Abstract
Introduction:
Reducing the compression rotation interval from 2 to 1 minute is expected to improve cardiopulmonary resuscitation (CPR) quality. This meta-analysis aimed to assess the effect of altering the compression rotation interval on key CPR quality parameters, including compression depth, rate, and rescuer fatigue.
Methods:
We systematically searched MEDLINE, EMBASE, Scopus, Google Scholar, Web of Science, and the Cochrane Controlled Register of Trials from their inception to May 15, 2025. We searched for randomized controlled trials, simulation studies, and crossover studies that compared 1-min and 2-min compression rotation times. The assessed outcomes included compression depth, rate, correctness, and rescuer fatigue, which were reported as the standard mean difference (SMD) with a 95% confidence interval (95% CI).
Results:
One randomized controlled trial and seven randomized crossover studies, involving 668 rescuers in total, using manikins, were included. The 1-min rotation group exhibited significantly greater compression depth, with an increase of 2.06 mm (SMD = 2.06, 95% CI: 0.44–3.68, p < 0.001). This group demonstrated lower levels of fatigue, as indicated by a significant reduction on the visual analog scale for fatigue (SMD = −1.27, 95% CI: −2.24 to −0.30, p < 0.001). However, there were no significant differences in the compression rate or percentage of compressions that achieved adequate depth.
Conclusion:
It seems that altering the chest compression rotation interval from 2 min to 1 min improves the compression depth and reduces rescuer fatigue. However, parameters, such as the compression rate and compression adequacy, remained unchanged. Notably, all the studies were conducted on manikins, thus necessitating further research to assess the applicability of these changes in real-world clinical settings.
Key Words: Cardiopulmonary Resuscitation, Time Factors, Heart Massage, Task Performance and Analysis, Heart Arrest
1. Introduction:
Cardiopulmonary resuscitation (CPR) is a life-saving procedure that is performed on patients who experience cardiac arrest, and its effectiveness depends predominantly on the quality of the rescuer-delivered chest compressions (1). However, maintaining consistent high-quality compression can be physically demanding and potentially lead to rescuer fatigue that diminishes CPR effectiveness over time (2, 3). Improving CPR quality has been the primary focus for enhancing outcomes in patients who have experienced cardiac arrest since the 2000s. Shorter compression rotation intervals may delay the onset of fatigue, thereby potentially improving CPR effectiveness (4-6). However, frequent rotation can interrupt chest compressions and adversely affect patient outcomes. In contrast, longer intervals may reduce interruptions and increase the risk of fatigue, thereby compromising compression quality. Current guidelines recommend a 2-minute chest compression rotation or earlier if rescuer fatigue is evident (7). Several clinical trials have recently investigated alternative strategies to those recommended in these guidelines. Manikin studies using 1-min compression rotation have shown varying results. Huseyin et al. reported a high percentage of effective compressions (8). Manders et al. noted reduced fatigue in the 1-min rotation group (6), although not all the trials yielded consistent findings. A study by Pechaksorn et al. showed that a 1-min rotation induced greater compression depth and less fatigue than a 2-min rotation (5), and similar outcomes were reported by Kim et al. (4). Considering these conflicting findings, this systematic review and meta-analysis aimed to determine whether altering the chest compression rotation interval from 2 min to 1 min enhances CPR quality and reduces rescuer fatigue.
2. Methods:
2.1 Search strategy
This systematic review and meta-analysis was conducted in accordance with the Cochrane recommendations and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under protocol number CRD42024528147.
We systematically searched for published articles in MEDLINE, EMBASE, Scopus, and the Cochrane Central Register of Controlled Trials (CENTRAL) from the inception of each database until March 13, 2024. The search was updated, with the inclusion of Web of Science on May 15, 2025. The search terms included: “CPR,” “chest compression,” “resuscitation,” “cardiopulmonary resuscitation,” “heart massage,” “rotate,” “rotation,” “switch,” “interval,” “time factors,” “quality,” “metric,” “effectiveness,” and “minute.” We limited our search to studies that involved human participants and were published in English. Examples of keyword combinations used in the MEDLINE database are listed in Table 1.
Table 1.
Search strategy for different databased
| Database | Key concept | Search terms |
|---|---|---|
| Medline | #1 CPR, Chest compression | (“CPR” [Text Word] OR “Chest compression” [Text Word]) OR (“Resuscitation” [MeSH Terms] OR “Heart massage” [MeSH Terms]) |
| #2 Rotation | (“Rotate” [Text Word] OR “Switch” [Text Word] OR “Interval” [Text Word]) OR (“Time factors” [MeSH Terms]) | |
| #3 Minute | “Minute” [Text Word] | |
| #4 CPR Quality | (“Quality” [Text Word] OR “Metrics” [Text Word] OR “Effectiveness” [Text Word]) OR (“Task Performance and Analysis” [MeSH Terms]) | |
| #5 | #1 AND #2 AND #3 AND #4 | |
| EMBASE | #1 CPR, Chest compression | ("CPR" OR "Chest compression") OR ("Cardiopulmonary resuscitation":mh OR "Heart massage":mh OR "Basic life support":mh) |
| #2 Rotation | ("Rotate" OR "Switch" OR "Interval") OR ("Time factor":mh) | |
| #3 Minute | ("Minute" OR "Minutes") | |
| #4 CPR Quality | ("Quality" OR "Metrics" OR "Effectiveness") OR ("Quality":mh OR "Treatment outcome":mh OR "Performance measurement":mh) | |
| #5 | #1 AND #2 AND #3 AND #4 | |
| Scopus | #1 CPR, Chest compression | TITLE-ABS-KEY ("CPR") OR TITLE-ABS-KEY ("chest compression") OR TITLE-ABS-KEY ("cardiopulmonary resuscitation") |
| #2 Rotation | TITLE-ABS-KEY ("rotat*") OR TITLE-ABS-KEY ("switch") OR TITLE-ABS-KEY ("interval*") | |
| #3 Minute | TITLE-ABS-KEY ("minute*") | |
| #4 CPR Quality | (TITLE-ABS-KEY ("quality") OR TITLE-ABS-KEY ("metric*") OR TITLE-ABS-KEY ("effectiveness")) | |
| #5 | #1 AND #2 AND #3 AND #4 | |
| CENTRAL | #1 CPR, Chest compression | (“CPR” OR “Chest compression”) OR (“Resuscitation” OR “Cardio Pulmonary Resuscitation” OR “Code Blue” OR “Basic Cardiac Life Support” OR “Heart massage”) |
| #2 Rotation | (“Rotate” OR “Switch” OR “Interval”) OR (“Time factors”) | |
| #3 Minute | (“Minut”) | |
| #4 CPR Quality | (“Quality” OR “Metrics” OR “Effectiveness”) OR (“Task Performance and Analysis”) | |
| #5 | #1 AND #2 AND #3 AND #4 | |
| Web of Science | #1 CPR, Chest compression | TS=("CPR" OR "chest compression" OR "resuscitation") |
| #2 Rotation | TS=("rotate*" OR "switch" OR "interval*" OR "time factors") | |
| #3 Minute | TS=("minute*" AND ("minute" OR "minutes")) | |
| #4 CPR Quality | TS=("quality" OR "metrics" OR "effectiveness" OR "task performance and analysis") | |
| #5 | #1 AND #2 AND #3 AND #4 |
CENTRAL: Cochrane Central Register of Controlled Trials.
2.2 Selection criteria
The inclusion criteria for this meta-analysis were based on the following PICO framework:
Population (P): Lay rescuers or medical personnel performing CPR on either manikins or real patients.
Intervention (I): 1-minute chest compression rotation interval.
Comparison (C): Standard 2-minute chest compression rotation interval.
Outcome (O): CPR quality metrics, such as chest compression depth, chest compression rate, percentage of adequate chest compressions, and provider fatigue.
Based on the inclusion criteria, randomized clinical trials (RCTs), randomized simulation studies, and crossover studies were included. Moreover, reviews, meta-analyses, poster presentations, conference abstracts, letters, animal studies, and case studies were excluded from the analysis. To reduce potential confounding and selection biases, observational and non-randomized trials were excluded. This strategy was adopted to maintain methodological rigor and ensure comparability between the intervention and control conditions.
2.3 Study selection
Using an online collaborative platform (Rayyan), two reviewers independently screened the articles based on their titles and abstracts to determine their eligibility. The full texts of potentially relevant studies were reviewed, and any conflicts were resolved through discussion. The reference lists of the included studies were manually screened to identify relevant articles.
2.4 Data extraction
To minimize data collection errors, two independent reviewers extracted data from the selected studies using a standardized data collection form. Any discrepancies were resolved through discussion, and a third reviewer was consulted when necessary. Regular team meetings were held to ensure continuous progress and resolve any challenges that were encountered during screening and article review. If full-text articles were unavailable, the corresponding authors were contacted to obtain the necessary documents. Studies for which the full text could not be retrieved were excluded. Each stage of the study-selection process has been documented in the PRISMA flowchart (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of the present meta-analysis.
2.5 Risk of bias assessment
Two authors independently assessed the risk of bias using RoB 2, with additional considerations for crossover trials. This tool evaluates domain-specific quality across five key aspects: bias arising from the randomization process, bias owing to deviations from intended interventions, bias owing to missing outcome data, bias in outcome measurements, and bias in the selection of reported results. Each study was rated as having a “low risk of bias,” “high risk of bias,” or “some concerns.” Any discrepancies in quality assessment were resolved by discussion with a third author.
2.6 Statistical analysis
A traditional pairwise meta-analysis approach was used for data synthesis. Statistical heterogeneity was assessed using the Cochrane Q test and I² statistics (9). Given the expected clinical and methodological heterogeneity among the studies, the DerSimonian and Laird random effects model was applied to estimate the pooled effect sizes with the corresponding 95% confidence intervals (CIs).
As the components of CPR quality vary across studies, the primary endpoint was analyzed using standardized mean difference (SMD). The interpretation of SMD was based on Cohen (10), where SMD values of 0.2, 0.5, and 0.8 represented a small, medium, and large effect, respectively. If the outcomes were reported using the same measurement scales, a weighted mean difference (WMD) was used. Statistical significance was set at p < 0.05, and all analyses were performed using R (version 4.4.2) with the meta package (version 8.0-1).
To identify potential sources of heterogeneity, subgroup analyses were performed based on provider type (lay rescuer vs. non-lay rescuer), compression duration, and study quality. Subgroup analyses were conducted in cases of moderate or high heterogeneity (I² > 50%) to explore potential sources of variation that were categorized by study design, provider type, study quality, CPR duration, and N95 mask usage. Furthermore, a sensitivity analysis was performed using the leave-one-out method. Funnel plots were used to assess publication bias. If the number of studies exceeded 10, the funnel plot asymmetry was evaluated using both visual inspection and Egger’s test.
3. Results:
3.1 Study characteristics
The initial search yielded 1,323 records. After removing duplicates and screening titles and abstracts, nine studies were selected for full-text review. Of these, eight full-text articles were successfully retrieved and included in the final analysis (Figure 1). The characteristics of the included studies are summarized in Table 2.
Table 2.
Characteristics of the studies included in the review
| Study | Year | Design | Study Site | Participants | Number | Male (%) | Duration* | Washout# |
|---|---|---|---|---|---|---|---|---|
| Manders et al. | 2009 | RCT | Australia | Nurse | 72 | 36.1 | 8 | N/A |
| Oliviera et al. | 2015 | C-RCT | Brazil | Lay rescuer | 148 | 84.5 | 2 | 30 |
| Kilic et al. | 2018 | C-RCT | Turkey | EM Resident | 36 | 68.4 | 4 | N/A |
| Gheibati et al. | 2019 | C-RCT | Iran | Lay rescuer | 70 | N/A | 16 | N/A |
| Pechaksorn et al. | 2020 | C-RCT | Thailand | Medical student | 104 | 51.0 | 8 | 30 |
| Heydari et al. | 2021 | C-RCT | Iran | Medical personnel | 80 | 53.8 | 10 | 30 |
| Kim et al. | 2023 | C-RCT | South Korea | Paramedic student | 100 | 56.0 | 20 | 180 |
| Mathew et al. | 2024 | C-RCT | India | Medical student | 58 | 48.2 | 12 | 24 |
*: CPR duration in minute. #: data are presented as minute. RCT, randomized control trial; C-RCT, crossover randomized control trial; EM, emergency medicine; N/A, not available or not applicable.
The eight studies that were included in this review comprised seven crossover RCTs and one parallel RCT, involving 668 participants in total. These studies evaluated the impact of different compression rotation intervals on CPR quality, specifically by assessing the chest compression depth, rate, and adequacy.
3.2 Quality assessment and risk of bias
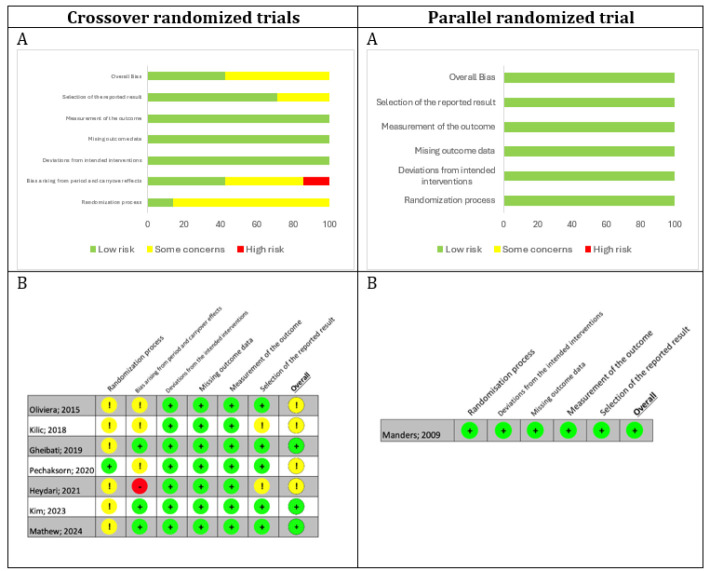
Quality and risk of bias for the included studies were ascertained using the revised risk of bias tool for crossover randomized trials (RoB 2) and RoB 2 for parallel randomized trials (11). The results of the assessment are shown in Figure 2.
Figure 2.
Summary of the risk of bias per item (A) and traffic light plots of the risk of bias assessment (B) of the studies according to the RoB2 for crossover and parallel randomized trial.
3.3 Meta-analysis
3.3.1 Depth of chest compression
Six studies reported the chest compression depth. Compared to the 2-min compression rotation interval, the 1-min compression rotation interval resulted in a significantly greater compression depth, with an SMD of 2.06 mm (95% CI: 0.44, 3.68; p = 0.01; Figure 3).
Figure 3.
A: Forest plot comparing chest compression depth between 1-min and 2-min compression rotation intervals; B: Forest plot of subgroup analysis of compression depth by provider type (lay rescuers vs. trained providers); C: Forest plot comparing chest compression rates between compression rotation intervals; D: Forest plot comparing the percentage of compressions within the recommended rate range; and E: Forest plot comparing rescuer fatigue scores between the two compression rotation intervals.
A subgroup analysis was conducted to assess the potential heterogeneity in the effect of compression rotation intervals between lay rescuers (n=1 trial) and non-lay rescuers (n=7 trials). In the lay rescuer group, only one trial was available, and it reported a mean difference (MD) of 5.89 (95% CI: 4.16–7.62) mm; heterogeneity (I²) could not be assessed owing to the inclusion of a single study. In the non-lay rescuer group, which included seven trials that evaluated trained healthcare providers, the pooled MD was 1.21 (95% CI: 0.45–1.97) mm, without any heterogeneity (I² = 0%). The absence of heterogeneity suggests consistent findings across studies in this group (Figure 3).
Furthermore, five studies reported the percentage of compressions that met the guideline-recommended depth. However, no significant differences were observed between the 1-min and 2-min rotation groups.
3.3.2 Rate of chest compression
Six studies evaluated the compression rate and percentage of compressions within the recommended range of 100–120 compressions per minute. No significant difference was observed between the 1-min and 2-min compression rotation intervals in terms of absolute compression rate (MD = −0.04 bpm, 95% CI: −1.60 to 1.53) or the percentage of compressions within the optimal rate range (MD = 0.04%, 95% CI: −8.02 to 7.94). The results are presented in Figure 3. The subgroup analysis revealed no sources of heterogeneity.
3.3.3 Rescuer fatigue
Four studies reported rescuer fatigue. The 1-minute compression rotation interval group exhibited lower levels of fatigue than did the 2-minute compression rotation interval group, with a significant reduction in the visual analog score for fatigue (MD = −1.27, 95% CI: −2.24 to −0.30; Figure 3). The subgroup analysis revealed no sources of heterogeneity.
3.3.4 Subgroup analysis of CPR quality in the studies
We conducted subgroup analyses of CPR quality outcomes, including compression depth, compression rate, and rescuer fatigue, based on the study quality (low risk vs. concerns regarding the risk of bias), and the results were consistent with those of the overall pooled analyses.
3.4 Publication bias
We assessed publication bias for chest compression depth using a funnel plot (Figure 4). The plot appeared asymmetric, with studies distributed unevenly around the mean effect size, which suggested a potential publication bias. However, given the small number of studies included (n=6), this outcome regarding bias should be interpreted with caution. The Egger’s test was not performed because of the limited sample size.
Figure 4.
Funnel plot assessing potential publication bias for chest compression depth.
Owing to the small number of included studies, a sensitivity analysis using the leave-one-out method was performed. These results were consistent with those of the main analyses. For chest compression depth, the pooled effect size estimates remained statistically significant across all iterations (range: 1.21–2.42), which demonstrated the robustness of our findings.
4. Discussion:
This systematic review and meta-analysis aimed to evaluate the impact of 1-min versus 2-min compression rotation intervals on CPR quality, focusing on chest compression depth, rate, adequacy, and rescuer fatigue. This analysis revealed that, compared to the 2-min interval, the 1-min compression rotation interval significantly improved chest compression depth. The subgroup analysis further highlighted a more pronounced effect in lay rescuers than in trained healthcare providers. These findings suggest that shorter compression rotation intervals may mitigate fatigue-related decline in compression quality, particularly in less experienced rescuers. Importantly, no significant differences were observed in the compression rate or adequacy, indicating that a shorter interval does not compromise adherence to the CPR guidelines.
The observed improvements in compression depth align with prior research, which emphasizes the negative impact of fatigue on CPR performance. Kim et al. (4) found that, compared to a 2-min interval, a 1-min compression rotation interval resulted in a significantly higher chest compression depth. Similarly, Pechaksorn et al. (5) reported that participants in the 1-min group achieved a significantly higher mean compression depth and significantly less fatigue than those in the 2-min group. These findings corroborate our results and demonstrate that reducing the compression rotation interval to 1 min allows rescuers to maintain adequate depth throughout the resuscitation process. The lack of significant differences in the compression rate or adequacy is consistent with the findings of Kim et al.(4), who found no significant difference in compression rate between the 1-min and 2-min groups. This suggests that the physical demands of depth rather than rhythm are more susceptible to fatigue over prolonged periods.
Reducing compression rotation intervals may improve CPR quality through several mechanisms. From a physiological perspective, Cobo-Vázquez et al. demonstrated that performing continuous chest compressions for 2 min decreased electromyographic activity in both the scapular and lumbar muscle groups, indicating muscle fatigue (12). Shorter compression rotation intervals may prevent fatigue and allow adequate muscle recovery. Biomechanically, Sugerman et al. observed that compression depth begins to decline after only 90 s of continuous compression, suggesting that earlier switching of providers could help maintain the optimal compression depth (13). Regarding perceived exertion, multiple studies have reported significantly lower fatigue scores with 1-min compression rotation intervals than with the standard 2-min protocol (4, 5, 14). Collectively, these findings support the multifactorial benefits of shorter rotational intervals during resuscitation.
Despite the modest increase in chest compression depth (mean difference, ~2 mm), even small improvements could significantly enhance perfusion during CPR. According to data from Kanakapriya et al., a 7-mm increase in compression depth resulted in a 27.64% increase in cardiac output among adult human participants, which demonstrated an almost linear relationship (15). Therefore, a 2-mm increase in depth could potentially lead to a meaningful improvement in cardiac output during resuscitation.
Regarding fatigue measurement, despite no standardized minimal clinically important difference (MCID) specifically for CPR-related fatigue, multiple clinical trials involving patients with cancer and chronic illnesses suggest that a change of approximately one-tenth of the visual analog scale (VAS) represents a clinically meaningful difference (16). Accordingly, a 1.27-point reduction in the VAS score likely reflects a clinically important reduction in rescuer fatigue.
These findings have direct implications for CPR guidelines and training programs. Current guidelines from the American Heart Association (AHA) and European Resuscitation Council (ERC) recommend a 2-minute compression rotation interval, primarily based on studies on rescuer fatigue and switching (17, 18). However, our results suggest that a 1-minute compression rotation interval may provide superior outcomes in terms of compression depth, particularly for lay rescuers who may lack the physical endurance of trained professionals. Adapting training programs to include shorter compression rotation intervals could improve CPR quality in real-world scenarios, especially during prolonged resuscitation efforts (13).
Despite the limited direct evidence linking specific chest compression rotation intervals to survival or neurological outcomes, the existing literature strongly supports the relationship between rescuer fatigue and reduced CPR quality. A systematic review by Maia et al. reported that physical fatigue significantly compromised the quality of chest compressions during resuscitation efforts (19). Deterioration in CPR quality owing to fatigue may, in turn, affect patient-centered outcomes, although this indirect relationship warrants further clinical research. In addition, extreme fatigue during CPR has been associated with rare but serious consequences for rescuers. One case report documented the onset of acute myocardial infarction in a healthcare provider after physically strenuous CPR efforts, underscoring the potential physiological toll of prolonged compression without rotation (20).
5. Strengths and limitations
The strengths of this review include the inclusion of RCTs and the use of subgroup analyses to explore heterogeneity. However, this study had some limitations. First, the small number of included studies limited the generalizability of the findings, particularly for lay rescuers, where only one trial was available. Second, the potential for publication bias, as indicated by the funnel plot asymmetry, underscores the need for further studies, including those with unpublished or null findings, to validate these results. Finally, there was a lack of in vivo studies, as all clinical trials included in this study were performed using manikins. No adverse clinical outcomes were observed. Owing to the inherent limitations of manikin-based simulation studies, direct clinical benefits cannot be conclusively established from our results. Although we observed an increase in compression depth, this finding may not necessarily translate into improved survival or neurological outcomes in real patients. The complex physiological responses during actual cardiac arrest scenarios involve variables that cannot be fully replicated in simulation environments, necessitating a cautious interpretation of our findings until they are validated in clinical settings.
Future research should focus on in vivo trials to study clinical outcomes, including survival rates and neurological recovery, associated with different compression rotation intervals. Furthermore, increasing the representation of lay rescuers in trials is critical for a better understanding of the effects of compression-rotation intervals in this population. Addressing publication bias by encouraging the reporting of null or negative results in CPR-related studies would further strengthen this evidence.
6. Conclusions:
This systematic review and meta-analysis suggests that a 1-minute chest compression rotation interval improves compression depth and reduces rescuer fatigue without compromising the compression rate or adequacy. These findings indicate the potential benefit of reconsidering the current CPR guidelines, particularly for lay rescuers and prolonged resuscitation efforts. However, further in vivo studies are required to confirm these results in clinical settings.
7. Declarations:
71 Acknowledgments
Not applicable.
7.2 Authors’ contributions
C. S. : Data curation, Formal analysis, Visualization, Writing – original draft
V. V. : Conceptualization, Data curation, Methodology, Supervision, Writing – review & editing
C. C. : Methodology, Supervision, Writing – review & editing
All authors read and approved the final version of manuscript.
7.3 Ethics approval and Patient consent
Not applicable.
7.4 Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information file.
7.5 Conflicting interests
The authors declare that they have no competing interests
7.6 Funding and supports
No funding or support was received.
7.7 Using artificial intelligence chatbots
The authors use a large language model, specifically ChatGPT-4o, accessed via chat.openai.com, for minor suggestions on the coding of the analysis and for drafting during the manuscript development process.
References
- 1.Talikowska M, Tohira H, Finn J. Cardiopulmonary resuscitation quality and patient survival outcome in cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2015;96:66–77. doi: 10.1016/j.resuscitation.2015.07.036. [DOI] [PubMed] [Google Scholar]
- 2.McDonald CH, Heggie J, Jones CM, Thorne CJ, Hulme J. Rescuer fatigue under the 2010 ERC guidelines, and its effect on cardiopulmonary resuscitation (CPR) performance. Emerg Med J. 2013;30(8):623–7. doi: 10.1136/emermed-2012-201610. [DOI] [PubMed] [Google Scholar]
- 3.Hightower D, Thomas SH, Stone CK, Dunn K, March JA. Decay in quality of closed-chest compressions over time. Ann Emerg Med. 1995;26(3):300–3. doi: 10.1016/s0196-0644(95)70076-5. [DOI] [PubMed] [Google Scholar]
- 4.Kim DH, Seo YW, Jang TC. CPR quality with rotation of every 1 versus 2 minutes as characteristics of rescuers: A randomized crossover simulation study. Medicine (Baltimore) 2023;102(10):e33066. doi: 10.1097/MD.0000000000033066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pechaksorn N, Vattanavanit V. CPR compression rotation every one minute versus two minutes: a randomized cross-over manikin study. Emerg Med Int. 2020;2020:5479209. doi: 10.1155/2020/5479209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manders S, Geijsel FE. Alternating providers during continuous chest compressions for cardiac arrest: every minute or every two minutes? Resuscitation. 2009;80(9):1015–8. doi: 10.1016/j.resuscitation.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 7.Berg KM, Bray JE, Ng KC, Liley HG, Greif R, Carlson JN, et al. 2023 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implemetation, and Teams; and First Aid Task Forces. Circulation. 2023;148(24):e187–e280. doi: 10.1161/CIR.0000000000001179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huseyin TS, Matthews AJ, Wills P, O'Neill VM. Improving the effectiveness of continuous closed chest compressions: an exploratory study. Resuscitation. 2002;54(1):57–62. doi: 10.1016/s0300-9572(02)00040-0. [DOI] [PubMed] [Google Scholar]
- 9.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. New York Routledge: 1988. p. 567 . [Google Scholar]
- 11.Sterne J, Savović J, Page M, Elbers R, Blencowe N, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 12.Cobo-Vázquez C, De Blas G, García-Canas P, Del Carmen Gasco-García M. Electrophysiology of muscle fatigue in cardiopulmonary resuscitation on manikin model. Anesth Prog. 2018;65(1):30–7. doi: 10.2344/anpr-65-01-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sugerman NT, Edelson DP, Leary M, Weidman EK, Herzberg DL, Vanden Hoek TL, et al. Rescuer fatigue during actual in-hospital cardiopulmonary resuscitation with audiovisual feedback: a prospective multicenter study. Resuscitation. 2009;80(9):981–4. doi: 10.1016/j.resuscitation.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gianotto-Oliveira R, Gianotto-Oliveira G, Gonzalez MM, Quilici AP, Andrade FP, Vianna CB, et al. Quality of continuous chest compressions performed for one or two minutes. Clinics (Sao Paulo) 2015;70(3):190–5. doi: 10.6061/clinics/2015(03)07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanakapriya K, Manivannan M. CPR Module with Variable Chest Stiffness in High Fidelity Mannequins. CIRP Design ; 2012 . [Google Scholar]
- 16.Khanna D, Pope JE, Khanna PP, Maloney M, Samedi N, Norrie D, et al. The minimally important difference for the fatigue visual analog scale in patients with rheumatoid arthritis followed in an academic clinical practice. J Rheumatol. 2008;35(12):2339–43. doi: 10.3899/jrheum.080375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S366–S468. doi: 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 18.Olasveengen TM, Semeraro F, Ristagno G, Castren M, Handley A, Kuzovlev A, et al. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation. 2021;161:98–114. doi: 10.1016/j.resuscitation.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 19.Maia F, Sousa L, Santiago P. Effects ofphysical fatigue on cardiopulmonary resuscitation quality by lifeguards: a systematic review and meta-analysis. International Journal of First Aid Education. 2023;6(1):70–80. [Google Scholar]
- 20.Akin S, Aribogan A, Giray S. Fatigue in CPR: A reason that causes myocardial infarction of a rescuer. Resuscitation. 2010;81(2):S73. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information file.