Abstract
Familial typical migraine is a common, complex disorder that shows strong familial aggregation. Using latent-class analysis (LCA), we identified subgroups of people with migraine/severe headache in a community sample of 12,245 Australian twins (60% female), drawn from two cohorts of individuals aged 23–90 years who completed an interview based on International Headache Society criteria. We report results from genomewide linkage analyses involving 756 twin families containing a total of 790 independent sib pairs (130 affected concordant, 324 discordant, and 336 unaffected concordant for LCA-derived migraine). Quantitative-trait linkage analysis produced evidence of significant linkage on chromosome 5q21 and suggestive linkage on chromosomes 8, 10, and 13. In addition, we replicated previously reported typical-migraine susceptibility loci on chromosomes 6p12.2-p21.1 and 1q21-q23, the latter being within 3 cM of the rare autosomal dominant familial hemiplegic migraine gene (ATP1A2), a finding which potentially implicates ATP1A2 in familial typical migraine for the first time. Linkage analyses of individual migraine symptoms for our six most interesting chromosomes provide tantalizing hints of the phenotypic and genetic complexity of migraine. Specifically, the chromosome 1 locus is most associated with phonophobia; the chromosome 5 peak is predominantly associated with pulsating headache; the chromosome 6 locus is associated with activity-prohibiting headache and photophobia; the chromosome 8 locus is associated with nausea/vomiting and moderate/severe headache; the chromosome 10 peak is most associated with phonophobia and photophobia; and the chromosome 13 peak is completely due to association with photophobia. These results will prove to be invaluable in the design and analysis of future linkage and linkage disequilibrium studies of migraine.
The classification of migraine has been impeded by the lack of pathognomonic markers, the co-occurrence of migraine subtypes and of migraine and tension-type headache within a single individual, and disputes over the validity of inclusion criteria and the boundaries between migraine and other headache subtypes (Merikangas et al. 1993, 1994). The two major subtypes of migraine defined by International Headache Society (IHS) criteria (Headache Classification Committee of the International Headache Society 1988), migraine without aura (MO) and migraine with aura (MA), frequently co-occur. A recent study found that 42% of individuals with active migraine with aura also reported having migraine attacks with no aura (Launer et al. 1999). Moreover, MO and MA frequently coexist within the same family; a headache center in Italy reported that 45% of families with MA also had members with MO (Mochi et al. 1993). The co-occurrence of the rare but severe familial hemiplegic form of migraine (FHM) and migraine with and without aura within families has also been reported (Joutel et al. 1994; Ophoff et al. 1994). Furthermore, changes in the presenting symptoms of migraine attacks, from hemiplegic to severe headache with or without aura in later life (Ophoff et al. 1994), as well as the development of aura among subjects with MO and the converse (Ophoff et al. 1994; Kallela et al. 2001), suggest overlapping etiology.
No study performed to date has led to the identification of a gene responsible for typical migraine. A gene on 19p13 has been identified for FHM1 (MIM 141500), a rare autosomal dominant subtype of migraine (Joutel et al. 1993; Ophoff et al. 1996). Mutations in this gene, CACNA1A (MIM 601011), a brain-specific P/Q-type calcium-channel gene, account for only a small fraction of all patients with migraine and for 50% of families with the FHM subtype (Ducros et al. 2001). Another 20% of families with FHM show linkage to 1q21-31 (FHM2 [MIM 602481] and FHM3 [MIM 607516]) (Ducros et al. 1997; Gardner et al. 1997). In a recent breakthrough, missense mutations in a chromosome 1q23 gene, ATP1A2 (MIM 182340), which encodes a Na+, K+-ATPase, were identified in four distinct pedigrees with FHM (De Fusco et al. 2003; Vanmolkot et al. 2003).
Several studies have suggested that the 19p13 CACNA1A locus may also be involved in nonhemiplegic migraine (MGR5 [MIM 607508]) (May et al. 1995; Ophoff et al. 1997; Nyholt et al. 1998b; Terwindt et al. 2001), although contradictory data have also been reported (Hovatta et al. 1994; Jones et al. 2001). Recently, loci at 1q31 (MGR6 [MIM 607516]) (Lea et al. 2002), Xq (MGR2 [MIM 300125]) (Nyholt et al. 1998a, 2000; Oterino et al. 2001), and 15q11-q13 (MGR7 [MIM 609179]) (Russo et al. 2005) have been implicated in typical familial migraine. In addition, a number of association studies have shown linkage and/or linkage disequilibrium between various gene loci and either MA or MO (Pardo et al. 1995; Peroutka et al. 1997; Del Zompo et al. 1998; Ogilvie et al. 1998; Kowa et al. 2000; Lea et al. 2000; Paterna et al. 2000; McCarthy et al. 2001; Tzourio et al. 2001; Yilmaz et al. 2001; Rainero et al. 2002; Trabace et al. 2002; Kusumi et al. 2003; Mochi et al. 2003; Colson et al. 2004, 2005). Unfortunately, most of these studies have remained single reports and await confirmatory replication studies or have been contradicted by studies done by other groups.
The first genomewide linkage screen for typical familial MA genes was conducted by a group in Helsinki (Wessman et al. 2002). They studied a sample of 50 Finnish families (comprising 252 individuals with MA) and found significant evidence for linkage on 4q24 (MGR1 [MIM 157300]). Interestingly, a genomewide scan in Iceland of 289 patients with MO also showed significant linkage to the chromosome 4q region (Bjornsson et al. 2003), further supporting the existence of trait loci common to both major IHS classes of migraine.
Three additional published genomewide screens have identified several new loci, with significant linkage on 6p12.2-p21.1 (MGR3 [MIM 607498]) (Carlsson et al. 2002), 11q24 (Cader et al. 2003), and 14q21.2-q22.3 (MGR4 [MIM 607501]) (Soragna et al. 2003), suggesting additional migraine genes in these regions. Hence, there is a growing body of evidence supporting the existence of both phenotypic and genetic heterogeneity, with multiple genes contributing to migraine susceptibility.
To diagnose migrainous headache more accurately and to examine whether MO and MA are two separate entities or not, we recently performed latent-class analysis (LCA)—a statistical method best characterized as a categorical analog of factor analysis for finding subtypes of related cases (latent classes) from multivariate categorical data (Rindskopf and Rindskopf 1986)—to investigate the presence and composition of migraine symptom subgroups in our twin sample (Nyholt et al. 2004).
Migraine data were obtained during the course of an extensive, semistructured telephone interview that included diagnostic assessments of migraine. Participants answering “yes” to the question of whether they have ever had migraine or recurrent attacks of headache then answered a number of questions, relating to their headaches, that were developed by an experienced migraine researcher (K.R.M.) on the basis of IHS diagnostic criteria (tables 1 and 2). The interview yielded diagnoses for MO and MA, with the use of visual prodromal symptoms as an index of MA.
Table 1.
IHS Diagnostic Criteria for MO[Note]
| Criteria for MO |
| A. At least five attacks fulfilling B through D |
| B. Headache lasting 4–72 h (untreated or unsuccessfully treated) |
| C. Headache has at least two of the following characteristics: |
| 1. Unilateral location |
| 2. Pulsating quality |
| 3. Moderate/severe (a) or prohibitive (b) intensity (inhibits or prohibits daily activities) |
| 4. Aggravation by walking stairs or by similar routine physical activities |
| D. During headache at least one of the following is present: |
| 1. Nausea and/or vomiting |
| 2. Photophobia (a) and phonophobia (b) |
Note.— Excerpted from IHS classification of headache (Headache Classification Committee of the International Headache Society 1988).
Table 2.
The 10 Symptom Response Variables Based on IHS Diagnostic Criteria
| Abbreviationfor Variable | Codea | Description |
| >5 Episodes | A | At least five migraines/episodes of headache during lifetime |
| 4–72 h | B | Average typical migraine/headache lasts between 4 and 72 h |
| Unilateral | C1 | Headache usually occurs on one side of the head |
| Pulsating | C2 | Usual headache pain is described as throbbing, pulsating, or pounding |
| Moderate/severe | C3a | Pain associated with headache is described as moderate or severe |
| Prohibitive | C3b | Headaches inhibit or prohibit daily activities |
| Nausea/vomiting | D1 | Associated and recurrent attacks of nausea, vomiting, or diarrhea |
| Photophobia | D2a | Enhanced sensitivity to light |
| Phonophobia | D2b | Enhanced sensitivity to noise |
| Aura | … | Associated and recurrent visual problems such as blurring, showers of light, blind spots, or double vision |
Codes correspond to the outline of diagnostic criteria in table 1.
In our younger cohort of twins born in 1964–1971 (3,438 females and 2,774 males), the use of IHS diagnostic criteria yielded an MO prevalence of 15.3% (20.4% female; 9.0% male), which is comparable to that found in other large epidemiologic studies in similar Western populations (Stewart et al. 1992), including a recent population-based Australian study (the Blue Mountains Eye Study [n=3,654]) that found that 22% of women and 9.6% of men satisfied the IHS criteria for MO (Wang et al. 1997). The total same-sex DZ relative risks (RRs)—applicable to first-degree relatives in the general population—associated with the IHS groups were surprisingly similar, with an RR of 1.53 (95% CI 0.61–3.83) for MO-MO and 1.77 (95% CI 1.00–3.13) for MA-MA (Nyholt et al. 2004).
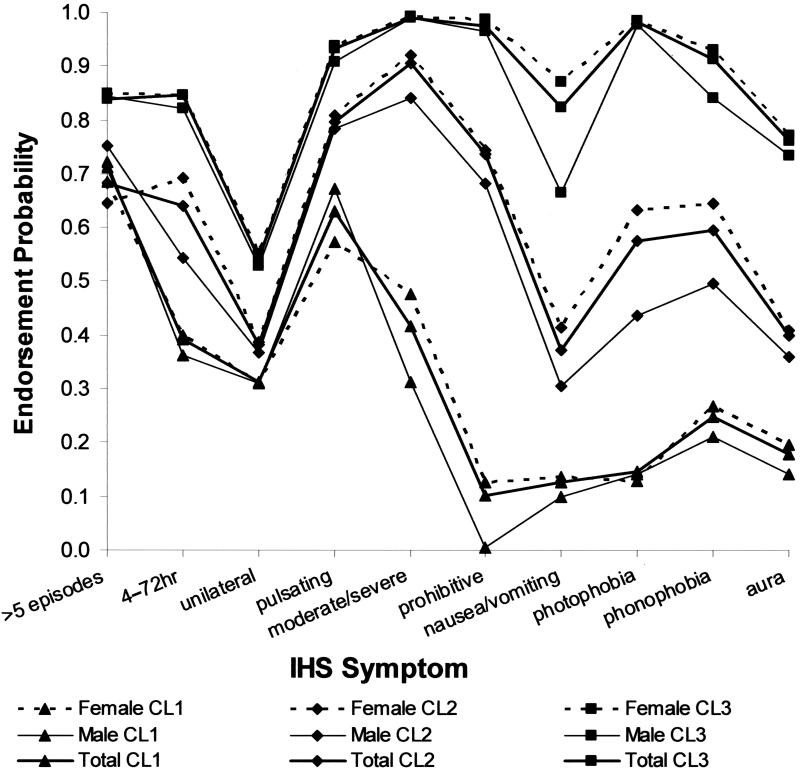
LCA, performed using the Latent GOLD 2.0 package (Statistical Innovations), identified one asymptomatic class (CL0) and three major symptomatic classes (fig. 1), representing a mild form of recurrent nonmigrainous headache (CL1); a moderately severe form of migraine, typically without visual aura, loading (i.e., had endorsement probability ⩾0.5) on all IHS MO symptoms except unilateral location and nausea/vomiting (CL2); and a severe form of migraine, typically with visual aura, loading on all IHS symptoms (CL3). Of particular importance is that although aura was often associated with other and more severe neurological symptoms and was predominantly found in latent class CL3, almost one quarter of CL3 individuals did not report aura. Furthermore, aura was present in 39.3% of individuals in CL2. Therefore, the LCA did not specifically separate MO from MA. Instead, the LCA classifications are based on the severity and combination of symptoms and do not support the hypothesis that MO and MA are separate subtypes. Moreover, both traditional (principal components) factor analysis using SPSS and latent factor analysis using Latent GOLD indicated that a single major factor best fit the data, supporting the existence of a severity continuum from mild to severe headache, of which the LCA classes and IHS classes MO and MA are a part. In other words, an individual’s liability to migraine is of a single dimension representing the contribution of all genetic and environmental influences; individuals whose liability exceeds a certain threshold manifest the disorder, with the more severely affected individuals assumed to have a higher liability than the less severely affected individuals. Also consistent with the threshold model is that three times as many females than males had migraine; thresholds for females were significantly lower than those for males. Therefore, in searching for predisposing genes, we should expect to find some trait loci common to both major classes of IHS migraine, with perhaps additional loci, or more-severe alleles, associated with more-severe types, such as MA or CL3 (Nyholt et al. 2004).
Figure 1.
Profile plot for the three symptomatic classes (CL1, CL2, and CL3) under the four-class model. Endorsement probabilities indicate the proportion of individuals in each class presenting with each symptom. All endorsement probabilities for CL0 were <0.005 (data not shown). Descriptions of symptom abbreviations are given in table 2.
We classified 407 individual twins (203 female [5.9% of total female sample]; 204 male [7.4% of total male sample]) in CL1, 1,267 twins (781 [22.7%] female; 486 [17.5%] male) in CL2, and 991 twins (793 [23.1%] female; 198 [7.1%] male) in CL3. Therefore, the prevalence of migrainous headache identified by LCA classification (hereafter, “LCA migraine,” which represents CL2 and CL3) was 36.5% (45.8% female; 24.7% male). Using the total same-sex data, the relative risks associated with the LCA groups were 1.40 (95% CI 1.03–1.90) for CL2-CL2 and 2.18 (95% CI 1.57–3.03) for CL3-CL3 (Nyholt et al. 2004). Importantly, these data did not support the presence of genetic sex-specific effects (i.e., effects expressed in one sex but not in the other) or significant sex differences in the magnitude of genetic influences (i.e., sex limitation) on risk of migraine.
The ability of LCA to weight each symptom by use of endorsement frequencies and to obtain for each symptom response profile the associated posterior class-membership probability allowed more individuals to be classified (table 3). That is, although the LCA and IHS classifications were highly correlated (Spearman’s correlation = 0.97), 1,305 individuals whose condition did not satisfy IHS criteria were considered to be affected under the LCA classification (i.e., were in CL2 or CL3). Importantly, the heritability (h2) estimate (by use of structural equation modeling) in our sample under the four-group LCA scheme was 0.40 (95% CI 0.29–0.46), compared with 0.36 (95% CI 0.22–0.42) under the IHS scheme.
Table 3.
IHS versus LCA Diagnoses[Note]
|
IHS Diagnosis |
||||
| LCADiagnosis | Negative | Positive | MO | MA |
| CL0 | 3,547 | … | … | … |
| CL1 | … | 407 | … | … |
| CL2 | … | 1,010 | 182 | 75 |
| CL3 | … | 295 | 173 | 523 |
Note.— “Negative” and “Positive” denote “No” and “Yes” responses to the screening question “Have you ever had migraine or recurrent attacks of headache?” Consequently, individuals who answered “No” gave no symptom data.
A slight increase in heritability was observed after the individuals who screened negative [CL0] were grouped with the latent class CL1, producing a heritability estimate of 0.43 (95% CI 0.29–0.50). This strategy makes sense conceptually, since, although we would not expect individuals who screen negative for “migraine or recurrent attacks of headache” to experience diagnostic criteria sufficient for inclusion in CL2/CL3, they may experience enough symptoms sufficient for inclusion in CL1. Moreover, the precision of the heritability estimate for the three-group LCA scheme remains similar to that for the four-group LCA scheme, which suggests no loss of genetic information.
In contrast, the grouping of individuals who screened negative with those who screened positive, produced a heritability estimate of 0.31 (95% CI 0–0.41) and a decrease in the precision of the heritability estimate (as reflected in the expanded CI), compared with the four-group IHS scheme. This suggests a poorer correspondence between genetic risk and IHS grouping.
Higher heritability was still observed for the LCA scheme (h2=0.41; 95% CI 0.23–0.49), compared with the IHS scheme (h2=0.33; 95% CI 0.05–0.44), when a clinically relevant “unaffected-affected” dichotomy was used. We therefore hypothesized that use of our LCA-based diagnostic scheme would provide considerably more power than use of the IHS criteria to identify genes underlying migraine susceptibility (Nyholt et al. 2004).
The present linkage study used an LCA-derived migraine sample comprising two cohorts drawn from the Australian Twin Registry. In 1993–1995, a telephone interview that included a diagnostic assessment of psychiatric disorders, including alcohol use and abuse, anxiety, depression, and phobias, was administered to an older cohort of twins, born in 1902–1964. A total of 5,996 individual twins completed the 1993–1995 interview (Heath et al. 1997). Between 1996 and 2000, a younger cohort of twins (born in 1961–1975) underwent a similar extensive semistructured telephone interview, designed to assess physical, psychological, and social manifestations of alcoholism and related disorders (Heath et al. 2001); 6,265 individual twins completed the interview. Both cohort samples were unselected with regard to personal or family history of alcoholism or other psychiatric or medical disorders. Migraine symptom data were obtained in the course of the telephone interviews. For the combined sample, the mean age at interview was 37.5±11.3 years (range 23–90 years). Although the wording of the questions was identical for both cohorts, the younger cohort was asked questions relating to all 10 symptoms in tables 1 and 2, whereas the older cohort were not asked questions relating to having at least five migraine/episodes of headache during lifetime (“>5 episodes”), average typical migraine/headache lasting between 4 and 72 h (“4–72 h”), and pain associated with headache described as moderate or severe (“moderate/severe”).
The younger and older cohort data were combined, thus allowing the LCA to impute class membership in the older cohort on the basis of the pattern of all 10 symptoms observed in the younger cohort. To examine the accuracy of imputed class memberships, we compared the classification results for the younger data set using all 10 available IHS symptoms with the classification results for the younger data set using only the 7 IHS symptoms that were available for the older cohort. Compared with analyses using all 10 symptoms, analyses using only 7 symptoms correctly classified 98.5% and 96.0% of individuals as unaffected and affected, respectively, which indicates that the three missing symptoms in the older cohort would have negligible effect on the accuracy of individual LCA migraine diagnoses.
LCA of the combined younger and older data set (12,245 individuals) identified 494 concordant affected DZ twin pairs (152 CL2-CL2, 217 CL2-CL3, and 125 CL3-CL3), 228 extreme discordant DZ twin pairs (CL0/1-CL3), and 194 extreme concordant MZ twin pairs (CL3-CL3) for LCA migraine.
The current study included linkage analysis using LCA migraine diagnoses and genotypic data from a compilation of four smaller genome scans performed for other studies at the Queensland Institute of Medical Research. Genotyping for the four scans was done at Gemini Genomics (426 microsatellite markers), Sequana Therapeutics (519 markers), the Center for Mammalian Genetics at the Marshfield Clinic Research Foundation (776 markers), and the University of Leiden (435 markers). Recruitment of participants for these studies was primarily based on participant involvement in previous phenotype collection studies. There was considerable overlap between the participants in the four studies and in the four marker sets used (see below). As a result, genotypic data for a subset of the younger and older cohorts was available. DNA collection, genotyping, and data-cleaning methods are discussed in brief below and in more detail elsewhere (Zhu et al. 2004; B. K. Cornes, S. E. Medland, K. I. Morley, M. A. R. Ferriera, S. Gordon, G. Zhu, D. L. Duffy, M. Campbell, H. Beeby, G. W. Montgomery, A. J. Birley, and N. G. Martin, unpublished data).
Pedigree structures for each scan were examined using Graphic Representation of Relationships (GRR) (Abecasis et al. 2001) and RELPAIR (Epstein et al. 2000; Duren et al. 2003), to identify inconsistencies between the genotypic data and pedigree relationships. Once any discrepancies were resolved, data for the four scans were merged and then checked again for pedigree errors by GRR and for Mendelian inconsistencies by SIB-PAIR (Duffy 2002). The combined genome scan data included 458 markers that were typed in two or more scans, which were included separately on the genetic map for the scan, separated by a very small distance (0.001 cM). The consistency of genotype information between these 458 markers was checked via cross-tabulations of allele calls between different scans. Markers with genotypic data inconsistent between different genome scans were removed from further analysis. Unlikely genotypes were identified and wiped using MERLIN (Abecasis et al. 2002). GENEHUNTER (Kruglyak et al. 1996) and MENDEL (Lange et al. 1988) were used to identify and examine potential map errors. Map positions were in Kosambi cM, estimated via locally weighted linear regression from the NCBI build 34.3 physical map positions and from published deCODE and Marshfield genetic map positions (Kong et al. 2004). Where the results suggested inconsistencies between genetic map distances and recombination fractions, the primer sequences for all markers in the region were blasted against the entire human genome sequence (Ensembl NCBI build 34.3). The genetic map was then revised to include the updated physical positions of all markers in problematic regions, with new map distances interpolated as above.
With the use of the revised map, the original genotype data (with inconsistent duplicated markers removed) were cleaned of unlikely genotypes by use of MERLIN, and map errors were resolved using GENEHUNTER. The cleaned genome-scan data included 1,881 markers, of which 422 were duplicates, leaving a total of 1,459 unique markers. The combined genome scan included a total of 5,199 individuals from 1,593 families.
Of the total 1,593 families for whom migraine symptom data were available, 426 families contained at least one affected (CL2/CL3) concordant or one discordant nonidentical-twin or sibling pair, 330 families contained one unaffected concordant sib pair, and the remaining families were uninformative for linkage (i.e., had <2 genotyped children for whom LCA migraine diagnoses were available). These 756 families contained 556 affected and 988 unaffected individuals. With allowance for nonindependence among sib pairs derived from the same sibship (i.e., a sibship of size S being equivalent to S-1 independent sib pairs [Suarez and Hodge 1979]), the 756 families informative for linkage to LCA migraine contained 790 independent sib pairs (130 affected concordant, 324 discordant, and 336 unaffected concordant).
For the linkage analyses, allele frequencies for marker loci were estimated from the founders across all 1,593 families by use of PEDMANAGER software (available online; see Web Resources). Autosomal linkage data were analyzed using the latest available versions of SOLAR (v2.1.4) (Almasy and Blangero 1998) and MERLIN-regress (v0.10.1) (Abecasis et al. 2002; Sham et al. 2002) analysis packages.
SOLAR uses a liability-threshold model within a variance-components (VC) framework to perform linkage analysis for a dichotomous trait (Duggirala et al. 1997). Briefly, the threshold model assumes a latent continuous variable (“liability”) underlying a categorical trait. The threshold can be regarded as the z value of the normal distribution that divides the area under the curve in such a way that it gives the correct proportion of individuals in each (diagnostic) group, thus reflecting the prevalence of each group (Neale and Cardon 1992). The tetrachoric correlation, also termed “correlation of liability,” assumes that underlying the observed dichotomous distribution of affection status is a continuous, normally distributed latent liability (Kendler 1993). That is, the tetrachoric correlation is an estimate of the correlation between two latent variables, where each latent variable is assumed to have a bivariate normal distribution. SOLAR LOD scores obtained via this approach do not require specification of a penetrance model and are asymptotically distributed the same way as standard LOD scores. Hence, nominal pointwise thresholds of P=.01 and P=.05 are equivalent to SOLAR LOD scores of 1.18 and 0.59, respectively (Nyholt 2000).
In addition to the SOLAR liability threshold model, the “model-specification-free” MERLIN-regress statistic was chosen because it has been shown to be comparable in power to the most powerful QTL linkage approach (i.e., VC) while being more robust to non–normally distributed trait values (Sham et al. 2002). Furthermore, the computationally simple MERLIN-regress statistic is ideally suited for empirical analyses (e.g., gene-dropping simulations) to obtain sample-specific significance levels. Indeed, multipoint analysis of our observed genomewide linkage data with SOLAR took ∼3.5 h on our Linux server, whereas it took a little less than 5 min with MERLIN-regress.
Affected individuals (CL2/CL3) were given a trait value of 1, and unaffected individuals (CL0/CL1) were given a value of 0. The validity of this, and indeed that of the original regression Haseman-Elston approach (Haseman and Elston 1972) for binary traits, has been pointed out numerous times (Elston et al. 2005).
To obtain empirical estimates of genomewide significance levels, simulations were performed using the pedigree structures in the data set and the observed patterns of genotyping, including any missing genotypes. These simulations allowed us to take account of uneven marker spacing and informativeness (see the work of Sawcer et al. [1997] and Kruglyak and Daly [1998] for a discussion of the utility of empirical significance levels in linkage analysis) and to calculate the probability of observing one or more peaks of a certain height (Wiltshire et al. 2002). Data for 5,000 simulated genome scans were generated using MERLIN-regress under the assumption that there were no susceptibility loci; each replicate was analyzed in the same way as the observed data, and the highest peak for each chromosome was recorded. The empirical significance level of an observed LOD score was then estimated by counting the proportion of genome scans containing one or more peaks of that size. The cut-off for suggestive linkage (MERLIN-regress LOD=1.62) was calculated as the LOD score that was observed on average once per genome scan (i.e., 5,000 times across the 5,000 replicates, or the 5,000th highest LOD score), thus representing the average maximum peak size expected once per genome scan by chance alone (Lander and Kruglyak 1995). The significant linkage threshold (MERLIN-regress LOD=2.99) was defined as the score occurring with probability 0.05 in a genome scan (Lander and Kruglyak 1995) (i.e., 250 peaks of equal or greater size observed across the 5,000 simulations, or the 250th highest LOD score). For confirmation (replication) of previously reported significant linkage findings, a nominal P value of .01 was used (Lander and Kruglyak 1995). We also included LOD score thresholds for nominal P=.05 to assist comparison with previous and future linkage studies, as recommended by Lander and Kruglyak (1995).
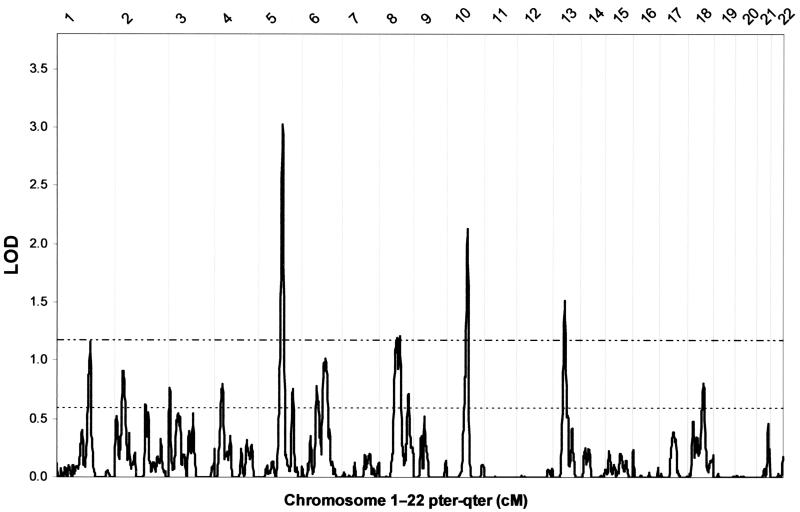
SOLAR multipoint LOD scores (by use of exact multipoint identity by descent [IBD] values obtained from MERLIN) calculated at 1-cM increments are presented in figure 2. The highest LOD score (table 4) was obtained on chromosome 5 at 115 cM from the pter (LOD=3.03; asymptotic pointwise P=9.37×10-5). The next highest LODs were found on chromosome 10 at 98 cM (LOD=2.13; P=8.68×10-4), chromosome 13 at 56 cM (LOD=1.52; P=.0041), chromosome 8 at 98 cM (LOD=1.22; P=.0089), chromosome 1 at 160 cM (LOD=1.16; P=.010), and chromosome 6 at 101 cM (LOD=1.02; P=.015). No other regions produced LOD scores >1.
Figure 2.
Results of SOLAR genomewide multipoint linkage analysis for LCA migraine, showing thresholds for nominal P=.01 (dash-dot-dot line) and P=.05 (dotted line).
Table 4.
Summary of Genomewide Linkage Scan Results
| Chromosome | Map Position(cM) | SOLARLOD | Map Position(cM) | MERLIN-regressLOD | NearestMarker | Marker Position(cM) |
| 1 | 160 | 1.16 | 159 | 1.53 | D1S1679 | 159.92 |
| 5 | 115 | 3.03 | 115 | 3.70a | D5S2501 | 116.63 |
| 6 | 101 | 1.02 | 102 | 1.22 | D6S1056 | 100.55 |
| 8 | 98 | 1.22 | 97 | 1.77b | D8S270 | 97.85 |
| 10 | 98 | 2.13 | 97 | 2.32b | D10S2327 | 98.72 |
| 13 | 56 | 1.52 | 56 | 1.63b | D13S1807 | 56.15 |
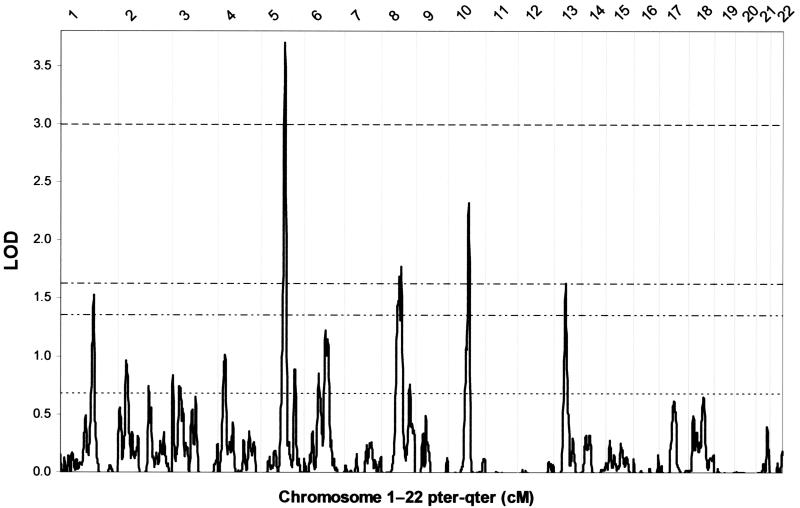
MERLIN-regress multipoint LOD scores calculated at 1-cM increments are presented in figure 3. The highest LOD score (table 4) was again obtained on chromosome 5 at 115 cM from the pter (LOD=3.70). The next highest LODs were found on chromosome 10 at 97 cM (LOD=2.32), chromosome 8 at 97 cM (LOD = 1.77), chromosome 13 at 56 cM (LOD=1.63), chromosome 1 at 159 cM (LOD=1.53), and chromosome 6 at 102 cM (LOD=1.22). As can be seen by comparing figures 2 and 3, the SOLAR and MERLIN-regress LOD scores were highly correlated (r=0.99). The resulting simple linear regression equation (1.1509×SOLAR LOD-0.0015=MERLIN-regress LOD) is an excellent predictor of small-to-moderate values. This equation estimated that the nominal P=.01 and P=.05 SOLAR LOD scores of 1.18 and 0.59 are equivalent to MERLIN-regress LOD scores of 1.35 and 0.68, respectively.
Figure 3.
Results of MERLIN-regress genomewide multipoint linkage analysis for LCA migraine, showing thresholds obtained via simulation for significant linkage (dashed line) and suggestive linkage (dash-dot line). Thresholds estimated via linear regression for nominal P=.01 (dash-dot-dot line) and P=.05 (dotted line) are also displayed.
The MERLIN-regress LOD scores were slightly higher than the SOLAR VC LOD scores. This increase could be explained by the fact that the regression test has been shown to be more powerful than VC in sibships of size ⩾3. Alternatively, the regression test has been shown to produce a slightly inflated type I error rate for a non–normally distributed trait in combination with incomplete (<100%) IBD information (Sham et al. 2002). Given that our sample contained 24 sibships of size 3 and 5 sibships of size 4 and that our trait was clearly not normally distributed, the increase in MERLIN-regress LOD scores may be the result of either of these two explanations or a combination of both. It was therefore important to verify MERLIN-regress significance levels by Monte Carlo methods (i.e., gene-dropping simulations).
Results of our 5,000 simulations indicated that the chromosome 5 peak easily surpasses our threshold for significant linkage, with only 56 peaks ⩾3.70 observed (genomewide P=.0112). The chromosome 10 peak is highly suggestive of linkage, with only 1,106 peaks ⩾2.78 observed. The chromosome 8 and chromosome 13 peaks also surpass our suggestive threshold, with 3,606 peaks ⩾1.77 and 4,996 peaks ⩾1.63 observed, respectively, whereas chromosome 1 and chromosome 6 peaks fall short of our suggestive threshold with 6,275 peaks ⩾1.53 and 11,984 peaks ⩾1.22 observed, respectively. Given that these simulations indicate, on average, only one LOD ⩾1.63 and that ∼1.3 LODs ⩾1.53 and 2.4 LODs ⩾1.22 are expected by chance, our data suggest the presence of multiple loci contributing to migrainous headache.
Whereas the chromosome 5, 8, and 10 loci are novel, the chromosome 6 region (major peak SOLAR LOD of 1.02 [P=.015] at 101 cM; secondary peak LOD of 0.85 [P=.024] at 71 cM) overlaps the 6p12.2-p21.1 (67.45–77.42 cM) critical region previously reported for a large Swedish family with 30 individuals who have MO or MA, spanning four generations (MGR3 [MIM 607498]) (Carlsson et al. 2002), which adds support to the presence of a QTL in this region. An even more interesting finding concerns the chromosome 1 peak at 159 cM, since it is within 3 cM of the FHM-implicated ATP1A2 gene (De Fusco et al. 2003; Vanmolkot et al. 2003), thus potentially implicating ATP1A2 in familial typical migraine for the first time. We did not find any support for linkage at other previously reported loci.
To investigate the effect of collapsing the CL2 and CL3 classes into one affection class, we reanalyzed our genomewide linkage data using a three-category phenotype CL0/1, CL2, and CL3. MERLIN multipoint LOD scores for this trichotomous phenotype were remarkably similar to the LOD scores obtained for our primary dichotomous LCA migraine phenotype (data not shown). Therefore, as indicated by our previous heritability analyses, our dichotomous LCA migraine phenotype provides a stable and accurate correspondence between genetic risk and migrainous headache.
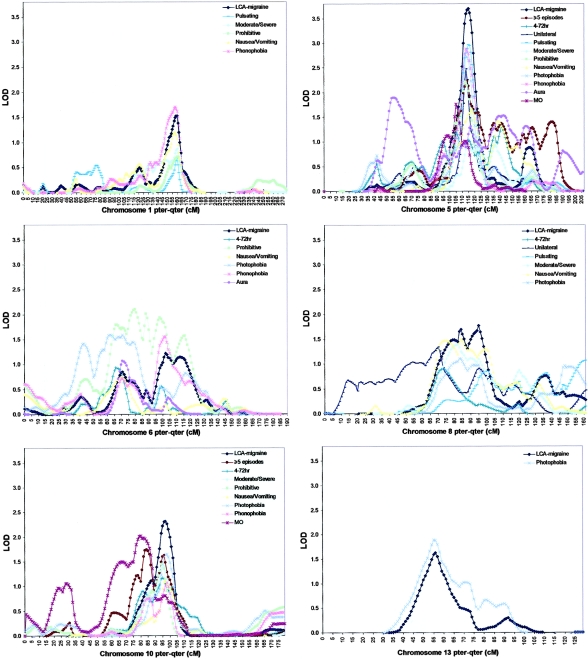
During our work on the classification and genetic epidemiology of migraine and its symptoms, genetic analysis of questionnaire data revealed that the answer to our screening question and each of the 10 IHS symptoms are heritable (h2=0.35–0.39). To see whether certain symptoms are more associated with our linkage peaks, we performed linkage analyses for LCA migraine conditional on each individual symptom (i.e., for each symptom, affected individuals must have both the individual symptom and LCA migraine). Figure 4 shows MERLIN-regress multipoint LOD scores for LCA migraine and individual IHS symptoms, with pointwise P⩽.05 for our six most interesting chromosomes.
Figure 4.
Results of MERLIN-regress chromosome-specific multipoint linkage analysis for LCA migraine and subphenotypes reaching nominal P⩽.05.
The subphenotype analyses clearly indicate that individual symptoms are differentially associated with particular linkage peaks in our data. Specifically, 5 of the 10 IHS symptoms produced nominally significant LOD scores at the chromosome 1 locus, with “nausea/vomiting” and “phonophobia” being the symptoms most associated. The chromosome 5 region probably contains a general migrainous headache gene, with all 10 IHS symptoms producing LOD scores with P⩽.05. In fact, although strict IHS diagnoses could only be determined for the younger cohort (because the older cohort was not asked questions relating to “>5 episodes,” “4–72 h,” and “moderate/severe”), a LOD of 1.76 was still obtained on chromosome 5 for IHS MO. The chromosome 6 locus is associated with six of the IHS symptoms, especially “prohibitive” and “photophobia.” The chromosome 8 locus is also associated with six IHS symptoms, in particular “nausea/vomiting” and “moderate/severe.” Finally, 7 of the 10 symptoms, plus IHS MO, are associated with the chromosome 10 locus, whereas the chromosome 13 peak is completely due to association with “photophobia.”
To further examine the relationship between individual symptoms and linkage to our six most interesting chromosomes, we performed subphenotype analyses for each symptom, in which affected individuals must simply have the individual symptom, regardless of LCA diagnosis (data not shown). These analyses further suggest that individual symptoms may be associated with particular linkage peaks in our data. Specifically, the chromosome 1 locus is most associated with “phonophobia” (LOD=1.79); the chromosome 5 peak is predominantly associated with “pulsating” (LOD=3.41); the chromosome 6 locus is associated with “prohibitive” (LOD=1.68) and “photophobia” (LOD=1.70); the chromosome 8 locus is associated with “nausea/vomiting” (LOD=1.46) and “moderate/severe” (LOD = 1.27); the chromosome 10 peak is most associated with “phonophobia” (LOD=1.44) and “photophobia” (LOD=1.63); and the chromosome 13 peak is completely due to association with “photophobia” (LOD = 1.55).
Although there is considerable correlation between the symptoms (i.e., by application of the approach of Cheverud [2001] and Nyholt [2004] to the subphenotype analyses conditioned on LCA migraine, the 10 IHS symptoms are equivalent to analyzing ∼2.4 independent phenotypes, whereas, for the IHS subphenotype analyses, regardless of LCA migraine, the 10 symptoms are equivalent to ∼5.7 independent phenotypes), we realize that the subphenotype analyses described above provide ample opportunity for false-positive results, given the amount of multiple testing. Nevertheless, these exploratory results provide tantalizing hints of the phenotypic and genetic complexity of migraine and will prove to be invaluable in the design and analysis of our future linkage and linkage disequilibrium studies. For example, we shall stratify our future fine-mapping analyses according to the individual symptoms associated with each implicated genomic region.
Moreover, to aid the replication of previously identified potential susceptibility loci, we strongly advocate that researchers analyze the individual symptoms of phenotypically complex traits such as migraine. By providing results from individual symptom analyses of implicated regions, researchers may examine whether failure to replicate a previous study's finding may be the result of genetic (locus) heterogeneity or differences in the subphenotypic makeup of the individual samples.
Finally, given the higher diagnostic specificity, the higher heritability, and the potential for larger sample sizes in our LCA-based approach, we favor this approach over a more restrictive IHS criteria–based classification. Our ongoing collection of DNA and more-detailed symptom data (which will allow strict IHS diagnosis of MO and MA) from the aforementioned 916 families, containing 494 DZ twin pairs concordant affected for LCA migraine, 228 extreme discordant DZ twin pairs, 194 extreme concordant MZ twin pairs, and additional siblings (86% mutually exclusive to the sample analyzed here), will thus provide an invaluable resource for replication and further investigation of the relationship between previously reported migraine susceptibility gene regions and individual migraine symptoms.
Acknowledgments
This research was supported in part by National Institute on Alcohol Abuse and Alcoholism (United States) grants AA007535, AA013320, AA013326, AA014041, AA07728, AA10249, and AA11998 and by National Health and Medical Research Council (NHMRC) (Australia) grants 941177, 951023, and 241916. D.R.N. was supported in part by NHMRC R. D. Wright Fellowship 339462. We sincerely thank Dixie Statham; Alison MacKenzie, for project coordination; Anjali Henders and Megan Campbell, for managing sample processing; David Smyth and Scott Gordon, for data management; and the twins, for their generous participation. We also acknowledge and thank the Mammalian Genotyping Service (Director: Dr. James Weber), for microsatellite marker genotyping; Dr. Eline Slagboom and Dr. Bas Heijmans, for the Leiden genome scan; Dr. Peter Reed, for the Gemini genome scan; and Dr. Jeff Hall, for the Sequana genome scan.
Web Resources
The URLs for data presented herein are as follows:
- Ensembl, http://www.ensembl.org/ (for NCBI build 34.3)
- Online Mendelian Inheritance in Man (OMIM), http://www.ncbi.nlm.nih.gov/Omim/ (for FHM1, FHM2, FHM3,CACNA1A, ATP1A2,MGR1, MGR2, MGR3, MGR4,MGR5, MGR6, and MGR7)
- PEDMANAGER, http://www.broad.mit.edu/ftp/distribution/software/pedmanager/
References
- Abecasis GR, Cherny SS, Cookson WO, Cardon LR (2001) GRR: graphical representation of relationship errors. Bioinformatics 17:742–743 [DOI] [PubMed] [Google Scholar]
- ——— (2002) Merlin—rapid analysis of dense genetic maps using sparse gene flow trees. Nat Genet 30:97–101 [DOI] [PubMed] [Google Scholar]
- Almasy L, Blangero J (1998) Multipoint quantitative-trait linkage analysis in general pedigrees. Am J Hum Genet 62:1198–1211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjornsson A, Gudmundsson G, Gudfinnsson E, Hrafnsdottir M, Benedikz J, Skuladottir S, Kristjansson K, Frigge ML, Kong A, Stefansson K, Gulcher JR (2003) Localization of a gene for migraine without aura to chromosome 4q21. Am J Hum Genet 73:986–993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cader ZM, Noble-Topham S, Dyment DA, Cherny SS, Brown JD, Rice GP, Ebers GC (2003) Significant linkage to migraine with aura on chromosome 11q24. Hum Mol Genet 12:2511–2517 [DOI] [PubMed] [Google Scholar]
- Carlsson A, Forsgren L, Nylander PO, Hellman U, Forsman-Semb K, Holmgren G, Holmberg D, Holmberg M (2002) Identification of a susceptibility locus for migraine with and without aura on 6p12.2-p21.1. Neurology 59:1804–1807 [DOI] [PubMed] [Google Scholar]
- Cheverud JM (2001) A simple correction for multiple comparisons in interval mapping genome scans. Heredity 87:52–58 [DOI] [PubMed] [Google Scholar]
- Colson NJ, Lea RA, Quinlan S, MacMillan J, Griffiths LR (2004) The estrogen receptor 1 G594A polymorphism is associated with migraine susceptibility in two independent case/control groups. Neurogenetics 5:129–133 [DOI] [PubMed] [Google Scholar]
- ——— (2005) Investigation of hormone receptor genes in migraine. Neurogenetics 6:17–23 [DOI] [PubMed] [Google Scholar]
- De Fusco M, Marconi R, Silvestri L, Atorino L, Rampoldi L, Morgante L, Ballabio A, Aridon P, Casari G (2003) Haploinsufficiency of ATP1A2 encoding the Na+/K+ pump α2 subunit associated with familial hemiplegic migraine type 2. Nat Genet 33:192–196 [DOI] [PubMed] [Google Scholar]
- Del Zompo M, Cherchi A, Palmas MA, Ponti M, Bocchetta A, Gessa GL, Piccardi MP (1998) Association between dopamine receptor genes and migraine without aura in a Sardinian sample. Neurology 51:781–786 [DOI] [PubMed] [Google Scholar]
- Ducros A, Denier C, Joutel A, Cecillon M, Lescoat C, Vahedi K, Darcel F, Vicaut E, Bousser MG, Tournier-Lasserve E (2001) The clinical spectrum of familial hemiplegic migraine associated with mutations in a neuronal calcium channel. N Engl J Med 345:17–24 [DOI] [PubMed] [Google Scholar]
- Ducros A, Joutel A, Vahedi K, Cecillon M, Ferreira A, Bernard E, Verier A, Echenne B, Lopez de Manain A, Boussier MG, Tournier-Lasserve E (1997) Mapping of a second locus for familial hemiplegic migraine to 1q21-q23 and evidence of further heterogeneity. Ann Neurol 42:885–890 [DOI] [PubMed] [Google Scholar]
- Duffy DL (2002) SIB-PAIR version 0.99.9, Queensland Institute of Medical Research, Brisbane, Australia [Google Scholar]
- Duggirala R, Williams JT, Williams-Blangero S, Blangero J (1997) A variance component approach to dichotomous trait linkage analysis using a threshold model. Genet Epidemiol 14:987–992 [DOI] [PubMed] [Google Scholar]
- Duren WL, Epstein MP, Li M, Boehnke M (2003) RELPAIR: a program that infers the relationships of pairs of individuals based on marker data, version 20 (available at: http://csg.sph.umich.edu/boehnke/relpair.php)
- Elston RC, Song D, Iyengar SK (2005) Mathematical assumptions versus biological reality: myths in affected sib pair linkage analysis. Am J Hum Genet 76:152–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein MP, Duren WL, Boehnke M (2000) Improved inference of relationship for pairs of individuals. Am J Hum Genet 67:1219–1231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner K, Barmada M, Ptacek LJ, Hoffman EP (1997) A new locus for hemiplegic migraine maps to chromosome 1q31. Neurology 49:1231–1238 [DOI] [PubMed] [Google Scholar]
- Haseman JK, Elston RC (1972) The investigation of linkage between a quantitative trait and a marker locus. Behav Genet 2:3–19 [DOI] [PubMed] [Google Scholar]
- Headache Classification Committee of the International Headache Society (1988) Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia (Suppl 7) 8:1–96 [PubMed] [Google Scholar]
- Heath AC, Bucholz KK, Madden PA, Dinwiddie SH, Slutske WS, Bierut LJ, Statham DJ, Dunne MP, Whitfield JB, Martin NG (1997) Genetic and environmental contributions to alcohol dependence risk in a national twin sample: consistency of findings in women and men. Psychol Med 27:1381–1396 [DOI] [PubMed] [Google Scholar]
- Heath AC, Howells W, Kirk KM, Madden PA, Bucholz KK, Nelson EC, Slutske WS, Statham DJ, Martin NG (2001) Predictors of non-response to a questionnaire survey of a volunteer twin panel: findings from the Australian 1989 twin cohort. Twin Res 4:73–80 [DOI] [PubMed] [Google Scholar]
- Hovatta I, Kallela M, Farkkila M, Peltonen L (1994) Familial migraine: exclusion of the susceptibility gene from the reported locus of familial hemiplegic migraine on 19p. Genomics 23:707–709 [DOI] [PubMed] [Google Scholar]
- Jones KW, Ehm MG, Pericak-Vance MA, Haines JL, Boyd PR, Peroutka SJ (2001) Migraine with aura susceptibility locus on chromosome 19p13 is distinct from the familial hemiplegic migraine locus. Genomics 78:150–154 [DOI] [PubMed] [Google Scholar]
- Joutel A, Bousser M-G, Biousse V, Labauge P, Chabriat H, Nibbio A, Maciazek J, Meyer B, Bach M-A, Weissenbach J, Lathrop GM, Tournier-Lasserve E (1993) A gene for familial hemiplegic migraine maps to chromosome 19. Nat Genet 5:40–45 [DOI] [PubMed] [Google Scholar]
- Joutel A, Ducros A, Vahedi K, Labauge P, Delrieu O, Pinsard N, Mancini J, Ponsot G, Gouttiere F, Gastaut JL, Maziaceck J, Weissenback J, Bousser MG, Tournier-Lasserve E (1994) Genetic heterogeneity of familial hemiplegic migraine. Am J Hum Genet 55:1166–1172 [PMC free article] [PubMed] [Google Scholar]
- Kallela M, Wessman M, Havanka H, Palotie A, Farkkila M (2001) Familial migraine with and without aura: clinical characteristics and co-occurrence. Eur J Neurol 8:441–449 [DOI] [PubMed] [Google Scholar]
- Kendler KS (1993) Twin studies of psychiatric illness: current status and future directions. Arch Gen Psychiatry 50:905–915 [DOI] [PubMed] [Google Scholar]
- Kong X, Murphy K, Raj T, He C, White PS, Matise TC (2004) A combined linkage-physical map of the human genome. Am J Hum Genet 75:1143–1148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowa H, Yasui K, Takeshima T, Urakami K, Sakai F, Nakashima K (2000) The homozygous C677T mutation in the methylenetetrahydrofolate reductase gene is a genetic risk factor for migraine. Am J Med Genet 96:762–764 [DOI] [PubMed] [Google Scholar]
- Kruglyak L, Daly MJ (1998) Linkage thresholds for two-stage genome scans. Am J Hum Genet 62:994–997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruglyak L, Daly MJ, Reeve-Daly MP, Lander ES (1996) Parametric and nonparametric linkage analysis: a unified multipoint approach. Am J Hum Genet 58:1347–1363 [PMC free article] [PubMed] [Google Scholar]
- Kusumi M, Ishizaki K, Kowa H, Adachi Y, Takeshima T, Sakai F, Nakashima K (2003) Glutathione S-transferase polymorphisms: susceptibility to migraine without aura. Eur Neurol 49:218–222 [DOI] [PubMed] [Google Scholar]
- Lander E, Kruglyak L (1995) Genetic dissection of complex traits: guidelines for interpreting and reporting linkage results. Nat Genet 11:241–247 [DOI] [PubMed] [Google Scholar]
- Lange K, Weeks D, Boehnke M (1988) Programs for pedigree analysis: MENDEL, FISHER, and dGENE. Genet Epidemiol 5:471–472 [DOI] [PubMed] [Google Scholar]
- Launer LJ, Terwindt GM, Ferrari MD (1999) The prevalence and characteristics of migraine in a population-based cohort: the GEM study. Neurology 53:537–542 [DOI] [PubMed] [Google Scholar]
- Lea RA, Dohy A, Jordan K, Quinlan S, Brimage PJ, Griffiths LR (2000) Evidence for allelic association of the dopamine β-hydroxylase gene (DBH) with susceptibility to typical migraine. Neurogenetics 3:35–40 [DOI] [PubMed] [Google Scholar]
- Lea RA, Shepherd GA, Curtain RP, Nyholt DR, Quinlan S, Brimage PJ, Griffiths LR (2002) A typical migraine susceptibility region localizes to chromosome 1q31. Neurogenetics 4:17–22 [DOI] [PubMed] [Google Scholar]
- May A, Ophoff RA, Terwindt GM, Urban C, van Eijk R, Haan J, Diener HC, Lindhout D, Frants RR, Sandkuijl LA, Ferrari MD, van Eijk R (1995) Familial hemiplegic migraine locus on 19p13 is involved in the common forms of migraine with and without aura. Hum Genet 96:604–608 [DOI] [PubMed] [Google Scholar]
- McCarthy LC, Hosford DA, Riley JH, Bird MI, White NJ, Hewett DR, Peroutka SJ, et al (2001) Single-nucleotide polymorphism alleles in the insulin receptor gene are associated with typical migraine. Genomics 78:135–149 [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Dartigues JF, Whitaker A, Angst J (1994) Diagnostic criteria for migraine: a validity study. Neurology 44:11–16 [PubMed] [Google Scholar]
- Merikangas KR, Whitaker AE, Angst J (1993) Validation of diagnostic criteria for migraine in the Zürich longitudinal cohort study. Cephalalgia 13:47–53 [DOI] [PubMed] [Google Scholar]
- Mochi M, Cevoli S, Cortelli P, Pierangeli G, Soriani S, Scapoli C, Montagna P (2003) A genetic association study of migraine with dopamine receptor 4, dopamine transporter and dopamine-beta-hydroxylase genes. Neurol Sci 23:301–305 [DOI] [PubMed] [Google Scholar]
- Mochi M, Sangiorgi S, Cortelli P, Carelli V, Scapoli C, Crisci M, Monari L, Pierangeli G, Montagna P (1993) Testing models for genetic determination in migraine. Cephalalgia 13:389–394 [DOI] [PubMed] [Google Scholar]
- Neale MC, Cardon LR (1992) Methodology for genetic studies in twins and families. Kluwer Academic Publishers, Dordrecht, The Netherlands [Google Scholar]
- Nyholt DR (2000) All LODs are not created equal. Am J Hum Genet 67:282–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ——— (2004) A simple correction for multiple testing for SNPs in linkage disequilibrium with each other. Am J Hum Genet 74:765–769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyholt DR, Curtain RP, Griffiths LR (2000) Familial typical migraine: significant linkage and localisation of a gene to Xq24-28. Hum Genet 107:18–23 [DOI] [PubMed] [Google Scholar]
- Nyholt DR, Dawkins JL, Brimage PJ, Goadsby PJ, Nicholson GA, Griffiths LR (1998a) Evidence for an X-linked genetic component in familial typical migraine. Hum Mol Genet 7:459–463 [DOI] [PubMed] [Google Scholar]
- Nyholt DR, Gillespie NA, Heath AC, Merikangas KR, Duffy DL, Martin NG (2004) Latent class analysis does not support migraine with aura and migraine without aura as separate entities. Genet Epidemiol 26:231–244 [DOI] [PubMed] [Google Scholar]
- Nyholt DR, Lea RA, Goadsby PJ, Brimage PJ, Griffiths LR (1998b) Familial typical migraine: linkage to chromosome 19p13 and evidence for genetic heterogeneity. Neurology 50:1428–1432 [DOI] [PubMed] [Google Scholar]
- Ogilvie AD, Russell MB, Dhall P, Battersby S, Ulrich V, Smith CA, Goodwin GM, Harmar AJ, Olesen J (1998) Altered allelic distributions of the serotonin transporter gene in migraine without aura and migraine with aura. Cephalalgia 18:23–26 [DOI] [PubMed] [Google Scholar]
- Ophoff RA, Terwindt GM, Vergouwe MN, Frants RR, Ferrari MD (1997) Involvement of a Ca2+ channel gene in familial hemiplegic migraine and migraine with and without aura. Headache 37:479–485 [DOI] [PubMed] [Google Scholar]
- Ophoff RA, Terwindt GM, Vergouwe MN, van Eijk R, Oefner PJ, Hoffman SM, Lamerdin JE, Mohrenweiser HW, Bulman DE, Ferrari M, Haan J, Lindhout D, van Ommen GJ, Hofker MH, Ferrari MD, Frants RR (1996) Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutation in the Ca2+ channel gene CACNL1A4. Cell 87:543–552 [DOI] [PubMed] [Google Scholar]
- Ophoff RA, van Eijk R, Sandkuijl LA, Terwindt GM, Grubben CP, Haan J, Lindhout D, Ferrari MD, Frants RR (1994) Genetic heterogeneity of familial hemiplegic migraine. Genomics 22:21–26 [DOI] [PubMed] [Google Scholar]
- Oterino A, Monton F, Cid C, Ruiz-Lavilla N, Gardner K, Barmada M, Pascual J (2001) A new locus for migraine with aura on Xq13. Cephalalgia 21:346 [Google Scholar]
- Pardo J, Carracedo A, Munoz I, Castillo J, Lema M, Noya M (1995) Genetic markers: association study in migraine. Cephalalgia 15:200–204 [DOI] [PubMed] [Google Scholar]
- Paterna S, Di Pasquale P, D’Angelo A, Seidita G, Tuttolomondo A, Cardinale A, Maniscalchi T, Follone G, Giubilato A, Tarantello M, Licata G (2000) Angiotensin-converting enzyme gene deletion polymorphism determines an increase in frequency of migraine attacks in patients suffering from migraine without aura. Eur Neurol 43:133–136 [DOI] [PubMed] [Google Scholar]
- Peroutka SJ, Wilhoit T, Jones K (1997) Clinical susceptibility to migraine with aura is modified by dopamine D2 receptor (DRD2) NcoI alleles. Neurology 49:201–206 [DOI] [PubMed] [Google Scholar]
- Rainero I, Pinessi L, Salani G, Valfre W, Rivoiro C, Savi L, Gentile S, Giudice RL, Grimaldi LM (2002) A polymorphism in the interleukin-1alpha gene influences the clinical features of migraine. Headache 42:337–340 [DOI] [PubMed] [Google Scholar]
- Rindskopf D, Rindskopf W (1986) The value of latent class analysis in medical diagnosis. Stat Med 5:21–27 [DOI] [PubMed] [Google Scholar]
- Russo L, Mariotti P, Sangiorgi E, Giordano T, Ricci I, Lupi F, Chiera R, Guzzetta F, Neri G, Gurrieri F (2005) A new susceptibility locus for migraine with aura in the 15q11-q13 genomic region containing three GABA-A receptor genes. Am J Hum Genet 76:327–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawcer S, Jones HB, Judge D, Visser F, Compston A, Goodfellow PN, Clayton D (1997) Empirical genomewide significance levels established by whole genome simulations. Genet Epidemiol 14:223–229 [DOI] [PubMed] [Google Scholar]
- Sham PC, Purcell S, Cherny SS, Abecasis GR (2002) Powerful regression-based quantitative-trait linkage analysis of general pedigrees. Am J Hum Genet 71:238–253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soragna D, Vettori A, Carraro G, Marchioni E, Vazza G, Bellini S, Tupler R, Savoldi F, Mostacciuolo ML (2003) A locus for migraine without aura maps on chromosome 14q21.2-q22.3. Am J Hum Genet 72:161–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart WF, Lipton RB, Celentano DD, Reed ML (1992) Prevalence of migraine headache in the United States: relation to age, income, race, and other sociodemographic factors. JAMA 267:64–69 [PubMed] [Google Scholar]
- Suarez BK, Hodge SE (1979) A simple method to detect linkage for rare recessive diseases: an application to juvenile diabetes. Clin Genet 15:126–136 [DOI] [PubMed] [Google Scholar]
- Terwindt GM, Ophoff RA, van Eijk R, Vergouwe MN, Haan J, Frants RR, Sandkuijl LA, Ferrari MD (2001) Involvement of the CACNA1A gene containing region on 19p13 in migraine with and without aura. Neurology 56:1028–1032 [DOI] [PubMed] [Google Scholar]
- Trabace S, Brioli G, Lulli P, Morellini M, Giacovazzo M, Cicciarelli G, Martelletti P (2002) Tumor necrosis factor gene polymorphism in migraine. Headache 42:341–345 [DOI] [PubMed] [Google Scholar]
- Tzourio C, El Amrani M, Poirier O, Nicaud V, Bousser MG, Alperovitch A (2001) Association between migraine and endothelin type A receptor (ETA −231 A/G) gene polymorphism. Neurology 56:1273–1277 [DOI] [PubMed] [Google Scholar]
- Vanmolkot KR, Kors EE, Hottenga JJ, Terwindt GM, Haan J, Hoefnagels WA, Black DF, Sandkuijl LA, Frants RR, Ferrari MD, Van Den Maagdenberg AM (2003) Novel mutations in the Na+, K+-ATPase pump gene ATP1A2 associated with familial hemiplegic migraine and benign familial neonatal convulsions. Ann Neurol 54:360–366 [DOI] [PubMed] [Google Scholar]
- Wang JJ, Mitchell P, Smith W (1997) Is there an association between migraine headache and open-angle glaucoma? Findings from the Blue Mountains Eye Study. Ophthalmology 104:1714–1719 [DOI] [PubMed] [Google Scholar]
- Wessman M, Kallela M, Kaunisto MA, Marttila P, Sobel E, Hartiala J, Oswell G, Leal SM, Papp JC, Hamalainen E, Broas P, Joslyn G, Hovatta I, Hiekkalinna T, Kaprio J, Ott J, Cantor RM, Zwart JA, Ilmavirta M, Havanka H, Farkkila M, Peltonen L, Palotie A (2002) A susceptibility locus for migraine with aura, on chromosome 4q24. Am J Hum Genet 70:652–662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiltshire S, Cardon LR, McCarthy MI (2002) Evaluating the results of genomewide linkage scans of complex traits by locus counting. Am J Hum Genet 71:1175–1182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yilmaz M, Erdal ME, Herken H, Cataloluk O, Barlas O, Bayazit YA (2001) Significance of serotonin transporter gene polymorphism in migraine. J Neurol Sci 186:27–30 [DOI] [PubMed] [Google Scholar]
- Zhu G, Evans DM, Duffy DL, Montgomery GW, Medland SE, Gillespie NA, Ewen KR, Jewell M, Liew YW, Hayward NK, Sturm RA, Trent JM, Martin NG (2004) A genome scan for eye color in 502 twin families: most variation is due to a QTL on chromosome 15q. Twin Res 7:197–210 [DOI] [PubMed] [Google Scholar]