Abstract
We have previously shown that intraperitoneal vaccination with the recombinant N terminus of Als1p (rAls1p-N) modestly improves survival during murine disseminated candidiasis. We now report marked efficacy with subcutaneous rAls1p-N vaccination. Efficacy is retained in neutropenic and corticosteroid-treated mice. The rAls1p-N vaccine is a promising candidate for the prevention of invasive candidiasis.
Candida spp. are the fourth most common nosocomial bloodstream isolates (14, 20), causing an attributable mortality of 40 to 50% during hematogenously disseminated disease (5, 10, 11, 19). The major clinical risk factors for disseminated candidiasis have been well described (17), allowing facile identification of at-risk patients. Furthermore, disseminated candidiasis typically occurs after multiple weeks of hospitalization (20), enabling the opportunity for prophylactic vaccination prior to disease onset.
We have developed a vaccine targeting Candida albicans, the most common species causing disseminated candidiasis (≈50% of cases) (1, 2, 9, 12, 13), based on the agglutination-like sequence 1 (ALS1) gene product, which is an adhesin that mediates C. albicans binding to human cells (3, 4). The recombinant N-terminal domain of Als1p (rAls1p-N) demonstrated modest efficacy as a vaccine when administered intraperitoneally to immunocompetent BALB/c mice (6). The mechanism of protection was induction of type 1 immunity, and protection correlated with induction of delayed-type hypersensitivity (DTH) to the antigen. The present studies were performed to evaluate the efficacy of the rAls1p-N vaccine when administered by a different route (subcutaneously [s.c.]) in both immunocompetent and immunocompromised mice.
Efficacy of the rAls1p-N vaccine in immunocompetent mice.
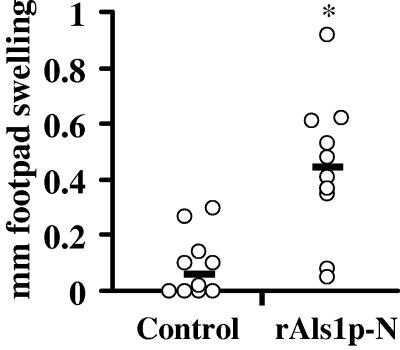
rAls1p-N, encompassing amino acids 19 to 433 of the full-length protein, was produced in Saccharomyces cerevisiae and purified as described previously (6). A control preparation was similarly purified from S. cerevisiae transformed with an empty plasmid. BALB/c retired breeder mice (25 to 30 g) were immunized by s.c. injection of rAls1p-N (20 μg) or control preparation mixed with complete Freund's adjuvant at day 0, followed by a booster dose in incomplete Freund's adjuvant at day 21. Two weeks following the boost, the immunogenicity of the vaccine was confirmed by evaluating the intensity of the footpad swelling reaction as a marker of DTH, as we have described previously (6). Vaccinated mice had marked increases in rAls1p-N-specific DTH (Fig. 1).
FIG. 1.
Subcutaneous vaccination with rAls1p-N induces an in vivo DTH response in immunocompetent mice. Footpad swelling was assessed 24 h after injection of 50 μg of rAls1p-N into the footpad in BALB/c mice (n = 10 per group). Median values are displayed as horizontal black bars. *, P = 0.002 versus control by Wilcoxon rank sum test.
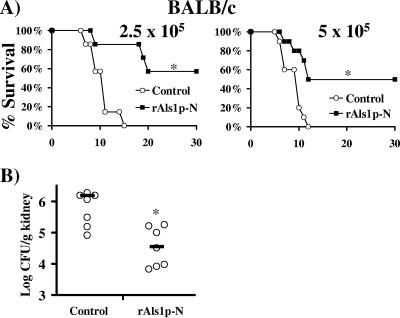
The efficacy of the rAls1p-N vaccine was evaluated by determining the impact of rAls1p-N vaccination on survival in infected BALB/c mice (Fig. 2A). Vaccinated or control mice were infected via the tail vein with rapidly lethal inocula (2.5 × 105 to 5 × 105 blastospores) of C. albicans. We have previously shown that mice infected with such inocula die of overwhelming septic shock (16). Vaccination markedly prolonged time to death (P < 0.05 for both inocula by log rank test) and improved 30-day survival (50 to 57% versus 0%, P < 0.05 for both inocula by Fisher's exact test).
FIG. 2.
The rAls1p-N vaccine improves survival of immunocompetent mice with hematogenously disseminated candidiasis and reduces tissue fungal burden. (A) Survival of vaccinated or control BALB/c mice (n = 7 or 10 per group for an inoculum of 2.5 × 105 or 5 × 105, respectively) subsequently infected via the tail vein with C. albicans. Each experiment was terminated at 30 days postinfection, with all remaining mice appearing well. *, P < 0.05 versus control by log rank test. (B) Kidney fungal burden in BALB/c mice (n = 7 per group) infected via the tail vein with 5 × 105 blastospores of C. albicans. The y axis reflects the lower limit of detection of the assay. Median values are displayed as horizontal black bars. *, P = 0.01 versus control by Wilxocon rank sum test.
The impact of vaccination on tissue fungal burden during hematogenously disseminated candidiasis was then determined. Fourteen days following the boost, vaccinated and control BALB/c mice were infected via the tail vein with 5 × 105 blastospores of C. albicans SC5314. Six days following infection, prior to onset of the first deaths in the control arm, kidneys were harvested, homogenized, and quantitatively cultured in Sabouraud dextrose agar (Difco) (18). Subcutaneous vaccination with rAls1p-N resulted in a median 1.5-log CFU/g decrease in kidney fungal burden compared to that of the control (P = 0.01 by Wilcoxon rank sum test, Fig. 2B).
Efficacy of the rAls1p-N vaccine in immunocompromised mice.
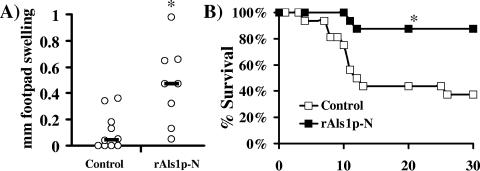
Having demonstrated efficacy in immunocompetent mice, the potential for the rAls1p-N vaccine to induce immunity in and protect neutropenic mice from disseminated candidiasis was evaluated. Vaccinated BALB/c mice were made neutropenic by administration of cyclophosphamide (200 mg/kg intraperitoneal on day −2 and 100 mg/kg intraperitoneal on day +9 relative to infection, resulting in approximately 12 days of neutropenia, as described previously [15]). The footpad swelling reaction was performed 2 days after the first dose of cyclophosphamide. Vaccinated neutropenic mice developed DTH reactions of similar magnitude to those in immunocompetent mice (Fig. 3A versus Fig. 1, experiments performed in parallel). In neutropenic mice infected via the tail vein with 2.5 × 104 blastospores of C. albicans, vaccination also resulted in significant improvements in time to death (P = 0.007 by log rank test versus control), median survival time (>21 versus 12 days, P = 0.008 by Wilcoxon rank sum test), and overall survival (88% versus 38%, P = 0.005 by Fisher's exact test) (Fig. 3B).
FIG. 3.
The rAls1p-N vaccine induces a DTH reaction in neutropenic mice and improves their survival during subsequent hematogenously disseminated candidiasis. (A) Footpad swelling was assessed 24 h after injection of 50 μg of rAls1p-N into the footpad in BALB/c mice (n = 10 for control, n = 8 for rAls1p-N). *, P = 0.006 versus control by Wilcoxon rank sum test. (B) Survival of neutropenic BALB/c mice (n = 16 per group from two experiments) infected with 2.5 × 104 blastospores of C. albicans. *, P = 0.007 versus adjuvant control by log rank test.
To determine the efficacy of rAls1p-N vaccination in mucosal infection, the vaccine was tested in our murine oropharyngeal candidiasis model (7, 8). Vaccinated or control mice were treated with cortisone acetate (225 mg/kg s.c. on days −1, 1, and 3 relative to infection) and infected sublingually as described previously (7, 8). In brief, mice were anesthetized by intraperitoneal injection with 8 mg xylazine and 110 mg ketamine per kg. Calcium alginate urethral swabs were saturated with C. albicans by placing them in a suspension of 106 organisms per ml in Hanks balanced salt solution at 30°C. The saturated swabs were placed sublingually in the oral cavity of the mice for 75 min. Tongues were excised on day 5 postinfection, fixed in zinc-buffered formalin, mounted in paraffin, and sectioned and stained with periodic acid Schiff.
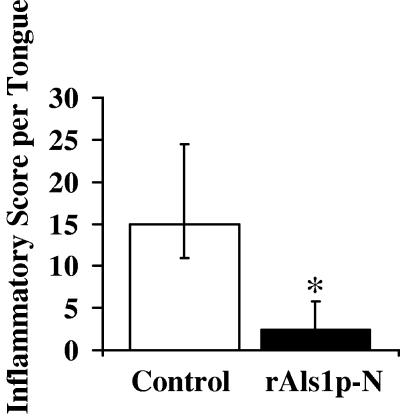
Because CFU of homogenized tongues cannot distinguish between invasive infection and surface-adherent colonization, we evaluated extent of invasion by histopathology. A blinded observer (B.J.S.) scored each section by scanning along the entire length of the tongues and quantifying the severity of fungal lesions per ×40 high-powered field (0 = no lesion, 1+ = mild mucosal inflammation, 2+ = significant inflammation restricted to the epithelium, 3+ = inflammation extending through the entire epithelial layer, and 4+ = inflammation extending into the subepithelium). To avoid sampling bias, two sections of each tongue, separated by at least five intervening tissue sections, were scored. All control mice developed marked fungal invasion of their tongues in numerous locations, while only two vaccinated mice developed any tongue lesions. In total, the median number (75th, 25th quartile) of lesions per tongue in control mice was 6.5 (8, 5.75) as compared to 1 (2.5, 0) for vaccinated mice (P = 0.03 by Wilcoxon rank sum test). Semiquantitative evaluation of the severity of infection demonstrated a significant reduction in vaccinated mice compared to that in controls (Fig. 4, P = 0.03 by Wilcoxon rank sum test). These data provide proof of principle of the potential for the rAls1p-N vaccine to provide mucosal protection as well as systemic protection.
FIG. 4.
The rAls1p-N vaccine diminishes the severity of histopathological fungal lesions on the tongues of mice with oropharyngeal candidiasis. n = 4 mice per group. Inflammatory score was generated by a blinded observer as described in the text. *, P = 0.03 by Wilcoxon rank sum test.
In light of the increasing incidence of candidemia and its continuing high mortality rate, development of a vaccine against Candida spp. is of great importance. Here we show that s.c. vaccination with rAls1p-N resulted in marked improvement in survival and significant reductions in fungal burden during otherwise rapidly fatal hematogenously disseminated candidiasis in both immunocompetent and immunocompromised mice. Of interest are the kidney fungal burden results from individual vaccinated mice, demonstrating that approximately half the mice had kidney fungal burdens under 5 log CFU/g. We have previously found that the threshold of kidney fungal burden indicative of a fatal infection is 5 log CFU/g; mice with kidney fungal burdens above this level typically die from infection, whereas mice with kidney fungal burdens below this burden survive the infection (16, 18). Therefore, breakthrough deaths in the vaccinated group likely reflect high fungal burden in spite of vaccination. The mouse-to-mouse variations in tissue fungal burden may reflect the complexities of host-pathogen interactions and/or variable vaccine responsiveness.
In summary, the rAls1p-N vaccine is a promising candidate for prevention of increasingly common and highly lethal disseminated candidiasis. The vaccine is efficacious in immunocompetent mice, and efficacy is retained even in neutropenic and corticosteroid-treated hosts. The successful development of an anticandidal vaccine would greatly impact care of at-risk patients.
Acknowledgments
This work was supported by NIAID/NIH grants PO1 AI37194 and RO1 AI19990 to J.E.E. J.E.E is also supported by an unrestricted Freedom to Discover Grant for Infectious Disease from Bristol Myers Squibb. B.J.S., A.S.I., and S.G.F are supported by NIAID grants KO8 AI060641, RO3 AI054531, and RO1 DE013974 and RO1 A1054928, respectively. A.S.I. is also supported by a Burroughs Wellcome New Investigator Award in Molecular Pathogenic Mycology.
Editor: T. R. Kozel
REFERENCES
- 1.Alonso-Valle, H., O. Acha, J. D. Garcia-Palomo, C. Farinas-Alvarez, C. Fernandez-Mazarrasa, and M. C. Farinas. 2003. Candidemia in a tertiary care hospital: epidemiology and factors influencing mortality. Eur. J. Clin. Microbiol. Infect. Dis. 22:254-257. [DOI] [PubMed] [Google Scholar]
- 2.Baran, J., Jr., B. Muckatira, and R. Khatib. 2001. Candidemia before and during the fluconazole era: prevalence, type of species and approach to treatment in a tertiary care community hospital. Scand. J. Infect. Dis. 33:137-139. [DOI] [PubMed] [Google Scholar]
- 3.Fu, Y., A. S. Ibrahim, D. C. Sheppard, Y.-C. Chen, S. W. French, J. E. Cutler, S. G. Filler, and J. E. J. Edwards. 2002. Candida albicans Als1p: an adhesin that is a downstream effector of the EFG1 filamentation pathway. Mol. Microbiol. 44:61-72. [DOI] [PubMed] [Google Scholar]
- 4.Fu, Y., G. Rieg, W. A. Fonzi, P. H. Belanger, J. E. Edwards, Jr., and S. G. Filler. 1998. Expression of the Candida albicans gene ALS1 in Saccharomyces cerevisiae induces adherence to endothelial and epithelial cells. Infect. Immun. 66:1783-1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gudlaugsson, O., S. Gillespie, K. Lee, J. Vande Berg, J. Hu, S. Messer, L. Herwaldt, M. Pfaller, and D. Diekema. 2003. Attributable mortality of nosocomial candidemia, revisited. Clin. Infect. Dis. 37:1172-1177. [DOI] [PubMed] [Google Scholar]
- 6.Ibrahim, A. S., B. J. Spellberg, V. Avenissian, Y. Fu, S. G. Filler, and J. E. Edwards, Jr. 2005. Vaccination with recombinant N-terminal domain of Als1p improves survival during murine disseminated candidiasis by enhancing cell-mediated, not humoral, immunity. Infect. Immun. 73:999-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamai, Y., M. Kubota, Y. Kamai, T. Hosokawa, T. Fukuoka, and S. G. Filler. 2002. Contribution of Candida albicans ALS1 to the pathogenesis of experimental oropharyngeal candidiasis. Infect. Immun. 70:5256-5258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamai, Y., M. Kubota, Y. Kamai, T. Hosokawa, T. Fukuoka, and S. G. Filler. 2001. New model of oropharyngeal candidiasis in mice. Antimicrob. Agents Chemother. 45:3195-3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kullberg, B. J., and A. M. Oude Lashof. 2002. Epidemiology of opportunistic invasive mycoses. Eur. J. Med. Res. 7:183-191. [PubMed] [Google Scholar]
- 10.Martino, P., C. Girmenia, A. Micozzi, R. Raccah, G. Gentile, M. Venditti, and F. Mandelli. 1993. Fungemia in patients with leukemia. Am. J. Med. Sci. 306:225-232. [DOI] [PubMed] [Google Scholar]
- 11.Nucci, M., W. Pulcheri, N. Spector, A. P. Bueno, P. C. Bacha, M. J. Caiuby, A. Derossi, R. Costa, J. C. Morais, and H. P. de Oliveira. 1995. Fungal infections in neutropenic patients. A 8-year prospective study. Rev. Inst. Med. Trop. Sao. Paulo 37:397-406. [DOI] [PubMed] [Google Scholar]
- 12.Pappas, P. G., J. H. Rex, J. Lee, R. J. Hamill, R. A. Larsen, W. Powderly, C. A. Kauffman, N. Hyslop, J. E. Mangino, S. Chapman, H. W. Horowitz, J. E. Edwards, and W. E. Dismukes. 2003. A prospective observational study of candidemia: epidemiology, therapy, and influences on mortality in hospitalized adult and pediatric patients. Clin. Infect. Dis. 37:634-643. [DOI] [PubMed] [Google Scholar]
- 13.Rangel-Frausto, M. S., T. Wiblin, H. M. Blumberg, L. Saiman, J. Patterson, M. Rinaldi, M. Pfaller, J. E. Edwards, Jr., W. Jarvis, J. Dawson, and R. P. Wenzel. 1999. National Epidemiology of Mycoses Survey (NEMIS): variations in rates of bloodstream infections due to Candida species in seven surgical intensive care units and six neonatal intensive care units. Clin. Infect. Dis. 29:253-258. [DOI] [PubMed] [Google Scholar]
- 14.Schaberg, D. R., D. H. Culver, and R. P. Gaynes. 1991. Major trends in the microbial etiology of nosocomial infection. Am. J. Med. 91:72S-75S. [DOI] [PubMed] [Google Scholar]
- 15.Sheppard, D. C., G. Rieg, L. Y. Chiang, S. G. Filler, J. E. Edwards, Jr., and A. S. Ibrahim. 2004. Novel inhalational murine model of invasive pulmonary aspergillosis. Antimicrob. Agents Chemother. 48:1908-1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spellberg, B., A. S. Ibrahim, J. E. Edwards, Jr., and S. G. Filler. 2005. Mice with disseminated candidiasis die of progressive sepsis. J. Infect. Dis. 192:336-343. [DOI] [PubMed] [Google Scholar]
- 17.Spellberg, B., and J. E. Edwards, Jr. 2002. The pathophysiology and treatment of Candida sepsis. Curr. Infect. Dis. Rep. 4:387-399. [DOI] [PubMed] [Google Scholar]
- 18.Spellberg, B., D. Johnston, Q. T. Phan, J. E. Edwards, Jr., S. W. French, A. S. Ibrahim, and S. G. Filler. 2003. Parenchymal organ, and not splenic, immunity correlates with host survival during disseminated candidiasis. Infect. Immun. 71:5756-5764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wey, S. B., M. Mori, M. A. Pfaller, R. F. Woolson, and R. P. Wenzel. 1988. Hospital-acquired candidemia. The attributable mortality and excess length of stay. Arch. Intern. Med. 148:2642-2645. [DOI] [PubMed] [Google Scholar]
- 20.Wisplinghoff, H., T. Bischoff, S. M. Tallent, H. Seifert, R. P. Wenzel, and M. B. Edmond. 2004. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin. Infect. Dis. 39:309-317. [DOI] [PubMed] [Google Scholar]