Abstract
Background
The efficacy of orthokeratology (Ortho-K) in controlling myopia is influenced by many complex factors, which makes predicting the effect of myopia control a complicated task. This study aimed to analyze the relevant factors that can predict the axial length elongation (ALE) in patients wearing Ortho-K, including baseline ocular parameters, genetic factors and lifestyle habits.
Methods
In this retrospective study, 542 eyes from 300 myopic children wearing Ortho-K were reviewed from the Optometry Centre of Peking University People’s Hospital from January 2022 to December 2023. Baseline characteristics such as age, gender, spherical equivalent refraction (SER), horizontal visible iris diameter (HVID), mean keratometry value (mean K), corneal astigmatism, corneal eccentricity (E-value), anterior chamber depth (ACD), central corneal thickness (CCT), pupil diameter (PD), treatment zone area (TZA) and treatment zone decentration distance were measured. Additionally, parental factors and lifestyle habits, including parental myopia status, continuous near-work time, weight change, height change, age of diagnosis of myopia, eating sweets, regular follow-ups, online-class, interest class, outdoor activity and reading and writing posture were collected via questionnaires. Linear mixed effect model was constructed to identify factors associated with ALE.
Results
Linear mixed effect model revealed that patients had a higher ALE who started wearing Ortho-k lenses at a younger age (P < 0.001), had less myopia (P < 0.001), high-myopia in both parents (P = 0.018). Conversely, patients had slower ALE with a larger decentration distance of the treatment zone (P = 0.002) and regular follow-ups (P = 0.001).
Conclusions
Age, SER and parental high myopia are critical factors to predict efficacy of orthokeratology in inhibiting axial elongation in myopic children. Orthokeratology lens decentration and regular follow-ups have a positive impact on myopia control. The decentration can be considered preserved when there is no obvious visual interference or complications.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12886-025-04265-8.
Keywords: Orthokeratology, Myopia, Axial elongation, Lifestyle habits
Introduction
In recent years, myopia has become a global concern regarding ocular health, with an increasingly younger demographic among myopic patients and a rising incidence of complications associated with myopia [1, 2].Many myopic individuals continue to experience the progression of myopia into adulthood [3, 4], indicating that myopia prevention and control may be a long-term issue. Holden et al. conducted a meta-analysis of data on the prevalence of myopia published since 1995 and projected that nearly half of the global population could be myopic by 2050, with 9.8% having high myopia, posing a significant healthcare burden [5].
The exact etiology of myopia remains unclear, and clinical practice mainly focuses on preventing and slowing its progression. The primary measure of myopia progression is axial length, where rapid elongation predicts higher myopia degrees and the occurrence of ocular fundus diseases. Orthokeratology (Ortho-K), which are rigid gas permeable contact lenses worn overnight, utilize a reverse geometry design to flatten the cornea, achieving myopia control. Ortho-K have demonstrated effective control of myopia progression in children and adolescents [6–8]. Therefore, understanding how to predict myopia progression earlier when using Ortho-K is significantly important for clinical efficacy assessment.
Several studies have investigated the influence of different ocular baseline parameters on the efficacy of Ortho-K in controlling myopia progression. Many studies suggest that older age at the time of Ortho-K fitting, higher baseline spherical equivalent refraction (SER), and smaller corneal eccentricity (E-value) in patients are associated with a reduced rate of axial length elongation (ALE) [9, 10]. Decentration of the treatment zone may slow axial elongation, possibly due to increased higher-order aberrations during corneal remodeling. Children with parents who have high myopia and those engaged in prolonged near work exhibit a faster rate of ALE [11–13].
However, some findings are controversial. Chen et al. reported that larger pupil diameter may facilitate the slowing of axial elongation [14], while Wang et al. found no correlation between pupil diameter and ALE [9]. Most studies agree that outdoor activity can slow myopia progression [15–17], but the threshold for the protective effect of outdoor activity remains unclear [18]. There is a lack of large-scale studies investigating the relationship between baseline ocular parameters, lifestyle habits, and the elongation of axial length in myopic children wearing Ortho-K. Identifying the children who are likely to gain the greatest benefit from myopic control using Ortho-K specifically is a clinical challenge. The purpose of this study was to comprehensively assess the impact of baseline ocular parameters, parental high myopia and other lifestyle habits on the treatment efficacy of Ortho-K.
Methods
Subjects
This retrospective study included clinical data from myopic children who wore Ortho-K at the Optometry Center of Peking University People’s Hospital from January 2022 to December 2023. Information regarding parental myopia status and visual habits was collected through questionnaires. Each patient was assigned a specific identification number, and the main purpose and details of the study were explained to the children and their parents or legal guardians. This study followed the tenets of the Declaration of Helsinki and was approved by the Medical Ethics Committee of Peking University People’s Hospital.
The inclusion criteria were as follows:
No prior history of orthokeratology lens fitting and fulfills the fitting criteria for Ortho-K;
No history of using atropine eye drops;
Cycloplegic refraction results with a spherical power of no less than − 0.75 diopters (D) and astigmatism no greater than 3.00 D;
Best-corrected visual acuity of log MAR 0.1 or better.
The exclusion criteria were as follows:
Patients with significant strabismus or amblyopia;
Those with ocular or systemic diseases that prevented them from adhering to ortho-k treatment, such as severe allergic conjunctivitis;
Those patients and guardians unwilling to cooperate with the study.
Data collection
Ocular parameters and measurement method
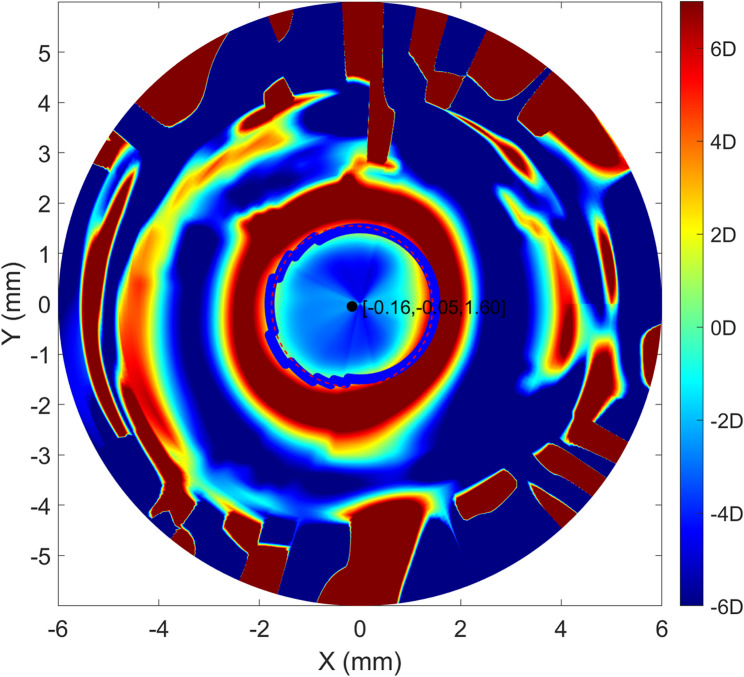
The data collected for this study included the initial age at first visit, gender, SER, central corneal thickness (CCT), mean keratometry value (mean K), corneal astigmatism, E-value, horizontal visible iris diameter (HVID), anterior chamber depth (ACD), pupil diameter (PD)and ALE. Corneal parameters were obtained using the Sirius corneal topography system (Costruzione Strumenti Oftalmici, Florence, Italy) and baseline and one-month post-Ortho-K treatment corneal sagittal height data were exported as CSV files from the Sirius system. A customized specific MATLAB program was utilized to calculate treatment zone area (TZA) and treatment zone decentration distance [19–21]. A total of 256 points defined the TZ boundaries as transition points from negative to positive values, automatically extracted from the tangential difference map. The best fit radius of the “ring” formed by these points was calculated using the least squares method. The TZ area was computed as π × r², and the eccentric distance of the treatment zone was also inferred from this ring. (Fig. 1)
Fig. 1.
Clinical tangential power difference map after Ortho-K treatment. The horizontal and vertical decentration of the patient were − 0.16 mm and − 0.05 mm, respectively. The radius of treatment zone size was 1.60 mm
The axial length was measured at baseline and every 3-month interval using the IOL Master 700(Carl Zeiss Meditec, Oberkochen, Germany), with data averaged from six repeated measurements for analysis. Cycloplegic refraction was only measured at baseline. After instilling compound tropicamide eye drops (Tropicamide 0.5%, Phenylephrine HCl 0.5%; Shenyang Xingqi Pharmaceutical Co.,Ltd, China) three times every five minutes, loss of direct light reaction and mydriasis was confirmed. Cycloplegic refraction was performed 30 min later to measure spherical diopter. Due to the practical circumstances in clinical settings, the time frame for patients to return for follow-up examinations often fluctuates within a one-month range. Therefore, this study attempts to mitigate the impact of varying time intervals through computational methods. The elongation in axial length was calculated as the difference between the follow-up axial length and the baseline axial length, divided by the time interval and multiplied by 365. The SER was calculated as the sum of the spherical diopter and half the astigmatic diopter.
Questionnaire
Factors related to genetic predisposition and lifestyle habits were assessed through a questionnaire. Incomplete or evidently insincere responses were discarded. Genetic factors primarily referred to the parental high myopia status, while lifestyle habits encompassed reading and writing posture, online class, interest class and outdoor activity which were recorded, graded, and assigned values. Other related variables included continuous near-work time, changes in height, changes in weight, age at diagnosis of myopia, eating sweets, and regular follow-up. According to the previous research results [22] and the actual time spent in daily activities of the research population, the questionnaire provided five options.: almost no time, level 1; <1.5 h, level 2; <3 h, level 3; <6 h, level4; >6 h, level5. Reading and writing postures included standard posture, left or right head tilt, close distance (< 30 cm) [23] and reading on bed. (Supplementary Table S1) Ordinal classification variables were used to categorize the duration and intensity of different activities, and nominal variables were processed through dummy coding. To mitigate the influence of fitting variations, orthokeratology lens fitting was conducted by experienced clinicians.
Statistical analysis
The data were analyzed using the SPSS statistical software package (Version 27.0, IBM Corp., US). Continuous data were expressed as mean ± SD, categorical data were expressed as counts and percentages. To account for inter-eye correlations within participants, a linear mixed-effects model (LMM) with a random intercept per participant was applied. The model structure included Participant ID as a random effect, allowing bilateral eye data to be analyzed without violating independence assumptions. Ocular biological parameters, parental myopia, and lifestyle habits were included as fixed effects to identify determinants of ALE [24]. Perform univariate analyses using LMM, and Benjamini-Hochberg method was used to correct and control the error detection rate (FDR = 0.15). The influence of each independent variable on ALE was evaluated, and the screened variables were included in the multiple regression model. We employed backward stepwise selection guided by the Akaike Information Criterion (AIC), prioritizing models that optimally balance complexity and goodness of fit. At each iteration, the fixed effect variable whose removal resulted in the lowest AIC (indicating the least detrimental effect on model quality) was eliminated. The process terminated when removing any remaining variable increased the AIC. Fixed effect estimates were reported as unstandardized coefficients (β) with 95% confidence intervals (CI) and P value. The significance level was set to be 0.05, 2-tailed.
Results
We collected the case data of 603 eyes, of which 61 eyes were discarded due to lack of data and poor quality of questionnaires, and 542 eyes from 300 patients were finally included in the analysis (binocular data of 242 patients and monocular data of 58 patients). The annual axial elongation of the study population was 0.17 ± 0.16 mm/year, of which 323 eyes (59.59%) had ALE less than 0.2 mm and 23 eyes (4.24%) had ALE greater than 0.45 mm (Fig. 2). Basic demographic statistics were shown in Table 1. Descriptions of classification variables were shown in Table 2.
Fig. 2.
Frequency distribution histogram of axial length elongation
Table 1.
Clinical characteristics of the study population
| Variables† | Mean ± SD, n (%) |
|---|---|
| Age (year) | 9.07 ± 1.59 |
| Gender (male) | 141 (47%) |
| Eye (R/L) | 278/264 |
| HVID (mm) | 11.90 ± 0.41 |
| Mean K(D) | 43.30 ± 1.46 |
| Cornea astigmatism (D) | 1.04 ± 0.43 |
| E-value | 0.47 ± 0.28 |
| ACD (mm) | 3.33 ± 0.24 |
| CCT (mm) | 0.55 ± 0.03 |
| SER (D) | −2.00 ± 1.10 |
| PD (mm) | 3.85 ± 0.71 |
| TZA (mm2) | 11.59 ± 2.81 |
| Horizontal decentration (mm) | −0.05 ± 0.50 |
| Vertical decentration (mm) | −0.15 ± 0.35 |
| Decentration (mm) | 0.57 ± 0.28 |
| Continuous near-work time (hour) | 2.27 ± 1.55 |
| Height change (cm) | 6.82 ± 2.73 |
| Weight change (kg) | 3.98 ± 2.35 |
| Age at diagnosis of myopia (year) | 8.01 ± 1.68 |
| Eating sweets | 164 (54.67%) |
| Regular follow-ups | 298 (99.33%) |
| ALE (mm) | 0.17 ± 0.16 |
Regular follow-ups were defined as patients being followed up according to the review cycle of Ortho-K lenses. Cases with excessively long intervals or missing reviews were considered unqualified for regular follow-ups
† The distribution of ocular biological parameters, including HVID, mean K, cornea astigmatism, E-value, ACD, CCT, SER, PD, TZA, horizontal decentration, vertical decentration, decentration and ALE were described based on the number of eyes (542 eyes), while other parameters were described based on the number of patients (300 patients)
Table 2.
Distribution of categorical variables
| Categorical variables† | n (%) | ||||
|---|---|---|---|---|---|
| Ordinal variables | Level1 | Level2 | Level3 | Level4 | Level5 |
| Online class | 24(8.00) | 161(53.66) | 83(27.67) | 21(7.00) | 11(3.67) |
| Interest class | 40(13.33) | 201(67.00) | 51(17.00) | 6(2.00) | 2(0.67) |
| Outdoor activity | 10(3.33) | 182(60.67) | 100(33.33) | 7(2.33) | 1(0.33) |
| Parents with high myopia | 213(71.00) | 78(26.00) | 9(3.00) | NA | NA |
| Unordered variables | |||||
| Reading and writing posture |
Correct posture 64(21.33) |
Head tilted left 115(38.33) |
Head tilted right 27(9.00) |
Short distance 86(28.67) |
Read on bed 8(2.67) |
| Direction of decentration |
Superonasal 13(2.40) |
Superotemporal 150(27.68) |
Inferotemporal 356(65.68) |
Inferonasal 23(4.24) |
|
†The direction of decentration was presented as number of eyes (542 eyes), other parameters were described based on the number of patients (300 patients)
Univariate analysis showed that age, SER, decentration, regular follow-ups, age at diagnosis of myopia, reading and writing posture and parental myopia status were associated with axial length progression. After including these factors in the multiple linear mixed effects model, the final model was determined according to the AIC-based backward selection. Table 3 presented the results of the best-fitting linear mixed model analyzing associations between basic characteristics, parental myopia and axial elongation. Older age (β=−0.027, P < 0.001), higher myopia (β = 0.027, P < 0.001), greater decentration distance (β=−0.062, P = 0.002) and regular follow-ups (β=−0.325, P = 0.001) were associated with slower axial elongation. Both parents with high myopia increased axial elongation risk (β = 0.117, P = 0.018).
Table 3.
Linear mixed models with 12-month axial length elongation as response variables
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| β (95%CI) | P † | β (95%CI) | P | |
| Age(year) | −0.033 (−0.043, −0.023) | 0.004†† | −0.027 (−0.037, −0.017) | < 0.001* |
| Gender (male as reference) | −0.004 (−0.038,0.031) | 0.140 | ||
| HVID (mm) | 0.015 (−0.02,0.049) | 0.091 | ||
| Mean K(D) | 0.002 (−0.01,0.013) | 0.128 | ||
| Cornea astigmatism(D) | −0.004 (−0.035,0.027) | 0.132 | ||
| E-value | 0.001 (−0.051,0.053) | 0.15 | ||
| ACD (mm) | −0.064 (−0.132,0.005) | 0.029 | ||
| CCT (mm) | −0.16 (−0.674,0.355) | 0.106 | ||
| SER (D) | 0.031 (0.017,0.045) | 0.007†† | 0.027 (0.014,0.041) | < 0.001* |
| PD (mm) | −0.012 (−0.033,0.008) | 0.062 | ||
| TZA (mm2) | −0.003 (−0.007,0.002) | 0.070 | ||
| Horizontal decentration (mm) | 0.01 (−0.005,0.026) | 0.044 | ||
| Vertical decentration (mm) | 0.012 (−0.017,0.041) | 0.095 | ||
| Decentration(mm) | −0.062 (−0.103, −0.022) | 0.018†† | −0.062 (−0.101, −0.022) | 0.002* |
| Continuous near-work time (hour) | −0.007 (−0.018,0.004) | 0.040 | ||
| Height change (cm) | 0.003 (−0.003,0.01) | 0.077 | ||
| Weight change (kg) | 0.004 (−0.003,0.011) | 0.080 | ||
| Age at diagnosis of myopia (year) | −0.02 (−0.03, −0.011) | 0.011†† | ||
| Eating sweets | 0.022 (−0.013,0.056) | 0.055 | ||
| Regular follow-ups | −0.336 (−0.549, −0.123) | 0.015†† | −0.325 (−0.522, −0.128) | 0.001* |
| Online class | ||||
| Level1 as reference | ||||
| Level2 | −0.007 (−0.07,0.055) | 0.135 | ||
| Level3 | −0.028 (−0.094,0.037) | 0.088 | ||
| Level4 | −0.056 (−0.143,0.03) | 0.051 | ||
| Level5 | −0.069 (−0.167,0.028) | 0.037 | ||
| Interest class | ||||
| Level1 as reference | ||||
| Level2 | 0.01 (−0.042,0.061) | 0.113 | ||
| Level3 | −0.01 (−0.073,0.053) | 0.121 | ||
| Level4 | 0.019 (−0.113,0.151) | 0.124 | ||
| Level5 | −0.071 (−0.285,0.143) | 0.102 | ||
| Outdoor activity | ||||
| Level1 as reference | ||||
| Level2 | -0.058 (-0.153,0.037) | 0.059 | ||
| Level3 | −0.021 (−0.119,0.076) | 0.110 | ||
| Level4 | 0.004 (−0.14,0.148) | 0.146 | ||
| Level5 | −0.011 (−0.318,0.296) | 0.143 | ||
| Parents with high myopia | ||||
| No high-myopia as reference | ||||
| one-high myopia | 0.03 (−0.009,0.068) | 0.033 | 0.028 (−0.009,0.064) | 0.137 |
| both-high myopia | 0.12 (0.02,0.221) | 0.026†† | 0.117 (0.02,0.214) | 0.018* |
| Reading and writing posture | ||||
| correct posture as reference | ||||
| head tilted left | 0.03 (−0.016,0.077) | 0.048 | ||
| head tilted right | 0.026 (−0.042,0.094) | 0.099 | ||
| short distance | 0.064 (0.015,0.113) | 0.022†† | ||
| read on bed | 0.045 (−0.056,0.146) | 0.084 | ||
| Direction of decentration | ||||
| Inferonasal as reference | ||||
| Superonasal | 0.013 (−0.068,0.095) | 0.117 | ||
| Superotemporal | 0.032 (−0.023,0.088) | 0.069 | ||
| Inferotemporal | 0.031 (−0.023,0.084) | 0.073 | ||
†P-value was adjusted by Benjamini-Hochberg method
†† These variables were screened and included in the multiple regression model. According to AIC principle, age at diagnosis of myopia and reading and writing posture were excluded
* P < 0.05 was statistically significant
Discussion
Ortho-K have become one of the effective methods for controlling myopia progression. However, some patients show poor responses to Ortho-K wear, failing to adequately slow axial elongation. Clinically, the effectiveness of myopia control with Ortho-K is often evaluated based on axial length changes over the first three to six months. During this period, children with insensitivity in their axial length may not receive effective control, leading to prolonged trial and error time. Therefore, predicting axial elongation based on baseline ocular parameters, lifestyle habits, and genetic factors could provide a more accurate and timely assessment of the effectiveness of Ortho-K for individual patients.
The effectiveness of Ortho-K in controlling myopia is influenced by various factors. Previous studies have analyzed the factors including the age of lens wear, SER and parental myopia status [13, 25, 26]. The findings of this study are consistent with most researches, showing that younger baseline age, less myopia and both parents having high myopia are associated with faster ALE. Leslie et al. suggested that younger age is a strong correlate of faster myopia progression [27], indicating that children who develop myopia earlier may have pathological myopia and potentially greater genetic risks for high myopia. Alternatively, older children may exhibit more stable refractive error, whereas younger children are still in their developmental and unstable phase. In clinical practice, various factors need to be comprehensively considered. The clinical benefits of using OK lenses to reduce axial length elongation and myopia progression in the early stage need to be balanced with the safety and practical limitations of wearing rigid permeable contact lenses. Pauline et al. found no correlation between ALE and initial SER among 37 children wearing Ortho-K [28]. Our study identified a positive correlation between these two factors, which aligns with the results of Jacinto and Wang [9, 29]. Some researchers suggested that creating myopic defocus on the peripheral retina of myopic eyes may slow down the progression of central myopia [10, 30]. This could explain why children with more negative SER tend to exhibit better myopia control when wearing Ortho-K, as the lenses may induce greater peripheral myopic defocus. It is possible that children with more myopia may inherently possess a greater degree of myopic defocus in the periphery due to the design of the Ortho-K, which could benefit myopia management. However, more research is necessary to clarify the exact mechanisms and interactions between SER and AL in the context of myopia control strategies, including the potential biological and optical influences affecting axial elongation.
A study analyzing the myopia prevalence among 1,437 children in Germany found that daily exposure to sunlight and reducing prolonged near work activity could reduce the progression of pathological myopia [25]. Some studies established a negative correlation between outdoor activity and the incidence of myopia, with similar effects observed across different ethnic groups [13, 26]. Surprisingly, outdoor activity was not included in the model. For behavioral factors such as outdoor activity, it depended on the self-report of the subjects, and there was a memory bias. Children’s outdoor activities were mostly concentrated in the evening or on weekends, with less outdoor activity on weekdays. The research subjects may overestimate their outdoor activity time and ignore the intensity of light. Lan et al. investigated the inhibitory effects of bright light on myopia development using animal models [31], and found that intermittent bright light was more effective in suppressing myopia in chickens than near exposure. Prolonged exposure to bright light did not achieve better results. These findings suggest that both the duration and frequency of outdoor activity may need further study.
Compared with the main predictive factors, the impact of outdoor activities may be relatively small. Lu et al. failed to find the relationship of outdoor activity and near activity in a rural Chinese population with a high prevalence of myopia [32]. The selected population may have high genetic susceptibility or have obvious myopia basis, which leads to the role of environmental factors being concealed by genetic factors. Some studies have found that outdoor activities mainly protect children who were not myopic, but have no significant effect on the average myopia progress of children who were already nearsighted, and have not enhanced the effect of atropine on delaying myopia progress [33]. Similar results may exist in the children who wears orthokeratology to control myopia. Moreover, The AIC rule used in model screening will comprehensively consider the goodness of fit and complexity of the model when selecting variables. Although the short reading distance was related to ALE in univariate analysis, adding multivariate model may make the model too complicated and not significantly improve the fitting effect of the model. The AIC rule tends to choose a relatively simple model that can fit the data well.
The roles of gender and pupil size in myopia progression remain controversial [14, 27, 29, 34]. And our study did not find significant correlations between these factors, similar to the findings of Saw et al. [34]. Li et al.. suggested that the consumption of sweet foods could impact myopia development [35]. However, our study did not find similar results. Regular follow-ups could reduce axial elongation in myopia progression, indicating that consistent monitoring may be beneficial in managing myopia. Research has shown that the correct answer rate for relevant medical knowledge among people who receive regular follow-up is greater than 80% [36]. People who cannot follow up on time do not recognize that axial length is an indicator for monitoring myopia progression and that Ortho-K requires at least 6 h of sleep to achieve normal daylight vision. Apart from cognitive aspects, patients who receive regular follow-up have less myopia, and the proportion of low myopia is 2.58 times higher than their peers who receive irregular follow-up. So regular follow-up is one of the indicators to control the rapid development of myopia.
The TZ of Ortho-K is designed as a relatively flat circular area that corrects myopia by flattening the cornea. However, decentration may occur due to corneal asymmetry and eyelid tension [37]. Historically, TZ decentration was often viewed as indicative of improper fitting parameters, but recent studies have suggested that TZ decentration can actually reduce ALE [38–40]. Our research found that decentration distance can affect the progression of myopia, but we did not find a relationship between decentration direction and myopia. Most patients showed temporal decentration, consistent with previous studies, which may be due to the steeper temporal side of the cornea, eye movement and eyelid force [41]. The treatment zone of Ortho-K lenses was usually circularly symmetrical, and different decentration directions will not change the amount of the peripheral retinal defocus [39, 42]. Decentration distance can control myopia progression and reduce retinal deformations [43]. Specifically, lens decentration towards the temporal side may suppress excessive stretching of the temporal retina, creating an asymmetric peripheral retinal defocus. Numerous studies have reported increases in spherical aberration, horizontal and vertical coma, and higher-order aberrations in the peripheral zones after wearing Ortho-K [44, 45]. The reason why Ortho-K deviation slows down the development of myopia may be the change of peripheral defocus and aberration. It may be that the magnitude of the decentration distance influences the effectiveness of myopia control. Wang et al. suggested that Ortho-K with eccentric distance less than 1.5 mm could effectively delay the development of myopia, and the glare and ghost problems were acceptable, which can be considered as an indicator to evaluate the effectiveness of orthokeratology [46].
The advantage of the study is that it incorporates as many influencing factors as possible in relative large-scale cases, including baseline ocular parameters, genetic factors, and lifestyle habits, affirming the role of regular follow-ups and treatment zone eccentricity in myopia control. It can be considered to further strengthen relevant intervention measures in behavior and encourage patients and parents to follow up regularly. The limitations of our study included its retrospective design, and some parents’ answers to questions such as lifestyle habits over the past year were uncertain. Patients may be influenced by memory bias, which leads to poor accuracy in answering some questions. The etiology of myopia was complex and easily influenced by environmental factors, and there were still many possible influencing factors. During the study, 10.12% of the cases were excluded due to lack of data or poor quality of the questionnaire. Patients with poor compliance or special family conditions were more likely to lose follow-ups, and these people often had poor myopia control effect and might introduce selection bias. Consider further prospective research, incorporate more potential influencing factors, fill out the questionnaire multiple times to enhance credibility.
Conclusions
Factors correlated with poor axial control include a younger baseline age, less myopia, a smaller decentration distance, irregular follow-up examinations and high myopia in both parents. This helped to evaluate and predict the effectiveness of myopia control based on patients baseline eye parameters and lifestyle habits, timely change control strategies, and reduce trial and error time. On the other hand, we encouraged parents to pay more attention to their children’s lifestyle habits. By providing more accurate information during medical visits, they could facilitate the selection of more effective myopia control methods in clinical practice, enabling timely interventions for incorrect behaviors and addressing axial length elongation.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- Ortho-K
Orthokeratology
- SER
Spherical equivalent refraction
- ALE
Axial length elongation
- CCT
Central corneal thickness
- E-value
Corneal eccentricity
- HVID
Horizontal visible iris diameter
- ACD
Anterior chamber depth
- PD
Pupil diameter
- TZ
Treatment zone
- TZA
Treatment zone area
Authors’ contributions
Y. Deng participated in conception and design of this work, data acquisition and analysis, and in literature search and manuscript writing. X. Li contributed to data collection, data analysis and revision of the manuscript for this study. Y. Li and M. Zhao contributed to the interpretation of data, and revision of the manuscript for this study. K. Wang contributed to design of the work, interpretation of data, and revision of the manuscript for this study. All authors read and approved the final version of the manuscript.
Funding
This work was supported by National Natural Science Foundation of China (Grant No. 82171092, 82371087), Capital’s Funds for Health Improvement and Research (No. 2022-1G-4083).
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study design adhered to the principles of the Helsinki Declaration and was approved by the Ethics Committee of Peking University People’s Hospital. Study approval number is 2022PHB119-001. The purpose and details of the study were explained to all the subjects and their parents, and they all signed the informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shah R, Vlasak N, Evans BJW. High myopia: reviews of myopia control strategies and myopia complications. Ophthalmic Physiol Opt. 2024;44(6):1248–60. PubMed PMID: 39082137. Epub 20240731. eng. [DOI] [PubMed] [Google Scholar]
- 2.Du R, Xie S, Igarashi-Yokoi T, Watanabe T, Uramoto K, Takahashi H, et al. Continued increase of axial length and its risk factors in adults with high myopia. JAMA Ophthalmol. 2021;139(10):1096–103. PubMed PMID: 34436537. PMCID: PMC8391777. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee JTL, Guo X, Li Z, Jong M, Sankaridurg P, He M. Progression and longitudinal biometric changes in highly myopic eyes. Invest Ophthalmol Vis Sci. 2020;61(4):34. PubMed PMID: 32334434. PMCID: PMC7401968. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bullimore MA, Lee SS, Schmid KL, Rozema JJ, Leveziel N, Mallen EAH, et al. IMI-Onset and progression of myopia in young adults. Invest Ophthalmol Vis Sci. 2023;64(6):2. PubMed PMID: 37126362. PMCID: PMC10153577. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and Temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–42. PubMed PMID: 26875007. Epub 20160211. eng. [DOI] [PubMed] [Google Scholar]
- 6.Jonas JB, Ang M, Cho P, Guggenheim JA, He MG, Jong M, et al. IMI prevention of myopia and its progression. Invest Ophthalmol Vis Sci. 2021;62(5):6. PubMed PMID: 33909032. PMCID: PMC8083117. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang J, Wen D, Wang Q, McAlinden C, Flitcroft I, Chen H, et al. Efficacy comparison of 16 interventions for myopia control in children: A network Meta-analysis. Ophthalmology. 2016;123(4):697–708. PubMed PMID: 26826749. Epub 20160127. eng. [DOI] [PubMed] [Google Scholar]
- 8.Xu S, Li Z, Zhao W, Zheng B, Jiang J, Ye G, et al. Effect of atropine, orthokeratology and combined treatments for myopia control: a 2-year stratified randomised clinical trial. Br J Ophthalmol. 2023;107(12):1812–7. PubMed PMID: 36229177. Epub 20231122. eng. [DOI] [PubMed] [Google Scholar]
- 9.Wang B, Naidu RK, Qu X. Factors related to axial length elongation and myopia progression in orthokeratology practice. PLoS ONE. 2017;12(4):e0175913. PubMed PMID: 28419129. PMCID: PMC5395222. Epub 20170418. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fu AC, Chen XL, Lv Y, Wang SL, Shang LN, Li XH, et al. Higher spherical equivalent refractive errors is associated with slower axial elongation wearing orthokeratology. Cont Lens Anterior Eye. 2016;39(1):62–6. PubMed PMID: 26254302. Epub 20150804. eng. [DOI] [PubMed] [Google Scholar]
- 11.Liang CL, Yen E, Su JY, Liu C, Chang TY, Park N, et al. Impact of family history of high myopia on level and onset of myopia. Invest Ophthalmol Vis Sci. 2004;45(10):3446–52. PubMed PMID: 15452048. eng. [DOI] [PubMed] [Google Scholar]
- 12.Scheiman M, Zhang Q, Gwiazda J, Hyman L, Harb E, Weissberg E, et al. Visual activity and its association with myopia stabilisation. Ophthalmic Physiol Opt. 2014;34(3):353–61. PubMed PMID: 24345071. PMCID: PMC3999267. Epub 20131218. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Enthoven CA, Tideman JWL, Polling JR, Yang-Huang J, Raat H, Klaver CCW. The impact of computer use on myopia development in childhood: the generation R study. Prev Med. 2020;132:105988. PubMed PMID: 31954142. Epub 20200115. eng. [DOI] [PubMed] [Google Scholar]
- 14.Chen Z, Niu L, Xue F, Qu X, Zhou Z, Zhou X, et al. Impact of pupil diameter on axial growth in orthokeratology. Optom Vis Sci. 2012;89(11):1636–40. PubMed PMID: 23026791. eng. [DOI] [PubMed] [Google Scholar]
- 15.He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in china: A randomized clinical trial. JAMA. 2015;314(11):1142–8. PubMed PMID: 26372583. eng. [DOI] [PubMed] [Google Scholar]
- 16.Jin JX, Hua WJ, Jiang X, Wu XY, Yang JW, Gao GP, et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: the Sujiatun Eye Care Study. BMC Ophthalmol. 2015;15:73 PubMed PMID: 26152123. PMCID: PMC4495846. Epub 20150709. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guggenheim JA, Northstone K, McMahon G, Ness AR, Deere K, Mattocks C, et al. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest Ophthalmol Vis Sci. 2012;53(6):2856–65. PubMed PMID: 22491403. PMCID: PMC3367471. Epub 20120514. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiong S, Sankaridurg P, Naduvilath T, Zang J, Zou H, Zhu J, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95(6):551–66. PubMed PMID: 28251836. PMCID: PMC5599950. Epub 20170302. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fan Y, Li Y, Wang K, Qu J, Zhao M. Weighted Zernike defocus coefficient of treatment zone is a meaningful indicator for myopia control efficacy of Ortho-K lenses. Eye Vis (Lond). 2022;9(1):24. PubMed PMID: 35773712. PMCID: PMC9248179. Epub 20220701. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li X, Zuo L, Zhao H, Hu J, Tang T, Wang K, et al. Efficacy of small back optic zone design on myopia control for corneal refractive therapy (CRT): a one-year prospective cohort study. Eye Vis (Lond). 2023;10(1):47. PubMed PMID: 37986014. PMCID: PMC10658859. Epub 20231120. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang T, Li X, Chen S, Xu Q, Zhao H, Wang K, et al. Long-term follow-up of changes in ocular biometric parameters in orthokeratology lens wearers with relatively large-scale axial length reduction. Eye Vis (Lond). 2023;10(1):6. PubMed PMID: 36726171. PMCID: PMC9893609. Epub 20230202. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115(8):1279–85. PubMed PMID: 18294691. Epub 20080221. eng. [DOI] [PubMed] [Google Scholar]
- 23.Lyu Y, Zhang H, Gong Y, Wang D, Chen T, Guo X, et al. Prevalence of and factors associated with myopia in primary school students in the Chaoyang district of beijing, China. Jpn J Ophthalmol. 2015;59(6):421–9. PubMed PMID: 26329826. Epub 20150902. eng. [DOI] [PubMed] [Google Scholar]
- 24.Armstrong RA. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol Opt. 2013;33(1):7–14. PubMed PMID: 23252852. eng. [DOI] [PubMed] [Google Scholar]
- 25.Philipp D, Vogel M, Brandt M, Rauscher FG, Hiemisch A, Wahl S, et al. The relationship between myopia and near work, time outdoors and socioeconomic status in children and adolescents. BMC Public Health. 2022;22(1):2058. PubMed PMID: 36357862. PMCID: PMC9650855. Epub 20221110. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2013;120(2):277–83. PubMed PMID: 23098368. Epub 20121023. eng. [DOI] [PubMed] [Google Scholar]
- 27.Hyman L, Gwiazda J, Hussein M, Norton TT, Wang Y, Marsh-Tootle W, et al. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. 2005;123(7):977–87. PubMed PMID: 16009841. eng. [DOI] [PubMed] [Google Scholar]
- 28.Cho P, Cheung SW. Retardation of myopia in orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53(11):7077–85. PubMed PMID: 22969068. Epub 20121011. eng. [DOI] [PubMed] [Google Scholar]
- 29.Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Factors preventing myopia progression with orthokeratology correction. Optom Vis Sci. 2013;90(11):1225–36. PubMed PMID: 24037063. eng. [DOI] [PubMed] [Google Scholar]
- 30.Charman WN, Radhakrishnan H. Peripheral refraction and the development of refractive error: a review. Ophthalmic Physiol Opt. 2010;30(4):321–38. PubMed PMID: 20629956. eng. [DOI] [PubMed] [Google Scholar]
- 31.Lan W, Feldkaemper M, Schaeffel F. Intermittent episodes of bright light suppress myopia in the chicken more than continuous bright light. PLoS ONE. 2014;9(10):e110906. PubMed PMID: 25360635. PMCID: PMC4216005. Epub 20141031. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu B, Congdon N, Liu X, Choi K, Lam DS, Zhang M, et al. Associations between near work, outdoor activity, and myopia among adolescent students in rural china: the Xichang pediatric refractive error study report 2. Arch Ophthalmol. 2009;127(6):769–75. PubMed PMID: 19506196. eng. [DOI] [PubMed] [Google Scholar]
- 33.Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120(5):1080–5. PubMed PMID: 23462271. Epub 20130222. eng. [DOI] [PubMed] [Google Scholar]
- 34.Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci. 2000;77(10):549–54. PubMed PMID: 11100893. eng. [DOI] [PubMed] [Google Scholar]
- 35.Li W, Tu Y, Zhou L, Ma R, Li Y, Hu D, et al. Study of myopia progression and risk factors in Hubei children aged 7–10 years using machine learning: a longitudinal cohort. BMC Ophthalmol. 2024;24(1):93. PubMed PMID: 38429630. PMCID: PMC10905806. Epub 20240301. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hung LL, Liao LL, Chen HJ, Lin HL, Chang LC. Factors associated with Follow-Up visits in parents with myopic children wearing orthokeratology Lens. J Nurs Res. 2022;30(6):e244. PubMed PMID: 36066497. Epub 20221201. eng. [DOI] [PubMed] [Google Scholar]
- 37.Sun L, Li ZX, Chen Y, He ZQ, Song HX. The effect of orthokeratology treatment zone decentration on myopia progression. BMC Ophthalmol. 2022;22(1):76. PubMed PMID: 35164702. PMCID: PMC8845411. Epub 20220215. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen R, Chen Y, Lipson M, Kang P, Lian H, Zhao Y, et al. The effect of treatment zone decentration on myopic progression during Or-thokeratology. Curr Eye Res. 2020;45(5):645–51. PubMed PMID: 31560222. Epub 20200211. eng. [DOI] [PubMed] [Google Scholar]
- 39.Zhang S, Zhang H, Li L, Yang X, Li S, Li X. Effect of treatment zone decentration on axial length growth after orthokeratology. Front Neurosci. 2022;16:986364. PubMed PMID: 36340764. PMCID: PMC9630831. Epub 20221020. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xiao K, Lu W, Zhang X, Lin S, Wei J, Lin X, et al. An integrative predictive model for orthokeratology lens decentration based on diverse metrics. Front Med (Lausanne). 2024;11:1490525. PubMed PMID: 39464268. PMCID: PMC11502374. Epub 20241011. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gu T, Gong B, Lu D, Lin W, Li N, He Q, et al. Influence of corneal topographic parameters in the decentration of orthokeratology. Eye Contact Lens. 2019;45(6):372–6. PubMed PMID: 31453820. eng. [DOI] [PubMed] [Google Scholar]
- 42.Lin W, Gu T, Bi H, Du B, Zhang B, Wei R. The treatment zone decentration and corneal refractive profile changes in children undergoing orthokeratology treatment. BMC Ophthalmol. 2022;22(1):177. PubMed PMID: 35436922. PMCID: PMC9016930. Epub 20220418. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li X, Huang Y, Zhang J, Ding C, Chen Y, Chen H, et al. Treatment zone decentration promotes retinal reshaping in Chinese myopic children wearing orthokeratology lenses. Ophthalmic Physiol Opt. 2022;42(5):1124–32. PubMed PMID: 35598145. PMCID: PMC9544447. Epub 20220522. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hiraoka T, Kakita T, Okamoto F, Oshika T. Influence of ocular wavefront aberrations on axial length elongation in myopic children treated with overnight orthokeratology. Ophthalmology. 2015;122(1):93–100. PubMed PMID: 25234013. Epub 20140916. eng. [DOI] [PubMed] [Google Scholar]
- 45.Xue M, Lin Z, Wu H, Xu Q, Wen L, Luo Z, et al. Two-Dimensional peripheral refraction and Higher-Order wavefront aberrations induced by orthokeratology lenses decentration. Transl Vis Sci Technol. 2023;12(10):8. PubMed PMID: 37824110. PMCID: PMC10587852. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang A, Yang C. Influence of Overnight Orthokeratology Lens Treatment Zone Decentration on Myopia Progression. J Ophthalmol. 2019;2019:2596953 PubMed PMID: 31827908. PMCID: PMC6881772. Epub 20191115. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.