Abstract
Various in vitro effects of staphylococcal enterotoxin B (SEB) on human peripheral blood mononuclear cells were mitigated by Bacillus anthracis edema toxin. In particular, levels of some SEB-induced cytokines (tumor necrosis factor alpha, gamma interferon) and chemokines (monocyte chemoattractant protein 1, macrophage inflammatory protein 1 alpha [MIP-1α], MIP-1β) were significantly diminished or even nonexistent, depending upon the timing of edema toxin administration. Overall, these results suggest a novel use of B. anthracis edema toxin against a bacterial superantigen.
Bacillus anthracis and Staphylococcus aureus are gram-positive pathogens involved in numerous human/animal diseases that include skin-linked maladies such as cutaneous anthrax, carbuncles, impetigo, and scalded-skin syndrome (16, 35). The various protein toxins produced by these bacteria (i.e., B. anthracis lethal toxin or S. aureus enterotoxins/toxic shock syndrome toxin 1) can profoundly affect a host in multiple ways, which may result in morbidity, shock, and even death. Furthermore, B. anthracis and staphylococcal enterotoxin B (SEB) are considered by the Centers for Disease Control and Prevention to be select agents that warrant monitoring by the federal government. Therefore, a renewed interest in B. anthracis and SEB as bioterror threats has caused some academic, government, and industrial institutions to further investigate (or in some cases, stop investigating) the respective “biology” of this microorganism and toxin, with an immediate focus upon generating vaccines and therapeutics. Additionally, the continuing rise in antibiotic resistance among diverse clinical isolates throughout the world (e.g., vancomycin-resistant S. aureus) demands further attention now by researchers and clinicians, ultimately necessitating “novel” means of controlling bacterial pathogens and their toxins (22).
SEB and other related toxins produced by S. aureus and Streptococcus pyogenes (i.e., toxic shock syndrome toxin 1 [TSST-1] plus the pyrogenic exotoxins) possess superantigenic properties that entail a marked activation of T lymphocytes with subsequent release of proinflammatory cytokines and chemokines (12-16). In large quantities, these molecules can play an important role in ill effects experienced by the host following exposure to SEB or other related protein superantigens. In vitro and in vivo studies by various groups have also shown that the adverse effects of the SEs and TSST-1 are naturally potentiated by a ubiquitous component of all gram-negative bacteria, namely, lipopolysaccharide (LPS) (4, 6, 30-32). It is this fact that suggests that an agent which blocks LPS effects might also abrogate SEB activity, as both commonly evoke elevated levels of proinflammatory cytokines and chemokines (8, 14-16).
A previous study by Hoover et al. (9) reveals that B. anthracis edema factor (EF), a calcium/calmodulin-dependent adenylate cyclase that enters various eucaryotic cells via B. anthracis protective antigen (PA) (17-19), substantially decreases the production of LPS-induced tumor necrosis factor alpha (TNF-α) from human monocytes even when given 2 to 4 h after LPS. A combination of EF and PA produces the edema toxin, which shares many attributes with other related bacillus and clostridial binary toxins (3, 5). Inherent characteristics of edema toxin and other procaryotic adenylate cyclases from Bordetella pertussis, Pseudomonas aeruginosa, and Yersinia pestis include transient effects upon cells of the immune system, thus decreasing the host's immunological response and enabling a pathogen to establish, and subsequently sustain, an infection (1, 19). Recent results from Tournier et al. (34) with murine dendritic cells and B. anthracis mutants further underscore this phenomenon, which includes suppression of cytokine production, dendritic cell function, and innate immunity by edema toxin.
An intracellular increase in cyclic AMP (cAMP) levels leading to diminished TNF-α release from mononuclear cells has been reported previously by various groups (11, 28), and this effect is linked to gene transcription (9). As evidenced with other cell types (18), the cAMP levels in human lymphocytes dramatically increase after dose-dependent exposure to edema toxin (17). In addition to results seen with TNF-α, a recent study by Paccani et al. (26) shows that anti-CD3 induced proliferation of human lymphocytes and production of gamma interferon (IFN-γ), and interleukin 2 (IL-2) and IL-5 are diminished substantially by edema toxin via inactivation of the transcription factors NFAT as well as AP-1. Such events elicited by B. anthracis edema toxin are transient (half-life of EF is ∼2 h in cytosol), generally considered nonlethal, and prevent anti-CD3-induced proliferation of T lymphocytes in vitro (17-19, 26, 29). In contrast to Vibrio cholerae cholera toxin, which activates host adenylate cyclase, intracellular amounts of cAMP elicited by B. anthracis edema toxin rise more rapidly to even higher levels with a minimal lag period (17, 18). Finally, in contrast to edema toxin, T-lymphocyte proliferation with subsequently elevated levels of proinflammatory cytokines/chemokines represents a classic effect caused by superantigen stimulation of the immune system (12-16). The results from the present study reveal a novel means of inhibiting SEB activity in vitro by using B. anthracis edema toxin.
Purified SEB was obtained from Toxin Technology (Sarasota, Fla.) with an endotoxin content of <1 ng/mg of protein, as determined by the Limulus amebocyte lysate assay (BioWhittaker, Walkersville, Md.). All cytokines and chemokines used as calibration standards in enzyme-linked immunosorbent assays (ELISA) were purified human recombinant proteins recognized by specific antibodies. IL-2, TNF-α, antibodies against TNF-α, and peroxidase-conjugates of anti-rabbit/anti-goat IgG were obtained from Boehringer-Mannheim (Indianapolis, Ind.). Monocyte chemoattractant protein 1 (MCP-1), macrophage inflammatory protein 1 alpha (MIP-1α), MIP-1β, and antibodies against IL-1β, IL-6, MIP-1α, and MIP-1β were purchased from R&D Systems (Minneapolis, Minn.). IL-1β was kindly provided by the National Cancer Institute (Frederick, Md.), while IFN-γ and IL-6 were purchased from Collaborative Research (Boston, Mass.). Antibodies against IFN-γ, IL-2, and MCP-1 were obtained from BD Pharmingen (San Diego, Calif.). All other reagents were from Sigma (St. Louis, Mo.).
Cytokines and chemokines were measured by ELISA with specific antibodies according to the manufacturer's instructions (12, 13). Human recombinant cytokines and chemokines (20 to 1,000 pg/ml) were used as calibration standards on each plate. The detection limit of each assay was ∼20 pg/ml, and all data were expressed as the means ± standard deviations (SD) of duplicate samples or means ± standard errors of the means (SEM) from multiple samples. Data were statistically analyzed by Student's t test with Stata software (Stata Corp., College Station, Tex.), and differences between edema toxin-treated and untreated groups were considered significant at a P value of <0.05.
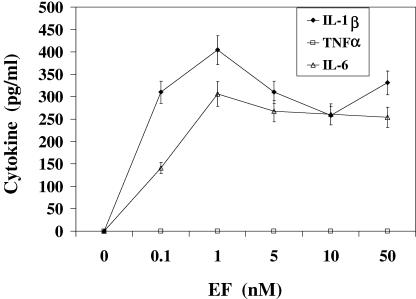
Initial work was done to investigate cytokine production elicited by purified edema toxin (EF + PA; List Biological Laboratories, Campbell, Calif.) in human peripheral blood mononuclear cells (PBMC). The PBMC were isolated by density gradient centrifugation (Ficoll-Hypaque) of heparinized blood from randomly selected, healthy donors. PBMC (106 cells/ml) were cultured at 37°C in 24-well plates containing RPMI 1640 medium and 10% heat-inactivated fetal bovine serum. Cells were incubated with various concentrations of EF + PA (edema toxin) for 16 h, and the harvested supernatants were subsequently analyzed for IL-1β, IL-2, IL-6, IFN-γ, TNF-α, MCP-1, MIP-1α, and MIP-1β. Background levels of cytokines/chemokines for nonstimulated PBMC were between 0 and 100 pg/ml. A range of EF concentrations (0.1 to 50 nM) was used with PA concentrations 2.5-fold higher than that of EF (Fig. 1). Maximal levels of IL-1β and IL-6 were evident in the medium with 1 to 50 nM EF, thus suggesting that our PBMC cultures were responding to edema toxin. All subsequent experiments were then done with EF and PA at 5 and 12.5 nM concentrations, respectively. Other EF:PA mole ratios were explored in preliminary experiments, but results were still the same even with PA concentrations 10-fold higher than those of EF (data not shown). This was not surprising, as the mole ratio of EF:PA in an edema toxin complex is optimal at 1:2.5 (24). Additionally, there was no PBMC cytotoxicity at any tested concentration of edema toxin, as evidenced by trypan blue exclusion (data not shown). For all of these experiments, and as reported before by Hoover et al. (9) for human monocytes, it was quite evident that edema toxin did not increase TNF-α levels from PBMC. Such results are also similar to those previously reported for mouse macrophages with elevated cAMP due to cholera toxin or prostaglandin E2 stimulation (11). Additionally, other cytokines (IFN-γ, IL-2) and chemokines (MCP-1, MIP-1α, MIP-1β) were not induced by edema toxin during our studies (data not shown). In contrast, various laboratories have shown that TNF, IFN-γ, and other proinflammatory cytokines, as well as chemokines, are readily produced by SEB-stimulated PBMC in vitro (12-14, 16), and such immune modulators are important for the biological effects of bacterial superantigens (10, 12, 23, 30, 31).
FIG. 1.
Production of IL-1β, IL-6, and TNF-α by PBMC in response to EF + PA (edema toxin), where PA concentrations are 2.5-fold higher than EF. SEB was not added to these cell cultures. Values are the means ± SD from two PBMC samples and three separate experiments. Results for IL-1β and IL-6 at all concentrations of edema toxin are significantly different (P < 0.05) from the control (0 nM EF) consisting of medium without EF and PA.
Our experiments next delved into the effects of edema toxin (EF [5 nM] + PA [12.5 nM]) on cytokine production by PBMC incubated concomitantly with SEB (7 nM) for 16 h (Table 1). These results revealed a marked decrease in SEB-induced TNF-α (66%) and IFN-γ (56%) versus SEB-only controls. Both of these cytokines are important for SE-induced toxicity in vivo (23, 30, 31). However, there was no effect of edema toxin upon SEB-induced IL-2 (Table 1), and this was clearly reflected by the lack of inhibition of SEB-stimulated proliferation among PBMC (data not shown). Proliferation assays with PBMC (2 × 105 cells/well) were done by triplicate plating of cells incubated with SEB, with or without edema toxin, for 48 h at 37°C in 96-well microtiter plates. The PBMC were pulsed with 1 μCi/well of [3H]thymidine (New England Nuclear, Boston, Mass.) during the last 5 h of culture as described previously (12). Cells were then harvested onto glass fiber filters, and incorporated [3H]thymidine was measured by liquid scintillation.
TABLE 1.
Effects upon SEB-induced cytokine and chemokine levels from PBMC with simultaneous addition of edema toxin
| Cytokine or chemokine | Result fora:
|
|||
|---|---|---|---|---|
| Medium only | SEB + edema toxinb | SEB | SEB + edema toxin/SEB (mean comparison) | |
| IL-1β | 48 ± 40 | 292 ± 77 | 140 ± 44 | 2.08 |
| IL-2 | 0 | 405 ± 145 | 402 ± 131 | 1.01 |
| IL-6 | 34 ± 23 | 300 ± 25 | 139 ± 15 | 2.24 |
| IFNγ | 0 | 854 ± 224 | 1937 ± 330 | 0.44 |
| TNFα | 0 | 178 ± 63 | 526 ± 34 | 0.34 |
| MCP-1 | 94 ± 60 | 101 ± 33 | 821 ± 37 | 0.12 |
| MIP-1α | 67 ± 32 | 84 ± 24 | 1086 ± 207 | 0.08 |
| MIP-1β | 63 ± 32 | 294 ± 98 | 1289 ± 272 | 0.23 |
Detected cytokine and chemokine concentrations (pg/ml) in culture supernatants are the means ± SEM from seven PBMC donors for all assays except IL-2 (n = 5). The SEM indicates inherent differences in SEB-stimulated cytokine and chemokine levels that naturally exist between human donors.
The same SEB (7 nM) and edema toxin (5 nM EF and 12.5 nM PA) concentrations were used for these experiments.
More profound than the cytokine effects was the percent inhibition of SEB-induced chemokines MCP-1 (88%), MIP-1α (92%), and MIP-1β (77%) by edema toxin versus cells treated with SEB alone (Table 1). Chemokines are important for migration and recruitment of T lymphocytes (21) as well as superantigen stimulation (12-14). Finally, in contrast to the other cytokines/chemokines, the IL-1β and IL-6 levels from edema toxin plus SEB-treated PBMC were above those from cells incubated with SEB alone. How elevated IL-1β and IL-6 levels might adversely affect cells and ultimately, the whole animal, following SEB and edema toxin exposure is rather complex and awaits further testing. However, as indicated by trypan blue exclusion and proliferation assays in vitro, the elevated IL-1β and IL-6 levels detected in our experiments were evidently not deleterious to human PBMC. Nonetheless, these results captured the overall trend and suggest that some specific, SEB-induced proinflammatory cytokines and chemokines are markedly decreased by B. anthracis edema toxin.
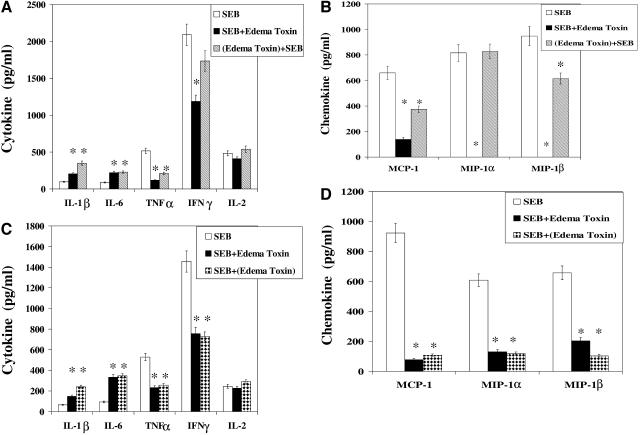
The next series of experiments investigated the effects of edema toxin preincubated for 3 h with PBMC before SEB exposure (Fig. 2a and b). Although effects upon SEB-induced TNF-α and IFN-γ levels were evident (59% and 18% decrease, respectively) (Fig. 2a) versus the SEB-only controls, they were clearly not as pronounced as those following concomitant administration of edema toxin (Table 1 and Fig. 2a). Decreased efficacy of edema toxin given before SEB might be linked to a rapid (∼2 h) half-life of EF in the cytosol (18, 19). These cytokine results were also reflected by a diminished impact of edema toxin upon SEB-induced chemokines, in which MCP-1 and MIP-1β decrements were, respectively, 43% and 35%, versus the SEB-only controls (Fig. 2b). Levels of MIP-1α were insignificantly different from the SEB-only controls.
FIG. 2.
(A) Production of IL-1β, IL-6, TNF-α, IFN-γ, and IL-2 by PBMC in response to SEB alone (SEB), SEB plus edema toxin incubated simultaneously (SEB+Edema Toxin), or pretreatment of cells with edema toxin for 3 h before SEB [(Edema Toxin)+SEB]. Values are the means ± SD for two PBMC samples and repeated experiments for each panel. (B) Production of MCP-1, MIP-1α, and MIP-1β by PBMC in response to SEB alone, SEB plus edema toxin incubated simultaneously, or pretreatment of cells with edema toxin for 3 h before SEB. (C) Production of IL-1β, IL-6, TNF-α, IFN-γ, and IL-2 by PBMC in response to SEB alone, SEB plus edema toxin incubated simultaneously, or SEB preincubated for 3 h with cells before edema toxin posttreatment [SEM+(Edema Toxin)]. (D) Production of MCP-1, MIP-1α, and MIP-1β by PBMC in response to SEB alone, SEB plus edema toxin incubated simultaneously, or SEB preincubated for 3 h before edema toxin posttreatment. The SEB, EF, and PA concentrations for all of these experiments are 7 nM, 5 nM, and 12.5 nM, respectively. *, P < 0.05 compared with cells treated with SEB alone.
The final experiments involved “therapeutic” administration of edema toxin to PBMC 3 h after SEB (Fig. 2c and 2d). SEB-induced TNF-α, IFN-γ, MCP-1, MIP-1α, and MIP-1β levels were again noticeably decreased (51%, 49%, 88%, 80%, and 84%, respectively) compared to the SEB-only controls. These results were very encouraging, as they were akin to those just described for SEB and edema toxin coadministration as well as mimic the reported therapeutic effects of edema toxin upon LPS-stimulated TNF-α from human monocytes (9). The latter effect is evident 2 to 4 h after LPS exposure, which is similar to the 3-h therapeutic window of edema toxin upon SEB-stimulated PBMC cultures and specific cytokines/chemokines.
Overall, the results gathered during this succinct study revealed that edema toxin effectively mitigated various proinflammatory cytokine and chemokine levels normally elevated after human lymphocyte exposure to SEB. Similar decreases in specific, SEB-induced cytokines/chemokines were evident if edema toxin was added to PBMC at the same time as, or even 3 h after, SEB. There were noticeably fewer effects upon SEB-induced cytokines/chemokines if edema toxin was preincubated with PBMC 3 h before SEB, which is perhaps linked to a short half-life of EF in the cytosol (18, 19). We have clearly shown that levels of important chemotactic cytokines induced by SEB were diminished by B. anthracis edema toxin. In particular, edema toxin modulated the SEB-induced effects not only by down-regulating TNF-α and IFN-γ, cytokines important for SE-induced effects in vitro and in vivo (10, 12-16, 23, 30, 31), but also by suppressing SEB-induced chemokines, such as MCP-1, MIP-1α, and MIP-1β (12-14). Chemokines play a pivotal role during an immune response by activating T lymphocytes and influencing their differentiation, recruitment, and migration to infection sites (21). Although this study focused upon SEB, it is quite likely that other bacterial superantigens would be similarly affected by B. anthracis edema toxin. Additionally, a logical extension of this in vitro data includes therapy-based studies in vivo (8, 15).
Some of our previous work on potential therapeutics has involved low-molecular-weight inhibitors of SEB and TSST-1 activity in vitro and in vivo (8, 12-15). However, as edema toxin contains an enzymatic component with transient effects upon cells, it represents a novel and potentially useful alternative to small molecule/peptide inhibitors for superantigen-induced shock (2, 8, 12-15, 18, 19, 27, 36, 38). To our knowledge, intravenous immunoglobulins have been used for humans with severe cases of superantigen-induced toxic shock (25, 33), but there are no other clinically available therapeutics against the SEs and related superantigenic toxins (16).
Finally, the use of a bacterial protein toxin to combat another represents a unique, but perhaps unappreciated, application of “tools” already assembled by Mother Nature. Chimeric forms of the anthrax toxins have already been used successfully by various groups as protein shuttles that effectively stimulate the immune system (7) and fight cancer (20). However, in contrast to results of previous in vitro studies, a recent report suggests that edema toxin can cause necrosis and cytotoxicity in a zebra fish embryo model (37). Further studies are clearly needed with edema toxin in other models for ascertaining inherent toxicity, and as with any potential therapeutic, relative amounts and route of administration critically represent the difference between therapy and toxicity. As per the encouraging results presented in this current in vitro study, future efforts will be made in vivo regarding edema toxin efficacy toward bacterial superantigens such as SEB; however, this is not trivial and will require a “proper” animal model that enables accurate interpretations of the results. Overall, our findings represent another logical extension of the constructive exploitation of a bacterial binary toxin, such as the B. anthracis edema toxin, via a “swords into plowshares” approach.
Editor: J. T. Barbieri
REFERENCES
- 1.Ahuja, N., P. Kumar, and R. Bhatnagar. 2004. The adenylate cyclase toxins. Crit. Rev. Microbiol. 30:187-196. [DOI] [PubMed] [Google Scholar]
- 2.Arad, G., R. Levy, D. Hillman, and R. Kaempfer. 2000. Superantigen antagonist protects against lethal shock and defines a new domain for T-cell activation. Nat. Med. 6:414-421. [DOI] [PubMed] [Google Scholar]
- 3.Barth, H., K. Aktories, M. R. Popoff, and B. G. Stiles. 2004. Binary bacterial toxins: biochemistry, biology, and applications of common Clostridium and Bacillus proteins. Microbiol. Mol. Biol. Rev. 68:373-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beezhold, D. H., G. K. Best, P. F. Bonventre, and M. Thompson. 1989. Endotoxin enhancement of toxic shock syndrome toxin 1-induced secretion of interleukin 1 by murine macrophages. Rev. Infect. Dis. 11:S289-S293. [DOI] [PubMed] [Google Scholar]
- 5.Collier, R. J., and J. A. Young. 2003. Anthrax toxin. Annu. Rev. Cell Dev. Biol. 19:45-70. [DOI] [PubMed] [Google Scholar]
- 6.Dalpke, A. H., and K. Heeg. 2003. Synergistic and antagonistic interactions between LPS and superantigens. J. Endotoxin Res. 9:51-54. [DOI] [PubMed] [Google Scholar]
- 7.Goletz, T. J., K. R. Klimpel, S. H. Leppla, J. M. Keith, and J. A. Berzofsky. 1997. Delivery of antigens to the MHC class I pathway using bacterial toxins. Hum. Immunol. 54:129-136. [DOI] [PubMed] [Google Scholar]
- 8.Hale, M. L., S. B. Margolin, T. Krakauer, C. J. Roy, and B. G. Stiles. 2002. Pirfenidone blocks the in vitro and in vivo effects of staphylococcal enterotoxin B. Infect. Immun. 70:2989-2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoover, D. L., A. M. Friedlander, L. C. Rogers, I.-K. Yoon, R. L. Warren, and A. S. Cross. 1994. Anthrax edema toxin differentially regulates lipopolysaccharide-induced monocyte production of tumor necrosis factor alpha and interleukin-6 by increasing intracellular cyclic AMP. Infect. Immun. 62:4432-4439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang, W., and L. D. Koller. 1998. Superantigen activation and kinetics of cytokines in the Long-Evans rat. Immunology 95:331-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Katakami, Y., Y. Nakao, T. Koizumi, N. Katakami, R. Ogawa, and T. Fujita. 1988. Regulation of tumour necrosis factor production by mouse peritoneal macrophages: the role of cellular cyclic AMP. Immunology 64:719-724. [PMC free article] [PubMed] [Google Scholar]
- 12.Krakauer, T. 1999. Induction of CC chemokines in human peripheral blood mononuclear cells by staphylococcal exotoxins and its prevention by pentoxifylline. J. Leukoc. Biol. 66:158-164. [DOI] [PubMed] [Google Scholar]
- 13.Krakauer, T. 2004. Caspase inhibitors attenuate superantigen-induced inflammatory cytokines, chemokines, and T-cell proliferation. Clin. Diagn. Lab. Immunol. 11:621-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krakauer, T., X. Chen, O. M. Howard, and H. A. Young. 2005. Triptolide attenuates endotoxin- and staphylococcal exotoxin-induced T-cell proliferation and production of cytokines and chemokines. Immunopharm. Immunotox. 27:53-66. [DOI] [PubMed] [Google Scholar]
- 15.Krakauer, T., and B. G. Stiles. 1999. Pentoxifylline inhibits superantigen-induced toxic shock and cytokine release. Clin. Diagn. Lab. Immunol. 6:594-598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krakauer, T., and B. G. Stiles. 2003. Staphylococcal enterotoxins, toxic shock syndrome toxin-1, and streptococcal pyrogenic exotoxins: some basic biology of bacterial superantigens. Recent Res. Dev. Infect. Immun. 1:1-27. [Google Scholar]
- 17.Kumar, P., N. Ahuja, and R. Bhatnagar. 2002. Anthrax edema toxin requires influx of calcium for inducing cyclic AMP toxicity in target cells. Infect. Immun. 70:4997-5007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leppla, S. H. 1982. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclic AMP concentrations in eukaryotic cells. Proc. Natl. Acad. Sci. USA 79:3162-3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leppla, S. H. 1999. The bifactorial Bacillus anthracis lethal and oedema toxins, p. 243-263. In J. E. Alouf and J. H. Freer (ed.), The comprehensive sourcebook of bacterial protein toxins. Academic Press, Inc., New York, N.Y.
- 20.Liu, S., R. L. Schubert, T. H. Bugge, and S. H. Leppla. 2003. Anthrax toxin: structures, functions and tumour targeting. Expert Opin. Biol. Ther. 3:843-853. [DOI] [PubMed] [Google Scholar]
- 21.Mackay, C. R. 2001. Chemokines: immunology's high impact factors. Nat. Immunol. 2:95-101. [DOI] [PubMed] [Google Scholar]
- 22.Menichetti, F. 2005. Current and emerging serious Gram-positive infections. Clin. Microbiol. Infect. 11(Suppl. 3):22-28. [DOI] [PubMed] [Google Scholar]
- 23.Miethke, T., C. Wahl, K. Heeg, B. Echtenacher, P. H. Krammer, and H. Wagner. 1992. T cell-mediated lethal shock triggered in mice by the superantigen staphylococcal enterotoxin B: critical role of tumor necrosis factor. J. Exp. Med. 175:91-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mogridge, J., K. Cunningham, and R. J. Collier. 2002. Stoichiometry of anthrax toxin complexes. Biochemistry 41:1079-1082. [DOI] [PubMed] [Google Scholar]
- 25.Norrby-Teglund, A., R. Kaul, D. E. Low, A. McGeer, D. W. Newton, J. Andersson, U. Andersson, and M. Kotb. 1996. Plasma from patients with severe invasive group A streptococcal infections treated with normal polyspecific IgG inhibits streptococcal superantigen-induced T cell proliferation and cytokine production. J. Immunol. 156:3057-3064. [PubMed] [Google Scholar]
- 26.Paccani, S. R., F. Tonello, R. Ghittoni, M. Natale, L. Muraro, M. M. D'Elios, W.-J. Tang, C. Montecucco, and C. T. Baldari. 2005. Anthrax toxins suppress T lymphocyte activation by disrupting antigen receptor signaling. J. Exp. Med. 201:325-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rajagopalan, G., M. M. Sen, and C. S. David. 2004. In vitro and in vivo evaluation of staphylococcal superantigen peptide antagonists. Infect. Immun. 72:6733-6737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Renz, H., J.-H. Gong, A. Schmidt, M. Nain, and D. Gemsa. 1988. Release of tumor necrosis factor-α from macrophages. Enhancement and suppression are dose-dependently regulated by prostaglandin E2 and cyclic nucleotides. J. Immunol. 141:2388-2393. [PubMed] [Google Scholar]
- 29.Skalhegg, B. S., B. F. Landmark, S. O. Koskeland, V. Hansson, T. Lea, and T. Jahnsen. 1992. Cyclic AMP-dependent protein kinase I mediates the inhibitory effects of 3′,5′ cyclic adenosine monophosphate on cell replication in human T-lymphocytes. J. Biol. Chem. 267:15707-15714. [PubMed] [Google Scholar]
- 30.Stiles, B. G., S. Bavari, T. Krakauer, and R. G. Ulrich. 1993. Toxicity of staphylococcal enterotoxins potentiated by lipopolysaccharide: major histocompatibility complex class II molecule dependency and cytokine release. Infect. Immun. 61:5333-5338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stiles, B. G., Y. G. Campbell, R. M. Castle, and S. A. Grove. 1999. Correlation of temperature and toxicity in murine studies of staphylococcal enterotoxins and toxic shock syndrome toxin 1. Infect. Immun. 67:1521-1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stone, R. L., and P. M. Schlievert. 1987. Evidence for the involvement of endotoxin in toxic shock syndrome. J. Infect. Dis. 155:682-689. [DOI] [PubMed] [Google Scholar]
- 33.Takei, S. Y. K. Arora, S. M. Walker. 1993. Intravenous immunoglobulin contains specific antibodies inhibitory to activation of T cells by staphylococcal toxin superantigens. J. Clin. Investig. 91:602-607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tournier, J.-N., A. Quesnel-Hellmann, J. Mathieu, C. Montecucco, W.-J. Tang, M. Mock, D. R. Vidal, and P. L. Goossens. 2005. Anthrax edema toxin cooperates with lethal toxin to impair cytokine secretion during infection of dendritic cells. J. Immunol. 174:4934-4941. [DOI] [PubMed] [Google Scholar]
- 35.Turnbull, P. C. 2002. Introduction: anthrax history, disease and ecology. Curr. Top. Microbiol. Immunol. 271:1-19. [DOI] [PubMed] [Google Scholar]
- 36.Visvanathan, K., A. Charles, J. Bannan, P. Pugach, K. Kashfi, and J. B. Zabriskie. 2001. Inhibition of bacterial superantigens by peptides and antibodies. Infect. Immun. 69:875-884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Voth, D. E., E. E. Hamm, L. G. Nguyen, A. E. Tucker, I. I. Salles, W. Ortiz-Leduc, and J. D. Ballard. 2005. Bacillus anthracis oedema toxin as a cause of tissue necrosis and cell type-specific cytotoxicity. Cell. Microbiol. 7:1139-1149. [DOI] [PubMed] [Google Scholar]
- 38.Won, S. J., W. T. Huang, Y. S. Lai, and M. T. Lin. 2000. Staphylococcal enterotoxin A acts through nitric oxide synthase mechanisms in human peripheral blood mononuclear cells to stimulate synthesis of pyrogenic cytokines. Infect. Immun. 68:2003-2008. [DOI] [PMC free article] [PubMed] [Google Scholar]