Summary
Electronic health records, biobanks, and wearable biosensors enable the collection of multiple health modalities from many individuals. Access to multimodal health data provides a unique opportunity for genetic studies of complex traits because different modalities relevant to a single physiological system (e.g., circulatory system) encode complementary and overlapping information. We propose a multimodal deep learning method, multimodal representation learning for genetic discovery on low-dimensional embeddings (M-REGLE), for discovering genetic associations from a joint representation of complementary electrophysiological waveform modalities. M-REGLE jointly learns a lower representation (i.e., latent factors) of multimodal physiological waveforms using a convolutional variational autoencoder, performs genome-wide association studies (GWASs) on each latent factor, then combines the results to study the genetics of the underlying system. To validate the advantages of M-REGLE and multimodal learning, we apply it to common cardiovascular modalities (photoplethysmogram [PPG] and electrocardiogram [ECG]) and compare its results to unimodal learning methods in which representations are learned from each data modality separately but are statistically combined for downstream genetic comparison. M-REGLE identifies 19.3% more loci on the 12-lead ECG dataset, 13.0% more loci on the ECG lead I + PPG dataset, and its genetic risk score significantly outperforms the unimodal risk score at predicting cardiac phenotypes, such as atrial fibrillation (Afib), in multiple biobanks.
Keywords: GWAS, AI, multimodal, deep learning, PRS, cardiovascular disease, representation learning, fusion model, variational autoencoder
Graphical abstract
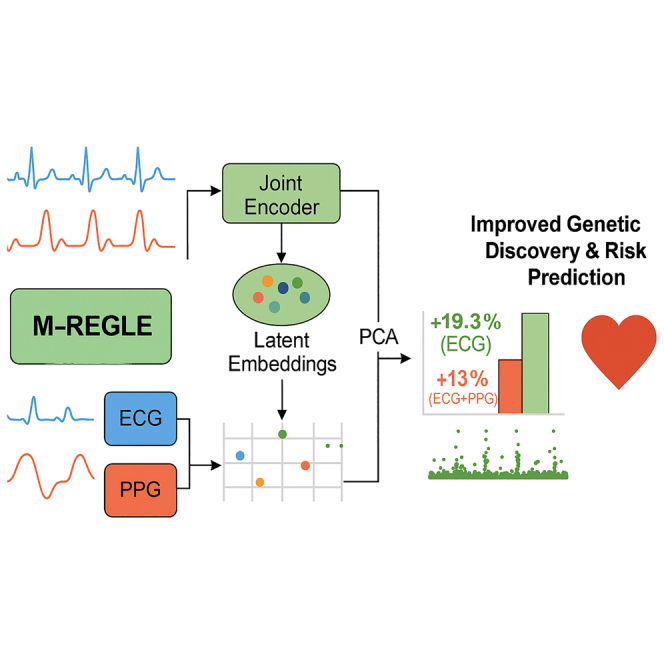
Health data are inherently multimodal; we developed a multimodal AI (M-REGLE) that jointly analyzes complementary physiological waveforms (like ECG and PPG) to enhance genetic discovery for cardiovascular traits. Compared to analyzing waveforms individually, our approach identifies significantly more genetic associations and improves out-of-sample prediction for cardiac conditions, including atrial fibrillation.
Introduction
Health data (e.g., electrocardiograms [ECGs], photoplethysmograms [PPGs], spirograms, magnetic resonance imaging [MRI]) are valuable assets for clinical diagnosis, treatment, and prognosis and provide a unique opportunity for studying the genetic basis of complex traits.1,2,3,4,5,6,7,8,9 Recent technological progress in electronic health record (EHR) systems enables access to multiple health-data modalities per individual.10,11,12 When multiple clinical modalities pertain to a single organ system (e.g., circulatory system) or disease process (e.g., cardiovascular diseases), these modalities may encode complementary information. To maximize information for genetic association analyses, such as genome-wide association studies (GWASs), we propose to extract information from these modalities via a joint representation model. Frequently, the term “multimodal data” is used to refer to different sensory modalities or distinct data types for the same underlying phenomenon. For example, this would include utilizing spirograms, PPG, and ECG in one study. Conversely, “multiview data” is used to refer to data gathered from a single modality from different perspectives, such as different views of MRI (T1-weighted images and T2-weighted images) or different leads of an ECG. Although there is a subtle difference between multimodal and multiview data, in this work, we reference both types as multimodal, as the main objective of this work is to develop an AI model to incorporate multiple data sources.
In the past few years, a large body of work has utilized multimodal learning in medicine and biology. The existing efforts in medicine range from disease progression prediction,13 disease subtyping,14,15 healthcare applications,12 disease diagnoses,16 and recently general medical capabilities utilizing foundation models.17,18,19,20 Furthermore, many biological datasets have utilized multimodal data such as chromatin accessibility, gene expression, protein, and others to improve the biological understanding of cell structure, subpopulations, and physiology.21,22,23,24,25 In this work, we expand these recent efforts into the field of genomics. Recently, a method has been developed to perform GWAS on health data, called representation learning for genetic discovery on low-dimensional embeddings (REGLE).8 REGLE uses convolutional variational autoencoders (VAEs) to compute a non-linear, low-dimensional, uncorrelated embedding of the data without clinical labels. Although REGLE’s performance in genetic analysis and downstream polygenic risk scoring (PRS) surpasses prior methods,8 it is limited to a single data modality. Recent studies have applied unsupervised learning methods to extract embeddings from multimodal data, such as ECG and MRI.26,27 However, there are multiple ways to model multimodal data using unsupervised learning, including different fusion strategies, and prior work has not systematically explored or compared their effectiveness. In our work, we addressed this gap by investigating and comparing different multimodal modeling strategies and showing the benefits of using a joint representation model.
Different clinical modalities can include both complementary and overlapping information. Modeling each modality separately with unimodal representation learning, as in the REGLE framework, does not fully leverage these properties. We hypothesized that jointly modeling multiple complementary modalities would increase signal relative to noise by learning more informative representations, boosting the biological signal, and mitigate noise, thus improving genetic discovery and polygenic risk prediction. Furthermore, the shared information among related modalities is captured more efficiently in the joint embedding space, as opposed to having duplicated information in separate representations for each modality. This reserves more modeling capacity for identifying independent biological signals that are unique to each modality. Incorporating such signals can lead to groundbreaking genetic discoveries.
In this work, we proposed a method, called multimodal REGLE (M-REGLE), where we extended REGLE to incorporate multimodal data. In M-REGLE, we first conducted a test to check whether two modalities contain complementary information. If they do, we jointly learned a lower-dimensional representation (i.e., latent factors) of the multimodal health data (physiological waveforms) using convolutional VAEs28 (i.e., using early fusion), orthogonalized the latent space, performed GWAS on each orthogonalized latent factor, and finally combined them to study the genetics of the underlying system. We validated the advantages of multimodal learning via M-REGLE by comparing it to unimodal learning in which representations were learned on each data modality separately, and downstream analyses were performed on the concatenation of all representations (i.e., late fusion). We call this unimodal REGLE (U-REGLE). Two sets of cardiovascular modalities in the UK Biobank dataset were used in the experiments: 12 leads of ECG as separate modalities and the lead I of ECG and PPG (the modalities prevalent in modern smart watches). In both sets of multimodal data, M-REGLE not only detected more previously unidentified loci but also significantly improved genetic risk scoring for cardiac phenotypes, such as atrial fibrillation (Afib).
Our main contributions are as follows: (1) we utilized 12-lead ECG and PPG data in UK Biobank to demonstrate the utility of multimodal modeling for genetic analysis and PRS. Most of the popular smart wearable devices contain sensors which allow users to record their ECG (equivalent to the lead I ECG) and PPG. Our experiments demonstrated that M-REGLE will enable researchers and users to optimally leverage this rapid acquisition of data for genetic discovery. (2) We observed that M-REGLE improved genomics discovery over existing methods for 12-lead ECG dataset and ECG lead I + PPG dataset for three metrics: Number of loci (19.3% more loci for 12-lead ECG and 13.0% more loci on the ECG lead I + PPG), number of hits (31.0% more loci for 12-lead ECG and 15.7% more loci on the ECG lead I + PPG), and expected chi-squared statistics as measure of power (22.0% higher for 12-lead ECG and 16.4% higher for ECG lead I + PPG). (3) We observed that PRS obtained from M-REGLE for 12-lead ECG significantly outperformed U-REGLE on cardiovascular traits and in particular Afib in UK Biobank. These results were independently validated in Indiana Biobank, EPIC-Norfolk datasets, and British Women’s Heart and Health Study. (4) We observed that M-REGLE improved genomics discovery over U-REGLE for lead I ECG, PPG, and spirograms dataset.
Methods
Overview of M-REGLE
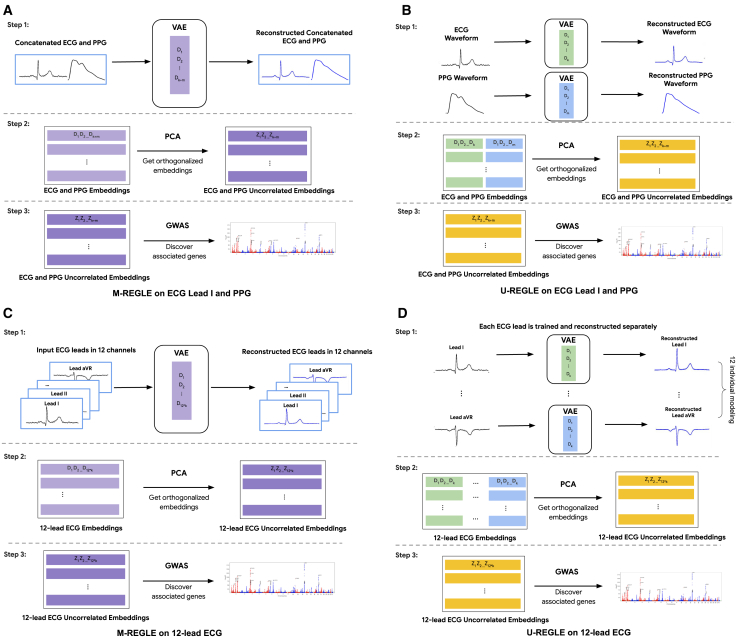
M-REGLE learns the low-dimensional embeddings of multiple modalities in a joint model to improve genetic analyses compared to learning embeddings from each modality individually then combining them for the genetic analyses. It is more effective in the presence of complementary and overlapping information across modalities. There are three steps in M-REGLE: (1) jointly learning a general non-linear, low-dimensional, largely uncorrelated representation from multimodal health data; (2) obtaining completely uncorrelated embeddings by computing principal components (PCs) of the embeddings; and (3) performing GWAS on each PC, combining them, then performing downstream analyses on combined summary statistics (Figure 1A).
Figure 1.
Overview of M-REGLE
(A) M-REGLE steps on lead I ECG and PPG, (B) U-REGLE steps on lead I ECG and PPG, (C) M-REGLE steps on 12-lead ECG, and (D) U-REGLE steps on 12-lead ECG. Step 1 in M-REGLE (A and C) obtains the raw embeddings from multimodal health data in a joint fit while step 1 in U-REGLE (B and D) obtains the raw embeddings for each modality separately. In step 2, to ensure completely uncorrelated embeddings, we applied PCA on the raw embeddings. Lastly, we ran GWAS on the uncorrelated embeddings and combined them.
In the first step, we combined the multimodal health data (e.g., by concatenation), and used the combined data as input to learn a low-dimensional representation by using a VAE. The VAE model contains two parts: an encoder that encodes the input data into lower-dimensional representations, and a decoder, which reconstructs the original data from the representation. During training, the VAE model learned to compress the information from multimodal data into a latent embedding vector with a prior that encouraged the VAE to learn uncorrelated embeddings. We obtained an almost uncorrelated joint representation for the input multimodal data. We observed a phenotypic correlation of for 12-lead ECG (Figure S1) and for ECG lead I + PPG (Figure S2). In the second step, to ensure completely uncorrelated embeddings, we ran PC analysis (PCA) on the VAE embeddings to project them into completely uncorrelated PCs where PCA results are identifiable up to sign indeterminacies (unique eigenvalues) or rotational indeterminacies (repeated eigenvalues). In the final step, the PCs of the multimodal joint embeddings were used as synthetic phenotypes for GWASs. We performed GWASs on each PC of the embeddings for all individuals. We then combined the preliminary GWAS results by summing the chi-squared statistics of each phenotype,29 deriving combined p values, and forming combined hits and loci (Figure 1A). It is worth mentioning that performing PCA on a multivariate outcome then summing the individual chi-squared statistics is a valid test (Table S1) and is equivalent to running the multivariate analysis of variance (MANOVA)29,30 (Table S2). Finally, to obtain a polygenic risk score (PRS), we used elastic net regression to learn a linear combination of the hits. The main difference between M-REGLE and U-REGLE is that M-REGLE learns the embeddings of all modalities in a joint model, while U-REGLE learns the embedding for each modality separately (Figure 1B). In addition to comparing M-REGLE with U-REGLE, we also compared the representations learned by multimodal and unimodal PCA and regular (non-variational) convolutional autoencoders (CAEs).
Data preparation for ECG and PPG waveform
12-lead ECG data were sourced from UK Biobank field 20205. We used the at-rest, median heartbeat (median complex) waveforms. This median complex is the composite of several consecutive complexes that are aligned and of which the median value was taken for each time point of the cardiac cycle. Each median waveform contains 600 points for all leads. The median data are cleaner compared to the raw ECG full waveform; therefore, it did not require extensive preprocessing. The PPG waveform was extracted from UK Biobank field 4205, but, unlike ECG, the PPG data have the median heartbeat waveform. Each PPG waveform contains 100 points, which are median values from single heartbeats. We made two multimodal datasets from the data: (1) 12-lead ECG as 12 different modalities, and (2) lead I of ECG and PPG. For both 12-lead ECG and PPG, we used data instance 2 in UK Biobank, which contains the most overlapping samples. We obtained 50,469 samples for 12-lead ECG and 55,041 samples of PPG as of April 17, 2023.
We first applied finite impulse response filters (FIRs) on all the ECG data to reduce noise. FIR filters are widely used in signal processing for removing unwanted frequency components from a signal. We set the cutoff frequencies to 0.05 and 40. We performed this step on ECG because it contains more noise compared to PPG. For quality control, we calculated several statistics (minimum, maximum, mean, and median) on each waveform and compared them with the statistics of all the other waveforms of the same type. We set a cutoff percentile of 0.1 and 99.9 for each statistic. The waveforms with at least one statistic that fell outside of these cutoffs were dropped. After this step, we had 48,259 samples for the 12-lead ECG and 41,282 samples in the ECG lead I and PPG dataset.
Dataset generation for machine-learning model
For both datasets, we created train/validation/test splits for hyper-parameter tuning, model evaluation, and a final test for the PRS model. We first created the splits by using a static hash on all the available ENCODED IDs (EIDs or participant identifier). Each EID was assigned to one of the training, validation, and test sets. Since we expect a uniform distribution from a hash function, the splits should exhibit the same properties for any feature of interest (e.g., the age of the individuals). The datasets were split by looking up each of the EIDs in the datasets in the created splits. The training, validation, and test dataset contained 70%, 20%, and 10% of the samples, respectively.
In order to standardize the magnitudes of waveforms from different modalities, we proceeded to scale each waveform type, ensuring their values fell approximately within . We calculated the scale factor of each modality separately by picking the 90th percentile of the absolute maximum values of all waveforms of the modality in the training dataset. Therefore, we avoided the impact of outlier waveforms with extreme maximum values. We then applied the scales for each modality on all training, validation, and test datasets by dividing the waveforms with the corresponding scale factor.
Learning 12-lead ECG representations with generative models
Variational autoencoder (VAE) models were trained to learn lower-dimensional representations from 12-lead ECG data. Autoencoders comprise as encoder and decoder function approximators linked by a narrow bottleneck layer, and autoencoders condense input data into a concise set of numbers at the bottleneck layer, with the decoder subsequently reconstructing the input data from this condensed representation.31 VAEs28 represent a distinctive variant of autoencoders, introducing stochasticity into the encoding process. For M-REGLE, one VAE model was trained on the combined 12-lead ECG data to reconstruct the 12 leads together. For U-REGLE, 12 separate VAE models were trained on each ECG lead.
We used similar model structures for M-REGLE and U-REGLE. The encoder of VAE models consists of 1D convolutional layers, each followed by maximum pooling, then fully connected layers to generate the mean and variance of the bottleneck layer. The decoder architecture is a mirror image of the encoder. It starts with fully connected layers, followed by transpose convolutional layers, each prepended by an upsampling layer (supplemental note). For unimodal VAEs, the ECG lead was directly used as one input channel. In M-REGLE, the 12 leads were first stacked to create an input in the shape of 600 points × 12 channels. The VAE models for single lead ECG all had eight latent dimensions. We explored the latent dimension number by performing PCA using various PC numbers on the ECG leads. When we used eight PCs, it explained 0.93 of total variance of the data, demonstrating that eight latent dimensions is sufficient for a linear model to learn good representations from single ECG leads. We used 96 latent dimensions for multimodal VAE so that the total number of dimensions in the unimodal representations and multimodal representations were the same. The standard VAE loss function consisting of the reconstruction loss and the (rescaled) Kullback-Leibler (KL) divergence loss were used as the objective during the training of all the VAE models. The Adam optimizer was used to optimize the objective.
For each of the VAE models, we performed a large-scaled hyper-parameter search independently (Table S3). Each unimodal VAE model was trained for at most 300 epochs. The multimodal VAE models were trained for, at most, 1,200 epochs. Unimodal models needed fewer training epochs to converge due to their smaller model size. We verified that the validation loss curves for all VAE models plateaued within the number of epochs we selected (Figures S3 and S4). We additionally checked that, even if the unimodal models were trained for up to 1,200 epochs, the resulting embeddings had minimal differences from the embeddings obtained after up to 300 epochs (Figures S5–S17). After training, the checkpoints with the lowest validation loss were selected. We also used how uncorrelated the resulting representation coordinates were as a metric to pick the hyper-parameter sets. We calculated the correlation matrix of the representations that the model checkpoint generates on the validation dataset and found the maximum absolute value of the correlation coefficients (among the non-diagonal values of the correlation matrix), which we used as the metrics for the disentangleness of generated representations. To decide which hyper-parameter set to use, we first set a threshold of 0.1 on the maximum absolute correlation value and chose the one with the lowest validation reconstruction loss among all the models that passed the maximum absolute correlation threshold (Table S4). To ensure our models were robust against random seeds, we retrained the selected hyper-parameter combination of every modality and datasetting on 100 different random seeds. The retrained models all reached similar reconstruction loss and overall loss on the validation dataset (Figure S18A).
As a baseline, PCA were trained on each of the ECG 12 leads separately (unimodal PCA) and a combination of ECG 12 leads (multimodal PCA). We used eight PCs for PCA on a single ECG lead and 96 PC numbers for the PCA on joint ECG 12 lead. The learned PCs were used in the same way as the lower representations learned by VAE models in GWAS and downstream analyses.
Learning lead I ECG and PPG representations with generative models
VAE models were trained to learn representations of ECG lead I and PPG. We compared M-REGLE, where we trained one VAE model to reconstruct both waveforms together, and U-REGLE, where we trained two separate VAE models to learn representations of the waveforms independently.
We used the same model structure here as the 12-lead ECG models, which consist of 1D convolution layers and fully connected layers. For unimodal VAEs, the waveform was directly used as a one-channel input. In M-REGLE, we connected each individual’s PPG waveform to their ECG waveform to form a 700-point-long one-channel input (supplemental note). We explored an alternative model architecture of using ECG and PPG (after upsampling) as two input channels, which led to inferior performance (Table S5). We used eight latent dimensions in the unimodal ECG model, four latent dimensions in the unimodal PPG model, and 12 latent dimensions in M-REGLE. We selected the latent dimension numbers by experimenting with different PC numbers.
The training, model-selecting strategy, and the baseline creation of ECG lead I and PPG followed the same procedure as the 12-lead ECG (Tables S3 and S4; Figure S18B).
Similar to the 12-lead ECG setting, we also created baselines using multimodal PCA and unimodal PCA. For multimodal learning, we first concatenated the ECG lead I and PPG waveform and then learned a PCA transformation that reduces the data to 12 dimensions. For unimodal learning, we learned a PCA that generates eight PCs for ECG lead I and a PCA that generates four PCs for PPG.
Learning lead I ECG and PPG and spirogram representations with generative models
To assess the generalizability of our findings across additional modalities, we also applied M-REGLE and U-REGLE to another set of multimodal data: lead I ECG, PPG, and spirogram. For M-REGLE, we first concatenated the three waveforms into a single sequence and trained one VAE model to jointly reconstruct all three modalities. For U-REGLE, we trained separate VAE models on each waveform independently. The ECG lead I and PPG data used are the same as in the previous experiment, and the spirogram data are also sourced from the UK Biobank data field 3066.8 We used the same VAE architecture as in the previous two experiments. For U-REGLE, we used eight latent dimensions for ECG, four for PPG, and three for spirogram. For M-REGLE, we used a total of 15 latent dimensions to match the combined latent dimensionality of the three individual modalities (Figure S35).
GWASs
We generated unimodal representations and multimodal representations for the 12-lead ECG and the ECG lead I + PPG on the combination of the training and validation datasets. We performed PCA on each set of representations of the dataset to transform the representations as uncorrelated coordinates. Then preliminary GWASes were performed on each of the PCs of the representations for each datasetting and modality type using REGENIE.32 All GWASes were adjusted for age, sex, body mass index (BMI), smoking status, genotyping array, and the top 15 genetic PCs.7,8
To get an overall result of genetic discovery on the multimodal waveform data, we combined the preliminary GWASs on the PCs of the representations. We computed the summation of the chi-squared statistics for each GWAS and computed the combined p value by applying the survival function of the combined chi-squared statistics using the number of the phenotypes as the degree of freedom. We utilized the combined chi-squared statistics to obtain the final GWAS result. More specifically, we considered that we had access to phenotypes denoted by that were not correlated and where indicated the chi-squared statistics of i-th SNP for phenotype. As phenotypes were not correlated, we computed chi-squared statistics for all phenotypes and then summed these statistics. The final p value was computed assuming that the summation followed a chi-squared distribution with m degree of freedom .29
GWAS was restricted to individuals with European ancestry to minimize confounding. For quality control, we retained variants with minor allele frequency 0.001, imputation INFO score 0.8, missing call fraction 0.05, and Hardy-Weinberg equilibrium p > 1.0E−10, among all genotyped and imputed variants provided by UK BiobankUK Biobank. Genome-wide significant “hits” were defined as the most significant variants with p < 5.0E−8 and independent at using the PLINK –clump command. A reference panel for linkage disequilibrium (LD) calculation contained 10,000 unrelated European samples from the UK Biobank. Significant “loci” were created based on the span of reference panel SNPs in LD (R2 0.1) with the hits. Loci separated by fewer than 250 kb were subsequently merged.
GWAS Catalog loci replication
The number of hits and loci may be misleading because some of them might be false positives. However, if the hits/loci are known to be related to ECG or PPG traits, they are less likely to be false positive. We investigated relevant hits/loci by examining whether they are previously reported in the literature to be ECG or PPG related. We performed a GWAS Catalog search using key words (case insensitive), such as “electrocardio,” “ecg,” “pr interval,” “ventricular rate,” “pulse wave,” and “notch position,” (Table S6).
GWAS power analysis via expected chi-squared statistics
We compared the GWAS power of M-REGLE and U-REGLE in terms of the high-quality hits by calculating the mean of the chi-squared stats of all the rediscovered hits (i.e., the ones with support by GWAS Catalog) from the GWAS of each modality and datasetting.
Simulated data for statistical power comparison
Comparing PCA-based combined Chi-squared statistics and MANOVA
We performed a series of simulations to illustrate that PCA model power is equivalent to MANOVA. We simulated 10 factors using the following model:
is the i-th factor, X is the set of variants (e.g., SNPs), and models the environment or measurement noise. is a vector of effect size where the first value is 0.001 (model alternative) and the rest are 0 (model null) and . Diagonal values of are set to 1 and off-diagonal are set to . We compare three models: naive model where we test each factor independently and then sum the chi square, PCA model where we perform PCA on each factor and then sum the chi square, and finally MANOVA. We computed type I error and power for all three models when we set to 0, 0.2, and 0.3 (Tables S1 and S2).
Simulated data for models with similar phenotype prediction and different statistical power
It is possible for two models to have very similar phenotype prediction while one has better GWAS power as it better captures the genetic signal. For simplicity of this toy example we assume we perform PCA. We assume the following generative model for our data modalities:
and the phenotype of interest is generated as follows:
where has two factors (i.e., non-genetic factors) and we have two data modalities ( and ). Both data modalities are generated from the F factors and (i.e., genetic factor), while the factors capture the main signal of both modalities. Thus, in the U-style model with four total dimensions, the model learns the primary F factors from both modalities, leading to an overall U-style embedding of [F, F] that has no component. In contrast, the M-style model can use just two dimensions to learn the contribution of F to both modalities, leading to an overall M-style embedding of [F, s]. Correlation of phenotype prediction between the models may remain very close given the strong contribution of F to phenotype; however, the M-style model will yield better genetic analysis and PRS prediction.
Functional enrichment using GREAT
Genomic Regions Enrichment of Annotations Tool (GREAT) enrichment analyses were performed on the human GRCh37 assembly using GREAT v4.0.433 using program defaults. Terms were considered statistically significant if the Bonferroni-corrected p values for both the region-based and gene-based tests were 0.05. Cardiovascular terms were identified by performing a case-insensitive match on enriched ontology term descriptions using the regular expression “cardiac cardio cardial heart circulatory.” Paired t tests were performed on -transformed raw region-based p values for statistically significant cardiovascular terms.
Creating PRSs from significant hits
To evaluate the improvement of one model over another (e.g., M-REGLE vs. U-REGLE), we utilized phenotypic prediction as a measure of comparison. We created PRSs from the significant hits obtained for each model by training an ElasticNet model. The significant hits reported by each model were used as features for ElasticNet, with the prediction target set as the phenotype of interest (e.g., Afib). The same training set that was used to train M-REGLE was used to fit ElasticNet and we performed 5-fold cross-validation to find the right hyperparameters. We applied sklearn.linear_model.ElasticNet to train our ElasticNet and performed a hyper-parameter search of l1_ratio over [0.1, 0.5, 0.7, 0.9, 0.95, 0.99, 1.0] values.
All the PRS values reported in the UK Biobank were obtained from the test dataset. Furthermore, we shared the variant weights derived from significant hits in the UK Biobank with our collaborators for assessment on the EPIC-Norfolk34 and Indiana Biobank datasets.35 Our collaborators assessed PRS across the phenotypic data available to them. Consequently, we obtained phenotype-prediction results for the Afib phenotype in the Indiana Biobank dataset,35 while, in the EPIC-Norfolk dataset, we obtained results for Afib, PPG pulse rate, and systolic blood pressure (SBP).
PRS validation on multiple datasets
Indiana Biobank dataset
Indiana Biobank samples were genotyped using Illumina Infinium Global Screening Array (GSA, Illumina, San Diego, CA) by Regeneron (Tarrytown, NY). Variants with palindromic alleles, missing rate >5%, minor allele frequency (MAF) <3%, and Hardy-Weinberg equilibrium P < 1E−4 were excluded. PCs of population stratification were calculated using Eigenstrat.36 Based on the first two PCs, those clustered with the European reference samples from the 1000 Genomes Project37 were grouped as European samples and they were used in this study (N = 4,030). Indiana Biobank samples were imputed using the Michigan Imputation Server38 with the 1000 Genomes project as the reference panel. Variants with imputation INFO < 0.3 or MAF < 0.01 were excluded. PRS were calculated by using imputation dosages. Afib cases (n = 778) were determined based on International Classification of Diseases (ICD-9) (427.3, 427.31, and 427.32) and ICD-10 (I48.0, I48.1, I48.2, and I48.9) codes. Those not having Afib in their electronic health records were considered as controls (n = 3,252).
EPIC-Norfolk dataset
Genotyping in EPIC-Norfolk used the Affymetrix UK Biobank Axiom Array with the Axiom GT1 algorithm used for calling. Quality-control exclusions were made for variants with Hardy-Weinberg P < 1.0E−6 and checks made for abnormal clustering or plate batch effect. Samples were excluded for SNP call rate <97% with further checks for heterozygosity and gender. Imputation was performed by the Sanger Imputation Service using the IMPUTE4 software and Haplotype Reference Consortium and UK10K plus 1000 Genomes phase 3 reference panels. Variants with a genotyping quality score (INFO) <0.4 were excluded. Afib (n = 3,554) was ascertained using Hospital Episode Statistics (HES) records maintained in a database containing medical records for all UK National Health Service (NHS) hospitals. Linkage to cohort participants used the unique NHS number. Cases were defined as ICD-10 I48.0, I48.1, I48.2, I48.9, or I48 unspecified (coded as I48X). Controls (n = 18,002) were defined as non-cases with available GWASs.
British Women’s Heart and Health Study
The British Women’s Heart and Health Study (BWHHS) utilized genotyping techniques employed in the Human Cardiovascular Disease (HumanCVD) BeadChip, also known as the ITMAT-Broad-CARe (IBC) v2 array. This array contained up to 49,240 SNPs. To ensure the reliability of the data, rigorous quality-control measures were implemented. All SNPs were clustered into genotypes via Illumina Beadstudio software and stringent quality-control filters were applied at both the sample and SNP level. Samples failing to meet criteria, including individual call rates below 90%, gender mismatches, and duplicate discordance, were excluded. Similarly, SNPs with call rates below 95% or exhibiting Hardy-Weinberg disequilibrium with a p < 1.0E–6 were removed. Furthermore, to capture low-frequency variants of significant effect across the extensive dataset, filtering was conducted based on an MAF threshold of less than 0.01. Incidence cases of Afib were identified through general practitioner (GP) information provided during BWHHS record reviews. Additionally, prevalent Afib cases were identified through ECG diagnosis, ensuring a comprehensive assessment of Afib prevalence within the study population.
Statistical tests for performance metrics
To assess the performance of phenotype-prediction and PRS models, we applied nonparametric bootstrapping. We created 100 bootstrap samples by randomly resampling the target dataset with replacement. We calculated the target metrics for each sample and reported the mean and standard error of the resulting distribution. To assess whether the performance difference between two models was statistically significant, we used paired nonparametric bootstrapping. For each of the 100 bootstrap samples, we calculated the difference of the target metrics by the two models. We reported that the first model had a significantly larger metric value than the second if the mean differences were positive and the confidence interval did not include zero. In contrast, the second model was reported to have significantly larger metric value if the mean difference was negative and the confidence interval did not include zero. However, if the confidence interval overlapped with zero, we concluded that the difference between the models was not statistically significant.
Results
Overview of cardiovascular modalities
We used the ECG and PPG health data in UK Biobank to define two multimodal tasks. Although both ECG and PPG are electrophysiological waveforms and are often analyzed together in healthcare settings, different sensor technologies are utilized to measure different physiological quantities: PPG employs optical sensors to detect volumetric changes in blood flow, while ECG relies on electrical sensors to measure the heart’s electrical activity. Therefore, we considered them as distinct data modalities in this work. First, we used the at-rest, median complex ECG waveforms from UK Biobank. This median complex is the composite of several consecutive complexes that are aligned and of which the median value was taken for each time point of the cardiac cycle. Second, we extracted median heartbeat PPG waveforms from UK Biobank. We studied two multimodal tasks: (1) 12-lead ECG at rest, where the leads form 12 different modalities; and (2) ECG lead I plus PPG (which are available in modern smartwatches). After performing quality control on the data, we created train, validation, and test splits for model training, hyper-parameter tuning and model evaluation, and PRS model evaluation, respectively (Figures S19 and S20). Overall, the training, validation, and test datasets contain 70%, 20%, and 10% of samples, and each dataset has similar phenotypic distributions (Figure S21; Table S7).
Multimodal training is more effective in the presence of complementary information across modalities. To understand signal overlap and whether jointly learning embeddings is helpful, we performed canonical-correlation analysis (CCA) to identify and measure the associations between the modalities. This measure ranges between 0 for no overlap and 1 for complete overlap. First, we performed both CCA and deep CCA (DCCA) to compute the maximum projected correlation between each pair of the 12 leads of ECG. We observed that, while some pairs have extremely high mapped correlation (e.g., 0.98 0.01 correlation between contiguous leads V5 and V6), other leads have lower correlation and thus contain complementary information (e.g., 0.62 0.01 correlation between limb lead III and precordial lead V2). Next, we analyzed ECG lead I plus PPG and observed a modest correlation, indicative of complementary signals (0.43 0.01) (Table S8). As a reference point, we observed that the spirogram data—a measure of lung function—in UK Biobank7,8 have a lower projected correlation with lead I ECG (0.29 0.03) and PPG (0.37 0.03). It is worth noting that we do expect to see some non-zero correlation as health data capture general health information of individuals such as age, sex, and BMI. Lastly, we observed a similar pattern when we utilized DCCA,39 which relaxes the linear assumption in CCA (Figure S22; Table S8) and when we utilized dynamic time warping (Figure S23).
M-REGLE produces better learned representations
When modalities have complementary and overlapping information, multimodal learning is expected to use the latent coordinates more effectively and thus produce better representations. One way to quantify a better representation is to have a lower overall reconstruction error, given a fixed latent dimension. We verified this hypothesis by applying step 1 of M-REGLE and U-REGLE (i.e., jointly or separately learn representations from multimodal data) to both 12-lead ECG and lead I ECG and PPG tasks and compared the reconstruction results.
We observed that M-REGLE reduced reconstruction error compared to U-REGLE on the validation set of the 12-lead ECG task. For M-REGLE, all the modalities needed to be combined as one input. We stacked the 12-lead waveforms as 12 channels (i.e., similar to the three channels of a color image). Then we trained a VAE model with 96 latent dimensions on the training data to reconstruct the 12-lead waveforms all together. For U-REGLE, we trained a VAE model independently on each ECG lead, getting 12 different VAE models. Each VAE had eight latent dimensions. In total each sample had latent dimensions, the same number as M-REGLE. We compared the mean squared error (MSE) of the reconstructed 12-leads ECG by M-REGLE with the average MSE of the 12 ECG leads reconstructed by U-REGLE (which makes them comparable). M-REGLE reduced the overall MSE by . The lower MSEs of M-REGLE were achieved consistently against different random seeds that were used in model training (Figure S18A). We observed the same trend across different numbers of latent dimensions. While both M-REGLE and U-REGLE showed decreasing reconstruction loss as latent dimensions increased, they eventually reached a point of diminishing returns. At this stage, U-REGLE failed to recover all the signals that M-REGLE captured (Figure 2A; Table S9). In addition, we compared multimodal PCA and CAE with unimodal PCA and CAE and the same trend was observed (Figure S24; Tables S10 and S11).
Figure 2.
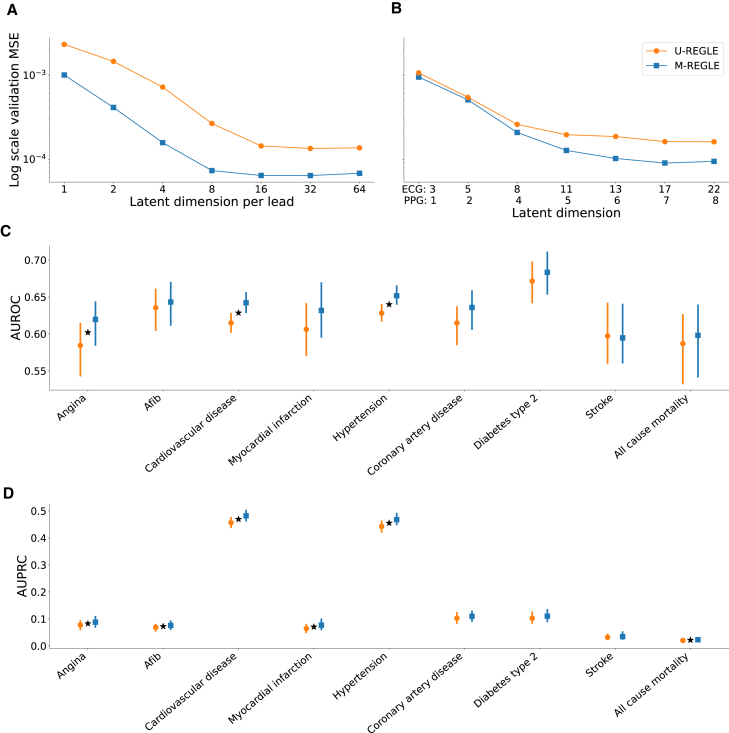
M-REGLE embeddings improve cardiovascular trait prediction
(A) Validation reconstruction losses in log scale of U-REGLE and M-REGLE on 12-lead ECG data. The x axis is the numbers of latent dimensions (1, 2, 4, 8, 16, 32, 64) per ECG lead. Standard errors (SEs) are too small to plot (see Table S9 for values of reconstruction losses and SEs. See Figure S25 for the normal scaled reconstruction loss plots.).
(B) Validation reconstruction losses in log scale of M-REGLE and U-REGLE across numbers of latent dimensions on lead I ECG and PPG data. The x axis is the numbers of latent dimensions used for each modality (see Table S13 for values of M-REGLE and U-REGLE reconstruction losses and SEs). All the difference between M-REGLE and U-REGLE in (A) and (B) are significant.
(C) AUROC prediction of nine phenotypes utilizing ElasticNet trained on the 12 embeddings obtained from ECG lead I and PPG.
(D) AUPRC prediction of nine phenotypes utilizing ElasticNet trained on the 12 embeddings obtained from ECG lead I and PPG.
Star sign indicates a statistically significant difference between the two methods using paired bootstrapping (100 repetitions) with 95% confidence.
The hypothesis was also verified on the lead I ECG and PPG task. We applied M-REGLE on ECG lead I and PPG. To combine the two modalities, we concatenated ECG and PPG waveforms to form a long one-channel input. We then trained a VAE model that learns to reconstruct the concatenated ECG and PPG waveforms. The VAE model generated 12 latent dimensions from the concatenated ECG and PPG waveforms. In U-REGLE, we trained a VAE model for each modality independently. We used eight latent dimensions in the ECG VAE model and four latent dimensions in the PPG VAE model. We assigned more dimensions to ECG, since ECG is more complex (Table S12), and we observed comparable variance explained ratios in PCA when using eight and four as PC numbers for ECG and PPG. We compared the overall reconstruction loss of M-REGLE with the weighted average of the U-REGLE reconstruction losses (weighted by the waveform lengths; see section “methods”). M-REGLE achieved lower overall reconstruction loss compared to U-REGLE, and this performance was robust against random seeds that models were trained on (Figure S18B). This reduction is lower compared to 12-lead ECG (72.5% vs. 20.23%), possibly due to the lower observed correlation between lead I ECG and PPG compared to 12-lead ECG, as computed using CCA. We hypothesize that, when more complementary information is available, the gap will be larger between M-REGLE and U-REGLE reconstruction. We observed the same trend for different numbers of latent dimensions in VAE and different methods such as PCA and CAE (Figures 2B, S24, and S25; Tables S13–S15).
M-REGLE embeddings improve cardiovascular trait prediction over U-REGLE on ECG + PPG dataset
To understand the M-REGLE embeddings, we computed the phenotypic correlation between M-REGLE embeddings obtained from the 12-lead ECG and lead I plus PPG with 10,602 UK Biobank phenotypes. Since these embeddings are highly associated with covariates age, sex, height, BMI, and smoking status, we first removed (residualized up to second-order polynomial) the effect of these covariates from M-REGLE embeddings prior to computing the phenotypic correlation. We observed that 1,989 out of all combinations of M-REGLE embeddings by phenotype pairs (10,602 phenotypes and 108 embeddings from 12-lead ECG and lead I ECG and PPG) had significant correlations after Bonferroni correction.These correlations included very strong phenotypic correlations between M-REGLE embeddings and cardiac phenotypes indicating M-REGLE embeddings captured considerable cardiovascular information. Examples of these phenotypes were position of the pulse wave peak (R = −0.69; p < 1.6E−300) with second embedding of PPG and ECG lead I, ventricular rate (R = 0.50; p < 1.77E−232) with seventh embedding of PPG and ECG lead I, R axis (R = −0.50; p < 3.25E−232) with 96th embedding of 12-lead ECG, QT interval (R = −0.42; p < 9.43E−158) with fourth embedding of PPG and ECG lead I, QRS num (R = 0.37; p < 3.80E−121) with seventh embedding of PPG and ECG lead I, Pulse rate (R = 0.36; p < 1.59E−118) with fourth embedding of PPG and ECG lead I, and heart rate during PWA (R = 0.36; p < 9.86E−117) with seventh embedding of PPG and ECG lead I (Table S16).
To further investigate the correlation between M-REGLE embeddings and other phenotypes, we fitted single-task elastic net models on M-REGLE embeddings to predict nine cardiovascular disease phenotypes in UK Biobank (Table S17). We used the 12 M-REGLE embeddings obtained from lead I ECG and PPG. We observed that, for the lead I ECG plus PPG embeddings, M-REGLE outperformed or matched U-REGLE in area under receiver operating curve (AUROC) and area under precision-recall curve (AUPRC) across all nine phenotypes (Figures 2C and 2D; Tables S18–S21). Based on a paired bootstrap analysis, M-REGLE was significantly better than U-REGLE, in terms of AUROC, for predicting hypertension, cardiovascular disease, and ever smoking, while M-REGLE was significantly better than U-REGLE, in terms of AUPRC, for predicting for Afib, cardiovascular disease, myocardial infarction, hypertension, and all-cause mortality. Although M-REGLE embeddings are created in an unsupervised manner, making them agnostic to any particular disease condition, these embeddings are nonetheless predictive of cardiovascular disease phenotypes. There are multiple established predictors or risk factors for cardiovascular disease, including age, sex, obesity, metabolic panel such as lipid, activity, and socioeconomic factors.40,41 We investigated whether M-REGLE embeddings provide additional and complementary information to these known features (289 features; Table S22). We compared known features prediction with M-REGLE embeddings plus known features and observed in all cases including M-REGLE embedding obtained from 12-lead ECG or lead I ECG and PPG outperform known features alone (Tables S23–S27).
Finally, we observed modest associations between cardiovascular medications and M-REGLE 12-lead ECG embeddings and PPG + ECG embeddings as shown in Table S28 and Figures S26–S28. These results indicated that M-REGLE embeddings, which are learned in an unsupervised and disease-agnostic fashion, can capture information concerning disease and medication status. Note that no causal interpretation should be ascribed to these associations.
Interpretability of M-REGLE embeddings
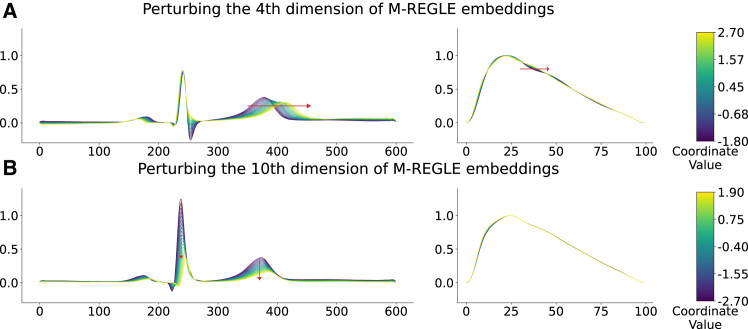
To examine the association between M-REGLE embeddings and cardiac traits, we investigated how perturbing individual embedding coordinates affects the decoded waveforms. Specifically, we identified coordinates that best differentiate samples labeled as Afib from those without Afib by analyzing the distribution of each coordinate in healthy and unhealthy samples. Dimensions 4, 6, and 10 emerged as the most distinctive. To assess the impact of these dimensions, we selected M-REGLE embedding pairs of one healthy sample and one unhealthy sample, where they were maximally separated along a single distinctive coordinate (4, 6, or 10) while remaining similar across all other dimensions. We then interpolated between these embeddings in 20 evenly spaced steps along the distinctive coordinate and decoded each step using the M-REGLE VAE model. The resulting waveforms were analyzed to determine physiological changes.
Our findings indicate that the fourth dimension is associated with the QT interval in ECG signals and the presence of a PPG notch. As the embedding transitioned from healthy to unhealthy along this dimension, the decoded ECG exhibited a prolonged QT interval, while the PPG notch disappeared (Figure 3A). Similarly, the 10th dimension is linked to ECG amplitude, with a progressive decrease in amplitude as the embedding shifted from healthy to unhealthy along this axis (Figure 3B).We validated these findings using an “average” M-REGLE embedding, where all coordinates were set to 0 (the mean value of the VAE prior). Next, we perturbed the 4th and 10th dimensions by varying their values between −2 and 2, corresponding to two standard deviations of the VAE prior. The decoded waveform showed the same effects from the two dimensions as our observations above (Figure S29).
Figure 3.
The effect of perturbing distinctive M-REGLE embedding dimensions on decoded ECG and PPG waveforms from a healthy toward an unhealthy sample
(A) The impact of the fourth dimension. As the embedding transitions from healthy to unhealthy, the decoded ECG (left) exhibits a prolonged QT interval, while the PPG (right) loses its notch.
(B) The impact of the 10th dimension. A shift from healthy to unhealthy along this dimension results in a progressive decrease in ECG amplitude.
M-REGLE on 12-lead ECG enhances genetic discovery
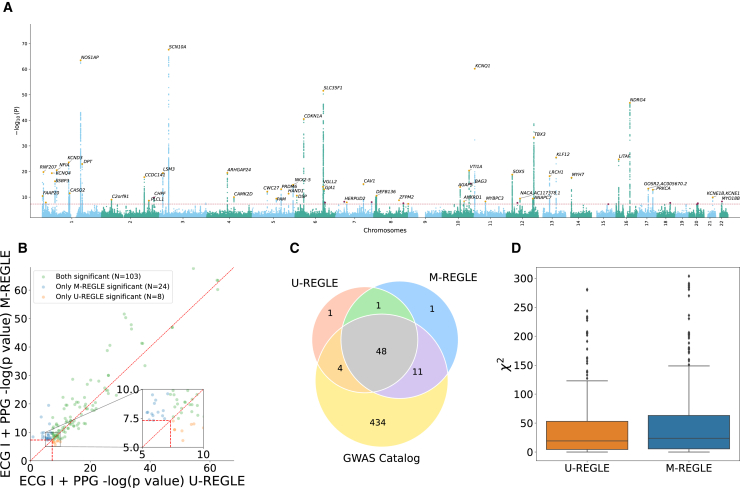
We compared the genetic discovery performance of M-REGLE with U-REGLE on the combined training and validation set (n = 38,697). M-REGLE generated 96 dimensional representations for each individual and then PCA was performed to project the raw embeddings into 96 uncorrelated PCs (i.e., there was no loss of information and this was done for orthogonalization). We performed GWAS on each of the 96 PCs using REGENIE32 (Table S29). As the 96 PCs were uncorrelated, we combined these 96 GWASs by summing the chi-squared statistics and computed the final combined p value from this summation by choosing 96 degrees of freedom.29 We observed similar genomics inflation of combined p value for M-REGLE and U-REGLE (Figures S30 and S31). We used the combined p values to create the hits and loci (see section “methods”). Hits were independent genome-wide significant (GWS) variants ( and ) and loci were obtained by merging hits within 250 kb together (Figure 4A).
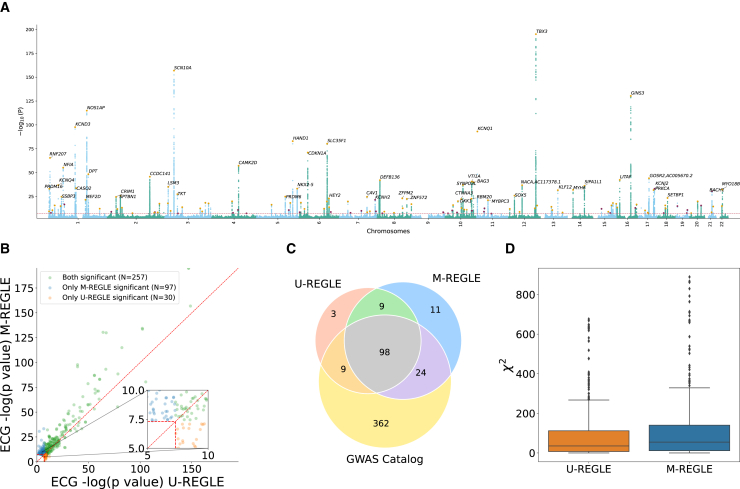
Figure 4.
M-REGLE on 12 ECG leads increases genomic discovery
(A and B) (A) Manhattan plot depicting M-REGLE GWAS p values for all 22 autosomal chromosomes. Black gene names indicate the closest gene for each locus with . Purple dots denote the GWS loci uniquely detected by M-REGLE. Orange dots indicate loci also identified in U-REGLE. (B) Comparison of M-REGLE GWS variants in hits with U-REGLE. The x axis is the p value of U-REGLE. The y axis is the p value of the M-REGLE. All p values in (A) and (B) are computed by summing the chi-squared statistics for all 96 embeddings to perform a single joint chi-squared test. The vertical and horizontal red lines indicate the GWS level. The diagonal red line indicates . The orange dots indicate variants in hits that are significant for U-REGLE but not significant for our M-REGLE and green dots indicate variants in hits that are significant for our M-REGLE but not significant for U-REGLE.
(C) A three-way Venn diagram of the GWAS Catalog loci, loci discovered by M-REGLE, and loci discovered by U-REGLE.
(D) Comparison of the chi-squared statistics for all known significant variants in GWAS Catalog for both U-REGLE and M-REGLE. The difference is statistically significant.
M-REGLE had higher strength of association compared to U-REGLE (Figure 4B; Table S30) where M-REGLE discovered 262 hits (62 more than U-REGLE) and 142 loci (23 more than U-REGLE) (Figure 4C; Table S31). To compare our results with known loci previously detected for ECG and cardiovascular traits (Table S6), we compiled all 989 ECG-related trait hits and 498 loci from the GWAS Catalog. From 262 hits and 142 loci discovered by M-REGLE, 231 (88.5%) hits and 122 loci (85.92%) were previously reported (Figure 3C; Table S32) leaving 20 loci genome-wide not previously associated with these traits. Lastly, we observed that 11 out of 20 loci are unique to M-REGLE compared to U-REGLE (Figure 4C). To further validate these additional loci, we observed that 9 out of 11 loci have been detected for cardiovascular traits in Open Targets42,43 (Table S33). To compare GWAS statistical power, we calculated the expected chi-squared statistics on all the variants reported as ECG-related traits in GWAS Catalog. We observed that M-REGLE had higher statistical power than U-REGLE ( vs. ) (Figure 4D; Table S32).
As a secondary analysis, we used PCA and CAE in multimodal and unimodal settings to obtain latent representations. We observed similar results where multimodal learning led to better genetics discovery and higher statistical power. Multimodal PCA discovered 215 hits and 122 loci, while unimodal PCA found 167 hits and 104 loci (Table S31). Similarly, most of the hits and loci were known to be ECG-related traits (see section “methods”). As for statistical power, the expected chi-squared statistic of multimodal PCA was 90.98 , which is significantly higher than that of unimodal PCA ( = 71.53 ). We observed similar trends for CAE (Table S32).
To assess functional enrichments, we used GREAT33 to quantify the number of cardiovascular terms significantly associated with loci identified by each method as well as the statistical significance of enriched terms. For both multimodal and unimodal models, REGLE outperformed the corresponding PCA method in all cases, and it outperformed CAE in three of the four cases with respect to cardiovascular term enrichments (Table S34) and overall term significance (Table S35).
M-REGLE on ECG lead I and PPG enhances genetic discovery
Similar to the 12-lead ECG case, in the ECG lead I and PPG task, we observed that M-REGLE had stronger genetic discovery results than U-REGLE. We generated 12-dimensional joint representations for all individuals in the training and validation sets (n = 33,192) by running the M-REGLE model on concatenated ECG lead I and PPG waveforms, then performed PCA to obtain 12 uncorrelated PCs of the joint representations. We performed GWASs using REGENIE on each of the 12 PCs (Table S36) and combined the GWAS result by summing the chi-squared statistics of the 12 PC GWAS (Figure 5A). We observed similar genomics inflation of combined p value for M-REGLE and U-REGLE (Figures S32 and S33).
Figure 5.
M-REGLE on ECG lead I and PPG increases genomic discovery
(A) Manhattan plot depicting M-REGLE GWAS p values. Black gene names indicate the closest gene for each locus with . Purple dots denote the GWS loci detected uniquely by M-REGLE. Orange dots indicate loci also identified in U-REGLE.
(B) Comparison of M-REGLE GWS variants-in-hits with U-REGLE. The x axis is the p value of baseline. The y axis is the p value of the M-REGLE. All p values (A) and (B) are computed by summing the chi-squared statistics for all 12 embeddings to perform a single joint chi-squared test. The vertical and horizontal red lines indicate the GWS level. The diagonal red line indicates . The orange dots indicate variants in hits that are significant for U-REGLE but not significant for our M-REGLE and green dots indicate variants in hits that are significant for our M-REGLE but not significant for baseline.
(C) A three-way Venn diagram of the GWAS Catalog loci, loci discovered by M-REGLE, and loci discovered by U-REGLE.
(D) Comparison of the chi-squared statistics for all known significant variants in GWAS Catalog for both U-REGLE and M-REGLE. The difference is statistically significant.
M-REGLE has higher strength of association compared to U-REGLE (Figure 5B) where GWAS on M-REGLE embeddings detected 103 GWS hits and 61 loci, 14 and seven more than U-REGLE, respectively (Table S37). We compared the loci with GWAS Catalog. Out of 61 GWS loci detected by M-REGLE from lead I ECG and PPG, 59 fall in the known loci (96.72%) and two were not previously known (Figure 5C; Table S38). To further show that M-REGLE improves statistical power, we calculated the expected chi-squared statistics on all GWAS Catalog variants for ECG- and PPG-related traits. We observed a significant power increase for M-REGLE compared to U-REGLE (Figure 5D; Table S39). We observed the same pattern for CAE, but multimodal and unimodal PCA were comparable (Table S39).
Similar to 12-lead ECG, functional enrichments of cardiovascular terms for ECG lead I and PPG models showed superiority of multimodal and unimodal REGLE over PCA and CAE modeling methods for both cardiovascular term enrichments (Table S34) and overall term significance (Table S35).
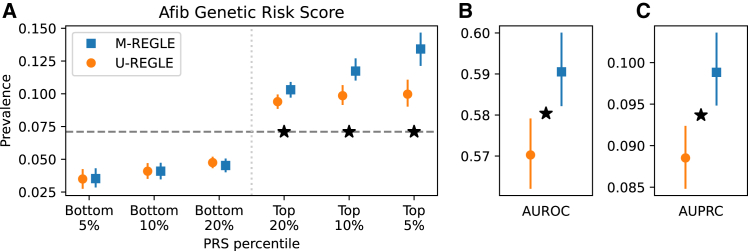
M-REGLE improves the PRS for cardiovascular traits
To ensure the previously unidentified hits detected by M-REGLE are biologically important, we created genetic risk scores by extracting all variants from the significant hits. For each set of embeddings, we trained an ElasticNet model to predict the phenotype of interest on the train dataset utilizing all significant variants (see section “methods”). We considered multiple ECG-derived (e.g., ECG QT interval, ECG P axis,) and PPG-derived (e.g., PPG pulse velocity) phenotypes as well as nine additional cardiovascular disease or cardiovascular risk phenotypes for which there is extensive knowledge available on genetic associations such as Afib, angina, BMI, coronary artery disease, hypertension, stroke, myocardial infarction (MI), type 2 diabetes (T2D), and SBP. In UK Biobank, we have 22 derived phenotypes from ECG and PPG while in total we utilized 31 phenotypes.
We observed that genetic risk for 5 out of 31 phenotypes were significantly improved by M-REGLE compared to U-REGLE after Bonferroni correction (Table S40). The most notable improvement was observed for Afib (Figure 6), with M-REGLE showing an AUROC of 0.59 (95% confidence interval [CI], 0.582–0.599) versus U-REGLE AUROC of 0.57 (95% CI, 0.562–0.578) and an AUPRC of 0.10 (95% CI, 0.094–0.103) versus 0.09 (95% CI, 0.084–0.092) when utilizing all 12 ECG leads (Table S40). Additionally, other phenotypes such as PPG pulse rate, ECG QT interval, SBP, and height also exhibit significant improvement in phenotypic prediction with M-REGLE loci compared to U-REGLE loci (Table S40).
Figure 6.
M-REGLE improves Afib genetic risk score
(A) The x axis is genetic risk score percentile and y axis is the prevalence. Lower is better for the bottom percentiles; higher is better for the top percentiles.
(B and C) (B) AUROC and (C) AUPRC (precision recall) Star sign indicates a statistically significant difference between the two methods using paired bootstrapping (100 repetitions) with 95% confidence.
The main PRS analysis was done with a standard disease definition where we considered cases as individuals who have the disease, and control are individuals who do not have the disease. In addition, for each disease, we considered an analysis where the cases are defined as before, but the controls are individuals who do not have any cardiovascular disease. With the second, more-conservative definition, we observed similar results for AUROC but significantly improved results for AUPRC (Tables S41–S44).
To further validate our PRS results, we computed the PRS in Indiana Biobank datasets,35 European Prospective Investigation into Cancer (EPIC)-Norfolk,34 and the BWHHS44,45,46 using the weights learned in the UK Biobank (see section “methods”). In the Indiana Biobank,35 we have access to Afib and observed that, for all metrics, M-REGLE outperforms U-REGLE among European samples. In the case of AUROC, M-REGLE was significantly better (Table S45). In EPIC-Norfolk,34 we have access to Afib, PPG pulse rate, ECG QT interval, and SBP. We observed that M-REGLE outperformed U-REGLE for all metrics. For Afib in particular, the AUROC, AUPRC, and top 5% prevalence were significantly better for M-REGLE compared to U-REGLE (Tables S46 and S47). Similar to EPIC-Norfolk, in BWHHS, we have access to Afib, PPG pulse rate, ECG QT interval, and SBP. We observed that, for all metrics, M-REGLE outperforms U-REGLE (Table S48) and, for Afib, AUPRC and top 5% prevalence were significantly better for M-REGLE compared to U-REGLE (Table S48). Lastly, for all other phenotypes, M-REGLE outperformed U-REGLE except for SBP in BWHHS (Table S49).
M-REGLE on ECG lead I and PPG and spirograms enhances genetic discovery
We conducted an experiment incorporating an additional data modality, the spirogram, alongside the ECG lead I and PPG dataset. We utilized a similar process and quality-control steps to those in our previous work for the spirogram data.8 We showed that M-REGLE continues to outperform U-REGLE, particularly in terms of the reconstruction error, where M-REGLE achieves significantly lower MSEs than U-REGLE across various numbers of latent dimensions (Figure S35; Table S50). M-REGLE also achieved slightly better performance than U-REGLE in the downstream phenotype-prediction task (Tables S51 and S52).
We performed GWAS learned representations using the same steps utilized in the previous section. We observed that M-REGLE has higher power than U-REGLE (Figure S36). To compare GWAS statistical power, we calculated the expected chi-squared statistics on all the variants reported as ECG-related, PPG-related, and spirogram traits in GWAS Catalog (Table S6). We observed that M-REGLE had higher statistical power than U-REGLE ( vs. ). These results highlight the adaptability of M-REGLE to new multimodal settings. It is worth noting that we cannot directly compare the power of M-REGLE on ECG lead I, PPG, and spirograms with previous results (ECG lead I and PPG) because the sample sizes are different. We have 37,144 samples for ECG lead I and PPG but only 27,213 for the combined analysis of ECG lead I, PPG, and spirograms.
Factors contributing to M-REGLE’s superiority over U-REGLE in genetic studies
We considered two main reasons M-REGLE can outperform U-REGLE in genetic analyses (GWAS and PRS): first, M-REGLE finds better representations of health-data modalities and these embeddings present the phenotype of interest better, thus improving the downstream genetic analysis. M-REGLE would increase signal relative to noise by learning more informative representations, which can improve genetic analyses. Second, the shared information among related modalities is captured more efficiently in the joint embedding space, as opposed to having duplicated information in separate representations for each modality (Figure S34). We simulated data to show an example in which two data modalities have both genetic and non-genetic underlying factors, with the non-genetic factors driving the main phenotypic signal. Under this phenotypic architecture, we observe that both M-REGLE and U-REGLE can capture the strong non-genetic factors, but M-REGLE also demonstrates the capability to capture the genetic factors. Interestingly, both models have very similar phenotype prediction (Figure S34) but very different statistical power in detecting the genetic factor.
Discussion
Access to multiple health-data modalities for many individuals in biobanks and EHR systems provides unique opportunities to study the genetics of complex traits. In particular, when several data modalities are related to a single organ system, these modalities together can provide a better picture of the organ’s function than any individual modality. However, we currently lack statistical methods to fully utilize these multimodal health data in genetic analyses. REGLE8 provides a means to study the genetic underpinnings of high-dimensional data, but it is limited to one data modality and does not leverage the shared and complementary information in multimodal health data. Here, we developed an unsupervised representation learning method, M-REGLE, which aims to utilize multimodal health data in a joint model to improve genetic analyses. We showcased the advantages of M-REGLE over applying REGLE independently on different health-data modalities and then combining the results. M-REGLE creates embeddings in an process that is agnostic to any disease status and medication; however, the obtained embeddings are associated with cardiovascular disease and medications.
We compared M-REGLE with the unimodal representation learning analog (U-REGLE) side by side on the same input data, and we observed significant performance improvements in several aspects. First, M-REGLE has lower reconstruction error compared to U-REGLE, which suggests it compresses and keeps more of the available signal in the dense representations for subsequent use in GWASs. Second, we validated that the joint embeddings learned by M-REGLE capture more genetic signals related to the input data compared to the collective U-REGLE embeddings and higher statistical power over known cardiovascular traits. Lastly, the genetic variants identified by M-REGLE enable better polygenic scoring for 14% (4 out of 28; excluding height from 5 out of 29 phenotypes reported in the “results” section) of tested cardiac phenotypes. Overall, M-REGLE provided greater statistical power for GWAS on health data, which could improve downstream applications such as biological discovery, better PRSs, and more possible drug targets. Additionally, we tested PCA and CAE as base models instead of VAE, applying the same M-style and U-style methods. Our results suggest that CAE and VAE were more effective at capturing meaningful signals and led to larger performance gaps between M-style and U-style methods (Tables S9–S11, S13–S15, S31, and S38). Based on these results, we recommend using a non-linear, deep-representation learning model alongside the M-style approach to maximize the extraction of informative signals from multimodal data.
The key for the effectiveness of M-REGLE is the existence of complementary and overlapping information in the modalities. On one end of the spectrum, when the information in different modalities is completely non-overlapping, there is no duplication of information (and consequently inefficiency). Hence, learning separately will not be wasteful, and M-REGLE is not expected to learn more effectively than U-REGLE. On the other hand, when some modality completely covers another modality, we will not expect to gain any boost from using M-REGLE either, because the duplicated information does not add additional signal to the learned representation. Health data of a single organ system or disease are usually measured through different methods and sensors and fall in the middle of this spectrum. However, before applying M-REGLE, we recommend performing a preliminary analysis to check that the modalities include complementary information (e.g., by performing CCA or DCCA).
With the presence of complementary and overlapping information, we expect that, when using a deep neural network, the compression of information in a low-dimensional dense representation happens more effectively and, as a result, we retain more signal that translates into better reconstruction by the decoder. Thus, the key question was whether the more effective compression also translates into better genetic discovery. We hypothesized that the answer would be positive, because, by using more than one source, the signal-to-noise ratio can be improved, which translates into better statistical power. On the one hand, the representation learning will be more efficient and can retain more information that improves the signal. Furthermore, the modality-specific noise can be reduced because one modality can correct the noise in the other. Our results using different data modalities, different learning methods, and multiple biobanks corroborate this hypothesis.
It is worth noting that our work has a connection to fusion models in deep learning. When dealing with multimodal data, there are three common paradigms often used when combining modalities. First, in early fusion, one combines modalities before the representation learning process and learns a joint latent that is used for the final task, such as prediction of Afib status. Second, in intermediate fusion, one learns representations for each modality separately, combines the independent representations (e.g., by concatenation), and performs the final task on this combined representation. Third, in late fusion, one learns the representations separately and also uses the separate latents to obtain a separate result using each modality for the final task. One then combines the final results. For example, we use PPG and ECG separately to obtain two separate probabilities for having Afib and then get their average as the final probability. Note that M-REGLE is an early fusion, while U-REGLE is an intermediate fusion. In contrast, a late-fusion method would be to run original REGLE on each modality separately (which includes the final task of GWAS) and then meta-analyze the resulting separate GWASs. We intentionally choose U-REGLE (i.e., intermediate fusion) as the baseline instead of the late fusion of separate REGLEs. This is to limit the difference to only multimodal vs. unimodal learning and have a better comparison.
Utilizing ECG parameters for cardiovascular disease have been well studied and multiple expert defined features (EDFs) have been shown to be important for cardiovascular disease. Some of these EDFs includes PR interval, where an abnormal PR interval is a risk factor for Afib and cardiovascular mortality47,48,49; QT interval, where a long QT interval is a risk factor for arrhythmic events and death50,51; P wave, which is associated with Afib52,53,54,55; and QRS complex, where QRS complex is associated with increased ventricular arrhythmic event and mortality.56,57,58 Furthermore, there are large bodies of works that performed GWAS58,59 on these EDFs; however, M-REGLE can utilize other electrophysiological waveforms in a joint model and can detect these embeddings unsupervised with no prior knowledge. Furthermore, we show that not only can M-REGLE GWASs rediscover known GWAS hits but they can also detect previously unidentified hits.
Our exploratory work on ECG and PPG data also opens up opportunities in the large-scale study of cardiovascular disease risk and the genetics of phenotypes derived from smart wearable or mobile phones. Most of the popular smart wearable devices contain sensors that allow users to easily record their ECG (equivalent to the lead I ECG) and PPG. Our experiments demonstrate that M-REGLE will enable researchers to optimally leverage this newly abundant data for genetic discovery. In particular, we emphasize the importance of early fusion of the data before the representation learning and compression into low-dimensional data as there is a large gap between before and after fusion. This is in contrast with the usual practice of using meta-analysis after GWAS to combine multiple sources of data in genetic analysis.
Our work has several limitations. First, our aim was to focus on the method and illustrate the advantage of M-REGLE for genetic discovery over combining the results of unimodal representation learning. As a result, many aspects of genetic discovery can be improved, and the goal was not to have the strongest GWAS on cardiovascular phenotypes. Second, we utilized the median of waveforms of heartbeats for both PPG and ECG. Alternative preprocessing methods can be explored on full ECG and PPG waveforms, which potentially could produce more comprehensive representations, when the focus is on the genetic architecture of heart function. However, recent work26 has shown that utilizing median ECG waveforms can reduce noise and improve results. Third, we performed the main experiments on samples with all the modalities available and have not fully explored M-REGLE’s potential in handling missing data. Being able to learn joint representations from a multimodal dataset with missing data would enable us to carry out larger-scale genetic studies that cover all individuals with only some of the data modalities available. Fourth, our 12-lead ECG task does not exhibit all properties of multi-modality as the different leads conceptually measure the same type of signal (i.e., voltage) and are correlated, but they still have enough non-overlapping signal to be a good choice for a proof of concept as discussed in section “overview of cardiovascular modalities.” Fifth, we observed that the value of in -VAE and scaling factor of inputs jointly have significant impact on M-REGLE embeddings (Figures S37 and S38), while we used a fixed scaling factor and performed hyper-parameter search over to find the optimal for the given scaling factor. A more systematic search over both and scaling factor can produce better embeddings. Sixth, all the genetic analyses were performed on individuals of European ancestry, and the specific impact of ancestry on M-REGLE and U-REGLE was not explored. Lastly, the learned representations obtained from VAEs are known to be non-identifiable without further assumptions.60 However, we observed that, in all of our experiments, the learned embeddings are robust up to a simple permutation and reversal of sign.
Despite these limitations, M-REGLE provides a means to better leverage multimodal health data for genetic discovery and has shown improved performance compared to unimodal representation learning. We demonstrated its advantages by using ECG and PPG data to study genetics of cardiovascular traits. We believe M-REGLE will become a standard method for using multimodal health data for GWAS and downstream analyses.
Data and code availability
Open-source code and trained model weights are available at https://github.com/Google-Health/genomics-research under the M-REGLE directory.
Acknowledgments
We thank all participants, dataset creators, and maintainers of UK Biobank, BWHHS, EPIC-Norfolk, and Indiana Biobank. This research has been conducted using the UK Biobank Resource under application number 65275. The EPIC-Norfolk study (https://doi.org/10.22025/2019.10.105.00004) has received funding from the Medical Research Council (MR/N003284/1 MC-UU_12015/1 and MC_UU_00006/1) and Cancer Research UK (C864/A14136). The genetics work in the EPIC-Norfolk study was funded by the Medical Research Council (MC_PC_13048). P.B.M. acknowledges the support of the National Institute for Health and Care Research Barts Biomedical Research Centre (NIHR203330). A.P.K. is supported by a UK Research and Innovation Future Leaders Fellowship, an Alcon Research Institute Young Investigator Award, and a Lister Institute of Preventive Medicine Award. This research was supported by the NIHR Biomedical Research Centre at Moorfields Eye Hospital and the UCL Institute of Ophthalmology. A.F.S. is supported by BHF grants PG/18/5033837, PG/22/10989, the UCL BHF Research Accelerator AA/18/6/34223 and by the UK Research and Innovation (UKRI) under the UK government’s Horizon Europe funding guarantee EP/Z000211/1. A.F.S. received additional support from the National Institute for Health Research University College London Hospitals Biomedical Research Centre and the Rosetrees Trust (supplemental note).
Declaration of interests
Y.Z., J.K., T.Y., H.Y., A.C., C.Y.M., B.B., and F.H. are current or former employees of Google, and own Alphabet Inc stocks. This study was funded by Google LLC. A.P.K. has acted as a paid consultant or lecturer to Abbvie, Aerie, Allergan, Google Health, Heidelberg Engineering, Novartis, Reichert, Santen, Thea, and Topcon. A.F.S. has received funding from New Amsterdam Pharma for an unrelated project.
Published: June 20, 2025
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.ajhg.2025.05.015.
Contributor Information
Babak Behsaz, Email: babak.behsaz@gmail.com.
Farhad Hormozdiari, Email: fhormoz@google.com.
Supplemental information
References
- 1.Elliott L.T., Sharp K., Alfaro-Almagro F., Shi S., Miller K.L., Douaud G., Marchini J., Smith S.M. Genome-wide association studies of brain imaging phenotypes in UK biobank. Nature. 2018;562:210–216. doi: 10.1038/s41586-018-0571-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jónsson B., Bjornsdottir G., Thorgeirsson T., Ellingsen L.M., Walters G.B., Gudbjartsson D.F., Stefansson H., Stefansson K., Ulfarsson M.O. Brain age prediction using deep learning uncovers associated sequence variants. Nat. Commun. 2019;10:5409. doi: 10.1038/s41467-019-13163-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verweij N., Benjamins J.-W., Morley M.P., van de Vegte Y.J., Teumer A., Trenkwalder T., Reinhard W., Cappola T.P., van der Harst P. The genetic makeup of the electrocardiogram. Cell Syst. 2020;11:229–238.e5. doi: 10.1016/j.cels.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alipanahi B., Hormozdiari F., Behsaz B., Cosentino J., McCaw Z.R., Schorsch E., Sculley D., Dorfman E.H., Foster P.J., Peng L.H., et al. Large-scale machine-learning-based phenotyping significantly improves genomic discovery for optic nerve head morphology. Am. J. Hum. Genet. 2021;108:1217–1230. doi: 10.1016/j.ajhg.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aung N., Vargas J.D., Yang C., Fung K., Sanghvi M.M., Piechnik S.K., Neubauer S., Manichaikul A., Rotter J.I., Taylor K.D., et al. Genome-wide association analysis reveals insights into the genetic architecture of right ventricular structure and function. Nat. Genet. 2022;54:783–791. doi: 10.1038/s41588-022-01083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pirruccello J.P., Di Achille P., Nauffal V., Nekoui M., Friedman S.F., Klarqvist M.D.R., Chaffin M.D., Weng L.-C., Cunningham J.W., Khurshid S., et al. Genetic analysis of right heart structure and function in 40,000 people. Nat. Genet. 2022;54:792–803. doi: 10.1038/s41588-022-01090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cosentino J., Behsaz B., Alipanahi B., McCaw Z.R., Hill D., Schwantes-An T.-H., Lai D., Carroll A., Hobbs B.D., Cho M.H., et al. Inference of chronic obstructive pulmonary disease with deep learning on raw spirograms identifies new genetic loci and improves risk models. Nat. Genet. 2023;55:787–795. doi: 10.1038/s41588-023-01372-4. [DOI] [PubMed] [Google Scholar]
- 8.Yun T., Cosentino J., Behsaz B., McCaw Z.R., Hill D., Luben R., Lai D., Bates J., Yang H., Schwantes-An T.-H., et al. Unsupervised representation learning on high-dimensional clinical data improves genomic discovery and prediction. Nat. Genet. 2024;56:1604–1613. doi: 10.1038/s41588-024-01831-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gomes B., Singh A., O’Sullivan J., Schnurr T.M., Goddard P.C., Loong S., Amar D., Hughes J.W., Kostur M., Haddad F., et al. Genetic architecture of cardiac dynamic flow volumes. Nat. Genet. 2024;56:245–257. doi: 10.1038/s41588-023-01587-5. [DOI] [PubMed] [Google Scholar]
- 10.Acosta J.N., Falcone G.J., Rajpurkar P., Topol E.J. Multimodal biomedical ai. Nat. Med. 2022;28:1773–1784. doi: 10.1038/s41591-022-01981-2. [DOI] [PubMed] [Google Scholar]
- 11.Kline A., Wang H., Li Y., Dennis S., Hutch M., Xu Z., Wang F., Cheng F., Luo Y. Multimodal machine learning in precision health: A scoping review. npj Digit. Med. 2022;5 doi: 10.1038/s41746-022-00712-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soenksen L.R., Ma Y., Zeng C., Boussioux L., Villalobos Carballo K., Na L., Wiberg H.M., Li M.L., Fuentes I., Bertsimas D. Integrated multimodal artificial intelligence framework for healthcare applications. npj Digit. Med. 2022;5 doi: 10.1038/s41746-022-00689-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tomašev N., Glorot X., Rae J.W., Zielinski M., Askham H., Saraiva A., Mottram A., Meyer C., Ravuri S., Protsyuk I., et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature. 2019;572:116–119. doi: 10.1038/s41586-019-1390-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reyes D.M., Chao H., Hahn J., Shen L., Yan P. Multimodal neurodegenerative disease subtyping explained by chatgpt. arXiv. 2024 doi: 10.48550/ARXIV.2402.00137. Preprint at. [DOI] [Google Scholar]
- 15.Yang Z., Wen J., Abdulkadir A., Cui Y., Erus G., Mamourian E., Melhem R., Srinivasan D., Govindarajan S.T., Chen J., et al. Gene-sgan: discovering disease subtypes with imaging and genetic signatures via multi-view weakly-supervised deep clustering. Nat. Commun. 2024;15 doi: 10.1038/s41467-023-44271-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mei X., Lee H.-C., Diao K.-y., Huang M., Lin B., Liu C., Xie Z., Ma Y., Robson P.M., Chung M., et al. Artificial intelligence–enabled rapid diagnosis of patients with covid-19. Nat. Med. 2020;26:1224–1228. doi: 10.1038/s41591-020-0931-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang L., Xu S., Sellergren A., Kohlberger T., Zhou Y., Ktena I., Kiraly A., Ahmed F., Hormozdiari F., Jaroensri T., et al. Advancing multimodal medical capabilities of gemini. arXiv. 2024 doi: 10.48550/ARXIV.2405.03162. Preprint at. [DOI] [Google Scholar]
- 18.Wu C., Zhang X., Zhang Y., Wang Y., Xie W. Towards generalist foundation model for radiology by leveraging web-scale 2d and 3d medical data. arXiv. 2023 doi: 10.48550/ARXIV.2308.02463. Preprint at. [DOI] [Google Scholar]
- 19.Zhang K., Yu J., Adhikarla E., Zhou R., Yan Z., Liu Y., Liu Z., He L., Davison B., Li X., et al. Biomedgpt: A unified and generalist biomedical generative pre-trained transformer for vision, language, and multimodal tasks. arXiv. 2023 doi: 10.48550/ARXIV.2305.17100. Preprint at. [DOI] [Google Scholar]
- 20.Belyaeva A., Cosentino J., Hormozdiari F., Eswaran K., Shetty S., Corrado G., Carroll A., McLean C.Y., Furlotte N.A. Machine Learning for Multimodal Healthcare Data. Springer Nature Switzerland; 2023. Multimodal llms for health grounded in individual-specific data; pp. 86–102. [DOI] [Google Scholar]
- 21.Peterson V.M., Zhang K.X., Kumar N., Wong J., Li L., Wilson D.C., Moore R., McClanahan T.K., Sadekova S., Klappenbach J.A. Multiplexed quantification of proteins and transcripts in single cells. Nat. Biotechnol. 2017;35:936–939. doi: 10.1038/nbt.3973. [DOI] [PubMed] [Google Scholar]
- 22.Mimitou E.P., Cheng A., Montalbano A., Hao S., Stoeckius M., Legut M., Roush T., Herrera A., Papalexi E., Ouyang Z., et al. Multiplexed detection of proteins, transcriptomes, clonotypes and crispr perturbations in single cells. Nat. Methods. 2019;16:409–412. doi: 10.1038/s41592-019-0392-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mimitou E.P., Lareau C.A., Chen K.Y., Zorzetto-Fernandes A.L., Hao Y., Takeshima Y., Luo W., Huang T.-S., Yeung B.Z., Papalexi E., et al. Scalable, multimodal profiling of chromatin accessibility, gene expression and protein levels in single cells. Nat. Biotechnol. 2021;39:1246–1258. doi: 10.1038/s41587-021-00927-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hao Y., Hao S., Andersen-Nissen E., Mauck W.M., Zheng S., Butler A., Lee M.J., Wilk A.J., Darby C., Zager M., et al. Integrated analysis of multimodal single-cell data. Cell. 2021;184:3573–3587.e29. doi: 10.1016/j.cell.2021.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuchroo M., Huang J., Wong P., Grenier J.-C., Shung D., Tong A., Lucas C., Klein J., Burkhardt D.B., Gigante S., et al. Multiscale phate identifies multimodal signatures of covid-19. Nat. Biotechnol. 2022;40:681–691. doi: 10.1038/s41587-021-01186-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedman S.F., Moran G.E., Rakic M., Phillipakis A. Genetic architectures of medical images revealed by registration of multiple modalities. Bioinf. Biol. Insights. 2024;18 doi: 10.1177/11779322241282489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Radhakrishnan A., Friedman S.F., Khurshid S., Ng K., Batra P., Lubitz S.A., Philippakis A.A., Uhler C. Cross-modal autoencoder framework learns holistic representations of cardiovascular state. Nat. Commun. 2023;14 doi: 10.1038/s41467-023-38125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kingma D.P., Welling M. Auto-encoding variational bayes. arXiv. 2013 doi: 10.48550/ARXIV.1312.6114. Preprint at. [DOI] [Google Scholar]
- 29.Aschard H., Vilhjálmsson B.J., Greliche N., Morange P.-E., Trégouët D.-A., Kraft P. Maximizing the power of principal-component analysis of correlated phenotypes in genome-wide association studies. Am. J. Hum. Genet. 2014;94:662–676. doi: 10.1016/j.ajhg.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Porter H.F., O’Reilly P.F. Multivariate simulation framework reveals performance of multi-trait gwas methods. Sci. Rep. 2017;7 doi: 10.1038/srep38837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rumelhart D.E., Hinton G.E., Williams R.J. Vol. 1. MIT Press; Cambridge, MA, USA: 1986. Learning internal representations by error propagation. (Parallel Distributed Processing: Explorations in the Microstructure of Cognition). [DOI] [Google Scholar]
- 32.Mbatchou J., Barnard L., Backman J., Marcketta A., Kosmicki J.A., Ziyatdinov A., Benner C., O’Dushlaine C., Barber M., Boutkov B., et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat. Genet. 2021;53:1097–1103. doi: 10.1038/s41588-021-00870-7. [DOI] [PubMed] [Google Scholar]
- 33.McLean C.Y., Bristor D., Hiller M., Clarke S.L., Schaar B.T., Lowe C.B., Wenger A.M., Bejerano G. GREAT improves functional interpretation of cis-regulatory regions. Nat. Biotechnol. 2010;28:495–501. doi: 10.1038/nbt.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Day N., Oakes S., Luben R., Khaw K.T., Bingham S., Welch A., Wareham N. EPIC-Norfolk: study design and characteristics of the cohort. european prospective investigation of cancer. Br. J. Cancer. 1999;80:95–103. doi: 10.17863/CAM.89388. [DOI] [PubMed] [Google Scholar]
- 35.Lai D., Schwantes-An T.-H., Abreu M., Chan G., Hesselbrock V., Kamarajan C., Liu Y., Meyers J.L., Nurnberger J.I., Plawecki M.H., et al. Gene-based polygenic risk scores analysis of alcohol use disorder in african americans. Transl. Psychiatry. 2022;12 doi: 10.1038/s41398-022-02029-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Price A.L., Patterson N.J., Plenge R.M., Weinblatt M.E., Shadick N.A., Reich D. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 2006;38:904–909. doi: 10.1038/ng1847. [DOI] [PubMed] [Google Scholar]
- 37.Auton A., Abecasis G.R., Altshuler D.M., Durbin R.M., Abecasis G.R., Bentley D.R., Chakravarti A., Clark A.G., Donnelly P., Eichler E.E., et al. A global reference for human genetic variation. Nature. 2015;526:68–74. doi: 10.1038/nature15393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Das S., Forer L., Schönherr S., Sidore C., Locke A.E., Kwong A., Vrieze S.I., Chew E.Y., Levy S., McGue M., et al. Next-generation genotype imputation service and methods. Nat. Genet. 2016;48:1284–1287. doi: 10.1038/ng.3656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Andrew G., Arora R., Bilmes J., Livescu K. In: Proceedings of the 30th International Conference on Machine Learning volume 28 of Proceedings of Machine Learning Research. Dasgupta S., McAllester D., editors. PMLR; Atlanta, Georgia, USA: 2013. Deep canonical correlation analysis; pp. 1247–1255. [Google Scholar]
- 40.Yang H., Zeng Y., Chen W., Sun Y., Hu Y., Ying Z., Wang J., Qu Y., Fang F., Valdimarsdóttir U.A., Song H. The role of genetic predisposition in cardiovascular risk after cancer diagnosis: a matched cohort study of the uk biobank. Br. J. Cancer. 2022;127:1650–1659. doi: 10.1038/s41416-022-01935-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rentsch C.T., Garfield V., Mathur R., Eastwood S.V., Smeeth L., Chaturvedi N., Bhaskaran K. Sex-specific risks for cardiovascular disease across the glycaemic spectrum: a population-based cohort study using the uk biobank. Lancet Reg. Health. Eur. 2023;32 doi: 10.1016/j.lanepe.2023.100693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ghoussaini M., Mountjoy E., Carmona M., Peat G., Schmidt E.M., Hercules A., Fumis L., Miranda A., Carvalho-Silva D., Buniello A., et al. Open targets genetics: systematic identification of trait-associated genes using large-scale genetics and functional genomics. Nucleic Acids Res. 2021;49:D1311–D1320. doi: 10.1093/nar/gkaa840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mountjoy E., Schmidt E.M., Carmona M., Schwartzentruber J., Peat G., Miranda A., Fumis L., Hayhurst J., Buniello A., Karim M.A., et al. An open approach to systematically prioritize causal variants and genes at all published human gwas trait-associated loci. Nat. Genet. 2021;53:1527–1533. doi: 10.1038/s41588-021-00945-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lawlor D.A., Ebrahim S., Davey Smith G., British women's heart and health study Socioeconomic position in childhood and adulthood and insulin resistance: cross sectional survey using data from british women’s heart and health study. BMJ. 2002;325:805. doi: 10.1136/bmj.325.7368.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lawlor D.A., Patel R., Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ. 2003;327:712–717. doi: 10.1136/bmj.327.7417.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim L.G., Carson C., Lawlor D.A., Ebrahim S. Geographical variation in cardiovascular incidence: results from the british women’s heart and health study. BMC Public Health. 2010;10:696. doi: 10.1186/1471-2458-10-696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rasmussen P.V., Nielsen J.B., Skov M.W., Pietersen A., Graff C., Lind B., Struijk J.J., Olesen M.S., Haunsø S., Køber L., et al. Electrocardiographic pr interval duration and cardiovascular risk: Results from the copenhagen ecg study. Can. J. Cardiol. 2017;33:674–681. doi: 10.1016/j.cjca.2017.02.015. [DOI] [PubMed] [Google Scholar]
- 48.van Setten J., Brody J.A., Jamshidi Y., Swenson B.R., Butler A.M., Campbell H., Del Greco F.M., Evans D.S., Gibson Q., Gudbjartsson D.F., et al. Pr interval genome-wide association meta-analysis identifies 50 loci associated with atrial and atrioventricular electrical activity. Nat. Commun. 2018;9 doi: 10.1038/s41467-018-04766-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ntalla I., Weng L.-C., Cartwright J.H., Hall A.W., Sveinbjornsson G., Tucker N.R., Choi S.H., Chaffin M.D., Roselli C., Barnes M.R., et al. Multi-ancestry gwas of the electrocardiographic pr interval identifies 202 loci underlying cardiac conduction. Nat. Commun. 2020;11 doi: 10.1038/s41467-020-15706-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ward D.E. Prolongation of the qt interval as an indicator of risk of a cardiac event. Eur. Heart J. 1988;9:139–144. doi: 10.1093/eurheartj/9.suppl_g.139. [DOI] [PubMed] [Google Scholar]
- 51.Robbins J., Nelson J.C., Rautaharju P.M., Gottdiener J.S. The association between the length of the qt interval and mortality in the cardiovascular health study. Am. J. Med. 2003;115:689–694. doi: 10.1016/j.amjmed.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 52.Magnani J.W., Gorodeski E.Z., Johnson V.M., Sullivan L.M., Hamburg N.M., Benjamin E.J., Ellinor P.T. P wave duration is associated with cardiovascular and all-cause mortality outcomes: the national health and nutrition examination survey. Heart Rhythm. 2011;8:93–100. doi: 10.1016/j.hrthm.2010.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Magnani J.W., Zhu L., Lopez F., Pencina M.J., Agarwal S.K., Soliman E.Z., Benjamin E.J., Alonso A. P-wave indices and atrial fibrillation: Cross-cohort assessments from the framingham heart study (fhs) and atherosclerosis risk in communities (aric) study. Am. Heart J. 2015;169:53–61.e1. doi: 10.1016/j.ahj.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nielsen J.B., Kühl J.T., Pietersen A., Graff C., Lind B., Struijk J.J., Olesen M.S., Sinner M.F., Bachmann T.N., Haunsø S., et al. P-wave duration and the risk of atrial fibrillation: Results from the copenhagen ecg study. Heart Rhythm. 2015;12:1887–1895. doi: 10.1016/j.hrthm.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 55.Christophersen I.E., Magnani J.W., Yin X., Barnard J., Weng L.-C., Arking D.E., Niemeijer M.N., Lubitz S.A., Avery C.L., Duan Q., et al. Fifteen genetic loci associated with the electrocardiographic p wave. Circ. Cardiovasc. Genet. 2017;10 doi: 10.1161/circgenetics.116.001667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Das M.K., Maskoun W., Shen C., Michael M.A., Suradi H., Desai M., Subbarao R., Bhakta D. Fragmented qrs on twelve-lead electrocardiogram predicts arrhythmic events in patients with ischemic and nonischemic cardiomyopathy. Heart Rhythm. 2010;7:74–80. doi: 10.1016/j.hrthm.2009.09.065. [DOI] [PubMed] [Google Scholar]
- 57.Kurl S., Mäkikallio T.H., Rautaharju P., Kiviniemi V., Laukkanen J.A. Duration of qrs complex in resting electrocardiogram is a predictor of sudden cardiac death in men. Circulation. 2012;125:2588–2594. doi: 10.1161/circulationaha.111.025577. [DOI] [PubMed] [Google Scholar]
- 58.Young W.J., Haessler J., Benjamins J.-W., Repetto L., Yao J., Isaacs A., Harper A.R., Ramirez J., Garnier S., van Duijvenboden S., et al. Genetic architecture of spatial electrical biomarkers for cardiac arrhythmia and relationship with cardiovascular disease. Nat. Commun. 2023;14 doi: 10.1038/s41467-023-36997-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kolder I.C.R.M., Tanck M.W.T., Bezzina C.R. Common genetic variation modulating cardiac ecg parameters and susceptibility to sudden cardiac death. J. Mol. Cell. Cardiol. 2012;52:620–629. doi: 10.1016/j.yjmcc.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 60.Locatello F., Bauer S., Lucic M., Raetsch G., Gelly S., Schölkopf B., Bachem O. In: Proceedings of the 36th International Conference on Machine Learning volume 97 of Proceedings of Machine Learning Research. Chaudhuri K., Salakhutdinov R., editors. PMLR; 2019. Challenging common assumptions in the unsupervised learning of disentangled representations; pp. 4114–4124. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Open-source code and trained model weights are available at https://github.com/Google-Health/genomics-research under the M-REGLE directory.