Abstract
Introduction
Diabetes mellitus (DM) and prediabetes represent significant public health challenges in Peru, with prevalence rates showing considerable variation across recent epidemiological studies.
Objective
To conduct a systematic review and meta-analysis to determine the pooled prevalence of diabetes and prediabetes in Peru and identify temporal trends and sources of heterogeneity.
Methodology
A comprehensive search was conducted in PubMed, Web of Science, SCOPUS, EMBASE and LILACS databases for studies reporting DM and prediabetes prevalence in Peru. Both national and subnational studies using standardized diagnostic criteria and representative sampling were included. Random-effects meta-analysis was performed, with subgroup analyses by sex, age and geographic scope. Meta-regression was conducted to explore temporal trends and sources of heterogeneity.
Results
Eight independent studies comprising 18,502 participants provided diabetes data, while five studies with 11,056 participants reported prediabetes data, spanning 2005–2018. The pooled DM prevalence was 7.47% (95% CI: 5.02–10.35%) and prediabetes prevalence was 10.66% (95% CI: 4.29–19.42%). Meta-regression revealed a significant increasing temporal trend for DM (p < 0.0001), with prevalence rising from 2.99% in 2005 to 16.97% in 2018. Substantial heterogeneity was observed for both conditions (I² = 98–99%).
Conclusions
Diabetes and prediabetes prevalence in Peru have increased significantly over the past decade, reaching concerning levels that require urgent public health attention. The substantial heterogeneity observed emphasizes the need for standardized diagnostic protocols and more comprehensive national surveillance systems to accurately monitor these conditions and guide evidence-based prevention strategies.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13098-025-01844-z.
Keywords: Prediabetic state, Diabetes mellitus, Prevalence, Peru, Systematic review, Meta-analysis
Introduction
Diabetes mellitus (DM) is a chronic disease that has seen a significant rise in prevalence globally over the past few decades, becoming a major public health concern [1]. Notably, the prevalence of DM in developing countries has been growing faster than in developed nations [2]. Peru is no exception among Latin American countries experiencing a steady increase in metabolic diseases [3, 4], including a documented rise in DM prevalence in recent years [5].
DM profoundly impacts individual health and places a substantial economic burden on health systems and national economies [6]. Complications from DM, such as cardiovascular disease, kidney failure, and blindness, can severely decrease quality of life and increase mortality [7, 8]. Additionally, managing DM and its complications leads to significant healthcare costs, loss of productivity, and indirect costs related to disability and premature death [9]. Therefore, effective prevention and control of DM are essential to improving public health and ensuring the sustainability of health systems in Peru.
Despite the rising prevalence of DM in Peru, accurately understanding its magnitude remains challenging. This difficulty is partly due to the lack of large-scale epidemiological studies and the variability in the quality of reported data. Recent research has shown significant disparities in prevalence figures, ranging from as low as 3%, as reported by the Nutritional Biochemical Indicators Survey (ENINBSC, acronym in Spanish) [10] or the study by Miranda JJ [11], to as high as 10% in the Nutritional and Food Surveillance by Life Stages (VIANEV, acronym in Spanish) study [12]. This variability underscores significant inconsistencies in the estimates and highlights the uncertainty about the real impact of DM on the Peruvian population.
Although Carrillo and Bernabé conducted a review in 2019 [13], their study did not perform an exhaustive meta-analysis, excluded key data such as the VIANEV study, and did not include prediabetes. Therefore, the present study aims to conduct an updated systematic review (SR) with a meta-analysis of the prevalence of DM and prediabetes in Peru.
Methods
Design
A SR with meta-analysis and pooled analysis of national cross-sectional studies was conducted, following the guidelines of the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [14], considering that this was an SR of prevalence studies [15, 16].
Additional data sources and justification
In addition to published studies, technical reports and national databases were included for a more comprehensive evaluation. When reports and manuscripts were unavailable, data were extracted from national databases. In these cases, the original study that generated the database was cited to provide complete methodological context and ensure transparency in the data source.
Search strategy
From January 2000 to June 3, 2025, a strategic search was conducted in six academic databases: Scopus, Web of Science, Embase, PubMed/Medline and LILACS. No language restrictions were applied during the search and study selection process to ensure comprehensive coverage of available evidence. The key terms used for the search across all sources were “prevalence,” “diabetes,” “prediabetes,” and “Peru.” The detailed search strategy for each database and technical report source, as well as national databases, is provided in Supplementary Material 1.
Selection criteria
Studies were eligible for inclusion if they: (1) Were observational studies published as full articles or technical reports in the absence of full articles; (2) Included adult participants of both sexes; (3) Had as primary objective the evaluation of diabetes and prediabetes prevalence, or allowed extraction of prevalence data for these conditions from their secondary objectives; (4) Evaluated the prevalence of diabetes and prediabetes in Peru, with at least one blood marker, such as fasting plasma glucose (FPG), oral glucose tolerance test (OGTT), or glycated hemoglobin (HbA1c), as recommended by the American Diabetes Association [17]; (5) Focused primarily on type 2 DM, as this represents the predominant form of diabetes in adult populations, though studies reporting combined diabetes types were included when type-specific data could not be disaggregated; (6) Used probabilistic sampling; and (7) Provided sufficient data to calculate prevalence or directly reported prevalence.
Narrative reviews, editorials, preclinical studies, and studies not pertinent to the objective of this study were excluded. When multiple publications reported data from the same study or database, the original study name and data collection year were used to prevent duplication and ensure proper temporal sequencing.
Study selection
The Rayyan software (https://rayyan.qcri.org) was used to manage and store articles identified from each database. Two independent reviewers (FEZM and LEMVR) conducted an initial review of the titles and abstracts of manuscripts, technical reports, and national databases. If both reviewers agreed that a source met the inclusion criteria, it was selected for a more detailed review. In cases of disagreement, a third reviewer (WR) acted as an arbitrator.
Subsequently, a thorough full-text review of all preselected articles, reports, and databases was conducted. The decision to include or exclude each source was recorded in an Excel spreadsheet. This process was also performed by three reviewers, and any discrepancies were resolved by a fourth reviewer. For databases, original studies were consulted to understand the methodology and ensure that the data were appropriate for inclusion.
Data extraction and qualitative analysis
For each selected source, meticulous data extraction was performed using a Microsoft Excel 2016 template designed for this study. Extracted data included author, year of publication, study design, sample size, prevalence of diabetes and prediabetes, and blood markers used (such as FPG, random glucose, glucose tolerance test, or glycated hemoglobin). Similar data were extracted for technical reports and national databases, and original studies were consulted to understand the methodology and ensure the quality of the extracted data. Additionally, measures of variability (such as the 95% confidence interval) were recorded when available.
Risk of bias assessment
Two of our researchers independently assessed the risk of bias for all included studies using the Joanna Briggs Institute Checklist for Prevalence Studies [15]. This tool was developed to increase consistency in SRs of prevalence data and is recommended as the most appropriate for such studies.
Bias in studies was assessed using nine specific criteria: (1) Adequacy of the sampling frame to address the target population; (2) Appropriate selection of participants; (3) Appropriateness of the sample size; (4) Detailed description of the subjects and study context; (5) Adequacy of data analysis covering the identified sample; (6) Use of valid methods to diagnose the condition; (7) Standard and reliable measurement of the condition in all participants; (8) Adequacy of the statistical methods employed; (9) Proper handling of the response rate or its impact if low.
A score of 1 to 9 was considered based on whether the response was correct to evaluate the level of bias. Studies scoring 4 points or less were considered to have a high risk of bias. Those scoring between 5 and 6 points were classified as having a medium risk of bias, and studies scoring 7 points or more were categorized as having a low risk of bias.
Quantitative analysis
This study employed comprehensive statistical analyses to evaluate diabetes and prediabetes prevalence in Peru using R statistical software (version 4.3.0) with the meta and metafor packages. The analytical approach included multiple complementary methods to ensure robust prevalence estimates and thorough exploration of between-study variability. Overall pooled prevalence estimates were calculated for both diabetes and prediabetes using random-effects models with the Freeman-Tukey double arcsine transformation to stabilize variance. The DerSimonian-Laird method was used for tau-squared estimation, and Wilson Score intervals were employed for confidence interval calculation. All analyses used inverse-variance weighting and reported 95% confidence intervals.
Systematic subgroup analyses were conducted to explore prevalence variations across key demographic and methodological characteristics. For diabetes, analyses included sex (male vs. female), age groups (< 60 vs. ≥ 60 years), geographic scope (national vs. subnational studies), and diagnostic test type (FPG, OGTT, HbA1c). For prediabetes, analyses focused on sex, age groups, and geographic scope, with all studies using consistent FPG criteria (100–125 mg/dL). Additional sensitivity analyses examined temporal trends, sample size effects, and outlier influence to assess result stability. Univariate meta-regression models were fitted to identify sources of heterogeneity, using publication year and diagnostic test type as moderators for diabetes, and publication year, sample size, and geographic scope for prediabetes. The percentage of heterogeneity explained (R²) was calculated for each model.
Between-study heterogeneity was quantified using the I² statistic, with values < 25%, 25–50%, 50–75%, and > 75% interpreted as low, moderate, high, and very high heterogeneity, respectively. Cochran’s Q-test was used to test for statistical significance of heterogeneity, and tau-squared (τ²) provided absolute measures of heterogeneity variance. Studies with statistical dependency (multiple diagnostic methods from identical populations) were handled through sensitivity analyses using unique populations only. Publication bias was assessed using Egger’s test when ≥ 6 studies were available, supplemented by visual inspection of funnel plots.
Results
Eligible studies
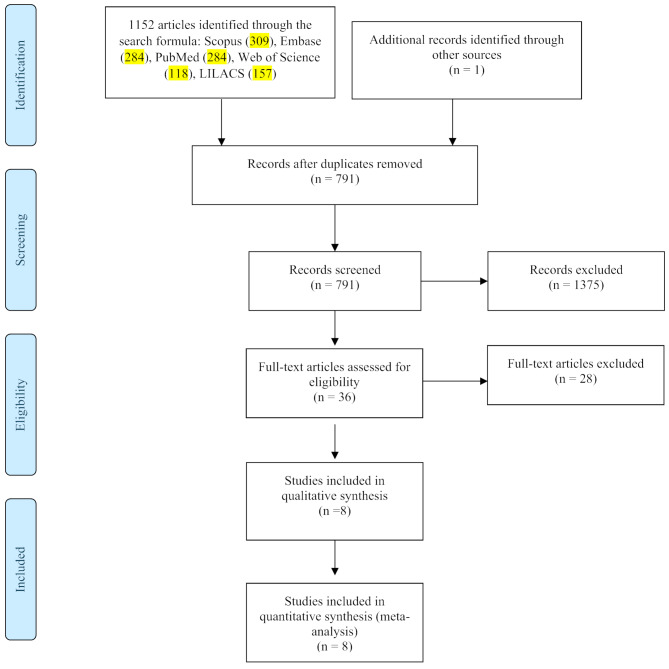
A total of 1152 publications were found. After removing duplicates, 791 manuscripts were analyzed based on title and abstract. After excluding 1375 studies, 36 full-text articles were retrieved. Finally, after applying the selection criteria, 8 articles [5, 10, 12, 18, 19, 20, 21, 22] were selected (see Fig. 1).
Fig. 1.
Flowchart of Study Selection
It is important to clarify that studies were identified and named according to the year of data collection rather than publication year to ensure accurate temporal analysis of prevalence trends. For example, the PERU MIGRANT study was conducted in 2010–2011 but published by Lazo-Porras et al. in 2020 [18]; therefore, it was referenced as “PERU MIGRANT (2011)” throughout the analysis rather than “Lazo-Porras (2020)” to maintain chronological accuracy. This nomenclature approach was consistently applied to all included studies to maintain chronological accuracy in meta-regression analyses and avoid temporal misclassification bias.
Characteristics of the studies
The characteristics of the eight included studies are summarized in Table 1. The studies spanned from 2004 to 2018, with data collection periods ranging from ENINBSC (2004–2005) [10] to VIANEV (2017–2018) [12]. Sample sizes varied considerably, from 976 participants in PERU MIGRANT (2011) [18] to 4,955 in ENINBSC 2004–2005 [10], with a total of 17,468 participants across all studies. The proportion of female participants ranged from 50.3% (Albitres-Flores, 2020) [21] to 62.4% (Revilla, 2014) [21], with most studies achieving relatively balanced sex distribution.
Table 1.
Summary of studies on the prevalence of DM and prediabetes in Peru
| First Author, Year | City | Inclusion Criteria | Exclusion Criteria | Sample Size | Gender (% women) | Mean Age | Diagnostic Criteria | Database (year of collection) |
|---|---|---|---|---|---|---|---|---|
| ENINBSC 2004–2005 | 5 strata - Metropolitan Lima, rest of coast, urban highlands, rural highlands, and jungle | Over 20 years old, oriented in time, space, and place, aware of not having a serious illness | Pregnant, breastfeeding, those who have altered their usual diet due to illness, party and/or celebrations, people with physical disabilities that do not allow normal evaluation of anthropometric indicators, bodybuilders, and qualified athletes | 4955 | 2498 (50.4%) | 42.2 | DM: FPG ≥ 126 mg/dl, Self-report; Prediabetes: FPG 100–125 mg/dl | ENINBSC (2004–2005) |
| Schargrodsky 2008 (CARMELA) | Lima | Over 25 to 64 years old | Life limits, pregnant, residents with an address different from their home, or residents who lived in areas considered dangerous for interviewers, and people who were visiting | 1652 | 883 (53.4%) | 43.6 | DM: FPG ≥ 126 mg/dl, Self-report | CARMELA (2008) |
| PERU MIGRANT 2011 | Lima, Tumbes | Over 30 years old who gave informed consent | Pregnant, with mental disorders preventing them from filling out the survey | 976 | 524 (53.7%) | 47.96 |
DM: FPG ≥ 126 mg/dl, HbA1c ≥ 6.5%, Self-report; Prediabetes: FPG 100–125 mg/dl |
PERU MIGRANT (2010–2011) |
| Revilla L. 2014 | Lima | Over 15 years old | Under 15 years old, residence less than a year in the study location, pregnant, and disabling conditions preventing adequate anthropometric evaluation | 1771 | 1105 (62.4%) | 39.5 | DM: FPG ≥ 126 mg/dl, Self-report; Prediabetes: FPG 100–125 mg/dl | FRENT LIMA CALLAO (2007) |
| Bernabé-Ortiz 2015 (CRONICAS) | Lima, Urban Puno, Rural Puno, and Tumbes | Over 35 years old, full-time residents in the area, who gave informed consent | Pregnant, with mental disorders preventing them from filling out the survey | 3238 | 1674 (51.7%) | 55.1 | DM: FPG ≥ 126 mg/dl, Self-report; Prediabetes: FPG 100–125 mg/dl | CRONICAS (2010–2011) |
| Seclén 2015 (PERUDIAB) | Lima, Rest of Coast, Highlands, and Jungle | Over or equal to 25 years old, who gave informed consent | Inability to locate or meet with the selected participant, refusal to participate in the survey, inability to validate the completed questionnaire and/or biological sample requirements. Mental disorders (according to relatives) and pregnant women. | 1677 | 851 (50.7%) | 44.8 | DM: FPG ≥ 126 mg/dl, Self-report; Prediabetes: FPG 100–125 mg/dl | PERUDIAB (2012–2015) |
| VIANEV 2017–2018 | Peru (Lima, Callao, rest of urban, rural) | Over 18 to 59 years old, fasting adults for no less than 9 h and no more than 12 h | Adults between 18 and 59 years old not on the identification list, pregnant/postpartum women, adults under treatment that alters glucose or lipid profile, those not fasting, gastrointestinal problems altering food intake, and genetic condition or malformation limiting anthropometric technique | 1040 | 573 (55.1%) | 38.4 | DM: FPG ≥ 126 mg/dl, Self-report | VIANEV (2017–2018) |
| Albitres-Flores 2020 (Tumbes) | Tumbes | Age between 30 and 69 years old, full-time resident in the study area (≥ 6 months), and capable of understanding procedures and giving informed consent | Pregnant or those with any physical disability preventing anthropometric measurements (weight, height, blood pressure, or waist circumference) or bedridden. Participants who did not complete laboratory analysis | 1609 | 810 (50.3%) | 48.2 | DM: FPG ≥ 126 mg/dl, OGTT ≥ 200 mg/dl, HbA1c ≥ 6.5%, Self-report | FINDRISCK (2014–2017) |
Geographic coverage included both national and subnational studies. Two studies provided national representation: ENINBSC 2004–2005 covered five geographical strata across Peru, and VIANEV 2017–2018 included urban and rural areas nationwide. The remaining six studies focused on specific regions, with Lima being the most frequently studied location and Tumbes represented specifically in the Albitres-Flores (2020) study [21]. Age inclusion criteria varied across studies, with minimum ages ranging from 15 years (Revilla, 2014) to 35 years (Bernabé-Ortiz, 2015) [22], and maximum ages extending to 69 years in the Tumbes study.
All studies employed FPG ≥ 126 mg/dL as the primary diagnostic criterion for diabetes, supplemented by self-reporting in all cases. The Albitres-Flores (202) study [21] was unique in incorporating all three ADA-recommended diagnostic methods: FPG ≥ 126 mg/dL, OGTT ≥ 200 mg/dL, and HbA1c ≥ 6.5%, while PERU MIGRANT (2011) included FPG and HbA1c criteria. For prediabetes diagnosis, relevant studies consistently used FPG 100–125 mg/dL criteria, with PERU MIGRANT (2011) also including HbA1c 5.7–6.4%. This comprehensive diagnostic approach in the Tumbes study provides valuable insights into the concordance and diagnostic accuracy of different diabetes detection methods in Peruvian populations.
Visual inspection of funnel plots revealed no clear evidence of publication bias for either diabetes or prediabetes studies, despite the limited number of studies available for analysis. For diabetes studies (upper panel, n = 11 assessments), the distribution of studies around the pooled estimate appears relatively symmetric, with studies scattered across different precision levels without obvious asymmetry suggesting small-study effects or publication bias. The prediabetes funnel plot (lower panel, n = 5 studies) shows a more limited distribution due to the smaller number of studies, but similarly does not demonstrate clear asymmetric patterns indicative of publication bias. While formal statistical tests for publication bias (such as Egger’s test) require a minimum of 6–10 studies and were therefore not applicable to the prediabetes analysis, the visual assessment suggests that the available evidence does not show strong indications of selective reporting or small-study effects that would significantly compromise the validity of the pooled prevalence estimates (See Supplementary file 2).
Risk of bias assessment
Risk of bias assessment using the Joanna Briggs Institute Checklist revealed that all eight studies scored between 8 and 9 points. Seven studies (87.5%) achieved maximum scores of 9 points, while one study scored 8 points (see Table 2). All studies met criteria for appropriate sampling (criterion 1), participant recruitment (criterion 2), adequate sample size (criterion 3), detailed subject description (criterion 4), sufficient data analysis coverage (criterion 5), valid diagnostic methods (criterion 6), standardized measurements (criterion 7), and appropriate statistical analysis (criterion 8). Response rate adequacy (criterion 9) was the most variable criterion, with two studies not meeting this requirement.
Table 2.
Risk of Bias in studies on the prevalence of diabetes and prediabetes in Peru
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study, Year | Was the sampling frame appropriate to address the target population? | Were the study participants recruited in an appropriate manner? | Was the sample size adequate? | Were the subjects and the setting of the study described in detail? | Was the data analysis conducted with sufficient coverage of the identified sample? | Were valid methods used for the identification of the condition? | Was the condition measured in a standard and reliable manner for all participants? | Was the statistical analysis appropriate? | Was the response rate adequate and, if not, was the low response rate adequately managed? | Total Score | Risk Level |
| ENINBSC (2004–2005) | * | * | * | * | * | * | * | * | * | 9 | Low |
| Schargrodsky 2008 | * | * | * | * | * | * | * | * | * | 9 | Low |
| PERU MIGRANT 2011 | * | * | * | * | * | * | * | * | * | 9 | Low |
| Revilla L. 2014 | * | * | * | * | * | * | * | * | 8 | Low | |
| Bernabe-Ortiz 2015 | * | * | * | * | * | * | * | * | 8 | Low | |
| Seclen 2015 | * | * | * | * | * | * | * | * | * | 9 | Low |
| VIANEV 2017–2018 | * | * | * | * | * | * | * | * | * | 9 | Low |
| Albitres-Flores 2020 (Tumbes) | * | * | * | * | * | * | * | * | 8 | Low |
Overall diabetes prevalence
The meta-analysis included 8 independent studies comprising 18,502 participants across Peru from 2005 to 2018 [5, 10, 12, 18, 19, 20, 21, 22] (see Fig. 2). The pooled DM prevalence was 7.47% (95% CI: 5.02–10.35%) using a random-effects model. Substantial heterogeneity was observed between studies (I² = 98%, p < 0.01).
Fig. 2.

Forest plot of diabetes prevalence studies in Peru (2005–2018)
Individual study prevalences ranged from 2.99% (ENINBSC, 2004–2005) [10] to 16.97% (Albitres-Flores 2020, HbA1c criteria). All studies used established diagnostic criteria: FPG ≥ 126 mg/dL, OTTG ≥ 200 mg/dL, or glycosylated hemoglobin ≥ 6.5%.
Subgroup and sensitivity analyses
Sex-specific analyses showed similar prevalence between males (4.80%, 95% CI: 1.87–8.97%) and females (4.50%, 95% CI: 2.05–7.83%), both based on 4 studies. High heterogeneity was observed in both groups (I² = 95% and 94%, respectively). Age-stratified analyses demonstrated prevalence of 4.33% (95% CI: 1.43–9.66%) in participants < 60 years and 5.43% (95% CI: 4.10–6.94%) in those ≥ 60 years, with markedly different heterogeneity patterns (I² = 98% vs. 0%) (See Table 3).
Table 3.
Sensitivity analysis of DM prevalence in Peru
| Number of studies | Prevalence | IC 95% | I2 | |
|---|---|---|---|---|
| Sex | ||||
| Female | 4 | 4.50 | 2.05–7.83 | 94% |
| Male | 4 | 4.80 | 1.87–8.97 | 95% |
| Age | ||||
| < 60 | 4 | 4.33 | 1.43–9.66 | 98% |
| ≥ 60 | 3 | 5.43 | 4.10–6.94 | 0% |
| Scope | ||||
| Subnational | 5 | 7.86 | 4.98–11.33 | 98% |
| National | 3 | 6.47 | 2.61–11.88 | 98% |
Geographic scope analysis revealed prevalence of 7.86% (95% CI: 4.98–11.33%) in subnational studies (5 studies) and 6.47% (95% CI: 2.61–11.88%) in national studies (3 studies). Both subgroups exhibited high heterogeneity (I² = 98%). The analysis of participants ≥ 60 years was the only subgroup showing homogeneous results across studies (See Table 3).
Meta-regression analysis for diabetes prevalence
Meta-regression analysis was conducted to explore sources of heterogeneity using publication year and diagnostic test type as moderators (see Fig. 3). Temporal analysis revealed a significant increasing trend in diabetes prevalence over time (QM = 21.83, p < 0.0001). The estimated annual increase was 0.0155 on the logit scale, with the model accounting for 69.05% of between-study heterogeneity (R² = 69.05%). Residual heterogeneity remained high (I² = 93.29%) after accounting for the temporal trend.
Fig. 3.
Meta-regression of diabetes prevalence by publication year in Peru (2005–2018)
Diagnostic test type analysis showed no significant overall effect (QM = 4.64, p = 0.0985). Compared to FPG as the reference, neither OGTT (estimate = 0.1371, p = 0.0783) nor HbA1c (estimate = 0.0866, p = 0.1371) demonstrated statistically significant differences in prevalence estimates. This analysis accounted for only 21.63% of between-study heterogeneity (R² = 21.63%), indicating that diagnostic method explains a smaller proportion of variability compared to temporal trends. The substantial residual heterogeneity (I² = 97.56%) suggests additional unmeasured factors contribute to the observed variation between studies.
Overall prediabetes prevalence
The meta-analysis included 5 independent studies comprising 11,056 participants across Peru from 2005 to 2015 [5, 10, 18, 21, 22]. The pooled prediabetes prevalence was 10.66% (95% CI: 4.29–19.42%) using a random-effects model. Substantial heterogeneity was observed between studies (I² = 99%, p < 0.01) (See Fig 4).
Fig. 4.
Forest plot of prediabetes prevalence studies in Peru (2005–2015)
Individual study prevalences ranged from 3.62% (ENINBSC 2004–2005) to 22.37% (Seclén, 2015). All studies used FPG criteria (100–125 mg/dL) for prediabetes diagnosis, ensuring methodological consistency across the analysis.
Sex-specific analyses showed higher prevalence in females (5.45%, 95% CI: 2.28–4.30%) compared to males (3.35%, 95% CI: 2.93–4.30%), both based on 2 studies [10, 18]. Heterogeneity differed markedly between groups, with high variability observed in females (I² = 92%) and homogeneous results in males (I² = 0%). Age-stratified analyses demonstrated higher prevalence in participants ≥ 60 years (7.23%, 95% CI: 5.44–9.23%) compared to younger adults (4.28%, 95% CI: 1.73–7.88%), with similar heterogeneity patterns showing homogeneous results in older adults (I² = 0%) and high variability in younger participants (I² = 94%) [10, 18] (See Table 4).
Table 4.
Sensitivity analysis of prediabetes prevalence in Peru
| Number of studies | Prevalence | IC 95% | I2 | |
|---|---|---|---|---|
| Sex | ||||
| Female | 2 | 5.45 | 2.28–4.30 | 92% |
| Male | 2 | 3.35 | 2.93–4.30 | 0% |
| Age | ||||
| < 60 | 2 | 4.28 | 1.73–7.88 | 94% |
| ≥ 60 | 2 | 7.23 | 5.44–9.23 | 0% |
| Scope | ||||
| Subnational | 3 | 15.20 | 2.81–34.93 | 100% |
| National | 2 | 16.03 | 6.16–29.38 | 99% |
Geographic scope analysis revealed similar prevalence between national studies (16.03%, 95% CI: 6.16–29.38%) and subnational studies (15.20%, 95% CI: 2.81–34.93%). Both subgroups exhibited very high heterogeneity (I² = 99% and 100%, respectively). Consistent with diabetes analyses, subgroups of participants ≥ 60 years and males showed homogeneous results, suggesting more stable prevalence estimates in these populations (See Table 4).
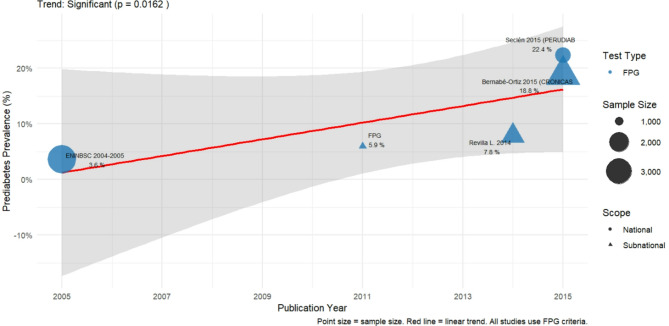
Meta-regression analysis for prediabetes prevalence
Meta-regression analysis was conducted to explore sources of heterogeneity using study characteristics as moderators. Analysis by sample size showed no significant association with prediabetes prevalence (QM = 0.10, p = 0.7576). The sample size effect was minimal (estimate = -0.0000, 95% CI: -0.0001 to 0.0001), and this covariate explained none of the between-study heterogeneity (R² = 0.00%). Residual heterogeneity remained extremely high (I² = 99.43%) after accounting for sample size effects.
Geographic scope analysis revealed no significant difference between national and subnational studies (QM = 0.01, p = 0.9115). The effect estimate for national versus subnational scope was 0.0153 (95% CI: -0.2549 to 0.2855), indicating virtually identical prevalence estimates between study types. This analysis also explained none of the observed heterogeneity (R² = 0.00%), with residual heterogeneity remaining at 99.42%. The temporal trend analysis showed a significant increasing trend over time (p = 0.0162), suggesting that publication year may be a more important predictor of prediabetes prevalence variation than study design characteristics (See Fig. 5).
Fig. 5.
Meta-regression of prediabetes prevalence by publication year in Peru (2005–2015)
Discussion
Prevalence of diabetes and prediabetes in Peru
Our SR and meta-analysis revealed a pooled diabetes prevalence of 7.47% (95% CI: 5.02–10.35%) in Peru, based on analysis of eight independent studies. These figures are consistent with global epidemiological patterns documented in large-scale international analyses. The NCD Risk Factor Collaboration’s comprehensive pooled analysis of 751 population-based studies with 4.4 million participants demonstrated substantial global variation in diabetes prevalence, with our Peruvian estimates falling within expected ranges for middle-income countries undergoing epidemiological transition [2]. This alignment with international data supports the validity of our findings while confirming that Peru faces a diabetes burden requiring sustained public health attention.
The observed DM prevalence, while concerning, reflects patterns consistent with regional Latin American trends rather than extreme outlier scenarios. Our estimates suggest that Peru maintains opportunities for effective prevention strategies before reaching the more alarming prevalence thresholds documented in some populations with unique genetic or environmental risk factors. The temporal trend analysis revealing significant annual increases (p < 0.0001) parallels global patterns of diabetes escalation, particularly in developing countries experiencing rapid socioeconomic transitions.
For prediabetes, our analysis revealed a pooled prevalence of 10.66% (95% CI: 4.29–19.42%). These findings are notably consistent with recent Latin American evidence, particularly the meta-analysis by Vera-Ponce et al. [23], which provided comprehensive regional prevalence estimates using standardized diagnostic criteria. Our estimates align well with their reported ranges, supporting the validity of our findings and suggesting that Peru’s prediabetes burden reflects broader regional patterns rather than country-specific anomalies. This concordance with regional meta-analytic evidence strengthens confidence in our prevalence estimates and indicates that Peru faces prediabetes challenges similar to neighboring countries undergoing comparable socioeconomic transitions [22].
Inconsistency with DM prevalence findings
Another fundamental issue in our analysis is the inconsistency observed in results related to the prevalence of diabetes, which appears to have increased over time. Notably, this variability reflects the well-documented phenomenon where diabetes prevalence estimates can differ substantially depending on the diagnostic criteria employed, as demonstrated in previous epidemiological studies where the choice between FPG [21, 24], oral glucose tolerance test, and HbA1c significantly influences prevalence determination within identical populations. For example, the Albitres-Flores 2020 study [21], conducted in Tumbes (a region known for its high prevalence of this disease), reported values as high as 10.94% using FPG criteria, 14.17% using OGTT, and 16.97% using HbA1c in the same population, illustrating this diagnostic variability. However, this result might not be representative of the entire country. Nevertheless, the VIANEV [12], a more recent national survey, also found a prevalence of 10.67% at the national level using similar FPG criteria, suggesting an upward trend in the prevalence of diabetes throughout Peru while demonstrating convergence of estimates when standardized diagnostic methods are applied.
On the other hand, the PERUDIAB [5] study reported a prevalence of 6.98%, which could be considered more in line with the national reality, although its scope was not entirely nationwide. This poses a significant dilemma: should we trust the results of VIANEV, a national survey, more, or the findings of PERUDIAB, which, while more specifically focused on diabetes, did not cover the entire country?
Inconsistency with prediabetes prevalence findings
The assessment of prediabetes prevalence in Peru highlighted important methodological considerations that influenced our analytical approach. During the SR process, we encountered prevalence estimates that warranted careful evaluation for epidemiological plausibility and methodological consistency. This experience underscores the complexity of synthesizing evidence from diverse study designs and populations while maintaining scientific rigor.
Two specific cases exemplified these methodological challenges. The VIANEV study reported prediabetes prevalence of 24.5% using FPG criteria of 110–125 mg/dL [12], but preliminary analysis suggested that applying the standard ADA threshold of 100–125 mg/dL could yield estimates approaching 40%. Such values would indicate that nearly half the working-age population has prediabetes, representing an epidemiological scenario that appears inconsistent with established patterns in comparable populations [25]. Similarly, the PERU MIGRANT study demonstrated a 6.5-fold discordance between HbA1c-based prevalence (38.5%) and FPG-based prevalence (5.9%) in identical participants [18], suggesting potential methodological artifacts or population-specific factors requiring further investigation.
Our analytical strategy prioritized epidemiological plausibility and methodological consistency to ensure that pooled estimates would provide meaningful guidance for public health planning. Studies with extreme prevalence values were carefully evaluated, and those with implausible estimates were excluded from primary analyses while being discussed transparently in our methodology. This approach prevented potential overestimation of disease burden that could mislead resource allocation decisions and ensured that our final estimates reflected realistic prevalence ranges consistent with established epidemiological patterns.
The substantial variation in diagnostic approaches and prevalence estimates across studies emphasizes the critical need for standardized methodological protocols in future prediabetes research. Our findings support the importance of consistent application of internationally recognized diagnostic thresholds, comprehensive reporting of study methodology and population characteristics, and careful validation of results within local epidemiological contexts. The final analysis incorporated studies with methodologically robust and epidemiologically coherent findings, providing a reliable evidence base for understanding prediabetes burden in Peru while acknowledging the limitations inherent in the available literature.
Public health implications and policy relevance
This study provides critical epidemiological intelligence that directly informs Peru’s capacity to address DM and prediabetes through evidence-based public health interventions. The pooled prevalence estimates of 7.47% for DM and 10.66% for prediabetes, combined with the documented significant temporal increases, establish these conditions as priority health challenges requiring immediate strategic response. In Peru’s resource-constrained healthcare environment, these findings enable policymakers to quantify disease burden, project future healthcare demands, and allocate limited resources toward interventions with maximum population-level impact.
The demographic patterns identified through our subgroup analyses offer actionable insights for targeted intervention design. The finding that participants ≥ 60 years demonstrate higher and more consistent DM prevalence (5.43% vs. 4.33% in younger adults, I² = 0%) suggests that age-specific screening programs could achieve high diagnostic yield with efficient resource utilization. Similarly, the observation that diagnostic method choice minimally influences prevalence estimates supports the feasibility of implementing standardized FPG-based screening protocols across diverse healthcare settings without compromising detection accuracy.
The substantial prediabetes burden documented in our analysis represents both a challenge and an opportunity for DM prevention at the population level. Evidence-based lifestyle modification programs targeting the identified 10.66% prediabetic population could significantly reduce progression rates to DM, offering cost-effective prevention strategies that align with Peru’s health system capabilities. The temporal trend analysis demonstrating increasing prevalence over time emphasizes the urgency of implementing prevention strategies before disease burden escalates further.
Our findings establish a robust epidemiological foundation for developing Peru’s national DM surveillance and response capacity. The prevalence estimates provide baseline data for monitoring intervention effectiveness, while the identified research gaps highlight priority areas for future epidemiological investigation. This evidence synthesis supports the development of comprehensive DM prevention and management strategies that can adapt to Peru’s demographic transitions and evolving health needs, ultimately strengthening the country’s preparedness to address the growing global burden of metabolic diseases through evidence-informed policy and practice.
Study limitations
One of this study’s main limitations is the diversity of glucose measurement methods and diagnostic criteria used in the analyzed studies. This variability can significantly affect the comparability of results. While some studies use FPG according to ADA criteria, others may use different thresholds, resulting in prevalences that are not directly comparable. This lack of uniformity complicates the interpretation of the true magnitude of DM and prediabetes at the national level.
Another important limitation is the uneven geographical coverage of the studies in the analysis. Many studies focus on urban areas or specific regions such as Tumbes or Lima and may not represent other regions of Peru, especially rural areas, or indigenous communities. This uneven distribution prevents the results from being generalizable to the entire Peruvian population, which could lead to an underestimation or overestimation of the national prevalence.
Most of the studies analyzed date back several years and may not reflect current trends in the prevalence of these metabolic conditions. The lack of more recent data prevents an analysis of the progress or worsening of the situation over time, which is crucial for the effective evaluation of health policies and programs implemented in recent years.
Conclusions
The analysis of the prevalence of DM and prediabetes in Peru reveals a complex situation with significant variations in reported figures over time and across different regions. While the prevalence of DM appears to be increasing, the situation with prediabetes is particularly alarming, with estimates suggesting a large portion of the population is at imminent risk of developing DM. This study highlights the importance of addressing these chronic conditions with well-founded and targeted public health strategies.
To effectively address the rising prevalence of DM and prediabetes in Peru, it is imperative to adopt uniform and standardized diagnostic criteria in all future research. This standardization will enable valid comparisons between studies and a more accurate assessment of public health interventions. Additionally, it is recommended that national studies be conducted that include representations from all regions of the country, both urban and rural, to gain a comprehensive and detailed understanding of the situation. These studies should be complemented by continuous monitoring systems to track disease trends and the effectiveness of implemented policies.
Simultaneously, it is essential to prioritize developing and implementing early detection and prevention programs that promote healthy lifestyles and facilitate access to preventive health services. Such programs should be accompanied by educational and awareness campaigns highlighting the importance of regular glucose level checks, proper nutrition, and regular physical activity. These initiatives must be supported by sustained investment to ensure their long-term impact, aimed not only at reducing the prevalence of these conditions but also at improving the quality of life of the Peruvian population.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
A special thanks to the members of Universidad Nacional Toribio Rodríguez de Mendoza de Amazonas (UNTRM), Amazonas, Peru for their support and contributions throughout the completion of this research.
Author contributions
V.J. V-P: Conceptualization, Investigation, Methodology, Resources, Writing - Original Draft, Writing - Review & Editing. F.E.Z-M: Investigation, Project Administration, Writing - Original Draft, Writing - Review & Editing. L.E.M. V-R: Investigation, Resources, Writing - Original Draft, Writing - Review & Editing. J. A. L-C: Software, Data Curation, Formal Analysis, Writing - Review & Editing. E.V-V: Validation, Visualization, Writing - Original Draft, Writing - Review & Editing. W. R: Methodology, Supervision, Funding Acquisition, Writing - Review & Editing.
Funding
This study was self-funded.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics and consent to participate
Not applicable.
Informed consent
Informed consent was not required for this study.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cho NH, Shaw JE, Karuranga S, Huang Y, Fernandes JD da, Ohlrogge R et al. AW,. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Research and Clinical Practice. 2018;138:271–81. 10.1016/j.diabres.2018.02.023 [DOI] [PubMed]
- 2.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–30. 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vera-Ponce VJ, Vásquez-Romero LEM, Zuzunaga-Montoya FE, Loayza-Castro JA, Hidalgo JRA, De Carrillo CIG. A metabolic epidemic? Prevalence and sex-based disparities of metabolic alterations in the Peruvian population using multiple diagnostic criteria. J Diabetes Metab Disord. 2025;24(1):110. 10.1007/s40200-025-01622-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vásquez-Romero LEM, Zuzunaga-Montoya FE, Loayza-Castro JA, Vigil-Ventura E, Ramos W, Vera-Ponce VJ. Prevalence of obesity according to body mass index, waist circumference, and waist-to-height ratio in peru: A systematic review and meta-analysis. Obes Pillars. 2025;13:100166. 10.1016/j.obpill.2025.100166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seclen SN, Rosas ME, Arias AJ, Huayta E, Medina CA. Prevalence of diabetes and impaired fasting glucose in peru: report from PERUDIAB, a National urban population-based longitudinal study. BMJ Open Diabetes Res Care. 2015;3(1):e000110. 10.1136/bmjdrc-2015-000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: A global systematic review. PharmacoEconomics. 2015;33(8):811–31. 10.1007/s40273-015-0268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Diabetes Association. Economic costs of diabetes In the U.S. In 2017. Diabetes Care. 2018;41(5):917–28. 10.2337/dci18-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vera-Ponce VJ, Zuzunaga-Montoya FE, Vásquez-Romero LEM, Loayza-Castro JA, Sanchez-Tamay NM, De Carrillo CIG. Geospatial analysis and determinant factors of comorbidity presence in patients with diabetes in Peru. Endocr Metabolic Sci. 2025;17:100222. 10.1016/j.endmts.2025.100222. [Google Scholar]
- 9.Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Bärnighausen T, et al. The global economic burden of diabetes in adults aged 20–79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017;5(6):423–30. 10.1016/S2213-8587(17)30097-9. [DOI] [PubMed] [Google Scholar]
- 10.Instituto Nacional de Salud. Encuesta Nacional de indicadores nutricionales, bioquimicos, socioeconomicos y culturales relacionados Con Las enfermedades cronicas degenerativas. Lima, Peru: Instituto Nacional de Salud: Centro Nacional de Alimentacion y Nutricion. 2006. [Google Scholar]
- 11.Miranda JJ, Gilman RH, Smeeth L. Differences in cardiovascular risk factors in rural, urban and rural-to-urban migrants in Peru. Heart. 2011;97(10):787–96. 10.1136/hrt.2010.218537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centro Nacional de Alimentación y Nutrición. Estado nutricional En Adultos de 18 a 59 Años VIANEV 2017–2018. Lima, Peru: Instituto Nacional de Salud; 2021, 191. [Google Scholar]
- 13.Carrillo-Larco R, Bernabé-Ortiz A. Diabetes mellitus Tipo 2 En perú: Una revisión Sistemática sobre La prevalencia e incidencia En Población general. Rev Peru Med Exp Salud Publica. 2019;36(1):26–36. 10.17843/rpmesp.2019.361.4027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13(3):147–53. 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 16.Munn Z, Stern C, Aromataris E, Lockwood C, Jordan Z. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol. 2018;18(1):5. 10.1186/s12874-017-0468-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Diabetes Association. Standards of medical care in Diabetes—2022 abridged for primary care providers. Clin Diabetes. 2022;40(1):10–38. 10.2337/cd22-as01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lazo-Porras M, Ruiz-Alejos A, Miranda JJ, Carrillo-Larco RM, Gilman RH, Smeeth L, et al. Intermediate hyperglycaemia and 10-year mortality in resource-constrained settings: the PERU MIGRANT study. Diabet Med. 2020;37(9):1519–27. 10.1111/dme.14298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schargrodsky H, Hernández-Hernández R, Champagne BM, Silva H, Vinueza R, Silva Ayçaguer LC, et al. CARMELA: assessment of cardiovascular risk in seven Latin American cities. Am J Med. 2008;121(1):58–65. 10.1016/j.amjmed.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 20.Revilla L, López T, Sánchez S, Yasuda M, Sanjinés G. Prevalencia de hipertensión arterial y diabetes En habitantes de Lima y callao, Perú. Revista Peruana De Med Experimental Y Salud Publica. 2014;31(3):437–44. [PubMed] [Google Scholar]
- 21.Albitres-Flores L, Bernabe-Ortiz A. Diagnostic accuracy of ADA 2020 criteria for undiagnosed diabetes in a Peruvian population. Diabetes Res Clin Pract. 2020;169:108475. 10.1016/j.diabres.2020.108475. [DOI] [PubMed] [Google Scholar]
- 22.Bernabé-Ortiz A, Carrillo-Larco RM, Gilman RH, Checkley W, Smeeth L, Miranda JJ, et al. Contribution of modifiable risk factors for hypertension and type-2 diabetes in Peruvian resource-limited settings. J Epidemiol Community Health. 2016;70(1):49–55. 10.1136/jech-2015-205988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vera-Ponce VJ, Loayza-Castro JA, Zuzunaga-Montoya FE, Sanchez-Tamay NM, Bustamante-Rodríguez JC, Valladolid-Sandoval LAM, et al. Prevalence and incidence of prediabetes in Latin america. A systematic review and meta-analysis. J Diabetes Metab Disord. 2025;24(1):25. 10.1007/s40200-024-01549-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vera-Ponce VJ, Zuzunaga-Montoya FE, Loayza-Castro JA, Vasquez-Romero LEM, Paucar CRI, Valladares-Garrido MJ, et al. Concordance and associated factors in diagnostic criteria for prediabetes and diabetes: an analysis of fasting glucose, postprandial glucose, and glycated hemoglobin. J Endocrinol Metabolism. 2024;14(1):48–58. 10.14740/jem.v14i1.919. [Google Scholar]
- 25.Vera-Ponce VJ, Zuzunaga-Montoya FE, Sanchez-Tamay NM, Bustamante-Rodríguez JC, De Carrillo CIG. Incidence rates of prediabetes and diabetes associated with sedentary behavior and night shifts among Peruvian workers (2014–2021). Dialogues Health. 2025;6:100204. 10.1016/j.dialog.2025.100204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.