Abstract
Introduction:
Osteomyelitis is a bone infection that may present acutely or chronically. Acute on chronic osteomyelitis refers to the exacerbation of symptoms in a patient with an underlying chronic infection. This case report presents a 19-year-old male diagnosed with acute on chronic osteomyelitis of the right distal femur, with no history of a discharging sinus for the past 6 months. Osteomyelitis is a bone infection commonly caused by bacteria, with Staphylococcus aureus being the most frequent pathogen. Chronic osteomyelitis can occasionally experience acute flare-ups, referred to as “acute on chronic osteomyelitis”. This report discusses the presentation, diagnosis, and management of a 19-year-old male with acute on chronic osteomyelitis of the right distal femur.
Case Report:
A 19-year-old male presented with increasing pain, swelling, and warmth over his right distal femur for 2 weeks. The pain was deep, throbbing, worsened by weight-bearing, and unrelieved by analgesics. He had similar complaints 6 months ago but had no symptoms such as fever or discharging sinus since then. There was no history of trauma or injury. On physical examination, the patient exhibited localized tenderness, mild swelling, broadening, irregularity, and warmth over the distal femur. Movements of the knee were restricted, and pain was elicited with direct palpation of the femur. No open wounds or discharging sinuses were present, and neurological and vascular examinations were unremarkable.Radiographs of the right femur showed sclerosis and focal cortical thickening, indicating chronic osteomyelitis. Magnetic resonance imaging confirmed the presence of marrow edema, cortical irregularity, and periosteal reaction, supporting the diagnosis of chronic osteomyelitis with an acute exacerbation. Blood tests revealed an elevated white blood cell count and C-reactive protein, indicating an acute inflammatory response. The patient received intravenous antibiotics preoperatively, followed by sequestrectomy, saucerization, and stimulan placement over the site where necrotic bone was removed to promote healing. Over 6 weeks, the patient experienced significant improvement in symptoms. Repeat imaging showed resolution of the acute infection, and long-term oral antibiotics were prescribed to manage chronic osteomyelitis.This case emphasizes the challenges of diagnosing and treating acute on chronic osteomyelitis, particularly when typical signs like a discharging sinus are absent. Early diagnosis and prompt, targeted antibiotic therapy is crucial for preventing complications such as deformities, limb loss, or sepsis.
Conclusion:
Effective management of acute on chronic osteomyelitis requires comprehensive evaluation through clinical history, imaging, and laboratory testing. Early intervention with surgical debridement and appropriate antibiotic therapy is vital to achieving favorable outcomes and preventing long-term complications.
Keywords: Acute on chronic osteomyelitis, stimulan, distal femur
Learning Point of the Article:
This case underscores the need for early recognition and prompt management of acute on chronic osteomyelitis using clinical, radiological, and laboratory evaluation, with surgical debridement and local antibiotic therapy being key to effective treatment.
Introduction
Osteomyelitis is an infection of the bone that can be acute or chronic [1, 2]. Chronic osteomyelitis is often associated with sequestrum formation and requires aggressive debridement. Culture-negative osteomyelitis presents an additional challenge as empirical antibiotic therapy is necessary [3, 4]. This case highlights the importance of surgical intervention in managing culture-negative chronic osteomyelitis.
Case Report
A 19-year-old male presents with a 6-month history of progressive pain and swelling in the left distal thigh, associated with difficulty in weight-bearing and walking. The pain is insidious, continuous, aggravated by activity, and relieved by rest. He reports intermittent fever and significant weight loss over the same period. There is history of knee aspiration done 6 months back for which medical records were not available. There is no history of trauma, tuberculosis, immunosuppression, or chronic illness.
Clinical examination reveals localized swelling, warmth, broadening, irregularity, and tenderness over the distal femur, with restricted knee movement (10–40°) but preserved distal neurovascular status. Laboratory investigations show marked leukocytosis, significantly elevated ESR (130 mm/h), and C-reactive protein (15.9 mg/dL), indicating an ongoing inflammatory or infectious process. Mantoux test was also negative. The findings are suggestive of a chronic infective or inflammatory condition, such as subacute osteomyelitis or a neoplastic process, warranting further imaging and possible biopsy [3, 4].
Radiological findings revealed an expansile lytic lesion with a wide zone of transition in the distal femur, cortical thickening and sclerosis, solid periosteal reaction, areas of cortical break with cloaca formation, and ill-defined soft tissue fluid collection-suggestive of acute on chronic osteomyelitis [5] (Fig. 1). Computed tomography imaging confirmed the presence of sequestrum, abscess formation, and cortical break, correlating with the radiographic findings (Fig. 2 and 3). Magnetic resonance imaging (MRI) revealed extensive marrow edema and confirmed the presence of sequestrum, further supporting the diagnosis (Fig. 4), whereas the MRI report corroborated the same (Fig. 5).
Figure 1.

Pre-operative X-ray.
Figure 2.
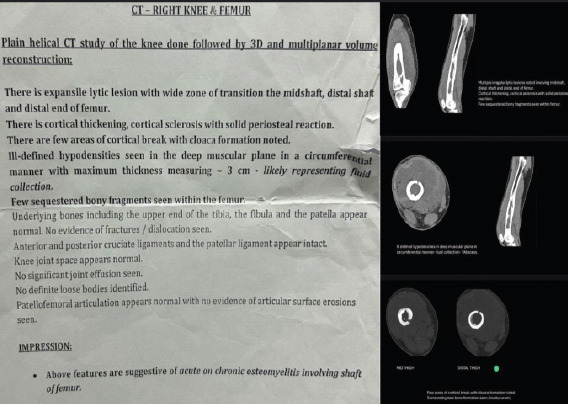
Computed tomography (CT) cuts showing sequestrum, abscess and cortical break along with CT report.
Figure 3.
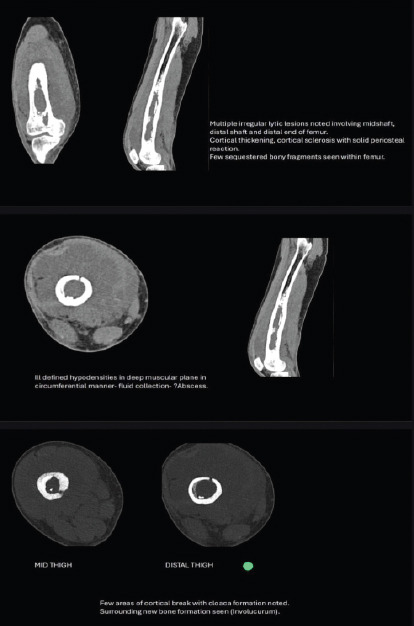
Computed tomography cuts showing sequestrum, abscess and cortical break.
Figure 4.
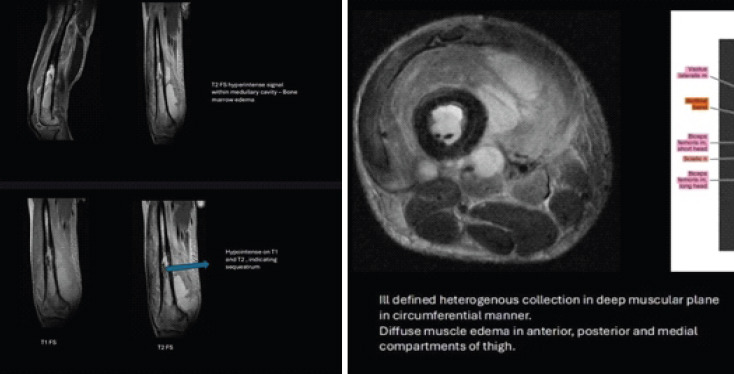
Magnetic resonance imaging sagittal and axial T1 and T2 images showing edema and sequestrum.
Figure 5.
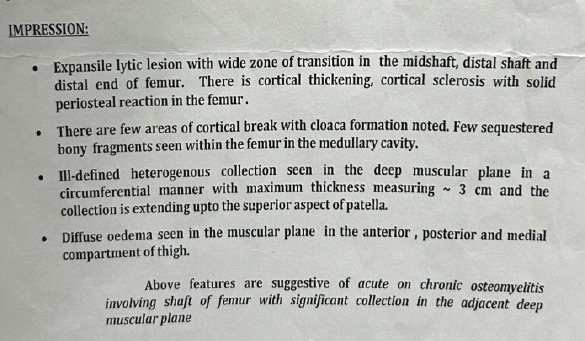
Magnetic resonance imaging report.
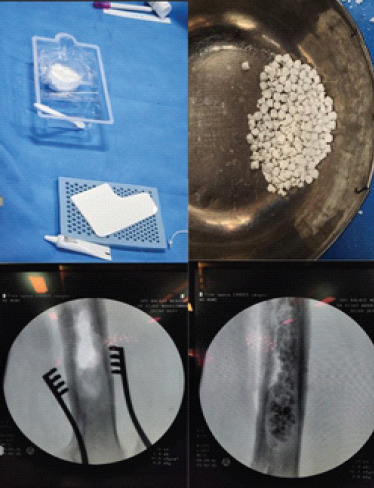
The patient underwent sequestrectomy with saucerization and bone stimulan placement under spinal anesthesia. Intraoperatively, the sequestrum was identified and removed (Fig. 6). The cavity was debrided, and stimulan (calcium sulfate antibiotic carrier) was placed to provide local antibiotic delivery (Fig. 7) [6-10]. Purulent collection was noted and was sent for cartridge-based nucleic acid amplification test, pus and wound culture and sensitivity, potassium hydroxide mount and acid-fast bacillus smear, all of which were negative. The sequestrum, tissue sample around the sequestrum, and generalized infective tissue were sent for histopathological analysis which confirmed the radiological diagnosis of acute on chronic osteomyelitis of distal femur (Fig. 8-10).
Figure 6.
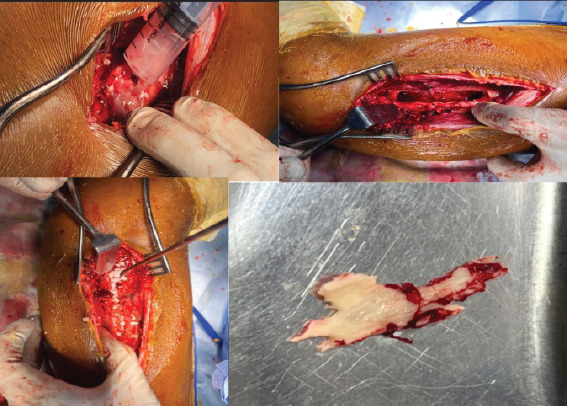
Intra operative pics showing pus and sequestrum.
Figure 7.

Stimulan preparation pics and C Arm pics.
Figure 8.
Post-operative X-ray.
Figure 10.
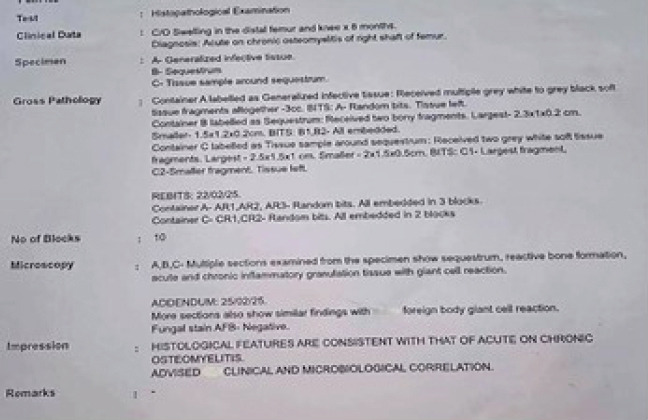
Histopathological report.
Broad spectrum antibiotics were started intravenously for 2 weeks, followed by oral antibiotics for 4 weeks. Above knee POP slab was applied to prevent fracture and non-weight-bearing walking with walker support for 6 weeks, followed by partial weight bearing for 2 months and then full weight bearing walking was started. Serial X-rays were taken and no signs of recurrence were noted (Fig. 8 and 9). The patient showed significant improvement in pain and mobility.
Figure 9.

Follow up post-operative X-ray.
Discussion
Chronic osteomyelitis is a challenging and persistent infection of the bone that often necessitates a multidisciplinary approach to treatment [1,2]. It is commonly caused by bacterial infections, particularly Staphylococcus aureus, but can also be caused by a variety of other pathogens, including those that are difficult to culture [3,4]. Culture-negative osteomyelitis, as in this case, complicates antibiotic therapy, as the specific pathogen responsible for the infection is not identified, making it difficult to select the most effective antibiotics. In these situations, broad-spectrum intravenous antibiotics are typically used initially, followed by tailored therapy based on clinical response and repeat cultures when available [3,4].
Surgical intervention remains the cornerstone of managing chronic osteomyelitis [2,5]. In this case, the patient’s treatment included sequestrectomy, which involves the removal of necrotic bone tissue (sequestrum) that provides a site for bacterial growth, thus preventing further infection. Adequate debridement is critical to eliminate infected and dead tissue, which can otherwise serve as a reservoir for bacteria. The use of local antibiotic carriers, such as stimulan, is an important adjunct in such cases [6-10]. These carriers allow for high local concentrations of antibiotics, providing more effective treatment directly at the site of infection while minimizing systemic toxicity. In addition, the prolonged use of oral antibiotics post-operatively is essential to control any residual infection and prevent relapse.
Advanced imaging and histopathological confirmation are essential, particularly in ambiguous or culture-negative cases. Techniques such as MRI and targeted tissue biopsies improve diagnostic accuracy [11]. The development of novel diagnostic modalities, including polymerase chain reaction-based methods and next-generation sequencing, has further enhanced our ability to identify causative organisms in difficult cases [4,12].
Overall, managing chronic osteomyelitis requires careful attention to surgical technique, antimicrobial therapy, and close follow-up to monitor for any signs of recurrent infection. The combination of these strategies can significantly improve clinical outcomes and reduce the risk of long-term complications such as bone deformities or loss of function [13].
Conclusion
Effective management of acute on chronic osteomyelitis requires a thorough and multidisciplinary approach, beginning with detailed clinical evaluation, imaging studies, and targeted laboratory investigations to assess the extent of infection. The use of local antibiotic carriers, such as calcium sulfate beads (stimulan), enhances localized drug delivery and supports infection control. Postoperative care, including immobilization and structured rehabilitation, is vital for optimal recovery. Early and aggressive treatment remains essential to prevent recurrence, chronic disability, and long-term complications.
Clinical Message.
This case highlights the importance of aggressive surgical debridement and local antibiotic therapy in the effective treatment of acute on chronic osteomyelitis. Even in culture-negative cases-where identifying the causative organism is challenging-timely surgical intervention combined with empirical broad-spectrum antibiotics can yield favourable outcomes.
Biography



Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004;364:369–79. doi: 10.1016/S0140-6736(04)16727-5. [DOI] [PubMed] [Google Scholar]
- 2.Calhoun JH, Manring MM. Adult osteomyelitis. Infect Dis Clin North Am. 2005;19:765–86. doi: 10.1016/j.idc.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Masters EA, Trombetta RP, de Mesy Bentley KL, Boyce BF, Gill AL, Gill SR, et al. Evolving concepts in bone infection:Redefining “biofilm”, “acute vs chronic osteomyelitis”, “the immune proteome”and “local antibiotic therapy”. Bone Res. 2019;7:20. doi: 10.1038/s41413-019-0061-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saeed K, McLaren AC, Schwarz EM. Diagnosing and managing chronic infection in orthopaedics:Practical implications of evolving techniques and technologies. J Bone Joint Surg Am. 2021;103:e57. [Google Scholar]
- 5.Llauger J, Palmer J, Amores S, Bagué S, Camins A. Osteomyelitis of the long bones:Radiologic diagnosis. Eur Radiol. 1998;8:1742–9. [Google Scholar]
- 6.Morgenstern M, Vallejo A, McNally MA, Moriarty TF, Ferguson JY. The effect of local antibiotic prophylaxis when using antibiotic-loaded biomaterials in orthopedic surgery:A review. Bone Joint Res. 2018;7:30111. doi: 10.1302/2046-3758.77.BJR-2018-0043.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferguson JY, Dudareva M, Riley ND, Stubbs D, Atkins BL, McNally MA. The use of a biodegradable antibiotic-loaded calcium sulphate carrier containing tobramycin for the treatment of chronic osteomyelitis:A series of 195 cases. Bone Joint J. 2014;96-B:829–36. doi: 10.1302/0301-620X.96B6.32756. [DOI] [PubMed] [Google Scholar]
- 8.Pande KC, Bandyopadhyay S, Ghosh S. Use of calcium sulfate beads as local antibiotic delivery system in chronic osteomyelitis:A prospective study. Indian J Orthop. 2013;47:591–6. [Google Scholar]
- 9.Qin L, Liu Y, Dang X, Wang K, Yang L. Efficacy of antibiotic-loaded calcium sulfate in the treatment of bone infections:A meta-analysis. BMC Musculoskelet Disord. 2021;22:449. [Google Scholar]
- 10.McNally MA, Ferguson JY, Lau AC, Diefenbeck M, Scarborough M, Ramsden AJ, et al. Single-stage treatment of chronic osteomyelitis with a new absorbable, gentamicin-loaded, calcium sulphate/hydroxyapatite biocomposite:A prospective series of 100 cases. Bone Joint J. 2016;98-B:1289–96. doi: 10.1302/0301-620X.98B9.38057. [DOI] [PubMed] [Google Scholar]
- 11.Kaim AH, Gross T, von Schulthess GK. Imaging of chronic posttraumatic osteomyelitis. Eur Radiol. 2002;12:1193–202. doi: 10.1007/s00330-001-1141-0. [DOI] [PubMed] [Google Scholar]
- 12.Thahir A, Lim JA, West C, Krkovic M. The use of calcium sulphate beads in the management of osteomyelitis of femur and tibia:A systematic review. Arch Bone Jt Surg. 2022;10:320–7. doi: 10.22038/ABJS.2021.53566.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mauffrey C, Herbert B, Young H, Wilson ML, Hake ME, Stahel PF. The role of biofilm on orthopaedic implants:The “Holy Grail”of post-traumatic infection management. Eur J Trauma Emerg Surg. 2016;42:411–23. doi: 10.1007/s00068-016-0694-1. [DOI] [PubMed] [Google Scholar]


