Abstract
Background
Adolescents living with HIV face unique challenges as they gain greater independence while transitioning into adulthood. They must adjust their self-management activities and take primary responsibility for their health, including adhering to medication regimens and attending clinic visits. These young individuals need to acquire knowledge about HIV and Antiretroviral treatment to manage their condition and improve their health outcomes effectively. This study aims to map existing interventions for adolescents with HIV, focusing on the types, content, and best practices that enhance their understanding of both HIV and Antiretroviral treatment.
Methods
The scoping review utilised a Joanna Briggs Institute (JBI) framework to map the relevant literature. We searched the CINAHL Complete, MEDLINE (via PubMed), ProQuest, Science Direct, and Scopus databases for studies published between January 1, 2000, and January 31, 2023. We selected studies using the inclusion criteria. Studies included health education programs as the intervention, which developed or implemented strategies to improve knowledge and skills related to HIV and self-management of antiretroviral treatment adherence among this population.
Results
Only five (5) studies met the eligibility criteria and were included in this review. Three (3) broad categories emerged from the analysis of the scoping review: the nature of interventions available for Adolescents living with HIV, the content of existing interventions, and best practices. The findings revealed limited evidence of programs aimed at adolescents in various settings. Most notable was the paucity of evidence on programs targeting Adolescents living with HIV, especially those that are designed to help them learn about their condition and associated treatment.
Conclusion
The review highlights the existence of limited evidence-based, context-specific, and consumer-tailored educational interventions for Adolescents living with HIV. More comprehensive, age-appropriate and personalised interventions are needed for adolescent self-management of HIV as a chronic health condition.
Keywords: Adolescents, Antiretroviral treatment, Human Immunodeficiency Virus, Health intervention, Programs, Scoping review
What is Already Known.
Antiretroviral therapy is vital for managing HIV in adolescents and youth, but barriers like stigma, limited knowledge, and lack of support hinder adherence.
Targeted interventions that address these challenges are needed, and more research is required to identify effective strategies for engaging in Antiretroviral programs.
What This Study Adds
This study reveals a significant lack of targeted educational interventions for Adolescents living with HIV.
Many adolescents lack access to resources tailored to their unique needs, which are vital for their well-being and clinical outcomes.
Our findings highlight the potential of interventions and best practices to improve knowledge of HIV, enhance antiretroviral treatment adherence, and promote effective disease management.
Alt-text: Unlabelled box
1. Introduction
Adolescence is a complex transitional stage characterised by significant physical, emotional, cognitive, and social changes that can significantly influence behaviour (Newman & Newman, 2017). During this period, adolescents often seek greater autonomy while establishing strong peer relationships and a distinct teenage culture. They may assert adult rights but frequently struggle to recognise and accept the accompanying responsibilities (Dow et al., 2020). Consequently, this desire for independence can lead to engagement in risky behaviours such as early sexual activity, substance abuse, and peer pressure, resulting in greater vulnerability to adverse health outcomes (Shayo & Kalomo, 2019).
The World Health Organization has recognised adolescents as a particularly vulnerable population, noting their limited capacity to advocate for themselves and access necessary care. This vulnerability necessitates special attention from healthcare providers. Adolescents' access to timely healthcare services can be hindered by various circumstances beyond their control (World Health Organization, 2016). Current statistics highlight this issue, with approximately 1.7 million adolescents living with HIV globally; 1.1 million (or 65%) of these cases are located in eastern and southern Africa. Alarmingly, in 2022, this region recorded about 77,000 new HIV infections among adolescents, accounting for more than half (55%) of global new infections in this age group (UNAIDS., 2023).
Adolescents living with HIV face numerous psychosocial challenges that complicate their ability to adhere to antiretroviral treatment, achieve viral suppression, and remain engaged in healthcare services (Agathis et al., 2021). For instance, in Eswatini, these individuals often lack family and community support and experience fear of stigma and discrimination. This fear frequently drives them to conceal their HIV status from family, friends, and peers (Nsibandze et al., 2021). Adolescents have voiced the need for a more effective healthcare system responsive to their unique challenges (Munyayi & Van Wyk, 2020). Research indicates that empowering these individuals with knowledge and skills to manage their health can significantly improve their overall well-being as they transition into adulthood (Chory et al., 2021; Laurenzi et al., 2021).
In response to these needs, various interventions have been implemented within clinical settings, one of which is the Teen Club. However, many of these interventions have struggled to engage adolescents effectively. A significant concern with the Teen Club has been the inconsistency in its activities, which diminishes its appeal. Additionally, the intervention's narrow focus has limited its ability to address the diverse needs of older adolescents. The voluntary nature of the club has further impacted participation, as many young people face competing priorities that hinder consistent involvement (Munyayi & Van Wyk, 2020).
Supporting evidence underscores the significance of health information and education in disease management, with a Zambian study finding these approaches acceptable and essential (St Clair-Sullivan et al., 2019). Furthermore, interventions aimed at supporting adolescents living with HIV can enhance self-worth, self-confidence, self-esteem, and overall quality of life (Willis et al., 2019). This review seeks to explore the various interventions available for adolescents living with HIV that enhance their knowledge and skills related to HIV and self-management of antiretroviral treatment adherence, identifying best practices for compelling content and delivery.
1.1. Scoping review process
The following questions guided the review:
-
1.
What evidence is available on health interventions for adolescents living with HIV?
-
2.
What are the content and best practices reported in the literature on interventions for Adolescents living with HIV?
2. Methods
This scoping review was guided by the Joanna Briggs Institute Model (2015), which is based on a specified research question, identifying the studies, selecting them, analysing the data, and summarising and reporting (Tricco et al., 2018; Peters et al., 2021).
2.1. Inclusion criteria
2.1.1. Participants
This review included adolescents living with HIV (aged 10-19 years as defined by the World Health Organization) and receiving Antiretroviral treatment in a healthcare facility. Studies with at least 50% of the participants aged 10-19 years or those with the reported mean or median age between 10-19 years or containing key search terms were also included. Only studies published between 2000 and 2023 were included.
2.1.2. Concept
The core concept in this review is health educational intervention as the phenomenon of interest. We considered studies that developed or implemented interventions to improve knowledge and skills related to HIV and self-management of antiretroviral treatment adherence among adolescents living with HIV.
2.1.3. Context
The context in this study was healthcare facilities, which refers to clinics, health centres, or hospitals for this review. Therefore, studies targeting schools, general community-based, or multi-purpose centres were not considered.
2.1.4. Type of studies
This review considered various study designs for inclusion, specifically randomised controlled trials, quantitative studies, and mixed-method studies that aimed to enhance knowledge and skills related to HIV and self-management of antiretroviral treatment adherence. Studies published in languages other than English or those without a full-text version were excluded due to practical constraints, such as cost and time considerations. The review did not include any reviews, conference abstracts, book chapters, protocols, guidelines, editorial letters, or commentaries. Furthermore, studies that focused solely on a single aspect of self-management, such as mental health, sexual and reproductive health, peer support, or counselling, were also excluded.
2.2. Search strategy
The researcher (NM) searched for empirical studies published in English through journals, databases, and a search of grey literature. The initial search was conducted on February 25, 2021, and updated on January 31, 2023. The choice of the database was based on its likelihood of containing articles relevant to the subject of interest. We utilised the University of Witwatersrand, Faculty of Health Sciences electronic databases to conduct the search, including CINAHL Complete, MEDLINE (via PubMed), ProQuest, Science Direct, Scopus, and the Google Scholar search engine. We employed a three-step search strategy using the JBI approach. In step one, did a limited initial search on PubMed and MEDLINE using the identified key terms: adolescent or youth, (antiretroviral therapy or antiretroviral treatment), (health programs or health educational program) OR (health educational intervention or health intervention), Human Immunodeficiency Virus or HIV. We then analysed the word text in the titles and abstracts of relevant studies and the index terms that described the studies.
All the identified keywords and index terms were used in the second step, and we undertook a search across all databases. The terms were adapted for each included information source. Thirdly, we screened the reference list of all included studies to identify any additional relevant studies. A complete search strategy for PubMed is included (Supplement 1). The researcher (NM) worked with the university's health sciences librarian to refine the search and ensure we captured crucial articles. This process was beneficial in defining some of the complex key terms such as "adolescent", which, in some studies, are referred to as "young adults" or "youth".
Medical Subject Headings (MeSH) terms were modified for different databases used. Then, the search combination or string for each database was finalised. For example, in PubMed, the following search string resulted: (adolescents or youth) AND (Antiretroviral therapy or antiretroviral treatment) AND (health programs or health education program or health educational intervention or health intervention) AND (Human Immunodeficiency Virus or HIV). We used truncations and Boolean operators "or" and "AND" in combination with singular terms. Finally, we documented and saved the outcome of each database search.
2.3. Selection of Studies
We consolidated the results of the searches conducted on all databases and manually removed duplicates. We retrieved the titles, abstracts, and citation information. We then reviewed the titles to determine eligibility based on the inclusion and exclusion criteria. At this stage, the researcher (NM) eliminated articles with uncertainty about the title. Secondly, the abstracts were screened using the eligibility criteria. The researcher (NM) and (SS) agreed on the inclusion criteria before the search.
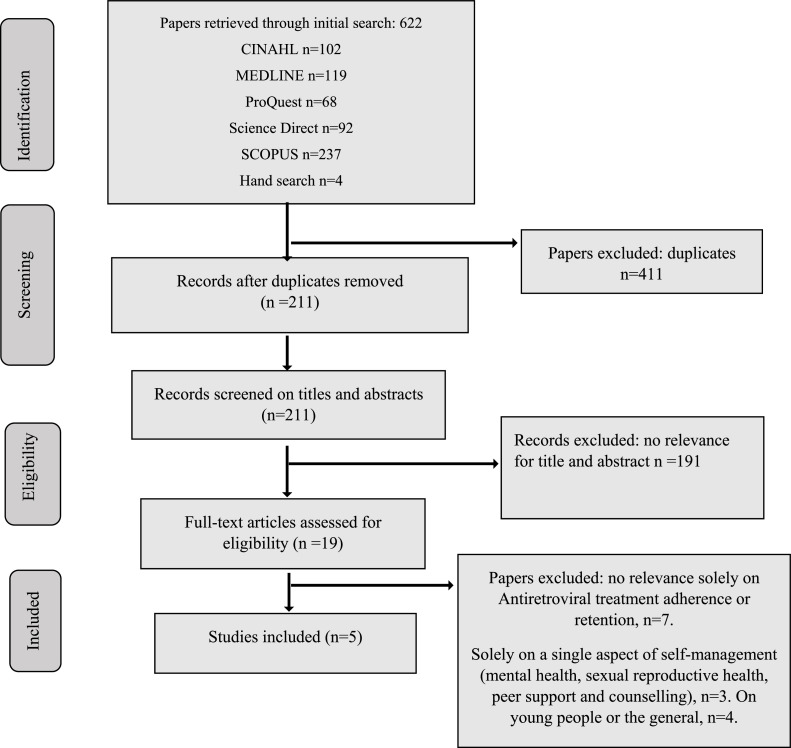
We retrieved full articles from each database and imported them into Mendeley's reference management software for the studies that fulfilled the eligibility criteria. The researchers (NM and SS) agreed upon the included studies. We resolved any disagreements through discussion and reached a consensus. The results are reported in a full report and presented in a PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) flow chart (Moher et al., 2009).
2.4. Data Extraction
Information was extracted from all studies that met the eligibility criteria using the data extraction sheet (Supplement 2), which we adopted from the Joanna Briggs Institute (Tricco et al., 2018; Peters et al., 2021). The researcher (NM) independently extracted data from the five studies: author and year of publication, country of origin, journal information, study objective, research design, study population, sample size, data analysis, outcome, and main findings related to the review questions. In collaboration with SS and NK research team members, we determined that the extracted data were relevant to the research questions and purpose. We extracted the data and entered it into a Microsoft Excel sheet. The charting process was iterative as the researcher (NM) continually updated the charting spreadsheet to fit the extracted study data. We employed content analysis to categorise and subcategorise the data.
3. Ethical consideration
The study was approved by the Ethics Committee in Human Research at the University of Witwatersrand (Ethics Clearance number M191118).
4. Results
4.1. Presentation of the Data
The scoping review focused on the nature and content of interventions available to enhance knowledge and skills related to HIV and self-management of antiretroviral treatment adherence for Adolescents living with HIV. The analysis of the collected data yielded insights into the existing body of research on the subject matter. The search of all databases yielded 618 citations. We conducted a hand search through the reference lists of relevant studies and identified four articles. After removing duplicates, we excluded 411 articles, and 211 articles underwent screening on titles and abstracts. Studies excluded at this point were either non-adolescent studies or did not target adolescents living with HIV. We performed a full-text screening of the remaining 19 studies, and five studies were deemed suitable for inclusion in this review. The remaining 14 studies did not meet the eligibility criteria, as most (n = 7) focused only on Antiretroviral treatment adherence or retention. Others (n=3) focused primarily on a single aspect, such as mental health, sexual reproductive health, peer support and counselling. Similarly, other studies (n=4) mainly aimed at young people or the general population of adolescents and not particularly those living with HIV. The excluded studies are shown in Table 1 below.
Table 1.
Studies excluded following full-text review (n = 14).
| Authors | Reasons for exclusion |
|---|---|
| Dulli, L., Ridgeway, K., Packer, C., Plourde, K.F., Mumuni, T., Idaboh, T., Olumide, A., Ojengbede, O. & McCarraher, D.R. JMIR Public Health and Surveillance Journal, 2018, 4(4) e12397 |
The study focused solely on Antiretroviral treatment adherence and retention. |
| Kourrouski, M.F.C. & Lima, R.A.G.D. Revista Latino-Americana de Enfermagem, 2009. 17 947-952 | The study focused solely on Antiretroviral treatment. |
| Belzer, M.E., MacDonell, K.K., Ghosh, S., Naar, S., McAvoy-Banerjea, J., Gurung, S., Cain, D., Fan, CA & Parsons, J.T. JMIR Research Protocols. 2018, 7(12) 11183 |
The study focused solely on Antiretroviral adherence. |
| Bhana, A., Mellins, C.A., Petersen, I., Alicea, S., Myeza, N., Holst, H., Abrams, E., John, S. Chhagan, M., Nestadt, D.F. & Leu, C.S. AIDS Care Journal. 2014, 26(1) 1-11 |
The study focused on adolescent mental health. |
| Bhana, A., McKay, M.M., Mellins, C., Petersen, I. & Bell, C. Journal of the International AIDS Society. 2010, 13 S8-S8 |
Study focused on adolescent HIV prevention . |
| Kuo, C., Atujuna, M., Mathews, C., Stein, D.J., Hoare, J., Beardslee, W., Operario, D., Cluver, L. & K. Brown, L. AIDS Care Journal. 2016. 28 supl 106-110 |
Study focused on the general adolescent population (not Adolescents living with HIV only) |
| Ridgeway, K., Dulli, L.S., Murray, K.R., Silverstein, H., Dal Santo, L., Olsen, P., Darrow de Mora, D. & McCarraher, D.R. PloS one. 2018, 13(1) e0189770 |
Study focused on Antiretroviral treatment adherence only . |
| Widman, L., Kamke, K., Evans, R., StewAntiretroviral, J.L., Choukas-Bradley, S. & Golin, C.E. The Journal of Sex Research. 2020, 57(2) 145-154. | The program was a sexual reproductive health intervention. |
| Whiteley, L., Brown, L., Lally, M., Heck, N. & van den Berg, J.J. JMIR mHealth and uHealth Journal. 2018 6(4) e8155 | The participants' mean age was above 1019 years. Mean age of participants was 22 years. |
| Sayegh, C.S., MacDonell, K.K., Clark, L.F., Dowshen, N.L., Naar, S., Olson-Kennedy, J., van den Berg, J.J., Xu, J. & Belzer, M. AIDS and Behavior. 2018 22(10) 3357-3362 | The study focused on Antiretroviral treatment adherence. |
| Abrams, E.A., Burke, V.M., Merrill, K.G., Frimpong, C., Miti, S., Mwansa, J.K. & Denison, J.A.PloS ONE. 2021 16(6) e0252349 |
The study focused on Antiretroviral treatment adherence |
| Chory, A., Callen, G., Nyandiko, W., Njoroge, T., Ashimosi, C., Aluoch, J., Scanlon, M., McAteer, C., Apondi, E. & Vreeman, R.AIDS and Behavior, 2022, 26(1) 232-242 |
The study focused on adolescent counselling and peer support. |
| DeSilva, M., Vu, C.N., Bonawitz, R., Hai, L.T., Van Lam, N., Yen, L.T., Gifford, A.L., Haberer, J., Linh, D.T. & Sabin, L. BioMedical Central Trial Journal. 2019. 20(1) 1-13 |
The study focused solely on Antiretroviral treatment adherence. |
| Mahat, G., Scoloveno, M.A. & Ayres, C. Journal of Cultural Diversity. 2014, 21(4) 152-158 | General adolescent population (not Adolescents living with HIV only). |
Figure 1 shows the steps undertaken in searching and selecting studies included in the review. We did not do critical or quality appraisal of the included studies as this was beyond the scope of the scoping reviews. The method is consistent with prior scoping reviews by Tricco et al. (2018) and the guidelines of JBI (Peters et al., 2021).
Fig 1.
Flow diagram of the search strategy and selection process for the included studies according to the PRISMA extension for Scoping Reviews.
4.2. Search and selection of studies
4.2.1. Characteristics of the studies
The review analysed quantitative and mixed-method studies to summarise the nature and content of educational interventions available for adolescents living with HIV. This section only presents the extracted information about the research questions the review should answer. Out of the 19 studies reviewed in full, only five (5) met the eligibility criteria and were included in this review. The results are presented with the study descriptors and the review question. Table 2. summarises the characteristics of the (n=5) included studies.
Table 2.
Summary characteristics of included studies.
| Citation details (Author/year | Country / Context / setting | Intervention and content | Study question/ study objective | Study design/ research design | Participants/ population/ sample size | Data analysis | Results / Findings |
|---|---|---|---|---|---|---|---|
| Fongkaew et al., 2017 | Chiang Mai, Thailand. | Intervention: Collaborative Multidisciplinary HIV Program for Youth Content: Promoting antiretroviral treatment adherence, condom use, and sexual self-efficacy. |
This study aimed to describe the development of a pilot test intervention for enhancing HIV treatment and risk reduction and to evaluate the feasibility of the intervention implementation |
Mixed-method research using both individual interviews, focus group discussions and questionnaires to collect data |
It included 45 participants (25 youths living with HIV, 18 caregivers and 12 healthcare providers) in a community hospital | Descriptive and inferential statistics using SPSS; Qualitative results were analysed with thematic analysis |
Findings provided preliminary evidence of the intervention's practicality in a clinical context in a community hospital The study provides supportive evidence that the information, motivation-behaviour model and method could be used to change behaviours among youths living with HIV |
| Shegog et al., 2012 | Southern metropolitan hospital, United States of America |
Intervention: Click (Web-Based Adherence Intervention) Content: Promoting activities that address attitudes, knowledge, skills, and self-efficacy related to antiretroviral treatment adherence. |
The purpose of the article was to pilot test the web-based Antiretroviral treatment adherence module, a tailored web-based application designed to enhance Antiretroviral treatment adherence among youths living with HIV |
Quantitative study using a single-group pre/post-test design | Ten (10) vertically HIV infected youths from a hospital-based HIV pediatric clinic | Descriptive and inferential statistic using SPSS |
The intervention demonstrated a significant improvement in knowledge about HIV and Antiretroviral treatment adherence and potential benefits of computer-based technology in a clinical setting to improve understanding of HIV and Antiretroviral treatment among participants, which will help facilitate dialogue with healthcare providers. The study concluded that ART adherence among youths living with HIV may be enhanced by providing systematic and confidential education |
| Hosek et al., 2018 | (Bronx, Chicago, Memphis and Miami) United States of America. |
Intervention: Adolescents Coping, Connecting, Empowering, and Protecting Together Content: Teaching an overview of HIV, HIV disclosure, healthy living, stress management, relaxation techniques, and promoting spirituality, sexuality, self-esteem, advocacy, and future planning. |
The study aimed to evaluate a new intervention for adolescents and young adults that was designed to improve psychosocial adjustment to an HIV diagnosis | It was a sequential mixed method design using both quantitative (pre- and post-test questionnaire) and qualitative (individual interviews and focused group discussion) methods |
The population was adolescents diagnosed with HIV. It had a sample size of 50 participants and was conducted at four selected sites of Adolescent Medicine Trials Network |
Descriptive and inferential statistics for quantitative data Thematic analysis for qualitative data |
Both participants and interventionists demonstrated high levels of satisfaction with the intervention and a high level of participation, suggesting good feasibility and acceptability. Data from this study also indicated improvement in peer and formal social support immediately after the intervention and an improved level of HIV knowledge, which was sustained over time. |
| Rogers et al., 2001 | Clinical sites for Adolescent Medicine HIV/AIDS Research Network in United States of America |
Intervention: Therapeutic Regimens Enhancing Adherence in Teens Content: Promoting HIV treatment adherence, peer connection, and self-efficacy. |
The purpose of this study was to produce and implement a theory-based clinical intervention to promote adherence to highly active antiretroviral therapy among youths infected with HIV. |
A quantitative, quasi-experimental design with a multifaceted intervention was used |
The study included 64 youths living with HIV and was conducted at clinical sites for Adolescent Medicine HIV/AIDS Research Network in the United States of America |
Descriptive and inferential statistics | This intervention employed multiple one-on-one sessions with materials specifically developed for delivery outside of routine clinical care. The lower completion rate precluded the ultimate assessment of the intervention's effectiveness in promoting long-term adherence to Antiretroviral treatment. The results reflected the prospects of the usefulness of the staging tool in the identification of Antiretroviral treatment initiation readiness Findings also suggest that clinical staff's adoption of an intervention may influence its success. |
| Nestadt et al., 2019 | Thailand | Intervention: Collaborative HIV Prevention and Adolescent Mental Health Content: Teaching HIV treatment, stress management, and promoting self-esteem enhancement and advocacy. |
The intervention aimed to evaluate short- and long-term impact on behavioural, health and psychosocial factors of adolescents, as well as determine the acceptability and feasibility of the intervention in a Thai context | Quantitative designs with pre-and post-test measures | The study included 88 adolescents who were recruited at four selected HIV clinics in Thailand | Descriptive and inferential statistics using STATA |
The intervention adopted a Collaborative HIV Prevention and Adolescent Mental Health Program model cartoon based on the South African curriculum, which was modified to their setting as Collaborative HIV Prevention and Adolescent Mental Health Program+ It consisted of 11 sessions, delivered over 6 months, one weekend per month, utilising a structured facilitator's manual. Results showed that the intervention was feasible, with 89% attendance of all sessions, improved HIV knowledge, medication-taking behaviours, communication, and social support among participants. |
4.2.2. Study location
In terms of the geographic distribution of the included studies, two (2) were from Thailand (Fongkaew et al., 2017; and Nestadt et al., 2029), three (3) studies were from the USA (Shegog et al., 2012; Hosek et al., 2018; Rogers et al., 2001).
4.3. The focus of the studies
All five included studies focused on adolescents living with HIV in different contexts and settings. For example, the study by Fongkaew et al. (2017) described developing a pilot test program for enhancing HIV treatment and risk reduction. One study aimed to pilot-test the Click web-based antiretroviral treatment adherence module, a tailored web-based application designed to enhance Antiretroviral adherence among youths living with HIV (Shegog et al., 2012). The study by Hosek et al. (2018) focused on evaluating a new intervention for adolescents and young adults designed to improve psychosocial adjustment to an HIV diagnosis. In their study, Rogers and colleagues (2001) aimed to design and implement a theory-based clinical intervention to promote adherence to highly active antiretroviral therapy among HIV-infected youth. The other program from the review results identified was the Collaborative Multidisciplinary HIV Program for Youth Intervention (Nestadt et al., 2019), which was developed for Adolescents living with HIV to improve treatment adherence and psychosocial and mental health challenges among this population.
4.4. Research design
Three (3) studies were quantitative, using quasi-experimental designs with a pre and post-test (Nestadt et al., 2019; Shegog et al., 2012; Rogers et al., 2001). The other two (2) were mixed-method studies using interviews or focused group discussions and questionnaires as data collection methods (Fongkaew et al., 2017; Hosek et al., 2018). Quantitative studies used random and convenience sampling. Mixed method studies used either random, purposive or convenience sampling.
4.5. Study population
Participants that were included in these studies were described as "adolescents," "young adults," or "youth." They have acquired HIV infection either vertically or horizontally. Their age ranged from 10-22 years, with a mean and median of 13-18 years across the studies. All studies featured adolescents as the primary participants, although three included healthcare workers, parents, or caregivers as additional key informants (Hodgson et al., 2012; Fongkaew et al., 2017; Nestadt et al., 2019). The sample size ranged from 10 to 88, with most studies (n = 4; 80%) citing more female participants than male participants, while one study reported an equal number of male and female participants (Nestadt et al., 2019).
4.6. Context
Participants were recruited from various settings, including a hospital-based pediatric clinic (Shegog et al., 2012), hospitals (Fongkaew et al., 2017; Nestadt et al., 2019), and health centres (Rogers et al., 2001; Hosek et al., 2018). Conducting recruitment in these familiar environments helps enhance participants' comfort and engagement with the interventions. Individuals in known surroundings are often more receptive to improving their health and accessing available resources and support (Fongkaew et al., 2017). Recruitment efforts took place during regular clinic hours, facilitated by personnel from the facility who personally invited potential participants. Additionally, flyers were posted within the locations to increase awareness (Shegog et al., 2012; Fongkaew et al., 2017; Nestadt et al., 2019). However, the limited timeframe for recruitment may hinder participants' quality engagement, and socioeconomic factors can further impact the overall effectiveness of the interventions. Ultimately, the environment in which recruitment occurs plays a significant role in shaping participants' experiences and outcomes (Bonisteel et al., 2021).
4.7. Outcome information
Among the reviewed studies, two focused on antiretroviral treatment knowledge and adherence as outcomes, while the other two examined knowledge of HIV, Antiretroviral Treatment adherence, and self-regulation as outcomes. Only one study assessed knowledge of HIV and Antiretroviral treatment self-management as an outcome measure. Of the interventions delivered in a group setting, participants had no concerns about participating in group discussions or activities because they already knew each other and interacted with each other frequently in other group activities (Nestadt et al., 2019).
4.8. The categories arising from the data
Generally, scoping review data is extracted and analysed based on the purpose of the review and dependent on the researcher's judgment. Although descriptive qualitative techniques and coding data into categories or themes may be helpful in some scoping reviews, this method is not within their remit (Peters et al., 2021). Therefore, it was deemed necessary in the current review to analyse the data using the content analysis method. Three broad categories emerged from this scoping review analysis: the nature of interventions available for adolescents living with HIV, the content of existing interventions, and best practices. These categories are discussed below.
4.9. Nature of interventions available for adolescents living with HIV
The review identified five studies on the interventions for Adolescents living with HIV that met the inclusion criteria. All the interventions were informed by preliminary data from studies with the stakeholders (adolescents/ youths, health care workers, and parents). Two of the studies used the Social Cognitive Theory model as a framework (Shegog et al., 2012; Hosek et al., 2018), while the other two programs utilised the Social Learning Theory, Information Motivation Behaviour model and Stages of Change model, respectively (Nestadt et al., 2019; Fongkaew et al., 2017; Rogers et al., 2001). A study in the United States of America by Rogers et al. (2001) developed and implemented a theory-based, adolescent-focused intervention called Therapeutic Regimens Enhancing Adherence in Teens. It was implemented in 64 participants to promote adherence among youths living with HIV over six to eight weeks with five group sessions. This intervention involved multiple one-on-one sessions outside of routine clinical care, which resulted in a lower completion rate. The additional time commitment required outside regular clinic visits posed a challenge for consistent attendance and retention.
In another American study by Shegog and colleagues (2012), they designed a web-based application intervention called the Click web-based intervention to enhance knowledge on Antiretroviral treatment adherence among youths living with HIV aged 13-24 years. Two theories were used to frame this study: Belief Motivation Enhancement Theory and Social Cognitive Theory. Ten (10) adolescents in the World Health Organization who acquired HIV through vertical transmission participated in this study, with tailored activities to address knowledge, skills, attitudes, and self-efficacy related to Antiretroviral adherence. The participants completed a pre-test before the intervention participation and an immediate post-test at the end (Shegog et al., 2012).
One intervention identified was the Adolescents Coping, Connecting, Empowering, and Protecting Together intervention. This intervention was a behavioural intervention developed for youths newly diagnosed with HIV to understand HIV and improve psychological adjustment to an HIV diagnosis, and piloted on 50 participants, aged 16-24 years, at four selected sites in the United States of America. Potential participants received information about the study during regular clinic visits and by telephone if they were willing to participate. It consisted of 12 sessions, which comprised a combination of two individual and nine group sessions, with a duration of two hours for each session. They completed a pre-test before the post-test immediately after the last individual session and a final post-test at three months (Hosek et al., 2018).
Lastly, in Thailand, Fongkaew et al. (2017) developed a program called Collaborative Multidisciplinary HIV Program for Youth to enhance youths' HIV treatment adherence, knowledge level, and risk reduction. Nine (9) youths participated. The basis for this intervention was the information-motivation-behaviour model, comprised of 14 training sessions with youths living with HIV delivered over two days. Participants completed a pre-test and a post-test 12 weeks after completing the intervention.
4.10. Content of existing interventions and best practices
The Adolescents Coping, Connecting, Empowering, and Protecting Together intervention was developed in the United States of America and is grounded in the disability-stress coping model. It incorporates skills-building activities guided by Social Cognitive Theory. The intervention combines individual and group sessions, providing personalised attention alongside group support. Participants reported high satisfaction and engagement levels, indicating that this mixed delivery mode effectively maintained their involvement. The sessions included digital recordings, which were used for feedback purposes for peer facilitators. Various techniques, including group discussions, role-playing, and creative skills-building activities, were employed to foster a deeper understanding and engagement. The use of digital recordings not only facilitated facilitator learning but also improved educational outcomes for participants.
Participants were grouped by biological sex into male and female categories. The intervention covered a comprehensive range of topics, including an overview of HIV, HIV disclosure, healthy living, stress management, relaxation techniques, spirituality, sexuality, self-esteem, advocacy, and future planning (Hosek et al., 2018)—the diverse content equipped participants with essential knowledge for living with HIV and promoting healthier lifestyles. The Adolescents Coping, Connecting, Empowering, and Protecting Together intervention successfully blended individual attention and group support, significantly enhancing participants' understanding and engagement.
The Therapeutic Regimens Enhancing Adherence in Teens intervention was designed for treatment-naïve HIV-infected youths, based on the Stage of Change Model. The study was conducted over six to eight weeks and involved one-on-one sessions outside standard clinical care, utilising tailored materials such as guidance manuals, audio tapes, and informational booklets. Participants learned about HIV, addressed concerns about starting therapy, and connected with experienced peers on treatment. This environment encouraged them to reassess their health behaviours, reinforce learned skills, and enhance self-efficacy, empowering them to take control of their health.
A key component was the preparation phase, where participants used surrogate pills for one to two weeks, documenting their experiences to gain insights into adherence. The intervention also provided strategies to overcome noncompliance and to build long-term adherence habits. For those facing challenges, additional support reinforced their commitment to treatment. Therapeutic Regimens Enhancing Adherence in Teens intervention focused on self-efficacy and skill-building, offering personalised experiences that strengthened participants' dedication to managing their health and treatment.
The Collaborative Multidisciplinary HIV Program for Youth intervention was conducted over two days at a training camp and utilised a participatory approach called "edutainment." This method incorporated various practical activities, including group discussions, case studies, role-playing, games, and video clips. The intervention focused on six key elements to enhance participants' problem-solving skills through brainstorming and experience sharing. Before the intervention, participants completed questionnaires to establish baseline data regarding their adherence to antiretroviral treatment, sexual self-efficacy, and attitudes toward condom use. Follow-up assessments were conducted 12 weeks after the intervention to evaluate its impact. Additionally, participants took part in individual interviews and focus group discussions to gauge the effectiveness and appropriateness of the program (Fongkaew et al., 2017).
The edutainment approach engaged participants by integrating interactive elements like role-playing and case studies. By promoting problem-solving skills and sharing experiences, the program provided valuable education on the practical aspects of antiretroviral treatment adherence and sexual self-efficacy. The information gathered from baseline and follow-up questionnaires offered important insights into health education outcomes, allowing for an assessment of the knowledge gained over time.
The Click web-based intervention utilised an electronic application that provided participants with interactive activities, animations, and videos featuring peers and experts. Each participant accessed the application using a unique identifier and entered important information, including demographic data, current adherence levels, barriers to adherence, and self-reported recent viral load and CD4 counts. The application offered tailored functions and activities based on the data provided, which included individual risk profiles—like missed doses and blood results for viral load and CD4 counts—as well as psychosocial factors and self-efficacy regarding adherence. The intervention content focused on educating participants about HIV, the importance of adhering to antiretroviral treatment, and strategies to overcome various adherence barriers (Shegog et al., 2012).
The intervention's digital format facilitated confidential and systematic education, which participants positively received. The platform's convenience and accessibility likely contributed to improved retention rates. This innovative approach to health education allowed participants to engage with the material interactively, enhancing their understanding of their health challenges and the critical nature of adherence. Additionally, the ability to track personal adherence and identify barriers encouraged active participation and deeper engagement with the content.
The Thai Collaborative Multidisciplinary HIV Program for Youth intervention effectively promoted health education through a structured curriculum tailored to the local context, enabling adolescents to grasp critical health issues, particularly those related to HIV. Adapting the South African Collaborative Multidisciplinary HIV Program for Youth intervention model ensured the program's relevance and engagement for Thai youth. Throughout 11 sessions delivered over six months, participants gained valuable knowledge about HIV prevention, healthy behaviours, and the psychosocial factors influencing their lives. The face-to-face format facilitated interactive discussions, allowing participants to address misconceptions surrounding various Health topics.
A facilitator manual was provided to support the program's implementation, equipping existing health facility staff to guide the sessions effectively. This approach fostered a supportive learning environment. Furthermore, by evaluating the intervention's acceptability and feasibility, the program aimed to influence individual behaviours and contribute to broader community health education initiatives. This groundwork is vital for promoting sustainable behavioural change among adolescents.
Overall, the best practices identified from these interventions included using tailored support materials, skills-building activities, group discussions, and digital feedback mechanisms. These strategies emphasised self-efficacy and adherence. Key content areas encompassed HIV education, stress management, self-esteem enhancement, and advocacy. Collectively, these findings underscore effective approaches to improving the psychological and practical aspects of living with HIV for adolescents.
5. Discussion
There is a noticeable lack of targeted educational interventions specifically designed for adolescents living with HIV. Only five studies met the eligibility criteria during the review, highlighting the scarcity of research in this critical area. The findings emphasise a significant focus on interventions aimed at enhancing various dimensions of health and psychosocial well-being among adolescents and young adults with HIV. Despite varying methodologies and contexts, a common theme emerges: the necessity for tailored interventions that address the unique challenges faced by this population.
The reviewed studies employed mixed-method and quantitative designs, reflecting a comprehensive approach to evaluating these interventions. For example, the studies conducted by Hosek et al. (2018) and Fongkaew et al. (2017) utilised mixed methods, allowing for a richer understanding of both quantitative outcomes and the qualitative experiences of participants. Researchers gained a multi-dimensional perspective that can inform future interventions by integrating individual interviews and focus group discussions with pre-and post-test measures. Interventions also drew on established theoretical frameworks, such as the Social Cognitive Theory, the Information-Motivation-Behavior Model, and the Stages of Change model, to guide their design and implementation. Some initiatives, like the Click web-based intervention adherence module, effectively used digital platforms for content delivery.
In contrast, others, such as the Adolescents Coping, Connecting, Empowering, and Protecting Together intervention and the Thai Collaborative Multidisciplinary HIV Program for Youth intervention, relied on face-to-face sessions. The outcomes of these studies suggest that these interventions are feasible and effective in improving knowledge, social support, and treatment adherence among adolescents. Reports of high participant satisfaction across studies further indicate that tailored and engaging interventions are well-received by this demographic.
Moreover, the mode of setting of participant recruitment can affect intervention delivery and significantly influence attendance and retention rates among adolescents living with HIV. For instance, Nestadt et al. (2019) observed increased attendance and engagement in the Collaborative Multidisciplinary HIV Program for Youth intervention, implying that structured and engaging programs can positively affect behaviour. As noted by Rogers et al. (2001), the high levels of participant satisfaction across studies highlight the importance of acceptability in the design of interventions. One intervention that stands out is the Thai Collaborative Multidisciplinary HIV Program for Youth intervention, characterised by its feasibility, cultural sensitivity, and potential cost-effectiveness in Southern Africa. This Thai intervention is based on the African Collaborative Multidisciplinary HIV Program for Youth intervention model, which was initially developed in alignment with the South African educational curriculum. This thoughtful adaptation ensures that the program resonates with local cultural values, norms, and the specific challenges faced by the region's adolescents. By tailoring the content to meet participants' unique needs and experiences, the intervention fosters a sense of relevance and accessibility.
The Thai Collaborative Multidisciplinary HIV Program for Youth Intervention has shown impressive attendance, with 89% of participants consistently attending all sessions. This high level of engagement underscores the program's acceptability among adolescents, suggesting it effectively addresses their needs and resonates with them. Successful participation is crucial for building trust and motivation within the group. Designed to address a wide array of critical factors affecting adolescents living with HIV, it tackles psychosocial challenges, medication adherence, and overall HIV knowledge (Nestadt et al., 2019). By adopting a holistic approach to health and well-being, the intervention empowers youth with the knowledge and skills necessary to take control of their Health.
The Thai Collaborative Multidisciplinary HIV Program for Youth Intervention employs a comprehensive facilitator's manual to ensure consistent program delivery. This structured framework enables facilitators to maintain high-quality standards and deliver coherent messages throughout the 11-session program, thereby increasing the likelihood of achieving desired outcomes. A significant feature of this Thai intervention is its dual focus on assessing short-term and long-term impacts. This focus is vital for understanding the sustainability of the benefits gained from the intervention, ultimately aiming to improve adolescents' quality of life over time. While other programs, such as the Click web-based intervention adherence module and various interventions evaluated by researchers like Shegog et al. (2012) and Hosek et al. (2018), provide valuable insights, they may lack the same depth of cultural alignment with the specific needs of adolescents in Southern Africa as the Collaborative Multidisciplinary HIV Program for Youth intervention does.
The study's geographical distribution, mainly concentrated in the United States of America and Thailand, highlights the necessity for culturally relevant adaptations of these programs. Given the diverse social, economic, and healthcare contexts that adolescents face in different regions, there is a pressing need for context-specific and culturally tailored interventions, particularly in areas with high HIV prevalence among adolescents, such as Eastern and Southern Africa. Future research should explore interventions across various settings to understand how cultural nuances influence implementation and efficacy. Furthermore, few studies assess the long-term impact of interventions on behavioural, health, and psychosocial outcomes, indicating the need for longitudinal studies to evaluate the sustainability of intervention benefits.
Finally, the collective findings suggest that engaging clinical staff and integrating interventions into routine care can enhance treatment adherence, as highlighted by Rogers et al. (2001). Engagement emphasises the importance of training and supporting healthcare providers to implement these interventions successfully.
6. Limitations
We acknowledge that this study had some limitations. Firstly, the articles that could not be accessed through the University of Witwatersrand online library databases were excluded due to resource constraints. Some potentially relevant papers could have been missed due to this. Additionally, published studies that were not available in the English version or without full text available may have been missed during the review. Finally, due to methodological limitations, the quality of the included studies could not be appraised, as it was beyond the scope of this method (Peters et al., 2020). Instead, we aimed to provide a comprehensive overview of available interventions for Adolescents living with HIV with aspects of self-management.
7. Conclusions
The review highlights the existence of limited evidence-based, context-specific, and consumer-tailored educational interventions for Adolescents living with HIV. Moreover, our results demonstrate the potential of interventions and best practices in enhancing knowledge on HIV, Antiretroviral treatment adherence, health behaviours, and overall disease management. More comprehensive, context-specific, age-appropriate and personalised interventions are needed for adolescent self-management of HIV as a chronic condition, as well as those that can reinforce adherence to treatment and viral suppression.
Given that the emergence of the HIV phenomenon has stimulated increased research interest among adolescents as a vulnerable population worldwide, it is apparent that current efforts toward viral suppression underserve adolescents. Current evidence shows a dire need for evidence-based innovations and interventions to inform policy and practice, bridge the gap in research and improve health outcomes for adolescents living with HIV.
Funding source
This research received no specific grant from public, commercial or non-profit funding agencies.
Data availability
All the data is available within the manuscript; additional data can be found in supplementary materials.
CRediT authorship contribution statement
Ndinohokwe Foibe Mukerenge: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Conceptualization. Shelley Schmollgruber: Visualization, Supervision, Methodology, Formal analysis, Conceptualization. Ntombifikile Klaas: Writing – review & editing, Visualization, Validation, Supervision, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
The authors thank the Librarian at the University of the Witwatersrand, Faculty of Health Sciences, for their contribution and support.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijnsa.2025.100359.
Appendix. Supplementary materials
References
- Agathis N.T., Annor F.B., Coomer R., Hegle J., Patel P., Forster N., O'Malley G., Ensminger A.L., Kamuingona R., Andjamba H., Manyando M. HIV prevention program Eligibility among adolescent girls and young women Namibia, 2019. Morb. Mortal. Wkly. Rep. 2021;70(45):1570. doi: 10.15585/mmwr.mm7045a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonisteel I., Shulman R., Newhook L.A., Guttmann A., Smith S., Chafe R. Reconceptualising recruitment in qualitative research. Int J Qual Methods. 2021;20(1) 16094069211042493. [Google Scholar]
- Chory A., Nyandiko W., Martin R., Aluoch J., Scanlon M., Ashimosi C., Njoroge T., McAteer C., Apondi E., Vreeman R. HIV-related knowledge, attitudes, behaviors and experiences of kenyan adolescents living with HIV revealed in WhatsApp group chats. J. Int. Assoc. Prov. AIDS Care. 2021;20 doi: 10.1177/2325958221999579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dow D.E., Mmbaga B.T., Gallis J.A., Turner E.L., Gandhi M., Cunningham C.K., O’Donnell K.E. A group-based mental health intervention for young people living with HIV in Tanzania: results of a pilot individually randomised group treatment trial. BMC Public Health. 2020;20(1):1–3. doi: 10.1186/s12889-020-09380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fongkaew W., Udomkhamsuk W., Viseskul N., Guptaruk M.M. Developing a program for enhancing youth HIV treatment adherence and risk reduction. Nurs. Health Sci. J. 2017;19(4):427–435. doi: 10.1111/nhs.12360. [DOI] [PubMed] [Google Scholar]
- Hodgson I., Ross J., Haamujompa C., Gitau-Mburu D. Living as an adolescent with HIV in Zambia–lived experiences, sexual health and reproductive needs'. AIDS Care J. 2012;24(10):1204–1210. doi: 10.1080/09540121.2012.658755. [DOI] [PubMed] [Google Scholar]
- Hosek S.G., Harper G.W., Lemos D., Burke-Miller J., Lee S., Friedman L., Martinez J. Project ACCEPT: evaluation of a group-based intervention to improve engagement in care for youth newly diagnosed with HIV. AIDS Behav. 2018;22:2650–2661. doi: 10.1007/s10461-018-2034-4. [DOI] [PubMed] [Google Scholar]
- Laurenzi C.A., du Toit S., Ameyan W., Melendez-Torres G.J., Kara T., Brand A., Chideya Y., Abrahams N., Bradshaw M., Page D.T., Ford N. Psychosocial interventions for improving engagement in care and health and behavioural outcomes for adolescents and young people living with HIV: a systematic review and meta-analysis. J Int AIDS Soc. 2021;24(8) doi: 10.1002/jia2.25741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group PRISMA. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Munyayi F.K., Van Wyk B. The effects of Teen Clubs on retention in HIV care among adolescents in Windhoek, Namibia. South Afr J HIV Med. 2020;21(1):1–9. doi: 10.4102/sajhivmed.v21i1.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nestadt D.F., Saisaengjan C., McKay M.M., Bunupuradah T., Pardo G., Lakhonpon S., Gopalan P., Leu C.S., Petdachai W., Kosalaraksa P., Srirompotong U. CHAMP+ Thailand: pilot randomised control trial of a family-based psychosocial intervention for perinatally HIV-infected early adolescents. AIDS Patient Care STDS. 2019;33(5):227–236. doi: 10.1089/apc.2019.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman B.M., Newman PR. Cengage Learning; 2017. Development through life: A psychosocial approach. [Google Scholar]
- Nsibandze B.S., Downing C., Poggenpoel M., Myburgh CP. I have been rejected so many times”: Experiences of female adolescents living with HIV in rural Manzini, Eswatini: A case study. Int. J. Afr. Nurs. Sci. 2021;14 doi: 10.2989/16085906.2020.1758735. [DOI] [PubMed] [Google Scholar]
- Peters M.D., Marnie C., Tricco A.C., Pollock D., Munn Z., Alexander L., McInerney P., Godfrey C.M., Khalil H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020;18(10):2119–2126. doi: 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- Peters M., Marnie C., Tricco A., Pollock D., Munn Z., Alexander L., McInerney P., Godfrey C., Khalil H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Implement. 2021;19(1):3–10. doi: 10.1097/XEB.0000000000000277. [DOI] [PubMed] [Google Scholar]
- Rogers A.S., Miller S., Murphy D.A., Tanney M., Fortune T. The TREAT (Therapeutic Regimens Enhancing Adherence in Teens) program: theory and preliminary results. J. Adolesc. Health. 2001;29(3):30–38. doi: 10.1016/s1054-139x(01)00289-0. [DOI] [PubMed] [Google Scholar]
- Shayo F.K., Kalomo M.H. Prevalence and correlates of sexual intercourse among sexually active in-school adolescents: an analysis of five sub-Sahara African countries for the adolescent’s sexual health policy implications. BMC Public Health. 2019;19(1):1–8. doi: 10.1186/s12889-019-7632-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shegog R., Markham C.M., Leonard A.D., Bui T.C., Paul M.E. +CLICK’: pilot of a web-based training program to enhance antiretroviral adherence among HIV-positive youth. AIDS Care. 2012;24(3):310–318. doi: 10.1080/09540121.2011.608788. [DOI] [PubMed] [Google Scholar]
- St Clair-Sullivan N., Mwamba C., Whetham J., Moore C.B., Darking M., Vera J. Barriers to HIV care and adherence for young people living with HIV in Zambia and mHealth. mHealth J. 2019;5 doi: 10.21037/mhealth.2019.09.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D., Horsley T., Weeks L., Hempel S. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- UNAIDS., Global HIV-AIDS Statistics-Fact sheet. 2023. https://www.unaids.org/en/resources/fact-sheet Available online at: (Accessed date June 07, 2024) [Google Scholar]
- Willis N., Milanzi A., Mawodzeke M., Dziwa C., Armstrong A., Yekeye I., Mtshali P., James V. Effectiveness of community adolescent treatment supporters (CATS) interventions in improving linkage and retention in care, adherence to antiretroviral and psychosocial well-being: a randomised trial among adolescents living with HIV in rural Zimbabwe. BMC Public Health. 2019;19(1):1–9. doi: 10.1186/s12889-019-6447-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2016. Guidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All the data is available within the manuscript; additional data can be found in supplementary materials.