance of these variables in leading to perioperative problems [22]. Crane et al.‘s study broadens the range of investigation to include both the ambulatory state before and after surgery, as well as the general medical condition [23]. Within our group, the most common additional health conditions are diabetes, high blood pressure, ischemic heart disease, and cerebrovascular diseases, which might include dementia. This work enhances the current body of research by highlighting the occurrence of these other medical conditions in elderly people with hip fractures, providing useful knowledge about their overall health status.
The simultaneous occurrence of fractures in the distal radius and hip among older individuals, as shown by Shabat et al., poses a multifaceted problem that necessitates extended hospitalization and rehabilitation [24]. Padegimas et al. observed that distal radius fractures in this specific population might indicate the presence of osteoporosis and an increased likelihood of falling, which could serve as early indicators of more serious hip fractures [25]. Levin et al. stress the need of tailoring therapy to each person, taking into account factors such as bone quality and amount of functional activity. They also note that nonsurgical alternatives are typically considered suitable [26]. Our research found that persons who had geriatric hip fractures with a prior history of distal radius fractures had a higher likelihood of being female, non-smokers, diabetic, and hypertensive. Nevertheless, there were no notable correlations found in relation to postoperative outcomes, including blood transfusion, ICU hospitalization, readmission, revision, or death.
Osteoporosis, which mostly affects the upper arm bone closest to the body (proximal humerus), presents specific difficulties, particularly in older populations where fractures often occur due to low-impact falls. Smith et al. observed notable issues in this particular situation, highlighting elevated frequencies of initial problems and the need for further surgical procedures [27]. Dealing with these fractures is complex since it is difficult to achieve and maintain proper alignment and secure the hardware, as highlighted by Stone et al. [28]. Egol et al. have emphasized that the use of locking plates might lead to possible issues such as screw penetration, implant failure, and osteonecrosis [29]. In order to address these problems and get favorable functional results, Mohanty et al. emphasized the need of meticulous pre-operative preparation, proactive osteoporosis treatment, and prudent rehabilitation [30]. Significantly, our analysis revealed no elevated risks associated with variables such as duration of hospitalization, blood transfusion, thromboembolic events, admission to the intensive care unit after surgery, readmissions, and overall mortality.
Individuals suffering from severe osteoporosis may have had a previous fracture in the hip on the opposite side. According to Sawalha et al., this particular subgroup is at a higher risk of being placed in institutions, being older in age, having limited mobility, and experiencing higher death rates within one year [31]. Yun et al. observed a higher likelihood of periprosthetic femoral fracture on the same side as the artificial joint, in cases where there was femoral osteolysis and degenerative alterations in the opposite hip [32]. Saxena et al. established a connection between certain medical problems and subsequent fractures in the opposite proximal femur [33]. Our research found that patients who had previously had a fragile fracture in the opposite hip had a greater occurrence of cardiovascular and cerebrovascular illnesses, dementia, higher rates of revision, and increased overall mortality after one year. These results support and expand upon previous findings.
Based on the authors’ understanding and the available literature, there is a lack of previous research examining how previous fragility fractures, particularly those affecting the distal radius, proximal humerus, and opposite hip, affect the outcomes and complications in elderly patients who are undergoing surgery to fix low-energy hip fractures. This research aims to address the lack of information by giving significant insights into the outcomes and complications of a particular subset of hip fracture patients. It will contribute to a more thorough understanding of their clinical profile.
An important consideration that was not fully explored in our analysis is the impact of multiple prior fragility fractures on patient outcomes. While our study primarily focused on comparing outcomes between patients with a single prior fracture and those without, the presence of multiple fractures could exacerbate the observed complications. Patients with multiple prior fractures may represent a higher-risk subgroup, with cumulative bone fragility and increased susceptibility to adverse outcomes following hip fracture surgery. This limitation highlights the need for future research to stratify patients based on the number and types of prior fractures to better understand the compounded effects on postoperative recovery.
The concept of a ‘fracture cascade’ is particularly relevant here. The fracture cascade refers to the phenomenon where one fragility fracture significantly increases the risk of subsequent fractures, contributing to a downward spiral of bone health deterioration and reduced physical function. This cascade effect could partially explain some of the outcomes observed in our study, such as higher rates of comorbidities and increased postoperative complications in patients with prior fractures. By acknowledging this effect, we recognize that our findings may be influenced by an underlying progression of bone fragility rather than isolated fracture events. Future studies should consider this phenomenon to account for potential bias and to develop targeted interventions that address the needs of patients experiencing multiple fractures.
Although our study yielded significant findings and conclusions, we must acknowledge several limitations. Specifically, our focus was on proximal humerus, distal radius, and contralateral hip fractures, with no inclusion of vertebral osteoporotic fractures due to insufficient data availability on this matter. Moreover, our mortality data were only recorded up to one year, with no subsequent follow-up conducted to track mortality rates beyond this period. Although the numerical imbalance between groups is recognized, the sample size was deemed sufficient for analysis. Future studies are encouraged to enhance statistical robustness by achieving a more balanced cohort. The study’s focus on prior fragility fractures, rather than imminent fracture risk, is acknowledged as a limitation. Future research should consider integrating imminent fracture risk to provide a more comprehensive assessment of clinical outcomes.
The disproportionate sample size between patients with and without prior fragility fractures may influence the statistical power of subgroup analyses. However, a post hoc power analysis confirmed sufficient overall power (85%) for primary comparisons, supporting the reliability of the main findings. Future studies with larger, balanced cohorts are recommended to strengthen subgroup analyses and validate these results. Although the overall study was adequately powered, the smaller sample sizes in subgroup analyses may have limited the ability to detect statistically significant differences, warranting cautious interpretation of those results.
Nonetheless, we believe that this research lays the groundwork for future investigations encompassing these two areas of concern.
Conclusion
While no statistically significant differences were found in postoperative ICU admission rates or overall comorbidity profiles, patients with prior contralateral hip fractures demonstrated a significant increase in blood transfusion requirements, likely associated with higher surgical blood loss. Additionally, trends toward higher prevalence of hypertension and dementia were observed. Although not statistically significant, these trends may hold clinical relevance in guiding tailored perioperative care for this high-risk subgroup.
Clinical implications
The clinical implications of our study convey three essential recommendations to orthopedic surgeons and the healthcare team involved in the care of patients undergoing hip fracture surgery.
Preoperative assessment
The study highlights the importance of considering a patient’s history of fragility fractures, especially contralateral hip fractures, during preoperative assessments. This information can help predict potential complications and assist with risk stratification. Early identification of this high-risk subgroup enables proactive measures and customized interventions, leading to better postoperative outcomes.
Specialized care for high-risk subgroup
The study emphasizes the heightened risk and comorbidities in patients with a history of contralateral hip fractures. To address this, orthopedic surgeons and healthcare teams should adopt a specialized care approach, including closer monitoring, optimization for comorbidities, and early assisted rehabilitation programs. This approach optimizes postoperative care and enhances patient outcomes.
Informed consent discussions
Informed consent discussions are crucial for informing patients about surgery risks. The study emphasizes the higher risks and complications from prior fragility fractures, including contralateral hip fractures. Surgeons should prioritize transparent communication during these discussions, presenting the risks and involving patients in decision-making. This patient-centered approach fosters collaboration and aligns with shared decision-making principles in orthopedic practice.
Author contributions
Moh’d S. Dawod conceptualized, designed, and conducted the study, curated data, and drafted the manuscript. Mohammad N. Alswerki performed formal analysis and contributed to methodology and manuscript editing. Mohamad Samih Yasin contributed to investigation, data curation, manuscript editing, and visualization. Anas AR Altamimi contributed to methodology, software, validation, and visualization. Yaser Saber contributed to conceptualization, resourcing, manuscript review, and supervision. Obada Alrawashdeh assisted in investigation and manuscript review. Tayseer Afifi performed formal analysis and participated in manuscript review. Jihad Alajlouni oversaw the study, provided supervision, administered the project, and secured funding.
Funding
All authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Data availability
The data that support the findings of this study are available upon appropriate request from the corresponding author. The data is not publicly available due to privacy or ethical restrictions.
Declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Appropriate Institutional Review Board (IRB) for this study was obtained by the Mutah University Medical Research Office, IRB number (Approval number 123/2023).
Human ethics and consent to participate
All participants consented to the study, understanding its purpose and voluntarily agreeing to partake. Ethical standards were adhered to per the World Medical Association’s Declaration of Helsinki, ensuring secure protection of all patient data and identifying information.
Consent to publish
Not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sözen T, Özışık L, Başaran NÇ. An overview and management of osteoporosis. Eur J Rheumatol. Mar. 2017;4(1):46. 10.5152/EURJRHEUM.2016.048. [DOI] [PMC free article] [PubMed]
- 2.Cosman F et al. Sep., Clinician’s Guide to Prevention and Treatment of Osteoporosis, Osteoporos. Int., vol. 25, no. 10, pp. 2359–2381, 2014, 10.1007/S00198-014-2794-2 [DOI] [PMC free article] [PubMed]
- 3.Reginster JY, Burlet N. Osteoporosis: A still increasing prevalence, Bone, vol. 38, no. 2 SUPPL. 1, pp. 4–9, 2006, 10.1016/J.BONE.2005.11.024 [DOI] [PubMed]
- 4.Pisani P, et al. Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop. 2016;7(3):171–81. 10.5312/WJO.V7.I3.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: A world-wide projection, Osteoporos. Int., vol. 2, no. 6, pp. 285–289, Nov. 1992, 10.1007/BF01623184 [DOI] [PubMed]
- 6.Rinonapoli G, Ruggiero C, Meccariello L, Bisaccia M, Ceccarini P, Caraffa A. Osteoporosis in Men: A Review of an Underestimated Bone Condition, Int. J. Mol. Sci. 2021, Vol. 22, Page 2105, vol. 22, no. 4, p. 2105, Feb. 2021. 10.3390/IJMS22042105 [DOI] [PMC free article] [PubMed]
- 7.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures, Osteoporos. Int., vol. 17, no. 12, pp. 1726–1733, Dec. 2006, 10.1007/S00198-006-0172-4 [DOI] [PubMed]
- 8.Pietri M, Lucarini S. The orthopaedic treatment of fragility fractures, Clin. Cases Miner. Bone Metab., vol. 4, no. 2, p. 108, May 2007, Accessed: Nov. 25, 2023. [Online]. Available: /pmc/articles/PMC2781236/ [PMC free article] [PubMed]
- 9.Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag. Nov. 2014;10:937. 10.2147/TCRM.S72456. [DOI] [PMC free article] [PubMed]
- 10.Rizkallah M, et al. Comparison of morbidity and mortality of hip and vertebral fragility fractures: which one has the highest burden? Osteoporos Sarcopenia. Sep. 2020;6(3):146. 10.1016/J.AFOS.2020.07.002. [DOI] [PMC free article] [PubMed]
- 11.Chang CY, Tang CH, Chen KC, Huang KC. The mortality and direct medical costs of osteoporotic fractures among postmenopausal women in Taiwan. Osteoporos Int. Feb. 2016;27(2):665–76. 10.1007/S00198-015-3238-3. [DOI] [PubMed]
- 12.Osterhoff G, Morgan EF, Shefelbine SJ, Karim L, McNamara LM, Augat P. Bone mechanical properties and changes with osteoporosis, Injury, vol. 47, no. Suppl 2, p. S11, Jun. 2016, 10.1016/S0020-1383(16)47003-8 [DOI] [PMC free article] [PubMed]
- 13.Wang CY, Fu SH, Sen Yang R, Shen LJ, Wu FLL, Hsiao FY. Age- and gender-specific epidemiology, treatment patterns, and economic burden of osteoporosis and associated fracture in Taiwan between 2009 and 2013. Arch Osteoporos. Dec. 2017;12(1). 10.1007/s11657-017-0385-5. [DOI] [PubMed]
- 14.Marques A, Lourenço JAP, da Silva. The burden of osteoporotic hip fractures in Portugal: costs, health related quality of life and mortality, Osteoporos. Int., vol. 26, no. 11, pp. 2623–2630, Nov. 2015, 10.1007/s00198-015-3171-5 [DOI] [PubMed]
- 15.Budhia S, Mikyas Y, Tang M, Badamgarav E. Osteoporotic fractures: A systematic review of US healthcare costs and resource utilization. PharmacoEconomics. 2012;30(2):147–70. 10.2165/11596880-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 16.Dunnewind T et al. Jun., Economic Consequences and Potentially Preventable Costs Related to Osteoporosis in the Netherlands, Value Heal., vol. 20, no. 6, pp. 762–768, 2017, 10.1016/j.jval.2017.02.006 [DOI] [PubMed]
- 17.Mears SC, Kates SL. A guide to improving the care of patients with fragility fractures, edition 2. Geriatr Orthop Surg Rehabil. Jun. 2015;6(2):58. 10.1177/2151458515572697. [DOI] [PMC free article] [PubMed]
- 18.Abrahamsen C, Nørgaard B, Draborg E, Nielsen MF. The impact of an orthogeriatric intervention in patients with fragility fractures: A cohort study. BMC Geriatr. Oct. 2019;19(1):1–11. 10.1186/S12877-019-1299-4/TABLES/6. [DOI] [PMC free article] [PubMed]
- 19.Ross AJ, Ross BJ, Lee OC, Guild GN, Sherman WF. The impact of prior fragility fractures on complications after total hip arthroplasty: A propensity Score–Matched cohort study. Arthroplast Today. Oct. 2021;11:41. 10.1016/J.ARTD.2021.07.008. [DOI] [PMC free article] [PubMed]
- 20.Mühlberg W, Sieber C. Sarcopenia and frailty in geriatric patients: implications for training and prevention. Z Gerontol Geriatr. Feb. 2004;37(1):2–8. 10.1007/s00391-004-0203-8. [DOI] [PubMed]
- 21.Tarantino U, Piccirilli E, Fantini M, Baldi J, Gasbarra E, Bei R. Sarcopenia and fragility fractures: molecular and clinical evidence of the bone-muscle interaction., J. Bone Joint Surg. Am., vol. 97 5, no. 5, pp. 429–37, Mar. 2015, 10.2106/JBJS.N.00648 [DOI] [PubMed]
- 22.Vendrami C et al. Apr., Muscle parameters in fragility fracture risk prediction in older adults: A scoping review, J. Cachexia. Sarcopenia Muscle, vol. 15, no. 2, pp. 477–500, 2024, 10.1002/JCSM.13418 [DOI] [PMC free article] [PubMed]
- 23.Hurtado Y, Hernández OA, Atencio DP, De Leon G, Duque. Challenges in delivering effective care for older persons with fragility fractures. Clin Interv Aging. 2024;19:133–40. 10.2147/CIA.S433999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoon SH, Kim BR, Lee SY, Beom J, Choi JH, Lim JY. Influence of comorbidities on functional outcomes in patients with surgically treated fragility hip fractures: a retrospective cohort study, BMC Geriatr., vol. 21, no. 1, Dec. 2021, 10.1186/S12877-021-02227-5 [DOI] [PMC free article] [PubMed]
- 25.Bliemel C, Buecking B, Oberkircher L, Knobe M, Ruchholtz S, Eschbach D. The impact of pre-existing conditions on functional outcome and mortality in geriatric hip fracture patients. Int Orthop. 2017;41:1995–2000. [DOI] [PubMed] [Google Scholar]
- 26.Liu Y, Wang Z, Xiao W. Risk factors for mortality in elderly patients with hip fractures: a meta-analysis of 18 studies. Aging Clin Exp Res. 2018;30:323–30. [DOI] [PubMed] [Google Scholar]
- 27.Meltzer-Bruhn AT, Esper GW, Herbosa CG, Ganta A, Egol KA, Konda SR, Meltzer-Bruhn A, Egol K, Konda S. The role of smoking and body mass index in mortality risk assessment for geriatric hip fracture patients. Cureus. 2022;14(7). [DOI] [PMC free article] [PubMed]
- 28.Crane, JG, Kernek CB. Mortality associated with hip fractures in a single geriatric hospital and residential health facility: A ten-year review. J Am Geriatr Soc. 1983;31(8):472–5. [DOI] [PubMed] [Google Scholar]
- 29.Shabat S, Gepstein R, Mann G, Stern A, Nyska M. Simultaneous distal radius and hip fractures in elderly patients–implications to rehabilitation. Disabil Rehabil. 2003;25(15):823–6. [DOI] [PubMed] [Google Scholar]
- 30.Padegimas EM, Osei DA. Evaluation and treatment of osetoporotic distal radius fracture in the elderly patient. Curr Rev Musculoskelet Med. 2013;6:41–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levin LS, Rozell JC, Pulos N. Distal radius fractures in the elderly. JAAOS-Journal Am Acad Orthop Surg. 2017;25(3):179–87. [DOI] [PubMed] [Google Scholar]
- 32.Smith AM, Mardones RM, Sperling JW, Cofield RH. Early complications of operatively treated proximal humeral fractures. J Shoulder Elbow Surg. 2007;16(1):14–24. [DOI] [PubMed] [Google Scholar]
- 33.Stone MA, Namdari S. Surgical considerations in the treatment of osteoporotic proximal humerus fractures. Orthop Clin. 2019;50(2):223–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available upon appropriate request from the corresponding author. The data is not publicly available due to privacy or ethical restrictions.