Abstract
Introduction
Envenomations induced by stonefish (Synanceia verrucosa) stings are among the most painful envenomations in the marine environment. Reunion Island in the Indian Ocean is not spared from these envenomations. The aim of this series is to characterize suspected cases of stonefish envenomation and to describe the associated clinical management.
Methods
This is a retrospective observational series of suspected stonefish envenomations recorded into the database of the Indian Ocean toxicovigilance Department between 1 January 2020 and 2 June 2024 on Reunion Island. Data on clinical characteristics were obtained from the patients’ electronic medical records, and additional information was obtained during telephone conversations with the victims if necessary.
Results
Between January 2020 and June 2024, 135 stonefish envenomations were recorded. Most victims were male, with a median age of 31.5 years. January recorded the highest number of cases. The majority of envenomations occurred on beaches, notably l’Ermitage (66 cases) and Saint-Pierre (39 cases), with the foot being the most affected area (94.8%). The pain was intense for most cases (Visual Analogue Scale 8–10), and skin symptoms included localized and extensive oedema, as well as necrotic halos in some instances. General symptoms like hypertension and paresthesia were rare. No fatalities occurred. Treatment involved opioids, paracetamol, and hot water immersion. Our findings demonstrated a statistically significant correlation between the number of stings and the extent of edema (p < 0.00003). However, no significant relationship was found between the number of stings and pain intensity (p = 0.86).
Conclusions
On Reunion Island, approximately 30 suspected stonefish stings occur annually, with a peak in January and frequent locations including l’Ermitage and Saint-Pierre. These envenomations mainly affect the foot and cause intense pain, sometimes accompanied by significant oedema correlated with the number of stings. While no deaths were recorded, emergency care is often necessary. In the absence of official guidelines, locoregional anaesthesia appears to be an effective strategy for pain relief.
Keywords: Stonefish, Indian ocean, Synanceia verrucosa, Poisson-pierre, Pain
Highlights
• Around 30 suspected stonefish stings occur each year on Reunion Island
• Pain is the main reason for visits to emergency departments
• Locoregional nerve block anaesthesia appears to be an effective solution to intense pain
Introduction
The stonefish (Several species, Synanceia verrucosa is the only species present in Reunion Island, a subtropical French territory located in the South-West Indian Ocean), with its 13 dorsal spines, each connected to a pair of venom sacs, is known to cause severe pain. This species, which can live between five and ten years, is vulnerable to rays and sharks (other bottom-feeding predators). Its venom can cause severe oedema of the stung limb [1]. General symptoms are rare, as are deaths, despite its reputation and some published cases [2, 3].
Its rough skin traps particles from the environment, allowing it to coat itself with the same microalgae as the corals and rocks around it. This camouflage allows it to hide on a rock. It can also bury itself in the sand, leaving only its mouth and eyes visible [4]. Since it is a very poor swimmer, blending in with its surroundings is its only solution for hunting. It is unafraid of human presence, and when a human foot approaches it, it raises its dorsal spines. The pressure exerted by the victim releases the venom.
Envenomations by stonefish stings often lead to emergency room visits, as the pain cannot be treated by general practitioners. Antivenom produced in Australia is not available on Reunion Island.
The main toxins identified in the venom of Synanceia verrucosa are:
Hyaluronidase [ 5, 6]: This enzyme degrades the hyaluronic acid in connective tissue, allowing the venom to spread more rapidly through the tissue. It also exacerbates local inflammation and oedema.
Verrucotoxin [ 6, 7, 8] (VTX): an isolated toxin specific to the Synanceia verrucosa species. It is responsible for the intense pain that lasts for several hours. It also has a vasodilatory effect that contributes to the formation of significant oedema.
Neoverrucotoxin [ 9] (neoVTX): a cytolytic toxin which could be responsible for necrotic halo and oedema.
Despite its notoriety, little is published on marine envenomations in the Indian Ocean, and clinical data on stonefish stings remain limited. This study aims to describe suspected cases involving Synanceia verrucosa recorded between 1 January 2020, and 2 June 2024, on Reunion Island, with a focus on clinical presentation and management.
Methods
Study design
This is a retrospective descriptive study of cases of suspected envenomation by stonefish (Synanceia verrucosa) between 1 January 2020, and 2 June 2024, from the Indian Ocean French Toxicovigilance Department database. The database has been updated in 2020 to be in line with the national database of French poison control centers, which explains the recruitment period.
Study area and data
The Indian Ocean Toxicovigilance Department is in charge of monitoring human poisonings on Reunion Island and Mayotte Island, two French Overseas Territories.
The data come mainly from admissions to the Reunion Island’s 4 emergency departments. The cases investigated are based on a weekly extraction of ICD 10 codings for main diagnoses related to envenomations from emergency room visits. Each case has been investigated by a member of the Indian Ocean Toxicovigilance Department. When necessary, telephone calls have been made to each patient to complete any missing information and to provide a follow-up.
Pain intensity was assessed using a Visual Analog Scale (VAS), a validated and widely used method in clinical settings. The VAS consists of a 10-centimeter horizontal line, where 0 indicates “no pain” and 10 represents “worst imaginable pain”. Patients were asked to indicate the point on the line that best represented their pain intensity at the time of assessment. In some cases, a simplified numeric rating scale from 0 to 10 was used instead. For consistency in data analysis, we converted simplified rating scale to VAS equivalents using established correspondences between the two scales, as suggested in the literature [10, 11]. This score was then recorded in their medical files.
Missing data was designated as “unknown” and were not included in the statistical analysis. The following data were described: socio-demographics, date of envenomation, circumstances of envenomation and location of the accident, clinical presentation, pain score, medical management and outcomes.
A case is defined as a person who has been stung by a stonefish whether clearly identified or suspected by the healthcare tea, based on the clinical context (sudden, intense pain following weight-bearing contact in a context of marine activity, presence of puncture wounds and absence of alternative diagnosis).
Statistical analysis
Continuous variables were reported as medians with ranges (minimum, maximum); categorical variables as counts and percentages. For bivariate analyses, we used two-sided Fisher’s Exact Test (α = 0.05), as it provides more accurate results in cases of small sample sizes or low expected frequencies in contingency tables. All statistical analyses were performed using R software, version 4.2.2.
Results
Between January 1, 2020, and June 2, 2024, a total of 135 suspected cases of human envenomation by stonefish (Synanceia verrucosa) were recorded in the database of the Indian Ocean Toxicovigilance Department (DTV-OI). Most cases involved young adult males, with a median age of 31.5 years. Nearly three-quarters of the affected individuals were residents of Reunion Island, while the remaining cases involved tourists. A detailed description of case characteristics is provided in Table 1.
Table 1.
Suspected envenomations by stonefish (Synanceia verrucosa) cases description. DTV-OI. N = 135. January 2020- June 2024. Reunion Island
| n | % | ||
|---|---|---|---|
|
Sex, M/F Sex ratio M/F |
79/56 1,6 M/1F |
||
| Age (year, range) | 31,5 (4,4–72,0) | ||
| Resident on Reunion Island | 104 | 77,0 |
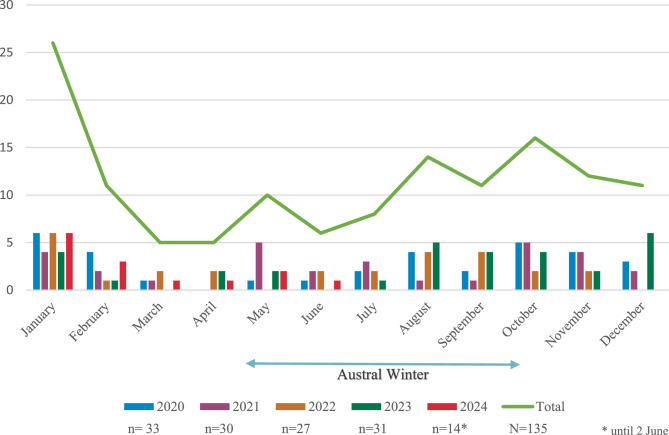
With regard to the monthly distribution of cases, January had the highest number of cases, with 26 envenomations, followed by October, August and November, with 16, 14 and 12 cases respectively (Fig. 1). March, April and June had the lowest cumulative number of cases, with 5, 5 and 6 envenomations respectively. On average, there are 30 envenomations per year.
Fig. 1.
Annual and monthly breakdown of suspected cases of envenomation by stonefish stings on Reunion Island. January 2020- June 2024. DTV-OI
The envenomations occurred in the Western, South-Western and Southern parts of the island (Fig. 2). These areas are seaside resorts with beaches and sometimes seawater pools.
Fig. 2.
Location of suspected stonefish exposures on Reunion Island January 2020- June 2024. N = 135, 13 location are unknown
The majority of cases of envenomation were recorded on the beaches of l’Ermitage with 66 cases, followed by the beach of Saint-Pierre with 39 cases, Saint-Leu with 13 cases, l’Etang-salé and Saint-Joseph with 2 cases each. It should be noted that the exact location of 13 cases is not known, but they concern the same areas already identified.
In the majority of cases, the envenomation was accidental (Table 2). Only 1 case was clearly identified where a person deliberately touched the stonefish with their finger. The foot was the most commonly injured area in 94.8% of cases, with the remaining 5.2% involving the hand. As regards the number of stings a victim may have undergone, most cases received 1 sting in 105 cases (77.8%), 2 stings in 20 cases (14.8%), and 3 and 4 stings in 1 case each (0.7%). This information was not available for 8 cases (5.9%). Finally, the stonefish responsible for the envenomation was clearly observed in only 8 cases (5.9%).
Table 2.
Circumstances and details of stonefish bite envenomation. N = 135. January 2020- June 2024. DTV-OI. Reunion Island
| n | (%) | |
|---|---|---|
| Circumstances of envenomation | ||
| Accidental | 134 | 99,3 |
| Deliberate | 1 | 0,7 |
| Location of the sting | ||
| Foot | 128 | 94,8 |
| Hand | 7 | 5,2 |
| Number of stings | ||
| 1 | 105 | 77,8 |
| 2 | 20 | 14,8 |
| 3 | 1 | 0,7 |
| 4 | 1 | 0,7 |
| unknown | 8 | 5,9 |
| Observation of the stonefish | ||
| Yes | 8 | 5,9 |
| No | 127 | 94,1 |
From a clinical point of view, 100% of the patients felt pain at the stung limb (Table 3). Pain assessment was not available for 7 cases (5.2%). The pain was very intense with a visual analog scale pain score (VAS) between 8 and 10 for 102 cases (75.6%), intense for 24 cases (17.8%) and moderate or weak for 1 case each (0.7%).
Table 3.
Clinical presentation of cases with stonefish poisoning. N = 135. January 2020- June 2024. DTV-OI. Reunion Island
| n | % | |
|---|---|---|
| Pain intensitya | ||
| VAS 1–3 | 1 | 0,7 |
| VAS 4–5 | 1 | 0,7 |
| VAS 6–7 | 24 | 17,8 |
| VAS 8-10b | 102 | 75,6 |
| VAS Unknown | 7 | 5,2 |
| Skin area | ||
| Localized oedema | 62 | 45,9 |
| Extensive oedema | 35 | 25,9 |
| Necrotic halo | 32 | 23,7 |
| Oedema not specified | 20 | 14,8 |
| Ecchymosis | 16 | 11,9 |
| Skin erythema | 13 | 9,6 |
| Blisters | 5 | 3,7 |
| Significant tissue injury | 3 | 2,2 |
| General symptoms | ||
| High blood pressure | 8 | 5,9 |
| Limb paresthesia | 4 | 3,0 |
| Vomiting | 2 | 1,5 |
| Lipothymia | 1 | 0,7 |
| Diffuse tremors | 1 | 0,7 |
| Pruritus | 1 | 0,7 |
| Complication | ||
| Dermohypodermitisc | 5 | 3,7 |
| Iatrogenic second-degree burn | 1 | 0,7 |
Please note that a patient may exhibited several clinical features
apain intensity is evaluated with visual analog scale pain scoring (VAS)
bincluding 77 cases with VAS score at 10/10
c4/5 had received antibiotic prophylaxis
Regarding skin symptoms, localized oedema was reported in 62 cases (45.9%) and extensive oedema in 35 cases (25.9%). Oedema without precise extent was reported in 20 cases (14.8%). A necrotic halo (defined by a slightly necrotic area of skin with the sting point at its center) was described in 32 cases (23.7%). Ecchymosis was observed in 16 cases (11.9%) and erythema in 13 cases (9.6%). More rarely, blisters and significant cutaneous lesions were reported in 5 cases (3.7%) and 3 cases (2.2%) respectively.
General symptoms were rare, with 8 cases (5.9%) suffering from hypertension, 4 (3.0%) limb paresthesia, 2 (1.5%) vomiting and 1 (0.7%) lipothymia, diffuse tremors and pruritus each.
Finally, with regard to the complications reported, 5 cases (3.7%) presented with dermohypodermitis and one case (0.7%) suffered an iatrogenic second-degree burn following the use of hot water immersion (HWI). It should be noted that of the 135 total cases, no one died as a result of envenomation.
Regarding non-medicinal treatments received following envenomation (Table 4); HWI was performed in 25 cases (18.5%), contrast bath therapy in 16 cases (11.9%); cold water, flame and alcohol pad were reported 1 time each (0.7%).
Table 4.
Treatments received for envenomation. N = 135. January 2020- June 2024. DTV-OI. Reunion Island
| n a | % | |
|---|---|---|
| Non-drug treatmentb | ||
| Hot water immersion | 25 | 18,5 |
| Contrast bath therapy | 16 | 11,9 |
| Cold water | 1 | 0,7 |
| Flame | 1 | 0,7 |
| Alcohol pad | 1 | 0,7 |
| Inhaled treatment | ||
| Methoxyflurane inhalation | 17 | 12,6 |
| Medical nitrous oxide | 11 | 8,1 |
| Drug therapy | ||
| Opioids | 93 | 68,9 |
| Paracetamol | 57 | 42,2 |
| Nefopam | 9 | 6,7 |
| Unknown analgesia | 8 | 5,9 |
| Antihistamine | 5 | 3,7 |
| Non-steroidal anti-inflammatory drugs | 4 | 3,0 |
| Anti-inflammatory drugs | 4 | 3,0 |
| Anxiolytic therapy | 3 | 2,2 |
| Ketamine | 2 | 1,5 |
| Midazolam | 1 | 0,7 |
| Topical corticosteroids | 1 | 0,7 |
| Topical antibiotic | 1 | 0,7 |
| Anesthesia | ||
| Local nerve block anesthesia | 68 | 50,4 |
| Local anesthesia | 20 | 14,8 |
| Prophylaxis | ||
| Antibiotic prophylaxis | 76 | 56,3 |
| Venous thromboembolism prophylaxis | 20 | 14,8 |
| Other | ||
| Hyperbaric oxygen therapy | 1 | 0,7 |
aPlease note that a patient may receive several treatments
bNon-drug treatments were administered during hospital care
Methoxyflurane inhalation was used in 17 cases (12.6%) and medical nitrous oxide in 11 cases (8.1%).
With regard to drug treatments, opioids were administered in 93 cases (68.9%), paracetamol in 57 cases (42.2%) and nefopam in 9 cases (6.7%).
Local nerve block anesthesia was used in 68 cases (50.4%) and local anesthesia in 20 cases (14.8%).
Antibiotic prophylaxis was prescribed in 76 cases (56.3%) and venous thromboembolism prophylaxis in 20 cases (14.8%).
Finally, one case (0.7%) received a hyperbaric session. As stonefish antivenom is not available on the island, it is normal not to find any in the treatments received at the hospital.
We aimed to assess whether a higher number of stings was associated with greater pain intensity (Table 5), but no significant association was found (p = 0.86). This suggests that pain severity remains high regardless of the number of stings.
Table 5.
Comparison between number of Sting and intensity of pain and number of Sting and extent of oedema in cases of suspected stonefish envenomation. January 2020- June 2024. DTV-OI. Reunion Island
| 1 sting | 2 stings or more | p-value* | |
|---|---|---|---|
| VASa < 6 | 2 | 0 | 0.86 |
| VAS 6–7 | 17 | 4 | |
| VAS 8–10 | 83 | 15 | |
| Localized oedema | 60 | 2 | < 0.00003 |
| Extensive oedema | 20 | 12 |
aVisual analog scale pain scoring (VAS)
*two-sided Fisher’s Exact test with a significance level of 0.05
In contrast, a statistically significant association was observed between the number of stings and the extent of oedema, with extensive oedema more frequently reported in cases involving two or more stings compared to a single sting (p < 0.00003). This finding highlights the clinical importance of sting count in predicting local tissue involvement.
Discussion
Between 1 January 2020 and 2 June 2024, 135 cases of marine envenomation suspected to have involved a stonefish were reported on Reunion Island by the Indian Ocean Toxicovigilance Department, which corresponds to around 30 envenomations per year.
The highest incidence of envenomation was observed in January, which corresponds to the austral summer and school holidays on Reunion Island. During this period, the local population frequently visits the lagoons of Ermitage and Saint-Pierre—two of the most popular and most affected beaches. These sites are characterized by fine sandy bottoms where stonefish may more easily bury themselves. In contrast, natural pools with volcanic rocks or sea urchins might encourage bathers to wear protective footwear, potentially reducing exposure. Although no data currently confirm a seasonal increase in stonefish abundance during the austral summer, environmental factors could contribute to the observed pattern. Warmer water temperatures might enhance the metabolic or feeding activity of stonefish, as well as that of their prey, such as small fish and crustaceans. Another hypothesis—yet to be studied—is whether the reproductive period of Synanceia verrucosa occurs during this season and whether calmer waters in lagoons might provide favorable conditions for spawning. Further ecological research would be necessary to explore these possibilities. Of the few cases of stings to hand, only one was deliberate and we will not comment on it. The other cases were involuntary and can be explained by the fact that people swim and put their hands on the ground because the water is not very deep in the lagoon.
Pain is the first symptom, and is often described by victims as starting with a sensation of being cut, followed by intense pain that progresses crescendo within an hour to very intense pain that moves up the limb (sensation of burning from the inside) [12, 13]. All of the cases in our series were affected by pain, and this was the main reason for visiting the emergency department. The intensity of pain does not seem to vary according to the quantity of venom injected, as we have shown.
The appearance and extent of oedema was less frequently reported than pain. It is likely that this information is not detailed enough in the medical record, as pain management is the main problem. We found that the greater the number of stings, and therefore the greater the quantity of venom inoculated, the more extensive the oedema. The stonefish has 13 dorsal spines, each connected to a pair of venom glands that can contain 5–10 mg of venom. [14]. The oedema associated with the envenomation may be more or less severe and therefore have a greater or lesser impact on activities of daily living [15].
There are very few general symptoms, as reported in other series [3, 16, 17], even though they are probably under-declared.
There were no deaths in our case series. In addition, the previous DTV-OI database, which covered the previous 10 years, did not reveal any deaths [18]. More recently, Maillaud et al. reported three cases of cardiorespiratory toxicity, including one death [2]. We keep in mind that intense pain can make the victim feel faint, so drowning is possible if this happens in water. In the event of life-threatening conditions, resuscitation is the first line of treatment.
Pain management
Hot water immersion and contrast bath therapy
Widely recommended in cases of marine envenomation, hot water immersion (HWI) involves immersing the affected area in water as hot as the person who has been stung can tolerate (max. 45 °C, 115 °F) for 30–90 min in order to denature supposed thermolabile venom proteins [19–21]. Another method involves alternating hot and cold water: contrast bath therapy (CBT). However, while generally effective, hot water immersion can present certain risks and potential dangers. If the water is too hot (above 45 °C/115°F), it can cause thermal burns [22], compounding the injury and potentially causing more damage than the venom itself. In stressful situations, it might be difficult to monitor or control the water temperature accurately, increasing the risk of scalding.
The pain relief provided by HWI is often temporary [13, 19].
In our series, 18.5% of cases received HWI and 11.9% CBT, which is lower than in other publications, 80% in Singapore for example [17]. The longer you are exposed to hot water, the greater the risk of burns, even at slightly lower temperatures. The elderly, children and those with more sensitive skin are more at risk and may suffer burns at lower temperatures. It should be noted that no robust study in humans has been able to demonstrate the effectiveness of this method in the management of stonefish envenomation [19, 23].
Stonefish venom is apparently thermolabile above 50°c (122 °F) [24, 25], However, it has been scientifically proven that exposure to water at 50 °C causes 3rd degree burns in humans in less than 9 min [22]. Cases of iatrogenic burns have been described in the literature [26, 27]. We also have one case of iatrogenic burn in our series, a woman who was the victim of a second-degree burn during her pain management at the emergency department. Despite in vivo studies supporting thermolability in stonefish envenomations [24, 25], it would appear that in the case of Synanceia verrucosa, the efficacy of HWI has been called into question.
Where there is uncertainty about the species involved, HWI may be effective for some envenomations. When in doubt, if HWI is proposed as a first-line treatment, it is imperative to control the temperature of the water, or at least to test it on the unaffected limb to prevent burns.
Local nerve block anesthesia
The aim of nerve block anesthesia is to inhibit the transmission of the impulse distal to a nerve terminal, thus putting an end to the pain signal perceived by the cortex [28]. In cases of stonefish envenomation, pain in the affected limb is completely relieved following administration of a local nerve block. The anaesthetic can be used for 4 to 6 h, allowing the patient to get over the intense pain.
We are convinced, as are our colleagues Maillaud et al. [13, 16], that locoregional nerve block anaesthesia is an effective solution to intense pain. Very often, there is a excess of level I, II and III analgesics, without any efficacy in bringing the victim back into a comfort zone. Opioids are time-consuming for healthcare teams, with the rigorous traceability of a highly controlled product, dose adjustments in the event of titration and side-effects (e.g., drowsiness, constipation, dizziness, nausea, etc.), and their effectiveness is not very clear. After a local nerve block anesthesia, no other analgesic treatment is administered to the patient, only preventive treatments in case of pain at home.
Skin complications
Aside from iatrogenic burns, we identified 5 cases (3.7%) that later developed dermohypodermitis. Among these, 4 had received antibiotic prophylaxis. In our series of the 135 cases, nearly half did not receive any antibiotic prophylaxis, yet none developed a secondary cutaneous infection distant from the envenomation site. This highlights the importance of thoroughly disinfecting the wound as soon as possible. Overall, the literature indicates a nuanced approach to antibiotic prophylaxis in cases of marine envenomation, and there are no official recommendations [2, 13, 29]. We have no further information from our study that would allow us to decide on this question. We recommend discussing the indications with infectious diseases specialists, who will be able to assess the benefits depending on the circumstances.
Writings from the end of the 19th century relate cases of death on Reunion Island, one most probably due to secondary infection of the limb, the other rapidly after envenomation [30]. However, deaths are still very rare these days. The reputation for lethal stings attributed to stonefish probably derives from cases of death resulting from infectious complications of marine envenomation, rather than from a purely systemic effect of the venom itself, although this cannot be ruled out [13].
Strengths and limitations
The species involved in envenomation is rarely identified. However, only one species of stonefish is found on Reunion Island, Synanceia verrucosa. It is found in the lagoon, camouflages itself and does not flee from man when he approaches, unlike Inimicus filamentosus, a species of venomous fish in the Scorpaenidae family. The latter is a nocturnal fish, so when it is disturbed by a diver or potential predator, it displays the bright colors of its pectoral and caudal fins as a warning and flees into hiding. In the case of the Pterois spp. (Lionfish), confusion is difficult as this species is easily spotted levitating under cavities and prefers reef slopes to the lagoon. Accidents most often involve over-enterprising divers.
Other limitations are related to the retrospective design of the study. The information in patients’ medical files is sometimes lacking in clinical details and circumstances. As part of its missions, the DTV-OI contacts victims whenever possible, and with their consent, in order to obtain further information. This has allowed us to complete and clarify data in a large number of cases.
Perspectives
In the absence of specific recommendations for the management of stonefish envenomations, each hospital manages pain management in its own way. A prospective, multi-center study of pain management could help to determine the effectiveness of the various possible therapies. However, we know that it is very difficult to carry out this type of study in an emergency context. This approach can also be applied to use of antibiotic prophylaxis.
There is a lack of information and awareness among sea users. For example, there are no notice boards near bathing areas to remind people of this risk and the associated recommendations.
In a context of warming waters, we could see an increase in the populations of venomous marine species and an extension of their habitat [31]. For example, the migration of lionfish and stonefish to the Mediterranean Sea via the Suez Canal has already been observed [32]. The rising population, fishing activities and nautical activities, combined with the increasing temperature of the oceans, are contributing to a rise in human interactions with marine species [33].
Conclusion
On Reunion Island, around 30 stonefish bites occur every year. Extreme pain is the main reason why people go to emergency departments, because of the difficulty general practitioners have in managing this intensive pain. Of all the pain relief treatments, local nerve block anesthesia would appear to be the most effective. Complications are rare, but vigilance is required in the case of hypodermatitis, which may be complicated by more severe tissue infections. No deaths occurred in our series.
Acknowledgements
We would like to thank the teams working in the emergency departments of the CHOR and the University Hospital of Reunion Island.
Abbreviations
- CBT
Contrast bath therapy
- DTV-OI
Indian ocean toxicovigilance department
- HWI
Hot water immersion
- neoVTX
Neoverrucotoxin
- VTX
Verrucotoxin
- VAS
Visual analog scale pain scoring
Authors’ contributions
Conceptualization, Adrien Maillot, Adrien Marteau; Data curation, Adrien Maillot, Adrien Marteau; Formal analysis, Adrien Maillot; Investigation, Adrien Maillot, Adrien Marteau, Flore Weisse, Férial Abi Nader; Methodology, Adrien Maillot, Olivier Maillard; Software, Adrien Maillot; Validation, Adrien Maillot, Adrien Marteau, Luc de Haro, Gaël Le Roux; Writing– original draft, Adrien Maillot; Writing– review & editing, Adrien Maillot, Adrien Marteau, Gaël Le Roux, Flore Weisse, Luc de Haro, Olivier Maillard and Férial Abi Nader.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Cases are anonymously registered in the Indian Ocean toxicovigilance department database. Informed consent of the patients is waived in agreement with French law. The Indian Ocean toxicovigilance department database is registered and approved by the French ethic commission on data storage (Commission Nationale Informatique et Libertés, CNIL) which is in line with the GPRD.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harris RJ, Youngman NJ, Chan W, Bosmans F, Cheney KL, Fry BG. Getting stoned: Characterisation of the coagulotoxic and neurotoxic effects of reef stonefish (Synanceia verrucosa) venom. Toxicol Lett. 2021;346:16–22. 10.1016/j.toxlet.2021.04.007. [DOI] [PubMed]
- 2.Maillaud C, Hoang-Oppermann T, Hoang-Oppermann V, Rigot H, Girardot S, Nour M. Is stonefish Synanceia verrucosa envenomation potentially lethal? Toxicon 2020;184:78–82. 10.1016/j.toxicon.2020.05.019. [DOI] [PubMed]
- 3.Armstrong J, Harris K, Wylie C, Isoardi KZ. Suspected stonefish envenomation in Queensland over eight years: a retrospective series. Clin Toxicol. 2023;61:956–60. 10.1080/15563650.2023.2287976. [DOI] [PubMed]
- 4.Kuiter RH, Tonozuka T. Pictorial guide to Indonesian reef fishes. Seaford, Vic., Australia: Zoonetics; 2001.
- 5.Ziegman R, Alewood P. Bioactive components in fish venoms. Toxins 2015;7:1497–531. 10.3390/toxins7051497. [DOI] [PMC free article] [PubMed]
- 6.Garnier P, Goudey-Perrière F, Breton P, Dewulf C, Petek F, Perrière C. Enzymatic properties of the stonefish (Synanceia verrucosa Bloch and Schneider, 1801) venom and purification of a lethal, hypotensive and cytolytic factor. Toxicon 1995;33:143–55. 10.1016/0041-0101(94)00151-w. [DOI] [PubMed]
- 7.Khoo HE. Bioactive proteins from stonefish venom. Clin Exp Pharmacol Physiol 2002;29:802–6. 10.1046/j.1440-1681.2002.03727.x. [DOI] [PubMed]
- 8.Breton P, Delamanche I, Buée J, Goudey-Perriére F, Perriére C. Evidence for a neurotoxic activity in crude venom of the stonefish (Synanceia verrucosa). J Nat Toxins 2002;11:305–13. [PubMed]
- 9.Ueda A, Suzuki M, Honma T, Nagai H, Nagashima Y, Shiomi K. Purification, properties and cDNA cloning of neoverrucotoxin (neoVTX), a hemolytic lethal factor from the stonefish Synanceia verrucosa venom. Biochimica et Biophysica Acta (BBA) - General Subjects 2006;1760:1713–22. 10.1016/j.bbagen.2006.08.017 [DOI] [PubMed]
- 10.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF‐MPQ), Chronic Pain Grade Scale (CPGS), Short Form‐36 Bodily Pain Scale (SF‐36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care & Research 2011;63. 10.1002/acr.20543. [DOI] [PubMed]
- 11.Bijur PE. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10:390–2. 10.1197/aemj.10.4.390. [DOI] [PubMed]
- 12.Lee JY, Teoh LC, Leo SP, et al. Stonefish envenomations of the hand–a local marine hazard: a series of 8 cases and review of the literature. Ann Acad Med Singap. 2004;33:515–20. [PubMed] [Google Scholar]
- 13.Maillaud C, Lefèvre Y. Guide de la faune marine dangereuse d’Océanie. Pirae (Tahiti): Au vent des îles éd.; 2007.
- 14.Wiener S. The production and assay of stonefish antivenene. Med J Australia. 1959;2:715–9. 10.5694/j.1326-5377.1959.tb129465.x. [PubMed]
- 15.Saggiomo SL, Firth C, Wilson DT, Seymour J, Miles JJ, Wong Y. The geographic distribution, venom components, pathology and treatments of Stonefish (Synanceia spp.) Venom. Marine Drugs 2021;19:302. 10.3390/md19060302. [DOI] [PMC free article] [PubMed]
- 16.Maillaud C, Maillard A. Prise en charge des envenimations par poissons-pierres et autres scorpénidés. Journal Européen des Urgences 2004;17:192–7. 10.1016/S0993-9857(04)96072-4.
- 17.Su Yin Adeline Ngo, Ngo SYA, Samuel Ong, Ong SHJ, R Ponampalam, Ponampalam R. Stonefish envenomation presenting to a Singapore hospital. Singap MedJ. 2009;50:506–9. [PubMed]
- 18.Dispositif Toxicovigilance Océan Indien. Les envenimations marines. POINT’ TOX.2020;(15). Repéré à https://054d7d44-09bd-46bb-aa54-acb2fbd0b46f.filesusr.com/ugd/9a211d_e5498f06c18c484abbc55e094879eeaa.pdf. n.d.
- 19.Atkinson PRT. Is hot water immersion an effective treatment for marine envenomation? Emerg Med J. 2006;23:503–8. 10.1136/emj.2005.028456. [DOI] [PMC free article] [PubMed]
- 20.Isbister GK. Venomous fish stings in tropical northern Australia. Am J Emerg Med. 2001;19:561–5. 10.1053/ajem.2001.28325. [DOI] [PubMed]
- 21.Samantha K. Barnett, Barnett SK, Silvia L. Saggiomo, Saggiomo SL, Michael Smout, Smout MJ, et al. Heat deactivation of the stonefish Synanceia horrida venom - implications for first-aid management. Diving and Hyperbaric Med. 2017;47:155–8. 10.28920/dhm47.3.155-158 [DOI] [PMC free article] [PubMed]
- 22.Moritz AR, Henriques FC. Studies of thermal injury: II. The relative importance of time and surface temperature in the causation of cutaneous burns. Am J Pathol. 1947;23:695–720. [PMC free article] [PubMed]
- 23.Niżnik Ł, Jabłońska K, Orczyk M, Orzechowska M, Jasińska J, Smoliniec B, et al. Hot-Water Immersion (HWI) or Ice-Pack Treatment (IPT) as first aid for human envenomation by marine animals? Review of literature. Toxins 2024;16:273. 10.3390/toxins16060273. [DOI] [PMC free article] [PubMed]
- 24.Françoise G-P, Perriere C. Pharmacological properties of fish venoms. Comptes Rendus Des Séances de La Société de Biologie et de Ses Filiales 1998;192:503–48. [PubMed]
- 25.Gwee MCE, Gopalakrishnakone P, Yuen R, Khoo HE, Low KSY. A review of stonefish venoms and toxins. Pharmacology & Therapeutics 1994;64:509–28. 10.1016/0163-7258(94)90022-1. [DOI] [PubMed]
- 26.Abdul Jalil KI, Qayyum MT. Iatrogenic thermal burn after hot water immersion for weever fish sting treatment: a case report. Scars, Burns & Healing 2020;6:205951312094404. 10.1177/2059513120944045. [DOI] [PMC free article] [PubMed]
- 27.Christopher J. Lewis, Lewis CJ, Fiona Wood, Wood FM, A. Goodwin-Walters, Anna Goodwin-Walters, et al. Iatrogenic thermal burns secondary to marine sting treatment. J Burn Care Res. 2020;41:878–81. 10.1093/jbcr/iraa042. [DOI] [PubMed]
- 28.Iederhold BD, Garmon EH, Peterson E, et al. Nerve Block Anesthesia. [Updated 2023 Apr 29]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431109/ n.d. [PubMed]
- 29.Diaz JH. Marine scorpaenidae envenomation in travelers: epidemiology, management, and prevention. J Travel Med. 2015;22:251–8. 10.1111/jtm.12206. [DOI] [PubMed]
- 30.Bottard, Alphonse. Les poissons venimeux, contribution à l’hygiene navale. Impr. du Journal Le Havre, 1889. n.d.
- 31.Needleman RK, Neylan IP, Erickson TB. Environmental and Ecological Effects of Climate Change on Venomous Marine and Amphibious Species in the Wilderness. Wilderness Environ Med. 2018;29:343–56. 10.1016/j.wem.2018.04.003. [DOI] [PubMed]
- 32.Edelist D, Spanier E, Golani D. Evidence for the occurrence of the Indo-Pacific stonefish, Synanceia verrucosa (Actinopterygii: Scorpaeniformes: Synanceiidae), in the Mediterranean Sea. Acta Icth et Piscat 2011;41:129–31. 10.3750/AIP2011.41.2.09.
- 33.Needleman RK, Neylan IP, Erickson TB. Environmental and Ecological Effects of Climate Change on Venomous Marine and Amphibious Species in the Wilderness. Wilderness Environ Med. 2018;29:343–56. 10.1016/j.wem.2018.04.003. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.