Abstract
Purpose
To evaluate the current clinical practice methods and the reported indications for biceps tenodesis in injured overhead throwing athletes.
Methods
This study combined a survey of experienced shoulder surgeons regarding their methods of establishing indications for tenodesis surgery with a systematic review of studies that reported performing biceps tenodesis in overhead throwing athletes. Both the survey and review were designed to identify methods of making the diagnosis to delineate the preoperative and intraoperative factors used to establish biceps involvement as a major component of the clinical presentation, as well as to attempt to establish a consensus for clinical practice.
Results
Eleven studies reporting on 249 overhead throwing athletes were analyzed. Elements of the history evaluation were described in 5 studies; physical examination, in 2 studies; advanced imaging, in 7 studies; and diagnostic arthroscopy, in 8 studies. One hundred nineteen responses to the survey showed a similar thought process regarding the reasoning to include biceps tenodesis, but several aspects of the process appeared to not be supported by contemporary literature. Also, there was inconsistent use of diagnostic components, with only 3 of 9 history components and 4 of 9 physical examination components being selected by more than 50% of the respondents.
Conclusions
The survey revealed there was an incompletely supported reasoning process regarding indications for tenodesis and there was no consensus regarding individual components of the history or physical examination. The literature review revealed a lack of consensus regarding which elements of the diagnostic process are integral in establishing biceps involvement in injured throwing shoulders.
Level of Evidence
Level IV, systematic review of Level III and IV studies and cross-sectional survey.
The frequency of biceps tenodesis in the treatment of the injured overhead throwing athlete is increasing in primary and revision cases. Determining whether the biceps tendon is part of the clinically significant pathoanatomy that leads to the injured overhead throwing shoulder is essential for establishing proper surgical indications for biceps tenodesis. Experience and available data suggest that current methods of establishing the diagnosis of biceps involvement and surgical indications are imprecise and inconsistently applied.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11 Therefore, improving the diagnostic process may lead to more consistency in these evolving treatment protocols.
This lack of precision, and the possible misuse of the procedure, is important in light of recent scholarship providing a more inclusive overview of the roles of the biceps and demonstrating key roles of the biceps in the function of the shoulder during the overhead throwing motion, whose higher loads, larger ranges of motion, faster rotational velocities, and higher translation forces require greater precision of ball-and-socket kinematics.12, 13, 14, 15, 16 The biceps plays a key role in facilitating glenohumeral joint (GHJ) stability through humeral head (HH) depression, by stabilization in abduction and external rotation motions, and by moderating small obligatory anterior HH translation, all of which potentiate concavity/compression by their effect on the GHJ stability ratio (translational shear force divided by GHJ stabilizing compression force), helping to minimize shear force and maximize compression force.12,14,15 In 2 biomechanical studies, loss of biceps-labral complex tension created posterior HH translation,13 and removal of the biceps-labral complex attachment by tenodesis significantly altered the GHJ stability ratio, leading to that study’s conclusion that tenodesis cannot be used as primary treatment in baseball players.12 Biceps tenodesis is an essentially irreversible procedure and has been shown to have the capability of producing consequential outcomes in the specific population of overhead throwing athletes, in whom the biceps plays a substantial role in optimal mechanics, stability, and performance.
A previous set of articles sought a consensus regarding the evolving treatment for SLAP injuries by including a physician survey and a systematic literature review.17,18 It was expected that this 2-part approach would result in a broad-based assessment of past and current thought, methodology, and clinical practice among surgeons. The purpose of this study was to evaluate the current clinical practice methods and the reported indications for biceps tenodesis in injured overhead throwing athletes The hypotheses were that there would be wide variability in the reported indications for biceps tenodesis in the injured overhead throwing athlete and that there would be limited areas of consensus (defined as at least 60% agreement) among surveyed physicians regarding the diagnosis of clinically significant biceps involvement in the injured overhead throwing athlete.
Methods
Systematic Review
Search Strategy
The goal of the literature review was to analyze studies that included biceps tenodesis and any aspect of preoperative or intraoperative evaluation as part of the reported treatment. This systematic review accessed 5 databases—PubMed, CINAHL (Cumulative Index to Nursing and Allied Health Literature), MEDLINE, Web of Science, and SportDiscus—on September 28, 2023, to search the terms listed in Figure 1. All articles from database inception until September 28, 2023, were included in the initial search without search modifiers. Once all articles were retrieved from the 5 databases, the articles were downloaded into Rayyan, a commonly used online public software application for article sorting in systematic reviews.19 All article screening was completed by 2 authors (A.D.S. and A.N.B.) independently; disagreements were solved by both authors actively discussing the disagreements and resolving them via collaboration. For the article-sorting process, duplicate articles were first removed manually, followed by screening by title and abstract. Next, full-text screening was performed for final article inclusion. A full reference search of the included articles was also undertaken after final text inclusion for completeness in this systematic review.
Fig 1.
Systematic review search flowchart. (CINAHL, Cumulative Index to Nursing and Allied Health Literature.)
Study Selection and Retention
Articles were retained based on the following inclusion criteria: full-text articles (Level I-IV evidence) in English investigating biceps tenodesis in overhead athletes. The exclusion criteria were articles determined to be literature reviews (non-systematic reviews), current concepts/opinion papers, articles not in English, articles without full text, wrong study population (not overhead athletes), or wrong procedure (not biceps tenodesis).
Data Extraction
The research question centered on the methods described in each article that were used to determine the indications contributing to the selection of biceps tenodesis as a treatment option in the overhead throwing athlete. The aim was to document which specific factors of patient history, physical examination, imaging, and diagnostic arthroscopy were used in each study. Each of these factors is commonly used to make the clinical diagnosis. In these cases, they should be used to establish a diagnosis that biceps involvement is clinically significant and support the selection of biceps tenodesis in the treatment. Each article was reviewed to see if descriptions of elements relating to preoperative history, preoperative physical examination, preoperative imaging, and/or operative findings relating to establishment of a diagnosis that biceps involvement is clinically significant were specifically listed. Critical appraisal or risk-of-bias evaluation was not performed as part of this review because the focus was on reporting of clinical examination and surgical indicators for choosing to perform biceps tenodesis as a treatment option rather than the outcomes of the procedure.
Survey
Orthopaedic surgeons who were active members of the American Shoulder and Elbow Surgeons (ASES) were invited to participate in an electronic survey that was focused only on the use of biceps tenodesis in the treatment of the injured overhead throwing athlete. Overhead throwing was defined in compliance with the International Classification of Functioning, Disability and Health as “using fingers, hands and arms to lift something and propel it with some force through the air, such as when tossing a ball.”20
Eligible subjects were active members of ASES, held an M.D. credential or D.O. credential (or both), and were practicing or non-practicing clinicians. An institutional review board reviewed and approved the survey for a consent waiver prior to its distribution (No. LCO-2024-001). The ASES administration office provided the cover letter, electronic survey link, and institutional review board approval to its membership via email. A reminder email was sent to the membership to complete the survey 2 weeks after the initial email invitation. General information such as age, sex, years in practice, number of overhead athletes surgically treated annually, and whether the physician used biceps tenodesis as a surgical procedure in overhead throwing athletes was obtained. To capture the survey information, participants completed a survey developed in a cloud-based survey system (SurveyMonkey, San Mateo, CA). The survey was divided into areas of basic practice information, rationale for using biceps tenodesis in overhead athletes, patient selection, examination criteria including imaging, and intraoperative findings. In each area, surgeons could select as many components as they usually used in their practice, either from the provided list or by adding their own.
Data Analysis
The results of the systematic review were compiled and tabulated through a standard frequency analysis to identify the commonly used rationale, patient selection, examination, and intraoperative components for supporting the selection of biceps tenodesis as a viable treatment option. All binary, multiple-choice, and check-all-that-apply responses from the survey were tabulated for each group and reported as frequencies and percentages. Open-ended responses were compiled and summarized within each applicable section. If a respondent answered yes to the survey question “Do you utilize biceps tenodesis as a surgical procedure in overhead athletes?,” the data were retained for analysis.
Sample size was determined based on the total number of members of ASES. Using the population (membership) of 1,300 possible respondents across the organization and accounting for a 10% margin of error, it was determined that the number of completed surveys required to achieve adequate power was 40 surveys at a β level of 80%, 50 surveys at a β level of 85%, 65 surveys at a β level of 90%, 90 surveys at a β level of 95%, and 149 surveys at a β level of 99%. All statistical analyses were performed using STATA/SE (version 18.0; StataCorp, College Station, TX).
Results
Systematic Review
A total of 300 articles were retrieved from the systematic search (Fig 1). Eleven articles reported the use of biceps tenodesis as some part of the treatment of shoulder injury, with 10 containing some overhead throwing athletes1, 2, 3, 4, 5, 6, 7, 8, 9,11 and 1 containing only overhead throwing athletes10 (Table 1). The research designs were either case series (55%) or cohort studies (45%). The total number of subjects in all 11 articles was 434 (age range, 15-64 years), and the number of overhead throwing athletes in the 11 articles was 249, including 113 participants in baseball,2, 3, 4, 5, 6, 7, 8, 9,11 67 in softball,2, 3, 4, 5, 6, 7,9, 10, 11 22 in swimming,2,3,5, 6, 7,9,11 20 in volleyball,3, 4, 5, 6, 7, 8, 9,11 18 in tennis,6, 7, 8, 9 6 in handball,7,9 2 in racquetball,2 and 1 in cricket.2 One study noted that 15 overhead athletes were included but did not provide the specific sports.1 A wide variety of inclusion and diagnostic criteria that were used in establishing the indications for tenodesis was observed in the 11 articles. In addition to determining biceps-specific pathology such as synovitis, hypertrophy, or instability,5 the inclusion criteria included isolated type II SLAP injuries,1,4,8,11 type II to IV SLAP injuries,2,7 and type I to IV SLAP injuries3 or mentioned SLAP injuries but did not specify type.6,9,10
Table 1.
Systematic Review Demographic Data
| Source | Design | Total Patients | Sex, n | Age, yr | Age Range, yr | Athletes, n | Athlete Type | Pathology Inclusion |
|---|---|---|---|---|---|---|---|---|
| Boileau et al.,1 2009 | Level III: cohort study | 25 | SLAP: 10 M BT: 9 M, 6 F |
SLAP: 37 BT: 52 |
SLAP: 19-57 BT: 28-64 |
19 (76%) | 15 overhead but type of sport not listed | Isolated type II SLAP injury |
| Gottschalk et al.,2 2014 | Level IV: case series | 26 | 16 M, 10 F | 47 | 19-63 | 16 (62%) | 6 weight lifting 3 tennis∗ 3 baseball/softball∗ 2 racquetball∗ 1 swimming∗ 1 cricket∗ 1 gymnastics |
Type II or IV SLAP injury; concomitant pathology allowed |
| Gupta et al.,3 2015 | Level III: cohort study | 28 | 18 M, 10 F | 44 ± 13 | NR | 8 (29%) | 2 baseball∗ 2 softball∗ 1 volleyball∗ 1 basketball 1 swimming∗ 1 golf |
BT and preoperative type I-IV SLAP injury |
| Pogorzelski et al.,4 2018 | Level IV: case series | 20 | 10 M, 10 F | 38 ± 6 | 21-45 | 16 (80%) | 3 weight lifting 2 volleyball∗ 2 skiing 1 basketball 1 baseball∗ 1 golf 1 martial arts 1 rock climbing 1 softball∗ 1 running 1 snowboarding 1 soccer |
BT and isolated type II SLAP injury |
| Griffin et al.,5 2019 | Level IV: case series | 36 | 13 M, 23 F | 20 ± 3 | NR | 34 (94%) | 10 baseball∗ 7 softball∗ 6 volleyball∗ 4 swimming∗ 3 football 3 golf 2 basketball 1 wrestling 1 crew 1 gymnastics |
Synovitis, hypertrophy, and instability |
| Lin et al.,6 2021 | Level IV: case series | 41 | 28 M, 13 F | 21 | 15-34 | 41 (100%) | 15 baseball∗ 4 lacrosse 3 softball∗ 3 basketball 3 tennis∗ 3 golf 3 swimming∗ 2 wrestling 2 crew 2 volleyball∗ 1 football |
BT, biceps transfer, or SLAP repair with BT (SLAP type or types NR) |
| Hurley et al.,7 2022 | Level III: cohort study | 107 SLAP: 78 BT: 29 |
SLAP: 62 M, 16 F BT: 23 M, 6 F |
SLAP: 24 ± 4 BT: 26 ± 4 |
NR | 81 (76%) SLAP: 38 BT: 18 |
50 baseball (9 pitcher)∗ 6 swimming∗ 5 softball∗ 5 CrossFit 4 rock climbing 3 volleyball∗ 3 tennis∗ 3 handball∗ 1 boxing 1 golf |
Isolated type II-IV SLAP injury |
| Lacheta et al.,8 2022 | Level III: cohort study | 44 SLAP: 28 BT: 16 |
SLAP: 24 M, 4 F BT: 12 M, 4 F |
SLAP: 24 ± 6 BT: 29 ± 6 |
SLAP: 17-35 BT: 18-35 |
34 (100%) | SLAP 6 baseball∗ 6 football 4 rock climbing 3 basketball 2 CrossFit 2 volleyball∗ 2 weight lifting 2 wrestling 1 kayak 1 mixed-martial arts BT 5 baseball∗ 3 rock climbing 2 football 1 acrobat 1 kayak 1 lacrosse 1 tennis∗ 1 volleyball∗ 1 weight lifting |
Isolated type II SLAP injury |
| Lorentz et al.,9 2022 | Level IV: case series | 44 | 35 M, 9 F | 35 ± 9 | 16-46 | 44 (100%) | 11 baseball∗ 8 tennis∗ 8 swimming∗ 5 softball∗ 4 rock climbing 3 handball∗ 2 CrossFit 2 volleyball∗ 1 boxing |
BT for isolated SLAP tear (SLAP type or types NR) |
| Rothermich et al.,10 2023 | Level III: cohort study | 47 SLAP: 18 BT: 29 |
47 F | 17 ± 2 | 14-23 | 47 (100%) | 47 softball∗ | BT or SLAP repair (SLAP type or types NR) |
| Waterman et al.,11 2023 | Level IV: case series | 16 | 11 M, 5 F | 21 ± 5 | NR | 16 (100%) | 9 baseball/softball∗ 2 gymnastics 2 swimming∗ 1 basketball 1 volleyball∗ 1 lacrosse |
Isolated type II SLAP injury |
BT, biceps tenodesis; F, female; M, male; NR, not reported.
Overhead athletes.
Elements of the history evaluation were described in only 5 articles (45%)1,3,5,8,11; these included presence of pain or tenderness along the biceps or with arm motion,1,3,5,8,11 prior medications,1,3 and failure of rehabilitation1,3,5,8 (Table 2). Only 2 articles (18%) described using some elements of the physical examination such as assessing motion and/or strength and performing special testing.8,11 Seven articles (64%) described using advanced imaging as part of the diagnostic evaluation.1,3,5,8, 9, 10, 11 Eight articles (73%) used the results of diagnostic arthroscopy in making the diagnosis for initiating treatment.1, 2, 3, 4, 5,8,9,11
Table 2.
Systematic Review Clinical Information
| Source | History | Motion | Strength | Special Tests | Imaging | Surgical Indications |
|---|---|---|---|---|---|---|
| Boileau et al.,1 2009 | Pain at rest, pain with overhead activity, failed medication and physical therapy for ≥6 mo | NR | NR | NR | CT, MRA, or DA for type II SLAP injury but not consistent across all patients | Type II SLAP injury |
| Gottschalk et al.,2 2014 | NR | NR | NR | NR | DA | Type II or IV SLAP injury |
| Gupta et al.,3 2015 | Tenderness to palpation in groove, failed medication and physical therapy | NR | NR | NR | MRI and DA | Consideration for BT based on clinical/imaging evidence of tendinitis such as groove pain or fluid in sheath |
| Pogorzelski et al.,4 2018 | NR | NR | NR | NR | DA | Type II SLAP injury had to be present for BT to be performed |
| Griffin et al.,5 2019 | Failed physical therapy and inability to return to sport, bicipital groove pain | NR | NR | NR | MRI with tendon inflammation and DA | Signs of synovitis, hypertrophy, and instability or biceps-labral complex injury |
| Lin et al.,6 2021 | NR | NR | NR | NR | NR | BT or transfer per surgeon preference; SLAP repair performed with BT if superior labral tissue was unstable after biceps was detached to prevent bucket handling and propagation of labral tear |
| Hurley et al.,7 2022 | NR | NR | NR | NR | NR | Patient decided which procedure preoperatively |
| Lacheta et al.,8 2022 | Persistent pain, failed physical therapy | Impaired function | Loss of strength | Active compression and Yergason tests | Radiologic signs of type II SLAP injury only and confirmed with DA (excluded pathology of long head of biceps) | Tissue quality of superior labrum decided procedure; SLAP repair used for solid impressed bucket-handle tear; BT used for degenerative multiple fraying of superior labrum |
| Lorentz et al.,9 2022 | NR | NR | NR | NR | MRI and DA | Pathology identified at biceps-labral complex |
| Rothermich et al.,10 2023 | NR | NR | NR | NR | Advanced imaging (type not specified) | BT used when pathology identified at biceps-labral complex—no specifics provided |
| Waterman et al.,11 2023 | Tenderness to palpation in groove | Motion obtained but not used to make diagnosis | NR | Active compression, modified dynamic labral shear, and crank tests | MRI for SLAP injury and DA | Anterior type IIa SLAP injury involving biceps anchor; attenuated/poor-quality biceps-labral tissue, structural long head of biceps pathology, and groove pain |
BT, biceps tenodesis; CT, computed tomography; DA, diagnostic arthroscopy; MRA, magnetic resonance arthrography; MRI, magnetic resonance imaging; NR, not reported.
Survey
A total of 185 surveys were initiated within the survey system. Twenty surveys were removed because the respondents opened the surveys but did not complete the items. An additional 14 surveys were removed because the respondents did not answer the question on whether they used biceps tenodesis in overhead athletes. This resulted in 151 surveys having complete information. Of the respondents with complete surveys, 21% reported they did not use biceps tenodesis in the overhead throwing athlete. The respondents in this group (n = 32; age, 55.7 ± 12.6 years) were significantly older than the respondents who reported using biceps tenodesis in the overhead throwing athlete (n = 119; age, 50.4 ± 10.9 years; P = .02). Demographic and practice characteristics of the 119 respondents who use biceps tenodesis in overhead throwing athletes are reported in Table 3.
Table 3.
Demographic Data of Survey Respondents
| Respondents Who Use BT in Overhead Throwing Athletes (n = 119) | |
|---|---|
| Age, yr | |
| Mean ± SD | 50.4 ± 10.9 |
| Range | 33-85 |
| Sex, n (%) | |
| Female | 7 (6) |
| Male | 112 (94) |
| Declined to answer | 0 (0) |
| Years in practice, n (%) | |
| 1-5 | 15 (13) |
| 6-10 | 20 (17) |
| 11-15 | 26 (22) |
| 16-20 | 13 (11) |
| >20 | 45 (38) |
| Annual procedures, n (%) | |
| 1-10 | 20 (17) |
| 11-25 | 31 (26) |
| 26-40 | 19 (16) |
| 41-60 | 16 (13) |
| 61-80 | 13 (11) |
| >80 | 20 (17) |
BT, biceps tenodesis; SD, standard deviation.
When survey participants were asked to report why biceps tenodesis is used in an overhead throwing athlete, the responses indicated the belief that the procedure helps with pain relief (87%), addresses symptoms after previous labral repair (80%), and addresses pathology not categorized as irritation or synovitis (78%) (Table 4). Regarding rationale, at least 50% of the respondents noted better outcomes compared with other techniques (55%), papers have shown effectiveness for overhead throwing athletes (59%), there is a decreased need for additional surgery after performing biceps tenodesis (62%), and pain relief is better after the procedure (67%). A similar number of respondents noted biceps tenodesis is used primarily to address the biceps tendon (88%) or for revision labral repair (86%), whereas approximately half also use the procedure for revision biceps surgery (55%) and primary labral surgery (49%). More than half of the respondents (58%) noted their use of biceps tenodesis in overhead throwing athletes has increased over the past 5 years.
Table 4.
Responses on Use of BT
| Responses (n = 119), % | |
|---|---|
| Why do you use biceps tenodesis in overhead throwing athletes? | |
| Pain relief | 87 |
| Address symptoms after previous labral surgery | 80 |
| Pathology (not irritation) | 78 |
| Decrease tension on labrum | 57 |
| Irritation/synovitis | 53 |
| Avoid post-op stiffness | 28 |
| Restore throwing mechanics | 10 |
| Other∗ | 2 |
| Rationale for using biceps tenodesis in overhead throwing athletes | |
| Pain relief is better after tenodesis | 67 |
| Decreased need for additional surgery after BT | 62 |
| Papers have demonstrated effectiveness for overhead throwing athletes | 59 |
| Better outcomes compared to other techniques | 55 |
| It is easy to perform | 30 |
| Discussions with colleagues | 28 |
| Restoration of throwing function | 18 |
| Other† | 8 |
| Improvement of glenohumeral kinematics | 7 |
BT, biceps tenodesis.
Other responses were as follows: “To reinforce the rotator cuff and superior capsule in cases of rotator cuff tears in conjunction with pain in the overhead throwing athlete” and “In conjunction with treatment of a tear/partial tear of the superior subscapularis border to eliminate the interaction between biceps and upper subscapularis tendon edge.”
Other responses were as follows: “I use it for treatment based on history and PE implication the biceps as part of the pathoanatomy. It is typically in a revision setting”; “I must state I would not do this in a competitive thrower only recreational thrower”; “1) failed SLAP repair and 2) want to return to play within 3 months”; “Demonstrated pathology in the biceps tendon”; “SLAP repair don't work so good”; “Addresses the pathology since only do for biceps involvement”; “My history of success when performed on right patient for right reason”; “Based on age and repairability of the labrum in the younger overhead athlete”; “My preference is to leave it unless it has pathology noted at the time of surgery or it is a revision SLAP repair”; “You can’t treat biceps tunnel disease with superior labrum surgery and you can’t repair delaminated” incarcerated junctional biceps tendon injuries.
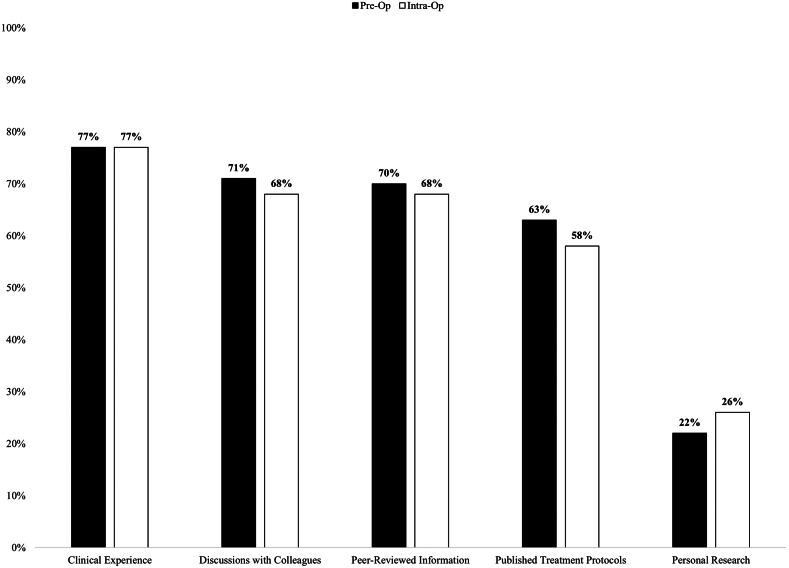
Sources of information used to establish preoperative and intraoperative factors for determining biceps tenodesis as a viable procedure for an injured overhead throwing athlete are summarized in Figure 2. Seventy-seven percent of respondents prioritized personal clinical experience and outcomes from their methods of evaluation and treatment of patients with biceps symptoms, whereas discussions with colleagues, peer-reviewed information on biceps anatomy and mechanics, and published treatment protocols also served as common and frequent sources (63%-71%) for treatment selection.
Fig 2.
Sources of information. (Intra-Op, intraoperative; Pre-Op, preoperative.)
Of the respondents, 71% indicated that the patient’s age is an important factor for choosing the procedure. In addition to using age greater than 26 to 50 years as an indication for surgery (55%), a proportion of the respondents use biceps tenodesis in other age groups: 51% indicated they would use it in patients older than 50 years; 25%, in patients aged between 18 and 25 years; and 7%, in patients younger than 18 years.
There was a scattering of responses regarding the use of specific components of the history evaluation as part of the diagnostic process. Only 3 of 9 history components were selected by more than 50% of the respondents—anterior biceps pain, self-reported biceps instability, and previous surgery—with other responses indicated by 10% to 45% (Fig 3). Similarly, a scattering of responses was observed in the use of components of the physical examination. Four of 9 components—Speed test, palpable biceps groove pain, employment of any special test that targets glenoid labrum pathology, and diagnostic injection—were selected by more than 50% of the respondents, with other responses indicated by 10% to 44% (Fig 4). Magnetic resonance imaging without (71%) and with (49%) arthrogram and plain radiography (41%) were the top selections in the diagnostic process, with diagnostic ultrasound being used the least among the respondents (19%).
Fig 3.
History item responses. (PT, physical therapy.)
Fig 4.
Physical examination item responses. (FAIR, flexion–adduction–internal rotation.)
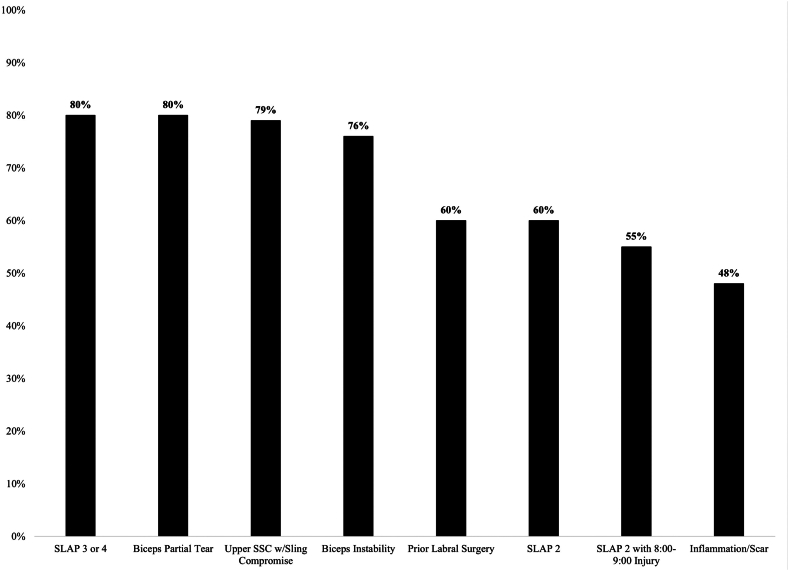
Multiple intraoperative findings were used by 55% or more of the respondents to help establish biceps pathology and provide indications for tenodesis (Fig 5). These included biceps partial tears, type III or IV SLAP tears, upper-border subscapularis injury with sling compromise, SLAP tears at the 11- to 1-o’clock position, and SLAP tears at the 11- to 1-o’clock position with extension into the 8- to 9-o’clock position.
Fig 5.
Surgical indications for biceps tenodesis. (SSC, subscapularis; w, with.)
Discussion
Review and analysis of the articles and the survey responses of experienced shoulder surgeons describing methods for establishing indications for tenodesis as part of the treatment or the entire treatment in the injured overhead throwing athlete showed wide variability in the methodology used. This variability involved differences in the utilization of both the areas of the evaluation process and the individual components within each area. These findings indicate that there is no consensus regarding the most effective combination of the traditional methods of evaluation that can establish the diagnosis of clinically significant biceps involvement in shoulder dysfunction. This lack of consensus cannot provide consistent treatment guidelines to include biceps tenodesis as a part of treatment in this specific population of injured overhead throwing athletes.
Our review of the articles that reported using biceps tenodesis in the treatment of the injured overhead throwing athlete showed no consensus regarding which elements of the diagnostic process should be integral to establishing biceps involvement in the presenting symptoms and dysfunction. This lack of ability to establish consensus was based on the varied evaluation components reported, but more important, there was a noticeable lack of reported use of many of the components traditionally used to make a clinical diagnosis of biceps tendon dysfunction. Articles that report a surgical technique should include a description of the surgical technique (the “how”) and the preoperative and intraoperative evaluation process used to establish surgical indications (the “what”). Only 5 articles reported using some type of component of the clinical history,1,3,5,8,11 and only 2 articles reported using components of the physical examination.8,11 Articles that address a surgical technique such as operative intervention on the biceps would be expected to include, in addition to a description of the surgical technique (the “how”), some information on the preoperative and intraoperative evaluation process used in establishing the diagnosis that pathology of some type involving the biceps is present and can be documented (the “what”). These flaws may be related to study design considering that more than half of the articles were retrospective case series, which are limited to the information available at the time of review. The review of the literature also uncovered variation in surgical indications such as using biceps tenodesis to treat SLAP injuries, to treat biceps pathology, or to revise a previous labral repair. In some instances, specific details regarding tissue integrity and/or appearance were described as the criteria for performing labral repair or biceps tenodesis,3,5,6,8,11 whereas in other instances, broad descriptions such as a type of SLAP injury1,2,4,11 or “pathology at the biceps-labral complex” without specific tissue appearance qualifiers were noted as the diagnostic criteria.9,10 One study noted that patients decided which procedure to receive prior to surgery based on discussions with the surgeon.7 This paucity of information limits the ability of clinicians to properly place the preoperative and intraoperative findings they develop into a consistent context.
In addition, no study provided an overview of the role of the biceps in shoulder function and dysfunction, which could serve as a basis for deciding whether including tenodesis in treatment will be beneficial or harmful to shoulder function in overhead activities. There was no mention of the stabilizing effect of the biceps and how it ensures a reproducible path of articulation of the GHJ in extremes of motion.21 In the review, no article described the clinical presentation of a patient with significant biceps involvement in dysfunction. In addition, papers did not present a rationale for determining what role the biceps involvement may have played in the clinical presentation of the injured overhead throwing athlete.
The literature review shows that these articles present the clinician with limited preoperative and intraoperative evaluation techniques to help make the clinically relevant diagnosis of pathologic biceps dysfunction. Readers attempting to use a literature review as a guide for establishing this diagnosis will find it of marginal benefit because there are no clear diagnostic principles in place to aid in the decision-making process on when to perform a biceps tenodesis in an overhead throwing athlete. This deficit is substantial given the need to establish more precise indications for the use of this procedure.
The survey of experienced shoulder surgeons shows that there is a relatively homogeneous grouping of responses regarding the individual reasoning process about the factors involved in deciding to include biceps tenodesis. This process consisted of (1) why tenodesis was used in overhead throwing athletes, (2) the rationale for deciding to use it, and (3) the sources of personal information to assist in the process. If all these responses had research backing, then they would provide a consistent context to the understanding of including tenodesis in the surgical decision-making process.
Among the 5 most common responses (>50% of respondents) regarding why biceps tenodesis was used was that tenodesis addresses pain relief or persistent clinical dysfunction after previous labral surgery; this was closely followed by the need to address and correct injury in the biceps or adjacent tissues, that is, the labrum (restore the demonstrated pathology, decrease the increased labral tension, or treat synovitis). It was not clear from the responses whether the pain would be derived from the long head of the biceps tendon itself or from an accompanying clinical condition such as a SLAP tear or exactly what pathoanatomic conditions, such as biceps injury or residual posterior labral injury, would be present in the failed labral surgical scenario that would determine the need for tenodesis. In the failed surgical scenario, it would be helpful if the specifics regarding anchor placement and restoration of the normal labral anatomy 2-component labral anatomy were detailed.22 Also, decreased tension in the labrum is frequently not beneficial in that it has been found to alter glenohumeral kinematics and increase pathologic posterior HH translation.13 The 4 most common responses regarding the rationale for using tenodesis included superior pain relief, decreased need for further surgery, and the conclusion that there is literature support for effectiveness in throwing athletes and for better outcomes compared with other techniques.
The 4 common responses listing sources of information reflect personal experience, either clinical experience with patients or interactions with colleagues, and reliance on the use of literature sources. The clinical or collegial experience may reflect disappointing outcomes from other surgical procedures or positive outcomes from the use of tenodesis and may reflect the variable experience from procedures that are shown to be nonanatomic.23 These responses may be altered as contemporary scholarship reveals more information on this subject. More recent biceps anatomy and mechanics publications have showed an important role in biceps function in the complex mechanics of the overhead throwing athlete that confers optimal dynamic glenohumeral kinematics and functional performance,13,24, 25, 26 and 1 recent biomechanical study showed a definite inferior outcome, due to loss of dynamic glenohumeral stability, after biceps tenodesis in baseball pitchers compared with other types of overhead throwing athletes.12 Moreover, as shown in the literature review in our study, the published treatment protocols do not establish a consistent basis for making consistent decisions regarding when to use tenodesis owing to the gaps in the published studies.
There was a high proportion of respondents who considered the patient’s age as a factor in deciding indications for tenodesis. The traditionally cited age cutoff of greater than 35 years was listed frequently, but over one-half of the respondents also listed patients aged between 26 and 35 years as possible candidates and one-third listed patients younger than 25 years as possible candidates. The generalized definition of an overhead throwing athlete presented in the survey allowed inclusion of athletes of all ages and skills to be considered. There are no contemporary studies that would indicate that athletes in these age groups have specific deficits in the physiological or biomechanical properties of the biceps tendon that would in and of themselves create the need to use tenodesis because of intrinsic deficiencies. This age cutoff appears to have its origin in some of the early studies reporting the use of tenodesis, which contained few overhead throwing athletes and whose age range was predominately older, so these recommendations probably have less application to the younger age group.1,27
The survey respondents reported using a scattering of responses regarding individual components from the history and physical examination areas of evaluation. This finding reflects the general lack of objective data concerning many of the evaluation techniques for biceps pathology.28, 29, 30 It was hoped that through the survey process, a more definitive picture of what an experienced group of surgeons was collectively using to make a diagnosis would emerge as a consensus. Only 3 individual components of the history and 4 individual components of the physical examination were selected by more than 50% of respondents, with a wide selection of other responses. There was also no consensus around the optimum number of history components or a grouping of testing components into a specific battery. For example, when examining the distribution of the number of history items selected among the respondents, approximately one-third (35.3%) noted using 2 or fewer items, another one-third (31.9%) noted using 3 to 5 items, and the remaining one-third (32.8%) noted using 6 or more items to help make a clinical diagnosis of biceps involvement. Conversely, just over half the respondents (55.4%) noted using 3 to 5 physical examination elements, with 23.5% using 2 or fewer and 21.1% using 6 or more. Although the largest portion of the respondents noted using several tests, which would align with other works advocating for a testing cluster for shoulder examinations,29,30 a specific testing battery with optimal clinical utility values for ruling in or ruling out biceps pathology has not been identified in the literature.
The survey revealed that there was a homogeneous reasoning process regarding the factors involved in deciding to include biceps tenodesis, but several aspects of the process, such as reliance on published literature, knowledge regarding biceps roles in GHJ stability, and use of a specific age cutoff, were not supported by contemporary literature and may need to be reassessed as foundational thoughts. Also, the responses did not reach a consensus regarding individual components of the history or physical examination areas of evaluation or regarding the appropriate number of components or a specific battery of components.
Limitations
This study has several limitations. First, the literature review is limited by the search criteria, which—although extensive—may have missed some relevant articles because it was directed toward aspects of diagnosis rather than treatment. Second, the survey, although compiled using traditional methods in the diagnostic process, requesting responses to a wide variety of well-established diagnostic questions, and adding an “other” category, may not have captured all of the possible responses. Finally, the study was focused on the population of overhead throwing athletes because of the specific current questions regarding the use of biceps tenodesis in this population. Even though the study was focused on a small segment of the total population of patients who might be treated by biceps tenodesis, the data that were used for analysis may represent heterogeneity within that population owing to the inclusion of patients representing several overhead sports that have differences in biomechanical requirements and demands. Therefore, the conclusions of the analysis may not be generalizable to all overhead athlete subgroups.
Conclusions
The survey revealed there was an incompletely supported reasoning process regarding indications for tenodesis and there was no consensus regarding individual components of the history or physical examination. The literature review revealed a lack of consensus regarding which elements of the diagnostic process are integral in establishing biceps involvement in injured throwing shoulders.
Disclosures
All authors (A.D.S., W.J.G., A.V.S., A.N.B., J.D.K., W.B.K.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Boileau P., Parratte S., Chuinard C., Roussanne Y., Shia D., Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: Biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37:929–936. doi: 10.1177/0363546508330127. [DOI] [PubMed] [Google Scholar]
- 2.Gottschalk M.B., Karas S.G., Ghattas T.N., Burdette R. Subpectoral biceps tenodesis for the treatment of type II and IV superior labral anterior and posterior lesions. Am J Sports Med. 2014;42:2128–2135. doi: 10.1177/0363546514540273. [DOI] [PubMed] [Google Scholar]
- 3.Gupta A.K., Chalmers P.N., Klosterman E.L., et al. Subpectoral biceps tenodesis for bicipital tendonitis with SLAP tear. Orthopedics. 2015;38:e48–e53. doi: 10.3928/01477447-20150105-60. [DOI] [PubMed] [Google Scholar]
- 4.Pogorzelski J., Horan M.P., Hussain Z.B., Vap A., Fritz E.M., Millett P.J. Subpectoral biceps tenodesis for treatment of isolated type II SLAP lesions in a young and active population. Arthroscopy. 2018;34:371–376. doi: 10.1016/j.arthro.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 5.Griffin J.W., Cvetanovich G.L., Kim J., et al. Biceps tenodesis is a viable option for management of proximal biceps injuries in patients less than 25 years of age. Arthroscopy. 2019;35:1036–1041. doi: 10.1016/j.arthro.2018.10.151. [DOI] [PubMed] [Google Scholar]
- 6.Lin B.J., Ling D.I., Calcei J.G., Altchek D.W., O'Brien S.J., Dines J.S. Return to play after biceps tenodesis and transfer in a young, athletic population. Orthopedics. 2021;44:e13–e18. doi: 10.3928/01477447-20201009-03. [DOI] [PubMed] [Google Scholar]
- 7.Hurley E.T., Colasanti C.A., Lorentz N.A., et al. Open subpectoral biceps tenodesis may be an alternative to arthroscopic repair for SLAP tears in patients under 30. Arthroscopy. 2022;38:307–312. doi: 10.1016/j.arthro.2021.07.028. [DOI] [PubMed] [Google Scholar]
- 8.Lacheta L., Horan M.P., Nolte P.C., Goldenberg B.T., Dekker T.J., Millett P.J. SLAP repair versus subpectoral biceps tenodesis for isolated SLAP type 2 lesions in overhead athletes younger than 35 years: Comparison of minimum 2-year outcomes. Orthop J Sports Med. 2022;10 doi: 10.1177/23259671221105239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lorentz N.A., Hurley E.T., Colasanti C.A., et al. Return to play after biceps tenodesis for isolated SLAP tears in overhead athletes. Am J Sports Med. 2022;50:1369–1374. doi: 10.1177/03635465211041698. [DOI] [PubMed] [Google Scholar]
- 10.Rothermich M.A., Ryan M.K., Fleisig G.S., et al. Clinical outcomes and return to play in softball players following SLAP repair or biceps tenodesis. J Shoulder Elbow Surg. 2023;32:924–930. doi: 10.1016/j.jse.2022.10.025. [DOI] [PubMed] [Google Scholar]
- 11.Waterman B.R., Newgren J., Richardson C., Romeo A.A. High rate of return to sporting activity among overhead athletes with subpectoral biceps tenodesis for type II SLAP tear. Arthroscopy. 2023;39:11–16. doi: 10.1016/j.arthro.2022.07.017. [DOI] [PubMed] [Google Scholar]
- 12.Klemt C., Toderita D., Reilly P., Bull A.M.J. Biceps tenodesis cannot be used as primary treatment option in baseball pitchers with intact rotator cuff muscles. Clin Biomech. 2022;100 doi: 10.1016/j.clinbiomech.2022.105819. [DOI] [PubMed] [Google Scholar]
- 13.Rauck R.C., Jahandar A., Kontaxis A., et al. The role of the long head of the biceps tendon in posterior shoulder stabilization during forward flexion. J Shoulder Elbow Surg. 2022;31:1254–1260. doi: 10.1016/j.jse.2021.12.026. [DOI] [PubMed] [Google Scholar]
- 14.Graichen H., Stammberger T., Bonel H., Karl-Hans E., Reiser M., Eckstein F. Glenohumeral translation during active and passive elevation of the shoulder—A 3D open-MRI study. J Biomech. 2000;33:609–613. doi: 10.1016/s0021-9290(99)00209-2. [DOI] [PubMed] [Google Scholar]
- 15.Kibler W.B., Sciascia A., Tokish J.T., et al. Disabled throwing shoulder 2021 update: Part 1—Anatomy and mechanics. Arthroscopy. 2022;38:1714–1726. doi: 10.1016/j.arthro.2022.02.001. [DOI] [PubMed] [Google Scholar]
- 16.McGarry M.H., Nguyen M.L., Quigley R.J., Hanypsiak B., Gupta R., Lee T.Q. The effect of long and short head biceps loading on glenohumeral joint rotational range of motion and humeral head position. Knee Surg Sports Traumatol Arthrosc. 2016;24:1979–1987. doi: 10.1007/s00167-014-3318-5. [DOI] [PubMed] [Google Scholar]
- 17.Kibler W.B., Sciascia A. Current practice for the diagnosis of a superior labral anterior to posterior (SLAP) lesion: Systematic review and physician survey. Arthroscopy. 2015;31:2456–2469. doi: 10.1016/j.arthro.2015.06.033. [DOI] [PubMed] [Google Scholar]
- 18.Kibler W.B., Sciascia A. Current practice for the treatment of superior labral anterior to posterior (SLAP) lesions: A systematic review. Arthroscopy. 2016;32:669–683. doi: 10.1016/j.arthro.2015.08.041. [DOI] [PubMed] [Google Scholar]
- 19.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—A web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization . World Health Organization; Geneva: 2013. How to use the ICF: A practical manual for using the International Classification of Functioning, Disability and Health. [Google Scholar]
- 21.Youm T., ElAttrache N.S., Tibone J.E., McGarry M.H., Lee T.Q. The effect of the long head of the biceps on glenohumeral kinematics. J Shoulder Elbow Surg. 2009;18:122–129. doi: 10.1016/j.jse.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 22.Bain G.I., Galley I.J., Singh C., Carter C., Eng K. Anatomic study of the superior glenoid labrum. Clin Anat. 2013;26:367–376. doi: 10.1002/ca.22145. [DOI] [PubMed] [Google Scholar]
- 23.Fourman M.S., Arner J.W., Bayer S., Vyas D., Bradley J.P. Type VIII SLAP repair at midterm follow-up: Throwers have greater pain, decreased function, and poorer return to play. Arthroscopy. 2018;34:3159–3164. doi: 10.1016/j.arthro.2018.06.055. [DOI] [PubMed] [Google Scholar]
- 24.Hwang E., Hughes R.E., Palmer M.L., Carpenter J.E. Effects of biceps tension on the torn superior glenoid labrum. J Orthop Res. 2015;33:1545–1551. doi: 10.1002/jor.22888. [DOI] [PubMed] [Google Scholar]
- 25.Eichinger J.K., Li X., Cohen S.B., et al. American Shoulder and Elbow Surgeons SLAP/Biceps Anchor Study Group evidence review: Pathoanatomy and diagnosis in clinically significant labral injuries. J Shoulder Elbow Surg. 2023;32:e179–e190. doi: 10.1016/j.jse.2022.12.015. [DOI] [PubMed] [Google Scholar]
- 26.Kibler W.B., Sciascia A., Grantham W.J. The shoulder joint complex in the throwing motion. J Shoulder Elbow Surg. 2024;33:443–449. doi: 10.1016/j.jse.2023.06.031. [DOI] [PubMed] [Google Scholar]
- 27.Provencher M.T., McCormick F., Dewing C., McIntire S., Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: Outcomes and factors associated with success and failure. Am J Sports Med. 2013;41:880–886. doi: 10.1177/0363546513477363. [DOI] [PubMed] [Google Scholar]
- 28.Hegedus E.J., Goode A., Campbell S., et al. Physical examination tests of the shoulder: A systematic review with meta-analysis of individual tests. Br J Sports Med. 2008;42:80–92. doi: 10.1136/bjsm.2007.038406. [DOI] [PubMed] [Google Scholar]
- 29.Hegedus E.J., Goode A.P., Cook C.E., et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46:964–978. doi: 10.1136/bjsports-2012-091066. [DOI] [PubMed] [Google Scholar]
- 30.Hegedus E.J., Cook C., Lewis J., Wright A., Park J.Y. Combining orthopedic special tests to improve diagnosis of shoulder pathology. Phys Ther Sport. 2015;16:87–92. doi: 10.1016/j.ptsp.2014.08.001. [DOI] [PubMed] [Google Scholar]