Abstract
Positive- and negative-reinforcement-based procedures typically have targeted acceptance for children with severe food refusal; however, these procedures do not always result in successful swallowing. Once acceptance is achieved, some children expel the food repeatedly or pack (hold or pocket) it in their mouths for extended periods of time. This study evaluated the effects of using food redistribution with a bristled massaging toothbrush to reduce packing and increase consumption in 4 children with severe feeding disorders. Packing was reduced for all children. In addition, latency to clean mouth (the duration of time from acceptance to food no longer being present in the child's mouth in the absence of expulsion) for 2 children decreased when the food-redistribution procedure was used. Results are discussed in terms of the potential operant functions of the food-redistribution procedure.
Keywords: food redistribution, negative reinforcement, packing, pediatric feeding disorders
Eating is a complex response consisting of a chain of behaviors that include accepting, chewing, and swallowing the food or drink. Problems in consumption may occur at any point along the chain. For example, Riordan, Iwata, Wohl, and Finney (1980) found that differential reinforcement of acceptance resulted in increased acceptance, but this increase in acceptance also was accompanied by increases in packing (holding or pocketing food). The treatment for packing consisted of altering the contingency such that the child was required to swallow the food or drink to receive reinforcement. However, no data on packing were presented, so it is not clear if this contingency change reduced packing.
Sevin, Gulotta, Sierp, Rosica, and Miller (2002) examined response covariation in a child with severe food refusal. In this case study, a series of procedures was implemented sequentially to address collateral increases in alternative topographies of inappropriate mealtime behaviors (i.e., refusal to accept, expulsion, and packing). A nonremoval-of-the-spoon procedure produced increased acceptance that was accompanied by increased expulsion. Re-presentation of expelled food reduced expulsion but was accompanied by increased packing. Therefore, food redistribution (placing the food back on the tongue) then was used to reduce the child's packing.
Even though packing is a behavior that has not been reported widely in the literature, it has the potential to be a serious, if not life-threatening, problem for individuals with pediatric feeding disorders. When a child packs food, accepted bites are not swallowed in a timely manner, and packed bites may remain in the child's mouth for extended periods of time. Thus, packing may lead to decreased caloric intake (i.e., malnutrition, failure to thrive) and increased risk for aspiration. Despite the potential negative consequences of packing, only Sevin et al. (2002) have operationally defined and systematically treated packing. Even though the Sevin et al. study is important, only 1 child participated, and no data were presented on the extent to which bites were swallowed in a timely manner or if intake increased as a result of treatment. Therefore, the purpose of the current investigation was to extend the work of Sevin et al. by examining the effects (i.e., reduction in packed bites and mean latency to clean mouth) of the food-redistribution procedure more fully by implementing the procedure with 4 participants.
Method
Participants and Setting
The participants were 4 children who had been admitted to an intensive 6- to 8-week day-treatment program for the assessment and treatment of chronic food refusal. Two of the children were 100% gastrostomy-(G-)tube dependent, with Sarah having no oral intake or history of eating by mouth prior to receiving a G-tube. However, Mary did take small amounts of food by mouth prior to and after the G-tube was placed (but never enough to sustain normal growth) and appeared to know how to chew and swallow. Devin and Carl also had some history of eating prior to the G-tube placement but again had inadequate intake to sustain normal growth. Mary was a 5-year-old girl with a history of failure to thrive (FTT), status post respiratory failure, left vocal cord paralysis, gastroesophageal reflux (GER), and status post Nissen fundoplication. Devin was a 2-year-old boy with a medical history including GER, FTT, and developmental delays. Carl was a 2-year-old boy with a medical history that included low facial muscle tone with delayed language and oral motor skills, and bottle dependence. Sarah was a 4-year-old girl with a medical history of septal optic dysplasia, optic nerve hypoplasia, seizure disorder, and “brain anomalies.”
Dependent Variables and Data Collection
The primary dependent variables were packing (any food larger than the size of a pea in the mouth 30 s after acceptance; this did not include the absence of food in the mouth as a result of expulsion) and latency to a clean mouth for Carl and Sarah (the duration of time from acceptance to food no longer being present in the child's mouth; this did not include the absence of food in the mouth as a result of expulsion). Only one pack was recorded per bite despite the fact that the redistribution procedure may have been used more than once per bite. Secondary variables were also collected: acceptances (food being placed in the mouth past the lips within 5 s of presentation), expulsions (any food or drink larger than the size of a pea that had not yet been swallowed, but that had already been placed in the mouth, visible outside the lips), and grams consumed (premeal minus postmeal food weights). Data on acceptances, expulsions, and packing were collected on laptop computers using an event-recording procedure. Packing was converted to a percentage by dividing the number of packs by the number of bites that entered the child's mouth multiplied by 100%. Latency to a clean mouth was measured by recording the duration from when the bite entered the child's mouth until food was no longer in the child's mouth (this did not include the absence of food in the mouth as a result of expulsion). Mean latency to clean mouth for each session was calculated by summing the durations of clean mouth for each bite and dividing by the number of bites that entered the child's mouth. Latency to clean mouth was recorded for Carl and Sarah because data from a previous analysis suggested that percentage of packs might not be sufficiently sensitive to measure treatment effects.
A second observer independently scored 64%, 23%, 32%, and 21% of sessions for Mary, Devin, Carl, and Sarah, respectively. Interobserver agreement for all participants was calculated by summing the frequency of the behavior within the session for each observer, dividing the smaller frequency by the larger frequency, and multiplying by 100%. Agreement coefficients for latency to clean mouth were calculated by summing the duration of the occurrence of the behavior within the session for each observer, dividing the smaller duration by the larger duration, and multiplying by 100%. The mean agreement was 98% (range, 87% to 100%) for packing, 95.6% (range, 80% to 100%) for acceptances, and 98.8% (range, 81.8% to 100%) for expulsions for Mary; 97% (range, 90% to 100%) for packing, 94.6% (range, 86% to 100%) for acceptances, and 99.6% (range, 96% to 100%) for expulsions for Devin; 96% (range, 88% to 100%) for packing, 93.8% (range, 82.1% to 100%) for acceptances, and 100% for expulsions for Carl; and 98% (range, 88% to 100%) for packing, 96.9% (range, 85.7% to 100%) for acceptances, and 100% for expulsions for Sarah. The mean agreement for latency to a clean mouth was 94% (range, 68% to 100%) for Carl and 97% (range, 91% to 100%) for Sarah. Interobserver agreement was not assessed for grams consumed.
Experimental Design
An ABAB design was used to evaluate the relative effects of food redistribution on packing for Mary, Carl, and Sarah (A was baseline and B was the food-redistribution procedure). A multielement design was used for Devin to evaluate packing with and without the use of food redistribution. The multielement design was used for Devin because his admission was very time limited and did not permit a lengthy treatment withdrawal design.
Procedure
Four foods, one from each food group (fruits, vegetables, starches, and meats), were presented in each session, and the order of food presentation was selected randomly prior to the session. However, the order of food presentation remained the same within a given session. Mary was presented with a chopped fine texture, and Devin, Carl, and Sarah were presented with a puree texture based on the recommendations of the speech or occupational therapist. The bolus size for each participant was 10 cc, 5.5 cc, 3.5 cc, and 1.9 cc for Mary, Devin, Carl, and Sarah, respectively. These bolus sizes could be presented on the brush without spilling, with the exception of the bolus for Devin. For Devin, one half tablespoon of Thick-It® was added to each 28 g of food to thicken the food throughout baseline and treatment. The brush was used instead of a spoon because it allowed the feeders to get better placement (because of its narrow shape and rubber tip) on the child's tongue. Also the brush was easier to maneuver in the child's mouth when collecting food present from the sides of the child's mouth.
Prior to the analysis of the food-redistribution procedure, a treatment was developed to increase each participant's acceptance of food. Even though food acceptance on average for all participants was above 90% and expulsions were near zero, increased acceptance was associated with increased packing (but not an increase in expulsion). The specific treatments for each participant are described below.
Mary was seated in a Rifton chair (i.e., a small wooden chair with an attached tray), Devin and Carl were seated in highchairs, and Sarah was seated in a regular chair. Sessions were bite based (20 bites) for Mary, and three to four meals were conducted per day with approximately one or two sessions per meal (approximately 40 min of total eating time per meal). Meals consisted of three to four 5-min sessions (15 to 20 min of total eating time per meal) for Devin, Carl, and Sarah. During treatment with nonremoval of the spoon for Devin, Carl, and Sarah, the meal may have exceeded 5 min because the child was required to swallow the last bite before the session ended. Sessions would have been terminated after 1 hr for all participants, independent of whether all bites had been swallowed. However, no meals exceeded the 1-hr time limit for any participant (M = 1,329 s, 312 s, 309 s, and 351 s for session duration for Mary, Devin, Carl, and Sarah, respectively). Meals were spaced approximately 1.5 to 2.5 hr apart (e.g., 9:00 a.m., 10:30 a.m., 12:30 p.m., 3:00 p.m., and 4:30 p.m.).
Baseline
A single bite was presented to Mary on a plate in front of her with the verbal prompt “take a bite.” The therapist presented a bite on a spoon to Devin and on a brush to Carl and Sarah while saying, “take a bite.” If Mary self-fed the bite within 5 s and Devin, Carl, and Sarah accepted the bite within 5 s, brief praise was given (e.g., “good job taking your bite”). If the bite was not accepted within 5 s, the spoon or brush was held to the child's lips (all participants) until the bite was taken (nonremoval of the spoon; Cooper et al., 1995; Hoch, Babbitt, Coe, Krell, & Hackbert, 1994). Any expelled food was collected on the spoon or brush and re-presented by holding the spoon or brush to the child's lips as in the initial presentation. A token and a preferred toy (Mary) or brief praise (Devin, Carl, and Sarah) was provided if the child swallowed the bite within 30 s. Mary also received a highly preferred item at the end of the session if she earned more than 18 tokens. Devin had continuous access to toys and adult attention (noncontingent reinforcement). Preferred items were identified based on the results of a preference assessment (Fisher et al., 1992) conducted prior to the treatment analysis. If the child packed the bite of food, he or she was prompted to finish the bite. This prompt was repeated every 30 s until no food was visible in the child's mouth in the absence of expulsion or until the session ended. No other consequences were delivered for packing. All inappropriate behaviors were ignored. Every 30 s, the verbal prompt “show me” was used to prompt the child to open his or her mouth to determine if food was present. This prompt was repeated every 30 s until no food larger than the size of a pea was in the child's mouth (clean mouth).
Food redistribution
The procedures were identical to baseline for all participants. That is, bites were presented on a plate (Mary), spoon (Devin), or brush (Carl and Sarah). Brief praise was delivered following acceptance, expelled bites were re-presented, refused bites were held at the child's lips until acceptance, and the availability of tokens (Mary) or toys and attention (Mary and Devin) was as described above. In addition, food present in the child's mouth was redistributed using a brush for all participants. Mary was the only child for whom the redistribution procedure was used contingent on packing. For Carl, Sarah, and Devin, redistribution was done either immediately after the bite was presented (Devin) or after 15 s (Carl and Sarah). Packed bites were still recorded for Carl, Sarah, and Devin, because in some cases they still packed despite already having received the redistribution procedure. The therapist placed the brush inside the participant's mouth while visually examining the mouth for food. Any food remaining in the participant's mouth was collected on the brush (i.e., the therapist placed the brush under the food and scooped the food onto the brush). Once all food remaining in the participant's mouth had been collected onto the brush, it was placed on the middle of the participant's tongue. The therapist rotated the brush on the tongue, alternating between clockwise and counterclockwise turns, while slowly pulling the brush out of the mouth, which resulted in the food being deposited on the tongue.
Food redistribution was implemented for Mary if the bite was not swallowed within 30 s of acceptance, immediately after acceptance for Devin, and 15 s after acceptance for Carl and Sarah. That is, 30 s (Mary), immediately (Devin), or 15 s (Carl and Sarah) after acceptance, the therapist prompted the child to “show me,” and if any food larger than the size of a pea remained in the child's mouth, it was collected on the brush and placed back on the tongue. The redistribution procedure was implemented at different times to see if using the procedure prior to checking for a clean mouth would facilitate an even faster swallow. The hope was that if the child was able to swallow before the check for a clean mouth, he or she would have the added benefit of receiving reinforcement for swallowing successfully. The redistribution procedure was repeated every 30 s for Mary and Devin and every 15 s for Carl and Sarah until no food was in the child's mouth during the “show me” check. However, a pack was scored only if food larger than the size of a pea was in the participant's mouth at the 30-s mouth check (as in baseline).
Results
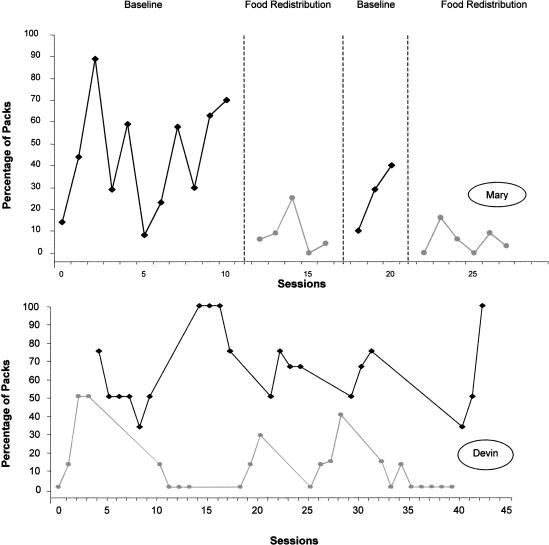
During baseline, the percentage of packs for Mary (Figure 1, top) was variable, ranging between 8% and 89%. Once food redistribution was introduced, packing decreased to low levels. Removal of the redistribution procedure resulted in an increase in percentage of packs; percentage of packs decreased again with the reintroduction of food redistribution. Percentage of acceptances remained high and stable during baseline and when food redistribution was introduced (M = 96%). Mean number of expulsions was near zero for both baseline and the redistribution procedure. Similarly, grams consumed were variable during baseline (M = 98 g) and increased slightly (M = 129 g) when food redistribution was introduced.
Figure 1. Percentage of packs for Mary (top panel) and for Devin (bottom panel).
Percentage of packs for Devin (Figure 1, bottom) was higher in baseline than in the redistribution procedure. Percentage of acceptances remained high and stable during baseline and when redistribution was introduced (M = 100%). Mean number of expulsions was near zero for both baseline and the redistribution procedure. Grams consumed were higher with food redistribution (M = 61.6) than in baseline (M = 36.4).
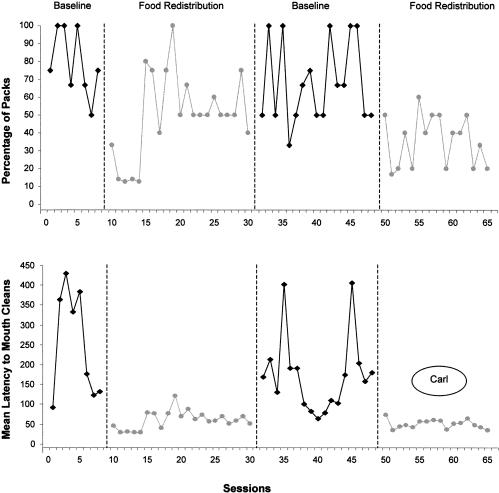
Percentage of packs for Carl (Figure 2, top) was high during baseline. Initially, when food redistribution was introduced the level of packing dropped, increased, and then leveled off to below 50%. After redistribution was withdrawn, packing increased. When redistribution was reintroduced, packing decreased to low and stable levels below 50%. Latencies to a clean mouth (Figure 2, bottom) were variable during baseline. Latency dropped below 50 s once redistribution was introduced. When redistribution was withdrawn, latency to clean mouth increased and decreased when redistribution was reintroduced. Even though the latency to clean mouth was on a downward trend in the first baseline, the levels of the latencies were equivalent in the two baselines, and the level of the latencies clearly was different between the baseline and treatment phases. The mean number of times redistribution was implemented was 1.46 per bite. Percentage of acceptances remained high and stable during baseline and when redistribution was introduced (M = 96%). Mean number of expulsions was near zero for both baseline and the redistribution procedure. Small differences were noted for grams consumed between the baseline (M = 11.3) and treatment (M = 14.5) phases.
Figure 2. Percentage of packs (top panel) and latency to clean mouth (bottom panel) for Carl.
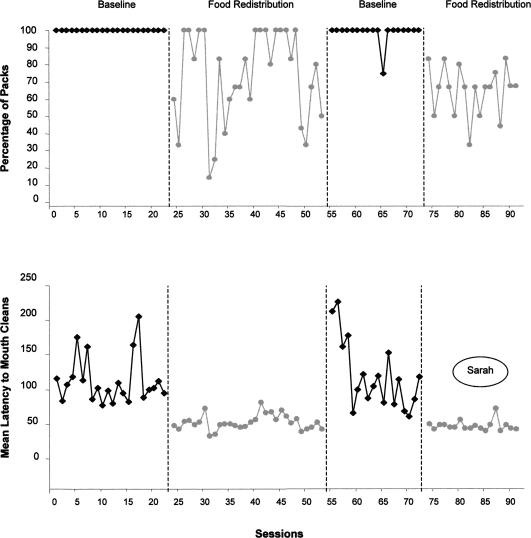
Percentage of packs for Sarah (Figure 3, top) was 100% during baseline. Percentage of packs decreased slightly with the introduction of food redistribution but remained variable throughout the first treatment phase. Percentage of packs increased when food redistribution was withdrawn. The reintroduction of food redistribution decreased packs to below 80%. During baseline, Sarah's latencies to clean mouth (Figure 3, bottom) ranged from 90 s to over 200 s. After the introduction of the redistribution procedure, her latency to a clean mouth decreased below 60 s. Even though latency to clean mouth was on a slight downward trend in the first baseline, the overall latency did not overlap during the first baseline and the first implementation of redistribution. Latencies again increased when the redistribution procedure was withdrawn. Latencies returned to below 50 s once food redistribution was reintroduced, and the overall level of the latencies was different from baseline to treatment. The mean number of times redistribution was implemented was 2.10 per bite across the two treatment phases. Percentage of acceptances remained high and stable during baseline and when redistribution was introduced (M = 97%). Mean number of expulsions was near zero for both baseline and food redistribution. Differences in grams consumed between baseline (M = 8.13) and treatment (M = 15.85) were minimal.
Figure 3. Percentage of packs (top panel) and latency to clean mouth (bottom panel) for Sarah.
Discussion
These data are significant in that there are almost no empirical demonstrations of treatment for packing in the literature. A notable exception is the study by Sevin et al. (2002) in which packing was treated with a food-redistribution procedure. Sevin et al. showed that percentage of bites packed decreased when food redistribution was implemented with 1 participant. The data from the current investigation extend those of Sevin et al. by examining the effects of food redistribution on packed bites and mean latencies to a clean mouth. The redistribution procedure was used with 4 children with a pediatric feeding disorder who packed accepted bites. We showed that the redistribution procedure was effective in reducing levels of packing by varying amounts for individual children. The data for Mary and Devin are similar to those of Sevin et al. in that food redistribution was associated with low levels of packing (less than 10% of bites packed by the end of treatment).
By contrast, even though the percentage of packing decreased from baseline for Carl and Sarah with the redistribution procedure, levels of packing remained relatively high from a clinical standpoint (50% or more bites packed). If we had taken data only on packing, we may have concluded that the redistribution procedure was not effective clinically. However, data for latency to a clean mouth showed that the implementation of food redistribution resulted in decreases in the amount of time bites of food remained in the child's mouth. That is, even though packing still occurred (i.e., bites remained in the child's mouth 30 s after acceptance), the overall length of time the bites remained in the child's mouth decreased, suggesting that participants were swallowing more quickly than in baseline. In addition, food redistribution was associated with increased grams consumed for all participants, which is important if decreased caloric intake is one of the problems associated with packing. Therefore, these data extend those of Sevin et al. (2002) by showing that multiple measures may be necessary to capture the effects of treatment for packing.
One important question that remains to be answered is why packing emerges. Sevin et al. (2002) hypothesized that packing may be part of a chain of negatively reinforced behaviors that a child may exhibit during the treatment of food refusal. In the Sevin et al. investigation, treatment of refusal resulted in increased acceptance (the food entered the child's mouth); however, the child then began expelling the food. Treatment of expulsion resulted in reduced expulsion (the food remained in the child's mouth), but then the child began packing (holding the food in her mouth). Thus, it appeared that the child engaged in a sequence of behaviors to avoid consumption.
By contrast, the participants in the current investigation did not exhibit the same hierarchy of refusal behaviors observed by Sevin et al. (2002). In the current investigation, treatment of refusal resulted in increases in acceptance and increases in packing, but not increases in expulsion. Acceptance remained high throughout the treatment for packing, and expulsion never emerged for any participant. One explanation for this difference is that expulsions and food refusal were immediately placed on extinction in the form of nonremoval of the spoon with re-presentation of expelled bites from the start of treatment. This was not done in the Sevin et al. study.
There may be a variety of reasons why avoidance of eating develops. Shore, Babbitt, Williams, Coe, and Snyder (1998) and Patel, Piazza, Santana, and Volkert (2002) proposed that avoidance of eating may develop when food has been paired with gagging or vomiting in the past. That is, some children may hold food in their mouth to avoid choking or gagging. The focus of the Shore et al. and Patel et al. studies was the effects of texture on acceptance and expulsion. Nevertheless, this same hypothesis could be applied to any texture if it has been associated with aversive stimulation.
If packing is an avoidance behavior, then the food-redistribution procedure may function as negative reinforcement. That is, the child can avoid redistribution by swallowing the food. However, the extent to which packing is maintained by negative reinforcement and the extent to which redistribution functions as negative reinforcement are unknown, because the functions of packing and the food-redistribution procedure were not evaluated.
If redistribution functions as negative reinforcement for swallowing, then presumably, packing should decrease fairly rapidly and the frequency of redistribution also should decrease. That is, the child should learn to avoid implementation of the procedure by swallowing the food prior to its implementation, thus eliminating the necessity of redistribution. Mary's data provide the best test of this effect because redistribution was implemented after the occurrence of packing was scored. That is, her mouth was checked 30 s after the bite was accepted and either a pack or a clean mouth (no food larger than the size of pea in the mouth) was scored. If food remained in her mouth at the 30-s check, then redistribution was implemented. Therefore, the only way packing would have been reduced for Mary is if she was avoiding the procedure altogether and swallowing the bite of food before the 30-s check (i.e., before redistribution could be implemented). Thus, Mary's data may be indicative of a negative reinforcement effect in that packing declined to near-zero levels, suggesting that the number of implementations of redistribution declined during treatment.
Alternatively, a child may pack food because he or she lacks the prerequisite skills (e.g., tongue lateralization and elevation) necessary to swallow. That is, typical eaters follow a progression of consuming consistencies from liquids to solids over a 12- to 18-month period. Experience with one consistency of liquid or solid aids in the development of appropriate oral motor skills necessary to process food at the next consistency (Stevenson & Allaire, 1991). Early or late introduction of these steps (e.g., introducing solids too early or too late) may result in medical or behavioral feeding problems (Brown, Black, Lopez de Romana, & Creed de Kanashiro, 1989; Christophersen & Hall, 1978; Kleinman, 2000). Thus, it is more likely that children with a history of food refusal who are inexperienced eaters might not have developed the skills to swallow efficiently (Christophersen & Hall). The food-redistribution procedure may facilitate swallowing because the procedure approximates one of the early behaviors in the chain that is necessary for swallowing (i.e., forming the food into a bolus and moving it back on the tongue).
If food redistribution resulted in acquisition of the skill to swallow, then the levels of packing should not have increased following removal of the redistribution procedure (i.e., the skill would have persisted independent of the procedure), as was the case with all of the participants. Thus, an alternative explanation is that redistribution may facilitate swallowing without improvement in the child's skills over the course of a brief analysis such as the one conducted in the current investigation. The data for Carl and Sarah may be indicative of this effect.
The redistribution procedure for Carl and Sarah was implemented 15 s after the bite was presented and every 15 s thereafter. As with Mary, mouth checks were conducted 30 s after the bite was accepted, and either a pack or a clean mouth was scored (as in baseline). Packing for both Carl and Sarah decreased during redistribution, but remained at relatively high levels clinically, suggesting that they were not avoiding implementation of the redistribution procedure. In addition, packing and latency to clean mouth increased once the redistribution procedure was withdrawn, suggesting that the participants also did not acquire the skill to swallow as a result of the procedure. In fact, the data suggested that the redistribution procedure was implemented approximately once or twice on each bite presentation. Thus, redistribution appeared to facilitate the swallow rather than to facilitate skill acquisition, because the effect of the procedure was to reduce the length of time the food remained in the participants' mouths and did not produce a more permanent change in packing (as one would expect if it were skill acquisition). In addition, the redistribution procedure did not seem to function as negative reinforcement (at least for Carl and Sarah) because there was an effect on latency to clean mouth rather than a large reduction in packing.
Earlier studies by Hoch et al. (1994) and Lamm and Greer (1988) showed that a posterior placement of food on the tongue resulted in swallow elicitation, which could result in a faster swallow. The procedure used in the current investigation differed from that of Hoch et al. and Lamm and Greer in that posterior placement was not used. In addition, no data were collected in the current investigation on latency to swallowing. A measurement of latency to swallowing would perhaps be a more sensitive measure of a swallow-facilitation effect relative to the measures used in the current investigation. Future research should compare middle and posterior placement of food on the tongue and measurement of latency to swallowing to examine swallow facilitation more fully. Also, no adverse clinical signs (i.e., choking, gagging, watery eyes) were observed for any of the children when the redistribution procedure was implemented. Typically, these clinical signs would be used as an indicator that a child might be aspirating. A more systematic evaluation of redistribution using a modified barium swallow study to assess a child's swallowing ability would provide more conclusive evidence that the procedure is a safer alternative to packing.
In conclusion, this study adds to the sparse literature on the assessment and treatment of packing. We showed that with a simple food-redistribution procedure, packing could be reduced significantly, resulting in improved eating in children with chronic food refusal.
Acknowledgments
This investigation was supported in part by Grant 1 K24 HD01380-01 received by the second author from the Department of Health and Human Services, the National Institute of Child Health and Human Development.
Study Questions
What is food packing, and what are some of its associated risks?
What were the dependent variables, and how were they measured?
What experimental design was used with the majority of participants, and why was a different design used with Devin?
How was packing treated differently during baseline and redistribution conditions?
Briefly summarize the results of this study. What supplementary data suggested that the reductions in packing were clinically significant?
What evidence did the authors provide to support the hypothesis that packing is part of a response chain?
The authors suggested that the redistribution procedure might function as negative reinforcement. What data support this interpretation?
What data suggest that packing was not due to swallowing-related deficits?
Questions prepared by Jessica L. Thomason and Jennifer Hammond, University of Florida
References
- Brown K.H, Black R.E, Lopez de Romana G, Creed de Kanashiro H. Infant feeding practices and their relationships with diarrhea and other diseases. Pediatrics. 1989;83:31–40. [PubMed] [Google Scholar]
- Christophersen E.R, Hall C.L. Eating patterns and associated problems encountered in normal children. Issues in Comprehensive Pediatric Nursing. 1978;3:1–16. doi: 10.3109/01460867809087345. [DOI] [PubMed] [Google Scholar]
- Cooper L.J, Wacker D.P, McComas J, Brown K, Peck S.M, Richman D, et al. Use of component analysis to identify active variables in treatment packages for children with feeding disorders. Journal of Applied Behavior Analysis. 1995;28:139–153. doi: 10.1901/jaba.1995.28-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher W.W, Piazza C.C, Bowman L.G, Hagopian L.P, Owens J.C, Slevin I. A comparison of two approaches for identifying reinforcers for persons with severe and profound disabilities. Journal of Applied Behavior Analysis. 1992;25:491–498. doi: 10.1901/jaba.1992.25-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoch T.A, Babbitt R.L, Coe D.A, Krell D.M, Hackbert L. Contingency contacting: Combining positive reinforcement and escape extinction procedures to treat persistent food refusal. Behavior Modification. 1994;18:106–128. doi: 10.1177/01454455940181007. [DOI] [PubMed] [Google Scholar]
- Kleinman R.E. Complementary feeding and later health. Pediatrics. 2000;106:1287–1288. [PubMed] [Google Scholar]
- Lamm N, Greer D. Induction and maintenance of swallowing responses in infants with dysphasia. Journal of Applied Behavior Analysis. 1988;21:143–156. doi: 10.1901/jaba.1988.21-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel M.R, Piazza C.C, Santana C.M, Volkert V.M. An evaluation of food type and texture in the treatment of a feeding problem. Journal of Applied Behavior Analysis. 2002;35:183–186. doi: 10.1901/jaba.2002.35-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riordan M.M, Iwata B.A, Wohl M.K, Finney J.W. Behavioral treatment of food refusal and selectivity in developmentally disabled children. Applied Research in Mental Retardation. 1980;1:95–112. doi: 10.1016/0270-3092(80)90019-3. [DOI] [PubMed] [Google Scholar]
- Sevin B.M, Gulotta C.S, Sierp B.J, Rosica L.A, Miller L.J. Analysis of response covariation among multiple topographies of food refusal. Journal of Applied Behavior Analysis. 2002;35:65–68. doi: 10.1901/jaba.2002.35-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shore B.A, Babbitt R.L, Williams K.E, Coe D.A, Snyder A. Use of texture fading in the treatment of food selectivity. Journal of Applied Behavior Analysis. 1998;31:621–633. doi: 10.1901/jaba.1998.31-621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson R.D, Allaire J.H. The development of normal feeding and swallowing. Pediatric Clinics of North America. 1991;38:1439–1453. doi: 10.1016/s0031-3955(16)38229-3. [DOI] [PubMed] [Google Scholar]