Abstract
Background
Prevalence estimates for autism spectrum disorder (ASD) in the Middle East and North Africa (MENA) region are not readily available, amid a lack of recent evidence. In this study, we estimated the prevalence of ASD in the MENA region by synthesising evidence from published studies.
Methods
We conducted a systematic review and meta-analysis, searching PubMed, EMBASE, Scopus, and CINAHL for studies assessing ASD prevalence in the MENA region. Risk of bias was assessed using the Newcastle Ottawa scale. A bias-adjusted inverse variance heterogeneity meta-analysis model was used to synthesize prevalence estimates from included studies. Cochran’s Q statistic and the I2 statistic were used to assess heterogeneity, and publication bias assessed using funnel and Doi plots.
Results
Of 3,739 studies identified, 19 met the inclusion criteria, published during the period 2007–2025, from Iran, Oman, Libya, Egypt, Saudi Arabia, Lebanon, United Arab Emirates, Bahrain, and Qatar, Iraq. Country specific prevalence estimates ranged from 0.01% in Oman in 2009 to 6.50% in one study from Iraq in 2024. The overall prevalence of ASD in the MENA region was 0.14% (95%CI 0.02– 0.36%), with significant heterogeneity (I2 = 99.8%). Overall ASD prevalence was 0.04% (95%CI 0.00–0.13, I2 = 99.4%) for studies done before 2015 and 0.45% (95%CI 0.17–0.87, I2 = 99.4%) for studies after 2015. Overall ASD prevalence was high in studies that used the Modified Checklist for Autism in Toddlers (M-CHAT) only [1.66% (95%CI 0.15–4.33, I2 = 97.5%)] while the overall ASD prevalence was 0.14% (95%CI 0.00-0.46, I2 = 99.9%) for studies that used the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for diagnosis.
Conclusion
Estimates of the prevalence of ASD vary widely across the MENA region, with variability in ASD prevalence estimates by diagnostic methods and sampling approaches. While the data suggest a possible increase in prevalence during the study period, this observation warrants further investigation through more robust, longitudinal, and methodologically consistent studies.
Registration
PROSPERO registration ID CRD42024499837.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-23651-x.
Keywords: Autism spectrum disorder, Prevalence, Middle East and North Africa
Introduction
The autism spectrum disorder (ASD) is a neurological and developmental disorder whose main features include difficulties with social communication and social interactions, restricted, repetitive behavioural patterns, and limited interests [1]. The disorder includes neuro-developmental disorders such as autistic disorder, pervasive developmental disorder, and Asperger’s syndrome [2]. Another neurodevelopmental disorder which was formerly part of ASD, Rett disorder, is no longer classified under the spectrum, according to the Diagnostic and Statistical Manual of mental disorders (5th ed.) (DSM-V) [1]. Individuals with ASD may exhibit symptoms from mild to severe, depending on where they lie on the spectrum [2, 3], and this may also affect long term outcomes such as independent living, employment social and independent functioning [4]. ASD symptoms usually manifest in early childhood and persist throughout life. ASD carries significant financial, social, and health-related burden to individuals, families, and society. Families of individuals with ASD often face significant emotional and financial challenges due to high levels of anxiety, stress, and isolation associated with caregiving, as well as the extensive financial resources required [5]. Co-occurring conditions, such as anxiety disorders, attention deficit/hyperactivity disorder (ADHD), depression, intellectual disability and seizures are common among individuals with ASD [6], with one study showing that over 70% of individuals with ASD have at least one co-occurring psychiatric condition, and more than 40% have two or more [7].
ASD affects all regional, racial, and socioeconomic groups. The global prevalence of ASD in 2023 was approximately 1 in 100 children [8], with higher prevalence estimates from high income countries [9]. ASD prevalence varies globally due to several reasons, which include variation in awareness in different countries, the absence of diagnostic tools that are culture sensitive, and cultural variation in interpreting the behaviour of children [5, 10]. The reported prevalence of ASD in the MENA region tends to be lower than in Western European countries [11]. This could be because of underestimation of ASD prevalence due to social stigma, limited access to diagnostic resources, and poor screening programs in some MENA countries [12].
Recent epidemiological studies indicate a significant global increase in the prevalence of ASD over the past few years [13, 14]. Data from one systematic review suggested that the prevalence of ASD in the MENA region has increased by 70% between 1990 and 2019, comprising 7.5% of the new ASD cases globally [12]. This increase in ASD prevalence has been attributed to several reasons including an expanded definition of the spectrum, updates in diagnostic criteria and screening tools, shifts in research methodologies, and greater awareness of ASD [7]. However, estimates of ASD prevalence in the MENA region were based on only a few studies, and current estimates of ASD prevalence are lacking. The aforementioned systematic review [12] left out many existing prevalence studies from the Middle East and North Africa region. This highlights the need for an up-to-date systematic review and meta-analyses to estimate the prevalence of ASD in the MENA region, which is the aim of the present study.
Methods
Study design and protocol registration
A systematic review and meta-analysis of ASD prevalence studies was carried out. The study adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Supplementary Table S1) [15]. The study protocol is registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the registration number CRD42024499837.
Search strategy and study selection
We searched PubMed, EMBASE, Scopus, and Cumulative Index to Nursing and Allied Health Literature (CINAHL) for relevant articles published until 30 April 2025. We used medical subject headings (MeSH terms) and keyword searches for ASD and the Middle East and North Africa (MENA) region in the PubMed search. No language restrictions were imposed. The detailed search strategy is shown in Supplementary Tables S2– S5. After removing duplicates using EndNote, the Rayyan systematic review management website (www.rayyan.ai) was used to screen studies for inclusion. Within Rayyan, two reviewers independently screened each study for inclusion based on the title and abstract. After this initial screening, two reviewers independently screened the full text of each preliminarily identified study for inclusion, based on the specified inclusion criteria. In cases of disagreement between reviewers, a third reviewer was consulted.
Eligibility criteria
This systematic review and meta-analysis included observational studies that investigated the prevalence of ASD in the MENA region. Studies were included if they documented the prevalence of ASD and were conducted in the following countries: Algeria, Bahrain, Djibouti, Egypt, Iran, Iraq, Jordan, Saudi Arabia, Kuwait, Lebanon, Libya, Mauritania, Morocco, Oman, Palestine, Qatar, Somalia, Sudan, Syria, Tunisia, United Arab Emirates, or Yemen. Studies were excluded if the study population included participants living outside of the MENA region. Studies were also excluded if they were experimental, case series, case reports, letters, opinions, narrative reviews, or other studies that did not contain primary data, if they were duplicates, or if they did not have full text. Case control studies were included only if they calculated prevalence by dividing all the known existing cases in a country by the country’s population rather than cases divided by controls.
Data extraction
In case of duplicate publications, the article that contained the most information was included in the review and all others were excluded as duplicates. The data extracted from the studies included: publication year, country, study design, study period, ASD screening tool used, mean age of participants, and sample size. The prevalence was extracted as the number of ASD cases (numerator) over the total sample size (denominator). For each study, two reviewers independently extracted the data into a standardized data extraction sheet using Microsoft Office Excel. Disparities in data extracted were resolved via discussion between the reviewers.
Assessment of the quality of included studies
The quality of the included studies was assessed using a modified version of the Newcastle Ottawa Scale (NOS) (Supplementary Tables S6– S7). The NOS assesses internal and external validity in cross sectional studies with scores ranging from 0 to 15 points [16]. Studies were categorized based on quality scores, with scores between 13 and 15 indicating high quality, 8 to 12 indicating moderate quality, and scores below 7 indicating low quality. Each included study was independently evaluated by two reviewers. In case of discrepancies, a third reviewer was consulted.
Synthesis of findings
We narratively described data that were not meta-analysed, and these data included author names, year of publication, country, study design, and sample size. Unadjusted prevalence estimates of ASD and their 95% confidence intervals were calculated for each included study, and they were then pooled, when possible. The quality-effects model was used for the subsequent meta-analysis [17]. This model depends on the use of additional data, including the quality ranking of each study, to modify the variance weights. The modified NOS was used to calculate the quality weights. In the meta-analysis, the variance of the prevalence data was stabilized using the Freeman-Tukey transformation and back transformed after synthesis. To assess the robustness of the results, sensitivity analysis using leave-one-out analyses was also performed. Forest plots were used to show the pooled prevalence estimate. Cochran’s Q p-values and the I2 statistic were used to measure heterogeneity [18]. I2 values of 25%, 50%, and 75%, respectively, were taken to represent low, moderate, and high levels of statistical inconsistency. Subgroup analyses were carried out by diagnostic methods and year of study. Funnel and Doi plots were used to evaluate publication bias. The LFK index was used to assess symmetry in Doi plots, with a value greater than 1 or less than − 1 indicating minor asymmetry, and a value greater than 2 or less than − 2 indicating major asymmetry [19]. Exact p-values were reported. Stata [18] statistical software was used to conduct all analyses, and PRISMA guidelines [20] were followed.
Results
Search results
A total of 3739 study reports were identified from database searches. After deduplication, and screening using title and abstracts, 238 study reports had full text retrieved for eligibility screening (Fig. 1, and Supplementary Table S8). The final number of studies included in the systematic review and meta-analysis was 19 [21–39].
Fig. 1.
PRISMA flowchart outlining the study selection process
Characteristics of included studies
The characteristics of the 19 studies in the systematic review and meta-analysis are shown in Table 1. Most of the studies were from Iran (n = 6) [23, 27–29, 31, 32], there were two each from Oman [21, 24], Saudi Arabia [30, 36], Bahrain ([35, 39] and Qatar [25, 37]. The following countries contributed one study each to the analysis: Egypt [33], Lebanon [26],, United Arab Emirates [22], Iraq [38] and Libya [34]. Most of the studies were published during the year 2019 (n = 5). There was one study from each of the years: 2007, 2010, 2011, 2013, 2015, 2016, 2022, 2024 and two studies from 2012, 2021 and 2025.
Table 1.
Characteristics of included studies
| Study | Prevalence Year | Country | Study Design | Total Number of Participants | ASD Number of participants | Mean age of participants (in years) | % of males in study | Screening tool used | ASD prevalence (per 10,000) |
|---|---|---|---|---|---|---|---|---|---|
| Eapen, 2007 [22] | Not specified | UAE | cross sectional | 694 | 2 | 3 | 49.4 | DSM-IV | 29 |
| Sasanfar, 2010 [23] | 2005 | Iran | case-cohort | 200,000 | 219 | Age range 5–11 (mean age not specified) | 51.6 | SCQ and DSM-IV TR | 11 |
| Al Farsi, 2011 [21] | 2009 | Oman | cross sectional | 798,913 | 113 | Age range 0–14 | 74.3 | DSM-IV-TR | 1.4 |
| Samadi, 2012 [31] | 2006–2009 | Iran | cross sectional | 1,320,334 | 826 | 5 | 51.4 | ADI-R | 6.3 |
| Zeglam, 2012 [34] | 2005–2009 | Libya | cross sectional | 38 508 | 128 | 4 (median age) | Not stated | DSM-IV | 30 |
| Al-Ansari, 2013 [35] | 2005 | Bahrain | Case- control | Not specified | 100 | 10.5 (± 6.4) (for cases) | 80 (cases only) | M-CHAT, DSM-IV-TR and CARS | 4.3 |
| Samadi, 2015 [32] | 2010 | Iran | cross sectional | 2941 | 28 | 3.3 | 54.8 | ADOS, ADI-R | 95.2 |
| Chaaya, 2016 [26] | 2014 | Lebanon | cross sectional | 998 | 15 | 2.3 | 54 | M-CHAT and a short questionnaire | 153 |
| Goodarzi, 2019 [27] | 2015–2016 | Iran | cross sectional | 1500 | 23 | 2(for cases) | 46.9 | M-CHAT | 150 |
| Al- Mamri, 2019 [24] | 2011–2018 | Oman | retrospective descriptive study | 837,655 | 1705 | 4.8 ± 2.4 (for cases) | 78.1 (cases only) | DSM-V | 20.4 |
| Mohammadi, 2019 [29] | Not specified | Iran | cross sectional | 31,000 | 37 | 6–18 | 49 | K-SADS-PL | 10 |
| Manzouri, 2019 [28] | 2017 | Iran | cross sectional | 1504 | 12 | 2 | 50.2 | M-CHAT-R/F | 80 |
| Alshaban, 2019 [25] | 2015 | Qatar | cross sectional | 133,781 | 1525 | Not specified | Not specified | DSM-V | 114 |
| Sabbagh, 2021[30] | 2020 | Saudi Arabia | cross sectional | 347,036 | 1023 | 9 | 76.6 (cases only) | DSM-V | 28.1 |
| Yousef, 2021 [33] | 2017 | Egypt | cross sectional | 3722 | 2 | Not specified | 50.7 | DSM-V, CARS | 54 |
| Albatti, 2022[36] | 2017–2018 | Saudi Arabia | cross sectional | 398 | 10 | Age range 2–4 ( | 51.7 | M-CHAT-R, ADOS-2 | 250 |
| Sameea, 2024 [37] | 2017–2018 | Qatar | cross-sectional | 600 | 26 | 2 | 48 | M-CHAT | 433 |
| Almohri, 2025 [39] | 2021–2022 | Bahrain | cross-sectional | 3729 | 19 | 2 | 51.3 | DSM-V, M-CHAT R | 51 |
| Majeed, 2025 [38] | 2024 | Iraq | Descriptive | 200 | 13 | 2 | 58.5 | M-CHAT R | 650 |
SCQ Social Communication Questionnaire, M-CHAT Modified Checklist for Autism in Toddlers, CARS Childhood Autism Rating Scale, DSM-IV-TR Diagnostic and statistical manual of mental disorders, 4th ed, text revision, ADOS Autism Diagnostic Observation Schedule, ADI Autism diagnostic interview, K-SADS-PL The Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version
A total of fifteen studies used a cross-sectional design, two studies used a descriptive unspecified design, one study used a case control design, and one study used a case-cohort design. Case control studies were included only if they calculated prevalence by dividing all the known existing cases in a country by the country’s population rather than cases divided by controls. The case control study [35], was only described in the systematic review and not included in the meta-analysis as it did not explicitly state the numerator and denominator used in the prevalence calculation. There was variability in diagnostic tools used across studies, with the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) and Modified Checklist for Autism in Toddlers (M-CHAT) being used by five studies each. Other tools used in defining ASD included The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V), Autism Diagnostic Interview-Revised (ADI-R), Social Communication Questionnaire (SCQ), Autism Diagnostic Observation Schedule (ADOS), Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) and Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (2009) (K-SADS-PL-2009).
Assessment of the quality of included studies
The quality assessment of the included studies was assessed using a modified version of the Newcastle-Ottawa Scale. Thirteen of the included studies were of moderate quality, the scores ranged from 8 to 15 and the average was 11 out of 15. Most of the cross-sectional studies had safeguards present in at least five domains that the Newcastle-Ottawa Scale assessed including representatives of the sample, sample size, assessment of outcome. The individual quality assessments of all the included studies are shown in Supplementary Tables S9– S10.
Prevalence of autism spectrum disorder
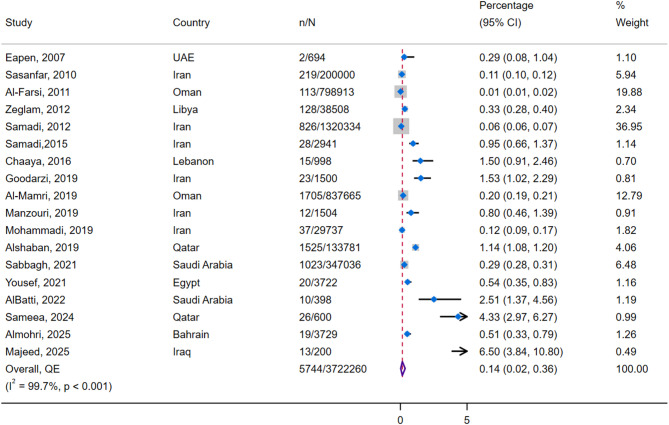
The metanalysis included a total of 3,722,260 participants, 5744 of whom had ASD. As shown in Fig. 2, the overall synthesised prevalence was 0.14% (95%CI 0.02–0.36%, n = 18 studies), with high heterogeneity (I2 = 99.7%). Assessment of publication bias showed major asymmetry (Supplementary Figures S1– S2). In sensitivity analysis, the prevalence ranged from 0.12 to 0.21% after successive removal of each study (Supplementary Figure S3).
Fig. 2.
Forest plot of overall prevalence of autism spectrum disorder
Due to the high heterogeneity observed, a descriptive analysis of ASD prevalence in each country was carried out. The ASD prevalence ranged from 0.01% in Oman to 6.50% in one study in Iraq. In the UAE, the prevalence of ASD was 0.43% (95%CI 0.15-1.26%), again from a single study published in 2007 [22]. In Oman, the prevalence varied from 0.01% (95%CI 0.01-0.02%) in 2009 [21] to 0.20% (95%CI 0.19-0.21%) between the years 2011–2018 [24]. In Qatar, ASD prevalence was 1.14% (95%CI 1.08-1.20%) [25] in one study published in the year 2015 and 4.33% (95%CI 2.97–6.27%) in a study using data from 2017 to 2018 [37]. Between the years 2005–2009 in Libya, the prevalence was 0.33% (95%CI 0.28-0.40%) [34]. In Bahrain for the year 2005, the prevalence was 0.043% [35] while between 2021 and 2022, the prevalence was 0.51% (95%CI 0.33-0.79%) [39]. In Lebanon, the prevalence was 1.50% (95%CI 0.91-2.46%) in 2014 [26]. In Egypt, the prevalence of ASD was 0.54% (95%CI 0.35-0.83%) in 2017 [33]. In Saudi Arabia, the prevalence of ASD was 2.51% (95%CI 1.37-4.56%) in one study done between the years 2017–2018 [36] and 0.29% (95%CI 0.28-0.31%) in another study carried out during 2020 [30]. In Iraq, based on data from one study, the prevalence in 2024 was 6.50% (95%CI 3.84-10.80%) [38].
Subgroup analysis
ASD prevalence by diagnostic method
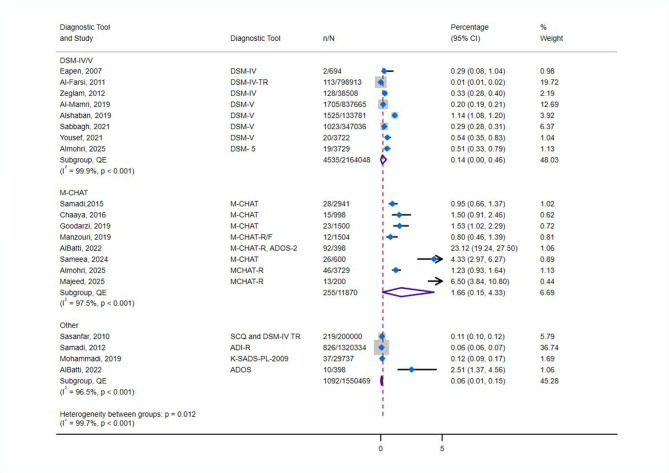
A subgroup analysis was carried out to evaluate the influence of diagnostic tools on the reported prevalence of ASD (Fig. 3). Two main categories of diagnostic tools were identified: DSM-based criteria (n = 8) and M-CHAT (n = 8). On the M-CHAT, children scoring in both the moderate and high risk of ASD score ranges were considered as a positive case of ASD. The remaining tools used by other studies were analysed together as a different category (n = 4).
Fig. 3.
Forest plot of autism spectrum disorder prevalence by diagnostic tool
Studies that used DSM-IV/V criteria had an overall synthesized prevalence of 0.14 (95%CI 0.00-0.46) with high heterogeneity (I2 = 99.9%). However, as expected, studies that utilised the M-CHAT only, had a much higher overall prevalence of 1.66% (95%CI 0.15–4.33) also with high heterogeneity (I2 = 97.5%). An overall estimate of studies that used all the other tools which included SCQ and DSM-IV TR, ADI-R, K-SADS-PL-2009 and ADOS, showed a prevalence of 0.06% (95%CI 0.01–0.15).
ASD prevalence by estimation method
A subgroup analysis based on prevalence methodology was also done to compare studies that calculated prevalence by dividing the number of individuals who tested positive over the total number of individuals screened to studies that calculated prevalence using registry-based data by dividing the total number of known cases from autism centres by similarly aged population from census data. The results are shown in Fig. 4. The overall prevalence from studies that estimated prevalence by the former method (n = 12) was an ASD prevalence of 0.19% (95%CI 0.00–0.55) with high heterogeneity (I² = 96.8%), while registry-based studies (n = 5) yielded a slightly lower overall prevalence of 0.11% (95%CI 0.00–0.31), also with high heterogeneity (I² = 99.9%).
Fig. 4.
Forest plot of autism spectrum disorder prevalence by method of prevalence calculation
ASD prevalence by year
Figure 5 shows a subgroup analysis of ASD prevalence by year. Using the year 2015 as a midpoint, the majority of the studies (n = 5/6) published before or during 2015 reported a prevalence lower than 0.50% while studies after 2015 tended to report a prevalence greater than 0.50% (n = 6/10). The overall prevalence estimate for studies that investigated prevalence before 2015 was 0.04% (95%CI 0.00–0.13, I2 = 99.4%), whereas the overall prevalence estimate for studies that investigated prevalence after 2015 was 0.45% (95%CI 0.17–0.87, I2 = 99.4%),
Fig. 5.
Forest plot of autism spectrum disorder prevalence by year
Prevalence by Country
To explore the high heterogeneity in the overall prevalence estimate, subgroup analysis was carried out by country, but because of sparse data from other countries, the analysis was restricted to Iran only, which had six studies (Fig. 6). In Iran, the prevalence of ASD ranged from 0.06% in a study carried out during 2006–2009 in a sample of 1,320,334 to a high of 1.53% in a sample of 1500 in a study carried out during 2015–2016. The overall synthesised prevalence was 0.06% (95%CI 0.00–0.19), with high heterogeneity (I2 = 97.5%), and some evidence of publication bias/small study effects (Supplementary Figures S4– S5). A leave-one-out analysis showed that the Samadi study [31] had the most significant influence on the overall prevalence and the prevalence without this study would have been 0.12% (95%CI 0.00–0.45) (Supplementary Figure S6). Subgroup analysis could not be done for the other countries as there were insufficient studies
Fig. 6.
Forest plot of autism spectrum disorder prevalence in Iran
Secondary outcomes
We also aimed to examine the prevalence of difference severity phenotypes of ASD in the MENA region. There were three studies that reported phenotype specific ASD data: one each from Libya, Egypt, and Saudi Arabia. A meta-analysis was not done due to few studies being available. In Libya, out of 180 children referred to Al-Khadra Teaching Hospital for delayed speech and language, six had Asperger syndrome [34]. In Egypt, out of the 104 children at high risk for ASD, 13 were diagnosed with mild to moderate ASD and 7 were diagnosed with severe ASD [33]. In Saudi Arabia, out of 205 children diagnosed with ASD, 62 were diagnosed with mild ASD, 106 with moderate ASD and 37 with severe ASD [30].
Discussion
In this systematic review and meta-analysis of 19 studies and a total of 3,722,260 participants, we found that the prevalence of ASD ranged from 0.01% in Oman to 6.50% in Iraq and an overall prevalence of 0.14% in the MENA region. The analysis revealed high heterogeneity which was expected due to differences in prevalence measurement methods and diagnostic tools employed by studies included in the metanalysis.
The overall prevalence of ASD in the MENA region reported in the present study of 0.14% is much lower than the global prevalence calculated by the WHO of 1%. Earlier meta-analyses, with fewer studies also reported a lower estimate of ASD prevalence in the MENA region similar to our meta-analysis. A regional meta-analysis conducted in 2014 by Salhia et al. estimated the prevalence of ASD in the Gulf region to be between 0.014 and 0.29% [40]. A more recent meta-analysis, published in 20222, on global ASD prevalence estimated the ASD prevalence to be 1% (95% CI 0.3–3.1%) in Africa, and 0.4% (95% CI 0.1-1%) in Asia with an overall worldwide prevalence of 0.6% (95% CI 0.4-1%) [5]. Notably, these existing meta-analyses did not include many of our included studies and therefore the current study offers the most up-to-date estimates of ASD prevalence in the region. The low reported prevalence of ASD in the MENA region when compared globally can likely be attributed to a combination of underdiagnosis and methodological limitations. Underdiagnosis may result from limited awareness and training among primary care providers, leading to delayed recognition and referral for assessment. Additionally, social stigma surrounding developmental and psychiatric disorders may discourage families, particularly those with children that are “high functioning” from seeking evaluation. Methodological factors could also be contributing to the relatively low prevalence. The lack of standardization in diagnostic approaches across countries and studies in the MENA region limits comparability between studies. While some included studies used locally adapted versions of tools like the M-CHAT, these were often self-translated and not formally validated. This lack of culturally and linguistically appropriate tools is a critical issue as it can reduce diagnostic sensitivity, hinder accurate interpretation, and contribute to underreporting of ASD in the region.
We observed a wide variation in the individual prevalence of MENA countries in the current systematic review and meta-analysis, with prevalence rates ranging 0.01% in Oman to 6.50% in Iraq. The differences in the individual prevalence could be due to the variations in diagnostic tools,, methods of calculating prevalence, and the time periods investigated by each study. Subgroup analysis by diagnostic tool, of which DSM-IV/V and MCHAT were the most commonly used, showed that studies where DSM-V was used reported relatively lower prevalence (overall prevalence of 0.14%) while studies using the M-CHAT reported much higher prevalence estimates (overall prevalence of 1.66%). This discrepancy is expected, as the M-CHAT is a screening tool with high sensitivity at the expense of specificity, whereas the DSM-V is a highly specific tool for formal ASD diagnosis. The use of various other tools across studies including ADOS and ADI-R, highlights the need for a standardized tool in prevalence research across the region. With regards to the method of calculating prevalence, studies that screened all members of a selected sample to calculate prevalence had a slightly higher overall prevalence (0.19%) compared to studies that used registry-based data (0.11%). The former method gives a better estimation of the true prevalence of ASD compared to studies that used registry-based data as it is more likely to identify undiagnosed ASD cases in the population. Therefore, future prevalence research should prioritise population-based screening over registry-based data to yield higher-quality data.
Some of the between-country differences in ASD prevalence may be explained by factors beyond study methodology. Underdiagnosis is more likely in low- and middle-income countries due to societal stigma and limited access to healthcare [41], while higher prevalence estimates in countries like Qatar may reflect more robust screening programs. Additionally, several risk factors have been attributed to the pathogenesis of ASD, including genetic [42] and parental factors such as advanced maternal age [43], consanguinity [44], and environmental factors such as infections during pregnancy [45], and the distribution of these risk factors varies between countries.
Our analyses suggested that ASD prevalence increased by at least 10-fold from 0.04% before 2015, the midpoint publication year in our analysis, to 0.45% in studies published after 2015. In countries with repeated prevalence assessments, such as Oman, this trend was particularly evident, with reported estimates rising from 0.01 to 0.20% in studies that use the same diagnostic tool [21, 24]. This generally agrees with the 70% increase in ASD prevalence in the MENA region reported by a 2023 global burden study [12]. Increases in ASD prevalence have been noted in almost all regions [46–48]. Although the reasons behind the increase in ASD prevalence remain contentious, there are strong data that suggest that this increase in ASD prevalence could be attributable to; more awareness of ASD and the use of highly sensitive screening tools such as the M-CHAT, screening of children at high age groups where ASD symptoms become more pronounced, instead of screening younger children only as was done historically, and increasing exposure to environmental risk factors [48]. The possibility that ASD prevalence has also increased, despite all these explanations, is also highly likely to be true. It is also true that the absolute numbers of individuals with ASD has increased and will likely continue to increase in the MENA and across all regions for the foreseeable future. While questions about the likely reasons for the increases in ASD prevalence are valid and need science-led answers, it is also important for public health authorities to expand the availability and quality of therapeutic and rehabilitation services for individuals with ASD. Many pharmacological and non-pharmacological treatments generally control some symptoms such as impulsivity and hyperactivity but have not shown much efficacy in relieving symptoms at the core of ASD, with probably the exception of cognitive behaviour therapy, and, to some extent, music therapy, which have shown some promising results [49]. It is therefore imperative to increase research on therapy and rehabilitative services for ASD.
It must also be noted that African countries within the MENA region were significantly underrepresented in the available literature. Only two studies from African MENA countries were included in this review [33, 34]. Several factors may contribute to this gap, including a lack of funding for ASD research, scarcity of dedicated ASD centres and specialists, lower public awareness of ASD, and underdiagnosis due to fewer diagnostic and referral resources.
The current study has several strengths. In this study, we provide the most recent estimates of the prevalence of ASD in the MENA region. Our included 19 studies are the biggest yet in all analyses from the region and the study employs a bias-adjusted synthesis method to weight and rank the studies based on methodological quality. This method is considered more robust than the random effects model when dealing with heterogeneous studies [50]. However, there are some limitations. Firstly, a few of the included studies calculated prevalence using registry based data which may underestimate the true prevalence. Secondly, based on the Egger’s p value, LFK index, and Doi plot in our syntheses, there is a possibility of publication bias affecting our study results. This underscores the need for more high-quality, large-scale studies in the MENA region to improve the robustness of future meta-analyses. Finally, we also observed a paucity of data regarding the prevalence of ASD particularly from African countries in the MENA region and of the different subtypes and severity of autism in the MENA region. Therefore, future studies should aim to fill these literature gaps.
Conclusion
Estimates of the prevalence of ASD varied widely across the MENA region, from 0.01% in Oman to 6.50% in Iraq, with an overall prevalence of 0.14%. While some data suggest a possible increase in prevalence, this observation warrants further investigation. In the future, more and better-quality research should explore the causes of these observed differences and provide up to date ASD prevalence estimates. Our findings also highlight the variability in ASD prevalence within the MENA region and underscore the need for standardized diagnostic criteria and reporting methods to better understand and address the burden of ASD across different populations in the region. Further research is warranted to explore the underlying factors contributing to the observed differences and to develop region-specific strategies for early diagnosis and intervention.
Supplementary Information
Acknowledgements
The authors acknowledge the valuable contributions of participants who provided data in the included primary studies.
Authors’ contributions
A. F. A.: Conceptualization, Methodology, Writing - Original Draft, Writing - Review & Editing, Project administration. B.M. A.: Methodology, Writing - Original Draft, Writing - Review & Editing, Project administration. F. R. M.: Conceptualization, Methodology, Writing - Original Draft, Writing - Review & Editing, Project administration. A.M. E.: Methodology, Software, Formal analysis, Data Curation. E.M.: Methodology, Software, Formal analysis. A.A.A.: Methodology, Writing - Original Draft. N.D.: Methodology, Writing - Original Draft. Y.D.: Methodology, Writing - Original Draft. D.Y.: Methodology, Writing - Original Draft. H.K.: Methodology, Writing - Original Draft. M. A.: Methodology, Writing - Original Draft. M.W.A.: Methodology, Writing - Review & Editing. M.K: Methodology, Writing - Review & Editing. D.S.: Methodology, Writing - Review & Editing. M.A.: Methodology, Writing - Review & Editing. S.M.K.: Conceptualization, Methodology, Supervision, Writing - Review & Editing Project administration, Funding acquisition. T.C.: Conceptualization, Methodology, Software, Validation, Investigation, Resources, Writing - Review & Editing, Formal analysis, Supervision, Project administration, Funding acquisition, Corresponding author. All authors made a significant contribution to the work reported and gave final approval of the version to be published.
Funding
This work was supported by the Qatar National Research Fund, Undergraduate Research Experience Program (UREP) (Grant ID: UREP30-211-3-073). Open Access Funding provided by the University of Washington Tacoma.
Data availability
The data used in this work are available upon reasonable request from the corresponding author.
Declarations
Ethics approval and consent to participate
This review used secondary data from peer-reviewed published studies and does not require ethical clearance or consent to participate.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aishat F. Akomolafe, Bushra M. Abdallah and Fathima R. Mahmood contributed equally to this work.
References
- 1.Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. American psychiatric association; 2013.
- 2.Bölte S, Girdler S, Marschik PB. The contribution of environmental exposure to the etiology of autism spectrum disorder. Cell Mol Life Sci. 2019;76:1275–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor MJ, Rosenqvist MA, Larsson H, Gillberg C, D’Onofrio BM, Lichtenstein P, et al. Etiology of autism spectrum disorders and autistic traits over time. JAMA Psychiatry. 2020;77(9):936–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henninger NA, Taylor JL. Outcomes in adults with autism spectrum disorders: A historical perspective. Autism. 2013;17(1):103–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salari N, Rasoulpoor S, Rasoulpoor S, Shohaimi S, Jafarpour S, Abdoli N, et al. The global prevalence of autism spectrum disorder: a comprehensive systematic review and meta-analysis. Ital J Pediatr. 2022;48(1):112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hodges H, Fealko C, Soares N. Autism spectrum disorder: definition, epidemiology, causes, and clinical evaluation. Transl Pediatr. 2020;9(Suppl 1):S55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu Y, Ozonoff S, Miller M. Assessment of autism spectrum disorder. Assessment. 2024;31(1):24–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Autism 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/autism-spectrum-disorders.
- 9.Lord C, Brugha TS, Charman T, Cusack J, Dumas G, Frazier T, et al. Autism spectrum disorder. Nat Reviews Disease Primers. 2020;6(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aylward BS, Gal-Szabo DE, Taraman S. Racial, ethnic, and sociodemographic disparities in diagnosis of children with autism spectrum disorder. J Dev Behav Pediatr. 2021;42(8):682–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zeidan J, Fombonne E, Scorah J, Ibrahim A, Durkin MS, Saxena S, et al. Global prevalence of autism: A systematic review update. Autism Res. 2022;15(5):778–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ebrahimi Meimand S, Amiri Z, Shobeiri P, Malekpour MR, Saeedi Moghaddam S, Ghanbari A, et al. Burden of autism spectrum disorders in North Africa and middle East from 1990 to 2019: A systematic analysis for the global burden of disease study 2019. Brain Behav. 2023;13(7):e3067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Talantseva OI, Romanova RS, Shurdova EM, Dolgorukova TA, Sologub PS, Titova OS, et al. The global prevalence of autism spectrum disorder: A three-level meta-analysis. Front Psychiatry. 2023;14:1071181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maenner MJ, Shaw KA, Baio J; EdS1; Washington A, Patrick M, DiRienzo M, Christensen DL, Wiggins LD, Pettygrove S, Andrews JG, Lopez M, Hudson A, Baroud T, Schwenk Y, White T, Rosenberg CR, Lee LC, Harrington RA, Huston M, Hewitt A; PhD-7; Esler A, Hall-Lande J, Poynter JN, Hallas-Muchow L, Constantino JN, Fitzgerald RT, Zahorodny W, Shenouda J, Daniels JL, Warren Z, Vehorn A, Salinas A, Durkin MS, Dietz PM. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016. MMWR Surveill Summ. 2020;69(4):1-12. https://doi.org/10.15585/mmwr.ss6904a1 . Erratum in: MMWR Morb Mortal Wkly Rep. 2020;69(16):503. 10.15585/mmwr.mm6916a4. PMID: 32214087; PMCID: PMC7119644. [DOI] [PMC free article] [PubMed]
- 15.Bernardo WM. PRISMA statement and PROSPERO. Int Braz J Urol. 2017;43:383–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.GA Wells BS, D O’Connell J, Peterson V, Welch M, Losos PT. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2011.
- 17.Doi SA, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials II: the quality effects model. Contemp Clin Trials. 2015;45(Pt A):123–9. [DOI] [PubMed] [Google Scholar]
- 18.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Furuya-Kanamori L, Barendregt JJ, Doi SAR. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int J Evid Based Healthc. 2018;16(4):195–203. [DOI] [PubMed] [Google Scholar]
- 20.Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ (Clinical Res ed). 2021;372:n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Farsi YM, Al-Sharbati MM, Al-Farsi OA, Al-Shafaee MS, Brooks DR, Waly MI. Brief report: prevalence of autistic spectrum disorders in the Sultanate of Oman. J Autism Dev Disord. 2011;41(6):821–5. [DOI] [PubMed] [Google Scholar]
- 22.Eapen V, Mabrouk AA, Zoubeidi T, Yunis F. Prevalence of pervasive developmental disorders in preschool children in the UAE. J Trop Pediatr. 2007;53(3):202–5. [DOI] [PubMed] [Google Scholar]
- 23.Sasanfar R, Haddad SA, Tolouei A, Ghadami M, Yu D, Santangelo SL. Paternal age increases the risk for autism in an Iranian population sample. Mol Autism. 2010;1(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Mamri W, Idris AB, Dakak S, Al-Shekaili M, Al-Harthi Z, Alnaamani AM, et al. Revisiting the prevalence of autism spectrum disorder among Omani children: A multicentre study. Sultan Qaboos Univ Med J. 2019;19(4):e305–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alshaban F, Aldosari M, Al-Shammari H, El-Hag S, Ghazal I, Tolefat M, et al. Prevalence and correlates of autism spectrum disorder in qatar: a National study. J Child Psychol Psychiatry. 2019;60(12):1254–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaaya M, Saab D, Maalouf FT, Boustany RM. Prevalence of autism spectrum disorder in nurseries in lebanon: A cross sectional study. J Autism Dev Disord. 2016;46(2):514–22. [DOI] [PubMed] [Google Scholar]
- 27.Faraji Goodarzi M, Taee N, Abbasi Hormozi PJECD, Care. Evaluation of autistic spectrum disorders screening in children of Khorramabad (West of Iran) between 2015 and 2016. 2019;189:1509–14.
- 28.Manzouri L, Yousefian S, Keshtkari A, Hashemi N. Advanced parental age and risk of positive autism spectrum disorders screening. Int J Prev Med. 2019;10:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mohammadi MR, Ahmadi N, Khaleghi A, Zarafshan H, Mostafavi SA, Kamali K, et al. Prevalence of autism and its comorbidities and the relationship with maternal psychopathology: A National Population-Based study. Arch Iran Med. 2019;22(10):546–53. [PubMed] [Google Scholar]
- 30.Sabbagh HJ, Al-Jabri BA, Alsulami MA, Hashem LA, Aljubour AA, Alamoudi RA. Prevalence and characteristics of autistic children attending autism centres in 2 major cities in Saudi arabia: A cross-sectional study. Saudi Med J. 2021;42(4):419–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Samadi SA, Mahmoodizadeh A, McConkey R. A National study of the prevalence of autism among five-year-old children in Iran. Autism. 2012;16(1):5–14. [DOI] [PubMed] [Google Scholar]
- 32.Samadi SA, McConkey R. Screening for autism in Iranian preschoolers: contrasting M-CHAT and a scale developed in Iran. J Autism Dev Disord. 2015;45(9):2908–16. [DOI] [PubMed] [Google Scholar]
- 33.Yousef AM, Roshdy EH, Abdel Fattah NR, Said RM, Atia MM, Hafez EM, et al. Prevalence and risk factors of autism spectrum disorders in preschool children in sharkia, egypt: a community-based study. Middle East Curr Psychiatry. 2021;28(1):36. [Google Scholar]
- 34.Zeglam AM, Maound AJ. Prevalence of autistic spectrum disorders in tripoli, libya: the need for more research and planned services. East Mediterr Health J. 2012;18(2):184–8. [DOI] [PubMed] [Google Scholar]
- 35.Al-Ansari AM, Ahmed MM. Epidemiology of autistic disorder in bahrain: prevalence and obstetric and Familial characteristics. East Mediterr Health J. 2013;19(9):769–74. [PubMed] [Google Scholar]
- 36.AlBatti TH, Alsaghan LB, Alsharif MF, Alharbi JS, BinOmair AI, Alghurair HA, et al. Prevalence of autism spectrum disorder among Saudi children between 2 and 4 years old in Riyadh. Asian J Psychiatr. 2022;71:103054. [DOI] [PubMed] [Google Scholar]
- 37.Sameea AA, Abd El-Wahab EW, Osman SO. Risk of autism spectrum disorder (ASD) among 18 to 48 month old children: A Multi-Center study in Qatar. Glob Pediatr Health. 2024;11:2333794x241284476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Majeed B. Screening for autism spectrum disorder among toddlers age children visiting dr. Jamal Ahamed Rashid pediatric teaching hospital in Sulaymaniyah City / Iraq. J Neonatal Surg. 2025;14:1184–95. [Google Scholar]
- 39.Almohri M, Alawainati M, Ayoob Z, Nasser N, Abdulaal N, Aldailami A, et al. Characteristics and outcomes of the screening program of autism spectrum disorder in primary healthcare centers in Bahrain. J Family Community Med. 2025;32:44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salhia HO, Al-Nasser LA, Taher LS, Al-Khathaami AM, El-Metwally AA. Systemic review of the epidemiology of autism in Arab Gulf countries. Neurosciences (Riyadh). 2014;19(4):291–6. [PMC free article] [PubMed] [Google Scholar]
- 41.Samms-Vaughan ME. The status of early identification and early intervention in autism spectrum disorders in lower- and middle-income countries. Int J Speech Lang Pathol. 2014;16(1):30–5. [DOI] [PubMed] [Google Scholar]
- 42.Rylaarsdam L, Guemez-Gamboa A. Genetic causes and modifiers of autism spectrum disorder. Front Cell Neurosci. 2019;13:385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang C, Geng H, Liu W, Zhang G. Prenatal, perinatal, and postnatal factors associated with autism: A meta-analysis. Med (Baltim). 2017;96(18):e6696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mamidala MP, Kalikiri MK, Praveen Kumar PT, Rajesh N, Vallamkonda OR, Rajesh V. Consanguinity in India and its association with autism spectrum disorder. Autism Res. 2015;8(2):224–8. [DOI] [PubMed] [Google Scholar]
- 45.Brynge M, Sjoqvist H, Gardner RM, Lee BK, Dalman C, Karlsson H. Maternal infection during pregnancy and likelihood of autism and intellectual disability in children in sweden: a negative control and sibling comparison cohort study. Lancet Psychiatry. 2022;9(10):782–91. [DOI] [PubMed] [Google Scholar]
- 46.Chiarotti F, Venerosi A. Epidemiology of autism spectrum disorders: a review of worldwide prevalence estimates since 2014. Brain Sci. 2020;10(5):274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fombonne E. The prevalence of autism. JAMA. 2003;289(1):87–9. [DOI] [PubMed] [Google Scholar]
- 48.Matson JL, Kozlowski AM. The increasing prevalence of autism spectrum disorders. Res Autism Spectr Disorders. 2011;5(1):418–25. [Google Scholar]
- 49.Sharma SR, Gonda X, Tarazi FI. Autism spectrum disorder: classification, diagnosis and therapy. Pharmacol Ther. 2018;190:91–104. [DOI] [PubMed] [Google Scholar]
- 50.Doi SA, Thalib L. A quality-effects model for meta-analysis. Epidemiology. 2008;19(1):94–100. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this work are available upon reasonable request from the corresponding author.