Abstract
PURPOSE
Body mass index (BMI) is the current standard body composition measurement. We examined BMI vs body fat percentage (BF%) for 15-year mortality risk among adults aged 20-49 years.
METHODS
In this nationally representative cohort of US adults in the National Health and Nutrition Examination Survey, Cox proportional hazard regression was computed for 15-year mortality risk. Healthy and overweight/obese BMI were 18.5-24.9 and ≥25 kg/m2, respectively. The unhealthy BF% and waist circumference (WC) thresholds were ≥27% and ≥44%, and >40 and >35 inches, for men and women, respectively. The 15-year mortality risk for BMI, BF%, and WC was computed.
RESULTS
Body fat percentage and WC are both significantly associated with 15-year, allcause mortality (BF%: unadjusted hazard ratio [HR] 2.01; 95% CI, 1.45-2.78; P < .001; adjusted HR 1.78; CI, 1.28-2.47; P < .001; WC: unadjusted HR 1.94; CI, 1.38-2.72; P < .001; adjusted HR 1.59; CI, 1.12-2.26; P = .009) and heart disease mortality (BF%: unadjusted HR 4.20; CI, 1.94-9.11; P < .001; adjusted HR 3.62; CI, 1.55-8.45; P = .003; WC: unadjusted HR 4.75; CI, 2.45-9.21; P < .001; adjusted HR 4.01; CI, 1.94-8.27; P < .001). Body mass index has no statistically significant relationship with all-cause mortality. Body mass index has a significant association with heart disease mortality in the unadjusted model but not in the adjusted model.
CONCLUSION
Body fat percentage is a better predictor of 15-year mortality risk in young adults than BMI. A move to using BF% rather than BMI may change how we measure body composition for risk stratification.
Key words: body composition, body mass index, BMI, body fat percentage, mortality, heart disease, waist circumference, bioelectrical impedance analysis, DXA scan, primary care
INTRODUCTION
Body composition has been shown to be associated with risk for cancer,1 cardiometabolic diseases like type 2 diabetes2 and cardiovascular disease (CVD),3 as well as mortality.1,3 Because of this strong association with increased risk, assessments of body composition have long been integrated into clinical practice to risk stratify patients using categories like overweight and obese. Body mass index (BMI) and body fat percentage (BF%) are 2 commonly used metrics for assessing an individual’s body composition and health risks.
Body mass index is an indirect measure of body fat based on measures of height and weight. Body mass index has been endorsed by the Centers for Disease Control and Prevention (CDC), National Institute of Health (NIH), World Health Organization (WHO), American Diabetes Association (ADA), American Heart Association (AHA), and many other health organizations as the standard measure for body composition.4-8 Body mass index is an estimate of body fat and a relatively good measure of a patient’s risk for certain diseases that can occur with overweight and obesity9-11 and is widely used in clinical settings because it is easy to compute and considered the standard body composition measurement.2,12
Over time, regardless of the ubiquitous nature of BMI, a variety of studies have suggested that there are significant limitations to using BMI as a measure of body composition.2,3,13-19 Body mass index can potentially misclassify individuals with a muscular physique as overweight or obese,20 and certain individuals with a normal BMI and elevated BF% (normal weight obesity) may be unaware of their significantly increased risk of metabolic syndrome, type 2 diabetes, and CVD.13,15,17-19 Furthermore, BMI categories (overweight, class I, class II, class III) lack clinical utility as they inaccurately predict both all-cause and cardiovascular mortality.3,11,21-24
Other data have suggested that direct measures of body composition might be better risk predictors than BMI.25 One such direct measure, dual-energy X-ray absorptiometry (DXA) scan, has shown significant value in making accurate assessments.26,27 Routine use of DXA scan, however, is difficult in the clinical setting compared with BMI due to cost and lack of seamless integration into clinic workflows.2,28
Recently, machines using bioelectrical impedance analysis (BIA) have improved to provide accurate, inexpensive, direct measures of body fat and are easily incorporated into a clinical setting.2,27,29,30
Body fat percentage varies with age and leads to further discrepancies in the association of BMI with CVD and mortality in younger vs older adults.21,31-33 Furthermore, in a phenomenon known as the “obesity paradox,” class I obesity is not associated with higher mortality and overweight BMI is associated with significantly lower mortality.24 The obesity paradox has thus been explained by directly measuring muscle (lean) mass, which appears to mediate BMI’s relationship with adiposity and mortality.34,35
With the introduction of BIA as an easy, reliable, and inexpensive measure of body composition, this technology may overcome some of the limitations of BMI.2 However, it is currently unclear if BF% is an improved measure of mortality risk compared with the industry standard of BMI. Moreover, given how adults with undiagnosed cardiometabolic disease have an increased risk of elevated inflammation,36 it is important to evaluate other markers of CVD risk that are associated with mortality. Thus, the purpose of this study is to examine the associations of accepted thresholds of BMI vs reported thresholds of BF% for 15-year mortality risk in young adults and further characterize the overweight/obese BMI and unhealthy BF% cohorts by comparing their respective prevalence of markers of cardiometabolic risk and inflammation.
METHODS
We analyzed the National Health and Nutrition Examination Survey (NHANES) 1999-2004 linked to the National Death Index through December 31, 2019. The NHANES uses a stratified multistage probability sample design to be representative of the US population. Further information about how NHANES conducted the complex survey for 1999-2006 can be found at https://www.cdc.gov/nchs/data/series/sr_02/sr02_155.pdf. Additional information on the weighting of the analyses in the NHANES to make population-based estimates can be found at 05-06-analytic-guidelines.pdf. This 1999-2004 baseline NHANES included 4,252 unweighted adults, with 2,821 males and 1,431 females, aged 20 to 49 years. These participants have complete information available for each body composition and control variables. As a population-based cohort with a complex survey design and appropriate weighting, it provides a population estimate representative of the noninstitutionalized US population of 131 million. All analyses were conducted using the survey package in R 4.3.3 (R Foundation for Statistical Computing) to account for the complex NHANES sampling design and to make population estimates.
Body Composition
Body mass index and waist circumference (WC) were derived from the physical examination in the NHANES. Body mass index is calculated using the body weight in kilograms divided by the square of the height in meters (kg/m2). Although this study is focused on the comparison of an indirect measure of body fat, BMI, with a direct measure of body fat percentage, we also added in one other body composition measure, WC, that is an indirect measure but does not depend on height or weight.37,38 Of note, one study has have shown that standardizing WC by height may make it a more predictive measure.39 Body mass index and WC were measured by trained technicians using a standard protocol. Although BMI is computed for adult patients with the same thresholds regardless of age, race, or sex, both WC and BF% are sex-specific numbers and are standardized by those sex-specific thresholds. Healthy BMI corresponds to previously defined levels from the WHO and NIH6,37 and healthy WC corresponds to previously defined levels from the NIH and CDC.37,38
Body fat percentage was derived from BIA. Bioelectrical impedance analysis measures the electrical impedance of body tissues and can be used to assess fluid volumes, total body water, and fat-free body mass. Even though previous studies defined healthy BF% based on cohorts with a healthy BMI,28,40 there is no consensus for a healthy BF% for young adults like for BMI and WC by the WHO, NIH, and CDC. Because our outcome variable is mortality, we defined healthy BF% thresholds in men and women based on risk of allcause mortality as reported in a 2022 systematic review and dose-response meta-analysis of prospective cohort studies.41
Cohort Definition
In this retrospective cohort analysis, healthy BMI was defined as 18.5-24.9 kg/m2 and overweight/obese BMI as ≥25 kg/m2. Healthy BF% was defined as <27% and <44% and unhealthy BF% as ≥27% and ≥44% in men and women, respectively. Healthy WC was defined as ≤40 and ≤35 inches and unhealthy WC as >40 and >35 inches for men and women, respectively.
Mortality
The National Center for Health Statistics (NCHS) has linked data collected from the NHANES with death certificate records from the National Death Index (NDI). The mortality status for each participant was censored at 15 years to create consistency among follow-up lengths between members of the different NHANES cohorts. This study used the public-use linked mortality files for the 9 cause-specific death categories produced by the NCHS (Public-use Linked Mortality File Readme cdc.gov). We examined all-cause mortality, heart disease mortality, and cancer mortality.
Control Variables in Cox Proportional Hazard Regressions
Control variables we used in our models included age, race, and poverty. Poverty was defined according to the poverty index ratio, a standard measure of total family income divided by the poverty threshold. The poverty threshold accounts for the size of the family and the number of related children in the household under the age of 18 years. Poverty at baseline simply defines whether the individual was living below the poverty line as a baseline exposure characteristic 1999-2004. We categorized individuals in the sample into 2 groups: (1) persons without poverty at baseline (“above poverty”) had a poverty income ratio above 1 indicating that the person was not in poverty at baseline and (2) persons with poverty at baseline (“poverty”) had a poverty income ratio at or below 1 indicating that the person was in poverty at baseline.
Analyses
We conducted descriptive statistics including population estimates and cross tabulation calculated for the 3 body composition measures, BMI, BF%, and WC. Listwise deletion was applied to exclude observations with missing values, ensuring complete cases were included in the regression. We also computed unadjusted Kaplan-Meier curves (KMCs) along with log-rank tests for the body composition measures with 15-year all-cause mortality. We computed both unadjusted and adjusted Cox proportional hazard regressions for 15-year all-cause, heart disease, and cancer mortality for the 3 body composition measures. The adjusted analyses controlled for the key variables of age, race, and poverty. The Cox proportional hazard regressions across all analyses provide a Wald test and likelihood-ratio test. Additionally, the assumption of proportionality in the Cox proportional hazard regressions across all the analyses was tested using the Schoenfeld residuals test.
RESULTS
Table 1 shows the population estimates for demographic characteristics in adults aged 20-49 years. Cross tabulation found that the overlap between BMI and BF% groups in designating healthy or unhealthy status was the lowest at 60%, meaning that BMI and BF% have the greatest difference in the way that healthy/unhealth status is defined. Similarly, the overlaps between the other groups (ie, BMI and WC; BF% and WC) were slightly below 75%. The hazard ratios of the body composition measures with 15-year mortality are shown in Table 2. The hazard ratios show that BMI has no statistically significant relationship with all-cause mortality or cancer mortality in either unadjusted or adjusted regressions. While the unadjusted model shows a statistically significant association between BMI and heart disease mortality, the relationship did not retain significance in the adjusted model. On the other hand, BF% has statistically significant relationships with all-cause mortality and heart disease mortality in both unadjusted and adjusted regressions. Similarly, WC has statistically significant relationships with all-cause mortality and heart disease mortality in both unadjusted and adjusted regressions. Neither BF% nor WC yielded significant relationships with 15-year cancer mortality. The residuals test yielded a P value of ≥ .98 indicating no violation of proportional hazards assumptions. The Wald test (at P < .05) shows that the predictors are statistically significantly associated with the survival.
Table 1.
Population Estimates for Demographic Characteristics in Adults Aged 20-49 Years (Unweighted n = 4,252; Weighted n = 137,341,368)
| Body mass index (BMI) | Body fat percentage (BF%) | Waist circumference (WC) | ||||
|---|---|---|---|---|---|---|
| Overweight/Obese BMI | Healthy BMI | Unhealthy BF% | Healthy BF% | Unhealthy WC | Healthy WC | |
| Race/ethnicity (%) | ||||||
| Hispanic | 46.6 | 53.4 | 28.3 | 71.7 | 35.4 | 64.6 |
| Non-Hispanic Black | 69.9 | 30.1 | 32.2 | 67.8 | 31.4 | 68.6 |
| Non-Hispanic White | 67.6 | 32.4 | 32.8 | 67.2 | 37.0 | 63.0 |
| Other | 66.0 | 34.0 | 33.8 | 66.2 | 40.9 | 59.1 |
| Age, y (%) | ||||||
| 20-29 | 52.3 | 47.7 | 25.6 | 74.4 | 27.7 | 72.3 |
| 30-39 | 60.2 | 39.8 | 27.7 | 72.3 | 35.4 | 64.6 |
| 40-49 | 68.1 | 31.9 | 35.0 | 65.0 | 43.7 | 56.3 |
| Poverty (%) | ||||||
| No poverty | 60.9 | 39.1 | 29.1 | 70.9 | 35.6 | 64.4 |
| Poverty | 57.8 | 42.2 | 32.0 | 68.0 | 37.5 | 62.5 |
| Sex (%) | ||||||
| Male | 64.8 | 35.2 | 35.1 | 64.9 | 28.4 | 71.6 |
| Female | 55.3 | 44.7 | 23.6 | 76.4 | 43.9 | 56.1 |
Table 2.
Cox Proportional Hazard Regression Analyses for All-Cause, Heart Disease, and Cancer Mortality Risk
| Body mass index | ||||||
|---|---|---|---|---|---|---|
| HR | Unadjusted 95% CI | P value | HR | Adjusted 95% CI | P value | |
| All-cause mortality | 1.442 | (0.970-2.145) | .071 | 1.246 | (0.845-1.837) | .268 |
| Heart disease mortality | 2.708 | (1.101-6.662) | .030 | 2.227 | (0.833-5.952) | .110 |
| Cancer mortality | 0.958 | (0.500-1.836) | .897 | 0.784 | (0.400-1.537) | .479 |
| Body fat percentage | ||||||
|---|---|---|---|---|---|---|
| HR | Unadjusted 95% CI | P value | HR | Adjusted 95% CI | P value | |
| All-cause mortality | 2.008 | (1.450-2.781) | < .001 | 1.780 | (1.282-2.471) | < .001 |
| Heart disease mortality | 4.203 | (1.939-9.111) | < .001 | 3.620 | (1.552-8.445) | .003 |
| Cancer mortality | 1.535 | (0.791-2.979) | .205 | 1.293 | (0.682-2.453) | .431 |
| Waist circumference | ||||||
|---|---|---|---|---|---|---|
| HR | Unadjusted 95% CI | P value | HR | Adjusted 95% CI | P value | |
| All-cause mortality | 1.940 | (1.384-2.720) | < .001 | 1.593 | (1.123-2.259) | .009 |
| Heart disease mortality | 4.753 | (2.453-9.209) | < .001 | 4.007 | (1.941-8.271) | < .001 |
| Cancer mortality | 0.895 | (0.420-1.905) | .774 | 0.675 | (0.309-1.476) | .325 |
HR = hazard ratio.
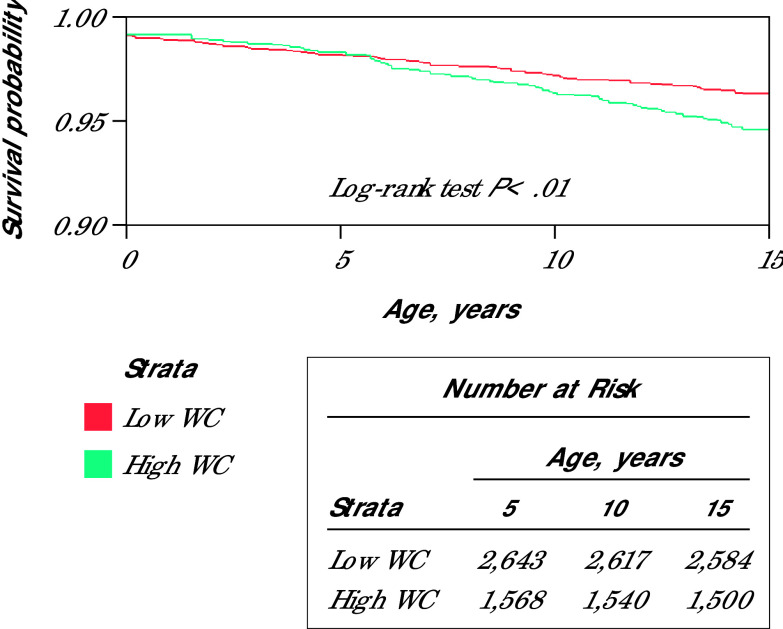
Figures 1-3 present the unadjusted KMCs for all 3 groups using different thresholds of BMI, BF%, and WC, respectively. Figure 1 uses a BMI threshold of 25 kg/m2 to define overweight/obesity, Figure 2 uses a BF% threshold of 27% for men and 44% for women to define unhealthy body fat, and Figure 3 uses a WC threshold of 40 inches for men and 35 inches for women to define unhealthy WC. The red line represents adults with low values of BMI, BF%, or WC, while the green line represents those with high values. The KMCs display the relationship between body composition and mortality over 15-years. Kaplan-Meier curves for BF% and WC indicate a stronger association with all-cause mortality over a 15-year period compared with BMI at specific thresholds across all 3 groups (Figures 1-3). The log-rank test P values suggest that BF% and WC (both P < .01) show stronger evidence of survival differences than BMI (P = .05). This suggests that BF% and WC are more reliable risk factors of all-cause mortality over 15 years than BMI.
Figure 1.
Unadjusted Kaplan-Meier Survival Curve for 15-Year All-Cause Mortality Among Adults Aged 20-49 Years With Healthy and Overweight/Obese Body Mass Index
BMI = body mass index.
Figure 3.
Unadjusted Kaplan-Meier Survival Curve for 15-Year All-Cause Mortality Among Adults Aged 20-49 Years With Healthy and Unhealthy Waist Circumference
WC = Waist circumference
Figure 2.
Unadjusted Kaplan-Meier Survival Curve for 15-Year All-Cause Mortality Among Adults Aged 20-49 Years With Healthy and Unhealthy Body Fat Percentage
BF% = Body fat percentage.
DISCUSSION
This study demonstrates the value of a new and relatively unused measure of body composition to predict health risk. Rather than using an indirect measure of body fat percentage, BMI, a direct measure of body fat percentage showed significantly greater utility in predicting downstream risk. Using BIA, body fat percentage had a much stronger association with 15-year mortality than the standard body composition measure of BMI in adults aged 20-49 years. These results suggest rethinking how we should measure body composition in the clinical setting.
Although BMI is the most commonly used measure of body composition in primary care, it is an indirect measure of body fat percentage and thus has some limitations.2,3,11,13-24 The obesity paradox does not appear in other measures of adiposity such as WC42 or body roundness index (ie, using WC),43 which have clear associations with mortality, and WC builds on the concept that fat located in certain body locations is more indicative of risk than other locations. Waist circumference is also an indirect measure, however, and unlike measurements of height and weight, it requires a specific technique that is complex (eg, timed to breath, requires measurement be equidistant from the anterior superior iliac spine and the lower rib margin in patients with a pannus), timely (eg, requires partial disrobing), and not standardized.44 Waist circumference measurements therefore have significant issues with inter-rater measurement error and reliability such that they lack both reproducibility and the ability to determine clinically relevant change.45 Our results suggest that there are significant advantages to measuring BF% directly to predict downstream risk of mortality. Although DXA has been shown to be an accurate predictor of body composition, it is not cost effective or practical in the primary care setting.2,27 As the price of BIA decreases and accuracy increases, this technology will become increasingly attractive to clinicians desiring an alternative, more accurate risk measurement to BMI.2,27,29,30 It should be noted that the current study used BIA technology from 25 years ago and that it still had stronger associations with mortality when compared with BMI. Current BIA models provide reproducible results in less than 1 minute, making their adoption compatible with current outpatient clinic workflows.
There are several strengths of this study, including using BF% in a nationally representative cohort. Second, this study provided a real-life comparison of downstream risk prediction of the current industry standard for body composition, BMI, vs another available measure of body composition, BF%. A common criticism of measures other than BMI is that they are not viable in a standard clinical setting. However, BIA is inexpensive, reliable, valid, and can be easily integrated into a clinic setting to measure BF%.2,27,29,30 This important tool allowed us to explore a range of body fat percentages as a predictor of mortality, independent of BMI, and therefore in line with those studies showing BF% to be a better measure of the health consequences of an unhealthy body composition.2,13,15,17-19,25,27 Further, we were able to use a very strong outcome, mortality, in a 15-year cohort, thereby looking at relatively long-term impacts of body composition.
There are several limitations to this study. First, our thresholds for BF% in men and women are based on allcause mortality data from a recent systematic review and meta-analysis.41 While these BF% thresholds are taken from a Level 2A study that also focused on mortality, healthy BF% thresholds have not been standardized like BMI and WC. Second, the age of the population for study was limited by the NHANES 1999-2004, but future studies should extend this comparison of BF% to BMI in older adults. Third, our study focused on mortality as an outcome. This is the strongest and most definitive health outcome, but morbidity outcomes like myocardial infarction or newly diagnosed cancer may help to flesh out our understanding of BF% as a body composition risk factor for developing disease. Fourth, the poverty index ratio is a global measure that does not account for geographic and other variations in poverty, but it is the best estimation of poverty that can be used in this data set. Fifth, even though there are demographics like smoking that have been shown to have an association with BMI and mortality,46,47 the goal of the study was to mirror the way that clinicians currently risk stratify patients by body composition in the office. The guidelines and thresholds for BMI, for example, are not dependent on age, sex, or smoking status. The healthy/unhealthy BMI threshold is used independently. Body fat percentage and WC are sex specific but not interpreted in the context of either age or smoking. Our goal was not to see if BMI is independent of smoking but rather to see if a different measure of body composition does a better job of downstream risk assessment than BMI as we currently use it.
Future directions include large prospective studies to evaluate the morbidity and mortality of different body fat percentages across populations to determine standard, healthy BF% ranges. Once these standards are validated, it is likely that measuring BF% with BIA will become standard of care. These data will drive better discussions in the doctor’s office as well as public health initiatives with the goal of improving the health of all.
CONCLUSION
Body fat percentage is an easily measured body composition variable that may have a stronger association with downstream mortality in young adults than BMI. This could ultimately lead to a change in how we measure body composition for risk stratification.
Footnotes
Conflicts of interest: authors report none.
References
- 1.Bradshaw PT. Body composition and cancer survival: a narrative review. Br J Cancer. 2024; 130(2): 176-183. doi: 10.1038/s41416-023-02470-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sneed NM, Morrison SA.. Body composition methods in adults with type 2 diabetes or at risk for T2D: a clinical review. Curr Diab Rep. 2021; 21(5): 14. doi: 10.1007/s11892-021-01381-9 [DOI] [PubMed] [Google Scholar]
- 3.Powell-Wiley TM, Poirier P, Burke LE, et al. ; American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council . Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021; 143(21): e984-e1010. doi: 10.1161/CIR.0000000000000973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention . What are overweight and obesity? Published May 20, 2024. Accessed Oct 18, 2024. Body mass index (BMI). https://www.cdc.gov/bmi/about/index.html
- 5.National Heart, Lung, and Blood Institute; National Institutes of Health . Published Mar 24, 2022. Accessed Jul 8, 2024. https://www.nhlbi.nih.gov/health/overweight-and-obesity
- 6.World Health Organization . Obesity and overweight. Published Mar 1, 2024. Accessed Jul 8, 2024. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- 7.American Diabetes Association (ADA) . Body mass index in adults. Accessed Jul 8, 2024. Obesity care and beyond. https://diabetes.org/obesity
- 8.American Heart Association (AHA) . Published 2024. Accessed Jul 8, 2024. https://www.heart.org/en/healthy-living/healthy-eating/losing-weight/bmi-in-adults
- 9.Centers for Disease Control and Prevention . National diabetes statistics report. Published May 15, 2024. Accessed Jul 8, 2024. https://www.cdc.gov/diabetes/php/data-research/index.html
- 10.Sinha A, Ning H, Carnethon MR, et al. Race- and sex-specific population attributable fractions of incident heart failure: a population-based cohort study from the lifetime risk pooling project. Circ Heart Fail. 2021; 14(4): e008113. doi: 10.1161/CIRCHEARTFAILURE.120.008113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan SS, Matsushita K, Sang Y, Ballew SH, Grams ME, Surapaneni A, et al. Development and validation of the American Heart Association’s PREVENT equations [published correction appears in Circulation. 2024; 149(11): e956. doi: 10.1161/CIR.0000000000001230]. Circulation. 2024; 149(6): 430-449. doi: 10.1161/CIRCULATIONAHA.123.067626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention . About adult BMI. Published Jun 2022. Accessed Jul 9, 2024. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
- 13.National Academies of Sciences, Engineering, and Medicine . Exploring the Science on Measures of Body Composition, Body Fat Distribution, and Obesity: Proceedings of a Workshop Series. The National Academies Press; 2024. doi: 10.17226/27461 [DOI] [PubMed] [Google Scholar]
- 14.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. [Published correction appears in Circulation. 2019; 140(11): e649-e650. doi: 10.1161/CIR.0000000000000725. Published correction appears in Circulation. 2020; 141(4): e60. doi: 10.1161/CIR.0000000000000755. Published correction appears in Circulation. 2020; 141(16): e774. doi: 10.1161/CIR.0000000000000771]. Circulation. 2019; 140(11): e596-e646. doi: 10.1161/CIR.0000000000000678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franco LP, Morais CC, Cominetti C.. Normal-weight obesity syndrome: diagnosis, prevalence, and clinical implications. Nutr Rev. 2016; 74(9): 558-570. doi: 10.1093/nutrit/nuw019 [DOI] [PubMed] [Google Scholar]
- 16.Sahakyan KR, Somers VK, Rodriguez-Escudero JP, et al. Normal-Weight central obesity: implications for total and cardiovascular mortality. Ann Intern Med. 2015; 163(11): 827-835. doi: 10.7326/M14-2525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Batsis JA, Sahakyan KR, Rodriguez-Escudero JP, Bartels SJ, Somers VK, Lopez-Jimenez F.. Normal weight obesity and mortality in United States subjects ≥60 years of age (from the Third National Health and Nutrition Examination Survey). Am J Cardiol. 2013; 112(10): 1592-1598. doi: 10.1016/j.amjcard.2013.07.014 [DOI] [PubMed] [Google Scholar]
- 18.Kim JY, Han SH, Yang BM.. Implication of high-body-fat percentage on cardiometabolic risk in middle-aged, healthy, normal-weight adults. Obesity (Silver Spring). 2013; 21(8): 1571-1577. doi: 10.1002/oby.20020 [DOI] [PubMed] [Google Scholar]
- 19.Gómez-Ambrosi J, Silva C, Galofré JC, et al. Body adiposity and type 2 diabetes: increased risk with a high body fat percentage even having a normal BMI. Obesity (Silver Spring). 2011; 19(7): 1439-1444. doi: 10.1038/oby.2011.36 [DOI] [PubMed] [Google Scholar]
- 20.Provencher MT, Chahla J, Sanchez G, et al. Body mass index versus body fat percentage in prospective National Football League athletes: overestimation of obesity rate in athletes at the National Football League scouting combine. J Strength Cond Res. 2018; 32(4): 1013-1019. doi: 10.1519/JSC.0000000000002449 [DOI] [PubMed] [Google Scholar]
- 21.Chen Y, Koirala B, Ji M, et al. Obesity paradox of cardiovascular mortality in older adults in the United States: a cohort study using 1997-2018 National Health Interview Survey data linked with the National Death Index. Int J Nurs Stud. 2024; 155: 104766. doi: 10.1016/j.ijnurstu.2024.104766 [DOI] [PubMed] [Google Scholar]
- 22.Mathur MB, Mathur VS.. Toward evidence-based communication on overweight body mass index and mortality. BMC Med. 2024; 22(1): 183. doi: 10.1186/s12916-024-03402-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khan SS, Ning H, Wilkins JT, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018; 3(4): 280-287. doi: 10.1001/jamacardio.2018.0022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flegal KM, Kit BK, Orpana H, Graubard BI.. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013; 309(1): 71-82. doi: 10.1001/jama.2012.113905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neamat-Allah J, Wald D, Hüsing A, et al. Validation of anthropometric indices of adiposity against whole-body magnetic resonance imaging—a study within the German European Prospective Investigation into Cancer and Nutrition (EPIC) cohorts. PLoS One. 2014; 9(3): e91586. doi: 10.1371/journal.pone.0091586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Potter AW, Chin GC, Looney DP, Friedl KE.. Defining overweight and obesity by percent body fat instead of body mass index. J Clin Endocrinol Metab. 2025; 110(4): e1103-e1107. doi: 10.1210/clinem/dgae341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cruz Rivera PN, Goldstein RL, Polak M, Lazzari AA, Moy ML, Wan ES.. Performance of bioelectrical impedance analysis compared to dual X-ray absorptiometry (DXA) in Veterans with COPD. Sci Rep. 2022; 12(1): 1946. doi: 10.1038/s41598-022-05887-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y.. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000; 72(3): 694-701. doi: 10.1093/ajcn/72.3.694 [DOI] [PubMed] [Google Scholar]
- 29.Holmes CJ, Racette SB.. The utility of body composition assessment in nutrition and clinical practice: an overview of current methodology. Nutrients. 2021; 13(8): 2493. doi: 10.3390/nu13082493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liao YS, Li HC, Lu HK, Lai CL, Wang YS, Hsieh KC.. Comparison of bioelectrical impedance analysis and dual energy X-ray absorptiometry for total and segmental bone mineral content with a three-compartment model. Int J Environ Res Public Health. 2020; 17(7): 2595. doi: 10.3390/ijerph17072595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bosello O, Vanzo A.. Obesity paradox and aging. Eat Weight Disord. 2021; 26(1): 27-35. doi: 10.1007/s40519-019-00815-4 [DOI] [PubMed] [Google Scholar]
- 32.Javed AA, Aljied R, Allison DJ, Anderson LN, Ma J, Raina P.. Body mass index and all-cause mortality in older adults: a scoping review of observational studies. Obes Rev. 2020; 21(8): e13035. doi: 10.1111/obr.13035 [DOI] [PubMed] [Google Scholar]
- 33.Winter JE, MacInnis RJ, Nowson CA.. The influence of age on the BMI and allcause mortality association: meta-analysis. J Nutr Health Aging. 2017; 21(10): 1254-1258. doi: 10.1007/s12603-016-0837-4 [DOI] [PubMed] [Google Scholar]
- 34.Qu Q, Guo Q, Sun J, et al. Low lean mass with obesity in older adults with hypertension: prevalence and association with mortality rate. BMC Geriatr. 2023; 23(1): 619. doi: 10.1186/s12877-023-04326-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abramowitz MK, Hall CB, Amodu A, Sharma D, Androga L, Hawkins M.. Muscle mass, BMI, and mortality among adults in the United States: a population-based cohort study. [Published correction appears in PLoS One. 2018; 13(5): e0198318. doi: 10.1371/journal.pone.0198318]. PLoS One. 2018; 13(4): e0194697. doi: 10.1371/journal.pone.0194697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mainous AG III, Sharma P, Jo A.. Systemic inflammation among adults with diagnosed and undiagnosed cardiometabolic conditions: a potential missed opportunity for cardiovascular disease prevention. Front Med (Lausanne). 2024; 10: 1327205. doi: 10.3389/fmed.2023.1327205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Heart, Lung, and Blood Institute; National Institutes of Health . Overweight and obesity symptoms and diagnosis. Published Mar 24, 2022. Accessed Jul 8, 2024. https://www.nhlbi.nih.gov/health/overweight-and-obesity/symptoms
- 38.Centers for Disease Control and Prevention . Diabetes: healthy weight. Published May 15, 2024. Accessed Oct 18, 2024. https://www.cdc.gov/diabetes/living-with/healthy-weight.html
- 39.Savva SC, Tornaritis M, Savva ME, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Relat Metab Disord. 2000; 24(11): 1453-1458. doi: 10.1038/sj.ijo.0801401 [DOI] [PubMed] [Google Scholar]
- 40.Pasco JA, Holloway KL, Dobbins AG, Kotowicz MA, Williams LJ, Brennan SL.. Body mass index and measures of body fat for defining obesity and underweight: a cross-sectional, population-based study. BMC Obes. 2014; 1: 9. doi: 10.1186/2052-9538-1-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jayedi A, Khan TA, Aune D, Emadi A, Shab-Bidar S.. Body fat and risk of all-cause mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Int J Obes (Lond). 2022; 46(9): 1573-1581. doi: 10.1038/s41366-022-01165-5 [DOI] [PubMed] [Google Scholar]
- 42.Cerhan JR, Moore SC, Jacobs EJ, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin Proc. 2014; 89(3): 335-345. doi: 10.1016/j.mayocp.2013.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang X, Ma N, Lin Q, et al. Body roundness index and all-cause mortality among US adults. JAMA Netw Open. 2024; 7(6): e2415051. doi: 10.1001/jamanetworkopen.2024.15051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Okamoto N, Hosono A, Shibata K, et al. Accuracy of self-reported height, weight and waist circumference in a Japanese sample. Obes Sci Pract. 2017; 3(4): 417-424. doi: 10.1002/osp4.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Verweij LM, Terwee CB, Proper KI, Hulshof CT, van Mechelen W.. Measurement error of waist circumference: gaps in knowledge. Public Health Nutr. 2013; 16(2): 281-288. doi: 10.1017/S1368980012002741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bigaard J, Tjønneland A, Thomsen BL, Overvad K, Heitmann BL, Sørensen TI.. Waist circumference, BMI, smoking, and mortality in middle-aged men and women. Obes Res. 2003; 11(7): 895-903. doi: 10.1038/oby.2003.123 [DOI] [PubMed] [Google Scholar]
- 47.Whitlock G, Lewington S, Sherliker P, et al. ; Prospective Studies Collaboration . Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009; 373(9669): 1083-1096. doi: 10.1016/S0140-6736(09)60318-4 [DOI] [PMC free article] [PubMed] [Google Scholar]