Abstract
Autophagy-dependent cell death (ADCD) presents a promising but challenging therapeutic strategy in cancer treatment. Autophagy regulates cellular breakdown and stress responses, serving a dual function—either inhibiting tumorigenesis or facilitating the survival of cancer cells in advanced stages. This paradox presents both opportunities and challenges in the exploration of autophagy as a potential target for cancer treatment. In this review, we explore various pharmacological agents, including autophagy inhibitors (e.g., chloroquine, 3-MA) and activators (e.g., rapamycin, metformin), which have demonstrated effectiveness in modulating autophagy-dependent cell death (ADCD). These agents either enhance cancer cell apoptosis or sensitize tumors to conventional therapies. Combination therapies, such as the use of autophagy modulators alongside chemotherapy, immunotherapy, or radiation therapy, offer enhanced therapeutic potential by overcoming drug resistance and improving overall treatment efficacy. Nonetheless, significant challenges remain, including tumor heterogeneity, treatment resistance, and off-target effects of autophagy-targeting agents. Future progress in biomarker discovery, precision medicine, and targeted medication development will be crucial for enhancing ADCD-based methods. Although autophagy-dependent cell death presents significant potential in cancer treatment, additional studies and clinical validation are necessary to confirm its position as a conventional therapeutic approach. Therefore, this review aims to identify the existing restrictions that will facilitate the development of more effective and personalized cancer therapies, hence enhancing patient survival and outcomes.
Keywords: autophagy, autophagy-dependent cell death, cancer therapy, molecular mechanisms, tumor microenvironment
1. Introduction
Cancer remains a significant worldwide health problem, responsible for millions of deaths annually, despite continuous progress in early identification, diagnostics, and treatment [1]. Traditional therapeutic methods, including chemotherapy, radiation, and immunotherapy, have markedly enhanced patient outcomes [2]. Nonetheless, treatment resistance, tumor heterogeneity, and severe side effects persist in constraining the efficacy of these strategies [3]. Therefore, there is an immediate necessity to investigate alternative therapeutic targets and innovative methods of cell death that might be utilized for cancer treatment.
Autophagy-dependent cell death (ADCD) is a form of regulated cell death (RCD) that utilizes the autophagy mechanism explicitly to facilitate cellular destruction. Unlike other programmed cell death mechanisms, such as apoptosis or necroptosis, where autophagy may be involved but is not solely responsible, ADCD relies on an efficient autophagy system for its successful execution [4]. In contrast to apoptosis, which is extensively described and commonly targeted in cancer treatment, ADCD is comparatively under-researched. Nonetheless, increasing evidence suggests that excessive or dysregulated autophagy may lead to cellular death, providing a potential method for eliminating cancer cells [5]. Autophagy, a catabolic mechanism that degrades and recycles cellular components, is crucial for sustaining cellular homeostasis [4,6]. It enables cells to endure adverse circumstances, including nutritional scarcity, oxidative stress, and hypoxia, by destroying impaired organelles and misfolded proteins [6]. In cancer, autophagy plays a dual role, functioning as a tumor suppressor in early-stage malignancies and as a tumor promoter in advanced tumors, facilitating cancer cell survival under metabolic and pharmacological stress [7]. The contradictory function of autophagy in cancer advancement emphasizes the intricacy of this phenomenon and stresses the necessity for a more profound comprehension of its molecular underpinnings.
Autophagy is meticulously regulated by a network of signaling pathways and autophagy-related genes (ATGs), which control its onset, advancement, and termination [8]. The process encompasses multiple essential stages: initiation, nucleation, elongation, and destruction, facilitated by a fundamental group of regulatory proteins [9]. Beclin-1 is a pivotal regulator of autophagy, forming a complex with class III phosphatidylinositol 3-kinase (PI3K) to commence autophagosome production [10]. The transformation of cytosolic LC3-I into membrane-associated LC3-II signifies the maturity of autophagosomes, enabling their fusion with lysosomes for the degradation and recycling of cellular constituents [11]. Although autophagy generally functions as a survival strategy, excessive autophagic activity can induce cell death, particularly when it leads to the indiscriminate destruction of vital cellular components.
The regulation of ADCD is influenced by numerous intracellular and extracellular factors, including metabolic stress, oxidative damage, and interactions with alternative cell death pathways [12]. The interaction among autophagy, apoptosis, and necroptosis is notably critical in cancer [13], as these pathways share regulatory factors and can influence one another's activation. Proteins, including p53, Bcl-2, and caspases, are recognized for their role in modulating both apoptotic and autophagic cell death, thereby introducing further complexity to the regulation of cancer cell fate [14]. Autophagy may serve as a precursor to apoptosis, facilitating cell survival under moderate stress while inducing cell death under extreme stress [15]. In certain instances, autophagy may function as an autonomous cell death mechanism, distinct from apoptosis and necroptosis, providing an alternative method for eradicating cancer cells that are resistant to conventional treatments [16].
Therefore, ADCD is an innovative and promising strategy for cancer treatment. The dual role of autophagy in cancer complicates therapeutic targeting; nonetheless, advancements in understanding its molecular underpinnings have facilitated the development of novel therapy regimens [17]. By specifically regulating autophagy, it may be possible to utilize this mechanism to enhance cancer cell mortality, overcome drug resistance, and improve the efficacy of current treatments. This review would like to suggest that autophagy-based therapeutic techniques could transform cancer treatment and offer renewed hope for patients with drug-resistant and aggressive malignancies.
2. Molecular Mechanisms of Autophagy and Autophagy-Dependent Cell Death
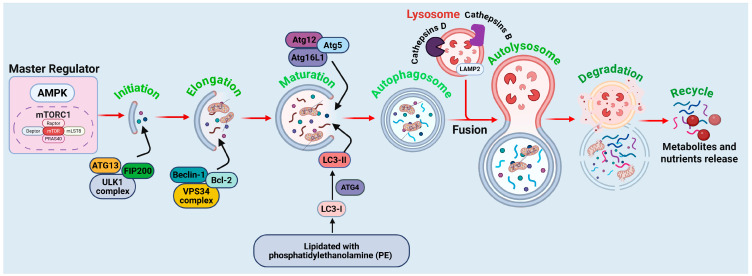
Considering the regulatory pathways of autophagy offers significant insights into potential therapeutic strategies for cancer treatment, especially in utilizing autophagy-dependent cell death as an innovative anticancer method. The molecular mechanisms of autophagy are illustrated in Figure 1, with detailed descriptions provided in the following sections.
Figure 1.
Molecular mechanism of autophagy. The initiation phase is governed by the ULK1 complex (comprising ULK1, ATG13, and FIP200), which is activated by AMPK and suppressed by mTORC1 signaling per food availability. Throughout elongation and maturation, the Beclin-1–VPS34 complex initiates the phagophore, whilst the ATG12-ATG5-ATG16L1 complex and lipidated LC3-II facilitate membrane extension and cargo encapsulation. Bcl-2 exerts an adverse regulatory effect on Beclin-1, hence inhibiting autophagy. During the autophagosome development phase, mature autophagosomes enclose cytoplasmic constituents, such as impaired organelles and proteins. The fusion step involves the docking of lysosomes through LAMP2, resulting in the formation of autolysosomes, where lysosomal enzymes, such as cathepsins B and D, destroy the cargo. The degradation and recycling phase facilitates the release of amino acids, lipids, and other metabolites, thus reinstating cellular equilibrium and aiding metabolic adaptability. The figure is original and was created and generated by BioRender.com, an online commercial platform.
2.1. Autophagy and Its Regulatory Pathways
Autophagy is a precisely regulated degradation mechanism that removes damaged organelles, misfolded proteins, and pathogens [18]. The process is facilitated by a collection of autophagy-related genes (ATGs) and can be generally classified into the following stages.
2.1.1. Initiation of Autophagy
The initial phase of autophagy is precisely controlled by the Unc-51-like kinase 1 (ULK1) complex, which functions as a crucial indicator of cellular stress [5]. Under typical circumstances, the mechanistic target of rapamycin complex 1 (mTORC1) suppresses ULK1 activity by phosphorylating ATG13 and FIP200, thereby preventing the initial phase of autophagy [19]. Under conditions such as nutritional deprivation or metabolic stress, AMP-activated protein kinase (AMPK) suppresses mTORC1 and directly activates ULK1 via phosphorylation [20]. The activated ULK1 complex, comprising ULK1, ATG13, and FIP200, subsequently phosphorylates downstream targets, facilitating the recruitment of other autophagy-related proteins essential for autophagosome formation [21]. This initial stage is crucial for determining whether autophagy serves as a survival or cell death mechanism in cancer cells.
2.1.2. Nucleation: Formation of the Phagophore
During the initiation of autophagy, the subsequent phase involves nucleation, which is governed by the Beclin-1 (ATG6)-Vps34 complex. Beclin-1, a tumor suppressor protein, forms a core complex with class III phosphatidylinositol 3-kinase (PI3K), also known as Vps34 [7]. This complex is crucial for synthesizing phosphatidylinositol-3-phosphate (PI3P), a lipid that attracts supplementary autophagy-related proteins required for phagophore formation. The activity of the Beclin-1 complex is stringently regulated by interactions with regulatory proteins, including Bcl-2 and Bcl-xL, which can obstruct autophagy by sequestering Beclin-1 [22]. In contrast, pro-autophagic signals, such as BH3-only proteins (e.g., Bad, Bnip3), can interfere with the Beclin-1-Bcl-2 connection, thereby facilitating autophagy [23]. The nucleation phase is pivotal in ascertaining whether autophagy promotes cell survival or advances to autophagy-mediated cell death.
2.1.3. Elongation and Maturation of Autophagosomes
After nucleation, the phagophore extends to create a double-membraned autophagosome that encases cytoplasmic material. This process is facilitated by two ubiquitin-like conjugation systems: the ATG12-ATG5-ATG16L1 complex and the LC3 (microtubule-associated protein 1A/1B-light chain 3) conjugation system [24]. In the initial system, ATG12 is covalently linked to ATG5 in a manner reliant on ATG7 and ATG10 [25]. The ATG12-ATG5 complex subsequently engages with ATG16L1, creating a scaffold essential for the elongation of the autophagosome membrane [26]. In the second conjugation method, LC3 is subjected to proteolytic cleavage by ATG4, resulting in the formation of LC3-I, which is subsequently lipidated with phosphatidylethanolamine (PE) to produce LC3-II [27]. LC3-II is a crucial indicator of autophagosome formation, playing a role in cargo selection and membrane expansion [28]. LC3-II on autophagosomes promotes their fusion with lysosomes, indicating the onset of the degradation phase.
2.1.4. Fusion with Lysosomes and Cargo Degradation
The finalizing phase of autophagy entails the fusion of autophagosomes with lysosomes, resulting in the formation of autolysosomes, where the enclosed cellular components undergo degradation and recycling [29]. The mediation of this process involves SNARE proteins, particularly syntaxin-17 (STX17), alongside small GTPases like Rab7 [30]. Cathepsin D, a lysosomal enzyme, degrades autolysosomal contents, facilitating the release of amino acids, fatty acids, and other macromolecules into the cytoplasm for reutilization [31]. The effective execution of this step influences the outcome of autophagic activity. Controlled autophagic degradation supports cellular survival by maintaining metabolic balance. Excessive autophagy may lead to autophagy-dependent cell death, particularly in cancer cells, through the depletion of essential cellular components and the initiation of a metabolic catastrophe.
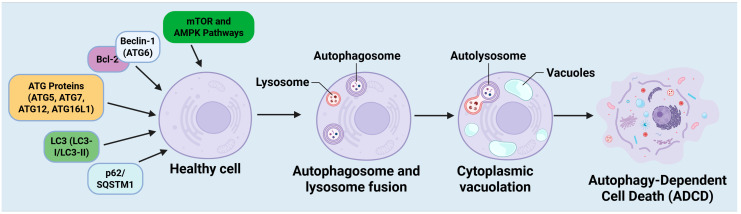
2.2. Molecular Mechanisms of Autophagy-Dependent Cell Death
Autophagy-dependent cell death (ADCD) is a regulated form of cell death characterized by excessive or dysregulated autophagy, which results in the degradation of vital cellular components and ultimately leads to cell death [32]. Multiple essential molecular components govern this process, encompassing autophagy-related proteins (ATGs), signaling pathways, and specific autophagic adaptors. The interaction among these elements dictates whether autophagy serves as a protective mechanism or facilitates cell death in cancer (Figure 2).
Figure 2.
Mechanism of autophagy-dependent cell death (ADCD). Initiation of ADCD from a healthy cell. Essential regulatory molecules, such as Beclin-1 (ATG6), ATG proteins (ATG5, ATG7, ATG12, ATG16L1), LC3 (LC3-I/LC3-II), p62/SQSTM1, and the upstream regulators mTOR and AMPK pathways, coordinate the onset and advancement of autophagy. In reaction to cellular stress, autophagosomes are formed and subsequently merge with lysosomes to create autolysosomes. Continuous autophagic activity causes cytoplasmic vacuolation and the breakdown of vital cellular components, ultimately culminating in ADCD. The function of excessive or dysregulated autophagy in facilitating non-apoptotic, planned cell death marked by significant vacuolization and organelle degradation. The figure was modified and created using the BioRender.com online commercial platform.
2.2.1. Beclin-1 (ATG6): A Principal Regulator of Autophagy
Beclin-1 (ATG6) is a fundamental regulator of autophagy and is essential for commencing the process [33]. It constitutes the fundamental element of the class III phosphatidylinositol 3-kinase (PI3K) complex, which is crucial for the nucleation of autophagosomes. Beclin-1 engages with many regulatory proteins, such as Bcl-2, Bcl-xL, and AMBRA1, to regulate autophagy [34]. In cancer, Beclin-1 is often dysregulated, exhibiting loss-of-function mutations or diminished expression in several malignancies, including breast, ovarian, and prostate cancers [35]. The downregulation of Beclin-1 hinders autophagy, allowing cancer cells to evade autophagic cell death and facilitating tumor progression [36]. In contrast, the overexpression of Beclin-1 can stimulate autophagy and augment ADCD, positioning it as a potential therapeutic target for cancer treatment [36]. The equilibrium between Beclin-1-mediated autophagy and apoptosis is crucial in determining cell fate, particularly in response to chemotherapeutic agents that induce autophagy-dependent cytotoxicity.
2.2.2. ATG Proteins: Crucial for Autophagosome Formation
Autophagy-related (ATG) proteins are essential for the development and maturation of autophagosomes. ATG5, ATG7, ATG12, and ATG16L1 are pivotal in the processes of autophagic membrane elongation and autophagosome maturation [37]. ATG5 is essential for the initiation of autophagy and the creation of autophagosomes [38]. It creates a conjugate complex with ATG12 and ATG16L1, promoting membrane expansion. Research indicates that ATG5 can interact with apoptotic pathways, as cleaved ATG5 translocates to the mitochondria, facilitating the release of cytochrome and apoptosis [39]. ATG5's dual function in autophagy and apoptosis highlights its significance in determining whether autophagy leads to cell survival or autophagic cell death [40]. ATG7 operates as an E1-like enzyme essential for the lipidation of LC3, a critical process in autophagosome maturation [41]. The absence of ATG7 hinders autophagy and exacerbates metabolic stress, potentially affecting tumor advancement [42]. Conversely, persistent ATG7 expression in certain cancer types has been linked to autophagy-induced cell death, suggesting its potential as a therapeutic target.
2.2.3. LC3: An Indicator of Autophagosome Formation
Microtubule-associated protein 1A/1B-light chain 3 (LC3) is a well-established indicator of autophagosome development [43]. LC3 appears in two forms: LC3-I (cytosolic) and LC3-II (membrane-bound), with LC3-II integrated into autophagosomal membranes [44]. The transformation of LC3-I to LC3-II is crucial for the maturation of autophagosomes and the breakdown of cargo [45]. Within the framework of ADCD, LC3 plays a pivotal role in selective autophagy, facilitating the degradation of impaired organelles and protein aggregates. Elevated LC3-II levels are linked to augmented autophagic flux, perhaps facilitating cell death in response to chemotherapeutic drugs [46]. LC3 additionally engages with specific autophagy adaptors, such as p62/SQSTM1, thereby modulating the equilibrium between cellular survival and autophagic cell death [47].
2.2.4. p62/SQSTM1: A Mediator of Autophagy and Apoptosis Interference
p62/SQSTM1 is a specific autophagy receptor that promotes the degradation of ubiquitinated proteins through its interaction with LC3-II [8]. It serves as a conduit between autophagy and apoptosis, affecting cellular destiny under stress conditions. Under typical circumstances, p62 increases when autophagy is compromised, resulting in the accumulation of protein aggregates and oxidative damage [48]. In the context of ADCD, excessive autophagic degradation of p62 may induce apoptosis, as p62 plays a crucial role in regulating the nuclear factor-κB (NF-κB) pathway, which is essential for cell survival [49]. In cancer, p62 exhibits a dual function, acting as a tumor suppressor in certain settings and facilitating carcinogenesis in others [50]. Targeting p62-mediated autophagy regulation has become a promising approach for enhancing the sensitivity of cancer cells to therapy-induced ADCD.
2.2.5. mTOR and AMPK Signaling: Principal Regulators of Autophagy
Autophagy is regulated by two principal signaling pathways: the mammalian target of rapamycin (mTOR) pathway and the AMP-activated protein kinase (AMPK) pathway [51]. The mTOR pathway serves as a principal negative regulator of autophagy, suppressing ULK1 activity in nutrient-abundant environments [52]. In the presence of enough nutrition, mTORC1 phosphorylates ULK1, hence inhibiting the beginning of autophagy [53]. In cancer, mTOR hyperactivation inhibits autophagy, hence enhancing tumor cell viability [54]. Pharmacological inhibition of mTOR with rapamycin or other mTOR inhibitors can elicit ADCD, rendering it a viable therapeutic strategy [46]. The AMPK pathway functions as a metabolic sensor, initiating autophagy in response to energy deficiency. Following ATP depletion, AMPK phosphorylates ULK1 and inhibits mTORC1, thereby initiating autophagy by ADCD [55]. In cancer, AMPK activation can either enhance cell survival or trigger ADCD, contingent upon the cellular context and metabolic condition [56]. Rapamycin induces autophagy in osteosarcoma cells (SaOS-2, U-2OS), triggering ADCD [57]. Targeting AMPK to regulate autophagy is being investigated as a method to increase cancer cell vulnerability to therapy-induced autophagic death.
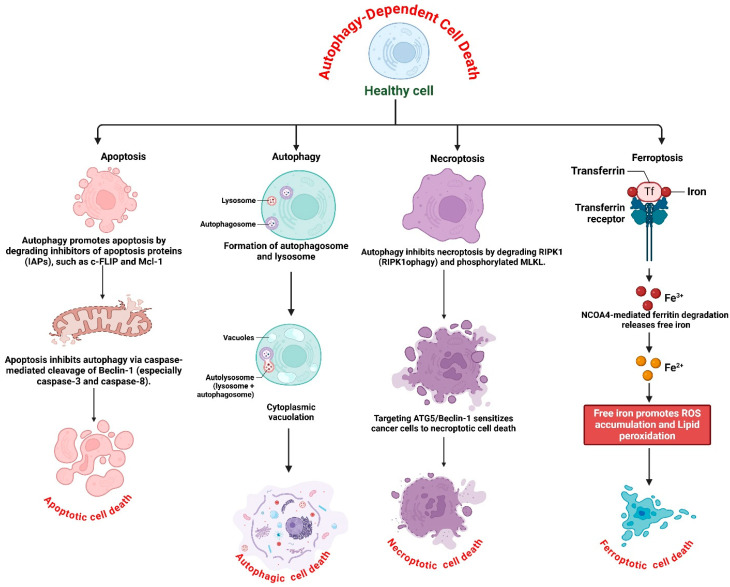
2.3. Crosstalk Between Autophagy-Dependent Cell Death and Other Cell Death Pathways
The interaction between ADCD and apoptosis, necroptosis, and ferroptosis influences cellular fate in various physiological and pathological contexts, including cancer. Understanding this interaction is crucial for developing modified therapeutic strategies that utilize autophagy modulation to enhance cancer treatment. The complex relationships between ADCD and three principal cell death pathways: apoptosis, necroptosis, and ferroptosis are presented in Figure 3.
Figure 3.
Interplay between autophagy-dependent cell death and other pathways. Modulating autophagy may serve as a potential therapeutic strategy in cancer treatment by influencing apoptosis, necroptosis, and ferroptosis. Autophagy modulates apoptosis by degrading anti-apoptotic proteins, including Mcl-1 and c-FLIP, hence enhancing apoptotic sensitivity. Conversely, apoptosis inhibits autophagy by caspase-3/8-mediated cleavage of Beclin-1, therefore favoring apoptotic cell death. Chemotherapeutic agents, such as doxorubicin and cisplatin, promote autophagy, thereby enhancing apoptosis in cancer treatment. Autophagy suppresses necroptosis by modulating RIPK1 (RIPK1ophagy) and phosphorylated MLKL, hence obstructing necroptotic execution. Autophagy inhibition leads to the accumulation of RIPK1, triggering necroptotic cell death. Targeting autophagy-related genes, such as ATG5 or Beclin-1, enhances the susceptibility of tumor cells to necroptosis. Ferritinophagy, facilitated by NCOA4, induces ferroptosis by liberating iron, enhancing ROS generation, and promoting lipid peroxidation. Inhibiting autophagy with chloroquine or bafilomycin A1 obstructs ferritinophagy, thereby averting ferroptosis. Conversely, ferroptosis inducers like erastin and RSL3 promote ferritinophagy, hence intensifying ferroptotic cell death. The figure was modified and created using the BioRender.com online commercial platform.
2.3.1. Autophagy and Apoptosis: A Dual Regulatory Mechanism
Apoptosis is a defined type of programmed cell death regulated by caspase activation, marked by DNA fragmentation, chromatin condensation, and membrane blebbing [58]. Autophagy and apoptosis are frequently interrelated, as autophagy may operate independently or modulate apoptosis via several molecular processes [59]. A critical element of this interaction is the degradation of anti-apoptotic proteins via autophagy. Autophagy can promote apoptosis by degrading inhibitors of apoptosis proteins (IAPs), including c-FLIP and Mcl-1, which impede apoptotic signals [60]. The depletion of these proteins may render cells more susceptible to apoptosis, hence increasing cell death in response to chemotherapeutic drugs. Conversely, apoptosis can inhibit autophagy by cleaving critical autophagy-related proteins. Caspases, particularly caspase-3 and caspase-8, have been shown to cleave Beclin-1, thereby inhibiting autophagy and directing the cell towards apoptosis [16]. This reciprocal regulation suggests that, whereas autophagy may delay apoptosis under specific conditions, excessive or prolonged autophagy may ultimately lead to apoptosis-dependent cell death [61]. In cancer treatment, the induction of autophagy alongside the targeting of apoptotic pathways has surfaced as a promising technique to augment tumor cell mortality [62]. Chemotherapeutic agents such as doxorubicin and cisplatin have been shown to induce autophagy, which, when combined with apoptosis-inducing medications, leads to increased cancer cell mortality [63]. Nonetheless, the result is significantly contingent on context, as autophagy may function as a survival strategy by destroying pro-apoptotic proteins.
2.3.2. Autophagy and Necroptosis: A Complex Interplay
Necroptosis is a type of controlled necrosis facilitated by receptor-interacting protein kinases (RIPK1 and RIPK3) and the mixed lineage kinase domain-like protein (MLKL) [64]. In contrast to apoptosis, necroptosis does not engage caspase activation and is frequently initiated by tumor necrosis factor-alpha (TNF-α) signaling in caspase-deficient environments [65]. Autophagy has been linked to the regulation of necroptosis through various pathways [66]. A key connection between these two processes is the role of autophagy in regulating the activity of RIPK1 and RIPK3. Research indicates that autophagy can selectively destroy RIPK1 through RIPK1ophagy, thereby inhibiting necroptosis and enhancing cell survival [67]. Conversely, the suppression of autophagy may result in the buildup of RIPK1, hence initiating necroptotic cell death. Furthermore, autophagy can modulate MLKL, the ultimate effector of necroptosis [68]. Following necroptotic stimulation, MLKL is phosphorylated and relocates to the plasma membrane, resulting in membrane rupture and cellular demise [69]. Autophagy has been shown to regulate MLKL activation by preferentially degrading phosphorylated MLKL, hence affecting the magnitude of necroptotic signaling [68]. The interplay between autophagy and necroptosis is particularly significant in cancer, as numerous tumor cells develop resistance to apoptosis due to alterations in key apoptotic genes [70]. In these instances, generating necroptosis via autophagy suppression may offer an alternate approach to elicit tumor cell death. Numerous studies have demonstrated that targeting autophagy-related proteins, such as ATG5 or Beclin-1, can increase the susceptibility of cancer cells to necroptotic death, highlighting the therapeutic potential of this interaction.
2.3.3. Autophagy and Ferroptosis: The Role of Ferritinophagy
Ferroptosis is a unique type of iron-dependent cellular demise characterized by the accumulation of lipid peroxides and oxidative stress [71]. In contrast to apoptosis and necroptosis, ferroptosis is predominantly governed by iron metabolism, lipid peroxidation, and antioxidant defense systems [72]. Ferritinophagy, a selective autophagic process that degrades ferritin, the iron-storage protein, provides a crucial connection between autophagy and ferroptosis [73]. Ferritinophagy is facilitated by nuclear receptor coactivator 4 (NCOA4), which promotes the autophagic breakdown of ferritin, resulting in the liberation of free iron [74]. The elevation of free iron concentrations amplifies the generation of reactive oxygen species (ROS) via the Fenton reaction, consequently facilitating lipid peroxidation and ferroptotic cell death [75]. The interaction between autophagy and ferroptosis in cancer has garnered interest as a potential treatment strategy [76]. Specific tumor cells demonstrate resistance to ferroptosis by enhancing antioxidant mechanisms, including glutathione peroxidase 4 (GPX4), to counteract lipid peroxides [76]. Nonetheless, the modification of autophagy can disrupt this equilibrium by enhancing ferritinophagy, consequently elevating iron availability and rendering cells more susceptible to ferroptosis [74]. Furthermore, specific autophagy inhibitors, such as chloroquine and bafilomycin A1, have demonstrated the capacity to block ferritinophagy, thereby reducing free iron concentrations and preventing ferroptosis [77]. In contrast, ferroptosis inducers such as erastin and RSL3 can promote autophagy-mediated degradation of ferritin, thereby intensifying ferroptotic cell death [78]. This suggests that targeting ferritinophagy in conjunction with ferroptosis inducers may be a practical approach to eliminate cancer cells.
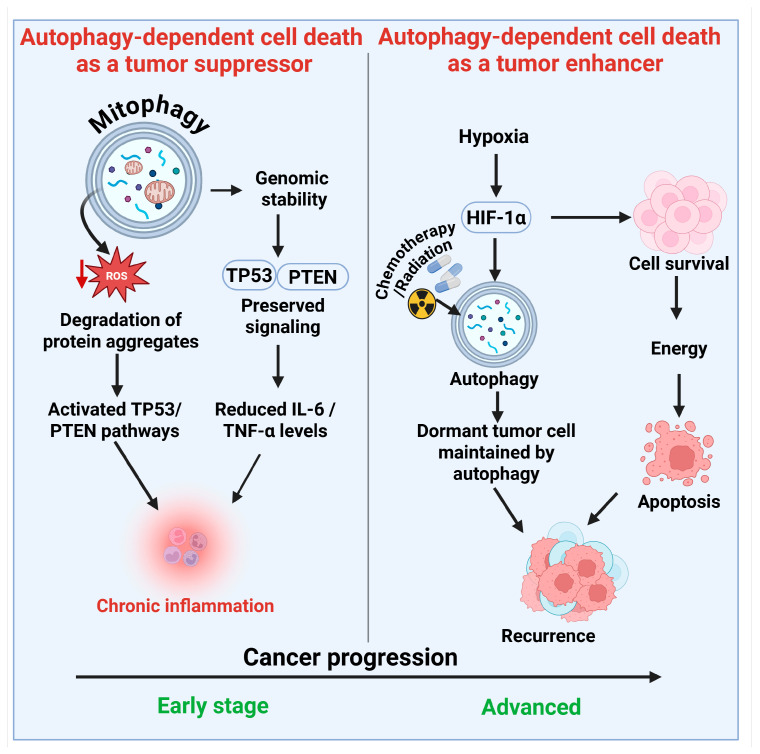
3. Role of Autophagy-Dependent Cell Death in Cancer Therapy
3.1. Dual Role of Autophagy-Dependent Cell Death in Cancer
Autophagy-dependent cell death (ADCD) plays a dual role in cancer therapy, acting both as a tumor suppressor and a cell survival mechanism. It can either promote or inhibit cancer cell death, depending on the context and specific cellular conditions (Figure 4).
Figure 4.
The dual role of autophagy-dependent cell death in cancer progression and therapy resistance. (Left Panel) (Tumor Suppressor Role): In the initial stages of cancer development, autophagy facilitates the removal of damaged organelles through mitophagy, decreases reactive oxygen species (ROS), and preserves genomic stability. It promotes the degradation of misfolded protein aggregates, activates tumor suppressor pathways (TP53 and PTEN), and suppresses chronic inflammation by reducing pro-inflammatory cytokines (IL-6, TNF-α), thereby inhibiting malignant transformation. (Right Panel) The right panel illustrates the role of autophagy as a tumor enhancer in advanced cancer, facilitating tumor cell survival during stress conditions such as hypoxia and nutrient deprivation, primarily through HIF-1α signaling. It improves resistance to chemotherapy and radiation by maintaining cellular integrity and inhibiting apoptosis. Autophagy sustains quiescent tumor cells in a dormant state, thereby facilitating recurrence after treatment. The shift in autophagy from a suppressive to a promotive role takes place throughout the cancer progression timeline, underscoring its complexity as a therapeutic target. The figure was modified and created using the BioRender.com online commercial platform.
3.1.1. Autophagy-Dependent Cell Death Functions as a Tumor Suppressor
Autophagy-dependent cell death may function as a tumor suppressor. Although autophagy may facilitate the survival of cancer cells, its role in removing damaged cells and maintaining genomic stability during the initial phases of carcinogenesis is crucial for preventing tumor progression [79].
Preservation of Cellular Homeostasis and Genomic Integrity
Autophagy serves as a quality control system, mitigating cellular stress that can lead to cancer development. It eliminates malfunctioning mitochondria by mitophagy, hence decreasing excessive ROS generation, which is recognized to induce DNA damage and genetic alterations [80]. The removal of impaired organelles reduces the likelihood of cellular transformation and tumorigenesis.
Regulation of Oncogenes and Tumor Suppressor Genes
Autophagy engages with essential tumor suppressor pathways, including the TP53 (p53) and PTEN signaling pathways, which are vital for inhibiting unregulated cell proliferation [81]. The absence of critical autophagy regulators, such as Beclin-1 (ATG6) and ATG5, has been linked to heightened vulnerability to tumorigenesis in multiple malignancies, including breast and ovarian cancers [82]. Furthermore, autophagy inhibits the accumulation of aberrant protein aggregates, which can disrupt cellular signaling pathways and promote oncogenesis. Autophagy serves as a preventive mechanism against malignant transformation by preserving cellular integrity.
Mitigation of Chronic Inflammation
Chronic inflammation is a recognized contributor to tumor genesis and progression. Dysfunctional autophagy is associated with heightened inflammatory signaling, fostering a pro-tumorigenic microenvironment. The targeted degradation of inflammasomes through autophagy mitigates excessive inflammatory responses, consequently diminishing the probability of tumor initiation [83]. Research indicates that the depletion of ATGs results in heightened release of pro-inflammatory cytokines, including interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), fostering a milieu favorable for tumorigenesis [84]. Consequently, autophagy helps mitigate carcinogenesis associated with chronic inflammation.
3.1.2. Autophagy-Dependent Cell Death as a Tumor Enhancer
Autophagy inhibits cancer initiation, but in established tumors, it facilitates tumor progression and therapeutic resistance. Cancer cells utilize autophagy to acclimate to adverse environments, such as hypoxia, nutritional scarcity, and chemotherapeutic duress [85].
Metabolic Adaptation and Resistance Under Stress
Autophagy primarily facilitates tumor growth by enhancing the survival of cancer cells during metabolic stress [86]. Within the microenvironment of a tumor, cancer cells frequently encounter nutritional scarcity and hypoxia resulting from insufficient blood flow [87]. Autophagy enables these cells to recycle intracellular constituents for energy production and to sustain survival. In hypoxic situations, hypoxia-inducible factor 1-alpha (HIF-1α) stimulates autophagy to supply an alternate energy source [88]. This metabolic adaptability enables cancer cells to survive and proliferate in environments that would otherwise be lethal. Furthermore, autophagy helps tumor cells mitigate oxidative stress by removing damaged mitochondria and reducing elevated levels of ROS [89]. This protective process enhances tumor cell viability and promotes resistance to various therapies.
Role in Therapy Resistance
Autophagy plays a crucial role in facilitating resistance to chemotherapy and radiation therapy. Numerous anticancer therapies function by eliciting cellular stress and facilitating apoptotic cell death [90]. Cancer cells can induce autophagy as a survival strategy, mitigating the damaging effects of these treatments. Cancer cells subjected to chemotherapy drugs including cisplatin, doxorubicin, and temozolomide, frequently demonstrate heightened autophagy activity [91]. This facilitates the degradation of impaired organelles and sustains cellular activity, hence diminishing the efficacy of chemotherapy. Radiation therapy causes DNA damage and oxidative stress in neoplastic cells [92]. Autophagy alleviates this damage by eliminating impaired organelles and facilitating cellular repair, hence enhancing tumor cells' resistance to radiation-induced apoptosis [93]. In tumors subjected to targeted therapy, such as tyrosine kinase inhibitors (e.g., erlotinib, imatinib), autophagy is frequently elevated as a compensatory mechanism to maintain tumor cell viability [94]. Autophagy inhibition has been proposed as a method to enhance the efficacy of targeted medications.
Role in Tumor Dormancy and Recurrence
Autophagy contributes to tumor dormancy and recurrence [95]. Specific cancer cells enter a latent state, characterized by a quiescent phase with diminished metabolic activity. This enables them to circumvent immune surveillance and withstand conventional therapy. Autophagy sustains these quiescent cells by preserving modest energy demands and inhibiting apoptosis. After therapy, dormant cells may reawaken and lead to the recurrence of cancers. This highlights the need for therapeutic approaches that focus on autophagy to prevent tumor recurrence.
3.2. Therapeutic Targeting of Autophagy in Cancer
Due to its dual nature, researchers have explored various techniques to regulate autophagy for therapeutic purposes. Inhibiting autophagy may enhance the efficacy of specific cancer therapies, while activating ADCD can also serve as a method to eliminate cancer cells. This section examines the principal strategies for modulating autophagy in cancer treatment, encompassing both the suppression and activation of autophagy.
3.2.1. Autophagy Inhibition in Cancer Therapy
Chloroquine (CQ) and Hydroxychloroquine (HCQ): Inhibiting Autophagosome-Lysosome Fusion
Chloroquine (CQ) and its derivative, hydroxychloroquine (HCQ), are extensively researched autophagy inhibitors that operate by obstructing the fusion of autophagosomes with lysosomes [96]. These pharmaceuticals elevate the pH of lysosomes, thereby hindering their degradative capabilities and leading to the accumulation of defective organelles and misfolded proteins [97]. CQ and HCQ have been examined in numerous preclinical and clinical trials for their potential to augment the effectiveness of standard cancer treatments [98]. In glioblastoma, pancreatic cancer, and melanoma, CQ/HCQ has demonstrated the ability to enhance chemotherapy efficacy by inhibiting cancer cells from utilizing autophagy as a survival strategy [99]. CQ has been shown to inhibit tumor angiogenesis and metastasis, positioning it as a promising candidate for combination therapy [100]. The efficacy of CQ and HCQ varies among different cancer types, necessitating further research to enhance their therapeutic applications. CQ and its analog hydroxychloroquine, inhibit lysosomal acidification, blocking autophagic flux and causing autophagosome accumulation. While often cytoprotective, in some contexts, this overload triggers ADCD or apoptosis. In liposarcoma cells, CQ, paired with rapamycin, caused extensive apoptosis via increased autophagosomes via the ADCD pathway [100].
mTOR Inhibitors: Inhibiting Autophagy Activation in Cancers
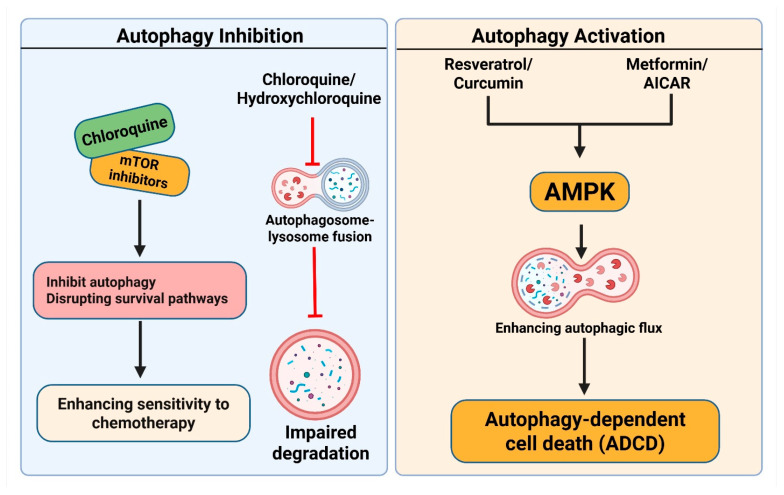
The mechanistic target of rapamycin (mTOR) serves as a primary regulator of autophagy [101]. The activation of mTOR inhibits autophagy, while the inhibition of mTOR increases it [102]. In certain tumors, paradoxically, overactive mTOR signaling inhibits autophagy and facilitates tumor proliferation [103]. In certain instances, cancer cells depend on autophagy for survival in stressful environments. mTOR inhibitors, including rapamycin and its analogs (temsirolimus and everolimus), have been studied for their ability to inhibit autophagy-mediated tumor growth [104]. mTOR inhibitors typically serve as autophagy inducers, although they may also work as indirect inhibitors when used in conjunction with other autophagy-inhibiting drugs. For instance, the concurrent suppression of mTOR and autophagy with a combination of rapamycin and CQ has demonstrated potential in preclinical investigations [105]. This method efficiently inhibits cancer cells from transitioning to an autophagy-dependent survival mechanism after mTOR inhibition (Figure 5).
Figure 5.
Pharmacological modulation of Autophagy-dependent cell death in cancer therapy. (Left panel): Autophagy Inhibition: Chloroquine (CQ) and hydroxychloroquine (HCQ) inhibit the fusion of autophagosomes and lysosomes by increasing lysosomal pH, resulting in compromised degradation of cellular components. mTOR inhibitors have been demonstrated to indirectly inhibit autophagy or act in conjunction with CQ, thereby disrupting survival pathways and enhancing sensitivity to chemotherapy. (Right panel): Autophagy Activation: Resveratrol, curcumin, metformin, and AICAR stimulate the AMPK signaling pathway, enhancing autophagic flux. This results in ADCD, which is especially advantageous in apoptosis-resistant cancer cells. The activation of AMPK through metabolic stress or pharmacological agents facilitates the formation of autophagosomes and the degradation of oncogenic proteins. The figure was modified and created using the BioRender.com online commercial platform.
3.2.2. Activation of Autophagy in Cancer Treatment
Although autophagy inhibition is advantageous in particular cancer types, the activation of autophagy may also serve as a practical approach to cause ADCD. This method is especially beneficial in apoptosis-resistant tumors, where autophagy may function as an alternate mechanism of cell killing. A variety of natural substances and pharmaceutical treatments have been examined for their capacity to enhance ADCD in cancer cells.
Resveratrol and Curcumin: Facilitating ADCD to Augment Apoptosis in Cancer Cells
Natural substances, such as resveratrol and curcumin, have been extensively researched for their anticancer properties, particularly their ability to regulate autophagy [106]. A polyphenolic compound present in grapes and red wine, resveratrol stimulates autophagy by blocking mTOR and activating the AMP-activated protein kinase (AMPK) pathway [107]. It has been demonstrated to elicit ADCD in multiple cancer cell lines, including those of breast, prostate, and colon cancers. Resveratrol additionally amplifies the cytotoxic effects of chemotherapy by facilitating autophagy-mediated degradation of anti-apoptotic proteins [108]. Extracted from turmeric, curcumin is a potent autophagy inducer with many anticancer properties [109]. It facilitates ADCD by augmenting autophagic flux and obstructing critical survival pathways in neoplastic cells. Research indicates that curcumin enhances the sensitivity of cancer cells to chemotherapy and radiotherapy by stimulating the ADCD pathway, while diminishing inflammation and oxidative stress [110]. Additionally, curcumin can induce non-apoptotic/autophagy-dependent death. In renal carcinoma, co-treatment with PP242 (mTORC1/2 inhibitor) and curcumin caused apoptosis and ADCD via lysosomal damage, which was suppressed by autophagy inhibitors [111]. Resveratrol and curcumin have been evaluated in combination with conventional medicines to enhance their anticancer effectiveness [112]. Nonetheless, their bioavailability poses a challenge, necessitating further research to improve their therapeutic applicability.
AMPK Activators: Augmenting Autophagic Flux to Induce Cytotoxicity in Cancer
AMPK is a crucial energy sensor that modulates cellular metabolism and autophagy. Activation of AMPK enhances autophagic flux and causes ADCD, positioning it as a potential target for cancer treatment [113]. A variety of pharmacological substances and metabolic stresses can stimulate AMPK activation [114]. A commonly utilized antidiabetic medication, metformin stimulates AMPK and promotes autophagy in neoplastic cells [115]. Preclinical chloroquine studies suggest that metformin-induced autophagy activation may enhance ADCD in certain cancer types, particularly those with metabolic vulnerabilities [116]. In H4IIE cells under glucose deprivation, metformin suppressed autophagy and triggered apoptosis through AMPK pathways by ADCD. In osteosarcoma, metformin was linked to reduced metastasis by affecting autophagy-related mechanisms in ADCD [117]. As a direct activator of AMPK, AICAR (5-Aminoimidazole-4-carboxamide ribonucleotide) has demonstrated the ability to induce autophagy and inhibit tumor growth in experimental animals [118]. AICAR increases cancer cell death by augmenting the autophagic breakdown of oncogenic proteins [119]. Lifestyle modifications, including exercise and intermittent fasting, have been shown to activate AMPK and autophagy, thereby enhancing their potential anticancer properties [120]. Although these techniques are not independent medicines, they may improve current treatment strategies by altering tumor metabolism.
3.3. Combination Strategies for Enhancing Cancer Therapy
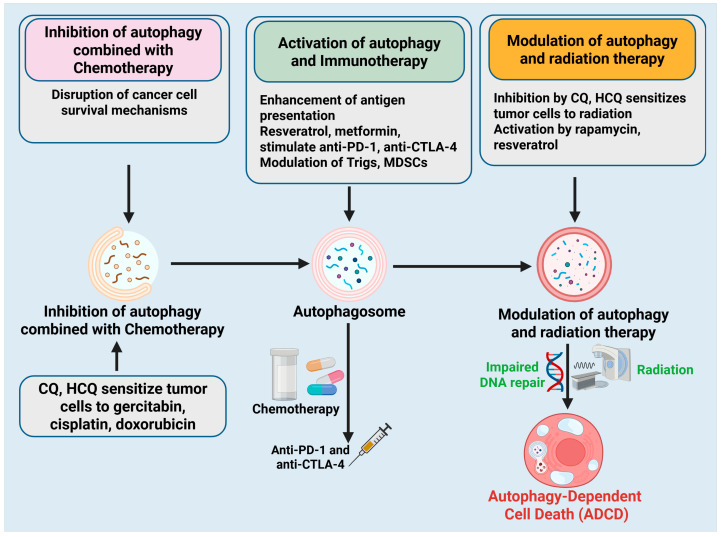
This complexity has prompted the investigation of combinatorial techniques that incorporate autophagy modulation with standard cancer therapies, including chemotherapy, immunotherapy, and radiation therapy. Researchers seek to enhance therapeutic efficacy and defeat drug resistance by modulating autophagy, either through inhibition or activation, in a context-dependent manner. This section examines essential combinatorial strategies that utilize autophagy modulation to improve cancer therapy (Figure 6).
Figure 6.
Combination strategies using Autophagy-dependent cell death modulation in cancer therapy. Three principal combinatorial techniques that employ autophagy manipulation to improve cancer treatment efficacy. (Left panel): Autophagy inhibition in conjunction with chemotherapy. Treatments like CQ and HCQ interfere with autophagy-dependent survival mechanisms in cancer cells, rendering them more susceptible to chemotherapeutic treatments such as gemcitabine, cisplatin, and doxorubicin. (Middle panel): The activation of autophagy augments immunotherapy. Autophagy inducers (e.g., resveratrol, metformin) enhance antigen presentation and immune cell activation, hence augmenting the efficacy of immune checkpoint inhibitors such as anti-PD-1 and anti-CTLA-4. Autophagy reprograms immunosuppressive cells, such as Tregs and MDSCs, into pro-inflammatory phenotypes. (Right panel): Regulation of autophagy in conjunction with radiation therapy. CQ and HCQ augment radiosensitivity by disrupting DNA repair processes, whereas compounds such as rapamycin and resveratrol may facilitate ADCD, hence amplifying the harmful effects of radiation. The figure was modified and created using the BioRender.com online commercial platform.
3.3.1. Inhibition of Autophagy Combined with Chemotherapy: Disrupting Mechanisms of Cancer Cell Survival
Chemotherapy is a fundamental component of cancer treatment; its efficacy is frequently constrained by drug resistance. Inhibiting autophagy has become a viable strategy to augment chemotherapy effectiveness by obstructing cancer cells from utilizing autophagy as a survival mechanism [121]. Numerous chemotherapeutic drugs elicit metabolic stress and DNA damage, activating protective autophagy in tumor cells [122]. This reaction enables cancer cells to evade apoptosis, resulting in therapy failure. Inhibitors like CQ and HCQ impede autophagy, hence undermining this survival mechanism and rendering cancer cells more vulnerable to chemotherapy-induced apoptosis [123]. In pancreatic cancer, CQ has demonstrated the ability to augment the effectiveness of gemcitabine, a conventional chemotherapy agent [124]. In breast and lung malignancies, the suppression of autophagy enhances the cytotoxic efficacy of cisplatin and doxorubicin [125]. These findings support the use of autophagy inhibitors in combination with chemotherapy to mitigate drug resistance and improve patient outcomes.
3.3.2. Activation of Autophagy and Immunotherapy: Augmenting Immune-Mediated Tumor Elimination
Immunotherapy has transformed cancer treatment by utilizing the body's immune system to identify and eliminate cancerous cells [126]. Nonetheless, immune evasion continues to pose a considerable obstacle, hindering the efficacy of checkpoint inhibitors, adoptive T-cell therapy, and cancer vaccines. Recent studies suggest that activating autophagy can enhance the efficacy of immunotherapy by facilitating antigen presentation and stimulating immune cell activation [127]. Autophagy improves tumor detection by cytotoxic T lymphocytes by augmenting the degradation of tumor-associated antigens and their presentation on major histocompatibility complex (MHC) molecules [128]. Furthermore, autophagy modulates the function of immune cells, encompassing the viability and activity of dendritic cells, macrophages, and natural killer (NK) cells [129]. Autophagy inducers, such as resveratrol and metformin, have demonstrated the ability to enhance the efficacy of immune checkpoint inhibitors (e.g., anti-PD-1, anti-CTLA-4) in models of melanoma and lung cancer [130]. Moreover, in solid tumors characterized by an immunosuppressive microenvironment, the activation of autophagy can facilitate the reprogramming of immune-suppressive cells, including regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs), into pro-inflammatory phenotypes [131]. This method increases immune-mediated tumor eradication and amplifies the enduring advantages of immunotherapy.
3.3.3. Modulation of Autophagy and Radiation Therapy: Enhancing Therapeutic Efficacy in Resistant Tumors
Radiation therapy is a prevalent treatment for several cancers, yet radioresistance continues to be a significant challenge. Modulating autophagy has emerged to increase the sensitivity of tumor cells to radiation. Radiation causes DNA damage and oxidative stress, prompting the activation of autophagy as a defensive mechanism. Inhibition of autophagy by CQ or HCQ has been demonstrated to augment radiosensitivity in glioblastoma, prostate cancer, and cervical cancer by obstructing DNA repair and promoting tumor cell mortality [132]. Conversely, in certain instances, the activation of autophagy may enhance radiation efficacy by facilitating ADCD. Autophagy inducers, such as rapamycin and resveratrol, have demonstrated an enhancement of radiation-induced cytotoxicity in particular cancer types, including colorectal and lung malignancies [133]. The context-specific function of autophagy in radiation therapy highlights the need for personalized treatment strategies based on tumor classification and autophagy status.
4. Therapeutic and Clinical Application of Autophagy-Dependent Cell Death in Cancer Therapy
As our knowledge of ADCD advances, researchers and clinicians are intensively investigating its practical uses to enhance patient outcomes. ADCD is essential in regulating cellular survival and apoptosis, rendering it a significant target for therapeutic strategies. In contrast to apoptosis, which genetic changes can circumvent, ADCD offers an alternate strategy for tumor eradication. Therapies aimed at activating ADCD can provoke autophagic stress in cancer cells, resulting in their self-destruction. Table 1 outlines several autophagy-modulating pharmaceuticals with therapeutic potential in cancer treatment, either by activating or suppressing autophagy to facilitate ADCD. These pharmaceuticals are being investigated in preclinical and clinical settings to enhance cancer treatment efficacy. In cancers where autophagy facilitates survival and therapeutic resistance, inhibiting autophagy is a feasible approach to improve treatment effectiveness. Conversely, stimulating autophagy may serve as an advantageous approach in tumors where autophagy-mediated cell death facilitates tumor reduction. Various substances efficiently induce ADCD via distinct pathways.
Table 1.
Pharmaceutical agents that modulate ADCD, their methods of action, and their clinical applications in cancer treatment.
| Drug Name | Cancer Type | Mechanism of Action | ADCD | Ref. |
|---|---|---|---|---|
| Chloroquine (CQ) | Glioblastoma, Breast Cancer | Inhibits autophagosome-lysosome fusion, preventing degradation of cellular components | Inhibition | [134] |
| Hydroxychloroquine (HCQ) | Pancreatic Cancer, Lung Cancer | Blocks lysosomal acidification, disrupting autophagic flux | Inhibition | [135] |
| Bafilomycin A1 | Liver Cancer, Leukemia | Inhibits lysosomal acidification, blocking autophagosome clearance | Inhibition | [136] |
| 3-Methyladenine (3-MA) | Colorectal Cancer, Lung Cancer | Blocks PI3K-mediated autophagy initiation | Inhibition | [137] |
| Rapamycin | Renal Cell Carcinoma, Breast Cancer | mTORC1 inhibitor, induces autophagy leading to ADCD | Activation | [138] |
| Everolimus | Neuroendocrine Tumors, Breast Cancer | mTORC1 inhibitor, enhances autophagic cell death in tumors | Activation | [139] |
| Temsirolimus | Renal Cell Carcinoma, Lymphoma | mTORC1 inhibition promotes sustained autophagy and tumor regression | Activation | [140] |
| Resveratrol | Colon Cancer, Melanoma | Induces oxidative stress and autophagic cell death via AMPK activation | Activation | [141] |
| Curcumin | Lung Cancer, Pancreatic Cancer | Triggers autophagy through Beclin-1 upregulation, enhancing ADCD | Activation | [142] |
| Metformin | Prostate Cancer, Ovarian Cancer | Activates AMPK, inhibits mTOR signaling, promoting autophagic cell death | Activation | [143] |
| Sunitinib | Renal Cell Carcinoma, Gastrointestinal Stromal Tumors | Induces autophagy-dependent cell death through mTORC1 inhibition | Activation | [144] |
| Doxorubicin | Breast Cancer, Osteosarcoma | Enhances autophagy-dependent apoptosis via ROS generation | Activation | [145] |
| Cisplatin | Ovarian Cancer, Bladder Cancer | Induces ER stress-mediated autophagic cell death | Activation | [146] |
| Vinblastine | Lymphoma, Breast Cancer | Disrupt microtubules, triggering autophagic stress and ADCD | Activation | [147] |
| Carbamazepine | Glioblastoma, Pancreatic Cancer | Enhances autophagic flux and degradation of damaged proteins | Activation | [148] |
Chloroquine (CQ) and Hydroxychloroquine (HCQ) are frequently utilized for the treatment of malaria and autoimmune diseases, but they have also been repurposed for cancer treatments. They operate by obstructing the union of autophagosomes and lysosomes, therefore averting the breakdown of impaired proteins and organelles. CQ and HCQ have demonstrated potential in glioblastoma, breast, pancreatic, and lung malignancies by augmenting sensitivity to chemotherapy and radiation [134,135]. Bafilomycin A1 is a potent lysosomal inhibitor that obstructs lysosomal acidification, thereby hindering autophagic flow. It has demonstrated efficacy in liver cancer and leukemia, wherein the inhibition of autophagy results in the accumulation of toxic waste within cancer cells, ultimately leading to cell death [136]. 3-Methyladenine (3-MA)-A is a recognized PI3K inhibitor. 3-MA obstructs the onset of autophagy, rendering it a valuable approach in the treatment of colorectal and lung cancer. 3-MA amplifies the cytotoxic effects of chemotherapeutic drugs by diminishing autophagic activity [137]. Rapamycin, Everolimus, and Temsirolimus are mTOR inhibitors that induce autophagy by inhibiting mTORC1, a key regulator of cellular growth and survival. Rapamycin has shown effectiveness in renal cell carcinoma and breast cancer [138], but everolimus is sanctioned for the treatment of neuroendocrine tumors [139]. Temsirolimus has been investigated in lymphomas, where it increases tumor susceptibility to chemotherapeutic therapies [140]. Resveratrol and Curcumin, being natural substances, facilitate autophagy by causing oxidative stress and activating Beclin-1, a crucial regulator of autophagy. Resveratrol has demonstrated efficacy in colon cancer and melanoma [141], whilst curcumin has exhibited potential in lung and pancreatic malignancies [142]. Metformin, widely used for diabetes control, activates AMPK, which in turn inhibits mTOR, thereby facilitating autophagy and ADCD. Research indicates its possible application in prostate and ovarian malignancies, where it amplifies the efficacy of chemotherapy [143]. Sunitinib, a multi-kinase inhibitor, promotes autophagy-dependent cell death via mTORC1 inhibition, rendering it an effective therapy for renal cell carcinoma and gastrointestinal stromal tumors [144]. Doxorubicin is a chemotherapeutic agent. Doxorubicin, a prominent chemotherapeutic agent, promotes autophagy-dependent apoptosis through ROS production, rendering it effective against breast cancer and osteosarcoma [145]. Cisplatin, a prevalent chemotherapy drug, produces autophagic cell death mediated by endoplasmic reticulum stress, rendering it effective against ovarian and bladder malignancies [146]. Vinblastine, a chemotherapeutic agent, interferes with microtubules, resulting in autophagic stress and ADCD, especially in lymphoma and breast cancer [147]. Carbamazepine, initially developed as an anticonvulsant, Carbamazepine has demonstrated the ability to augment autophagic flux and the breakdown of damaged proteins, positioning it as a possible treatment candidate for glioblastoma and pancreatic cancer [148].
5. Limitations and Future Directions of Autophagy-Dependent Cell Death in Cancer Therapy
Although ADCD holds promise in cancer treatment, several obstacles and limitations must be addressed to enhance its clinical implementation. By overcoming these challenges, autophagy-targeted therapies have the potential to transform cancer treatment, thereby improving patient outcomes and reducing therapeutic resistance. During early carcinogenesis, autophagy mitigates genomic instability, whereas in advanced malignancies, it facilitates survival in the face of metabolic stress. Cancer cells within a singular tumor demonstrate varied responses to autophagy regulation. Specific cells may experience ADCD, whereas others may acquire resistance, resulting in variable treatment results. Numerous autophagy-targeting pharmaceuticals, including CQ, HCQ, and rapamycin, have off-target effects that disrupt normal cellular homeostasis and induce detrimental side effects [5]. Extended regulation of autophagy may induce adaptive resistance in cancer cells, diminishing therapeutic effectiveness over time. This requires the formulation of combination medicines to maintain enduring advantages. Identifying precise biomarkers for autophagy activity in cancers will facilitate the development of targeted treatment techniques, thereby enhancing drug selection for patients. The integration of autophagy modulators with chemotherapy, immunotherapy, or radiation therapy may augment efficacy and surmount drug resistance [125]. For instance, the suppression of autophagy might augment chemotherapy-induced apoptosis, whilst the activation of autophagy can promote immunological responses [15]. Future research should concentrate on the development of targeted autophagy modulators that reduce off-target effects and specifically target neoplastic tissues. Translational research and the addition of clinical trials are required to evaluate the long-term advantages and safety of autophagy-based therapy for various types of cancer.
Defining and displaying Autophagy-Dependent Cell Death (ADCD) in cancer models is challenging because of its dual role in determining cell fate. Autophagy frequently fulfills a cytoprotective role, allowing cancer cells to deal with stressors such as chemotherapy and hypoxia. Determining ADCD requires unequivocal evidence that the autophagy machinery is not only active but also crucial for the execution of cell death, independent of apoptosis or necrosis. This distinction is contentious, as many studies indicate that autophagy enhances survival rather than induces mortality. Furthermore, pharmacological and genetic instruments exhibit a lack of selectivity, complicating the differentiation between autophagy-dependent effects and off-target toxicity or interactions with alternative cell death pathways.
6. Conclusions
Autophagy-Dependent Cell Death (ADCD) is a significant and complex domain in cancer treatment, providing the possibility of eradicating tumor cells by the regulated initiation of self-digestive processes. In contrast to conventional apoptosis-targeted therapies, ADCD utilizes a fundamentally different cellular pathway, providing an alternate method for eradicating resistant cancer morphologies. Nonetheless, its utilization is constrained by an inadequate comprehension of the conditions under which autophagy transitions from a survival process to a fatal one. A significant barrier exists in accurately differentiating ADCD from cytoprotective autophagy and other modalities of cell death, both in terms of mechanisms and experimental approaches. Furthermore, the influence of tumor-specific contexts, such as microenvironmental stress, genetic alterations, and metabolic state-introduces further complexity to the targeting of autophagy for therapeutic benefit. Going forward, a comprehensive strategy that integrates molecular profiling, real-time autophagic flux monitoring, and targeted genetic or pharmacological manipulation will be essential. Identifying predictive biomarkers that indicate the functional involvement of autophagy in a certain tumor could facilitate patient classification and customized treatment. Ultimately, although ADCD presents potential as a revolutionary approach in oncology, its clinical use relies on a comprehensive molecular understanding, context-specific validation, and meticulous therapy design to minimize off-target effects and enhance efficacy. Subsequent studies must address these deficiencies to realize their medicinal potential fully.
Author Contributions
M.A.R. writing—original draft, editing and modifying draft preparation, and preparing figures. M.A.-Z. and E.H.A. writing—editing and reviewing, and visualization. M.J. and A.H.H. conceptualization, writing—editing and reviewing, visualization, and funding acquisition. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This work was supported and funded by the Deanship of Scientific Research at Imam Mohammad Ibn Saud Islamic University (IMSIU) (grant number IMSIU-DDRSP2501).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Tobore T.O. On the need for the development of a cancer early detection, diagnostic, prognosis, and treatment response system. Future Sci. OA. 2020;6:FSO439. doi: 10.2144/fsoa-2019-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaur R., Bhardwaj A., Gupta S. Cancer treatment therapies: Traditional to modern approaches to combat cancers. Mol. Biol. Rep. 2023;50:9663–9676. doi: 10.1007/s11033-023-08809-3. [DOI] [PubMed] [Google Scholar]
- 3.Gu Y., Yang R., Zhang Y., Guo M., Takehiro K., Zhan M., Yang L., Wang H. Molecular mechanisms and therapeutic strategies in overcoming chemotherapy resistance in cancer. Mol. Biomed. 2025;6:2. doi: 10.1186/s43556-024-00239-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bialik S., Dasari S.K., Kimchi A. Autophagy-dependent cell death–where, how and why a cell eats itself to death. J. Cell Sci. 2018;131:jcs215152. doi: 10.1242/jcs.215152. [DOI] [PubMed] [Google Scholar]
- 5.Rahman M.A., Saikat A.S.M., Rahman M.S., Islam M., Parvez M.A.K., Kim B. Recent update and drug target in molecular and pharmacological insights into autophagy modulation in cancer treatment and future progress. Cells. 2023;12:458. doi: 10.3390/cells12030458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rahman M.A., Rhim H. Therapeutic implication of autophagy in neurodegenerative diseases. BMB Rep. 2017;50:345–354. doi: 10.5483/BMBRep.2017.50.7.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jalali P., Shahmoradi A., Samii A., Mazloomnejad R., Hatamnejad M.R., Saeed A., Namdar A., Salehi Z. The role of autophagy in cancer: From molecular mechanism to therapeutic window. Front. Immunol. 2025;16:1528230. doi: 10.3389/fimmu.2025.1528230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang Q., Tang K., Markby G.R., Parys M., Phadwal K., MacRae V.E., Corcoran B.M. Autophagy regulates cellular senescence by mediating the degradation of CDKN1A/p21 and CDKN2A/p16 through SQSTM1/p62-mediated selective autophagy in myxomatous mitral valve degeneration. Autophagy. 2025;21:1433–1455. doi: 10.1080/15548627.2025.2469315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coutts A.S., La Thangue N.B. Regulation of actin nucleation and autophagosome formation. Cell. Mol. Life Sci. 2016;73:3249–3263. doi: 10.1007/s00018-016-2224-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan W.W.R., Chow J., Chau D.D.-L., Zhai Y., Lau K.-F. Beclin 1-Mediated Autophagy Is Potentiated by an Interaction with the Neuronal Adaptor FE65. Biology. 2025;14:97. doi: 10.3390/biology14010097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Y., Wang H., Xu H. Autophagy-lysosome pathway in insulin & glucagon homeostasis. Front. Endocrinol. 2025;16:1541794. doi: 10.3389/fendo.2025.1541794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qian Z., Li Z., Peng X., Mao Y., Mao X., Li J. Annexin A: Cell Death, Inflammation, and Translational Medicine. J. Inflamm. Res. 2025;18:5655–5672. doi: 10.2147/JIR.S511439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang X., Yan H., Xu Z., Yang B., Luo P., He Q. The inducible role of autophagy in cell death: Emerging evidence and future perspectives. Cell Commun. Signal. 2025;23:151. doi: 10.1186/s12964-025-02135-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palabiyik A.A. The role of Bcl-2 in controlling the transition between autophagy and apoptosis. Mol. Med. Rep. 2025;32:172. doi: 10.3892/mmr.2025.13537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cabrera-Serrano A.J., Sánchez-Maldonado J.M., González-Olmedo C., Carretero-Fernández M., Díaz-Beltrán L., Gutiérrez-Bautista J.F., García-Verdejo F.J., Gálvez-Montosa F., López-López J.A., García-Martín P. Crosstalk between autophagy and oxidative stress in hematological malignancies: Mechanisms, implications, and therapeutic potential. Antioxidants. 2025;14:264. doi: 10.3390/antiox14030264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang H., Zhou J., Lu Y., Gao H., Ning E., Yang X., Hao Y., Hu D. The interplay between autophagy and programmed cell death in osteoarthritis: Insights into mechanisms and therapeutic targets. Mol. Cell. Biochem. 2025:1–20. doi: 10.1007/s11010-025-05279-y. [DOI] [PubMed] [Google Scholar]
- 17.Yun C.W., Jeon J., Go G., Lee J.H., Lee S.H. The dual role of autophagy in cancer development and a therapeutic strategy for cancer by targeting autophagy. Int. J. Mol. Sci. 2020;22:179. doi: 10.3390/ijms22010179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar P., Raj A. Protein Misfolding in Neurodegenerative Diseases. Elsevier; Amsterdam, The Netherlands: 2025. Degradation of misfolded proteins by ubiquitin-proteasome system and autophagy lysosomal proteolytic pathways; pp. 253–289. [Google Scholar]
- 19.Chen R., Yang C., Yang F., Yang A., Xiao H., Peng B., Chen C., Geng B., Xia Y. Targeting the mTOR-Autophagy Axis: Unveiling Therapeutic Potentials in Osteoporosis. Biomolecules. 2024;14:1452. doi: 10.3390/biom14111452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lyu J., Kim J.-S., Shin J. Herbal Medical Products for Metabolic Diseases-New Integrated Pharmacological Approaches. Frontiers in Pharmacology; Lausanne, Switzerland: 2024. Autophagy flux via AMPK/mTOR/ULK1 signaling pathway; p. 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang B., Pareek G., Kundu M. ULK/Atg1: Phasing in and out of autophagy. Trends Biochem. Sci. 2024;49:494–505. doi: 10.1016/j.tibs.2024.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sousa C., Videira M. Dual Approaches in Oncology: The Promise of siRNA and Chemotherapy Combinations in Cancer Therapies. Onco. 2025;5:2. doi: 10.3390/onco5010002. [DOI] [Google Scholar]
- 23.Ahmed K.R., Rahman M.M., Islam M.N., Fahim M.M.H., Rahman M.A., Kim B. Antioxidants activities of phytochemicals perspective modulation of autophagy and apoptosis to treating cancer. Biomed. Pharmacother. 2024;174:116497. doi: 10.1016/j.biopha.2024.116497. [DOI] [PubMed] [Google Scholar]
- 24.Rao S., Skulsuppaisarn M., Strong L.M., Ren X., Lazarou M., Hurley J.H., Hummer G. Three-step docking by WIPI2, ATG16L1, and ATG3 delivers LC3 to the phagophore. Sci. Adv. 2024;10:eadj8027. doi: 10.1126/sciadv.adj8027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noda N.N. Structural biology of the Atg8 and Atg12 conjugation systems. Autophagy Rep. 2023;2:2277582. doi: 10.1080/27694127.2023.2277582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gammoh N. The multifaceted functions of ATG16L1 in autophagy and related processes. J. Cell Sci. 2020;133:jcs249227. doi: 10.1242/jcs.249227. [DOI] [PubMed] [Google Scholar]
- 27.Tanida I., Ueno T., Kominami E. Autophagosome and Phagosome. Humana Press; Totowa, NJ, USA: 2008. LC3 and Autophagy; pp. 77–88. [DOI] [PubMed] [Google Scholar]
- 28.Zhou Y., Wang Z., Huang Y., Bai C., Zhang X., Fang M., Ju Z., Liu B. Membrane dynamics of ATG4B and LC3 in autophagosome formation. J. Mol. Cell Biol. 2021;13:853–863. doi: 10.1093/jmcb/mjab059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lőrincz P., Juhász G. Autophagosome-lysosome fusion. J. Mol. Biol. 2020;432:2462–2482. doi: 10.1016/j.jmb.2019.10.028. [DOI] [PubMed] [Google Scholar]
- 30.Arora K., Liyanage P., Zhong Q., Naren A.P. A SNARE protein Syntaxin 17 captures CFTR to potentiate autophagosomal clearance under stress. FASEB J. 2021;35:e21185. doi: 10.1096/fj.201903210R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mijanovic O., Petushkova A.I., Brankovic A., Turk B., Solovieva A.B., Nikitkina A.I., Bolevich S., Timashev P.S., Parodi A., Zamyatnin A.A., Jr. Cathepsin D—Managing the delicate balance. Pharmaceutics. 2021;13:837. doi: 10.3390/pharmaceutics13060837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Denton D., Kumar S. Autophagy-dependent cell death. Cell Death Differ. 2019;26:605–616. doi: 10.1038/s41418-018-0252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu H.-D., Qin Z.-H. Autophagy: Biology and Diseases: Basic Science. Springer; Singapore: 2019. Beclin 1, Bcl-2 and autophagy; pp. 109–126. [DOI] [PubMed] [Google Scholar]
- 34.Kaur S., Changotra H. The beclin 1 interactome: Modification and roles in the pathology of autophagy-related disorders. Biochimie. 2020;175:34–49. doi: 10.1016/j.biochi.2020.04.025. [DOI] [PubMed] [Google Scholar]
- 35.Tran S., Fairlie W.D., Lee E.F. BECLIN1: Protein structure, function and regulation. Cells. 2021;10:1522. doi: 10.3390/cells10061522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cao Z., Tian K., Ran Y., Zhou H., Zhou L., Ding Y., Tang X. Beclin-1: A therapeutic target at the intersection of autophagy, immunotherapy, and cancer treatment. Front. Immunol. 2024;15:1506426. doi: 10.3389/fimmu.2024.1506426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nakatogawa H. Mechanisms governing autophagosome biogenesis. Nat. Rev. Mol. Cell Biol. 2020;21:439–458. doi: 10.1038/s41580-020-0241-0. [DOI] [PubMed] [Google Scholar]
- 38.Li W., Zhang L. Autophagy: Biology and Diseases: Basic Science. Springer; Singapore: 2019. Regulation of ATG and autophagy initiation; pp. 41–65. [DOI] [PubMed] [Google Scholar]
- 39.Changotra H., Kaur S., Yadav S.S., Gupta G.L., Parkash J., Duseja A. ATG5: A central autophagy regulator implicated in various human diseases. Cell Biochem. Funct. 2022;40:650–667. doi: 10.1002/cbf.3740. [DOI] [PubMed] [Google Scholar]
- 40.Goncu E., Tinartas E.P., Gunay B., Ordu T., Turgay Izzetoglu G. Role of Atg3, Atg5 and Atg12 in the crosstalk between apoptosis and autophagy in the posterior silk gland of Bombyx mori. Insect Mol. Biol. 2025;34:470–485. doi: 10.1111/imb.12985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu Y., Qian C., Wang Q., Song L., He Z., Liu W., Wan W. Deacetylation of ATG7 drives the induction of macroautophagy and LC3-associated microautophagy. Autophagy. 2024;20:1134–1146. doi: 10.1080/15548627.2023.2287932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Collier J.J., Suomi F., Oláhová M., McWilliams T.G., Taylor R.W. Emerging roles of ATG7 in human health and disease. EMBO Mol. Med. 2021;13:e14824. doi: 10.15252/emmm.202114824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bussi C., Iribarren P., Rodriguez C.M. Microtubule-associated protein 1A/1B-light chain 3 (LC3)’decorates’ intracytoplasmic inclusions in a patient with chronic lymphocytic leukaemia. Br. J. Haematol. 2017;179:529. doi: 10.1111/bjh.14893. [DOI] [PubMed] [Google Scholar]
- 44.Runwal G., Stamatakou E., Siddiqi F.H., Puri C., Zhu Y., Rubinsztein D.C. LC3-positive structures are prominent in autophagy-deficient cells. Sci. Rep. 2019;9:10147. doi: 10.1038/s41598-019-46657-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang R., Xu Y., Wan W., Shou X., Qian J., You Z., Liu B., Chang C., Zhou T., Lippincott-Schwartz J. Deacetylation of nuclear LC3 drives autophagy initiation under starvation. Mol. Cell. 2015;57:456–466. doi: 10.1016/j.molcel.2014.12.013. [DOI] [PubMed] [Google Scholar]
- 46.Rahman M.A., Bishayee K., Sadra A., Huh S.-O. Oxyresveratrol activates parallel apoptotic and autophagic cell death pathways in neuroblastoma cells. Biochim. Biophys. Acta BBA-Gen. Subj. 2017;1861:23–36. doi: 10.1016/j.bbagen.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 47.Kumar A.V., Mills J., Lapierre L.R. Selective autophagy receptor p62/SQSTM1, a pivotal player in stress and aging. Front. Cell Dev. Biol. 2022;10:793328. doi: 10.3389/fcell.2022.793328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carroll B., Otten E.G., Manni D., Stefanatos R., Menzies F.M., Smith G.R., Jurk D., Kenneth N., Wilkinson S., Passos J.F. Oxidation of SQSTM1/p62 mediates the link between redox state and protein homeostasis. Nat. Commun. 2018;9:256. doi: 10.1038/s41467-017-02746-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Orlandi G., Roncucci L., Carnevale G., Sena P. Different roles of apoptosis and autophagy in the development of human colorectal cancer. Int. J. Mol. Sci. 2023;24:10201. doi: 10.3390/ijms241210201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tang J., Li Y., Xia S., Li J., Yang Q., Ding K., Zhang H. Sequestosome 1/p62: A multitasker in the regulation of malignant tumor aggression. Int. J. Oncol. 2021;59:77. doi: 10.3892/ijo.2021.5257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Y., Zhang H. Autophagy: Biology and Diseases: Basic Science. Springer; Singapore: 2019. Regulation of autophagy by mTOR signaling pathway; pp. 67–83. [DOI] [PubMed] [Google Scholar]
- 52.Datkhayeva Z., Iskakova A., Mireeva A., Seitaliyeva A., Skakova R., Kulniyazova G., Shayakhmetova A., Koshkimbayeva G., Sarmuldayeva C., Nurseitova L. The Multifactorial Pathogenesis of Endometriosis: A Narrative Review Integrating Hormonal, Immune, and Microbiome Aspects. Medicina. 2025;61:811. doi: 10.3390/medicina61050811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chao P., Zhang X., Zhang L., Han Z., Jie R., Duan P., Cao M., Yang A. Electroacupuncture as a promising therapeutic strategy for doxorubicin-induced heart failure: Insights into the PI3K/AKT/mTOR/ULK1 and AMPK/mTOR/ULK1 pathways. Colloids Surf. B Biointerfaces. 2025;251:114590. doi: 10.1016/j.colsurfb.2025.114590. [DOI] [PubMed] [Google Scholar]
- 54.Zhang C., Shu X., Yin C., Hu S., Liu P. The role of the mTOR pathway in breast cancer stem cells (BCSCs): Mechanisms and therapeutic potentials. Stem Cell Res. Ther. 2025;16:156. doi: 10.1186/s13287-025-04218-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tian H.-Y., Lei Y.-X., Zhou J.-T., Liu L.-J., Yang T., Zhou Y., Ge J.-W., Xu C., Mei Z.-G. Insight into interplay between PANoptosis and autophagy: Novel therapeutics in ischemic stroke. Front. Mol. Neurosci. 2025;17:1482015. doi: 10.3389/fnmol.2024.1482015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tang L., Zhang W., Liao Y., Wang W., Deng X., Wang C., Shi W. Autophagy: A double-edged sword in ischemia–reperfusion injury. Cell. Mol. Biol. Lett. 2025;30:1–47. doi: 10.1186/s11658-025-00713-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liao Y.X., Yu H.Y., Lv J.Y., Cai Y.R., Liu F., He Z.M., He S.S. Targeting autophagy is a promising therapeutic strategy to overcome chemoresistance and reduce metastasis in osteosarcoma. Int. J. Oncol. 2019;55:1213–1222. doi: 10.3892/ijo.2019.4902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wei S., Han C., Mo S., Huang H., Luo X. Advancements in programmed cell death research in antitumor therapy: A comprehensive overview. Apoptosis. 2025;30:401–421. doi: 10.1007/s10495-024-02038-0. [DOI] [PubMed] [Google Scholar]
- 59.Jalouli M. Emerging Role of Hypoxia-Inducible Factors (HIFs) in Modulating Autophagy: Perspectives on Cancer Therapy. Int. J. Mol. Sci. 2025;26:1752. doi: 10.3390/ijms26041752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mosadegh M., Noori Goodarzi N., Erfani Y. A Comprehensive Insight into Apoptosis: Molecular Mechanisms, Signaling Pathways, and Modulating Therapeutics. Cancer Investig. 2025;43:33–58. doi: 10.1080/07357907.2024.2445528. [DOI] [PubMed] [Google Scholar]
- 61.Selvarani R. Ph.D. Thesis. The University of Oklahoma Health Sciences Center; Oklahoma City, OK, USA: 2024. Using Novel RIPK3 and Mlkl Knock-In Mouse Models to Study the Role of Necroptosis in Chronic Liver Disease and Liver Cancer. [Google Scholar]
- 62.Wang G., Jiang X., Torabian P., Yang Z. Investigating autophagy and intricate cellular mechanisms in hepatocellular carcinoma: Emphasis on cell death mechanism crosstalk. Cancer Lett. 2024;588:216744. doi: 10.1016/j.canlet.2024.216744. [DOI] [PubMed] [Google Scholar]
- 63.Singh R., Jadhav K., Rawat N., Verma R.K., Kumar J. Role of Autophagy and Reactive Oxygen Species in Cancer Treatment: Principles and Current Strategies. Springer; Berlin/Heidelberg, Germany: 2024. Current strategies for targeting autophagy and ros for cancer treatment; pp. 287–307. [Google Scholar]
- 64.Karlowitz R., Van Wijk S.J. Surviving death: Emerging concepts of RIPK3 and MLKL ubiquitination in the regulation of necroptosis. FEBS J. 2023;290:37–54. doi: 10.1111/febs.16255. [DOI] [PubMed] [Google Scholar]
- 65.Snyder A.G., Oberst A. The antisocial network: Cross talk between cell death programs in host defense. Annu. Rev. Immunol. 2021;39:77–101. doi: 10.1146/annurev-immunol-112019-072301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhao S., Guo Y., Yin X. Autophagy, ferroptosis, apoptosis and pyroptosis in metabolic dysfunction-associated steatotic liver disease. Front. Biosci.-Landmark. 2024;29:30. doi: 10.31083/j.fbl2901030. [DOI] [PubMed] [Google Scholar]
- 67.Yuan J., Amin P., Ofengeim D. Necroptosis and RIPK1-mediated neuroinflammation in CNS diseases. Nat. Rev. Neurosci. 2019;20:19–33. doi: 10.1038/s41583-018-0093-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Martinez-Osorio V., Abdelwahab Y., Ros U. The many faces of MLKL, the executor of necroptosis. Int. J. Mol. Sci. 2023;24:10108. doi: 10.3390/ijms241210108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Samson A.L., Zhang Y., Geoghegan N.D., Gavin X.J., Davies K.A., Mlodzianoski M.J., Whitehead L.W., Frank D., Garnish S.E., Fitzgibbon C. MLKL trafficking and accumulation at the plasma membrane control the kinetics and threshold for necroptosis. Nat. Commun. 2020;11:3151. doi: 10.1038/s41467-020-16887-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gao J., Xiong A., Liu J., Li X., Wang J., Zhang L., Liu Y., Xiong Y., Li G., He X. PANoptosis: Bridging apoptosis, pyroptosis, and necroptosis in cancer progression and treatment. Cancer Gene Ther. 2024;31:970–983. doi: 10.1038/s41417-024-00765-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zheng J., Conrad M. Ferroptosis: When metabolism meets cell death. Physiol. Rev. 2025;105:651–706. doi: 10.1152/physrev.00031.2024. [DOI] [PubMed] [Google Scholar]
- 72.Guo Z., Liu Y., Chen D., Sun Y., Li D., Meng Y., Zhou Q., Zeng F., Deng G., Chen X. Targeting regulated cell death: Apoptosis, necroptosis, pyroptosis, ferroptosis, and cuproptosis in anticancer immunity. J. Transl. Intern. Med. 2025;13:10–32. doi: 10.1515/jtim-2025-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Li S., Huang P., Lai F., Zhang T., Guan J., Wan H., He Y. Mechanisms of ferritinophagy and ferroptosis in diseases. Mol. Neurobiol. 2024;61:1605–1626. doi: 10.1007/s12035-023-03640-0. [DOI] [PubMed] [Google Scholar]
- 74.Li J.Y., Feng Y.H., Li Y.X., He P.Y., Zhou Q.Y., Tian Y.P., Yao R.Q., Yao Y.M. Ferritinophagy: A novel insight into the double-edged sword in ferritinophagy–ferroptosis axis and human diseases. Cell Prolif. 2024;57:e13621. doi: 10.1111/cpr.13621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sui X., Wang J., Zhao Z., Liu B., Liu M., Liu M., Shi C., Feng X., Fu Y., Shi D. Phenolic compounds induce ferroptosis-like death by promoting hydroxyl radical generation in the Fenton reaction. Commun. Biol. 2024;7:199. doi: 10.1038/s42003-024-05903-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhou Q., Meng Y., Li D., Yao L., Le J., Liu Y., Sun Y., Zeng F., Chen X., Deng G. Ferroptosis in cancer: From molecular mechanisms to therapeutic strategies. Signal Transduct. Target. Ther. 2024;9:55. doi: 10.1038/s41392-024-01769-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Feng F., He S., Li X., He J., Luo L. Mitochondria-mediated ferroptosis in diseases therapy: From molecular mechanisms to implications. Aging Dis. 2024;15:714. doi: 10.14336/AD.2023.0717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Feng J., Wang Z.-X., Bin J.-L., Chen Y.-X., Ma J., Deng J.-H., Huang X.-W., Zhou J., Lu G.-D. Pharmacological approaches for targeting lysosomes to induce ferroptotic cell death in cancer. Cancer Lett. 2024;587:216728. doi: 10.1016/j.canlet.2024.216728. [DOI] [PubMed] [Google Scholar]
- 79.Shao B., Bu H., Li G., Kang D., Ju Q. Autophagy-dependent apoptosis induction by oridonin are mediated by ROS-dependent AMPK-mTOR-ULK1 pathway in colon cancer. Am. J. Cancer Res. 2025;15:1902. doi: 10.62347/CGIO2604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Van Houten B., Hunter S.E., Meyer J.N. Mitochondrial DNA damage induced autophagy, cell death, and disease. Front. Biosci. Landmark Ed. 2016;21:42. doi: 10.2741/4375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mrakovcic M., Fröhlich L.F. p53-mediated molecular control of autophagy in tumor cells. Biomolecules. 2018;8:14. doi: 10.3390/biom8020014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rahman M.A., Jalouli M., Bhajan S.K., Al-Zharani M., Harrath A.H. The Role of Hypoxia-Inducible Factor-1α (HIF-1α) in the Progression of Ovarian Cancer: Perspectives on Female Infertility. Cells. 2025;14:437. doi: 10.3390/cells14060437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Takahama M., Akira S., Saitoh T. Autophagy limits activation of the inflammasomes. Immunol. Rev. 2018;281:62–73. doi: 10.1111/imr.12613. [DOI] [PubMed] [Google Scholar]
- 84.Cau R., Saba L. Interlinking pathways: A narrative review on the role of IL-6 in cancer and atherosclerosis. Cardiovasc. Diagn. Ther. 2024;14:1186. doi: 10.21037/cdt-24-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Silva V.R., Neves S.P., Santos L.D.S., Dias R.B., Bezerra D.P. Challenges and therapeutic opportunities of autophagy in cancer therapy. Cancers. 2020;12:3461. doi: 10.3390/cancers12113461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wang H., Sun P., Yuan X., Xu Z., Jiang X., Xiao M., Yao X., Shi Y. Autophagy in tumor immune escape and immunotherapy. Mol. Cancer. 2025;24:85. doi: 10.1186/s12943-025-02277-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhao Y., Zhong B., Cao J.-Y., Wang Q., Liang J., Lu K., Lu S.-M. Tumor hypoxia: Classification, detection, and its critical role in cancer progression. Biomol. Biomed. 2025 doi: 10.17305/bb.2025.12318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Daskalaki I., Gkikas I., Tavernarakis N. Hypoxia and selective autophagy in cancer development and therapy. Front. Cell Dev. Biol. 2018;6:104. doi: 10.3389/fcell.2018.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kuo C.-L., Ponneri Babuharisankar A., Lin Y.-C., Lien H.-W., Lo Y.K., Chou H.-Y., Tangeda V., Cheng L.-C., Cheng A.N., Lee A.Y.-L. Mitochondrial oxidative stress in the tumor microenvironment and cancer immunoescape: Foe or friend? J. Biomed. Sci. 2022;29:74. doi: 10.1186/s12929-022-00859-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yoshida G.J. Therapeutic strategies of drug repositioning targeting autophagy to induce cancer cell death: From pathophysiology to treatment. J. Hematol. Oncol. 2017;10:1–14. doi: 10.1186/s13045-017-0436-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hou X., Jiang J., Tian Z., Wei L. Autophagy: Biology and Diseases: Clinical Science. Springer; Singapore: 2020. Autophagy and tumour chemotherapy; pp. 351–374. [DOI] [PubMed] [Google Scholar]
- 92.Wei J., Wang B., Wang H., Meng L., Zhao Q., Li X., Xin Y., Jiang X. Radiation-induced normal tissue damage: Oxidative stress and epigenetic mechanisms. Oxidative Med. Cell. Longev. 2019;2019:3010342. doi: 10.1155/2019/3010342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Roy A., Bera S., Saso L., Dwarakanath B.S. Role of autophagy in tumor response to radiation: Implications for improving radiotherapy. Front. Oncol. 2022;12:957373. doi: 10.3389/fonc.2022.957373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Elshazly A.M., Xu J., Melhem N., Abdulnaby A., Elzahed A.A., Saleh T., Gewirtz D.A. Is Autophagy Targeting a Valid Adjuvant Strategy in Conjunction with Tyrosine Kinase Inhibitors? Cancers. 2024;16:2989. doi: 10.3390/cancers16172989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Akkoc Y., Peker N., Akcay A., Gozuacik D. Autophagy and cancer dormancy. Front. Oncol. 2021;11:627023. doi: 10.3389/fonc.2021.627023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ferreira P.M.P., de Sousa R.W.R., de Oliveira Ferreira J.R., Militão G.C.G., Bezerra D.P. Chloroquine and hydroxychloroquine in antitumor therapies based on autophagy-related mechanisms. Pharmacol. Res. 2021;168:105582. doi: 10.1016/j.phrs.2021.105582. [DOI] [PubMed] [Google Scholar]
- 97.Chen J.-L., Wu X., Yin D., Jia X.-H., Chen X., Gu Z.-Y., Zhu X.-M. Autophagy inhibitors for cancer therapy: Small molecules and nanomedicines. Pharmacol. Ther. 2023;249:108485. doi: 10.1016/j.pharmthera.2023.108485. [DOI] [PubMed] [Google Scholar]
- 98.Shi T.-T., Yu X.-X., Yan L.-J., Xiao H.-T. Research progress of hydroxychloroquine and autophagy inhibitors on cancer. Cancer Chemother. Pharmacol. 2017;79:287–294. doi: 10.1007/s00280-016-3197-1. [DOI] [PubMed] [Google Scholar]
- 99.Abdel-Aziz A.K., Saadeldin M.K., Salem A.H., Ibrahim S.A., Shouman S., Abdel-Naim A.B., Orecchia R. A critical review of chloroquine and hydroxychloroquine as potential adjuvant agents for treating people with cancer. Future Pharmacol. 2022;2:431–443. doi: 10.3390/futurepharmacol2040028. [DOI] [Google Scholar]
- 100.Hassan A.M.I.A., Zhao Y., Chen X., He C. Blockage of autophagy for cancer therapy: A comprehensive review. Int. J. Mol. Sci. 2024;25:7459. doi: 10.3390/ijms25137459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Uddin M.S., Rahman M.A., Kabir M.T., Behl T., Mathew B., Perveen A., Barreto G.E., Bin-Jumah M.N., Abdel-Daim M.M., Ashraf G.M. Multifarious roles of mTOR signaling in cognitive aging and cerebrovascular dysfunction of Alzheimer’s disease. Iubmb Life. 2020;72:1843–1855. doi: 10.1002/iub.2324. [DOI] [PubMed] [Google Scholar]
- 102.Paquette M., El-Houjeiri L., Pause A. mTOR pathways in cancer and autophagy. Cancers. 2018;10:18. doi: 10.3390/cancers10010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xu Z., Han X., Ou D., Liu T., Li Z., Jiang G., Liu J., Zhang J. Targeting PI3K/AKT/mTOR-mediated autophagy for tumor therapy. Appl. Microbiol. Biotechnol. 2020;104:575–587. doi: 10.1007/s00253-019-10257-8. [DOI] [PubMed] [Google Scholar]
- 104.Ihlamur M., Akgül B., Zengin Y., Korkut Ş.V., Kelleci K., Abamor E.Ş. The mTOR Signaling pathway and mTOR Inhibitors in cancer: Next-generation inhibitors and approaches. Curr. Mol. Med. 2024;24:478–494. doi: 10.2174/1566524023666230509161645. [DOI] [PubMed] [Google Scholar]
- 105.Masaki N., Aoki Y., Obara K., Kubota Y., Bouvet M., Miyazaki J., Hoffman R.M. Targeting autophagy with the synergistic combination of chloroquine and rapamycin as a novel effective treatment for well-differentiated liposarcoma. Cancer Genom. Proteom. 2023;20:317–322. doi: 10.21873/cgp.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tian Y., Song W., Li D., Cai L., Zhao Y. Resveratrol as a natural regulator of autophagy for prevention and treatment of cancer. OncoTargets Ther. 2019;12:8601–8609. doi: 10.2147/OTT.S213043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Utpal B.K., Mokhfi F.Z., Zehravi M., Sweilam S.H., Gupta J.K., Kareemulla S., Rao A., Kumar V.V., Krosuri P., Prasad D. Resveratrol: A Natural Compound Targeting the PI3K/Akt/mTOR Pathway in Neurological Diseases. Mol. Neurobiol. 2024;62:5579–5608. doi: 10.1007/s12035-024-04608-4. [DOI] [PubMed] [Google Scholar]
- 108.Yang R., Dong H., Jia S., Yang Z. Resveratrol as a modulatory of apoptosis and autophagy in cancer therapy. Clin. Transl. Oncol. 2022;24:1219–1230. doi: 10.1007/s12094-021-02770-y. [DOI] [PubMed] [Google Scholar]
- 109.Zhu Y., Bu S. Curcumin induces autophagy, apoptosis, and cell cycle arrest in human pancreatic cancer cells. Evid.-Based Complement. Altern. Med. 2017;2017:5787218. doi: 10.1155/2017/5787218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Aggarwal B.B., Yuan W., Li S., Gupta S.C. Curcumin-free turmeric exhibits anti-inflammatory and anticancer activities: Identification of novel components of turmeric. Mol. Nutr. Food Res. 2013;57:1529–1542. doi: 10.1002/mnfr.201200838. [DOI] [PubMed] [Google Scholar]
- 111.Seo S.U., Woo S.M., Lee H.-S., Kim S.H., Min K.-J., Kwon T.K. mTORC1/2 inhibitor and curcumin induce apoptosis through lysosomal membrane permeabilization-mediated autophagy. Oncogene. 2018;37:5205–5220. doi: 10.1038/s41388-018-0345-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Arena A., Romeo M.A., Benedetti R., Masuelli L., Bei R., Gilardini Montani M.S., Cirone M. New insights into curcumin-and resveratrol-mediated anti-cancer effects. Pharmaceuticals. 2021;14:1068. doi: 10.3390/ph14111068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yuan W., Fang W., Zhang R., Lyu H., Xiao S., Guo D., Ali D.W., Michalak M., Chen X.-Z., Zhou C. Therapeutic strategies targeting AMPK-dependent autophagy in cancer cells. Biochim. Biophys. Acta BBA-Mol. Cell Res. 2023;1870:119537. doi: 10.1016/j.bbamcr.2023.119537. [DOI] [PubMed] [Google Scholar]
- 114.Han F., Li C.-F., Cai Z., Zhang X., Jin G., Zhang W.-N., Xu C., Wang C.-Y., Morrow J., Zhang S. The critical role of AMPK in driving Akt activation under stress, tumorigenesis and drug resistance. Nat. Commun. 2018;9:4728. doi: 10.1038/s41467-018-07188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zamanian M.Y., Golmohammadi M., Yumashev A., Hjazi A., Toama M.A., AbdRabou M.A., Gehlot A., Alwaily E.R., Shirsalimi N., Yadav P.K. Effects of metformin on cancers in experimental and clinical studies: Focusing on autophagy and AMPK/mTOR signaling pathways. Cell Biochem. Funct. 2024;42:e4071. doi: 10.1002/cbf.4071. [DOI] [PubMed] [Google Scholar]
- 116.Xia H., Tai X.-J., Cheng W., Wu Y., He D., Wang L.-F., Liu H., Zhang S.-Y., Sun Y.-T., Liu H.-Z. Metformin inhibits the growth of SCLC cells by inducing autophagy and apoptosis via the suppression of EGFR and AKT signalling. Sci. Rep. 2025;15:6081. doi: 10.1038/s41598-025-87537-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Park D.-B. Metformin promotes apoptosis but suppresses autophagy in glucose-deprived H4IIE hepatocellular carcinoma cells. Diabetes Metab. J. 2015;39:518. doi: 10.4093/dmj.2015.39.6.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Palomer X., Wang J.-R., Escalona C., Wu S., Wahli W., Vázquez-Carrera M. Targeting AMPK as a potential treatment for hepatic fibrosis in MASLD. Trends Pharmacol. Sci. 2025;46:551–566. doi: 10.1016/j.tips.2025.03.008. [DOI] [PubMed] [Google Scholar]
- 119.Mohanty S.S., Warrier S., Rangarajan A. Rethinking AMPK: A Reversible Switch Fortifying Cancer Cell Stress-Resilience. Yale J. Biol. Med. 2025;98:33. doi: 10.59249/JKBB6336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Psara E., Poulios E., Papadopoulou S.K., Tolia M., Vasios G.K., Giaginis C. Intermittent fasting against cancer development and progression: Highlighting potential anticancer molecular mechanisms. Anti-Cancer Agents Med. Chem.-Anti-Cancer Agents. 2023;23:1889–1909. doi: 10.2174/1871520623666230816090229. [DOI] [PubMed] [Google Scholar]
- 121.Liu T., Zhang J., Li K., Deng L., Wang H. Combination of an Autophagy Inducer and an Autophagy Inhibitor: A Smarter Strategy Emerging in Cancer Therapy. Front. Pharmacol. 2020;11:408. doi: 10.3389/fphar.2020.00408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang Y., Ding C., Zhu W., Li X., Chen T., Liu Q., Zhou S., Zhang T.C., Ma W. Chemotherapeutic drugs induce oxidative stress associated with DNA repair and metabolism modulation. Life Sci. 2022;289:120242. doi: 10.1016/j.lfs.2021.120242. [DOI] [PubMed] [Google Scholar]
- 123.Agalakova N.I. Chloroquine and Chemotherapeutic Compounds in Experimental Cancer Treatment. Int. J. Mol. Sci. 2024;25:945. doi: 10.3390/ijms25020945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fu Z., Cheng X., Kuang J., Feng H., Chen L., Liang J., Shen X., Yuen S., Peng C., Shen B. CQ sensitizes human pancreatic cancer cells to gemcitabine through the lysosomal apoptotic pathway via reactive oxygen species. Mol. Oncol. 2018;12:529–544. doi: 10.1002/1878-0261.12179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Rahman M.A., Jalouli M., Bhajan S.K., Al-Zharani M., Harrath A.H. A Comprehensive Review of Nanoparticle-Based Drug Delivery for Modulating PI3K/AKT/mTOR-Mediated Autophagy in Cancer. Int. J. Mol. Sci. 2025;26:1868. doi: 10.3390/ijms26051868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sareen G., Mohan M., Mannan A., Dua K., Singh T.G. A new era of cancer immunotherapy: Vaccines and miRNAs. Cancer Immunol. Immunother. 2025;74:163. doi: 10.1007/s00262-025-04011-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chen D., Ling X., Wang Y., Zhang Q., He X., Dong Z., Li M., He Q. Autophagy-activating aluminum hydroxide nanovaccine for enhanced antigen presentation and anti-tumor immunity. J. Control. Release. 2025;377:223–235. doi: 10.1016/j.jconrel.2024.11.018. [DOI] [PubMed] [Google Scholar]
- 128.Jiang G.M., Tan Y., Wang H., Peng L., Chen H.T., Meng X.J., Li L.L., Liu Y., Li W.F., Shan H. The relationship between autophagy and the immune system and its applications for tumor immunotherapy. Mol. Cancer. 2019;18:17. doi: 10.1186/s12943-019-0944-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Germic N., Frangez Z., Yousefi S., Simon H.U. Regulation of the innate immune system by autophagy: Monocytes, macrophages, dendritic cells and antigen presentation. Cell Death Differ. 2019;26:715–727. doi: 10.1038/s41418-019-0297-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Delmas D., Hermetet F., Aires V. PD-1/PD-L1 Checkpoints and Resveratrol: A Controversial New Way for a Therapeutic Strategy. Cancers. 2021;13:4509. doi: 10.3390/cancers13184509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.He S., Zheng L., Qi C. Myeloid-derived suppressor cells (MDSCs) in the tumor microenvironment and their targeting in cancer therapy. Mol. Cancer. 2025;24:5. doi: 10.1186/s12943-024-02208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Rahman M.A., Jalouli M., Yadab M.K., Al-Zharani M. Progress in drug delivery systems based on nanoparticles for improved glioblastoma therapy: Addressing challenges and investigating opportunities. Cancers. 2025;17:701. doi: 10.3390/cancers17040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gu X., Xiang D., Zhu H., He X., Yang C., Chen R. Dual role of autophagy in bone metastasis: Mechanistic insights and therapeutic targeting. Am. J. Clin. Exp. Urol. 2025;13:92. doi: 10.62347/QCPV6064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ye H., Chen M., Cao F., Huang H., Zhan R., Zheng X. Chloroquine, an autophagy inhibitor, potentiates the radiosensitivity of glioma initiating cells by inhibiting autophagy and activating apoptosis. BMC Neurol. 2016;16:1–8. doi: 10.1186/s12883-016-0700-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cufí S., Vazquez-Martin A., Oliveras-Ferraros C., Corominas-Faja B., Cuyàs E., López-Bonet E., Martin-Castillo B., Joven J., Menendez J.A. The anti-malarial chloroquine overcomes primary resistance and restores sensitivity to trastuzumab in HER2-positive breast cancer. Sci. Rep. 2013;3:2469. doi: 10.1038/srep02469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mauvezin C., Neufeld T.P. Bafilomycin A1 disrupts autophagic flux by inhibiting both V-ATPase-dependent acidification and Ca-P60A/SERCA-dependent autophagosome-lysosome fusion. Autophagy. 2015;11:1437–1438. doi: 10.1080/15548627.2015.1066957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zhang X., Wang H., Yu M., Ma K., Ning L. Inhibition of autophagy by 3-methyladenine promotes migration and invasion of colon cancer cells through epithelial mesenchymal transformation. Transl. Cancer Res. 2022;11:2834. doi: 10.21037/tcr-22-1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Alayev A., Berger S.M., Kramer M.Y., Schwartz N.S., Holz M.K. The combination of rapamycin and resveratrol blocks autophagy and induces apoptosis in breast cancer cells. J. Cell. Biochem. 2015;116:450–457. doi: 10.1002/jcb.24997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Demirkesen Ş., İriağaç Y., Şeber E.S., Aral C. Melatonin enhances everolimus efficacy in breast cancer by suppressing mTOR pathway activation and promoting apoptosis and mitochondrial function. BMC Pharmacol. Toxicol. 2025;26:1–12. doi: 10.1186/s40360-025-00907-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rangwala R., Chang Y.C., Hu J., Algazy K.M., Evans T.L., Fecher L.A., Schuchter L.M., Torigian D.A., Panosian J.T., Troxel A.B. Combined MTOR and autophagy inhibition: Phase I trial of hydroxychloroquine and temsirolimus in patients with advanced solid tumors and melanoma. Autophagy. 2014;10:1391–1402. doi: 10.4161/auto.29119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Park W.Y., Song G., Boo M., Kim H.I., Park J.Y., Jung S.J., Choi M., Kim B., Kim Y.D., Kim M.-H. Anmyungambi decoction ameliorates obesity through activation of non-shivering thermogenesis in Brown and white adipose tissues. Antioxidants. 2022;12:49. doi: 10.3390/antiox12010049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zhang L., Xu S., Cheng X., Wu J., Wu L., Wang Y., Wang X., Bao J., Yu H. Curcumin induces autophagic cell death in human thyroid cancer cells. Toxicol. Vitr. 2022;78:105254. doi: 10.1016/j.tiv.2021.105254. [DOI] [PubMed] [Google Scholar]
- 143.Chen C., Wang H., Geng X., Zhang D., Zhu Z., Zhang G., Hou J. Metformin exerts anti-AR-negative prostate cancer activity via AMPK/autophagy signaling pathway. Cancer Cell Int. 2021;21:1–12. doi: 10.1186/s12935-021-02043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cao P., Jiang X., Xi Z. Sunitinib induces autophagy via suppressing Akt/mTOR pathway in renal cell carcinoma. Beijing Da Xue Xue Bao Yi Xue Ban J. Peking Univ. Health Sci. 2016;48:584–589. [PubMed] [Google Scholar]
- 145.Jawad M.H., Jabir M.S., Ozturk K., Sulaiman G.M., Abomughaid M.M., Albukhaty S., Al-Kuraishy H.M., Al-Gareeb A.I., Al-Azzawi W.K., Najm M.A. Induction of apoptosis and autophagy via regulation of AKT and JNK mitogen-activated protein kinase pathways in breast cancer cell lines exposed to gold nanoparticles loaded with TNF-α and combined with doxorubicin. Nanotechnol. Rev. 2023;12:20230148. doi: 10.1515/ntrev-2023-0148. [DOI] [Google Scholar]
- 146.Bahar E., Kim J.-Y., Kim D.-C., Kim H.-S., Yoon H. Combination of niraparib, cisplatin and twist knockdown in cisplatin-resistant ovarian cancer cells potentially enhances synthetic lethality through ER-stress mediated mitochondrial apoptosis pathway. Int. J. Mol. Sci. 2021;22:3916. doi: 10.3390/ijms22083916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zhou Y., Rucker E.B., III, Zhou B.P. Autophagy regulation in the development and treatment of breast cancer. Acta Biochim. Biophys. Sin. 2016;48:60–74. doi: 10.1093/abbs/gmv119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Galluzzi L., Bravo-San Pedro J.M., Levine B., Green D.R., Kroemer G. Pharmacological modulation of autophagy: Therapeutic potential and persisting obstacles. Nat. Rev. Drug Discov. 2017;16:487–511. doi: 10.1038/nrd.2017.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study.