Abstract
Stellate ganglion block (SGB) is not only used for treating cervical thoracic, and upper limb pain-related diseases but also for treating sympathetic nervous system dysfunction-related diseases, and it is a widely used clinical treatment method. This study has demonstrated that utilizing ultrasound to measure pupillary diameter (PD) changes and significant inter-eye differences offers a more objective assessment of stellate ganglion block (SGB) efficacy compared to the traditional subjective evaluation based on Horner’s syndrome (HS). However, there is currently no objective standard to evaluate the efficacy of SGB. Pupillary ultrasonography can observe precise dynamic changes in the pupils, and is less affected by peripheral light, non-invasive, and convenient. We performed SGB under ultrasound guidance, and evaluated the effectiveness of SGB according to HS in 60 patients. All patients were scored using a visual analogue scale (VAS) before and 24 h after stellate ganglion block treatment. We compared the changes in pupil diameter (PD) and pupillary constriction ratio during pupil light reflex (PLR) in the blocked side and the opposite side. Then we calculated the inter-eye difference of PD before and after SGB, and the inter-eye difference of PD in the blocked side and the opposite side (BO-IED) at each time point. We found that the area under the curve (AUC) for evaluating the effectiveness of SGB was statistically significant at each time points for BO-IED and blocked side inter-eye difference. Additionally, the BO-IED at 15 min after SGB has the largest AUC, when the BO-IED is greater than 0.5 mm, which shows a sensitivity of 86.5 %, and a specificity of 100 %. Our findings suggested an association between pupil reduction and symptom reduction in patients, with the degree of pupil reduction serving as a reference for evaluating the effectiveness of SGB and the degree of symptom relief.
Keywords: Stellate ganglion block, Regional nerve block, Pupillary ultrasonography, Horner's syndrome, Pain disorders
Highlights
-
•
Pupil diameter (PD) was significantly reduced after stellate ganglion block (SGB).
-
•
The inter-eye difference of PD can serve as an objective basis for evaluating the effectiveness of SGB.
-
•
PD change can be used in combination with HS as a reference value for evaluating SGB effectiveness.
1. Introduction
Stellate ganglion block (SGB) is a widely used clinical treatment not only for painful disorders of head, neck, chest, and upper extremities in its innervated regions, but also for improving sleep quality (Yang et al., 2023), post-traumatic stress disorder and other dysfunctional disorders of the sympathetic nervous system. Horner's Syndrome (HS) is the most widely used and important method for evaluating the success of stellate ganglion block. The classic triad in HS is unilateral ptosis, miosis, and anhidrosis. The symptoms of which are subjectively observed by the physician, but in some patients the clinical presentation is not obviously (Yamazaki et al., 2012). Therefore, a number of scholars have proposed the use of other objective indicators to evaluate the effect of SGB. These objective indicators include hemodynamic changes (Nitahara, Dan, 1998), Skin Sympathetic Nerve Activity (Doytchinova et al., 2017, Kusayama et al., 2020), pulse oximetry perfusion (Sahin et al., 2018), Pulse transit time (Kim et al., 2015), changes in temperature (Samen et al., 2022). Therefore, the evaluation of the effect of SGB requires multiple objective indicators to make a comprehensive judgment in addition to the appearance of HS, and there is no uniform objective standard. Ideal objective indicators should achieve the advantages of non-invasive, stable, reliable, real-time monitoring, easy to use, and less influenced by the environment to help clinicians make accurate judgments. Ultrasound pupillary measurement can observe precise dynamic changes in the pupils, and is less affected by peripheral light, non-invasive, and convenient (Farina et al., 2017, Farina et al., 2021). At present, there are few studies using ultrasound to observe pupil changes in SGB. Therefore, in this study, we used ultrasound to measure the precise changes in pupil diameter in SGB, providing an objective basis for evaluating the effectiveness of SGB.
2. Materials and methods
2.1. Study subjects
This project has been reviewed and approved by the Ethics Committee of the Second Affiliated Hospital of Soochow University (No. JD-LK-2022–027–02). This project was re-registered on 27 October 2022 on the China Clinical Trial Centre website (No. ChiCTR2200064945, https://www.chictr.org.cn/). We collected 60 patients who attended the pain department of the Second Affiliated Hospital of Soochow University from May 2022 to December 2022 and needed SGB treatment. All of them voluntarily signed the informed consent for the research project. The first patient registration date is 2022 June 14th.
2.2. Inclusion and exclusion criteria
Inclusion criteria: 18–70 years old, clinically diagnosed and in line with the indications for SGB treatment, including Neurodynia, Cervical spondylosis, Tinnitus, and Insomnia. Exclusion criteria: physiologic anisocoria; ophthalmologic diseases; neurological diseases; circulatory diseases; taking drugs affecting the function of sympathetic nerves; anatomical abnormalities of the neck and common contraindications to local anesthetics; need for intervention with vasoactive drugs during the observation period and subjects with poor compliance, unable to complete ultrasound pupil measurements.
2.3. Ultrasound-guided SGB
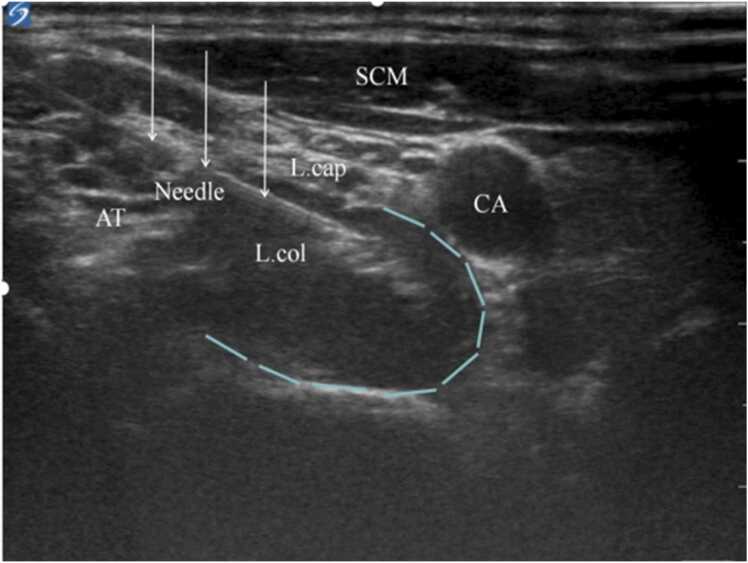
The SGB operation was performed in an operating room with in-door light of 100–120 lux and room temperature of 21°C - 26°C. SGB was performed by the same surgeon under ultrasound guidance using the transverse process of C6 as a localization marker and injected at the target point by injecting 4 mL of 1 % lidocaine local anesthetic (Fig. 1). The presence of Horner's syndrome after completion of the block was evaluated as positive.
Fig. 1.
Target point of SGB puncture. CA internal carotid artery; L.cap longissimus cephalicus; L.col longissimus cervicis; AT anterior tubercle of the transverse process of C6; SCM sternocleidomastoid muscle. The area framed by the dotted line is the area of diffusion of the local anesthetic. ↓referred to needle. n = 60.
2.4. Ultrasound pupillometry
All assessments were performed by the same experienced doctor with a Sonosite X-porte system equipped with a 6–15-MHz linear probe. The probe was placed below the orbit on top of the zygomatic bone while applying gentle pressure and then tilted downwards to approximately 45° in order to insonate the iris plane. After instructing the patient to look upward and achieving a stable image, the image is frozen, and the pupil diameter can be measured by placing a circular ruler on the left and right sides of the pupil. Pupil light reflex (PLR) were tested by the doctor with a pen light of fixed intensity (9 lumens) turned on approximately 2 cm in front of the subject's closed eyes for about 2 s, and record in continuous recording mode for 5 s. The coupling agent uses physiological saline, and the total examination time should be as short as possible (Farina et al., 2017, Farina et al., 2021) (Fig. 2, Fig. 3).
Fig. 2.
Ultrasound pupillometry. (A) proper angle of the probe for pupil insonation; (B) example of measurement of PD; (C) PLR testing; (D) PD after PLR. The scale applies to the (B) and (D). n = 60.
Fig. 3.
Comparison of bilateral pupils in patients after successful SGB. n = 60.
2.5. Data acquisition
Using SPSS23 statistical software, a random number table was generated. An experienced doctor performed stellate ganglion blockades based on this random number table, while another doctor carried out the eye ultrasonography examination. All observations of HS were made by a third doctor who was unaware of the nature of the experiment. The data acquisition was divided into block measurement (Block side, B side), and opposite side (Opposite side, O side). Data were collected before SGB treatment (Baseline), 3 min after block (T3), 5 min after block (T5), 10 min after block (T10), and 15 min after block (T15), respectively. The data collection content includes: pupil diameter (PD), Inter-eye difference before and after block on the same side; Inter-eye difference between left and right pupil diameter (BO-IED). Index calculation formula: Inter-eye difference before and after block on the same side (mm) = pre PD – post PD; BO-IED (mm) = opposite PD – blocked PD. At T0 and T15, collect the pupillary constriction ratio during PLR as ([resting pupil diameter - the smallest pupil diameter during constriction]/resting pupil diameter) × 100 and expressed as a percentage. Visual analogue scoring was performed before and 24 h after SGB treatment (Fig. 4).
Fig. 4.
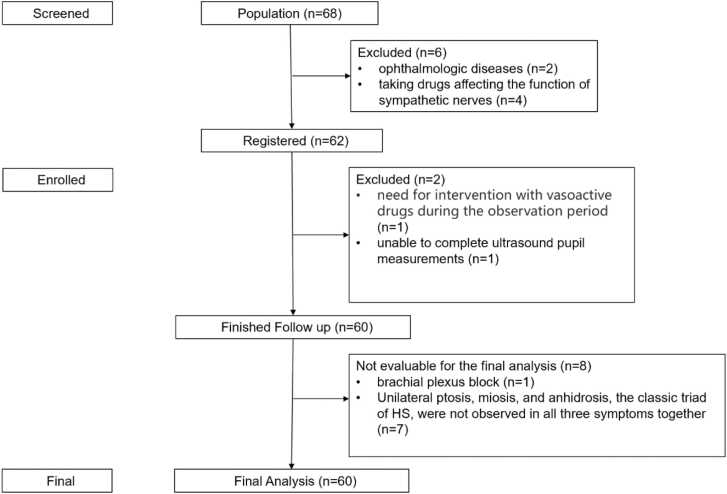
The procedure for this study. 2.6 Sample size.
This study is a clinical observational trial. The study subjects were patients with SGB, and the observed outcome indicator was the Inter-eye difference of pupil diameters between both sides. In the pilot study, the AUC for the inter-eye difference in pupil diameters to evaluate the efficacy of SGB was 0.725. Based on the pre-experimental results, the sample size calculated using PASS 15 software is 52 cases, with a power of 0.90 and α of 0.05. Considering a 15 % dropout rate, 60 patients needed to be included at baseline.
2.6. Statistical analysis
Paired t-test was used to compare the pupil data of the blocked side and the opposite side. PD, inter-eye difference, and PLR of the same side at each time point were analyzed by repeated measurement ANOVA. The usefulness of inter-eye difference before and after block on the same side and BO-IED in evaluating the effectiveness of SGB were assessed using the area under the receiver operating characteristic curve (AUC). Inter-eye difference and symptom score changes were used Spearman's rank correlation coefficient. Analyses were performed using SPSS 23.0 statistical software. Data were presented as mean ± standard deviation. The criterion for significant difference was P < 0.05.
3. Results
Stellate ganglion block (SGB) was performed on 60 patients within the study period. The efficacy of SGB was evaluated on the basis of the observation of Horner's Syndrome (HS); and the results showed that SGB was effective in 52 patients (87 %). The remaining 8 cases did not develop HS, one of which developed brachial plexus block (Table 1).
Table 1.
Patient diagnosis requiring treatment with SGB.
| N = 60 | |||
|---|---|---|---|
| Diagnosis | Neurodynia | 28 (47 %) | |
| Cervical spondylosis | 10 (17 %) | ||
| Tinnitus | 11 (18 %) | ||
| Insomnia | 11 (18 %) | ||
| Age (years) | 53.7 (20−70) |
Note: Data shown are number (percentage) or mean (range). Abbreviation: SGB = stellate ganglion block.
3.1. Pupil diameter changes following stellate ganglion block
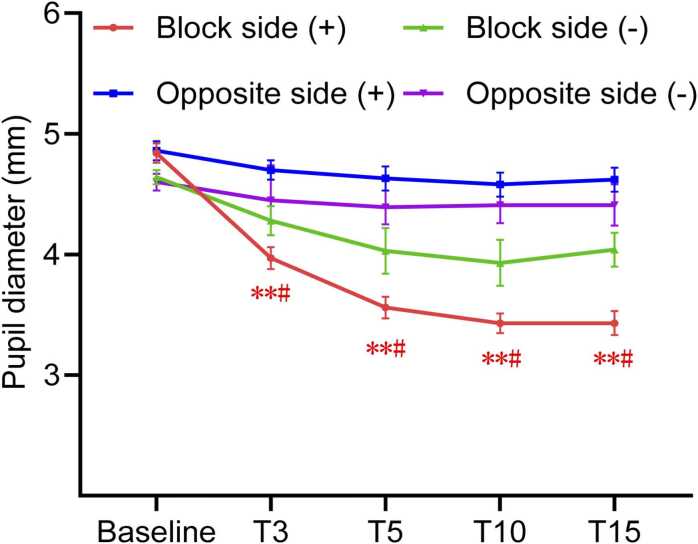
In patients for whom SGB was effective, the baseline mean pupil diameter (PD) was 4.8 mm on both sides, and the difference in PD between the two sides was between 0.01 mm. During the 15 min observation period, PD on the block side was consistently smaller than at baseline and was smaller than the opposite side (Table 2, Fig. 5). On the side of the SGB, PD decreased continuously during the 15 min observation period. At 15 min, PD decreased by 1.44 mm from baseline (P < 0.01). Differences from baseline were significant. On the side opposite the SGB there was also a reduction in PD but no change over time (Table 3). BO-IED rose continuously during the 15 min observation period after SGB. At 15 min, BO-IED increased by 1.44 mm from baseline (P < 0.01). No changes were found in the pupil light reflex (PLR) before and after block, as well as on both sides (P > 0.05). The data from the 8 patients who were negative for Horner’s syndrome did not show statistical significance (P > 0.05).
Table 2.
Changes in pupil diameter and response during SGB.
| Side |
Baseline |
T3 |
T5 |
T10 |
T15 |
F |
|
|---|---|---|---|---|---|---|---|
| N = 52 | |||||||
| PD (mm) |
B | 4.84 ± 0.57 | 3.97 ± 0.61**# | 3.56 ± 0.61**# | 3.43 ± 0.57**# | 3.43 ± 0.64**# | 125.98 |
| O | 4.86 ± 0.56 | 4.70 ± 0.59** | 4.63 ± 0.70** | 4.58 ± 0.69** | 4.62 ± 0.76** | 8.25 | |
| PLR (%) |
B | 40.02 ± 11.82 | - | - | - | 41.71 ± 12.82 | |
| O | 40.83 ± 10.97 | - | - | - | 38.40 ± 10.76 | ||
| BO-IED (mm) |
0.01 ± 0.16 | 0.58 ± 0.06** | 0.94 ± 0.07** | 1.02 ± 0.08** | 1.02 ± 0.09** | 79.37 | |
| N = 8 | |||||||
| PD (mm) |
B | 4.64 ± 0.16 | 4.28 ± 0.35 | 4.03 ± 0.55 | 3.93 ± 0.54 | 4.04 ± 0.40 | 7.52 |
| O | 4.6 ± 0.19 | 4.45 ± 0.29 | 4.39 ± 0.39 | 4.41 ± 0.42 | 4.41 ± 0.48 | 1.93 | |
| PLR (%) |
B | 39.88 ± 11.10 | - | - | - | 30.25 ± 5.50 | |
| O | 43.63 ± 10.60 | - | - | - | 36.75 ± 13.65 | ||
| BO-IED (mm) |
0.04 ± 0.09 | 0.18 ± 0.44 | 0.37 ± 0.59 | 0.49 ± 0.58 | 0.38 ± 0.48 | 3.78 |
Note: *P < 0.05 vs T0; **P < 0.01 vs baseline; #P < 0.05 vs opposite side. Abbreviations: B = block side; O = opposite side; PD = Pupil diameter; PLR = pupillary constriction ratio during pupil light reflex; BO-IED = Inter-eye difference between block side and opposite side; T3 = 3 min after SGB; T5 = 5 min after SGB; T10 = 10 min after SGB; T15 = 15 min after SGB.
Fig. 5.
Changes in Pupil diameter. Note: *P < 0.05 vs baseline; **P < 0.01 vs baseline; #P < 0.05 vs opposite side. (+), HS positive, n = 52; (-), HS negative, n = 8.
Table 3.
Changes in Inter-eye difference after SGB.
| T3 |
T5 |
T10 |
T15 |
F |
|
|---|---|---|---|---|---|
| N = 52 | |||||
| B-IED | 0.87 ± 0.47 | 1.27 ± 0.44**# | 1.41 ± 0.47**# | 1.44 ± 0.51**# | 37.60 |
| O-IED | 0.16 ± 0.26 | 0.22 ± 0.35 | 0.28 ± 0.46 | 0.24 ± 0.44 | 1.76 |
| N = 8 | |||||
| B-IED | 0.36 ± 0.39 | 0.61 ± 0.62 | 0.71 ± 0.60 | 0.60 ± 0.46 | 4.69 |
| O-IED | 0.15 ± 0.14 | 0.21 ± 0.27 | 0.19 ± 0.28 | 0.19 ± 0.35 | 0.35 |
Note: **P < 0.01 vs T3; #P < 0.05 vs opposite side. Abbreviations: B-IED = Inter-eye difference before and after SGB of block side; O-IED = Inter-eye difference before and after SGB of opposite side; T3 = 3 min after SGB; T5 = 5 min after SGB; T10 = 10 min after SGB; T15 = 15 min after SGB.
3.2. Pupil diameter change as a reference value for evaluating SGB effectiveness
Out of 60 SGBs, 8 results without HS were negative, and 52 results with HS were positive. The performance of each parameter for evaluating SGB effectiveness was assessed using the AUC (Table 4). The best parameters for evaluating SGB effectiveness were BO-IED (AUC = 0.97) and B-IED (AUC = 0.92), both observed at 15 min after completion of SGB (Fig. 6). With a cutoff value of 0.5 mm, the sensitivity and specificity of the BO-IED at 15 min was 86.5 % and 100 %, respectively. As for the B-IED at 15 min, the sensitivity and specificity were 86.5 % and 87.5 % with a cutoff value of 0.8 mm.
Table 4.
AUC of pupil response parameters to help determination of the efficacy of SGB.
| AUC | P value | 95 % CI | Cut off value | Sensitivity (%) | Specificity (%) | ||
|---|---|---|---|---|---|---|---|
| T3 | B-IED(mm) | 0.83 | 0.0001 | 0.71–0.91 | > 0.6 | 67.3 | 87.5 |
| O-IED(mm) | 0.64 | 0.11 | 0.51–0.76 | ||||
| BO-IED(mm) | 0.93 | 0.0001 | 0.84–0.98 | > 0.40 | 73.1 | 100 | |
| T5 | B-IED(mm) | 0.87 | 0.00 | 0.76–0.95 | > 0.5 | 94.2 | 75.0 |
| O-IED(mm) | 0.56 | 0.57 | 0.43–0.69 | ||||
| BO-IED(mm) | 0.94 | 0.00 | 0.85–0.98 | > 0.30 | 94.2 | 100 | |
| T10 | B-IED(mm) | 0.89 | 0.00 | 0.78–0.96 | > 0.6 | 94.2 | 75.0 |
| O-IED(mm) | 0.57 | 0.55 | 0.43–0.69 | ||||
| BO-IED(mm) | 0.94 | 0.00 | 0.85–0.99 | > 0.50 | 86.5 | 100 | |
| T15 | B-IED(mm) | 0.92 | 0.00 | 0.82–0.98 | > 0.8 | 86.5 | 87.5 |
| O-IED(mm) | 0.58 | 0.51 | 0.45–0.71 | ||||
| BO-IED(mm) | 0.97 | 0.00 | 0.89–0.99 | > 0.50 | 86.5 | 100 |
Note: AUC = area under the receiver operating characteristic curve; B-IED = Inter-eye difference before and after SGB of block side; O-IED = Inter-eye difference before and after SGB of opposite side; BO-IED = Inter-eye difference between block side and opposite side PD; T3 = 3 min after SGB; T5 = 5 min after SGB; T10 = 10 min after SGB; T15 = 15 min after SGB.
Fig. 6.
The sensitivity and specificity of the B-IED and BO-IED. (A) Receiveroperating characteristic curve of the changes in PD of block side at 15 min after SGB. The maximum area under the curve were 0.92 (95 % Confidence interval (CI), 0.82–0.98; P < 0.01). With a cutoff value of B-IED > 0.8 mm, the sensitivity and specificity of B-IED was 86.5 % and 87.5 %. (B) Receiveroperating characteristic curve of BO-IED at 15 min after SGB. The maximum area under the curve were 0.97 (95 % Confidence interval (CI), 0.89–0.99; P < 0.01). With a cutoff value of BO-IED > 0.5 mm, the sensitivity and specificity of BO-IED was 86.5 % and 100 %. HS positive, n = 52; HS negative, n = 8.
3.3. Relationship between inter-eye difference and changes in patients' symptom scores
When the change in the block side PD and their VAS scores were measured, a positive linear correlation was found. In 60 patients, VAS scores decreased as the block side PD decreased. The correlation coefficient (r) was 0.823 for patients with neuralgia, 0.945 for patients with cervical spondylosis, 0.935 for patients with tinnitus, and 0.843 for patients with insomnia, with some variability in the strength of the correlation between patients with different diagnoses (Fig. 7).
Fig. 7.
Correlation between T15 B-IED and changes in patients' symptom scores. Note: T15 B-IED = Inter-eye difference before and 15 min after SGB of block side. Symptom scores = pre VAS score – post VAS score. (A) Pain scores in Neurodynia, n = 28. Some of the data points are so close that they appear to overlap. (B) Pain scores in Cervical spondylosis, n = 10. Some of the data points are so close that they appear to overlap. (C) Tinnitus scores in Tinnitus, n = 11. (D) Insomnia scores in Insomnia, n = 11. The red dots in the four figures represent HS negative, n = 8.
4. Discussion
To provide an objective basis for evaluating the effectiveness of SGB, our study used ultrasound to measure the precise changes in pupil diameter in SGB. The postganglionic fibers that innervate the eyes pass through the stellate ganglion to the superior cervical ganglion and are emitted by the superior cervical ganglion. Therefore, accurate and complete stellate ganglion block can lead to Horner's syndrome, which is now widely recognized as the method for judging the effectiveness of SGB block. In clinical work, patients often have factors that affect doctors' subjective observation, such as acquired ptosis, which is more common in elderly women (Chaudhuri and Demer, 2013); the heaviness of the eyelids and redness caused by perimenopausal dry eye syndrome (Garcia-Alfaro et al., 2021); cases of physical eye injuries, etc. At the same time in bright light, parasympathetic tone is maximal and sympathetic tone is minimal, when differences in pupils are observed under the naked eye, unequal pupils may be overlooked (Martin, 2018).
The resting pupil diameter before SGB measured in this test was 4.84 ± 0.57 mm and 4.86 ± 0.56 mm on both sides respectively, which is close to the findings of Schmidt et al. (2017) and Farina et al. (2021), which illustrates the feasibility of using ultrasound method to measure the pupil in stellate ganglion block and the reliability of the data. Pupil light reflex is a contractile response of the eye after external light enters the eye, which responds to the optical properties of the human eye. Previous studies have shown that parasympathetic modulation plays a major role in pupil light reflex, while sympathetic nerves innervating the pupil opening muscles play a weak role in the contraction of the pupil light reflex (Marumo and Nakano, 2021). In this experiment, the stellate ganglion belongs to the sympathetic nerves in the neck, and after performing SGB, the ultrasonic measured contraction rate of the pupil to light reflex on both sides did not change before and after the block, which is in line with the results of the above studies.
Of the 60 patients in this trial, 52 developed HS, and their results showed that the block side was reduced at each time points compared with baseline, which is consistent with the successful development of HS and miosis with SGB block. The magnitude of pupil constriction on the blocked side increased with time, and PD was reduced by an average of 1.44 mm after 15 min compared with baseline, reaching the maximum value in this study. The difference in PD between the two sides also increased with time, reaching the maximum value of 1.02 mm at 15 min after block, which may be related to the diffusion of local anesthetics, which took some time to diffuse to the stellate ganglion under the anterior fascia of the vertebrae, and at the same time, some of the drugs may be injected in the longissimus dorsi muscle, which prolonged the diffusion time of the drugs. The pupil in opposite side was also reduced at each time points compared with baseline, with an average reduction in diameter of between 0.16 and 0.28 mm, which did not change over time. A possible explanation for the slight reduction of the pupil in opposite side is that for the whole body of the nervous system, SGB blocks a part of the sympathetic nerves, resulting in parasympathetic dominance for a certain period, which causes a small reduction of the contralateral pupil. In subsequent trials, we will conduct heart rate variability monitoring to verify this point. However, the phenomenon of contralateral pupil narrowing after SGB has not been reported in the previous literature, and there are many factors that influence sympathetic and parasympathetic input to the pupil, including the amount of light entering the eyes, the state of accommodative tone, but also emotional factors, systemic medications, and disease states (Castaldi et al., 2021), so the possible mechanisms need to be further investigated.
The results of this trial showed that the AUC of BO-IED to evaluate the SGB effectiveness was greater than 0.9 at all-time points, and the AUC of B-IED was greater than 0.8, indicating that the sensitivity of ultrasound pupil measurements is reliable. Yoo et al. (2017) used digital pupillometers in a study of 19 patients with unilateral Horner's syndrome, and their findings showed that the pupil diameters of the affected eye and contralateral eye and the total time for the pupil to return from peak constriction to 75 % of its maximum pupil diameter during light reflex (T75) showed significant differences at baseline examination. The diagnostic criteria for Horner syndrome relying on baseline pupillary measurements was defined as one of the two major findings; firstly, small maximal pupil diameter with inter-eye difference of > 0.5 mm, and secondly, T75 > 2.61 s in the affected eye. The BO-IED critical values of 0.3–0.5 mm at each time point in this trial are close to the study of Yoo et al. (2017). It can be used as a reference for assessing the validity of SGB. The area under the curve of BO-IED versus effective SGB at 15 min after block was the maximum of 0.97, and at this time, the sensitivity of BO-IED for evaluating the effectiveness of SGB block was 86.5 % and the specificity was 100 %. Therefore, the difference between the left and right pupil diameters of more than 0.5 mm at 15 min after SGB is a reliable and objective basis for assessing the effectiveness of SGB.
Eight patients in this trial did not develop HS, some of whom only exhibited one or two components of the Horner’s triad. Among these, one patient only developed a brachial plexus block and experienced no change in VAS score, leading the observers to judge the block as ineffective, classified as negative. In this trial, 1 % lidocaine 4 mL was used for the block according to previous literature (Fujiwara et al., 2016, Kim et al., 2017, Yoo et al., 2019) and was not individualized according to the patient's height, weight, neck circumference and neck length, which may be the reason for the failure of the block. Notably, in 3 patients, although ultrasound observation revealed a PD difference exceeding 0.5 mm before and after SGB, the observing personnel only found one or two of the signs of Horner’s triad, thus judging the block as ineffective. However, the VAS score did decrease in these three patients. From our statistical results, there was a positive correlation between the reduction of the PD and the patient's VAS score, so we judged that the observation of Horner's syndrome is more subjective, and it is inaccurate to judge the effectiveness of the SGB based solely on visual observation, while judging the therapeutic effect of the SGB based on the change of the pupil under ultrasound is more objective and clinically significant.
One limitation of this study is the small sample size due to the pilot nature of this study. A second limitation of this study was no comparison of pupillary changes before and after SGB with different volumes and local anesthetics. The third limitation is that our follow-up period was only 24 h post-SGB, which is short. Long-term outcomes could provide more comprehensive insights. The fourth limitation is that although the observer was the same doctor, there may still be observer bias. Regarding the limitation of using a single metric, this is indeed a limitation of this trial. We will include additional metrics such as ear lobe sweating index, nasal congestion, and temperature difference in future studies. The optimal BO-IED cutoff (0.5 mm) is derived from a single lidocaine dose (4 mL of 1 %). Volume/concentration variations may alter cutoff validity. We acknowledge this limitation and test robustness at different doses in future work.
5. Conclusion
When the difference in pupil diameter between the two sides measured by ultrasound is greater than 0.5 mm after 15 min of SGB using 4 mL of 1 % lidocaine, it can be used as an objective basis for assessing the effectiveness of stellate ganglion block.
Author contributions
This study was designed by Z-H.F., J-X.Y. and H-L.Z. The experiments were performed by Z-H.F., J-X.Y. and Y.N. The data were analyzed by Z-H.F., and the results were critically examined by all authors. Z-H.F. had a primary role in preparing the manuscript, which was edited by J-X.Y. and H-L.Z. All authors have approved the final version of the manuscript and agree to be accountable for all aspects of the work
CRediT authorship contribution statement
Zhu-Hong Fang: Writing – original draft, Investigation, Conceptualization. Yong Ni: Investigation. Hai-Long Zhang: Writing – review & editing, Investigation, Conceptualization. Hong Xie: Methodology. Jia-Xuan Yang: Writing – review & editing, Investigation, Conceptualization.
Ethics Approval and consent to participate
This project has been reviewed and approved by the Ethics Committee of the Second Affiliated Hospital of Soochow University (No. JD-LK-2022–027–02). This project was re-registered on 27 October 2022 on the China Clinical Trial Centre website (No. ChiCTR2200064945, https://www.chictr.org.cn/).
Funding
This research received no external funding.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors gratefully thank the doctors in the pain department and anesthesiology department of the Second Affiliated Hospital of Soochow University, for their kind support in this research.
Contributor Information
Hong Xie, Email: hongx93044@126.com.
Hai-Long Zhang, Email: hlzhang76@suda.edu.cn.
Jia-Xuan Yang, Email: youngjason@163.com.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
- Castaldi E., Pome A., Cicchini G.M., Burr D., Binda P. The pupil responds spontaneously to perceived numerosity. Nat. Commun. 2021;12:5944. doi: 10.1038/s41467-021-26261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhuri Z., Demer J.L. Sagging eye syndrome: connective tissue involution as a cause of horizontal and vertical strabismus in older patients. JAMA Ophthalmol. 2013;131:619–625. doi: 10.1001/jamaophthalmol.2013.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doytchinova A., Hassel J.L., Yuan Y., Lin H., Yin D., Adams D., Straka S., Wright K., Smith K., Wagner D., et al. Simultaneous noninvasive recording of skin sympathetic nerve activity and electrocardiogram. Heart Rhythm. 2017;14:25–33. doi: 10.1016/j.hrthm.2016.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farina F., Brunner C., Schreiber S.J., Palmieri A., Struhal W., Baracchini C., Vosko M.R. Ultrasound examination of the pupil suggestive for carotid dissection. Neurology. 2017;89:973–974. doi: 10.1212/WNL.0000000000004299. [DOI] [PubMed] [Google Scholar]
- Farina F., Vosko M.R., Baracchini C., Ermani M., Sommer P., Greisenegger S., Laubichler P., Struhal W., Kellermair L., Ransmayr G., et al. Ultrasound examination of the pupil - a new tool for the neuro-ophthalmological assessment. Ultraschall Med. 2021;42:84–91. doi: 10.1055/a-1208-1482. [DOI] [PubMed] [Google Scholar]
- Fujiwara S., Komasawa N., Kido H., Minami T. A rare case of accidental arterial local anesthetic injection under ultrasound-guided stellate ganglion block. J. Clin. Anesth. 2016;29:3–4. doi: 10.1016/j.jclinane.2015.10.010. [DOI] [PubMed] [Google Scholar]
- Garcia-Alfaro P., Garcia S., Rodriguez I., Verges C. Dry eye disease symptoms and quality of life in perimenopausal and postmenopausal women. Climacteric. 2021;24:261–266. doi: 10.1080/13697137.2020.1849087. [DOI] [PubMed] [Google Scholar]
- Kim W.J., Park H.S., Yi M.S., Koo G.H., Shin H.Y. Evaluation of lung function and clinical features of the ultrasound-guided stellate ganglion block with 2 different concentrations of a local anesthetic: a randomized controlled trial. Anesth. Analg. 2017;124:1311–1316. doi: 10.1213/ANE.0000000000001945. [DOI] [PubMed] [Google Scholar]
- Kim Y.U., Cheong Y., Kong Y.G., Lee J., Kim S., Choi H.G., Suh J.H. The prolongation of pulse transit time after a stellate ganglion block: An objective indicator of successful block. Pain. Res Manag. 2015;20:305–308. doi: 10.1155/2015/324514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusayama T., Wong J., Liu X., He W., Doytchinova A., Robinson E.A., Adams D.E., Chen L.S., Lin S.F., Davoren K., et al. Simultaneous noninvasive recording of electrocardiogram and skin sympathetic nerve activity (neuECG) Nat. Protoc. 2020;15:1853–1877. doi: 10.1038/s41596-020-0316-6. [DOI] [PubMed] [Google Scholar]
- Martin T.J. Horner syndrome: a clinical review. ACS Chem. Neurosci. 2018;9:177–186. doi: 10.1021/acschemneuro.7b00405. [DOI] [PubMed] [Google Scholar]
- Marumo C., Nakano T. Early phase of pupil dilation is mediated by the peripheral parasympathetic pathway. J. Neurophysiol. 2021;126:2130–2137. doi: 10.1152/jn.00401.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitahara K., Dan K. Blood flow velocity changes in carotid and vertebral arteries with stellate ganglion block: measurement by magnetic resonance imaging using a direct bolus tracking method. Reg. Anesth. Pain. Med. 1998;23:600–604. doi: 10.1016/s1098-7339(98)90088-8. [DOI] [PubMed] [Google Scholar]
- Sahin O.F., Tarikci Kilic E., Aksoy Y., Kaydu A., Gokcek E. The importance of perfusion index monitoring in evaluating the efficacy of stellate ganglion blockage treatment in Raynaud's disease. Libyan J. Med. 2018;13 doi: 10.1080/19932820.2017.1422666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samen C.D.K., Sutton O.M., Rice A.E., Zaidi M.A., Siddarthan I.J., Crimmel S.D., Cohen S.P. Correlation between temperature rise after sympathetic block and pain relief in patients with complex regional pain syndrome. Pain. Med. 2022;23:1679–1689. doi: 10.1093/pm/pnac035. [DOI] [PubMed] [Google Scholar]
- Schmidt F.A., Ruprecht K., Connolly F., Maas M.B., Paul F., Hoffmann J., Harms L., Schreiber S.J. B-mode ultrasound assessment of pupillary function: Feasibility, reliability and normal values. PLoS One. 2017;12 doi: 10.1371/journal.pone.0189016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamazaki H., Nishiyama J., Suzuki T. Use of perfusion index from pulse oximetry to determine efficacy of stellate ganglion block. Local Reg. Anesth. 5. 2012:9–14. doi: 10.2147/LRA.S30257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang R.Z., Li Y.Z., Liang M., Yu J.J., Chen M.L., Qiu J.J., Lin S.Z., Wu X.D., Zeng K. Stellate ganglion block improves postoperative sleep quality and analgesia in patients with breast cancer: a randomized controlled trial. Pain. Ther. 2023;12:491–503. doi: 10.1007/s40122-022-00473-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo Y., Lee C.S., Kim Y.C., Moon J.Y., Finlayson R.J. A randomized comparison between 4, 6 and 8 ml of local anesthetic for ultrasound-guided stellate ganglion block. J. Clin. Med. 2019;8 doi: 10.3390/jcm8091314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo Y.J., Yang H.K., Hwang J.M. Efficacy of digital pupillometry for diagnosis of Horner syndrome. PLoS One. 2017;12 doi: 10.1371/journal.pone.0178361. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.