Abstract
Introduction
Plasma ablation tonsillectomy has rapidly increased in popularity and is now the most popular technique in children. This study aims to evaluate the impact of plasma ablation tonsillectomy on the incidence of post-operative haemorrhage requiring surgical intervention in children, a complication affecting patient safety and healthcare resource utilisation.
Methods
15 years (2009/10–2023/24) of Hospital Episode Statistics for children 14 years or under, capturing all tonsillectomies in NHS England hospitals was analysed. The proportion performed by plasma ablation and rate of surgical intervention for post-tonsillectomy haemorrhage were calculated. Pearson’s Correlation Coefficient was used to statistically analyse the relationship.
Results
Data from 359,241 tonsillectomies was analysed. The proportion of tonsillectomies performed with plasma ablation has grown yearly from 7% in 2009/10–47% in 2023/24. A change in trend in the rate of return to theatre for haemorrhage control was not identified across the study period. (Pearson Correlation Coefficient −0.15, p = 0.59).
Conclusion
These findings do not support a superior safety profile of plasma ablation tonsillectomy with regard to post-operative haemorrhage. However, due to dataset limitations it was not possible to analyse intracapsular and extracapsular procedures independently. There remains a need for continued evaluation of tonsillectomy techniques to inform optimal surgical practice.
Introduction
Background and rationale
Tonsillectomy is one of the most commonly performed operations with approximately 40–50,000 procedures performed annually in the UK National Health Service with more than half of all cases performed in children. Common indications are recurrent tonsillitis and paediatric obstructive sleep apnoea. Morbidity associated with tonsillectomy includes post-operative haemorrhage (primary within 24 hours, or secondary from 24 hours to 28 days post-operatively [1]) from the tonsillar bed which can potentially be profuse, leading to airway and circulatory crisis. Minor bleeding is not uncommon, with one study reporting a 44% incidence of ‘blood in saliva’ or greater [2]. Conservative management may be appropriate for minor bleeds but post-tonsillectomy haemorrhage may require an emergency return to theatre for haemorrhage control, especially in younger children with lower circulating blood volume.
Techniques for tonsillectomy have been widely debated. Factors affecting choice of surgical technique include patient outcomes, cost, duration of procedure, environmental impact and surgeon preference. ‘Plasma ablation’ (Coblation®, Smith&Nephew) is a technology that utilises a single use ‘wand’ to create a plasma field. This allows precise disintegration of tissues with significantly lower thermal exposure than techniques such as bipolar, monopolar or laser dissection [1,3]. Plasma ablation tonsillectomy can be performed through extracapsular dissection (the same dissection plane as traditional cold steel or bipolar technique) or the more recently developed intracapsular ablation of tonsillar tissue which avoids disruption to the tonsillar capsule. Preservation of the capsule is thought to minimise trauma to underlying nerves and larger vessels resulting in a reduction in postoperative pain and reduced incidence of post-tonsillectomy haemorrhage [4].
Tonsillectomy has been shown in the recent NAtional Trial of Tonsillectomy IN Adults (NATTINA) to be a clinically effective and cost-effective way of managing recurrent acute tonsillitis [5]. The National Prospective Tonsillectomy Audit (NPTA) was performed in 2003, with results showing primary bleed rates across all techniques of 0.6% and secondary bleed rates of 3% [6]. Total tonsillar haemorrhage rates reported by the NPTA were most favourable for cold steel at 1.7%, with bipolar diathermy forceps 4.6% and extracapsular plasma ablation 4.6%. Return to theatre rates were 0.8% for cold steel, 1.0% for bipolar diathermy forceps and 1.8% for extracapsular plasma ablation [6]. A subsequent Cochrane systematic review reported a non-statistically significant elevated secondary bleeding risk with extracapsular plasma ablation with absolute risk of 5% in the plasma ablation group vs 3.6% in the control group [7].
Since these publications the intracapsular plasma ablation tonsillectomy technique has grown in popularity with evidence suggesting that compared to extracapsular plasma ablation it results in reduced late post-operative pain and a much lower incidence of post-tonsillectomy haemorrhage [8]. A single surgeon case series of 1,257 paediatric patients who underwent intracapsular plasma ablation reports a post-tonsillectomy haemorrhage rate of 0.5% with 0% requiring return to theatre [9]. A retrospective cohort study of four centres exclusively performing paediatric plasma ablation tonsillectomy reports a return to theatre rate for primary haemorrhage of 0.1% and of secondary haemorrhage of 0.2% [10]. Due to such promising data, intracapsular plasma ablation has been promoted in national guidance and it has been steadily growing in popularity in United Kingdom paediatric tonsillectomy practice [11].
Hospital Episode Statistics (HES) refer to routinely collected data for all UK National Health Service (NHS) care episodes in England, including elective and emergency care, capturing demographic information, diagnoses and procedures. This anonymised data is published annually and made publicly available by NHS Digital.
The aim of this study was to use HES data to assess UK trends in paediatric tonsillectomy practice and to assess if the reported reduction in post-tonsillectomy haemorrhage rate is reflected in national level data.
Objectives
To assess the trend in the use of plasma ablation tonsillectomy in the UK over the last 15 years.
To evaluate the association between the increased use of plasma ablation tonsillectomy and the rate of return to theatre for post-tonsillectomy haemorrhage.
To evaluate the association between increased use of plasma ablation tonsillectomy and rates of surgery to remove remnant tonsils.
Hypothesis
As the proportion of tonsillectomies performed by plasma ablation increases the rate of return to theatre for arrest of post-tonsillectomy haemorrhage will decrease.
As the proportion of tonsillectomies performed by plasma ablation increases the rate of excision of tonsillar remnants will increase.
Methods
Study design & setting
This study employed a historical observational design utilising publicly available routinely collected data over a sequential 15-year period from the United Kingdom National Health Service (NHS). This approach allowed for the examination of long-term trends and outcomes associated with different tonsillectomy techniques providing insights into surgical practice and patient outcomes. We have reported our findings in accordance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Participants
Hospital Episode Statistics (Admitted Patient Care Dataset) was accessed providing fifteen sequential years of data capturing all NHS England hospital care episodes including day case surgery from years 2009/10–2023/24 [12]. Only data for patients 14 years or under was extracted for analysis in the study. 14 years of age was chosen as datasets from 2011/12 and earlier grouped 15- and 16-year-olds together with adults rather than children. Data extracted included total number of tonsillectomy procedures by technique and complications of surgical arrest of postoperative bleeding from tonsillar bed and excision of remnant tonsil.
Ethical considerations
HES data does not include patient identifiable information and no additional data collection was performed. Therefore no significant ethical concerns were identified and formal ethical approval was not sought.
Variables
Data detailing annual tonsillectomy procedures performed across several techniques, including dissection, guillotine, laser, excision not elsewhere classified (NEC), and plasma ablation as available from HES data.
Bias
Given the historical nature of the study and the reliance on existing records for data collection, several sources of bias were considered:
Selection Bias: The study population was derived from a dataset that included all patients undergoing tonsillectomy within the specified time frame. This approach minimises the risk of selection bias related to the inclusion criteria, however varying geographical preferences for surgical technique could introduce bias. Specifically, the decision to use plasma ablation versus other tonsillectomy techniques may be influenced by institutional practices or surgeon preferences/case volume, which are not accounted for in our dataset.
Information Bias: Inaccuracies in clinical coding could lead to misclassification bias, for example revision surgery for tonsillar remnant may be incorrectly recorded as a primary procedure by whichever technique was used.
Confounding Bias: The absence of individual patient-level data, such as age, sex, and indication for tonsillectomy, limits our ability to adjust for possible confounding factors. These unmeasured confounders could influence both the choice of tonsillectomy technique and the risk of postoperative haemorrhage.
Study size
The size of our study cohort was determined by the availability of recorded data within the specified timeframe.
Data handling and statistical methods
The total number of tonsillectomies was calculated by summing figures for OPCS (Office for Population and Censuses Surveys) codes F34.1 (Bilateral dissection tonsillectomy), F34.2 (Bilateral guillotine tonsillectomy), F34.3 (Bilateral laser tonsillectomy), F34.4 (Bilateral excision of tonsil NEC) and F34.7 (Bilateral coblation tonsillectomy). Percentages were calculated each year for numerators of F34.7 (Bilateral coblation tonsillectomy) and F36.5 (Surgical arrest of postoperative bleeding from tonsillar bed). For the final 2023/24 dataset, in addition to the code F34.7 (Bilateral coblation tonsillectomy, n = 8005) additional codes were introduced not found in previous years. These were F35.1 (Bilateral intracapsular tonsillectomy NEC, n = 213), F35.2 (Bilateral intracapsular coblation tonsillectomy, n = 4080), F35.8 (Other specified intracapsular excision of tonsil, n = 17) and F35.9 (Unspecified intracapsular excision of tonsil, n = 23). Absolute numbers for non-plasma ablation intracapsular procedures (F35.1, F35.8 and F35.9) are very low and we suspect these represent coding errors for intracapsular plasma ablation procedures as non-plasma ablation intracapsular tonsillectomy does not represent typical practice. Therefore these four codes were summed to represent intracapsular coblation tonsillectomy and these numbers were added to F34.7 to calculate the total number of coblation tonsillectomies that year to allow comparison with datasets from previous years.
To assess the association between the use of plasma ablation tonsillectomy and (a) the rate of return to theatre for post-tonsillectomy haemorrhage and (b) excision of remnant tonsil, Pearson’s correlation coefficient was calculated to quantify the strength and direction of association between variables. Statistical analyses were conducted using Python, and a two-tailed p-value <0.05 was considered statistically significant.
Results
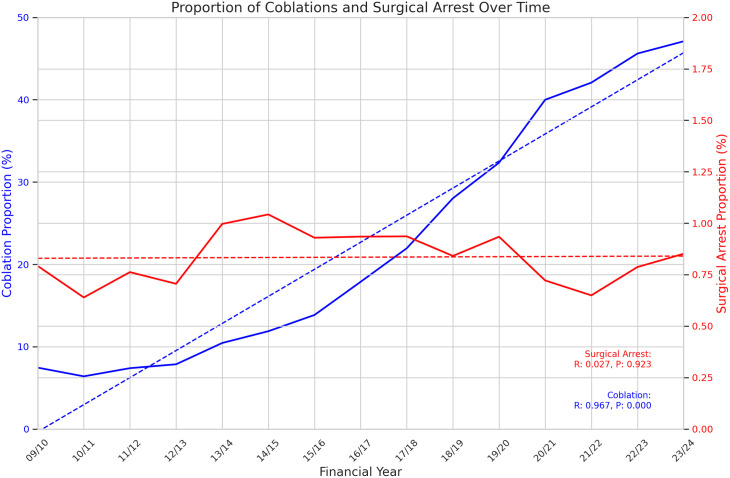
359,241 tonsillectomies were included over the fifteen years of study data. Data are summarised in Table 1. Total tonsillectomies fell sharply for the year 2020/2021 before recovering in the subsequent two years. The proportion of tonsillectomies performed with plasma ablation technique hovered around 7% until 2011/12, after which it has risen steadily year on year up to 47.1% in 2022/23, now representing the single most frequently used technique. (See Fig 1) The rate of return to theatre for arrest of postoperative haemorrhage hovered around 0.7% for the first four years of data before jumping to 1% in 2013/14. It stayed between 0.84% and 1.04% for the next 6 years, before dipping in 2020/21 and 2020/22 before rising again to 0.79% in 2022/23 and 0.85% in 2023/24. (See Fig 2) Pearson’s Correlation Coefficient was calculated as −0.15 (p = 0.59) indicating no clear correlation between use of plasma ablation technique tonsillectomy and rate of return to theatre for control of post-tonsillectomy haemorrhage. Excision of remnant tonsil (F34.5) rate demonstrated a non-statistically significant moderate upward trend over the study period (Pearson Correlation Coefficient 0.42, p = 0.11) with low absolute numbers (range 4–23). (See Fig 3) Data from 2023/24 includes new OPCS codes as explained above and confirms at least 33% of plasma ablation tonsillectomies were performed with intracapsular technique.
Table 1. Annual Tonsillectomy Procedures and Proportions.
| Year | Dissection | Guillotine | Laser | Excision NEC | Plasma ablation | Total Procedures | % Plasma ablation | % Dissection | % Return to theatre |
|---|---|---|---|---|---|---|---|---|---|
| 2009/10 | 21,854 | 198 | 14 | 2,576 | 1,985 | 26,627 | 7.45% | 82.07% | 0.79% |
| 2010/11 | 21,281 | 120 | 21 | 2,302 | 1,621 | 25,345 | 6.40% | 83.97% | 0.63% |
| 2011/12 | 20,725 | 147 | 41 | 2,415 | 1,861 | 25,189 | 7.39% | 82.28% | 0.76% |
| 2012/13 | 20,862 | 101 | 21 | 2,653 | 2,016 | 25,653 | 7.86% | 81.32% | 0.71% |
| 2013/14 | 22,332 | 120 | 11 | 2,884 | 2,957 | 28,304 | 10.45% | 78.90% | 1.00% |
| 2014/15 | 22,436 | 149 | 12 | 2,762 | 3,418 | 28,777 | 11.88% | 77.97% | 1.04% |
| 2015/16 | 21,218 | 113 | 15 | 2,571 | 3,845 | 27,762 | 13.85% | 76.43% | 0.93% |
| 2016/17 | 19,610 | 99 | 14 | 3,034 | 4,954 | 27,711 | 17.88% | 70.77% | 0.93% |
| 2017/18 | 18065 | 91 | 25 | 2,165 | 5,723 | 26,069 | 21.93% | 69.30% | 0.94% |
| 2018/19 | 16,276 | 86 | 32 | 2,348 | 7,299 | 26,041 | 28.03% | 62.50% | 0.84% |
| 2019/20 | 13,558 | 63 | 16 | 2,078 | 7,514 | 23,229 | 32.35% | 58.37% | 0.93% |
| 2020/21 | 4,180 | 52 | 6 | 917 | 3,436 | 8,591 | 40.00% | 48.66% | 0.72% |
| 2021/22 | 6,874 | 34 | 8 | 1,737 | 6,285 | 14,938 | 42.07% | 46.02% | 0.65% |
| 2022/23 | 7,970 | 27 | 12 | 2,220 | 8,577 | 18,806 | 45.61% | 42.38% | 0.79% |
| 2023/24 | 11,199 | 21 | 18 | 2,623 | 12,338* | 26,199 | 47.09% | 42.75% | 0.85% |
Note: The “%” columns for Plasma ablation and Dissection are calculated as the proportion of those techniques relative to the total procedures performed each year. NEC, Not Elsewhere Classified. *Please see ‘Data handling and statistical methods’.
Fig 1. Annual number of paediatric tonsillectomies by technique.
The proportion of tonsillectomies performed by plasma ablation technique has risen steadily from 6.4% in 2010/11 to 47.1% in 2023/24.
Fig 2. Proportion of surgical arrests of post-tonsillectomy haemorrhage and proportion of plasma ablation tonsillectomies over time.
Pearson Correlation Coefficient −0.15, p = 0.59.
Fig 3. Proportion of remnant tonsil excision and plasma ablation tonsillectomies over time.
Pearson Correlation Coefficient 0.42, p = 0.11.
Discussion
This analysis of national routinely collected data has shown that the proportion of paediatric tonsillectomies performed by plasma ablation technique in the United Kingdom has been steadily rising however a fall in the return to theatre rate for post-tonsillectomy haemorrhage rate has not been identified. Indeed, the return to theatre rate was higher in 2023/24 when nearly half of paediatric tonsillectomies were performed by plasma ablation compared to 2010/11 when only 6% of tonsillectomies were performed by plasma ablation. There was a small drop in return to theatre rate in 2020/21 and 2021/22, which likely represents a predilection for conservative management during the covid-19 pandemic. It is noteworthy that there was also no positive correlation identified suggesting plasma ablation is not an inferior technique with regard to post-tonsillectomy haemorrhage.
A key point of discussion with this analysis is that HES data does not distinguish between extracapsular dissection and intracapsular ablation approaches of using plasma ablation with only a single code for ‘Coblation tonsillectomy’ (F34.7) for datasets prior to 2023/24. The previously published studies supporting lower rates of post-tonsillectomy haemorrhage with plasma ablation technique are only in support of the intracapsular approach [9,10]. We may therefore not be seeing return to theatre rates fall if the benefits of intracapsular plasma ablation are being masked by a large proportion of extracapsular plasma ablation procedures which are reported to carry an increased bleeding risk [6,7]. For the 2023/24 dataset, as well as F34.7, new codes for intracapsular procedures have been introduced. This follows calls for HES data to provide better granularity on plasma ablation technique [10,11,13]. Unfortunately despite confirming at least 33% of plasma ablation tonsillectomies were performed with intracapsular technique, these do not facilitate confirmation of whether the remaining plasma ablation procedures were intracapsular or extracapsular as F34.7 ‘Bilateral coblation tonsillectomy’ was still included. However, even accounting for a proportion of extracapsular procedures in the plasma ablation group, we are surprised not to identify some degree of trend considering the strength of the previously published data in favour of the intracapsular technique [9,10].
We suspect most of the procedures represented by F34.7 are intracapsular as the increased bleeding risk for extracapsular technique was reported by the NPTA four years prior to our study period beginning. We think it unlikely surgeons or industry taught courses would promote what is established to be an inferior technique [6]. Furthermore, for the 2023/24 dataset, the new OPCS codes will be unfamiliar to surgeons and theatre staff and we suspect many will continue to code as they did previously, therefore under-reporting the proportion of intracapsular plasma ablation procedures. We cannot be sure of this however and if a significant proportion of the plasma ablation group is in fact extracapsular then this would affect our conclusions. We would encourage all surgeons to ensure their procedures are accurately coded to allow future HES data to be best utilised for analysing different techniques of plasma ablation tonsillectomy. We would also recommend for OPCS code F34.7 ‘Bilateral coblation tonsillectomy’ to be removed and replaced with ‘Bilateral extracapsular coblation tonsillectomy’ so in conjunction with the new 2023/24 codes the number of procedures performed by each technique is clear.
It is recognised that optimal use of plasma ablation has a learning curve, and a possible influence on the data is that as the technique grows in popularity there may be more novice operators failing to achieve optimal results [14]. However this would only apply to a small subset of plasma ablation operations and should also be balanced by a corresponding increase in the number of experienced operators performing or supervising tonsillectomies.
Another explanation for the data is that the benefits of plasma ablation technique could be masked if the return to theatre rate for non-plasma ablation techniques such as bipolar dissection has risen. For example if trainees or less experienced surgeons who fail to achieve optimal results prefer traditional techniques this may increase the bleed rate in the data. However, we would expect that while under supervision trainees would adopt and learn the preferred technique of their supervisor. It could also be suggested that more challenging cases with a higher rebleed risk such as those of recurrent quinsy are less likely to be performed with plasma ablation. While for such situations this is probably the case it would only infrequently apply to a paediatric population 14 years and under.
An advantage of this analysis is that we have a very large dataset including all tonsillectomies in NHS England hospitals for children 14 years and under over a sequential fifteen-year period. This gives excellent power to the study for detecting a real change if one is present. Furthermore, the existing evidence base originates from a small number of expert centres for which there may be factors within such a set up that limit external validity. This study uses national level data and therefore represents the heterogeneity of real-world usage of coblation tonsillectomy.
The upward trend in rate of ‘Remnant tonsil excision’ (F34.5) demonstrated considerable variation and did not reach statistical significance. We suspect the very low absolute numbers partially reflect inaccurate coding of re-excisions as primary procedures instead of F34.5. A lag time of multiple years is to be expected between a primary procedure and a re-excision procedure. We therefore feel this outcome is inadequately assessed by the current study. However, a non-statistically significant moderate upward trend was identified and we recommend that this outcome continues to be monitored.
Conclusion
Despite the theoretical advantages of plasma ablation, this study of a fifteen-year dataset of paediatric tonsillectomies across NHS hospitals in England has not supported its adoption being linked with a reduction in the rate of surgical intervention for post-tonsillectomy haemorrhage. As it has not been possible to separate intracapsular from extracapsular procedures we cannot conclude that intracapsular plasma ablation does not have a lower return to theatre rate, however this reported advantage has not been corroborated in this national level dataset. Considering the enormous case load of tonsil surgery and in view of the additional financial and environmental costs of coblation technique, our findings suggest that carefully designed large studies are justified to clarify the evidence base around optimal tonsillectomy technique.
Key points
Tonsil surgery is very common with post-operative bleeding from the tonsillar bed being a potentially life threatening complication
Current evidence points to a lower incidence of post-tonsillectomy haemorrhage with intracapsular plasma ablation tonsillectomy compared to extracapsular techniques
This analysis of 15 years of national level paediatric tonsillectomy data has not identified a correlation between the rising popularity of plasma ablation technique tonsillectomy and falling return to theatre rates for post-tonsillectomy haemorrhage
Differentiating between intracapsular and extracapsular plasma ablation technique in this dataset has not been possible which limits the certainty of the conclusions
Supporting information
(PDF)
Data Availability
All data available from NHS Digital. Hospital Admitted Patient Care Activity. Available: https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Metcalfe C, Muzaffar J, Daultrey C, Coulson C. Coblation tonsillectomy: a systematic review and descriptive analysis. Eur Arch Otorhinolaryngol. 2017;274(6):2637–47. doi: 10.1007/s00405-017-4529-4 [DOI] [PubMed] [Google Scholar]
- 2.Heward E, Rocke J, McNally G, Thompson G, Oladokun D, Timms S, et al. The post-operative tonsillectomy (POPT) study: A multi-centre prospective paediatric cohort study. Clin Otolaryngol. 2024;49(2):176–84. doi: 10.1111/coa.14110 [DOI] [PubMed] [Google Scholar]
- 3.Smith and Nephew. Coblation Technology for Adenotonsillectomy. [Internet]. [cited 8/2/2024]. Available: https://www.smith-nephew.com/en-gb/health-care-professionals/products/ear-nose-and-throat/coblation-technology-for-adenotonsillectomy#overview
- 4.Roje Z, Racić G, Dogas Z, Pisac VP, Timms M. Postoperative morbidity and histopathologic characteristics of tonsillar tissue following coblation tonsillectomy in children: a prospective randomized single-blind study. Coll Antropol. 2009;33(1):293–8. [PubMed] [Google Scholar]
- 5.Wilson JA, O’Hara J, Fouweather T, Homer T, Stocken DD, Vale L, et al. Conservative management versus tonsillectomy in adults with recurrent acute tonsillitis in the UK (NATTINA): a multicentre, open-label, randomised controlled trial. Lancet. 2023;401(10393):2051–9. doi: 10.1016/S0140-6736(23)00519-6 [DOI] [PubMed] [Google Scholar]
- 6.The Royal College of Surgeons. National Prospective Tonsillectomy Audit. 2005 [cited March 2024]. Available from: https://www.rcseng.ac.uk/-/media/Files/RCS/Library-and-publications/Non-journal-publications/National-Prospective-Tonsillectomy-Audit-Final-Report-2005.pdf
- 7.Pynnonen M, Brinkmeier JV, Thorne MC, Chong LY, Burton MJ. Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev. 2017;8(8):CD004619. doi: 10.1002/14651858.CD004619.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daskalakis D, Tsetsos N, Karagergou S, Goudakos J, Markou K, Karkos P. Intracapsular coblation tonsillectomy versus extracapsular coblation tonsillectomy: a systematic review and a meta-analysis. Eur Arch Otorhinolaryngol. 2021;278(3):637–44. doi: 10.1007/s00405-020-06178-2 [DOI] [PubMed] [Google Scholar]
- 9.Amin N, Bhargava E, Prentice JG, Shamil E, Walsh M, Tweedie DJ. Coblation intracapsular tonsillectomy in children: A prospective study of 1257 consecutive cases with long-term follow-up. Clin Otolaryngol. 2021;46(6):1184–92. doi: 10.1111/coa.13790 [DOI] [PubMed] [Google Scholar]
- 10.Powell S, Tweedie DJ, Jonas NE, Bateman ND, Keltie K, Sims AJ. Coblation intracapsular tonsillectomy: A cohort study of NHS practice in England using Hospital Episode Statistics. Clin Otolaryngol. 2022;47(3):471–7. doi: 10.1111/coa.13929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marshall A. Ear, Nose and Throat Surgery: GIRFT Programme National Specialty Report. 2019 [cited 25 Jan 2024] Available from: https://gettingitrightfirsttime.co.uk/wp-content/uploads/2019/10/ENT-Report-Nov19-L-FINAL.pdf
- 12.NHS Digital. Hospital Admitted Patient Care Activity. [cited Jan 2024] Available from: https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity
- 13.NHS Digital. OPCS-4.9 to OPCS-4.10 Summary of Core Changes. 2022 [cited March 2024]. Available from: https://digital.nhs.uk/binaries/content/assets/website-assets/isce/0084/0084362022changesummary.pdf
- 14.Carney AS, Harris PK, MacFarlane PL, Nasser S, Esterman A. The coblation tonsillectomy learning curve. Otolaryngol Head Neck Surg. 2008;138(2):149–52. doi: 10.1016/j.otohns.2007.10.031 [DOI] [PubMed] [Google Scholar]