Abstract
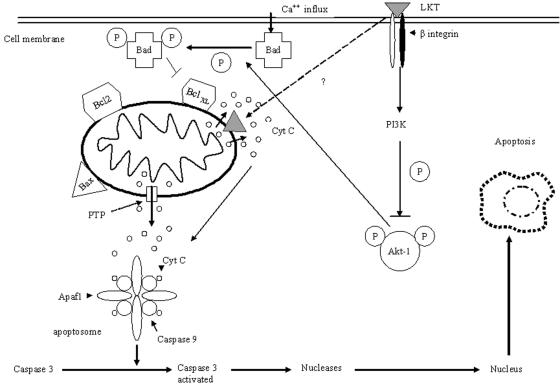
Mannheimia haemolytica is a key pathogen in the bovine respiratory disease complex. It produces a leukotoxin (LKT) that is an important virulence factor, causing cell death in bovine leukocytes. The LKT binds to the β2 integrin CD11a/CD18, which usually activates signaling pathways that facilitate cell survival. In this study, we investigated mechanisms by which LKT induces death in bovine lymphoblastoid cells (BL-3). Incubation of BL-3 cells with a low concentration of LKT results in the activation of caspase-3 and caspase-9 but not caspase-8. Similarly, the proapoptotic proteins Bax and BAD were significantly elevated, while the antiapoptotic proteins Bcl-2, BclXL and Akt-1 were downregulated. Following exposure to LKT, we also observed a reduction in mitochondrial cytochrome c and corresponding elevation of cytosolic cytochrome c, suggesting translocation from the mitochondrial compartment to the cytosol. Consistent with this observation, tetramethylrhodamine ethyl ester perchlorate staining revealed that mitochondrial membrane potential was significantly reduced. These data suggest that LKT induces apoptosis of BL-3 cells via a caspase-9-dependent mitochondrial pathway. Furthermore, scanning electron micrographs of mitochondria from LKT-treated BL-3 cells revealed lesions in the outer mitochondrial membrane, which are larger than previous reports of the permeability transition pore through which cytochrome c is usually released.
Mannheimia (Pasteurella) haemolytica is the principal bacterial pathogen of the bovine respiratory disease complex (23, 49). Among the most important virulence factors produced by this pathogen is a 104-kDa leukotoxin (LKT) that both activates and kills bovine leukocytes (2, 41). The M. haemolytica LKT is a member of the “repeats in toxin” (RTX) family of gram-negative bacterial exotoxins (34). It has been demonstrated that M. haemolytica LKT binds to the β2 integrin CD11a/CD18 (also known as leukocyte functional antigen 1 [LFA-1]) (2, 15, 21). Paradoxically, LFA-1 is usually a survival receptor whose signaling pathways protect cells against death (31, 37, 41). It is not clear how binding of LKT to LFA-1 results in apoptosis of bovine leukocytes.
The molecular mechanisms leading to apoptosis are complex. There are two major pathways that initiate apoptosis in cells (3, 7, 14). The first involves ligand binding to a death receptor (e.g., Fas or tumor necrosis factor receptor) that initiates a signaling pathway, which activates caspase-8 (5, 19). The second pathway involves mitochondrial activation of caspase-9. Both activated caspase-8 and caspase-9 can then activate the effector caspase-3 that cleaves macromolecules, leading to apoptotic cell death (35, 42). The caspase-9-dependent mitochondrial pathway is induced by cellular stress, which results in deployment of an array of proapoptotic members of the Bcl-2 family of proteins (e.g., BAD and Bax) to the outer mitochondrial membrane (OMM) (4, 52, 54). This destabilizes the membrane, resulting in pore formation and release of cytochrome c (cyt c) from the mitochondria, which in turn activates caspase-9 (11, 18, 51). During this process, the OMM also becomes permeable to other apoptogenic proteins, such as Smac/DIABLO (for second mitochondrion-derived activator of caspase/direct inhibitor of apoptosis-binding protein with low pI), apoptosis-inducing factor, and endonuclease G (1).
In this study, we attempted to identify the pathway by which M. haemolytica LKT causes apoptosis in of bovine leukocytes, using the susceptible BL-3 bovine lymphoblastoid cell line as a model system. We show that M. haemolytica LKT binding results in elevation of caspase-9 and the proapoptotic proteins Bax and BAD and a comparable decrease in the antiapoptotic proteins Bcl-2, BclXL, and Akt-1. We also used the mitochondrial redox potential sensitive agent tetramethylrhodamine ethyl ester perchlorate (TMRE) to assess mitochondrial transition pore changes in response to LKT and scanning electron microscopy (EM) to evaluate morphological changes in mitochondria from LKT-treated cells. Our findings suggest that mitochondrial dysfunction is associated with LKT-mediated apoptosis.
MATERIALS AND METHODS
LKT production and purification.
Crude LKT was prepared as described previously (29). Briefly, M. haemolytica A1 was inoculated onto blood agar (Remel, Lenexa, KS) and incubated overnight at 37°C. The bacteria were washed from the agar surface with 10 ml of brain heart infusion broth containing 0.5% yeast extract (Difco, Detroit, Mich.) and incubated at 37°C for 1 h while being rotated (8 rpm) in 15-ml polypropylene tubes. A 10-ml aliquot of this suspension was then used to inoculate 200 ml of brain heart infusion broth-0.5% yeast extract in a 500-ml flask, which was incubated for 2 h at 37°C with shaking (120 rpm). The bacteria were collected by centrifugation (1,600 × g for 15 min), resuspended in 200 ml of RPMI 1640 supplemented with l-glutamine (4.0 mM), and incubated on a shaker apparatus (at 120 rpm) for 4 h at 37°C. The bacteria were pelleted by centrifugation (1,600 × g for 20 min), and the crude LKT-containing supernatant was collected and passed through a 0.45-mm-pore-size bottletop filter (Nalgene, Rochester, N.Y.) to remove any residual bacteria. Aliquots of crude LKT were concentrated with an Amicon ultrafiltration unit equipped with a 62-mm-diameter XM-50 ultrafiltration membrane. The volume was then reduced to 10 to 20 ml over a 2- to 3-h period by application of a transmembrane pressure of 60 lb/in2 with nitrogen gas. To remove lipopolysaccharide (LPS), the partially purified LKT was treated with sodium dodecyl sulfate (SDS) (final concentration of 0.4%), and the LPS and SDS were removed by passing the LKT preparation sequentially through SDS-Out reagent and Detoxi-Gel columns (Pierce, Rockford, IL), respectively. LPS content in the LKT preparation was <0.2 endotoxin units (EU)/ml as determined by a Limulus amebocyte assay (Bio-Whittaker, Walkersville, Md.). In addition, we observed no extraneous protein bands on a silver-stained SDS-polyacrylamide gel electrophoresis (PAGE) gel.
One unit of LKT activity was defined as the LKT dilution causing 50% killing of BL-3 cells (106 cells suspended in 1 ml of RPMI 1640 medium) when incubated at 37°C for 1 h, as determined by trypan blue exclusion. LKT was stored at −70°C until used in experiments. An lktC gene mutant of M. haemolytica (SH 1562) that produces a LKT protein with no biological activity (generously provided by S. V. Highlander, Houston, TX) was prepared in a manner similar to that for wild-type M. haemolytica strain A1.
Cell line and cell culture.
BL-3 cells were used as a target for LKT-mediated killing in this study (kindly provided by Ron Schultz, Madison, WI). These nonadherent cells were grown at 37°C in 5% CO2 in RPMI medium supplemented with 10% fetal bovine serum (Gibco BRL, Burlington, VT).
Cell proliferation assays.
BL-3 cells (106 cells per ml) were washed, resuspended in antibiotic-free RPMI, and incubated at 37°C with 0.2 U of LKT for the designated time periods. Cell proliferation was quantified using the Cell Titer 96 AQueous One assay system (Promega Cooperation, Madison, WI). Optical density of the color change in the assay reagent was measured at 450 nm using an automated enzyme-linked immunosorbent assay reader (Mini plate EL 312; Bio-Tek Instruments, Inc., Winooski, VT).
Caspase-3, caspase-8, caspase-9, and LDH assays.
BL-3 cells (106 per ml) were incubated at 37°C with 0.2 U of LKT or with the inactive LKT produced by the lktC mutant for the designated time periods; caspase-3, caspase-8, and caspase-9 colorimetric assays were performed according to protocols provided by the commercial supplier (G7792, Promega Cooperation, Madison, Wis., and BF4100 and BF10100, R&D Systems, Minneapolis, MN, respectively). These colorimetric assays quantify the enzymatic activity of caspases in apoptotic cells by addition of a synthetic peptide that upon cleavage by its specific caspase undergoes a color change detected at the appropriate wavelength. In some experiments, BL-3 cells were incubated with 25 μM pan-caspase inhibitor (Z-VAD-fmk), 50 μM of caspase-8 inhibitor (Z-EITD-fmk), or caspase-9 inhibitor (Z-LEHD-fmk) before incubation with LKT. Incubation of BL-3 cells with staurosporine (0.3 μM) for 1 h at 37°C served as a positive control for apoptosis (R&D systems, Minneapolis, MN). In some experiments, lactate dehydrogenase (LDH) release was quantified on BL-3 cells incubated with 0.2 U of LKT for the designated time periods, according to the manufacturer's protocol (Promega Cooperation, Madison, WI).
Western immunoblotting.
Protein samples from LKT-treated BL-3 cells (70 μg/lane) were boiled in Laemmli loading buffer containing sodium dodecyl sulfate before being subjected to SDS-PAGE and transferred onto a polyvinylidene difluoride membrane (Millipore, Netean, Ontario, Canada). After being blocked overnight in Tris-buffered saline-Tween-5% skimmed milk, membranes were washed and incubated at room temperature for 1 h with anti-Bcl-2, anti-Bax, anti-BAD, anti-phospho-Akt-1 (Ser473), or anti-cytochrome c antibodies (Calbiochem, EMD Biosciences, Inc., La Jolla, CA). After being washed, membranes were incubated with horseradish peroxidase-conjugated secondary antibodies, and proteins were visualized by enhanced chemiluminescence (ECL, Western Chemiluminescence Reagent Plus; Pierce, Rockford, Ill.). Western blots were then stripped using Restore Western blot stripping buffer (Pierce, Rockford, Ill.), and membranes were reprobed with anti-β-actin, anti-Akt-1, or anti-porin polyclonal antibody (Santa Cruz Biotechnology, Inc., CA, and Molecular Probes, Inc., Eugene, OR). The resulting bands were quantified with a Personal Densitometer SI (Molecular Dynamics, Sunnyvale, CA).
Isolation of mitochondria.
BL-3 cells were incubated with 0.2 U of LKT for 4 h at 37°C, and their mitochondria were isolated as described previously (26). Briefly, BL-3 cells were lysed for 5 min in a buffer containing 100 mg/ml digitonin, 250 mM sucrose, 20 mM HEPES (pH 7.4), 1.5 mM MgCl2, 10 mM KCl, 1 mM EDTA, 1 mM EGTA, 1 mM dithiothreitol, 1 mM phenylmethylsulfonyl fluoride, and 10 mg/ml each of the protease inhibitors aprotinin, pepstatin, and leupeptin. Cells were centrifuged at 200 × g for 10 min at 4°C to remove cell nuclei. The supernatant was transferred to a fresh tube and centrifuged at 10,000 × g for 15 min at 4°C. The pelleted mitochondria were washed twice with the same buffer without digitonin, EGTA, and EDTA. The mitochondrial pellet was boiled in loading buffer for 2 min, loaded on a 4 to 15% SDS-PAGE gradient gel, and subjected to electrophoresis. The resulting bands were blotted onto polyvinylidene difluoride membrane and analyzed by immunoblotting for cytochrome c.
TMRE staining.
BL-3 cells were incubated with 0.2 U of LKT and then stained with TMRE as recommended by the supplier (Molecular Probes, Inc., Eugene, OR) to evaluate mitochondrial activity. Fluorescent microscopy was performed at an emission of 575 nm. Fluorescent images of mitochondrial flickers from TMRE staining were analyzed and processed using the Image J system (National Institutes of Health; http://rsb.info.nih.gov/ij).
Scanning EM.
Mitochondria isolated from LKT-treated BL-3 cells (0.2 U for 6 h) were processed for scanning EM as described previously. Briefly, samples were fixed in 2% gluteraldehyde, dehydrated through an ethanol series (30, 50, 70, 80, 90, and 95%), and washed three times in 100% ethanol. The samples were then dried at a critical point and coated with platinum using an ion beam. Samples were imaged at 5 kV with both secondary and backscattered electrons with a Hitachi S-900 field-emission scanning EM (Hitachi High Technologies, Pleasanton, CA).
Statistical analysis.
Group means were compared by analysis of variance and the Turkey-Kramer pairwise comparison test, using the Instat statistical package (GraphPad, San Diego, CA). The level of statistical significance was set at P < 0.05.
RESULTS
Cytotoxic activity of M. haemolytica LKT for BL-3 cells.
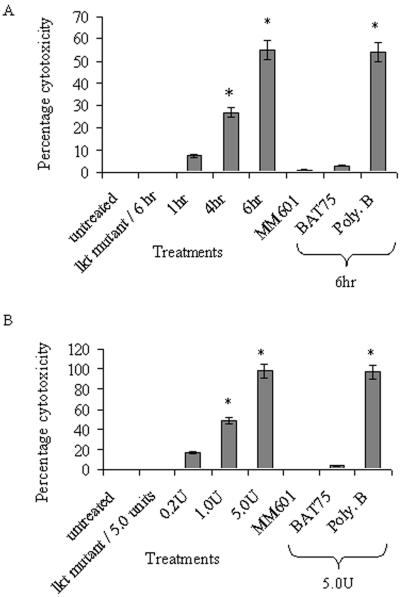
We first examined how the dose and time of exposure to LKT affected the death of BL-3 cells. Incubation of BL-3 cells with 0.2 U of LKT resulted in the death of 55% of the cells within 6 h (Fig. 1A). For several reasons, we believe that the response was not due to contaminating LPS. First, cytotoxicity was completely abolished when the LKT was preincubated with the anti-LKT monoclonal antibody (MAb) MM601 (5 μg). Similarly, blocking the LFA-1 receptor by preincubation of the cells with the BAT75 MAb (anti-CD11a/CD18) reduced LKT-mediated cytotoxicity by 96%. In addition, the SDS extraction procedure described in Materials and Methods removed 85% of the detectable LPS from the LKT preparations (data not shown). Addition of the lipid A-inactivating agent polymyxin B did not decrease the cytotoxic activity of LKT (Fig. 1A). Incubating BL-3 cells for 6 h with increasing amounts of LKT resulted in a dose-dependent increase in cytotoxic activity that was blocked by both the MM 601 and BAT75 MAbs (Fig. 1B). The inactive LKT protein produced by the lktC gene mutant did not exhibit cytotoxic activity for BL-3 cells.
FIG. 1.
Cytotoxicity of M. haemolytica LKT for BL-3 cells. In panel A, 106 BL-3 cells were incubated at 37°C with 0.2 U of M. haemolytica LKT or LKT prepared from the lktC gene mutant for the designated time periods. Cells were washed three times with RPMI, and viability was assessed as described in Materials and Methods. LKT preincubated with 5 μl of anti-LKT MAb (MM601) or preincubating BL-3 cells with 5 μl anti-CD11a/CD18 (BAT75) blocked LKT-mediated cytotoxicity. LKT pretreated with 10 μg/ml polymyxin B (Poly-B) did not diminish cytotoxicity, suggesting that LPS was not responsible for cell death. The inactive LKT produced by the lktC gene mutant did not cause any cytotoxicity when incubated with BL-3 cells for 6 h at 37°C. (B) BL-3 cells were incubated for 6 h with the indicated amounts of LKT. The figure illustrates the mean ± standard error of the mean (SEM) for five separate experiments (*, P < 0.05).
M. haemolytica LKT results in a significant increase in caspase-9 and caspase-3 activity but not caspase-8 activity and does not cause LDH release from BL-3 cells.
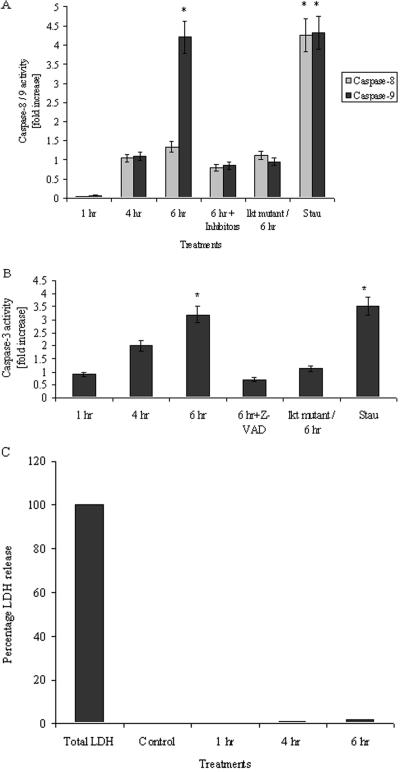
As an initial approach to distinguish between the two main pathways of apoptosis, we demonstrated that LKT-treated BL-3 cells did not exhibit a significant increase in caspase-8 activity (1.3 fold) (Fig. 2A). In contrast, a 4-fold increase in caspase-9 activity (Fig. 2A) and a 3.2-fold increase in caspase-3 activity (Fig. 2B) were seen that were maximal after 6 h incubation. Upon the addition of selective inhibitors, caspase-9 and caspase-3 activities remained at near-basal levels in LKT-treated cells (Fig. 2A). BL-3 cells incubated with the inactive LKT produced by the lktC gene mutant did not show a significant increase in caspase-8, caspase-9, or caspase-3 activities. To exclude the possibility that cell death was due to cytoplasmic membrane damage caused by LKT (0.2 U), we performed an LDH assay, which showed no significant release of LDH from LKT-treated BL-3 cells (Fig. 2C).
FIG. 2.
M. haemolytica LKT activates caspase-3 and caspase-9 but does not increase caspase-8 activity or LDH release in BL-3 cells. BL-3 (106) cells were incubated at 37°C with LKT (0.2 U) or LKT prepared from lktC gene mutant for the designated time periods. The cells were washed three times with RPMI and lysed, and caspase-8 and caspase-9 (A) and caspase-3 (B) activity assays were performed. Some cultures of BL-3 cells were preincubated with 50 μM of a caspase-8 inhibitor (Z-EITD-fmk), caspase-9 inhibitor (Z-LEHD-fmk), or a caspase-3 and caspase-7 inhibitor (Z-VAD-fmk) for 1 h at 37°C before the addition of LKT for 6 h. Incubating BL-3 cells with 0.3 μM staurosporine for 1 h at 37°C served as a positive control for apoptosis. (C) LDH release assay showed no significant release of LDH in BL-3 cells treated with 0.2 U of LKT for the designated time periods. The data illustrate the mean ± SEM for five separate experiments (*, P < 0.05).
Incubation of BL-3 cells with M. haemolytica LKT results in upregulation of proapoptotic proteins and downregulation of antiapoptotic proteins.
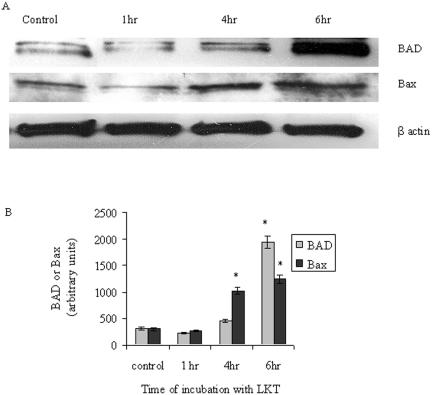
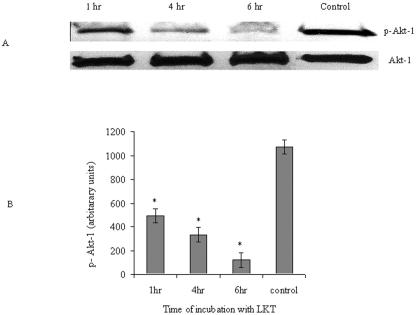
Based on the above results, we investigated the regulation of other apoptosis-related proteins in LKT-treated BL-3 cells. Western immunoblotting for the proapoptotic proteins BAD and Bax demonstrated a 6-fold and a 4.2-fold increase, respectively (Fig. 3A and B). Conversely, the antiapoptotic proteins Bcl-2 and BclXL exhibited an 89% and 71% fold decrease, respectively, following LKT exposure (Fig. 4A and B). It is known that p-Akt-1 phosphorylates BAD kinase and thus inactivates the apoptotic effect of BAD on mitochondria. Because we observed an upregulation of BAD, we investigated whether this would be reflected in a reduced level of activated Akt-1 in BL-3 cells. This proved to be the case, as we found that incubation of BL-3 cells with LKT for 6 h resulted in an 89% decrease in Akt-1 phosphorylation (Fig. 5A).
FIG. 3.
M. haemolytica LKT upregulates the proapoptotic proteins BAD and Bax. BL-3 cells (106) were incubated with LKT (0.2 U) for the designated time periods at 37°C. Cells were washed three times with RPMI and lysed with Triton-X lysis buffer at 4°C for 20 min, and Western immunoblotting was performed for BAD, Bax, and β-actin. (B) Images shown were quantified with a densitometer. The data are presented as means ± SEM of three separate experiments (*, P < 0.05).
FIG. 4.
M. haemolytica LKT downregulates the antiapoptotic proteins Bcl-2 and BclXL. BL-3 cells were incubated with LKT (0.2 U) for the designated time periods at 37°C. Cells were washed three times with RPMI, lysed with Triton-X lysis buffer at 4°C for 20 min, and Western immunoblotting was performed for Bcl-2, BclXL, and β-actin. (B) Images shown were quantified with a densitometer; the data are illustrated as means ± SEM of three separate experiments (*, P < 0.05).
FIG. 5.
M. haemolytica LKT downregulates p-Akt-1 in BL-3 cells. BL-3 cells (106) were treated with 0.2 U of LKT for the designated time periods at 37°C. Cells were washed three times with RPMI and lysed with Triton-X lysis buffer at 4°C for 20 min, and Western immunoblotting was performed for p-Akt-1. Blots were stripped and reprobed for Akt-1. (B) Images shown were quantified with a densitometer, and the data are illustrated as means ± SEM of three separate experiments (*, P < 0.05).
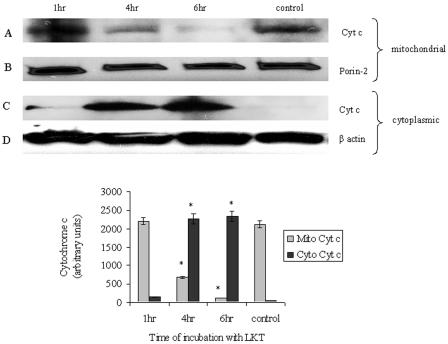
M. haemolytica LKT depletes mitochondrial cytochrome c in BL-3 cells.
Because the data in Fig. 2 and 3 point to mitochondrial involvement in the LKT-mediated apoptosis of BL-3 cells, we analyzed the mitochondrial and cytosolic fractions of cytochrome c in LKT-treated BL-3 cells. Mitochondrial cytochrome c showed a 94% decrease (Fig. 6A), while cytosolic cytochrome c showed a 40-fold increase, following LKT treatment of BL-3 cells (Fig. 6C). These data suggests that there is leakage of cytochrome c from mitochondria into the cytoplasm of BL-3 cells following LKT exposure, as would be expected for cells undergoing apoptosis via the mitochondrial pathway.
FIG. 6.
Incubation of BL-3 cells with M. haemolytica LKT results in mitochondrial release of cytochrome c. BL-3 cells (106) were incubated with of LKT (0.2 U) at 37°C for the designated time periods. Cells were washed three times with RPMI and lysed with mitochondrial lysis buffer at 4°C for 20 min, and the mitochondrial pellet and cytosolic proteins were used separately for Western immunoblotting for cytochrome c. Blots were stripped and reprobed for the mitochondrial marker protein porin and the cytosolic protein β-actin. The latter was not observed in the mitochondrial extracts (data not shown). The top two rows of blots represent mitochondrial extracts and the bottom row of blots represents cytosolic extracts from LKT-treated BL-3 cells. In the bottom panel, images shown were quantified with a densitometer, and the data are illustrated as means ± SEM of three separate experiments (*, P < 0.05).
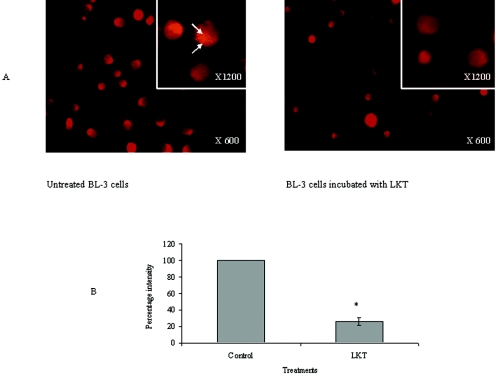
M. haemolytica LKT decreases the mitochondrial membrane potential (Δψm) in BL-3 cells.
Next, we investigated the effect of M. haemolytica LKT on mitochondrial membrane potential (Δψm), by staining BL-3 cells with the mitochondrial membrane potential sensitive fluorescent dye TMRE (Fig. 7A). We observed a 74% decrease in TMRE uptake and retention in the mitochondria of LKT-treated cells, compared to untreated control cells. These data suggest there was damage to the mitochondrial membrane as a result of LKT exposure (Fig. 7B).
FIG. 7.
M. haemolytica LKT diminishes mitochondrial membrane potential (Δψm). BL-3 cells (106) were treated with LKT (0.2 U) for 6 h at 37°C. Cells were washed with RPMI, stained with 0.5 mM TMRE for 10 min, and washed three times with PBS. (A) Fluorescent microscopy was performed at an emission wavelength of 575 nm (magnification, ×600). The insert panels show images of individual cells stained with TMRE at a magnification of ×1,200. Untreated control BL-3 cells show staining of mitochondria as orange-red specks distributed in the cytoplasm (arrows). BL-3 cells incubated with LKT show a significant reduction in staining of the mitochondrial matrices, due to the loss of mitochondrial membrane potential. Arrows indicate individual mitochondria stained with TMRE. (B) Images were quantified using the Image J system and statistically analyzed. The graph represents means ± SEM fluorescent intensities of 200 cells, randomly counted, in each of three separate experiments (*, P < 0.05).
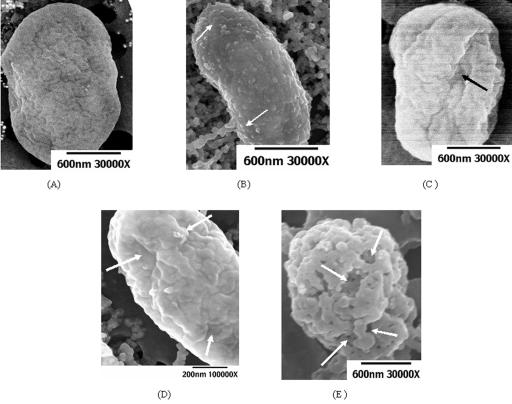
M. haemolytica LKT changes the surface morphology of mitochondria from BL-3 cells.
Because we had biochemical and physiological evidence of mitochondrial involvement in LKT-mediated apoptosis of BL-3 cells, we next performed a scanning EM analysis of mitochondria isolated from BL-3 cells after a 6-h incubation with LKT. These images revealed distortion of the mitochondrial surface (Fig. 8A) due to formation of bleb-like projections that were uniformly distributed on the mitochondrial surface (Fig. 8B). Some mitochondria were grossly distorted, with formation of depressions, ridges and furrows (Fig. 8C and 8D) that extended across the entire longitudinal length of the mitochondria, without obvious changes in the shape or size of the mitochondria. However, a few mitochondria from BL-3 cells that exhibited this mitochondrial phenotype also had punched-out lesions ranging in size from 50 to 100 nm in diameter, with an irregular edge that exposed the inner mitochondrial membrane. The average size of these mitochondria was reduced compared to mitochondria from control BL-3 cells (Fig. 8E).
FIG. 8.
Scanning electron microscopy of mitochondria isolated from BL-3 cells incubated with M. haemolytica LKT shows morphological evidence of OMM damage. Scanning electron micrographs of mitochondria isolated from control BL-3 cells (A) or BL-3 cells incubated with 0.2 U LKT for 6 h (B). (C to E) Arrows indicate blebs on the surface (C), furrows and ridges with gross deformities of the outer mitochondrial membrane (D), and large perforations and punched-out lesions (E) on mitochondria from LKT-treated BL-3 cells.
DISCUSSION
Apoptosis is a complex process of programmed cell death in multicellular organisms. Several bacteria and their products are known to activate this process by different pathways. For example, the uropathogenic Escherichia coli toxin complex is known to induce apoptosis in a caspase-independent manner, using the extracellular signal-regulated kinase pathway (10). Other examples include activation of p38 mitogen-activated protein kinases in macrophages by anthrax lethal factor and caspase activation in human fibroblast cells incubated with Shiga toxin (27, 33, 36). Our laboratory, as well as other investigators, has previously shown that incubating bovine peripheral blood leukocytes with M. haemolytica LKT causes caspase-3 activation and apoptosis in vitro (12, 29, 45-47).
In this study, we first showed that LKT-mediated cytotoxicity of BL-3 cells can be almost completely inhibited by MAbs to LKT or LFA-1. As indicated in Materials and Methods, our LKT preparation was nearly devoid of LPS (<0.2 EU/ml) as evaluated by Limulus amebocyte assay. Addition of polymyxin B had no effect on LKT-mediated cytotoxicity of BL-3 cells (Fig. 1A and B), which further indicates that the response of BL-3 cells to LKT is not dependent on contaminating LPS. In addition, we have found that a biologically inactive LKT preparation from the lktC gene mutant M. haemolytica strain SH 1562 gave results similar to untreated control cells.
BL-3 cells showed a 56% loss of viability after being incubated with 0.2 U of LKT for 6 h (Fig. 1A). At the same, LKT concentration and time of incubation, LDH release remained near basal levels, while caspase-3 activation showed a 3.2-fold increase (Fig. 2A and B). These observations suggest that loss of viability of BL-3 cells was due to caspase-3-dependent apoptotic cell death, rather than cell membrane damage typical of necrosis. Although it has been reported that higher concentrations of LKT can induce cell death by cytoplasmic membrane pore formation, the cytotoxicity that we observed at relatively low LKT concentrations (0.2 U) appears to be independent of gross cytoplasmic membrane damage (8, 32, 34).
In our experiments, we observed a significant increase in caspase-9 activity but not caspase-8 activity. The latter finding suggests that direct or indirect activation of a death domain (e.g., of Fas) by LKT is an unlikely initial event in the induction of apoptosis in BL-3 cells. These observations led us to further investigate the role of Bcl-2 protein family members in the activation of the caspase-9-dependent apoptotic pathway in LKT-treated BL-3 cells.
As anticipated, the proapoptotic, monomeric cytosolic protein Bax was significantly increased (4.2 fold) in BL-3 cells exposed to LKT for a 6-h incubation period. Once oligomerized, Bax is translocated to the outer mitochondrial membrane surface, where it forms tetrameric channels through which cyt c may escape into the cytoplasm (6, 48, 54). In our experiments, we measured total cytosolic Bax, which largely represents oligomerized Bax bound to the OMM. Binding of Bax to the OMM is triggered by both p53-dependent and p53-independent mechanisms. In the p53-dependent pathway, formation of a RAD17/9-1-1 complex results in phosphorylation of CHK2 (checkpoint kinases) which in turn activates p53. This in turn facilitates translocation of Bax while inhibiting mitochondrial binding of Bcl-2 and BclXL (39, 53). Whether a p53-dependent pathway is involved in the BL-3 response to LKT was not evaluated in the present study.
Likewise, the proapoptotic protein BAD was increased 6.0 fold during the same 6-h incubation period. Increase in total BAD is associated with apoptosis triggered by chemicals, UV radiation, and deprivation. Once BAD is inactivated by phosphorylation, it binds to 14-3-3 proteins, resulting in liberation of the antiapoptotic proteins Bcl-2 and BclXL. (13, 25, 30, 43). Thus, we observed a significant reduction in the expression of the antiapoptotic proteins Bcl-2 (9.0 fold) and BclXL (3.5 fold). These proteins also prevent oligomerization of Bax and tBid on the mitochondria and stabilize the outer mitochondrial membrane surface, thus preventing cyt c release (17). From these observations, we infer that LKT generally mobilizes proapoptotic proteins and downregulates antiapoptotic proteins that control mitochondrial damage and cyt c release.
Total BAD was upregulated following LKT exposure of BL-3 cells. We investigated the status of activated Akt-1 (phosphorylated Akt-1 [p-Akt-1]), which acts as a BAD kinase, in LKT-treated BL-3 cells. Consistent with the above observation, p-Akt-1 was downregulated (by 9.0 fold) by LKT exposure. This was somewhat of a surprising finding because stimulation of survival receptors such as β-integrins (i.e., LFA-1) normally activates phosphatidylinositol 3-kinase, which then activates the antiapoptotic Akt-1 (16, 50). p-Akt-1 in-turn acts as a BAD kinase, which inhibits the binding of BAD to the outer mitochondrial membrane (13, 24, 25). Thus, the mechanism by which LKT binding to LFA-1 leads to downregulation of p-Akt-1 is not clear.
Although it is clear that M. haemolytica LKT initially binds to LFA-1, perhaps our data reflect transient binding of LKT to LFA-1, which results in an inadequate stimulus for the activation of phosphatidylinositol 3-kinase and hence Akt-1. Alternatively, perhaps LKT binding activates a different signaling pathway that downregulates Akt-1 activity (25, 30). These observations conflict with the findings of Jeyaseelan et al., who reported phosphorylation of the cytoplasmic tail of LFA-1 following LKT exposure (22). However, it is possible that the latter response was due to inside-out rather than outside-in signaling (16, 50). Perhaps these data suggest that LFA-1 provides the initial anchor for LKT binding before it exerts its apoptotic effects via a more complicated mechanism.
Normal mitochondrial function is associated with protein complexes in the inner mitochondrial membrane that mediate electron transfer from reduced flavin adenine dinucleotide or NADH to oxygen as a final acceptor (9, 14, 48). Cytochrome c, which resides in the inner mitochondrial membrane, shuttles electrons from these proteins complexes and maintains a proton motive force and a membrane electron potential (Δψm) (28, 38). In this study, we observed a significant reduction in mitochondrial cyt c concentration and a substantial increase in cytoplasmic cyt c during the 6-h incubation period. Although we observed damage to the OMM of mitochondria isolated from LKT-treated cells by electron microscopy, it is unclear whether cyt c leakage is brought about by active opening of a permeability transition pore or by LKT-mediated damage to the OMM. Although release of mitochondrial cyt c can occur without a significant decrease in mitochondrial electric potential, we observed a significant reduction of mitochondrial membrane potential, as determined by the uptake of TMRE in LKT-treated BL-3 cells (40, 44).
The deformities we observed on the OMM may reflect the binding of proapoptotic proteins (e.g., Bax and Bak) to the OMM or perhaps are due to the intracellular transport and direct binding of LKT to the OMM. It has been shown that the diameter of a typical permeability transition pore on the OMM surfaces ranges from 3.0 to 8.2 nm and has a smooth raised edge (20). The mitochondria we isolated from LKT-treated BL-3 cells have much larger OMM lesions, which suggests direct damage to mitochondria. In support of the latter possibility, we have preliminary evidence suggesting that M. haemolytica LKT might be internalized and transported to the mitochondria (data not shown).
A limitation to our study was the unavailability of antibodies that react with bovine Bak, Bim, phosphorylated BAD and tBid proteins, or the published nucleotide sequences of their bovine homologues. Bim in particular has been designated a sensor of cytoskeleton integrity and cellular stress.
In summary, we have shown that exposure of the bovine BL-3 cell line to M. haemolytica LKT results in upregulation of caspase-9 and the proapoptotic proteins BAD and Bax and downregulation of the antiapoptotic proteins Bcl-2, BclXL, and Akt-1. The loss of mitochondrial cyt c, decreased mitochondrial membrane potential, and the lesions seen in the outer mitochondrial membrane together suggest that M. haemolytica LKT has the propensity to adversely affect mitochondria in bovine leukocytes (Fig. 9). Future efforts will assess whether this reflects the signaling cascade initiated by LKT binding or the transport of LKT to the mitochondrial membrane. We hope that identifying cellular mechanisms triggered by LKT will increase our understanding of how M. haemolytica LKT and perhaps other RTX toxins induce apoptosis in leukocytes.
FIG. 9.
Schematic representation of mechanisms by which M. haemolytica LKT may induce apoptotic cell death in BL-3 cells.
Acknowledgments
We thank S. Srikumaran of the University of Nebraska, Nebraska, for providing the MM 601 antibody; S. V. Highlander of Baylor College of Medicine, Texas, for providing the M. haemolytica lktC gene mutant; and R. Albrecht and Phil Oshel of the University of Wisconsin—Madison for providing scanning electron microscopy facilities.
This study was supported by grants from the USDA NRI (2004-01278) and The Wisconsin Agricultural Experiment Station (WIS04884).
Editor: J. T. Barbieri
REFERENCES
- 1.Adrain, C., E. M. Creagh, and S. J. Martin. 2001. Apoptosis-associated release of Smac/DIABLO from mitochondria requires active caspases and is blocked by Bcl-2. EMBO J. 20:6627-6636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ambagala, T. C., A. P. Ambagala, and S. Srikumaran. 1999. The leukotoxin of Pasteurella haemolytica binds to beta(2) integrins on bovine leukocytes. FEMS Microbiol Lett. 179:161-167. [DOI] [PubMed] [Google Scholar]
- 3.Antonsson, B. 2004. Mitochondria and the Bcl-2 family proteins in apoptosis signaling pathways. Mol. Cell. Biochem. 256-257:141-155. [DOI] [PubMed] [Google Scholar]
- 4.Araya, R., T. Uehara, and Y. Nomura. 1998. Hypoxia induces apoptosis in human neuroblastoma SK-N-MC cells by caspase activation accompanying cytochrome c release from mitochondria. FEBS Lett. 439:168-172. [DOI] [PubMed] [Google Scholar]
- 5.Aronis, A., J. A. Melendez, O. Golan, S. Shilo, N. Dicter, and O. Tirosh. 2003. Potentiation of Fas-mediated apoptosis by attenuated production of mitochondria-derived reactive oxygen species. Cell Death Differ. 10:335-344. [DOI] [PubMed] [Google Scholar]
- 6.Atlante, A., L. de Bari, A. Bobba, E. Marra, P. Calissano, and S. Passarella. 2003. Cytochrome c, released from cerebellar granule cells undergoing apoptosis or excytotoxic death, can generate protonmotive force and drive ATP synthesis in isolated mitochondria. J. Neurochem. 86:591-604. [DOI] [PubMed] [Google Scholar]
- 7.Brenner, C., and G. Kroemer. 2000. Apoptosis. Mitochondria—the death signal integrators. Science 289:1150-1151. [DOI] [PubMed] [Google Scholar]
- 8.Brown, J. F., F. Leite, and C. J. Czuprynski. 1997. Binding of Pasteurella haemolytica leukotoxin to bovine leukocytes. Infect. Immun. 65:3719-3724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cairns, C. B., J. Walther, A. H. Harken, and A. Banerjee. 1998. Mitochondrial oxidative phosphorylation thermodynamic efficiencies reflect physiological organ roles. Am. J. Physiol. 274:R1376-R1383. [DOI] [PubMed] [Google Scholar]
- 10.Chen, M., T. Jahnukainen, W. Bao, E. Dare, S. Ceccatelli, and G. Celsi. 2003. Uropathogenic Escherichia coli toxins induce caspase-independent apoptosis in renal proximal tubular cells via ERK signaling. Am. J. Nephrol. 23:140-151. [DOI] [PubMed] [Google Scholar]
- 11.Cosulich, S. C., P. J. Savory, and P. R. Clarke. 1999. Bcl-2 regulates amplification of caspase activation by cytochrome c. Curr. Biol. 9:147-150. [DOI] [PubMed] [Google Scholar]
- 12.Cudd, L. A., C. L. Ownby, C. R. Clarke, Y. Sun, and K. D. Clinkenbeard. 2001. Effects of Mannheimia haemolytica leukotoxin on apoptosis and oncosis of bovine neutrophils. Am. J. Vet Res. 62:136-141. [DOI] [PubMed] [Google Scholar]
- 13.Datta, S. R., H. Dudek, X. Tao, S. Masters, H. Fu, Y. Gotoh, and M. E. Greenberg. 1997. Akt phosphorylation of BAD couples survival signals to the cell-intrinsic death machinery. Cell 91:231-241. [DOI] [PubMed] [Google Scholar]
- 14.Desagher, S., and J. C. Martinou. 2000. Mitochondria as the central control point of apoptosis. Trends Cell Biol. 10:369-377. [DOI] [PubMed] [Google Scholar]
- 15.Deshpande, M. S., T. C. Ambagala, A. P. Ambagala, M. E. Kehrli, Jr., and S. Srikumaran. 2002. Bovine CD18 is necessary and sufficient to mediate Mannheimia (Pasteurella) haemolytica leukotoxin-induced cytolysis. Infect. Immun. 70:5058-5064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dib, K. 2000. BETA 2 integrin signaling in leukocytes. Front. Biosci. 5:D438-D451. [DOI] [PubMed] [Google Scholar]
- 17.Gajkowska, B., U. Wojewodzka, and J. Gajda. 2004. Translocation of Bax and Bid to mitochondria, endoplasmic reticulum and nuclear envelope: possible control points in apoptosis. J. Mol. Histol. 35:11-19. [DOI] [PubMed] [Google Scholar]
- 18.Garland, J. M., and C. Rudin. 1998. Cytochrome c induces caspase-dependent apoptosis in intact hematopoietic cells and overrides apoptosis suppression mediated by bcl-2, growth factor signaling, MAP-kinase-kinase, and malignant change. Blood 92:1235-1246. [PubMed] [Google Scholar]
- 19.Green, D., and G. Kroemer. 1998. The central executioners of apoptosis: caspases or mitochondria? Trends Cell Biol. 8:267-271. [DOI] [PubMed] [Google Scholar]
- 20.Guo, L., D. Pietkiewicz, E. V. Pavlov, S. M. Grigoriev, J. J. Kasianowicz, L. M. Dejean, S. J. Korsmeyer, B. Antonsson, and K. W. Kinnally. 2004. Effects of cytochrome c on the mitochondrial apoptosis-induced channel MAC. Am. J. Physiol. Cell Physiol. 286:C1109-C1117. [DOI] [PubMed] [Google Scholar]
- 21.Jeyaseelan, S., S. L. Hsuan, M. S. Kannan, B. Walcheck, J. F. Wang, M. E. Kehrli, E. T. Lally, G. C. Sieck, and S. K. Maheswaran. 2000. Lymphocyte function-associated antigen 1 is a receptor for Pasteurella haemolytica leukotoxin in bovine leukocytes. Infect. Immun. 68:72-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jeyaseelan, S., M. S. Kannan, R. E. Briggs, P. Thumbikat, and S. K. Maheswaran. 2001. Mannheimia haemolytica leukotoxin activates a nonreceptor tyrosine kinase signaling cascade in bovine leukocytes, which induces biological effects. Infect. Immun. 69:6131-6139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jeyaseelan, S., S. Sreevatsan, and S. K. Maheswaran. 2002. Role of Mannheimia haemolytica leukotoxin in the pathogenesis of bovine pneumonic pasteurellosis. Anim. Health Res. Rev. 3:69-82. [DOI] [PubMed] [Google Scholar]
- 24.Khor, T. O., Y. A. Gul, H. Ithnin, and H. F. Seow. 2004. Positive correlation between overexpression of phospho-BAD with phosphorylated Akt at serine 473 but not threonine 308 in colorectal carcinoma. Cancer Lett. 210:139-150. [DOI] [PubMed] [Google Scholar]
- 25.Khwaja, A. 1999. Akt is more than just a Bad kinase. Nature 401:33-34. [DOI] [PubMed] [Google Scholar]
- 26.Kluck, R. M., E. Bossy-Wetzel, D. R. Green, and D. D. Newmeyer. 1997. The release of cytochrome c from mitochondria: a primary site for Bcl-2 regulation of apoptosis. Science 275:1132-1136. [DOI] [PubMed] [Google Scholar]
- 27.Lazebnik, Y. 2001. Why do regulators of apoptosis look like bacterial toxins? Curr. Biol. 11:R767-768. [DOI] [PubMed] [Google Scholar]
- 28.Lecoeur, H., A. Langonne, L. Baux, D. Rebouillat, P. Rustin, M. C. Prevost, C. Brenner, L. Edelman, and E. Jacotot. 2004. Real-time flow cytometry analysis of permeability transition in isolated mitochondria. Exp. Cell Res. 294:106-117. [DOI] [PubMed] [Google Scholar]
- 29.Leite, F., S. O'Brien, M. J. Sylte, T. Page, D. Atapattu, and C. J. Czuprynski. 2002. Inflammatory cytokines enhance the interaction of Mannheimia haemolytica leukotoxin with bovine peripheral blood neutrophils in vitro. Infect. Immun. 70:4336-4343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li, Y., G. I. Tennekoon, M. Birnbaum, M. A. Marchionni, and J. L. Rutkowski. 2001. Neuregulin signaling through a PI3K/Akt/Bad pathway in Schwann cell survival. Mol. Cell. Neurosci. 17:761-767. [DOI] [PubMed] [Google Scholar]
- 31.Melero, I., M. A. Balboa, J. L. Alonso, E. Yague, J. P. Pivel, F. Sanchez-Madrid, and M. Lopez-Botet. 1993. Signaling through the LFA-1 leucocyte integrin actively regulates intercellular adhesion and tumor necrosis factor-alpha production in natural killer cells. Eur. J. Immunol. 23:1859-1865. [DOI] [PubMed] [Google Scholar]
- 32.Murphy, G. L., L. C. Whitworth, K. D. Clinkenbeard, and P. A. Clinkenbeard. 1995. Hemolytic activity of the Pasteurella haemolytica leukotoxin. Infect. Immun. 63:3209-3212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nakagawa, I., M. Nakata, S. Kawabata, and S. Hamada. 1999. Regulated expression of the Shiga toxin B gene induces apoptosis in mammalian fibroblastic cells. Mol. Microbiol. 33:1190-1199. [DOI] [PubMed] [Google Scholar]
- 34.Narayanan, S. K., T. G. Nagaraja, M. M. Chengappa, and G. C. Stewart. 2002. Leukotoxins of gram-negative bacteria. Vet. Microbiol. 84:337-356. [DOI] [PubMed] [Google Scholar]
- 35.Palmer, A. M., P. M. Greengrass, and D. Cavalla. 2000. The role of mitochondria in apoptosis. Drug News Perspect. 13:378-384. [PubMed] [Google Scholar]
- 36.Popov, S. G., R. Villasmil, J. Bernardi, E. Grene, J. Cardwell, A. Wu, D. Alibek, C. Bailey, and K. Alibek. 2002. Lethal toxin of Bacillus anthracis causes apoptosis of macrophages. Biochem. Biophys. Res. Commun. 293:349-355. [DOI] [PubMed] [Google Scholar]
- 37.Porter, J. C., M. Bracke, A. Smith, D. Davies, and N. Hogg. 2002. Signaling through integrin LFA-1 leads to filamentous actin polymerization and remodeling, resulting in enhanced T cell adhesion. J. Immunol. 168:6330-6335. [DOI] [PubMed] [Google Scholar]
- 38.Poso, A. R. 1979. Shuttles for translocation of NADH in isolated liver cells from fed rats during oxidation of xylitol. Acta Chem. Scand. B Org. Chem. Biochem. 33:93-99. [DOI] [PubMed] [Google Scholar]
- 39.Robles, A. I., and C. C. Harris. 2001. p53-mediated apoptosis and genomic instability diseases. Acta Oncol. 40:696-701. [DOI] [PubMed] [Google Scholar]
- 40.Ruitenberg, M., A. Kannt, E. Bamberg, K. Fendler, and H. Michel. 2002. Reduction of cytochrome c oxidase by a second electron leads to proton translocation. Nature 417:99-102. [DOI] [PubMed] [Google Scholar]
- 41.Sanchez-Martin, L., N. Sanchez-Sanchez, M. D. Gutierrez-Lopez, A. I. Rojo, M. Vicente-Manzanares, M. J. Perez-Alvarez, P. Sanchez-Mateos, X. R. Bustelo, A. Cuadrado, F. Sanchez-Madrid, J. L. Rodriguez-Fernandez, and C. Cabanas. 2004. Signaling through the leukocyte integrin LFA-1 in T cells induces a transient activation of Rac-1 that is regulated by Vav and PI3K/Akt-1. J. Biol. Chem. 279:16194-16205. [DOI] [PubMed] [Google Scholar]
- 42.Shi, Y. 2001. A structural view of mitochondria-mediated apoptosis. Nat. Struct. Biol. 8:394-401. [DOI] [PubMed] [Google Scholar]
- 43.Shimamura, H., Y. Terada, T. Okado, H. Tanaka, S. Inoshita, and S. Sasaki. 2003. The PI3-kinase-Akt pathway promotes mesangial cell survival and inhibits apoptosis in vitro via NF-kappa B and Bad. J. Am. Soc. Nephrol. 14:1427-1434. [DOI] [PubMed] [Google Scholar]
- 44.Shimizu, S., and Y. Tsujimoto. 2000. Proapoptotic BH3-only Bcl-2 family members induce cytochrome c release, but not mitochondrial membrane potential loss, and do not directly modulate voltage-dependent anion channel activity. Proc. Natl. Acad. Sci. USA 97:577-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stevens, P. K., and C. J. Czuprynski. 1996. Pasteurella haemolytica leukotoxin induces bovine leukocytes to undergo morphologic changes consistent with apoptosis in vitro. Infect. Immun. 64:2687-2694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sun, Y., K. D. Clinkenbeard, C. L. Ownby, L. Cudd, C. R. Clarke, and S. K. Highlander. 2000. Ultrastructural characterization of apoptosis in bovine lymphocytes exposed to Pasteurella haemolytica leukotoxin. Am. J. Vet Res. 61:51-56. [DOI] [PubMed] [Google Scholar]
- 47.Wang, J. F., I. R. Kieba, J. Korostoff, T. L. Guo, N. Yamaguchi, H. Rozmiarek, P. C. Billings, B. J. Shenker, and E. T. Lally. 1998. Molecular and biochemical mechanisms of Pasteurella haemolytica leukotoxin-induced cell death. Microb. Pathog. 25:317-331. [DOI] [PubMed] [Google Scholar]
- 48.Wang, X. 2001. The expanding role of mitochondria in apoptosis. Genes Dev. 15:2922-2933.11711427 [Google Scholar]
- 49.Whiteley, L. O., S. K. Maheswaran, D. J. Weiss, T. R. Ames, and M. S. Kannan. 1992. Pasteurella haemolytica A1 and bovine respiratory disease: pathogenesis. J. Vet Intern. Med. 6:11-22. [DOI] [PubMed] [Google Scholar]
- 50.Xia, H., R. S. Nho, J. Kahm, J. Kleidon, and C. A. Henke. 2004. Focal adhesion kinase is upstream of phosphatidylinositol 3-kinase/Akt in regulating fibroblast survival in response to contraction of type I collagen matrices via a beta 1 integrin viability signaling pathway. J. Biol. Chem. 279:33024-33034. [DOI] [PubMed] [Google Scholar]
- 51.Zhang, M., H. Q. Zhang, and S. B. Xue. 2000. Effect of Bcl-2 and caspase-3 on calcium distribution in apoptosis of HL-60 cells. Cell Res. 10:213-220. [DOI] [PubMed] [Google Scholar]
- 52.Zhao, Y., S. Li, E. E. Childs, D. K. Kuharsky, and X. M. Yin. 2001. Activation of pro-death Bcl-2 family proteins and mitochondria apoptosis pathway in tumor necrosis factor-alpha-induced liver injury. J. Biol. Chem. 276:27432-27440. [DOI] [PubMed] [Google Scholar]
- 53.Zhivotovsky, B., and G. Kroemer. 2004. Apoptosis and genomic instability. Nat. Rev. Mol. Cell Biol. 5:752-762. [DOI] [PubMed] [Google Scholar]
- 54.Zimmermann, K. C., N. J. Waterhouse, J. C. Goldstein, M. Schuler, and D. R. Green. 2000. Aspirin induces apoptosis through release of cytochrome c from mitochondria. Neoplasia 2:505-513. [DOI] [PMC free article] [PubMed] [Google Scholar]