Abstract
Background
The treatment of ST-elevation myocardial infarction (STEMI) has significantly advanced with the introduction of primary percutaneous coronary intervention (PCI). While primary PCI with drug-eluting stents is widely accepted as the standard treatment, concerns regarding in-stent restenosis and stent thrombosis persist. Drug-coated balloons (DCBs) offer a promising alternative, delivering antiproliferative drugs directly to the vessel walls without leaving any metal behind.
Methods
This clinical registry evaluated the clinical safety and efficacy of the Selution SLRTM DCB in 36 STEMI patients who underwent primary PCI with Selution SLRTM DCBs between July 2021 and April 2023 in a tertiary center in Singapore. Immediate angiographic outcomes, procedural details and 12-month clinical outcomes were analyzed.
Results
The mean age of the patients was 56.6 years with male predominance (86.1%). Most patients presented with inferior STEMI (61.1%) and received Selution SLRTM DCBs primarily in the left circumflex artery (41.7%). No patients required bailout stenting, and most achieved significant luminal gain with < 30% residual stenosis post-PCI. At 12 months, the mortality rate was 11.1%, 5.4% of the patients required target lesion revascularization, and 5.4% had angina.
Conclusions
Our preliminary findings showed that the Selution SLRTM DCB was safe and effective in primary PCI with low rates of adverse events at 12 months. Further research, including randomized controlled trials, is warranted to corroborate these findings and evaluate long-term outcomes.
Keywords: Drug-coated balloon, Percutaneous coronary intervention, Sirolimus, STEMI
Abbreviations
CABG, Coronary artery bypass graft
DAPT, Dual antiplatelet therapy
DCB, Drug-coated balloon
DES, Drug-eluting stent
ECG, Electrocardiogram
EMRs, Electronic medical records
IHD, Ischemic heart disease
ISR, In-stent restenosis
IVL, Intravascular lithotripsy
IVUS, Intravascular ultrasound
LAD, Left anterior descending artery
LCX, Left circumflex artery
LVEF, Left ventricular ejection fraction
NYHA, New York Heart Association
OM, Obtuse marginal
PCI, Percutaneous coronary intervention
POBA, Plain old balloon angioplasty
RCA, Right coronary artery
SCAI, Society for Cardiovascular Angiography and Intervention
SIROOP, Prospective Registry Study to Evaluate the Outcomes of Coronary Artery Disease Patients Treated With SIROlimus Or Paclitaxel Eluting Balloon Catheters
STEMI, ST-elevation myocardial infarction
TIMI, Thrombolysis in myocardial infarction
TLR, Target lesion revascularization
INTRODUCTION
The treatment of ST-elevation myocardial infarction (STEMI) has been significantly improved by the introduction of primary percutaneous coronary intervention (PCI). However, the 1-year mortality rate for STEMI patients remains considerable at around 10%.1,2 Primary PCI with implantation of drug-eluting stents (DESs) has become the cornerstone of STEMI management; however, challenges including in-stent restenosis (ISR) and stent thrombosis, continue to pose substantial risks to patient outcomes.3,4
Addressing these concerns, drug-coated balloons (DCBs) offer a promising alternative. These balloons are coated with antiproliferative drugs which are released upon balloon inflation, thus delivering therapeutic benefits with no permanent metallic implant. First-generation DCBs use paclitaxel as the antiproliferative drug, with many studies supporting their use in de novo lesions in many clinical settings.
The emergence of limus-coated DCBs represents a novel development in the field of interventional cardiology. This clinical registry aims to evaluate the clinical safety and efficacy of the Selution SLRTM DCB (MedAlliance, Nyon, Switzerland) in primary PCI.
METHODS
A retrospective analysis was conducted on patients presenting with STEMI who underwent primary PCI with the Selution SLRTM DCB at a single center in Singapore between July 2021 and April 2023. Patients receiving DCBs for STEMI to non-culprit lesions or for non-STEMI indications were excluded from this study. Culprit vessels were categorized into the left anterior descending (LAD), left circumflex (LCX) and right coronary artery (RCA), with any side branch culprit lesions recorded under these vessel categories.
The PCI approach involved pre-dilatation of the culprit lesion using plain old balloon angioplasty (POBA) with semi-compliant, non-compliant, scoring, and cutting balloons, or intravascular lithotripsy (IVL) as deemed necessary before deploying the sirolimus DCB. Adequate lesion preparation was determined to be angiographic residual stenosis of < 30% after POBA using the above devices. All DCBs were inflated to their nominal pressure, with inflation maintained for 30 to 60 seconds. Post-DCB procedural success was defined as < 30% residual stenosis of the lesion with no flow limiting dissection. Bail-out stenting was done for cases with significant vessel recoil or high-grade coronary dissection (C or above). Aspiration thrombectomy was performed in patients with a high thrombus burden, i.e. Thrombolysis in myocardial infarction (TIMI) thrombus grade ≥ 3 or more, aiming to reduce the thrombus burden to a TIMI thrombus grade of ≤ 2. The duration of dual antiplatelet therapy (DAPT) was planned for 1 year if the patients did not develop any complications, followed by lifelong single antiplatelet therapy thereafter.
Patient demographics and risk factors such as diabetes mellitus, hypertension, hyperlipidemia, smoking history etc. were retrieved from electronic medical records (EMRs). Angiographic findings, PCI procedural details, echocardiographic findings and in-hospital outcomes were also collected.
Clinical data extraction from the EMRs was performed to evaluate 12-month clinical outcomes.
These outcomes included the occurrence of repeat coronary angiography or PCI with target lesion revascularization (TLR), angina symptoms, recurrence of acute coronary syndrome, New York Heart Association (NYHA) Class III/IV heart failure, or death within a 12-month period. Data from patients lost to follow-up were censored at the date of their last clinical contact, and all data analyses were conducted using Microsoft Excel 2018.
RESULTS
Baseline clinical characteristics
A total of 36 patients were included, and their baseline clinical characteristics are summarized in Table 1. The study was conducted from July 2021 to April 2023. All patients were followed up until 12 months from the date of PCI or death. The mean age of the cohort was 56.6 ± 10.9 years, with male predominance (31 patients, 86.1%). Regarding ethnicity, 18 patients were Chinese (50.0%), 9 were Indian (25.0%), 6 were Malay (16.7%), and 3 belonged to other racial groups (8.3%).
Table 1. Baseline characteristics of the patients.
| Variable | Number |
| Age in years | 56.6 ± 10.9 |
| Number of male sex (%) | 31 (86.1) |
| Number of each race (%) | |
| Chinese | 18 (50.0) |
| Malay | 6 (16.8) |
| Indian | 9 (25.0) |
| Others | 3 (8.3) |
| Risk factors (%) | |
| Diabetes mellitus | 13 (36.1) |
| Hypertension | 21 (58.3) |
| Hyperlipidemia | 15 (41.7) |
| Number of smokers (%) | 18 (50.0) |
| Number in cardiogenic shock (%) | 10 (27.8) |
| Mean LVEF (%) | 43 ± 11 |
LVEF, left ventricular ejection fraction.
Ten (27.8%) patients presented with Society for Cardiovascular Angiography and Intervention (SCAI) Stage C or Stage D cardiogenic shock. The mean left ventricular ejection fraction (LVEF) was 43 ± 11%.
Nature of STEMI and PCI
Most of the 36 patients (61.1%) presented with inferior STEMI, followed by anterior STEMI (22.2%) and lateral STEMI (16.7%), as shown in Table 2.
Table 2. Characteristics of STEMI.
| Type of characteristic | Number (%) |
| Nature of STEMI (%) | |
| Anterior | 8 (22.2) |
| Inferior | 22 (61.1) |
| Lateral | 6 (16.7) |
| Culprit vessel (%) | |
| Left main | 0 (0) |
| Left anterior descending artery | 11 (30.6) |
| Left circumflex artery | 15 (41.7) |
| Right coronary artery | 10 (27.8) |
| Number of in stent restenosis (%) | 4 (11.1) |
STEMI, ST-elevation myocardial infarction.
None of the patients had left main disease as the culprit artery. The most common culprit vessel was the LCX (41.7%), followed by the LAD (30.6%) and RCA (27.8%). Notably, in 4 (11.1%) cases, the culprit lesion resulted from ISR following a prior PCI procedure.
Aspiration thrombectomy was performed in 7 (19.4%) of the patients (Table 3). None of the patients had significant recoil or type C or worse coronary artery dissection, hence no patients required bailout stenting. After lesion preparation, the mean lesion stenosis improved to 31.3 ± 7.5% after POBA. After successful deployment of the Selution SLRTM DCB, the final residual stenosis was 32.1 ± 8.2%.
Table 3. Details of PCI.
| Nature of details | Number of patients (%) |
| Mean lesion stenosis in % | |
| Pre-POBA | 97.2 ± 5.0 |
| Post-POBA | 31.3 ± 7.5 |
| Post DCB | 32.1 ± 8.2 |
| Number of DCB used for culprit lesion | |
| 1 (%) | 25 (69.4) |
| 2 (%) | 10 (27.8) |
| 3 (%) | 1 (2.8) |
| Mean DCB size in mm | |
| Length | 22.1 ± 6.3 |
| Diameter | 2.48 ± 0.46 |
| Aspiration thrombectomy performed (%) | 7 (19.4) |
| Bail out stenting | 0 (0) |
| Type C or worse coronary artery dissection (%) | 0 (0) |
| Used in large vessels (> 3 mm), (%) | 13 (36.1) |
| Number with less than 30% residual stenosis post PCI (%) | 23 (63.9) |
| DCB delivered within 2 minutes (%) | 36 (100) |
| Usage of glycoprotein IIb/IIIa inhibitors (%) | 32 (88.9) |
DCB, drug-coated balloon; PCI, percutaneous coronary intervention; POBA, plain old balloon angioplasty.
Twenty-five patients (69.4%) required a single DCB for treatment of the culprit lesion. In one patient, up to three DCBs were required for the culprit lesion. The mean DCB length was 22 ± 6.3 mm, and the mean DCB diameter was 2.48 ± 0.46 mm. DCBs were deployed in large vessels (diameter ≥ 3mm) in 13 patients (36.1%). Twenty-three (63.9%) patients had < 30% residual stenosis of the culprit vessel at the end of the PCI. All patients had DCBs deployed within 2 minutes, and 32 (88.9%) patients received glycoprotein IIb/IIIa inhibitors.
12-month outcomes
Mortality
At 12 months of follow-up (Table 4) there were 4 deaths, of which 2 were cardiac related.
Table 4. 12-month outcomes.
| Nature of outcome | Number of patients with outcome (%) |
| Cardiac death (%) | 2 (5.4) |
| Angina (%) | 2 (5.4) |
| Target lesion revascularization (%) | 2 (5.4) |
| Acute myocardial infarction (%) | 2 (5.4) |
| NYHA Class III/IV heart failure (%) | 2 (5.4) |
NYHA, New York Heart Association.
The first patient was a 78-year-old man with no prior medical history who presented with inferior STEMI complicated by cardiogenic shock and complete heart block (requiring intravenous dopamine infusion and transcutaneous pacing). On arrival to hospital, he was intubated due to respiratory distress and hypoxia. The culprit lesion was an acute thrombotic occlusion of the ostial right posterolateral artery, with moderate disease in the RCA, LCX, and LAD not requiring intervention. Primary PCI with two Selution SLRTM DCBs was performed, resulting in < 30% residual stenosis and no significant coronary dissection. He subsequently developed ventilator-acquired pneumonia and died from septic shock during the same admission.
The second patient was a 79-year-old woman with a history of chronic kidney disease (KDIGO Stage 4), prior type 2 myocardial infarction, diabetes, hypertension, and hyperlipidemia. She presented with inferior STEMI complicated by complete heart block and SCAI C-D cardiogenic shock. The culprit lesion was a dominant LCX, which supplied a large vascular territory. A successful primary PCI was performed with a Selution SLRTM DCB. Despite this, she remained in cardiogenic shock, requiring an intra-aortic balloon pump; however, she quickly deteriorated and died. Repeat electrocardiograms (ECGs) did not show any ST elevation in the inferior leads.
The third patient was a 67-year-old woman with a history of diabetes, hypertension, hyperlipidemia, and prior ischemic heart disease (IHD) with an LVEF of 30%. She had multiple previous PCIs to the RCA and LAD with known ISR. She presented with anterior STEMI complicated by SCAI C-D cardiogenic shock secondary to a mid-LAD very late stent thrombosis acute stent occlusion. She underwent primary PCI with DCB-only angioplasty but developed recurrent unstable arrhythmias and subsequently died.
The fourth patient died 9 months after PCI from cellulitis and peritoneal dialysis peritonitis, with no evidence of recurrent myocardial infarction. This patient had a background of end-stage renal failure on peritoneal dialysis, and previous IHD for which they received PCI with a DES to the LAD in 2020. The patient had developed massive diverticular bleeding while on aspirin monotherapy complicated by an in-hospital cardiac arrest needing massive transfusion and urgent angioembolization in January 2022. The patient presented with inferior STEMI in July 2022 and received a DCB to the RCA, with a planned DAPT duration of 1 year if the hemoglobin level remained stable. However, the patient developed worsening anemia with intermittent bloody stool needing multiple blood transfusions. The decision was made to stop DAPT, and the patient’s hemoglobin level remained stable thereafter on aspirin monotherapy. At 9 months, the patient developed severe cellulitis and peritoneal dialysis peritonitis complicated by septic shock and subsequently died. There was no evidence of recurrent myocardial infarction.
TLR
Two patients (5.6%) required TLR.
The first patient was a 71-year-old woman with poorly controlled diabetes, hypertension, hyperlipidemia, and known IHD with a prior coronary artery bypass graft (CABG) of the left internal mammary artery to the LAD and hybrid PCI with a DES to the LCX and obtuse marginal (OM) 7 years earlier. She presented with inferior STEMI secondary to acute thrombotic occlusion at the LCX and OM2 bifurcation ISR. Two Selution SLRTM DCBs were deployed at the LCX and OM2, resulting in TIMI 3 flow. Her LVEF was 40%. Twelve months later, she presented with an inferoposterior STEMI complicated by acute pulmonary edema requiring intubation. The culprit lesion was ISR in the LCX and OM2. Intravascular ultrasound (IVUS) revealed that the ISR was due to neoatherosclerosis with heavily calcified plaque. IVL was required to modify the lesion, which was then treated with a DES/DCB hybrid strategy. The stent was extended proximally to the ostial left main as the patient had a chronically occluded ostial LAD. The ISR was treated with a Paclitaxel DCB. The patient was discharged hemodynamically stable.
The second patient was a 57-year-old man with a background of retroviral disease (viral load suppressed). He presented with inferior STEMI in March 2022 with the culprit lesion being an acute thrombotic occlusion in the mid-LCX after OM2. Primary PCI with a Selution SLRTM DCB was performed, resulting in good angiographic outcomes (residual stenosis 30%). After declining CABG for residual disease in the LAD and RCA, staged PCI was planned for three months post-STEMI. However, coronary angiography demonstrated diffuse, calcified 70-80% stenosis of the LCX with ostial OM2 90% stenosis, and IVUS showed concentric calcium. PCI with a Paclitaxel DCB to the LCX was performed, again achieving good angiographic results (residual stenosis 30%). The staged PCI to the RCA was rescheduled for five months later at the patient’s request. At this follow-up, coronary angiography showed 100% total occlusion in the LCX after OM2. Two DESs were placed in the LCX. The staged PCI to the RCA was done the next month (9 months post-STEMI), and it showed a widely patent DES in the LCX.
Angina
During the follow-up period, 7 patients (22.2%) had recurrent chest pain, with 2 (5.4%) cases classified as angina.
The first patient had triple vessel disease at the initial presentation with STEMI originating from the LCX, which was treated with a Selution DCB. He also had significant disease in the LAD, OM, and RPDA and was scheduled for elective CABG. While awaiting surgery, he experienced angina likely due to residual unrevascularized non-culprit lesions, which resolved after the surgery.
The second patient did not require further investigation as his symptoms resolved following the uptitration of anti-anginal medications.
Five patients had chest pain of non-cardiac origin. Three of these patients underwent repeat coronary angiograms, which showed patent vessels with no target lesion restenosis. Two patients underwent myocardial perfusion imaging, which revealed no significant ischemia.
Repeat coronary angiography
Seven patients received repeat coronary angiography (Table 5). None of the patients required a relook coronary angiography within 48 hours of the primary PCI, and there were no cases of acute closure. Three angiographies were for staged PCI, all of which showed widely patent post-DCBs at the prior culprit lesion. Five of these patients (71.4%) had widely patent DCB segments. The other two patients required revascularization, as described in the TLR section.
Table 5. Repeat coronary angiogram.
| Nature of repeat coronary angiogram | Number of patients (%) |
| Number of patients with repeat coronary angiogram (%) | 7 (19.4) |
| Indication for repeat coronary angiogram | |
| Chest pain (%) | 3 (8.3) |
| Acute myocardial infarction (%) | 1 (2.8) |
| Staged PCI (%) | 3 (8.3) |
| Number of patients with widely patent DCB site (%) | 5 (71.4%) |
DCB, drug-coated balloon; PCI, percutaneous coronary intervention.
Figures 1 and 2 show the angiographic results (immediately post-PCI and on relook coronary angiogram) of 2 patients with anterior STEMI treated with Selution SLRTM DCBs.
Figure 1.

The patient was a 68 year old gentleman who was admitted for anterior myocardial infarction (MI). (A) Initial coronary angiogram showing an occluded mid left anterior descending artery (LAD). (B) Immediate post percutaneous coronary intervention (PCI) result after drug-coated balloon (DCB) angioplasty with Selution SLR. (C) Re-look coronary angiogram 3 months later.
Figure 2.
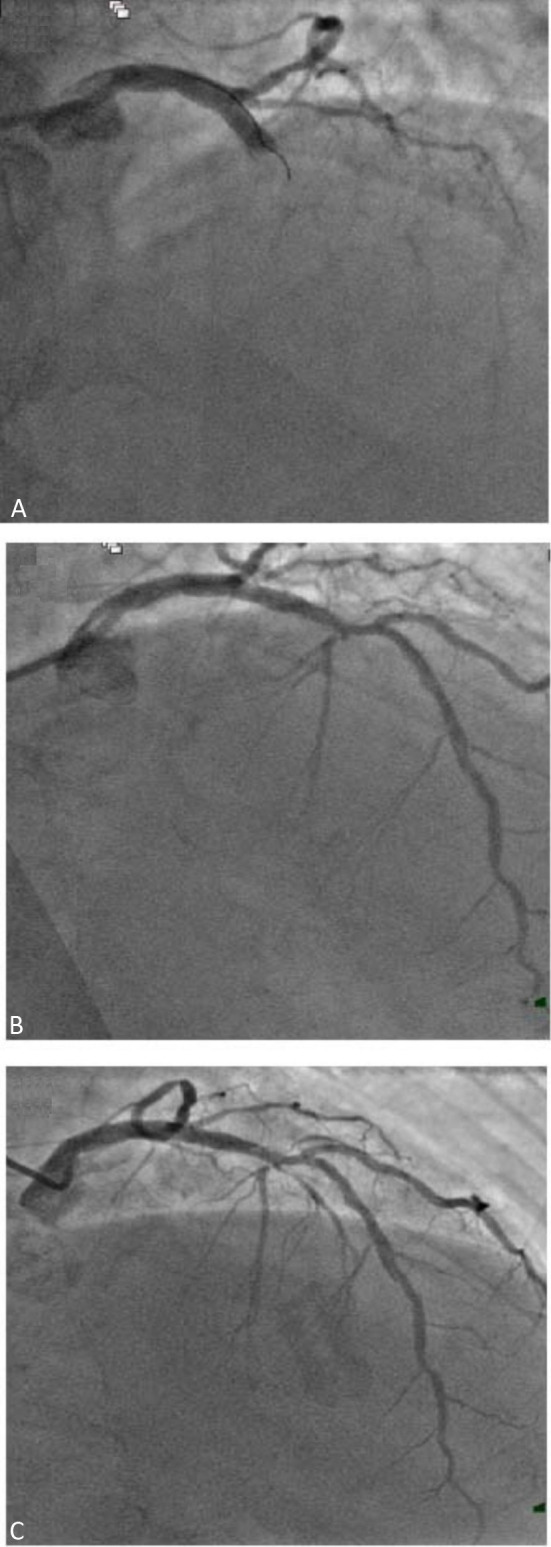
The patient was a 70 year old lady who was admitted for anterior myocardial infarction (MI). (A) Initial coronary angiogram showing an occluded mid left anterior descending artery (LAD). (B) Immediate post percutaneous coronary intervention (PCI) result after drug-coated balloon (DCB) angioplasty with Selution SLR. (C) Re-look coronary angiogram 6 weeks later.
Heart failure
Two patients developed NYHA Class III heart failure, likely due to non-compliance with medication and fluid restriction. No repeat ischemic evaluation was required. They were managed with guideline-directed medical therapy.
Early cessation or change to DAPT
One patient had to stop DAPT due to anemia as described above (the patient subsequently died from sepsis).
One patient was initiated on DAPT post-STEMI, but developed atrial fibrillation. He presented with triple vessel disease, and CABG was required. He was placed on triple therapy with aspirin, clopidogrel and aspirin, but had per rectal bleeding needing a blood transfusion and colonoscopy, which revealed Clostridium difficile colitis. Aspirin was then stopped, and he continued on apixaban and clopidogrel. He subsequently went for CABG, and the surgical team stopped clopidogrel post-CABG. He remained well on apixaban monotherapy, and had no adverse outcomes at 12 months of follow-up.
DISCUSSION
DCBs already have a class I indication for the treatment of ISR according to the 2018 ESC/EACTS (European Society of Cardiology/European Association for Cardio-Thoracic Surgery) myocardial revascularization guidelines.5 The clinical efficacy of DCBs has also been demonstrated in small vessel disease, with many studies supporting their use in de novo lesions in many clinical settings.6,7
Stent implantation with a DES is currently considered the standard of care for primary PCI, with DESs being associated with better outcomes compared to bare metal stents.8,9 In treating patients with STEMI, a previous study showed that most operators in the Asia-Pacific region would still opt for DESs over DCBs.10 An important limitation of stent implantation in patients with STEMI is the persistent risk of stent thrombosis in addition to the risk of ISR, especially if DAPT absorption is compromised. Moreover, DCBs afford the primary operator greater flexibility in patients with high bleeding risk, compliance issues, and in those who develop complications such as atrial fibrillation or left ventricular thrombus.11
Several studies have reported their experiences of using paclitaxel-based DCBs in the primary PCI setting with favorable outcomes.12-14 The REVELATION study showed the non-inferiority of DCBs compared to DESs in patients with STEMI when evaluating mean fractional flow reserve post-PCI. The above studies primarily examined paclitaxel-coated DCBs.
Previous animal studies15 have suggested that sirolimus has a more effective anti-proliferative effect than paclitaxel on atherosclerosis-related hypoxic cells, which may contribute to the lower ISR seen in limus-eluting stents compared to paclitaxel-eluting stents. Traditionally, this advantage has been offset by the relative lack of lipophilicity of limus compared to paclitaxel, which can compromise the transfer of the drug into the vessel wall during inflation of the DCB.
The Selution SLRTM DCB uses proprietary micro-reservoir technology to deliver sirolimus into the vessel walls. The micro-reservoirs facilitate a controlled and sustained release of sirolimus, maintaining clinically therapeutic levels for over 90 days, which is the longest release profile compared to other DCBs currently available on the market. Moreover, the Cell Adherent TechnologyTM contains and protects the micro-reservoir during inflation of the DCB to optimize drug transfer into the vessel wall.
The currently available data on Selution SLRTM appear promising. Preliminary data16 from the Prospective Registry Study to Evaluate the Outcomes of Coronary Artery Disease Patients Treated With SIROlimus Or Paclitaxel Eluting Balloon Catheters (SIROOP) demonstrated a 100% procedural success rate and low rates of adverse events at 1 year in patients with complex lesions treated with Selution SLRTM.
The Selution SLRTM Coronary Clinical Program has enrolled more than 4000 patients, studying the clinical efficacy of Selution SLRTM across multiple trials. The Selution ISR IDE study will evaluate Selution SLRTM in the treatment of ISR, and the Selution DeNovo study will evaluate Selution SLRTM in the treatment of all lesions, although patients with STEMI will be excluded from this study.
In this study, DCB angioplasty was performed according to the protocol recommended by the Third Report of the International DCB Consensus Group when possible.17 Most of the patients achieved < 30% residual stenosis, and none had significant flow-limiting dissections (defined as type C or above dissections). Lesion preparation was achieved with semi-compliant and non-compliant balloons, with scoring and cutting balloons used as clinically indicated.
We also recommend aspiration thrombectomy when faced with a high thrombus burden, i.e., TIMI thrombus grade ≥ 3, with the aim of reducing the thrombus burden to TIMI thrombus grade ≤ 2. A thrombus-laden lesion is more likely to hamper effective drug delivery to the vessel wall. Removal of the thrombus will enable the DCB to have better contact with the vessel wall to facilitate effective drug transfer. In our registry, 19.4% of the patients underwent aspiration thrombectomy.
Two of our patients were non-compliant to medical therapy (including DAPT) and fluid restriction, resulting in readmission for heart failure. No new acute coronary events were noted in these patients based on ECG and troponin levels. After the resumption and titration of medical therapy, none of the patients had repeat admissions at up to 12 months. We hypothesize that better compliance with medical therapy may have avoided these outcomes of heart failure.
One patient had to stop DAPT early due to anemia requiring blood transfusion. Nevertheless, this patient did not develop any adverse outcomes despite being on only single antiplatelet therapy. This highlights a possible benefit of DCB, where it can be used for patients with higher bleeding risk, whereas a DES approach may be associated with a higher incidence of stent thrombosis with cessation of DAPT for anemia.
For the two patients who required TLR, IVUS showed the presence of calcified plaque, and poor clinical results were noted even after repeating PCI with paclitaxel DCBs. We hypothesize that a DCB may still be a valid approach to manage patients with heavily calcified plaque. Heavily calcified plaque is a risk factor for restenosis regardless of whether a DCB or stenting strategy is employed during PCI. If there is sufficient lumen gain, leaving no metal behind may be a better option for the patient. There may also be concerns regarding technical feasibility of proceeding with stenting of vessels with heavily calcified plaque, given that there may be significant stent under expansion, which increases the risk of stent thrombosis. Moreover, DCB angioplasty allows for a simpler procedure that can avoid complex bifurcation stenting in certain settings.
In our registry, most of the Selution SLRTM DCB deployments were in the LCX (41.7%). This may reflect a reluctance to use a novel DCB in larger vessels supplying a larger vascular territory. This may change in the future as more data become available and clinicians become more comfortable with the Selution SLRTM DCB.
Our initial experience with Selution SLRTM DCB demonstrated good procedural success, consistent with the preliminary data from the SIROOP study. All patients had successful deployment of the Selution SLRTM DCB, with none requiring bailout stenting. The Selution SLRTM is also a deliverable DCB, and all were delivered to the target site within 2 minutes. This contrasts with previous concerns about paclitaxel DCBs, which are bulkier and have a larger crossing profile, making them less deliverable.
Only one DCB was needed to achieve revascularization in 69.4% of our patients, and most achieved good luminal gain with < 30% residual stenosis. The Selution SLRTM DCB also showed encouraging results in 13 patients (36.1%) with large vessels (defined as > 3 mm), with none requiring TLR at 1 year.
Our preliminary results also reflect the clinical safety profile of the Selution SLRTM DCB with a low incidence of adverse events. Two patients (5.4%) had angina within 1 year, but none required revascularization to the vessel treated with the Selution SLRTM DCB. Only two patients (5.6%) required TLR, one of whom presented with STEMI, and the other for a staged procedure. However, both patients had suboptimal cardiovascular risk factor control and heavily calcified plaque, predisposing them to a higher risk of restenosis.
Four patients (11.1%) died, however two of them presented with profound SCAI stage C-D cardiogenic shock and two died from non-cardiac-related causes (sepsis) with no evidence of a recurrent cardiac events. In these patients, there were no ST elevations on ECGs suggestive of recurrent myocardial infarction. Two patients (5.6%) developed heart failure, likely due to medication non-compliance and fluid indiscretion rather than DCB failure. Neither of these patients had ischemic ECG changes or symptoms.
Strengths
To our knowledge, this is the first clinical study investigating the clinical efficacy and safety outcomes of limus-based DCBs, specifically the Selution SLRTM DCB, in patients with STEMI undergoing primary PCI.
Limitations
There were several limitations to this study. First, it was a single-arm study with no control group for comparison. In addition, the sample size was small, with only 36 patients, which may limit the generalizability of our conclusions. Analysis of variance would not have yielded meaningful results as the sample size was small, and the number of outcome events (including death, TLR) was fairly low. Therefore, we present combined outcomes. Further studies with a larger sample size may provide better insights in subgroup analysis on anatomical location of the culprit vessels.
New knowledge gained
Sirolimus DCBs are a viable and safe option for primary PCI in patients who present with STEMI (Central Illustration).
Central Illustration.
Protocol and outcomes of deploying of sirolimus drug coated balloon. DCB, drug coated balloon; SCAI, Society for Cardiovascular Angiography and Interventions; STEMI, ST-elevated myocardial infarction.
CONCLUSIONS
This clinical registry demonstrates that the Selution SLRTM DCB is a safe and effective therapeutic tool in primary PCI, associated with high rates of procedural success and favorable 1-year clinical outcomes with a low incidence of adverse cardiac events.
Further research, including randomized controlled trials, is warranted to corroborate these findings and evaluate long-term outcomes.
DECLARATION OF CONFLICT OF INTEREST
All the authors declare no conflict of interest.
Acknowledgments
The authors thank the staff of the Invasive Cardiac Laboratory, Tan Tock Seng Hospital for their assistance with primary PCI and facilitating data collection.
REFERENCES
- 1.Pedersen F, Butrymovich V, Kelbæk H, et al. Short- and long-term cause of death in patients treated with primary PCI for STEMI. J Am Coll Cardiol. 2014;64:2101–2108. doi: 10.1016/j.jacc.2014.08.037. [DOI] [PubMed] [Google Scholar]
- 2.Fokkema ML, James S, Thorvinger B, et al. Population trends in percutaneous coronary intervention: 20-year results from the SCAAR (Swedish Coronary Angiography and Angioplasty Registry). J Am Coll Cardiol. 2013;61:1222–1230. doi: 10.1016/j.jacc.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Magalhaes MA, Minha S, Chen F, et al. Clinical presentation and outcomes of coronary in-stent restenosis across 3-stent generations. Circ Cardiovasc Interv. 2014;7:768–776. doi: 10.1161/CIRCINTERVENTIONS.114.001341. [DOI] [PubMed] [Google Scholar]
- 4.Kim MC, Kim IS, Jeong MH, et al. Incidence of cardiac death and recurrent stent thrombosis after treatment for angiographically confirmed stent thrombosis. J Cardiol. 2019;74:267–272. doi: 10.1016/j.jjcc.2019.02.019. [DOI] [PubMed] [Google Scholar]
- 5.Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165. doi: 10.1093/eurheartj/ehy855. [DOI] [PubMed] [Google Scholar]
- 6.Jeger RV, Farah A, Ohlow MA, et al. Drug-coated balloons for small coronary artery disease (BASKET-SMALL 2): an open-label randomised non-inferiority trial. Lancet. 2018;392:849–856. doi: 10.1016/S0140-6736(18)31719-7. [DOI] [PubMed] [Google Scholar]
- 7.Cortese B, Di Palma G, Guimaraes MG, et al. Drug-coated balloon versus drug-eluting stent for small coronary vessel disease: PICCOLETO II randomized clinical trial. JACC Cardiovasc Interv. 2020;13:2840–2849. doi: 10.1016/j.jcin.2020.08.035. [DOI] [PubMed] [Google Scholar]
- 8.Dibra A, Kastrati A, Mehilli J, et al. Paclitaxel-eluting or sirolimus-eluting stents to prevent restenosis in diabetic patients. N Engl J Med. 2005;353:663–670. doi: 10.1056/NEJMoa044372. [DOI] [PubMed] [Google Scholar]
- 9.Kaul U, Bangalore S, Seth A, et al. Paclitaxel-eluting versus everolimus-eluting coronary stents in diabetes. N Engl J Med. 2015;373:1709–1719. doi: 10.1056/NEJMoa1510188. [DOI] [PubMed] [Google Scholar]
- 10.Ang AS, Li CKF, Tan JWC, et al. A survey of drug-coated balloon usage patterns in the Asia-Pacific region. JAPSC. 2023;2:e18. [Google Scholar]
- 11.Scheller B, Eccleshall S. Drug-coated balloons for acute coronary syndromes. Eurointervention. 2024;20:e791–e792. doi: 10.4244/EIJ-E-24-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vos NS, Fagel ND, Amoroso G, et al. Paclitaxel-coated balloon angioplasty versus drug-eluting stent in acute myocardial infarction: the REVELATION randomized trial. JACC Cardiovasc Interv. 2019;12:1691–1699. doi: 10.1016/j.jcin.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Merinopoulos I, Gunawardena T, Corballis N, et al. Assessment of paclitaxel drug-coated balloon only angioplasty in STEMI. JACC Cardiovasc Interv. 2023;16:771–779. doi: 10.1016/j.jcin.2023.01.380. [DOI] [PubMed] [Google Scholar]
- 14.Ho HH, Tan J, Ooi YW, et al. Preliminary experience with drug-coated balloon angioplasty in primary percutaneous coronary intervention. World J Cardiol. 2015;7:311–314. doi: 10.4330/wjc.v7.i6.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Y, Zeng Y, Zhu X, et al. Significant difference between sirolimus and paclitaxel nanoparticles in anti-proliferation effect in normoxia and hypoxia: the basis of better selection of atherosclerosis treatment. Bioact Mater. 2020;6:880–889. doi: 10.1016/j.bioactmat.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Madanchi M, Cioffi GM, Attinger-Toller A, et al. Metal free percutaneous coronary interventions in all-comers: first experience with a novel sirolimus-coated balloon. Cardiol J. 2022;29:906–916. doi: 10.5603/CJ.a2022.0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jeger RV, Eccleshall S, Wan Ahmad WA, et al. Drug-coated balloons for coronary artery disease: third report of the International DCB Consensus Group. JACC Cardiovasc Interv. 2020;13:1391–1402. doi: 10.1016/j.jcin.2020.02.043. [DOI] [PubMed] [Google Scholar]



