Abstract
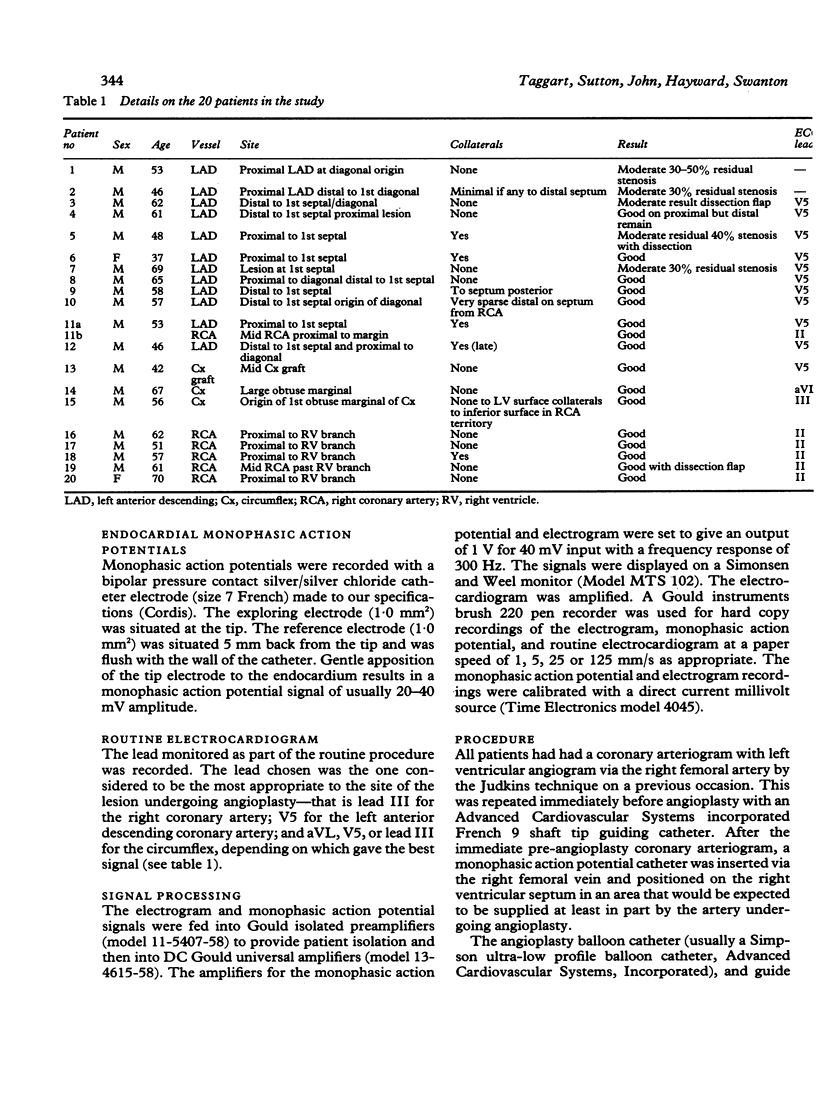
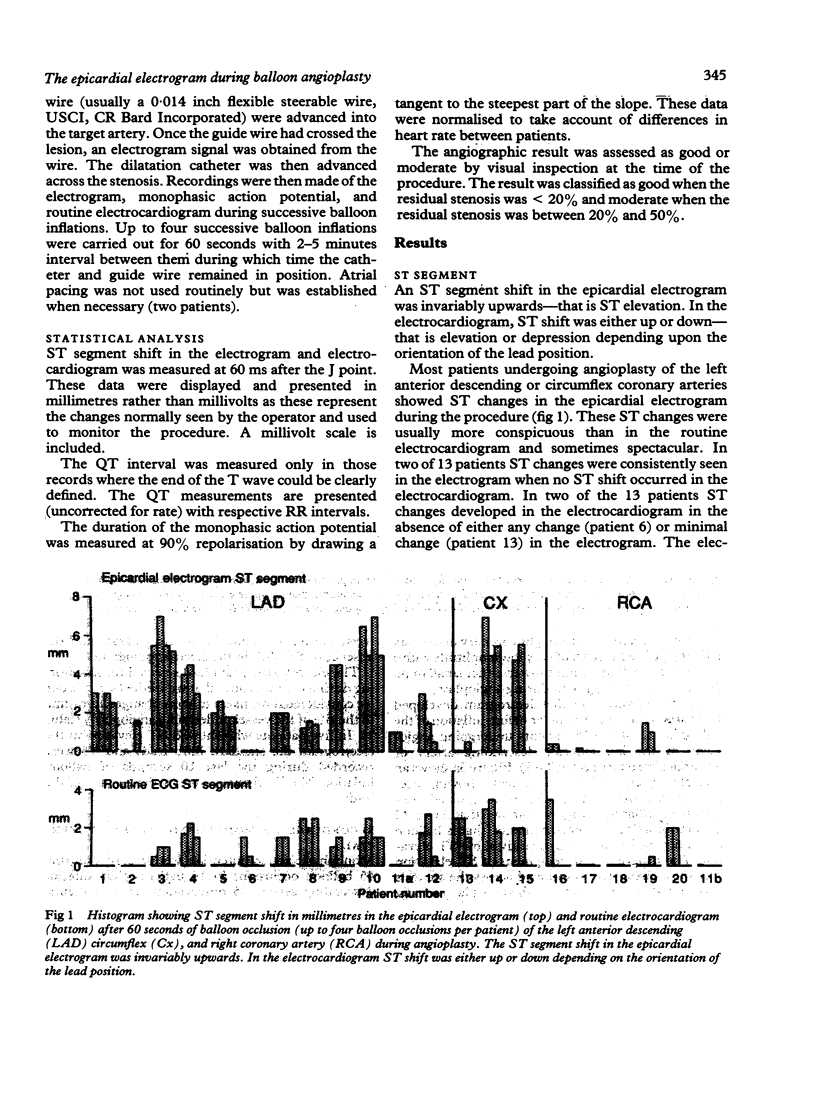
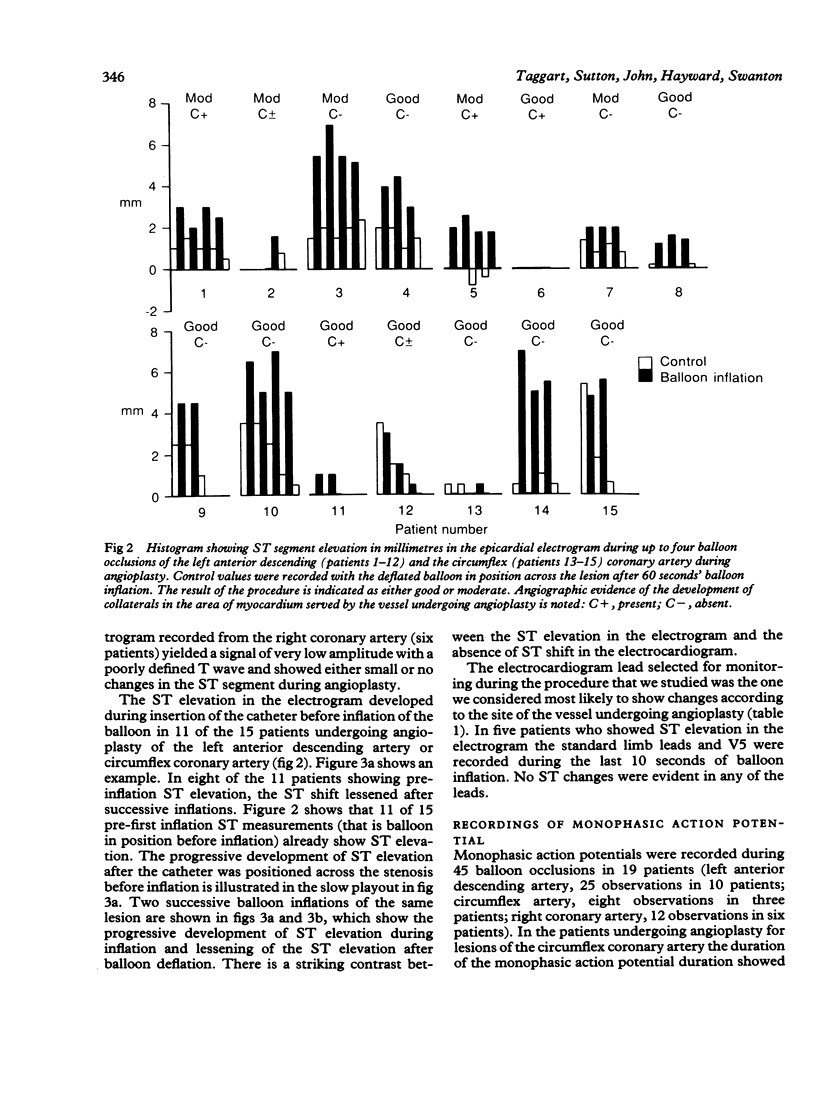
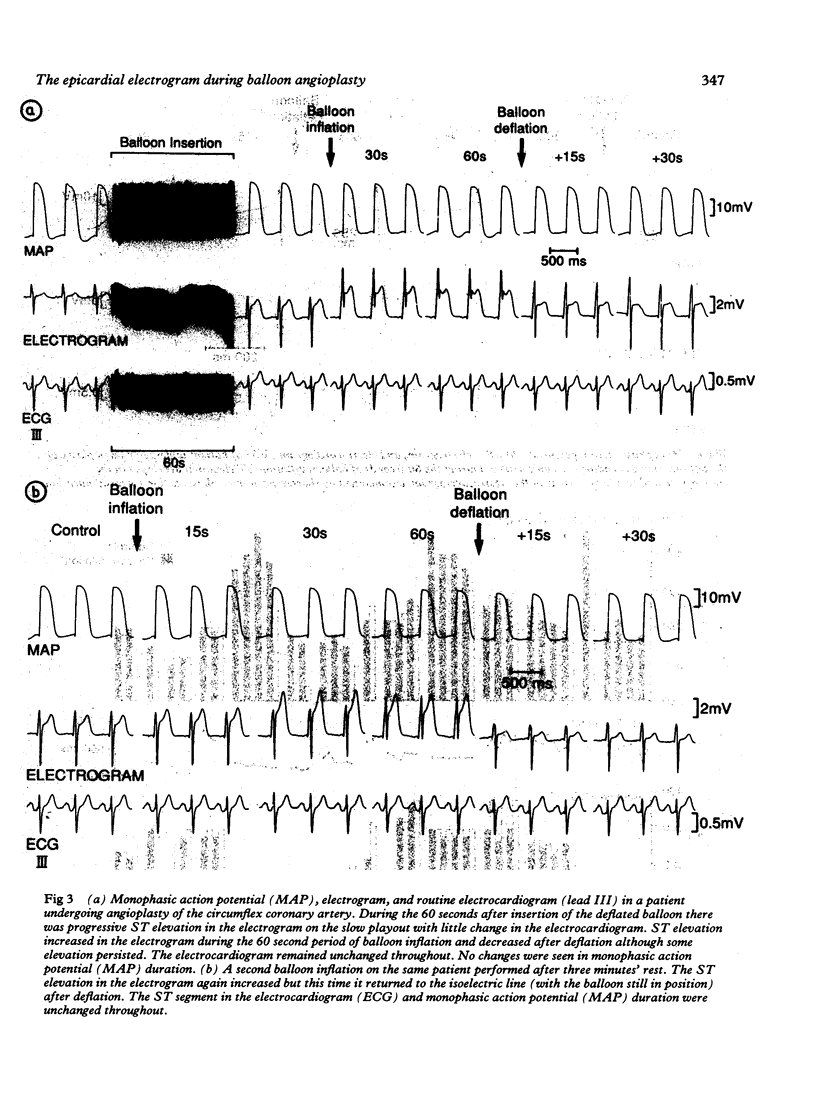
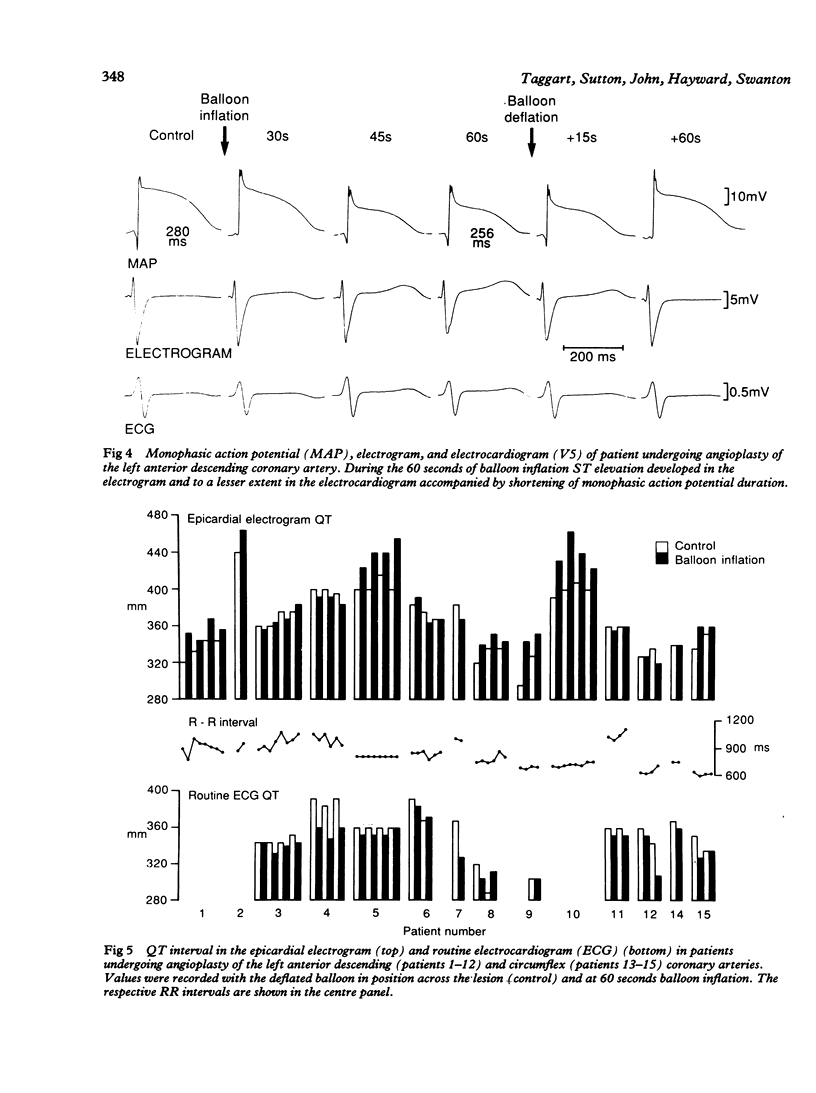
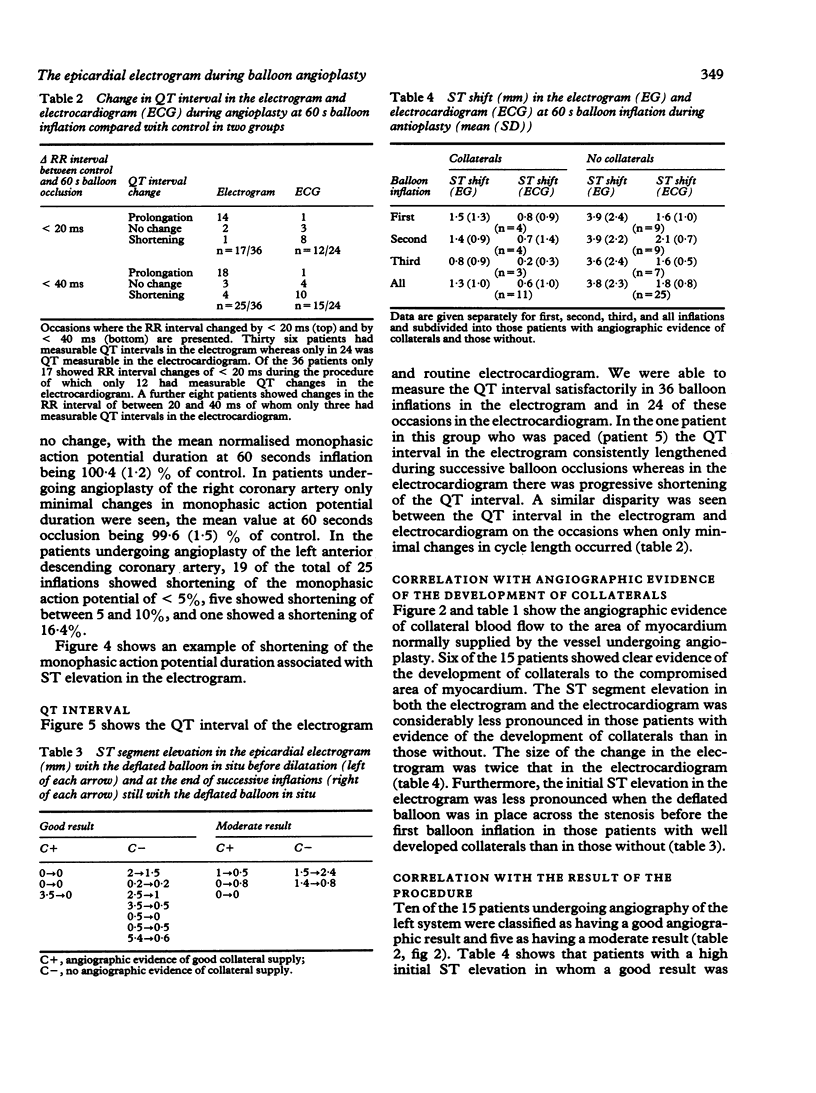
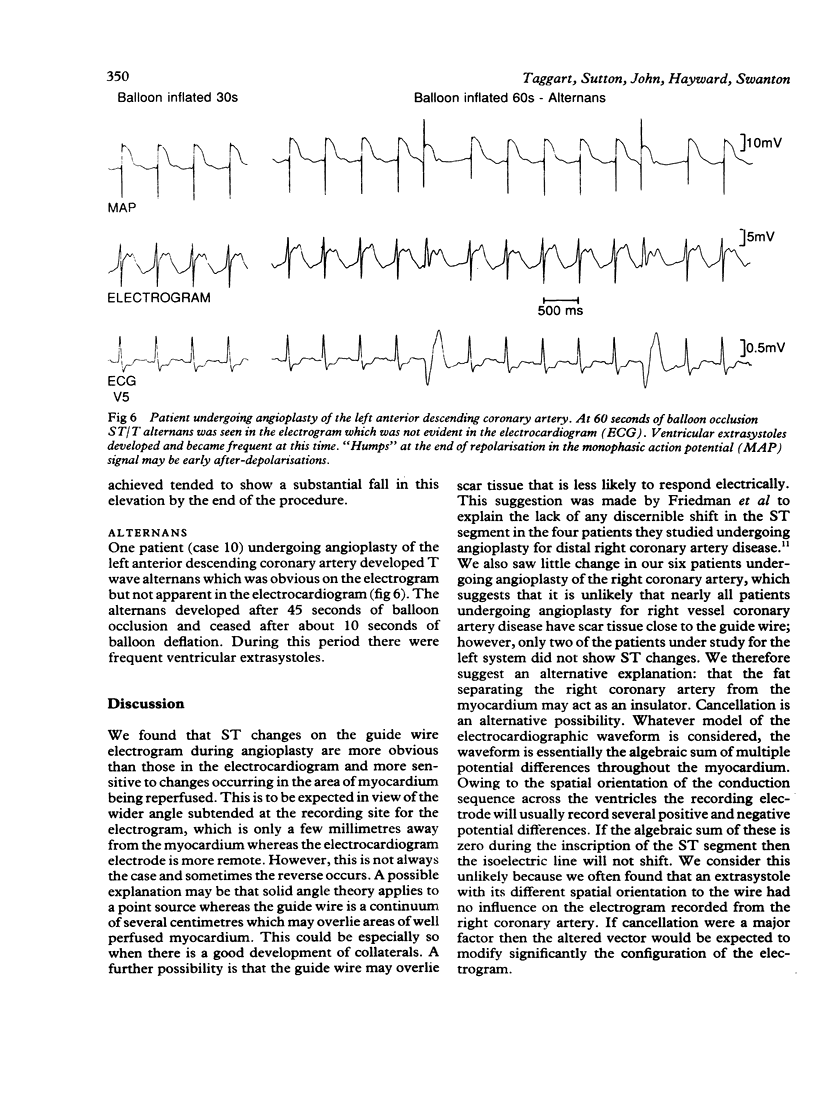
An electrogram was recorded from the angioplasty catheter guide wire when coronary blood flow was interrupted in 20 patients undergoing percutaneous transluminal coronary angioplasty. Monophasic action potentials were recorded from the right ventricular septum together with the routine electrocardiogram. The patients were studied during angioplasty for lesions in the left anterior descending (12), circumflex (3), and right coronary arteries (6). ST elevation in the electrogram recorded in the left anterior descending and circumflex systems was usually more obvious than that in the electrocardiogram. Signals obtained from the right coronary artery were of very low amplitude and registered only minimal ST changes. The ST elevation developed in the electrogram during insertion of the catheter before inflation of the balloon in 11 of the 15 patients undergoing angioplasty of the left system. In eight of the patients showing pre-inflation ST elevation the ST shift lessened after successive inflations. Monophasic action potential recordings were obtained during 45 balloon inflations in 19 patients. In those patients undergoing angioplasty for lesions of the circumflex coronary artery the monophasic action potential showed no change during balloon inflation. In patients undergoing angioplasty for the right coronary artery the mean normalised duration at 60 seconds' occlusion was 99.6 (1.5)% of control. Of a total of 25 occlusions in the patients undergoing angioplasty for the left anterior descending coronary artery 19 showed shortening of less than 5%, five showed shortening between 5 and 10%, and one showed a shortening of 16.4% in the monophasic action potential. The QT interval was satisfactorily measured in the electrogram during 36 balloon inflations, and in 24 of these it was also measured in the electrocardiogram. QT changes in the electrogram tended to be the opposite of those in the electrocardiogram. When changes in RR interval were minimal (less than 20 ms) during the balloon inflation 14 of 17 electrograms showed QT prolongation but only one of 12 electrocardiograms showed prolongation. Conversely one of 17 electrograms showed shortening compared with eight of 12 electrocardiograms. There was angiographic evidence of the development of collaterals in six of 15 patients undergoing angioplasty of the left system. ST segment elevation in both the electrogram and electrocardiogram was less pronounced in these patients than in those without evidence of the development of collaterals. ST segment changes recorded from the angioplasty guide wire provide a more sensitive index of ischaemia than the surface 12 lead electrocardiogram, and fall in ST segments on balloon deflation is a prognostic index of a good angiographic result in the left anterior descending and circumflex arteries, but not in the right coronary artery.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blake K., Clusin W. T., Franz M. R., Smith N. A. Mechanism of depolarization in the ischaemic dog heart: discrepancy between T-Q potentials and potassium accumulation. J Physiol. 1988 Mar;397:307–330. doi: 10.1113/jphysiol.1988.sp017003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne K. F., Zipes D. P., Heger J. J., Prystowsky E. N. Influence of the autonomic nervous system on the Q-T interval in man. Am J Cardiol. 1982 Nov;50(5):1099–1103. doi: 10.1016/0002-9149(82)90425-8. [DOI] [PubMed] [Google Scholar]
- Burchell H. B. Did Einthoven invent a string galvanometer? Br Heart J. 1987 Feb;57(2):190–193. doi: 10.1136/hrt.57.2.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilly S. G., Lab M. J. Electrophysiological alternans and restitution during acute regional ischaemia in myocardium of anaesthetized pig. J Physiol. 1988 Aug;402:315–333. doi: 10.1113/jphysiol.1988.sp017206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson R. M., Taggart P., Bennett J. G., Rickards A. F. Study of electrophysiological ischemic events during coronary angioplasty. Tex Heart Inst J. 1984 Mar;11(1):24–30. [PMC free article] [PubMed] [Google Scholar]
- Franz M. R., Burkhoff D., Spurgeon H., Weisfeldt M. L., Lakatta E. G. In vitro validation of a new cardiac catheter technique for recording monophasic action potentials. Eur Heart J. 1986 Jan;7(1):34–41. doi: 10.1093/oxfordjournals.eurheartj.a061954. [DOI] [PubMed] [Google Scholar]
- Franz M. R., Flaherty J. T., Platia E. V., Bulkley B. H., Weisfeldt M. L. Localization of regional myocardial ischemia by recording of monophasic action potentials. Circulation. 1984 Mar;69(3):593–604. doi: 10.1161/01.cir.69.3.593. [DOI] [PubMed] [Google Scholar]
- Friedman P. L., Shook T. L., Kirshenbaum J. M., Selwyn A. P., Ganz P. Value of the intracoronary electrocardiogram to monitor myocardial ischemia during percutaneous transluminal coronary angioplasty. Circulation. 1986 Aug;74(2):330–339. doi: 10.1161/01.cir.74.2.330. [DOI] [PubMed] [Google Scholar]
- HOFFMAN B. F., CRANEFIELD P. F., LEPESCHKIN E., SURAWICZ B., HERRLICH H. C. Comparison of cardiac monophasic action potentials recorded by intracellular and suction electrodes. Am J Physiol. 1959 Jun;196(6):1297–1301. doi: 10.1152/ajplegacy.1959.196.6.1297. [DOI] [PubMed] [Google Scholar]
- Holland R. P., Arnsdorf M. F. Solid angle theory and the electrocardiogram: physiologic and quantitative interpretations. Prog Cardiovasc Dis. 1977 May-Jun;19(6):431–457. doi: 10.1016/0033-0620(77)90009-3. [DOI] [PubMed] [Google Scholar]
- Krikler D. M. Electrocardiography then and now: where next? Br Heart J. 1987 Feb;57(2):113–117. doi: 10.1136/hrt.57.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lab M. J. Contraction-excitation feedback in myocardium. Physiological basis and clinical relevance. Circ Res. 1982 Jun;50(6):757–766. doi: 10.1161/01.res.50.6.757. [DOI] [PubMed] [Google Scholar]
- Lau C. P., Freedman A. R., Fleming S., Malik M., Camm A. J., Ward D. E. Hysteresis of the ventricular paced QT interval in response to abrupt changes in pacing rate. Cardiovasc Res. 1988 Jan;22(1):67–72. doi: 10.1093/cvr/22.1.67. [DOI] [PubMed] [Google Scholar]
- Lazzara R., el-Sherif N., Scherlag B. J. Early and late effects of coronary artery occlusion on canine Purkinje fibers. Circ Res. 1974 Sep;35(3):391–399. doi: 10.1161/01.res.35.3.391. [DOI] [PubMed] [Google Scholar]
- Meier B., Rutishauser W. Coronary pacing during percutaneous transluminal coronary angioplasty. Circulation. 1985 Mar;71(3):557–561. doi: 10.1161/01.cir.71.3.557. [DOI] [PubMed] [Google Scholar]
- Sarma J. S., Venkataraman K., Samant D. R., Gadgil U. G. Effect of propranolol on the QT intervals of normal individuals during exercise: a new method for studying interventions. Br Heart J. 1988 Nov;60(5):434–439. doi: 10.1136/hrt.60.5.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seed W. A., Noble M. I., Oldershaw P., Wanless R. B., Drake-Holland A. J., Redwood D., Pugh S., Mills C. Relation of human cardiac action potential duration to the interval between beats: implications for the validity of rate corrected QT interval (QTc). Br Heart J. 1987 Jan;57(1):32–37. doi: 10.1136/hrt.57.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spach M. S., Barr R. C., Lanning C. F., Tucek P. C. Origin of body surface QRS and T wave potentials from epicardial potential distributions in the intact chimpanzee. Circulation. 1977 Feb;55(2):268–268. doi: 10.1161/01.cir.55.2.268. [DOI] [PubMed] [Google Scholar]
- Taggart P., Sutton P., Runnalls M., O'Brien W., Donaldson R., Hayward R., Swanton H., Emanuel R., Treasure T. Use of monophasic action potential recordings during routine coronary-artery bypass surgery as an index of localised myocardial ischaemia. Lancet. 1986 Jun 28;1(8496):1462–1465. doi: 10.1016/s0140-6736(86)91500-x. [DOI] [PubMed] [Google Scholar]


