Abstract
Coronary artery bypass grafting (CABG) is an exceedingly rare procedure in pediatric cardiac surgery, primarily due to the low incidence of coronary artery disease in this population. However, when indicated, the use of the internal thoracic artery (ITA) as a graft is crucial for ensuring long-term success. This case report describes a patient with a coronary artery anomaly where the right coronary artery is taking its origin from the left main coronary artery and transversing along the right ventricle outflow tract. The patient experienced late coronary compression after Rastelli operation, highlighting the critical role of ITA grafts in the surgical treatment.
Introduction
Coronary artery complications in pediatric patients, especially post-congenital heart surgery, are uncommon but can have serious implications. This report discusses the case of a pediatric patient who developed severe coronary artery stenosis after congenital heart surgery and underwent CABG using the internal thoracic artery (ITA).
Case presentation
A 11-year-old female patient with a history of previous central shunt procedure between the ascending aorta and the right pulmonary artery in 2013, Rastelli procedure in 2018 presented with recurrent syncope and shortness of breath. Before the Rastelli procedure, diagnostic cardiac catheterization and angiography were performed. The central shunt was found to be functioning well, and it was observed that the right coronary artery (RCA) originated from the left coronary system without any stenosis (Fig. 1). In 2024, the patient presented with symptoms of dyspnea following exercise and syncope on exertion. Echocardiography revealed turbulent flow within the pulmonary conduit, particularly at the distal anastomosis site, with systolic gradients of 95–100 mmHg on Doppler imaging. Significant narrowing was observed at the bifurcation level and at the proximal right pulmonary artery. Preoperative coronary angiography revealed a long-segmental stenosis in the portion of the right coronary artery located beneath the pulmonary conduit. (Fig. 2). No significant elevation in cardiac enzyme levels was detected preoperatively and postoperative cardiac troponin levels remained within normal limits.
Fig. 1.
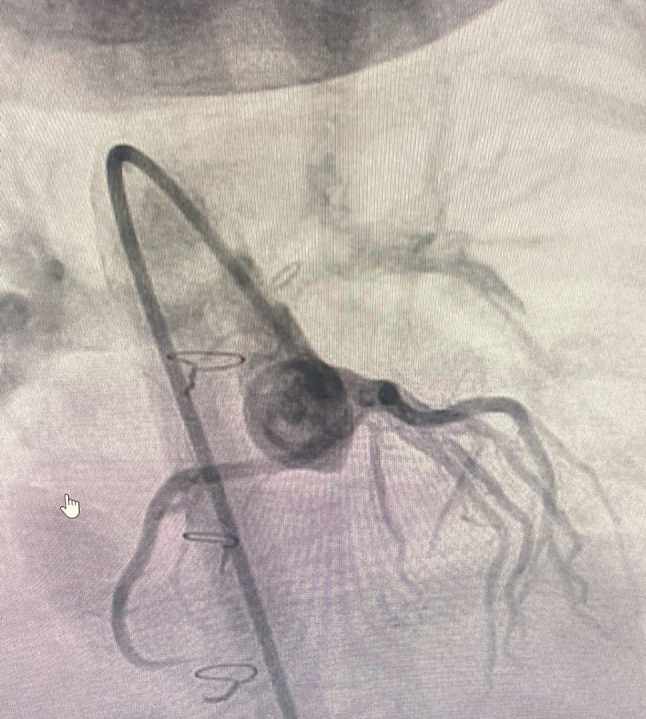
Right coronary artery (RCA) originated from the left coronary system without any stenosis
Fig. 2.
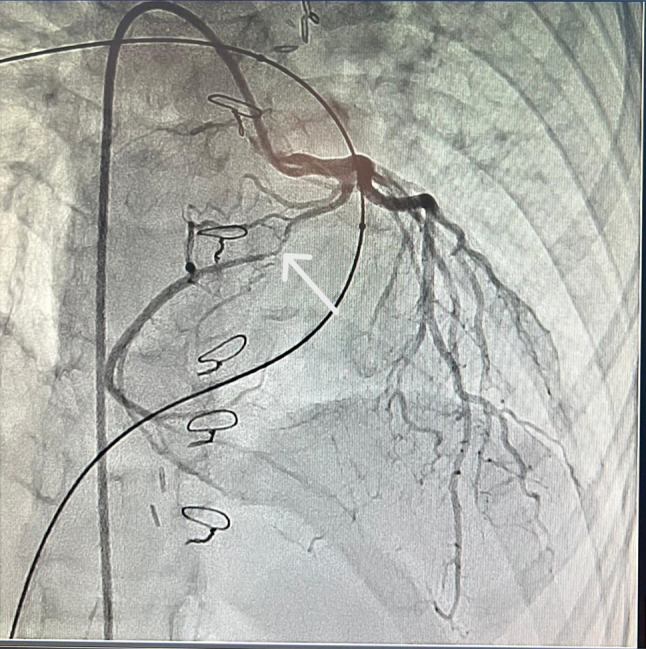
Stenotic RCA segment under the pulmonary graft
The patient, who was symptomatic due to pulmonary conduit stenosis and coronary artery compression, was taken for surgery. Following a median sternotomy, the right internal thoracic artery (RITA) was prepared as a graft for bypassing the RCA. Arterial cannulation from the ascending aorta and direct bicaval venous cannulation were performed, followed by initiation of cardiopulmonary bypass. Systemic hypothermia at 28 °C was achieved, and cardiac arrest was induced with antegrade Del Nido cardioplegia under cross-clamp. Subsequently, the pulmonary graft was excised via longitudinal incision. Due to the posterior part of the graft being adherent to surrounding tissues, it was left in place to avoid potential complications (Fig. 3). The pulmonary artery (PA) and right ventricular outflow tract (RVOT) were reconstructed with a hand-sewn trileaflet polytetrafluoroethylene (PTFE) pulmonary graft. (Fig. 4). The non diseased segment of RCA was inspected near the pulmonary conus (Fig. 5). The segment beyond the stenotic portion of the RCA was prepared for the RITA anastomosis. The RITA-in situ-RCA anastomosis was then performed (Fig. 6). After an uneventful surgery, the patient was transferred to the intensive care unit (ICU). Postoperative echocardiography revealed laminar flow in the pulmonary conduit and confluent main pulmonary arteries and branches. The patient was discharged on postoperative day 14 with surgical recovery and has not presented to the hospital for any reason except routine outpatient follow up since discharge.
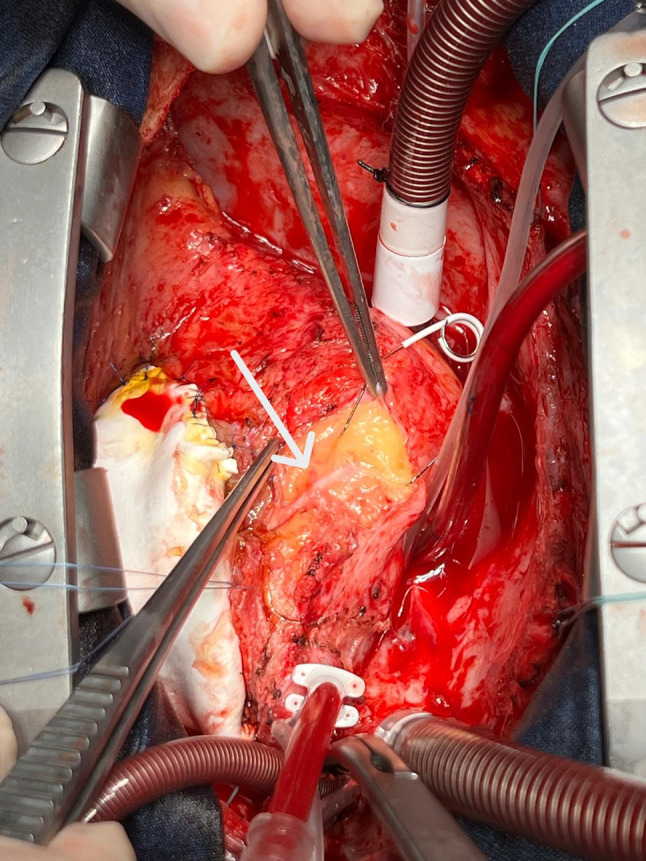
Fig. 3.
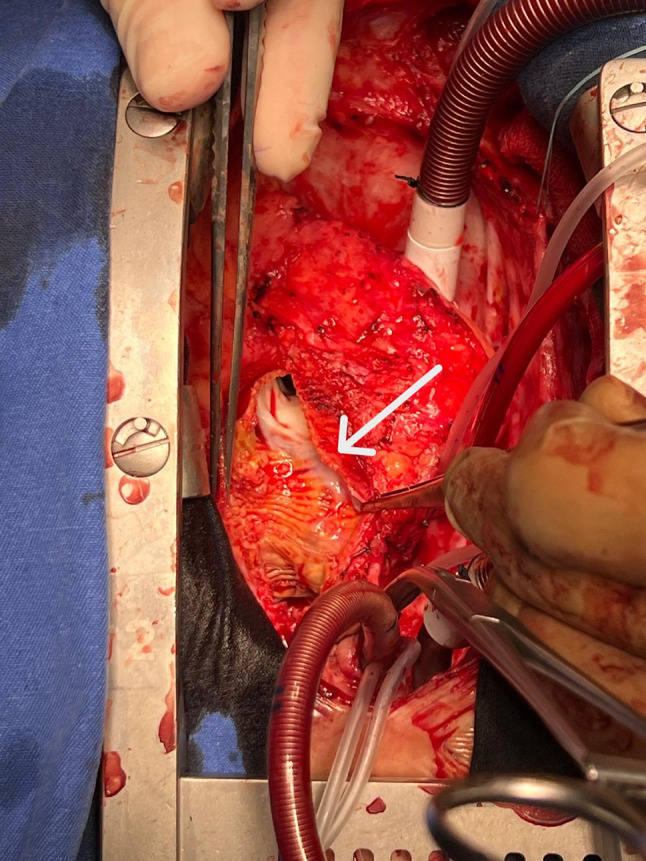
Posterior wall of the pulmonary graft after longitudinal incision
Fig. 4.
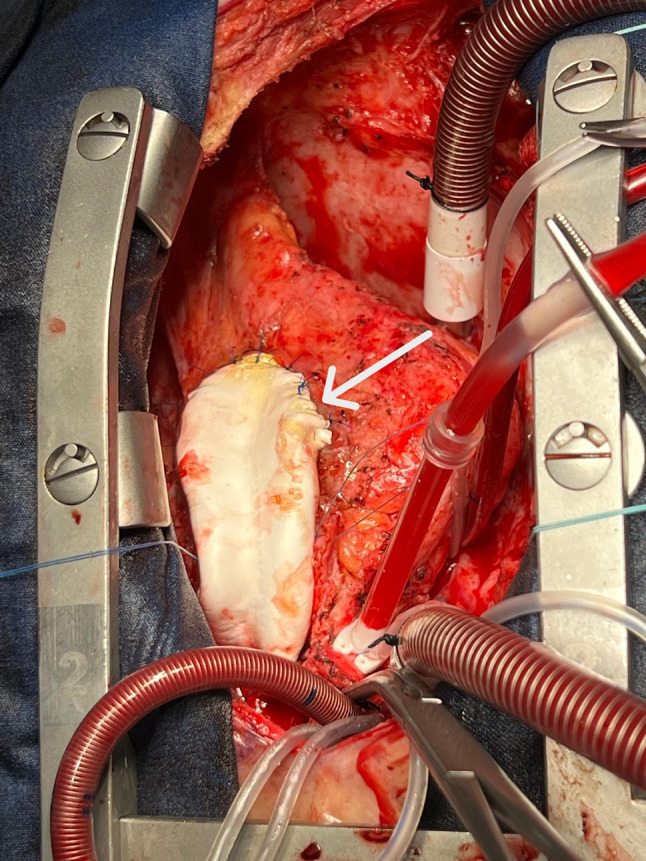
New trileaflet PTFE pulmonary conduit
Fig. 5.
The non diseased segment of RCA was inspected near the pulmonary conus
Fig. 6.

RITA-RCA coronary anastomosis
Discussion
Coronary artery complications in pediatric patients, especially post-congenital heart surgery, are rare and infrequent. In this case, the RCA’s compression led to critical stenosis, necessitating surgical intervention. The choice of graft material is crucial in pediatric CABG, as the long-term patency of the graft directly influences patient outcomes.
The internal thoracic artery (ITA) is favored in pediatric patients due to its superior long-term patency rates compared to venous grafts. Studies, including those by Kitamura et al. [1], have demonstrated that ITA grafts in pediatric patients yield excellent long-term results, reducing the likelihood of graft failure and subsequent morbidity. Similarly, Legendre et al. [2] reported on the outcomes of pediatric coronary artery bypass surgery, emphasizing the importance of ITA usage. Mavroudis et al. [3] also discussed the critical role of ITA in pediatric CABG, particularly in cases following the arterial switch procedure.
In this case, the patient had a coronary artery anomaly that caused severe RCA stenosis after initial surgery. Previous studies have shown that timely and proper surgical intervention is crucial in such situations [4]. Additionally, Vida et al. [5] reported on the results of pediatric coronary artery revascularization, highlighting the challenges and the need for careful follow-up in these cases.
This case underlines the importance of vigilant long-term follow-up in pediatric patients with coronary artery anomalies. Early identification and appropriate surgical intervention, particularly the use of ITA grafts, can significantly improve outcomes and prevent life-threatening complications.
Conclusion
CABG in pediatric patients is a rare but crucial intervention in cases of severe coronary artery stenosis. The use of the internal thoracic artery as a graft material is essential for ensuring long-term graft patency and patient survival. This case contributes to the limited body of literature on pediatric CABG, reinforcing the necessity of ITA grafts in these rare surgical procedures.
Author contributions
B.B. took responsibility for writing the main text. M.Ç. contributed to the design of the text by performing data screening. N.A.A. assisted in the editing and English translation of the manuscript, while also providing supervision and supporting the inclusion of images. F.Ö. contributed to the revision of the main text.O.Y contributed to the revision of the main text. All authors actively participated in the writing process.
Funding
This study was not funded.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kitamura S, Kawata T, Mori T, Sakakibara Y. Twenty-five-year outcome of pediatric coronary artery bypass surgery for Kawasaki disease. Circulation. 2009;120(1):60–8. 10.1161/CIRCULATIONAHA.108.840603. [DOI] [PubMed] [Google Scholar]
- 2.Legendre A, Losay J, Houyel L, Serraf A, Belli E, Planche C. Outcome of coronary artery bypass grafting performed in young children. J Thorac Cardiovasc Surg. 2010;139(2):349–53. 10.1016/j.jtcvs.2009.07.061. [DOI] [PubMed] [Google Scholar]
- 3.Mavroudis C, Backer CL, Duffy CE, Pahl E, Wax DF. Pediatric coronary artery bypass for Kawasaki congenital post-arterial switch and iatrogenic lesions. Ann Thorac Surg. 1999;68(2):506–12. 10.1016/S0003-4975(99)00588-3. [DOI] [PubMed] [Google Scholar]
- 4.Bacha EA, Quinones J, Kahana MD, Baron JM, Hijazi ZM. Embolic coronary occlusion after the arterial switch procedure. J Thorac Cardiovasc Surg. 2001;122(5):1028–30. 10.1067/mtc.2001.116465. [DOI] [PubMed] [Google Scholar]
- 5.Vida VL, Guzzetti L, Bottio T, Milanesi O, Padalino MA, Stellin G. Pediatric coronary artery revascularization: a European multicenter study. Ann Thorac Surg. 2013;96(3):898–903. 10.1016/j.athoracsur.2013.05.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.


