Abstract
Purpose of Review
To position relative fat mass (RFM) as a more accurate, physiologically grounded, and clinically useful alternative to body mass index (BMI) for assessing adiposity and predicting cardiometabolic risk, including heart failure.
Recent Findings
RFM estimates body fat percentage using a sex-specific formula based on waist circumference and height. RFM not only correlates more strongly with fat mass than BMI, but also shows a weaker correlation with muscle mass. This distinction helps reduce lean mass-related confounding in the assessment of adiposity. In clinical studies, RFM has emerged as a robust predictor of incident heart failure, cardiometabolic disease, and all-cause mortality.
Summary
RFM avoids misclassification of adiposity in individuals with high muscle mass and better reflects abdominal adiposity than BMI. As the prevalence of heart failure and other obesity-related diseases continues to rise, RFM offers a practical and intuitive tool for assessment of adiposity and heart failure risk – challenging the long-standing dominance of BMI.
Keywords: Relative Fat Mass, Body Mass Index, Muscle Mass, Obesity Paradox, Cardiometabolic Disease, Heart Failure
Introduction
For decades, body mass index (BMI) has been the standard tool for classifying overweight and obesity – not only in clinical practice and guidelines, but also in clinical trial eligibility criteria and public health messaging.
However, BMI does not distinguish between fat mass and lean muscle mass [1, 2]. For example, a sedentary individual and an athletic individual may share the same BMI despite substantial differences in “fat versus muscle” content. Similarly, a bodybuilder or a person with high muscle mass may be misclassified as “overweight” or even “obese.” Additionally, BMI fails to measure the degree of abdominal adiposity and does not account for sex-based differences in fat percentage. These limitations are problematic not only for clinical risk assessment – where actual adiposity, rather than elevated BMI, is more closely linked to the risk of developing heart failure and cardiovascular disease – but also when determining eligibility for clinical trials, potentially excluding or misclassifying individuals based on a flawed metric.
Relative Fat Mass: A Superior Alternative to BMI
To address these limitations, the relative fat mass (RFM) index was introduced in 2018 by Woolcott and Bergman [3]. RFM is a sex-specific anthropometric measure that estimates body fat percentage using waist circumference and height. The formula, RFM = 64 – (20 × height/waist) + (12 × sex), where sex = 0 for males and 1 for females, was derived and validated in large, diverse population datasets and shows strong correlation with dual-energy X-ray absorptiometry (DEXA) measurements of body fat. In the general population, average RFM values are approximately 25% in males and 35% in females [4], with obesity defined as RFM > 30% in males and > 40% in females [5].
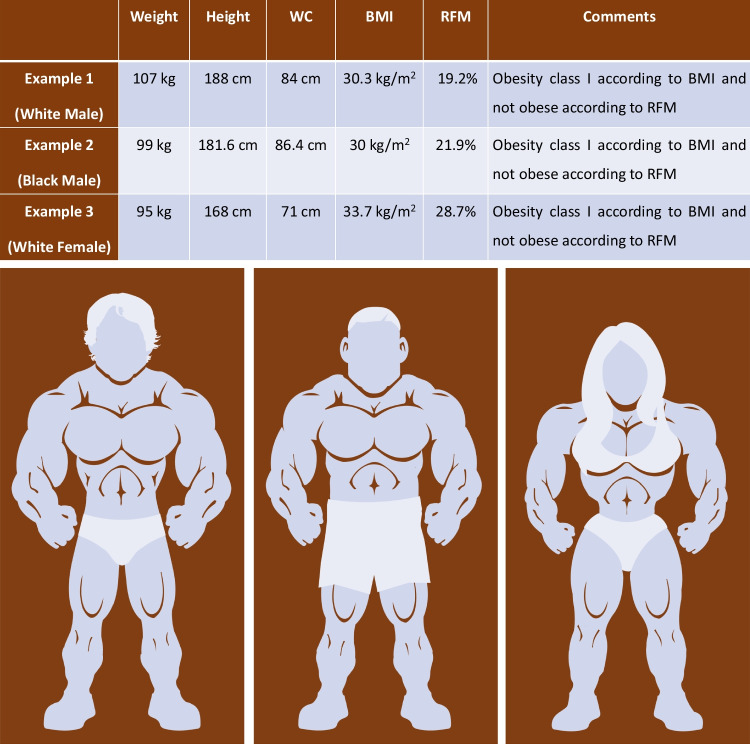
Notably, RFM offers two advantages of particular relevance over BMI. First, as RFM is calculated using waist circumference, it provides a more accurate estimate of abdominal fat mass. Second, by excluding body weight from its formula, RFM reduces confounding by muscle mass in the estimation of obesity-related risk [6] – which is an important limitation of BMI (Fig. 1).
Fig. 1.
Misclassification of adiposity by body mass index (BMI) in muscular individuals. Three athletic individuals – a White male, a Black male and a White female – are shown with their weight, height, and waist circumference (WC). While BMI (based on weight and height) classifies them as obese, relative fat mass (RFM, based on WC and height) does not. BMI-defined obesity is ≥ 30 kg/m2 in both sexes and RFM-defined obesity is > 30% in males and > 40% in females. The images presented are original creations and are used solely for educational and illustrative purposes under fair use.
Copyright held by Navin Suthahar, © 2025
Clinical Relevance of RFM: Risk Prediction and the Obesity Paradox
In Table 1, we summarize key studies highlighting the superiority of RFM over BMI in predicting incident cardiometabolic disease including heart failure (HF) [10]. In addition to being a robust predictor of incident HF and other cardiometabolic outcomes, the use of RFM may also help resolve the “obesity paradox” commonly observed with BMI.
Table 1.
Key studies highlighting the predictive value of RFM for incident cardiometabolic disease and mortality in the general population
| Cohort/Trial | Primary Outcome | Comments |
|---|---|---|
|
General Population • PREVEND Study • LifeLines Study • Rotterdam Study |
Incident type-2 diabetes | Relative fat mass (RFM) was an excellent predictor of incident type-2 diabetes in the general population, and performed better than body mass index (BMI), waist circumference (WC) and waist-to-hip ratio (WHR) [4] |
|
General Population • Lookup 7 + Study |
Prevalent hypertension, diabetes and hyperlipidaemia | RFM was an excellent predictor of hypertension and diabetes in elderly individuals, and generally performed better than BMI [7] |
|
General Population • PREVEND Study |
Incident heart failure (HF) | RFM was an excellent predictor of incident HF in the general population, and performed better than BMI, WC and WHR [8] |
|
General Population • LifeLines Study |
Incident cardiovascular disease (CVD) | RFM was the most consistent predictor of incident CVD and its subtypes in the general population [9] |
|
General Population • PREVEND Study |
All-cause mortality | RFM was a stronger predictor of mortality than BMI, and its usage showed no evidence supporting the “obesity-survival paradox” in the general population [6] |
This table is reproduced with permission from Suthahar N, et al. Nature Reviews Endocrinology; 2025 Jul;21(7):393–394. PREVEND, Prevention of Renal and Vascular End-stage Disease
A likely reason, why this paradox arises, is because BMI is a composite measure reflecting both fat mass and lean muscle mass. Since higher muscle mass is associated with reduced mortality [11, 12] and a higher fat mass with increased mortality [6], BMI — particularly when elevated due to muscle mass — can misleadingly suggest that higher BMI is protective/not deleterious.
Indeed, the BMI-mortality paradox has also been extensively reported in patients with HF (particularly among those with reduced ejection fraction), where a higher BMI has been associated with better survival outcomes. However, this paradox may simply reflect the inability of BMI to distinguish between protective muscle [13] and harmful fat accumulation. Clearly, a patient with HF and preserved muscle mass (higher BMI) would be expected to have better outcomes than one with significant muscle loss (lower BMI) [14]. In such scenarios, usage of RFM, which does not include body weight in its calculation, might help minimize the confounding effect of muscle mass and provide a more accurate assessment of adiposity-related risk.
Conclusion
In summary, RFM maintains the practical advantages of BMI by requiring two simple non-invasive measurements, while addressing its most significant limitations. By preserving the simplicity and relatability needed for real-world use [10], RFM combines (patho)physiological relevance with clinical practicality. The ability of RFM to reflect abdominal fat distribution, limit the confounding effect of muscle mass, perform consistently across diverse outcomes, and its ease of implementation position it as a strong candidate to replace BMI in routine care.
Author Contributions
N.S. drafted the manuscript and prepared the figure. E.S.L. and G.S. critically revised the manuscript for important intellectual content and approved the final version.
Funding
This research received no specific external funding. N.S. acknowledges support from the Netherlands Organization for Scientific Research (Nederlandse Organisatie voor Wetenschappelijk Onderzoek), co-funded by ERA4Health through the CARDINNOV 2023 call, as part of the EnerLIGHT project (Grant Agreement No. 101095426 of the EU Horizon Europe Research and Innovation Programme).
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Competing interests
N.S. declares no competing interests related to this manuscript. E.S.L. has served as a consultant for SystoleHealth, Amissa Health, and Roon, and is supported by grants from the National Institutes of Health (K23-HL159243), the Massachusetts Life Sciences Center, and the Tiangiao and Chrissy Chen Institute. G.S. reports grants and personal fees from CSL Vifor, Boehringer Ingelheim, AstraZeneca, Servier, Novartis, Cytokinetics, Pharmacosmos, Medtronic, and Bayer; personal fees from Roche, Abbott, Edwards Lifesciences, TEVA, Menarini, INTAS, GETZ, and Laboratori Guidotti; and grants from Boston Scientific and Merck, all outside the submitted work.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rubino F, Cummings DE, Eckel RH, Cohen RV, Wilding JPH, Brown WA, et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025;13:221–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gurunathan U, Myles PS. Limitations of body mass index as an obesity measure of perioperative risk. Br J Anaesth. 2016;116:319–21. [DOI] [PubMed] [Google Scholar]
- 3.Woolcott OO, Bergman RN. Relative fat mass (RFM) as a new estimator of whole-body fat percentage ─ A cross-sectional study in American adult individuals. Sci Rep. 2018;8:10980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suthahar N, Wang K, Zwartkruis VW, Bakker SJL, Inzucchi SE, Meems LMG, et al. Associations of relative fat mass, a new index of adiposity, with type-2 diabetes in the general population. Eur J Intern Med. 2023;109:73–8. [DOI] [PubMed] [Google Scholar]
- 5.Woolcott OO, Bergman RN. Defining cutoffs to diagnose obesity using the relative fat mass (RFM): Association with mortality in NHANES 1999–2014. Int J Obes. 2020;44:1301–10. [DOI] [PubMed] [Google Scholar]
- 6.Suthahar N, Zwartkruis V, Geelhoed B, Withaar C, Meems LMG, Bakker SJL, et al. Associations of relative fat mass and BMI with all-cause mortality: confounding effect of muscle mass. Obesity (Silver Spring). 2024;32:603–11. [DOI] [PubMed]
- 7.Cacciatore S, Calvani R, Marzetti E, Coelho-Júnior HJ, Picca A, Fratta AE, et al. Predictive values of relative fat mass and body mass index on cardiovascular health in community-dwelling older adults: Results from the Longevity Check-up (Lookup) 7. Maturitas. 2024;185:108011. [DOI] [PubMed] [Google Scholar]
- 8.Suthahar N, Meems LMG, Withaar C, Gorter TM, Kieneker LM, Gansevoort RT, et al. Relative fat mass, a new index of adiposity, is strongly associated with incident heart failure: data from PREVEND. Sci Rep. 2022;12:147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zwartkruis VW, Suthahar N, Idema DL, Mahmoud B, van Deutekom C, Rutten FH, et al. Relative fat mass and prediction of incident atrial fibrillation, heart failure and coronary artery disease in the general population. Int J Obes (Lond). 2023;47:1256–62. [DOI] [PubMed] [Google Scholar]
- 10.Suthahar N, Bergman RN, de Boer RA. Replacing body mass index with relative fat mass to accurately estimate adiposity. Nat Rev Endocrinol. 2025;21:393–4. [DOI] [PubMed]
- 11.Oterdoom LH, Gansevoort RT, Schouten JP, de Jong PE, Gans ROB, Bakker SJL. Urinary creatinine excretion, an indirect measure of muscle mass, is an independent predictor of cardiovascular disease and mortality in the general population. Atherosclerosis. 2009;207:534–40. [DOI] [PubMed] [Google Scholar]
- 12.Abramowitz MK, Hall CB, Amodu A, Sharma D, Androga L, Hawkins M. Muscle mass, BMI, and mortality among adults in the United States: A population-based cohort study. Gorlova OY, editor. PLoS ONE. 2018;13:e0194697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cai X, Liu M, Qin P, Tang S, He L, Lei J, et al. Skeletal muscle mass and mortality in heart failure. JACC: Advances. 2025;4:101553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miura Y, Higuchi S, Kohno T, Shiraishi Y, Kitamura M, Nagatomo Y, et al. Cachectic biomarkers as confounders behind the obesity paradox in patients with acute decompensated heart failure. Int J Obes. 2025;49:888–95. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.