Abstract
This study explores the impact of Artificial Intelligence (AI) curricula on medical students’ perceptions of AI, a critical topic given AI’s transformative potential in healthcare and its rapid integration into medical practice and education. Using data from a global cross-sectional survey involving 4,596 students across 48 countries, we employed Coarsened Exact Matching (CEM) to address selection bias and Structural Equation Modeling (SEM) to examine mediating effects. Regression models were also applied to estimate the relationships between AI curricular and students’ knowledge about and attitudes towards AI. Results reveal that participation in AI curricula significantly enhances students’ knowledge about AI (β = .140, p < .001), equipping them with essential skills for AI-driven healthcare systems. However, it concurrently diminishes their enthusiasm for integrating AI into medical education (β = -.108, p < .001), reflecting potential concerns about ethical and professional implications. No significant effects were observed on students’ attitudes towards Artificial Intelligence application in medicine, the physician’s role, or AI-related ethical and legal conflicts. Heterogeneity analysis shows stronger positive effects on knowledge for veterinary students and those from developing countries, where AI education addresses critical resource gaps. Conversely, the negative effect on enthusiasm for AI teaching is more pronounced among students from developed countries, where advanced AI applications are more prevalent. SEM results reveal that preparedness for work with AI partially mediates the relationship between AI curricula and students' knowledge (β = .062, p < .001) and attitudes (β = .023, p < .001), adding theoretical depth to the findings. These results underscore the importance of balanced AI education to enhance knowledge while addressing concerns about its integration in education. This research has significant practical and theoretical implications, emphasizing the need for tailored AI curricula that align with students’ professional goals and regional educational contexts. The study offers pathways for optimizing AI literacy globally, bridging resource disparities, and preparing future healthcare professionals for AI-driven advancements.
Keywords: Artificial intelligence, Medical students, AI curricular, Coarsened exact matching, Structural equation modeling
Artificial Intelligence (AI) is revolutionizing healthcare by improving diagnostic accuracy, personalizing treatments, and enhancing operational efficiency [1, 8, 128]. Techniques such as deep learning and natural language processing enable AI to analyze complex medical data, facilitating early disease detection and tailored patient care [18, 64, 79, 98, 110]. For instance, AI algorithms outperform traditional methods in identifying diseases from imaging data, synthesizing patient histories, and optimizing care [46, 52, 55, 65]. Studies highlight the critical role of AI curricula in shaping medical students’ competencies and attitudes toward Artificial Intelligence integration in healthcare. For example, in Malaysia, 87% of students recognized AI’s importance, yet only 44.5% felt adequately prepared to work with AI, reflecting gaps in curricular design [121]. Similarly, in Oman, 78.7% of students supported AI education but expressed concerns about its application in decision-making [7]. These findings underscore the need to explore how AI education influences students’ preparedness and perceptions.
Misconceptions about AI in healthcare, especially among medical students, can significantly affect future clinical practice, ethical decision-making, and patient safety. While AI shows promise in improving diagnostics and reducing errors, misunderstandings about its limits may impede its adoption [70]. Ethical concerns include AI’s potential to replicate biases, lack transparency, and cannot replace nuanced human judgment [15].
In this context, focusing on medical students is essential as they are future healthcare professionals who will use and decide on AI in clinical practice. Early AI education improves their literacy and ethical awareness, preparing them to safely integrate AI tools [78]. This aligns with broader educational reforms promoting digital competencies and lifelong learning to ensure patient safety amid technological advances [29, 118].
The need for adapting medical education to AI
The rapid advancement of AI in healthcare necessitates parallel evolution in medical education. Curricula must prepare students to utilize AI technologies effectively, interpret complex datasets, and collaborate with AI systems in clinical settings [28, 80, 116, 130]. Integrating AI into medical education equips students with tools like machine learning and neural networks to enhance patient care [94, 120]. Early exposure helps demystify AI applications and ensures proficiency in understanding both its benefits and limitations [66, 105].
Adjustments to curricula are necessary to foster AI-driven competencies, including diagnostics and virtual healthcare delivery. Competency-based AI courses have successfully equipped students with skills to interpret AI-assisted diagnostics and incorporate insights into evidence-based decisions, aligning education with the digital transformation of healthcare [22, 92, 105]. Studies underscore the importance of embedding AI literacy within both foundational and clinical training [73, 92, 124].
The current status and challenges of ai integration in medical education
Despite the acknowledged potential of AI to revolutionize healthcare, significant obstacles impede its integration with medical education. These include a lack of faculty expertise in AI, the absence of standardized guidelines for implementation, and limited resources [41, 57, 101]. Furthermore, current medical curricula generally fall short in addressing essential AI competencies like data analysis, ethical implications, and practical clinical applications [117]. Addressing these gaps is crucial for the advancement of AI in medical education.
Students encounter significant hurdles in acquiring AI knowledge, largely due to inadequate resources, time constraints, and insufficient practical exposure [40, 131]. These limitations result in students being inadequately prepared for AI-integrated healthcare systems [3, 61]. Despite their keen interest in learning about AI and their recognition of its vital role in future medical practice, the current educational environment falls short in providing the necessary support [23, 127]. This gap between interest and preparation underscores the need for more robust AI education to ensure students are well-equipped to navigate and contribute to the evolving healthcare landscape.
Curricular interventions to enhance AI Literacy and adoption
AI literacy programs are vital for equipping future clinicians with both technical skills and ethical judgment in AI‐driven healthcare [33, 88, 113]. Targeted curricular events—ranging from machine‐learning workshops to ethics seminars—bridge critical knowledge gaps [97], boost learner confidence [24], and employ simulation‐based learning to improve readiness despite faculty expertise and standardization challenges [61]. Real‐world applications in radiology and pathology further sharpen students’ critical thinking and meaningful engagement with AI tools, ultimately enhancing diagnostic accuracy and treatment outcomes [32, 47, 56, 63].
Structured AI curricula also shape attitudes toward future AI use: hands‐on electives foster enthusiasm and readiness [2, 43, 74], yet persistent misconceptions—such as fears of clinician obsolescence—can provoke resistance and deter specialties like radiology [19, 36, 39]. A balanced approach that integrates technical training with ethical discussion is therefore essential to address these concerns, cultivate responsibility, and ensure sustainable AI adoption in clinical practice [5, 16, 26, 53, 93].
Unresolved issues
Although AI’s clinical potential in healthcare is well documented, the role of AI education in preparing medical students remains underexplored. Prior studies note AI’s impact on healthcare and its educational implications but do not specify how curricula develop students’ competencies and attitudes. This study fills that gap by examining how AI education is integrated into medical programs and its effects on students’ readiness for modern practice. By analyzing pedagogical strategies that enhance AI understanding and acceptance, our findings will guide educators and policymakers in designing AI curricula tailored to contemporary healthcare needs.
Literature
AI education and literacy: curricular overview, foundations, and impact
The integration of AI into medical education is advancing globally, particularly in developed nations where institutions such as Emory University, the University of Toronto, and European initiatives like ESMPE offer structured courses and innovative experiences that build both technical skills and ethical understanding [2, 51, 74, 86, 89, 129]. In contrast, developing countries such as India face resource constraints and variable educational capacity: a survey there found significant AI knowledge gaps among students, who favor workshops and lectures to enhance learning [109]. Concerns about overreliance on AI and its impact on clinical empathy further underscore the need for balanced, ethics-focused curricula [77, 90, 95].
A robust theoretical foundation is essential: understanding core concepts such as machine learning, neural networks, and data science is crucial for interpreting AI’s role in data analysis and clinical insights [96, 104, 107]. Leading programs integrate ethical and legal training to address algorithmic bias and privacy issues, ensuring responsible AI use [71, 74, 125]. Practical application through AI tools in medical workflows and simulation-based learning translates theory into skills—enhancing diagnostic accuracy and patient safety [45, 69, 88, 103]). Such initiatives not only build competence but also instill confidence and adaptability, equipping future healthcare professionals to harness AI effectively for improved patient outcomes [112].
Students’ attitudes toward ai: confidence, concerns, and future adoption
Medical students generally demonstrate positive attitudes and growing confidence in the use of AI in healthcare. For instance, studies revealed that 87% in Saudi Arabia and 89% in the UK seeing significant benefits, including improved diagnostic accuracy [9, 114]. However, ethical concerns persist. For example, 58.3% of German students fear increased workplace monitoring. Additionally, 68.4% of Jordanian students emphasize the need for cautious AI introduction to mitigate biases and liability [82, 102]. These findings stress the importance of educational curricula addressing AI’s limitations and ethical challenges.
A vast majority of medical students globally are eager to use AI in their future practices, with 99% in a multinational survey and 96% in a U.S. study expressing enthusiasm for AI’s potential to improve clinical efficiency and diagnostic confidence [17, 100]. Despite this, a significant minority harbor concerns over AI’s ethical implications, bias, and potential to dehumanize care [4, 39, 50]. Furthermore, studies found that some students lack trust in AI’s accuracy for critical decisions, preferring traditional methods [10, 76, 114, 119].
Differences in AI applications across specializations and development levels
AI is revolutionizing healthcare, yet its applications differ significantly across medicine, dentistry, and veterinary medicine due to variations in focus, data availability, and technological requirements. In medical practice, AI excels in diagnostics, using advanced imaging analysis for conditions like cancer, and in radiology, it aids in personalized treatment plans [122]. Dental AI specializes in interpreting X-rays to detect cavities and gum diseases, and it’s crucial for orthodontic and prosthetic treatments [13, 38, 83, 111]. Veterinary AI stands out with wearable technology for real-time health monitoring in animals. It enables early detection of health issues and assists in radiographic assessments. These advances improve healthcare outcomes for both humans and animals [6, 11, 108].
AI adoption in medical education reveals stark differences between developed and developing countries, influenced by resource availability and infrastructure. In developed nations like the U.S. and Germany, AI is integral to curricula, promoting personalized learning with tools and simulations. Conversely, in developing countries, infrastructure limitations and resource constraints impede AI integration. For instance, An Indian study found only 19.4% of medical students had practical AI exposure despite recognizing its importance [54]. Similarly, rural areas in these nations use AI to improve healthcare access and training, yet face challenges due to inadequate guidelines and support [42, 62, 87].
Research gaps
Although AI is gaining traction in medical education globally, the implementation of AI curricula remains inconsistent and fragmented across regions, institutions, and specialties. High-income countries have begun integrating AI-focused content into their medical curricula, but disparities persist in program quality, pedagogical design, and ethical depth. While early initiatives have demonstrated promise in fostering technical proficiency and ethical awareness, there is limited consensus on best practices for curricular design and delivery, particularly in resource-limited settings.
Furthermore, current literature lacks a unified framework to evaluate how AI education translates into measurable learning outcomes and professional readiness. Much of the existing evidence is descriptive or self-repor ted, with few studies employing longitudinal or comparative approaches. Additionally, AI instruction is often isolated from core clinical training, resulting in limited contextualization and practical application. These inconsistencies hinder students’ ability to meaningfully engage with AI tools in real-world healthcare settings. There is a clear need for a more cohesive, evidence-based understanding of how AI education can be effectively designed, implemented, and adapted. This understanding should consider diverse educational and regional contexts. Its goal is to prepare future healthcare professionals for the evolving demands of AI-enabled medicine.
Research questions
AI is rapidly transforming healthcare by enhancing diagnostic precision, personalizing treatment plans, and improving overall clinical efficiency. Leveraging advanced technologies like machine learning and natural language processing, AI has demonstrated the potential to outperform traditional methods in disease detection and clinical decision-making [79, 110]. These advancements underscore the necessity of equipping future physicians with the knowledge and skills to integrate AI into clinical workflows. However, as AI becomes increasingly prevalent in healthcare, understanding how medical education prepares students for this integration remains critical. Specifically, questions regarding how exposure to AI education influences students’ attitudes, subgroup-specific attitudes, and the role of preparedness in shaping these perceptions require further exploration.
Existing literature highlights the potential and challenges of integrating AI literacy into medical education. AI curricular events have been shown to enhance students’ knowledge and confidence in using AI tools while addressing ethical concerns and practical applications. Studies have demonstrated the positive impact of structured AI education on student readiness, with programs in North American countries leading advancements in this area [2, 74]. However, challenges such as limited resources, faculty expertise, and inconsistent curricula remain significant barriers to widespread AI education [41, 71]. Furthermore, subgroup differences, such as variations in attitudes based on field of study and regional development status, highlight the need for tailored educational approaches [106]. These findings emphasize the importance of examining how AI education influences diverse student populations and their preparedness for AI integration in clinical practice.
Building on these insights, this study aims to address the following research questions:
How does participation in AI curricular events impact medical students’ attitudes on Artificial Intelligence?
How does participation in AI curricular events impact students’ attitudes towards Artificial Intelligence applications across different subgroups, such as field of study and country development status?
What roles do preparedness for working with AI play in the factors influencing medical students’ attitudes towards Artificial Intelligence?
Problem statement
RQ1 statement
The first research question focuses on whether participating in AI curricular events influences medical students’ overall perceptions of artificial intelligence. This inquiry seeks to clarify if structured exposure to AI content during medical training contributes to enhanced understanding, increased interest, or potential skepticism toward AI in clinical settings.
RQ2 statement
The second research question explores the variability in students’ attitudes across subgroups, particularly by field of study (e.g., medicine, dentistry, veterinary medicine) and by country development status (developed vs. developing). This allows for a nuanced examination of how contextual and disciplinary factors shape the effects of AI education.
RQ3 statement
The third research question investigates the role of students’ self-perceived preparedness for working with AI. Specifically, it examines whether this sense of preparedness mediates the relationship between AI curricular exposure and students’ knowledge and attitudes, thereby revealing the underlying mechanisms through which education shapes AI-related perceptions.
Methodology
Research design and strategy
Data
This study used data from a global cross-sectional survey conducted by Charité-University Medicine Berlin. The survey focused on student attitudes toward Artificial Intelligence in medical, dental, and veterinary education and practice. It aimed to explore the perspectives of students in these fields. Participation was open from April 1st to October 1st, 2023. To be eligible, participants had to be at least 18 years old, actively pursuing a degree in medicine, dentistry, or veterinary medicine, and respond within the survey period. They also needed proficiency in English or Spanish. In total, 4,900 responses were collected, with a final cohort of 4,596 participants from 192 faculties across 48 countries [20]. Participants had to be at least 18 years old, actively enrolled in a medical, dental, or veterinary degree program, proficient in either English or Spanish (depending on their faculty location), and confirmed their enrollment status before proceeding with the survey. The demographic details are shown in Table 1.
Table 1.
Demographic table
| Demographic characteristic | Declaration | N | Percentage | |
|---|---|---|---|---|
| Gender | Male | 1,929 | 42.48% | |
| Female | 2,565 | 56.49% | ||
| Diverse | 25 | 0.55% | ||
| Prefer not to disclose | 22 | 0.48% | ||
| Course of study | (Human) Medicine | 4,264 | 93.86% | |
| Dentistry | 201 | 4.42% | ||
| Veterinary Medicine | 78 | 1.72% | ||
| Location | Asia | 928 | 20.43% | |
| Europe | 2,326 | 51.20% | ||
| North America | 160 | 3.52% | ||
| South America | 899 | 19.79% | ||
| Australia | 104 | 2.29% | ||
| Africa | 126 | 2.77% | ||
| Level of development of the countrya | Developed country | 2,765 | 60.20% | |
| Developing country | 1,828 | 39.80% | ||
| Variables | Mean | S.D | Max | Min |
| Age | 22.70 | 3.59 | 56 | 17 |
| Total academic years | 5.82 | 0.60 | 8 | 4 |
aThe classification of whether students were in a developed country or developing country was based on Organization for Economic Co-operation and Development (OECD) membership. This study categorizes the countries into developed countries (OECD member countries) and developing countries (non-OECD member countries)
Participants were recruited via non-probability convenience sampling through official faculty channels. The survey was distributed through newsletters and academic courses at participating institutions. Depending on the faculty, either a QR code or a direct survey link was used. During the data collection period, 4,596 valid responses were received from students across 48 countries, with medical students comprising 93.8% of the sample. Based on publicly available enrollment data, the estimated average response rate was approximately 0.2%, though this figure may underestimate actual participation due to uncertainties in survey reach. The survey assessed technological literacy, AI knowledge, and attitudes towards AI education. Considerable variation was observed in AI curricular duration and content across institutions, with most students reporting limited or no standardized AI education within their programs, highlighting that AI education remains in its early stages and requires further development and standardization globally. Eligibility was confirmed by asking respondents about their current degree program and age. Only fully or partially completed surveys from eligible students were included in the analysis.
Variables
Dependent variables
To better describe medical students’ perceptions of AI, this study selects several dependent variables. These include knowledge about AI and attitudes towards the application of AI in medicine. It also considers the influence of AI on the profession of physicians and attitudes towards including AI teaching in medical education. Additionally, the study examines the relationship between the use of AI in medicine and the increase in legal and ethical conflicts. The specific items are presented in Table 2.
Table 2.
Survey items
| Dependent Variable | Question/Item | Options |
|---|---|---|
| Knowledge about AI | How would you rate your general knowledge of artificial intelligence (AI)? |
1 = No knowledge 2 = Little knowledge 3 = Good knowledge 4 = Expert |
| Attitude towards the application of AI in medicine | What is your general attitude toward the application of artificial intelligence (AI) in medicine? |
1 = Extremely negative 2 = Rather negative 3 = Neutral 4 = Rather positive 5 = Extremely positive |
| Influence of AI on the profession of physicians | What is your view on the influence of artificial intelligence (AI) on the profession of physicians? |
1 = Extremely negative 2 = Rather negative 3 = Neutral 4 = Rather positive 5 = Extremely positive |
| Attitude towards the inclusion of AI teaching in medicine | I would like to have more teaching on artificial intelligence (AI) in medicine as part of my studies |
1 = Completely disagree 2 = Rather disagree 3 = Neutral 4 = Rather agree 5 = Completely agree |
| Relationship between the use of AI in medicine and the increase in legal and ethical conflicts | The use of artificial intelligence (AI) in medicine will increasingly lead to legal and ethical conflicts |
1 = Completely disagree 2 = Rather disagree 3 = Neutral 4 = Rather agree 5 = Completely agree |
| Independent Variable | Question/Item | Options |
| AI curricular | As part of my studies, there are curricular events on artificial intelligence (AI) in medicine |
1 = Yes 0 = No |
| Control Variables | Question/Item | Options |
| Gender |
1 = Male 0 = Female |
|
| Age | Years | |
| Total academic years | Years | |
| Experience of programming code | Have you already programmed code? |
1 = Yes 0 = No |
| Experience of technical devices usage | Which of these technical devices do you use at least once a week? |
Smartphone PC/Laptop Game console Tablet E-reader Smartwatch |
| Mediating Variable | Question/Item | Options |
| Preparedness for work with AI | With my current knowledge, I feel sufficiently prepared to work with artificial intelligence (A1) in my future profession as a physician |
1 = Completely disagree 2 = Rather disagree 3 = Neutral 4 = Rather agree 5 = Completely agree |
Independent variable
This study employs whether participants have taken AI curricular as the independent variable, which is measured in the dataset by the item “As part of my studies, there are curricular events on artificial intelligence (AI) in medicine.” The specific items are presented in Table 2.
Control variables
Studies have confirmed that gender, age, and prior experience with technology usage are correlated with students’ attitudes towards technology [21, 27, 115]. Thus, this study employs the following control variables: gender, age, total academic years, experience with programming code, and experience with technology usage. Since few respondents chose “diverse” or “prefer not to disclose” for gender, these responses are treated as missing values. The specific items are presented in Table 2.
Mediating variable: preparedness for working with AI
This study employs medical students’ preparedness for working with AI as mediating variable. In the dataset, medical students’ preparedness for work with AI was measured by the item “With my current knowledge, I feel sufficiently prepared to work with artificial intelligence (AI) in my future profession as a physician.” The specific items are presented in Table 2.
Analytical techniques
Regression modeling for baseline estimation
To explore the effect of AI curricular on medical students’ views on AI, this study constructs five regression models using STATA 18:
| 1 |
| 2 |
| 3 |
| 4 |
| 5 |
AIknowledge represents medical students’ knowledge about AI, AIapplication represents medical students’ attitudes towards the application of AI in medicine, AIprofession represents medical students’ attitudes on the influence of AI on the profession of physicians, AIteaching represents medical students’ attitude towards the inclusion of AI teaching in medicine, AIconflicts represents medical students’ attitude towards relationship between the use of AI in medicine and the increase in legal and ethical conflicts, AIcurricular represents whether there are curricular events on AI in medicine of medical students, Gender represents medical students’ gender, Age represents medical students’ age, TAY represents medical students’ total academic years, EPG represents medical students’ experience of programming code, ETU represents medical students’ experience of technical devices usage. β0, β7, β14, β21, β28 are the intercepts, β1-β6, β8-β13, β15-β20, β22-β27, β29-β34 are the regression coefficients, and ε, μ, ζ, δ, λ are the error terms.
Coarsened Exact Matching (CEM) for robustness checks
To addresses the endogeneity of the effect of AI curricular on medical students’ views on AI, this study employs Coarsened Exact Matching (CEM) to conduct a robustness test. CEM is a non-parametric method that stratifies the sample into treatment and control groups based on grouping variables. This approach allows researchers to preselect the balance between the treatment and control groups before matching. As a result, it eliminates the need for extensive post-hoc tests and repeated re-evaluation processes to achieve the target. CEM’s non-parametric approach and ability to handle large datasets with multiple variables make it ideal for our research, providing a robust comparison without relying on linear assumptions [48].
Structural Equation Modeling (SEM) for mediation analysis
In the final step, this study established a Structural Equation Modeling (SEM) (see Fig. 1) to explore the mechanisms by which mental health support affects postdoctoral researchers’ leaving intention to leave scientific filed using STATA 18.
Fig. 1.

SEM pathway linking AI curricular to medical students’ attitudes on artificial intelligence
Results
Regression results addressing key research question
The results of the regression model (see Table 3) reveal that AI curricular exerts a significant positive effect on medical students’ knowledge about AI (β = 0.140, p < 0.001), and has a significant negative on medical students’ attitude towards the inclusion of AI teaching in medicine (β = −0.108, p < 0.001). However, AI curricular exhibits no significant effect on medical students’ attitudes towards the application of AI in medicine, medical students’ view on the influence of AI on the profession of physicians, and medical students’ attitude towards relationship between the use of AI in medicine and the increase in legal and ethical conflicts (p > 0.05). The data show a significant decrease in students’ enthusiasm for including AI teaching, despite increased knowledge. This effect is specific to curricular inclusion attitudes, with no significant changes in other AI-related perceptions. These results reveal a nuanced response to AI curricular exposure.
Table 3.
Results of regression model
| Independent Variable | AIknowledge | AIapplication | AIprofession | AIteaching | AIconflicts | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | S.E | t | β | S.E | t | β | S.E | t | β | S.E | t | β | S.E | t | |
| AIcurricular | .140*** | .018*** | 7.68 | -.002 | .031 | −0.07 | .014 | .029 | 0.51 | -.108*** | .033 | −3.25 | .048 | .036 | 1.35 |
| Gender | -.162*** | .015 | −10.83 | -.186*** | .026 | −7.23 | -.140*** | .023 | −5.97 | -.131*** | .027 | −4.80 | .082** | .029 | 2.81 |
| Age | .006** | .002 | 2.77 | .001 | .004 | 0.22 | .003 | .003 | 0.76 | .001 | .004 | 0.35 | .021*** | .004 | 4.97 |
| Total academic years | -.019 | .013 | −1.54 | .108*** | .022 | 5.00 | .114*** | .020 | 5.79 | .049* | .023 | 2.16 | .048** | .015 | 3.13 |
| Experience of programming code | .229*** | .019 | 11.76 | .157*** | .034 | 4.68 | .104*** | .030 | 3.41 | .116*** | .035 | 3.29 | .208*** | .038 | 5.49 |
| Experience of technical devices usage | .055*** | .008 | 7.05 | .070*** | .014 | 5.13 | .080*** | .012 | 6.50 | .077*** | .014 | 5.36 | -.049* | .024 | −1.99 |
| Constant | 2.230*** | .097 | 23.09 | 3.190*** | .166 | 19.17 | 2.981*** | .151 | 19.73 | 3.691*** | .176 | 20.94 | 3.366*** | .188 | 17.90 |
| N | 4,270 | 4,263 | 4,264 | 4,256 | 4,264 | ||||||||||
| R2 | .1026 | .0329 | .0315 | .0203 | .0203 | ||||||||||
* p < .05
** p < .01
*** p < .001
Importantly, the standardized coefficients indicate a moderate effect size for both knowledge improvement and attitude change: knowledge scores increased by approximately 14% of a standard deviation post-intervention, while enthusiasm for AI curricular inclusion decreased by about 10%. These magnitudes highlight that while AI education effectively enhances understanding, it simultaneously challenges student attitudes towards curricular expansion, underscoring the complexity of educational impact.
Robustness checks supporting model validity
The results of CEM (see Table 4) demonstrate a notable reduction in the L1 value for medical students, declining from 0.334 before matching to 0.247 after matching. An in-depth examination of the matching outcomes for each control variable (see Table 5) further elucidates that the disparities in the quantiles of the control variables were effectively alleviated. Consequently, this improvement in the distribution of control variables resulted in a markedly better balance between the treatment and control groups, enhancing the validity of the subsequent comparisons. This significant reduction in imbalance indicates that the CEM successfully controlled for confounding variables, thereby reducing selection bias and increasing confidence that observed effects of AI curricular exposure on knowledge and attitudes are not driven by pre-existing differences between groups. Such methodological rigor strengthens the practical credibility of the findings and supports their application in guiding medical education policy.
Table 4.
Results of CEM
| Taking AI curricular | Not taking AI curricular | |
|---|---|---|
| Number of successfully matched samples | 964 | 3,108 |
| Number of unsuccessfully matched samples | 82 | 389 |
| L1 before matching | .334 | |
| L1 after matching | .247 | |
Table 5.
Matching status for control variables
| Variable | L1 | mean | min | 25% | 50% | 75% | max | |
|---|---|---|---|---|---|---|---|---|
| Before matching | Gender | .016 | -.023 | 0 | 0 | 0 | 0 | 0 |
| Age | .078 | .200 | 1 | 1 | 0 | 0 | −9 | |
| Total academic years | .049 | -.076 | 0 | 0 | 0 | 0 | 0 | |
| Experience of programming code | .073 | .073 | 0 | 0 | 0 | 1 | 0 | |
| Experience of technical devices usage | .057 | .016 | 0 | 0 | 0 | 0 | 0 | |
| After matching | Gender | 3.6E-15 | 1.6E-14 | 0 | 0 | 0 | 0 | 0 |
| Age | .039 | -.028 | 1 | 0 | 0 | 0 | 0 | |
| Total academic years | 1.9E-15 | 4.0E-14 | 0 | 0 | 0 | 0 | 0 | |
| Experience of programming code | 1.8E-15 | 3.1E-15 | 0 | 0 | 0 | 0 | 0 | |
| Experience of technical devices usage | 3.5E-15 | 3.8E-14 | 0 | 0 | 0 | 0 | 0 |
Then, this study incorporates the CEM weights into the regression model. The results (see Table 6) show that after controlling the selection bias, the effect of AI curricular on medical students’ knowledge about AI remains significant positive (β = 0.137, p < 0.001), while the effect of AI curricular on medical students’ attitude towards the inclusion of AI teaching in medicine remains significant negative (β = −0.105, p = 0.003). The results of the robustness test based on CEM closely align with those obtained from the original regression model, providing strong evidence that the findings of this study are reliable and not driven by selection bias or confounding factors.
Table 6.
Results of regression model with CEM weights
| Independent Variable | AIknowledge | AIteaching | ||||||
|---|---|---|---|---|---|---|---|---|
| β | S.E | t | p | β | S.E | t | p | |
| AIcurricular | .137 | .019 | 7.17 | < .001 | -.105 | .035 | −3.00 | .003 |
| Gender | -.162 | .017 | −9.84 | < .001 | -.135 | .030 | −4.48 | < .001 |
| Age | .005 | .003 | 1.73 | .084 | .009 | .005 | 1.89 | .059 |
| Total academic years | -.009 | .013 | −0.73 | .466 | .038 | .024 | 1.60 | .110 |
| Experience of programming code | .255 | .019 | 13.14 | < .001 | .142 | .035 | 4.03 | < .001 |
| Experience of technical devices usage | .049 | .009 | 5.81 | < .001 | .091 | .016 | 5.86 | < .001 |
| Constant | 2.218 | .106 | 20.93 | < .001 | 3.547 | .193 | 18.34 | < .001 |
| N | 3,784 | 3,772 | ||||||
| R2 | .1025 | .0262 | ||||||
Subgroup analysis highlighting contextual differences
This study carried out a heterogeneity analysis to examine the effect of AI curricular on medical students’ knowledge of AI and their attitude towards the inclusion of AI teaching in medicine. The significance of these effects was validated by regression model. The heterogeneity analysis was conducted by segmenting medical students into various subgroups according to their case of study and level of development of the country. The results of heterogeneity analysis (see Table 7) suggest that the positive effect of AI curricular on veterinary medicine students’ knowledge about AI (β = 0.480, p = 0.002) is significantly stronger than that for dentistry students (β = 0.338, p < 0.001) and (human) medicine students (β = 0.123, p < 0.001). Additionally, the positive effect of AI curricular on medical students from developing country (β = 0.154, p < 0.001) is significantly stronger than that for medical students from developed country (β = 0.123, p < 0.001). These differences indicate that the impact of AI curricular varies by discipline and regional development, likely reflecting differing baseline exposure and educational needs.
Table 7.
Results of heterogeneity analysis
| Subgroup | Independent Variable | AIknowledge | AIteaching | ||||||
|---|---|---|---|---|---|---|---|---|---|
| β | S.E | t | p | β | S.E | t | p | ||
| (Human) Medicine | AIcurricular | .123 | .019 | 6.56 | < .001 | -.100 | .034 | −2.93 | .003 |
| Gender | -.154 | .015 | −10.00 | < .001 | -.135 | .028 | −4.87 | < .001 | |
| Age | .007 | .002 | 3.06 | .002 | -.003 | .004 | −0.73 | .465 | |
| Total academic years | -.018 | .013 | −1.35 | .176 | .018 | .024 | 0.77 | .441 | |
| Experience of programming code | .235 | .020 | 11.85 | < .001 | .127 | .036 | 3.52 | < .001 | |
| Experience of technical devices usage | .053 | .008 | 6.53 | < .001 | .068 | .015 | 4.58 | < .001 | |
| Constant | 2.197 | .101 | 21.66 | < .001 | 4.016 | .184 | 21.84 | < .001 | |
| N | 4,021 | 4,008 | |||||||
| R2 | .1006 | .0187 | |||||||
| Dentistry | AIcurricular | .338 | .091 | 3.73 | < .001 | -.143 | .171 | −0.84 | .405 |
| Gender | -.255 | .083 | −3.07 | .003 | -.183 | .157 | −1.17 | .244 | |
| Age | -.001 | .011 | −0.06 | .953 | .041 | .020 | 2.05 | .042 | |
| Total academic years | .004 | .071 | 0.06 | .952 | .365 | .133 | 2.75 | .007 | |
| Experience of programming code | .120 | .125 | 0.97 | .335 | -.435 | .234 | −1.86 | .065 | |
| Experience of technical devices usage | .086 | .039 | 2.23 | .027 | .109 | .072 | 1.50 | .135 | |
| Constant | 2.244 | .422 | 5.32 | < .001 | .916 | .793 | 1.15 | .250 | |
| N | 173 | 172 | |||||||
| R2 | .1605 | .1265 | |||||||
| Veterinary Medicine | AIcurricular | .480 | .148 | 3.23 | .002 | .041 | .315 | 0.13 | .896 |
| Gender | -.275 | .121 | −2.27 | .026 | .139 | .257 | 0.54 | .592 | |
| Age | .006 | .011 | 0.55 | .582 | .048 | .024 | 2.00 | .049 | |
| Total academic years | -.377 | .114 | −3.32 | < .001 | -.334 | .241 | −1.38 | .171 | |
| Experience of programming code | .161 | .130 | 1.24 | .219 | .477 | .275 | 1.73 | .087 | |
| Experience of technical devices usage | .043 | .054 | 0.79 | .431 | .070 | .114 | 0.61 | .541 | |
| Constant | 4.423 | .776 | 5.70 | < .001 | 4.140 | 1.649 | 2.51 | .014 | |
| N | 76 | 76 | |||||||
| R2 | .3242 | .1187 | |||||||
| Developing Country | AIcurricular | .154 | .031 | 4.97 | < .001 | -.063 | .054 | −1.17 | .243 |
| Gender | -.155 | .027 | −5.83 | < .001 | -.107 | .046 | −2.34 | .019 | |
| Age | .003 | .004 | 0.70 | .483 | .007 | .007 | 0.98 | .328 | |
| Total academic years | -.007 | .022 | −0.30 | .763 | .060 | .038 | 1.57 | .116 | |
| Experience of programming code | .157 | .038 | 4.16 | < .001 | .080 | .065 | 1.22 | .223 | |
| Experience of technical devices usage | .068 | .013 | 5.28 | < .001 | .092 | .022 | 4.11 | < .001 | |
| Constant | 2.225 | .163 | 13.67 | < .001 | 3.386 | .281 | 12.06 | < .001 | |
| N | 1,622 | 1,616 | |||||||
| R2 | .0714 | .0203 | |||||||
| Developed Country | AIcurricular | .123 | .022 | 5.48 | < .001 | -.130 | .043 | −3.05 | .002 |
| Gender | -.158 | .018 | −8.83 | < .001 | -.154 | .034 | −4.53 | < .001 | |
| Age | .009 | .003 | 3.55 | < .001 | -.003 | .005 | −0.70 | .484 | |
| Total academic years | -.027 | .015 | −1.79 | .073 | .037 | .029 | 1.28 | .201 | |
| Experience of programming code | .269 | .022 | 12.21 | < .001 | .126 | .042 | 3.00 | .003 | |
| Experience of technical devices usage | .054 | .010 | 5.34 | < .001 | .055 | .019 | 2.83 | .005 | |
| Constant | 2.176 | .120 | 18.12 | < .001 | 4.000 | .230 | 17.41 | < .001 | |
| N | 2,647 | 2,639 | |||||||
| R2 | .1353 | .0200 | |||||||
Furthermore, AI curricular exerts a significant negative effect on medical students’ attitudes towards the inclusion of AI teaching in medicine (β = −0.100, p = 0.003). However, its effect on dentistry students is not statistically significant (p > 0.05). Additionally, AI curricular has a significant negative effect on the attitude towards the inclusion of AI teaching in medicine of medical students from developed country (β = −0.130, p = 0.002), whereas its effect on medical students from developing countries is not significant (p > 0.05). This pattern suggests that concerns or reservations about expanding AI education may be more pronounced in developed countries and vary across fields. These heterogeneity results show that AI curricular exposure impacts subgroups differently. Veterinary medicine students saw large knowledge gains—about half a standard deviation—greater than dentistry and general medicine students, who improved by roughly one-third and one-eighth, respectively. Students from developing countries also experienced stronger knowledge increases (~ 15%) compared to developed countries (~ 12%). Attitudes toward AI curricular inclusion declined moderately by around 10%, mainly among medical students from developed countries. These effect sizes highlight the complex and varied educational impact of AI curricula across groups.
Structural equation modeling: testing mediating pathway
This study establishes SEM models for two dependent variables (AIknowledge and AIteaching) with significant regression results. This study assessed model fit through the Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Root Mean Squared Error of Approximation (RMSEA), and Standardized Root Mean Squared Residual (SRMR).1 The SEM model for AIknowledge yielded CFI, TLI, RMSEA, and SRMR values of 0.942, 0.827, 0.075, and 0.032, respectively, and SEM model for AIknowledge yielded CFI, TLI, RMSEA, and SRMR values of 0.923, 0.768, 0.057, and 0.024, suggesting that the SEM models adequately represents the intrinsic relationships within the data.
The results of SEM model for AIknowledge (see Fig. 2) show that AI curricular has a significant positive direct effect on medical students’ knowledge about AI (β = 0.158, p < 0.001). The indirect effect of AI curricular on medical students’ knowledge about AI is estimated to be 0.062 (0.530 * 0.117), and this coefficient is statistically significant (p < 0.001). The results of SEM model for AIteaching (see Fig. 3) show that AI curricular has a significant negative direct effect on medical students’ attitude towards the inclusion of AI teaching in medicine (β = −0.103, p < 0.001). The indirect effect of AI curricular on medical students’ attitude towards the inclusion of AI teaching in medicine is estimated to be 0.023 (0.527 * 0.044), and this coefficient is statistically significant (p < 0.001). These findings suggest that preparedness for work with AI partially mediates the relationship between AI curricular and medical students’ knowledge about AI and their attitude towards the inclusion of AI teaching in medicine. The SEM models showed good fit. AI curricular exposure significantly increased AI knowledge by about 16% of a standard deviation and decreased enthusiasm for AI teaching by around 10%. Preparedness for work with AI partially mediated these effects, indicating complex pathways influencing student outcomes.
Fig. 2.

Results of SEM for AIknowledge
Fig. 3.
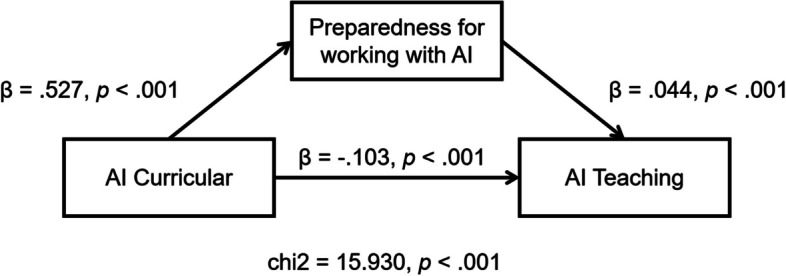
Results of SEM for AIteaching
Discussion
RQ1: impact of AI curricular events on medical students’ attitudes on artificial intelligence
The current results demonstrated that students exposed to AI education reported increased confidence in understanding AI applications and acknowledged its transformative role in improving diagnostic accuracy and patient outcomes. However, the findings also revealed that in some cases, exposure to AI education reduced enthusiasm for integrating AI into medical education. This aligns with prior literature highlighting that poorly designed or overly technical curricula can create barriers to student engagement, particularly when misconceptions about AI replacing human clinicians are not adequately addressed [19, 39]. These results suggest that while AI education fosters confidence, it must also balance technical training with discussions on AI’s limitations to prevent unintended negative perceptions.
The improved perceptions among students reflect the efficacy of structured AI education in addressing knowledge gaps and demystifying AI technologies. For instance, students expressed a clearer understanding of AI’s practical benefits, such as enhanced decision-making precision in clinical practice, which corroborates the argument in the introduction about AI’s capability to revolutionize diagnostics and treatment [28, 55]. However, consistent with the literature, students who perceived AI education as overly complex or insufficiently aligned with clinical practice goals expressed reduced interest in engaging further with AI [54, 74]. These findings underscore the importance of integrating AI curricula that not only bridge knowledge gaps but also foster positive attitudes by addressing fears and ethical concerns among medical students.
These findings can directly inform medical curriculum developers by highlighting the importance of integrating AI education not only as standalone technical modules but as interdisciplinary content embedded within clinical and ethical training. For instance, the observed decline in enthusiasm suggests that overly abstract or disconnected AI instruction may alienate students. Therefore, future curricula should emphasize practical AI applications through simulation, interdisciplinary problem-solving, and reflective discussion to sustain engagement.
These findings can directly inform medical curriculum developers by emphasizing the need for curricula that combine technical competence with clear communication about AI’s realistic capabilities and ethical implications. Curriculum development should integrate applied learning through clinical simulations and case-based scenarios that contextualize AI tools in real-world practice, thus reducing misconceptions and anxiety [34]. Furthermore, addressing common fears such as job displacement or dehumanization through reflective discussions and ethical debates can build trust and acceptance among students [58].
Potential barriers to implementation include overloaded medical curricula, limited faculty expertise in AI, and resource constraints, particularly in low-resource settings [67]. To overcome these, institutions could adopt interdisciplinary collaborations with computer science and bioethics departments, leverage online and modular AI education platforms to ease curricular integration, and prioritize faculty development programs to build educator capacity [29, 88]. Moreover, incremental curriculum changes paired with continuous feedback from students can enhance relevance and feasibility.
RQ2: differences in the impact across subgroups
Heterogeneity analysis reveals that the positive effect of AI education on knowledge is particularly strong for veterinary medicine students. Veterinary students benefit significantly from AI tools designed for monitoring animal health, wearable device integration, and real-time data analysis, which align closely with their professional needs [6, 11]. By contrast, students in general medical fields exhibited comparatively less pronounced benefits. These findings underscore the necessity of tailoring AI education to align with the distinct practical demands of each specialization, ensuring all students recognize and capitalize on its relevance to their future professional roles.
Results indicate that students in developing regions experienced greater positive effects on their knowledge and attitudes toward Artificial Intelligence. In developed countries, where AI is already integrated into curricula through advanced tools such as intelligent tutoring systems and gamified platforms, students benefit from precision training and personalized learning. However, the relative impact of these resources is smaller as students may view them as standard educational practices [23, 126]. By contrast, in developing regions, AI curricula often provide students with their first exposure to cutting-edge technologies, resulting in greater appreciation and enthusiasm [42].
The contradiction between increased knowledge and decreased enthusiasm for AI among medical students can be explained by several factors. Greater AI understanding often raises concerns about job security, especially in diagnostic fields [37, 75]. Students also become more aware of ethical risks, like data privacy and algorithmic bias, which can lead to hesitation about AI’s role in patient care [60, 84]. Additionally, when AI education lacks clinical relevance or practical training, it may feel disconnected from real-world medicine [69]. The added workload from AI modules can further dampen enthusiasm, especially in already intense medical curricula [99]. These factors suggest the need for balanced, applied, and ethical AI instruction.
RQ3: role of preparedness in shaping students’ attitudes toward artificial intelligence
Preparedness for working with AI plays a critical role in shaping medical students’ attitudes, with greater preparedness correlating with increased confidence and positive perceptions. Students who reported feeling prepared after participating in AI curricula were more optimistic about AI’s potential, aligning with prior literature emphasizing the link between education and confidence in AI adoption [33, 121].
Preparedness not only influences students’ willingness to adopt AI but also mitigates fears of AI replacing human decision-making. This resonates with earlier findings that structured educational interventions, including hands-on training, alleviate concerns about algorithmic bias and dehumanization in clinical care [7, 23]. Conversely, students with limited exposure expressed skepticism and uncertainty, reinforcing the notion that preparedness is a key mediator between education and attitudes. These results highlight the necessity of comprehensive AI curricula that prioritize experiential learning to ensure students feel equipped to integrate AI into their future practice confidently.
Addressing misconceptions through targeted curriculum design
One key to mitigating learner misconceptions about AI is to embed conceptual-change strategies directly into course modules, dedicating early lessons to debunking common myths—such as “AI systems have human-like understanding” or “AI will imminently replace professionals”—using concrete examples and interactive refutation texts can foster conceptual reconstruction rather than mere fact‐listing [16]. Additionally, problem-based case studies that contrast system capabilities (e.g., pattern recognition) with known limitations (e.g., lack of contextual reasoning) encourage students to actively reconcile their prior beliefs with empirical evidence, strengthening accurate mental models of AI.
Explaining the drop in enthusiasm: content and delivery factors
Several studies have observed a decline in student enthusiasm after initial exposure to AI topics, often linked to a mismatch between high expectations and subsequent curriculum depth [49, 68, 91, 123]. In particular, courses that emphasize ethical debates and speculative futures without sufficient hands‐on practice tend to leave learners feeling underprepared for real‐world applications, dampening engagement [31]. Conversely, curricula that balance technical skill‐building with ethical and societal context maintain higher sustained interest. Detailing the variability in curriculum content—for instance, contrasting programs that allocate 60% of contact hours to coding exercises vs. those that spend 80% on policy discussion—can help clarify how content emphasis drives both misconceptions and motivation [35].
Innovative contributions
First, unlike most descriptive investigations limited to a single discipline or country, this research draws on a cross-disciplinary, global sample of 4,596 medical, dental, and veterinary students from 48 countries, providing unprecedented breadth and representativeness. Second, on the methodological front, this study is the first in AI education for health professions to employ CEM to reduce selection bias, supplemented by SEM to test the mediating role of preparedness mindset on knowledge and attitude outcomes—thereby delivering stronger causal inferences than standard regression approaches. Third, we reveal heterogeneous effects of AI course participation across disciplines (medicine vs. dentistry vs. veterinary) and country development levels (developed vs. developing), filling a critical gap in differentiated, cross-disciplinary impact mechanisms. In sum, by integrating a global, multi-disciplinary sample with rigorous causal-inference techniques, this study offers systematic, generalizable insights for AI education design and policy in the health professions.
Conclusion
This study provides valuable insights into the impact of AI education on medical students’ attitudes towards Artificial Intelligence. Our findings reveal a complex interplay between AI curricular and students’ knowledge and attitudes towards Artificial Intelligence in medical education. While AI education significantly enhances medical students’ knowledge about AI, it concurrently diminishes their enthusiasm for integrating AI into medical education. Importantly, no significant effects were observed on students’ attitudes towards AI application in medicine, the profession of physicians, and the relationship between AI use and legal and ethical conflicts.
The use of Coarsened Exact Matching (CEM) confirms the robustness of our results. Furthermore, heterogeneity analysis suggests that the positive effect on knowledge is more pronounced for veterinary medicine students and those from developing countries. In contrast, the negative effect on attitudes towards AI teaching is more pronounced for students from developed countries. This finding underscores the need for tailored AI education programs that consider the diverse backgrounds and needs of medical students. The results of Structural Equation Modeling (SEM) indicate that preparedness for work with AI partially mediates the relationship between AI curricular and medical students’ knowledge and attitudes.
In conclusion, this study highlights the importance of balanced AI education in medical schools. While it is crucial to improve medical students’ knowledge about AI, equal attention should be given to addressing their concerns regarding the integration of AI in medical education. By adopting a nuanced approach to AI education, we can better prepare future physicians to harness the potential of AI in healthcare while maintaining a positive and ethical approach to its application.
Recommendations for stakeholders
Based on the findings of this study, we propose the following recommendations for stakeholders involved in the design and implementation of artificial intelligence (AI) education in medical training programs:
Design Balanced Curricula That Address Both Technical Knowledge and Ethical Concerns
While AI curricula significantly improve students' knowledge, they may simultaneously reduce enthusiasm for further AI instruction. Therefore, curriculum designers should ensure that AI education not only focuses on technical competencies but also addresses students’ concerns about AI's impact on clinical roles, ethical dilemmas, and human-centered care. Embedding reflective discussions, case studies, and interdisciplinary dialogues into AI courses can foster deeper engagement.
-
2.
Implement Tailored AI Education Based on Disciplinary and Regional Needs
Given the heterogeneous effects observed across disciplines and development levels, AI education should be customized. For example, veterinary and dental students may benefit from more applied, domain-specific content, while students in developing countries may require foundational exposure with accessible resources. Stakeholders should consider resource availability, technological infrastructure, and students' baseline familiarity when designing interventions.
-
3.
Prioritize Experiential and Practice-Oriented Learning
The findings emphasize that preparedness plays a mediating role in shaping positive attitudes. To improve students’ readiness to work with AI, educators should incorporate hands-on experiences, including simulation-based learning, problem-based case analysis, and guided interaction with AI-enabled clinical tools. This will help students build confidence and apply theoretical knowledge to real-world contexts.
-
4.
Monitor and Evaluate AI Curricula with Evidence-Based Metrics
Ongoing assessment of AI curricula is essential to ensure their relevance, effectiveness, and alignment with clinical and technological developments. Institutions should systematically gather student feedback, conduct pre- and post-course assessments, and track changes in knowledge, attitudes, and preparedness. These evaluations enable continuous improvement in content and pedagogy. Moreover, data-driven evaluation helps identify specific areas of weakness and informs targeted adjustments. Where possible, institutions should also consider longitudinal tracking to assess the sustained impact of AI education on students’ competencies and professional readiness.
Limitation and future directions
This study has several limitations. First, the sample may not fully represent the global medical student population, potentially limiting generalizability. Future research should include a more diverse range of schools and regions to enhance external validity. Second, self-reported data may be affected by response and perception biases; mixed-method approaches such as interviews or clinical observations could provide deeper insights. Additionally, the study did not control for confounders like prior AI knowledge, clinical exposure, or curriculum quality. Although the survey was pilot tested and reviewed by experts, further validation across cultural and linguistic contexts is recommended. Finally, selection bias may have occurred due to the online distribution of the survey and the voluntary nature of participation, potentially leading to an overrepresentation of students with a pre-existing interest in AI.
In terms of future directions, longitudinal studies are essential to examine the long-term effects of AI curricular on medical students’ knowledge retention, attitudes towards Artificial Intelligence, and job satisfaction. Experimental designs or quasi-experimental studies could be employed to establish a causal relationship between AI education and changes in students’ perceptions. Research should also explore the potential for interdisciplinary AI education that balances technical knowledge with ethical, legal, and societal implications. Furthermore, investigations into the most effective teaching methods and integration strategies for AI in medical education would be valuable for educators and policymakers in designing comprehensive and balanced AI curricula. Lastly, exploring the role of mentorship and peer interactions in shaping students’ perceptions of AI could provide additional insights into the educational process.
Acknowledgements
Not applicable.
Abbreviations
- AI
Artificial Intelligence
- CEM
Coarsened Exact Matching
- SEM
Structural Equation Modeling
- SD
Standard Deviation
- CFI
Comparative Fit Index
- TLI
Tucker-Lewis Index
- RMSEA
Root Mean Squared Error of Approximation
- SRMR
Standardized Root Mean Squared Residual
- STATA
Statistics and Data Software (StataCorp)
Authors’ contributions
LZ and YX contributed to the conception and design of the study. The data analysis was conducted by LZ. LZ and YX contributed to the drafting of the manuscript and all of the authors approved the final version to be submitted.
Funding
This research receive grant from the Ministry of Education of the People’s Republic of China (22JJD880002).
Data availability
The dataset analyzed in this study is available at 10.6084/m9.figshare.24422422.v1.
Declarations
Ethics approval and consent to participate
Ethical approval was obtained by the original research team from the Institutional Review Board at Charité-University Medicine Berlin (EA4/213/22) in compliance with the Declaration of Helsinki and its later amendments. To ensure participant anonymity, the necessity for informed consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Indices such as CFI and TLI, which are closer to 1, indicate a superior fit of the model, with an RMSEA value of less than .08 and an SRMR value of less than .05 being considered indicative of a satisfactory model fit [44, 59, 72]
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abbaoui W, Retal S, El Bhiri B, Kharmoum N, Ziti S. Towards revolutionizing precision healthcare: a systematic literature review of artificial intelligence methods in precision medicine. Inf Med Unlocked. 2024;46:101475. 10.1016/j.imu.2024.101475. [Google Scholar]
- 2.Abid A, Murugan A, Banerjee I, Purkayastha S, Trivedi H, Gichoya J. AI education for fourth-year medical students: two-year experience of a web-based, self-guided curriculum. JMIR Med Educ. 2024;10:e46500. 10.2196/46500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmad MN, Abdallah SA, Abbasi SA, Abdallah AM. Student perspectives on the integration of artificial intelligence into healthcare services. Digit Health. 2023;9:20552076231174096. 10.1177/20552076231174095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akingbola A, Adeleke O, Idris A, Adewole O, Adegbesan A. Artificial intelligence and the dehumanization of patient care. J Med Surg Public Health. 2024;3:100138. 10.1016/j.glmedi.2024.100138. [Google Scholar]
- 5.Alam F, Lim MA, Zulkipli IN. Integrating AI in medical education: embracing ethical usage and critical understanding. Front Med. 2023;10:1279707. 10.3389/fmed.2023.1279707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Albadrani BA, Abdel-Raheem MA, Al-Farwachi MI. Artificial intelligence in veterinary care: a review of applications for animal health. Egypt J Vet Sci. 2024;55(6):1725–36. 10.21608/ejvs.2024.260989.1769. [Google Scholar]
- 7.Al Hadithy ZA, Al Lawati A, Al-Zadjali R, Al Sinawi H. Knowledge, attitudes, and perceptions of artificial intelligence in healthcare among medical students at sultan Qaboos university. Cureus. 2023;15(9):e44887. 10.7759/cureus.44887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alowais SA, Alghamdi SS, Alsuhebany N, Alqahtani T, Alshaya AI, Almohareb SN, Aldairem A, Alrashed M, Saleh KB, Badreldin HA, Al Yami MS, Al Harbi S, Albekairy AM. Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC Med Educ. 2023;23(1):689. 10.1186/s12909-023-04698-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alwadani F, Lone A, Hakami M, Moria AH, Alamer W, Alghirash RA, Alnawah AK, Hadadi AS. Attitude and understanding of artificial intelligence among Saudi medical students: an online cross-sectional study. J Multidiscip Healthc. 2024. 10.2147/JMDH.S455260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amoozadeh M, Daniels D, Nam D, Kumar A, Chen S, Hilton M, Ragavan SS, Alipour MA. Trust in generative AI among students: An exploratory study. In Proceedings of the 55th ACM Technical Symposium on Computer Science Education V. 2024;1 (pp. 67-73). 10.1145/3626252.3630842
- 11.Appleby RB, Basran PS. Artificial intelligence in veterinary medicine. J Am Vet Med Assoc. 2022;260(8):819–24. 10.2460/javma.22.03.0093. [DOI] [PubMed] [Google Scholar]
- 12.Bates DW, Levine D, Syrowatka A, Kuznetsova M, Craig KJT, Rui A, Jackson GP, Rhee K. The potential of artificial intelligence to improve patient safety: a scoping review. NPJ Digit Med. 2021;4:54. 10.1038/s41746-021-00423-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Batra AM, Reche A. A new era of dental care: harnessing artificial intelligence for better diagnosis and treatment. Cureus. 2023;15(11):e49319. 10.7759/cureus.49319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baurasien BK, Alareefi HS, Almutairi DB, Alanazi MM, Alhasson AH, Alshahrani AD, Almansour SA, Alshagag ZA, Alqattan KM, Alotaibi HM. Medical errors and patient safety: Strategies for reducing errors using artificial intelligence. Int J Health Sci. 2023;7(S1):3471–87. 10.53730/ijhs.v7nS1.15143. [Google Scholar]
- 15.Benzinger L, Ursin F, Balke WT, Kacprowski T, Salloch S. Should artificial intelligence be used to support clinical ethical decision-making? A systematic review of reasons. BMC Med Ethics. 2023;24:48. 10.1186/s12910-023-00929-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bewersdorff A, Zhai X, Roberts J, Nerdel C. Myths, mis-and preconceptions of artificial intelligence: a review of the literature. Comput Educ. 2023;4:100143. 10.1016/j.caeai.2023.100143. [Google Scholar]
- 17.Bisdas S, Topriceanu CC, Zakrzewska Z, Irimia AZ, Shakallis L, Subhash J, Casapu MM, Leon-Rojas J, dos Santos DP, Andrews DM, Zeicu C, Bouhuwaish AM, Lestari AN, Abu-Ismail L, Sadiq AS, Khamees A, Mohammed KMG, Williams E, Omran AI, Ismail DYA, Ebrahim EH. Artificial intelligence in medicine: a multinational multi-center survey on the medical and dental students’ perception. Front Public Health. 2021;9:795284. 10.3389/fpubh.2021.795284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buchlak QD, Esmaili N, Bennett C, Farrokhi F. Natural language processing applications in the clinical neurosciences: a machine learning augmented systematic review. Machine Learn Clin Neurosci. 2022;134:277–89. 10.1007/978-3-030-85292-4_32. [DOI] [PubMed] [Google Scholar]
- 19.Burney IA, Ahmad N. Artificial Intelligence in medical education: a citation-based systematic literature review. J Shifa Tameer-E-Millat Univ. 2022;5(1):43–53. 10.32593/jstmu/Vol5.Iss1.183. [Google Scholar]
- 20.Busch F, Hoffmann L, Truhn D, Ortiz-Prado E, Makowski MR, Bressem KK, Adams LC. Global cross-sectional student survey on AI in medical, dental, and veterinary education and practice at 192 faculties. BMC Med Educ. 2024;24(1):1066. 10.1186/s12909-024-06035-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cai Z, Fan X, Du J. Gender and attitudes toward technology use: a meta-analysis. Comput Educ. 2017;105:1–13. 10.1016/j.compedu.2016.11.003. [Google Scholar]
- 22.Çalışkan SA, Demir K, Karaca O. Artificial intelligence in medical education curriculum: an e-Delphi study for competencies. PLoS ONE. 2022;17(7):e0271872. 10.1371/journal.pone.0271872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan KS, Zary N. Applications and challenges of implementing artificial intelligence in medical education: integrative review. JMIR Med Educ. 2019;5(1):e13930. 10.2196/13930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charow R, Jeyakumar T, Younus S, Dolatabadi E, Salhia M, Al-Mouaswas D, Anderson M, Balakumar S, Clare M, Dhalla A, Gillan C, Haghzare S, Jackson E, Lalani N, Mattson J, Peteanu W, Tripp T, Waldorf J, Williams S, Tavares W, Wiljer D. Artificial intelligence education programs for health care professionals: scoping review. JMIR Med Educ. 2021;7(4):e31043. 10.2196/31043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choudhury A, Asan O. Role of artificial intelligence in patient safety outcomes: systematic literature review. JMIR Med Inform. 2020;8(7):e18599. 10.2196/18599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chustecki M. Benefits and risks of AI in health care: narrative review. Interact J Med Res. 2024;13(1):e53616. 10.2196/53616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen A, Soffer T, Henderson M. Students’ use of technology and their perceptions of its usefulness in higher education: international comparison. J Comput Assist Learn. 2022;38(5):1321–31. 10.1111/jcal.12678. [Google Scholar]
- 28.Dave M, Patel N. Artificial intelligence in healthcare and education. Br Dent J. 2023;234(10):761–4. 10.1038/s41415-023-5845-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6(2):94–8. 10.7861/futurehosp.6-2-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Panfilis L, Peruselli C, Tanzi S, Botrugno C. AI-based clinical decision-making systems in palliative medicine: ethical challenges. BMJ Support Palliat Care. 2023;13(2):183–9. 10.1136/bmjspcare-2021-002948. [DOI] [PubMed] [Google Scholar]
- 31.Duan S, Liu C, Rong T, Zhao Y, Liu B. Integrating AI in medical education: a comprehensive study of medical students’ attitudes, concerns, and behavioral intentions. BMC Med Educ. 2025;25:599. 10.1186/s12909-025-07177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ennab M, Mcheick H. Enhancing interpretability and accuracy of AI models in healthcare: a comprehensive review on challenges and future directions. Front Robot AI. 2024;11:1444763. 10.3389/frobt.2024.1444763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Esmaeilzadeh P. Challenges and strategies for wide-scale artificial intelligence (AI) deployment in healthcare practices: a perspective for healthcare organizations. Artif Intell Med. 2024;151:102861. 10.1016/j.artmed.2024.102861. [DOI] [PubMed] [Google Scholar]
- 34.Esteva A, Robicquet A, Ramsundar B, Kuleshov V, DePristo M, Chou K, Cui C, Corrado G, Thrun S, Dean J. A guide to deep learning in healthcare. Nat Med. 2021;25(1):24–9. 10.1038/s41591-018-0316-z. [DOI] [PubMed] [Google Scholar]
- 35.Feigerlova E, Hani H, Hothersall-Davies E. A systematic review of the impact of artificial intelligence on educational outcomes in health professions education. BMC Med Educ. 2025;25:129. 10.1186/s12909-025-06719-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Franco D’Souza R, Mathew M, Mishra V, Surapaneni KM. Twelve tips for addressing ethical concerns in the implementation of artificial intelligence in medical education. Med Educ Online. 2024;29(1):2330250. 10.1080/10872981.2024.2330250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gandhi R, Parmar A, Kagathara J, Lakkad D, Kakadiya J, Murugan Y. Bridging the artificial intelligence (AI) divide: do postgraduate medical students outshine undergraduate medical students in AI readiness? Cureus. 2024;16(8):e67288. 10.7759/cureus.67288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ghaffari M, Zhu Y, Shrestha A. A review of advancements of artificial intelligence in dentistry. Dentistry Review. 2024;4(2):100081. 10.1016/j.dentre.2024.100081. [Google Scholar]
- 39.Gong B, Nugent JP, Guest W, Parker W, Chang P, Khosa F, Nicolaou S. Influence of artificial intelligence on Canadian medical students’ preference for radiology specialty. Acad Radiol. 2019;26(4):566–77. 10.1016/j.acra.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 40.Gordon M, Daniel M, Ajiboye A, Uraiby H, Xu NY, Bartlett R, Hanson J, Haas M, Spadafore M, Grafton-Clarke C, Gasiea RY, Michie C, Corral J, Kwan B, Thammasitboon S. A scoping review of artificial intelligence in medical education: BEME guide no. 84. Med Teach. 2024;46(4):446–70. 10.1080/0142159X.2024.2314198. [DOI] [PubMed] [Google Scholar]
- 41.Grunhut J, Marques O, Wyatt ATM. Needs, challenges, and applications of artificial intelligence in medical education curriculum. JMIR Medical Education. 2021;8(2):e35587. 10.2196/35587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guo J, Li B. The application of medical artificial intelligence technology in rural areas of developing countries. Health Equity. 2018;2(1):174–81. 10.1089/heq.2018.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Güven GÖ, Yilmaz Ş, Inceoğlu F. Determining medical students’ anxiety and readiness levels about artificial intelligence. Heliyon. 2024;10(4): e25894. 10.1016/j.heliyon.2024.e25894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate Data Analysis (7th Edition). Pearson. 2012.
- 45.Hamilton, V., Brisco, R., & Grierson, H. How can AI support the creation of novel ideas in product design. In 26th International Conference on Engineering and Product Design Education: Rise of the Machines: Design Education in the Generative AI Era. The Design Society. 2024:133-138. 10.35199/EPDE.2024.23.
- 46.Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts HJ. Artificial intelligence in radiology. Nat Rev Cancer. 2018;18(8):500–10. 10.1038/s41568-018-0016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hui ML, Sacoransky E, Chung A, Kwan BY. Exploring the integration of artificial intelligence in radiology education: a scoping review. Curr Probl Diagn Radiol. 2024. 10.1067/j.cpradiol.2024.10.012. [DOI] [PubMed] [Google Scholar]
- 48.Iacus SM, King G, Porro G. Multivariate matching methods that are monotonic imbalance bounding. J Am Stat Assoc. 2011;106(493):345–61. 10.1198/jasa.2011.tm09599. [Google Scholar]
- 49.Iweuno BN, Orekha P, Ojediran O, Imohimi E, Adu-Twum HT. Leveraging Artificial Intelligence for an inclusive and diversified curriculum. World J Adv Res Rev. 2024;23(2):1579–90. 10.30574/wjarr.2024.23.2.2440. [Google Scholar]
- 50.Jalal R, Prajapati AK, Bora P. Exploring the intersection of psychology and artificial intelligence: Implications and challenges. In Artificial intelligence: A modern approach in different fields (pp. 41–52). Laxmi Book Publication. 2024.
- 51.Jamal A, Solaiman M, Alhasan K, Temsah MH, Sayed G, Soliman M. Integrating ChatGPT in medical education: adapting curricula to cultivate competent physicians for the AI era. Cureus. 2023;15(8):e43036. 10.7759/cureus.43036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, Wang Y, Dong Q, Shen H, Wang Y. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2(4):230–43. 10.1136/svn-2017-000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jongsma KR, van Solinge WW, Haitjema S. Eight misconceptions about AI in healthcare. Ned Tijdschr Geneeskd. 2023;167:D7578–D7578. [PubMed] [Google Scholar]
- 54.Kansal R, Bawa A, Bansal A, Trehan S, Goyal K, Malhotra K. Differences in knowledge and perspectives on the usage of artificial intelligence among doctors and medical students of a developing country: a cross-sectional study. Cureus. 2022;14(1):e21434. 10.7759/cureus.21434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Khalifa M, Albadawy M. AI in diagnostic imaging: revolutionising accuracy and efficiency. Comput Methods Programs Biomed Update. 2024;5:100146. 10.1016/j.cmpbup.2024.100146. [Google Scholar]
- 56.Khalifa M, Albadawy M, Iqbal U. Advancing clinical decision support: the role of artificial intelligence across six domains. Comput Methods Programs Biomed Update. 2024;5:100142. 10.1016/j.cmpbup.2024.100142. [Google Scholar]
- 57.Khan MJ, Lajber M, Bilal N, Khan S, Ahmad A. The barriers and solution to Artificial intelligence adoption in medical education: a qualitative study. J Saidu Med College Swat. 2024;14(4):341–7. 10.52206/jsmc.2024.14.4.957. [Google Scholar]
- 58.Khogali HO, Mekid S. Perception and ethical challenges for the future of AI as encountered by surveyed new engineers. Soc (Basel). 2024;14(12):271. 10.3390/soc14120271. [Google Scholar]
- 59.Kline RB. Principles and Practice of Structural Equation Modeling. Guilford Press; 2005. [Google Scholar]
- 60.Kimmerle J, Timm J, Festl-Wietek T, Cress U, Herrmann-Werner A. Medical students’ attitudes toward AI in medicine and their expectations for medical education. J Med Educ Curric Dev. 2023;10:23821205231219344. 10.1101/2023.07.19.23292877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Krive J, Isola M, Chang L, Patel T, Anderson M, Sreedhar R. Grounded in reality: artificial intelligence in medical education. JAMIA Open. 2023;6(2):00ad037. 10.1093/jamiaopen/ooad037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lamem MFH, Sahid MI, Ahmed A. Artificial intelligence for access to primary healthcare in rural settings. J Med Surg Public Health. 2024;5:100173. 10.1016/j.glmedi.2024.100173. [Google Scholar]
- 63.Lee J, Wu AS, Li D, Kulasegaram K. Artificial intelligence in undergraduate medical education: a scoping review. Acad Med. 2021;96(11S):S62–70. 10.1097/ACM.0000000000004291. [DOI] [PubMed] [Google Scholar]
- 64.Locke S, Bashall A, Al-Adely S, Moore J, Wilson A, Kitchen GB. Natural language processing in medicine: a review. Trends Anaesth Crit Care. 2021;38:4–9. 10.1016/j.tacc.2021.02.007. [Google Scholar]
- 65.Li M, Jiang Y, Zhang Y, Zhu H. Medical image analysis using deep learning algorithms. Front Public Health. 2023;11:1273253. 10.3389/fpubh.2023.1273253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li Q, Qin Y. AI in medical education: medical student perception, curriculum recommendations and design suggestions. BMC Med Educ. 2023;23(1):852. 10.1186/s12909-023-04700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Longoni C, Bonezzi A, Morewedge CK. Resistance to medical artificial intelligence. J Consum Res. 2019;46(4):629–50. 10.1093/jcr/ucz013. [Google Scholar]
- 68.Lund BD, Mannuru NR, Agbaji DA. AI anxiety and fear: A look at perspectives of information science students and professionals towards artificial intelligence. J Inf Sci. 2024. 10.1177/01655515241282001. [Google Scholar]
- 69.Ma Y, Song Y, Balch JA, Ren Y, Vellanki D, Hu Z, Brennan M, Kolla S, Guan Z, Armfield B, Ozrazgat-Baslanti T, Rashidi P, Loftus TJ, Bihorac A, Shickel B. (2024). Promoting AI competencies for medical students: a scoping review on frameworks, programs, and tools. arXiv preprint arXiv:2407.18939. 10.48550/arXiv.2407.18939.
- 70.Macruz F. Misconceptions in the health technology industry that are delaying the translation of artificial intelligence technology into relevant clinical applications. Radiol Bras. 2021;54:243–5. 10.1590/0100-3984.2020.0151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Malerbi FK, Nakayama LF, Gayle Dychiao R, Zago Ribeiro L, Villanueva C, Celi LA, Regatieri CV. Digital education for the deployment of artificial intelligence in health care. Journal of Medical Internet Research. 2023;25:e43333. 10.2196/43333. [DOI] [PMC free article] [PubMed]
- 72.Markus KA. Principles and practice of structural equation modeling by Rex B. Kline. Struct Equ Modeling A Multidiscip J. 2012;19(3):509–12. 10.1080/10705511.2012.687667. [Google Scholar]
- 73.Masters K. Artificial intelligence in medical education. Med Teach. 2019;41(9):976–80. 10.1080/0142159X.2019.1595557. [DOI] [PubMed] [Google Scholar]
- 74.McCoy L, Nagaraj S, Morgado F, Harish V, Das S, Celi L. What do medical students actually need to know about artificial intelligence? NPJ Digital Med. 2020;3(1):86. 10.1038/s41746-020-0294-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mehta N, Harish V, Bilimoria K, Morgado F, Ginsburg S, Law M, Das S. Knowledge of and attitudes on artificial intelligence in healthcare: A provincial survey study of medical students. Medrxiv, 2021–01. 2021. 10.1101/2021.01.14.21249830
- 76.Melisa R, Ashadi A, Triastuti A, Hidayati S, Salido A, Ero PEL, Marlini C, Zefrin Z, Fuad ZA. Critical thinking in the age of AI: A systematic review of AI’s effects on higher education. Educ Process Int J. 2025;14:e2025031. 10.22521/edupij.2025.14.31. [Google Scholar]
- 77.Mennella C, Maniscalco U, De Pietro G, Esposito M. Ethical and regulatory challenges of AI technologies in healthcare: a narrative review. Heliyon. 2024;10(4):e26297. 10.1016/j.heliyon.2024.e26297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mesko B, Hetényi G, Győrffy Z. Will artificial intelligence solve the human resource crisis in healthcare? BMC Health Serv Res. 2018;18(1):545. 10.1186/s12913-018-3330-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Miotto R, Wang F, Wang S, Jiang X, Dudley JT. Deep learning for healthcare: review, opportunities and challenges. Brief Bioinform. 2018;19(6):1236–46. 10.1093/bib/bbx044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mir MM, Mir GM, Raina NT, Mir SM, Mir SM, Miskeen E, Alharthi MH, Alamri MMS. Application of artificial intelligence in medical education: current scenario and future perspectives. J Adv Med Educ Prof. 2023;11(3):133–40. 10.30476/JAMP.2023.98655.1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mittal A, Afsar A, Tayal A, Shetty M. Artificial intelligence and healthcare. MAMC J Med Sci. 2023;9(2):81–7. 10.4103/mamcjms.mamcjms_27_23. [Google Scholar]
- 82.Moldt JA, Festl-Wietek T, Madany Mamlouk A, Nieselt K, Fuhl W, Herrmann-Werner A. Chatbots for future docs: exploring medical students’ attitudes and knowledge towards artificial intelligence and medical chatbots. Med Educ Online. 2023;28(1):2182659. 10.1080/10872981.2023.2182659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Musleh D, Almossaeed H, Balhareth F, Alqahtani G, Alobaidan N, Altalag J, Aldossary MI. Advancing dental diagnostics: a review of artificial intelligence applications and challenges in dentistry. Big Data Cogn Comput. 2024;8(6):66. 10.3390/bdcc8060066. [Google Scholar]
- 84.Naqvi WM, Sundus H, Mishra G, Muthukrishnan R, Kandakurti PK. AI in medical education curriculum: the future of healthcare learning. Eur J Ther. 2024;30(2):e23–5. 10.58600/eurjther1995. [Google Scholar]
- 85.Narayanan S, Ramakrishnan R, Durairaj E, Das A. Artificial intelligence revolutionizing the field of medical education. Cureus. 2023;15(11): e49604. 10.7759/cureus.49604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Naseer MA, Saeed S, Afzal A, Ali S, Malik MGR. Navigating the integration of artificial intelligence in the medical education curriculum: a mixed-methods study exploring the perspectives of medical students and faculty in Pakistan. BMC Med Educ. 2025;25(1):273. 10.1186/s12909-024-06552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nwankwo EI, Emeihe EV, Ajegbile MD, Olaboye JA, Maha CC. Integrating telemedicine and AI to improve healthcare access in rural settings. Int J Life Sci Res Archive. 2024;7(1):59–77. 10.53771/ijlsra.2024.7.1.0061. [Google Scholar]
- 88.Paranjape K, Schinkel M, Nannan Panday RN, Car J, Nanayakkara P. Introducing artificial intelligence training in medical education. JMIR Med Educ. 2019;5(2):e16048. 10.2196/16048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Park SH, Pinto-Powell R, Thesen T, Lindqwister A, Levy J, Chacko R, Gonzalez D, Bridges C, Schwendt A, Byruma T, Fong J, Shasavari S, Hassanpour S. Preparing healthcare leaders of the digital age with an integrative artificial intelligence curriculum: a pilot study. Med Educ Online. 2024;29(1):2315684. 10.1080/10872981.2024.2315684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Passi S, Vorvoreanu M. Overreliance on AI literature review. Microsoft. 2022.
- 91.Petrescu MA, Pop EL, Mihoc TD. Students’ interest in knowledge acquisition in artificial Intelligence. Proc Comput Sci. 2023;225:1028–36. 10.48550/arXiv.2311.16193. [Google Scholar]
- 92.Pizzolla I, Aro R, Duez P, De Lièvre B, Briganti G. Integrating artificial intelligence into medical education: lessons learned from a Belgian initiative. J Interact Learn Res. 2023;34(2):401–24. [Google Scholar]
- 93.Polevikov S. Advancing AI in healthcare: a comprehensive review of best practices. Clin Chim Acta. 2023;548:117519. [DOI] [PubMed] [Google Scholar]
- 94.Pucchio A, Eisenhauer EA, Moraes FY. Medical students need artificial intelligence and machine learning training. Nat Biotechnol. 2021;39(3):388–9. 10.1038/s41587-021-00846-2. [DOI] [PubMed] [Google Scholar]
- 95.Quinn TP, Senadeera M, Jacobs S, Coghlan S, Le V. Trust and medical AI: the challenges we face and the expertise needed to overcome them. J Am Med Inform Assoc. 2021;28(4):890–4. 10.1093/jamia/ocaa268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Raihan A. A comprehensive review of artificial intelligence and machine learning applications in energy sector. J Technol Innov Energy. 2023;2(4):126–42. 10.32628/IJSRST2411587. [Google Scholar]
- 97.Rasouli S, Alkurdi D, Jia B. The role of artificial intelligence in modern medical education and practice: A systematic literature review. medRxiv. 2024:2024–07. 10.1101/2024.07.25.24311022
- 98.Rawas S, Tafran C, Alsaeed D, Al-Ghreimil N. Transforming healthcare: AI-NLP fusion framework for precision decision-making and personalized care optimization in the era of IoMT. Comput Mater Contin. 2024;81(3):4575–601. 10.32604/cmc.2024.055307. [Google Scholar]
- 99.Rizwan S, Rizwan S, Rizwan M, Hashim A, Batool S. Perceptions of medical students towards artificial intelligence: Medical students towards artificial intelligence. Pakistan J Health Sci. 2025;6(1):36–41. 10.54393/pjhs.v6i1.2364. [Google Scholar]
- 100.Robleto E, Habashi A, Benites Kaplan MA, Riley RL, Zhang C, Bianchi L, Shehadeh LA. Medical students’ perceptions of an artificial intelligence (AI) assisted diagnosing program. Med Teach. 2024;46(9):1180–6. 10.1080/0142159X.2024.2305369. [DOI] [PubMed] [Google Scholar]
- 101.Rosenheck M. AI in medical education: Challenges and opportunities. Digital Health. 2025:27–40. 10.1016/B978-0-443-23901-4.00003-9
- 102.Saad M, Shehadeh A, Alanazi SM, Alenezi M, Abu alez A, Eid H, Alfaouri MS, Aldawsari S, Alenezi R. Medical students’ knowledge and attitude towards artificial intelligence: an online survey. Open Public Health J. 2022;15(1):e187494452203290. 10.2174/18749445-v15-e2203290. [Google Scholar]
- 103.Sapci AH, Sapci HA. Artificial intelligence education and tools for medical and health informatics students: systematic review. JMIR Med Educ. 2020;6(1):e19285. 10.2196/19285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sarker IH. Machine learning: algorithms, real-world applications and research directions. SN Comput Sci. 2021;2(3):160. 10.1007/s42979-021-00592-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sarfaraz S, Khurshid Z, Zafar MS. Use of artificial intelligence in medical education: a strength or an infirmity. J Taibah Univ Med Sci. 2023;18(6):1553–4. 10.1016/j.jtumed.2023.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Schwalbe N, Wahl B. Artificial intelligence and the future of global health. The Lancet. 2020;395(10236):1579–86. 10.1016/S0140-6736(20)30226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Seth P, Hueppchen N, Miller SD, Rudzicz F, Ding J, Parakh K, Record JD. Data science as a core competency in undergraduate medical education in the age of artificial intelligence in health care. JMIR Med Educ. 2023;9:e46344. 10.2196/46344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Shahab H, Iqbal M, Sohaib A, Rehman A, Bermak A, Munir K. Design and implementation of an IoT-based monitoring system for early detection of lumpy skin disease in cattle. Smart Agricultural Technol. 2024;9:100609. 10.1016/j.atech.2024.100609. [Google Scholar]
- 109.Sharma, P. The Use of AI in English Learning among Students: Case Study in English Department. Global Institute of Technology and Managment. 2023.
- 110.Shastry KA, Shastry A. An integrated deep learning and natural language processing approach for continuous remote monitoring in digital health. Dec Analytics J. 2023;8:100301. 10.1016/j.dajour.2023.100301. [Google Scholar]
- 111.Shinde S, Patil Y, Jamkhande A, Shah Y, Kakde N, Waghmare P, Sonone R, Pote S, Vaidya I. Artificial intelligence in dentistry. J Indian Assoc Public Health Dent. 2024;22(1):6–10. 10.4103/jiaphd.jiaphd_272_22. [Google Scholar]
- 112.Simms RC. Generative artificial intelligence (AI) literacy in nursing education: a crucial call to action. Nurse Educ Today. 2025;146:106544. 10.1016/j.nedt.2024.106544. [DOI] [PubMed] [Google Scholar]
- 113.Singh, V., Singh, G., & Sharma, G. (2025). The future of the healthcare workforce in the age of automation. In Driving Global Health and Sustainable Development Goals with Smart Technology (pp. 453–472). IGI Global Scientific Publishing. 10.4018/979-8-3373-0240-9.ch019
- 114.Sit C, Srinivasan R, Amlani A, Muthuswamy K, Azam A, Monzon L, Poon DS. Attitudes and perceptions of UK medical students towards artificial intelligence and radiology: a multicentre survey. Insights Imaging. 2020;11:14. 10.1186/s13244-019-0830-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Staddon RV. Bringing technology to the mature classroom: age differences in use and attitudes. Int J Educ Technol High Educ. 2020;17(1):11. 10.1186/s41239-020-00184-4. [Google Scholar]
- 116.Sun L, Yin C, Xu Q, Zhao W. Artificial intelligence for healthcare and medical education: a systematic review. Am J Transl Res. 2023;15(7):4820. [PMC free article] [PubMed] [Google Scholar]
- 117.Tolentino R, Baradaran A, Gore G, Pluye P, Abbasgholizadeh-Rahimi S. Curriculum frameworks and educational programs in AI for medical students, residents, and practicing physicians: scoping review. JMIR Med Educ. 2024;10(1):e54793. 10.2196/54793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Topol E. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25(1):44–56. 10.1038/s41591-018-0300-7. [DOI] [PubMed] [Google Scholar]
- 119.Tossell CC, Tenhundfeld NL, Momen A, Cooley K, de Visser EJ. Student perceptions of ChatGPT use in a college essay assignment: implications for learning, grading, and trust in artificial intelligence. IEEE Trans Learn Technol. 2024;17:1069–81. 10.1109/TLT.2024.3355015. [Google Scholar]
- 120.Tozsin A, Ucmak H, Soyturk S, Aydin A, Gozen AS, Fahim MA, Güven S, Ahmed K. The role of artificial intelligence in medical education: a systematic review. Surg Innov. 2024;31(4):415–24. 10.1177/15533506241248239. [DOI] [PubMed] [Google Scholar]
- 121.Tung AYZ, Dong LW. Malaysian medical students’ attitudes and readiness toward AI (Artificial Intelligence): a cross-sectional study. J Med Educ Curric Dev. 2023;10:23821205231201164. 10.1177/23821205231201164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Vodanović M, Subašić M, Milošević D, Savićpavičin I. Artificial intelligence in medicine and dentistry. Acta Stomatol Croat Int J Oral Sci Dental Med. 2023;57(1):70–84. 10.15644/asc57/1/8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wang L, Li W. The impact of AI usage on university students’ willingness for autonomous learning. Behav Sci. 2024;14(10):956. 10.3390/bs14100956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wartman SA, Combs CD. Medical education must move from the information age to the age of artificial intelligence. Acad Med. 2018;93(8):1107–9. 10.1097/ACM.0000000000002044. [DOI] [PubMed] [Google Scholar]
- 125.Weidener L, Fischer M. Proposing a principle-based approach for teaching AI ethics in medical education. JMIR Med Educ. 2024;10:e55368. 10.2196/55368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Weidener L, Fischer M. Artificial intelligence in medicine: cross-sectional study among medical students on application, education, and ethical aspects. JMIR Med Educ. 2024;10:e51247. 10.2196/51247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wobo KN, Nnamani IO, Alinnor EA, Gabriel-Job N, Paul N. Medical students’ perception of the use of artificial intelligence in medical education. Int J Res Med Sci. 2025;13(1):82. 10.18203/2320-6012.ijrms20244099. [Google Scholar]
- 128.Zahlan A, Ranjan RP, Hayes D. Artificial intelligence innovation in healthcare: literature review, exploratory analysis, and future research. Technol Soc. 2023;74:102321. 10.1016/j.techsoc.2023.102321. [Google Scholar]
- 129.Zanca F, Hernandez-Giron I, Avanzo M, Guidi G, Crijns W, Diaz O, Kagadis GC, Rampado O, Lønne PI, Ken S, Colgan N, Zaidi H, Zakaria GA, Kortesniemi M. Expanding the medical physicist curricular and professional programme to include artificial intelligence. Phys Med. 2021;83:174–83. 10.1016/j.ejmp.2021.01.069. [DOI] [PubMed] [Google Scholar]
- 130.Zarei M, Mamaghani HE, Abbasi A, Hosseini MS. Application of artificial intelligence in medical education: a review of benefits, challenges, and solutions. Med Clín Práct. 2024;7(2):100422. 10.1016/j.mcpsp.2023.100422. [Google Scholar]
- 131.Zhang W, Cai M, Lee HJ, Evans R, Zhu C, Ming C. AI in medical education: global situation, effects and challenges. Educ Inf Technol. 2024;29(4):4611–33. 10.1007/s10639-023-12009-8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analyzed in this study is available at 10.6084/m9.figshare.24422422.v1.


